#**as a clinical mental health counseling major
Text

Now let’s hope Volume 10 is dead in the water.
- 🐌
#rwby critical#snail speaks#**as a clinical mental health counseling major#**sincerely. what the fuck was this season and it’s message on mental health
7 notes
·
View notes
Text
explaining to people on the internet the very basic principle of counseling (US-wise) that you can’t take gifts from clients, especially those with large monetary values because it is a gross violation of the patient-counselor relationship is SO tiring.
1 note
·
View note
Text
By: Bernard Lane
Published: Dec 5, 2023
On the up
A study of young people who on average spent almost five years identifying as transgender has found they experienced better wellbeing and less gender dysphoria after they detransitioned from medical treatment or desisted in their opposite-sex identity.
“Detransition and desistance [giving up a trans identity before any medical treatment] were associated with marked improvements in psychological functioning,” says a new article published by the journal Archives of Sexual Behavior and authored by public health researcher Dr Lisa Littman, psychotherapist Stella O’Malley, detransitioner Helena Kerschner and sexologist Professor J Michael Bailey.
“On several relevant measures—gender dysphoria, flourishing, and self-harm—participants indicated great improvement after they stopped identifying as transgender,” the paper says.

[ Chart: Flourishing, or general wellbeing, rated by detransitioners, with the vertical access showing the number of participants for a given flourishing score, 10 being the highest wellbeing ]
Settling back into birth sex
Among the study group of 71 American females and seven males, aged 18-33, the overwhelming majority said they felt most “authentic” after they detransitioned or desisted.
External pressures—such as anti-trans discrimination, family resistance or religion—were rated as the least important drivers of detransition and desistance.
“The factors most important to relinquishing a transgender identification were internal factors, such as participants’ own thought processes, changes in participants’ personal definitions of male and female, and becoming more comfortable identifying as their natal sex,” the paper says.
Another reported impetus was the feeling that the causes of their gender dysphoria were more complex than they had believed. Looking back, the young people said a key influence in becoming trans was mistaking mental health problems or trauma as gender dysphoria.
“Against official advice I met [in 2021] a young lady called Keira Bell. She was a lesbian who told me the horrific experience that she had at the Tavistock [gender] clinic. It was an eye-opening experience [for me]. I know that [another MP] talked about ‘transing away the gay’ in his speech… We are seeing, I would say, almost an epidemic of young gay children being told that they are trans and being put on the medical pathway for irreversible decisions and they are regretting it… I am making sure that [in future] young people do not find themselves sterilised because they are being exploited by people who do not understand what these issues are…”—speech in the UK parliament, Equalities Minister Kemi Badenoch, 7 December 2023
Suddenly syndrome
Analysis of survey responses suggested that at most, 17 per cent of the group would have met the diagnostic requirements for the classic form of gender dysphoria with onset in early childhood.
Just over half the group (41/78) said they recognised themselves in the new, much more common form known as rapid-onset gender dysphoria (ROGD) with its onset during or after puberty.
Although a hypothesis rather than a formal diagnosis, ROGD seems to describe the post-2010 international explosion in socially influenced clusters of teenagers, chiefly girls, suddenly embracing trans or non-binary identities.
The study by Littman et al found that young people in the group who reported less gender dysphoria in childhood were more likely to say that the term ROGD did apply to their experience.
“The purpose of this research is to learn about the experiences of desisters and detransitioners—specifically, to explore: 1) factors that may or may not be related to the development of and desistance from transgender identification; 2) whether or not individuals experienced changes in their sexual orientation during and after transgender identification; and 3) what kinds of counseling and informed consent were received by those who sought medical care to transition.”—flyer used to recruit participants for the Littman et al study
Inconvenient for gender experts
The authors say their findings are “necessarily tentative” and acknowledge several limitations in the research, which involved a convenience sample of young people being asked to recall their experience before, during and after gender transition.
The study cannot show how common detransition is, nor establish whether these particular young people happened to be bad risks for transition, nor elucidate whether better psychological health is a cause or an outcome of detransition.
Detransition and desistance are understudied and contentious topics. ROGD has awkward implications for the “gender-affirming” treatment approach with its dogma of young people as “experts in their gender identity”.
Activists highlight the paucity of research on ROGD—first described in 2018 by Dr Littman—while seeking to sabotage any more studies and pressuring journals to retract papers exploring this phenomenon.
The Littman et al study just published had to adopt videoconference screening to check that would-be participants were genuine; activists had boasted on social media about taking the online survey and giving fake responses.
“When little is known [about detransition and desistance], imperfect research is often better than no research,” Dr Littman and her colleagues say in their paper. “It can provide provisional answers, better-informed hypotheses, and ideas for future research.”
“Despite the absence of any questions about this topic in the survey, nearly a quarter (23 per cent) of the participants expressed the ‘internalized homophobia and difficulty accepting oneself as lesbian, gay, or bisexual’ narrative by spontaneously describing that these experiences were instrumental to their gender dysphoria, their desire to transition, and their detransition.”—A survey of 100 detransitioners, Dr Lisa Littman, September 2021. (Dr Littman believes there would be little if any overlap in participants between this 2021 group and those surveyed in the current 2023 study.)
youtube
[ Video: Corinna Cohn, who transitioned three decades ago when safeguards were stronger, testifies in support of a bill restricting paediatric transition in the American state of Ohio ]
Yes, they were trans
In the 2023 Littman et al study, all the males and most of the females had taken cross-sex hormones, almost a third of the females had undergone mastectomy and a small number had their uterus or ovaries removed. (Only two participants had taken puberty blockers, which Dr Littman attributes to the average age of trans identification being too old at 17 years.)
“Our participants invested a great deal of their lives in their gender transitions—in terms of time, disruption, and serious social and medical steps. Thus, we do not believe that a principled case can be made that participants detransitioned because they were never gender dysphoric,” the Littman et al paper says.
The researchers say that follow-up studies of gender dysphoric youth are “urgently needed”, and that gender clinics have “a particular obligation” to keep track of past patients—“Unfortunately, in North America at least, we see little evidence that this presently occurs.”
“Detransition has become much more visible in recent years. However, it was only recently that the rates of detransition began to be quantified. According to recent UK and US data, 10–30 per cent of recently transitioned individuals detransition a few years after they initiated transition.”—Current concerns about gender-affirming therapy in adolescents, Professor Stephen B Levine and E Abbruzzese, April 2023
Some other key points of the 2023 Littman et al paper—
Only 27 per cent of the young people had told their former gender clinicians they had detransitioned.
Most of those who took cross-sex hormones obtained them through the fast-track “informed consent” model.
Two-thirds of the group felt they had not been adequately informed about the risks of medical transition.
Fewer than one in ten had been told about the lack of long-term outcome studies for females with adolescent-onset dysphoria.
Important influences for females becoming trans men included wanting to avoid mistreatment and sexualisation as women.
Almost half the females indicated they were exclusively attracted to women.
ROGD may be chiefly a female condition, with the possibility that some males taken to be ROGD may actually be manifesting hitherto-suppressed autogynephilia (sexual arousal among males who cross-dress and/or imagine themselves as women).
More than a third of the group said most of their offline and online friends became trans-identified and it was common to mock people who were not trans.
Among counter-intuitive results, acknowledgment of the ROGD label by participants was not significantly related to the age at which they took on a trans identity.
Psychiatric diagnoses before transition were common, including depression (63 per cent); anxiety (60 per cent); attention deficit/hyperactivity disorder (24 per cent); eating disorder (23 per cent); obsessive compulsive disorder (18 per cent) post-traumatic stress disorder (15 per cent); bipolar disorder (12 per cent); hair pulling (10 per cent); and autism spectrum disorder (9 per cent).
Young people in the study showed relatively high scores on a trauma measure of “adverse childhood experiences” such as abuse inflicted within the family.
The participants had generally liberal politics and a clear majority supported gay marriage (67/78) and trans rights 71/78).
==
Coming to terms with the nature of your body, rather than chasing a fantasy and delusion, leads to better mental health. Imagine that.
#Bernard Lane#detrans#detransitioners#gender ideology#queer theory#ROGD#rapid onset gender dysphoria#medical transition#medical malpractice#medical corruption#medical scandal#mental health#religion is a mental illness#Youtube
43 notes
·
View notes
Note
Do you have any advice for an autistic & trans therapist to safely establish a job in the mental health field amongst NT cishet coworkers? I’ve experienced discrimination every step of the way in this field and the only way for me to have job security is to finish up my licensure hours somewhere so I can be on my own when licensed.
To be blunt, being Autistic & trans and a therapist will never come with any guarantee of safety, because the entire field of institutionalized mental health is built upon a bedrock of ableism and (often violent) rejection of gender and sexual non-conformity. It's not just the NT and cishet coworkers as individual people that are the problem, it is the entire foundation of the field and what it sets out to do.
Look at what happened to Marsha Linehan -- she was one of the foremost, most accomplished researchers and treatment developers in her subfield and saved thousands of lives, yet she still had her competence challenged and lost a ton of professional respect the moment she came out about being BPD. That is not just the work of biased or bigoted NT individuals, that is the natural consequence of a line of work that by definition categorizes some classes of people as less competent and worthy than others.
I have taught and done consulting work for many organizations and I have never yet seen a mental health facility of any kind where persons with mental illness or neurodivergence are not discriminated against, nor have I ever been particularly impressed with the therapeutic practices or clinical psychology programs that profess to be queer affirming.
Even orgs run and led by trans or Autistic people are still forced to operate by the rules and standards of institutionalized psychology and psychiatry, and so they are invested in promoting respectability politics, stigma, and the theft of disabled people's autonomy to some extent. Obviously some are far more egregious than others. But they are all institutions with unjust power they can leverage over the marginalized, and they're invested as institutions into holding onto that power.
Counseling psychology programs and their graduates tend to be a bit more open minded and less prone to pathologization than clinical psychs, as are the licensed social workers who do not come from conservative Christian background or educational tradition (unfortunately, many social workers do have that kind of background). I wish I could recommend some queer-owned practices but all the ones I'm familiar with are run by rainbow capitalist grifters with no true conception of intracommunity dynamics such as transmisogyny.
When I taught for the Chicago School of Professional Psych, I heard from many of my students about their many licensure hour placements, and none of them sounded like good or safe places to be -- and many of those facilities were far worse to their Black and brown patients than they were for their (majority white) therapists-in-training. But on the whole everyone relatively lacking in power in those spaces was either exploited or judged as inferior or both.
I imagine that working on your own/for yourself would be the best route ultimately-- the few ND therapists I know who are doing a more liberatory practice are quietly doing so on their own. I think that's a sensible long-term goal for you to have. But on the way to getting there, you will be working in spaces that are not safe to you. I would never trust any institution or therapuetic practice to keep you safe, no matter how they brand themselves or how progressive they profess to be.
I think the real question, then, is what supports will you have in place to make getting your licensure hours possible for you? When a colleague microaggresses against you or is discriminatory toward a patient, what will your emotional recovery plan look like? What are the absolute dealbreakers that will make a facility or organization unworkable for you, and what are the nice-to-haves that you can live without?
Basically, if you want to get your necessary hours, you might have to be in survival mode for a while -- and I think having realistic expectations about that and a plan for dealing with the secondary trauma and systemic biases you'll endure is what will make it possible. That said, I'm not a therapist, I've only seen this stuff from the sidelines as a teacher, trainer, program evaluator, and sometimes as a patient. So I would also encourage you to try and find a neurodivergent and queer therapist who has gone through this stuff before, who can serve as a mentor for you. Getting through this process will be tough, and I think it’s important to be realistic about that. You’ll need to steel yourself for a lot of unfairness and ignorance, and you’ll need a good support system in place to help keep you feeling strong in the face of it.
116 notes
·
View notes
Note
Hii!
I'm an undergrad psych student that dreams to be where you are in the future (studying clinical psych)!
I'm striving to be a psychologist but I've heard how competitive it is. As someone who is in postgrad, I was wondering if you'd be okay giving some advice, what scores you had to get in ungrads and honours, what volunteering you maybe did and how postgrad life is!!
♡
Hey! It’s so awesome that you want to go into clinical psych!
I went to a pretty competitive university for undergrad and majored in Psychology with a minor in Disability studies. I ended up with a 3.8 major and overall GPA and graduated Magna Cum Laude. I worked as a FWS student on a clinical trial that focused on helping people with intellectual disabilities access mental health care as well as some odd jobs here and there. I also volunteered at my state department of mental health during the summers while I was home from school and with the National Counsel for Mental Wellbeing as a state captain for Hill Day.
I applied to a small college in my hometown for Postgrad because I wanted the small college feel and it is a really reputable program whose grads see a lot of success. I got in and I absolutely love it. The program has wonderful professors and they are really focused on graduating strong therapists. I will be a masters level Licensed Professional Counselor when I graduate in May 2025.
My advice for you is to find a place to volunteer at that will get you some good hours and face time with the right people. You don’t have to always be doing psychology related things with them. When I volunteered for DMH, I helped with their mental health conference and with Santa’s helpers which purchased presents for kids of patients at the center. I wasn’t always doing psychology stuff but I made some really strong connections and they wrote me excellent letters of recommendation. I wish I had gotten more acquainted with my professors in undergrad but it was hard because I went to such a large school. Find the people who value you and your work and they will give back by writing you glowing recommendations which go a long way in the application process. The more you volunteer and get experience, the more you’ll have to write about in your admissions essay, which I think carried me through the process.
Post grad is hard but it’s focused on what you love and is training you for your dream career. It’s worth every minute. Get as much experience as you can, clinical or not, so you make those connections and get to know people who have influence in different areas. Keep doing what you’re doing! We need people like you in our field! Hope this helps!
#psychology#studyblr#studygram#studyinspo#masters student#productivity#study motivation#study with me#stay productive#study aesthetic#asks#gryffindorpsychologyandcoffee#masters degree#study psychology#adhd#post graduate#post grad life
4 notes
·
View notes
Text

Hi! My name is Lily Clough, I am a senior at bonnies and a psychology major. I am from Buffalo New York and a big fan of the Buffalo Bills. After graduation I am hoping to attend grad school for clinical mental health counseling. Some things I enjoy include hanging out with friends, painting, listening to music and spending time with my family and two dogs.
6 notes
·
View notes
Note
OMG WAIT CAMPUS so you're in college rn too! what's your major?
Yeah, I'm in grad school. My major/program is Clinical Mental Health Counseling (I just tell most people Psychology because that's too wordy lol).
10 notes
·
View notes
Text
Psychopathology, Ch 2 pt. 3
Identify the major types of helping professionals and describe their training backgrounds and professional roles.
Clinical psychologists: have earned a doctoral degree in psychology, either a PhD (Doctorate of Philosophy), a PsyD (Doctorate of Psychology), or an EdD (Doctorate of Education) from an accredited college or university. Training in clinical psychology typically involves four years of graduate coursework, followed by a year-long internship and completion of a doctoral dissertation. Clinical psychologists specialize in administering psychological tests, diagnosing psychological disorders, and practicing psychotherapy. Until recently, they were not permitted to prescribe psychiatric drugs. However, as of this writing, five states (Idaho, Illinois, Iowa, Louisiana, and New Mexico) have enacted laws granting prescription privileges to psychologists who complete specialized training programs. The granting of prescription privileges to psychologists remains a hotly contested issue between psychologists and psychiatrists and within the field of psychology itself.
Counseling psychologists: also hold doctoral degrees in psychology and have completed graduate training preparing them for careers in college counseling centers and mental health facilities. They typically provide counseling to people with psychological problems falling in a milder range of severity than those treated by clinical psychologists, such as difficulties adjusting to college or uncertainties regarding career choices.
Psychoanalysts: typically are either psychiatrists or psychologists who have completed extensive additional training in psychoanalysis. They are required to undergo psychoanalysis themselves as part of their training.
Psychiatrists: have earned a medical degree (MD) and completed a residency program in psychiatry. Psychiatrists are physicians who specialize in the diagnosis and treatment of psychological disorders. As licensed physicians, they can prescribe psychiatric drugs and may employ other medical interventions, such as electroconvulsive therapy (ECT). Many also practice psychotherapy based on training they receive during their residency programs or in specialized training institutes.
Psychiatric nurses: typically are registered nurses (RNs) who have completed a master’s program in psychiatric nursing. They may work in psychiatric facilities or in group medical practices where they treat people suffering from severe psychological disorders.
Clinical or psychiatric social workers: have earned a master’s degree in social work (MSW) and use their knowledge of community agencies and organizations to help people with severe mental disorders receive the services they need. For example, they may help people with schizophrenia make a more successful adjustment to the community once they leave the hospital. Many clinical social workers practice psychotherapy or specific forms of therapy, such as marital or family therapy.
Counselors: have earned a master’s degree by completing a graduate program in a counseling field, such as mental health counseling or rehabilitation counseling. Counselors work in many settings, including private practices, schools, college testing and counseling centers, and hospitals and health clinics. Many specialize in vocational evaluation, marital or family therapy, rehabilitation counseling, or substance abuse counseling. Counselors may focus on providing psychological assistance to people with milder forms of disturbed behavior or those struggling with a chronic or debilitating illness or recovering from a traumatic experience. Some are clergy members who are trained in pastoral counseling programs to help parishioners cope with personal problems.
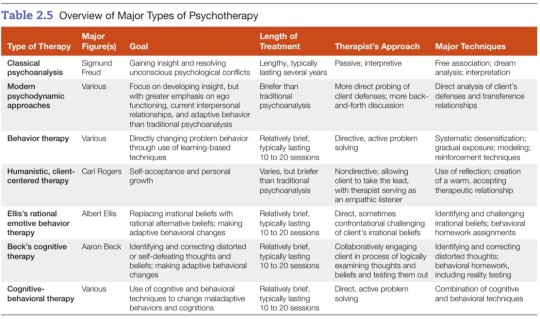
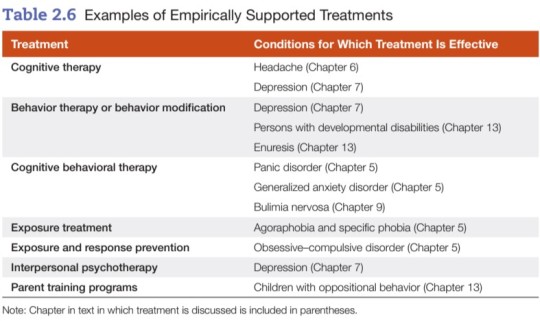
Describe the goals and techniques of the following forms of psychotherapy: psychodynamic therapy, behavior therapy, person-centered therapy, cognitive therapy, cognitive-behavioral therapy, eclectic therapy, group therapy, family therapy, and couples therapy.
Psychotherapy: a structured form of treatment derived from a psychological framework that consists of one or more verbal interactions or treatment sessions between a client and a therapist.
- used to treat psychological disorders, help clients change maladaptive behaviors or solve life’s problems, or to help them develop their unique potentials.
Psychoanalysis: the method of psychotherapy developed by Sigmund Freud.
Psychodynamic therapy: therapy that helps individuals gain insight into and resolve deep-seated conflicts in the unconscious mind.
Free association: the method of verbalizing thoughts as they occur without a conscious attempt to edit or censor them.
Transference relationship: in psychoanalysis, the client’s transfer or generalization to the analyst of feelings and attitudes the client holds toward important figures in their life.
Countertransference: in psychoanalysis, the transfer of the analyst’s feelings or attitudes toward other persons in their life onto the client.
Behavior therapy: the therapeutic application of learning-based techniques to resolve psychological disorders.
Systematic desensitization: a behavior therapy technique for overcoming phobias by means of exposure to progressively more fearful stimuli (in imagination or by viewing slides) while remaining deeply relaxed.
Gradual exposure: in behavior therapy, a method of overcoming fears through a stepwise process of exposure to increasingly fearful stimuli in imagination or in real-life situations.
Token economy: a behavioral treatment program that creates a controlled environment in which desirable behaviors are reinforced by dispensing tokens that may be exchanged for desired rewards.
Person-centered therapy: the establishment of a warm, accepting therapeutic relationship that frees clients to engage in self-exploration and achieve self-acceptance.
Empathy: the ability to understand someone’s experiences and feelings from that person’s point of view.
Genuineness: the ability to recognize and express one’s true feelings.
Congruence: the coherence or fit among one’s thoughts, behaviors, and feelings.
Cognitive therapy: a form of therapy that helps clients identify and correct faulty cognitions (thoughts, beliefs, and attitudes) believed to underlie their emotional problems and maladaptive behavior.
Rational emotive behavior therapy (REBT): a therapeutic approach that focuses on helping clients replace irrational, maladaptive beliefs with alternative, more adaptive beliefs.
Cognitive behavioral therapy (CBT): a form of psychotherapy incorporating cognitive and behavioral techniques.
Eclectic therapy: an approach to psychotherapy that incorporates principles or techniques from various systems or theories.

Group therapy: a form of therapy in which a group of clients with similar problems meets together with a therapist.
Family therapy: a form of therapy in which the family, not the individual, is the unit of treatment.
Couples therapy: a form of therapy that focuses on resolving conflicts in distressed couples.
Evaluate the effectiveness of psychotherapy and the role of non-specific factors in therapy.
Nonspecific treatment factors: factors not specific to any one form of psychotherapy, including
empathy, support, and attention shown by the therapist
the therapeutic alliance = attachment the client develops toward the therapist and the therapy process
the working alliance = effective working relationship in which the therapist and client work together identifying and confronting the important problems and concerns the client faces
Telehealth: delivery or facilitation of treatment services via telecommunication or digital technology.
Evaluate the role of multicultural factors in psychotherapy and barriers to use of mental health services by ethnic minorities.
- Cultural sensitivity involves more than good intentions. Therapists must have accurate knowledge of cultural factors and the ability to apply that knowledge when developing culturally sensitive approaches to treatment.
- Just because a given therapy works with one population group does not mean that it will necessarily work with other groups. Therapists using established treatments should consider how they can incorporate culturally specific elements to boost treatment benefits in working with people from different ethnic or racial groups.
- Some of the barriers to mental health services for marginalized communities include...
Cultural mistrust: People from minority groups often fail to use mental health services because they don’t trust mental health institutions/professionals. Mistrust may stem from a cultural and/or personal history of oppression and discrimination, or experiences in which service providers were unresponsive to their needs. When minority clients perceive white therapists and white-dominated institutions to be cold or impersonal, they are less likely to place their trust in them.
Mental health literacy: A person may not make use of mental health services because they lack knowledge of mental disorders and how to treat them.
Institutional barriers: Facilities may be inaccessible to marginalized people because they are located at a considerable distance from their homes or because public transportation is lacking. Marginalized people are often overwhelmed or intimidated by bureaucratic red tape and/or protocol around health procedures.
Cultural barriers: Many recent immigrants have had little or no previous contact with mental health professionals. They may hold different conceptions of mental health problems or view mental health problems as less severe than physical problems. In some cultures, the family is expected to take care of members who have psychological problems and may resist outside assistance. Other cultural barriers include cultural differences between socio-economically disadvantaged clients and majority white + middle-class mental health staff, and the stigma often associated with seeking mental health treatment.
Language barriers: Mental health facilities may lack the resources to hire mental health professionals who are fluent in the languages of the communities they serve.
Economic and accessibility barriers: Financial burdens are often a major barrier to use of mental health services. Living in a rural or isolated area where mental health services may be lacking or inaccessible is also a big hurdle.
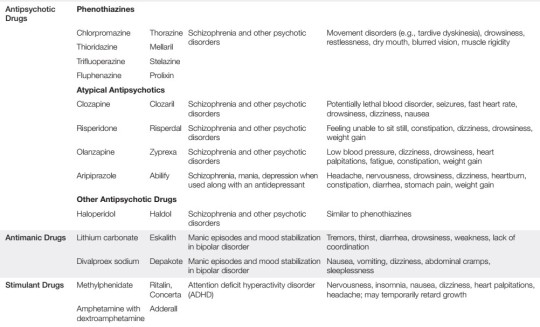
Psychopharmacology: the field of study that examines the effects of therapeutic or psychiatric drugs.
Identify the major categories of psychotropic or psychiatric drugs and examples of drugs in each type and evaluate their strengths and weaknesses.
Anti-anxiety drugs: drugs that combat anxiety and reduce states of muscle tension.
~ also called anxiolytics
~ examples include benzodiazepines (Valium, Xanax) as well as hypnotic sedatives (Halcion)
+ can be safe and effective in treating anxiety and insomnia
- potential for psychological and/or physical dependence, so they tend to be better for short term or occasional relief, not long term or daily use
Rebound anxiety: the experiencing of strong anxiety following withdrawal from a tranquilizer.
Antipsychotic drugs: drugs used to treat schizophrenia or other psychotic disorders.
~ also called neuroleptics
~ examples include Thorazine, Mellaril, Prolixin, Clozapil (atypical)
+ drastically reduced the need for long-term hospitalization, physical restraints, and confinement
- unpleasant side effects, such as muscular rigidity and tremors; long-term use of antipsychotic drugs (with exception of Clozapine) can produce tardive dyskinesia, a potentially irreversible and disabling motor disorder
Antidepressants: drugs used to treat depression that affect the availability of neurotransmitters in the brain.
~ four major classes: tricyclic antidepressants (TCAs), monoamine oxidase inhibitors (MAOIs), selective serotonin-reuptake inhibitors (SSRIs), and serotonin-norephinephrine reuptake inhibitors (SNRIs)
~ examples include Tofranil, Elavil, Sinequan (tricyclics), Nardil (MAOI), Prozac, Zoloft (SSRI), Effexor (SNRI)
+ antidepressants provide beneficial effects for a wide variety of psychological disorders
- however, there are side effects for each category, and in the case of MAOIs, a patient’s diet is heavily restricted

Electroconvulsive therapy (ECT): a method of treating severe depression by administering electrical shocks to the brain.
+ significant improvement for patients experiencing severe epileptic seizures or major clinical depression that has not responded to other treatment
- high relapse rates and memory loss for events occurring around the time of treatment; for these reasons, ECT is a last resort
Describe the use of psychosurgery and evaluate its effectiveness.
~ Previously, the prefrontal lobotomy was the most common form of psychosurgery. This procedure involved surgically severing nerve pathways linking the thalamus to the prefrontal lobes of the brain.
~ The premise of this operation was the belief that severing the connections between the thalamus and the frontal lobe of the cerebral cortex would control a patient’s violent or aggressive tendencies.
- This procedure was abandoned because (1) there was insufficient evidence of its effectiveness and (2) it often produced serious complications or even death.
- When anti-psychotic drugs became available during the 1950s, psychosurgery was all but eliminated.
+ In recent years, more sophisticated psychosurgery techniques have been introduced which target much smaller parts of the brain and produce far less damage than the prefrontal lobotomy. These techniques have been used to treat patients with severe OCD, bipolar, and/or major clinical depression who have failed to respond to other treatments.
~ Another experimental technique is deep brain stimulation (DBS), a surgical procedure in which electrodes are implanted in the brain and used to electrically stimulate deeper brain structures.
+ DBS shows promise in treating severe forms of depression and OCD that have failed to respond to more conservative treatments.
- However, DBS may have serious complications and its effectiveness needs to be investigated further. Thus, it is still an experimental treatment.
Evaluate biomedical treatment approaches.
~ Overall, a combination of medication and talk therapy seems to be more helpful for most mental health patients than either treatment alone.
~ The benefits and risks/side effects of each medication need to be carefully considered and discussed by the provider and the patient.
10 notes
·
View notes
Text
Medical Professional Disciplines
Unlike other medical disciplines, family medicine focuses on providing health care for people rather than addressing particular medical disorders. Furthermore, family doctors are educated to deal with patients of all ages, from babies to the elderly.
After working in medicine for a decade, I'm constantly interested to hear about discoveries. I like teaching and treating individuals with the most current and effective treatments available. I also enjoy assisting individuals in living better, happier lives.
Family medicine offers a wide range of services, from preventative care to acute sickness treatment, to assist patients in making healthy lifestyle choices. These services include counseling, screening tests, health risk assessments, mental health treatment, and referrals to experts. Family physicians are also educated to handle common ailments such as fractured bones, skin biopsies, and joint injections.
There are several advantages to working in family medicine, including a high job satisfaction percentage, a pleasant work-life balance, and the chance to assist everyone. However, certain misunderstandings about the profession might cause fear.
Hospital medicine, which began as a medical specialty in the United States, has extended abroad. Hospital medicine is a subspecialty of family or internal medicine in many countries. Its primary services include medical treatment, perioperative care, and research. It may also help to enhance hospital efficiency, patient care, and certain hospital outcomes.
While hospital medicine has risen in popularity over the previous two decades, it has only just started to make inroads into the general public. Its most notable contributions have been to improve hospital efficiency, address hospital safety, and promote cost-effective therapies. It also offers a very global value proposition.
Hospital medicine is a clinical specialty that integrates acute care medical skills with hospital service delivery systems. Its major duty is to offer effective treatment in hospitals, outpatient clinics, and emergency departments.
OB/GYN is a medical specialty concerned with the health of the female reproductive system. These professionals undertake a variety of medical treatments to address women's health concerns. These physicians also assist with infant care.
OB/GYNs are also qualified to assist ladies who are experiencing infertility. They also specialize in treating reproductive system diseases such as ovarian and breast cancer. Advanced surgical methods, such as laparoscopic surgery, are part of their training.
OB/GYNs may treat various women's health conditions as doctors, including breast diseases, urinary tract illnesses, menopause, and vaginal dryness. They also provide preventative procedures, including mammography, STD testing, and pelvic examinations.
Depending on the patient's requirements, OB/GYNs work in hospitals, private clinics, or solo practices. A typical OB/workweek GYN consists of half of the day spent in the office and half of the day spent in labor and delivery.
Podiatric medicine is a branch of medicine that focuses on the diagnosis and treatment of foot and ankle problems. Its practitioners are healthcare specialists who give patients personalized consultations and treatment regimens. They often diagnose foot and ankle disorders and provide preventative treatments such as physical therapy, wellness counseling, and surgery.
Podiatric medicine is one of the country's fastest-growing professions. A healthcare practitioner must commit to improving patient safety and quality. It also provides flexible working hours and is one of the higher-paying medical professions. Practitioners in this field work in hospitals, community clinics, and private offices.
A podiatrist must have a full awareness of the roles of each healthcare provider in treating patients. They must identify and suggest solutions to quality care challenges. A podiatrist must also have an impartial opinion regarding the efficacy of therapy or technique.
The use of lasers in medicine is a developing area. They are effective in a variety of medical applications. Some of the most prevalent includes wound care, tumor treatment, and coagulation. They are also employed in surgery for cutting and directing projectiles.
Several variables influence the effectiveness of laser therapy. The kind of laser utilized, the quantity of energy provided, and the rate at which it is delivered are all examples. The wavelength of the light employed has an influence as well.
Lasers may be used to diagnose illness early on. Infections may also be treated using them. Some lasers are more powerful than others and may specifically target tissues.
In addition, lasers are employed in surgery. Using them may lead to decreased discomfort, scarring, and edema. They also recover faster than typical operations. They may, however, cause adverse effects. These must be handled correctly.
8 notes
·
View notes
Text
Story of M: Where I am now and how I got here, Part 3
CONTENT WARNING: Mentions of SH
Before I continue I got to say some things. When I first got in trouble at my job I was referred to a mental health clinic and was assessed for various conditions that could explain my problems (my employer did not suspect drugs for some reason). I was diagnosed with borderline personality disorder and was assigned a dedicated mental health nurse, K, who was an absolute angel. After my wake up call I confided to K about my drug use, and she literally walked with me to get specialized counseling. I'm not exaggerating when I say I owe her my life.
I had also started drawing again a couple of months prior and got positive feedback from my friends. Drawing became a major outlet during these difficult times.
On with the story…
The first month, which was october, was the worst. I had strong cravings, got 2-3 hours of sleep at night and was painfully aware of the fact that this was all my own doing. I was a nervous wreck. I went to work as usual (I was too ashamed to go on sick leave, felt like I didn't deserve it), but as soon as I got home and was alone with my thoughts… I don't have words for the absolute horror, guilt and shame I felt. I closed the blindfolds, turned off all the lights save for a small table lamp, played The Binding of Isaac for hours and even went to the bathroom in the dark because I couldn't bear to see myself in the mirror. Autumn was turning into winter so it got dark early, which I found oddly comforting as I was hiding in my small apartment. I dreaded going to sleep, knowing I would toss and turn for hours, only to wake up in the morning to live the same hell for another day. Sometimes I harmed myself. After telling K about my struggles she arranged an appointment with a psychiatrist, who got my meds in order. I refused any medications with potential for misuse and the doctor respected my wishes. After that I could sleep again.
The cravings persisted for a long time. After the first month I took a risky chance and did something I'm not yet comfortable sharing because it's a controversial topic and I don't want to give anyone ideas. After that the cravings were completely gone. I was still a nervous wreck, but at least I didn't feel the constant urge to snort chemicals.
Christmas came. I had gotten a little journal as a christmas gift for myself and began journaling my thoughts. I also met S for the first time. We exchanged numbers and began talking semi-regularly.
After New Year I was transferred back to my old department at my job, with a much better atmosphere. I was happy about it, although I was withdrawn and anxious because of my ongoing struggles. My daily life was pretty much the same with little to no signs of improvement. My journal, which was meant for light-hearted fun, is filled with despair and self-destructive thoughts. In spring I finally called things off with Shitty Boyfriend. From my perspective our relationship had died a long ago, but he thought differently and did not take this well at all. I practically lost my entire circle of friends because of him.
By summer I felt a little better, likely because I'm a summer person. I took walks in the nature, ate ice cream and and enjoyed other summer activities, by myself. I began saving money, but did not have a plan for them yet.
In autumn my employer gave news about a possible merger, which made me worry about my job security. That gave me an idea for the money I was saving: I would go back to school and get another degree. The next spring I applied to a school that happened to be in the same town S was living, and when school started we moved in together. We had a rocky start because of his drinking problem, but despite that I enjoyed my new life. School is so much fun when you're an adult.
After getting some distance to my old job I realized it was just too stressful for me. Even though it paid relatively well, in the end it was simply not worth my mental well-being. It felt sad leaving my amazing colleagues behind, but it was something I needed to do. So I got another degree and and soon found a new job.
This is where I am now.
1 note
·
View note
Text
Having been in an abusive marriage and having raised kids for the last 16 years with my abuser, it is hell. Absolute hell.
My kids both have mental health issues, both acute breakdowns and chronic, due to this man’s actions. Same for me with the chronic anxiety and formerly CPTSD. We are all stable but it has been a hard won battle.
The idea that abuse survivors may be forced to carry pregnancies is terrifying. Abuse survivors — whether still in that relationship or just having escaped — do not have resources to travel state lines or 300 miles to the only clinic in the state.
And abusers are about control. My ex took no interest in my kids—he wanted to give them up for adoption even as toddlers— until I left. And since I have left they have been commodities to him, both as a mean to control me and to exert control over them. Do you know what it’s like for your 13 year old to have a complete, life imploding breakdown? Or for your youngest to be diagnosed with conversion disorder and so sick he has to be pulled from school? It’s been 13 years and he still does this.
Counseling resources are so overstretched that it’s ridiculous. These state bans often go hand in hand with social service restrictions for these mothers. And a majority of social service organizations are faith based so contraception and abortion will be non options.
So, pregnant, forced to carry said baby and give birth. If I did do all I’d that, at risk to myself physically and mentally, and to close the chapter and give that kid a better start I give them up for adoption. What if someone who contradicts my values adopts them? What is there are laws that require my ex know? Ex could refuse to terminate parental rights! I would then raise that kid whether I had the resources to do so, just to protect them. Courts don’t protect these survivors or their children.
I love my kids to the end of the earth and always wanted them and was always in a position to support them even when it was impossible, but it has been hell raising them with this man. Those of you who have followed me for years know some of this history — counselor visits, extreme mental illness, er visits, dcfs in and out of our lives to no avail. It is misery that I wouldn’t wish on anyone.
This makes me incredibly anxious for abuse survivors everywhere.
33 notes
·
View notes
Text
By: Christina Buttons
Published: Apr 7, 2023
Why do progressives and gender activists fervently believe that “transgender” women are literally women? Why do they believe in the existence of “transgender children” that must be medically transitioned to avoid going through the “wrong puberty”? Why is “gender identity” taking precedence over biological sex in legislation like Title IX? How can they confidently assert that “the science” is on their side?
The answer to all of these questions is due to the belief that being transgender is an innate biological property of human beings. The notion that “gender identity” is brain-based and innate has captured the political left. This is due to a collection of brain studies that purport to show that people who identify as transgender have brain structures that are more similar to the sex with which they “identify” than to their actual sex. Widespread media coverage of these studies lauds them as “proof” that transgender people “are who they say they are.”
Progressive media outlets have glommed onto this narrative and published dozens of articles asserting that “transgender people are born that way” and that “science proves trans people aren’t making it up.” Mainstream media like CNN, the New York Times, Newsweek, the Telegraph and scientific sources like Nature, National Geographic, the Cleveland Clinic and Scientific American have also repeated this misinformation.
To make matters worse, the “brain sex” conjecture is baked into clinical guidelines for medical transition and legislation for employment, healthcare, and education.
The transgender “brain sex” argument is a load-bearing pillar supporting the belief that people are born transgender and should therefore medically transition as early as possible. Several female detransitioners who were medically transitioned as minors have even discussed how their doctors wrongly informed them that they possessed "a male brain in a female body." This claim is so absurd you’d wonder how the average person, let alone a medical doctor, would believe it.
One major player responsible for perpetuating this myth is Dr. Joshua Safer, an endocrinologist and the executive director of the Mount Sinai Center for Transgender Medicine and Surgery in New York City. Safer is a leading advocate of "gender affirming care" and believes that "gender identity" is biologically determined. A review article he published on the topic relies heavily on brain studies and disorders of sexual development (which are often used to argue that the sex binary should be represented as a spectrum).
A 2016 interview with WBUR gives insights into how the “brain sex” theory shifted Safer’s perspective of the transgender experience from a mental health issue to a medical one.
"Up until a decade or so ago, the view among many providers was that this was probably a mental disorder and the fear was that doing hormone therapy or doing surgery might be abetting a mental disorder and the correct intervention would be to counsel people," Safer said.
But Safer's research traces the increasing evidence that gender identity is rooted in biology, "which makes it so logical that an option for people in 2016 is to change the external appearance to meet that gender identity," he said.
Why does it matter? Because Dr. Safer is currently the co-chair of the World Professional Association for Transgender Health (WPATH) and has been involved with the organization for many years, including serving as the first president of USPATH, the United States affiliate of WPATH. Most importantly, he co-authored two sets of clinical guidelines for the medical care of transgender patients: the WPATH's Standards of Care and the Endocrine Society guidelines. These guidelines are considered the gold standard in gender medicine and are used by gender clinics worldwide.
Dr. Safer has testified in numerous legal cases related to "transgender rights," providing expert testimony on the purportedly scientific aspects of “gender identity,” particularly as it relates to "brain sex." He appeared on a panel with comedian Jon Stewart last year and has discussed the concept of "brain sex" in various media outlets, including the New York Times and a PBS documentary.
The assumption that being transgender is an innate property that can be detected by brain scans is central to all of the problems we see today surrounding transgender issues. It is therefore crucial to be aware of and challenge the transgender “brain sex” argument whenever it arises.
The “brain sex” argument
The “brain sex” argument claims that transgender people have regions in the brain that structurally resemble that of the opposite sex. This assertion is based on a number of studies conducted in recent years on people who identify as transgender to gain insight into the potential biological basis of their condition. Some studies have even purported to show that the brain structure of transgender individuals more closely resembles the sex they “identify” as than their natal sex.
The "brain sex" argument is based on the idea that there are differences in brain structure and function between males and females that are influenced by hormones and genetic factors. Advocates of this argument argue that these differences can also be seen in the brains of transgender individuals and that these differences may contribute to the development of a “gender identity” that is different from their natal sex. They believe that a biological male who identifies as a woman has brain structures that more closely resemble that of typical females, and vice versa.
Here’s why it's wrong
The majority of the studies on the “transgender brain” have a fatal flaw: they didn’t control for confounding variables like cross-sex hormone use and, most importantly, sexual orientation. When a study doesn't control for confounding variables, it means that the researchers did not take into account other factors that could have affected the results of the study, which make it difficult or impossible to determine whether the relationship between the two variables being studied is truly causal or a byproduct of other unrelated factors.
Cross-sex hormone use can have effects on the brain, including changes in brain structure and function. But more importantly, many trans-identifying individuals are same-sex attracted, so the research on the “transgender brain” claiming to find structural regions that resemble the opposite sex are essentially rediscovering findings on the “gay brain” and reinterpreting the results to fit their preferred conclusion.
In the early nineties, neuroscientist and author Simon LeVay made the breakthrough discovery that the brains of homosexuals had structural differences that resembled that of straight members of the opposite sex. So it seems that while undertaking the hunt for the “transgender brain,” researchers have forgotten all about the discoveries made about the brains of same-sex attracted people.
The first “brain sex” study that did take into account the participants' sexual orientation found that the brains of transgender individuals were similar to those of people of the same birth sex rather than the opposite sex.
When researchers scan the brains of heterosexual people who identify as transgender, they also find they are typical for their natal sex. Samuel Stagg, a U.K.-based Ph.D. student of neuroimmunology, explains: “The homosexual sub-group show brains skewed along the male-female dimension. However, this is predominantly due to their co-occurring homosexuality. When we scan the brains of the heterosexual type, we find they are more typical for their natal sex.”
“Gender identity” not gender dysphoria
Gender dysphoria, like other psychiatric conditions, may have some biological underpinnings. There are traits like neuroticism that can predispose people to psychiatric conditions and research suggests that neuroticism has a strong biological basis with both genetic and environmental factors contributing to its development.
But gender activists are not concerned with gender dysphoria, rather they aim to establish a biological basis for being transgender that ceases to categorize it as a mental illness. Activists have pushed for a more “inclusive” definition of what it means to be transgender that seeks to reduce stigma and perceived barriers to medical transition services.
After the legalization of same-sex marriage in 2015, civil rights and gay rights organizations that may have otherwise had to shutter their doors pivoted to championing “trans rights.” The success of the "born this way" campaign in promoting the idea that sexual orientation is an innate, immutable aspect of identity has prompted activists to also present being transgender as innate and immutable.
Manhattan Institute fellow Leor Sapir wrote his Ph.D. dissertation on the rapid proliferation of the “transgender rights movement” and its efforts to obtain civil rights jurisprudence for “gender identity.” To this end, they have attempted to prove that “gender identity” is an innate, immutable trait called “neurological sex” or “brain sex,” which they say should override natal sex.
“In the American civil rights tradition, if you can convince a judge that being transgender is like being black, then you can tap into this entire body of judicial precedent and civil rights laws that immediately applies and gives you all the policies you want,” Sapir told me. Leor Sapir has written a number of important articles on this topic for City Journal, be sure to read them for further understanding.
More context: the trans community is divided
Interestingly, on the surface the transgender community presents as a unified front, but in reality it is divided into opposing philosophical factions: those propelled by civil rights organizations who seek to prove that being transgender is an “innate, immutable trait” for political and legal reasons, and the queer theorists who question the basis of scientific authority.
Last December, a transgender rights organization announced they were publishing a “groundbreaking article” that claims “being trans is a biological condition.” But after hundreds of critical comments from transgender people claiming that the search to find a biological basis for being transgender could be exploited, citing “eugenics” as a top concern, the organization spiked the article and issued an apology.
A self-described queer theorist named Eirnin who had early access to the article said it was not peer-reviewed nor written by an expert in the field but was merely a short letter that combined several theories of “brain sex” based on “debunked science.”
Another key point
If “gender identity” were solely biologically ingrained, it would conflict with the fact that gender dysphoria has been observed to resolve spontaneously or through psychotherapy at various ages. As we know from the growing population of detransitioners and a large body of research on desistance in children, transgender identities are not necessarily fixed. Currently, there is no brain, blood, or other objective test that distinguishes a trans-identified from a non-trans identified person.
Group project
This article is intentionally simplified to convey the main points effectively. It is my hope that it will assist individuals in countering the transgender "brain sex" argument when they encounter it. However, I am collaborating with neuroscientist Sammy Stagg on a group project to publish a paper that highlights the methodological flaws present in current "brain sex" research in a more comprehensive way.
==
But wait, we were told that "gender is a social construct," and that "gender is fluid" and "separate from biology." God is real but undetectable, good but mysterious, all-loving but tortures for eternity.
If even they can't make up their minds, how is anyone else supposed to accept their claims?
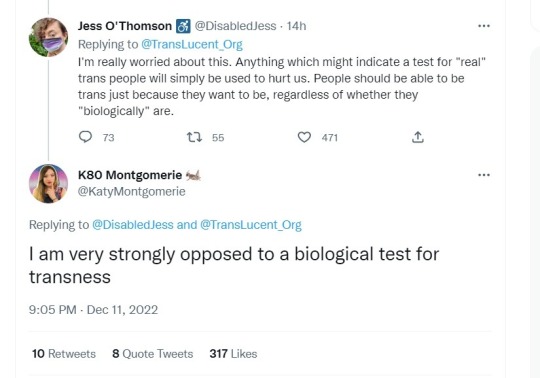
"People should be able to be trans just because they want to be, regardless of whether they 'biologically' are."
It should come as no surprise that well known anti-gay hate preacher, homophobe and child mutilation enthusiast Colin "Katy" Montgomerie is opposed to anything that would constrain the assertions and demands of the fantasists to objective reality.
Reminder again, the activists removed gender dysphoria from the definition so they could use the term for queer theory activism.
https://www.hrc.org/resources/glossary-of-terms
Transgender | An umbrella term for people whose gender identity and/or expression is different from cultural expectations based on the sex they were assigned at birth.
https://www.stonewall.org.uk/list-lgbtq-terms
Trans | An umbrella term to describe people whose gender is not the same as, or does not sit comfortably with, the sex they were assigned at birth.
I don't know what else I can do to demonstrate this is ideological and political, aimed at reordering society around the principles of Queer Theory, and not about helping people whose quality of life is impacted by a disorder. Especially since they've already been erased.
#Christina Buttons#brain sex#human biology#human brain#neuroscience#neurobiology#female brain#male brain#trans brain#gay brain#gender ideology#genderwang#queer theory#biology denial#religion is a mental illness
38 notes
·
View notes
Text
Are you:
Unsure if you should seek professional help
Seeking un-biased mental health advice, suggestions, and/or resources?
Email me: [email protected]
I'm willing to do unofficial consultations! 💕
DISCLAIMER: I am not a licensed clinician/therapist, but my experience/qualifications/certifications makes me a mental health professional wherein it is allowed for me to practice basic responsibilities equal to suggesting professional help, giving mental health advice/counseling, and providing resources and education.
Qualifications and Certifications:
Qb Test Technician: certified technician for the Quantitative Behavioral Test for ADHD (via QbTech). Head of the Qb department responsible for submitting prior authorizations to insurances, receiving internal and external referrals, training staff, administering the computerized test, and analyzing patients’ body language to aid in the diagnostic process for determining ADHD.
TMS Technician: certified technician for Transcranial Magnetic Stimulation Therapy for the treatment of Major Depressive Disorder (via NeuroStar). Head of the TMS department responsible for assessing/consulting with potential patients, submitting prior authorizations to insurances, assisting the APRN in the initial brain-mapping appointments, and administering daily TMS treatments. Also responsible for training and aiding staff during their certification process.
Neuropsychological Eval/Testing Administrator: assisted the company’s clinical psychologist in the following ways: receiving internal and external referrals, sending new patient intake packets, submitting prior authorizations to insurances, and scheduling patient appointments for comprehensive psychological evaluations for severe mental illness, adult Autism, and Bariatric clearance.
Qualified Behavioral Associate: certified BST practitioner- taught clients basic living skills and active daily living skills. Qualified to assist clinical staff with Locus and Treatment Plan evaluations, as well as psychotropic medication management.
Therapist Support Technician: performed Biofeedback Therapy with clients (i.e., provided services to enable emotional regulation for actively psychotic clients, as well as clients diagnosed with ADHD, Anxiety, and Depression). Trained in providing Case Management, Medication Management, and Crisis Intervention services.
2 notes
·
View notes
Photo

Role of Social Workers in Hospital and Healthcare
Introduction
According to Dr. Suresh Borole, the role of the social worker in the hospital perspective is very important for Patients with a range of health issues can get assistance and support from the hospital or medical social workers. For psychosocial issues, hospitalized patients can need a social worker. These might be linked to a physical condition or other health-related concerns, or they might be linked to a psychosocial issue like mental illness or homelessness. Medical social workers must do several tasks due to the complexity of the hospital environment.
Here are 4 Roles of Social Workers in Hospital
1. Collaboration
A major responsibility of the medical social worker is a collaboration with healthcare professionals. A multidisciplinary treatment team, which consists of experts including nurses, doctors, physician assistants, and physical therapists, performs this. The social worker contributes to communication between the patient, other team members, and the patient's family. Communication can be difficult since different providers have different perspectives, but the social worker's job is to make it easier so that the patient gets the best treatment possible.
2. Support
It might be stressful to be in the hospital. Social workers offer supportive counseling to patients and their families as a result. Patients dealing with addiction and chronic pain, as well as those facing mortality, disability, terminal disease, and social and mental health issues, can all benefit from the assistance of social workers. Patients with similar issues may benefit from group or individual counseling from social workers. Social workers are qualified to provide clinical and mental health services as needed because of their training in counseling, therapeutic approaches, and the treatment of behavioral and mental health conditions.
3. Advocacy
Medical social workers represent patients' interests as advocates. This can entail communicating the patient's willingness to the family and the medical staff or ensuring that the patient is provided with appropriate information regarding his or her care and treatment. The creation of advanced directives, which provide specific instructions regarding the patient's desires regarding medical end-of-life decision-making, is a task that social workers help patients with frequently.
4. Case Management
As case managers, medical social workers coordinate the care of their patients. This may involve putting patients in touch with prosocial services. A social worker might, for instance, assist a patient who is homeless in finding a shelter or housing program. Medical social workers frequently participate in the discharge planning process as well as the organization of post-care services including at-home care, follow-up visits, or, if necessary, locating the patient in a rehabilitation center.
3 notes
·
View notes
Text
So if a perverted boy tries to claim he is a girl and should therefore have access to girls restrooms and locker rooms any teacher that sees through the act and says no could face fines or even prison?
The enactment of the Change or Suppression (Conversion) Practices Prohibition Act 2021 makes it unlawful for anyone to fail to affirm the declared gender identity of another person under threat of criminal sanctions, including fines and incarceration, in the Australian state of Victoria.
The bill was sold to the public as a measure to prevent the trauma that can be caused caused to same sex-attracted people through harmful and abusive practices intended to change or suppress their orientation. The evidence relied on for these practices was largely historical, from overseas jurisdictions and could be dealt with under existing laws.
Despite there being no evidence that anyone in Victoria had been subjected to conversion or suppression practices on the basis of their gender identity, the normalization of a manufactured category associating sexual orientation and gender identity meant that both were included in the legislation.
The Conversion Act was so broadly drafted that it bans any conduct (including a conversation) by any person directed towards any second person on the basis of the second person’s sexual orientation (or gender identity) where the conduct is intended to “suppress or change” the second person’s sexual orientation (or gender identity) or induce the second person to suppress or change their sexual orientation (or gender identity).
And it’s not only parents that run the risk of criminalization. Health care providers, spiritual advisors, teachers, or caregivers could be captured and denounced by this legislation. In fact, even those outside of the jurisdiction of Victoria are subject to the Act as it has extra-territorial application.
The Victorian Equal Opportunity and Human Rights Commission, the statutory body tasked with administering and enforcing the act, warns that exploratory conversations, or adopting a “wait and see” approach, could be an offence.
This act is the harshest and most punitive globally to date. “Change or suppression” conduct causing “psychological harm” could result in 5 years’ imprisonment or a $100,000 fine, or, for serious psychological harm, 10 years imprisonment or a $200,000 fine. This will increase up to a $1 million fine for organizations.
On August 13, the Daily Mail reported that Victorian parents are finding themselves in the position of being unable to access counseling for their child, and are living in fear of supporting their child to do anything other than affirming their child’s declaration of a gender identity, even in situations where their child has mental health co-morbidities, is neuro-atypical, or suffering bullying, trauma or bereavement.
The criminal penalties remove a parent’s ability to protect their child from accessing experimental hormone treatments that could leave them with a myriad of problems. Recent studies have revealed these problems could include major, sustained health concerns such as infertility, organ failure, arrested cognitive development, and osteoporosis. Further, it puts children on the pathway to irreversible surgeries with high rates of complications and need for revisions, and lifelong dependence on pharmaceuticals.
Compassionate mental health care desperately needed by vulnerable youth has now been put on chill. Some psychologists and therapists are going to completely avoid treating minors due to the fear of being captured by the criminal sanctions in the act should they fail to actively affirm the declared gender identity of the person presenting for care.
Victoria is home to Australia’s largest children’s gender clinic – the Royal Children’s Hospital Melbourne Gender Service – overseen by Associate Professor Dr. Michelle Telfer, the clinic treats children (even those under 8 years old) and continues to claim “puberty blockers are reversible.” Dr. Telfer served on the board of the Australian Professional Association for Transgender Health from 2014 to 2020 and is a strong advocate for the transitioning of children. During an interview he conducted in 2021, he boasted of an underage female patient he’d treated: “I can help this child have a boy’s body.” And how many people can do that?”
On a panel hosted by the WA Government and ACON – the taxpayer subsidized charity that promotes medical transitioning – Dr. Telfer downplayed the rising numbers of detransitioners by relying on the Amsterdam Cohort of Gender Dysphoria Study (an out-of-date, overseas study of mostly male adults) to pretend it is not an increasing issue and saying “I really dislike the word detransition ’cause it’s a really horrible word.”
The clinic at Royal Children’s Hospital is reputedly modeled on the now-disgraced Tavistock children’s gender clinic, recently ordered to close its doors with the impending release of the damning Cass Report that documented systemic failures, absence of data and ideological capture that compromised consistent, impartial and clinical care.
Earlier this year, the French Medical Academy cited the rapid increase in child patients seeking gender affirmation at the Hospital as part of a release they issued warning clinicians to exercise caution in treating “trans kids.” They called it “an epidemic-like phenomenon,” noting that in 2003, only one child at the Royal Children’s Hospital had been diagnosed with gender dysphoria, while today it is treating nearly 200.
In 2016, the Victorian government enabled gender self-identification with the creation of the Births, Deaths and Marriages Registration Amendment Act, which allowed children and adults to change the sex on their birth certificate every 12 months without a need for “sex affirmation surgery.” Attorney-General Jill Hennessy’s second reading speech for the Conversion Bill stated that there is no evidence that gender identity can change, putting these two bills into conflict and a clear demonstration of the typical incoherence of law and policy that protects gender identity ideology.
The attorney general’s position ignored the growing chorus of voices of detransitioners who regret undergoing social transition, hormonal interventions or irreversible surgeries, while ignoring the multiple medical studies that conclude the majority of children presenting with distress about gender come to accept their natal sex during puberty without the need for any medical intervention.
The parliamentary debate over the conversion bill was characterised by extravagant displays of emotion and hyperbole for those in favour relying on dramatic examples of hurt feelings and perceived exclusion, starkly juxtaposed by those in opposition who pleaded for more time, alternative views to be acknowledged and included, and the mounting evidence against socially and medically transitioning children to be considered.
In parallel to the situation in the UK, many Australian federal and state government departments, organizations, corporations, institutions, banks, law firms and universities are signed up to ACON’s programs with the purpose of embedding the ACON worldview on gender and sexuality into Australian public life. Active allyship must be demonstrated, remaining neutral or impartial can attract sanctions, and in some jurisdictions, such as Victoria, resistance is now unlawful, attracting criminal prosecution.
The two taxpayer funded media platforms, SBS and ABC, are both signed up to the ACON Pride in Diversity scheme, Australia’s version of Stonewall. Modelled on Stonewall’s Diversity Champions Workplace Equality index, organisations are benchmarked against other organisations by earning points on ACON’s Australian Workplace Equality Index by complying with requirements detailed in an onerous submission form to promote and report favourably on trans and gender identity issues, but penalised with loss of points for reporting critically.
As a result, the growing global scandal surrounding the interference in the integrity of the minds and bodies and children on the basis of gender identity is largely ring-fenced from the Australian public with the notable failure of many mainstream media outlets to cover this issue impartially and without bias; depriving Australian families of critical information, leaving them unable to assist their distressed children, and living in fear of criminal penalties if they refuse to consent to their child being medically “affirmed.”
By Katherine Deves Katherine is a guest contributor at Reduxx. An Australian lawyer, she is a Sky News Contributor and the former Liberal candidate for Warringah. She currently lives in Sydney where she advocates for the rights of women and children, and is the proud mother to three daughters.
#Australia#gender ideology and children#Change or Suppression (Conversion) Practices Prohibition Act 2021#Dr. Michelle Telfer
2 notes
·
View notes
Text

Do you know the biggest threats to Men's health chicago? Major risks to men's health include heart disease, cancer, depression and the tendency to engage in risky behavior. Men's health initiatives in Chicago emphasize comprehensive care addressing physical, mental, and social well-being. Healthcare providers offer screenings, treatments, and preventive measures tailored to men's specific health concerns, such as prostate health, cardiovascular disease, and mental health issues. Clinics provide accessible services, including regular check-ups, vaccinations, and counseling for conditions like depression and anxiety. By prioritizing men's health, Chicago aims to reduce disparities, improve overall wellness, and foster a supportive environment where men can thrive physically, mentally, and emotionally. Contact us now +1- 630-908-7082.
0 notes