#inflammatory molecules
Text
Studying middle-aged brain can give us clues to dementia, ET HealthWorld
New Delhi: Cork and Yvonne Nolan, University College Cork Cork (Ireland), Mar 20 (The Conversation) Our brains change more rapidly at various times of our lives, as though life’s clock was ticking faster than usual.
Childhood, adolescence and very old age are good examples of this. Yet for much of adulthood, the same clock seems to tick fairly regularly. One lap around the Sun; one year…

View On WordPress
#cognitive decline#cognitive functions#Cork and Yvonne Nolan#health News#immune system#inflammatory molecules#University College Cork#university college cork cork#university of mississippi#white matter connections
0 notes
Text
The unbearable itch that accompanies the chronic inflammatory skin condition eczema has a new culprit.
Scientists have discovered that a familiar bacteria, Staphylococcus aureus, ignites persistent itches by directly triggering sensory neurons in the skin, a finding that could help researchers devise new treatments.
Eczema, which is also known as atopic dermatitis, is common in children and teenagers but also affects one in ten adults.
Up until now, immune cells and the inflammatory molecules they secrete were thought to be the main drivers of the insufferable itch that occurs with eczema. That itch so often drives a vicious urge to scratch which only damages the skin further, leaving it red, raw, swollen, and cracked.
Years ago, researchers figured out that people lacking a skin protein called filaggrin were more likely to develop eczema; but what specifically caused the itch that enflames eczema still bugged them.
Continue Reading.
348 notes
·
View notes
Text
HERBS AND THEIR BENEFITS.

Ginger:
Eating ginger can cut down on fermentation, constipation and other causes of bloating and intestinal gas. Wear and tear on cells. Ginger contains antioxidants. These molecules help manage free radicals, which are compounds that can damage cells when their numbers grow too high. It is useful in minimizing menstrual cramps, and it relaxes the muscular spasms as well
Cinnamon:
high in antioxidants, which may help protect against disease, inflammation and ageing It may improve gut health, dental hygiene, reduce cholesterol levels and lower blood pressure.
Garlic:
Garlic offers an immune system boost to help prevent colds and the flu virus. One study found that allicin, an active component of freshly crushed garlic, had antiviral properties and was also effective against a broad range of bacteria
Chamomile:
commonly used for many human ailments such as hay fever, inflammation, muscle spasms, menstrual disorders, insomnia, ulcers, wounds, gastrointestinal disorders, rheumatic pain, and hemorrhoids.
Rosemary:
antimicrobial, anti-inflammatory, anti-oxidant, anti-apoptotic, anti-tumorigenic, antinociceptive, and neuroprotective properties. It could prevent hair follicles from being starved of blood supply, dying off, and leading to hair loss.
Tumeric :
Turmeric has been used in both Ayurvedic and Chinese medicine as an anti-inflammatory, to treat digestive and liver problems, skin diseases, and wounds.
146 notes
·
View notes
Text
Debunking Wellness Trends: Seed Oils
One aspect of the growing wellness trends on social media is the idea that seed oils are poisoning the population and need to be avoided to reach better health/heal health conditions/conserve fertility/etc. They’re being called “the hateful eight”, and there’s a lot of people doing the #seedoilfree lifestyle. Seed oils are being blamed for headaches, low immunity, disrupted attention and thinking, diabetes, and more.
(Seed oils include canola, corn, cottonseed, grapeseed, rice bran, safflower, soy and sunflower oil)
Toxicity Claims
Current scientific evidence does NOT support claims that seed oils are “toxic”.
Now, if you begin to cut out foods such as fried foods (like fries) or packaged snacks, you may feel better. A lot of people are attributing this feeling to removing seed oils, but these foods are usually high in refined carbohydrates, sodium and sugar which is why they’re associated with more negative health outcomes.
Another fear is that the “toxicity” comes from production byproducts. Heat and solvents like hexane are used to extract oil from seeds, which apparently introduces chemical additives and unstable molecules, which then can turn polyunsaturated fats into harmful trans fats. Realistically, hexane is a bigger threat to the environment and workers in case of inhalation – trace amounts in the oil are still being studied, but so far there’s no concerning data. They’re also heated for short periods, and actually have fewer trans fats than products like milk or butter.
Omega-6
Additionally, omega-6 (found in nuts and seeds, and a dominant polyunsaturated fat in seed oils) is also not “toxic”. In fact, it’s been scientifically linked to lower cholesterol, lower blood sugar and reduced heart disease risk. The argument against omega-6 is that it’s responsible for chronic inflammation – omega-6 linoleic acid is converted into arachidonic acid in the body, which is a component of inflammatory compounds. Only 0.2% of linoleic acid we eat turns into arachidonic acid, and not all the compounds cause inflammation – arachidonic acid is a complex molecule, and it also has some anti-inflammatory effects. Linoleic acid is also an essential fatty acid that our body can’t make itself, and we use it to produce cell membranes and for skin health.
Another claim is that our omega-3: omega-6 ratio is out of balance, and that this is because our ancestors ate a much more balanced ratio than we do today. We DO eat more omega-6 fats than omega-3, but the claim that we eat 20 to 50x more is misinformation – it’s closer to 10:1. Instead of cutting omega-6, the better solution is to try and introduce more omega-3 fats into your diet.
Realistically, a lot of the online discourse about seed oils is misunderstanding scientific reports + deliberate fear-mongering. If you do have concerns about something in your diet causing health issues, seek advice from a trained medical professional who can give you evidence-based ideas and solutions to help you!
(Some articles to start if you want to know more on this topic 1 2 3)
#ive been promising to say something about this forever lmao i finally got to it#wellness trends#<- my tag for this stuff#i honestly feel bad for people who i see getting anxious about these kinds of things!!! :((#katie rambles
126 notes
·
View notes
Text
So ME/CFS (myalgic encephalomyelitis/Chronic Fatigue Syndrome) and fibromyalgia are two syndromes (collections of symptoms often found together, with unknown causative mechanisms) with largely overlapping symptoms. They're currently classified as different diagnoses, but there are plenty of people who aren't convinced that they're actually different things. The biggest diagnostic difference seems to be whether the pain or the fatigue is the biggest problem.
I'm sure there are plenty of people who, like me, couldn't possibly say which of those is ruining my life more. I, like many, fulfill all the diagnostic criteria for both. I have the specific patterns of pain and inflammation characteristic of fibro, but I also have the postural orthostatic problems (Stand Up Feel Real Bad disorder) and extreme fatigue of ME/CFS. There's no test; diagnosis is an inherently subjective thing.
This is just gonna keep being about medical problems, so have a cut.
I also have problems that may be related or may be separate or may be part of the constellation of physical issues associated with ADHD, like loose tendons that lead to terrible core strength and janky joints. So while generally the pain spots for fibromyalgia are considered to have no actual material cause, I am pretty sure that my right hip and shoulder are in fact fucked up, and fibro is just making it experientially worse. I've also got a rib that spends more than half its time in just slightly the wrong goddamn place. I have multiple friends who have hypermobility problems that make mine look like a papercut, but combining them with fibro isn't a lot of fun.
A few months back, at my bestie's prompting and with his help, I started eating keto, which is essentially just restricting carbohydrates so harshly that they represent less than 20% (or less than 10%, this seems to be bioindividual) of your diet, at which point your body begins building energy transport molecules out of fat (ketones) instead of glucose. This has a history of treating several conditions (originally, seizures, but now also diabetes and inflammatory conditions), well before it became popular for weight loss.
It was an experiment. Believe me, I have mixed feelings about the fact that it worked. At first, it worked really, really well. I went from mostly bedbound to up and working full days outside. I've started to hit diminishing returns and having to nap more often, but it's still a radical improvement. I just forget how bad it was too fast. I hate how fast we forget how far we've come.
I haven't talking about it though, because I am so conflicted about restrictive diets as a thing. This started as an experiment, and as an experiment I could sell myself on no apples no potatoes no rice no crackers no no no no etc for a few weeks. After a few weeks I could decide whether it was worth it. And now here we are and it works.
But I've gone through So Much food restriction, starting when Phantom was two and we discovered that gluten fucks us both up. Then the Boy was sensitive to so many things as a baby that I cut out the entire Top Eight allergens (let's see, can I remember? Milk, eggs, peanuts, gluten, corn, soy, uhh....others...) for a year while he was nursing. Once you've cut wheat AND eggs AND corn out there is almost no commercial product you can eat and you have to prepare everything from scratch. With a toddler and a baby. I was literally starving. I used a calorie tracker for a while and found that I was nearly a thousand calories short per day, on average. I could barely think.
It's become a huge depression trigger for me. I tell people that my last major depressive episode was triggered by not being able to eat dairy, and I'm not kidding. I'm struggling with it now, too. Most of the time I'm good, but still, despite medication, I get very low and I just want to be able to fucking eat something tasty and comforting and EASY. I just want...cheese and crackers. A whole piece of fruit. A baked potato. Rice with my stir fry. But then I eat too much fucking watermelon and I can tell the difference in my wellbeing the next day.
Food becomes a minefield. Every meal becomes a struggle. You question every bite, every symptom. At least once a day the whole thing is just too annoying and I decide to just not eat, because fuck it. I dunno if it reaches eating disorder levels, but it's certainly maladaptive. I hate that I've gotten here because what you eat actually DOES matter. it's like the question of how you talk yourself out of anxiety when the world is objectively falling apart.
But I can do the things I love. I owe all this garden progress to not having had a glass of juice or a bowl of pasta in four months. Not to mention the abrupt cessation of all my dermatitis problems, frequent "silent" heartburn, a ton of digestive problems, migraines, most headaches, and more. "Nothing is worth risking depression" but is it though?
I'm holding on to the hope that these changes will allow me to heal. That I'll be able to make long-term progress, as many people say they have, and reintroduce restricted foods gradually. That I'll be able to cement the opportunity diet gave me with regular movement and conditioning and slowly claw my way up the spiral.
But on days when I feel like shit anyway, and I can't have some fucking chips about it....yeah. It's not great.
21 notes
·
View notes
Text
With cold and flu season fast approaching, I want to post herbal recipes I am finding. These are not mine, and not medical advice!!!
Plant Origins of Thieves Oil
Clove: clove buds originate from the evergreen tree Syzygium aromaticum or Eugenia caryophyllata. These flower buds contain up to 20 percent essential oil, and are incredibly pungent, thanks to the major active chemical component called eugenol.
Rosemary: rosemary is a popular herb that comes from a small evergreen plant that belong to the mint family. It is native to the Mediterranean region, and possesses strong anti-inflammatory properties .
Eucalyptus: eucalyptus trees are native to Australia, Tasmania, and nearby islands. They’re the popular plant exclusively enjoyed by koala bears, and come in many different species. The oil is derived from the leaf of the eucalyptus tree, and is commonly used in cold remedies.
Cinnamon: cinnamon oil and the dried spice cinnamon both come from the bark of the true cinnamon tree (Cinnamomum zeylanicum). Essential oils that come from the leaf, bark and root of the cinnamon tree are much different, but the most common used version in Thieves oil is the cinnamon leaf. The active component in cinnamon bark essential oil is cinnamaldehyde.
Lemon: lemons come from a small tree in the Rutacea family. Lemon essential oil is derived by cold-pressing the peel of the lemon fruit, which is rich in different phytonutrients and beneficial compounds.
Thieves Oil Recipe
As long as you have all of the necessary essential oils on hand, you can easily make your own version of Thieves oil at home.
Ingredients: Master Blend
80 drops of clove essential oil
70 drops of lemon essential oil
40 drops of cinnamon essential oil
30 drops of eucalyptus essential oil
20 drops of rosemary essential oil
Method:
Combine all of the above essential oils in a dark amber coloured 15 milliliter (0.5 fluid ounce) glass bottle. Make sure you store it a cool, dry place, away from heat and light.
Benefits and Uses of Thieves Oil
This thieves oil recipe can be used to address certain health ailments, check out the benefits and uses below! Not medical advice
1. Relief from Aches and Pains
This Thieves oil recipe is loaded with plenty of anti-inflammatories to ease muscular and joint aches and pains. Rosemary and eucalyptus oil have actually been found to relieve rheumatoid arthritis, as well as muscle and joint aches and pains. You can dilute Thieves oil in a carrier oil (like jojoba oil, almond oil or grapeseed oil) to be used topically on the ache or pain. Typically the ratio is 1 drop essential oil to 4 drops carrier oil.
2. Immune System Support
Thieves oil was used to protect the “thieves” from the Black Plague, so you can be rest-assured that this oil provides some hefty immune support. Clove and rosemary essential oils are powerful antibacterials and anti-fungals. They’ve both been shown to have significant anti-microbial effects against dangerous bacteria like Staphylococcus epidermidis, Escherichia coli, and Candida albicans.
Massage the blend on your feet, lower back, neck and behind your ears for daily immune support. You can also diffuse Thieves oil to allow the essential oil molecules to enter your blood stream after they’ve entered your lungs! To get Thieves oil into your lungs is to diffuse the oil in a diffuser. Diffuse 15-20 drops of Thieves oil for 15 minutes, 3-4 times a day.
By live life fruit.
#witchcraft#witchy vibes#witch aesthetic#witchy#witchblr#witchythings#witches#witch#spells#witchcore#spellcraft#spellwork#spellcasting#witch tips#witchy herbs
70 notes
·
View notes
Text
A healthy immune system defends the body against disease and infection. However, for one in 10 people, mostly women, the immune system malfunctions and attacks its own cells. This causes more than 80 types of autoimmune diseases, such as lupus, multiple sclerosis, and rheumatoid arthritis. The reason women may be more affected, according to a couple of recent studies, may be linked to a faulty mechanism that is supposed to shut down one of a woman’s two X-chromosomes.
One study from Stanford University shows that a molecule called Xist (pronounced ‘exist’), which turns off one copy of the X-chromosome in every cell in the female body, can trigger a rogue immune response. Another study from France, not yet peer-reviewed, shows that when certain genes on the silenced X-chromosome become active again, it can cause lupus-like symptoms in older mice.
Since most autoimmune diseases are diagnosed after puberty, more in girls than in boys, sex hormones were thought to be the primary driver of this difference. For example, four in five patients with autoimmune diseases are women. Ten times more women than men get lupus. And 20 times more women develop Sjögren's syndrome, an illness that mainly causes dry eyes and dry mouth.
“Our study shows that you do not need female sex hormones; you don't even need a second X-chromosome; just this Xist [molecule] could have a major role in developing some autoimmune diseases,” says Howard Chang, a dermatologist and molecular geneticist at Stanford University School of Medicine in California, who led the study.
“There is clear evidence now that the sex bias in autoimmune disease is not only linked to hormones but also to the presence of the number of X chromosomes and to the process of X chromosome inactivation,” says Claire Rougeulle, an epigeneticist who led the second study at the National Centre for Scientific Research (CNRS) in the Université Paris Cité in France.
That so many antibodies exist that target/destroy the molecules required to silence or shut-off the X-chromosome, “was not known at all,” says Jean-Charles Guéry, an immunologist at the Toulouse Institute for Infectious and Inflammatory Diseases (Infinity) in France.
Paradoxically, the increased risk of autoimmune disease in women may even be an evolutionary adaptation to protect the lives of their children. “Women have a better immune system to fight things,” says Johann Gudjonsson, a dermatologist at the University of Michigan, Ann Arbor.
Women tend to produce more antibodies than men, which protects both them and their babies through breastmilk, says Vanessa Kronzer, a Rheumatologist at the Mayo Clinic in Rochester, Minnesota.
Hormones are also involved. Female estrogen hormones boost immunity while male hormones not only suppress immunity but also protect against autoimmunity. These differences in sex hormones were thought to explain why women have more robust immunity, making them also more vulnerable to developing autoimmune diseases than men. But that may not be the only reason.
SILENCING ONE X CHROMOSOME
Each cell in a woman’s body has two X-chromosomes, one from the mother and one from the father. Men have an X-chromosome from their mother and a much smaller Y-chromosome from their father.
The Y-chromosome contains just about a hundred genes, but the X-chromosome contains more than 900.
To make sure the activity of genes located on the X-chromosome is equal in both men and women, one of the two X-chromosomes in every female cell randomly shuts down. This happens early in fetal development when the Xist molecule and its partner proteins coil around one of the X-chromosomes and switch it off. If both X-chromosomes remain equally active, the cell will die.
As a result, the female body contains a mosaic of cells in which either the mother’s or the father’s X-chromosome is silenced. This X-chromosome inactivation is the reason female Calico cats develop a patchwork of orange and brown fur. While some of their hairs express a black color from one active X-chromosome, others develop an orange color from the other.
However, X-chromosome inactivation is far from perfect, and 15 to 23 percent of genes remain active. One such gene that continues to function, when it should not, has been linked to lupus. More evidence comes from boys and men who are born with an extra X chromosome who also have an increased risk of developing autoimmune diseases, suggesting the critical role of the X chromosome.
XIST TRIGGERS AUTOANTIBODIES
Chang has been studying the Xist molecule for many years and in 2015 he discovered that many proteins working together with Xist were involved in autoimmune disorders and were attacked by rogue antibodies, called autoantibodies. Instead of fighting foreign invaders, such as germs, autoantibodies mistakenly target an individual’s own cells.
To test whether faulty X-chromosome inactivation was the reason more women suffer from autoimmune diseases than men, Chang’s team engineered male mice that produce the Xist molecule, which is usually only present in female cells.
However, Xist molecule alone did not cause the autoimmune disease in the engineered male mice.
Only when researchers injected an irritant into these genetically modified male mice did the levels of autoantibody rise and trigger a lupus-like disease. With the addition of the irritant, the autoantibody levels in Xist-producing males matched those in females and were higher than in normal males without Xist. These engineered mice also showed more extensive tissue damage and signs of heightened inflammation when exposed to the irritant.
That suggests that even with Xist, either a genetic susceptibility or an environmental trigger is needed to cause the female-biased autoimmune disease. The study hints that only when cells get damaged, either by an environmental trigger or due to genetic susceptibility, Xist molecules and its protein partners leak outside of the cell and cause the immune system to produce autoantibodies against the Xist-protein complex, which then initiates an autoimmune disease.
“So that's one major reason why, of course, most women do not get autoimmune disease,” says Chang. “Even though every woman is expressing Xist throughout their body.”
X-CHROMOSOME TIES TO LUPUS
Rougeulle collaborated with Céline Morey, a fellow epigeneticist in Paris, to understand what happens when the X-chromosome is not completely turned off.
They engineered female mice to display imperfect X-chromosome inactivation—in which most, but not all, the genes on the second X-chromosome were shut off. The researchers resorted to incomplete inactivation because blocking all Xist activity would keep both X-chromosomes fully functional and kill the mice. While French scientists weren’t expecting their mice to develop an autoimmune disease, they were surprised when engineered female mice showed symptoms of a lupus-like condition.
“You don't see the symptoms of autoimmune disease in these mice right away, but you begin to see it as they get older,” says Morey.
This supports Guéry’s 2018 study that showed that when a gene that promotes inflammation escapes inactivation in immune cells, it increases risk of developing lupus.
The common theme between the Stanford and French study is that both link the X-chromosome, and the process of X-chromosome inactivation, to autoimmunity, says Rougeulle.
Mechanisms linked with X-chromosome inactivation do seem to explain the sex differences in some autoimmune diseases such as lupus and Sjögren's, says Guéry. “[But] you cannot have a single mechanism for all autoimmune diseases.”
PREDICTING WHO MIGHT DEVELOP AN AUTOIMMUNE DISEASE
The Stanford study discovered that autoantibodies against many proteins associated with Xist are found in the blood of patients suffering from auto-immune diseases, such as lupus, scleroderma, or dermatomyositis.
While some autoantibodies were specific to certain autoimmune diseases, others were common among several. So, it might be possible to develop a panel of autoantibodies that could be used to distinguish between different disorders.
Rougeulle warns, however, that the current studies do not show whether the autoantibody levels rise significantly preceding the diseases, so more studies are needed before a diagnostic tool can be developed.
20 notes
·
View notes
Text
The Cause of Depression Is Probably Not What You Think (Joanna Thompson, Quanta Magazine, Jan 26 2023)
"A literature review that appeared in Molecular Psychiatry in July was the latest and perhaps loudest death knell for the serotonin hypothesis, at least in its simplest form.
An international team of scientists led by Joanna Moncrieff of University College London screened 361 papers from six areas of research and carefully evaluated 17 of them.
They found no convincing evidence that lower levels of serotonin caused or were even associated with depression.
People with depression didn’t reliably seem to have less serotonin activity than people without the disorder.
Experiments in which researchers artificially lowered the serotonin levels of volunteers didn’t consistently cause depression. (…)
Although serotonin levels don’t seem to be the primary driver of depression, SSRIs show a modest improvement over placebos in clinical trials.
But the mechanism behind that improvement remains elusive.
“Just because aspirin relieves a headache, [it] doesn’t mean that aspirin deficits in the body are causing headaches,” said John Krystal, a neuropharmacologist and chair of the psychiatry department at Yale University.
“Fully understanding how SSRIs produce clinical change is still a work in progress.”
Speculation about the source of that benefit has spawned alternative theories about the origins of depression. (…)
Repple warns, however, that another explanation for the effects his team observed is also possible: Perhaps the depressed patients’ brain connections were impaired by inflammation.
Chronic inflammation impedes the body’s ability to heal, and in neural tissue it can gradually degrade synaptic connections.
The loss of such connections is thought to contribute to mood disorders.
Good evidence supports this theory.
When psychiatrists have evaluated populations of patients who have chronic inflammatory diseases like lupus and rheumatoid arthritis, they’ve found that “all of them have higher-than-average rates of depression,” said Charles Nemeroff, a neuropsychiatrist at the University of Texas, Austin.
Of course, knowing that they have an incurable, degenerative condition may contribute to a patient’s depressed feelings, but the researchers suspect that the inflammation itself is also a factor.
Medical researchers have found that inducing inflammation in certain patients can trigger depression.
Interferon alpha, which is sometimes used to treat chronic hepatitis C and other conditions, causes a major inflammatory response throughout the body by flooding the immune system with proteins known as cytokines — molecules that facilitate reactions ranging from mild swelling to septic shock.
The sudden influx of inflammatory cytokines leads to appetite loss, fatigue and a slowdown in mental and physical activity — all symptoms of major depression.
Patients taking interferon often report feeling suddenly, sometimes severely, depressed.
If overlooked chronic inflammation is causing many people’s depression, researchers still need to determine the source of that inflammation.
Autoimmune disorders, bacterial infections, high stress and certain viruses, including the virus that causes Covid-19, can all induce persistent inflammatory responses.
Viral inflammation can extend directly to tissues in the brain. Devising an effective anti-inflammatory treatment for depression may depend on knowing which of these causes is at work.
It’s also unclear whether simply treating inflammation could be enough to alleviate depression.
Clinicians are still trying to parse whether depression causes inflammation or inflammation leads to depression. “It’s a sort of chicken-and-egg phenomenon,” Nemeroff said.
Increasingly, some scientists are pushing to reframe “depression” as an umbrella term for a suite of related conditions, much as oncologists now think of “cancer” as referring to a legion of distinct but similar malignancies.
"And just as each cancer needs to be prevented or treated in ways relevant to its origin, treatments for depression may need to be tailored to the individual."
82 notes
·
View notes
Text
Abstract
Early stages of deadly respiratory diseases including COVID-19 are challenging to elucidate in humans. Here, we define cellular tropism and transcriptomic effects of SARS-CoV-2 virus by productively infecting healthy human lung tissue and using scRNA-seq to reconstruct the transcriptional program in “infection pseudotime” for individual lung cell types. SARS-CoV-2 predominantly infected activated interstitial macrophages (IMs), which can accumulate thousands of viral RNA molecules, taking over 60% of the cell transcriptome and forming dense viral RNA bodies while inducing host profibrotic (TGFB1, SPP1) and inflammatory (early interferon response, CCL2/7/8/13, CXCL10, and IL6/10) programs and destroying host cell architecture. Infected alveolar macrophages (AMs) showed none of these extreme responses. Spike-dependent viral entry into AMs used ACE2 and Sialoadhesin/CD169, whereas IM entry used DC-SIGN/CD209. These results identify activated IMs as a prominent site of viral takeover, the focus of inflammation and fibrosis, and suggest targeting CD209 to prevent early pathology in COVID-19 pneumonia. This approach can be generalized to any human lung infection and to evaluate therapeutics
Comment from Dr. Harry Spoelstra on twitter:
"Macrophages, white blood cells that normally kill microorganisms, like viruses, but SARS-CoV-2 predominantly INFECTS these activated interstitial macrophages (IMs) and takes control.....
➡️ I remember some specialists telling us Sars2 doesn't infect WBC's 😬"
#mask up#covid#covid 19#covid isn't over#pandemic#covid conscious#long covid#covid is airborne#wear a mask#coronavirus
14 notes
·
View notes
Text
The T Cell Landscape
T cells, a critical component of the adaptive immune system, stand as the body's elite force in combatting infections and diseases. These specialized lymphocytes boast remarkable diversity, each type playing a distinct role in orchestrating a targeted and effective immune response.
T cells, like all blood cells, originate from hematopoietic stem cells residing in the bone marrow. However, their training ground lies within the thymus, a specialized organ located in the chest. Here, they undergo a rigorous selection process known as thymocyte education. During this process, immature T cells, called thymocytes, are presented with self-antigens (molecules unique to the body) by special cells. Thymocytes that bind too strongly to these self-antigens are eliminated, preventing them from attacking healthy tissues later. Only thymocytes that demonstrate the ability to recognize foreign invaders while exhibiting tolerance to self are released into the bloodstream as mature T cells.
Following this rigorous training, mature T cells exit the thymus and embark on their patrol, circulating throughout the bloodstream and lymphatic system. They remain vigilant, constantly scanning for their specific targets – antigens. Antigens are foreign molecules, such as fragments of viruses, bacteria, or even cancerous cells, that trigger the immune response.
The hallmark of a T cell is its T cell receptor (TCR), a highly specialized protein complex embedded on its surface. This receptor acts like a lock, uniquely shaped to fit a specific antigen, the "key." Each T cell develops a unique TCR capable of recognizing only a single antigen, enabling a highly specific immune response.
But how do T cells encounter these hidden antigens lurking within infected or cancerous cells? This critical role is played by antigen-presenting cells (APCs). APCs, such as macrophages and dendritic cells, engulf pathogens or abnormal cells, break them down into smaller fragments (peptides), and present them on their surface complexed with major histocompatibility complex (MHC) molecules. MHC molecules act as identification tags, allowing T cells to distinguish between "self" and "non-self." When a T cell's TCR encounters its specific antigen bound to an MHC molecule on an APC, a dance of activation begins. The T cell becomes stimulated, and a cascade of signaling events is triggered. This leads to the T cell's proliferation, producing an army of clones specifically tailored to combat the recognized threat.
T cells are not a single, monolithic entity. They comprise a diverse population, each type with a specialized function:
Helper T Cells (Th Cells):
Helper T cells, often abbreviated as Th cells, play a central role in coordinating immune responses. They express the CD4 surface marker and can recognize antigens presented by major histocompatibility complex class II (MHC-II) molecules. Subtypes of helper T cells include Th1, Th2, Th17, and regulatory T cells (Tregs), each with distinct functions and cytokine profiles.
Th1 cells mediate cellular immunity by activating macrophages and cytotoxic T cells, crucial for defense against intracellular pathogens.
Th2 cells are involved in humoral immunity, promoting B cell activation and antibody production, thus aiding in defense against extracellular parasites.
Th17 cells contribute to the immune response against extracellular bacteria and fungi, producing pro-inflammatory cytokines. Regulatory T cells (Tregs) maintain immune tolerance and prevent autoimmunity by suppressing excessive immune responses.
Cytotoxic T Cells (Tc Cells):
Cytotoxic T cells, also known as Tc cells or CD8+ T cells, are effector cells responsible for directly killing infected or aberrant cells. They recognize antigens presented by MHC class I molecules on the surface of target cells. Upon activation, cytotoxic T cells release perforin and granzymes, inducing apoptosis in target cells and eliminating the threat.
Memory T Cells:
Memory T cells are a long-lived subset of T cells that persist after the clearance of an infection. They provide rapid and enhanced immune responses upon re-exposure to the same antigen, conferring immunological memory. Memory T cells can be either central memory T cells (TCM), residing in lymphoid organs, or effector memory T cells (TEM), circulating in peripheral tissues.
γδ T Cells:
Unlike conventional αβ T cells, γδ T cells express a distinct T cell receptor (TCR) composed of γ and δ chains. They recognize non-peptide antigens, such as lipids and metabolites, and are involved in immune surveillance at epithelial barriers and responses to stress signals.
Beyond the Battlefield: The Expanding Roles of T Cells: The remarkable capabilities of T cells have opened doors for several groundbreaking applications in medicine:
Vaccines: By presenting weakened or inactivated forms of pathogens, vaccines "train" the immune system to generate memory T cells. This prepares the body to recognize and rapidly eliminate the real pathogen upon future exposure, preventing disease.
Cancer immunotherapy: CAR T-cell therapy, a revolutionary approach, genetically engineers a patient's own T cells to express chimeric antigen receptors (CARs) that recognize and target specific cancer cells. These "supercharged" T cells are then reintroduced into the patient, unleashing a potent attack against the tumor.
Autoimmune disease treatment: Researchers are exploring ways to manipulate T cells to suppress harmful immune responses that underlie autoimmune diseases like rheumatoid arthritis and multiple sclerosis.
The diverse array of T cells underscores the immune system's complexity and adaptability in mounting tailored responses against a myriad of threats. From orchestrating immune reactions to maintaining tolerance and establishing long-term immunity, T cells play multifaceted roles in safeguarding the body's health. Understanding the intricacies of T cell biology not only sheds light on immune-mediated diseases but also paves the way for developing novel therapeutic strategies harnessing the power of the immune system.
T cells represent a fascinating aspect of immunology, with their diversity and specificity driving the complexity of immune responses. As research advances, further insights into T cell biology promise to revolutionize immunotherapy and enhance our ability to combat diseases ranging from infections to cancer. By understanding and harnessing their power, we can unlock new avenues for protecting and improving human health.
#science sculpt#life science#science#molecular biology#biology#biotechnology#artists on tumblr#t cells#T helper cells#autoimmune#autoimmunity#helathcare#immunology#immunotherapy#medical care#cancer#human health#research#scientific research#the glass scientists#scientific illustration#research scientist
11 notes
·
View notes
Text
Plant chemicals are so cool! Unit 9
The most amazing thing I know about nature is the ability of plants to produce compounds that serve incredible health benefits to humans. I think it is other-worldly that the flora that has existed alongside humans for so many years can provide us with so many cures to various ailments. Getting personal, I have a very unfortunate family history containing cancer, diabetes, and immune deficiencies that has taken a lot from me. These devastating occurrences have made me all-too-aware of the impacts that lifestyle and food have on human health, and in many ways being in science does not ease my anxieties. However; learning about plant secondary metabolites that serve as phytonutrients in the human body has made me hopeful and inspired to learn more, not just for interest, but to serve my health as well. Buckle up for many science terms and lots of plant facts that I have stored in my brain through my academic career!
Throughout my summary on plant phytonutrients (plant compounds that serve proven health benefits in humans), I will strive to present this information as a whole by connecting plants to human health to satisfy some of Tilden's Principle's of Interpretation (Beck et al. 2018, p. 84). Did you know that the colour of the fruits and vegetables you eat actually correlate to their nutrition? The different pigments produced in plants, such as your orange carrots and red peppers, are caused by secondary metabolites. Orange colouring is caused by the production of beta-carotene, this is then utilized by our body to make vitamin A, making it crucial to our health because we cannot synthesize this on our own. Colours such as purple and dark reds are caused by anthocyanins, these are compounds that aid in our bodies ability to fight tumour producing cells. Actually many plant metabolites, such as glucosinolates from Broccoli, aid in tumour-suppression and have anti-inflammatory properties. Spices such as turmeric have been used for centuries as a treatment for inflammation and diabetes due to the compound 'curcumin'. This bioactive molecule has been increasingly applied to modern medical studies due to its efficacy in improving glucose regulation and suppressing various cancer cell formations.
I won't add in too much more, as I know that was a lot of information. One more area I do want to touch on is the use of genetic engineering to increase yields/improve taste, but decreasing health benefits in the process. An example of this is removing the class of compounds "cucurbitacins" from common cucumbers due to the bitter taste it gives them. These compounds provide various health benefits such as anti-inflammatory and anti-cancer effects, and through the removal of these it has made cucumbers far less beneficial to our health.
I believe much of what our bodies need is provided by nature, not to say I disprove of modern medicine in any way, but our values in food as a society has been greatly impacted due to prices/availability. I want to work plants to improve nutritional concentrations of food, and helping humans be healthier through what has already been granted to us by nature.
Thanks for reading!
Alleeya
Beck, L., Cable, T. T., & Knudson, D. M. (2018). Interpreting Cultural and Natural Heritage: For A Better World. Sagamore Publishing.
7 notes
·
View notes
Text
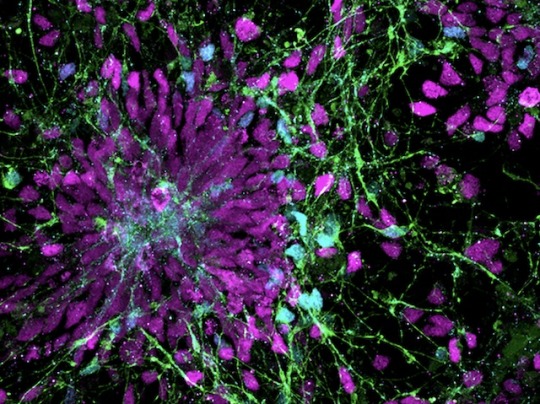
Culture of Disorder
Human neural progenitor cells generated from induced pluripotent stem cells – cells from reprogrammed mature cells – for modelling effects of pro-inflammatory molecule IL-6 released in maternal immune activation, a potential contributor to neurodevelopmental disorders in the offspring
Read the published research paper here
Image from work by Kseniia Sarieva and colleagues
Hertie Institute for Clinical Brain Research, University of Tübingen, Tübingen, Germany
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in and cover image of Disease Models & Mechanisms, November 2023
You can also follow BPoD on Instagram, Twitter and Facebook
10 notes
·
View notes
Text

Boost Your Fitness and Performance with the Right Supplements
In the pursuit of improved fitness and performance, many athletes and fitness enthusiasts turn to supplements to give them an edge. While a balanced diet should always be the foundation, certain supplements can complement your training regimen and help you reach your goals faster. Let’s explore some of the most effective supplements for enhancing fitness and performance.
1. Protein Powders
Protein is essential for muscle repair and growth, making it a cornerstone of any fitness program. Protein powders, such as whey, casein, and plant-based options like pea or hemp protein, offer a convenient way to increase your protein intake. They can be consumed as shakes or added to smoothies, providing a quick and easy source of high-quality protein.
2. Creatine
Creatine is one of the most researched supplements for improving strength and power. It works by increasing the body’s stores of phosphocreatine, which helps regenerate adenosine triphosphate (ATP), the primary energy currency of cells. This can lead to improved performance during high-intensity activities like weightlifting and sprinting.
3. Branched-Chain Amino Acids (BCAAs)
BCAAs, including leucine, isoleucine, and valine, are essential amino acids that play a crucial role in muscle protein synthesis. Supplementing with BCAAs can help reduce muscle breakdown during exercise, enhance recovery, and promote muscle growth.
4. Beta-Alanine
Beta-alanine is a non-essential amino acid that combines with histidine to form carnosine, a compound that helps buffer acid in muscles during high-intensity exercise. By increasing muscle carnosine levels, beta-alanine supplementation may delay fatigue and improve endurance during activities like sprinting and interval training.
5. Caffeine
Caffeine is a well-known stimulant that can enhance performance in various ways. It increases alertness, reduces perceived exertion, and can improve endurance by stimulating the release of adrenaline and mobilizing fatty acids for energy. Caffeine can be consumed in supplement form or obtained from sources like coffee and tea.
6. Omega-3 Fatty Acids
Omega-3 fatty acids, found in fish oil supplements, have anti-inflammatory properties that can benefit athletes by reducing exercise-induced inflammation and promoting faster recovery. Additionally, omega-3s support cardiovascular health, which is crucial for overall fitness and performance.
7. Vitamin D
Vitamin D plays a vital role in bone health, muscle function, and immune function, making it important for athletes and active individuals. Many people have suboptimal levels of vitamin D, especially those who live in northern latitudes or spend limited time outdoors. Supplementing with vitamin D can help ensure adequate levels for optimal performance and overall health.
8. Electrolytes
Electrolytes such as sodium, potassium, and magnesium are essential for hydration, muscle function, and nerve signaling. During intense exercise, especially in hot conditions, electrolyte losses through sweat can impair performance and increase the risk of cramping. Electrolyte supplements or sports drinks can help replenish these crucial minerals and maintain electrolyte balance.
9. Nitric Oxide Boosters
Nitric oxide (NO) is a molecule that dilates blood vessels, increasing blood flow to muscles and improving nutrient and oxygen delivery. Supplements containing ingredients like citrulline and beetroot extract can enhance NO production, leading to better endurance and performance during workouts.
Conclusion
Supplements can be valuable tools for enhancing fitness and performance when used appropriately alongside a well-rounded diet and training program. However, it’s essential to choose high-quality supplements, stay within recommended dosages, and consult with a healthcare professional or nutritionist if you have any concerns or underlying health conditions. With the right combination of supplements and dedication to your fitness goals, you can maximize your potential and achieve the results you desire.
#fitness motivation#health#fitness#supplements#gymlife#workout#health and wellness#healthy lifestyle#wellness#gym#diet#healthcare#health tips#healthy living#weight loss#nutrition#healthy diet
4 notes
·
View notes
Text
asked by @ghost-in-a-player-piano: Which body part is the biggest problem for using the badwrong instructions that can make cancer? Is it the liver? Since the liver can regrow itself as part of everyday normal business, I bet it's up there.
extension of this thread.
oh! fantastic observation; with respect to liver cancers, this is a big area of discussion. you're right: tissue regeneration, by default, can predispose it to regenerating just a little too well. cancer emerging from hepatocytes (hepatocellular carcinoma), which make up most of the liver, is indeed one of the most common forms of adult cancer.
(note: it's up there, but not the furthest up! more on that later.)
i want to be a bit careful though: the liver's ability to regrow has the potential to influence cancer development, but that's one player among many.
we should consider what makes the liver a potential breeding ground for tumours beyond its powerful ability to regrow itself by asking why it's regrowing so much at all. existing liver tissue likely sustained some damage. this could be through a lot of means, such as excess alcohol consumption or hepatitis. damage means inflammation: tissue becomes swollen, and the affected tissue experiences something called oxidative stress.
you can think of oxidative stress as the production of very hostile molecules that carry oxygen atoms with the potential to mess up DNA. these reactive oxygen species are always present in the cells of the body, because oxygen is key to our ability to get the most energy possible out of sugar (glucose, specifically). they just exist at levels the body can handle. in cases like long-term inflammation, however, there's a fair chance they'll reach overwhelming levels.
the liver's efforts to regenerate are, ironically, an effort to resolve this inflammation—that's the organ trying to heal! however, when cells get ready to divide, they make copies of their DNA, and pass on new mistakes to their descendants. the source of the mistakes might come from the copying process itself, or it might come from our nasty reactive oxygen species hitting our DNA repeatedly until critical instructions get tampered with. following liver damage, both of these things are happening... so things might go awry.
so! chronic inflammation sounds like a big fucking deal, and it is. when it comes to body parts that are the "biggest problem for using the badwrong instructions," a noticeable pattern emerges: several are organs highly susceptible to inflammation. more common than liver cancer are lung cancer and colorectal cancer, to name two.
to showcase the phenomenon that is chronic inflammation in more concrete examples:
tobacco users are more susceptible to lung cancer; cigarette smoke irritates the lungs. that is, it induces inflammation.
asbestos is an extremely infamous cancer-causing substance. this is because asbestos, at the microscopic level, is made up of extremely small, sharp fibers. they quite literally can embed into lung cells and cause long-term inflammation. most often, it causes a form of cancer called malignant mesothelioma.
you'll never guess what inflammatory bowel disease can do. people affected tend to be prescribed anti-inflammatory medications, which both lowers the risk of colorectal cancer while reducing pain.
inflammation and growth capacity are, again, two among many things that can set a healthy cell down the path of evil, but they are extremely common culprits in the world of cancer.
thank you! i hope this was informative. hearts and love and all those nice things
#again posting separately to avoid a massive frankenpost lol#scitag#<- new tag. because i am insane.#cancer mention
13 notes
·
View notes
Text
Abstract
Therapeutic applications of synthetic mRNA were proposed more than 30 years ago, and are currently the basis of one of the vaccine platforms used at a massive scale as part of the public health strategy to get COVID-19 under control. To date, there are no published studies on the biodistribution, cellular uptake, endosomal escape, translation rates, functional half-life and inactivation kinetics of synthetic mRNA, rates and duration of vaccine-induced antigen expression in different cell types. Furthermore, despite the assumption that there is no possibility of genomic integration of therapeutic synthetic mRNA, only one recent study has examined interactions between vaccine mRNA and the genome of transfected cells, and reported that an endogenous retrotransposon, LINE-1 is unsilenced following mRNA entry to the cell, leading to reverse transcription of full length vaccine mRNA sequences, and nuclear entry. This finding should be a major safety concern, given the possibility of synthetic mRNA-driven epigenetic and genomic modifications arising. We propose that in susceptible individuals, cytosolic clearance of nucleotide modified synthetic (nms-mRNAs) is impeded. Sustained presence of nms-mRNA in the cytoplasm deregulates and activates endogenous transposable elements (TEs), causing some of the mRNA copies to be reverse transcribed. The cytosolic accumulation of the nms-mRNA and the reverse transcribed cDNA molecules activates RNA and DNA sensory pathways. Their concurrent activation initiates a synchronized innate response against non-self nucleic acids, prompting type-I interferon and pro-inflammatory cytokine production which, if unregulated, leads to autoinflammatory and autoimmune conditions, while activated TEs increase the risk of insertional mutagenesis of the reverse transcribed molecules, which can disrupt coding regions, enhance the risk of mutations in tumour suppressor genes, and lead to sustained DNA damage. Susceptible individuals would then expectedly have an increased risk of DNA damage, chronic autoinflammation, autoimmunity and cancer. In light of the current mass administration of nms-mRNA vaccines, it is essential and urgent to fully understand the intracellular cascades initiated by cellular uptake of synthetic mRNA and the consequences of these molecular events.
4 notes
·
View notes
Text
Guess what? Long Covid is real. "Long Covid has a “real biological basis”
2 notes
·
View notes