#and act like endometrium outside the uterus but also in the other reproductive tissues. Such cells respond to the hormonal changes
Text

#The issue with Endometriosis isn't just the pain and disruption of lifestyle#but the fact that diagnosis may take anything upto 7 years#with a surgical procedure being required for a definitive diagnosis. The gold standard confirmatory test for endometriosis is Laparoscop#as such#is not curable but specially trained experts like Dr Chaitanya Ganapule offer state-of-the-art treatment options including 3 D Laparoscopic#Pune.#10 % of menstruating women suffer silently due to endometriosis. During the normal menstruation process#the cells of the uterus lining called endometrium build up & if there is no pregnancy#the cells shade up causing menstrual flow. Women with Endometriosis#too#develop such cells#which not only look#and act like endometrium outside the uterus but also in the other reproductive tissues. Such cells respond to the hormonal changes#so there is build-up & shedding of cells#causing small bleeding in the pelvis. This causes inflammation and scarring of endometrium tissues. The result is painful#heavy#long periods#and cramps.#The exact reason for this pain may be due to chemicals released during the process#hormonal changes etc.#Suffering in silence not only delays the diagnosis but complicates the treatment further. Medical management may have to be replaced by hig#So#when you feel#or realize that your menses or periods are far more painful and heavy compared to your friends and cousins#do visit a specialist who has extensive & practical knowledge of female reproductive issues & is capable of fixing the issue well in time.#Dr Chaitanya Ganapule MD has taken training from a specialized Endometriosis surgery institute in France for surgical management of Endomet#When you go to seek answers from the specialist It is important to jot down the questions#you need to seek answers for:#What causes the pain in the abdomen in Endometriosis?#Why it is so intense & not seem to be routine periods pain?
1 note
·
View note
Link
#Bloating#Constipation#Diarrhoea#endometriosis#Infertility#PainfulIntercourse#PainfulPeriods#PelvicPain
0 notes
Text
Endometriosis Treatment Market Stand Out As The Biggest Contributor To Global Growth 2018-2026
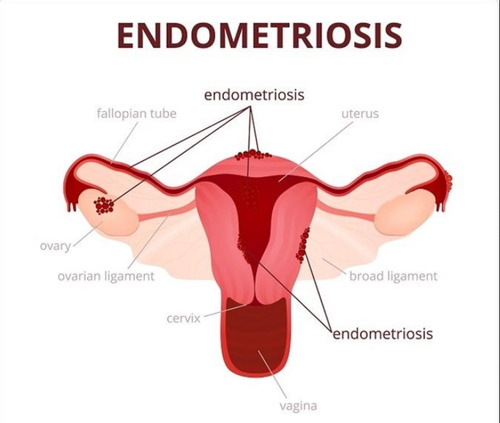
Endometriosis is a painful medical condition in which the tissue that lines in the inner part of the uterus i.e. endometrium grows outside the uterus. Endometriosis tissue is found in fallopian tubes, ovaries, and tissue lining the pelvis. In endometriosis, endometrial tissue which is displaced acts in the usual way i.e. it thickens, breaks down and eventually bleeds like in every menstrual cycle. As the displaced tissue has no other way to exit the body it gets trapped outside the uterus. Involvement of ovaries in endometriosis leads to formation of cysts called endometriomas. Due to this the surrounding tissues form an adhesion (abnormal bands of fibrous tissue that cause pelvic organs and tissues to stick to each other) or a scar tissue near the ovaries.
For In depth Information Get Sample Copy of this Report @ https://www.coherentmarketinsights.com/insight/request-sample/1999
Primary symptom of endometriosis is pain in pelvic area, which is associated with menstrual cycle. Other signs and symptoms of endometriosis include pain in pelvic region before menstrual cycle, pain in lower back during menstrual period, pain after intercourse in pelvic area, pain during urination, excessive bleeding between periods, fatigue, diarrhea, constipation, and nausea during menstrual cycle. Risk factors of endometriosis include infertility, onset of menstrual cycle at early age, short menstrual cycles, menopause at an older age, low body mass index, uterine abnormalities, and medical condition, which prevents normal passage of menstrual flow.
Endometriosis Treatment Market Drivers:-
Increasing research activities for development of new drugs for the global endometriosis treatment market is expected to be a major driver for growth of the market over the forecast period. For instance in 2017, AbbVie, biopharmaceutical company in co-operation with Neurocrine Biosciences Inc submitted New Drug Application (NDA) to the U.S. Food and drug Administration (FDA) for a new drug named elagolix. It is an orally administering gonadotropin releasing hormone antagonist, which is being evaluated for management of pain associated with endometriosis.
Launch of products by manufacturer is also expected to drive global endometriosis treatment market growth. For instance, in 2018, LASCO distributors in association with Bayer healthcare launched new drug visanne, which is indicated for endometriosis treatment.
Other factors such as increase in prevalence of endometriosis, robust pipeline, awareness about endometriosis is expected to support endometriosis treatment market growth. For instance, Triptoreline sponsored by University Hospital, Rouen is in Phase 3 Clinical Trials; Triptoreline cures deep endometriosis in the rectum , Myovant Sciences has Relugolix in phase 3 Clinical Trials; Relugolix ceases non-menstrual pelvic pain, Indocyannine Green sponsored by University Hospital in Phase 4 Clinical Trials; Indocyannine Green treats recto vaginal endometriosis, Dienogest sponsored by the University Of Hong Kong is in Phase 4 Clinical Trials; dienogest stops the reoccurance of endometriosis cyst, Merional sponsored by Cario University is in phase 3 Clinical Trials; Merional controls intrauterine insemination cycles in women having endometriosis.
According to a survey conducted by National Center for Biotechnology Information (NCBI), 2014, endometriosis is estimated to affect 10% of female in the reproductive age and more than 50% in infertility patients, which in turn is expected to fuel growth of the endometriosis treatment market over the forecast period.
Availability of alternative treatment options such as Intrauterine Systems (IUS) is key factor restarting growth of the market. IUS is a T-shaped device inserted in womb by the doctor. Moreover, treatment of endometriosis consists of use of oral contraceptives or GnRH agonists. Most of these therapies have adverse effects on the body due to hormonal changes and it also includes the risk of recurrence of endometriosis.
Endometriosis Treatment Market Regional Analysis:-
Asia Pacific endometriosis treatment market is projected to witness significant growth over the forecast period due to initiative taken by the government to improve health of women in Australia. According to the George institute of global health, in 2018, government of Australia allocated about US$ 2.5 million for research in the field of endometriosis. It includes around US$ 120,000 for campaigns, which will provide education and awareness regarding endometriosis and also a research grant for National Health and Medical Research Council.
Europe region is projected to witness growth in the endometriosis market over the forecast period due to robust drugs pipeline. For instance, Pleyris sponsored by University Magna Graecia is in Phase 3. According to a study conducted by BJOC: An International Journal of Obstetrics and Gynaecology, 2015, in Europe endometriosis affects more than 10% of premenopausal women and 30-50% of the women suffering from symptoms of endometriosis. Increasing number of endometriosis patients is fueling Europe endometriosis treatment market growth.
Endometriosis Treatment Market Key Players:-
Key players operating in global endometriosis treatment market include Astra Zeneca Plc., Eli Lilly and Company, AStellas Pharma, Bayer AG, Meditrina Pharmaceuticals, Abbvie, PfizerInc, Takeda Pharmaceutica, and Neurocrine Biosciences Inc
Request For Customization of Research Report @ https://www.coherentmarketinsights.com/insight/request-customization/1999
0 notes
Text
Common Gynecologic Problems and Treatment in Women
Most of the menstrual bleeding issues happen due to imbalance in the hormones within your body. Read this article to know the common gynecologic problems and their treatment procedures. This guide will also give you tips on finding the best gynecologist in New York.
Abnormal Uterine Bleeding
It refers to the issues linked to vaginal bleeding. It can be connected to the menstrual cycle but there are times where abnormal bleeding takes place before the beginning of the menstrual cycle. In some cases, it can occur when you are pregnant or after your menopause.
Most of the abnormal vaginal bleeding issues occur due to hormones imbalance which control the menstrual cycle. In cases where the vaginal bleeding is not associated with the menses it should be of great concern to you. This can occur in childhood when menstruation has not begun or during your pregnancy or after you get into menopause.
When Do You Need to Call Healthcare Provider?
You need to call the healthcare provider when you experience pelvic pain which occurs during sexual intercourse or menstruation, when the menstrual bleeding is in excess and when the menstrual periods last longer than 7 days.
The abnormal bleeding is associated with the following:
Young Pre-Puberty Girl
• Occurrence of an injury
• Sexual abuse
• Early Puberty
• Vaginal irritation
Woman of Reproductive Age
• An imbalance in the hormones
• Some types of tumors
• Use of birth control pills
Diagnosis and Treatment of Early Bleeding
The common evaluation of the early bleeding involves ultra sound. The diagnosis includes unexpected pregnancies and endometriosis. The treatment procedure involves the use of hormone birth control by the use of an injection to reduce the internal bleeding. There are also other prescriptions to slow down the internal bleeding and they should only be recommended to you by the doctor.
Endometriosis
The name of the condition comes from the word ‘endometrium’ which is the tissue aligning the uterus. When the woman is not pregnant, the tissue will build up and be shed at the end of each month. In the endometriosis condition, a tissue which acts like the endometrial is found outside the uterus.
However, unlike in the menstrual flow, the blood from the uterus will have no place to go. The tissues which surround the endometrium will become inflamed or swollen. This inflammation can then produce a scar tissue around the area of endometriosis.
Treatment
They are based on the symptoms displayed by the patient and the desire for pregnancy. When looking for treatment or diagnosis of any of the above conditions, it is always good to make sure you take your time to choose the best gynecologist in New York.
0 notes
Text
What is endometriosis?
Endometriosis is a chronic condition, and as such, there is no cure. However, it can be treated to control the pain and prevent the symptoms from worsening. One treatment option that is suitable for many women is hormone therapy. This uses a combination of estrogen and progestin to cease menstruation.
With endometriosis, the endometrial-like tissue acts as endometrial tissue would — it thickens, breaks down, and bleeds with each menstrual cycle. But because this tissue has no way to exit your body, it becomes trapped. When endometriosis involves the ovaries, cysts called endometriomas may form. Surrounding tissue can become irritated, eventually developing scar tissue and adhesions — abnormal bands of fibrous tissue that can cause pelvic tissues and organs to stick to each other.
Endometriosis can cause pain — sometimes severe — especially during menstrual periods. Fertility problems also may develop. Fortunately, effective treatments are available.
There is no cure for endometriosis. Hormone therapy or taking out tissue with laparoscopic surgery can ease the pain. But pain often returns within a year or two. Taking out the ovaries (oophorectomy) and the uterus (hysterectomy) usually relieves pain.
Symptoms
The primary symptom of endometriosis is pelvic pain, often associated with menstrual periods. Although many experience the cramping during their menstrual periods, those with endometriosis typically describe menstrual pain that’s far worse than usual. Pain also may increase over time.
Common signs and symptoms of endometriosis include
Painful periods (dysmenorrhea). Pelvic pain and cramping may begin before and extend several days into a menstrual period. You may also have lower back and abdominal pain.
Pain with intercourse. This is the number one complaint with endometriosis.
Pain with bowel movements or urination. You’re most likely to experience these symptoms during a menstrual period.
Excessive bleeding. You may experience occasional heavy menstrual periods or bleeding between periods (intermenstrual bleeding).
Infertility. Sometimes, endometriosis is first diagnosed in those seeking infertility treatment.
Other signs and symptoms. You may experience fatigue, diarrhea, constipation, bloating, or nausea, especially during menstrual periods.
The severity of your pain isn’t necessarily a reliable indicator of the extent of the condition. You could have mild endometriosis with severe pain, or you could have advanced endometriosis with little or no discomfort.
Endometriosis is sometimes mistaken for other conditions that can cause pelvic pain, such as pelvic inflammatory disease (PID) or ovarian cysts. It may be confused with irritable bowel syndrome (IBS), a condition that causes bouts of diarrhea, constipation, and abdominal cramping. IBS can accompany endometriosis, which can complicate the diagnosis.
When to see a doctor
See your doctor if you have signs and symptoms that may indicate endometriosis.
Endometriosis can be a challenging condition to manage. An early diagnosis, a multidisciplinary medical team, and an understanding of your diagnosis may result in better management of your symptoms.
Now the Hard Truth
Although the exact cause of endometriosis is not absolute, possible explanations include:
Retrograde menstruation. In retrograde menstruation, menstrual blood containing endometrial cells flows back through the fallopian tubes and into the pelvic cavity instead of out of the body. These endometrial cells stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to thicken and bleed throughout each menstrual cycle.
Transformation of peritoneal cells. In what’s known as the “induction theory,” experts propose that hormones or immune factors promote the change of peritoneal cells — cells that line the inner side of your abdomen — into endometrial-like cells.
Embryonic cell transformation. Hormones such as estrogen may transform embryonic cells — cells in the earliest stages of development — into endometrial-like cell implants during puberty.
Surgical scar implantation. After a surgery, such as a hysterectomy or C-section, endometrial cells may attach to a surgical incision.
Endometrial cell transport. The blood vessels or tissue fluid (lymphatic) system may transport endometrial cells to other parts of the body.
Immune system disorder. A problem with the immune system may make the body unable to recognize and destroy endometrial-like tissue that’s growing outside the uterus.
Risk factors
Several factors place you at greater risk of developing endometriosis, such as:
Never giving birth
Starting your period at an early age
Going through menopause at an older age
Short menstrual cycles — for instance, less than 27 days
Heavy menstrual periods that last longer than seven days
Having higher levels of estrogen in your body or greater lifetime exposure to estrogen your body produces
Low body mass index
One or more relatives (mother, aunt or sister) with endometriosis
Any medical condition that prevents the standard passage of menstrual flow out of the body
Reproductive tract abnormalities
Endometriosis usually develops several years after the onset of menstruation (menarche). Signs and symptoms of endometriosis may temporarily improve with pregnancy and may go away entirely with menopause unless you’re taking estrogen.
Complications
Infertility
Fertilization and implantation
The main complication of endometriosis is impaired fertility. Approximately one-third to one-half of women with endometriosis have difficulty getting pregnant.
For pregnancy to occur, an egg must be released from an ovary, travel through the neighboring fallopian tube, become fertilized by a sperm cell, and attach itself to the uterine wall to begin development. Endometriosis may obstruct the tubes and keep the egg and sperm from uniting. But the condition also seems to affect fertility in less-direct ways, such as by damaging the sperm or egg.
Even so, many with mild to moderate endometriosis can still conceive and carry a pregnancy to term. Doctors sometimes advise those with endometriosis not to delay having children because the condition may worsen with time.
Cancer
Ovarian cancer does occur at higher than expected rates in those with endometriosis. But the overall lifetime risk of ovarian cancer is low, to begin with. Some studies suggest that endometriosis increases that risk, but it’s still relatively low. Another type of cancer, endometriosis-associated adenocarcinoma, can develop later in life in those who have had endometriosis.
https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
More Hard Facts
In women with endometriosis, the tissue typically spreads into the pelvic area but, in some cases, can travel as far as the chest cavity. The endometrium, no matter where it applies in the body, is on the same cycle as a woman’s period, which is regulated by the female hormone estrogen.
The most recent studies have shown that endometriosis recurs at a rate of 20% to 40% within five years following conservative surgery. The use of oral contraceptives, other suppressive hormonal therapy, or progesterone intrauterine device (IUD) after surgery has been shown to reduce the recurrence of pain symptoms.
Where else can endometriosis spread to in the body?
Bowels
Stomach/ Stomach Cavity
Anus
Vagina
Kidneys
Liver
Intestines
Lungs
Kidneys
This slideshow requires JavaScript.
Can Endometriosis Become Life Threatening?
YES, yes it can. If not correctly diagnosed in time and treated and the endometriosis has spread to your other organs or attached to the ovaries and caused ovarian cancer, it can become life-threatening.
Diet
Because endometriosis is an autoimmune disorder, dairy is the number one anti-inflammatory food to avoid! Period!
Studies show that you should void gluten, beer, and fried foods.
Some evidence suggests that a high intake of red meat may be associated with higher levels of estrogen in the blood ( 12, 13 ). Since endometriosis is an estrogen-dependent disease, higher levels of estrogen in the blood may increase the risk of the condition (14 ).
“Too much caffeine once again creates inflammation in the body and aggravates the digestive system.” “Dairy products can cause inflammation through hormones,” Hartung said. “Dairy products containing growth hormones and antibiotics can also worsen endometriosis symptoms.”
Some people can easily digest yogurt, but not milk, or butter, but not cheese. In the context of endometriosis, it’s ideal for eliminating all dairy entirely for at least a period. You can always consider slowly reintroducing it after you’ve found sustainable relief from endometriosis.
Several Personal Stories
At the age of 17, after my second son was born, I was diagnosed with endometriosis. I went on Depo-Provera at the time. This caused me not to have monthly menstrual cycles. I did not go off of this medication until around 1996. Once off of this medication, my monthly cycles were not consistent; they were painful and very gross, to say the least. My first laparoscopy discovered that the endometriosis was on my small bowel and my ovaries. The doctor did his best to remove it and suggested I have a hysterectomy. I was stubborn and wanted to have another child. After 3 years of unsuccessful fertility treatments, I could no longer take it. I opted for a second laparoscopy to remove more endometriosis growth and spread and went back on the Dep-Provera. By 2005, I was again attempting to have another child, with no success; also, my cycles were horrific. I was in the process of planning a hysterectomy in Septemeber of 2009, and low and behold, I began hemorrhaging basically. I had an emergency hysterectomy on 9/11/2009. The endometriosis covered my ovaries, bowels, parts of my intestines, my entire uterus, part of my bladder. It also spread to my cervix and fallopian tubes. My doctor said my ovaries were the size of plums, and my uterus was the size of a grapefruit. After my hysterectomy, I felt much better. That was my first bought with an autoimmune disease. I genuinely believe that was just the beginning. If you have read this blog prior, you know I have numerous autoimmune illnesses, and they are still rearing their ugly heads.
My cousin, at the age of 21, had a hysterectomy for endometriosis.
Her sister, my other cousin, by the age of 30, had a hysterectomy due to endometriosis. After her hysterectomy, the doctors later found that the endometriosis spread into her stomach cavity.
My aunt had endometriosis and hysterectomy in her late 20’s, early 30’s. She has stomach issues too.
My grandmother also dealt with endometriosis. She then developed lupus, lung issues, rheumatoid arthritis, etc.
I know numerous ladies that are suffering now, and it has spread to their anus, lungs, and other parts of their bodies.
This slideshow requires JavaScript.
I genuinely see a pattern with this painful autoimmune illness that is still so unresearched and not enough attention surrounding. Most autoimmune diseases are underfunded; people are unaware; the saying goes, “you don’t get it until you get it.” It is true, it is a fact!
You learn to become a warrior, a true survivor, you learn coping mechanisms become pain medications are no longer prescribed, the doctors are baffled, and treatment is scarce. It’s a mystery: trial and error.
So that is the skinny on endometriosis.
If you have a story about your personal experience with endometriosis, I would love to feature you here on the blog; this will help spread awareness, and honestly talking about it may help you and others.
You are NOT alone!
Endometriosis affects about 200 million women worldwide and nearly 1 out of every 10 women in the United States. Yet the disease is often misdiagnosed or missed altogether, says the Endometriosis Foundation of America (EndoFound) as of March 2020.
https://www.everydayhealth.com/endometriosis/awareness-month/#:~:text=Endometriosis%20affects%20about%20200%20million,Foundation%20of%20America%20(EndoFound
Dedicated to my friend Dawn!
When things are tough, you are tougher, you are a warrior and ENDO Strong!
September Awareness – Topic #1 – Endometriosis What is endometriosis? Endometriosis is a chronic condition, and as such, there is no cure. However, it can be treated to control the pain and prevent the symptoms from worsening.
#autoimmune disease#autoimmune illness#awareness#chronic illness#chronic pain#endo strong#endometriosis#faith#fighter#health#hope#Mental well-being#need a cure#personal#self awareness#Self care#self healing#warriors#well-being
0 notes
Text
What Is Endometriosis? Symptoms, Causes, Treatment, And Diet Tips
New Post has been published on http://healingawerness.com/getting-healthy/getting-healthy-women/what-is-endometriosis-symptoms-causes-treatment-and-diet-tips/
What Is Endometriosis? Symptoms, Causes, Treatment, And Diet Tips
Shaheen Naser Hyderabd040-395603080 June 24, 2019
Endometriosis is a medical condition that affects 1 in 10 premenopausal women worldwide (1). That is approximately 176 million women! It is a serious issue, which may cause complications like infertility and even cancer if left untreated.
Is your menstrual cycle irregular but extremely painful? Have you been experiencing unusually heavy bleeding as well? Chances are you could be dealing with endometriosis. Keep reading to find more about this condition and how you can manage it.
Table Of Contents
What Is Endometriosis?
Shutterstock
Endometriosis is a painful medical condition that causes the lining of the uterus (endometrium) to grow outside it. It mainly affects the ovaries, fallopian tubes, and the lining of the pelvis (2). In rare cases, the endometrial tissue may also spread beyond the pelvic organs.
The displaced endometrial lining acts as it normally would and will thicken, break down, and bleed every cycle. However, since the endometrium is outside the uterus, it doesn’t have any way to exit your body, thereby becoming trapped.
If endometriosis involves the ovaries, cysts referred to as endometriomas may develop.
Depending on the location, size, number, and depth of the endometrial implants, endometriosis can be classified into the following stages.
Stages Of Endometriosis
Endometriosis can be divided into four stages (3):
Stage 1 – Minimal: Small lesions, along with shallow endometrial implants on the ovaries, characterize minimal endometriosis. Inflammation in or around the cavity may also be noticed.
Stage 2 – Mild: Mild endometriosis is characterized by light lesions accompanied by shallow implants on the ovary and pelvic lining.
Stage 3 – Moderate: This stage is characterized by deep implants on your ovary as well as your pelvic lining. More lesions may also be observed.
Stage 4 – Severe: Stage 4 is the most severe stage of endometriosis. It involves deep implants on your pelvic lining and ovaries. This may also be accompanied by lesions on your fallopian tubes and/or bowels.
The exact cause of endometriosis is yet to be fully understood. Researchers have stated multiple theories, but none of them have been fully understood.
What Causes Endometriosis?
Possible factors that could be causing endometriosis include (4):
Embryonic cells that are lining the abdomen and pelvis may end up developing into endometrial tissue within these cavities.
Instead of leaving the body as it usually does, menstrual blood could have entered the pelvis and fallopian tubes.
Endometriosis could be present in the developing fetus, which may be triggered by estrogen levels.
Surgical procedures like hysterectomy or C-section.
An immune system disorder can prevent your body from recognizing and destroying the endometrial tissue that has been growing outside your uterus.
The following section lists the signs and symptoms of the condition.
Symptoms Of Endometriosis
The signs and symptoms associated with endometriosis include (3):
Dysmenorrhea or painful periods
Pain during intercourse
Pain while urinating or during a bowel movement
Excessive bleeding during or in between your periods
Infertility or inability to conceive
Other signs often associated with endometriosis include constipation or diarrhea, bloating, nausea, and fatigue.
Certain factors may put a woman at an increased risk of developing endometriosis. They are as follows.
Risk Factors
Factors that can increase your risk of getting endometriosis include (5):
Opting never to give birth
Early onset of the menstrual cycle
Late onset of menopause
Short menstrual cycles that are less than 27 days
Heavy menstrual bleeding that lasts for more than 7 days
High estrogen levels in your body
A low body mass index
Having one or more family members (women) with endometriosis
Having any medical condition that prevents normal passage of menstrual blood during your menstrual cycle
Abnormalities with your reproductive tract
If endometriosis is severe or left untreated, it may eventually lead to the following complications.
Complications
Two of the most severe complications associated with endometriosis are infertility and cancer.
About half of the women with endometriosis may experience impaired fertility or may have difficulties in conceiving.
The incidence of cancer, especially ovarian cancer and endometriosis-associated adenocarcinoma, is also observed to be higher in women dealing with endometriosis. However, it should be noted that the risk of developing ovarian cancer is low generally.
If you notice any of the symptoms associated with endometriosis or if you think you may be at risk, it is best to get yourself diagnosed to rule out the possibilities.
How Is Endometriosis Diagnosed?
Diagnosis of endometriosis is usually based on your symptoms. Tests that your doctor may suggest to check your symptoms and detect physical clues are (6):
A pelvic examination to look for abnormalities like cysts or scars behind the uterus
An ultrasound to detect cysts that surface with endometriosis
Magnetic Resonance Imaging (MRI) to find out the exact location and size of the endometrial implants
Laparoscopy to help in looking for signs of endometriosis outside your uterus
Depending on the severity of your condition, your doctor may discuss different treatment approaches with you to deal with endometriosis.
How To Treat Endometriosis
Treatment for endometriosis can include (7):
Warm Baths Or Heating Pads
Heating pads and warm baths can help in alleviating pain in mild to moderate cases of endometriosis.
Alternative Medicine
Alternative treatment approaches for endometriosis include acupuncture, which may help relieve symptoms of pain.
Surgery may be conservative, where only the endometrial implants are removed while the uterus and ovaries are preserved. This procedure is known as laparoscopic surgery.
Hysterectomy (surgical removal of the uterus) and oophorectomy (surgical removal of the ovaries) were previously thought of as the most effective treatments for endometriosis. But, of late, doctors are focusing more on only the removal of the endometrial implants.
Fertility Treatment
Fertility treatment may involve stimulation of your ovaries or producing more eggs in vitro. Discuss the treatment options with your doctor to find which one will work best for you.
Pain Medications
Over-the-counter medications like nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB) or naproxen sodium (Aleve) may also be prescribed to relieve symptoms of pain usually associated with menstrual cramps.
Your diet may also play a significant role if you have endometriosis. The following are some diet tips that may help.
What Foods To Eat If You Have Endometriosis?
Certain foods may reduce one’s risk of developing endometriosis. They include (8):
Fresh fruits and vegetables
Fish oils and omega-3 fatty acid-rich foods like fatty fish and flax seeds
Dairy products
Vitamin D-rich foods like tuna, mackerel, cheese, and egg yolks
Foods that are associated with an increased risk of endometriosis and must be avoided are:
Red meat
Alcohol
Trans fats like junk foods and deep fried foods
There is no cure for endometriosis as the exact causes haven’t been determined yet. But this does not mean that you cannot go on with your daily routine. The treatment methods mentioned in the article can help you manage the pain and other associated issues.
We hope all your doubts and queries related to endometriosis were covered in this post. Do you have any further questions? Do not hesitate to ask us in the comments section below.
Expert’s Answers for Readers Questions
What happens if endometriosis is left untreated?
Leaving endometriosis untreated can increase your risk of developing complications from it like infertility and cancer, which may become life-threatening as well.
Is eating chicken bad for those with endometriosis?
Chicken is lean meat like fish and turkey. It is thus a healthier diet choice than red meat.
Can endometriosis cause weight gain?
While endometriosis is associated with weight gain in a few affected women, the exact relationship between the two is yet to be determined. One possible explanation is estrogen dominance, which may manifest itself externally as weight gain.
Can stress make endometriosis worse?
The pain associated with endometriosis can trigger high levels of stress, which, in turn, has an exacerbating effect on endometriosis.
Can treating endometriosis improve my fertility?
Yes, treating endometriosis can have a positive effect and may improve a woman’s fertility.
Can you get pregnant if you have endometriosis?
Almost one-third of women with endometriosis were observed to conceive naturally, without the need for any fertility treatment.
What is the difference between endometriosis and menstrual cramps?
Though a few symptoms of endometriosis and menstrual cramps may be similar, both the conditions are, in fact, different.
Menstrual cramps are caused due to the contraction of the uterus. Pain, nausea, constipation, and diarrhea are some of the common signs associated with menstrual cramps, which are quite similar to the symptoms experienced by those with endometriosis.
Endometriosis, on the other hand, is caused when the endometrial tissues are implanted outside the uterus instead of inside it. This implantation may cause inflammation, which triggers the pain.
References
“Endometriosis Fact Sheet” The American College of Obstetricians and Gynecologists.
“Endometriosis: Epidemiology, Diagnosis and Clinical Management.” Current Obstetrics and Gynecology Reports, US National Library Of Medicine, National Institutes of Health.
“Endometriosis: Epidemiology, Diagnosis and Clinical Management” Current Obstetrics and Gynecology Reports, US National Library Of Medicine, National Institutes of Health.
“What causes endometriosis?” Institute for Quality and Efficiency in Health Care, US National Library Of Medicine, National Institutes of Health.
“Risk factors associated with endometriosis: importance of study population for characterizing disease in the ENDO Study” American Journal of Obstetrics and Gynecology, US National Library Of Medicine, National Institutes of Health.
“Endometriosis” BMJ, US National Library Of Medicine, National Institutes of Health.
“Treatment options for endometriosis” Institute for Quality and Efficiency in Health Care, US National Library Of Medicine, National Institutes of Health.
“Influence of diet on the risk of developing endometriosis.” Ginekologia Polska, US National Library Of Medicine, National Institutes of Health.
The following two tabs change content below.
Latest posts by Shaheen Naser (see all)
What Is Endometriosis? Symptoms, Causes, Treatment, And Diet Tips – June 24, 2019
11 Natural Remedies To Get Rid Of A Staph Infection + Causes And Symptoms – May 28, 2019
16 Easy Ways To Fall Asleep Faster – May 21, 2019
What Is Hepatitis B – Symptoms, Causes, Diagnosis, And Treatment – May 16, 2019
10 Natural Remedies To Get Rid Of Impetigo + Causes And Symptoms – May 14, 2019
Shaheen Naser
RELATED ARTICLES
Source: https://www.stylecraze.com/articles/endometriosis-causes-symptoms-treatment-diet/
0 notes
Text
Because it's important enough to share
Endometriosis
Endometriosis (en-doe-me-tree-O-sis) is an often painful disorder in which tissue that normally lines the inside of your uterus — the endometrium — grows outside your uterus. Endometriosis most commonly involves your ovaries, fallopian tubes and the tissue lining your pelvis. Rarely, endometrial tissue may spread beyond pelvic organs.
With endometriosis, displaced endometrial tissue continues to act as it normally would — it thickens, breaks down and bleeds with each menstrual cycle. Because this displaced tissue has no way to exit your body, it becomes trapped. When endometriosis involves the ovaries, cysts called endometriomas may form. Surrounding tissue can become irritated, eventually developing scar tissue and adhesions — abnormal bands of fibrous tissue that can cause pelvic tissues and organs to stick to each other.
Endometriosis can cause pain — sometimes severe — especially during your period. Fertility problems also may develop. Fortunately, effective treatments are available.
Symptoms
The primary symptom of endometriosis is pelvic pain, often associated with your menstrual period. Although many women experience cramping during their menstrual period, women with endometriosis typically describe menstrual pain that's far worse than usual. They also tend to report that the pain increases over time.
Common signs and symptoms of endometriosis may include:
• Painful periods (dysmenorrhea). Pelvic pain and cramping may begin before your period and extend several days into your period. You may also have lower back and abdominal pain.
• Pain with intercourse. Pain during or after sex is common with endometriosis.
• Pain with bowel movements or urination. You're most likely to experience these symptoms during your period.
• Excessive bleeding. You may experience occasional heavy periods (menorrhagia) or bleeding between periods (menometrorrhagia).
• Infertility. Endometriosis is first diagnosed in some women who are seeking treatment for infertility.
• Other symptoms. You may also experience fatigue, diarrhea, constipation, bloating or nausea, especially during menstrual periods.
The severity of your pain isn't necessarily a reliable indicator of the extent of the condition. Some women with mild endometriosis have intense pain, while others with advanced endometriosis may have little pain or even no pain at all.
Endometriosis is sometimes mistaken for other conditions that can cause pelvic pain, such as pelvic inflammatory disease (PID) or ovarian cysts. It may be confused with irritable bowel syndrome (IBS), a condition that causes bouts of diarrhea, constipation and abdominal cramping. IBS can accompany endometriosis, which can complicate the diagnosis.
When to see a doctor
See your doctor if you have signs and symptoms that may indicate endometriosis.
Endometriosis can be a challenging condition to manage. An early diagnosis, a multidisciplinary medical team and an understanding of your diagnosis may result in better management of your symptoms.
Causes
Although the exact cause of endometriosis is not certain, possible explanations include:
• Retrograde menstruation. In retrograde menstruation, menstrual blood containing endometrial cells flows back through the fallopian tubes and into the pelvic cavity instead of out of the body. These displaced endometrial cells stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to thicken and bleed over the course of each menstrual cycle.
• Transformation of peritoneal cells. In what's known as the "induction theory," experts propose that hormones or immune factors promote transformation of peritoneal cells — cells that line the inner side of your abdomen — into endometrial cells.
• Embryonic cell transformation. Hormones such as estrogen may transform embryonic cells — cells in the earliest stages of development — into endometrial cell implants during puberty.
• Surgical scar implantation. After a surgery, such as a hysterectomy or C-section, endometrial cells may attach to a surgical incision.
• Endometrial cells transport. The blood vessels or tissue fluid (lymphatic) system may transport endometrial cells to other parts of the body.
• Immune system disorder. It's possible that a problem with the immune system may make the body unable to recognize and destroy endometrial tissue that's growing outside the uterus.
Risk factors
Several factors place you at greater risk of developing endometriosis, such as:
• Never giving birth
• Starting your period at an early age
• Going through menopause at an older age
• Short menstrual cycles — for instance, less than 27 days
• Having higher levels of estrogen in your body or a greater lifetime exposure to estrogen your body produces
• Low body mass index
• Alcohol consumption
• One or more relatives (mother, aunt or sister) with endometriosis
• Any medical condition that prevents the normal passage of menstrual flow out of the body
• Uterine abnormalities
Endometriosis usually develops several years after the onset of menstruation (menarche). Signs and symptoms of endometriosis end temporarily with pregnancy and end permanently with menopause, unless you're taking estrogen.
Infertility
The main complication of endometriosis is impaired fertility. Approximately one-third to one-half of women with endometriosis have difficulty getting pregnant.
For pregnancy to occur, an egg must be released from an ovary, travel through the neighboring fallopian tube, become fertilized by a sperm cell and attach itself to the uterine wall to begin development. Endometriosis may obstruct the tube and keep the egg and sperm from uniting. But the condition also seems to affect fertility in less-direct ways, such as damage to the sperm or egg.
Even so, many women with mild to moderate endometriosis can still conceive and carry a pregnancy to term. Doctors sometimes advise women with endometriosis not to delay having children because the condition may worsen with time.
Ovarian cancer
Ovarian cancer does occur at higher than expected rates in women with endometriosis. But the overall lifetime risk of ovarian cancer is low to begin with. Some studies suggest that endometriosis increases that risk, but it's still relatively low. Although rare, another type of cancer — endometriosis-associated adenocarcinoma — can develop later in life in women who have had endometriosis.
Transvaginal ultrasound
To diagnose endometriosis and other conditions that can cause pelvic pain, your doctor will ask you to describe your symptoms, including the location of your pain and when it occurs.
Tests to check for physical clues of endometriosis include:
• Pelvic exam. During a pelvic exam, your doctor manually feels (palpates) areas in your pelvis for abnormalities, such as cysts on your reproductive organs or scars behind your uterus. Often it's not possible to feel small areas of endometriosis, unless they've caused a cyst to form.
• Ultrasound. This test uses high-frequency sound waves to create images of the inside of your body. To capture the images, a device called a transducer is either pressed against your abdomen or inserted into your vagina (transvaginal ultrasound). Both types of ultrasound may be done to get the best view of your reproductive organs. Ultrasound imaging won't definitively tell your doctor whether you have endometriosis, but it can identify cysts associated with endometriosis (endometriomas).
• Magnetic resonance imaging (MRI). An MRI is an exam that uses a magnetic field and radio waves to create detailed images of the organs and tissues within your body. For some women, an MRI helps with surgical planning, giving your surgeon detailed information about the location and size of endometrial implants.
• Laparoscopy. In some cases, your doctor may refer you to a surgeon for a procedure (laparoscopy) that allows the surgeon to view inside your abdomen. While you're under general anesthesia, your surgeon makes a tiny incision near your navel and inserts a slender viewing instrument (laparoscope), looking for signs of endometrial tissue outside the uterus.
A laparoscopy can provide information about the location, extent and size of the endometrial implants to help determine the best treatment options. Your surgeon may take a tissue sample (biopsy) for further testing. Often, with proper surgical planning, your surgeon can fully treat endometriosis during the laparoscopy so that you only need one surgery.
Treatment
Treatment for endometriosis usually involves medication or surgery. The approach you and your doctor choose will depend on how severe your signs and symptoms are and whether you hope to become pregnant.
Doctors typically recommend trying conservative treatment approaches first, opting for surgery if initial treatment fails.
Pain medication
Your doctor may recommend that you take an over-the-counter pain reliever, such as the nonsteroidal anti-inflammatory drugs (NSAIDs) ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve, others), to help ease painful menstrual cramps.
If you find that taking the maximum dose of these medications doesn't provide full relief, you may need to try another approach to manage your signs and symptoms.
Hormone therapy
Supplemental hormones are sometimes effective in reducing or eliminating the pain of endometriosis. The rise and fall of hormones during the menstrual cycle causes endometrial implants to thicken, break down and bleed. Hormone medication may slow endometrial tissue growth and prevent new implants of endometrial tissue.
Hormone therapy isn't a permanent fix for endometriosis. You could experience a return of your symptoms after stopping treatment.
Therapies used to treat endometriosis include:
• Hormonal contraceptives. Birth control pills, patches and vaginal rings help control the hormones responsible for the buildup of endometrial tissue each month. Most women have lighter and shorter menstrual flow when they're using a hormonal contraceptive. Using hormonal contraceptives — especially continuous cycle regimens — may reduce or eliminate pain for some women.
• Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists. These drugs block the production of ovarian-stimulating hormones, lowering estrogen levels and preventing menstruation. This causes endometrial tissue to shrink. Because these drugs create an artificial menopause, taking a low dose of estrogen or progestin along with Gn-RH agonists and antagonists may decrease menopausal side effects, such as hot flashes, vaginal dryness and bone loss. Your periods and the ability to get pregnant return when you stop taking the medication.
• Progestin therapy. A variety of progestin therapies, including an intrauterine device (Mirena), contraceptive implant, contraceptive injection (Depo-Provera) or progestin pills, can halt menstrual periods and the growth of endometrial implants, which may relieve endometriosis signs and symptoms.
• Aromatase inhibitors. Aromatase inhibitors are a class of medicines that reduce the amount of estrogen in your body. Your doctor may recommend an aromatase inhibitor along with a progestin or combination hormonal contraceptive to treat endometriosis.
Conservative surgery for endometriosis
If you have endometriosis and are trying to become pregnant, surgery to remove the endometriosis implants while preserving your uterus and ovaries (conservative surgery) may increase your chances of success. If you have severe pain from endometriosis, you may also benefit from surgery — however, endometriosis and pain may return.
Your doctor may do this procedure laparoscopically or, less commonly, through traditional abdominal surgery in more-extensive cases. Even in severe cases of endometriosis, most women can be treated with laparoscopic surgery.
In laparoscopic surgery, your surgeon inserts a slender viewing instrument (laparoscope) through a small incision near your navel and inserts instruments to remove endometrial tissue through another small incision. After surgery, your doctor may recommend taking hormone medication to help improve your pain.
Fertility treatment
Women with endometriosis can have trouble conceiving. If you're having difficulty getting pregnant, your doctor may recommend fertility treatment supervised by a fertility specialist. Fertility treatment ranges from stimulating your ovaries to make more eggs to in vitro fertilization. Which treatment is right for you depends on your personal situation.
Hysterectomy with removal of the ovaries
Surgery to remove the uterus (hysterectomy) and ovaries (oophorectomy) was once considered the most effective treatment for endometriosis. But endometriosis experts are moving away from this approach, instead focusing on the careful and thorough removal of all endometriosis tissue.
0 notes
Text
5 Natural Proven-Effective Steps to Cure Endometriosis
How To Cure Endometriosis
Endometriosis affects approximately 1 in 10 women during their reproductive years (ie. ages 15 to 49).
Endometriosis is the abnormal growth of cells (endometrial cells), similar to those that form the inside of the uterus, but in areas outside of the uterus including: fallopian tubes, ovaries, intestines and other tissues lining your pelvis. Rarely, endometrial tissue may spread beyond pelvic organs.
Over time, this displaced endometrial tissue continues to act as it normally would inside your uterus— it thickens, breaks down and bleeds with each menstrual cycle.
Since this displaced tissue has no way to escape your body, it becomes trapped. If endometriosis involves the ovaries, cysts called endometriomas may also form. The tissue surrounding these cysts may also become irritated, eventually developing more scar tissue and thick adhesions — abnormal bands of fibrous tissue that can also cause pelvic tissues and other organs to stick to each other.
The result? Pain.
Endometriosis is primarily characterized by hormonal imbalances, high circulating estrogens and progesterones, pelvic pain—especially during periods and PMS.
SYMPTOMS OF ENDOMETRIOSIS
Symptoms of endometriosis range from mild to severe, and may include:
Painful periods (dysmenorrhea)
Pelvic pain, lower back and abdominal pain—especially before your period
Pain with sexual intercourse
Pain with bowel movements or urination
Excessive bleeding—both during and between periods
Infertility or fertility problems
Fatigue
Diarrhea
Abnormal amounts of reproductive hormones (often high estrogen, low progesterone)
Constipation
Bloating
Nausea
Low immunity
Fluctuating blood pressures
Rapid or irregular heartbeat
Unwanted weight gain or difficulty losing weight
CAUSES OF ENDOMETRIOSIS
Most medical literature states the exact cause of endometriosis is unknown, but researchers believe that certain genes predispose women to get the disease and have developed other theories to explain it.
Conventional Explanations of Endometriosis
Popular conventional medicine theories behind the cause of endometriosis include:
“Retrograde” menstruation. In retrograde menstruation, menstrual blood containing thick endometrial cells flows back through the fallopian tubes and into the pelvic cavity instead of out of the body. Researchers speculate that displaced endometrial cells then stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to thicken and bleed over the course of each menstrual cycle. The problem with this theory is that more than 90% of menstruating women without endometriosis also have this, but typically their immune system id able to prevent cell tissue implantation and growth. (1)
Translocation of cells. Other researchers believe that gut cells that line the inner side of the abdomen get displaced into endometrial cells, instead of where they should be (in the gut)—making these endometrial cells thicker.
Embryonic cell overgrowth. This theory states that hormones, like estrogen, may transform embryonic cells — cells in the earliest stages of development — into endometrial cell implants during puberty.
Surgical scar implantation. After a surgery, such as a hysterectomy or C-section, endometrial cells may attach to a surgical incision.
Immune system dysfunction. The immune system theory states that immune dysfunction makes the body unable to recognize and destroy endometrial tissue that’s growing outside the uterus.
Unfortunately, these theories leave patients with little hope—if any—that they can be in control of their health, prevent or cure endometriosis.
Functional Medicine Explanations of Endometriosis
The functional medicine approach, on the other hand, looks at endometriosis a little bit differently. Functional medicine is a scope of practice in medicine and allied health that seeks first to understand the roots of disease and dysfunction—rather than just the symptoms.
Functional medicine also views the body as a whole—not parts—so when seeking to understand what causes endometriosis looks to other systems in the body—outside the endometrial tissues and cells, and surrounding areas.
There are two things that we know quite confidently about endometriosis:
It’s an inflammatory disease
It’s dependent on estrogen (ie. When estrogen is high and you have tissue overgrowth outside the uterus, you experience symptoms)
From a functional medicine lens, we must explore WHY this inflammation and hormone imbalance happening in the first place.
Current research points to several root causes including:
Gut Dysfunction
GI symptoms and endometriosis go hand in hand. On top of endometriosis symptoms, many patients report experiencing IBS, constipation, bloating, allergies, skin conditions, metabolic dysfunction, blood sugar and/or hormonal imbalances regularly—all highly connected to gut health as well. In fact, research shows that 75-80% of endometriosis sufferers also have SIBO (small intestinal bacterial overgrowth) (2), and endometriosis is described as having similar features as colitis and Crohn’s Disease—or “irritable bowel disease.” (3, 4)
The gut is the gateway to health: 80% of your immune system and more than 50% of your hormones are produced in your gut. In addition, you have 100 trillion gut bacteria living inside you—10 times more bacteria than cells in your human body.
Your gut bacteria play a vital role in maintaining overall balance in your body. Hence, if or when your gut health is off, your body’s ability to fend off foreign invaders (immune system) and keep your hormones balanced also goes down. Hello inflammation and dysfunction! Gut bacteria have been shown to affect practically every modern chronic disease to date (5).
Endometriosis is no exception, and this may greatly explain why the symptoms of hormonal imbalance, constipation, bloating, and blood sugar imbalances are also common. Additionally, given that endometriosis is characterized by elevated estrogen, this points to poor liver function in the GI tract, since liver is the master clean sweeper of excess hormones in the body. If the liver and GI system is down, hormone imbalances are a given.
A 2017 study review of 99 different studies on endometriosis and gut health in the Journal of Medical Research, found the most common themes amongst endometriosis sufferers were: gut bacteria imbalances within endometrium tissues, reduction of immune function and pathogenic bacteria triggering local tissue inflammation (6).
Another study suggested that the health of the intestinal bacteria played a critical role in the development and progression of endometriosis (7).
While many people still believe endometriosis is greatly genetically based, genetics only “load the gun,” and gut health, environmental and lifestyle factors pull the trigger. The bottom line: If you have an underlying gut pathology, such as SIBO (small intestinal bacterial overgrowth), fungal or bacterial infection, low stomach acid or intestinal permeability (“leaky gut”), you’re more at risk for endometriosis—especially if you have genetics for it.
Cortisol Imbalance (Stress)
Endometriosis is characterized by hormonal imbalance. Hormones are chemical messengers that control every organ in the body. In particular, the hormones estrogen and progesterone are in charge of regulating a woman’s reproductive functions, such as her menstrual cycle and fertility. When imbalances occur, organs don’t receive the correct signals to function adequately, so hormonal disorders are more likely to occur as well (like endometriosis).
However, although many people think hormonal imbalances come AFTER a endometriosis diagnosis, often times hormonal imbalances set the stage for endometriosis from the beginning—making your body a prime candidate to succumb to the side effects of tissue overgrowth in endometriosis.
The biggest driver of them all? Cortisol (i.e. your stress hormone).
Stress is the #1 driver of all disease and dysfunction. The more stressed out your body is (physically and mentally), the more likely shifts and imbalances in estrogen and progesterone are likely to happen.
One study on the effects of stress in rats with endometriosis found that prior exposure to stress increased both the number and severity of tissue overgrowth found in their pelvic area. Stress also increased colonic inflammation, gut motility, and numbers of mast cells that contributed to their condition. Researchers concluded that prior stress may contribute to the development and severity of endometriosis (8).
Another study found that in two groups of rats with endometriosis, the rats who were purposely subjected to physiological stress (overtraining exercise), versus rats who were not, had significantly more inflamed endometrial tissues than the rats with less stress.
Common stressors that often are overlooked, but that can trigger cortisol and hormonal imbalances include:
Long term medication use
Birth control pills
History of C-section birth, formula fed and/or antibiotic use
Tap water and environmental toxins
GMO’s, pesticides and conventional meats/dairy
Poor diet
Overtraining
Sedentary lifestyles
Lack of sleep
High caffeine, sugar or stimulant use
High screen exposure
All work, not play, rest or leisure
Lack of exposure to natural light and nature
Circadian rhythm dysfunction
Surgery and illness
Blood sugar imbalance and dysregulatoin
Low fat diets
Low carb diets
Low protein/no protein diets
Ultimately, the body desires balance and when it gets out of balance, then hormonal imbalances are one of the first dysfunctions to arise.
Toxic Burden
On the topic of hormonal imbalances and stress, environmental and toxic exposures are some of the top endocrine disruptors, with the majority of more than 80,000 approved chemicals unregulated and untested on humans—in everything from our skin care products, to makeup, household cleaners, hand sanitizers and more. Environmental toxins are believes to increase the risk of endometriosis by altering immune cells, hormones and cell growth factors. Common known endocrine disrupting toxins include:
PCB’s and dioxins. Found in pesticides in foods, conventional meat.
Flame retardants. Found in: Plastics, paint, furniture, electronics, food.
Phytoestrogens. Found in: Soy & other foods.
Phthalates. Found in: Plastics, food packaging, cosmetics, cleaning agents. If a product has “fragrance” or “perfum” it probably has phthalates.
BPA. Found in: Plastics, food packaging, the lining of many food/beverage containers.
UV Filters. Found in: Sunscreens, cosmetics.
Parabens. Found in: Wide range of products. Often in deodorants. Might also be in polyester fabrics.
Autoimmunity
Autoimmunity is defined as “an organism against its own healthy cells and tissues.” In other words, the body, or body cells, that “attacks itself.”
In the case of endometriosis, studies reveal the presentation tissue-specific antibodies and inflammatory cytokines intertwined in the disease (9). What causes autoimmunity in the first place? While genetics do play a big role in your predisposition to develop an autoimmune disease, countless studies show that all autoimmune diseases share a common thread of leaky gut or intestinal permeability in their presentation. (10, 11, 12).
DIAGNOSIS
Although the symptoms of endometriosis often speak for themselves, formal diagnosis is typically made through a combination of pelvic exam, ultrasound imagery, CT Scans or MRI scans, and laparoscopy—using a scope to look inside your abdomen.
Of all methods, however, laparoscopy is the only current “official” method to confirm a diagnosis.
TREATMENT: THE CONVENTIONAL MEDICINE APPROACH
Conventional medicine currently states there is no known cure for endometriosis. Therefore, most treatment of endometriosis in conventional medicine focuses on managing the symptoms—primarily through NSAIDs and medications, including synthetic hormones to try to balance the hormone imbalance. Surgery to remove endometriosis lesions and scar tissue may also be effective, but success rates are dependent on the extent of disease and a case-by-case basis.
Unfortunately however, all of these methods only manage endometriosis; they do not reverse the condition.
Many medicines, like synthetic hormones, steroids and NSAIDs, are not suitable for long-term use due to side-effects, including mood swings, further hormone imbalances, GI problems, toxic burden, liver overload and suppression of your body’s own hormone production.
In fact, when you take synthetic hormones, the levels of those hormones go up in the bloodstream and your pituitary gland reduces your own internal production of that hormone, causing hormone resistance. Over time, the more these hormones are added to your blood, the more the receptors for those hormones become down-regulated. Eventually, you’ll need higher and higher doses to get the same effect you initially got from your original prescription—and the cycle continues.
Additionally, pain killers, like Motrin, Aleve and Ibuprofen, do little to treat other symptoms that are part of endometriosis, such as fatigue, bloating, constipation, diarrhea, low back pain, ovarian mass, and a heavy flow during your period.
The bottom line? Conventional endometriosis treatment leaves patients with no other options other than to manage the symptoms and “deal with it.”
TREATMENT: THE FUNCTIONAL MEDICINE APPROACH
Functional medicine is aimed at addressing the roots of disease rather than managing the symptoms.
Lifestyle and nutrition interventions—aimed at healing the gut, addressing stress and bringing the hormones back to balance are typically used first before medications and surgical procedures. Treatment and remission of endometriosis is often achieved through the following approaches:
1. Address Underlying Gut Pathologies & Hormonal Imbalances
Work with a functional medicine practitioner or other skilled practitioner to evaluate and address any underlying gut dysfunction (SIBO, leaky gut, fungal overgrowth), HPA Axis Dysfunction, blood sugar imbalances, toxic burden, or other conditions driving your body into a state of stress and inflammation in the first place. Lab testing may include things such as stool analysis, organic acids urine testing, comprehensive blood testing, and SIBO breath testing to get to the root of your disease triggers.
2. Eat Real Anti-inflammatory Foods
An anti-inflammatory diet can be tremendously beneficial in the early stages of iron overload—primarily because it is an anti-inflammatory diet that can help keep inflammation at bay. Opt for real, colorful foods including:
Clean Filtered Water
Sustainable proteins (wild caught, pastured poultry, grass-fed beef)
Fiber rich veggies (greens, broccoli, asparagus, summer squash, cauliflower, etc)
Fermented Foods (sauerkraut, kimchi, pickled veggies, etc.)
Starchy tubers in moderation (potatoes, sweet potatoes, winter squashes, carrots). 1-2/day
Fresh fruits in moderation. 1-2/day.
For at least 30 days, avoid inflammatory foods including: eggs/egg whites, nuts, seeds, grains, beans and legumes, conventional meat and dairy, nightshade vegetables
Avoid completely: packaged and processed foods, gluten, industrial seed oils, and added sugar/sweeteners
3. Love Your Gut
Since the gut is the gateway to health, love your gut bugs every day with these 5 daily habits:
Take a soil based probiotic and prebiotic fiber (partially hydrolyzed guar gum, pectin, glucomannan)
Add 1 tbsp. Apple cider vinegar to 2-4 oz of water at meals, and take 1-2 digestive enzymes as needed with meals
Drink half your bodyweight in ounces of water daily
Eat lots of color at every meal (2-3 veggies, especially cooked, steamed and sautéed; and dark leafy greens)
Sip herbal tea (ginger, chamomile, dandelion)
Bonus: Love your liver! Add lemon to your water, sip low-sugar green juice and bone broth as snacks, and take a liver support enzyme with meals for 60-90 day
4. Address Stress
Assess what top stressors are driving your condition. Cut stress with several of these actionable stress-busters:
Sleep 7-9 hours
Get at least 30-60 minutes of sun exposure/light daily
Turn off screens 1-2 hours before bed (at least)
Refuse to overtrain
Move your body if you’ve been sedentary 3-5 times per week
Replace toxic beauty, cleaning and hygiene supplies gradually with toxin free versions
Just say NO (to something)
Use Natural Anti-Inflammatory Remedies to Subside Pain
DHA/EFA Fish Oil
Magnesium
Liposomal Curcumin
Zinc
B Vitamins
Adrenal Adaptogen (Ashwaganda, Rhodiola)
Blend of Blood Sugar Balancing Herbs & Substances, such as: Alpha Lipoic Acid, Chromium, Gymnema, Berberine, Banaba, Fenugreek, Ginseng, Tocopherols, Green Tea Extract (to balance blood sugar, associated with high cortisol)
Resources
1. Murray & Pizzorno. Endometriosis. 2012. The Encyclopedia of Natural Medicine. Atria Paperback. pp. 565.
2. Mathias, John R et al. 1998. Relation of endometriosis and neuromuscular disease of the gastrointestinal tract: new insights Fertility and Sterility , Volume 70 , Issue 1 , 81 – 88. https://www.ncbi.nlm.nih.gov/pubmed/9660426
3. Jess T, Frisch M, Jørgensen KT, et al Increased risk of inflammatory bowel disease in women with endometriosis: a nationwide Danish cohort study Gut 2012;61:1279-1283.
4. Glover, L. E., Fennimore, B., & Wingfield, M. (2016). Inflammatory Bowel Disease: Influence and Implications in Reproduction. Inflammatory Bowel Diseases, 22(11), 2724–2732. http://doi.org/10.1097/MIB.0000000000000884
5. Zhang, Y.-J., Li, S., Gan, R.-Y., Zhou, T., Xu, D.-P., & Li, H.-B. (2015). Impacts of Gut Bacteria on Human Health and Diseases. International Journal of Molecular Sciences, 16(4), 7493–7519. http://doi.org/10.3390/ijms16047493
6. Puca & Hoyne. 2017. Microbial dysbiosis and disease pathogenesis of endometriosis, could there be a link? Journal of Medical Research. https://www.alliedacademies.org/articles/microbial-dysbiosis-and-disease-pathogenesis-of-endometriosis-could-therebe-a-link.pdf
7. Laschke, Matthias W. et al. 2016. The gut microbiota: a puppet master in the pathogenesis of endometriosis? American Journal of Obstetrics & Gynecology , Volume 215 , Issue 1 , 68.e1 – 68.e4. doi: 10.1016/j.ajog.2016.02.036.
8. Cuevas, M., Flores, I., Thompson, K. J., Ramos-Ortolaza, D. L., Torres-Reveron, A., & Appleyard, C. B. (2012). Stress Exacerbates Endometriosis Manifestations and Inflammatory Parameters in an Animal Model. Reproductive Sciences, 19(8), 851–862. http://doi.org/10.1177/19337191124384433
9. Eisenberg et al. 2012. Is there an association between autoimmunity and endometriosis? Autoimmunity Reviews. 11 (11): 806-814. https://www.sciencedirect.com/science/article/pii/S1568997212000195?via%3Dihub
10. Megan Ciara Smyth; Intestinal permeability and autoimmune diseases, Bioscience Horizons: The International Journal of Student Research, Volume 10, 1 January 2017, hzx015, https://doi.org/10.1093/biohorizons/hzx015
11. Mu, Q., Kirby, J., Reilly, C. M., & Luo, X. M. (2017). Leaky Gut As a Danger Signal for Autoimmune Diseases. Frontiers in Immunology, 8, 598. http://doi.org/10.3389/fimmu.2017.00598
12. Fasano, A. (2012). Zonulin, regulation of tight junctions, and autoimmune diseases. Annals of the New York Academy of Sciences, 1258(1), 25–33. http://doi.org/10.1111/j.1749-6632.2012.06538.x
The post 5 Natural Proven-Effective Steps to Cure Endometriosis appeared first on Meet Dr. Lauryn.
Source/Repost=>
https://drlauryn.com/hormones-metabolism/steps-cure-endometriosis/ ** Dr. Lauryn Lax __Nutrition. Therapy. Functional Medicine ** https://drlauryn.com/
5 Natural Proven-Effective Steps to Cure Endometriosis via http://drlaurynlax.tumblr.com/
0 notes
Text
5 Natural Proven-Effective Steps to Cure Endometriosis
How To Cure Endometriosis
Endometriosis affects approximately 1 in 10 women during their reproductive years (ie. ages 15 to 49).
Endometriosis is the abnormal growth of cells (endometrial cells), similar to those that form the inside of the uterus, but in areas outside of the uterus including: fallopian tubes, ovaries, intestines and other tissues lining your pelvis. Rarely, endometrial tissue may spread beyond pelvic organs.
Over time, this displaced endometrial tissue continues to act as it normally would inside your uterus— it thickens, breaks down and bleeds with each menstrual cycle.
Since this displaced tissue has no way to escape your body, it becomes trapped. If endometriosis involves the ovaries, cysts called endometriomas may also form. The tissue surrounding these cysts may also become irritated, eventually developing more scar tissue and thick adhesions — abnormal bands of fibrous tissue that can also cause pelvic tissues and other organs to stick to each other.
The result? Pain.
Endometriosis is primarily characterized by hormonal imbalances, high circulating estrogens and progesterones, pelvic pain—especially during periods and PMS.
SYMPTOMS OF ENDOMETRIOSIS
Symptoms of endometriosis range from mild to severe, and may include:
Painful periods (dysmenorrhea)
Pelvic pain, lower back and abdominal pain—especially before your period
Pain with sexual intercourse
Pain with bowel movements or urination
Excessive bleeding—both during and between periods
Infertility or fertility problems
Fatigue
Diarrhea
Abnormal amounts of reproductive hormones (often high estrogen, low progesterone)
Constipation
Bloating
Nausea
Low immunity
Fluctuating blood pressures
Rapid or irregular heartbeat
Unwanted weight gain or difficulty losing weight
CAUSES OF ENDOMETRIOSIS
Most medical literature states the exact cause of endometriosis is unknown, but researchers believe that certain genes predispose women to get the disease and have developed other theories to explain it.
Conventional Explanations of Endometriosis
Popular conventional medicine theories behind the cause of endometriosis include:
“Retrograde” menstruation. In retrograde menstruation, menstrual blood containing thick endometrial cells flows back through the fallopian tubes and into the pelvic cavity instead of out of the body. Researchers speculate that displaced endometrial cells then stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to thicken and bleed over the course of each menstrual cycle. The problem with this theory is that more than 90% of menstruating women without endometriosis also have this, but typically their immune system id able to prevent cell tissue implantation and growth. (1)
Translocation of cells. Other researchers believe that gut cells that line the inner side of the abdomen get displaced into endometrial cells, instead of where they should be (in the gut)—making these endometrial cells thicker.
Embryonic cell overgrowth. This theory states that hormones, like estrogen, may transform embryonic cells — cells in the earliest stages of development — into endometrial cell implants during puberty.
Surgical scar implantation. After a surgery, such as a hysterectomy or C-section, endometrial cells may attach to a surgical incision.
Immune system dysfunction. The immune system theory states that immune dysfunction makes the body unable to recognize and destroy endometrial tissue that’s growing outside the uterus.
Unfortunately, these theories leave patients with little hope—if any—that they can be in control of their health, prevent or cure endometriosis.
Functional Medicine Explanations of Endometriosis
The functional medicine approach, on the other hand, looks at endometriosis a little bit differently. Functional medicine is a scope of practice in medicine and allied health that seeks first to understand the roots of disease and dysfunction—rather than just the symptoms.
Functional medicine also views the body as a whole—not parts—so when seeking to understand what causes endometriosis looks to other systems in the body—outside the endometrial tissues and cells, and surrounding areas.
There are two things that we know quite confidently about endometriosis:
It’s an inflammatory disease
It’s dependent on estrogen (ie. When estrogen is high and you have tissue overgrowth outside the uterus, you experience symptoms)
From a functional medicine lens, we must explore WHY this inflammation and hormone imbalance happening in the first place.
Current research points to several root causes including:
Gut Dysfunction
GI symptoms and endometriosis go hand in hand. On top of endometriosis symptoms, many patients report experiencing IBS, constipation, bloating, allergies, skin conditions, metabolic dysfunction, blood sugar and/or hormonal imbalances regularly—all highly connected to gut health as well. In fact, research shows that 75-80% of endometriosis sufferers also have SIBO (small intestinal bacterial overgrowth) (2), and endometriosis is described as having similar features as colitis and Crohn’s Disease—or “irritable bowel disease.” (3, 4)
The gut is the gateway to health: 80% of your immune system and more than 50% of your hormones are produced in your gut. In addition, you have 100 trillion gut bacteria living inside you—10 times more bacteria than cells in your human body.
Your gut bacteria play a vital role in maintaining overall balance in your body. Hence, if or when your gut health is off, your body’s ability to fend off foreign invaders (immune system) and keep your hormones balanced also goes down. Hello inflammation and dysfunction! Gut bacteria have been shown to affect practically every modern chronic disease to date (5).
Endometriosis is no exception, and this may greatly explain why the symptoms of hormonal imbalance, constipation, bloating, and blood sugar imbalances are also common. Additionally, given that endometriosis is characterized by elevated estrogen, this points to poor liver function in the GI tract, since liver is the master clean sweeper of excess hormones in the body. If the liver and GI system is down, hormone imbalances are a given.
A 2017 study review of 99 different studies on endometriosis and gut health in the Journal of Medical Research, found the most common themes amongst endometriosis sufferers were: gut bacteria imbalances within endometrium tissues, reduction of immune function and pathogenic bacteria triggering local tissue inflammation (6).
Another study suggested that the health of the intestinal bacteria played a critical role in the development and progression of endometriosis (7).
While many people still believe endometriosis is greatly genetically based, genetics only “load the gun,” and gut health, environmental and lifestyle factors pull the trigger. The bottom line: If you have an underlying gut pathology, such as SIBO (small intestinal bacterial overgrowth), fungal or bacterial infection, low stomach acid or intestinal permeability (“leaky gut”), you’re more at risk for endometriosis—especially if you have genetics for it.
Cortisol Imbalance (Stress)
Endometriosis is characterized by hormonal imbalance. Hormones are chemical messengers that control every organ in the body. In particular, the hormones estrogen and progesterone are in charge of regulating a woman’s reproductive functions, such as her menstrual cycle and fertility. When imbalances occur, organs don’t receive the correct signals to function adequately, so hormonal disorders are more likely to occur as well (like endometriosis).
However, although many people think hormonal imbalances come AFTER a endometriosis diagnosis, often times hormonal imbalances set the stage for endometriosis from the beginning—making your body a prime candidate to succumb to the side effects of tissue overgrowth in endometriosis.
The biggest driver of them all? Cortisol (i.e. your stress hormone).
Stress is the #1 driver of all disease and dysfunction. The more stressed out your body is (physically and mentally), the more likely shifts and imbalances in estrogen and progesterone are likely to happen.
One study on the effects of stress in rats with endometriosis found that prior exposure to stress increased both the number and severity of tissue overgrowth found in their pelvic area. Stress also increased colonic inflammation, gut motility, and numbers of mast cells that contributed to their condition. Researchers concluded that prior stress may contribute to the development and severity of endometriosis (8).
Another study found that in two groups of rats with endometriosis, the rats who were purposely subjected to physiological stress (overtraining exercise), versus rats who were not, had significantly more inflamed endometrial tissues than the rats with less stress.
Common stressors that often are overlooked, but that can trigger cortisol and hormonal imbalances include:
Long term medication use
Birth control pills
History of C-section birth, formula fed and/or antibiotic use
Tap water and environmental toxins
GMO’s, pesticides and conventional meats/dairy
Poor diet
Overtraining
Sedentary lifestyles
Lack of sleep
High caffeine, sugar or stimulant use
High screen exposure
All work, not play, rest or leisure
Lack of exposure to natural light and nature
Circadian rhythm dysfunction
Surgery and illness
Blood sugar imbalance and dysregulatoin
Low fat diets
Low carb diets
Low protein/no protein diets
Ultimately, the body desires balance and when it gets out of balance, then hormonal imbalances are one of the first dysfunctions to arise.
Toxic Burden
On the topic of hormonal imbalances and stress, environmental and toxic exposures are some of the top endocrine disruptors, with the majority of more than 80,000 approved chemicals unregulated and untested on humans—in everything from our skin care products, to makeup, household cleaners, hand sanitizers and more. Environmental toxins are believes to increase the risk of endometriosis by altering immune cells, hormones and cell growth factors. Common known endocrine disrupting toxins include:
PCB’s and dioxins. Found in pesticides in foods, conventional meat.
Flame retardants. Found in: Plastics, paint, furniture, electronics, food.
Phytoestrogens. Found in: Soy & other foods.
Phthalates. Found in: Plastics, food packaging, cosmetics, cleaning agents. If a product has “fragrance” or “perfum” it probably has phthalates.
BPA. Found in: Plastics, food packaging, the lining of many food/beverage containers.
UV Filters. Found in: Sunscreens, cosmetics.
Parabens. Found in: Wide range of products. Often in deodorants. Might also be in polyester fabrics.
Autoimmunity
Autoimmunity is defined as “an organism against its own healthy cells and tissues.” In other words, the body, or body cells, that “attacks itself.”
In the case of endometriosis, studies reveal the presentation tissue-specific antibodies and inflammatory cytokines intertwined in the disease (9). What causes autoimmunity in the first place? While genetics do play a big role in your predisposition to develop an autoimmune disease, countless studies show that all autoimmune diseases share a common thread of leaky gut or intestinal permeability in their presentation. (10, 11, 12).
DIAGNOSIS
Although the symptoms of endometriosis often speak for themselves, formal diagnosis is typically made through a combination of pelvic exam, ultrasound imagery, CT Scans or MRI scans, and laparoscopy—using a scope to look inside your abdomen.
Of all methods, however, laparoscopy is the only current “official” method to confirm a diagnosis.
TREATMENT: THE CONVENTIONAL MEDICINE APPROACH
Conventional medicine currently states there is no known cure for endometriosis. Therefore, most treatment of endometriosis in conventional medicine focuses on managing the symptoms—primarily through NSAIDs and medications, including synthetic hormones to try to balance the hormone imbalance. Surgery to remove endometriosis lesions and scar tissue may also be effective, but success rates are dependent on the extent of disease and a case-by-case basis.
Unfortunately however, all of these methods only manage endometriosis; they do not reverse the condition.
Many medicines, like synthetic hormones, steroids and NSAIDs, are not suitable for long-term use due to side-effects, including mood swings, further hormone imbalances, GI problems, toxic burden, liver overload and suppression of your body’s own hormone production.
In fact, when you take synthetic hormones, the levels of those hormones go up in the bloodstream and your pituitary gland reduces your own internal production of that hormone, causing hormone resistance. Over time, the more these hormones are added to your blood, the more the receptors for those hormones become down-regulated. Eventually, you’ll need higher and higher doses to get the same effect you initially got from your original prescription—and the cycle continues.
Additionally, pain killers, like Motrin, Aleve and Ibuprofen, do little to treat other symptoms that are part of endometriosis, such as fatigue, bloating, constipation, diarrhea, low back pain, ovarian mass, and a heavy flow during your period.
The bottom line? Conventional endometriosis treatment leaves patients with no other options other than to manage the symptoms and “deal with it.”
TREATMENT: THE FUNCTIONAL MEDICINE APPROACH
Functional medicine is aimed at addressing the roots of disease rather than managing the symptoms.
Lifestyle and nutrition interventions—aimed at healing the gut, addressing stress and bringing the hormones back to balance are typically used first before medications and surgical procedures. Treatment and remission of endometriosis is often achieved through the following approaches:
1. Address Underlying Gut Pathologies & Hormonal Imbalances
Work with a functional medicine practitioner or other skilled practitioner to evaluate and address any underlying gut dysfunction (SIBO, leaky gut, fungal overgrowth), HPA Axis Dysfunction, blood sugar imbalances, toxic burden, or other conditions driving your body into a state of stress and inflammation in the first place. Lab testing may include things such as stool analysis, organic acids urine testing, comprehensive blood testing, and SIBO breath testing to get to the root of your disease triggers.
2. Eat Real Anti-inflammatory Foods
An anti-inflammatory diet can be tremendously beneficial in the early stages of iron overload—primarily because it is an anti-inflammatory diet that can help keep inflammation at bay. Opt for real, colorful foods including:
Clean Filtered Water
Sustainable proteins (wild caught, pastured poultry, grass-fed beef)
Fiber rich veggies (greens, broccoli, asparagus, summer squash, cauliflower, etc)
Fermented Foods (sauerkraut, kimchi, pickled veggies, etc.)
Starchy tubers in moderation (potatoes, sweet potatoes, winter squashes, carrots). 1-2/day
Fresh fruits in moderation. 1-2/day.
For at least 30 days, avoid inflammatory foods including: eggs/egg whites, nuts, seeds, grains, beans and legumes, conventional meat and dairy, nightshade vegetables
Avoid completely: packaged and processed foods, gluten, industrial seed oils, and added sugar/sweeteners
3. Love Your Gut
Since the gut is the gateway to health, love your gut bugs every day with these 5 daily habits:
Take a soil based probiotic and prebiotic fiber (partially hydrolyzed guar gum, pectin, glucomannan)
Add 1 tbsp. Apple cider vinegar to 2-4 oz of water at meals, and take 1-2 digestive enzymes as needed with meals
Drink half your bodyweight in ounces of water daily
Eat lots of color at every meal (2-3 veggies, especially cooked, steamed and sautéed; and dark leafy greens)
Sip herbal tea (ginger, chamomile, dandelion)
Bonus: Love your liver! Add lemon to your water, sip low-sugar green juice and bone broth as snacks, and take a liver support enzyme with meals for 60-90 day
4. Address Stress
Assess what top stressors are driving your condition. Cut stress with several of these actionable stress-busters:
Sleep 7-9 hours
Get at least 30-60 minutes of sun exposure/light daily
Turn off screens 1-2 hours before bed (at least)
Refuse to overtrain
Move your body if you’ve been sedentary 3-5 times per week
Replace toxic beauty, cleaning and hygiene supplies gradually with toxin free versions
Just say NO (to something)
Use Natural Anti-Inflammatory Remedies to Subside Pain
DHA/EFA Fish Oil
Magnesium
Liposomal Curcumin
Zinc
B Vitamins
Adrenal Adaptogen (Ashwaganda, Rhodiola)
Blend of Blood Sugar Balancing Herbs & Substances, such as: Alpha Lipoic Acid, Chromium, Gymnema, Berberine, Banaba, Fenugreek, Ginseng, Tocopherols, Green Tea Extract (to balance blood sugar, associated with high cortisol)
Resources
1. Murray & Pizzorno. Endometriosis. 2012. The Encyclopedia of Natural Medicine. Atria Paperback. pp. 565.
2. Mathias, John R et al. 1998. Relation of endometriosis and neuromuscular disease of the gastrointestinal tract: new insights Fertility and Sterility , Volume 70 , Issue 1 , 81 – 88. https://www.ncbi.nlm.nih.gov/pubmed/9660426
3. Jess T, Frisch M, Jørgensen KT, et al Increased risk of inflammatory bowel disease in women with endometriosis: a nationwide Danish cohort study Gut 2012;61:1279-1283.
4. Glover, L. E., Fennimore, B., & Wingfield, M. (2016). Inflammatory Bowel Disease: Influence and Implications in Reproduction. Inflammatory Bowel Diseases, 22(11), 2724–2732. http://doi.org/10.1097/MIB.0000000000000884
5. Zhang, Y.-J., Li, S., Gan, R.-Y., Zhou, T., Xu, D.-P., & Li, H.-B. (2015). Impacts of Gut Bacteria on Human Health and Diseases. International Journal of Molecular Sciences, 16(4), 7493–7519. http://doi.org/10.3390/ijms16047493
6. Puca & Hoyne. 2017. Microbial dysbiosis and disease pathogenesis of endometriosis, could there be a link? Journal of Medical Research. https://www.alliedacademies.org/articles/microbial-dysbiosis-and-disease-pathogenesis-of-endometriosis-could-therebe-a-link.pdf
7. Laschke, Matthias W. et al. 2016. The gut microbiota: a puppet master in the pathogenesis of endometriosis? American Journal of Obstetrics & Gynecology , Volume 215 , Issue 1 , 68.e1 – 68.e4. doi: 10.1016/j.ajog.2016.02.036.
8. Cuevas, M., Flores, I., Thompson, K. J., Ramos-Ortolaza, D. L., Torres-Reveron, A., & Appleyard, C. B. (2012). Stress Exacerbates Endometriosis Manifestations and Inflammatory Parameters in an Animal Model. Reproductive Sciences, 19(8), 851–862. http://doi.org/10.1177/19337191124384433
9. Eisenberg et al. 2012. Is there an association between autoimmunity and endometriosis? Autoimmunity Reviews. 11 (11): 806-814. https://www.sciencedirect.com/science/article/pii/S1568997212000195?via%3Dihub
10. Megan Ciara Smyth; Intestinal permeability and autoimmune diseases, Bioscience Horizons: The International Journal of Student Research, Volume 10, 1 January 2017, hzx015, https://doi.org/10.1093/biohorizons/hzx015
11. Mu, Q., Kirby, J., Reilly, C. M., & Luo, X. M. (2017). Leaky Gut As a Danger Signal for Autoimmune Diseases. Frontiers in Immunology, 8, 598. http://doi.org/10.3389/fimmu.2017.00598
12. Fasano, A. (2012). Zonulin, regulation of tight junctions, and autoimmune diseases. Annals of the New York Academy of Sciences, 1258(1), 25–33. http://doi.org/10.1111/j.1749-6632.2012.06538.x
The post 5 Natural Proven-Effective Steps to Cure Endometriosis appeared first on Meet Dr. Lauryn.
Source/Repost=>
https://drlauryn.com/hormones-metabolism/steps-cure-endometriosis/ ** Dr. Lauryn Lax __Nutrition. Therapy. Functional Medicine ** https://drlauryn.com/
5 Natural Proven-Effective Steps to Cure Endometriosis via https://drlaurynlax.weebly.com/
0 notes
Text
5 Natural Proven-Effective Steps to Cure Endometriosis
How To Cure Endometriosis
Endometriosis affects approximately 1 in 10 women during their reproductive years (ie. ages 15 to 49).
Endometriosis is the abnormal growth of cells (endometrial cells), similar to those that form the inside of the uterus, but in areas outside of the uterus including: fallopian tubes, ovaries, intestines and other tissues lining your pelvis. Rarely, endometrial tissue may spread beyond pelvic organs.
Over time, this displaced endometrial tissue continues to act as it normally would inside your uterus— it thickens, breaks down and bleeds with each menstrual cycle.
Since this displaced tissue has no way to escape your body, it becomes trapped. If endometriosis involves the ovaries, cysts called endometriomas may also form. The tissue surrounding these cysts may also become irritated, eventually developing more scar tissue and thick adhesions — abnormal bands of fibrous tissue that can also cause pelvic tissues and other organs to stick to each other.
The result? Pain.
Endometriosis is primarily characterized by hormonal imbalances, high circulating estrogens and progesterones, pelvic pain—especially during periods and PMS.
SYMPTOMS OF ENDOMETRIOSIS
Symptoms of endometriosis range from mild to severe, and may include:
Painful periods (dysmenorrhea)
Pelvic pain, lower back and abdominal pain—especially before your period
Pain with sexual intercourse
Pain with bowel movements or urination
Excessive bleeding—both during and between periods
Infertility or fertility problems
Fatigue
Diarrhea
Abnormal amounts of reproductive hormones (often high estrogen, low progesterone)
Constipation
Bloating
Nausea
Low immunity
Fluctuating blood pressures
Rapid or irregular heartbeat
Unwanted weight gain or difficulty losing weight
CAUSES OF ENDOMETRIOSIS
Most medical literature states the exact cause of endometriosis is unknown, but researchers believe that certain genes predispose women to get the disease and have developed other theories to explain it.
Conventional Explanations of Endometriosis
Popular conventional medicine theories behind the cause of endometriosis include:
“Retrograde” menstruation. In retrograde menstruation, menstrual blood containing thick endometrial cells flows back through the fallopian tubes and into the pelvic cavity instead of out of the body. Researchers speculate that displaced endometrial cells then stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to thicken and bleed over the course of each menstrual cycle. The problem with this theory is that more than 90% of menstruating women without endometriosis also have this, but typically their immune system id able to prevent cell tissue implantation and growth. (1)
Translocation of cells. Other researchers believe that gut cells that line the inner side of the abdomen get displaced into endometrial cells, instead of where they should be (in the gut)—making these endometrial cells thicker.
Embryonic cell overgrowth. This theory states that hormones, like estrogen, may transform embryonic cells — cells in the earliest stages of development — into endometrial cell implants during puberty.
Surgical scar implantation. After a surgery, such as a hysterectomy or C-section, endometrial cells may attach to a surgical incision.
Immune system dysfunction. The immune system theory states that immune dysfunction makes the body unable to recognize and destroy endometrial tissue that’s growing outside the uterus.
Unfortunately, these theories leave patients with little hope—if any—that they can be in control of their health, prevent or cure endometriosis.
Functional Medicine Explanations of Endometriosis
The functional medicine approach, on the other hand, looks at endometriosis a little bit differently. Functional medicine is a scope of practice in medicine and allied health that seeks first to understand the roots of disease and dysfunction—rather than just the symptoms.
Functional medicine also views the body as a whole—not parts—so when seeking to understand what causes endometriosis looks to other systems in the body—outside the endometrial tissues and cells, and surrounding areas.
There are two things that we know quite confidently about endometriosis:
It’s an inflammatory disease
It’s dependent on estrogen (ie. When estrogen is high and you have tissue overgrowth outside the uterus, you experience symptoms)
From a functional medicine lens, we must explore WHY this inflammation and hormone imbalance happening in the first place.
Current research points to several root causes including:
Gut Dysfunction
GI symptoms and endometriosis go hand in hand. On top of endometriosis symptoms, many patients report experiencing IBS, constipation, bloating, allergies, skin conditions, metabolic dysfunction, blood sugar and/or hormonal imbalances regularly—all highly connected to gut health as well. In fact, research shows that 75-80% of endometriosis sufferers also have SIBO (small intestinal bacterial overgrowth) (2), and endometriosis is described as having similar features as colitis and Crohn’s Disease—or “irritable bowel disease.” (3, 4)
The gut is the gateway to health: 80% of your immune system and more than 50% of your hormones are produced in your gut. In addition, you have 100 trillion gut bacteria living inside you—10 times more bacteria than cells in your human body.
Your gut bacteria play a vital role in maintaining overall balance in your body. Hence, if or when your gut health is off, your body’s ability to fend off foreign invaders (immune system) and keep your hormones balanced also goes down. Hello inflammation and dysfunction! Gut bacteria have been shown to affect practically every modern chronic disease to date (5).
Endometriosis is no exception, and this may greatly explain why the symptoms of hormonal imbalance, constipation, bloating, and blood sugar imbalances are also common. Additionally, given that endometriosis is characterized by elevated estrogen, this points to poor liver function in the GI tract, since liver is the master clean sweeper of excess hormones in the body. If the liver and GI system is down, hormone imbalances are a given.
A 2017 study review of 99 different studies on endometriosis and gut health in the Journal of Medical Research, found the most common themes amongst endometriosis sufferers were: gut bacteria imbalances within endometrium tissues, reduction of immune function and pathogenic bacteria triggering local tissue inflammation (6).
Another study suggested that the health of the intestinal bacteria played a critical role in the development and progression of endometriosis (7).
While many people still believe endometriosis is greatly genetically based, genetics only “load the gun,” and gut health, environmental and lifestyle factors pull the trigger. The bottom line: If you have an underlying gut pathology, such as SIBO (small intestinal bacterial overgrowth), fungal or bacterial infection, low stomach acid or intestinal permeability (“leaky gut”), you’re more at risk for endometriosis—especially if you have genetics for it.
Cortisol Imbalance (Stress)
Endometriosis is characterized by hormonal imbalance. Hormones are chemical messengers that control every organ in the body. In particular, the hormones estrogen and progesterone are in charge of regulating a woman’s reproductive functions, such as her menstrual cycle and fertility. When imbalances occur, organs don’t receive the correct signals to function adequately, so hormonal disorders are more likely to occur as well (like endometriosis).
However, although many people think hormonal imbalances come AFTER a endometriosis diagnosis, often times hormonal imbalances set the stage for endometriosis from the beginning—making your body a prime candidate to succumb to the side effects of tissue overgrowth in endometriosis.
The biggest driver of them all? Cortisol (i.e. your stress hormone).
Stress is the #1 driver of all disease and dysfunction. The more stressed out your body is (physically and mentally), the more likely shifts and imbalances in estrogen and progesterone are likely to happen.
One study on the effects of stress in rats with endometriosis found that prior exposure to stress increased both the number and severity of tissue overgrowth found in their pelvic area. Stress also increased colonic inflammation, gut motility, and numbers of mast cells that contributed to their condition. Researchers concluded that prior stress may contribute to the development and severity of endometriosis (8).
Another study found that in two groups of rats with endometriosis, the rats who were purposely subjected to physiological stress (overtraining exercise), versus rats who were not, had significantly more inflamed endometrial tissues than the rats with less stress.
Common stressors that often are overlooked, but that can trigger cortisol and hormonal imbalances include:
Long term medication use
Birth control pills
History of C-section birth, formula fed and/or antibiotic use
Tap water and environmental toxins
GMO’s, pesticides and conventional meats/dairy
Poor diet
Overtraining
Sedentary lifestyles
Lack of sleep
High caffeine, sugar or stimulant use
High screen exposure
All work, not play, rest or leisure
Lack of exposure to natural light and nature
Circadian rhythm dysfunction
Surgery and illness
Blood sugar imbalance and dysregulatoin
Low fat diets
Low carb diets
Low protein/no protein diets
Ultimately, the body desires balance and when it gets out of balance, then hormonal imbalances are one of the first dysfunctions to arise.
Toxic Burden
On the topic of hormonal imbalances and stress, environmental and toxic exposures are some of the top endocrine disruptors, with the majority of more than 80,000 approved chemicals unregulated and untested on humans—in everything from our skin care products, to makeup, household cleaners, hand sanitizers and more. Environmental toxins are believes to increase the risk of endometriosis by altering immune cells, hormones and cell growth factors. Common known endocrine disrupting toxins include:
PCB’s and dioxins. Found in pesticides in foods, conventional meat.
Flame retardants. Found in: Plastics, paint, furniture, electronics, food.
Phytoestrogens. Found in: Soy & other foods.
Phthalates. Found in: Plastics, food packaging, cosmetics, cleaning agents. If a product has “fragrance” or “perfum” it probably has phthalates.
BPA. Found in: Plastics, food packaging, the lining of many food/beverage containers.
UV Filters. Found in: Sunscreens, cosmetics.
Parabens. Found in: Wide range of products. Often in deodorants. Might also be in polyester fabrics.
Autoimmunity
Autoimmunity is defined as “an organism against its own healthy cells and tissues.” In other words, the body, or body cells, that “attacks itself.”
In the case of endometriosis, studies reveal the presentation tissue-specific antibodies and inflammatory cytokines intertwined in the disease (9). What causes autoimmunity in the first place? While genetics do play a big role in your predisposition to develop an autoimmune disease, countless studies show that all autoimmune diseases share a common thread of leaky gut or intestinal permeability in their presentation. (10, 11, 12).
DIAGNOSIS
Although the symptoms of endometriosis often speak for themselves, formal diagnosis is typically made through a combination of pelvic exam, ultrasound imagery, CT Scans or MRI scans, and laparoscopy—using a scope to look inside your abdomen.
Of all methods, however, laparoscopy is the only current “official” method to confirm a diagnosis.
TREATMENT: THE CONVENTIONAL MEDICINE APPROACH
Conventional medicine currently states there is no known cure for endometriosis. Therefore, most treatment of endometriosis in conventional medicine focuses on managing the symptoms—primarily through NSAIDs and medications, including synthetic hormones to try to balance the hormone imbalance. Surgery to remove endometriosis lesions and scar tissue may also be effective, but success rates are dependent on the extent of disease and a case-by-case basis.
Unfortunately however, all of these methods only manage endometriosis; they do not reverse the condition.
Many medicines, like synthetic hormones, steroids and NSAIDs, are not suitable for long-term use due to side-effects, including mood swings, further hormone imbalances, GI problems, toxic burden, liver overload and suppression of your body’s own hormone production.
In fact, when you take synthetic hormones, the levels of those hormones go up in the bloodstream and your pituitary gland reduces your own internal production of that hormone, causing hormone resistance. Over time, the more these hormones are added to your blood, the more the receptors for those hormones become down-regulated. Eventually, you’ll need higher and higher doses to get the same effect you initially got from your original prescription—and the cycle continues.
Additionally, pain killers, like Motrin, Aleve and Ibuprofen, do little to treat other symptoms that are part of endometriosis, such as fatigue, bloating, constipation, diarrhea, low back pain, ovarian mass, and a heavy flow during your period.
The bottom line? Conventional endometriosis treatment leaves patients with no other options other than to manage the symptoms and “deal with it.”
TREATMENT: THE FUNCTIONAL MEDICINE APPROACH
Functional medicine is aimed at addressing the roots of disease rather than managing the symptoms.
Lifestyle and nutrition interventions—aimed at healing the gut, addressing stress and bringing the hormones back to balance are typically used first before medications and surgical procedures. Treatment and remission of endometriosis is often achieved through the following approaches:
1. Address Underlying Gut Pathologies & Hormonal Imbalances
Work with a functional medicine practitioner or other skilled practitioner to evaluate and address any underlying gut dysfunction (SIBO, leaky gut, fungal overgrowth), HPA Axis Dysfunction, blood sugar imbalances, toxic burden, or other conditions driving your body into a state of stress and inflammation in the first place. Lab testing may include things such as stool analysis, organic acids urine testing, comprehensive blood testing, and SIBO breath testing to get to the root of your disease triggers.
2. Eat Real Anti-inflammatory Foods
An anti-inflammatory diet can be tremendously beneficial in the early stages of iron overload—primarily because it is an anti-inflammatory diet that can help keep inflammation at bay. Opt for real, colorful foods including:
Clean Filtered Water
Sustainable proteins (wild caught, pastured poultry, grass-fed beef)
Fiber rich veggies (greens, broccoli, asparagus, summer squash, cauliflower, etc)
Fermented Foods (sauerkraut, kimchi, pickled veggies, etc.)
Starchy tubers in moderation (potatoes, sweet potatoes, winter squashes, carrots). 1-2/day
Fresh fruits in moderation. 1-2/day.
For at least 30 days, avoid inflammatory foods including: eggs/egg whites, nuts, seeds, grains, beans and legumes, conventional meat and dairy, nightshade vegetables
Avoid completely: packaged and processed foods, gluten, industrial seed oils, and added sugar/sweeteners
3. Love Your Gut
Since the gut is the gateway to health, love your gut bugs every day with these 5 daily habits:
Take a soil based probiotic and prebiotic fiber (partially hydrolyzed guar gum, pectin, glucomannan)
Add 1 tbsp. Apple cider vinegar to 2-4 oz of water at meals, and take 1-2 digestive enzymes as needed with meals
Drink half your bodyweight in ounces of water daily
Eat lots of color at every meal (2-3 veggies, especially cooked, steamed and sautéed; and dark leafy greens)
Sip herbal tea (ginger, chamomile, dandelion)
Bonus: Love your liver! Add lemon to your water, sip low-sugar green juice and bone broth as snacks, and take a liver support enzyme with meals for 60-90 day
4. Address Stress
Assess what top stressors are driving your condition. Cut stress with several of these actionable stress-busters:
Sleep 7-9 hours
Get at least 30-60 minutes of sun exposure/light daily
Turn off screens 1-2 hours before bed (at least)
Refuse to overtrain
Move your body if you’ve been sedentary 3-5 times per week
Replace toxic beauty, cleaning and hygiene supplies gradually with toxin free versions
Just say NO (to something)
Use Natural Anti-Inflammatory Remedies to Subside Pain
DHA/EFA Fish Oil
Magnesium
Liposomal Curcumin
Zinc
B Vitamins
Adrenal Adaptogen (Ashwaganda, Rhodiola)
Blend of Blood Sugar Balancing Herbs & Substances, such as: Alpha Lipoic Acid, Chromium, Gymnema, Berberine, Banaba, Fenugreek, Ginseng, Tocopherols, Green Tea Extract (to balance blood sugar, associated with high cortisol)
Resources
1. Murray & Pizzorno. Endometriosis. 2012. The Encyclopedia of Natural Medicine. Atria Paperback. pp. 565.
2. Mathias, John R et al. 1998. Relation of endometriosis and neuromuscular disease of the gastrointestinal tract: new insights Fertility and Sterility , Volume 70 , Issue 1 , 81 – 88. https://www.ncbi.nlm.nih.gov/pubmed/9660426
3. Jess T, Frisch M, Jørgensen KT, et al Increased risk of inflammatory bowel disease in women with endometriosis: a nationwide Danish cohort study Gut 2012;61:1279-1283.
4. Glover, L. E., Fennimore, B., & Wingfield, M. (2016). Inflammatory Bowel Disease: Influence and Implications in Reproduction. Inflammatory Bowel Diseases, 22(11), 2724–2732. http://doi.org/10.1097/MIB.0000000000000884
5. Zhang, Y.-J., Li, S., Gan, R.-Y., Zhou, T., Xu, D.-P., & Li, H.-B. (2015). Impacts of Gut Bacteria on Human Health and Diseases. International Journal of Molecular Sciences, 16(4), 7493–7519. http://doi.org/10.3390/ijms16047493
6. Puca & Hoyne. 2017. Microbial dysbiosis and disease pathogenesis of endometriosis, could there be a link? Journal of Medical Research. https://www.alliedacademies.org/articles/microbial-dysbiosis-and-disease-pathogenesis-of-endometriosis-could-therebe-a-link.pdf
7. Laschke, Matthias W. et al. 2016. The gut microbiota: a puppet master in the pathogenesis of endometriosis? American Journal of Obstetrics & Gynecology , Volume 215 , Issue 1 , 68.e1 – 68.e4. doi: 10.1016/j.ajog.2016.02.036.
8. Cuevas, M., Flores, I., Thompson, K. J., Ramos-Ortolaza, D. L., Torres-Reveron, A., & Appleyard, C. B. (2012). Stress Exacerbates Endometriosis Manifestations and Inflammatory Parameters in an Animal Model. Reproductive Sciences, 19(8), 851–862. http://doi.org/10.1177/19337191124384433
9. Eisenberg et al. 2012. Is there an association between autoimmunity and endometriosis? Autoimmunity Reviews. 11 (11): 806-814. https://www.sciencedirect.com/science/article/pii/S1568997212000195?via%3Dihub
10. Megan Ciara Smyth; Intestinal permeability and autoimmune diseases, Bioscience Horizons: The International Journal of Student Research, Volume 10, 1 January 2017, hzx015, https://doi.org/10.1093/biohorizons/hzx015
11. Mu, Q., Kirby, J., Reilly, C. M., & Luo, X. M. (2017). Leaky Gut As a Danger Signal for Autoimmune Diseases. Frontiers in Immunology, 8, 598. http://doi.org/10.3389/fimmu.2017.00598
12. Fasano, A. (2012). Zonulin, regulation of tight junctions, and autoimmune diseases. Annals of the New York Academy of Sciences, 1258(1), 25–33. http://doi.org/10.1111/j.1749-6632.2012.06538.x
The post 5 Natural Proven-Effective Steps to Cure Endometriosis appeared first on Meet Dr. Lauryn.
Source/Repost=>
https://drlauryn.com/hormones-metabolism/steps-cure-endometriosis/ ** Dr. Lauryn Lax __Nutrition. Therapy. Functional Medicine ** https://drlauryn.com/
0 notes
Text
Turmeric and flax seed are natural treatments for endometriosis
Turmeric and flax seed are natural treatments for endometriosis
This is a gynecological condition which is affecting approximately 10% of girls and women all around the world. This condition is happening when the endometrium which is tissue that makes up inside the surface of the uterus, grows outside the uterine cavity. It can grow on the tissues lining the pelvis, bowel and ovaries. This misplaced endometrial tissue follows the normal menstrual cycle (it grows, thickens and breaks down) due to the hormonal changes that are happening in woman’s body. It has no way to exit her body and it becomes trapped and it is causing irritation and formation of scars and adhesions. This is causing severe pain during periods and possible fertility. Both factors can have a massive impact on the life of woman. Women from all ages are having risk of developing endometriosis. In the most cases it affects women from 25 – 40. The exact cause for this condition is now known. A key role in endometriosis can play backflow of menstrual fluid and the retrograde menstruation. Also there are other factors that could lead to endometriosis such as the reproductive system, the immune system, environmental toxins like dioxins that affect the body, a weak immune system and genetics. The most common symptoms of endometriosis are nausea, constipation, diarrhea, indigestion, swollen abdomen, infertility, fatigue, heavy or irregular bleeding during menstrual periods, painful bowel movements, pain during sexual intercourse, sharp pain during ovulation and pelvic pain and cramping during menstruation. The symptoms of endometriosis can vary from woman to woman. In the most cases women who suffer from endometriosis have no symptoms. This condition tends to get better when menopause begin. You can try some of the below mentioned home remedies to control the severity of endometriosis and alleviate the main symptoms of pain and infertility. You need to talk with your doctor before you start using some of the below mentioned home remedies for endometriosis if they are suitable for you and for the proper dosage.
Home remedies for endometriosis
Wild asparagus: Wild asparagus in Ayurveda was known as shatavari. It is rich in folic acid and it can help to treat anemia as well as endometriosis that is caused by a deficiency of folic acid. Also it has Vitamin E which can help to alleviate the pain, particularly cramps. You should mix one teaspoon of wild asparagus powder in one glass of warm milk. You should drink this home remedy 2 times per day until you feel better.
Dandelion: There are many herbalists which are recommending dandelion as a natural treatment for alleviating the symptoms of endometriosis. It can strengthen kidneys and liver and also it can help to regulate the hormone levels. You should put one teaspoon of dried dandelion root in one cup. You should pour hot water in the cup, cover it and let it steep for ten minutes. Strain it and add honey for taste. You should drink this tea 2 or 3 times per day until you get better.
Turmeric: Turmeric has curcumin which has anti – inflammatory benefits which can be used as natural treatment for endometriosis. It has been shown that it has anti – endometriotic property. You should bring 2 cups of water to boil and you should add one teaspoon each of ginger powder and turmeric powder and one tablespoon each of lemon juice and honey. Drink this home remedy once per day until you rid of the problem. Also you can take turmeric capsules (300 mg) 3 times per day. You should avoid turmeric remedies if you are taking blood – thinning medications.
Flaxseed: This is a very effective home remedy for endometriosis. It has Omega – 3 fatty acids and antioxidants which can help to slow the growth of abnormal endometrial tissue. The flaxseed can help the body to eliminate the harmful toxins. You should soak 3 – 4 tablespoons of flaxseeds in one cup of water overnight. You should strain it and drink the water in the next morning. You should follow this home remedy until your symptoms subside. Also you can add ground flaxseeds to salads, soups, smoothies and yogurt.
Pelvic massage: You should massage your pelvic area and abdomen with essential oils like sandalwood or lavender because it can help a lot to relax and soothe minor pain that is associated with endometriosis. You should lie on the bed and stretch out your body. You should rub some essential oil on your stomach. You should gently massage in a rotating pattern for 5 – 10 minutes. You should do this natural treatment once per day. You should not do this massage during your menstrual cycle. You should try to maintain a healthy weight and you should avoid fatty foods. You should not drink homogenized milk. You should try to drink filtered water or spring water. Also you should avoid alcohol and do not smoke. You need to take all the necessary steps to reduce the stress.
Natural treatments for endometriosis
Sitz bath: Many naturopathy practitioners are recommending a contrast hot and cold sitz bath because it can help to reduce the symptoms of endometriosis. The hot bath will help to relax the pelvic muscles which in turn can reduce pain and cramping. The cold bath can help to reduce the inflammation and alleviate the pain. You should fill 2 large bathtubs, one with cold water and another with hot water. You should add ten drops of lavender essential oil or rosemary essential oil to each bath and stir well. You should sit in the tub with hot water up to your waist for 3 – 5 minutes. Then, you should sit in the tub of cold water up to your waist for one minute. You should repeat this natural treatment for 2 – 5 rounds. You should do this natural treatment 3 – 5 times a week. You should avoid this natural treatment during menstruation.
Castor oil: This is one of the most effective home remedies for endometriosis. It can help your body to rid of the excess toxins and tissues. This home remedy should be used at the beginning of the menstrual cycle, when the cramping is first noticed. It can help to reduce the severity of symptoms throughout the cycle. You should mix ¼ cup of castor oil with 8 drops of lavender essential oil. You should soak a washcloth in this home remedy, fold it and heat it in the microwave until it is comfortably warm. You should place warm cloth directly on your lower stomach. You should put a piece of plastic on top of the cloth and you should place a hot water bottle on the top of that. You should use this pack once per day for thirty to sixty minutes. You should rinse it off with lukewarm water after each application. You should not use this home remedy during the menstrual flow.
Chamomile: This home remedy has anti – inflammatory properties which can help to reduce the inflammation as well as swelling that is often associated with endometriosis. Also it acts as a natural diuretic which can help to flush out the bladder. You need to steep two teaspoons of dried chamomile in one cup of hot water for 5 minutes. Strain it, add a little honey and drink this tea. You should drink 2 – 3 cups of chamomile tea on daily basis until you feel better. Also you can take chamomile in the form of capsules or tincture but always talk with your doctor before you start taking them.
Ginger: This home remedy has strong anti – inflammatory properties which can relieve menstrual cramps and reduce inflammation. Also it can relive the nausea that is happening with endometriosis. It plays a big role in clearing the liver of excess toxins. You should boil one tablespoon of grated ginger root in 2 cups of water for ten minutes. You should strain it, add honey and drink 2 – 3 cups of this herbal tea on daily basis. Also you can chew fresh ginger pieces several times per day to recover quickly.
Motherwort: This is also a very effective home remedy for endometriosis. There are several components in the motherwort which can help to enhance the blood volume in the reproductive system which is very important for the proper functioning. This in turn can help to combat menstrual problems like poor flow or blood clots. You should steep one teaspoon of the dried motherwort in one cup of hot water for about fifteen minutes. You should drink this herbal tea at least two times per day until your condition improves. Also you can take motherwort in capsule or tincture form but talk with herbalist before you start taking them. if you are using any kind of sedating medications, then you should avoid this herb.
1 note
·
View note
Text
Turmeric and flax seed are natural treatments for endometriosis
Turmeric and flax seed are natural treatments for endometriosis
This is a gynecological condition which is affecting approximately 10% of girls and women all around the world [1]. This condition is happening when the endometrium which is tissue that makes up inside the surface of the uterus, grows outside the uterine cavity. It can grow on the tissues lining the pelvis, bowel and ovaries. This misplaced endometrial tissue follows the normal menstrual cycle (it grows, thickens and breaks down) due to the hormonal changes that are happening in woman’s body. It has no way to exit her body and it becomes trapped and it is causing irritation and formation of scars and adhesions. This is causing severe pain during periods and possible fertility. Both factors can have a massive impact on the life of woman. Women from all ages are having risk of developing endometriosis. In the most cases it affects women from 25 – 40. The exact cause for this condition is now known. A key role in endometriosis can play backflow of menstrual fluid and the retrograde menstruation. Also there are other factors that could lead to endometriosis such as the reproductive system, the immune system, environmental toxins like dioxins that affect the body, a weak immune system and genetics. The most common symptoms of endometriosis are nausea, constipation, diarrhea, indigestion, swollen abdomen, infertility, fatigue, heavy or irregular bleeding during menstrual periods, painful bowel movements, pain during sexual intercourse, sharp pain during ovulation and pelvic pain and cramping during menstruation. The symptoms of endometriosis can vary from woman to woman. In the most cases women who suffer from endometriosis have no symptoms. This condition tends to get better when menopause begin. You can try some of the below mentioned home remedies to control the severity of endometriosis and alleviate the main symptoms of pain and infertility. You need to talk with your doctor before you start using some of the below mentioned home remedies for endometriosis if they are suitable for you and for the proper dosage.
Home remedies for endometriosis
Wild asparagus: Wild asparagus in Ayurveda was known as shatavari. It is rich in folic acid and it can help to treat anemia as well as endometriosis that is caused by a deficiency of folic acid. Also it has Vitamin E which can help to alleviate the pain, particularly cramps. You should mix one teaspoon of wild asparagus powder in one glass of warm milk. You should drink this home remedy 2 times per day until you feel better. [2] Dandelion: There are many herbalists which are recommending dandelion as a natural treatment for alleviating the symptoms of endometriosis. It can strengthen kidneys and liver and also it can help to regulate the hormone levels. You should put one teaspoon of dried dandelion root in one cup. You should pour hot water in the cup, cover it and let it steep for ten minutes. Strain it and add honey for taste. You should drink this tea 2 or 3 times per day until you get better. [3] Turmeric: Turmeric has curcumin which has anti – inflammatory benefits which can be used as natural treatment for endometriosis. It has been shown that it has anti – endometriotic property [4]. You should bring 2 cups of water to boil and you should add one teaspoon each of ginger powder and turmeric powder and one tablespoon each of lemon juice and honey. Drink this home remedy once per day until you rid of the problem. Also you can take turmeric capsules (300 mg) 3 times per day. You should avoid turmeric remedies if you are taking blood – thinning medications. Flaxseed: This is a very effective home remedy for endometriosis. It has Omega – 3 fatty acids and antioxidants which can help to slow the growth of abnormal endometrial tissue. The flaxseed can help the body to eliminate the harmful toxins. You should soak 3 – 4 tablespoons of flaxseeds in one cup of water overnight. You should strain it and drink the water in the next morning. You should follow this home remedy until your symptoms subside. Also you can add ground flaxseeds to salads, soups, smoothies and yogurt. [5] Pelvic massage: You should massage your pelvic area and abdomen with essential oils like sandalwood or lavender because it can help a lot to relax and soothe minor pain that is associated with endometriosis. You should lie on the bed and stretch out your body. You should rub some essential oil on your stomach. You should gently massage in a rotating pattern for 5 – 10 minutes. You should do this natural treatment once per day. You should not do this massage during your menstrual cycle. You should try to maintain a healthy weight and you should avoid fatty foods. You should not drink homogenized milk. You should try to drink filtered water or spring water. Also you should avoid alcohol and do not smoke. You need to take all the necessary steps to reduce the stress.
Natural treatments for endometriosis
Sitz bath: Many naturopathy practitioners are recommending a contrast hot and cold sitz bath because it can help to reduce the symptoms of endometriosis. The hot bath will help to relax the pelvic muscles which in turn can reduce pain and cramping. The cold bath can help to reduce the inflammation and alleviate the pain. You should fill 2 large bathtubs, one with cold water and another with hot water. You should add ten drops of lavender essential oil or rosemary essential oil to each bath and stir well. You should sit in the tub with hot water up to your waist for 3 – 5 minutes. Then, you should sit in the tub of cold water up to your waist for one minute. You should repeat this natural treatment for 2 – 5 rounds. You should do this natural treatment 3 – 5 times a week. You should avoid this natural treatment during menstruation. Castor oil: This is one of the most effective home remedies for endometriosis. It can help your body to rid of the excess toxins and tissues. This home remedy should be used at the beginning of the menstrual cycle, when the cramping is first noticed. It can help to reduce the severity of symptoms throughout the cycle. You should mix ¼ cup of castor oil with 8 drops of lavender essential oil. You should soak a washcloth in this home remedy, fold it and heat it in the microwave until it is comfortably warm. You should place warm cloth directly on your lower stomach. You should put a piece of plastic on top of the cloth and you should place a hot water bottle on the top of that. You should use this pack once per day for thirty to sixty minutes. You should rinse it off with lukewarm water after each application. You should not use this home remedy during the menstrual flow. Chamomile: This home remedy has anti – inflammatory properties which can help to reduce the inflammation as well as swelling that is often associated with endometriosis. Also it acts as a natural diuretic which can help to flush out the bladder. You need to steep two teaspoons of dried chamomile in one cup of hot water for 5 minutes. Strain it, add a little honey and drink this tea. You should drink 2 – 3 cups of chamomile tea on daily basis until you feel better. Also you can take chamomile in the form of capsules or tincture but always talk with your doctor before you start taking them. [6] Ginger: This home remedy has strong anti – inflammatory properties which can relieve menstrual cramps and reduce inflammation [7]. Also it can relive the nausea that is happening with endometriosis. It plays a big role in clearing the liver of excess toxins. You should boil one tablespoon of grated ginger root in 2 cups of water for ten minutes. You should strain it, add honey and drink 2 – 3 cups of this herbal tea on daily basis. Also you can chew fresh ginger pieces several times per day to recover quickly. Motherwort: This is also a very effective home remedy for endometriosis. There are several components in the motherwort which can help to enhance the blood volume in the reproductive system which is very important for the proper functioning. This in turn can help to combat menstrual problems like poor flow or blood clots. You should steep one teaspoon of the dried motherwort in one cup of hot water for about fifteen minutes. You should drink this herbal tea at least two times per day until your condition improves. Also you can take motherwort in capsule or tincture form but talk with herbalist before you start taking them. if you are using any kind of sedating medications, then you should avoid this herb. [8] References: [1] Giudice LC. Clinical practice. Endometriosis. The New England Journal of Medicine. 2010;362(25):2389-98. [2] Kumar S, Mehla RK, Kumar Dang A. Use of shatavari (asparagus racemosus) as a galactopoietic and therapeutic herb - a review. Agricultural Reviews. 2008;29(2):132-138. [3] Wang T, Xue B, Shao H, et al. Effect of dandelion extracts on the proliferation of ovarian granulosa cells and expression of hormone receptors. Chinese Medical Journal. 2018;131(14):1694-1701. [4] Arablou T, Kolahdouz-Mohammadi R. Curcumin and endometriosis: Review on potential roles and molecular mechanisms. Biomedicine & Pharmacotherapy. 2018;97:91-97. [5] Chang VC, Cotterchio M, Boucher BA, et al. Effect of dietary flaxseed intake on circulating sex hormone levels among postmenopausal women: A randomized controlled intervention trial. Nutrition and Cancer. 2019;71(3):385-398. [6] Ali B, Al-Wabel NA, Shams S, et al. Essential oils used in aromatherapy: A systemic review. Asian Pacific Journal of Tropical Biomedicine. 2015;5(8):601-611. [7] Chen CX, Barrett B, Kwekkeboom KL. Efficacy of oral ginger (Zingiber officinale) for dysmenorrhea: A systematic review and meta-analysis. Evidence-based Complementary and Alternative Medicine. 2016;2016:6295737. [8] Lans C, Taylor-Swanson L, Westfall R. Herbal fertility treatments used in North America from colonial times to 1900, and their potential for improving the success rate of assisted reproductive technology. Reproductive Biomedicine & Society Online. 2018;5:60-81.
0 notes
Text
Turmeric and flax seed are natural treatments for endometriosis
Turmeric and flax seed are natural treatments for endometriosis
This is a gynecological condition which is affecting approximately 10% of girls and women all around the world. This condition is happening when the endometrium which is tissue that makes up inside the surface of the uterus, grows outside the uterine cavity. It can grow on the tissues lining the pelvis, bowel and ovaries. This misplaced endometrial tissue follows the normal menstrual cycle (it grows, thickens and breaks down) due to the hormonal changes that are happening in woman’s body. It has no way to exit her body and it becomes trapped and it is causing irritation and formation of scars and adhesions. This is causing severe pain during periods and possible fertility. Both factors can have a massive impact on the life of woman. Women from all ages are having risk of developing endometriosis. In the most cases it affects women from 25 – 40. The exact cause for this condition is now known. A key role in endometriosis can play backflow of menstrual fluid and the retrograde menstruation. Also there are other factors that could lead to endometriosis such as the reproductive system, the immune system, environmental toxins like dioxins that affect the body, a weak immune system and genetics. The most common symptoms of endometriosis are nausea, constipation, diarrhea, indigestion, swollen abdomen, infertility, fatigue, heavy or irregular bleeding during menstrual periods, painful bowel movements, pain during sexual intercourse, sharp pain during ovulation and pelvic pain and cramping during menstruation. The symptoms of endometriosis can vary from woman to woman. In the most cases women who suffer from endometriosis have no symptoms. This condition tends to get better when menopause begin. You can try some of the below mentioned home remedies to control the severity of endometriosis and alleviate the main symptoms of pain and infertility. You need to talk with your doctor before you start using some of the below mentioned home remedies for endometriosis if they are suitable for you and for the proper dosage.
Home remedies for endometriosis
Wild asparagus: Wild asparagus in Ayurveda was known as shatavari. It is rich in folic acid and it can help to treat anemia as well as endometriosis that is caused by a deficiency of folic acid. Also it has Vitamin E which can help to alleviate the pain, particularly cramps. You should mix one teaspoon of wild asparagus powder in one glass of warm milk. You should drink this home remedy 2 times per day until you feel better. Dandelion: There are many herbalists which are recommending dandelion as a natural treatment for alleviating the symptoms of endometriosis. It can strengthen kidneys and liver and also it can help to regulate the hormone levels. You should put one teaspoon of dried dandelion root in one cup. You should pour hot water in the cup, cover it and let it steep for ten minutes. Strain it and add honey for taste. You should drink this tea 2 or 3 times per day until you get better. Turmeric: Turmeric has curcumin which has anti – inflammatory benefits which can be used as natural treatment for endometriosis. It has been shown that it has anti – endometriotic property. You should bring 2 cups of water to boil and you should add one teaspoon each of ginger powder and turmeric powder and one tablespoon each of lemon juice and honey. Drink this home remedy once per day until you rid of the problem. Also you can take turmeric capsules (300 mg) 3 times per day. You should avoid turmeric remedies if you are taking blood – thinning medications. Flaxseed: This is a very effective home remedy for endometriosis. It has Omega – 3 fatty acids and antioxidants which can help to slow the growth of abnormal endometrial tissue. The flaxseed can help the body to eliminate the harmful toxins. You should soak 3 – 4 tablespoons of flaxseeds in one cup of water overnight. You should strain it and drink the water in the next morning. You should follow this home remedy until your symptoms subside. Also you can add ground flaxseeds to salads, soups, smoothies and yogurt. Pelvic massage: You should massage your pelvic area and abdomen with essential oils like sandalwood or lavender because it can help a lot to relax and soothe minor pain that is associated with endometriosis. You should lie on the bed and stretch out your body. You should rub some essential oil on your stomach. You should gently massage in a rotating pattern for 5 – 10 minutes. You should do this natural treatment once per day. You should not do this massage during your menstrual cycle. You should try to maintain a healthy weight and you should avoid fatty foods. You should not drink homogenized milk. You should try to drink filtered water or spring water. Also you should avoid alcohol and do not smoke. You need to take all the necessary steps to reduce the stress.
Natural treatments for endometriosis
Sitz bath: Many naturopathy practitioners are recommending a contrast hot and cold sitz bath because it can help to reduce the symptoms of endometriosis. The hot bath will help to relax the pelvic muscles which in turn can reduce pain and cramping. The cold bath can help to reduce the inflammation and alleviate the pain. You should fill 2 large bathtubs, one with cold water and another with hot water. You should add ten drops of lavender essential oil or rosemary essential oil to each bath and stir well. You should sit in the tub with hot water up to your waist for 3 – 5 minutes. Then, you should sit in the tub of cold water up to your waist for one minute. You should repeat this natural treatment for 2 – 5 rounds. You should do this natural treatment 3 – 5 times a week. You should avoid this natural treatment during menstruation. Castor oil: This is one of the most effective home remedies for endometriosis. It can help your body to rid of the excess toxins and tissues. This home remedy should be used at the beginning of the menstrual cycle, when the cramping is first noticed. It can help to reduce the severity of symptoms throughout the cycle. You should mix ¼ cup of castor oil with 8 drops of lavender essential oil. You should soak a washcloth in this home remedy, fold it and heat it in the microwave until it is comfortably warm. You should place warm cloth directly on your lower stomach. You should put a piece of plastic on top of the cloth and you should place a hot water bottle on the top of that. You should use this pack once per day for thirty to sixty minutes. You should rinse it off with lukewarm water after each application. You should not use this home remedy during the menstrual flow. Chamomile: This home remedy has anti – inflammatory properties which can help to reduce the inflammation as well as swelling that is often associated with endometriosis. Also it acts as a natural diuretic which can help to flush out the bladder. You need to steep two teaspoons of dried chamomile in one cup of hot water for 5 minutes. Strain it, add a little honey and drink this tea. You should drink 2 – 3 cups of chamomile tea on daily basis until you feel better. Also you can take chamomile in the form of capsules or tincture but always talk with your doctor before you start taking them. Ginger: This home remedy has strong anti – inflammatory properties which can relieve menstrual cramps and reduce inflammation. Also it can relive the nausea that is happening with endometriosis. It plays a big role in clearing the liver of excess toxins. You should boil one tablespoon of grated ginger root in 2 cups of water for ten minutes. You should strain it, add honey and drink 2 – 3 cups of this herbal tea on daily basis. Also you can chew fresh ginger pieces several times per day to recover quickly. Motherwort: This is also a very effective home remedy for endometriosis. There are several components in the motherwort which can help to enhance the blood volume in the reproductive system which is very important for the proper functioning. This in turn can help to combat menstrual problems like poor flow or blood clots. You should steep one teaspoon of the dried motherwort in one cup of hot water for about fifteen minutes. You should drink this herbal tea at least two times per day until your condition improves. Also you can take motherwort in capsule or tincture form but talk with herbalist before you start taking them. if you are using any kind of sedating medications, then you should avoid this herb.
0 notes