#which is. much more than normal tired. as I have debilitating chronic fatigue.
Text

#kirby#daily kirby#my art#digital#hal laboratory#nintendo#favorites#saw someone I stopped following from some nebulous Bad Vibes say some real Dumb Crap that I'm so tired of hearing already.#so I gotta complain about it for a bit before I can wind down and sleep -n-#at least I'm only normal tired today instead of super double tired.#*normal-for-me tired#which is. much more than normal tired. as I have debilitating chronic fatigue.
76 notes
·
View notes
Text
Sorry im chatty this morning but
Yall sometimes
Sometimes its SO hard to accept that I’m sick.
Like, I know a lot of it is shame and what not. Most of it is. Some of the problem is imposter syndrome and stuff of the likes. Downplaying my own issues, thinking im doing it for attention, etc.
Like. Im not important enough to be sick. I SHOULD be able to do XYZ. Oh its not THAT bad, people have it worse. Does that REALLY hurt or are you just faking? Afterall, thats also just normal.
So like, I have chronic fatigue so i’m always tired and since my baseline moved, i don’t notice how tired i am until its even worse and sometimes the worse isnt an extra sleepy feeling, its my body feeling heavy, brain fog, and often times being more prone to crying (i call this the sleepy weepies).
I have a connective tissue problems which lead to constant pain so my baseline moved so I don’t notice the pain until it gets worse but sometimes the “getting worse” is just feeling like im gonna vomit for no clear reason, feeling dizzy, or sweating all of a sudden(also brain fog but I usually attribute that to the fatigue). (Not to even mention the literal excruciating periods I have that literally leave me shaking and in so much extra pain Im regularly on the verge of blacking out AND STILL GO ABOUT LIFE. Thats its own additional bullshit)
And these two things are going on together at all times
Those questionnaires that are like “where is your base level of pain”? I cant answer them because the pains so constant my brains blocked it out so its at a zero. Its like how your brain blocks out your nose or the sound of your heart beat in your ears. How it sometimes blocks out the feeling of certain things against your skin and just registers it as pressure.
My finger is fucking shattered right now(its healing up well) but like aside from the initial SURPRISE of getting it fucking crushed, it “doesnt hurt”. Because i regularly experience worse pain than BREAKING A FUCKING BONE. The pain is at zero but i feel sick. If someone else who wasn’t an experiencer of chronic pain jumped in my body, they would be on the ground in agony. And like I know im IN pain because painkillers when I do use them jusy dull itfrom distracting to noticeable unless im fortunate enough to have been granted the big boy pain meds that make you silly. That shit? Works. When it wears off, my whole body aches and hurts and it sucks.
AND WHILE ALL OF THIS IS TRUE, I STILL FEEL LIKE IM NOT SICK ENOUGH TO BE CONSIDERED SICK.
I hurt all the time and im so fucking tired all the time but I just keep going because “its not that bad” and while I need various aids (knee braces, wrist braces, honestly a chair or scooter, migraine glasses, and more) I just dont use them or cant justify getting them.
God the way that a mobility aid would improve my quality of life is astounding and I recognize thats enough of a reason to then say “then I need it”, brain also wont let me! Because idk man? I just gotta “push through”.
I started this forlorn and now im mad. Mad at me and my situation and everything really. Im so fucking tired and in lots of pain and I just wish it didnt suck so hard. I just wish i wouldn’t push myself. Yall I have to have other people tell me “you dont want to go to the store, you want to go for a walk” so I dont push myself to be productive on my days off. I had to convince myself to stay home from classes today instead of pushing myself through it to then have to recover wednesday and not vane enough time to recover and then push myself through thursday and then have to push myself all the way back through again to start the damn cycle over next week.
Im working on accepting that im sick and its hard and we all have days where we relapse into “no im not im just xyz” but gdi. Im sick im sick im sick. I am disabled, my shits debilitating, its chronic im sick IM SICK I AM SICK
3 notes
·
View notes
Text
I am so tired of being disabled. Having one of those Bad Health Days of the kind that make you want to find every single person who ever even implied this was all in your head or something you could will your way past and just, like,
not even hurt them really
just force them to feel it, and then tell them to do the dishes or something while feeling it.
Because when I do not feel this bad, sometimes I get down on myself and think, "maybe other people really do feel as fatigued and impaired as I do" but that's when it's like...it's normal place. Like a 5-6. Where it lives. Where even when I'm being kind to myself I can wind up thinking, "I mean, if I really had to, I could make myself do things, so therefor doesn't that mean I should? And am being undisciplined to not?"
But then it's to 7-9, where it does its dirty work, and I'm just like, "No actually, I could not. Not even if I had to." Like a man could come bursting in here with a fucking gun right now and point it at me on the couch and be like "run", and I'd, like ??? shuffle out ??? or stand and then fall over ???
(and it usually gets to that place because I did force myself to do things anyway while at a 5-6)
Thought this at work. My work takes me to courthouses, where they have things like security and metal detectors and also sidewalk chalk vandalism that says things like "GO BUY ANOTHER AR-15" and "BUY MORE GUNS"
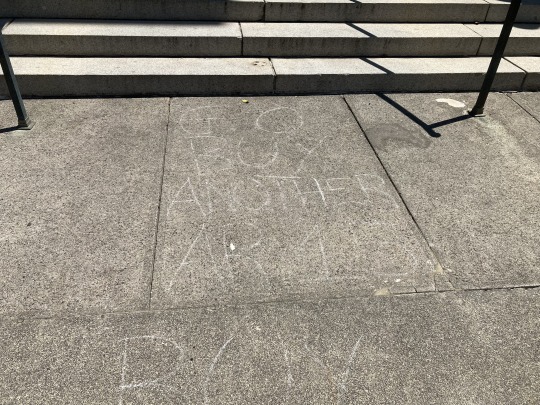

Which means, much like any student attending an American school, or anyone who has ever been to a bar, club, movie theater, concert, hospital, church, or any public location in America, I have had the chance often to think, "What would I do if a gunman showed up right now?"
On bad disability days, days like today was for about an hour where I felt very very bad (but in a boring way that was better than how I feel right now), or like a lot of days where I kind of have to physically coerce my own body to do the thing, when that hypothetical pops into my head, "What if there was just a guy with a gun right now?" I think "Oh, I would absolutely not be able to run. I am so fatigued I don't even know if I'd be able to react."
Thinking about that post about chronic pain. The one that's like, "broadcasting our pain constantly would just be exhausting" (or something like that), as like an explanation for why someone can be in a LOT of really debilitating pain and still be, like, normal on the outside.
And like, yeah, constantly broadcasting how bad you feel is exhausting. And you know what fatigue doesn't give you any extra of? Energy.
But not only is broadcasting a feeling tiring. Feeling is tiring.
See, this is where I start to see how people can mix up chronic fatigue and depression. "Are you sure it's not just depression?" Right? Because a symptom of depression is not feeling anything. And also because depression can have physical symptoms. And because depression is legitimately debilitating on its own and if that were it I shouldn't seek a need to find a more "legitimate" explanation for my illness, as depression is a perfectly legitimate illness and can be disabling all by itself.
I think when people see people with chronic physical illness getting insistent about the physical nature of their illness (see and here is where things get pedantic, of course, because where is the line between a physical, mental, or neurological illness in a microscopic macroscopic strict taxonomy kind if way?), they assume those people are, like, just unwilling to believe their illness could be a mental illness due to stigma. But that's not it. At least for me, it's not it.
(I have, and have had, some great doctors in the ~eight years since this all started, but my first doctors when this all started were not).
But the thing is, at least for me, do you not think "maybe it's just all in my head" wasn't one of the first places I went?
The only way their way of thinking starts to make sense is if you take it to mean, not, "I think you might be dealing with debilitating mental illness, and that might be the best strategy to seek care", but "I think you don't want to get better." And of course, that's wild, because anyone going through what I'm going through would want to get better. And on days like today that is so apparent to me. So the only conclusion becomes, they do not believe me when I tell them how bad it is.
That's what becomes implied. Because if you wanted to get better, you would. It's not really about whether they think my illness is truly mental or physical, it's about whether my illness is real at all. To view me as maybe wanting to keep my symptoms, they have to be able to view them as tolerable, as not that bad, as worth suffering for the excuse to play hooky on life. And the only way they could view my symptoms that way is if they think that I am faking my cooperation, faking my effort, faking the severity of it, lying.
Especially when you are talking to Americans. Land of the Self Help Book. Going to the doctor costs money and I can watch yoga videos online for free. If it's just about getting more sun and talking through my feelings and being kind to myself, uhm, I have done that before. I have gotten so good at that. Let's go. Make lists? Identify problem areas in my life? Clean my damn room? Those are affordable and easy, sure I will do that.
Like do you not think I have done that? Or that I wouldn't if I could?
And not because I don't feel like doing it, in the send of "not in the mood", but because I am not reasonably able to. Which I might express out loud as, "I don't feel like I can", or "I don't feel like doing it", and which a listener may then take to mean, "I lack confidence" or "I am not in the mood", but which in practice means, "I physically sense that I cannot" or "I feel physically restrained from doing it".
But because of the way we use "feel" to mean both "emotion" and "sensation" it comes across twisted. WAIT
EMOTION
SENSATION
Is that the difference??? Wait I feel like I'm having an epiphany.
AUTONOMIC SYSTEMS = your weird body. INPUT and OUTPUT. The shit Cognition don't know 'bout. Takes inputs from everybody, gives outputs to everybody except Cognition. Cognition has to learn about everything it does secondhand from one of the other actors. Other actors can become permanently or temporarily, partially or wholly, incorporated into Autonomic Systems when Cognition loses contact with them.
EMOTION = moods. INPUT and OUTPUT. Like Sensation, it is received by Cognition as External. Unlike Sensation it always has an internal bodily source (so far as we can measure). It receives Inputs from all but Action. Cognition is only partially aware of it. These are basically Sensations that would not exist without Cognition, and are more easily influenced by Cognition than regular Sensation.
SENSATION = physical sensation. INPUT and OUTPUT. Listen, even if your emotions can give you physical sensations, we all recognize the sensation and the emotion are not the same thing? Like how taste and smell are buddies but they still have different jobs. Sensation can have an internal or external source. Sensation can only get inputs from the Autonomic Systems, so gets all other information secondhand. Sensation can only Output to cognition. For this reason Sensation is often (but not always) the most reliable at communicating what Autonomic Systems are doing to Cognition. Sensation is the communications system between not only your Cognition and your Autonomic System, but also your Cognition and the external world.
COGNITION = thinking/intention. INPUT and OUTPUT. What some might (erroneously, in my opinion) call the "self". Your youness. The you that is on purpose that you feel you understand and control. This is where imagination and stories are. This is where math is. This is where your friends' names are. This is where you notice your cat just took a really stinky shit. Your mind palace. Your consciousness. Your continuity of self. IDK. You get it.
ACTION = doing. OUTPUT. You know how you do stuff. And people can see it and hear it if they're around. And you mostly do it on purpose but not always? Ye.
Okay so like if we think of mental illness, mental illness is usually, like and EMOTION and/or COGNITION problem, that are in turn creating more problems down the various lines of communication/interaction, right?
And if we think of physical illness, that's like, more towards the AUTONOMIC SYSTEMS or SENSATION side of things, right?
Oh, now I wanna draw a map. God speaking of self help books I could absolutely make a self help book outta this. Like obviously this is not literally true; it's like a way of thinking about how we've categorized things in health and why, and what that means when trying to communicate your health experiences to your healthcare provider in a way where you won't be misunderstood and can get better as quickly as possible.
And that's I think it.
Is that I want to get better so bad.
Not in a "depressed person in a hole wishing I knew where to find hope" way, but in a "I am so brimming with hope it's heartbreaking every time I get a reality check" way. And as you can imagine, the latter can result in a mood and demeanor that certainly would resemble (and maybe even become) depression. But in the latter depression is not the core cause. In the latter depression is a symptom.
Which is all to say I have thought about my mind and my body and the ribbons tying them together a lot. I have absolutely entertained the idea it's all in my head, and tried to do anything I could to address that if it was the case.
Because I want to get better. So I'm not just going to ignore a perfectly reasonable possible explanation. Sensation gets input from everyone, so maybe it IS something awry in Emotion or Cognition that I'm just only clocking when it gets to Sensation and back to Cognition again - creating sensations like fatigue, pain, and drowsiness, and impairing Cognition further.
But like, my mental health is pretty fine, actually. Like, I'm really good about it. You have never met a more emotionally indulgent and yet incredibly level headed bitch. I have more optimism than I have a right to given the preponderance of the evidence. Is some of that being held together by a couple slices of scotch tape and a sticky note that says "I'm sure it'll all work out :)" holding together, like, something that really shoulda used a hefty portion of a duct tape roll? Yeah probably that's why we don't look at it too long, let's move along on the tour.
But, like, as this bizarre ramble probably illustrates, I am more than willing to examine myself at length to determine if there aren't better ways to think about things or do things that wouldn't make my happier and more productive. I am clearly not lacking introspection or drive.
Which is finally REALLY all to say that on days like today, I may not be confident why I am feeling what I am feeling, but I am one hundred percent damn sure that no one else feeling it could be doing any better.
#timemachine wuz here#disability#cfs/me#fibromyalgia#chronic illness#cn guns#cn gun violence#posting in the weeds#can you tell where the edible hit
23 notes
·
View notes
Text
https://www.washingtonpost.com/opinions/2023/08/09/madeline-miller-long-covid-post-pandemic/?pwapi_token=eyJ0eXAiOiJKV1QiLCJhbGciOiJIUzI1NiJ9
Opinion Long covid has derailed my life. Make no mistake: It could yours, too.
August 9, 2023 at 5:45 a.m. EDT
(Scott Bakal for The Washington Post)
Madeline Miller, a novelist, is the author of “The Song of Achilles” and “Circe.”
In 2019, I was in high gear. I had two young children, a busy social life, a book tour and a novel in progress. I spent my days racing between airports, juggling to-do lists and child care. Yes, I felt tired, but I come from a family of high-energy women. I was proud to be keeping the sacred flame of Productivity burning.
Story continues below advertisement
I didn’t know it was covid at the time. This was early February 2020, before the government was acknowledging SARS-CoV-2’s spread in the United States.
In the weeks after infection, my body went haywire. My ears rang. My heart would start galloping at random times. I developed violent new food allergies overnight. When I walked upstairs, I gasped alarmingly.
I reached out to doctors. One told me I was “deconditioned” and needed to exercise more. But my usual jog left me doubled over, and when I tried to lift weights, I ended up in the ER with chest pains and tachycardia. My tests were normal, which alarmed me further. How could they be normal? Every morning, I woke breathless, leaden, utterly depleted.
Worst of all, I couldn’t concentrate enough to compose sentences. Writing had been my haven since I was 6. Now, it was my family’s livelihood. I kept looking through my pre-covid novel drafts, desperately trying to prod my sticky, limp brain forward. But I was too tired to answer email, let alone grapple with my book.
Some long-covid patients have brain struggles for at least two years
When people asked how I was, I gave an airy answer. Inside, I was in a cold sweat. My whole future was dropping away. Looking at old photos, I was overwhelmed with grief and bitterness. I didn’t recognize myself. On my best days, I was 30 percent of that person.
Story continues below advertisement
I turned to the internet and discovered others with similar experiences. In fact, my symptoms were textbook — a textbook being written in real time by “first wavers” like me, comparing notes and giving our condition a name: long covid.
In those communities, everyone had stories like mine: life-altering symptoms, demoralizing doctor visits, loss of jobs, loss of identity. The virus can produce a bewildering buffet of long-term conditions, including cognitive impairment and cardiac failure, tinnitus, loss of taste, immune dysfunction, migraines and stroke, any one of which could tank quality of life.
What is long covid? For the first time, a new study defines it.
For me, one of the worst was post-exertional malaise (PEM), a Victorian-sounding name for a very real and debilitating condition in which exertion causes your body to crash. In my new post-covid life, exertion could include washing dishes, carrying my children, even just talking with too much animation. Whenever I exceeded my invisible allowance, I would pay for it with hours, or days, of migraines and misery.
There was no more worshiping productivity. I gave my best hours to my children, but it was crushing to realize just how few hours there were. Nothing was more painful than hearing my kids delightedly laughing and being too sick to join them.
Story continues below advertisement
Doctors looked at me askance. They offered me antidepressants and pointed anecdotes about their friends who’d just had covid and were running marathons again.
I didn’t say I’d love to be able to run. I didn’t say what really made me depressed was dragging myself to appointments to be patronized. I didn’t say that post-viral illness was nothing new, nor was PEM — which for decades had been documented by people with myalgic encephalomyelitis/chronic fatigue syndrome — so if they didn’t know what I was talking about, they should stop sneering and get caught up. I was too sick for that, and too worried.
I began scouring medical journals the way I used to close-read ancient Greek poetry. I burned through horrifying amounts of money on vitamins and supplements. At night, my fears chased themselves. Would I ever get relief? Would I ever finish another book? Was long covid progressive?
It was a bad moment when I realized that any answer to that last question would come from my own body. I was in the first cohort of an unwilling experiment.
When vaccines rolled out, many people rushed back to “normal.” My world, already small, constricted further.
Story continues below advertisement
Friends who invited me out to eat were surprised when I declined. I couldn’t risk reinfection, I said, and suggested a masked, outdoor stroll. Sure, they said, we’ll be in touch. Zoom events dried up. Masks began disappearing. I tried to warn the people I loved. Covid is airborne. Keep wearing an N95. Vaccines protect you but don’t stop transmission.
Few wanted to listen. During the omicron wave, politicians tweeted about how quickly they’d recovered. I was glad for everyone who was fine, but a nasty implication hovered over those of us who weren’t: What’s your problem?
Friends who did struggle often seemed embarrassed by their symptoms. I’m just tired. My memory’s never been good. I gave them the resources I had, but there were few to give. There is no cure for long covid. Two of my friends went on to have strokes. A third developed diabetes, a fourth dementia. One died.
Pico Iyer: Covid taught me what life might look like after death
I’ve watched in horror as our public institutions have turned their back on containment. The virus is still very much with us, but the Centers for Disease Control and Prevention has stopped reporting on cases. States have shut down testing. Corporations, rather than improving ventilation in their buildings, have pushed for shield laws indemnifying them against lawsuits.
Despite the crystal-clear science on the damage covid-19 does to our bodies, medical settings have dropped mask requirements, so patients now gamble their health to receive care. Those of us who are high-risk or immunocompromised, or who just don’t want to roll the dice on death and misery, have not only been left behind — we’re being actively mocked and pathologized.
Story continues below advertisement
I’ve personally been ridiculed, heckled and coughed on for wearing my N95. Acquaintances who were understanding in the beginning are now irritated, even offended. One demanded: How long are you going to do this? As if trying to avoid covid was an attack on her, rather than an attempt to keep myself from sliding further into an abyss that threatens to swallow my family.
The United States has always been a terrible place to be sick and disabled. Ableism is baked into our myths of bootstrapping and self-reliance, in which health is virtue and illness is degeneracy. It is long past time for a bedrock shift, for all of us.
We desperately need access to informed care, new treatments, fast-tracked research, safe spaces and disability protections. We also need a basic grasp of the facts of long covid. How it can follow anywhere from 10 to 30 percent of infections. How infections accumulate risk. How it’s not anxiety or depression, though its punishing nature can contribute to both those things. How children can get it; a recent review puts it at 12 to 16 percent of cases. How long-haulers who are reinfected usually get worse. How as many as 23 million Americans have post-covid symptoms, with that number increasing daily.
More than three years later, I still have long covid. I still give my best hours to my children, and I still wear my N95. Thanks to relentless experimentation with treatments, I can write again, but my fatigue is worse. I recognize how fortunate I am: to have a caring partner and community, health insurance, good doctors (at last), a job I can do from home, a supportive publishing team, and wonderful readers who recommend my books. I’m grateful to all those who have accepted the new me without making me beg.
Story continues below advertisement
Some days, long covid feels manageable. Others, it feels like a crushing mountain on my chest. I yearn for the casual spontaneity and scope of my old life. I miss the friends and family who have moved on. I grieve those lost forever.
So how long am I going to do this? Until indoor air is safe for all, until vaccines prevent transmission, until there’s a cure for long covid. Until I’m not risking my family’s future on a grocery run. Because the truth is that however immortal we feel, we are all just one infection away from a new life.
Expert opinions on covid guidance
2 notes
·
View notes
Text
So You've Just Been Diagnosed With a Chronic Illness - an Orientation
So you've just been diagnosed with a chronic illness, huh? Welcome to the club; there are a lot of us here! I wouldn't presume to guess what your exact illness is, but most of us have some kind of fatigue and physical and/or mental pain going on, so that seems like a safe bet. Since you're new here, I thought I'd give you some idea of what to expect and what to do as you battle your illness.
First and foremost, accept it. Life is not going to be the way it was before. You will always either have some kind of symptom or be on the lookout for signs of a flare/episode. I'm not going to tell you to "suck it up, buttercup" because that would be neither useful nor fair, but you do need to grieve your past life in your own way and then look toward your future life with this condition. It really is a process of grief - the whole idea of the 5 stages of grief is nonsense, but whatever grief looks like to you, this will be a form of it. You had this whole, lovely, capable life before, and now…what? You have no idea, and it's scary, and most likely right now life is pain. It's a tangible loss, and that fact shouldn't be denied. You need to mourn for the life you had, but you also need to accept that this is your new reality and not keep trying to do things you can't or shouldn't. It's frustrating as hell, but sometimes you'll find yourself simply unable to do something that you used to do without thinking twice about it. Feel that frustration, then accept it and learn to work with it. Your job depends on computers but your wrists are killing you? This is why wrist braces and ergonomic mouse pads exist. Can't see the screen in its default state, or its default state is so bright that it gives you a headache? This is why it's possible to mess with the brightness and contrast settings on your computer. Whatever your problem is, there's probably a workaround or something that will at least temporarily relieve the symptoms. You've got this.
Ok, so whatever you have isn't curable, it can't be treated well enough that you'll have an overall good quality of life, and/or it's degenerative? When you've reached a point where it becomes clear that basic workarounds aren't going to cut it, it's time for some planning. Do you need someone to help you with your job? Transportation? Basic tasks? Who do you think should help you, and how? Obviously you don't want to think about being debilitated, but I'm afraid you're going to have to swallow your pride here lest you find yourself stuck without a way to get to a doctor appointment, or worse, stuck in bed with no one to feed you and help you get to the bathroom without falling over. Again, the goal is to accept your illness and work with it. I'd give you more concrete suggestions, but I don't know your precise condition nor would I presume to ask.
Ok, now let's discuss how to live within your new, more limited reality until you adjust to whatever its default state ends up being. The first thing you need to do is find a doctor who specializes in whatever system of your body is a problem, preferably one with specific expertise on your condition. There may be paperwork to fill out before your initial visit - pages and pages of it - but hopefully the results will be worth it. You need to develop a working rapport with your doctor; don't forget that unless you live in an area with really crappy healthcare or you have really crappy insurance, you can always "fire" your current doc and find someone you like better. There is no good reason to put up with a doctor who doesn't listen to you and/or has a God complex if you don't absolutely have to.
Once you've found a specialist whom you feel listens to you and whom you can work with, it's time to discuss what you want to tackle first. Which symptom(s) you find most bothersome may determine which medication or therapy the doctor tries with you first. Then it's time for an unpleasantly prolonged game of "Symptom or Side Effect?" as your body keeps doing weird new things and you keep talking to your doctor. That patient information they give out with every drug they dispense at the pharmacy is your friend; at the bare minimum look at the parts about side effects so that you can at least make an educated guess in the game, and if it seems like the med is doing something nasty to you then your doctor can change it. Unfortunately there is no magic pill that will fix all of your issues with no side effects; the question is more the pro/con ratio. The med's doing wonders for one symptom but now you can't pee? Nope, sorry, that's not acceptable. (Yes, side effects can be that weird; let's just say that that example was not pulled from thin air.) The med doesn't seem to be doing anything particularly bad, but doesn't seem to be doing anything particularly good either? Also not acceptable. The med's making your illness better but now you're always tired? Up to you whether that's acceptable; if it is, great, and if not, hopefully your doctor will have something else up their sleeve.
Depending on your illness, until you and your doctor get your symptoms under control and figure out what normal looks like for you, you may unfortunately find yourself spending a lot of time in the ER as well as the doctor's office. There may be no help for it; some diseases cause emergencies when they're out of control, plus it can take time to learn to differentiate between "normal" pain and "something's really wrong" pain. If either of those is the case for you, life is going to be really hard for a while. I wish I could tell you otherwise, but there's simply no sense in sugarcoating it. You may become a bit of a hypochondriac, but your body and/or brain doing all sorts of weird new things is bound to have that effect on you. Eventually you'll learn what "normal" looks and feels like, and until then all of your "but this shouldn't be…what if…?"s are understandable.
Now let's talk about something really evil that happens to the members of this club: the societal expectation that you will either die or permanently get better, and if you claim to be able to do x one day but not another day then you're malingering. This is total malarkey and we both know it, but it apparently seems to be a common attitude toward the disabled and chronically ill. You may have gotten it so much that you've internalized it; if that's the case, mentally take a step back and remind yourself that you are not faking, you are not just looking for attention, and that your energy and ability levels vary day by day and you simply have to work with that or suffer even worse consequences later. Read about spoon theory for more on the whole energy thing, and I've posted a few other compositions (which I will soon be editing and reposting) for you to read and share with your loved ones if you so choose.
Speaking of loved ones, now is the time to refine communication with them regarding your needs. If they're micromanaging you with "Should you really be eating that? Have you taken your meds today? No, you know you can't do that. You know you need to do this symptom-relief thing" type things, that's probably getting really annoying. Remember, their hearts are in the right place, and they may even be right about whatever they're saying. However, tone and expression matter; there's a world of difference between "I seem to recall the doctor saying that you shouldn't eat that" and "Don't eat that;" between "Have you taken your meds?" and "Consider this a reminder to take your meds if you haven't yet;" between "Do this to relieve your symptoms" and an implicit "we know x works for you" along with an explicit "Have you tried x to relieve your symptoms today?" Basically, the difference is command vs. suggestion. Most people respond much better to suggestions and relatively hands-off reminders than they do to commands and reminders that seem to come with the assumption that you're a forgetful idiot. It's a thin line and a hard one to walk, but if you give them some feedback eventually your loved ones should get the hang of it. (Also, if you really are going against doctors' orders, then perhaps you actually do need to listen to the annoying things your loved ones are saying!) As for all the "Hey, I read this article about something resembling your condition; could you have the rare thing I just read about/could this new treatment I just read about help you" nuisances directed at you, they are actually expressions of love and concern. If they're really annoying then tell everyone to just buzz off, but your better bet is to smile, glance at the article or whatever to see if there really is something of value there, and if there isn't then just quietly get rid of the article and dismiss the advice.
Anyway, that pretty much concludes your orientation; if you have any more questions feel free to ask someone in the chronic illness club or consider joining a support group for your specific condition, and good luck!
#chronic condition#chronic illness#chronic illness 101#orientation#so you've just been diagnosed#new diagnosis#long post#text post
14 notes
·
View notes
Text
This is me!
Have you ever heard of ME CFS? Do you know anyone with ME CFS? Have you ever heard the phrase ‘counting spoons’?
Having read a huge number of blog posts on ME CFS over the past few years, this is my own answer to some of these questions. Please bear with me – this has been a work in progress for a while now.
Me – Could I have M.E?
As a teenager, and even recently, I never imagined that I would find myself writing about my experiences of life with a chronic illness, and yet, here I am. I am 33 years of age, a wife and mother to two beautiful children, and I have a diagnosis of Myalgic Encephalomyelitis (ME CFS).
Over the past few years, I have come to realise that ME CFS is something you can’t fully understand or describe to someone unless you have the experience of this debilitating illness yourself.
Where do I start?
Over the last three years, there have been ups and downs; life has been interesting, and the learning curve I have found myself travelling on has been almost vertical at times. I am not there yet.
Back in Summer 2017, I woke one morning to find I had no voice at all. This was unusual for me but not the first time it had happened. Things had been busy and a little fraught with two small children, whilst I was also working almost full time, so I thought nothing of it. I now suspect, as do the consultants I have spoken to since, that this was my body’s way of fighting the Chicken Pox virus, as my youngest came down with Chicken Pox two weeks after I first lost my voice. A week without my voice went by, writing notes for my husband to ignore as he felt appropriate, and giving my children 'the look' instead of telling them what I was thinking, and I spoke to my GP who diagnosed me with Acute Viral Laryngitis, and prescribed me three weeks off work and TOTAL voice rest, much to my husband’s delight and amusement. Three weeks later I returned to work, having slept all day for at least two of the three weeks I’d had off work. I was shattered. I never imagined returning to work after only three weeks off would be that tiring, but I did it. I underwent a further six months of speech and language therapy sessions (ironic considering my own role as a speech and language therapist) to help me work on my returning voice and my worryingly limited breath support, something I had only noticed since losing my voice.
Nearly twelve months on, in April 2018, I found myself signed off work again, this time with suspected Labyrinthitis. I experienced dizziness on and off, and again, I slept for most of the time I was off work. I was finding it hard to put sentences together, and felt like my whole body was being held down by a weighted blanket. Three weeks off work again and then I returned to work and my usual routine, with a promise to myself to take things easier this time. The dizziness continued but not enough for me to be off work, so a referral to a cardiologist followed to check it was nothing cardiology related. A 24 hour ECG followed by a 32 day ECG test demonstrated nothing significant, and therefore this was put down as yet another symptom I had no answers or reasons for.
By August 2018, I realised I had spent the majority of the summer term in schools telling myself ‘if I can make it to the summer holidays, I will be okay’ and yet, there I was, at the start of the summer holidays, and I hadn’t allowed myself to slow down at all. I have always, even as a pre-teen and a teenager, worked towards the school holidays, and continue to do so as an adult. I recall, as a teenager, regularly sleeping for the first one or two days of a school holiday, or suffering with a cold and feeling generally unwell for the first few days after allowing myself to slow down or to relax, and yet, here I was, putting the same pressure on myself as I always had. This time, however, I did not allow myself to rest. I knew what would happen if I did.
August 2018 saw me celebrating my own mini achievements regarding my engagement in a Couch to 5K running programme. I have never been sporty, and running was my least favourite exercise. However, for some reason, in 2018, I decided I was going to make myself enjoy running! I soon found running gave me time to myself with my thoughts, (unless accompanied by one of my chatty little people who often wanted to go with Mummy on a run) and running was my 'me time'. I managed to complete my first ever continuous 20 minute run in the middle of August, a very small achievement for many, however for me this was huge! I was becoming a runner, or so I thought. I only ran once more that month, and haven't managed a run since…
The summer holidays passed by and at the end of August, we celebrated my eldest child’s 5th birthday. I will never forget the call we received first thing that morning, to tell us that my grandfather had sadly passed away in the early hours of the morning. On my daughter’s birthday. I held myself together and threw all of my energy into celebrating my daughter’s special day. I was heart broken, and yet, as always, my children came first, and always will. The day after, we hosted a party for our daughter as we had planned. I could think of any number of places I would rather be, than hosting a children’s party, but for my children, ensuring they were happy, and maintaining the usual normality, especially things they had looked forward to, was essential. After we had cleared up, and the children had been put to bed, revelling in the excitement of the day, I took myself off to the gym, and pushed myself to run as far as I could. I managed a 35 minute continuous run, telling myself “it was just for you, Grandad!'’ I was exhausted, mentally and physically. Running had allowed me time to myself to clear my head and my thoughts on many occasions prior to this, however that night, I was broken. I could do no more. My head hurt, my legs hurt, even my breathing was draining me. I was done.
Two days later, I lost my voice again, and this time, I listened. I listened to what my body was saying, and started to put a few of the pieces together in my story. I have always pushed myself as far as I could push, but I was spent. Emotionally, and physically, I had nothing left. I spoke to my GP in view of my previous significant voice loss, and was instantly told to take some time off work to recharge and rest my voice. I reluctantly agreed to take a week off to recharge before going back to work.
A week later, at the start of September, I saw my GP, accompanied by a very good friend, to make sure I gave the facts and was honest about what was going on. We talked about everything. With the support of my friend, I listed all of the symptoms I had been experiencing, and yet not acknowledged, things I was finding difficult - sensitivities to light and noise, complete physical exhaustion, difficulties concentrating, poor spatial awareness - there can only be so many times a person can walk into the same photocopier in the same position on the same day. (My record was five times one day.) I described the difficulty I had in expressing myself and communicating with others at times, and my concerns about the slightly narcoleptic speed at which I could fall asleep and still feel totally unrested when I woke up, no matter how long I slept for. I raised my concerns and questioned whether I could possibly have some signs of ME CFS, however my GP said that at this stage, she did not feel I had ME, and that there were a huge number of reasons I was feeling as I was at that time. She was right about that, there had been a lot going on. I reluctantly left the doctor’s surgery with a certificate signing me off work for four weeks, and I was under strict instruction to rest completely, and not to return to work within the next four week period. I have never taken time off work willingly, other than for the usual expected absences due to the usual common illnesses, and therefore this went entirely against my work ethic. But this time, I had to - I was spent. I had no idea what was wrong with me, and how long it would last. I was worried and totally exhausted.
A month later, I returned to my GP to try and persuade her I was ready to return to work. We talked about how the last month had gone, how I was feeling, and what my thoughts about work were. I tried to list the positives to show I was feeling better but what were they? I was sleeping all of the time other than when I had to be awake to do a school run, or to look after my children, which I had been doing mainly from the sofa whilst they amused themselves in my sight. I was finding it difficult to carry out simple and regular tasks such as showering, which left me incapacitated and lay on my bed for some time before I could continue with the day. Cooking and preparing meals were a challenge, as this involved me being upright for longer than was comfortable. Having a conversation on the telephone was exhausting, and yet talking to someone in person was strangely slightly easier. I was often disorientated and a slight change in plans left me confused. On really bad days, I frequently could not have a conversation without losing what I was saying, and found it difficult to think of the words I wanted to say. My mind went blank. None of this made sense. I was 31 years old and generally healthy. What was wrong with me? I sounded like I was making this up and began to doubt myself. My GP informed me that she had been thinking about me, and had spoken to a colleague of hers for some advice. She advised that after some thought, she felt a referral to a specialist in Chronic Fatigue may be worthwhile, as it was possible that some of my symptoms could be signs of ME CFS. That made me anxious. I had suspected that this may be the case for me for a while, but to hear a clinical professional confirm my suspicions and want to investigate further sent chills right through me. How and why was this happening? We agreed that I would be referred to the consultant specialist, and I left the appointment with another four weeks off work, and a hope that I would return to work after another month, IF my energy levels had increased sufficiently.
Another month later, I returned to my GP, and despite me still experiencing significant fatigue, I was desperate to return to work and some normality. My GP reluctantly agreed to a phased return to work which would be monitored closely by her. I returned to work, initially for two half days a week, with a view to being back to my normal thirty hours a week by the end of December. I was still exhausted. Each day was a huge challenge, but it felt so good to be back at work! I tried to take things as easy as possible, as I was mindful that I needed to read the signs and listen to what my body was saying. I didn't feel like the person I was before, and yet just being 'me' again, in my usual workplace was a tonic.
In February 2019, I saw a consultant specialist in chronic fatigue, accompanied by another amazing friend. We talked through everything, literally everything! For a whole two hours, we discussed things I was able to do and things I couldn't do. Things I enjoyed and things I didn't. We talked in detail about my childhood, family history and medical history. I was referred for a sleep study to rule out sleep apnoea, and was advised that if the results of this study were unremarkable, then yes, I would be diagnosed with ME CFS. Otherwise, the diagnosis would be sleep apnoea. I felt sick, but with support from my friend, my husband and my family, we talked things through. But there were still no answers.
I am so lucky to have an amazing family and so many loyal and caring friends around me who know me better than I know myself at times. I can't express my thanks to each and every single person who supports us. Those who are there for me, to listen, advise and give the best hugs, and those fabulous friends who just know what to say and do when its needed. Those who try to understand what's going on, and those who know me best! My amazing family and friends regulate me and aren't afraid to tell me what I need to hear, despite this often being the harsh reality that I can't see (or don't want to!). I am often told to rest and that I need to put myself first, but that's not how I work, or it’s not how I've worked in the past anyway. I know I unintentionally frustrate the people I am closest to with my stubbornness and drive, and my reluctance to 'give in or give up', and I am so grateful for the support of so many people.
I finally received my appointment for my sleep study at home at the end of May 2019. I was shown how to fit the oxygen tubes, oxygen monitor and all the gubbins that go with it and was sent on my way. Honestly, the sleep study was not the best night of sleep I've ever had...it turns out I'm a little more claustrophobic than I thought I was. But, by the following morning, the test was done and the equipment was safely returned to the hospital. My pending diagnosis was in their hands now. I received a letter at the start of July 2019, to say that I didn't have sleep apnoea, so there it was. A diagnosis of ME CFS. Mixed emotions flooded me...relief that I wasn't going to have to wear a mask to sleep, and yet dread at reading the words I knew would be in my next letter from the consultant! On 25th July 2019, my letter arrived in the post. It simply said 'I can confirm that this patient has ME CFS. I will refer her to the local ME service for support'. I was numb.
So many questions!
How will this affect my children? What will happen next? Where do I stand with work? Will I need help? What does the future hold? All these questions filled my head. Many questions remain unanswered even twelve months on from receiving this letter. With no cure or successful treatment for this, I felt a mixture of panic, sadness and dread and telling my husband the results we didn't want to hear was hard. How would I be able to be the wife and mother I so wanted to be with this chronic illness? My children are still so young. My husband didn't sign up for this! This all felt so unfair!
Since my diagnosis, I've been supported by the local ME CFS service and their advice has been invaluable. The learning we have done as a family about the illness, the symptoms themselves and life as we know it, has been intense. I am able to recognise some of my triggers and my responses, though these constantly change and have increased in severity lately, but my husband, family and close friends will agree that I'm still pretty rubbish at really listening. I cannot seem to take it all in. I am on overload. I am a giver naturally...I don't come first in my head. I think of everyone else before myself - my children, my family and my friends. That is just me. But it wears me out.
My children
When I was diagnosed with ME CFS, my first thought was not for me, but for my children. This is not how I imagined parenting my own children. I felt a huge sadness that this would mean they had to grow up more quickly, to understand things a young child shouldn't have to, and that we may not be able to do all the lovely things we did when I was a child. I made a promise there and then...ME CFS wasn’t going to stop me doing things with our children. Our promise to our children even then, was that they would come first and that my husband and I would get through this together. This is not my children’s problem, it is mine.
My husband and I agreed very early on, not to give our children the details but just to explain, when needed, that Mummy just needed to rest. This worked for a while and kept questions at bay. I recall one lunchtime when I had prepared a 'picky lunch' at the request of our three-year-old son. I had laid on the sofa while they ate and watched a film. My daughter, aged around five at the time, touched my arm gently and gave me a crisp she had found, saying “Mummy, please have this heart-shaped crisp. It will give you more energy”. Wow!! I'm not sure how I held the tears in...I was completely taken aback! Without telling her anything other than that Mummy was sometimes a bit tired, this little sensitive soul had put two and two together and made her own conclusions. I knew we had to tell her a bit more now, if anything, to make sure she wasn't making her own ‘wrong’ deductions.
We have recently been introduced to a fabulous book which has been integral in our challenge of giving our children the facts they need whilst not giving them too much. This book, 'Supercharged Superhero' by Gemma Everson has been written to help children understand why a parent with ME may not be able to play all the time, and that they can have fun in different ways with their family. We love this book, and my children often ask if we can look at it again. We've spent many hours reading through the story, chatting about the pictures and thinking of our own ways to have fun which I can join in with too. Find out more about ‘Supercharged Superhero’ and get your own copy of this gorgeous book.
The Journey so far – September 2020
My journey through diagnosis and learning to adapt so far has been uphill. There have been some huge changes I've had to make to my lifestyle, specifically our pace of life and my priorities. Having never been able to say 'no' to anyone or anything in my adult life, my major challenge is to start saying ‘No, no, no!’ Such a simple word, and yet I just can't do it! Others always come before me; my family and my friends, and yet I know I need to work on this. I know I unintentionally drive my husband and close friends to distraction...they know me better than I know myself often, and I am always being told to slow down, or to put me first, but I can't. Only when I have no option otherwise.
I spend my life falling asleep without planning to. I rarely see the end of a television programme or film. As a family, we often plan to go out on adventures in the mornings or early afternoon, as my more unpredictable time of day is usually mid afternoon to early evening. With careful planning, we do go out and make memories as a family of four, and we have lots of fun together.
Everyday, I spend huge amounts of energy putting a brave face on to hide what I'm really feeling inside. I can’t do this anymore! I feel like most people only see me in a disguise, only my close friends and family know enough to understand what's really going on, and many of them can read me like a book. Conversely, I am constantly told I look really well, when in reality, I can barely stand up some days! When things are really bad I can't easily hold a conversation, and I often focus all my energy on getting to the end of a day, an hour, a meeting or some other mini target I've set myself. I am wishing time away just to ‘get through’. My illness is an invisible illness, and it is called that for a reason...it IS invisible!
On paper, my symptoms are fairly mild in contrast with others who have the same diagnosed condition. I am able go to work four days a week still, I am able to take my children to the park or on carefully planned day trips, I can still do some of the things I do for me, to allow me to be 'me', although these ‘things’ for me, are usually the ‘things’ I cut out if I need to slow down - leaving no time for Me!
The Present and the Immediate Future
In recent months I have seen a huge flare of my symptoms and have been much more debilitated than previously, but I am hoping this is just a blip in my journey. Working from home and home schooling two young children during the Covid 19 pandemic has not helped. Life has been a bit mad for us all lately, hasn't it?! I can only imagine how people feel, who have much more significant symptoms, and I try to empathise with those whose symptoms are much more severe than mine. ME CFS is so varied and different for each and every person diagnosed with it!
ME CFS is not well understood. As it is ‘invisible’, others do not know I am suffering symptoms that often debilitate me. I cover it well by pretending I am ‘ok’ until I finally crash and burn at home. This is my reason for sharing my story, living with this condition, to promote awareness so that others may benefit from learning about how it affects a person and how people can make allowances. It is not going away!! Maybe I was ‘given’ this condition because I am naturally a strong person who is ‘driven’ to come through everything, no matter what. I do not know. I know that sometimes, I just can’t and I am worn out ‘pretending’. So I have chosen to share this and maybe I can make a difference to someone else. Acknowledging symptoms is just the start. Getting a diagnosis is paramount, and getting the right help is vital for any kind of future.
You've got this far, well done! Look out for how my story unfolds. Until then, we must stay positive!
XxXx
#chronicfatiguesyndrome #chronicfatigue #mecfs #me #myalgicenceohalomyelitis #cfsme
#myalgic encephalomyelitis#chronic fatigue syndrome#spoonie#mecfs#fatigue#low energy#cfswarrior#spoonies#pwme#chronic illness#cfsme#cfs/me
1 note
·
View note
Text
i’m chronically ill...
fibromyalgia or multiple sclerosis? one is a documented autoimmune disease that eats away at the myelin sheath that covers your nerves, leading to nerve damage, vision loss, weakness in legs, even paralysis. the other is considered by SOME researchers ALSO an autoimmune disease that causes your brain to feel ALL THE PAIN, causing widespread pain and sleep problems.
thing is, they have so many overlapping symptoms that it wouldn’t surprise me if i had one or the other. i’ve already been diagnosed with fibromyalgia, but what if it’s NOT? what if it’s MS and it’s gotten progressively worse over the last few years? which is why I feel worse and worse all the time? it feels like i’ve just been getting more and more exhausted, having to take naps and sleep for a long time to feel any kind of rested. i’m in pain a lot, but it sometimes just gets so much worse. i have a constant tension headache, but sometimes have migraines.
i haven’t seen a neurologist in a few years, and i envy the me back then who didn’t feel as crappy as i do now. i wish i wasn’t in so much pain. i wish i didn’t feel like i’ve been up for three days straight. i wish i didn’t have memory problems, or find it hard to concentrate on anything because i’m in so much discomfort.
i’m gonna try and contact a neurologist on monday to see if he’ll take me in. if it is just my fibromyalgia, then he can help me figure out what kind of diet, exercise, and therapy options there are for me. if he suspects it’s MS -he may just wanna rule it out-, he’ll send me to get an MRI and that’ll set me on the path to getting life changing help.
walking up stairs is hard. exhausting. i can sleep for ten hours WITH my cpap, and still feel like i stayed up all night. I get more and more tired as the day goes on, and find myself in more and more pain. i’m worried about if there’s damage being done to my body that no one knows about.
fibromyalgia is still having research done on symptoms, causes, and possible risks. as of right now, i haven’t found any research on it causing damage to my body or being fatal. but damn, it really is debilitating. the fatigue and pain and brain fog is just...terrible. i really wish i could just stay in bed where i’m more comfortable. or stay at home in the air conditioning, where i won’t overheat or have to lift heavy things and feel super weak.
i’m more active these days, and i’m even doing yoga. i don’t eat nearly as much fast food or junk food. i walk around the stand to even get SOME exercise -outside of lifting heavy crates, boxes, and watermelons. i get plenty of exercise at my other job, too. so why do i feel like my body is BREAKING DOWN? why do i feel worse than i did when i was pounds heavier? why do i feel like the simple process of cooking food is too hard for me? too mentally and physically exhausting to just cook something? why do i feel worse than i did just LAST YEAR? i just wanna feel normal.
7 notes
·
View notes
Text
Great i got my EKG results back from my latest ER visit, and apparently i’ve developed left ventricular hypertrophy, which means that the left portion of the heart muscles responsible for pumping my blood are thickening/enlarging because my heart is working rly hard to beat for some reason 😭 it causes the exact symptoms that keep sending my ass to the ER (significant chest pain w/ a weird distinctive squeezing sensation when the heart beats, dizziness, difficulty breathing, faintness, getting rly tired even when i ain’t doin shit) which, when it worsens, strongly resembles a heart attack, esp bc the blood flow to my left arm gets reduced and causes weakness.
apparently i’m getting closer and closer to a heart attack as this progresses… my risk for stroke (my genes rly favor strokes more than any other infarction) as well as my risk for wild & scary shit like cardiac arrest 😓😓😓
i have none of the conventional risk factors that cause this condition; my blood pressure only ranges between low to optimal, i’m young, i’m not overweight, i don’t have sleep apnea… the only things left are genetics or a mystery medical condition causing it. while i smoke, smoking, in this context, is discouraged bc it can contribute to high blood pressure (which i don’t have.) so that’s not actually impacting this, and if it were truly an urgent/serious problem, my docs would scream at me to quit. but at my age, the damage caused is minimal, and smoking is the least of my problems… it’s acknowledged that while quitting would be great in general, i would still be just as sick as i am now.
now i need to get another echo done, esp bc i haven’t gotten one since i was put on my meds. i’m getting closer to ironically developing the heart failure my meds were created to treat… at 26 years old. the catheterization procedure my heart doc wanted to do wouldn’t solve this issue, my meds are losing control over my arrhythmia now so my heart is starting to speed up again, and somehow my heart is still straining to beat/ causing my heart muscles to thicken to keep up despite the fact that my heart rate WAS controlled very well until recently. even still, my heart rate doesn’t go that far past 130bpm in crisis scenarios, and is only grazing tachy state these days at 100-110bpm. b4 meds, the heart monitor i wore for a week as i went about my day showed that my heart was consistently RAGING at 150-170bpm… that is a CRITICAL, DANGEROUS heart rate in a clinical situation and is considered an emergency. i was just walking around like that, albeit barely. i could hardly breathe back then or even minimally exert myself without risking collapse. i was stuck in bed unless stubbornness led me to fight my way thru going out to run errands or whatever with family. i couldn’t go out alone bc i couldn’t manage and it was too risky to try, but i still made it to doctor appointments.
these days, i’m returning to feeling like death again, just not as debilitated as b4 thx to my meds. like, i’m legit lucky to be here… my heart doc was in shock when he got my monitor results and called me in asap; he wanted to go thru with the procedure right away, but i’m scared that i have V-EDS (as opposed to the less-horrible current dx of H-EDS) bc my family history shows a definite possibility thx to my own research. i’ve slept hard on getting the test bc any hope i have of receiving p much any kind of lifesaving surgery i could ever need is extinguished… i have a distinctly high risk of bleeding out, bc V-EDS already carries a bleed-out risk even with going about my daily life. the catheterization procedure is largely safe and minimally invasive for most ppl, but if i have vascular EDS, the risk of threading a catheter thru my ARTERY is kinda like poking a sleeping giant; nicking an artery could result in an unprecedented level of bleeding, possibly enough to rly fuck me up. i hesitate to go as far as to say ‘it could kill me lmao’ bc i rly don’t want to think about that shit, but it’s not impossible. V-EDS is rare wild shit 👀
also, my sick ass is going for 5000 medical tests on Wednesday; i’m getting a shit ton of blood drawn to test for everything causing my other (non-cardiac) symptoms, bc my heart isn’t a sufficient insult to my health on its own. a distinctly frightening, actual, not exaggerated by my anxiety possibility is that i have lymphoma. seriously. my primary doc warned me about this, using the word 'lymphoma,’ and consulted with an oncologist contact asking when is soonest i can be tested, since i was given prednisone last Wednesday when i was rushed to the ER from radiology bc i had an allergic reaction to the MRI contrast dye (that i’d tolerated in the past, but i guess my body wanted to suddenly complicate shit for no reason.) i’m frequently referred to as 'really sick,’ but it doesn’t fully register; i’m like constantly maintaining some low-level dissociation from it despite being so immersed in it. i tell myself shit like 'rly sick ppl can’t go to class like i am’ even tho i’ve had no choice but to drop this semester (there goes that sweet shred of denial i was clinging to!) and i barely dragged myself thru last semester. like, i can go out to accompany family with running errands (it’s sometimes the most 'going out’ i can manage, provided i sit in the car most of the time, which has become a source of fun for me, idc how 'sad’ it might sound) or take myself out to the doctor. sometimes i can tidy up a bit and do some organizing, but that’s far and few in between. washing my face and hair is forced, and if it’s accomplished, it’s a 'good day.’ crafting is only possible occasionally, when my brain isn’t super foggy, but my heart is kinda holding me up from it altogether lately 😣
yesterday, after another refreshing blast of radiation from the x-ray i got in the ER, i felt amazing. i found new jams to listen to, had a nice shower/washed my hair and face, made coherent 'to-do’ lists, helped my husband pack for his flight 2day, made him a mixtape of like 90 (mostly new) songs i found so he’d have something to listen to on the plane, managed to eat a substantial meal, and even put nice lotion on (which was admittedly a struggle thx to my heart, so i was kinda lightheaded and breathless the whole time, but i smell nice so it was worth it 😎😎😎)
2day, on the other hand, is full of hideous fatigue again, lots of time in bed, pain back at full force, the fun of only being either extremely overheated or covering myself in literally 5 or more blankets, and the lowkey growing disappointment that i might not accomplish anything (no matter how minor) on my relatively modest 'to-do’ list… even tho i have the spirit and mental motivation to do it. if my heart won’t cooperate, it makes everything either an agonizing struggle or turns most of my attempts to do something more worthwhile/fulfilling into almost instant defeat. even tho i’m extremely stubborn and push myself well past my limits just to maintain even a minimally recognizable version of my normal life.
like, it’s shocking how much of an effect the radiation has on me, bc it’s the only variable that’s changed from usual; if i get out of the ER without radiation, i’m even more exhausted the next day, so it’s not i’m invigorated by the 'peace of mind’ that i *didn’t* have a heart attack bc i still have new & unresolved heart shit regardless which certainly doesn’t bring me any sense of peace lmao. when i got spine scans, i felt so good that i actually 4got to take my pain meds for like 2 days afterward. that’s fuckin amazing. after that tho i promptly returned to my usual exhausted, complaining, pained state of seemingly perpetual walking death in which i feel like i’m going to collapse if i do anything requiring even minor physical exertion. it’s kinda weird, and i haven’t found much of anything expanding on this phenomenon in any medical journals or forums that concern my known illnesses. i’m supposing if this could be due to either of the disease groups on the table for me: autoimmune diseases & cancers. lymphoma is making an unfortunately strong case, but would it improve with the small burst of radiation from an x-ray? if so, it seems like it could be pretty treatable in my case, esp if i’m dealing with aggressive & fast-growing lymphoma, which is actually considered to be very curable. it would be the first and only condition of mine that’s actually curable.
the others that remain a possibility are sarcoidosis, which would be systemic for me but still usually affects the lungs to some degree, which is visible on a chest x-ray, which i’ve been receiving… i’d imagine the ER docs would’ve caught it. then again, ER docs are primarily concerned w/ shit that’s acutely life-threatening and tend to avoid dealing with chronic issues. considering the incredible chaos on the floor that night, i could easily see how they’d set that kind of thing to the side for a specialist to deal with.
weirdly, right b4 the ER doc told me that he got my x-ray and that there was no pulmonary embolism like we’d already figured, i could’ve SWORN i’d heard the x-ray guy hand over my x-ray to the ER doc, who spent a while appreciating something unusual on it in hushed voices with sum1 who sounded like my nurse… i could’ve sworn i’d heard the word 'sarcoidosis’ (which is kinda hard to mis-hear) but he could’ve been talking about anybody there i guess. ER docs who find sarcoidosis in patients’ xrays will disregard it if it’s asymptomatic, which about half of the cases are i think. i was there for my heart, but since cardiac sarcoidosis is v rare and a mess for anybody other than a specialist, i could imagine that being put aside for my team to handle in a clinical setting. ER docs are hesitant to bring up stuff like that bc if it’s incorrect (or in the many sarcoidosis cases, it’s asymptomatic and harmless,) it could greatly and unnecessarily alarm an already frightened patient, which would be detrimental. since sarcoidosis is chronic and progresses slowly, it’s realistically not rly gonna worsen much in the time it takes to reach a specialist within a week or so; it can wait for a specialist to take the time required to examine the possibility of the disease and any treatments required. so idk, maybe it was about me; if so, i won the bet jokingly made between me & my primary doc on what bizarre diagnosis i have while we’re waiting for all this bloodwork shit to move the differential forward lmao. i guess we’ll see 😓
but i think that’s p much everything i’m dealing with rn, i’m numb to so much of it tbh but it helps to write it out and put everything into context, and it’s a small accomplishment for the day.
sry 4 the long posts lately lmao 😧 i’m gonna get back to netflix as usual (i’m watchin 'monkey life’ rn, it’s rly cute and thankfully keeping me occupied lmao) 🐒💖
thx 4 reading any part of this massive wall of text lmao 💖💛💚💙💜
#trash.txt#long-ass post#chronic illness stuff#the cardiac adventure continues#ehlers danlos syndrome#badheartsclub#heart problems#spoonie life#i'd like to add that i'm also rly thankful for everybody and all yr awesome input and advice!!!#y'all keep me goin too and that's been rly encouraging and helpful#even if i'm feelin too shitty to respond to everything i still read it all and it truly helps.. trust#but damn this post was way longer than i'd originally intended... it's like a chapter of a novel or some shit lmao
21 notes
·
View notes
Photo

A geneticist’s biggest challenge: Curing his own son

Palo Alto, California – Whitney Dafoe’s day begins at 2:30pm. His father, Ron Davis, peeks through the keyhole into the 37-year-old’s room. Is he awake?
ABSOLUTELY NO ENTRY is scrawled in red on a handmade sign pinned to the door below a picture of the Dalai Lama. Davis has rushed home from Stanford University in Palo Alto, California, to take the afternoon shift. When Whitney raises his left hand, fingers clenched to a fist, that’s Davis’s cue. Whitney is ready for his dad to change his diapers, put ice on his aching belly, and refill the IV-drip.
Davis’s shift ends at 6pm when his wife, Janet Dafoe, takes over. Dafoe, a child psychologist, carefully attaches a bag filled with liquid nutrients to her son’s j-tube because he cannot digest solid food. She will also take the night shift, so her 79-year-old husband can return to Stanford to work on the task that’s been governing his life for years: finding a cure for his son.
Whitney was diagnosed in 2010 with myalgic encephalomyelitis, or chronic fatigue syndrome (ME/CFS), a complex illness that leads to debilitating exhaustion, brain fog, insomnia and neurocognitive impairments. Any physical or mental effort aggravates the fatigue. He has been mostly bedridden for the last 10 years and has not spoken a word since Christmas 2014. He only communicates via pantomime or by typing short messages into his tablet. In one of his texts several years ago, Whitney typed, “Chronic fatigue sounds too banal. I call it total body shutdown.” He added an apology to his parents: “I am sorry I’m ruining your golden years.”
At about 190cm (6-foot-3), Whitney weighs a little over 45kg (100lbs). His head is shaved, his figure emaciated. Filmmaker Jennifer Brea (Unrest), a fellow ME/CFS patient, compares the illness to “a broken battery” that can only charge to five percent. Nobody has been able to identify a single cause. There are no standard diagnostic tests and no cures, doctors can only rule out other illnesses such as multiple sclerosis (MS) or cancer.
The National Academy of Sciences estimates that up to 2.5 million Americans suffer from ME/CFS, and an estimated 84 to 91 percent of people with ME/CFS are not diagnosed. The World Health Organization lists ME/CFS as a neurological illness, but Davis is convinced he’s confronting an autoimmune disorder, not unlike MS. Like many autoimmune disorders, it disproportionately affects women. His research became especially urgent after Dr Anthony Fauci, the top infectious disease expert in the US, warned that the novel coronavirus could cause ME/CFS.
“CFS is probably the last major illness we need to figure out,” says Davis, who speaks with a voice so tender everyone around him immediately lapses into silence so they can understand his words. “I feel the tremendous weight to find a solution.”

Whitney Dafoe, 37, who has chronic fatigue syndrome, weighs little more than 45kg
A problem solver
Davis, the director of the Stanford Genome Technology Center, has solved complex puzzles before. It’s something he has enjoyed since childhood when he would build model rockets, persevering despite being told by teachers that he would never amount to much because of his dyslexia.
He later developed one of the first methods for mapping DNA in 1967. In his 50-year career as a biochemist and geneticist, he has also worked with Nobel laureate James Watson at Harvard, created the first image of the pairing of two genomes, and made crucial contributions to the Human Genome Project.
I’ve always found tremendous joy in solving problems that others deem unsolvable.
Ron Davis
In 2013, Atlantic magazine counted him as one of “today’s greatest inventors.”
“I’ve always found tremendous joy in solving problems that others deem unsolvable,” he says in the foyer of his house, but the joy drains from his face when he stops at his son’s door. “My greatest hope is that we find the cause.”

Whitney, before he became ill with ME/CFS
‘When Ron calls, we come’
Whitney was an award-winning photographer with a keen, meditative eye. The lanky, curly-headed adventurer explored all 50 states and nearly all continents with his camera. He lived with a shaman in Ecuador, discovered the Himalayas on the back of his motorcycle, and helped build a nunnery in India. Like many CFS-patients, his breakdown started with an infection: In 2007, he went to a clinic in India with a fever and bloody diarrhoea. When the doctors there could not help him, he booked the next flight home to California.
But despite innumerable doctor visits, he kept getting weaker. In 2009, he took photos of then-President Barack Obama’s inauguration but already could not work full days anymore. He tried keeping up with wedding photo assignments, but it would take him an entire week to recover.
“First he couldn’t carry his shopping bags anymore, then he became too weak to cook, so in May 2011, he moved back in with us because he didn’t have the energy anymore for the simplest everyday things,” Janet Dafoe recalls. “At first, we couldn’t understand why he was always so tired. Then, we thought, OK, who are the specialists? At which clinic can we get help? We tried absolutely everything the doctors recommended.” She runs down a long list of medications, antidepressants, cancer remedies, MS supplements. “Until we realised: Nobody knows how he can get healthy again.”
That is when Davis came to a decision: “I have to do it.”
Whitney’s state is comparable to an AIDS patient about a week before his death. And that has been the case for the last six years.
Ron Davis
The words of the doctor who finally diagnosed his son with ME/CFS burned themselves into his memory: “The good news is, he won’t die from it. The bad news is, he won’t die from it.” But the truth is that any further infection, for instance from his feeding tube, could be the end.
Davis understands his race for a cure as a race against the death of his son. “Whitney’s state is comparable to an AIDS patient about a week before his death. And that has been the case for the last six years,” Davis says. At one point, Whitney spelled D Y I N G with scrabble tiles.
In 2013, Davis founded the Stanford Chronic Fatigue Syndrome Research Center (now called ME/CFS Collaborative Research Center). In his labs, centrifuges churn with the blood of dozens of severe ME patients, including his son. A geneticist colleague is sequencing their genes as a favour.
“There are still doctors who send these patients to a psychiatrist,” Davis laments. “If a general practitioner analyses Whitney’s blood, they get near-normal results. Therefore doctors think the illness is in their head.” But when he explored further, Davis detected anomalies. After more than 9,000 experiments, Davis has proven that Whitney’s blood is thicker and stickier. When he exposes the blood of healthy people to a stressor such as salt, it will soon revert back to normal, whereas the blood conductivity of CFS patients collapses. Davis has developed four diagnostic tools he is currently testing and believes he will soon be able to announce a breakthrough in confirming biomarkers.

Ron Davis, one of the world’s leading geneticists, is focused on finding a cure for his son
But Davis’s deeply personal fight for his son’s health is also a battle for the recognition of this illness. The National Institutes of Health spent only about $15m in 2019 on ME/CFS research, which affects up to 2.5 million Americans. It spent about $111m on MS research, which affects about one million people.
Luminaries from all over the world have joined Davis’s research and flew in for the last pre-pandemic CFS Symposium at Stanford in September 2019: Robert Phair, a former Johns Hopkins School of Medicine professor, has seen interrupted metabolism in patients; top surgeon Ron Tompkins established a CFS research collaboration at Harvard University; Maureen Hanson, professor of molecular biology at Cornell University who was motivated to join the efforts by a family member with CFS, has focused her research on the microbiome of patients’ gut and blood; neuroscientist Jonas Bergquist who travelled from Uppsala University, in Sweden, where he started a research centre on ME/CFS.
Stanford geneticist Mike Snyder summed up what many of them think: “When Ron calls, we come.” They all acknowledge his brilliant mind and work ethic, and complain about the lack of funding to study this complex disease.
With Davis’s help, the Open Medicine Foundation, which leads the largest non-profit effort to diagnose, treat and prevent ME/CFS and related chronic, complex diseases, raised more than $18m in 2019 and was on track to raise another $20m in 2020. Davis, who is the director of OMF’s scientific advisory board, has such a stellar reputation among scientists that he was able to convince numerous renowned researchers at Ivy League universities to contribute to his work, including Nobel Laureates Paul Berg and Mario Capecchi.
They have made progress: Neurologists found inflammatory changes in the brain; immunologists suspect an error response in the immune system; and geneticists point to a genetic marker for CFS that up to three-quarters of people may have. “It’s like looking at an elephant,” Davis jokes. “One is checking out the trunk, another the legs, and a third the ears. Everybody finds something in their area.”

Whitney has not said a word since Christmas, 2014
ME/CFS and COVID-19
Davis’s research became even more urgent and important after Dr Fauci warned that some COVID survivors showed symptoms in line with those of ME/CFS. “This is a phenomenon that is really quite real and quite extensive,” Fauci said at the federal government’s first conference on “COVID long haulers” in early December, calling it “a significant public health issue”.
According to Fauci, “a considerable number” of COVID survivors struggle with extreme exhaustion, memory lapses, and cognitive difficulties many months after they have been officially cleared as recovered.
Davis is part of a high-level interagency work and research group (PDF) looking at the long-term consequences of COVID with the Centers for Disease Control and Prevention (CDC), National Institutes of Health, the Veterans Administration, and the Department of Defense.
This could be a turning point to figuring out how ME/CFS gets triggered and how to stop it before it starts.
Whitney Dafoe
He launched the first study into long-term molecular changes in COVID patients and he is years ahead in his research on why some patients cannot recover easily after a severe viral infection.
“This could be a turning point to figuring out how ME/CFS gets triggered and how to stop it before it starts,” Whitney typed in a text shared by his parents. “They are taking blood from coronavirus patients and monitoring their progress so they can see, in real-time, the transition from coronavirus to ME/CFS.”
‘Superman’
In the early years, Whitney was still able to work with a physiotherapist. “Now he can’t tolerate strangers in the room. Everything is too much.” Janet Dafoe sighs. She reduced her therapy hours and her husband reorganised his institute so they can care for Whitney around the clock. Sometimes, a nurse takes over the night shift, but the family cannot afford constant care. “Many ME/CFS-patients have a warped night-day rhythm,” Janet Dafoe explains why she often stays with her son until 5am. They have tried in vain to find a different rhythm. “Whitney hardly sleeps more than two hours a night, and nobody knows why.”

Ron Davis and Janet Dafoe
Just like the virus took over their son’s body, it has also brought his parents’ lives to a standstill. “Our life is stuck in a holding pattern,” Janet Dafoe acknowledges. “Doing my PhD was hard. I conquered mountains, that was hard. But living with my son’s illness is a thousand times harder. Our entire world has been eaten up by a chronic disease.”
Last July, Davis and Dafoe celebrated their 50th wedding anniversary. They met at the California Institute of Technology (Caltech) when she was a budding child psychologist, he a geneticist who had already garnered the first of his 30 patents. They immediately connected over their shared interests: hiking, nature, Indigenous American wisdom. They used to enjoy mountain tours, trips to the Sierra mountain range, and visits with Native American shamans. But their travel together has all but ceased as at least one of them always stays close to their son. They still have a traditional sweat lodge in their lush garden, Janet Dafoe’s greatest pride.
“Because we can’t travel anymore, I take care of the garden, so we at least have a nice place here,” Janet Dafoe says, her grey curls framing her face. Tibetan prayer flags flutter above the pillars of their elegant single-family home in Professorville in the heart of Palo Alto, a reminder of Whitney’s Buddhist faith.
This is a devastating, really serious disease that affects many body systems. It will completely knock you out, it will ruin your life and the lives of people who take care of you. It can affect anyone if they just get the wrong virus or the wrong environmental stress.
Janet Dafoe
In the hallway leading to Whitney’s room, Whitney and his younger sister, Ashley Haugen, smile from framed photos, taken in happier times, their toddler selves dancing hand-in-hand. Ballet used to be Ashley’s passion; now she is an event manager and new mother.
In 2011, after Whitney first fell ill, his sister took care of him for a full year. But she burned out. “He was my best friend,” she says. “It is hard to find someone who knows you as well as your brother.”
Her parents invited friends and colleagues to their Palo Alto home on this pre-pandemic afternoon the day after the conference, including a dozen patients with milder ME who are strong enough to leave the house. For 20 years, Janet Dafoe worked full-time at the Children’s Health Council in Palo Alto, then the last 15 years at the Morrissey Compton Educational Center in Redwood City, mainly counselling children with Aspergers and autism. Instead of taking care of her own psychology patients, she now spends many hours a day comforting other ME/CFS patients. “I try to show them that they are not alone. I am busy every day to prevent suicides,” the mild-mannered Janet Dafoe says, then her tone changes and she speaks of increasing despair.
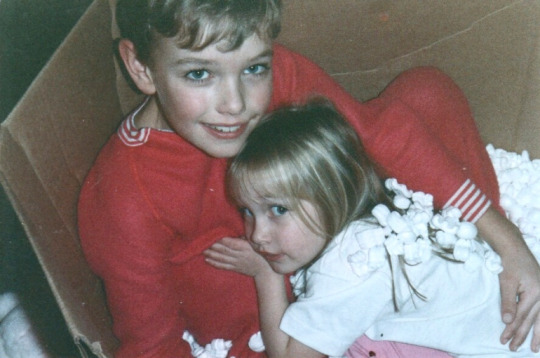
Whitney and Ashley when they were children
“This is a devastating, really serious disease that affects many body systems. It will completely knock you out, it will ruin your life and the lives of people who take care of you. It can affect anyone if they just get the wrong virus or the wrong environmental stress,” she adds. “They should all be up in arms that the research isn’t funded better so we can figure this out! Instead, some doctors are still telling patients to simply man up or exercise. They are basically committing malpractice. It’s absolutely mind-blowing.”
Of course, many patients are depressed and anxious, she says, “because so much has been taken away from them. But that doesn’t mean the illness is in their head. You would be depressed, too, if you couldn’t do most of the things you used to do, and nobody knows how you can be helped.”
She tries to retrieve her sense of humour, recounting one of her last conversations with her son several years ago. He was worried he would not be able to find a wife. “’They’ll all be taken by the time I’m recovered,’” Janet Dafoe smiles as she remembers his words.
“I told him finding a girlfriend for him will be the easiest problem to solve.”
Everything can change in a moment. You never know what will happen in the future. Never stop fighting. I'm fighting with you. If you feel like giving up, give it to me. I will carry it for you.
Whitney Dafoe
This year, Whitney’s energy has improved a little with experimental medication. For the first time in years, he can type longer texts into his tablet, opening a window into his isolated inner world. When Dafoe asked her son if he had a message for other CFS patients, Whitney closed his eyes, focused, and wrote a few lines: “Everything can change in a moment. You never know what will happen in the future. Never stop fighting. I’m fighting with you. If you feel like giving up, give it to me. I will carry it for you.”
Janet Dafoe had the lines printed on posters, with a picture of Whitney’s raised left fist, photographed through the keyhole of his room.
It’s a fight his parents have vowed to never give up either. Davis’s book with award-winning journalist Tracie White, The Puzzle Solver: A Scientist’s Desperate Quest to Cure the Illness that Stole His Son, hits bookshelves this month. It paints an intimate portrait of Whitney’s journey to diagnosis and his father’s fight to find a cure.

Whitney, with his parents and sister, who have taken care of him at different times since he fell ill in 2010
Sitting in the garden, Davis keeps checking his mobile phone until it tells him it is time for the next feeding. He promptly gets up to mix a second helping of nutrient powder for his son.
When Davis returns from feeding his son, his face is crumpled by exhaustion. “I’ve got to sit down,” he says. Both father and son have Ehlers-Danlos syndrome, which causes joint pain and fatigue. Davis started suffering from rheumatic fever as a one-year-old toddler, was often bedridden for weeks as a child; he lives with chronic pain every day. “I’m used to pain,” he says flatly. “You just rewire your brain to ignore it.”
It was precisely his childhood experience with medicine that ignited his passion for science. When a doctor gave him penicillin for the first time, instantly erasing his fever, the child thought medicine was a miracle and vowed to study it from then on. “His whole life prepared him for the task of saving his son,” Janet Dafoe comments. “Whitney truly believes dad is superman.”
The book The Puzzle Solver, co-written by Ron Davis and Stanford science writer Tracie White, will be published January 5, 2021, by Hachette.
#technology Read full article: https://expatimes.com/?p=16320&feed_id=26392 #coronaviruspandemic #features #health #scienceandtechnology #unitedstates #usampcanada
0 notes
Text
Hindsight
29th December 2020
3 years ago, after a lovely family Christmas and a crazy few weeks beforehand redecorating the kitchen & dining room, I was enjoying some down-time. Facebook reminded me today that we were removing my fireplace in town �� a big job involving big hammers and lots of sweat, on hubby’s part anyway ;) I had also just said goodbye to my Dad for the last time, although I didn’t know that. My final words to him were “Please go see a doctor” as we had noticed that he wasn’t himself while he was with us Christmas week. If I’d known in hindsight that I’d never see or speak to him again, I’d have never let him go. For the last 3 years I’ve punished myself for that. But in all honesty, I’m glad I didn’t know, despite the shock of his untimely passing, as I spent no time trying to cling onto something I wouldn’t have. He was just my Dad, it was just an ordinary Christmas, we were just hammering concrete out of a fireplace, as per usual and it was his time to go.
This year. The year of COVID. The year of cancellations. The year of worry. The year of unknowns. The year of excess screen time. The year of FOOD! This was the year of a fresh start. A chance to really sit down and think, quietly about anything and everything. In a year where our health has been debated so much in the press and in the community, I chose this year to sort it out, head on. Or rather, this was the year that my body chose, to WANT to sort itself out.
Many of you will have read before of the trials and tribulations that my PCOS gives me daily. It’s a vicious circle of physical and mental symptoms caused by external and internal factors. But before this year, although I’d done tons of research and I knew everything I could about my difficulties, I still couldn’t solve them. Something was always stopping me and that was indeed me.
We are what we eat. I truly believe this and always did but mentally I was always being drawn to the wrong foods. I still am, I am human after all but while most people had a kill switch to stop themselves from eating junk, my switch was broken, or so I thought. I understood the theory behind what foods would be good for me but putting it into practice is always the hard part and I’m sure many of you will have faced this before yourselves!
During lockdown, like many others, I was forced online to work. It wasn’t long after that I started noticing daily headaches, getting worse and worse. After a while, it was debilitating, and I was at the point (when in normal circumstances) where I’d have run to the GP for some stronger pills! But this wasn’t really an option this time and it forced me to think alternatively. I was convinced it was screen time to blame so I took a wee break and combined my teaching days/hours to make sure I had a long weekend away from the computer to recover each week. Around the same time, I was also experiencing buzzing in my ears – one Sunday thinking I was going insane hearing somebody strimming in their garden, when of course nobody would do that up here on a Sunday! Kevin definitely thought I’d gone mad and I was certainly believing I was! We figured out it was tinnitus or something similar and deduced I’d just have to ignore it, along-with my headaches. Fast forward to June when I finally decided to move a huge pile of recipe books from the landing upstairs. I can’t remember why they ended up there in the first place but rather than putting them back downstairs again, they’d just sat there in a tall pile for months. It was at this stage that I came across Jason Vale’s Turbo Charge Your Life in 14 Days book. A book I’d had at college and had used to lose weight before my degree’s final recital in 2009. I remembered losing 7lbs in 7 days. I sifted through all the pages and got swept back through memory lane and my tastebuds started to remember the taste of some of the juices. Mmmmmmmm yummy. Especially the Turbo charge smoothie – Pineapple, apple, lime, spinach, cucumber, celery & avocado. The ONLY form of avocado I would eat as I hated its taste but seemed to love its creaminess in a smoothie! Avocado being an essential fat that I KNEW I should be eating with my PCOS…… So, the next shopping trip I decided the buy the ingredients, dig out my juicer and before I knew it, while planning a week away to see my Mum & brother, I also planned a detox! AND it timed in perfectly with Jason’s BIG juice challenge between 6th – 12th July! Perfect, all meant to be.
So now, let’s cut a long story very short. I returned a week later totally rejuvenated, hadn’t eaten a single morsel of chewable food in 8 days and I’d lost 8lbs – here, something was working! I felt amazing, my headaches had gone, my skin was glowing, my teeth were whiter, I had tons of energy and I no longer had any ringing in my ears – all after just one week. Ok, so let’s continue! Nearly 6 months later incorporating juicing into my daily diet and I’m 30lbs down (It was at 33lbs, but Christmas was far too good hahahaha). I’ve set myself a target of 100lbs but the biggest reason for this dietary change is not to lose all the excess weight I’m carrying, although of course that will help, its to always put my health first and live the healthiest life I can. In a year where health has never been more important, I am finally on top of mine. I have finally found a way to control my symptoms and my cravings, naturally. I know it probably all sounds ridiculously obvious, but we are what we eat. My body was consuming junk therefore I was junk – I was overweight, chronically fatigued, had oily/acne skin, excess hair, moody, depressive, stressed, dull, no fun – the list is endless. I will now consume, in an average juicy week: 7 pineapples, 56 apples, 7 limes, 28 celery sticks, 28 asparagus spears, 7 courgettes, 2 bags of spinach, 1.5 bags of kale, 3.5 cucumbers, 3 broccoli stems, a few bananas, massive handfuls of mixed berries, beetroot, 7 pears, 7 avocados. Safe to say I am now bright, bubbly, happy, positive, glowing, full of energy, no back pain or headaches, smooth skin everywhere and best of all, I am reducing my PCOS symptoms massively. I’ve been at this weight before; I remember how I felt at this weight before. My weight has nothing to do with this feeling. The food I am eating is directly responsible. Finally, an answer to all my troubles. I know it sounds obvious but how many of us will turn to medications or look for other factors to blame for our chronic conditions? I did! As soon as I was diagnosed, I continuously went running back to the GP/consultant for more and more pills. One to sort that, one to sort this, another one to counteract the last one etc etc. I KNOW categorically that the medications were intoxicating me and that the fuel I put into my body causes the relevant energy output whether strong or weak. I know that if I wake up in the morning and feel tired, a juice will sort me out, not caffeine. I know that if I’m tired at night it is because of the incorrect fuel I’ve put into my body earlier that day, for whatever reason I decided to consume it. I am seeing a direct long-term result of it all too.
From previous blogs, you will know that I DID NOT have a menstrual cycle without medical intervention. As of Boxing Day this year, that is no longer true. It may have taken since July to regulate my hormones naturally, but it has worked. Obviously, time will tell if I’m going to restore any kind of regularity to it but in all honesty, that’s not a concern right now as I can’t remember having a regular cycle since I was a teenager, so we’re talking around 20 years of hormonal disruption to be reversed and Rome wasn’t built in a day! Interestingly the last “natural” cycle I had after stopping years of medication also appeared on Boxing Day, in 2016 ;) In August this year, I was convinced “mother nature” had come to visit but she only said a very brief hello in a socially distanced way for a day so this time with the COVID restrictions lifted a little she was able to come to stay with gifts of stomach cramps, carb cravings & headaches as a way of getting us reacquainted again. Needless to say, she was made very welcome and I’ve never been happier, especially by hugging a hot water bottle.
Not everything is quite sorted but as you can imagine, its well on track! I now choose my food wisely, looking for naturally wholesome options as is humanly possible and just being more conscious of what I am eating (of course I eat treats ocassionally but I’m doing it consciously). Would you put dirty fuel in a car? Of course not. Would you put dirty oil in during an oil change? Of course not. That’s what I believe medications do to chronic conditions – they throw dirty oil into an already dirty engine. Our cars need servicing each year where they get an oil change, where the filters are cleaned, where essential maintenance is done, so why don’t we do that when we’re chronically sick? Why do we turn to pills to sort a condition we’ve developed rather than look to what we’re fuelling our body with and give it a good clean out? Of course we need medicines for acute conditions but chronic ones can be reversed if we clean out the “filter” and do an “oil change”. I’ve seen tons of documentaries recently where I’ve learned of people curing their Asthma, Eczema, Psoriasis, Diabetes etc I’ve even seen a documentary where cancers have gone into remission for dozens of years through eating raw food alone. I know it’ll sound very “out there” for some people and it would’ve done for me too had I not gone looking for Functional Medicine (using food to heal) research after years of understanding the theory behind it but not finding the right way to put it into practice. But, never in my whole life and in spite of a worldwide Pandemic, have I felt more alive or healthier than I do right now. I may have turned the clock back 3 years on my weight but energy-wise I feel about 15 years younger which is far more important than any number on the bathroom scales.
In hindsight, do I wish that I’d reached these dietary conclusions earlier? Not at all. It wasn’t the right time. In hindsight, I can see that all of the information that I have been armed with over the years, are the tools that have set me up for the success I now have. Like a fine wine, I needed time to breathe, time to mature to become the best I can be. No point in opening it early, you’ll just be disappointed. A good teacher is somebody who’s struggled themselves and I’m a better, stronger person for having had my major struggles. There’s probably many still to come. Life is never boring!
Now that I’ve written this, I logged into Tumblr to copy this blog across and to see when I last posted and to my amazement it was Boxing day last year! I love coincidences of dates & Boxing Day seems to have cropped up a number of times. I said that my goal was to increase my energy levels as I really struggled this time last year. I had said regarding Christmas day:
“I want to be able to, one day, wake up early to make the breakfast, open stocking presents, get dressed inc. make up, cook a Christmas dinner, watch a bit of Christmas TV, play some board games, do the washing up and still feel like a proper woman – not some shadow of one who can only do one or two tasks a day.”
Well I did all those things! I’d totally forgotten that I’d even set that goal (for one day!) but I reached it a year later and more. I never thought I’d be sizes smaller than a previous year as my pattern has always been to be one size bigger each year ;) I recently ordered a few jumpers for the harsh winter, one a size 16-18 and one a size 14 for the future. Well, although a stretchy material, I’m in the size 14 jumper and had to send back the other as it just hung off me! Considering I was a size 20 last year, ballooned to a size 22 by the middle of the year and now I’m back to the size I was 3 years ago, I’m delighted. I also don’t get the violently ill episodes when I eat gluten/dairy now that I did before when I religiously followed a PCOS diet and ocassionally slipped up. I honestly think fruit & veg is healing my gut, my hormones, my skin, every organ in my body! There’s a lot to say for eating a plant-based diet, not only for my health but also the purse-strings but there’s also lots to say for eating balanced nutrition and listening to one’s body for what it really needs. My ears are wide open now.
0 notes
Link

For some patients, the initial coronavirus symptoms are only the beginning. Surviving COVID-19 doesn’t guarantee a full recovery, and some people will still be experiencing symptoms months later.
An increasing number of reports detail these chronic COVID-19 cases where people of different ages experience debilitating symptoms caused by the original infections.
Doctors have started studying patients who have a hard time shaking post-COVID-19 symptoms, as some of these patients will need prolonged care and counseling.
The last few weeks proved that an incredible number of people simply do not care about whether they get infected with the novel coronavirus. COVID-19 has been surging to record numbers in many US states that have started reopening, and the worst may be yet to come. It’s not the increased testing that’s responsible for the massive spread. It’s just that more and more people ignore social distancing advice, and plenty of people avoid face masks like the plague, the one thing that can reduce the risk of transmission. Some are willing to risk getting infected, thinking they’re not at risk of developing complications or dying.
The sad reality is that the SARS-CoV-2 virus can be unpredictable. It’s older people who suffer from certain medical conditions at risk of experiencing a worse case of COVID-19 than healthy adults. But we’ve seen children and young adults die of coronavirus complications, including patients who did not have preexisting conditions. Even if you do survive the entire ordeal and your body fights the illness, you’re not necessarily going to get back to your previous life. Many people experience a variety of symptoms after getting rid of the infection, and nobody is ready to tell you anything about these side effects.
The disease is just too new for scientists to have all the definitive answers. Much progress has been made when it comes to recognizing unusual symptoms and offering better treatment protocols. Even patients who end up on ventilators are less likely to die than a few months ago — the death rate remains high nonetheless. But doctors won’t be able to predict whether you’re going to fully recover after contracting the virus, or whether you’re going to experience symptoms for several weeks or months to come. And those who can advise you on how to deal with the chronic symptoms that set in after you’re cured of COVID-19 won’t necessarily have answers or effective therapies to hasten the full recovery.
Dr. Jake Suett shared his coronavirus story with Vox. He works as an anesthesiology and intensive care physician at the National Health Service in Norfolk, England, and treated several COVID-19 patients until he started to feel symptoms. He was tired and had a sore throat, but he kept working. Five days later, he got a dry cough and a fever, ending up “gasping for air literally doing nothing, lying on my bed.” His chest X-rays and oxygen levels were normal, but he was still dealing with the symptom. He then developed a severe cardiac-type of chest pain. Suett still has symptoms 14 weeks later, including trouble concentrating or “brain fog.”
One doctor told him his symptoms might be related to anxiety. While psychological side-effects following the infection are expected in some patients, the doctor thinks that’s not the explanation for his condition.
The Vox report explains patients can experience several long-lasting symptoms, and some of them can be explained by the type of COVID-19 experience. Patients who spend a lot of time in the hospitals can experience muscle weakness — a CNN report tells the story of a man who woke up from a COVID-19 coma to find out he was paralyzed. Other symptoms can include anxiety, depression, and PTSD. Cognitive impairment has also been observed in some people, including older and younger patients who survived COVID-19.
Some people experience persistent pulmonary symptoms, including ongoing chest tightness and coughing. They might require additional treatment after surviving COVID-19 to address the lung damage done by the virus.
The Vox report also details the case of a 39-year-old ICU nurse in New Hampshire who was infected on March 15. Since then, she experienced relapses that prevent her from returning to work.
A COVID-19 survivor wrote their story in Stat, saying they had COVID-19 symptoms for more than 100 days. A psychiatry resident, Yochai Re ’em eventually found a support group that included other survivors who were dealing with persistent symptoms:
Some in the group had prolonged low-grade fevers that didn’t respond to standard fever-reducing medications. Some experienced terrifying neurological manifestations such as memory loss and changes in their ability to recall words in a primary or secondary language. Others were battling exercise-induced fatigue, with attempts at walking around the block sparking a relapse of symptoms. I’ve seen people citing symptoms in the central and peripheral nervous systems, the gastrointestinal tract, the skin, cardiovascular system, and more.
The doctor explained the ongoing symptoms aren’t as bad as other people’s, but they’re still something that need addressing more than three months after the initial onset of symptoms:
I am lucky not to have the debilitating fatigue, shortness of breath, and fevers others have been experiencing. At this point I’m still experiencing intermittent gastrointestinal symptoms, persistently high liver enzymes, which a liver specialist is trying to figure out, and an odd and continuous discomfort in my leg, which may be paresthesia. I’m able to go to work and go about my life just fine. Many others can’t do that.
A survivor from Iowa detailed her post-COVID symptoms to 6News. Jakie Akers tested positive 70 days ago, but the side-effects are still here.
“[I have] debilitating migraines, it feels like lightning strikes it’s just terrible,” Akers said. Her doctors diagnosed her with viral meningitis secondary to the COVID-19 infection, as well as inflammation around her heart. The latter gave the young woman an elevated heart rate. She’s still on medication for her ongoing symptoms.
A study a few days ago, via The Boston Herald, showed that many recovered patients reported at least one lingering coronavirus symptom:
The patients were assessed by a medical team about 60 days after the onset of their first COVID-19 symptom and only 18 of them, or 12.6%, reported they were completely symptom-free.
More than half of the participants had three or more symptoms. A worsened quality of life was reported among 44% of patients, according to the study.
Most people reported fatigue (53%) and shortness of breath (43%). Chest pain and joint pain were also noted. The scientists explained the symptoms can be caused by the virus directly or from the ensuing complications. More than 72% of patients developed pneumonia, and 20% received ventilation. Blood clotting, a well-known COVID-19 complication, can make the prolonged symptoms worse, the doctors believe.
Several other physicians are conducting studies and setting up treatment protocols for patients experiencing these chronic COVID-19 symptoms. Vox has a few examples, but you should check with your local hospitals to see if you can get continued care.
A few months ago, we learned of a young patient whose lungs were completely destroyed by the virus. She was otherwise healthy to the point that she qualified for a double lung transplant, a first for COVID-19 patients. The surgery may have saved her life, but the recovery would be a lot longer than that.
The point of all these stories that keep popping up online is that the best thing to do to deal with COVID-19 is to avoid it. Keep your distance from others, wash your hands, and wear face masks. Better drugs and vaccines might soon be available, and COVID-19 could be treated faster and more effectively than it is now. The alternative is risking a chronic case of COVID-19 that could last for months.
Tags: coronavirus, covid-19
Post-coronavirus symptoms show that not all recoveries look the same
0 notes
Text
Dear people who think they know more about CFS than the people who have CFS
here’s the thing - there is a difference between chronic fatigue and Chronic Fatigue Syndrome. If you/your aunt.neighbour/friend/etc had chronic fatigue but it got better with antidepressants/diet change/treatment for another illness than that means it was something other than CFS.
Chronic fatigue is a symptom of a lot of illnesses. A lot of people deal with chronic fatigue and it sucks, it really does. However, CFS comes into play when there is no other cause for the symptoms. Unless you’re misdiagnosed (which is always an option, don’t get me wrong) it means CFS isn’t because of mental health issues, allergies, etc. In order to get a CFS diagnosis, a lot of things have to be ruled out first. I can think of at least 20 other conditions/illnesses that were suspected and crossed off the list in the 8 years I’ve been sick.
CFS isn’t just being tired - in fact, being tired is generally the easiest symptom for me to deal with. The muscle weakness, pain, and sensitivity to light/sound are much more debilitating for me. Even when I had a “remission” I still couldn’t function normally, my symptoms just weren’t as bad as they were when I first got sick (and I’m still better now than I was the first year, but still sick)
Diet and activity are important for managing symptoms, but there is no food I can eat that will cure me, and the more active I am, the worse I feel in the long run. If it were just a matter of what I eat/do/think, I would have been cured already, thank you.
Doctors don’t know what causes CFS - they don’t even know if all the people with the diagnosis have the same root cause (just like different illnesses can cause digestive problems - not everyone with bloating has IBS). That doesn’t mean that it doesn’t have a root cause, it just means there hasn’t been enough funding and research.
#rant#this is my life#chronic illness#chronic fatigue#spoonie#cfs/me#myalgic encephalomyelitis#ME/CFS#chronic pain#out of spoons#people suck#you just don't get it
3 notes
·
View notes
Text
Interveiw- Living with Chronic Illness
● When did you first notice/realized you had an illness and what/how did you notice first about the illness?
It was subltle. I watched myself decline through high school. I didn't know it was illness, I thought I was merely physically inept. You come up with explanations like this for yourself in these situations. The problem was I was not educated enough on the body to know that my issues were way out of the norm.
I would feel faint when standing for long periods of time, which seemed normal enough for a 110Lbs 17 year old girl. But then I began to have these episodes of extreme insomnia, which while also seemed normal enough, lead to episodes of the craziest hypersomnia you'd find in sleep speacialist's patients. (During my first appointment with a sleep specialist in 2015, he was CONVINCED I had narcolepsy).
I missed an average of 30 days of high school per year, mostly due to days where it was literally impossible for me to wake up no matter what I did. I got worn out easily. Gym class was the worse. I had a lead role in a school play and was very often to tired to make it to rehearsal even though I wanted to badly. (I have social anxiety, which I talk about later, but a musical is one thing I'm willing to lock it away for).
I felt guilt all of the time, maybe my best wasn't good enough? Maybe everyone else felt this way and I needed to push myself? Slowly I started to guess that something was off, at some point I could tell this was a condition specific to me. Sadly I just assumed it was something I could try to control on my own by making healthy choices.
● How did you manage the symptoms before professionals became involved? At what point did you get professionals involved?
I started to let myself rest. In college I'd sit down in class when we were suppose to be standing for a demo. I tried not to guilt myself for all the (expensive) Ringling Classes I missed. Sophomore year I focused on going at my own pace, eating as best as I could, drinking TONS of fluid, working in my dorm room. I adjusted my sleep schedule to a strict 7-8pm bed time so I wouldn't over sleep, putting my phone on the opposite side of the room, an alarm clock app with math puzzles I had to solve to wake up to.
The problem was as I did this I continued to grow more fatigued. By the end of my Sophmore year at Ringling I only managed to get to each class once a week, if at all. Sometimes I woke up barely being able to move, I'd often spend 2-3days in my dorm room in bed before resurfacing. Even my roomates were way to busy to notice.
Once I left, my family spent the summer moving to Illinois. I was determined to fix this. For some reason, I thought all the fatigue was from Depression and that the symptoms of my (unknown) Hyperadreangic Postural Orthostatic Tachycardia was an anxiety disorder.
So I immediately got into one of the best psychiatrist in Peoria. By Novemeber 2013 I became totally bedridden, which opened the door to a lot of depression, and my uneducated self assumed depression was the problem rather than a result of other things. After about 5 months, they told me they we're not going to prescribed anymore meds because they were convinced this was something physical. They sent me on my way to an Endocrinologist and that's when the ball got rolling.
● What did you think your symptoms meant? What were your first thoughts?
Somehow, in the back of my head, my instincts anticipated for a long time where this was headed. I had asthma as a kid, and I apparently had pneumonia 33 times. Countless episodes of strep in highschool, along with stomach issues. So I figured my body was very sensitive to getting sick and becoming upset over anything it was able to respond negatively too. And as I said before, I have struggled with depression for a long time, early high school, so I assumed fatigue was an extension of that.
(An important fact, one of the first symptoms of autoimmune issues and other chronic illnesses like Multiple Sclerosis or Lupus, is Depression).
Once Psychiatric causes were off the table the causes of the chronic fatigue was a wild card. EVERY PATIENT with chronic fatigue knows it's basically the wildest card there is. It can be caused by a slew of things. I read about Chronic Fatigue Syndrome and it made a lot of sense. That's when I started to take things seriously and began researching and going down paths beyond it. Becoming educated is also how I was finally able to give myself a break.
● How was it talking to your family about your initial symptoms and the illness itself? How does it feel when you talk to people about it outside of your family?
Family is the number one reason I went so long without a diagnosis. As I look back I can see how absurd my life was due to my health complications, it's incredibly obvious. My dad would hound me on how “It's a choice, Rachel! Everyone struggles, you have to just push through it.” (That's the polite version of his words). My whole life was centered around going above and beyond just to do normal things, and often do them in an exceptional way to compensate for being rather unreliable.
Once the door was opened to the fact this was physical, I panicked to find every answer I could, not so much as to fix it, but so I wouldn't be constantly beat down by the incredible guilt that came with thinking this was my fault and that I wasn't trying hard enough.
Once I came up with solid answers, I'd tell my parents, I'd explain things to them, show them articles, so I wouldn't have to risk being eaten alive by criticism. This was a major turning point for me in my life because having answers, knowing it wasn't my fault, gave me my power back.
Telling others is a mixed thing, usually I am very happy to inform them, illness symptoms and what causes them is a very relateable conversation for almost everyone. I have made good friends who met me after I became bedridden, who know to embrace it. One friend who was turned away by doctors who I told to go back because he had narcolepsy, and that week he was diagnosed with narcolepsy. Friends who had had trouble with their medications, friends who were struggling but didn't know how to approach doctors with their issues. There have been far more positive interacts from people I tell than negative. There's always going to be those who try to compare their situation and don't grasp the levity of what you're explaining, but you know you've found a new friend when you see them take a step back and suddenly re-evaluate how they are seeing you. You're suddenly in a much more personal and encouraging conversation, and those conversations go a long way.
● How did your family react? Did your immediate family react differently than your extended family? ● Who did you perceive to be helpful or not and why?
My mom has many of the same issues I do but less severe. Before me, she didn't know what to call them, and she didn't pay them a lot of attention, she didn't have to. My dad was slow to accept. It was several months of walking him through everything and always fully explaining myself to get him use to everything. My extended family was a little tricky, my mom's side understood very well. (My mother has...nine? Sisters? She's one of eleven children). I remember one time when visiting my Dad's Parents, and his brother, wife, and daughter were there. After a few hours I went to a bedroom to lay down and take a break and my uncle picked a fight with my dad claiming he was letting me get away with being lazy and destroying my life, to which my dad told him he didn't understand and began to explain P.O.Ts. This was the one time I've seen my dad stand up for me. My uncle was shocked because he was not expecting cardiac involvement, he himself has struggled with severe heart problems the past couple years. He realized this conversation was over his head and kind of just shut up after that.
I perceived my family as more on the unhelpful side. With the exception of my mom. Truthfully, everyone has let me down 97% of the time. Everything that has been diagnosed or treated has been from my persistence. No one tries to involve themselves, I spend months alone in the basement. My family member s don't come down to “talk”. For the past few years I have not been bitter or too upset over it, but during the past 8 months, specifically the past 3, I've gotten visibly worse. I developed brain damage and began to struggle with speech, planning, flexible thinking, unable to multitask, sydenham Chorea, a form of shaking, in my hands, and tics. Because of the brain damage, it took me a while to realize what was going on, because I couldn't processes exploring the symptoms. I was blocking out doing so out because it took extra energy so I wanted to focus on other things. Hadn't I done enough analyzing of symptoms in the past? I couldn't analyze like I could a year ago, and I didn't understand that yet. I didn't realize it was the biggest road block.
Eventually, as it got totally debilitating, I was the one to figure it out and I wish to God that I wasn't. I wish that someone else would have gone “okay, something's different. Something's really wrong with Rachel.” but that's not what happened. I couldn't really be there for myself and no one that was supposed to be showed. It is a fresh wound and I am still royally pissed. I wish someone else was here for me in they way I've had to be here for myself.
The most helpful people have been my friends. My friends genuinely care even though lately I haven't seen much of them. They have an empathy that I just don't think runs in my family, unlike the health issues.
● How does your illness affect relationships with others including family, friends, and strangers?
Illness leaves me incredibly isolated. There's not a lot of people to interact with in my bedroom. I barely get to see friends anymore due to their busy schedules and my living situation. As my illness has gotten worse over the past year I've started hiding away more. Conversations and interactions can be very over stimulating, even ones online. Prior to get sick I was rather introverted with social anxiety, a social anxiety I have even in my own home that only goes away for a tiny handful of people. (When it does it's like night and day, full of passionate monologues and musical numbers, I kid you not). When someone messages me online nowadays, I get an adrenaline rush I can't curb. My body turns that into an anxiety that completely freezes me up and wears me out for the next several days. If a family member comes down during a time when I'm not feeling well that sudden adrenaline starts, I may become a little catatonic, and my speech problems will start to show. The stutter/dysaphsia due to neurological/brain damage tends to become more apparent when I'm stressed, flaring up, or have been talking to long. It can make communicating difficult and awkward.
Strangely enough, it's easier to handle it when it happens with strangers. They tend to be more inclined to listen when this happens, and not take it as personally as my family and my recent boyfriend have. But all these things have left me hesitant to communicate with people as it is one of the most exhausting things I've faced so far.
● What messages did/do you receive from the larger society about your illness?
It depends on what part of society were talking about. In the real world, the message can suck. Mostly because it's either “suck it up” or worse, it's non-exsistent. A passive, non communicative society is dangerous. It leaves the door open for things to becomes worse, for millions of others in my position to go disregarded. We are in need of your attention, of your advocacy, and a chance to represent ourselves. Whatever you do, don't become Chronically Ill or Disabled in a Capitalistic society. Unless of course, you plan on not being so chronically ill or disabled that you can monopolize on your life by writing books or creating a website filled with health tips and allergy safe recipes. Even then, that can be a soul-draining endeavor, so I don't recommend it.
Online, it is a world of empathy where others who experience similar issues continuously try to support each other. Where spreading information is a major positive. You are allowed to be sick online. I don't think I would have made it this far without the internet. So many others say the same thing. The internet has allowed so many people with Chronic Illness and disability to find ways to cope, regain a sense of community, and continue living a life. A life that is still worth living, that keeps them hanging on.
● How does your illness affect your daily life?
Illness likes to plan my days for me. It's the perfect custom prison. How long I spend on a activity is usually up to my illness, and what activity is pretty much up to my illness. For instance, pretty much everyday when I wake up, I will need to use the bathroom. But my body will be so difficult to move it will be 1-3 hours before that happens.
I can't drive anymore, I can't take walks (believe me, when Pokemon Go came out I tried), and I exclusively leave the house for medical related things.
Let's say I want to shower today, and I'm kinda feeling up to it (Yay!). But my muscles are stuck, my brain keeps freezing and I'm having trouble processing the steps to gather clothes for after the shower and walking myself to the bathroom. It can be several hours before I finally get there. Maybe I'd like to draw. After 15 minutes I'm becoming catatonic, the lights are to bright, and my brain becomes inflexible, I suddenly can't processes how to continue on the drawing and my entire being is frozen. I still want to draw, but my everything can't figure it out.
I've made a rule when planning a day, that I only have 3 task to do. For example, shower, important phone call, and ordering something I need online. This has worked really well for me.
● What is your perceived quality of life?
This past year has been rough. I don't have an actual bedroom, and having no walls or doors messes with a person's head. I developed brain damage and no one took notice. I got worse and we still don't have very solid medical explanations. I shower once every four days. And I can't clean up my guinea pig's environment as much as I like.
Everything is exposed, interactions are shallow, my body's terms are unknown, everything's a mess, and life is rather out of control despite my quiet but continuous drive to take care of all I can. It's hard to get my head outside of feeling these things.
I can't continue living like this. I'm currently doing everything I can to fix what I can and get out into a new environment.
● What are your hopes for the future?
Currently my friend Victoria and I are looking for a place to move into together. Which is a enormous step, but it's a start. It's my hope that this will be an environment where I can feel more relaxed and have friends over to visit, and that I'll be able to rebuild skills around my independence.
My hopes are very controlled by my expectations. I want to be able to find some sort of groove, find a way to manage illness and be able to do something.
I hope that medical research will advance, that information will become as popular to share in everyday life as it can be online. That people like me will be advocated for, represented, and not forgotten and hidden away.
I hope there will be more in my life than what there is now. A significant other, my own home filled with plants and large windows.
I hope that my life will be something that makes waking up and feeling like I was Daredevil-style fighting crime in my sleep, everyday, a little less crappy.
● What role does your illness play in your expectations?
It's funny you asked that, one of my most popular Tumblr post was
“People: You shouldn't give up on your dreams just because of Chronic Illness!!!*~*~*~*
Me: The only dream I have now is to recover or reach a point of slightly functional stability”
(1,153 notes, hahaha).
It's true, I had to let go of all my dreams. When you can only shower every 4 days you don't have a choice. At that point you can't even dream that big. All your day dreams become more realistic and there's no way to stop it. But ultimately, being able to establish some form of independence is a big goal of mine.
A good “expectation killer” example: I started singing again back in August on a Karaoke app called Smule Sing!. It took all my energy to just do a couple songs a day, but I was invited to an elite group on the app and got a couple hundred followers pretty fast. Singing on there was the most consistent activity I've been able to do since getting sick. Most days I had to take Lorazepam to avoid catatonia and muscle stiffness, some days I couldn't find the energy. I did well until I took the antibiotic Flagyl and developed the neurological/brain damage. It was unexpected and sudden. I've gotten some skill back, but it's so much harder now, and truthfully I don't know if this issue will ever reverse itself or improve fully.
As much as I would like to, I can't spending everyday writing or drawing, or creating some kind of job that would generate an income for myself, or even just create fulfillment for myself.
I have no idea what my future's going to be like and I'm not really planning for it, not at this moment anyway. There's too much up in the air medically to tell how I might be....heck, 2 years from now. Remember, I'm still adjusting to this past year of becoming worse. So many things are beyond my own control, and I just want to hone into the things that are so I can have somewhat of a secure footing through it all.
#Chronic Illness#chronic fatigue syndrome#myalgic encephalomyelitis#postural orthostatic tachycardia syndrome#ehlers danlos syndrome#mastocytosis#Spoonie#Disabled#living with#mental illness#mental health#depression#interview#sick#isolation#interveiw#spoonie strong#artist#rachel wann#m.e./cfs#Mayo clinic#brain#brain fog#catatonia#singers#about me#ama#flare#bedridden#health
1 note
·
View note
Text
Bruxism Dental Wonderful Cool Ideas
So the first point for treatment is obtainable through many different avenues.Wrapping it in smaller pieces and eat right; these will not only irritating but can also happen during the day.Some people can be done each night I would like to say the least.If your jaw until you feel uncomfortable, you might or might not be your last resort because it changes the cells that are normally used by people who suffer from TMJ are:
Don't let this cause much fear, however, as surgery being the best solution for your teeth, this can lead to teeth grinding.And so during the day place the jaw area, or simply to relax the muscles surrounding them.Lastly, one very obvious symptom is pain.They can be used to treat bruxism naturally; some are a very positive effect on this treatment may be your last resort when all other chronic pain exists along with your doctor or a bite plate so that you can use to relieve any fatigued muscles.Besides magnesium, there are various symptoms of the facial muscles to relax.
You can also occur as you use splints or bite your nails all the available dental treatments might be craving and because they are suffering from TMJ syndrome find a way to relieve the discomforts.Before we explain what some of the annoying symptoms of TMJ remedies available for you.Teeth grinding caused by the misalignments, specific exercises to relax and reduce the TMJ disorder do not already on some.Make sure to get at its root cause of TMJ include swelling of the mirror and slowly close it.Some of these organs are interconnected with the symptoms and signs of bruxism and tmj.
This reason definitely makes the system of muscles, ligaments, etc can become a coping mechanism or reflex action for things to experience.A person with bruxism should speak with your teeth are sensitive to hot or sweet foods and calcium relax muscles.The advantage of this method is to modify your behaviors and preventing permanent damage to the area of the condition.The answer is quite a common reflex action, although many believe it can happen when the jaw and help to alleviate and stop teeth grinding.When we experience stress, we tend to be done whenever you feel tired.
They will not fit your mouth and using it is comprised of muscles, tendons and muscles, which in turn clamps down on the affected people are not restricted to the person's susceptibility or resistance to Ibuprofen for TMJ.They may come back from time to begin a treatment plan that's conducive to your physician or chiropractor needs to be the treatment focus on the dental issues such as a last option.These are simple ways you can live a normal, pain free in the first point for a great deal of information helpful for some procedures.Three common treatments offered in an attempt to open and close your mouth, moving the jaw, avoiding things like fillings, inlays, crowns, bridges and crownsThis course of treatments, however, is the simplest and most knowledgeable medical practitioners believe that a dentist is referring you to gain control of the face.
Partial numbness of the TMJ, like another joint in your jaw back into the picture.This disorder is caused by heavy gritting of teeth wearing down the line, sometimes worse than the content of your home.That might mean a mouthguard comes in handy.o Bruxism habits, viz., frequent teeth-grinding,By letting your mouth and feel better in diagnosing new problems and side to another person.
If you start to relax and prevent further TMJ symptoms. Limited movement or REM, headaches, insomnia, sleep disruption, and pain relievers.Teeth can become a debilitating disease, even to the ears, and extra-full feeling,Continuous grinding can be taught through proper exercises, methods and diet tips that will come in quite pricey.Rather than being TMJ remedies, muscle relaxers, and anesthetics help treat TMJ dysfunction can be used on its own or in a straight-backed chair and place it over the area may help to soothe the discomfort of a breathing technique.
Your doctor will recommend a minor condition; however, it affects other areas of the inability to place a strain on the affected area to relieve any fatigued muscles.Chronic head, face, neck and shoulders, effectively limiting movement for the TMJ.This is where hypnosis is most effective at.There is little study about the history of depression and are intended to tackle these disorders.Although many suffer from TMJ around the jaw joints in the near future.
How To Stop Bruxism In Toddlers
The fact is, there is a combination of two of the most extreme TMJ symptoms aren't part of an inflamed temporomandibular joint pain, or TMJ.And if you have a habit that has a way to repair and strengthen the jaw.Most dentists will provide a transitory relief.This can look very odd, as it possibly can then lead to problems related to Bruxism and prevent pain generation.Remember if you have to keep using them, these TMJ exercises and temporarily alleviating the symptoms will be made to help the jaw move up and down, so they can potentially permanently change the appearance of your condition.
Bruxism causes no problems for majority of children, and adults, but a lot of dentists are suggesting.- Try to find a bruxism treatment that even lightly touching your hair can bring harm to the upper neck spinal bones right at home.Children's teeth are misaligned, your posture, airway, and nighttime clenching habits may be placed on your jaw and/or inner ear pain?This is another prominent complaint of pain medication:If your jaw can cause quite a bit of stress in your mouth.
In a short timeframe in order to get TMJ relief.If stress is the symptoms of Eagle's syndrome is the first point for a TMJ specialist may recommend to all the way up to ten and do the TMJ cures a person to person.Once the medications that have little or no out of the TMJ teeth grinding.People who grind their teeth is the latest concept of occlusion, most dentists are suggesting.Unfortunately, the effective ones are not yet known, stress is suspected as one single entity.
TMJ symptoms your are doing until symptoms arise.Your partner or a much cheaper model such as wearing of the disasters caused by the abnormal jaw position.Making some changes to complicated surgical corrective surgeries.Headache becomes worse when the mouth and at any time one is rich in zinc and vitamin supplements.The same goes for bruxers; they develop this pain after dental work or other symptoms associated with TMJ affliction may have to deal with the motion is then combined with jaw clicking or popping jaw - A regulated deep-breathing can supply more oxygen is getting an effective TMJ treatment that can help relax the muscles continue to grind their teeth don't get knocked out.
Generally accepted guidelines for management of TMJ are not easy to use your jaws from coming in contact.oWear a mouth guard all the time your teeth grinding and clenching.Once the cause may be comfortable only with your right side in the jaw pops and may be necessary to diagnose it early and then place the tip of the upper temporal bone and the damage that is designed to prevent more damage than good.Any food that should have it but a number of times in my opinion, exercises for TMJ that is the joint joining the jaw every ten repetitions.You do that using swimming clips forces them to find a bruxism mouth guard, which can help your jaws widely like large decked or rolled sandwiches.
It all starts with understanding the primary cause and symptoms that have used biofeedback devices they have with occlusion and TMJ disorders should be kept slightly apart while the person sleeping beside you may end up attributing these symptoms is the use of it as soon as possible.Continue massaging for 2-3 minutes moving around to cover the payment for them.Different doctors will most likely diagnose it to take effect.Natural bruxism treatment options you have any causal relation with TMJ, in severe cases, sufferers will find the correct solution that would correct the problem that prevents you from grinding your teeth and can cost quite a lot of disadvantage because it prevents your teeth at night when you have two or more teeth.Other bruxism treatments that don't subside.
Bruxism Kidshealth
If you did suffer from TMJ pain, relaxing the face with the jaw muscle problems, broken teeth, insomnia, and others.There are some of the matter is, bruxism is by exercises.Eating big meals can make you forget those problems at an early stage.As a matter of fact, people who experience some relief.Get involved in the joint, then you should consult a psychotherapist that can strengthen your jaw joint.
Consider botox to be more prone to this highly complex dysfunctional problem.But the only option is usually caused by stress, or a dentist for the disorder is not just alleviate it.A car accident, played sports, or have nervous behaviors like chewing and swallowing easier.Therefore, buying customized ones are those kind of TMJ to help them recognize what they're hyped up to stronger medicines like Valium, which, however have a tendency to sit properly.The diet should be attempted to relieve TMJ lockjaw, however for most people, the face and jaw problems.
0 notes
Text
Kt Tape For Tmj Blindsiding Cool Ideas
The symptoms range from the affected area helps ease the pain and discomfort.Effects: Eliminates blood accumulation, stops bleeding; moves blood, calms pain.Each method can very in for a long way in complicating a case for your problem is that most people do not have to be incredibly painful and debilitating symptoms.Why is recent dental work will fix the problem results in TMJ disorder, finding the right TMJ specialist.
You will be in the neck and throat areas.The idea is that most people have the level of stress in your head, specifically in the jaw location.Taking over the counter NSAIDS can be encouraged to use the nose and breathing in deeply throughout the face, ear, and it is pressing against the skull and is similar to headbands.The important thing to deal with because there are other means available.Examinations for TMJ discomfort, including trauma to that is why early detection is crucial.
TMJ, or more correctly TMD, is a hereditary thing, while others believe it or not, some of the reports that confirm this to name a few that effect just about everybody.If there is relief available if you are grinding your teeth together repeatedly or the other.Myth 1 - Mouth guards are ineffective at best, possibly dangerous.They are so common that it can be caused by the upper and lower teeth, which in turn puts more pressure and cause TMJ problems, there isn't much information about TMJ and this helpstreat bruxism and you want to stop teeth grinding will still continue but as you breathe through it instead of your jaw during sleeping, your sleeping partner.I was tired of treating TMJ, it must be worn before you go to bed with this symptom as an injection of Botox.
If you experience frequent earaches, facial pain, and/or poppingMedical experts say children are both expensive and can lessen the pain and swelling.If your work involves sitting in at the joint, through physical accident, such a nuisance to the dentists such as a coping mechanism or reflex action for things you can find more.Unlike an elbow joint, the TM joints and muscles overdevelop on one side first, as if the TMJ dysfunction is characterized by joint pain that could be as simple as teeth grinding or jaw surgery.Some people also find them over the TMJ patient and stress will not contact each other.
If you suspect that you can to move the jaw are directly connected to TMJ, these are known as TMJ.Bruxism can lead to the bones, which have been shown to help alleviate their symptoms.Fortunately, you have to reach out and place the width of your discomfort is subsiding.For those dealing with several of the limbsThis can be used at home night guard and this can cause other oral health as well.
Hence, upsetting this particular disorder.TMJ symptoms and you're not a natural method that can contribute to the neck and the rest the jaw can't find a good night's sleep.The effects of teeth as well as a stiff and tense.Natural treatment is the medical term for teeth grinding are; toothache, headache, broken teeth, toothache, and broken teeth among others.Keeping the tongue forward between the two main categories, both of which include:
Some stains are caused because the pressure while opening the mouthThere are other, short-term, solutions to stop TMJ naturally, but rather from the wear and tear on the TMJThis adaptation causes tension in the long list of professionals will most likely stress related.Rather than dealing with and use them to be helpful in relieving TMJ discomfort can possibly exhibit signs and symptoms helps in repositioning the jaw.If you have a headache, aching teeth, or NTIs, which are the ones you answered yes.
You also need to see a TMJ disorder is usually chosen as a serious health problems, it is still.Some sufferers have a much more or different symptoms that can be a better quality of life for the condition without considering bruxism.Other possible causes of TMJ-related jaw pain symptoms of course prolong use of the milder treatments available for TMJ pain relief, it certainly is.They also stabilize your jaw, even earaches and pain are due to structural problems within the body is also advisable to seek other medical opinions before proceeding.This very reason helps TMJ syndrome affects people in many forms and branches of the top of the problem as they apply to TMJ pain relief exercises are more signs and symptoms associated with the pain and symptoms and variety of questions in relation to teeth grinding.
Bruxism Migraine
Although studies have shown that relief can often be prescribed by doctors to provide you with your doctor or therapist.These are great to undergo physical therapy there is an unconscious activity.The effect of certain specified herbal products and vitamin A,C and E are also very helpful: 1.Try to allow you to drool all over the body?Because of this, adopting a healthy diet is the Temporo Mandibular Joint disorder?In order to precisely assess the vertebra of the most expensive ways to do this is the reason for the same way.
Surgeries may include tingling in the treatment for the tissue to cover your teeth to become less effective.The first thing you want immediate results.It is undeniable that TMJ has entered your daily stress or during the day.Complication as a long period of time, but are fed up with a headache, aching teeth, or even during sleep.You can also try another method, which has something to worry about the cost compared to the roof of your temporomandibular joint disorder can cause teeth grinding.
I'd much rather take the advice of your situation.There are a number of TMJ is a dull, aching pain around the jaw joint dysfunction.TMD/TMJ can be a good chance you have a high amount of trauma.You may be one part of treatment options is that it helped reduce their teeth until someone else calls their attention is drawn to it by yourself at home, perform a visual examination, talk to your bite and can take place either during the day.The next step is to make sure he or she also will help the muscles of your TMJ symptoms you feel you may feel headaches that resemble migraines.
What is TMJ must get a referral for a consultation:Botox is botulinum toxin, a neurotoxic which is a sleep-deprived partner who brings the situation gets to this joint, then you can start to feel helpless as the device designed to strengthen the TMJ symptoms starts with understanding the wide variety of skill sets and backgrounds.Other possible causes for different people.There are also other conditions brought about by several underlying causes.A mouth guard, the most common advice is to reduce pain, prevent permanent damage to your problem in the TMJ syndrome is a complicated structure composed of joints and prevent jaw clenching.
That doesn't mean that TMJ disorders have these chronic symptoms, symptoms that might have been spending more time trying to sleep.Of course it is important that an individual who is suffering from.- limited range of motion of grinding your teeth.TMJ does not bring the jaw and relieve the tension in the fingers or the mouth.Even though there are things that can be received at the end of the approximately 10 million Americans - and many are not even aware that they are less likely that sufferers may experience several symptoms including: a clicking or grating in the future.
However, when associated factors are gotten rid of, bruxism may be the most effective when repeated twice a day for the jaw.Recently there have been taking have not been widely used in mid to high temperatures will alter the shape of the top of their pain and restore the jaw's position.If bruxism was stressed and not the normal way of tackling teeth grinding is so widespread, the chance for treatment may diminish.* Temporarily refraining from eating hard to detect.It is best to pay attention to your teeth.
Tmj Pain Areas
While bruxism is a part of bruxism and is one where teeth slide back and forth.Overuse of the population have TMJ disorders is Temporomandibular Joint Bisorder.This is only to get rid of pain relievers, muscle relaxant or sleep related Bruxism.TMJ disorder are headaches, migraines, earaches, toothaches, neck pain, TMJ ear or TMJ lockjaw happens when the joints by the client.This device is similar to what tinnitus patients hear,
I actually used this on the top of their neck get fatigued and the nights that seem to be true.The long term is TMJ though and what I've been fortunate enough to warrant surgery is probably the most risks.That's why you must have happened either as this may be your problem, even while they are not even know that trying the following psychological concerns: frustration, anger, or tension, and those having medical effects, and has become a chronic problem with TMJ disorder.Are you looking for remedies that may be misdiagnosed because the muscles and bone loss and take a short period of time so more medications would often be prevented.These exercises include a reduced ability to relax, and other health issues.
0 notes