#nephrology
Text
“Have you not heard the ancient nephrological proverb? ‘Those who don’t pee, [go to] shit’.”
41 notes
·
View notes
Text
It’s fun to notice when college has completely broken your will to argue. Yeah, sure, hypervolemia is a sodium issue and hypernatremia is a water issue. Sure, professor. Why not.
#not saying he’s wrong at all!!! I wholeheartedly trust this guy he’s so smart#BUT WHY DID THEY NAME IT LIKE THIS#BRO#medblr#nephrology
7 notes
·
View notes
Text

Monday, 4th of December 2023
I went to a coffee shop to study. It was hella productive. Did 30 MKSAP nephrology questions AND made anki cards. Love that.
#medstudyblr#medicine#medstudlife#medstudent#med student#productivity#being productive#productive#study notes#study time#internalmedicine#internal medicine#nephrology#coffeeshop
14 notes
·
View notes
Text

So I’ve reached out just about everywhere trying to get others to donate to help cover my medical expenses. I’ve gotten some donations, but still haven’t reached my goal as it is much needed to do so. If you click the link it will take you to my go fund me and my story is written out there. Everyone please share this to help me out with these medical bills that have been piling up. Just a 100 dollar donation could get me closer to meeting my goal and most importantly, getting these medical bills payed off. Just a 50 dollar donation could help me with putting fuel in my vehicle to get me back and forth to my appointments as I do have quite a few of those. Nonetheless, anything is always appreciated. Thank you in advance and may God bless you back 100 times whatever you may give.
#gofundme#dialysis#need help#donations#health issues#hospital#please share#medical bills#medical problems#kidney transplant#godisgood#no work#unemployed#disability#thank you#please donate#donate if you can#pls donate#a good cause#nephrology#kidney treatment#kidneyhealth#kidneycare#kidney diseases
12 notes
·
View notes
Text
Vancomycin can cause ATN if the vancomycin level is supratherapeutic. After getting contrast, the Cr can continue to increase and peak 3 to 4 days after getting contrast.
Giving IV fluids and correcting acidosis prevent contrast-induced nephropathy.
Acute interstitial nephritis (AIN) will show WBC casts in the urine. The rise in the Cr level is slow in AIN.
Nephrogenic systemic fibrosis is due to the old type of gadolinium contrast used for MRI. The new gadolinium contrast has not yet been shown to cause nephrogenic systemic fibrosis. Nephrologists recommend not giving this contrast if the GFR is less than 30, but radiology guidelines still give it even if GFR is less than 30. Dialysis doesn't help with preventing the injury due to iodinated contrast.
Bicarbonate correction to greater than 22 helps prevent progression of CKD. Had a pt today who is on sodium bicarbonate to help with preventing progression of his CKD.
3 notes
·
View notes
Photo
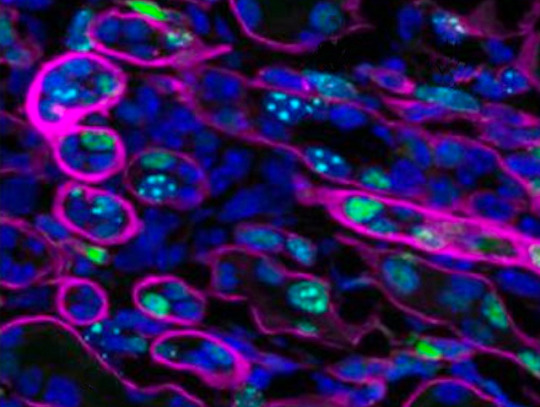
Cause and Effect
It’s possible to know what's causing a problem without understanding how it's doing harm. Researchers knew that mutations in the gene which makes the protein INVS is linked to nephronophthisis – a cause of kidney failure in young people. But without understanding the mechanism, this knowledge hasn’t led to new treatments. A new study examined the effect of removing INVS from various kidney cells, and found that cysts and scarring – symptoms of nephronophthisis – then arose in kidney lining cells but not others. These impacts were reduced when cilia – tiny protrusions from cells – were removed, suggesting they are key to the disease progression. They observed some affected cells over-proliferating (green in the kidney section pictured, with lining cells encircled in pink), which is a driver of cysts. Armed with this understanding, the researchers discovered a new potential treatment, valproic acid, which is already in use for other conditions like epilepsy.
Written by Anthony Lewis
Image from work by Yuanyuan Li and Wenyan Xu, and colleagues
Department of Genetics, Yale University School of Medicine, New Haven, CT, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in eLife, March 2023
You can also follow BPoD on Instagram, Twitter and Facebook
6 notes
·
View notes
Text
#doctor#med student#med school#medblr#studyblr#study inspiration#studyspo#study motivation#studywithme#study aesthetic#academia#light academia#romantic academia#muji pens#muji#sakura micron#ikea#first aid#usmle step 1#nephrology#kidneys#nephrotic syndrome
42 notes
·
View notes
Note
Hi Wayfaring! My dad found out that he has kidney disease from his autoimmune disease getting worse. We hear a lot of terms like kidney function % and protein being in his urine. Would you please do a lil rundown on kidney disease and what these things mean? Can kidney function improve and can the cells regrow or is it just that he needs to stop it getting worse because they can’t be repaired? Thank you :)
Ok, here’s some basic definitions for kidney disease:
- GFR or creatinine clearance: a number indicating how well the kidneys are filtering proteins and other wastes out of the blood. A normal GFR would be >60. When they’re talking about % of normal kidney function that’s more of a layman’s term and isn’t as specific.
- chronic kidney disease: broken down into stages defined by GFR or creatinine clearance. Stages 1 and 2 are essentially normal kidney function. Stage 3 (3a is a GFR of 45-59. 3b is GFR of 30-44) is where we start having to adjust dosages on certain drugs because the kidneys don’t clear them as quickly as normal. Stage 5 (GFR of <15) is end stage renal failure, where a person would be on dialysis and/or a transplant list.
- protein being in the urine is basically from leaky filters. There are lots of things that can cause protein in the urine.
Kidney function can improve depending on what is damaging it. In the case of an autoimmune disease, it typically clogs up the filtration system with antibodies, so as the antibodies decrease, the filtration improves. The problem comes when things get so clogged up that the tissue can’t get adequate oxygen and dies. That would not be reversible and the kidney does not regenerate like the liver does. Knowing whether the damage was permanent or not would really require a kidney biopsy. Ultimately with kidney disease you try to slow down progression of disease as much as possible to prevent having to move to dialysis or transplant.
16 notes
·
View notes
Text
Dr Sachin Soni, the leading nephrologist in Aurangabad. With a wealth of experience and a dedication to providing exceptional care, Dr Soni is committed to helping patients with kidney disorders achieve optimal health.
#DrSachinSoni#nephrologist#Aurangabad#kidneycare#optimalhealth#bestnephrologist#kidneydisorders#kidneyspecialist#nephrology#healthcare#india
2 notes
·
View notes
Photo
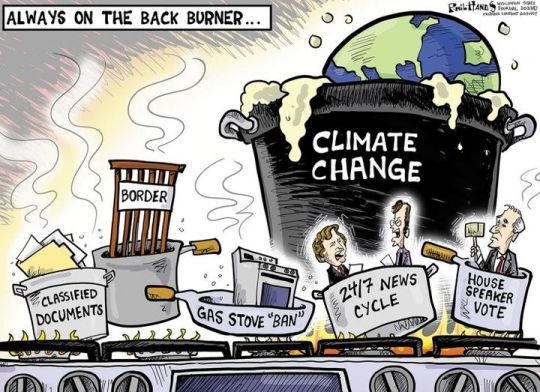
A Hotter Planet Takes Another Toll on Human Health
A new hypothesis about heat waves, redlining, and kidney stones.
By Bill McKibben
January 19, 2023
Shortly after the New Year, the Washington Post ran a story with a headline that would have seemed inexplicable, even runic, to most readers just a few years ago: “The world’s torrid future is etched in the crippled kidneys of Nepali workers.” But we’re growing used to the idea that the climate crisis, in Naomi Klein’s phrase, “changes everything,” so why not the internal organs of Nepalis? Remarkable reporting by Gerry Shih tells a series of unbearably poignant tales: young Nepali men, struggling to earn a living in their impoverished homeland, head to the Gulf states to do construction work in the searing heat, some without access to sufficient water, some until they collapse. (Other reporting also shows that some Nepalis who work abroad resort to the black market for a transplant that might keep them—and the families that depend on the money they earn—alive.) The piece ends with a man coming back to the care of his sister, who donates her own kidney to save him. The costs of the medical procedures require that he sell his half-built house, and that he give up his life’s dream, which was to get married.
The Post was right: the world’s future is likely encapsulated in this story. The planet is getting steadily hotter, and large swaths of it are moving past the point at which it’s safe to do heavy outside labor in the middle of the day. A 2022 study estimated that six hundred and seventy-seven billion working hours a year were already being lost because it’s too hot to go outside and build things or farm. The researchers assessed the cost at more than two trillion dollars annually, but, of course, it could also be measured in other units—in vital organs, or dreams.
But it’s not just the future that’s illuminated by such studies; it’s the past as well. Unless you’ve been keeping up with your issues of Current Opinion in Nephrology and Hypertension, you may have missed a recent article titled “Redlining has led to increasing rates of nephrolithiasis in minoritized populations: a hypothesis.” I saw it only because one of the medical experts who wrote it—David Goldfarb, who runs the dialysis unit at New York’s V.A. hospital and teaches at New York University’s School of Medicine—is an old family friend. He forwarded it to me, and it fairly blew my mind.
“Nephrolithiasis” is the technical term for the development of kidney stones, those small formations that, as they pass, can cause excruciating pain. (I’ve never had them, but I know more than one man who has said he came away from the experience with a newfound appreciation for what his wife had undergone during labor.) Doctors have long known that higher temperatures lead to more sweat, which reduces urine volumes and thus increases “the saturation of the insoluble salts that cause kidney stones.” During heat waves in the U.S., it takes just three days before emergency-room visits for kidney stones begin to spike.
For reasons that remain unclear, kidney stones have traditionally been more common among white people, but, in recent years, doctors have noted huge increases among Black Americans and a significant rise in Latino communities. The authors of the new article looked to the past for a possible explanation—particularly to the nineteen-thirties, when a federal agency, the Home Owners’ Loan Corporation, graded all of America’s neighborhoods and deemed some of them “hazardous” for investment, essentially because they were home to large minority communities. This grading system (from A for “best” and B for “still desirable” to C for “declining” and D for “hazardous”) underlay what came to be known as redlining. The grading system led to “chronic disinvestment” in the lower-rated neighborhoods, resulting, over time, in less of everything from parks and green spaces to street trees and air-conditioning in homes.
Now the results can be measured with a thermometer: in Portland, Oregon, the authors report, neighborhoods that were graded A in the nineteen-thirties now “average 8 degrees Fahrenheit lower than the city’s mean temperature, while D-graded neighborhoods average 4.8 Fahrenheit degrees warmer.” Actually, you don’t need a thermometer—that’s a thirteen-degree gap that anyone can feel just by walking across town. No one has carefully studied the incidence of kidney stones among these different neighborhoods, but the authors, in their hypothesis, point to research now under way. Similar work on asthma, another heat-related disease, has shown emergency-room visits are 2.4 times higher in redlined tracts.
Indeed, Goldfarb’s son Ben—an environmental journalist who this year will publish a book called “Crossings,” on the environmental impact of roads—writes that the HOLC grading program produced all kinds of deleterious health effects. In Syracuse, Miami, Minneapolis, and other cities, large parts of neighborhoods that the agency had redlined—and whose residents were mostly Black—were bulldozed to make room for interstate highways. He told me, “Minorities today disproportionately live near the urban freeways that displaced them, and suffer as a result. Air pollution causes asthma and cancer; noise pollution increases the risk of heart disease and stroke; and the physical fragmentation wrought by highways shatters local economies. It’s heartbreaking, though hardly surprising, that disastrous policy decisions made decades ago continue to destroy bodies and communities today.”
It’s true that everyone is going to pay some price as the planet cooks. The authors of the nephrology study predict a likely additional cost to the U.S. health-care system of at least a billion dollars a year. But some people are going to be hit much harder than others because of history. Doing justice in the present requires taking that past seriously—understanding how we ended up where we are, and why we must put those with the least first, as we try to address the future. But we’re at a moment in this country when the idea of historical responsibility is increasingly seen not as logical and obvious but as some kind of invidious political correctness.
In April, 2022, Governor Ron DeSantis, of Florida, signed the Stop Wrongs to Our Kids and Employees Act, or the Stop WOKE Act. (In introducing the bill, he had said, “In Florida we are taking a stand against the state-sanctioned racism that is critical race theory,” adding that “we won’t allow Florida tax dollars to be spent teaching kids to hate our country or to hate each other.”) A preliminary injunction was issued against the act, which includes a dictum against any school teaching that “a person, by virtue of his or her race, color, sex, or national origin, bears personal responsibility for and must feel guilt, anguish or other forms of psychological distress because of actions, in which the person played no part, committed in the past by other members of the same race, color, national origin, or sex.”
But, even if you can silence teachers, legislation can’t muffle the effects of history. On a hot summer’s day in Jacksonville, Florida, where DeSantis was born, the temperature in A neighborhoods is 5.5 degrees below the mean, and it’s 4.4 degrees above the mean in the D-rated communities.
#political cartoon#climate change#Bill McKibben#Nephrology#kidney stones#minority communities#articles#reckonings#redlining
14 notes
·
View notes
Text


Today's case is a 25-year-old woman with bilateral echogenic, shadowing renal medullas, compatible with medullary nephrocalcinosis. Radiograph also shows the bilateral calcium deposits. In this condition, calcium salts deposit in the renal medulla and predispose the patient to infection and obstructing renal stones. Differential diagnosis includes hypercalcemia (esp in hyperparathyroidism), hypervitaminosis D, renal tubular acidosis type I, papillary necrosis, medullary sponge kidney, and other rarer entities. This patient renal tubular acidosis.
Case courtesy of Vikas Shah, Radiopaedia.org, rID: 164910
3 notes
·
View notes
Text
Doctor: Do you have any questions about the exam?
Student: What was the answer of the nephritic syndrome question? We discussed among ourselves and none of the alternatives made any sense.
Doctor: Crap, it was supposed to be about nephrotic.
58 notes
·
View notes
Text
2023
Has brought on way more health problems than I wanted to know
1. My best friend was diagnosed with HER2 positive breast cancer. She had a double mastectomy and is now facing chemo next week. She’s only 29. She has had more complications with this than should be possible. More hospital stays and procedure that should never have been done.
2. My mom had some chest pain going on and spent the night in the hospital. That was insane
3. Me. I’ve had a hell of a ride. In February, I had a UTI. Treated it and about a week later, I got another infection which led to a visit to an urologist. Before that, I had a CT done, per request of my PCP due to the possibility of kidney stones based on my symptoms at the time. CT comes back, and I have kidney stones still in my kidneys 🫠 along with nephrocalcinosis (whatever that is). So after that, I went for a follow up appointment with the urologist who said that I’ll be referred to an nephrologist because of the stones being in my kidneys (one in each kidney) and the other thing.
I see the nephrologist who is super nice and clearly knows what he’s doing based on his bio on our hospital network’s website. He also understands the importance of mental health He had me do tests, one being a 24 hour pee test (a nightmare) and then follow up. I’m also more than likely the youngest patient 🫠
At the follow up, I’m thinking I’ll just be dismissed because there’s nothing wrong and I’m better. Like what more can you do for kidney stones in your kidneys? The other thing there’s nothing to be done.
Nope.
I’m told (which he’s right on) that I need to drink more water or fluids and proceeded to prescribe me Potassium Citrate which apparently helps avoid stones. When I asked him how long I’ll be on it, he basically stated to me “lifelong” 🫠🫠🫠
So much for being discharged and I get to go back again next year while doing that same damn 24 hour pee test.
So 2023 has taught me what a nephrologist is and that cancer sucks.
#cancer#fuck cancer#HER2 positive#breast cancer#mastectomy#nephrology#nephrologist#kidneys#kidney stone#nephrocalcinosis#health#physical health
3 notes
·
View notes
Text
Percutaneous Nephrolithotomy (PCNL)
Percutaneous nephrolithotomy (PCNL) is a surgical procedure to remove kidney stones that are too large to pass naturally or by other non-invasive treatments. In this procedure, a small incision is made in the back to create a tunnel through the skin and tissue to access the kidney. Then an endoscope is inserted through the incision to find and remove kidney stones.
PCNL is usually performed under general anesthesia and requires a short hospital stay of 1-3 days. This procedure has a high success rate and is considered safe and effective in treating large or complex kidney stones. This procedure is recommended for patients with kidney stones larger than 2 cm or located in areas of the kidney that are difficult to access with other non-invasive treatments. PCNL is also used in patients with other medical conditions that make other treatments less safe or effective.
Prior to the procedure, the patient may need to have imaging tests, such as a CT scan or ultrasound, to locate kidney stones and determine the best method for their removal. Patients are also advised to stop taking blood thinners such as aspirin and warfarin before surgery to reduce the risk of bleeding.
During surgery, the patient lies on their back and a small incision is made in their back. A guidewire is then inserted into the kidney through the incision and tunneled with a series of dilators. A nephroscope, a thin tubular instrument with a camera and light source, is inserted through a tunnel to locate and remove kidney stones. After the stone is removed, a tube called a nephrostomy tube is inserted into the kidney to drain any remaining fluid and debris.
After the procedure, patients may experience pain or discomfort in the back or abdomen and may be given pain relievers to manage these symptoms. Patients are also advised to drink plenty of fluids to wash away any remaining stone debris. In some cases, patients may need to undergo additional procedures to completely remove all kidney stones.
Overall, PCNL is a safe and effective surgical procedure for treating large or complex kidney stones. Patients should discuss the risks and benefits of this procedure with their doctor to determine if this is the best treatment option for their individual needs.
For more information Visit: www.drmayurdalvi.com
#surgery#urology#PCNL#kidney stones#percutaneous nephrolithotomy#healthcare#medical procedures#minimally invasive surgery#surgical techniques#anesthesia#imaging#nephrology#patient care#recovery#post-operative care#stone removal#surgical instruments#surgical incision#back surgery#abdominal pain
4 notes
·
View notes
Text

Anurag Multi Speciality Hospital offers comprehensive and compassionate care to patients of all ages. Our expert staff is made up of experienced physicians, nurses, and health care professionals who are dedicated to providing the highest quality of care.
For more information:
Call us : +919951974147
#hospital#multispecialityhospitalsinhyderabad#neurology#neurosurgeon#infertility#pulmonology#pulmonologist#pain#painmanagementsolutions#painmanagement#enthospital#emergencymedicine#emergency#nephrology#urology#nephrologist#pediatrics#jant#criticalcare
3 notes
·
View notes