#STI treatment options
Text
The Three Most Prevalent STIs: Chlamydia, Gonorrhea, and HPV
Introduction:
Chlamydia, gonorrhea, and human papillomavirus (HPV) are among the most common sexually transmitted infections (STIs). These infections can cause serious health problems if left untreated and can affect anyone who is sexually active. In this post, we’ll explore the causes, symptoms, and treatments of these three prevalent STIs.
Chlamydia:
Causes and Risk Factors:
Chlamydia is…

View On WordPress
#Chlamydia causes#Chlamydia symptoms#Common STIs#Gonorrhea causes#Gonorrhea symptoms#HPV transmission#HPV types#HPV vaccination#prevalent sexually transmitted infections#regular STI testing#safe sex practices#STI treatment options
0 notes
Text
Remus: STDs ARE A STATUS SYMBOL. THE MORE YOU HAVE THE COOLER YOU ARE!
Patton, heavy sighs: ... kiddo, if only you’d seen what I’d seen in that infirmary.
Remus, enthusiastically claps: You GOTTA tell me who had the MOST on ‘em? I bet they-
Patton, forcefully smiling: If you mean sick as dog in the middle of- you know what? How about we talk about something... else.
Remus: Uh. How about no?
Patton, crossing arms: Don’t say I didn’t warn you...
#sanders sides#remus sanders#patton sanders#(mod: blood)#(mod: soy)#stds/#(pat was a combat medic ~2002+)#(pat chooses to be bubbly/kind... but he's Seen Shit)#(also i'm over here gonna say the obv - STIs say jack shit abt someone's character/value)#(just do your best to screen + practice safely + TALK)#(talk w/ partners and especially talk w/ HCPs)#(treatment and support options are out there too)#(one of the big agencies to help there would be planned parenthood but see also your local county resources too)#(mod soy getting off their s3x-posi med nerd pedestal now)
5 notes
·
View notes
Text
CSE post 2/2
The below text is from a pamphlet handed out by my grandma’s church to get their members to attend school board meetings to block Sex education.
Needless to say this is bad and will cause so much harm.
8. PROMOTES EARLY SEXUAL AUTONOMY
Teaches children they can choose to have sex when they feel they are ready or when they find a trusted partner. Fails to provide data about the well-documented negative consequences of early sexual debut. Fails to encourage sexually active children to return to abstinence.
9. FAILS TO ESTABLISH ABSTINENCE AS THE EXPECTED STANDARD
Fails to establish abstinence (or a return to abstinence) as the expected standard for all school-age children. May mention abstinence only in passing. May teach children that all sexual activity-other than "unprotected" vaginal and oral sex- is acceptable, and even healthy. May present abstinence and "protected" sex as equally good options for children.
10. PROMOTES TRANSGENDER IDEOLOGY
Promotes affirmation of and/or exploration of diverse gender identities. May teach children they can change their gender or identify as multiple genders, or may present other unscientific and medically inaccurate theories. Fails to teach that most gender-confused children resolve their confusion by adulthood and that extreme gender confusion is a mental health disorder (gender dysphoria) that can be helped with mental health intervention.
11. PROMOTES CONTRACEPTION / ABORTION TO CHILDREN
Presents abortion as a safe or positive option while omitting data on the many potential negative physical and mental health consequences. May teach children they have a right to abortion and refer them to abortion providers. May encourage the use of contraceptives, while failing to present failure rates or side effects.
12. PROMOTES PEER-TO-PEER SEX ED OR SEXUAL RIGHTS ADVOCACY
May train children to teach other children about sex or sexual pleasure, through peer-to-peer initiatives. May recruit children as spokespeople to advocate for controversial sexual rights (including a right to CSE itself or to promote abortion.
13. UNDERMINES TRADITIONAL VALUES AND BELIEFS
May encourage children to question their parents' beliefs or their cultural or religious values regarding early sex, sexual orientation or gender identity.
14. UNDERMINES PARENTS OR PARENTAL RIGHTS
May instruct children they have rights to confidentiality and privacy from their parents.
May teach children about accessing sexual commodities or services, including abortion, without parental consent. May instruct children not to tell their parents what they are being taught about sex in school.
15. REFERS CHILDREN TO HARMFUL RESOURCESRefers children to harmful websites, materials or outside entities. May also specifically refer children to Planned Parenthood or their affiliates or partners for their lucrative services or commodities (i.e., sexual counseling, condoms, contraceptives, gender hormones, STI testing and treatment, abortions, etc.) Please Note: A conflict of interest exists whenever an entity that profits from sexualizing children is involved in creating or implementing sex education programs. (For more information on how Planned Parenthood sexualizes children for profit see www.WaronChildren.org and www.InvestigateIPPF.org)
#sex education#comprehensive sex education#sex ed#consent#safe sex#lgbtq#school boards#transgender#christianity cw
7 notes
·
View notes
Text
A lot of the comments I get, when arguing that sex workers should not be forced to leave sex work for other jobs which may be worse for them, are like this one:
This is an abuse fantasy. By "fantasy" I don't necessarily mean a sexual one, though there are certainly a lot of people who get off to the idea of sex workers being abused. Lots of SWERFs and radfems fantasize about sex workers being abused in the worst ways possible, and imagine all of us that way, so they can feel more righteous when campaigning for the prohibition of prostitution.
Even among high-volume sex workers, 30 men is an incredibly high number. I worked in brothels where I sometimes did a 12 or 14 hour day, and in that time I saw 12 clients. Seeing 30 clients in one day would be incredibly difficult to achieve, and it's certainly not something that a large proportion of sex workers are doing on a daily basis. Friends I've had who moved countries and sold sex to pay off their debts to the people who made it possible for them to immigrate, under their control, weren't seeing more than 10 clients a day and most days saw far less. This number is pulled from thin air to be more shocking. The vast majority of sex workers are not seeing double-digits of men per day.
The scenario where a sex worker is experiencing constant vaginal and anal tearing, STIs, pregnancy and forced abortions (which seems to assume all sex workers are under the control of 3rd parties), absolutely does not apply to all sex workers. I've never had tearing, never gotten an STI from a client, never gotten pregnant from one... and I've been doing this for 8 years. I've been lucky, certainly, but that demonstrates that these aren't universal experiences. Some of these things do happen to sex workers, with certain issues being more common than others, and these aren't things to be thrown in their faces. There are sex workers I love who get STIs from clients sometimes, or who experience frequent injuries, and they still do sex work because it's the best of their options.
Naturally, I never said sex work is the same as selling coffee, I said that many people will try to rescue sex workers only to push us into worse and more exploitative jobs.
During stints where clients have been treating me well, I've been much less physically damaged and mentally drained by doing sex work than I have by doing bar jobs. SWERFs try to tell me I should leave, and view a bar job as far preferable, even though it was worse for me!
It is the treatment of all sex work as if it is the same, as if it is all uniquely traumatizing, that is endlessly frustrating to me. Sometimes a different job is preferable, and it is the circumstances which prevent us from getting them, and other times sex work is genuinely better than the other jobs available to us. Either way, the solution is to make other jobs better and more accessible, not to try to force us out of sex work!
5 notes
·
View notes
Text
The Pathophysiology Of Spondylitis
Spondylitis is a comprehensive term used to describe a group of chronic inflammatory diseases that primarily affect the joints of the spine and the sacroiliac region, which includes the pelvis and lower spine. These conditions are characterized by arthritis-like symptoms and can lead to significant discomfort, reduced mobility, and other systemic complications. This detailed exploration will indulge into the nature of spondylitis, how it differs from the related condition known as spondylosis, the various types of spondylitis, diagnostic methods, treatment options, and complementary therapies.
What is Spondylitis?

Spondylitis involves inflammation of the joints, tendons, and ligaments within the spine and sacroiliac region. Tendons are connective tissues that attach muscles to bones, while ligaments connect bones to other bones. This inflammation can result in the fusion of bones (ankylosis) and the formation of new bone, leading to stiffness and reduced flexibility in the spine. In severe cases, excessive bone growth can cause significant curvature of the spine, known as kyphosis.
Spondylitis vs. Spondylosis
While both spondylitis and spondylosis cause pain in the hip and back, they are distinct conditions with different etiologies and characteristics.
Spondylitis is an autoimmune disorder where the immune system mistakenly attacks the joints, causing inflammation, bone fusion, and excessive bone formation. This condition typically develops in teenagers and young adults and can affect multiple organs and systems within the body.
Spondylosis, on the other hand, is a degenerative condition associated with aging and the natural wear and tear of the spine. It involves the degeneration of spinal joints and discs, often accompanied by the formation of bone spurs (osteophytes). Spondylosis primarily affects older individuals, with more than 85% of people over the age of 60 experiencing this condition.
Types of Spondylitis
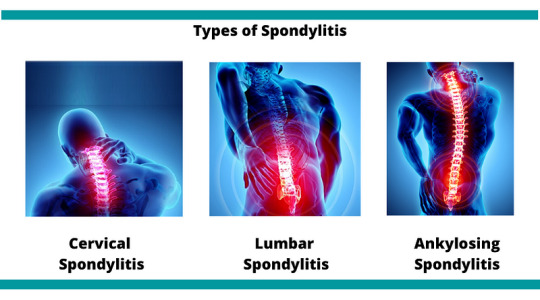
Medical professionals categorize spondylitis using two primary classification systems: the traditional system and the newer system. The traditional system recognizes six specific types of spondylitis, whereas the newer system categorizes spondylitis into two broad types based on the affected body region.
Traditional Spondylitis Classifications:
a) Ankylosing Spondylitis (AS)
Symptoms: Ankylosing spondylitis primarily affects the spine, causing symptoms such as fatigue, chronic back pain, stiffness, and inflammation in various areas of the body, including joints and tendons. Over time, the vertebrae may fuse, leading to reduced mobility and flexibility.
Causes: The exact cause of AS is unknown, but a strong genetic association exists with the HLA-B27 gene. Approximately 90% of individuals with AS carry this gene, although not all carriers develop the disease.
b) Reactive Arthritis
Symptoms: Reactive arthritis typically presents with a triad of symptoms including arthritis (swelling and pain in joints), conjunctivitis (inflammation of the eyes with a sticky discharge), and urethritis (genital and bladder inflammation with painful urination). However, not all patients exhibit all three symptoms.
Causes: often follows a gastrointestinal infection or a sexually transmitted infection (STI). The immune system overreacts to the initial infection, leading to inflammation and joint pain. The HLA-B27 gene is also strongly linked to ReA, with 30–50% of affected individuals carrying this gene.
c) Psoriatic Arthritis (PsA)
Symptoms: Psoriatic arthritis is associated with the inflammatory skin condition psoriasis. Symptoms include dactylitis (swelling in toes and fingers), changes in nails (such as pitting), eye pain, joint pain, reduced range of motion, and fatigue. PsA typically affects people aged 30–50.
Causes: PsA often follows psoriasis, but it can also develop in individuals without skin symptoms. There is a genetic predisposition to PsA, with at least 10% of the population inheriting genes that increase susceptibility to psoriasis and PsA.
d) Enteropathic Arthritis (EnA)
Symptoms
Enteropathic arthritis is linked to inflammatory bowel diseases (IBDs) such as ulcerative colitis and Crohn’s disease. Symptoms include abdominal pain, bloody diarrhea, and joint swelling and pain.
Causes
The precise cause of EnA is unclear, but it is associated with chronic inflammation in the bowel. This inflammation may allow bacteria to penetrate the bowel wall, triggering an immune response that leads to joint inflammation. The HLA-B27 gene is also linked to EnA.
d) Juvenile Spondyloarthritis (JSpA)
Symptoms
Juvenile spondyloarthritis begins in individuals aged 16 or younger and typically affects the leg joints. Symptoms include joint pain, tenderness, and bowel inflammation.
Causes
Similar to adult spondylitis, JSpA is often associated with the HLA-B27 gene. The exact cause remains unknown, but genetic and environmental factors likely play a role.
e)Undifferentiated Spondyloarthritis (USpA)
Symptoms
USpA is characterized by a variety of symptoms that do not fit neatly into a specific rheumatoid disorder. Symptoms may include persistent lower back pain, joint pain in small and large joints, heel pain, swelling in hands and feet, general stiffness, eye inflammation, rash, urinary tract symptoms, and intestinal inflammation.
Causes
The causes of USpA are diverse and not fully understood. It encompasses a range of symptoms that do not meet the criteria for other specific types of spondylitis.
Newer Spondylitis Categorizations
Peripheral Spondyloarthritis (pSpA)
Peripheral spondyloarthritis affects joints and tendons outside the spine and sacroiliac joints, such as the hands, wrists, elbows, shoulders, knees, ankles, and feet. It includes forms of spondylitis such as reactive arthritis, enteropathic arthritis, and undifferentiated arthritis.
2. Axial Spondyloarthritis (AxSpA)
Axial spondyloarthritis involves inflammation and pain in the pelvis and spine. This category covers a broad range of spondylitis types and includes individuals with and without sacroiliac joint fusion. AxSpA is further subdivided into non-radiographic AxSpA (without visible joint damage on X-rays) and radiographic AxSpA (visible joint damage).
Diagnosis
Diagnosing spondylitis involves abroad approach, combining physical examination, medical history, and various diagnostic tests. There is no single definitive test for spondylitis, making a comprehensive evaluation essential.
a) Physical Examination
During a physical examination, the doctor will assess the patient’s symptoms, medical history, and family history of autoimmune diseases such as psoriasis and spondyloarthritis. The examination may include evaluating joint tenderness, swelling, and range of motion.
b) Diagnostic Tests
Blood Tests: Blood tests can help identify markers of inflammation, such as elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Testing for the presence of the HLA-B27 gene can also provide valuable information, although not all individuals with spondylitis carry this gene.
Imaging Tests: Imaging techniques are crucial for diagnosing spondylitis and assessing the extent of joint and bone damage.
X-rays: X-rays can reveal changes in the spine and sacroiliac joints, such as joint fusion and bone spurs.
MRI Scans: MRI scans provide detailed images of soft tissues and can detect early signs of inflammation and joint damage that may not be visible on X-rays.
Ultrasound Scans: Ultrasound scans can be used to assess inflammation in peripheral joints and tendons.
Genetic Testing: Testing for the HLA-B27 gene can support the diagnosis, particularly in cases where clinical symptoms and imaging findings are inconclusive.
Treatment
While there is no cure for spondylitis, various treatments can help manage symptoms, reduce inflammation, and improve the patient’s quality of life. Treatment plans are often tailored to the individual’s specific symptoms and disease severity.
Medications
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs are commonly used to reduce inflammation and pain in spondylitis patients. Examples include ibuprofen and naproxen.
Corticosteroids: Corticosteroids, such as prednisone, can be prescribed for short-term use to control severe inflammation and pain.
Disease-Modifying Antirheumatic Drugs (DMARDs): DMARDs, including methotrexate and sulfasalazine, can help manage symptoms and slow disease progression in some types of spondylitis.
Biologic Agents: Biologic agents, such as tumor necrosis factor (TNF) inhibitors (e.g., adalimumab, etanercept) and interleukin-17 (IL-17) inhibitors (e.g., secukinumab), target specific components of the immune system to reduce inflammation and prevent joint damage.
Analgesics: Pain relievers, such as acetaminophen, may be used to manage pain when inflammation is not the primary issue.
Physical Therapy
Physical therapy plays a crucial role in managing spondylitis by improving and maintaining spine flexibility and overall mobility. Techniques may include:
Massage Therapy: Therapeutic massage can help reduce muscle tension, improve circulation, and alleviate pain.
Spinal Manipulation: Performed by a trained physical therapist or chiropractor, spinal manipulation can enhance mobility and reduce pain.
Exercises: Tailored exercise programs can help strengthen muscles, improve posture, and enhance flexibility. Stretching exercises are particularly beneficial for maintaining spine and joint flexibility.
Breathing Exercises: Breathing exercises are essential for individuals with ankylosing spondylitis, as the condition can affect chest expansion and respiratory function. These exercises help maintain normal lung function and prevent restrictive lung disease.
Surgery: Surgery is generally considered a last resort and is reserved for severe cases where conservative treatments have failed. Surgical options include:
Joint Replacement: For patients with severe joint damage, joint replacement surgery (e.g., hip or knee replacement) can restore function and relieve pain.
Spinal Surgery: In cases of severe spinal deformity or nerve compression, spinal surgery may be necessary to correct curvature and alleviate pressure on nerves.
Complementary Therapies
In addition to conventional treatments, complementary therapies can provide additional symptom relief and improve overall well-being. These therapies are often used alongside standard medical treatments.
Massage Therapy: Massage therapy can help reduce muscle tension, improve blood circulation, and alleviate pain and stiffness in the affected areas.
Relaxation Techniques: Techniques such as deep breathing, progressive muscle relaxation, and meditation can help manage stress and reduce pain perception.
Yoga: Yoga combines physical postures, breathing exercises, and meditation to improve flexibility, strength, and relaxation. Yoga can be particularly beneficial for maintaining spine flexibility and reducing pain.
Acupuncture: Acupuncture involves the insertion of thin needles into specific points on the body to stimulate the nervous system and promote natural pain relief and healing.
Cupping: Cupping is a traditional therapy that involves placing suction cups on the skin to improve blood flow and reduce muscle tension. It can be used to alleviate pain and stiffness in the back and other affected areas.
Summary
Spondylitis encompasses a range of chronic inflammatory diseases that affect the spine and sacroiliac region. It is characterized by autoimmune-driven inflammation, leading to joint pain, stiffness, and potential bone fusion. Spondylitis is distinct from spondylosis, a degenerative condition associated with aging. Medical professionals classify spondylitis into various types based on symptoms and affected body regions. Diagnosis involves a combination of physical examination, medical history, blood tests, imaging, and genetic testing. While there is no cure, treatments such as medications, physical therapy, and complementary therapies can help manage symptoms and improve the quality of life for those affected by spondylitis. By understanding the nature of spondylitis and the available management strategies, individuals can better navigate their condition and maintain an active, fulfilling life.
Medical students and healthcare professionals need to stay informed about the latest advancements in diagnosing and treating spondylitis. Continuous education and expert guidance are crucial for managing these complex conditions. For additional support with challenging medical units, clinical studies, research projects, assignments, and exam preparation, Expert Academic Assignment Help offers professional resources and online classes. For personalized assistance, contact [email protected] Accessing expert guidance can significantly enhance your understanding and proficiency in medical education.
#medical students#assignment help#nursing school#nursing student#medicine#healthcare#student life#medical student#studyblr#case study#student#online writing#do my online class#essay writing#phd research#clinical research#research#phd thesis writing service#phdjourney#phd life#phdblr#studying#study blog#study motivation#studyspo#study aesthetic
4 notes
·
View notes
Note
Hey just one small note: people who have HIV and on medications are still immune compromised so they unfortunately aren't fully 'healthy" like everyone else ("they’ll be as healthy as anyone else") they are still at greater risk of getting sick / more sick from other things such as but not limited to covid.
I'm struggling to form the sentence but the medication makes the virus non transmitable but unfortunately there are still other side effects/ symptoms from having the virus.
But here are some other ways to protect yourself and others: have open and honest conversation with partners about STIs and status, use protection, if you amab look into PrEP options to reduce the risk of infection even further, it's so important to have conversations with partners and friends to get tested and get yourself tested regularly (and especially between partners) know your status.
I have a family member living with HIV, I really appreciate you writing this fic and thoroughly enjoyed it (looking forward to another part!). I just wanted to clarify and inform so I hope this hasn't come off the wrong way 🧡🖤
Hello, yes. Thank you for your concern and for reaching out to me. You are right with the points that you make (I’ll explain more)
Most people can have their immune cells recover to the point of Immuno competency, but that doesn't mean everyone does. According to this research, HIV treatment can greatly improves immune functions. Typically, the rate of immune cells (CD4) recovery will be most rapid in the first 3 months, followed by gradual increase over time, for at least a decade. While most individuals who's on meds can have their immune cells recover to the point of Immuno competency again (CD4 > 500), approximately 15-20% of individuals who initiates meds at a very low immune cells (CD4 count <200) may plateau at abnormally low immune cell count (CD4), making them still immunocompromised and susceptible to infections. In other words, most people will not be immunocompromised after being treated, but some may still be. Not every case will be the same.
And I'm aware of the side effects of the medications, and symptoms of the virus that people can still have. These are something that varies between person to person, meds to meds, case to case. It is possible for someone to not experience this at all, while others may have them mildly, some may affect their lives. Even people who take the same meds can have different side effects from each other.
But newer generation meds cause fewer side effects than medication used in the past. And overall, the benefits of HIV medicines far outweigh the risk of side effects. And health care providers are assigned to screen and manage these symptoms in the best of their abilities. (Cite 1, 2)
I do believe that as time has passed, the less likely people will get these side effects, as treatment will get better. Hell, a cure might even be available in the future, who knows!
I want to write this so that people won't be scared of the present and can remain hopeful of the future. Because despite of the limitations that we're still facing, it is inevitable that things will get better. I do wish your family well, and I'm so glad you found this fic helpful and a joy to read. I will publish the next part soon. I hope you'll enjoy it too ❤️❤️
2 notes
·
View notes
Text
Understanding Urethral Stricture: Causes, Symptoms, and Treatment
Urethral Stricture: Causes, Symptoms, and Treatment
Urethral stricture is a narrowing of the urethra, the tube that carries urine from the bladder out of the body. This condition can lead to various urinary problems and discomfort. Understanding the causes, symptoms, and treatment options for urethral stricture is essential for proper management.
Causes of Urethral Stricture
Urethral stricture can be caused by several factors, including:
Trauma: Trauma to the urethra, such as from a pelvic fracture or a straddle injury, can lead to the formation of scar tissue, which can narrow the urethra.
Infection: Infections, such as sexually transmitted infections (STIs) like gonorrhea or chlamydia, can cause inflammation and scarring of the urethra, leading to stricture formation.
Inflammation: Chronic inflammation of the urethra, often due to conditions like urethritis or balanitis, can result in the narrowing of the urethra over time.
Medical Procedures: Certain medical procedures, such as catheterization or surgery involving the urethra, can increase the risk of developing a urethral stricture.
Congenital Factors: Some individuals may be born with a narrow urethra, predisposing them to developing strictures later in life.
Symptoms of Urethral Stricture
The symptoms of urethral stricture can vary depending on the severity of the narrowing. Common symptoms include:
Difficulty Urinating: Narrowing of the urethra can make it difficult to start urination or maintain a steady stream.
Urinary Retention: In severe cases, urethral stricture can lead to the inability to urinate, which requires immediate medical attention.
Urinary Tract Infections (UTIs): Narrowing of the urethra can increase the risk of UTIs due to incomplete bladder emptying.
Urinary Frequency and Urgency: Strictures can cause the bladder to contract more frequently, leading to a constant urge to urinate.
Spraying or Dribbling of Urine: The narrowing of the urethra can cause the urine stream to spray or dribble instead of flowing in a steady stream.
Pain or Discomfort: Some individuals may experience pain or discomfort during urination, ejaculation, or while passing urine.
Treatment Options for Urethral Stricture
Treatment for urethral stricture depends on the severity of the condition and may include:
Dilation: This involves stretching the narrowed portion of the urethra using a series of dilators of increasing size. It is a common treatment option for less severe strictures.
Urethrotomy: This procedure involves using a special instrument to cut the stricture, widening the urethra. It is often used for short strictures.
Urethroplasty: In more severe cases, surgery may be required to remove the narrowed portion of the urethra and reconstruct it using tissue from other parts of the body.
Medication: In some cases, medications may be prescribed to help reduce inflammation and prevent further scarring of the urethra.
Self-Catheterization: Some individuals may need to perform self-catheterization regularly to help keep the urethra open and maintain urine flow.
Conclusion
Urethral stricture is a condition that can cause significant urinary problems and discomfort. Understanding the causes, symptoms, and treatment options for urethral stricture is crucial for effectively managing the condition. If you experience symptoms of urethral stricture, it is important to consult with a healthcare professional for proper evaluation and treatment.
#Urethral stricture#urethral penetration#urethral stricture symptoms#urethral stricture causes#urethral stricture treatment#best doctor for urethral stricture#best urologist for urethral stricture
2 notes
·
View notes
Note
are you still alive?
oops-
yeah, i'm alive and here. i've just been incredibly busy with school stuff. i'll be done with school (mostly) on april 26 and after that i will have so. much. time.
i'll put it under the cut so no one has to see it if they don't want, but if anyone is interested in pharmacy school stuff then here's what i've been doing lately:
For one, I started my rotations at the university hospital! I'm doing admissions medication reconciliation, which basically means I get assigned a few patients and I spend the rest of the day contacting the patients, family, pharmacies, whoever I need to in order to get the most up-to-date list of medications, how they're supposed to be taken, how they're actually taken, and when the last dose was taken. It's been extremely rewarding and I love getting more exposure to hospital work but it's definitely exhausting.
It's also comprehensive final time for our IP class. IP is integrated pharmacotherapy, so basically it's the course where we go disease state by disease state and learn background, etiology, diagnosis, treatment options, as well as science of the medications such as structure/medicinal chemistry, pharmacology, drug interactions/contraindications, monitoring parameters, counseling points, and how to choose between all of them. For this comprehensive final we're covering GI diseases, such as GERD, PUD, IBS, IBD, Ulcerative Colitis, Crohn's Disease, as well as Infectious Disease which is a ton of antibiotic/antifungal information as well as treatment for HAP/VAP/CAP, Fungal Infections, Helminths/Ectoparasites/Protozoa, TB, Malaria, C. Diff, Skin Infections, Intra-Abdominal Infections, AOM, Pharyngitis, Sinusitis, UTIs, and STIs. It's. A. Lot.
I also have my Top 200 drugs exam coming up. This is where they test us on the Top 200 outpatient drugs, the Top 50 OTC drugs, and the Top 50 inpatient drugs. For this, we have to know brand name, generic name, mechanism of action, monitoring parameters, side effects, drug interactions, counseling points, contraindications, and any black box warnings they have.
Also, it's program-level assessment time. What does this mean? Well, at the end of every year, we have to take a written exam and a practical exam for all of the content we've learned this far in pharmacy school. So, my 2 hour written exam will cover all content from last year and this year, and my practical exam will have us interviewing a patient and doing that kind of work for 2 hours based on disease states we've covered thus far. It's exactly as stressful as it sounds and I've been studying like wild.
Overall, I'm so excited to finally be learning treatment stuff and really getting exposure to working in the places I hope to work in as a career someday, but it's also been pretty stressful this past month especially. People say the post-spring break of this year is notoriously some of the most difficult anyone in the program will go through, so we're working hard!
10 notes
·
View notes
Text
Hello . This is kind of weird and left field but I would like to talk about the unprotected sex tags in fic that are followed by the “(wrap it up irl)” disclaimer or some variation of it, and why it. Bothers me a little?
Don’t get me wrong, this is good advice! But… a lot of times that same fic will have, say, oral sex, which is also unprotected but is not followed by a similar warning. Also, there are cases where protection might not be strictly necessary! Let me break this down a little bit.
My hunch is that most of the time these disclaimers are aimed to remind people reading the fic who might be hooking up or dating irl that the fic is, indeed, fiction, and irl you need to be careful about protection when you don’t know someone else’s situation when it comes to STIs and birth control. Which is fair! If you don’t know someone’s STI status, you should absolutely wear protection out of an abundance of caution. Also, even if your partner is on birth control, condoms can still help prevent pregnancy; BC is still only 99% effective when used perfectly, and less effective with typical use (about 93%). Condoms when used perfectly are about 98% effective, and about 87% effective with typical use. Obviously you can’t just add these together and say using both at the same time is 100% effective, no matter how many precautions you take there is still SOME chance, but using both can get you damn close to 100%.
However, many people making those disclaimers fail to follow up other tags with the same disclaimer, from oral sex to fingering to anal to whatever else. Penis in vagina sex is not the only way to pass on STIs! During oral sex (whether that’s eating someone out or rimming), if you’re unsure what your partner’s STI status is, you can use dental dams and condoms to prevent transmission. During fingering, you can use gloves. In my opinion you should always use condoms when doing anal sex regardless; for a penis-haver doing the penetrating, it’s a pretty good way to get a UTI. (Also, putting condoms on toys can help cleanup afterwards and prevent transmission as well!) (Double also, the fecal oral route is very real and rimming without a dental dam could quite literally give you food poisoning so… y’know)
THAT SAID, if you’re positive everyone involved has been tested and is negative for STIs, and folks who can get pregnant are on birth control, and you’re willing to risk that birth control potentially failing without the additional buffer of barrier protection… you probably can get away with not, in fact, wrapping it up irl. And it’s really really easy to get tested for STIs. Just roll up to your local health department, planned parenthood, or ask your primary care provider. There are also home testing kits available. And please get tested regularly if you’re active with multiple partners, even if you are using barrier protection! The peace of mind is worth it, and if you have contracted something, getting it detected early will usually help you with treatment options!
Anyway. All of this is to say that while the disclaimer it’s good advice, there’s a lot of nuance to it, and you should make the best decisions for your health and your body!
6 notes
·
View notes
Photo

Ovaries are present on both sides of the pelvis, which release eggs and have an extremely important role in the fertilization process. If you are suffering from ovarian pain, it can be for two reasons, menstruation and ovulation! This pain can generally be felt in the pelvis, lower back, and lower abdomen.
Though the pain is associated with the menstrual cycle, it can also be caused due to certain other reasons that you should not ignore! It can be endometriosis or STI, leading to unbearable ovarian pain. Apart from these, specific health conditions of the digestive and urinary systems can be the underlying cause of ovarian pain. To know the real cause behind this pain, you need to consult with your doctor and undergo the prescribed diagnosis and get a proper treatment to heal the same! Here’s everything you should know about ovarian pain, its causes, and the different treatment options available.
Read More: https://www.drshubhragoyal.com/welcome/blogs/an-overview-of-types-of-ovarian-pain-and-treatment-options
#stabbing pain in the left ovary#types of ovarian cysts#ovary pain location#ovary pain on the right side#left ovary pain before period#ovarian pain or appendix#Best Gynecologist Doctor In Agra#Top Gynaecologist In Agra
2 notes
·
View notes
Text
I have a pt in Descovy for PrEP. Their website has all the info you should know about how to monitor for adverse effects on this medication.
What is DESCOVY for PrEP?
DESCOVY for PrEP (pre-exposure prophylaxis) is a once-daily prescription medicine for adults and adolescents at risk of HIV. It helps lower the chances of getting HIV through sex.
DESCOVY for PrEP is not for everyone:
It is not for use in people assigned female at birth who are at risk of getting HIV from vaginal sex, because its effectiveness has not been studied.
You must be HIV-negative before and while taking DESCOVY for PrEP. Talk to a healthcare provider to see if DESCOVY for PrEP may be an option for you.
Important Safety Information
What is the most important information I should know about DESCOVY for PrEP?
Before and while taking DESCOVY for PrEP:
You must be HIV-negative before you start and while taking DESCOVY for PrEP. You must get tested for HIV-1 immediately before and at least every 3 months while taking DESCOVY. If you think you were exposed to HIV-1, tell your healthcare provider right away. They may want to do more tests to confirm that you are still HIV-negative.
Many HIV-1 tests can miss HIV-1 infection in a person who has recently become infected. Tell your healthcare provider if you had a flu-like illness within the last month before starting or while taking DESCOVY. Symptoms of new HIV-1 infection include tiredness, fever, joint or muscle aches, headache, sore throat, vomiting, diarrhea, rash, night sweats, and/or enlarged lymph nodes in the neck or groin.
DESCOVY by itself is not a complete treatment for HIV-1. Do not take DESCOVY for PrEP unless you are confirmed to be HIV-1 negative.
DESCOVY does not prevent other sexually transmitted infections (STIs). Practice safer sex by using a latex or polyurethane condom to reduce the risk of getting STIs.
To further help reduce your risk of getting HIV-1:
Do not miss any doses of DESCOVY. Missing doses may increase your risk of getting HIV-1.
Know your HIV status and the HIV status of your partners. If your partner is living with HIV, your risk of getting HIV is lower if your partner consistently takes HIV treatment every day.
Get tested for other STIs. Some STIs make it easier for HIV-1 to infect you.
Talk to your healthcare provider about all the ways to help reduce HIV risk.
DESCOVY can cause serious side effects:
Worsening of hepatitis B (HBV) infection. Your healthcare provider will test you for HBV. If you have HBV and stop taking DESCOVY, your HBV may suddenly get worse. Do not stop taking DESCOVY without first talking to your healthcare provider, as they will need to check your health or give you HBV medicine.
Who should not take DESCOVY for PrEP?
Do not take DESCOVY for PrEP if you:
Already have HIV-1 or if you do not know your HIV-1 status. If you have HIV-1, you need to take other medicines with DESCOVY to treat HIV-1. If you have HIV-1 and take only DESCOVY, your HIV-1 may become harder to treat now and in the future.
What are the other possible side effects of DESCOVY for PrEP?
Serious side effects of DESCOVY may also include:
Kidney problems, including kidney failure. Your healthcare provider should do blood and urine tests to check your kidneys before and during treatment with DESCOVY. If you develop kidney problems, your healthcare provider may tell you to stop taking DESCOVY.
Too much lactic acid in your blood (lactic acidosis), which is a serious but rare medical emergency that can lead to death. Tell your healthcare provider right away if you get these symptoms: weakness or being more tired than usual, unusual muscle pain, being short of breath or fast breathing, stomach pain with nausea and vomiting, cold or blue hands and feet, feel dizzy or lightheaded, or a fast or abnormal heartbeat.
Severe liver problems, which in rare cases can lead to death. Tell your healthcare provider right away if you get these symptoms: skin or the white part of your eyes turns yellow, dark "tea-colored" urine, light-colored stools, loss of appetite for several days or longer, nausea, or stomach-area pain.
Common side effects in people taking DESCOVY for PrEP are diarrhea, nausea, headache, fatigue, and stomach pain. Tell your healthcare provider if you have any side effects that bother you or do not go away.
What should I tell my healthcare provider before taking DESCOVY for PrEP? All your health problems. Be sure to tell your healthcare provider if you have or have had any kidney or liver problems, including hepatitis. All the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. DESCOVY may interact with other medicines. Keep a list of all your medicines and show it to your healthcare provider and pharmacist when you get a new medicine.v You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch, or call 1-800-FDA-1088.
What is DESCOVY for PrEP?
DESCOVY for PrEP (pre-exposure prophylaxis) is a once-daily prescription medicine for adults and adolescents at risk of HIV. It helps lower the chances of getting HIV through sex.
DESCOVY for PrEP is not for everyone:
It is not for use in people assigned female at birth who are at risk of getting HIV from vaginal sex, because its effectiveness has not been studied.
You must be HIV-negative before and while taking DESCOVY for PrEP. Talk to a healthcare provider to see if DESCOVY for PrEP may be an option for you.
2 notes
·
View notes
Note
need: resources (im in canada if that makes any difference)
tw references sexual assault
do you guys have a link to that post about what tests and vaccines/treatments you can get after you were forced too have sexual contact with someone and you dont know if they have anything? im tryg to find it somewhere and i really need its advice
thank you a tonn
Hi anon,
I'm sorry about what happened to you. I'm not sure which post you're referring to so I can give you some resources here.
Firstly I would recommend taking note of any symptoms you may be having right now, if any. Even if you don't have any symptoms at the moment, it's important to remember that you may still be carrying a dormant STI, so an examination may still be necessary. It will be convenient to have an inventory of your symptoms to make a potential medical examination easier.
You may want to look into an appointment with a healthcare provider such as a gynecologist or urologist. Depending on how long ago the assault occurred and what local hospitals are participating, you may be able to receive a sexual assault forensic medical examination. Also depending on what STIs are suspected, they may also need to conduct a blood or urine test (for cases such as HIV).
This resource also says that there are at-home STI tests available in Canada, which is especially convenient if you do not have a family physician. Looking further into this however, it looks like the only available test through their website is for HPV testing. So it may be a better option to seek professional medical care to be able to get tested for multiple STIs.
This resource states that you can get tested via your healthcare provider, a sexual health clinic such as Planned Parenthood, a local public health unit, or a walk-in clinic.
Here is a list of Canadian sexual assault hotlines you can also reach out to. Here is also a list of Canadian sexual health services.
I hope I could help. Best of luck with everything. Please let us know if you need anything.
-Bun
3 notes
·
View notes
Text
Preventive Measures for Pelvic Inflammatory Disease (PID)

Pelvic Inflammatory Disease (PID) is a significant concern for women’s health, often causing discomfort, complications, and potential long-term effects on fertility. It’s a condition that arises from untreated or inadequately treated infections, primarily sexually transmitted infections (STIs) like chlamydia and gonorrhea. However, with proactive steps and awareness, it’s possible to significantly reduce the risk of developing PID.
10 tips to prevent PID and enhance reproductive health.
1. Practice Safe Sex: Consistent and correct use of condoms during sexual intercourse can significantly reduce the risk of contracting STIs, which are the primary culprits behind PID. Additionally, limiting sexual partners and being mindful of the sexual history of partners can further mitigate the risk of exposure to infections.
2. Regular STI Screening: Early detection leads to preventing PID. Regular screenings for STIs, especially if you’re sexually active or have multiple partners, can help identify and treat infections promptly, preventing them from progressing to PID. Consult with your healthcare provider to determine the frequency of screenings based on your risk factors.
3. Prompt Treatment of Infections: If diagnosed with an STI, seek prompt treatment and ensure that your partner(s) also receive treatment to prevent reinfection. Untreated STIs can lead to the spread of infection to the reproductive organs, increasing the likelihood of developing PID.
4. Maintain Good Hygiene Practices: Practicing good hygiene, including regular washing of the genital area, can help prevent the spread of bacteria and reduce the risk of infections that could lead to PID. However, avoid douching, as it can disrupt the natural balance of bacteria in the vagina and increase susceptibility to infections.
5. Communicate with Your Healthcare Provider: Honest communication with your healthcare provider is crucial for maintaining reproductive health. Discuss any concerns or symptoms you can have promptly, as early intervention can prevent complications such as PID. Your healthcare provider can also guide preventive measures tailored to your individual needs.
6. Consider Vaccination: Vaccines are available for certain STIs, such as human papillomavirus (HPV) and hepatitis B, which can indirectly reduce the risk of PID by preventing related infections. Talk to your healthcare provider about vaccination options and whether they are appropriate for you.
7. Avoid Risky Sexual Behaviors: Engaging in high-risk sexual behaviors, such as unprotected sex with multiple partners or engaging in sexual activity while under the influence of drugs or alcohol, increases the likelihood of exposure to STIs. Taking steps to avoid these behaviors can significantly lower your risk of developing PID.
8. Follow-up Care: If you’ve been treated for an STI or PID, adhere to any follow-up care suggested by your gynecologist. This may include additional screenings or tests to ensure that the infection has been fully resolved and to monitor for any potential complications.
9. Educate Yourself and Others: Knowledge is empowering when it comes to protecting your health. Take the time to educate yourself about STIs, PID, and preventive measures you can take. Share this information with friends, family, and peers to promote awareness and encourage proactive health practices.
10. Prioritize Self-care and Overall Health: Maintaining a healthy lifestyle, including eating a balanced diet, exercising regularly, managing stress, and getting enough sleep, can support your immune system and overall well-being. A healthy body is better equipped to fight off infections and recover from illnesses, reducing the risk of complications like PID.
Final word of advice
While PID is a serious condition, it is largely preventable with the proper precautions and proactive measures. By prioritizing safe sex practices, regular screenings, prompt treatment of infections, and overall self-care, women can significantly reduce their risk of developing PID and promote their reproductive health and well-being. Remember, your health is in your hands, so take charge and take steps to protect it.
0 notes
Text
Key Roles Gynecologist Fulfill In Family Planning!
Gynecologists play a crucial role in family planning by providing comprehensive healthcare services related to reproductive health. The Best Gynecologist In Thane offers everyone excellent quality medical assistance, and here are some key roles they fulfill in family planning:

Contraceptive Counseling: Gynecologists offer personalized counseling to individuals and couples regarding various contraceptive methods available for family planning. They discuss the benefits, risks, and effectiveness of different birth control options to help patients make informed decisions based on their preferences and medical history.
Prescribing Contraceptives: Based on the patient's health status, reproductive goals, and preferences, gynecologists prescribe contraceptive methods such as oral contraceptives (birth control pills), contraceptive injections, intrauterine devices (IUDs), contraceptive implants, and barrier methods like condoms or diaphragms.
Family Planning Consultations: Gynecologists provide consultations to individuals and couples who are planning to start or expand their families. They offer guidance on optimal timing for conception, fertility awareness methods, preconception counseling, and lifestyle modifications to enhance fertility.
Fertility Assessment: Gynecologists assess and evaluate the fertility of individuals or couples facing challenges in conceiving. They conduct tests and investigations to identify underlying factors contributing to infertility and provide treatment options such as fertility medications, assisted reproductive technologies (ART), or referral to fertility specialists when necessary.
Prenatal Care: Gynecologists offer prenatal care services to pregnant individuals to ensure a healthy pregnancy and safe delivery. They monitor maternal and fetal health, perform routine screenings and diagnostic tests, provide guidance on nutrition, exercise, and childbirth preparation, and address any concerns or complications that may arise during pregnancy.
Postpartum Care: Gynecologists provide postpartum care to new mothers, including physical and emotional support, breastfeeding guidance, contraceptive counseling, and monitoring for postpartum complications. They play a vital role in promoting maternal well-being and facilitating the transition to parenthood.
Reproductive Health Screenings: Gynecologists perform routine screenings and tests for sexually transmitted infections (STIs), cervical cancer (Pap smear), breast cancer (clinical breast exam), and other reproductive health conditions. Early detection and treatment of these conditions are essential for maintaining overall reproductive health and fertility.
If you are looking for the Best Gynecologist in Waghbil, then you don’t have to search for it because Dr. Vidya Shetty is here at your service.
About Dr. Vidya Shetty
Dr. Vidya Shetty is one of the leading names because it is offering different types of gynecological treatment at nominal prices. The doctor has access to a wide range of tools and technology, with the help of which she assures that everything is done flawlessly and as per the needs of the patient.
Credit:- https://penzu.com/p/37559b8f97b6e19a
0 notes
Text
Health Matters: Insights into Adolescent and Young Adult Well-being
Introduction
Adolescence and young adulthood are critical periods in life, characterized by significant physical, emotional, and social changes. During this time, establishing healthy habits and addressing mental and physical health challenges is crucial for long-term well-being. In this blog, we'll explore key aspects of adolescent and young adult health, providing insights and tips to help navigate these transformative years.
Physical Health
1. Nutrition and Diet: Proper nutrition is fundamental to supporting the rapid growth and development occurring during adolescence and young adulthood. A balanced diet rich in fruits, vegetables, lean proteins, and whole grains provides the necessary vitamins and minerals. Adolescents should be encouraged to develop healthy eating habits, avoid excessive consumption of junk food, and understand the importance of hydration.
2. Physical Activity: Regular physical activity is essential for maintaining a healthy weight, building strong bones and muscles, and reducing the risk of chronic diseases. Activities like sports, dance, or even daily brisk walks can be highly beneficial. Aim for at least 60 minutes of moderate to vigorous physical activity each day.
3. Sleep: Adequate sleep is vital for physical and mental health. Adolescents need about 8-10 hours of sleep per night. Sleep deprivation can lead to issues such as decreased academic performance, mood swings, and increased susceptibility to illness. Establishing a consistent sleep routine and creating a restful environment can help improve sleep quality.
Mental Health
1. Stress Management: Adolescents and young adults often face stress related to school, social relationships, and future uncertainties. Learning effective stress management techniques, such as mindfulness, deep breathing exercises, and time management skills, can significantly improve mental health.
2. Mental Health Awareness: It's crucial to break the stigma surrounding mental health. Encouraging open conversations about mental health issues

3. Social Connections: Strong social connections are important for emotional well-being. Encouraging positive relationships with peers, family, and mentors can provide a support system during challenging times. Engaging in community activities or clubs can also help build a sense of belonging.
Important Information:
Conference Name: 15th American Healthcare, Hospital Management, Nursing, And Patient Safety Summit
Short Name: # 15AHNPSUCG2025
Dates: May 14-16,2025
Venue: San Francisco, United States & Virtual
Email: [email protected]
Visit: https://health.universeconferences.com/
Call for Papers: https://health.universeconferences.com/call-for-paper/Register here: https://health.universeconferences.com/registration/Call/WhatsApp Us: +442033222718
Substance Use and Abuse
1. Education and Awareness: Education about the risks of substance use, including alcohol, drugs, and tobacco, is essential. Understanding the long-term consequences and the impact on physical and mental health can deter adolescents from experimenting with substances.
2. Prevention Programs: Participation in prevention programs at school or in the community can provide adolescents with the skills and knowledge to make informed choices. These programs often include strategies to resist peer pressure and information on healthy coping mechanisms.
3. Support for Addictions: For those struggling with substance abuse, seeking help early is crucial. Support can come from healthcare providers, counselors, or specialized addiction treatment programs. Family and peer support also play a significant role in recovery.
Sexual and Reproductive Health
1. Comprehensive Sex Education: Access to comprehensive sex education helps adolescents make informed decisions about their sexual health. This includes understanding consent, contraception options, and the prevention of sexually transmitted infections (STIs).
2. Access to Healthcare Services: Adolescents should have access to confidential and youth-friendly healthcare services. Regular check-ups, vaccinations, and screenings are important aspects of maintaining reproductive health.
3. Healthy Relationships: Promoting healthy relationships and understanding the dynamics of consent, respect, and communication in romantic and sexual relationships is vital. Encouraging adolescents to set boundaries and recognize unhealthy behaviors can prevent issues such as dating violence and coercion.
Conclusion
Adolescence and young adulthood are foundational periods for establishing lifelong health and well-being. By focusing on physical health, mental health, substance use prevention, and sexual and reproductive health, we can equip young individuals with the tools they need to navigate these years successfully. Through education, support, and access to resources, we can help ensure that the journey to adulthood is a healthy and fulfilling one.
0 notes
Text
Best Urologist In Kukatpally Hyderabad.
My health hospital is a leading surgery provider in the area of Kphb, Kukatpally, Hyderabad and is associated with one of the best urologists and andrologists in hyderabad who are trained in treatment of urological and andrological problems with 10+ years of experience . We have listed some of the most common problems & their treatments provided at My health hospital below. Book an appointment and meet your doctor today to know the best treatment option for the problem .
Urologist / Urology Specialist / Urology Doctor is a super specialist in the field of surgery dealing with problems related to Male and Female Urinary Tract which includes Kidney Stones treatment (laser), Prostate surgery (laser and conventional), treatment of urinary tract infections (simple and complex), urinary incontinence treatment (medical and surgical), circumcision(laser/stapler/conventional), treatment of testicular infections( Epidydimitis , orchitis, Epidydimo orchitis), surgical treatment of scrotal swellings(Hydrocele/Hernia), Renal cysts, kidney, bladder/prostate cancer, and treatment of lower urinary tract symptoms( Frequency/urgency/dysuria /blood in urine( Haematuria )/ Nocturia /poor stream) and performs necessary procedures for diagnosis (cystoscopy) and therepeutic purposes for the best treatment of patients having any of the above urological problems.
Andrologist / Male infertility specialist / ED (Ejaculatory dysfunction) doctor is a urologist trained in dealing with problems related to male reproductive system(penis/urethra/testis/seminal vesicles) which include problems related to unprotected sex (STD/STI- Sexually transmitted infections/sexually transmitted diseases) and problems with sexual intercourse( ED(Ejaculatory Dysfunction)/Premature ejaculation) and treatment of male infertility problems related to pregnancy(medical and surgical -varicocele and its treatment )
#best urologist in kukatpally hyderabad#urologist#best hospital in hyderabad#best kidney stone treatment in kukatpally#best hospital#hospitals near me
2 notes
·
View notes