#infectious disease
Text
Incubation Periods List
Hi all!
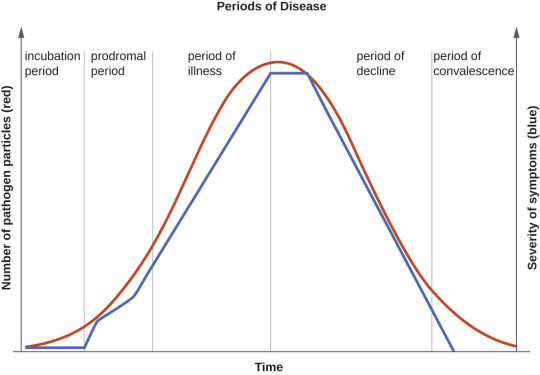
The following is a list of incubation periods for various infectious diseases for all your writing needs. An incubation period is the amount of time between exposure to an infectious agent (bacteria, virus, protozoa or prion) and the person having the first symptoms of the resulting illness. Knowing this is helpful in creating a timeline for your story.
Anthrax: Incubation period of 1-60 days
Avian Flu: Incubation period 3-9 days
Botulism: Incubation period 12-72 hours
Chikungunya: Incubation period 3-7 days
Chlamydia: incubation period 7-21 days
COVID-19: Incubation period 5-10 days
Creutzfeldt-Jacob Disease: Incubation period 10-20 years
Dengue: Incubation period 5-7 days
Diphtheria: Incubation period 2-5 days
Ebola: Incubation period 2-21 days
Hantavirus: incubation period 1-8 weeks
Hepatitis A: incubation period about 28 days
Herpes: Incubation period 2-12 days
Herpes Zoster/Varicella (Chickenpox): Incubation period 14-16 days
Herpes Zoster (Shingles): Incubation period- technically none, as this is a reactivation of the virus that causes chickenpox
HIB: Incubation period 2-10 days
HIV: Incubation period 1-6 weeks to prodrome, approximately 10 years to AIDS
Influenza: Incubation period 1-4 days
Legionnaires Disease: Incubation period 5-6 days
Leprosy: Incubation period 9 months to 20 years
Lyme Disease: Incubation period 3-30 days
Malaria: Incubation period 7-30 days
Measles: Incubation period 10-12 days
Meningitis, Bacterial: Incubation period 2-10 days
Meningitis, Viral: Incubation period 3-10 days
Monkeypox: Incubation period 1-2 weeks
Mumps: Incubation period 16-18 days
Norovirus: Incubation period 12-48 hours
Pertussis: Incubation period 7-10 days
Plague: Incubation period 2-8 days
Pneumococcal Pneumonia: Incubation period 1-3 days
Polio: Incubation period 7-10 days
Q-Fever: Incubation period 2-3 weeks
Rabies: Incubation period 20-90 days
RSV: Incubation period 4-6 days
Smallpox: Incubation period 7-17 days
Syphilis: Incubation period 10-90 days
Tetanus: Incubation period 3-21 days
Tuberculosis: Incubation period 2-10 days
Typhoid: Incubation period 6-30 days
Typhus: Incubation period 1-2 weeks
West Nile Virus: Incubation period 2-6 days
Yellow Fever: Incubation period 3-6 days
Zika: Incubation period 3-14 days
164 notes
·
View notes
Text
Q Fever
Aka, Query fever. What a weird name for a disease. Imagine telling people that's what you got.

in the 30s-40s, an Australian pathologist in QLD/Brisbane, came across an outbreak of the same or similar illness among abbatoir or slaughterhouse workers.
At the time, he called the disease "Q" fever or query as a temporary name until the pathogen could be identified. Unfortunately it stuck.
decades later, now nobel prize winner and virologist, MacFarlane Burnett isolated and identified the microbe responsible. I think this discovery contributed to his prize. i forget already.
Microbe responsible: Coxiella burnetti. Named for Burnett and HR Cox, the American bacteriologist who found the genus Coxiella where C burnetti falls under.
Initially they felt it was related to Rickettsia, responsible for Rocky Mountain Spotted Fever, but as science progressed, this was disproven.
Now for a Case Report
A 55 yo Italian man with a history of aortic valve replacement was diagnosed with pyrexia of unknown origin twice. Further signs included myalgias/splenomegaly/night sweats. The 2nd time he was admitted for PUO he deteriorated rather dramatically and was put on meropenem and teicoplanin.
A host of organisms was tested for on serological testing based on the man's travel and epidemiological history, all negative. Even a rheumatological panel was done, also less revealing. He also had a history of MGUS (a haem disoder), which is kind of a red herring here.
Cultures were negative, no vegetations were seen on a TTE - so they did consider IE. Which is an important differential for PUO.
Eventually a PET-CT was done (often favoured when investigations do not yield much for a sick patient with fevers), finally revealing a focus of infectious on his ascending aorta, where he'd also had previous surgery done. And in a round about way, they also further identified Coxiella Burnetti. He was treated doxycycline and hydroxychloroquine. As it's so rare in Italy, it wasn't really considered even though he mentioned rural travel.
Bottomline: Q Fever is an important consideration in the work up for culture negative IE. Further to this, always consider IE in the differentials for PUO particularly if they're at increased risk for IE (prosthetic valves, damaged valves, select congenital heart issues, previous IE). IE can present with night sweats, fevers, weight loss and splenomegaly. It can be insidious and chronic in nature. other risk factors can be more suggestive as we'll get into below.
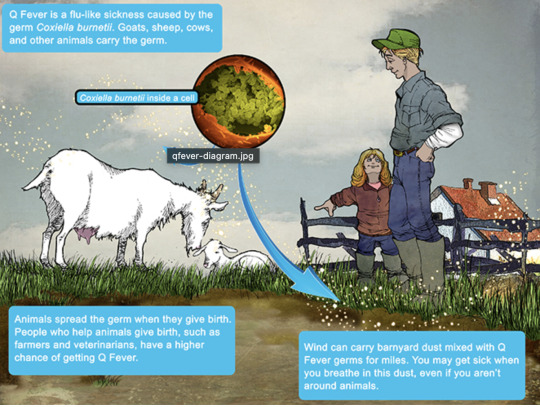
Causative organism
Coxiella burnetti, it's a zoonoses - i.e. transmissible from animals. Special powers: very tough/hardy, can survive extreme environments (high temps and UV light etc.) over prolonged periods and is resistant to many common disinfectants/surface cleaners.
It's an intracellular pathogen and gram negative coccobacilli (PINK!)
name coccobaccili reminds me of cocopuffs.
it's mainly associated with farm animals, which the CDC so wholesomely displays on its website on Q fever (wtf).

goats, sheep, cattle typically (but many other animals, even birds, dogs and horses can be reservoirs)
in particular bodily fluids - amniotic fluid, placenta, faeces/urine, milk etc.
you can get it through unpasteurized milk and through inhaling it if it lands on dust in the area
ever visit a farm or petting zoo lately? OMG WASH YOU HANDS.

That said, it's typically inhaled in inorganic dust. You inhale it, it goes to the lungs, and then the bloodstream.
Increased risk for Coxiella burnetti (What to take on history of exposures and when to strongly consider it)
live on a farm or near one
exposure to a farm
work as a vet on a farm
farm worker, dairy workers, researchers on these animals/facilities
slaughterhouse/abbatoir
Also from CDC:
Clinical presentation
Most won't get sick after exposure and remain asymptomatic, a very small minority does. even though it is highly infectious.
incubation time is 2-3 weeks (consider this time in your history of exposure, did they work on the farm 2-3 weeks ago as opposed to yesterday).
Nonspecific acute infectious symptoms:
nonspecific systemic fevers/malaise/arthralgias/myalgias--> key is high fevers though and can be associated with headache and photophobia.
non specific GI - N/V/diarrhoea
respiratory ones - SOB or cough, consider it as atypical cause of community acquired pneumonia.
rare: hepatitis and jaundice (granulomatous) or encephalitis with neurological complications such as demyelinating disease or CN palsies, also haemolytic anaemia and HLH (yikes)

really it's the history of exposure that will lead you down the garden path to Q fever.
Chronic Q fever is perhaps worse, and can present as culture negative IE/PUO. Months/years later, as B symptoms as above above + LOW/LOA, night sweats. More likely to occur if you are predisposed for IE as above, have a weakened immune system for any reason, including pregnancy.
Chronic Q fever has a mortality of 10% if left untreated. About <5% of those with acute Q fever develop this if left untreated. Speculation is that it's more of an autoimmune process or abnormal immunological response to the bacteria.
To be honest, most who walk in the door with community acquired pneumonia get treated empirically for atypicals anyway, (standard course of doxycycline), so we hardly really ponder the question of Q fever in every patient. But if they present chronically and did not have atypical cover at the onset of acute symptoms, then it's something important to consider.
Other important conditions - can cause complications in pregnant women and 20% will get post Q fever syndrome. like chronic fatigue.
investigations
Serology! nice and easy. Look for IgG antibodies in the chronic presentation. Or PCR. Down side to serology - can take 2-3 days for the body to make said antibodies to the bacteria for detection. PCR can be done on any fluids/tissue sent.
Cultures useless, hence it fall under the umbrella of culture negative (hard to grow outside a host cell, it is an obligate intracellular pathogen).
Other hints on bloods (as serology/PCR takes time to return) - elevated or low platelet's, transaminitis with normal bili, opacities in CXR with hilar lymphadenopathy, CSF will show raised protein levels if done when encephalitis is suspected.
imaging can also support the diagnosis.. as illustrated by the case report.
Treatment
Acute disease - as standard for atypical bugs, doxycycline 100 mg BD for 14 days. Alternatives - TMP SMX or Clarithromycin.
Chronic Q fever or IE:
native valves: doxycycline and hydroxychloroquine (200 TDS) for 18 months
prosthetic: same but 24 months
why hydroxy: enhances the action of doxycycline (increases the pH of the phagolysosome)
Follow-up: look for 4 fold decrease in IGG
Sources:
CDC
Stat Pearls
Wiki as linked above
#australian history#medblr#medblrs#infectious disease#infectious diseases#q fever#coxiella#coxiella burnetti
66 notes
·
View notes
Text
“If you ever prescribe an aminoglycoside, and the patient doesn’t come back complaining because it fucked up their digestion, it’s because they didn’t take it.”
34 notes
·
View notes
Text
Grudgingly I had to give up dicking around on the Internet and go do some house cleaning. I'm listening to Mary Roach tell me about cholera dynamics when I remember, and I want to tell Tumblr—
Did you know that the same specialist predator/prey population dynamics over time that you usually see described in terms of Canadian lynx and snowshoe hare also apply perfectly well to Vibrio cholerae and its most common bacteriophage?
And that this is a major factor in why pathogenic cholera outbreaks — caused mostly by only one lineage of V. cholerae bacteria — eventually fade even if the population isn't wholly infected by cholera or wiped out by it?
The world is a wild and fascinating place.
46 notes
·
View notes
Text
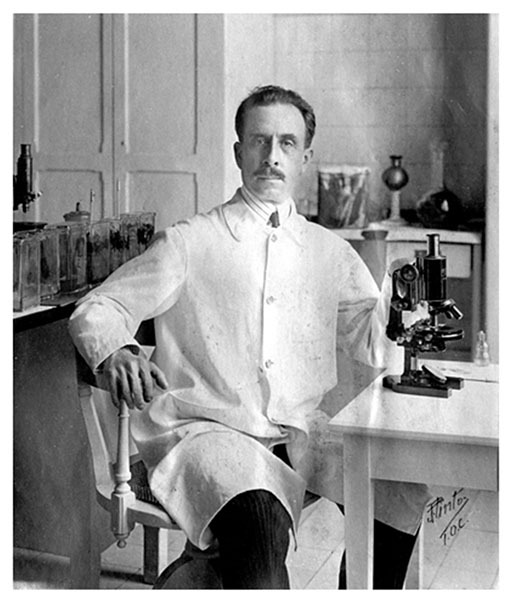



Carlos Chagas – Scientist of the Day
Carlos Chagas, a Brazilian clinical physician and microbiologist, died Nov. 8, 1934, at the age of 55.
read more...
#Carlos Chagas#microbiology#infectious disease#histsci#histSTM#20th century#history of science#Ashworth#Scientist of the Day
28 notes
·
View notes
Text
Q. Do you recognize this rash?
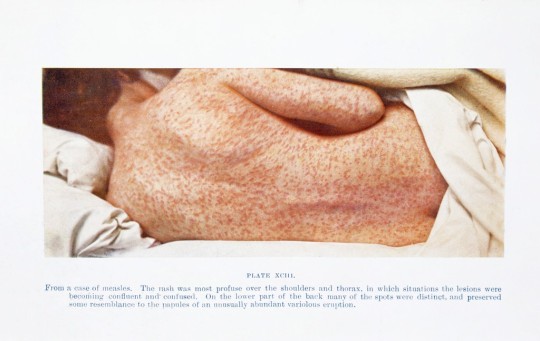
A. Measles (rubeola) is an infectious disease caused by a single-stranded Paramyxoviridae RNA virus. After infection, the virus incubates for ~10 days. First come fever, congestion, conjunctivitis, and a highly infectious "barking" cough that spreads respiratory droplets. 3-4 days later a rash appears. All symptoms intensify for 3-4 days and then resolve. Late winter and spring is prime time for measles infections.
Source: Craft, Fox, Goldsmith, "Measles in Child"; image from Wellcome Collection
5 notes
·
View notes
Text
A thought, regarding Cujo: I think Donna's apparent symptoms of rabies at the end were psychosomatic.
Cujo's rapid infection is just barely within the bounds of plausible, but Donna's next-day symptoms and later recovery aren't. She also doesn't actually display normal human symptoms of rabies, in particular biting the paramedic: the urge to bite things doesn't really show up in rabid humans. If rabies causes aggression in humans at all, they display it via the usual human means of expressing aggression, such as using fists or their voice.
She does, however, display stereotypical canine symptoms of rabies. Donna doesn't really know how rabies works, medically, but she has a common knowledge understanding of it combined with the hellish example Cujo set. After the horrific experience she just went through, she loses it from stress and trauma and temporarily embodies what her subconscious thinks is happening. For a little while there, she believed her rage was coming from a rabies infection, and her mind made it real.
The paramedic she bit went through the rabies treatment course because you do not fuck around with rabies and he did get bitten by someone who might have been rabid, but the treatment Donna got was in fact the normal rabies immune globulin and vaccination course, along with treating her wounds.
#original posts#what's up I just read the book#waiting for the film to come in from one of the other libraries in my local library system#stephen king#cujo#meta#rabies#infectious disease
10 notes
·
View notes
Text
Fish it never fry
Salmon are my favorite guy
Steak, are you prepared
Tell the chef, "stop at rare"
Swish hear the pan go hiss
Have a body eat the fish
Teriyaki overload
Everybody seafooood
7 notes
·
View notes
Text
No paywall.
5 notes
·
View notes
Note
RES anon. Thank you for replying! I'll switch the tank as a whole to collard greens/pellets until the little guy gets released, the shrimps and fish shouldn't mind. I also have mealworms. Still adjusting the basking area temperature, need to get the platform's distance from the basking lights right, but the water is a consistant 80F which I read is what baby RES should have. Water quality should be ok, it's a very established tank with a lot of cleaners and I'll do water changes if needed. Would you be willing to talk more about the disease transmission you mentioned in your tag, please?
Sounds like a good set up! I mention infectious disease transmission because turtles are particularly susceptible to certain pathogens, especially when it comes to commingling species. For example, a herpesvirus that is asymptomatic in RES can be fatal to the western pond turtle (a vulnerable species). For that reason I get nervous about introducing a turtle with unknown pathogens to a new environment.
To be safe, I’d recommend reaching out to Fish and Wildlife in the county you plan on releasing the turtle (make it very clear that this is not a pet) to ask for their recommendations. The will likely be able to give you better answers about the local ecology and if it’s advisable to release there. Would also be a good idea to call your local F&W to get their thoughts as there are some regional pathogens that should be taken into consideration. If transporting a RES out of Florida for example I’d be concerned about spreading turtle fraservirus. If you are unable to release the turtle in its native range, you may be able to find a museum, garden, or educational facility with a turtle pond that would be able to take him in.
14 notes
·
View notes
Text
Made this for my virology students as a prize. Remember the Taiwan CDC gijinkas of infectious diseases? I made a drawing in that style but for the disease they were studying, the Infectious Pancreatic Necrosis Virus (IPNV)
#my art#i guess my ocs?#my ocs#kinda a commission too since i put down hours for this#commission#art#artwork#illustration#microbiology#tw animal sickness#tw gore#infectious disease#molecular biology#virology#viruses#virus
12 notes
·
View notes
Text
Psittacosis
Let's open with a case report, like we're on an episode of house.
Case Report
35 yo otherwise well, suddenly presents with 2/52 of high fevers and a headache (usually this means > 39)
a/w chills and rigours, responsive to medication/presumably panadol and intermittent (would resolve then come back)
no respiratory symptoms
She had neutrophilia and intrestingly, a CRP of merely 30.
CXR revealed nonspecific consolidation in 2 lobes, they followed this up with a CT revealing pretty impressive ground glass opacities (or GGOs)

She was empirically treated on IV tazocin only (I'm used to atypical coverage empirically started if there's even a whiff of resp, which she may not have had symptoms but her CXR confirms this)
eventually she was on referred to the authors, who felt her CT findings with consistent with psittacosis and treated her with doxycycline which resolved her symptoms in 48 hrs
on further history, it was revealed that she had parrots at home, one had died 2 days preceding her symptoms and she was sleeping next to its body at night (crazy)

What is it:
psittacosis is a zoonoses (transmitted by animals, animals = reservoirs), in this case, transmitted by birds. Orthinoses if birds in general, but psittacosis if referred to macaws, parrots etc. YOu can also catch it from chickens and turkeys.
Some what related is Bird fancier's lungs. Which just sounds fancy.. I'm sure it's just an old term.

Bird fancier's lung refers to a hypersensitivty pneumonitis (ILD) caused by bird exposure. DIfferent disease process, but birds is the come denominator. INhaled bird particles
Psittacosis specifically refers to the infective disease process caused by a bacteria. It was 'identified" or reported in the 1870s, when a cluster of 7 swiss patients developed the same symptoms and found to have possessed tropical birds.
Similarly, in the 1930s there was an outbreak in the US with a mortality of up to 20% (80% in pregnant women), also attributed to parrots from South America.
Eventually, with further scientific development, the causative pathogen was identified as chlamydia psittaci, an atypical intracellular organism.
Psittacosis is a significant differential to consider in community acquired pneumonia as it has a high mortality if left untreated. But it is rare, and causes about 1% of cases in the US. Part of this is due to improved hygiene practices and strict importation guidelines of tropical birds.
It's spread through the inhalation of dust with either dried faeces or respiratory secretions from infected birds.
Clinical features
Variable! but the key thing on history is birds
incubation time can be anywhere from 2 days to 20
Flu-like (fevers/chills/myalgias/arthralgias/malaise/headache)
high fevers is key
respiratory symptoms - does not always present as per the case report, and can be mild on spectrum (dry cough) to more severe
if systemic, can also get photophobia, deafness and epistaxis
Rare (particularly where doxycycline or azith are prescribed at a low threshold): hepatosplenomegaly (look out for LFTs), GI symptoms (remember CAP can present with diarrhoea, nausea/vomiting --> always do a CXR)
even rarer: endocarditis or myocarditis, encephalitis or hepatitis (usually the complications of untreated disease)

Increased risk groups:
pet shop owners
bird owners
farmers
zoo, lab workers where birds are kept, vets, avian quarantine station workers
poultry handlers/workers
So ask if they live or work with birds, or had recent exposure.
INvestigations
serology is gold standard - so looking for antibodies in blood tests
it's intracellular - so hard to culture if even possible on standard blood cultures
elevated ESR/CRP may see LFT derangement and creatinine rise in systemic illness
CXR- usually lower lobe changes, if CT is done, you can get pulmonary infiltrates with GGOs
Treatment:
usual culprits for atypical coverage: azithromycin 3 days or doxycycline 100 mg BD for 14/7
Differentials
always broad if systemic features only (also consider IE and other causes of sepsis)
with resp symptoms - legionella, Q fever, mycoplasma, tularaemia (except for tularaemia, the rest are also covered by doxycycline)
In clinical practice, I'm so used to just having atypicals on board for any cases of atypical pneumonia. I really take it for granted. But will consider this differential more myself in cases of PUO - but I feel like there should be at least CXR findings regardless.
Anyway, prognosis is very good so long as it is treated.
Sources:
CDC guidelines
Case Report: Importance of Clinical history in Psittacosis
StatPearls
Wiki
#psittacosis#chlamydia psittaci#community acquired pneumonia#infectious diseases#infectious disease#medblr
9 notes
·
View notes
Text
“An infectious disease specialist without beta-lactams, is like a cardiologist without beta blockers.”
28 notes
·
View notes
Text
Hi guys, what's your local policy for fluid resuscitation in patients with sepsis (not septic shock) with oliguric CKD or reduced ejection fraction? Some literature supports the aggressive use of crystalloid in patients with septic shock even if they're normally at risk of volume overload, but I wonder if that can be extended to systemically ill patients with a clear source of infection without overt hypotension.
#sepsis#septic shock#fluid resuscitation#iv fluids#critical care#emergency medicine#a&e#intensive care#infectious disease#id
3 notes
·
View notes
Text
“I myself am a trained disease detective. I have led outbreak investigations for HIV and syphilis. I am a published scientist. And I know a lot about public health and infectious disease transmission. I emphasize my training and my experience because if I had to go to three different places before I got diagnosed, imagine what the average gay man has to do?”
2 notes
·
View notes
Text
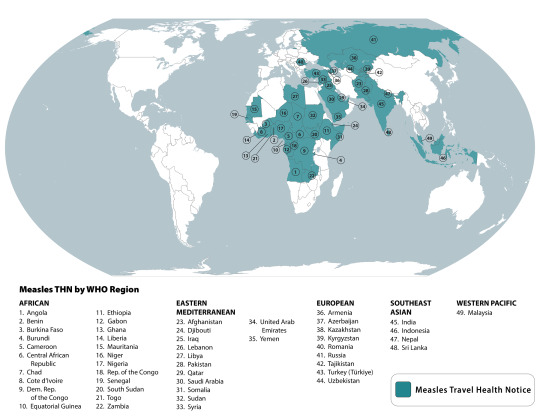
Q. Where in the world is there measles?
A. It's not just the United States: the United Kingdom, the Philippines, and Austria (among other countries) are experiencing measles outbreaks.
#TeachingRounds#FOAMed#public health#epidemiology#pediatrics#vaccine preventable disease#infectious disease
2 notes
·
View notes