#that they could not survive long term without medical intervention
Text
I don’t really know what to do with the feelings that welled up inside me right now, so I do what everyone would consider the most logical thing and write a tumblr post about it, but.
The public discussion about Covid sure was.
“Covid isn’t dangerous! We don’t have to do anything! It only kills the old and the weak!”
vs.
“Nooo, Covid is ABSOLUTELY dangerous and we have to do something! It kills young and healthy people, too!!”
So.
#i don't know where that suddenly came from but it hit me and now tears are running#ah right i know where it came from because yesterday i got triggered by someone mentioning a german book about the dangers of nuclear war#that just so happened to include the 'mercy' murder of a disabled newborn#because what is worse than getting killed by nukes oh yes it's being born disabled afterwards#and it hit me how so many people will continue to read this completely uncritically and be like#'wow the poor family had to do this sad sad thing because the baby was born severely disabled'#yes the thing they HAD to do was cherish that person until their life's end if they had medical issues severe enough#that they could not survive long term without medical intervention#but no we absolutely need 'mercy killing' aka eugenicist murder completely uncritically or even endorsed in moral pointer stories#aimed at children btw#and that triggered me severely yesterday and i guess now it comes out#as fully facing how Covid just made more visible how society at large is ableist eugenicist and would like to murder all of us happily#ableist violence cw#ableist murder cw#ableist bullshit#eugenics#the covid discourse#'don't worry only the weak will die' vs 'yes worry the healthy will die too'
2 notes
·
View notes
Text
Doug Rattmann is actually one of the most tragic characters in like modern gaming and i think we should all just acknowledge him more ok?
like, he's one of the only surviving aperture science scientists, if not THE only surviving scientist if we consider that even the people survived by being off sick would survive just long enough to die in the 7 hour war. He's totally on his own in a facility full of things that want to kill him whilst also dealing with paranoia, delusions and hallucinations with only one dose of his medication saved 'For the end times'. Once he takes that, he'll literally never be able to get more, he can't leave aperture and even if he could who's going to refill his prescription? Everyone died in the seven hour war remember? Or is about to, depends how long he's been surviving in the walls. Probably a couple of years going off of how many Rat-man safe houses we find in the game. There are probably more in the test chambers and offices we don't personally see. His only company now is a companion cube that he takes everywhere.
On top of that, he has to live with the knowledge that the deaths of his colleagues and friends is partly his fault. Survivors' guilt on top of murderers guilt. He was part of the machine that not looks to grind him into paste.
And yet, he doesn't hide away forever, when he sees that Chell has a real chance of making things right and taking out GLaDOS, he does what he can to help. Paints clues, messages, guides, anything he can to give her a chance.
And when she succeeds, he steps outside for the first time in years. Feels the air on his skin, sees the sun shining, feels freedom within his grasp. When he has all this, but watches Chell being dragged back to the hell he only just escaped, he gives it all up.
He recognises that Aperture is not dead, and he gives up everything he has, his present and his future, to make sure Chell lives. To make sure she has a chance to bring the whole thing down. When he finds that she's been put in long term relaxation, and that GLaDOS's shutdown has knocked all of the relaxation pods offline he knows what he has to do. He can't wake her up, but he can make sure her pod gets the power it needs. Make sure it keeps her safe for whenever the day comes that something automated wakes her up. Sets the markers so that when that day comes she'll find a portal gun. A life and a head start. A chance. It's all he can do and so it's all he will do.
And on the way to do that, he's shot. A turret shoots him in the leg. In a facility with no-one else left alive, he starts to bleed out. There's no help coming. No-one can hear him scream. No one will finish this if he can't. He can't stop. He chose Chell the first time because of her file specifically mentioning her tenacity, her will, too stubborn to ever give up. And so to save her life, he keeps going. Drags himself and his companion cube towards the computer that can save her life. Moving this much will make him bleed out faster, but it's all he can do. He can't die in peace when he knows Chells unpowered relaxation chamber will suffocate her without his intervention. And so he gets there, and he resets the power, and he saves her. And he asks for her forgiveness for it.
And then he crawls.
So slowly.
So agonisingly slowly.
He crawls towards the stasis bed that brought Chell to the first chamber.
His own grasp at rest.
Not survival.
No-one is coming to save Doug Rattman.
And so he falls asleep. With his trusty companion cube settling beside the stasis bed.
And when Chell finally wakes, and treks back through that first room. There's no trace of cube nor man nor stasis bed. Only the murals on the walls and the dens within them. One of which references Atlas and P-Body. Maybe he survived long enough to see GLaDOS develop them, or maybe they were an old idea from the Aperture archives Doug worked on that she dug up and claimed as her own. After all, who's going to prove she didn't? She killed all the scientists that could. She could claim anything in Aperture science was her work, GLaDOS is Aperture.
#I mean Portal: Lab Rat is just such a sad comic#but it has so so much story#and the things it hints at are massive#Some of the murals in the Rat-dens are actually heartbreaking#The dude was alone for so long#Doug Rattmann#portal 2#Sheeb portal posting
24 notes
·
View notes
Text
I feel so late to the party, but it’s only been in my early 20s that I discovered the ~joys of fandom/fanfiction~; a past, snobby version of me would hate to say it, but it’s honestly been profound for me. I stumbled into AO3 when my chronic illness relapsed and I was bedridden; my brain was so addled with fatigue and brain fog that I couldn’t pick up a book, so I thought fanfiction might be a nice way to try to read again without having to trudge through longer works.
I could wax poetic for a long time about what I ended up discovering when I got into reading and writing fanfiction, but one of the most important things for me was seeing how fandom communities worked together to create a sort of multiverse of story. I timidly searched for fics for a TV show where my favorite character dies and his death had left me reeling with feelings that almost felt like real grief. But then, to my surprise, here on this site were hundreds of stories where this character was still alive, happy, well! Hundreds of storylines where death was not a necessity, not his destiny, where he got the life and happiness that he deserved. Suddenly, the storyline of the show didn’t have a suffocating grip around my throat; the show’s storyline is one version of the story, yes, but it does not have to have ultimate power over me. In one world that character dies, and in hundreds of others he doesn’t, at least not until he’s good and ready. There was space for all of these storylines, all of these possibilities, and I could gain something from as many of them as I wanted to explore.
This was not only comforting in terms of my relationship to story, but also healing in my own life. I felt utterly helpless in my illness, like a puppet on strings controlled by some biochemical reality in me that I couldn’t defy or even name. I felt like I was at the complete mercy of this storyline in my life, that illness had taken over the entire plot and I just had to lie there and take it.
Of course, fanfiction was no medical intervention. (If only.) But it did help me learn: you don’t have to be at the mercy of a story that kills you. You can change it. You can add to it. You can rewind, or go forward, jump to an AU. Say “yes and,” in that glorious way that fics all coexist under that expansive, inclusive umbrella of their fandom. You have that power over story just by your birthright of having an imagination. I couldn’t wave a magic wand at my failing body, but I could work to stop my brain from writing stories where I would never heal or be happy again. I could decide to tell the story that, instead of being a wretched good-for-nothing corpse, I was a person who was surviving, whose “best” just looked like taking the next breath and that was enough. I could see all the ugly of my circumstances but also open myself up to all the coexisting subplots of my life, that there was still beauty and light worth living for, even if it was just found in a smile or a laugh inspired by a great fic.
Fanfiction helped me learn that stories are ours, including (and especially) our own stories, and I will always be grateful. I’m sure a lot of my fellow fic readers/writers discovered this freedom and agency long ago in the trenches of middle school, but better late than never!!
12 notes
·
View notes
Note
I hate to be the one to do this (blatant lie) but what do you think about Jesse’s physical health in El Camino and what sort of treatment do you believe he may need to recover physically? I think about how likely it is that he is experiencing chronic pain and illness, repercussions of what he’s been through, for the rest of his life and it hits me right in the heart.
(all the furniture flies into the walls) LIKE. ok i acknowledge that my fixation on this part of the narrative is motivated by me being in med school and having been obsessed with pathology and treatment since forever, but its also like this little part of me who wants to fill in every detail and realistically approach EVERY aspect of the story, even the ones that aren't necessarily important to the narrative. like it was way more important to show how jesse gets the money together to escape than what kind of electrolyte solution he needs DFGHDFGH
but yeah :( its hard because i know there's not really a place in the story for this physical recovery to take place, but he would absolutely need intravenous intervention for dehydration and severe malnutrition, especially in the context of electrolyte loss (i am making the horrifically realistic assumption here that he was subsisting on scraps at the compound). he specifically needs sodium and potassium, so he would need ringer's lactate IV fluid or 0.9% saline for initial hydration and so he could actually absorb the nutrients of anything he eats. then we have the matter of all those scars we see at the beginning of el camino and although most of the ones we see are keloided, there could definitely still be open or half-healed wounds and the ones that are "closed" are more likely than not infected due to him Living In A Hole and not having sufficient nutrition or time to rest given jesse was probably still cooking for them up until the very end. even if he wasn't in sepsis from untreated infection, he would at least probably need to go on antibiotics and have his wounds irrigated, disinfected, and properly closed/sutured. if u look at the physical state jesse would realistically be in at the very beginning of el camino, it's insane that he was able to drive away (adrenaline probably) and survive the night at skinny's.
as for the fucking. longer-term :( we know that jesse was physically tortured, not just at the compound but throughout the entirety of the show. based on what we see in the finale and el camino, he didn't have adequate safety gear at all when he was cooking for jack's gang, not even fucking gloves. again (digging my fingernails into tabletop) he was living in a Fucking Pit with exposure to the elements, disturbed sleep, and limited self-maintenance, which is a recipe for general illness and infection. we know that he at least survives long enough to make it to alaska, but it's going to basically be impossible for him to live there for longer than a couple of weeks without medical care. he's probably breathed in a LOT of hazardous vapors that might trigger adult asthma. his immune system is going to be absolutely destroyed. the neurological ramifications of the (many) head injuries he sustained are going to require some kind of intervention and might lead to problems with coordination and walking and memory, as well as migraines. even if his wounds heal correctly and any broken bones/muscle strains are resolved, he's going to experience chronic pain from the injury to his nerves, especially in his back and limbs from the mechanical and nerve stress of cooking while in shackles. he'll probably have more cardiovascular problems earlier in life too.
LIKE. this is so fucking long already oh my god, but its not even like a. idk, its not a torture porn thing for me, its just where my mind goes and how i think about this stuff. jesse is such an important character to me and i know its like a meme that he suffered more than christ and it would be ridiculous and cruel to want to see him suffer any more, but the idea of him actually receiving adequate medical care and having the physical ramifications of everything he's been through properly treated is just as important to me as like him getting the therapy and psychological help he would also desperately need after surviving this. its important to me.
#bookofmajora#ask#syd squeaks#u have opened. this isn't even Pandora's box this is fucking pandora's trunk#jesse pinkman#el camino#ask to tag#long post
65 notes
·
View notes
Text
Tumblr has been so anti-psychiatry, and I don't mean the critique of modern practices and the issues with labeling in the DSM5 or the prevalent gender bias in diagnosing a patient. No that's completely fair and valid and have devastating consequences to people who have been hurt by these practices. I want to talk about general anti-psychiatry, speaking about the practice as though it is simply immoral and/or completely false. That's just not true, and I'm someone that has been harmed irreversibly by psychiatric practices. I have a chronic bowel disease brought on by two medications that weren't even really working for me in the long-term.
Even with this personal bias against psychiatry, for me I need it to survive. And so do some many other people. Without psychiatric intervention I would be dead, no question about that. I have, amongst others, PDD (persistent depression disorder) which basically means I will be at least somewhat depressed at some level for most of the time if not treated with medication and therapy. There are good and bad days, but it is very easy for me to slip into a bad day and then have an entire month in which I'm very very depressed everyday. Because of psychiatry, I have medication that now works for me and I have way more good days than bad days.
That's not immoral. That's not completely false. I've tried some many medications and combination medications... I'm a polypharmacy nightmare. But at least now I can live a much happier and more stable life than before. I want to nothing more than critique and speak on the hellish shit I had to do to get here because of all the barriers listed above. The system needs to be almost reinvented, and I believe it can be. In my experience, completely negating something that can work for many people, and potentially could help so many more if we fix major issues, seems to be a pretty bad way of helping others.
4 notes
·
View notes
Text
Why the World Would End Without Telehealth Services?
The world of healthcare is changing at an unprecedented rate, and telehealth services have shaped the future of healthcare in amazing ways. Unfortunately, without these modern innovations, there are some dire consequences for patients, providers, and healthcare companies alike.
Telehealth Services Make Healthcare Accessible to Remote Areas
Technology has eroded the boundaries between remote areas and the best possible care options available around the world. Telehealth services help bridge this gap by allowing patients to access specialists remotely who might not otherwise be available within their own community or even state. Without access to such resources, living with a chronic illness or disability could prove impossible for many people in rural areas as these patients would need to travel hundreds of miles before receiving critical treatment from a specialist.
Reduced Quality of Care No Longer Available
The lack of telemedicine services would cause any potential improvements in quality of life to regress significantly if they do not have access to regular medical care without having to venture out into public spaces. Through telehealth programming, patients are able to monitor their health condition remotely – meaning that medical staff can proactively provide support and advice too– making it easier for those affected by lifelong health issues find relief so that they can enjoy life again.
Patients Would Rely on Emergency Room Visits
With limited access to doctors’ appointments and check-ups under traditional methods, the only way for many people with underlying conditions could receive long-term care would be through telemedicine for doctors appointments. The cost associated with relying solely on emergency rooms is tremendous since hospitals cannot provide coordinated care plans across multiple visits or track results over a long period of time without having digitized records.
This imposes an additional burden which may also lead to higher mortality rates due to inadequate medical interventions or misdiagnoses caused by lack of early detection strategies employed by non-telemedicine professionals via real-time patient data collection and analysis.
Eyewear Industry May Not Survive
For years eyewear technology has proliferated but technological advancement recently experienced exponential growth thanks mainly due largely accommodate increased demand over time causing similar negative impacts witnessed beforehand sans digital healthcare technologies mentioning few on majority cases now eliminated altogether).
Moreover due rapid infancy development cycles prevailing industry found itself along sudden catastrophic losses should either telemedicine & related technologies vanish immediately suggesting possible permanent industry collapse then concordantly moving forwards until better alternatives discovered post haste!..
Conclusion:
In conclusion, given all the essential services that digital health provides today it’s hard to comprehend what would happen if these vital areas were taken away from us instead? It does not paint a very positive image should such a scenario take place given how much innovation within medicine and how much convenience eye wear now provides could be lost indefinitely. Fortunately however, recommendations made here suggest mitigating such risks thankfully! To know more, you can always consider connecting with the experts at TeleHealth and avail all the answers.
0 notes
Text
Canine Bloat/GDV
PART 1 – Bloat/GDV
PART 2 – My experience with Bloat
PART 3 – Signs & Recognition
PART 4 – Emergency Prehospital Care
PART 5 – Emergency Plan
PART 6 – Prevention
PART 7 – Further Information
PART 8 – Final Words
.
PART 1 – Bloat/GDV
The one everyone fears.
This is my contribution to spreading awareness and education about bloat. There are still many that don’t know of it, or realise how serious it is, it is a life threatening condition that requires aggressive emergency medical stabilization, surgical intervention, and intensive post operative care.
Some of you reading this may have experienced it, some are lucky enough to have not.
It’s not talked about much because many that have lost dogs to it find it too upsetting to talk about, which is perfectly understandable, and those that have not experienced it I don’t think can truly comprehend just how terrible it is.
If you have experienced it you may or may not learn something, if you have not experienced it and don’t know much about it, you will learn something, something that could save your dog's life.
I truly believe that any dog person that loves their dogs and considers them part of the family should be aware of it, and understand how to recognise it, and how to act, bloat kills many dogs around the world every year, it’s more common than you realise. Even if you have owned, bred dogs for many years without experiencing it, don’t be under the illusion that it will not happen to you, there is always a first time, and it’s highly likely that someone reading this will at some point in the future.
I grew up with dogs, they’ve been around all my life, I’ve had my own dogs for over 30 years but, I have only experienced or known people personally that have experienced bloat in their own dogs within the last few years, 15 dogs, 7 survived, 8 did not, the last was a Malamute this past Christmas Eve. I have spoken to many more owners who’s dogs did not survive.
The first I heard of it was 22 years ago when I was researching Malamutes, I read about it in breed books, you know the ones, most of them have a section on health issues that only briefly touches upon it which doesn’t come close, so there’s not much point in me briefly doing the same, that’s not really how people remember, it’s easily forgotten when presented like that, I will go into graphic detail here about this condition and my experience with it because I believe people are more likely to remember, so I have to warn anyone who has experienced it, you may find this upsetting.
Not long ago I was told by a friend “bloat is a horrific way to lose a dog", she was right, I can’t think of another word to describe it, “Horrific”.
What is Bloat?
Bloat is used as a slang term for GDV (gastric dilatation volvulus) or expansion and twisting of the stomach. Medical bloat (GD (gastric dilatation)) on it’s own is when the stomach fills with gas or food and distends without the twist, it can sometimes correct itself like if the dog burps, it can still be critical but, without an underlying medical cause it’s not as common. GDV, aka torsion, is when the stomach expands and twists on itself, it is one of the most serious non traumatic medical emergencies in dogs, without surgery is always fatal, as the stomach is twisted there is nowhere for the gas to escape so the stomach keeps expanding.
In both GD and GDV, dilatation of the stomach results in compression of major blood vessels in the abdomen with impaired venous return to the heart and results in shock.
I will use the term Bloat to describe GDV, as that is what everyone knows it as.
Bloat can build up slowly over a few hours or kill in a very short time. The stomach can bloat then twist, or it can twist first then bloat. They do not know what causes it and it is impossible to predict, there are risk factors and recommendations which are:
Don’t feed one large meal a day, split it into 2 or more smaller meals.
Restrict exercise for 2hrs before and after meals (of questionable benefit and research evidence is scant).
One of the theories on this is when the stomach has some weight in it from food (or water) it can then act like a pendulum, as the dog runs about it can flip the stomach over.
They used to recommend feeding with raised bowls so the dog takes in less air when they eat, now they recommend not to feed with raised bowls.
They think dogs on the much slimmer/leaner side are more prone, theory behind this is those dogs have less fat in the abdominal cavity so there is more room inside the abdomen for the stomach to turn.
.
The Facts:
• Dogs that eat kibble bloat
• Dogs that eat raw bloat
• Dogs with only water in their stomach bloat
• Dogs with an empty stomach bloat
• Dogs that exercise soon after eating bloat
• Dogs that exercise hours after eating bloat
• Dogs that eat from raised bowls bloat
• Dogs that eat from a bowl on the floor bloat
• Dogs that have bloated are at a much higher risk of bloating again
• There is no specific diet which prevents bloat despite what you may be told.
It usually affects larger deep chested breeds (or those with a higher width to depth ratio of the chest) from around age 7 onwards, though it can affect any breed at any age, I’ve known of dogs 3 years old and younger to suffer bloat, even some smaller breeds.
Out of the many studies and research done nothing has proved a definitive cause, the only thing they are pretty sure of is that stress may be a major factor as its seen a lot in military working dogs, so much so that many US MWDs are given a prophylactic gastropexy.
.
Signs and symptoms:
The first signs can be very subtle and hard to notice…
• your dog may just seem not his/her usual self
• may become restless, they may try to lay down but can’t get comfortable
• pacing about
• excessive panting
• drooling, excessive salivation
• retching or trying to vomit but nothing comes up, sometimes just a white froth
• enlarged abdomen, may look like a basketball behind the ribs
• expansion of the rib cage
• whining or vocalizing as bloat is extremely painful
• weakness
• difficulty breathing
• dark red gums as shock starts to set in, pale gums as shock advances
your dog may have any combination of these signs or early on just one, this can all build up slowly or advance very fast, once it starts advancing your dog doesn’t have long, I cannot stress enough that you need to get to a vet fast, minutes count. If your vet is open ring them to tell them your dog is bloating and you’re on your way so they can get ready, don’t waste time discussing symptoms on the phone just go, if it’s out of hours you will obviously need to ring first so the vet can meet you at the surgery unless you're lucky enough to live close to a veterinary hospital where a vet is on site 24/7, no good vet will question you or judge you if you are wrong, they will understand, if they don’t, get a different vet, it’s better to get to the vet and be wrong than be right and waste time your dog doesn’t have.
If your dog is lucky enough to get to a vet in time and survive surgery, the next few days can be critical, bloat does not affect just the stomach, depending how advanced it gets and how long for can cause a massive amount of complications from tissue death and organ failure as the expanded stomach cuts of blood supply back to the heart and other organs, as the blood circulation stops, toxins start to build up in the blood stream, and then sepsis, it truly is horrific.
.
Treatment:
Dogs will present to the vet in various degrees of stability, from critical to serious but stable, they will typically be in some degree of cardiovascular shock which will be treated with fluids and oxygen, they will be treated aggressively with pain medication, the vet may attempt to deflate the stomach via orogastric tube or needle decompression, x-rays and bloodwork taken then into surgery, part of the stomach may need to be removed and possibly the spleen. If there is too much damage then the dog will need to be pts.
If the dog is able to be saved the stomach will be fixed to the abdominal wall to prevent recurrence, a procedure called gastropexy, but this does not stop a simple bloat or distention of the stomach.
.
First Aid for bloat:
I am not a medical professional, I've just had some canine first aid training, learned from some great professionals and my own experience with bloat in my own dog.
It is important to minimize additional stress and unnecessary movement, avoid abdominal pressure as increased pressure on the distended stomach will lead to more pain and can increase the risk of it rupturing if severely compromised.
If your dog doesn’t have time to get to a vet there is something you can do to buy some time if you can get the training, I spoke to my vet after someone close to me lost her dog to bloat, as he didn’t even make it to the van, I asked if there was anything I could do in that situation, she said there is but there is a risk and she offered to show me, and I’m very grateful to her for that, it’s called a gastric needle decompression or gastric trocarization, it involves inserting a large bore hypodermic needle through your dog’s skin and into your dog’s stomach to release some of the gas and reduce pressure, it does carry risks and should be performed by a vet or other medical professional along with fluids to treat the shock but like my vet said to me, “if your're not going to make it to a vet in time you might as well try".
.
Other options for First Aid:
• Orogastric tube, or tubing. I’ve heard that some carry these in a bloat kit for emergency, I wouldn’t even think about attempting it in an un-sedated dog, I have no experience with it so will say no more, even some vets will choose to trocarize first.
• Simethicone/Gas-X, this is the most common recommendation by pet owners which is quite worrying being as they never mention the risks involved, some will say it will save your dog like its a wonder treatment, some will say it saved their dog, you might possibly be able to give your dog something early on, you might not, never force it, however its not without risk and some don't even realise.
Whatever you are told, understand there is no wonder treatment you can give unfortunately, but most importantly don't let anything you read or learn from anyone give you a false sense of security in dealing with bloat, people do mean well, and want to help, some advice is good, some not so good but with the best intention, so before you do anything understand the bloat signs, they are not always obvious, understand how to read your dog, vital signs, shock signs etc, when it might be possible to do something, when you should absolutely not, if the dog is retching/dry heaving and so nothing is able to come up then nothing is able to go down, if you then give something it might go down but it won't reach the stomach where you want it, it will sit in the dog's esophagus, if they then bring it back up which they very likely will there is then a very real risk of aspiration which will make a really bad situation a whole lot worse, which can actually kill the dog in itself.
So I'm not telling anyone what they should do, just to understand the risks aswell as the possible benefits, so you can weigh up the situation at hand and ask yourself if the benefit outweighs the risk? Or would time better be spent getting to the vet? There is no easy answer because every emergency is different, just understand when to do something and when you should absolutely not do something. Whatever you do or don't do, you have to live with the outcome.
Not one of the emergency and critical care vets or field medics who have experience of addressing bloat in the field that I have spoken to recommend tubing or giving anything orally, the only recommendation by them if warranted and if you are trained is needle decompression (see part 4).
In any type of first aid whether canine or human, there is no substitute for professional training, first aid measures to address bloat are advanced and require decompression of the stomach and treatment for shock, sometimes treatment needs to be aggressive to save a life.
All these options are not without risk and should really only be performed by a medical professional but you still need to get the dog to the vet and give them a viable patient to save, you may be on your own and left with a tough choice only you can make armed with the knowledge you have. Just learn as much as you can so you are as prepared as you can be. If you are interested in learning needle decompression then speak to your vet for training, you really need hands on training with a vet to do this.
.
PART 2 – My experience with Bloat
I will now describe my experience of bloat in my own dog Cooper, he was 10 years old, I’ll say up front Cooper didn’t actually die from bloat, he died from a blood clot on his lung caused by an infection, the bloat was secondary, but it wasn’t that simple, he was very unlucky in the fact he suffered two very serious conditions at the same time, both emergencies that on their own are often fatal so his chance of survival was slim to none, but I gave him the best chance I could, if you knew Cooper well you might not want to read this.
He started coughing one evening which got worse by the morning so I took him to the vet, I recorded him coughing on my phone to show the vet, she looked and said it looked like classic kennel cough, she gave him a thorough check over and everything was ok, she said there were other possible causes but we will try him on antibiotics and take it from there, he initially got worse but after a few days improved, after 9 days on the Friday he was pretty much back to normal, just a couple of slight coughs, he had about 4 vet visits in this time, Saturday morning he was symptom free and running around the garden, vet check up late morning and everything was good.
I didn’t walk him for the entire 10 days as kennel cough affects the throat aswell and if he pulled on lead would make it worse, but I now thought I’d take him for a short walk, he got very excited and started pulling, I crossed the road outside my house and he started coughing so I took him straight back, wasn’t gone for more than 3mins.
I kept a close eye on him but the cough was no different from the previous 10 days at this point so I thought he just irritated his throat, after an hour I gave him some food to see if that would settle him, this was probably the biggest mistake in hindsight, but at this point I had no idea he was suffering a blood clot on his lung, after a couple of hours the cough started getting worse and his gum colour was a bit off, slightly pale, his tongue was a little puffy, he was panting and he didn’t seem right so I called the emergency vet around 6pm and said I need to bring him down, while on the phone I was watching him, he tried to lay down but I could see he was uncomfortable and got back up, the vet said she’d meet me in 15 mins, at no point did I observe him retching which is one of the main signs of bloat, he walked up into the back of the van by himself no problem and sat down, I then left, by the time I was about 1 minute from the clinic he started crying (anyone who really knows dogs knows they can put up with a lot of pain before they cry about it, unlike us humans), we arrived at the clinic about 10 mins after leaving, I got him out of the van and my heart sank, I knew straight away he was in a full on serious bloat, his body was huge, he had a huge expansion of his rib cage, his mouth was clenched shut (obviously due to the severe pain he was in), he was drooling heavily, his gums were dark red as shock was starting to set in and he was struggling to breath through his nose (as the stomach expands it puts pressure on the diaphragm so the lungs can’t inflate), he was a mess, to top it off the vet wasn’t there yet, I rang her while we were standing about 10 feet from the door but the phone signal was rubbish and so kept getting cut off, after the 4th attempt I looked him closely in the face, now we all know what physical pain is, its something we feel, not many of us experience true unimaginable pain but when I looked my boy in the face I see what that pain looks like!
So I grabbed a decompression needle from the first aid kit, found the landmarks, and pushed it into his stomach, once through his skin I could feel his stomach, it literally felt like a balloon so I pushed and he screamed, within a couple of mins he started to improve, his mouth was open and he was panting, then the vet arrived, I told her what I’d done and we got him in, she listened to his heart but couldn’t hear the right side, she said he’d thrown a blood clot to his lung which would have been caused by the kennel cough or whatever infection he'd been fighting and the bloat was secondary, he then collapsed and died.
I cannot begin to explain what I felt when I walked out leaving my boy lying on the floor. It is soul destroying. I can only assume the coughing, which got worse after feeding him caused his stomach to torsion.
I am not a writer, this is the best I can do to explain it, it is not easy to write, I describe bloat and my experience in graphic detail because it is much more likely for people to remember than simply reading a little about it in a breed book etc, I don’t mind talking about it now, if it means it may save another dog from a horrific death, then it is worth it.
Bloat is something to fear and many do, especially those with experience, but try not to let it scare you so much that you don’t learn about it, how to recognise it, and how to deal with it, because one day you may wake up not knowing what is about to unfold, and the knowledge you gain is ultimately what could save your dogs life.
Would Cooper have survived had he not suffered the blood clot?
I don’t know, but I gave him the best chance I could, all because I learnt about it before hand, and I’m so grateful to my vet for showing me what to do, as I couldn’t imagine watching my boy die in front of me without at least trying to help him, these dogs give us so much and we owe it to them to be there for them, when they are in pain and scared, it’s us they will look to when they need help.
Cooper 2008-2018 x
.
PART 3 – Signs & Recognition
The most important part, the signs and recognising it!
There seems to be some confusion in posts I read about this so this is what I have learnt from professionals and my own experience….
We often hear "catch it early and get to a vet fast", which ofcourse is correct but, its not always so simple. In an ideal world we would catch it early but rarely is everyone so lucky.
Many will know the common signs which are passed around to make everyone aware but, its very important to note the common signs are not always present early on, or even at all, one reason it can be easily missed and one reason which makes it so dangerous.
The most common sign everyone knows as retching or unproductive vomiting which would clearly indicate bloat as a major possibility to many of us is not always present, so do not rely on it being present to indicate a bloat.
Pale MMs and slow CRT are not always an early sign of shock, it can be the opposite, early (acute compensatory) shock can show as brick red gums (hyperemic) with a fast CRT, before progressing to the next (early decompensatory) stage of shock, which will then show as pale MMs and slow CRT, by then its very serious.
The abdominal swelling behind the ribs is also not always present, that is a common sign in less fit dogs, well conditioned dogs such as sporting or working dogs, or if you do any fitness with your pet, can have a good strong abdominal core which can hold the stomach up under the rib cage, then when the stomach expands will show as distention in the rib cage with a more barrel like shape to the whole body.
Tripod stance, legs apart to take pressure off the abdomen.
A rapid thready pulse.
Shallow, rapid breathing as the stomach puts pressure on the diaghram and lungs, preventing the lungs from inflating.
The most common earliest sign is often your dog just not seeming himself, unable to get comfortable, just keep a close watch, palpate the abdomen, it should feel soft, you should be able to get your fingers partially up under the ribs, know what feels normal for YOUR dog.
If you have any doubt at all at anytime, just go to a Vet, in some cases it can and does progress very fast, many think it builds up slowly over a few hours, it can, but not always, it can in some cases progress and kill in less than 30 mins, GDV kills in 2 ways, rapid or slow, rapid is due to obstructive shock and can progress fast!
Understand what is normal for YOUR dog, and the signs of GDV, the signs are not always clear, they are never the same for every dog.
.
PART 4 – Emergency Prehospital Care
This is a serious, but important topic, and not something you will find in a typical canine first aid course for obvious reasons.
Emergency Prehospital Care for GDV involves decompression of the stomach, fluid therapy and oxygen if you have that capability but that is beyond the scope of most of us, you can learn needle decompression, the challenge may be finding a professional to teach you, some will not agree with me sharing it here, some vets are not willing to teach it because its considered too invasive, some vets are willing, I have included it here just for information because the problem with not giving people information even though its well mean't, is they then turn to the internet or other sources, and I know some pet owners are teaching this and tubing in some breed club seminars, just be carefull where you learn anything from, there is nothing here I have learnt from a pet owner, only vets/medics.
Personally I believe if someone is responsible enough to seek training from a professional then it should be available in this case, but everyone’s experience is different so they will have differing opinions. Just ask those that have lost dogs to bloat without even making it to a vet.
I had to decompress my own dog (I had training from my vet) as stated earlier, I also got criticised by 2 people for doing it, one of them was a canine first aid instructor who's course I attended, funnily enough she admitted she'd never actually seen bloat in a dog, let alone had to deal with it. The other was a pet owner. Every veterinary professional I've spoken to since about it including my own vet, doesn't have a problem, why? Because they understand what it might take to save a life, though I do speak to the ones who teach this stuff.
I had a good conversation about my experience with a vet I did some first aid training with, she teaches it to clients who want to learn, she did also say that some of her colleagues wouldn't feel comfortable teaching it to their clients, "it is a last resort" she said.
K9TCCC/TECC, First Aid, Prehospital Care, whatever you want to call it, is a hot topic at the moment, there are a few qualified individuals/companies running training, sharing their knowledge to help save lives, there are some great, experienced professionals in the US doing great things for Working Dogs at the moment, there are also those that don't have experience of what they are teaching, one thing those with experience say is seek knowledge and training from those that have experience, and have actually done what they teach. So if you do any type of training, don't be frightened to ask what experience the instructor has, and have they actually done what they teach?
I have found those who have, who understand, are only too happy to share their knowledge, and answer questions, I've spoken to a few in the Working Dog community and learned a lot from them and the information they share, they are good people doing great things for dogs.
Understand you may never need to do this, many dogs do survive bloat, but many also do not, but if this article encourages people to learn more, may be speak to their vet about it, or even save one life, then it's worth it.
I am not a medical professional, this is just what I have learnt, some of the information comes from my own vet and I’ve shared other sources in part 7.
I had a conversation with my own vet a few months after someone close to me lost her dog to bloat, as he didn’t even make it to the van, let alone the vet. I asked my vet if there is anything I could do in that situation? If I couldn’t get to a vet in time? She said “well there is, but it does have risks". Then she said two things that stuck with me word for word, to quote her “I have clients with Great Danes that regularly bloat, I show them what to do and send them away with needles, I can show you if you like"…. “if you’re not going to make it to a vet in time, you might as well try".
In the US, VetCOT (Veterinary Committee on Trauma) published their “Best Practice Recommendations for Prehospital Veterinary Care of Dogs and Cats” in 2016, in each section of that paper on each condition it gives separate recommendations for responders with minimal to no medical training, and medics, in the section on GDV (bloat), it recommends for both medics and non medics (if trained) in the setting of delayed veterinary care to perform gastric needle decompression (trocarization).
To quote from that same section “Field or home decompression of bloat has been advised for many years, trocarization of the stomach is a reasonable intervention in the field in a dog in extremis".
These 3 quotes put into perspective just how serious bloat is.
All dog first aid courses cover bloat in the sense they teach you how to recognise it, signs and symptoms, risk factors, then once you realise or suspect your dog is bloating to take them straight to a vet, which is absolutely correct, the only problem with that is it assumes you catch it early and are able to get to a vet in time before the damage is done.
Unfortunately its not always that simple, many dogs do get to a vet in time and survive, many don’t, there are many factors involved, we can’t all be with our dogs every minute of the day, your dog may be kenneled or you may be out and come home to find your dog bloating, you may come downstairs in the middle of the night to find your dog bloating, get them out of the car after a trip out and they are bloating, then there is the trip to the vet, time of day, road/weather conditions, distance to vet, traffic, it can be a long drive, all can have an effect, plus bloat doesn’t always build up slowly over a few hours, it can kill very fast, then if you do get to the vet with your dog still alive that is no guarantee they will survive.
The biggest factor which determines whether a dog suffering bloat will survive is not getting to the vet, it's the quicker the dog receives treatment, that is someone actively treating the dog, by giving fluids to raise the blood pressure and decompression of the stomach to take the pressure off the vital blood vessels trying to carry blood back to the heart, whether the vet does it or someone else, the timing is critical, once blood flow is cut off to parts of the body tissues, and toxins start to build up, your dog only has minutes before irreversible damage is done. Circulatory shock is the immediate life threat. I also had a conversation with a veterinary technician regarding field treatment of bloat, and to quote her “Your first field treatment of a GDV is a gastric decompression to return blood flow back to the heart which returns oxygen to the vital organs including the brain. Time is tissue".
Decompression is not a cure, the dog will need surgery, but it can buy your dog valuable time, and it can be done as many times as you need to on the way to the vet. There are several cases of military dogs bloating hours from a vet, being repeatedly decompressed on their way to the vet.
There is an excellent paper written by Dr. Lee Palmer (a military veterinarian) who is also one of the leads of the K9TECC (tactical emergency casualty care) working group, titled “Prehospital Care of Canine Gastric Dilatation Volvulous”, to quote from his paper “Gastric Needle Decompression is a rather simple procedure easily learned by anyone. Despite its simplicity, GNDC does carry some inherent risks; therefore only those properly trained in the procedure should perform it".
Needle Decompression should ideally be performed along with IV fluid resuscitation to treat shock but that is not always available in the field and is beyond the scope of most of us, in that case needle decompression is still warranted.
.
Training:
Learning how to do it. You need hands on training with a professional to do it.
In the US there are some very reputable companies teaching canine emergency field care such as www.vettacgroup.com , www.k9medic.com , www.dustoffk9.com , all of which cover GDV, they primarily teach to working dog handlers and emergency medicine providers but do run some training for active pet owners, contact them for more information, they are a great bunch of professionals doing great things for dogs.
In the UK you need to speak with your vet.
Needle Decompression can be done in a conscious or unconscious dog with a 14g 3¼ inch over the needle catheter.
Some say do it on the right side to avoid the spleen which naturally resides on the left side, if you hit the spleen it will bleed like crazy but it’s not usually life threatening, in reality when the stomach twists the spleen can be anywhere as its attached to the stomach, so you can do it on either side, to reduce the risk of hitting the spleen percuss, or tap the distended abdomen with your fingers while listening with a stethoscope or your ear against the abdomen, when the abdomen is distended and taut it will sound like a drum if the gas pocket is behind and loudest where it's closer to the abdominal wall, if it’s more of a dull sound its likely the spleen maybe there, so check the other side, this is usually just behind the last rib at the most distended point.
Don’t delay transport, transport immediately and treat en-route to the vet, pull over, do it, then get going, if it’s a long drive and you need to, pull over and do it again. If successful you should see a rapid Improvement.
When you get to the vet, make sure you tell them you’ve done it whether successful or not, how many times, and where, they need to know.
RISKS:
Hitting the spleen
It not being bloat and hitting the bowel.
Both these injuries are usually well tolerated.
Reperfusion Injury
Releasing toxins if it's gone on for too long.
Complications with trocarizing are rare if performed by someone trained in the procedure.
The benefits out way any risks if you're not going to make it to a vet in time.
IMPORTANT: you should only do this if you have hands-on training in distinguishing bloat from other medical conditions, proper anatomical landmarks, and handling the needle.
You could say it’s similar to a cardiac arrest and performing CPR, in the sense that time may not be on the patients side, and to quote one trauma vet “if it needs doing, then it needs doing”.
Bloat is a Killer…. “if you’re not going to make it to a vet in time, you might as well try".
It’s something to consider.
.
PART 5 – Emergency Plan
Do you have an emergency plan for your dog?
I see posts on FB of dog owners asking if anyone knows of an emergency vet, and they are asking when its an emergency, I'm not criticising, some people don't realise or just don't think about this because they've never had a real emergency before, so….
You may know how to spot it, and act quickly, but do you have an emergency plan?
• Do you know your vet's out of hours emergency procedure?
• Does your vet have their own out of hours emergency service or do they subscribe to an out of hours service elsewhere?
• Do you have a backup vet if you can't get hold of your usual vet? That's happened to me once.
• Not all vets and clinics are capable of dealing with a major condition or trauma, the closest may not be the best choice, check!
• Even if your vet can deal with your emergency, are they willing and able to keep your sick dog in over night after treatment or do you need to transport your dog to another vet to stay in over night for monitoring? Yes, that does happen!
• If you are on holiday with your dog do you know where the nearest suitable emergency vet is located?
Remember, time is against you, every minute counts, all too often I hear people say "catch it early, get to a vet fast"…. "you may have a couple of hours", you may, but not always, no matter how early you catch it!
And not just in the case of bloat.
Something to think about, especially at this time with a shortage of vets.
.
PART 6 – Prevention
The only prevention tactic with a very high success rate is a prophylactic Gastropexy, it does not prevent a simple bloat but stops the stomach rotating.
Some owners will tell you it doesn't work because they had their dog gastropexied and the dog still bloated, in some cases died, nothing is 100% guaranteed, however it does have a very high success rate in the prevention of GDV if it is performed correctly.
It's more commonly done at the time of the emergency surgery when treating a dog suffering a GDV, it seems more popular as a preventative measure in the US than here in the UK, I don't know about other countries. Its commonly done in bitches at the same time as a spay.
The goal of a gastropexy is to create a permanent adhesion between the gastric wall and the abdominal wall. Ideally, a gastropexy should create a strong adherence, have minimal complications, not affect the stomach's natural orientation or markedly alter gastric outflow, and require minimal postoperative management. Gastropexy is usually performed by attaching the pyloric antrum to the right abdominal wall to prevent further gastric rotation.
There are several types of gastropexies, including incorporating, tube, circumcostal, belt-loop, laparoscopic-assisted, and incisional. No controlled studies have compared adhesion strength, clinical outcome, and physiologic impact of all the gastropexy techniques, so the choice of procedure is often based on the veterinarian's preference.
The US military gastropexy all DoD Working Dogs before they enter training and they have an extremely high success rate, they have gone from losing about 10% per year to GDV to losses of 0.1%.
Other prevention strategies such as limiting exercise before and after feeding, restricting water after feeding and feeding certain diets have no scientific evidence that they work.
Some will tell you that raw fed dogs don’t bloat and that is simply not true, all the dogs I’ve known that bloated were all fed either kibble or raw.
I can say that I’ve known people personaly who follow these strategies religiously and still have their dog bloat, some don’t have a dog bloat and so they think they work, I know people who limit exercise and don’t have a dog bloat and some do, I’ve known people who have for many years given their dogs light exercise such as a walk close after feeding and never had a dog bloat, you have to do what you think is right for your dog, just understand nothing is guaranteed to prevent bloat so don’t let anything you are told or read give you a false sense of security.
.
PART 7 – Further Information:
Veterinary Tactical Group's GDV Webinar presented by Dr. Janice Baker, DVM.
An excellent 1hr 30min presentation covering the facts, risk factors, signs & recognition, field treatment and prevention.
https://veterinary-tactical-group.square.site/product/2020-gastric-dilation-volvulus-a-working-dog-dilemma/333?cs=true
Prehospital Care of Canine Gastric Dilatation and Volvulous by Dr. Lee Palmer, DVM.
https://www.jsomonline.org/jsomstorefront/index.php?rt=product/product&keyword=Canine&category_id=0&product_id=2542
VetCOT's Best Practice Recommendations for Prehospital Veterinary Care of Dogs and Cats:
The objective of these guidelines were to examine available evidence on prehospital care in human and veterinary trauma and emergency medicine and develop best practice guidelines for use by both paramedical and nonparamedical personnel in the approach to the prehospital care of dogs and cats.
Section 12: GDV, is on page 213.
http://users.neo.registeredsite.com/1/2/1/13151121/assets/Best_Recommendations_for_Prehospital_Veterinary_Care_of_Dogs_and_Cats.pdf
Clinical Management of Military Working Dogs by Joint Trauma System:
There is a brief but informative 6min section on GDV in this video presentation from the Joint Trauma System's continuing education conference Clinical Management of Military Working Dog's Presentation for human HCP's.
Presented by Dr. Michael Lagutchik, a civilian Veterinarian from the Military Working Dog centre at Lackland, USA.
https://deployedmedicine.com/content/1265
Gastric Dilatation And Volvulus In Working Dogs:
World Small Animal Veterinary Association World Congress Proceedings, 2013
Kate Hill
Centre for Service and Working Dog Health, Institute of Veterinary, Animal and Biomedical Sciences, Massey University, Palmerston North, New Zealand
https://www.vin.com/apputil/content/defaultadv1.aspx?pId=11372&catId=35321&id=5709943
Bloat – What You Know Can Save Your Dog's Life by Dr. Alexis Newman, DVM
https://issuu.com/workingdogmagazine/docs/vetcheck_1acd1b26c1c6ce
Bloating Akita
A video showing a dog in the middle to late middle stages of bloat. Used by some as a training video, some may find it a difficult watch. This dog, Roscoe, was saved.
https://m.youtube.com/watch?v=U1WrT2719yo&feature=youtu.be
Another video example of a dog bloating, it doesn't look as serious as the previous example but this dog is in a serious condition, apart from his stomach distension he looks pretty good in himself while at the vet waiting to go to the ER, those who might not have a good understanding of bloat may be tempted to wait and see.
This video along with the previous shows the variation in how bloat can present, it is never the same for every dog, know what is normal for YOUR dog.
https://m.youtube.com/watch?v=37Xs10PQEmk&feature=youtu.be
A good visual presentation of what GDV/Bloat is, and does, if you are not familiar, and may help you understand why it may present with some of the signs & symptoms which it sometimes does.
https://m.youtube.com/watch?v=rf3bZUpMlN8&feature=youtu.be
Needle Decompression
Here is a video of a vet demonstrating needle decompression, albeit in a clinic setting.
https://www.atdove.org/video/gdv-gastric-trocarization
FREE Webinar – BLOAT: What Every Dog Owner Needs to Know.
Published 2014
Presented by Dr. Elizabeth Rozanski DVM - a board-certified specialist in emergency and critical care medicine.
http://www.vetvine.com/article/164/bl
FREE Webinar – GDV: What we know, and what we wish we knew.
Published 2021
The 2nd Webinar Presented by Dr. Elizabeth Rozanski DVM
In this webinar Dr. Rozanski provides updates on our current knowledge and understanding about GDV in dogs. Her discussion includes:
•What is known about the genetic aspects of GDV
•The pathophysiology and treatment of GDV
•Why some dogs who develop GDV do poorly
•Preventative measures including surgical gastropexy
•Our current challenges with GDV in dogs, ongoing research efforts, and possible targets
Running time: 57 minutes followed by 7 minutes of Q&A
https://www.vetvine.com/article/704/gdv-what-we-know-and-what-we-wish-we-knew#global_content
.
PART 8 – Final Words
Many have experienced bloat, many have lost dogs to bloat, some never even made it to the vet, some dogs died shortly after arriving at the vet.
Some dog owners and vet professionals may not agree with everything here, some vet professionals don’t even agree with each other.
There is a lot of misinformation out there on bloat, I have tried to give an honest picture of this condition with accurate information, a condition which takes the lives of many dogs in a horrific way, I am not a medical professional, this is just what I have learnt from my own experience and knowledgeable professionals who have real world experience with this.
With bloat I have learnt there are 2 types of people, those that can't or don't want to face it or even talk about (which is understandable), and those like me that want to learn everything they can incase they have to deal with it again and give their dog the best chance of survival, unfortunately for some, it happens more than once.
I was never satisfied with the only choice available to me being to put my dog in the car and drive to the vet, depending on the degree of bloat and distance/time to the vet that can be a roll of the dice, a 50/50 chance for the dog or less, to me that is not good enough, granted some wouldn't be able to put a needle in their own dog, I know I've done it and it's not easy, well not mentally, I had to look my dog in the face, see the pain in his face and watch him struggling to breath, there was no one else but me to help him and I wouldn't wish it on anyone.
I'm afraid life can be cruel, and sometimes you need to take aggressive measures to save a life.
I can guarantee 3 things if you ever experience bloat in your own dog, you will be scared, you will pray you make it to a vet in time and, no matter what the outcome, you will never forget.
Many of the sources of information I mention in this article are professionals that have experience with bloat and prehospital care of bloat (clinical and prehospital care are not the same, a more clinical aspect of care doesn’t always work in emergency field care), they know what they are talking about.
If you are new to this hopefully this will help or at least give you a starting point but as they say “hope is not a good plan” and the last thing you will want to be in a bad situation with your dog is helpless, so don’t be, the knowledge you gain is ultimately what can save your dog's life, along with your Mindset and Training, staying calm so you can make good decisions quickly.
For the dogs 🐾
1 note
·
View note
Text
What Are The Benefits Of Owning Home Medical Equipment?

It can be difficult to seek help fast when you suffer from a condition that requires constant supervision. Certain medical equipment, such as the hospital bed or wheelchair can be very useful especially for families with members or seniors with limited mobility living together. It's a good idea to keep medical equipment readily accessible for those who may experience modifications in their health.
The advantages of purchasing quality, reliable medical equipment that is easy to use includes symptom tracking and monitoring for emergencies to ensure you're receiving the proper medical treatment, while avoiding worst-case scenarios.
Reduces the need for expensive medical procedures.
Patients with chronic, lifestyle or terminal diseases require constant treatment and supervision. It is expensive to provide care for those with these conditions because they require frequent hospital visits.
The use of home medical equipment, like medical beds, ECG units, and urine, blood, and glucose analyzers, can be cost-effective in the long-term. Home medical equipment gives patients comfort and ease of access and eliminates the expense of paying a fee to an external third party each when tests are required. To discover more info on medical products, you've to visit affordable medical supplies site.
Hospitals break down their fees so that patients only need to pay for the things they use for their care. This includes food and other supplies as well as medical and nursing services. By investing in-home medical equipment like nebulizers and wheelchairs patients can save money that they would otherwise be spending on rental or hospital trips.
The organization encourages patients to live an active lifestyle
Patients with chronic ailments utilize various diagnostic tools over the long term to help maintain their health.
Test results from these devices act as reminders to patients to take care of their health. These devices are able to aid patients in living better lives by altering their long-term behavior.
Helps in the surveillance of Chronic Diseases
Asthma, cancer, and diabetes all need long-term treatment and management.
Home medical equipment is a huge aid to both caregivers and patients. The equipment is used to monitor the health of the patient on a daily basis and helps the caregiver give an accurate account when they visit a doctor of how the patient is doing.
Can Save Lives in the event of an Medical Emergency
Some of these medical supplies are intelligent and are programmed to alert emergency contacts if a patient is rapidly declining. A patient's life could be saved with a quick intervention.
This medical equipment is available to patients when they need it. Emergency care can be provided while you wait for the first emergency responders. This action is crucial in determining whether a patient survives or dies during an emergency.
Patient Security Boosted
Medical equipment at home helps caregivers to offer care.
This equipment allows you to care for and monitor patients who are critically ill without having to worry that they will not receive the proper support once they quit the hospital.
Family members and the loved ones of patients can utilize the equipment with confidence under the supervision and guidance by medical professionals. They will feel confident in the knowledge that they're providing medical care for loved ones, and are not risking their own health risk.
0 notes
Text
What Are The Benefits Of Owning Home Medical Equipment?

If you have a health condition that requires continuous monitoring it might be difficult to find a quick healthcare professional whenever there's a problem. A hospital bed or wheelchair is a great option for seniors or family members with limited mobility. As they sometimes encounter modifications in their health conditions it's a great idea to have readily availableaffordable medical supplies.
It is possible to purchase reliable and easy-to use medical supplies. This will allow you to keep track of your health conditions and avoid the situations that could be catastrophic.
Reduces the necessity for costly medical procedures
Patients with chronic, lifestyle, or terminal illnesses need constant medical attention and surveillance. It can be very costly to care for patients with chronic illnesses due to the frequent hospital visits.
Home medical equipment that is long-term and durable including ECG units medical beds, medical beds, urine, blood, or glucose analyzers can save money. Patients are able to save money by using their own home medical equipment instead of having to pay extra for tests. To learn more info on medical equipment, you must browse medical supplies express delivery site.
Hospitals also breakdown the cost of their services, meaning that patients pay for each item needed for their treatment, which includes food, beds, and doctors' and nurses' services. Patients may save money by purchasing home medical supplies, such as adult diapers with tabs and nebulizers.
Encourages patients to lead an active lifestyle
Chronic conditions patients use a variety of diagnostic tools to manage their health for the long term.
These devices remind patients to take care of their health, and serve as reminders. These devices are able to help patients live healthier lives by changing their habits over time.
Monitors chronic diseases
Chronic diseases like asthma as well as cancer and diabetes require ongoing care and treatment.
Home medical equipment is a huge help tool for patients and home health caregivers. The equipment is used to monitor the health of the patient on a daily basis and assists caregivers in giving an accurate report whenever they consult a physician about how their patient's health is.
Could save lives in the event of an Medical Emergency
The medical devices can be programmed to alert emergency contacts in the event that the patient's condition quickly decreases. This swift action and prompt intervention can save a patient's life.
This medical equipment is readily available to patients when they require it. Emergency care can be offered while waiting for the first response. This action is crucial in determining whether a patient survives or dies during an emergency.
Improves Patient Safety
Home medical equipment makes it easy for caregivers to offer care.
This equipment helps to monitor and treat seriously ill patients without worry they will not receive the right support after they quit the hospital.
Family members and other loved ones can also use the equipment in confidence under the help of medical professionals. They can have the confidence that they are helping to take care of their loved ones without placing their health in danger.
0 notes
Link
Fourteen out of 15 severe COVID-19 patients who were treated in an investigator-initiated interventional open-label clinical study of the drug TriCor (fenofibrate) didn’t require oxygen support within a week of treatment and were released from the hospital, according to the results of a new Hebrew University of Jerusalem study.
Fenofibrate is an FDA-approved oral medication. The results were published on Researchsquare.com and are currently under peer review.
Specifically, the team that was led by HU’s Prof. Yaakov Nahmias carried out the study at Israel’s Barzilai Medical Center in coordination with the hospital’s head of the Infectious Disease Unit, Prof. Shlomo Maayan, and with support from Abbott Laboratories.
The 15 treated patients all had pneumonia and required oxygen support. They were also older with multiple comorbidities, ranging from diabetes and obesity to high blood pressure.I
n addition to standard of care, the patients were given 145 mg/day of fenofibrate for 10 days.
“The results were dramatic,” Nahmias told The Jerusalem Post. “Progressive inflammation markers, which are the hallmark of deteriorative COVID-19, dropped within 48 hours of treatment. Moreover, 14 of the 15 severe patients didn’t require oxygen support within a week of treatment.” The 15th patient was off oxygen within 10 days.

When looking at the data on other similar severe patients, less than 30% of them on average are removed from oxygen support within a week. In other words, fenofibrate could dramatically shorten the treatment time for severe COVID patients.
“We know these kinds of patients deteriorate really fast, develop a cytokine storm in five to seven days and that it can take weeks to treat them and for them to get better,” Nahmias said. “We gave these patients fenofibrate and the study shows inflammation dropped incredibly fast. They did not seem to develop a cytokine storm at all.
”Cytokine storms are aggressive inflammatory responses to illness.
youtube
In general, patients who do not require oxygen can be treated at home,” he said. “Additionally, despite the high number of COVID deaths in Israel and abroad, the majority of severely sick patients survive.“
If you look over a 28-day period, I would have expected all of them to survive with or without the drug,” Nahmias explained. “The question is how fast we can get them home or how quickly we can get a severe patient to a mild condition.”
All of the patients completed a 10-day home treatment after discharge and, according to Maayan, “no drug-related adverse events” were reported.
FENOFIBRATE WAS approved by the FDA back in 1975 for long-term use and is considered safe. Moreover, it is an inexpensive pill, Nahmias said. It costs less than $1.50 a day, meaning the entire treatment per patient was around $15.
Nahmias has been studying the use of fenofibrate for treating COVID-19 almost since the start of the pandemic. He first ran a pre-clinical trial and then a multi-center retrospective study, both of which supported the effectiveness of the drug.
“Viruses are parasites,” Nahmias explained. “They cannot replicate by themselves. They have to get inside a human cell and hijack their machinery to replicate.
”Working with collaborators in the United States, Nahmias demonstrated that the coronavirus prevents the burning of fat in lung cells, resulting in large amounts of fat accumulating inside lung cells – a condition the virus needs to reproduce. Fenofibrate, he hoped, would reverse that effect, and eliminate virus replication.
“By understanding how the SARS-CoV-2 controls our metabolism, we can wrestle back control from the virus and deprive it of the very resources it needs to survive,” Nahmias told the Post, noting that this also may help explain why patients with high blood sugar and cholesterol levels are often at a particularly high risk to develop COVID-19.
The professor is now involved with a series of Phase III studies being carried out in South America, the United States and Israel. Those studies are placebo-controlled and double-blind.
Nahmias said his team had been struggling to get patients enrolled in the study before the onset of the Delta variant, but efforts are now progressing more rapidly. He hopes that results could be available as early as within the next two months.In the meantime, the drug is available, and physicians can decide to give treatment with it based on available data.
“There are no silver bullets,” he said, “but fenofibrate is far safer than other drugs proposed to date, and its mechanism of action makes it less likely to be variant-specific.
”In the meantime, the drug is available, and physicians can decide to give treatment with it based on available data.
“There are no silver bullets,” he said, “but fenofibrate is far safer than other drugs proposed to date, and its mechanism of action makes it less likely to be variant-specific.”
33 notes
·
View notes
Text
Let’s get into some Ben 51 angst today lads, and hopefully little me’s cruelty is watered down and given decent explanation. Oh it’s still definitely cruel but probably not mindless.
Firstly, let’s set the situation, the tech-xperts of the facility rigged up a cheap Omnitrix controller. It’s not the highest quality, but it’s relatively bug free. Unfortunately it requires a receiver. How is this unfortunate? Because the Omnitrix has retreated into Ben’s systems. This means an embedded receiver, hard to remove and easily adaptable, needed to be installed.
As a collar.
The Omnitrix is never put into rest mode so it can help be Ben’s life support system, and while that does mean he gives off an energy signature at all times, it reduces the signature of his transformations. This I believe is because there’s a degree of separation between canon Ben and the Omnitrix that the alien forms are kept at their peak.
Ben 51, who would be energy deficient, can’t afford to be peak performance nor without the support, so the Omnitrix is less effective at its peak than canon.
SO! Moving on to the specifies, Ben’s stay at Area 51 consists of 3 rotating activities with varying times and lengths. Starting off we have the Isolation stage. As it implies, this ‘activity’ as Ben calls it out of sarcastic boredom has him spending a nonspecific but long duration of time in his claustrophobic cell.
However, that’s not the main event. This is a chance for the faculty to observe Ben’s behaviour... without invasive intervention, relatively speaking. During the isolation period, the Omnitrix remote is set to random selection, changing Ben into a different alien every time. He used to constantly try to escape, using the abilities he had as an alien to find any weaknesses, but he only accidentally helped Area 51 develop better tech to keep him in.
How did they stop him?
Well, the collar is not only a receiver, but a ‘disciplinary tool’ (read: shock collar).
So, overall, Ben doesn’t try to use his Isolation activity as a time to escape. Unless he randomly unlocks a new alien. Which finally worked when he got Alien X, who he would probably name Freyd (based on freed and frayed, yeah I know, on the nose and everything, but it’s BEN) after how Bellicus and Serena are named.
But I’m getting ahead of myself.
The second activity is the most energetic, Physicals! And by energetic, I ACTUALLY mean life threatening, because unlike PE at schools, this little activity is designed to find physical weaknesses of Ben’s alien selection.
What this involves typically are either battle scenarios or environmental scenarios, depending on what the suits up top wanna test. This isn’t meant to train Ben to be better, this is meant as a test for any tech the science team have developed, before sending them off to any dispatch team for on field use. Of course, they can’t just kill Ben, that’ll leave them with highly inefficient leftover alien test subjects, who have less chance of survival than Ben.
Needless to say, quite horrific.
New aliens get subjected to nonspecialised but definitely dangerous bots and environments, and the longer this goes for, the longer Ben refuses to play along. Of course, he’s ‘disciplined’ into doing as he’s told eventually.
Freyd was spared of the experiment, but it’s not like they could ever begin to try.
Last but not least, the Medicals! Probably the most gruesome, so proceed with caution, this sounds exactly like it does on the tin. This is the activity that Ben spends the least awake out of all 3, and at least there’s enough mercy to do so. Sure, Area 51 is cruel and inhumane (or perhaps the term should be xenophobic) but at least logistically, it would be a detriment for them to do live surgery.
Unfortunately, aliens have quite the different biology in comparison to humans, so sometimes the types and dosages of anaesthetics don’t... exactly... last through the dissection.
New aliens may have this issue, especially species with wildly different physiology to humans and even other aliens. Ben can’t count on his fingers how many times he’s awoken to glaring fluorescent lights and bloodstained silhouettes, but he can’t exactly list an exact number either. But he’s definitely got some bad memories about that, and knows a little more about alien biology that canon Ben does.
Whenever he’s Big Chill, using a more gender neutral name Ava (lanche), he mourns.
And feel free to beat me until I’m blue for that one this addition wasn’t even on baby me’s mind this is recent angst laddies!
In Ben’s escape, however, does he accidentally leave behind a treat for Area 51’s medical and biological staff. Having violently removed the embedded collar, the hidden tracker less effective if it’s taken out before teleporting, the faculty of Area 51 now have a sample of a Celestialsapien.
The missing chunk of Freyd’s neck.
With that piece of DNA.
They are now one step closer to capturing a God.
#ben tennyson#area 51 au#ben 51#ben 10#there’s a little section on#experimentation#medical horror#gore#xenophobia#in like the literal way with aliens and everything#there’s also#implied infanticde#and feel free to tear me apart for that one#what if i tag the aliens too names and everything#except for maybe serena and bellicus because they play such an insignificant role in this post#celestialsapien#freyd#necrofriggian#ava#so anyway that’s what little me was thinking about at the time#don’t read too heavily into it i was born into the edgy phase#but like lighthearted edgy?#i would say these things with a giddy smile on my face is what i’m saying#me: oh i love little chills#also me: does this
25 notes
·
View notes
Note
Few questions. Do insecticons, exist in your AU? not just beastformers, but the ones that can generate energon by eating things? (maybe its low quality energon? or the process is inefficient?) and how powerful can self repair systems be? i.e while i think you said that losing limbs would require a doctors visit, are there exceptions? i.e Rampage or some beastformers? i could see it being energy and material intensive?
Insecticons do exist, they just aren’t people!
While there are beastformers with bug or insect alt modes like Shrapnel, Blackarachnia, Scorponok, etc, they aren’t called insecticons, because that refers specifically to mechanimals. The term “insecticon” is about as broad as the way we use the term “bug”, in that it refers to basically any creepy-crawly cyberfauna within a vague category. Regional names for different species vary, and often entire groups of unrelated mechanimals will be clumped under the name insecticon because they look similar. Different types of insecticons include buzzflies, arachnicons and spiderbots, rustbugs, reedmechs, groundcrawlers and wormazoids, cyberticks, mechamoths and robotterflies, antroids, and decapodians. Just like insects on Earth, the vast majority of cyberfauna are in fact insecticons of some sort, found all across the planet and well into its understrata.
Like most mechanimals and cyberflora, they do have a part in the energon cycle, with each species programmed to best suit its niche. Some extract raw energon from liquid veins and lay “eggs” or pods of gelatinous energon for other mechanimals to pick up for sustenance, sort of like brollypalms. Some drill through sheets of sediment and metal underground to erode into new veins, rivers, and leylines. Some nibble crystal energon deposits and grind them into sand to be swept away by acid rains and liquified into refinable energon.
Cybertron’s wildlife are, as a whole, a sort of repair system and maintenance network that keeps all the environmental processes and technological ecosystems running. Mechanimals even have their own hotspots from which they erupt like Cybertronians do, different hotspots for different species. Since “insecticon” refers to so many different things, there’s no one thing they’re known for like energon production. Like many mechanimals, alloygators for example, there are folk tales and mythologies around them that vary by culture and region. A common thread is some mysterious final moulting from common bug into enormous beast, a monster sent to rout all civilization or perhaps a sentinel standing guard. Despite this, there is no known evidence that any insecticon species is able to grow larger than a size two adult.
Now, as for self repair systems...
While mecha are less delicate than humans and thus less likely to be wounded, that same toughness means their bodies aren’t easily mutable, so self repair is not as extensive compared to a human’s ability to heal. A human could have a huge chunk of flesh gouged out and heal with a scar. A mech, without medical intervention, would have that gouge permanently, with the self repair systems only capable of sealing off the edges and, if it isn’t deep enough to damage important internals, construct a plastoid shield between internal systems and outside exposure. Self repair systems can’t just conjure a replacement to what was lost, and “growing” new body parts is limited to only a few inches of extra layers on a body part that already exists in order to replace or heal.
Medical intervention to a major injury like that involves creating a scaffolding over the wound for self repair systems to grow over, cloning and wholesale replacing system parts that were lost, and, if serious enough, immersing the wound in sentio metallico. A severed limb can be reattached this way if the limb is recovered and medical intervention occurs immediately, much like how humans can have limbs reattached. For cases like Terminus, left too long, the self repair systems seal off the wound, quarantine the parts that aren’t getting enough energy to survive, and reroute all systems to no longer support the dead area. Once that happens, it can’t be undone.
This is fairly different from canon, I know. There’s plenty of mythologies about heroes and monsters capable of shrugging off deadly wounds, regenerating body parts, and creating kibble out of thin air, but it just isn’t something Cybertronians are capable of doing. They can’t drastically change their frames, or switch bodies, or mass shift, or take new or multiple alt modes. There’s just limitations to what a species is capable of, you know!
... and then the heroes show up, and blow all of that out of the water. Nothing medical science has established seems to apply to them. They all heal ridiculously quickly, some more than others, and a few seem to regenerate entire body parts from nothing! One of them even dies over and over and then gets back up!!! These heroes are either impossible, or everything that medics know is wrong.
#transformers#cybertronian biology#cybertronian culture#insecticons#cybertron#worldbuilding#heehee hoohoo gee i wonder why medical science might be wrong???
26 notes
·
View notes
Note
im super new to the idea of anti-psychiatry and if u have a chance/the time or energy i had a question as someone who is seen as “treatment resistant” & has been in the system for many years. im curious if u think that seeing a therapist/having a dr/patient relationship in any scenario is unhealthy/harmful and it is impossible to see real reward from any type of treatment like that? i dont generally have much energy to research/read long bodies of text so i was hoping i could ask! thank u!
no problem, thanks for asking! as a fellow-supposedly "treatment resistant" (im still here bitch!) person, i've given a *lot* of thought as to what an anarchist treatment model, as it were, might look like, particulalry with se/lf-harm/su/cidal dep. + eati//ng dis/orders. many people ask me this and i ask myself; it's an important question for anyone seriously thinking about deinstitutionalization + antipsychiatry.
also, before i start, i think a great way to begin engaging with antipsychiatry is to turn a critical lens back to your own usage of language: what do you mean by "unhealthy/harmful"? that reads as psychopathologizing language in and of itself! this isn't to say you said something "wrong" or w/e but instead to point out that medico-psychiatric hegemony is everywhere, including in our critiques of it. we struggle to find a framework for our thoughts about right and wrong without framing them as well/sick; cured/diseased; sane/insane. a great exercise for someone starting out might be to keep track of some of the quotidian judgements you make and look at their indebtedness to ableist/saneist norms.
ok, so to address your q!! below is a little long, i tried to keep it as brief as possible but if you're having trouble with it (re: having trouble with long bodies of text) please feel free to ask clarifying questions in my inbox or DMs. :)
in terms of dr/patient relationships - whether you're a materialist or a poststructuralist (personally, i'm nonbinary); whether you think the access to material transformation/isolation/etc. is the locus of the power differential there, or whether you see the locus of power in the act of naming someone a doctor or marking someone as "sick," you're going to find a clear, unavoidable hierarchy between the professional and the patient, of whatever stripe.
the most decent drs and therapists are well-aware of this, are unafraid to name it, and are willing to act as collaborators w/ patients to engineer a liveable mode of non-compliance, to game "the system", and to prioritize survival over cure. the mere fact of having a certain type of medical/psychological knowledge doesn't suddenly render someone an evil person, nor do i think individuals are "innately" good or bad or anything at all!
however, virtually every dr, psych, social worker, therapist, etc. is to some extent educated in a system that continues to reify medical/psychiatric conditions. this training predisposes them all to understand "patients" as "afflicted" subjects. to see us as "cases" to (re)solve. some have the courage and wherewithal to resist what in many cases amounts to academic brainwashing. most don't. all have internalized the systems of oppression embedded in scientific disciplines & the world we live in and are capable of inflicting harms based on these on marginalized patients, up to and including death.
all this being said, let's return to awareness of hierarchy. my best dr (and current GP), as well as my most recent 2 therapists, are aware of this hierarchy. i see a doctor because, uh, i'm actually a reasonably decent fan of being alive and an even bigger fan of getting the fuck VACCINATED! and also like, participating in college and other stuff that requires check-ups. i started seeing a therapist consensually, for the first time ever, when i was eighteen and seeking primarily 1) a "gender dysphoria" dx and thus access to biomedical intervention and 2) an adult autism dx in order to get the living accommodations i needed at college. i remained "in therapy," as it were, after i no longer *needed* it, because, surprise! it's nice to have someone to talk to whose job it is to hang out with you. the notion of talking out your problems in order to find ways of dealing with them is a good one. everyone does it. i'm not currently in therapy for reasons that are probably obvious, but i certainly wouldn't make carte blanche statements of therapy's "uselessness."
drs that are aware of hierarchy also understand that the constructions of the "treatment resistant" patient are embedded in this notion of compulsory cure. the patient becomes treatment resistant when they "fail" in pursuit of the successful cure they are presupposed to want. mind you, these are the cures drs themselves dream up for us –– hence the word "resistant". treatment resistant often = resisting medical authority. that is, noncompliant; that is, lacking insight, that is, Mad. rather than take apart the relationship between antipsychiatry and those who "can't get better" (including myself!) i'm far more interested in looking at ways to make life survivable outside the binary of sickness and health. how do the conditions under which a "patient" lives determine their resistance to treatment (e.g., is it treatment-resistant depression, or is it "i'm poor, jobless, estranged, and subjugated by capitalism"? if it's the latter, hell, who wouldn't be suicidal?).
further, are they treatment-resistant because they object to the form or method a treatment might take? because they're traumatized? because they feel unsafe with those doing the treating? all of these are questions that can only be addressed when we make visible the dr./patient power relationship. i have had recent medical and therapeutic experiences that have helped me and even felt affectively rewarding, and recent experiences that have made me feel like utter garbage. the difference isn't that in one case, i was fixed, and the other, i was ill, but instead that some providers are willing to engage with me where i'm at and trust me as author(ity) of my own life, and others treat me like a lineage of problems that can't be fixed.
i don't know if that helped, this is more an infodump but i tried to organize it in a potentially helpful way! again, please hmu with questions.
#survivingpsych#suicide m ////#saneism#ableism#medical industrial complex#psychiatric industrial complex#ask#Anonymous#madness#critical mad studies
43 notes
·
View notes
Text
I am so fucking tired of hearing the "well only 1% of ppl die from getting covid" bs
You know how many kids died from polio? About 3% on average. Adults faired worse, but even then about 70% of polio cases were asymptomatic. The remaining 30% ranged from mild to death, with mild taking up the lion's share.
At our peak year, the US had about 52,000 reported cases of polio (which means that the actual number of people who had it but were asymptomatic was almost about 200,000).
Out of those 50k+ symptom diagnoses cases, only 3k died. The other 47k recovered.
Yet even those numbers were sufficient to create the March of Dimes and a public pressure to find cures, vaccinations, etc.
Within 15 years, doctors started to notice that adult survivors were developing similar symptoms and these patients were the first to show what are now called "post-polio syndrome" patients.
But even before that, the 20-25% of cases with symptoms but who recovered often had mobility issues, bent legs or arms, 'frozen' joints, etc because of how poliomyelitis attacks nerves.
With Covid, if you say "well 99% of ppl survive" a) you're wrong, it's more like 93-95% and b) you're saying '99% are fine' ie survival means complete recovery.
Nope.
It's like saying that 99% of people survive amputation of multiple fingers.
Well sure, they survive, if it's a binary alive/dead count.
They didn't die from it, so they survived.
But how does having 6 fingers change your life from having 10? How does losing a thumb change your ability to do things in every day life? How much extra wear or stress will your remaining fingers, hand, etc take on due to you having to switch to a non-dominant hand as primary use or accelerate repetitive motion conditions like carpal tunnel?
How long would it take you to adapt to having fewer fingers, adapt to a prostethic, gain confidence in the reuse of your hand(s)? How much more would you have to pay every year for medical stuff and how much on non-covered items that you'd have to replace or just start buying for convenience?
Scissors? Can openers? Button hooks?
What if your job was typing, like a court stenographer? Or a music teacher? Would you be able to adapt?
Alive doesn't mean unchanged or unharmed.
Surviving doesn't mean returning to the status quo.
People aren't just dying from Covid or surviving it, everyone. A large portion of people who have recovered from covid have serious damage to their heart, lungs, brain and other organs that may never fully heal, complications that change their lives forever—just like lots of people who survived Smallpox or polio or rubella were never back to the way they were prior to catching those diseases. Going through it doesn't end with you being 100% fine if you survive.
It's more like :
Out of 100, 95 ppl survive initial infection
- of those 95, X (let's say 35) end up with a long-term issue
- of those 35, 25 have more than one longterm issue (lasting over 6 months, requiring medical checks or adaptation of work/life) that may be treatable or improve over time without much intervention
- the remaining 10 have conditions that are chronic and less likely to improve over time and in turn could make the patient more likely to die from other illness, decrease their overall quality of life and decrease their lifespan overall.
So suddenly it isn't a 5/95 issue, it's a 35/95 issue and a 10/35 issue, so your odds of surviving haven't changed but your odds of surviving unharmed and exactly as you were before are greatly decreased.
Now it's more of a 1/3, where you swap from 5% dying to 30~% having long-lasting illness, symptoms or developing conditions that continue for anywhere from 6mo post-infection to end of life 20, 30 or 40 years from now.
If I cut off, say, your right thumb and left forefinger, you're 99% likely to live afterward, but you're certainly going to have a ton of fucking issues with doorknobs, buttons, typing, getting dressed, etc which will require months or years of you adapting along with costing you a shit ton of money in costs for medical, assitive devices, potential career change and all the time involved in learning how to use your hands/body. But hey you're part of the 99% who survived so why are you mad?
So to review -
5 die.
35 survive with potential life-long issues.
60 survive with little to no symptoms or complications (but also no long-term immunity so could be reinfected and/or still subject to secondary development of issues related to their exposure in the future)
Sounds more like a 40/60 split than a 5/95 now, right?
That's because IT ALWAYS IS
3k deaths out of 50k from polio doesn't give you the # who were permanently paralyzed in a limb, two limbs, left unable to walk, etc. or that up to 50% of polio survivors developed a condition from their original exposure decades later (and that no one even knew existed at the peak of polio infections in the US) even if they survived without permanent paralysis of any part of their body.
We're on track to see 400k+ deaths by the end of the year in the US alone and that doesn't include the people with chronic or permanent issues who survived.
It isn't binary.
It isn't something to dismiss because of the percentage of fatality is 'low'.
It also isn't only your life that is being endangered.
Don't travel for the holidays.
Don't gather with people outside your household.
Don't go all over shopping for gifts.
Don't hold your tongue around people you care about: tell them to stay home, tell them to not gather, tell them to be patient and think of others.
It isn't just covid. It's all the cancer patients having to delay treatments that compromise their immune systems. It's all the patients needing organ transplants who cannot get surgeries. It's the backups of CT/MRI for emergency patients bc of protocol to avoid contagion. It's about all the people who need care only hospitals can provide being rescheduled or shuffled down the weeks. It's about full hospitals, people forced to find ways to get basic needs met in areas that don't have many options for at-risk people, and a domino effect of selfish behavior directly leading to the injury and death of thousands who could be alive today if people just did the bare fucking minimum and masked up, distanced and stayed home.
Stay the fuck home.
#covid 19#Covid#Covidits#Trumpsterfire#Wtf#Stay home#Don't gather#Wear a mask#Jfc people#Rants#Coronavirus#Disease#Ffs#Polio#Vaccines
6 notes
·
View notes
Note
In the world my story takes place in, there are creatures called razorfish.(not related to actual razorfish) They have four razor strips that are almost one (1) cm long surrounding their torso area(I forgot what it’s called) My main character is attacked by a school of them. She needs to lose at least 25% of her blood(which would be 1.25 kg) in order to pass out. How many razorfish wounds would she need in order to pass out in ten minutes?
So this is really gonna depend.
1 cm razor blades are enough to do plenty of damage depending on where on the body the wound is. I have seen people bleed out from a 2mm puncture site in an artery. But this happened BECAUSE it was an artery. This isn’t a hard and fast rule obviously. So let’s dig into this a bit.
The body has two vascular systems basically. There’s arteries and veins. Arteries are incredibly high pressure and all it takes is a tiny hole in certain large arteries (think femoral artery) in order for someone to bleed out fairly quickly. The arterial system is very high pressure as it’s the system that delivers oxygen/nutrients/etc. to all of your body tissues. So in order to do that it needs to be under pressure and move along a pressure gradient from high to low (heart generates pressure when it contracts and is the source of the pressure gradient. high pressure/arterial—> low pressure/venous, and then blood returns to the heart and the cycle restarts). Obviously this mechanism works great for that, but the side effect of that is when the structural integrity of the artery is compromised it can be really hard to control the bleeding, and holes in the arteries don’t close up like more superficial/venous wounds as the pressure from the blood gushing out of the hole maintains the patency of the opening.
On the other hand, more superficial, non-arterial wounds typically don’t have the bleeding powder for someone to lose so much blood that they pass out. They bleed for a bit and then close up on their own. There are some exceptions, like with the great veins of the body, but those are usually pretty deep and inaccessible (vena cava), or are located fairly close to arteries (example: the femoral artery and vein are right next to each other) so at the point that large veins would be compromised, it would probably be the least of your characters problems because either they’d have organ damage, or their arteries would also be gushing blood (probably). In order for someone to pass out from these kinds of more superficial wounds, it would have to be pretty darn extreme - probably superficial full body wounds. (Side note: with that extensive kind of damage to the skin they’d be a massive infection risk after this)
Anyway, there’s another issue here that I can see and it’s that once you’re at the point of passing out from blood loss, you’re already deep in hemorrhagic shock. Brain perfusion is the body’s priority, and as such it will receive blood at the expense of basically the rest of the body. If you’re passing out from blood loss, you’re in pretty critical shape. Losing enough blood for brain perfusion to be decreased (leading to unconsciousness) in ten minutes is a pretty significant gush that isn’t going to fix itself, and things are going to start going downhill really fast at the point that they’ve passed out. This would not be a gentle loss of consciousness for this character. This would be a massive crash, and the situation would continue to escalate. They would be in major peril and would require some kind of medical intervention in order to survive this.
Assuming they survive that kind of rapid blood loss, recovery and resuscitation will be necessary. Whoever is on the receiving end of this narrative treatment is probably going to have a rough go of things after this. People who lose that amount of blood are usually going to deal with complications, organ damage (especially the kidneys and intestines!), and limb ischemia at various levels. They may have issues with clotting and stroke. Depending on the severity, they may have brain damage. Etc. what I’m saying is that they’re gonna be in bad shape.
Without knowing all the context here (idk, maybe you really need this character to ACTUALLY lose enough blood to pass out), if the narrative goal is JUST for them to lose consciousness: an alternative is that rather than passing out from blood loss the character could have whats called a vasovagal response. This is a fairly common phenomenon. You know those people who faint when they get stuck with needles or when they donate blood? They’re vagaling. This is where there is a very sudden drop in heart rate and blood pressure that causes unconsciousness in some people. A lot of things can trigger it - anything from bearing down to poop, to the sight of blood, to fear responses. You’d be shocked how many people I’ve found down in the bathroom because they were constipated but especially determined to get one out. It’s also not uncommon to have people vagal when we’re holding pressure in sensitive areas (like if we’re holding pressure in the groin because there’s an arterial puncture). The unconsciousness is usually brief and fairly harmless, and unlike passing out from blood loss you don’t have to deal with the long term side effects and complications that occur as a result of major blood loss, e.g. injured cleanie-beanies.
So, to recap - if you really need them to pass out from legit blood loss in 10 minutes:
From superficial wounds, it would have to be pretty excessive/all over the body and they’d probably pass out from pain before they got to that level of severity wrt blood loss.
From arterial, you just need one good puncture in the right place - most accessible arteries would be radial or ulnar arteries (in the arm and wrist) or the femoral/popliteal (in the groin or behind the knee) but the caveat there is that if you don’t want your character to die, that arterial wound absolutely needs to be dealt with quickly as it won’t close up on its own and if your character is down and out, they’re realistically about to die. You also should probably take into consideration the potential complications and the recovery from hemorrhagic shock.
Does it need to be blood loss? Or is the goal just unconsciousness? Because if that’s the case: have them vagal. It can still be the result of them being wounded/blood loss but the mechanism and severity would be different. They could look down and see one decent sized gash that looks much worse than it is and pass the fuck out. Some of their symptoms leading up to that would be similar - shakiness, dizziness, nausea/vomiting, etc. but there won’t be any long term consequences for their internal organs.
Anyway! Good luck and hope this helps.
9 notes
·
View notes
Text
Code Black 1.11: “Black Tag“
Okay Folks, are you ready to talk about triage? About the National Incident Management System? About acronyms? About why doctors and firefighters do different jobs for a reason? About MORE ACRONYMS?
Then you’re ready for this post.

The other night I watched Code Black’s “Black Tag” at the suggestion of @7thchevronlocked. I’d never watched the show, but from what people have said, I was expecting a fair amount of accuracy.
I... didn’t find it. But what makes this episode so interesting is that while they portray procedure very poorly, they managed to very accurately represent the consequences of doing things the way they did them. If you ever want to know the why of “why do we manage emergencies that way” this episode does an excellent job of explaining it (I assume without trying to? Eh?).
The episode “Black Tag” centers around a multi-car pileup Mass Casualty Incident (MCI) on an LA freeway. The show’s main doctor characters are deployed to the scene of the accident to perform triage on the wounded and provide lifesaving medical interventions. The episode deals with having to make difficult triage decisions in order to care for as many people as possible while pushing the characters well out of their comfort zones.
Emergency Management Frameworks:

Before we get into the episode, I want to give you some background on Mass Casualty Incidents, or MCIs, as a whole. In very basic terms, MCIs are events in which the number of victims exceeds the minimum number of people required to care for them. This can be anything from someone giving birth in the back of an ambulance (2 patients, 1 EMT), to something like 9/11 or Hurricane Katrina where multiple large agencies have to pool resources in order to respond.
Disclaimer: This, and a lot of things I talk about in this review, are outside of my normal scope of expertise. I do know more about it than your average bear, but if you see something that needs changed or could be explained better, let me know.
There is a standard system for how to deal with any and all emergencies (not just MCIs) in the US called the National Incident Management System (NIMS). NIMS is an overarching document that lays the foundation for everything from how to share resources among multiple agencies to how to manage information to how to plan and coordinate a response to how to train staff and plan for the next emergency.
How NIMS uses people in emergencies is called is the Incident Command System (ICS- in hospitals specifically, this is called the Hospital Incident Command System, or HICS). ICS outlines a specific set of jobs and responsibilities for each person involved in an emergency response.
The first trained person to respond becomes the Incident Commander (IC). This responsibility can be handed off to someone else later if appropriate. In small scale emergencies, the IC may be the only activated part of the ICS. In larger emergencies requiring more people, people can be added to a command structure that looks like this:
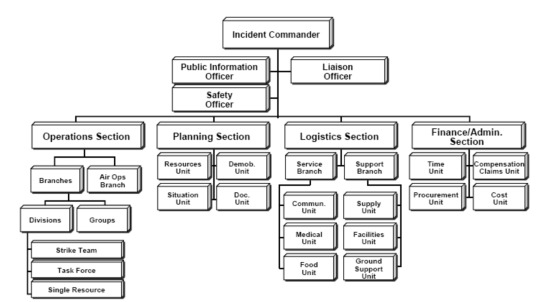
Very few emergencies will require the activation of everyone and every group on this chart, but it provides a framework that can grow and shrink according to the needs of the emergency. For example, the EMT helping someone give birth would assume the role of IC, but all they may need to do as the IC is call in another squad to take care of the second patient. Meanwhile, this framework could encompass thousands of people in the event of a major natural disaster or act of terror.
In the case of an MCI like in the episode, the hospital would set up an Emergency Operations Center (EOC) somewhere in the hospital. EOCs are basically rooms with tables set up and people organized with differently colored vests that indicate their job during the emergency (this can be very different from their job the rest of the time).
At the EOC would be the IC, Command Staff (people with “Officer” in their title), and the Section Chiefs, along with a few people reporting to them each. At the scene, the rest of the Operations Section would provide the hands-on triage and immediate care and transport of the victims. If it goes on long enough, there may be people from the Logistics Section there as well providing additional supplies, as well as food and medical care for the responders.
For a hospital, the portion of the Operations Section in the field doing triage, care, and decontamination if necessary is called the Hospital Emergency Response Team (HERT) lead by the HERT Leader.
In the episode there’s someone called the “Doctor in Charge”. I’ve never heard of this terminology being used (probably because there are only very rarely doctors who deploy to a scene, more on that later), but he was essentially acting as the HERT Leader. The location he was at with the tent would be called the Emergency Treatment Area (ETA).
That’s like, the barest-bones explanation of that. If that thrilled you, FEMA has free online courses (IS-100, IS-200, and IS-700) that will give you a much more comprehensive understanding for all different kinds of emergencies.
Also, are you, like, really done with the acronyms? I’m really done with the acronyms...
Assuming I haven’t now totally lost you, let’s talk about a few things that happened in the episode:
Just In Time Training:

The episode opens in the back of an ambulance that’s transporting the characters to the scene. Residency director Dr. Rorish and surgical attending Dr. Hudson provide something called “Just In Time” (JIT) training to the residents by describing triage and what will be expected of the docs once they arrive at the scene.
JIT training is a recognized way within NIMS to impart necessary training for situations that don’t come up often, but that require specialized training to resolve. Usually, this is emergency-themed training, such as Point Of Dispensation (POD) deployment, mass casualty decontamination procedures, ICS/HICS, or as in this episode, mass casualty triage. JIT works well because it means vital information is fresh in the minds of those using it, and requires very few resources (versus training and drilling everyone several times per year to keep the same level of readiness).
Triage might get a passing mention in medical school, but its not something any hospital-based doctor would be reasonably expected to know. That’s why they would need a JIT training to be able to do what they do in the episode (i.e. it wasn’t just exposition, it might have actually happened like this).
Unfortunately, as I got further and further in this post, I started to realize that a good 75% of the stuff that is poorly done in this episode could be traced back to the doctors’ super inadequate JIT.
Triage:
JIT is usually provided by someone who is very familiar with the material, something neither Dr. Rorish nor Dr. Hudson appear to be. In the episode, they describe triage in the following way:
Dr. Rorish: This is not first come, first served. Your primary job in your initial eval is to prioritize the patient.
Dr. Hudson: *handing out bags of triage tags* Each of you take a packet of tags. There are 4 colors. Green is for minor injuries. Yellow is for more serious injuries but not immediately life threatening. Red is for critical patient who won’t survive without treatment and transport. The black tag is for death or expectant death.
Dr. Leighton: Wait, expectant death? You’re saying we put a black tag on a living patient?
Dr. Savetti: You want us to decide who lives and dies?
Dr. Rorish: We want you to decide who’s life you *can* save- and prevent the next doctor or EMT who comes along from spending precious time on an unsalvageable patient.
In this exchange, Dr. Rorish is fundamentally right- when you have to process dozens or even hundreds of patients, you can’t get to them one at a time. The point of triage is to quickly classify patients by the order in which they require care. Then someone else comes through and provides care in the order indicated.
There are many different triage methods available, but the one shown in the episode is called START. START uses a 4-color system to sort patients and is widely used throughout the US. Dr. Hudson’s explanation of the categories is also technically correct, if significantly oversimplified. IRL, there are very specific criteria for the categories:
Green (Minor): Patient can walk
Yellow (Delayed): Patient can’t walk, but can control their own airway, are breathing less than 30/minute, have a radial (wrist) pulse, and can follow commands/answer questions appropriately.
Red (Immediate): Patient can’t walk, and one or more of the other conditions listed for yellow are not met (they may be breathing more than 30/minute, lack a radial pulse, and/or are confused).
Black (Expectant): Patient is either clearly dead, unconscious and not breathing on their own, or are otherwise unlikely to survive due to severity of injury and availability of resources.
Using this criteria does not mean a patient will be perfectly sorted every time (in fact, according to a study done in 2009, even well-administered START probably overestimates injury severity in about half of patients when compared to what the patient would eventually need medically), but the algorithm used to sort the patients is very fast and easy to teach and use, which is vital in this situation:
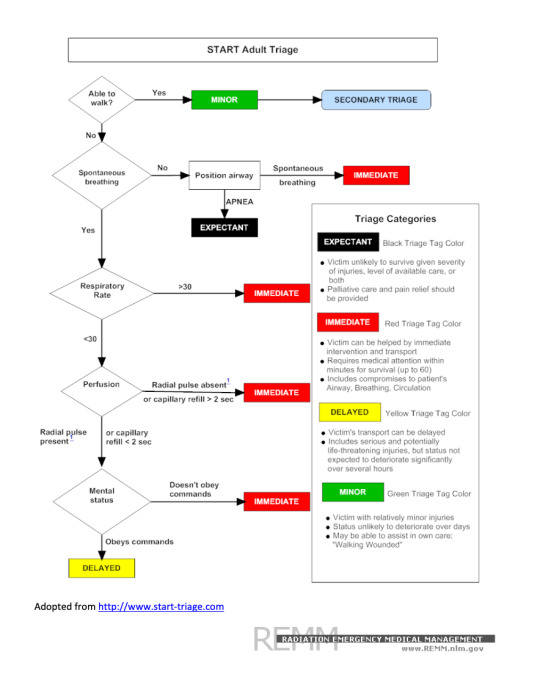
Triage is a dedicated job. A person working triage generally does not give any medical care- their only task is to determine what category each person fits into. The only exceptions to this are putting patient in recovery position to keep their airway open and the application of a tourniquet for severe limb bleeding. These are two very quick, bang-for-buck procedures that can be relatively easily used in this setting and won’t slow down the triager.
Speaking of that, time spent with each person is minimal. It may be a few seconds with someone who is obviously Minor, Immediate, or Expectant, but up to a few minutes for someone who is Delayed (due to needing to go through the whole algorithm). As soon as a determination is made, however, the triage person needs to move on to the next victim. The goal is to get through as many people as possible.
The consequence of not having a great JIT training becomes very pronounced here- in addition to spending way too much time with each patient, they also have to spend a lot of energy determining who falls into what categories. This then makes it a lot more difficult for them when a family member urges them to make another triage decision.
Doctors at the Scene:

In the episode, there were a lot of doctors who went out to the crash site to provide care. IRL, you don’t want doctors on the scene at all if you can avoid it. Here’s a couple of reasons why:
1. Doctors are not trained for fieldwork. Working in a hospital emergency department is very, very different from working on the side of the road in poor visibility with an overturned car that’s also on fire. EMTs, paramedics, firefighters, and police are all trained to be able to keep themselves safe in inherently dangerous situations. Since docs are not (at least, not in the same way), they’re a lot more likely to become another victim (as ____ did in the episode when she fell down the hill).
2. Pretty much any life-saving intervention that would need done on a scene like this could be done by a paramedic. Things like airways, emergency meds, tourniquets, IVs, IOs, fluids, splints, chest darts and occlusive dressings can all be provided by a paramedic or in some cases an EMT. Anyone needing more than this would be black tagged anyway, if only because you’re not going to have things like a portable ultrasound machine or chest tubes to do doc-level procedures.
3. Doctors are much more useful receiving patients at the hospital. In the hospital, not only are the docs kept safe, but they’re needed to do full trauma assessments and surgery and other definitive care. There’s about to be a surge of high-acuity patients that need care only docs can provide, and you want as many of them as possible ready to give it.
4. Doctors (and nurses, and paramedics) actually suck at triage. One thing about triage not talked about above is that anyone can do it. A good JIT instructor can train someone to use that algorithm in about 10 minutes even if they’ve never put hands on a patient before. And they’re probably going to be better at it than the clinical staff. Why? Because clinical staff know how to treat injuries. They know if they do just this one thing the patient has better odds of survival. You want someone who will go in and sort people without being able to do anything about their situation. Aides, transporters, techs, and students are great for this. Doctors and nurses? Not so much. Plus, as mentioned above, you need them to receive patients.
I understand they were doing this because the main characters were docs and it would be hard to do a whole ep of them waiting around in the ED for the incoming patients. But really. Doctors are expensive. Keep them where they’re useful. And alive.
A Note on Firefighters:
It’s not wholly fair to say that doctors would never, ever be at a scene. In certain cases it would be beneficial to have a doc on scene to do something a more field-friendly professional couldn’t do. I can’t think of a scene where the benefits would outweigh the risks at the moment, but it is technically a possibility.
If this happens, however, the doc is still just doing those specific medical procedures- they’re not triaging, they’re not managing resources, and they’re certainly not providing rescue services.
There were a lot of firefighters hanging out in the background of this ep. Do you know what firefighters do at a scene like this? They make it safe and they rescue people. Got an overturned car? Get a firefighter to stabilize it before you climb in. Car on fire? Firefighters are pretty good at putting those suckers out. Car fell down a hill? A firefighter can help you with that too. Got a car full of cement with a guy trapped inside whose slowly losing the ability to breathe and regulate his body temp? Slap a red tag on that bad boy and get a firefighter to pry open the door.
Rescue is their job. It’s what they’re trained for and what they’re good at. Half of the crappy things that happened in this ep only happened because the docs had no idea that firefighters are a lot better at rescue than they are.
Admittedly, their JIT training should have covered that. But once again, here we are.
Last Points:

That was a cool macgyverism warming the saline on the car engine. But hot damn, 4-5 L of fluid is a LOT of fluid to pump into someone with normal blood volume in a very short amount of time. That in itself could kill him by causing fluid overload or seriously low (relative) electrolyte levels.
Also that’s a lot of fluid someone else could use. I would have preferred to just support his breathing and warm him up later than waste all that fluid.
Stapling shut wounds doesn’t stop the bleeding. It just makes it internal bleeding. The blood is still lost. You could tourniquet that leg though.
Also who the hell brought staples to this scene??
You wouldn’t do a chest tube at the scene- you’d do a needle thoracostomy (chest dart) if absolutely necessary and transport ASAP.
You really, really, really wouldn’t do CPR on scene. Someone who needs CPR needs a black tag.
“If you knew how strong she was you wouldn’t be doing this” they captured a difficult part of triage really well with this line.
Promising someone that it will be alright or that you’ll find one of their family members is a really, really dangerous thing to do (and that does come back to bite Dr. Rorish, who should know better, in the episode).
That is not how you reduce (set) a shoulder in a remote setting. It can be done by tying weight to the arm and letting it hang over the edge of something. This doesn’t work quickly but it (probably) won’t screw your shoulder up too bad. Also she could have done a cricothyrotomy with one hand as long as she had an assistant.
Also even if she did reduce her shoulder, she wouldn’t have use of it back, just less pain.
There’s a monitor screen at the front desk too. If a monitor alarms at the bedside, it’s also alarming there. And the monitors can tell whether it’s actual asystole or the leads fell off.
And, finally, it wouldn’t have been nearly as dramatic (or even worth making an episode about) had the responders been given an adequate training, the doctors stayed at the hospital, and the firefighters been utilized according to their job description. In fact, they probably couldn’t have had an episode. ...And that’s kinda the point.
Okay, Whew, Done. Hope you all learned something!
104 notes
·
View notes