#list of open access medical journals
Text
Impact of a Model of Educational Intervention on Intestinal Parasitism in Children of Havana. 2021 Second Post- Evaluation and Intervention Study
Impact of a Model of Educational Intervention on Intestinal Parasitism in Children of Havana. 2021 Second Post-Evaluation and Intervention Study in Biomedical Journal of Scientific & Technical Research
https://biomedres.us/fulltexts/BJSTR.MS.ID.006019.php
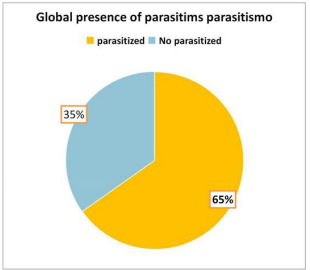
In order to determine the influence of educational work on hygienic practices and the prevalence of parasitism, an educational intervention on intestinal parasitism was carried out in schoolchildren belonging to six primary schools in the Municipality of Marianao, Havana during the first quarter of 2021. The study included 210 (5 children were chosen from each grade of the six schools), children enrolled from preschool to sixth grade, who were collected stool samples and in the anal region by the Graham method. A survey was applied to the parents to know the hygienic practices and the hygienicepidemiological conditions. The variables studied were the presence of parasitism, the type of parasite, associated symptoms and hygienic practices present. Absolute numbers and percentages were used to summarize the information and tables for its presentation. It was obtained that the prevalence of parasitism was 65.2 % and Enterobius vermicularis was the most frequent. Anal itching and irritability were the predominant symptoms for which treatment was applied. The learning needs and modifications of attitudes were identified, for which a study program was designed, after six months of the educational intervention, the second sample collection and application for the second time of the parent survey was indicated. A significant decrease in parasitism was found, as well as positive modifications in the hygienic practices of the studied population.
For more articles in Journals on Biomedical Sciences click here bjstr
Follow on Twitter : https://twitter.com/Biomedres01
Follow on Blogger :https://biomedres01.blogspot.com/
Like Our Pins On : https://www.pinterest.com/biomedres/
#medical journal in usa#American Medical Journal#list of open access medical journal#biomedical journal impact factor#journals on biomedical engineering
0 notes
Text
Biomed Grid | Relation of a Pulse Transit Time to the Blood Pressure in Bifurcated Cardiovascular Networks
Introduction
Pulse Arrival Time (PAT) is the generally established empirical marker for continuous non-intrusive blood pressure monitoring, which is defined as a time required for a pulse wave to travel from the heart to a peripheral site. A popular estimate of PAT is the timebased delay between R wave peak of Electrocardiogram (ECG) and a characteristic point of a Photoplethysmogram (PPG). PAT consists of two components: the non-constant Pre-Ejection Period (PEP), which is a duration of the ventricle contraction up to aortic valve opening, and the Pulse Transit Time (PTT), which defines the period for the arterial pulse wave to travel from the aortic valve to the peripheral site.
A simple measurement setup consisting of arm Electrocardiogram (ECG) and Peripheral Site Photoplethysmogram (PPG) allows to assess PAT as the time delay between ECG R peak and one of the optional points in the PPG waveform: peak, foot, maximum values of the slope, or the second derivative of PPG waveform. PEP can be derived noninvasively using for instance thoracic Impedance Plethysmogram (IPG) as described in [1, 2, 3]. Estimation of a systolic and diastolic BP is based on equivalence of the measured and model- based prediction of PTT. In general, prediction methods can be categorized into data-driven, physics-based and hybrid approaches. Data-driven approaches investigate relationship between BP and PTT through the linear or nonlinear regression analysis, employing a simple set of basic functions, or using artificial intelligence (neural network). Physics-based approaches assume that a reliable physical model describing connection of a PTT to BP is available. Hybrid approaches combines the methods to calibrate the personalized bio-physical properties, improving prediction.
As follows from the physical modelling, PTT and PWV are mainly affected by four factors: arterial compliance, cardiac output, peripheral resistance, and a blood pressure. Most data driven approaches select the only single parameter as an independent variable, which is a PTT or the averaged PWV, to predict systolic and diastolic blood pressures. The physics-based approach automatically accounts for the full set of factors affected BP according to the physical model, i.e. cardiac output, stroke volume, vascular compliance, peripheral resistance. The following sections describe PTT based blood pressure estimation according to the classification. Since many of the papers using data driven regression analysis are listed in several reviews, we will not cite relating individual papers, focusing mainly on a physical modeling as a foundation for linking PTT to systolic and diastolic BP.
Data-Driven BP Estimation
Multiple linear and nonlinear regressions have been explored by different authors using combinations of exponential, power, logarithm, polynomial and logistics functions to fit the experimental dataset of PTT (or PWV) vs BP [3, 4, 5]. In [6] the heart rate as a second independent variable in addition to PTT is introduced in a linear regression, which according to the authors improves the accuracy of BP prediction. In the monograph [7] the Young’s modulus is presented as an exponential function of pressure, where E0- is the Yong modulus at zero pressure, and α -empirical coefficient. As a result, the formal substitute of the modified elastic modulus E into the Moens-Korteweg expression for the PWV results in a pulse wave velocity dependent on a blood pressure, is the Moens-Korteweg speed of propagation at zero pressure, α-is a calibrating constant.
The mentioned approach is completely empirical, since it does not fit the paradigm of classical mechanics, which specifies physical nonlinearity by appropriate constitutive equations in terms of stress – strain components. The described expression cannot be derived from the fluid-structure interaction model using any constitutive equations. It could be converted to the linear regression (in a log scale) by application of logarithm to the expression for PWV, which results in
where is the distance of a pulse propagation, a, b-are determined from the best fit procedure. Equation (2) remains nowadays a one of the most widely used technique for noninvasive continuous BP monitoring. The modified logarithm-based regression was successfully applied in [8] to monitor BP as a function of PTT under the effect of hydrostatic pressure due to hand elevations. The effect of including PEP in BP estimation is under investigation in different papers based on empirical regression analysis over different cohorts of human subjects [4, 9, 10]. The simplest approach is an attempt to estimate PEP as a percentage of the RR interval, with the following subtraction from PAT to obtain PTT [11]. There is still a controversial evidence from different authors regarding effect of PEP on BP. The impact of PEP on the overall PAT decreases with distance from the heart, so that for the short PATs, like ones extracted from the ear-worn device, correction with PEP is required.
Neural Network (NN) modeling has recently been in place predicting BP as a function of a set of measured parameters. In [12] a total of 17 parameters were selected as the set of independent variables being chosen as characteristic feature points from ESG and PPG signals. Two different neural networks have been used to predict separately brachial systolic and diastolic blood pressures as functions of ECG and PPG measurements. The maximum error range in the brachial BP prediction is reported in terms of a root mean square error RMSE=±5.2mmHg. In [13] the SVR (Support Vector Machine Regression) algorithm is applied to establish relationship between human physiological data and systolic and diastolic BPs. The different number of main physiological indexes, obtained from ECG and PPG, include PTT, HR, SPO2 and others, are explored in application of NN modeling. The maximum error range of a brachial BP prediction is reported as ±10mmHg.
Few studies managed to compare different noninvasive BP estimations in a wide physiological BP range. None of data driven approaches proved to be ubiquitous, being able to monitor with a reasonable accuracy the only single feature of a BP, either systolic, or diastolic or a mean [3, 4, 5].
Physical Modeling BP Estimation
In this section, we assess physics-based models’ capabilities to predict systolic and diastolic BP as a function of model required independent parameters. Considering an arbitrary pressure-area connection, P = P(A) ,we present system of conservation laws in the following non-conservative quasi-linear form
where fluid density. This system could be transformed to the decoupled system of equations for the characteristic variables (Riemann variables), which read
Relating characteristic directions (eigenvalues) read
and forward and backward running characteristics can be found accordingly
Since the slope of a forward running characteristic line is determined by PWV =
Equation (7) serves to calculate the PTT required for the pulse wave to propagate through the Nv vessels, each of the length along the flow pathway from the left ventricle to the peripheral site.
Nonlinear Vs Linear Models
In this section three type of nonlinear models are reviewed following the papers [14, 15]: the infinitesimally Small Deformation Linear Elasticity Model (SDL), Small Deformation Hyperplastic Model (SDH) and Finite Deformation hyper elastic Model (FDH). The Fung’s exponential descriptor for passive behavior of arteries [16] presents strain energy density function for the pseudo elastic wall deformation in a form
Here are material constants, are the circumferential and axial strain components. In a 1D problem strain energy of the wall can be simplified by setting Equilibrium condition results in a generalized tube law for the hyperelastic wall the Moens-Korteweg speed at
Equations (10) and (6) present the instantaneous PWV for the SDH model in a compliant hyperelastic artery as the following
Model SDL is achieved by setting hyperelastic material coefficient to zero so that the expressions for PWV in model 2 follows from (10) at
Model FDH, which considers finite deformation, is derived based on the same expression for strain energy (8), where and is interpreted as the Green-Lagrange strain components in circumferential and axial directions accordingly. Relating Cauchy stress components.
are governed by equilibrium conditions
Here: are the stretch ratios in circumferential, radial and axial directions accordingly; r, h-are the luminal radius and thickness in a deformed state,
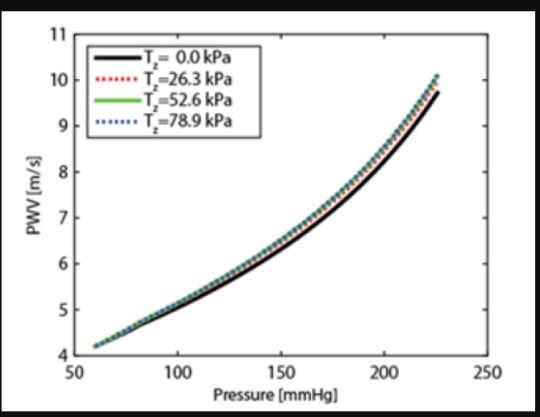
All three models have been tested against Histand and Anliker results on a PWV measurements presented in [17, 18] and reproduced in (Figure 1) by square markers. The experimental curve notably exhibits curvature starting from elevated level of pressure exceeding 140mmHg. Material parameters have been identified for each model independently, based on a best fit procedure. The Finite Deformation Hyper Elasticity (FDH) model and Small Deformation Hyper Elasticity (SDH) model have the highest quality of fitting process, creating practically the same regression line in (Figure 1) within the physiological range of BP. The Small Deformation Model with Linear Elasticity (SDL) was not able to fit the experimental curve at the quality of FDH or SDH models.
Figure 1: The nonlinear model FDH produced the best fit of the PWV vs. transmural pressure function.
Figure 2: Simulation results show that within a physiological longitudinal pre-stress load effects PWV by ~ 3%. Tz denotes the axial physiological Lagrangian stress.
Dash lines indicate theoretical prediction. Square markers illustrate the total set of experimental points. Using the properties extracted from the nonlinear model the lower (solid) line shows the effect on PWV using the partially nonlinear model SDH, combining hyper elasticity with small deformation. To illustrate the effect of a longitudinal force on PWV the variation of PWV due to the variability of a longitudinal pre-stress force is presented in (Figure 2). According to simulation within the realistic physiological range of a longitudinal stress, the relative deviation in PWV does not exceed 3%.
Several PWV estimations presented in literature is based on its correlation with the BP and an arterial wall compliance. The study in [19]examined the impact of a systolic flow correction of a measured PWV on blood pressure prediction accuracy using data from two published in vivo studies. Both studies examined the relationship between PWV and blood pressure under pharmacological manipulation, one in mongrel dogs and the other in healthy adult males. Systolic flow correction of the measured PWV improves the R2 correlation to blood pressure from 0.51 to 0.75 for the mongrel dog study, and 0.05 to 0.70 for the human subjects’ study. The results support the hypothesis that systolic flow correction is an essential element of non-invasive, cuff-less blood pressure estimation based on PWV measures.
Thick Wall Vessels
A novel mathematical model predicting PWV propagation with rigorous account of, blood vessel elasticity, and finite deformation of multi-layer thick wall arterial segments was studied in [20]. It was found that the account for the multilayer model affects distribution of local parameters in the proximity of the external layer (adventitia) and does not affect stiffness related to the internal layer. The latter means that the single thick layer model is enough to predict PWV of an arterial segment. (Figure 3) depicts the dependence of PWV on pressure for the Systole Phase (marked as “SBP”) and a Diastole Phase (marked as “DBP”) for three vessels of different thicknesses of a human aorta. All results have been compared with the simplified thin walled model of a membrane shell interacting with an incompressible fluid.
Figure 3: Simulation results show that within a physiological longitudinal pre-stress load effects PWV by ~ 3%. Tz denotes the axial physiological Lagrangian stress.
To explore inaccuracies induced by use of the less complex thin wall model, error in both PWV and blood pressure were calculated for a blood pressure of SBP/DBP = 150/95mmHg representing the median of stage 1 hypertension. The single layer thick wall model improves PWV accuracy by (4.0-8.4%) corresponding to the relative wall thickness (H/R1) range of 0.07-0.38. One of the goals for the model is PWV based blood pressure prediction, where the thick wall model offers an improvement of (3.3-19.4%).
Calibration Free Approaches
Willemet et al. [21, 22] proposed approach to use cardiovascular simulator for generation of a database of “virtual subjects” with sizes limited only by computational resources. In their study, the databases were generated using one-dimensional model of wave propagation in an artery network comprising of 55 largest human arteries. A linear elastic model was employed to describe deformation of arterial walls. The database is created by running the cardiovascular model repeatedly. The seven model parameters were varied: elastic artery PWV, muscular artery PWV, the diameter of elastic arteries, the diameter of muscular arteries, Heart Rate (HR), SV and peripheral vascular resistance. 3325 healthy virtual subjects presented a diversity of hemodynamic, structural and geometric characteristics. For each virtual subject, all characteristics are known at every point of the systemic arterial tree, i.e. anatomical and structural properties, as well as pressure, flow, pulse wave velocity and area waves at the larger arteries, therefore allowing the computation of the exact value of the diagnostic tool.
Huttunen et al. [23] used cardiovascular modelling of the entire adult circulation to create a database of “virtual subjects”, which is applied with machine learning to construct predictors for health indices. They carry out theoretical assessment of estimating aortic pulse wave velocity, diastolic and systolic blood pressure and stroke volume using pulse transit/arrival timings derived from photoplethysmography signals. The generated database was then used as training data for Gaussian process regressors applied finally to simulation. Simulated results provide theoretical assessment of accuracy for predictions of the health indices. For instance, aortic pulse wave velocity was estimated with a high accuracy (r>0.9. Similar accuracy has been reached for diastolic blood pressure, but predictions of systolic blood pressure proved to be less accurate (r > 0.75).
Conclusion
Developed technologies in general allow to implement a PTT/ PAT-based system to predict continuously cardiovascular health markers such as arterial blood pressure, cardiac output, arterial stiffness. However, none of approaches is able so far to monitor accurately all cardiac markers for the wide range of physiological conditions. The limitations to be addressed in future are the following. First, each model must be investigated for its limitations. We believe that a calibration stage is required to build a reliable simulator within the range of investigated conditions. Also, most of the research addresses healthy population, which is characterized by different behavior of a vascular system rather than group with medical conditions. In the current review we only consider pulse transit and arrival type of time information as the input to the predictor. It would be beneficial to develop approaches that do not need reference measurement for the aortic valve opening/R-peak.
Read More About this Article: https://biomedgrid.com/fulltext/volume7/relation-of-a-pulse-transit-time-to-the-blood-pressure-in-bifurcated-cardiovascular-networks.001135.php
For more about: Journals on Biomedical Science :Biomed Grid | Current Issue
#biomedgrid#american journal of biomedical science & research#list of open access medical journal#american medical journal
0 notes
Text
Researching as a Writer
Start Broad
begin with a list of more general topics and get specific as you go.
for example, research for a historical fantasy novel might follow a chain that looks like this:
life in the 1700s -> life in 1700s france -> 1700s french etiquette and lifestyle depending on class -> 1720s french fashion for middle and upper-middle class women.
starting with a general understanding of the topic you want to cover and narrowing down to specifics will make it easier to build on your knowledge as you go.
Think Critically
consider the source. if it doesn’t cite primary sources (for example, letters and photographs from a specific era and location), what sources does it cite? follow those sources if possible.
is the information reliable? is it provided by an educational institution or an expert on the subject?
who is the author? do they present any bias? what do they have to gain by promoting a specific mindset or conclusion? has any of their research been debunked?
Anecdotes
in general, anecdotal evidence is not sufficient for academic writing. luckily for you, this is a fiction writing page, and anecdotal evidence is usually fine!
work with a combination of scholarly sources and personal experience. if you’re trying to depict a specific health condition, you might consult medical sources about the technical details of the condition, as well as seeking firsthand accounts from people who have that condition.
remember that people are not monolithic! there are often forums online where people are more than happy to discuss their experiences; cross-consult these for common elements.
Lists
keep track of your sources!! if you ever need to consult something later on, it will be way easier to open a list of resources than go digging through your search history.
additionally, if you come across lists of sources compiled by other people, save those!! you are probably not the first person to research the specific topic you’re looking into, and there are entire websites dedicated to gathering research!
wordsnstuffblog.com/research has compilations of sources for everything from writing injuries to global period pieces by century.
Resources
if you can, check out your school or public library’s websites! they will often compile scholarly resources to access for free.
look for open access or open source sites like project gutenberg that archive and digitize historical documents and other works. scienceopen and the directory of open access journals are more of these. search using keywords!
keep an eye out for websites made specifically for educational purposes (those with .edu at the end of their addresses).
#🌿 writing#writing tips#writing advice#writing resources#i'm trying to compile some instagram posts on here for easier reference#writing research
902 notes
·
View notes
Text
I get very irritated by transphobic politicians pretending to care about "evidence" because I've yet to find one who actually does.
Look at this horseshit:
The Florida Department of Health wants to clarify evidence recently cited on a fact sheet released by the US Department of Health and Human Services and provide guidance on treating gender dysphoria
for children and adolescents...
Due to the lack of conclusive evidence, and the potential for long-term, irreversible effects, the Department's guidelines are as follows:
Social gender transition should not be a treatment option for children or adolescents.
The... The long term "irreversible" effects of being referred to by a different name or pronoun and possibly wearing different clothes than people might expect?
I mean I feel like you could reverse the effects by just... not doing that stuff anymore.
Anyway, they link, as evidence for their opposition to social transition, to this paper:
Title:
Not social transition status, but peer relations and family functioning predict psychological functioning in a German clinical sample of children with Gender Dysphoria
Literal first line of the abstract:
Research provides inconclusive results on whether a social gender transition (e.g. name, pronoun, and clothing changes) benefits transgender children or children with a Gender Dysphoria (GD) diagnosis.
Right in the introduction:
prepubescent children are not advised to receive any medical treatment before the onset of puberty (Tanner stage 2; Coleman et al., 2012). However, they often transition socially from one gender to another during childhood (Coleman et al., 2012). This reversible nonmedical step towards a life in the identified gender may include changing one’s name or pronoun, being introduced as the experienced gender in public, as well as gender typical appearance in terms of e.g., hair length and clothing (Steensma et al., 2013; Wong et al., 2019).
(Bolding mine)
Hey, big important Florida Surgeon General guy who wears a tie and influences the lives of millions of people:
I had to read your evidence for less than five fucking minutes before it openly contradicted what you say in your guidance.
People like this complain all the time about how evidence in trans medicine is hard to come by and uses small sample sizes, but then they link to a paper that has a sample size of 54 German kids.
Oh, and a paper which explicitly says,
Caution is also warranted in generalizing the results to all children with a GD because of the small and relative unique sample. All 54 children in the analysis sample were referred to the clinic for their GD, most of them came from families with a medium or high socio-economic background and the family support of the children’s gender identity was generally high. Due to the health care situation in Germany for children and adolescents with a GD diagnosis, some families go to considerable length to get access to treatment which they probably would not do if they did not generally support their child’s personal situation. At the same time, the clinical guidelines of the Hamburg GIS are quite liberal and allow for individual treatment pathways. Thus, these findings might not apply to a more diverse sample of transgender children who are not supported in their gender identity or expression by parents or clinicians, or children who identify themselves on a broader gender spectrum.
These people really, really fucking hope you don't actually read the evidence on this stuff.
I want to be clear: This isn't, like, one paper in a huge list of evidence against social transition, this is literally the only thing the Florida Surgeon General cites in opposing social transition.
30 notes
·
View notes
Text
Free tactical medicine learning resources
If you want to learn first aid, emergency care or tactical medical care for real, you will need to practice these skills. A lot. Regularly. There’s no way to learn them just from books. But if you’re looking to supplement your training, can’t access hands on training, are a layperson doing research for your writing or otherwise just curious, here are some free resources (some may need a free account to access them).
TCCC
The current gold standard in the field is Tactical Combat Casualty Care (TCCC), developed by the US army but used by militaries around the world. There is also a civilian version of the system called Tactical Emergency Casualty Care (TECC). Training materials, Standards of Care, instructional videos, etc. can be accessed at deployedmedicine.com. You’ll need a free account. This should be your first and possibly only stop.
There’s also an app and a podcast if those are more your thing, although I haven’t personally tried them.
More TCCC (video) resources
STOP THE BLEED® Interactive Course
TCCC-MP Guidelines and Curriculum presentations and training videos
EURMED’s Medical Beginner's Resource List has suggested list of video materials (disclaimer: I haven’t watched the playlists, but I have been trained by nearly all of the linked systems/organisations and can vouch for them)
Tactical Medical Solutions training resource page (requires registration; some of the courses are free)
North American Rescue video downloads
Emergency medicine
WHO-ICRC Basic Emergency Care: approach to the acutely ill and injured — an open-access course workbook for basic emergency care with limited resources
Global Health Emergency Medicine — open-access, evidence-based, peer-reviewed emergency medicine modules designed for teachers and learners in low-resource health setting
AFEM Resources — curricula, lecture bank, reviews, etc.
Global Emergency Medicine Academy Resources (links to more resources)
OpenStax Anatomy and Physiology textbook
Open-access anatomy and physiology learning resources
Principles of Pharmacology – Study Guide
Multiple Casualty Incidents
Management of Multiple Casualty Incidents lecture
Bombings: Injury Patterns and Care blast injuries course (scroll down on the page)
Borden Institute has medical textbooks about biological, chemical and nuclear threats
Psychological first aid: Guide for field workers
Prolonged field care
When the evac isn’t coming anytime soon.
Prolonged Field Care Basics lecture (requires registration)
Aerie 14th Edition Wilderness Medicine Manual (textbook)
Austere Emergency Medical Support (AEMS) Field Guide (textbook)
Prolonged Casualty Care (PCC) Guidelines
Wilderness Medical Society Clinical Practice Guidelines
Austere Medicine Resources: Practice Guidelines — a great resource of WMS, PFC, TCCC, etc. clinical practice guidelines in one place
The Wilderness and Environmental Medicine Journal (you can read past issues without a membership)
Prolonged Field Care Collective: Resources
National Park Services Emergency Medical Services Resources
Guerilla Medicine: An Introduction to the Concepts of Austere Medicine in Asymmetric Conflicts (article)
Mental health & PTSD
National Center for PTSD
Psychological first aid: Guide for field workers
Combat and Operational Behavioral Health (medical textbook)
Resources for doctors and medical students
Or you know, other curious people who aren’t afraid of medical jargon.
Borden Institute Military Medical Textbooks and Resources — suggestions: start with Fundamentals of Military Medicine; mechanism of injury of conventional weapons; these two volumes on medical aspects of operating in extreme environments; psychosocial aspects of military medicine; or Combat Anesthesia
Emergency War Surgery textbook and lectures
Disaster Health Core Curriculum — online course for health professionals
Médecins Sans Frontières Clinical guidelines
Pocket book of hospital care for children: Second edition — guidelines for the management of common childhood illnesses in low resource settings
Grey’s Quick Reference: Basic Protocols in Paediatrics and Internal Medicine For Resource Limited Settings
The Department of Defense Center of Excellence for Trauma: Trauma Care Resources (links to more resources)
#feel free to share and add more#tactical medicine#tactical combat casualty care#prolonged field care#austere medicine#military medicine#tccc#tecc#disaster medicine#wilderness medicine#emergency medicine#emergency medical services#learning resources#writing resources#mandalorian medics#paramedicine#medicine
17 notes
·
View notes
Text





By: SEGM
Published: Aug 17, 2023
A major medical journal Ugeskrift for Læger, the Journal of the Danish Medical Association, confirmed that there has been a marked shift in the country’s approach to caring for youth with gender dysphoria. Most youth referred to the centralized gender clinic no longer get a prescription for puberty blockers, hormones or surgery—instead they receive therapeutic counseling and support.
In the course of less than a decade, like every other Western country, Denmark experienced an exponential increase in the number of young people presenting with gender dysphoria. In 2014, there were only 4 documented pediatric cases who requested gender reassignment. By 2022, the number of referrals grew by 8700% to 352, similar to the several-thousand-percent increase in less than a decade witnessed by a number of Western countries. As the number of young people wishing to undergo gender reassignment increased, so did the rates at which Danish gender clinicians transitioned them. By 2018, Denmark's centralized gender service was medically transitioning 65% of referred youth. This was similar to the proportion of referred children who got transitioned reported by other pediatric gender clinics. For purposes of comparison, the Netherland’s Amsterdam gender clinic reports transitioning 73% of late-onset referrals and 85% of early-onset referrals and in the US, researchers analyzing data from Seattle Children’s Hospital gender clinic reported that over 60% of the referrals underwent medical transition with puberty blockers or cross-sex hormones within one year of intake.
However, following systematic reviews of evidence conducted in Europe and the subsequent reversal of the “gender-affirmation” paradigm in favor of a cautious, developmentally-informed approach that prioritizes psychosocial support and noninvasive resolution of gender distress in Sweden and Finland, Denmark appears to have made a quiet but resolute shift to treat most youth presenting with gender dysphoria with supportive counseling rather than puberty blockers, hormones, or surgery. In 2022, only 6% of those referred to Denmark’s centralized gender clinic were prescribed endocrine interventions (puberty blockers and/or cross-sex hormones).*
The rationale for this shift was explained in a recent publication in Ugeskrift for Læger (“Weekly Journal for Physicians”), the Journal of the Danish Medical Association. This Danish-language article provides one of the most sober discussions to date of the inherent medical and ethical uncertainties of providing minors with profound, life-altering interventions in the context of very limited understanding of the epidemiological shift in the population presenting for care, the growing rates of detransition, and the profound uncertainty about long-term outcomes.
The authors can hardly be accused of being “armchair critics.” They are the very clinicians responsible for assessing youth and approving them for gender transitions in Denmark. Realizing that their well-meaning intentions were based on insufficient evidence, and seeing the growing evidence of harm, they sharply reversed course. Today, only 6% of the referrals are approved for hormonal transition, and no minors are allowed to transition surgically.
The article is open-access, and only available in Danish. Below, we provide a synopsis.
The Danish centralized pediatric gender service was launched in 2016. Denmark opened a centralized gender transition service for minors in 2016, using a multidisciplinary approach that encompasses intake, evaluation, consultation, and referrals for puberty blockers and cross-sex hormones.
The rationale for launching the pediatric gender transition service was the Dutch studies’ reported success. The Danish youth gender transition service was launched based on the experience of the Amsterdam gender clinic and reports of its positive outcomes “suggesting that early hormone therapy resulted in better psychological and physical outcomes and less need for surgery in adulthood” as well as “body satisfaction, low rates of regret, and few side effects.” The two studies supporting this premise were the Dutch protocol as described by the Dutch clinicians in 2012, and the famous 2014 “Dutch study.”
A key assumption, now in question, was the permanence of transgender identity in youth with longstanding gender dysphoria that intensified in puberty. According to the authors, the Dutch “trials” of gender transition were justified insofar as it was believed that a cross-sex identity in adolescents with longstanding gender dysphoria that intensified in adolescence would be permanent, or “stable.” However, the authors now concede that there are significant questions brought about the growing rate of detransition, and concerns “about the generalizability of these studies,” especially their applicability to the young people referred to gender clinics today.
The significant “underexplained” increase in referrals of adolescents over age 11 “mainly made up of birth-assigned girls” became a major red flag. The authors describe a profound change in the epidemiology of gender dysphoria in youth following the launch of the centralized pediatric gender clinic service. “In Denmark, the number of referred persons has increased from 97 in 2016 to 352 in 2022, of which birth-assigned girls aged 11-18 make up 70%”. Noting the “excess of birth-assigned girls” among gender dysphoric youth, the authors express concern that “the background for the change is underexplained.”
Another red flag is the high rate of psychiatric comorbidities in currently-presenting cases. The authors note that unlike the Netherlands, where gender dysphoric youth reportedly have a relatively low rate of psychiatric comorbidities (33%), in Denmark and other countries there is a much greater proportion of gender dysphoric youth with comorbid mental illness (e.g., 75% in Finland). These conditions include depression, anxiety, suicidal thoughts/self-harm, autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD).
The authors raise a new concern: gender dysphoric youth have a younger age of pubertal onset. They reference a Danish study that found earlier puberty in youth with gender dysphoria compared to the general population of adolescents. They do not elaborate on the implications of this finding, but note that overall the pubertal age has been declining.
The authors call out more generally the growing rates of gender nonconformity in youth, and especially females, independent of the youths’ wish to medicalize. The study authors cite the results of the Danish Project SEXUS study which found a sharp increase in gender nonconformity (21.2% of females and 15.7% of males ages 15–24 years). The authors note a generally “higher incidence of non-gender-normative behavior among girls” and “low tolerance for non-gender-normative behavior in boys.”
The authors explicitly identify “social influence” as a contributor to the concerning epidemiological shift in gender dysphoria presentation. The idea that teens are products of their social environments and can adopt transgender identities following social influence does not appear to be controversial in Denmark. The authors openly discuss the possibility of social influence as directly contributing to the rapid rise of post-pubertal onset of gender dysphoria in youth. They also opine that the availability of treatment itself may have contributed to rapid rise of trans-identification in youth.
The Danish clinicians are concerned by growing rates of detransition among those who initiated transition in youth and a lack of research into the detransition phenomenon. “In recent years, there have been reports of reversal of hormone-induced permanent changes to the body that began in youth. There are no systematic estimates of the frequency or reasons why hormone treatment is discontinued.”
The Danish clinicians are now concerned that the basis for gender-transition of large numbers of minors with diverse presentations of gender dysphoria is a single short-term Dutch study based in a different population and which has failed replication outside the Netherlands. Throughout the article, the Danish clinicians describe their initially positive view of the Dutch research, and their now growing concern about the lack of applicability of the Dutch experience from years past to the current clinical realities in the rest of the Western world. They appear to be signaling a widening gap between the positive trends that the Dutch clinicians continue to report (youth with low rates of mental illness, low rates of detransition, and positive short-term transition outcomes), and the problems emerging in the rest of the Western world (much higher rates of comorbid mental illness, an inability to show robust and reliable improvements in mental health, and growing rates of detransition).
International changes, and especially those in the Nordic European countries, appear to have directly influenced Demarks’ move to a more cautious approach. In Finland and Sweden, youth with post-puberal onset of gender dysphoria are not typically considered to be candidates for medical transition in adolescence. Denmark’s gender clinicians quoted these changes in their new move to base treatment eligibility in part on the “duration” of gender dysphoria.
As a result of the above-mentioned concerns and international changes, Denmark has sharply restricted eligibility for hormone interventions for youth. The authors state that Denmark has “adopted a more cautious approach to hormone therapy until more evidence of its beneficial effects is available.” While the article does not provide year-over-year referral-to-treated ratios, another source confirms that in 2018, two-thirds (65%) of referred youth were transitioned and by 2022 this percentage fell to 6% (22/352).
The authors conclude with a call for more research and international collaboration:
"Several countries, including Denmark, have adopted a more cautious approach to hormone therapy until more evidence of its beneficial effects is available [2, 17]. In particular, there is a lack of knowledge about the increasing proportion of young people with onset of gender-related discomfort after puberty [2, 17, 23] and the presumably increasing proportion with mental disorders, as new studies suggest that the positive effects are not replicated in this group [22, 29]. There is a need for healthcare services that can be flexibly adapted in the future and systematic international cooperation in research and exchange of experience."
The current Danish treatment guidelines were published in 2018 and are due to be updated later this year. While the specifics of the changes have not yet been made public, the new approach described in the article foreshadows the likely principles and practices that will be included in the updated guidelines, specifically:
Thorough psychological assessments are required to determine whether gender dysphoria is related to a mental health disorder such as ASD, or psychosis. All young people are to be thoroughly assessed using broad and lengthy diagnostic interviews with multiple reporters including schools and parents as well as cognitive testing. The assessment aims to determine whether gender discomfort may be an aspect of a psychiatric disorder or mental illness.
Minors whose gender dysphoria differs from the classic “Dutch” definition (i.e., early onset of gender dysphoria that worsens after puberty, no significant mental health comorbidities) will only be offered psychosocial, supportive treatment. The centralized team will assess for the appropriateness of medical transition. Most presenting cases are rejected from consideration for medical transition and instead are referred to “support or advisory conversations.” Of note, while the authors reference the longstanding duration of gender-related distress that worsens in puberty they do not explicitly require early childhood onset of gender dysphoria. It remains to be seen how explicit this requirement is in the updated guidelines.
Not every otherwise eligible minor will be considered able to consent. The authors explain that“…the level of functioning, stability and how any psychopathology, cognitive level and psychosocial conditions affect identity development and the ability to reflect on and make decisions about gender reassignment treatment.”
Teens ages 15 and older retain the right to consent to treatment without parental agreement or consent, but the treatments offered will prioritize counseling. According to the current 2018 Danish treatment guidelines, when a 15-year-old minor and their parents disagree about gender transition, the minor can proceed without parental consent. This is because Denmark’s laws consider 15-year-olds competent to make medical decisions. While these laws will not change, the authors recognize the important role of parents in this unusual situation, and underscore that the treatments offered to the teens will be “psychosocial support for the young person” and they further assert that “ideally all decisions are made in consultation with the parents.”
For the remaining few cases that will qualify for transition, significant uncertainties are explicitly identified. Irreversible changes are called out, along with the health risks: “…both types of sex hormones cause reduced fertility, however the degree and reversibility of this remains unknown. Contraindications to hormone therapy are abuse, suicidal ideation/self-harm, severe psychological distress and worrisome somatic conditions (eg cancer, thromboembolic disease).” It is acknowledged that hormone treatment will be lifelong.
Surgical interventions in minors, already rare, will likely be removed as an option. The current treatment guidelines do not allow genital surgeries for those under 18, but it appears that mastectomies for some older teens are still an option (although perhaps an option on paper only). Recent comments by the Danish Minister of Health suggest that mastectomies may be officially disallowed in the updated guidelines.
“I can also inform you that the National Board of Health [“Sundhedsstyrelsen”] issued a new guideline for gender reassignment surgery on March 28 this year at the latest, which is now in consultation. In the new referral guidelines, it is no longer possible to offer surgical treatment to children under the age of 18... An option that, by the way, has never been used in Denmark.” **
SEGM Take-Away
In the last several weeks, health journalists have reported that change may be afoot in Denmark. The article in Denmark’s Medical Association journal Ugeskrift for Læger leaves very little doubt that Denmark too has made a course correction in youth gender transitions, restricting this option to very few cases, while prioritizing counseling for the vast majority of the currently presenting youths. The article is an excellent summary of the rise-and-fall-of the “gender affirmation” model of care in Denmark. It describes how in 2016, following the influence of other northern European countries, Denmark chose to offer “a treatment approach with few barriers to hormone treatment for children and young people with gender dysphoria.” The treatment was justified by the foundational Dutch studies, “which indicated better well-being and body satisfaction after hormone treatment, a low degree of regret and few side effects.” However, the increasing number of referrals, changes in the presentation in gender dysphoria, and growing reports of regret—combined with a lack of long-term outcomes of the one and only sample of youth (n=55) on which the entire practice of gender transition rests—led the Danish clinicians to reverse course.
This change is notable. In 2014, Denmark became the first European country to pass a “self-id” law for adults whereby adults did not need a diagnosis of gender dysphoria to register a legal sex change. Denmark continued to be a leader in destigmatizing transgender identities and in 2017, becoming the first country in the world to remove “Gender Identity Disorder” (DF64) from the its public health authority's list of mental illnesses. To provide treatment, healthcare practitioners were instructed to use a “Z” code, “contact due to gender identity” (DX78X)." The barrier-free transition of minors, launched in 2016, was the logical next step.
To fully appreciate the scope of the changes underway in the treatment approaches for minors, it is helpful to review Denmark’s 2018 official practice guidance, Health professional help with gender identity issues (English-language version here). The guidance does not preclude any presentation of gender dysphoria from eligibility for transition; there is no minimum age for transition; and at age 15 minors who are considered able to understand the consequences of treatment for gender dysphoria may obtain medical transition services without parental consent.
Recently, Danish Minister of Health Sophie Løhde acknowledged that country’s national pediatric center for gender dysphoria in Copenhagen has grown “reluctant to offer hormone treatment compared to before,” particularly to youth with post-pubertal onset of gender dysphoria. The Danish Health Minister praised this change in practice, noting that “it is a positive thing that there is a response to research and experience... both in Denmark, but also abroad, which we must follow closely. And this knowledge and experience lead to adjustments in the current treatment options.”
While countries in Europe are increasingly leaning on one another’s experience and collective knowledge to devise an approach to intake, screening, and support of gender-dysphoric youth in order to safeguard them from inappropriate, non-evidence-based gender reassignment practices, the American medical establishment continues to double-down and “do it alone.” Earlier this month, the American Academy of Pediatrics (AAP) finally conceded to conduct an independent review of the evidence and update its guidance. This decision has come several years too late: the first call for these actions came from AAP members in 2019 and has been repeated every year since.
However, at the same time, at its 2023 Annual Leadership Forum earlier this month, AAP paradoxically reaffirmed its current “transition for all those who want it” affirmative care approach, refusing to acknowledge or consider the problems that have been documented by the recent European systematic reviews and react in real time. Rather than working collaboratively, as the Danish clinicians have suggested in their article, the CEO of the AAP has described a decidedly American-exceptionalism approach: “they engaged in their process, we’re engaging in our process.” And just earlier this week, the official AAP website platformed another article promoting gender transition of minors by two gender clinicians who reassured America’s pediatricians that "affirmation" is beneficial while caution is harmful: “When pediatricians lack knowledge about the needs of transgender and gender-diverse youth, they may default to the “watch and wait” approach. This method is outdated and harmful….” (The article does carry a footnote, "The views expressed in this article are those of the author, and not necessarily those of the American Academy of Pediatrics.)
America was fast to import and accelerate the European approach to treating minors, putting it “on steroids” and adding the scalpel. However, when it comes to reversing course, it intends to take its time. Why AAP staunchly refuses to accept the conclusions of multiple systematic reviews of evidence that found the practice of youth gender transition to either not be clearly beneficial, or net-harmful is unclear. Although the AAP has finally agreed to commission its own systematic review, it has already presaged the review's conclusion, which is that it will support the current pro-affirmation AAP position. In the meantime, thousands of American children and parents continue to be misinformed that science and evidence support the practice of gender transitions for youth who desire them, and that those raising concerns are merely science-deniers spreading “scientific misinformation” at best, and likely ill-intentioned. Therefore, it is not surprising that in America, the debate will continue to be politicized, and may ultimately be adjudicated in the court of law rather than due to the diligence and responsible actions and course corrections of the medical community itself, as is currently underway in Europe.
Intakes vs Approvals for Endocrine Interventions for Minors by Year, Denmark*:

Footnotes:
* The referrals and treated numbers for the Danish national gender clinic service are available at the Danish Rainbow Council website. While SEGM cannot independently verify the accuracy, we have no reason to doubt these statistics. Specifically, the number of referrals for 2017 (n=97) and 2022 (n=352) matches the data reported in this source and the numbers quoted in the referenced official Dutch medical journal.
** The speech by the Danish Minister of Health, Sophie Løhde, is available at this link. The English language transcript is available at this link.
#SEGM#Society for Evidence Based Gender Medicine#medical scandal#medical transition#gender ideology#genderwang#queer theory#puberty blockers#sex trait modification#religion is a mental illness
8 notes
·
View notes
Text
Cutting to the "shopping list" section:
We focused on using “off the shelf” components and open-source software to develop the wireless endoscope. This significantly lowered the cost with the goal to make the device accessible for resource-constrained environments. While the technology described is applicable to a variety of rigid lens applications, we attempted to replicate the 4 mm cystoscope lens and separately a clip-on universal endoscope camera.
2.1 Hardware systems
A miniature single-board computer (SBC) module the Raspberry Pi Zero W (Raspberry Pi Foundation, Caldecote, UK) was used because of its size, its low cost (US$10) and its ability to handle high-definition (720p) video.
A 3.7-mm tube camera (model: 1001LG, Shenzhen Eastern International Corporation Limited, Shenzhen, China) was used. It delivers 1280 × 720 high-definition video using a 1/7″ colour CMOS sensor. Lens construction allows a wide (115 degree) field of view and an extended depth of field allowing object in the range of 5 to 50 mm to be in focus. Connectivity is via a USB 2.0 interface with the SBC. The camera is certified IP67 waterproof and the manufacturer is ISO 13485:2016 certified for the design and manufacturer of medical endoscope cameras.
Illumination is via 6 high luminous 0603 white colour LEDs incorporated into the tube camera. The system was powered by a 1200mAh lithium polymer battery and incorporated into a fireproof acrylonitrile butadiene styrene enclosure.
For the clip-on wireless camera module, an 18–35 mm optical zoom coupler (Ouman Medical, Jiangsu Ouman Electronic Equipment Co., ltd, Jiangsu, China) and an 8-megapixel camera module (model: IMX219, Arducam) were used.
2.2 Software systems
Open-source Linux software was used on the SBC as follows:
1. The SBC runs on the Raspbian Pi operating system Lite, a minimal image of Debian Buster [9].
2. The SBC Wi-Fi module is placed in monitor mode (“hotspot”) using RaspAP [10]. This makes wireless video transmission possible.
3. The video signal is streamed via the UV4L module of “Video 4 Linux 2” [11].
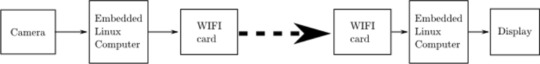
4. Lastly, the wireless video signal is viewed on a standard computer via any internet browser. Figure 2 illustrates the entire software setup.
Fig. 2:
7 notes
·
View notes
Text
“Ella Roe” (USA 2009–2010)
A paper in the Obstetrics & Gynecology medical journal in 2011 reported the death of a woman who died after taking the abortion pill because of Planned Parenthood’s negligence.
“Ella Roe” legally bought the abortion pill from a Planned Parenthood facility in 2009 or 2010. Planned Parenthood apparently failed to competently examine her in advance and most likely did not bother to give her an ultrasound. If they had, it would have been easy to diagnose Ella’s ectopic pregnancy.
Unaware that her life was in danger, Ella took the RU-486 pill. She trusted her health to an abortion facility and paid the price for their malpractice.
Ella died from the ruptured ectopic pregnancy. The condition could have and should have been diagnosed with a simple ultrasound, but Planned Parenthood didn’t care enough to examine her before selling her the pill.
The publication does admit to severe side effects, but claims that their work “reinforces the safety” of the abortion pill. However, there are severe limitations and conflicts of interest that most likely prevented significant amounts of data from being included.
First, the data used was obtained mostly from Planned Parenthood, with the corporation even listed as one of the authors. They have been known to lie about statistics relating to abortion and would directly benefit from withholding data that made them look bad. Second, nobody is legally required to report abortion pill deaths or complications to authorities, meaning that it would be very easy to simply not report a case. One of the authors of the study was also noted to “receive compensation” from Danco Laboratories (the manufacturer of the abortion pill) in exchange for “providing third-party telephone consults to clinicians who call for expert advice on mifepristone.”
Other studies on the abortion pill have observed a high level of danger. Even one pro-abortion source showed that as many as 1 in 12.5 abortion pill clients had to go to the ER. Still, even this statistic could easily be underestimated because it’s hard to get accurate data on complications form American abortions because of the flawed reporting system full of discrepancies. The chemical abortion pill can cause excessive bleeding, sepsis, gas gangrene, hypovolemia, uterine inversion, cryptogenic stroke, tachycardia, leukocytosis, edema, hypotension, metabolic acidosis, necrosis, immunological weakening, cardiac arrest and excruciating pain.
As surprising as it is for something including Planned Parenthood’s input to admit to a client death, the publication alone is by no means proof that the abortion pill is safe.
#tw abortion#pro life#unsafe yet legal#tw murder#tw ab*rtion#abortion#abortion debate#death from legal abortion#unidentified victim#planned parenthood#tw negligence#tw malpractice#the abortion pill kills#kill pill#this is chemical abortion#abortion pill
5 notes
·
View notes
Text
I do not like my life and I don’t know what to do. I feel like I’ve exhausted all my efforts. I’ve tried to do the healthy eating, and waking up early, and get enough sleep, and don’t abuse substances, and go for a walk, journal, yoga. I tried accessing mental health resources on my campus when I was a college student and it actually was so traumatizing. I had a male psychologist ask me why I was on birth control & if it made my boobs bigger. another male counselor I was paired with got angry at me once for getting off topic during our session. a female counselor once immediately suggested I be put in a psych ward because I said I was experiencing symptoms that made me wonder if I had bpd. I went through probably at least 10 different counselors while I was in school and had access to them and in the end I realized none of them were equipped to help with the kind of problems I was experiencing and still experience to this day. I ended up failing so many classes and just dropping out of school because I was so depressed and overwhelmed. I feel as though the education system failed me. I believe I have some sort of learning disability like possibly adhd or autism that inhibits me from functioning in my daily life like a typical adult. this has caused me to carry such a weight of feeling broken, not good enough, “crazy”, incompetent and other horrible feelings about myself because it’s truly so difficult at times just to take care of myself and complete all the normal tasks that seem to come so easily to others. I moved states away from everyone I know. developed a drinking problem. have jumped around from unfulfilling minimum wage job to unfulfilling minimum wage job. have burned so many bridges and caused an embarrassing amount of public outbursts because of my impulsive nature. I’ve tried seeking medical help under my insurance that I just got this last year but I was only ever met with a robot on the other side of the calls and then when I finally did reach actual humans after multiple hours of struggling I was told the soonest available appointment is over a year from now. I recently found Open Path which is supposed to help connect you with affordable therapists in your area so I’m waiting for a response email and keeping my fingers crossed. but I can’t help but feel so hopeless. I have not had a good year. I feel so unstable and like things only get progressively worse. if I began to list everything that has happened to me this post would become extremely long no one would want to read it and just scroll past. I’d just like some support but I don’t know where to find it. I feel like I’ve ostracized myself from many of my friends when my symptoms begin to come out. and it hurts because I know there’s so much more to me than all the useless suffering I’ve endured.
2 notes
·
View notes
Note
Hello Black Bird Brewster! I'm the anon from chaotic archeologist who thinks they are autistic and am going to a dr for pain. I would like to hear any advice and thoughts you have about disclosing information to a dr about 'self diagnosed autism' and maybe how to convey my pain symptoms so I'm not brushed aside?
I grew up with weird ass parents so I've been suffering for quite a long time so I'm real good at 'masking'
Hello Anon,
Thanks for reaching out! For context, I live with multiple disabilities/chronic illnesses. My first dx on this list was about a decade ago. I am also ADHD, that was dx as a kid but I haven't actually had 'treatment' since I was like 10? A couple of years ago I realised I'm also Autistic! Self-diagnosis is extremely important and valid. Because I am a seemingly 'well-adjusted' adult there is literally NO way for me to seek medical dx for autism in my country. There's also no support or benefit to me getting a medical dx. It just isn't accessible, so that's not a thing I care about. I know I'm autistic and that's what's important.
Okay! Now for your question. Approaching any doctor or specialist to discuss chronic pain/illness is ALWAYS nerve-wracking. We unfortunately live in a world where most doctors think they are the know-all be-all of medical knowledge and as soon as you try to suggest your own findings or possible dx of what's going on, they just shut you down. Doctors are taught to 'fix' things. They are trained to deal with acute illnesses that they can slap a band-aid on and heal the patient.
When it comes to CHRONIC illnesses, they don't usually knwo what the fuck they're doing. So they tend to be dismissive because dismissing your symptoms/experiences, is easier than them simply admitting they don't have the answer: they don't know what's going on or what is causing your symptoms. The bar is so low it's on the fucking floor. All we want is to have doctors who actually LISTEN and who are open to discussion, but that isn't always the case. And I know seeking second opinions can be costly and inaccessible, depending on your situation. So what are we to do?
My best advice for your appointment to discuss your pain: Be prepared!!
Start a daily journal that you can track your daily pain symptoms. Note anything that seems to make things better or worse. You can do this in a journal or use an app! I use Daylio for mood tracking and all of my symptoms. It's a great app!
Make a symptom tracked of all the things you have been experiencing. You can also do this in Daylio which is hella handy because it's fully customisable. And I can pull up my phone at appointments and immediately report 'Well after I started this medication I logged ten straight days of anxiety, so maybe we need to try something else'
Prepare a detailed medical history that you can print out and hand over as soon as you walk through the door. (This especially helps me because sometimes my autistic anxiety of talking to a new specialist makes me suddenly minimise everything in the moment. But having things pre-written helps so much!) [Here's a template I made]
Bring a support person!! Bring someone you trust, who knows everything you've been going through so they can help fill in blanks and they can take notes during the appointment. My partner takes notes for me because otherwise, I will instantly forget what the doctor said. I get so stressed about my appointments that I usually am half-dissociative during them, so having my partner there is SO helpful.
BRING SOME COMFORT ITEMS!! I do NOT go to any appointment without my favourite fidget AND a stuffed animal. Fuck what people think about it. It's the only way I can pay attention at appointments and I am unashamed to stimm in order to be functional.
The more prepared you are, the more serious doctors seem to take you. (Again, it should NOT be this hard but we're just trying to survive a medical system that does NOT want to help disabled people.)
Now, in terms of your autism:
This is entirely a personal choice. I am extremely lucky to have a GP who listens to me and is 100% supportive when I go 'Hey, I think all these symptoms could be x,y,z' I had already been seeing ehr for years when I realised I'm autistic, so when I realised it I was in the same dilemma you are in. Ultimately, I never had a sort of 'coming out' as autistic convo with her. I simply just started talking about it casually in regards to my treatment. 'Well, my autistic sensory needs would not be able to cope with that medication. Is there something else we could try?' Stuff like that. I also always have my medical bracelet on that states I'm autistic. And I'm always sporting my pronoun badges and at least one badge that clearly states I'm autistic. She has never asked about it, she just has just begun to take my autism into account as we discuss treatments.
But for new doctors/specialists, I have a very clear disclaimer on my little medical document. It is highlighted at the top and it simply says: I am autistic, please be patient with me.
I will also tell doctors this up front and I try to name my needs throughout the appointment. Things like asking for them to email me a copy once they finish their full report of our appointment, or asking them to explain something further if I don't understand, or asking them for more information about treatments before I can make a decision.
I never declare 'Hey, I'm self-dx autistic and here's all the reasons why I believe this.' because that is NOT the important part. What's important is that I am able to voice what I need in terms of accessibility in regards to my autism.
If you're seeing a doctor for anything other than an actual autism assessment/treatment (like a psychdoc), then I don't see any reason why you need to over disclose things. You don't need to try and validate the fact you are autistic to a doctor who is simply trying to treat your chronic pain.
You are autistic. Full stop. You don't need to expend any extra emotional energy in order to convince other people of that fact. If you WANT to talk to your doctor about these things, then go for it. But if you're concern lies with 'what do I NEED to disclose' the answer is absolutely nothing you're uncomfortable with.
I hope this helps and I really hope your appointment goes well. I hope your pain eases soon, my anon love. Please always remember that your feelings and needs are completely valid and you should never have to compromise your comfort levels for anyone.
I love you. I am proud of you. I am here for you. x
2 notes
·
View notes
Text
Differential Effects of Unsaturated Fatty Acids and Saturated Fatty Acids on Lipotoxicity and Neutral Lipid Accumulation in Neuro-2a Cells

Differential Effects of Unsaturated Fatty Acids and Saturated Fatty Acids on Lipotoxicity and Neutral Lipid Accumulation in Neuro-2a Cells in Biomedical Journal of Scientific & Technical Research
https://biomedres.us/fulltexts/BJSTR.MS.ID.006017.php
Long-chain free fatty acids (FFA) play many important roles in cell growth and metabolism. Accumulation of excess saturated fatty acids (SFA) leads to deleterious lipotoxic effects in non-adipose tissues while unsaturated fatty acids (UFA) often exert protective effects against SFA lipotoxicity, yet the lipotoxic effects of SFA in neuronal cells have not been well characterized. This study examined the differential effects of SFA and UFA on the viability of Neuro-2a (N2a) cells and the accumulation of neutral lipids in these cells. Our study found that all the UFA tested, namely oleic acid (OA), linoleic acid (LA), α-linolenic acid (ALA), and docosahexaenoic acid (DHA), were able to abolish PAinduced decrease in cell viability regardless of the position of the double bond or degree of unsaturation, and that 200 μM LA, OA, and DHA significantly enhanced the amount of neutral lipid staining than BSA control while PA did not, suggesting that LA, OA, and DHA, but not PA, increased the amount of neutral lipid synthesis and accumulation. The neutral lipid staining also appeared more in particulates in UFA-treated cells than PAtreated cells, suggesting that UFA, but not PA, enhanced LD formation. We also found that the amount of neutral lipid staining in cells co-treated with UFA and PA was comparable to that in cells treated with BSA or PA alone, and that the neutral lipid staining in cells co-treated with UFA and PA appeared more concentrated in particulates than PA-treated cells, suggesting that UFA may not enhance neutral lipid accumulation, but may increase LD formation in PA-treated cells. Our results suggest that UFA and SFA have differential effects on cell viability, neutral lipid accumulation, and LD formation in N2a cells. Further studies will be needed to examine the role of LD formation in UFA protection against PA lipotoxicity.
For more articles in Journals on Biomedical Sciences click here bjstr
Follow on Twitter : https://twitter.com/Biomedres01
Follow on Blogger :https://biomedres01.blogspot.com/
Like Our Pins On : https://www.pinterest.com/biomedres/
#journal on medical science#list of open access medical journal#American Medical Journal#journals on biomedical engineering#journals on biomedical science
0 notes
Text
Biomed Grid | Future of Biotech Equipment/Medical Device Research & Development: A Case for Redemption of the Neglect
Introduction
The global healthcare industry is undergoing a progressive transformation at a rapid pace. Ground breaking innovation across multiple fields including biotechnology, pharmaceutical and medical devices is driving this transformative journey, the main outcome of which is improved patient health and decreased cost burden resulting in enhanced quality of life.
Small molecule drug development and advances in bio therapeutic formulations by various pharmaceutical and biotechnological companies respectively, either alone, or in collaboration with dedicated research groups in academia tend to garner the majority of government and non-governmental funding. However, a critical area of biomedical research that lags behind in comparison with its peers in this category are biomedical devices that are also an integral part of patient therapy. While this disparity is most evident in the developing countries beset with social inequalities and a lack of medical infrastructure [1] , even in developed nations leading in biotech innovation such as the US there has been a steady decline in the investment poured into this field with a fall in available funding from 11% in 2010 to approximately 5% in 2016 [2] . Collectively, this imbalance could perhaps be applied to the term “10/90 Gap” coined by Global Forum for Health Research [3] to reflect that only 10% of health research funds are spent on the problem of developing optimum biotech equipment and devices for 90% of the world’s population.
Traditionally, most of the research and development (R&D) of new and efficient biotech equipment especially smaller medical devices are undertaken by startup companies which invariably depend on funding provided by private equity/venture capitalists. But the risks associated with market stability coupled with slow pace of development including the prolonged process of getting FDA approval oftentimes result in the redirection of finances from these sources towards more lucrative non-medtech sectors wherein the time gap from development to actualization of return is less. The big players, namely the corporate sharks on the other hand are more prone to withhold investing in smaller startups and rather play a wait and watch approach to let the completion of the development and testing process before paying to acquire the business in its entirety.
Despite these setbacks the tides are starting to turn in favor of greater opportunities for those involved in R&D in the biotech equipment/medical device sector at both the industry and academic levels. The potential for crowd sourcing funds to support startups and establishment of grants to sponsor seed money by Research Institutions is a step in the right direction. It is indeed heartening to note that in the 2018 cycle of the LEAP Inventor Challenge Awards administered by the Skandalaris Center for Interdisciplinary Innovation & Entrepreneurship at the Washington University in St Louis, 3 out of the 5 awards conferred were in the area of medical device development. As the transformative journey in this previously eclipsed field gathers renewed momentum the hope for further advancements in the future holds promise.

Read More About this Article: https://biomedgrid.com/fulltext/volume7/future-of-biotech-equipment-medical-device-research-development.001134.php
For more about: Journals on Biomedical Science :Biomed Grid | Current Issue
#biomedgrid#american journal of biomedical science & research#open access clinical and medical journal#list of open access medical journal
0 notes
Text

Grace / ( she/her ) / 24
portrait artist & character designer
jewelry & pendulum crafter
book-binder & OOAK grimoire crafter
I am a queer, disabled artist but am also an avid TTRPG fan, board game nerd, cosplayer, gamer, witch bitch, cat mom and wife ~ <3
-{ ASKS, DMs & COMMISSIONS OPEN }-
find me elsewhere as ->
GalacticGraceArt
ON cara / bluesky / instagram / facebook / etsy



a bit about me :
At 15 I was diagnosed with psychotic depression. Hearing ‘you have psychosis' as a 15 year old was truly terrifying; I didn't really understand what it meant and what parts of myself weren’t “normal”
I spent a very long time trying different methods of healing; anti-depressants, anti-psychotics, anti-anxiety medications, mood stabilizers, two in-patient hospitalizations, three TMS treatments, four self help workbooks and TONS of therapy later; I'm now 24
As someone with daily visual and / or auditory hallucinations, life can feel like a lot like a survival horror game, especially when my hallucinations tend to stick to themes of gore. In an attempt to fill the world with a little more magic, I create whimsical and body positive art.




Commissions & Customs Info!
my artistic specialties :
high fantasy, whimsical character art
body positive & nude portraits
ethereal and surrealist themes
plus size, femme and magical characters
detail-oriented artwork
With inflation driving prices up and extra money being a luxury few can afford, I really try to keep my prices as low as I can. I believe art and handmade goods should be accessible to everyone. All my costs are mainly meant to cover supply costs so I can continue creating ~
So for total transparency into what I charge for a custom piece, my pricing process is as follows :
cost of supplies ( divided by use, not full cost )
+ my pay per hour I spend on a piece ( 10$ USD )
+ price of shipping, if any
When I have the description and an understanding of the project in mind, I will be able to calculate more specific pricing for the client. Listed below are the starting prices per medium, subject to change depending on complexity



starting prices per medium :
*shipping costs are not added to the prices here, those are dependent on your location and package size / weight*
~ if it helps at all, I am a TX / US based artist ~
graphite sketch : 20$ USD
comes with a shaded graphite sketch of one full body character and a simplistic background, on watercolor strength paper
digitally rendered character art : 40$ USD
comes with a fully rendered and colored bust-style portrait with a simplistic background done in the Procreate app
gouache & marker portrait : 60$ USD
comes with a fully colored waist-up portrait done with a mix of gouache paints, ink, and markers, done on watercolor strength paper
hand-bound journal / grimoires : 85$ USD
comes with a handbound journal with 50 pages of watercolor strength paper, some decorative paper and handmade covers
prices vary depending on design complexity, canvas size, extra characters if any, requested supplies I don’t already have, etc.

#artists on tumblr#meet the artist#commissions open#commission#lgbtq#witchy#cottage witch#ttrpg character art#dnd character art#oc artist#d&d commission#character design#fantasy art#dnd character#dnd art#character art#gouache#ttrpg character#d&d#d&d 5e#d&d art#d&d character#d&d oc#dungeons and dragons#ttrpg#tabletop roleplaying#fantasy#ttrpg art#artwork#my art
1 note
·
View note
Text
Pursue Your MBBS Dream in Maharashtra: A Comprehensive Guide

Maharashtra, one of India's most dynamic and assorted states, offers uncommon openings for students aspiring to study MBBS. With top-tier medical colleges, reasonable charge structures, and a student-friendly environment, Maharashtra has ended up a centre for medical education in India. This web journal will explore the key angles of examining MBBS in Maharashtra, counting expenses, beat colleges, and the admission preparation, centering on eminent education like DY Patil Medical College and Symbiosis Medical College for Women in Pune.
Why Study MBBS in Maharashtra?
Studying MBBS in Maharashtra comes with a share of benefits. The state is home to a few of the finest medical colleges in India, known for their amazing academic infrastructure, experienced workforce, and cutting edge offices. Furthermore, Maharashtra's different culture, dynamic way of life, and various openings for commonsense exposure make it a perfect put for medical students.
Top Medical Colleges in Maharashtra
DY Patil Medical College, Pune
DY Patil Medical College, Pune, is one of the foremost prestigious medical colleges in Maharashtra. Built up in 1996, the college is partnered with the Dr. D. Y. Patil Vidyapeeth, a regarded college. The college is known for its state-of-the-art foundation, comprehensive educational programs, and profoundly qualified workforce. It offers different undergraduate, postgraduate, and doctoral programs in medical sciences.
Symbiosis Medical College for Women, Pune
Symbiosis Medical College for Women, Pune, is an interesting institution devoted to engaging ladies in the medical field. Subsidiary with Symbiosis Worldwide College, the college offers a steady and supporting environment for female medical students. The college is prepared with cutting edge offices and gives broad clinical exposure through its related clinics.
Other Outstanding Medical Colleges
Allow Medical College, Mumbai: One of the most seasoned and most prestigious medical colleges in India, advertising great medical education and research opportunities.
KEM Clinic and Seth GS Medical College, Mumbai: Famous for its quality education, inquire about offices, and healthcare administrations.
Outfitted Strengths Medical College (AFMC), Pune: A chief institution known for creating high-calibre medical experts who serve in the Indian Outfitted Strengths.
B. J. Government Medical College, Pune: Offers a wealthy legacy of medical education with broad common sense preparation.
MBBS Fees in Maharashtra
The MBBS fees in Maharashtra can shift altogether based on the sort of institution (government or private) and the particular college. Government medical colleges for the most part have lower expenses compared to private education. For occurrence:
Government Medical Colleges: The yearly fees can run from INR 70,000 to INR 1,00,000.
Private Medical Colleges: The fees can be essentially higher, extending from INR 5,00,000 to INR 25,00,000 per annum.
It is basic for students to consider these variables and arrange their funds appropriately.
Admission Process for MBBS in Maharashtra
The MBBS admission process in Maharashtra is fundamentally based on the National Eligibility cum Entrance Test (NEET) scores. Here are the key steps included:
Qualify NEET: Aspirants must qualify for the NEET exam with a substantial score.
Enlistment: Enrol for the Maharashtra State Directing conducted by the Directorate of Medical Instruction and Research (DMER).
Justify List: Based on NEET scores, a justified list is ready.
Advising: Take part within the guiding preparation where seats are apportioned based on the justify list, inclinations, and accessibility.
Admission: After situate assignment, candidates must total the admission conventions, counting expense instalment and record verification.
Best Medical Colleges in Maharashtra
When trying to find the most excellent medical college in Maharashtra, students ought to consider components such as academic notoriety, staff, framework, clinical presentation, and student support administrations. DY Patil Medical College and Symbiosis Medical College for Women stand out due to their all encompassing approach to medical education and student welfare.
DY Patil Medical College, Pune
DY Patil Medical College is eminent for its broad research offices, progressed research facilities, and a tremendous organisation of hospitals for clinical preparation. The college emphasises research-oriented educational programs, empowering students to lock in in innovative medical research.
Symbiosis Medical College for Women, Pune
Symbiosis Medical College for Women,Pune on making a conducive environment for ladies in pharmaceuticals. The college offers comprehensive medical education with a centre on viable aptitudes and moral jones. The related Symbiosis College Hospital and Research Middle gives adequate clinical exposure and hands-on training.
Conclusion
Choosing to study MBBS in Maharashtra could be a choice that can essentially shape your medical career. With its cluster of top-notch medical colleges, reasonable fees, and strong admission process, Maharashtra stands out as a favoured goal for medical hopefuls. Whether it's the notable Give Medical College or the dynamic Symbiosis Medical College for Women, Maharashtra's medical education offers a mix of quality education and all encompassing advancement. Begin your journey towards a fulfilling medical career by considering Maharashtra's regarded medical colleges.
0 notes
Text
Packing Like a Pro: Essentials for Your Study Abroad Experience

Embarking on a study abroad journey is an exciting and enriching experience that opens doors to new cultures, perspectives, and adventures. Whether you're heading to a bustling city in Europe, a serene countryside in Asia, or a vibrant university town in Australia, packing smartly can make all the difference in how smoothly your time abroad goes. To help you prepare like a pro, let's delve into the essentials for your study abroad experience.
1. Research Your Destination
Before diving into packing, take some time to research your destination. Consider the climate, local customs, and any specific cultural norms that may impact your wardrobe and lifestyle. For instance, if you're going to a tropical region, lightweight and breathable clothing will be key, while a colder climate will require warm layers and waterproof gear.
2. Essential Documents
Ensure you have all necessary documents in order, including your passport, visa (if required), acceptance letter from your host institution, travel insurance, medical records, and any other important paperwork. Keep digital copies backed up online and carry physical copies in a secure travel document organizer.
3. Clothing Essentials
Pack versatile clothing items that can be mixed and matched for different occasions. Include comfortable walking shoes, a waterproof jacket or coat, layers for varying temperatures, formal attire for special events or presentations, and swimwear if you'll be near beaches or pools. Don't forget accessories like scarves, hats, and sunglasses.
4. Electronics and Adapters
Bring along essential electronics such as your laptop, smartphone, chargers, power banks, and any adapters or converters needed for the local electrical outlets. Consider investing in a portable hotspot or SIM card for reliable internet access, especially if you'll be working or studying remotely.
5. Medications and First Aid
Pack an ample supply of any prescription medications you require, along with a basic first aid kit containing bandages, pain relievers, antiseptic wipes, and any personal health items. Familiarize yourself with local healthcare options and emergency numbers in case you need medical assistance during your stay.
6. Travel Essentials
Include travel essentials like a sturdy backpack or carry-on luggage, travel-sized toiletries, a reusable water bottle, snacks for the journey, a travel pillow and blanket for long flights or train rides, and entertainment such as books, music, or podcasts.
7. Money and Banking
Plan your finances ahead by notifying your bank of your travel plans, obtaining local currency or a travel card for convenience, and keeping emergency cash in a safe place. Familiarize yourself with currency exchange rates and budgeting tips to manage your expenses effectively while abroad.
8. Cultural and Language Resources
Bring along language guides, dictionaries, or translation apps to help you navigate language barriers and communicate effectively with locals. Research cultural etiquette and customs to show respect and adapt to your new environment with ease.
9. Personal Comfort Items
Don't forget to pack items that bring you comfort and familiarity, such as photos of loved ones, favorite snacks or treats from home, a journal for documenting your experiences, and any hobbies or activities you enjoy (e.g., art supplies, musical instruments, sports gear).
10. Safety and Security
Prioritize your safety by researching local safety tips, registering with your embassy or consulate, sharing your itinerary with family or friends, and staying vigilant in unfamiliar surroundings. Use secure locks for your belongings and avoid carrying valuables unnecessarily.
Final Thoughts
Packing like a pro for your study abroad experience involves thoughtful planning, research, and organization. By considering the essentials outlined above and tailoring your packing list to suit your destination and personal needs, you'll be well-prepared to embark on a memorable and rewarding journey of learning, exploration, and growth. Bon voyage!
0 notes
Text
The Leading 10 Search Engines for Research Papers [2024]

In the contemporary digital research sphere, the accessibility of scholarly materials is redefined by specialized search engines tailored explicitly for research papers. These platforms serve as indispensable tools, granting scholars unrestricted entry to an extensive array of academic information. Among these platforms, Google Scholar stands as a pinnacle, symbolizing the broadening of academic knowledge accessibility and setting the stage for specialized tools in the field.
The transition from conventional library-centric research to digital platforms has brought convenience but also presents a challenge—selecting the most suitable search engines amid a multitude of options. Each platform varies in the quality and relevance of search results, demanding effective navigation of this diverse landscape.
ScholarsEdge introduces an all-encompassing guide to the top 10 search engines for research papers, designed to amplify the efficiency of academic research. These search engines are not only free but also grant swift access to a wide spectrum of scholarly resources, effectively breaking down the barriers of paywalled academic content.
Understanding Academic Search Engines
Comprehending the intricacies of what defines an effective research engine for academics is paramount. Academic search engines, distinct from general ones, offer advanced features such as precise filtering, citation tracking, and complete text access. Their emphasis on academic precision and relevance caters specifically to scholarly content.
The Foremost 10 Search Engines for Research Papers
Google Scholar: A multidisciplinary platform providing extensive access to scholarly literature across disciplines, citation tracking, and seamless integration with academic profiles.
SciSpace by Typeset: Multidisciplinary, specializing in scientific fields, offering advanced filtering, citation data, full-text access, and an AI research assistant.
Semantic Scholar: Strong in computer science and biomedical fields, featuring AI-powered semantic analysis, citation and reference tracking, and comprehensive scholarly articles.
ResearchGate: Focused on science and research, facilitating networking for scientists and researchers, providing access to various academic papers, and tracking impact.
PubMed: Specialized in biomedical and life sciences, granting access to over 30 million citations, with a focus on medical and healthcare literature and links to full-text articles.
IEEE Xplore: Focused on engineering and technology, delivering technical literature in electrical engineering, computer science, and electronics.
JSTOR: Multidisciplinary, particularly strong in arts and humanities, providing access to thousands of academic journals, books, and primary sources.
Scopus: A multidisciplinary platform with an extensive abstract and citation database, offering advanced analytics and tracking tools.
Consensus: Multidisciplinary and AI-focused, offering AI-driven search capabilities for efficient retrieval of academic papers and data.
CORE: An open access multidisciplinary platform featuring millions of open access research papers, promoting open knowledge and accessibility.
This comparison table delineates the unique features and expertise of each academic search engine, providing a snapshot of their offerings. Whether you're seeking the top search engines for research papers, a comprehensive list of reliable academic search engines, or the finest websites for research papers, ScholarsEdge is here to guide you toward the perfect resource for your scholarly pursuits.
1 note
·
View note