#Diagnosi Medica
Text
Quali sono le cause della malattia di Alzheimer?
Le cause e i trattamenti della demenza sono fondamentali da comprendere per l’era in cui viviamo.
Source: 13 NOV 2022; by A Midwestern Doctor on The Forgotten Side of Medicine
Continue reading Untitled

View On WordPress
#AD#Altre Condizioni#Alzheimer#Amiloide#Anticorpi Monoclonali#Autoimmunità#Carenze Nutrizionali#Carenze Ormonali#Cause#Cellule Staminali#Cervello#Circolazione Cerebrale#Circuiti Neurologici#Colesterolo#Declino Cognitivo#Demenza#Diagnosi Medica#Disinformazione Scientifica#Esposizione a Tossine#Farmaci#Fattori Trofici#Industria#Ipotesi Circolatorie#Irradiazione Sangue#Lesioni da Vaccino#Linfatici Cerebrali#Malattia#Malattia Lyme#Malattie Cardiovascolari#Malattie Croniche
12 notes
·
View notes
Text
Appena uscita dall’ultimo incontro di diagnosi con la mia psi perché sospetta che io abbia l’ADHD
Mezzo che non so se mi viene da ridere o da piangere
#tipo wow ho una effettiva diagnosi medica sul fatto che i miei problemi non siano solo colpa mia ™️???#dopo 26 anni??#dopo la quantità di terapia che ho fatto per capire che cazzo di problema avessi#e non usciva mai nessun problema#e ora una diagnosi??#boh forse non ci credo#poi vabbè deve ancora mandarmi la relazione finale#ma era abbastanza convinta#personal
2 notes
·
View notes
Text
L'Intelligenza Artificiale nel Settore Sanitario - Innovazioni e Impatti
Nel tessuto sempre più intricato della tecnologia, l’Intelligenza Artificiale (IA) si presenta come il catalizzatore rivoluzionario nel settore sanitario. Questo connubio tra medicina e innovazione tecnologica sta disegnando nuovi orizzonti, gettando le basi per una trasformazione epocale. Nell’approfondire il ruolo cruciale dell’IA nel contesto sanitario, ci addentreremo nei meandri delle…
View On WordPress
#assistenza virtuale#diagnosi#gestione sanitaria#IA#innovazione medica#Intelligenza Artificiale#privacy#ricerca farmaceutica#salute digitale#sanità#sicurezza dati
0 notes
Text
you ever see someone play sage in such a way that just immediately tells you they usually only play white mage or...
#if i see you cast diagnosis one more time i swear to GOD its on sight#listen. ok. do you have very few options as a sage in stone vigil. yes.#but TRUST ME. EUKRASIAN DIAGNOSIS SOTERIA & PHYSIS ARE ENOUGH IF THE DPS IS HIGH ENOUGH#i did stone vigil with duty support afterwards. exact same pulls. even with the garbage single target dps of the npc allies#i casted diagnosis ONCE.#and were this someone who is levelling id just say. yk. ahatever. theyre learning#amazing manderville milpreves. mentor. we barely made it through the final boss because they died halfway through#their key issue was that they played it as white mage. essentially#you wouldnt use medica 2 in a trash pull so why would you use physis?#proactive reactive etc etc#your raw healing is miserable as a sage even on level 90 like you cant. rely on being reactive.#but that is what this person was doing#if i could analyse art the way i analysed people playing my main in ffxiv i would have such good grades tbh#this could maybe also go for scholar but i touch scholar so rarely i just have NO clue
0 notes
Text
How Cigna Saves Millions by Having Its Doctors Reject Claims Without Reading Them
by Patrick Rucker, Maya Miller and David Armstrong for ProPublica
March 25, 5 a.m. EDT
Internal documents and former company executives reveal how Cigna doctors reject patients’ claims without opening their files. “We literally click and submit,” one former company doctor said.
When a stubborn pain in Nick van Terheyden’s bones would not subside, his doctor had a hunch what was wrong.
Without enough vitamin D in the blood, the body will pull that vital nutrient from the bones. Left untreated, a vitamin D deficiency can lead to osteoporosis.
A blood test in the fall of 2021 confirmed the doctor’s diagnosis, and van Terheyden expected his company’s insurance plan, managed by Cigna, to cover the cost of the bloodwork. Instead, Cigna sent van Terheyden a letter explaining that it would not pay for the $350 test because it was not “medically necessary.”
The letter was signed by one of Cigna’s medical directors, a doctor employed by the company to review insurance claims.
Something about the denial letter did not sit well with van Terheyden, a 58-year-old Maryland resident. “This was a clinical decision being second-guessed by someone with no knowledge of me,” said van Terheyden, a physician himself and a specialist who had worked in emergency care in the United Kingdom.
The vague wording made van Terheyden suspect that Dr. Cheryl Dopke, the medical director who signed it, had not taken much care with his case.
Van Terheyden was right to be suspicious. His claim was just one of roughly 60,000 that Dopke denied in a single month last year, according to internal Cigna records reviewed by ProPublica and The Capitol Forum.
The rejection of van Terheyden’s claim was typical for Cigna, one of the country’s largest insurers. The company has built a system that allows its doctors to instantly reject a claim on medical grounds without opening the patient file, leaving people with unexpected bills, according to corporate documents and interviews with former Cigna officials. Over a period of two months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the documents show. The company has reported it covers or administers health care plans for 18 million people.
Before health insurers reject claims for medical reasons, company doctors must review them, according to insurance laws and regulations in many states. Medical directors are expected to examine patient records, review coverage policies and use their expertise to decide whether to approve or deny claims, regulators said. This process helps avoid unfair denials.
But the Cigna review system that blocked van Terheyden’s claim bypasses those steps. Medical directors do not see any patient records or put their medical judgment to use, said former company employees familiar with the system. Instead, a computer does the work. A Cigna algorithm flags mismatches between diagnoses and what the company considers acceptable tests and procedures for those ailments. Company doctors then sign off on the denials in batches, according to interviews with former employees who spoke on condition of anonymity.
“We literally click and submit,” one former Cigna doctor said. “It takes all of 10 seconds to do 50 at a time.”
Not all claims are processed through this review system. For those that are, it is unclear how many are approved and how many are funneled to doctors for automatic denial.
Insurance experts questioned Cigna’s review system.
Patients expect insurers to treat them fairly and meaningfully review each claim, said Dave Jones, California’s former insurance commissioner. Under California regulations, insurers must consider patient claims using a “thorough, fair and objective investigation.”
“It’s hard to imagine that spending only seconds to review medical records complies with the California law,” said Jones. “At a minimum, I believe it warrants an investigation.”
Within Cigna, some executives questioned whether rendering such speedy denials satisfied the law, according to one former executive who spoke on condition of anonymity because he still works with insurers.
“We thought it might fall into a legal gray zone,” said the former Cigna official, who helped conceive the program. “We sent the idea to legal, and they sent it back saying it was OK.”
Cigna adopted its review system more than a decade ago, but insurance executives say similar systems have existed in various forms throughout the industry.
In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
Cigna said its review system was created to “accelerate payment of claims for certain routine screenings,” Cigna wrote. “This allows us to automatically approve claims when they are submitted with correct diagnosis codes.”
When asked if its review process, known as PXDX, lets Cigna doctors reject claims without examining them, the company said that description was “incorrect.” It repeatedly declined to answer further questions or provide additional details. (ProPublica employees’ health insurance is provided by Cigna.)
Former Cigna doctors confirmed that the review system was used to quickly reject claims. An internal corporate spreadsheet, viewed by the news organizations, lists names of Cigna’s medical directors and the number of cases each handled in a column headlined “PxDx.” The former doctors said the figures represent total denials. Cigna did not respond to detailed questions about the numbers.
Cigna's explanation that its review system was designed to approve claims didn’t make sense to one former company executive. “They were paying all these claims before. Then they weren’t,” said Ron Howrigon, who now runs a company that helps private doctors in disputes with insurance companies. “You’re talking about a system built to deny claims.”
Cigna emphasized that its system does not prevent a patient from receiving care — it only decides when the insurer won’t pay. “Reviews occur after the service has been provided to the patient and does not result in any denials of care,” the statement said.
"Our company is committed to improving health outcomes, driving value for our clients and customers, and supporting our team of highly-skilled Medical Directors,” the company said.
PXDX
Cigna’s review system was developed more than a decade ago by a former pediatrician.
After leaving his practice, Dr. Alan Muney spent the next several decades advising insurers and private equity firms on how to wring savings out of health plans.
In 2010, Muney was managing health insurance for companies owned by Blackstone, the private equity firm, when Cigna tapped him to help spot savings in its operation, he said.
Insurers have wide authority to reject claims for care, but processing those denials can cost a few hundred dollars each, former executives said. Typically, claims are entered into the insurance system, screened by a nurse and reviewed by a medical director.
For lower-dollar claims, it was cheaper for Cigna to simply pay the bill, Muney said.
“They don’t want to spend money to review a whole bunch of stuff that costs more to review than it does to just pay for it,” Muney said.
Muney and his team had solved the problem once before. At UnitedHealthcare, where Muney was an executive, he said his group built a similar system to let its doctors quickly deny claims in bulk.
In response to questions, UnitedHealthcare said it uses technology that allows it to make “fast, efficient and streamlined coverage decisions based on members benefit plans and clinical criteria in compliance with state and federal laws.” The company did not directly address whether it uses a system similar to Cigna.
At Cigna, Muney and his team created a list of tests and procedures approved for use with certain illnesses. The system would automatically turn down payment for a treatment that didn’t match one of the conditions on the list. Denials were then sent to medical directors, who would reject these claims with no review of the patient file.
Cigna eventually designated the list “PXDX” — corporate shorthand for procedure-to-diagnosis. The list saved money in two ways. It allowed Cigna to begin turning down claims that it had once paid. And it made it cheaper to turn down claims, because the company’s doctors never had to open a file or conduct any in-depth review. They simply denied the claims in bulk with an electronic signature.
“The PXDX stuff is not reviewed by a doc or nurse or anything like that,” Muney said.
The review system was designed to prevent claims for care that Cigna considered unneeded or even harmful to the patient, Muney said. The policy simply allowed Cigna to cheaply identify claims that it had a right to deny.
Muney said that it would be an “administrative hassle” to require company doctors to manually review each claim rejection. And it would mean hiring many more medical directors.
“That adds administrative expense to medicine,” he said. “It’s not efficient.”
But two former Cigna doctors, who did not want to be identified by name for fear of breaking confidentiality agreements with Cigna, said the system was unfair to patients. They said the claims automatically routed for denial lacked such basic information as race and gender.
“It was very frustrating,” one doctor said.
Some state regulators questioned Cigna’s PXDX system.
In Maryland, where van Terheyden lives, state insurance officials said the PXDX system as described by a reporter raises “some red flags.”
The state’s law regulating group health plans purchased by employers requires that insurance company doctors be objective and flexible when they sit down to evaluate each case.
If Cigna medical directors are “truly rubber-stamping the output of the matching software without any additional review, it would be difficult for the medical director to comply with these requirements,” the Maryland Insurance Administration wrote in response to questions.
Medicare and Medicaid have a system that automatically prevents improper payment of claims that are wrongly coded. It does not reject payment on medical grounds.
Within the world of private insurance, Muney is certain that the PXDX formula has boosted the corporate bottom line. “It has undoubtedly saved billions of dollars,” he said.
Insurers benefit from the savings, but everyone stands to gain when health care costs are lowered and unneeded care is denied, he said.
Speedy Reviews
Cigna carefully tracks how many patient claims its medical directors handle each month. Twelve times a year, medical directors receive a scorecard in the form of a spreadsheet that shows just how fast they have cleared PXDX cases.
Dopke, the doctor who turned down van Terheyden, rejected 121,000 claims in the first two months of 2022, according to the scorecard.
Dr. Richard Capek, another Cigna medical director, handled more than 80,000 instant denials in the same time span, the spreadsheet showed.
Dr. Paul Rossi has been a medical director at Cigna for over 30 years. Early last year, the physician denied more than 63,000 PXDX claims in two months.
Rossi, Dopke and Capek did not respond to attempts to contact them.
Howrigon, the former Cigna executive, said that although he was not involved in developing PXDX, he can understand the economics behind it.
“Put yourself in the shoes of the insurer,” Howrigon said. “Why not just deny them all and see which ones come back on appeal? From a cost perspective, it makes sense.”
Cigna knows that many patients will pay such bills rather than deal with the hassle of appealing a rejection, according to Howrigon and other former employees of the company. The PXDX list is focused on tests and treatments that typically cost a few hundred dollars each, said former Cigna employees.
“Insurers are very good at knowing when they can deny a claim and patients will grumble but still write a check,” Howrigon said.
Muney and other former Cigna executives emphasized that the PXDX system does leave room for the patient and their doctor to appeal a medical director’s decision to deny a claim.
But Cigna does not expect many appeals. In one corporate document, Cigna estimated that only 5% of people would appeal a denial resulting from a PXDX review.
“A Negative Customer Experience”
In 2014, Cigna considered adding a new procedure to the PXDX list to be flagged for automatic denials.
Autonomic nervous system testing can help tell if an ailing patient is suffering from nerve damage caused by diabetes or a variety of autoimmune diseases. It’s not a very involved procedure — taking about an hour — and it costs a few hundred dollars per test.
The test is versatile and noninvasive, requiring no needles. The patient goes through a handful of checks of heart rate, sweat response, equilibrium and other basic body functions.
At the time, Cigna was paying for every claim for the nerve test without bothering to look at the patient file, according to a corporate presentation. Cigna officials were weighing the cost and benefits of adding the procedure to the list. “What is happening now?” the presentation asked. “Pay for all conditions without review.”
By adding the nerve test to the PXDX list, Cigna officials estimated, the insurer would turn down more than 17,800 claims a year that it had once covered. It would pay for the test for certain conditions, but deny payment for others.
These denials would “create a negative customer experience” and a “potential for increased out of pocket costs," the company presentation acknowledged.
But they would save roughly $2.4 million a year in medical costs, the presentation said.
Cigna added the test to the list.
“It’s Not Good Medicine”
By the time van Terheyden received his first denial notice from Cigna early last year, he had some answers about his diagnosis. The blood test that Cigna had deemed “not medically necessary” had confirmed a vitamin D deficiency. His doctor had been right, and recommended supplements to boost van Terheyden’s vitamin level.
Still, van Terheyden kept pushing his appeal with Cigna in a process that grew more baffling. First, a different Cigna doctor reviewed the case and stood by the original denial. The blood test was unnecessary, Cigna insisted, because van Terheyden had never before been found to lack sufficient vitamin D.
“Records did not show you had a previously documented Vitamin D deficiency,” stated a denial letter issued by Cigna in April. How was van Terheyden supposed to document a vitamin D deficiency without a test? The letter was signed by a Cigna medical director named Barry Brenner.
Brenner did not respond to requests for comment.
Then, as allowed by his plan, van Terheyden took Cigna’s rejection to an external review by an independent reviewer.
In late June — seven months after the blood test — an outside doctor not working for Cigna reviewed van Terheyden’s medical record and determined the test was justified.
The blood test in question “confirms the diagnosis of Vit-D deficiency,” read the report from MCMC, a company that provides independent medical reviews. Cigna eventually paid van Terheyden’s bill. “This patient is at risk of bone fracture without proper supplementations,” MCMC’s reviewer wrote. “Testing was medically necessary and appropriate.”
Van Terheyden had known nothing about the vagaries of the PXDX denial system before he received the $350 bill. But he did sense that very few patients pushed as hard as he had done in his appeals.
As a physician, van Terheyden said, he’s dumbfounded by the company’s policies.
“It’s not good medicine. It’s not caring for patients. You end up asking yourself: Why would they do this if their ultimate goal is to care for the patient?” he said.
“Intellectually, I can understand it. As a physician, I can’t. To me, it feels wrong.”
55 notes
·
View notes
Note
Oh possente latore di konoscenza, ho una domanda.
Il mio percorso di indagine medica è lungi dall'essere vicino a una conclusione, l'equipe medica ha ritrattato la diagnosi di sclerosi multipla e si accingono a inoltrare i dati a una clinica che studia le malattie rare. Nel frattempo, per aiutarmi, vogliono sottopormi a una terapia immunosoppressiva (visto che in fase acuta aveva portato benefici).
Quello che mi chiedo, da persona ignorante, è se vaccinarmi contro influenza e covid abbia una qualche efficacia, se non proprio se abbia senso o meno.
Probabilmente la risposta è ovvia ma ultimamente il ragionamento logico non riesco ad applicarlo a me stesso.
Non così ovvia, purtroppo.
Ribadendo un concetto che giustamente sfugge a chi crede che il sistema immunitario siano solo i ciccio-poliziotti bianchi di 'Siamo Fatti Così - Esplorando il corpo umano'

(In realtà è più una roba tipo questa di Cell at Work!)
Non è che se prendi farmaci immunosoppressori automaticamente ti becchi ogni canchero che c'è in giro.
D'altro canto, però, non è detto che l'equipe che ti ha in carico salti di gioia a pensare che il tuo organismo entri in contatto con una sostanza immunostimolante specifica (il vaccino) proprio quando sta cercando di indurti farmacologicamente una condizione contraria cioè tenere a bada il tuo sistema immunitario che per cazzi suoi ha deciso che il suo peggiore nemico era la guaina mielinica dei tuoi nervi.
O magari, proprio al contrario, l'equipe ti cazzia perché ti devi vaccinare il prima possibile.
Dipende... e, ovviamente, dipende dalla loro preziosa valutazione in scienza, coscienza e diligenza.
Un abbraccio ed esigo aggiornamenti dettagliati su telegram :)
12 notes
·
View notes
Note
Salve doc. Come mai quando torno a mangiare verdure mi si riempie la pancia di aria ed inizio a soffrire di flatulenza? Troppe fibre, intestino irritabile? Come posso risolvere, diminuendo le porzioni? I fermenti lattici (da supermercato) aiutano? Grazie e scusi se le ho fatto troppe domande.
chiedi "come mai" e io ti rispondo citandoti: "quando torno a mangiare verdure".
Non sono un medico e la diagnosi la lascio volentieri a loro, prendi le mie parole come pura impressione personale senza nessun tipo di valenza sulla tua salute:
hai il microbiota intestinale a pu***ne.
I microrganismi che vivono nel tuo intestino si cibano di quello che gli dai da mangiare. Alcuni microrganismi preferiscono certi tipi di alimenti, altri ne preferiscono altri. Un basso apporto di fibre porta a far crescere una flora intestinale poco avvezza ad esse, con la conseguenza che quando arrivano quantità superiori di fibre, questi producono quantità di gas tali da risultare fastidiosi.
Dato il "quando torno a mangiare verdure", è possibile che tu non mangi verdure spesso, o in generale le tue fonti di fibre siano scarse, o quantomeno monotone. Ecco quindi che i tuoi batteri e lieviti e tutto il bel firmamento del micromondo intestinale è stato selezionato da una vita povera di fibre, e quando le incontra reagisce schifato spruzzandogli del gas repellente addosso (più o meno... diciamo che questa cosa è uno spunto per chi volesse rifare le puntate di Siamo Fatti Così).
Chi mangia tante fibre invece ha un intestino e una flora intestinale allenati alla quantità e alla qualità diversa delle fibre, quindi ha meno problemi di gas. In soldoni: non esiste un vegano gonfio (anche questa è un'iperbole).
Come si risolve?
Sì, vari fermenti lattici possono aiutare, ma devono essere accompagnati da un cambio di dieta che preveda un apporto costante e gradualmente crescente di fibre. Costante significa che devono essere assunte più volte al giorno, gradualmente crescente significa che se esageri all'inizio ti senti male, quindi è meglio se ci vai piano per un po', per poi abbondare sempre di più.
Consiglio: visita medica per escludere patologie, visita dal nutrizionista per sistemare le fibre, acquisto di un passino manuale per poter passare i chicchi di legumi e separarli comodamente dalla pellicina, per diminuire un po' le fibre assunte con essi.
Fonti di fibre: cereali (soprattutto integrali), legumi (più con pellicina che decorticati), frutta, verdura, frutta secca. Le verdure cotte ti fanno mangiare più fibre nell'unità di spazio perché sono più compatte di quelle crude, quindi è più facile mangiarne di più. Vacci piano, soprattutto all'inizio.
4 notes
·
View notes
Note
Hi hi im starting to question if i have depersonalization disorder? My body feels present but my mind isnt? Idk how to explain my mind is always fuzzy and i have bad memory it also feels like im not myself but i get random snaps of reality? Idk im not sure its starting to mess w me and idk who to ask bc i dont have a therapist
I just i get some shed of light^^ thank u for reading!
Hi hello! :33
Well, we understand depersonalization as a symptom which can be an aspect of a bunch of different mental illnesses! We don’t really know about specifically depersonalization disorder… do you mean maybe DPDR (depersonalization/derealization) disorder?
Depersonalization can be a symptom in a lot of different illnesses. Um, we can’t diagnose you and we won’t ever claim to! But we can pass along some info and resources on DPDR disorder and depersonalization specifically so you can do your own research!!
(Gonna plug our own infographic on depersonalization vs. derealization!)
Um, as far as we understand, having a bad memory isn’t necessarily a sign of depersonalization in and of itself. There’s a bunch of reasons why someone might feel foggy, hazy, and fuzzy and have poor memory or lots of memory issues! >w<
We know you said you currently don’t have a therapist, but if your symptoms are starting to cause you distress, it may be time to look into finding one! Let us know if you need help, and if you tell us the country you live in, we can try to help you find links to therapy resources in your area!! Therapy is really really important for folks struggling with all sorts of mental illnesses. We’re not saying therapy works for everyone 100% of the time, but if you haven’t already brought your concerns up to a therapist, it may be a good idea to do so! :3
Good luck with everything! We personally know how scary it can be to grapple with symptoms of mental illness without support or answers as to what you’re going through >_<” but we hope you’re able to find the support you need very soon!
💚 Ralsei and 🌸 Margo
10 notes
·
View notes
Text
La sindrome di Stendhal
chiamata anche sindrome del viaggiatore o sindrome dell'arte, è un fenomeno psicofisiologico che può verificarsi in individui particolarmente sensibili di fronte a opere d'arte o a situazioni di grande bellezza estetica. Prende il nome dallo scrittore francese Stendhal, che descrisse l'esperienza durante una visita a Firenze nel 1817.
I sintomi della sindrome di Stendhal possono includere vertigini, tachicardia, confusione mentale, palpitazioni, senso di svenimento, euforia o, al contrario, ansia e panico. Questi sintomi possono essere provocati dalla sovrastimolazione sensoriale e dalla forte emozione suscitata dall'esperienza artistica.
Non è una condizione clinica riconosciuta ufficialmente come disturbo psicologico, ma viene considerata un'esperienza transitoria. Tuttavia, in alcuni casi estremi, possono essere necessarie cure mediche o psicologiche per gestire i sintomi.
La sindrome di Stendhal è un termine colloquiale usato per descrivere una reazione intensa a opere d'arte, ma non è una diagnosi medica formale. È importante consultare un professionista sanitario qualificato per una valutazione accurata di eventuali sintomi o disturbi che si possano manifestare.
2 notes
·
View notes
Text
Qual è la storia dietro le sindromi da morte improvvisa?
Quando studi la storia della medicina, osserverai spesso che la natura della malattia cambia completamente a seconda dell’epoca e questi lati dimenticati della medicina …
Source: 17 ago 2022; by A Midwestern Doctor on The Forgotten Side of Medicine
(more…)
View On WordPress
#Anthony Fauci#Approcci Terapeutici#Arresto Cardiaco#Arseniato Piombo#Atleti#Autismo#Autorità Sanitarie#Bias Conferma#Brevetti#Cambiamenti#Cambiamenti Clinici#Cardiomegalia Ipertrofica#Censura#Classificazione#Danno Cerebrale#DDT#Diagnosi#Diagnosi Medica#Distrofia Genere#Disturbo#Effetti Collaterali#Farmaci#Fibromialgia#Herpes Zoster#HIV#Ictus Pediatrici#Infezioni Gravi#Justin Bieber#Malattia 11 Settembre#Malattia Aggressiva
2 notes
·
View notes
Text
Have you ever thought, "man, I have too many doctor's appointments every year!" Want to inject some extra uncertainty into moving to a new city? Are you sick of having all of that medication just lying around for you to take?
Try the American Healthcare System™!
In just a few easy steps, you too can experience the thrills and chills of not knowing whether you get medication this month:
- Move to a new city!
- Wait 4 months for your benefits to kick in, and get the privilege of paying a tenth of your paycheck after taxes for the company health insurance plan!
- Hope your med refills won't run out, because your doctor from your hometown 3 hours away won't prescribe refills unless you see him in person, for some reason!
- Go through a list of doctors from the company's insurance that they decide they'll cover... Partially, of course. What, you didn't think the people you're paying to cover your health expenses would cover all of them, did you? Better hope that they cover a doctor that doesn't tell you to go outside instead of prescribing antidepressants!
- Call the local hospital and ask for an appointment. The closest one is two weeks out, but you should be able to make it that long if you underdose your medication. You'll feel like shit, but at least it'll stave off SSRI withdrawal.
- The insurance info your employer gave you wasn't enough for the hospital to confirm you have it. You can't book the appointment.
- Go to HR the next day. They email you more info. Call the hospital again, give them every bit of info from your insurance, and it still won't show up in their system. The insurance company must have not updated their records. The hospital says they'll call you back tomorrow after they contact the insurance company. You smile and say it's no problem. you have twenty-one days of medication left.
- you have twenty days of medication left.
- You get a call back from the hospital. They say the appointment you were booked for before is taken now. The closest appointment is 27 days away. You check that the doctor it's with is covered by your insurance and take it. you have nineteen days of medication left.
- you have eighteen days of medication left. You don't need to take your meds on the weekend, right? You can tough it out. You got good at fighting off the suicidal thoughts when you were a teenager. You hope you've still got it.
- you have seventeen days of medication left. you've felt more tired since you started underdosing. you feel awake. you just can't bring yourself to do anything. why bother.
- you have seventeen days of medication left. it's the weekend. no meds today. you lay in bed and try to ignore the nausea and aches. nothing got done today. you wonder if anything will ever get done in your life. you wonder what the point is if you'll never get anything done.
- you have seventeen days of medication left. still the weekend. no meds. you eat to try and give some feeling to your stomach besides nausea. you keep eating. it's free serotonin, as long as you don't mind the fact that it's making you fatter and uglier with every bite. you mind. you play video games until 1 in the morning to try and distract yourself. you have to get up at 7 tomorrow.
- it's monday. you're tired, but at least you got to take your meds that day. your boss asks if you've been doing okay. you force a smile and say you're fine. you're pretty sure he doesn't care about you anyway, just like everyone else. you have sixteen days of medication left.
- you wonder if the doctor will believe you have adhd. you hope he does. you have a diagnosis, but it wouldn't be the first time someone has denied you treatment because you look "too normal." you have fifteen days of medication left.
- you forgot to turn off the lights when you left the house today. your roommate asked you politely to remember to turn them off to keep the electric bill down. you're positive he hates you. you have fourteen days of medication left.
- you have thirteen days of medication left.
- you have twelve days of medication left
#vent writing#depression#american healthcare#american health insurance#health insurance#cw: suicide mention#cw: depression#vent#cw sui thoughts
3 notes
·
View notes
Text
Diet and cure are need constantly.
My grandchildren is on 1.5 y.old , her body covered with red spots and pimples, they are itching, she is wordiness and nervousness.Doctor put diagnosis as atopic dermatitis, allergy to the protein in cow milk, and failure for ferments a digestion system.All milk products avoided, effect is zero, ointments are not helping, relieving not beginning, disease is keeping, advice to her something, please.
A children with atopic dermatitis are constantly checking in dermatologists, and pediatrist and receive supporting cure as for preventing a recidive a disease answers dermatologist Kuleshov, and constantly keeping these recommendations:
1.Using hypo-allergy diet with limiting animal fats, sea meal, smoked,spicy, salted and marinades, eggs, nuts, honey.
2. Limiting contact with water and items of household chemicals.
3. In household carrying are elimination/avoiding contact with allergen/activities.
Everyday house cleaning, wetting.
Minimal quantity at home are soft furnitures, carpets.
Using pillows with filling of synthetic materials.
Removing at home a tick dust.
Avoiding a children skin s contact with woollen fur fabrics.
At home, removing abundant humidity and sources for mold on the wall.
Avoiding contact with home animals.
Limiting using synthetic washing items.
4.And using for preventing and on acuting time or long time for till 30 days and more on rashes of atopic dermatitis as for medicament cure are creams Bepanthen, Panthenol, or vitamin F99 for two times/day, if doctor allows and cream Protopin for one time/day for 3 months, concrete remedy selecting individually by skin peculiarity, season, climate, time of a day, and patient s preferences.
5.Using for base care a skin softening and moisturizing remedies/Emollients as of lotions, creams, ointments, they are fighting dryness, itch, inflammation skin, and common recommendations by using: Self using, after water procedures by principle to wet-grease, and bathe baby at warm on 27-30 C bath for 5 min with adding for 2 min till procedure ending a oil for bath and apply on wetting skin, and wipe her needing after bath by blotting moves, avoiding friction a softening remedy.
On the colt time a year use softening and moisturizing remedies with a most oily ingredients.
Emollient as of cream apply for 15 min, or in 15 min after using a anti-inflammatory preparation/in a case more oilyness base a Emollient .
from Valga s health news,gardening,and cooking ,and beauty . https://ift.tt/5bGIeQz
via https://ift.tt/YifrK3L
0 notes
Text
ARRIVA LA TERAPIA PER IL TUMORE AVANZATO DEL FEGATO
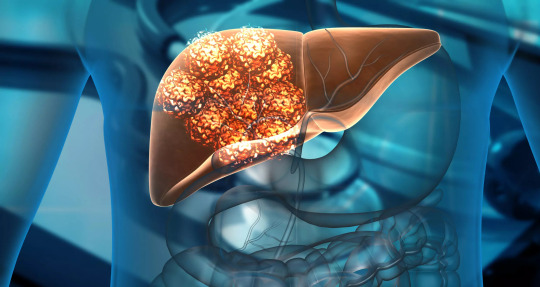
Una rivoluzionaria cura in grado di prolungare la vita dei pazienti con la forma più comune di tumore del fegato, il carcinoma epatocellulare.
L’Agenzia Italiana del Farmaco (Aifa) ha approvato due nuovi farmaci che riescono a ridurre del 42% il rischio di morte per i pazienti in stadio avanzato o non operabili. L’Atezolizumab e il Bevacizumab rendono meno letale le manifestazioni tumorali causate dell’epatite B e C, da cirrosi e altre malattie del fegato non operabili per cui solo un quinto dei pazienti è vivo a cinque anni dalla diagnosi.
“Sono i dati migliori finora ottenuti nella storia della terapia dell’epatocarcinoma e sono confortanti sotto il profilo di maneggevolezza e tollerabilità con ottimi risultati anche sulla qualità di vita dei pazienti – spiega Fortunato Ciardiello, Ordinario di Oncologia Medica dell’Università degli Studi della Campania Luigi Vanvitelli – L’interazione tra l’immunoterapia e la terapia anti angiogenetica rappresenta il nuovo standard terapeutico in questa categoria di malati”.
L’epatocarcinoma è uno dei tumori più aggressivi e una delle prime cause di decessi oncologici nel mondo. Ogni anno 1,8 milioni di persone muoiono a causa di questa malattia: in Italia, nel 2020 i nuovi casi stimati di tumori epatici sono stati 13.000 dove l’epatocarcinoma rappresenta il 75-85% delle diagnosi. Finora solo il 50% dei pazienti arrivava alla diagnosi quando ancora la patologia era curabile mentre per gli altri l’aspettativa di vita era molto bassa.
____________________
Fonte: Agenzia Italiana del Farmaco; Università di Trieste; Cancers; Roche

✔ VERIFICATO ALLA FONTE | Guarda il protocollo di Fact checking delle notizie di Mezzopieno
✖ BUONE NOTIZIE CAMBIANO IL MONDO | Firma la petizione per avere più informazione positiva in giornali e telegiornali
Se trovi utile il nostro lavoro e credi nel principio del giornalismo costruttivo non-profit | sostieni Mezzopieno
2 notes
·
View notes
Text
Risarcimento per Danno Medico, chi può richiederlo?
Il risarcimento per danno medico rappresenta un tema delicato e di rilevante importanza nel contesto del diritto civile e della tutela della salute in Italia.

In questo documento, esamineremo in dettaglio la natura del danno medico, il processo attraverso il quale si può richiedere un risarcimento, e chi sono i soggetti legittimati a farlo.
Il tono sarà professionale, con l'obiettivo di fornire informazioni precise e basate su dati e normative vigenti.
Cosa è il Danno Medico?
Il danno medico si verifica quando un paziente subisce lesioni fisiche, psichiche o un deterioramento delle condizioni di salute a seguito di un trattamento sanitario non conforme agli standard di cura attesi.
Questo include errori di diagnosi, errori in interventi chirurgici, trattamenti inappropriati, mancanza di consenso informato, e ogni altra forma di negligenza medica.
Tipologie di Danno
Danno fisico: Qualsiasi lesione che impatti l’integrità fisica del paziente.
Danno morale: Sofferenze psicologiche e disagio emotivo derivante dal trattamento medico.
Danno biologico: Compromissione permanente o temporanea delle capacità funzionali dell’individuo.
Danno estetico: Cambiamenti nell'aspetto esteriore che possono influenzare la percezione di sé e le relazioni sociali.
Come Funziona il Risarcimento?
Il risarcimento per danno medico si basa su principi di responsabilità civile.
Il paziente (o i suoi eredi) deve dimostrare che il danno subito è diretta conseguenza di un trattamento medico che non ha rispettato i le regole dell'arte medica.
Fasi del Processo di Richiesta
Consulenza medico-legale: È fondamentale acquisire un parere da parte di un consulente tecnico, che possa attestare la sussistenza del nesso causale tra il trattamento e il danno.
Raccolta della documentazione: Documentazione medica, testimonianze, e qualsiasi altro elemento utile a supportare la tesi del paziente.
Notifica e negoziazione: Spesso si cerca un accordo extragiudiziale con la struttura sanitaria o il professionista coinvolti.
Azione legale: Se non si raggiunge un accordo, sarà necessario intraprendere un'azione legale, per cui è consigliabile l'assistenza di un avvocato specializzato in malpractice medica.
Chi può Richiedere il Risarcimento?
Il risarcimento può essere richiesto da:
Il paziente direttamente danneggiato: La persona che ha subito direttamente il danno a seguito di malpractice.
Gli eredi legali: In caso il danno medico abbia causato la morte del paziente.
Altri soggetti indirettamente danneggiati: Come i familiari che hanno subito un danno morale o psicologico a seguito degli eventi accaduti al paziente.
Quadro Normativo
La legislazione italiana prevede una serie di norme che regolano la responsabilità medica, inclusi il Codice Civile e specifiche leggi che disciplinano la professione medica e la tutela dei diritti dei pazienti.
Inoltre, recenti riforme hanno cercato di chiarire ulteriormente i diritti dei pazienti e le procedure di risarcimento.
Conclusioni
Il percorso per ottenere un risarcimento per danno medico è complesso e richiede una precisa documentazione e spesso l'assistenza legale specializzata.
È essenziale che i pazienti siano consapevoli dei loro diritti e delle procedure da seguire per tutelare la propria salute e integrità.
Le riforme legislative continuano a svilupparsi in questo ambito, mirando a garantire una maggiore trasparenza e giustizia per le vittime di malpractice medica.
0 notes
Note
Ciao! Posso chiederti un parere, please? Mio zio, obeso, forse prediabetico, che non si era mai fatto seguire da medici/professionisti sanitari prima, ha appena visto una nutrizionista. Gli ha detto di fare un'analisi lipodomica. Ora, ho una leggera infarinatura sulle applicazioni cliniche della biochimica, ma dopo qualche ora su Wikipedia prima, e poi su PubMed, non ho ancora capito che senso ha far fare una cosa del genere (molto costosa, che non fanno in ospedale e che non passa la mutua) per una persona che ha ancora fatto nemmeno un test da carico di glucosio.
Che idea ti sei fatto su questa situazione in particolare? E in generale (per curiosità) sai dirmi se davvero, allo stato dell'arte, le analisi lipodomiche possono avere un impatto su diagnosi e terapia di patologie?
Grazie in anticipo. Scusa per la domanda strana.
Ciao, intanto è lipidomica, non lipodomica. Si tratta di un'analisi volta a capire la composizione e la distribuzione degli acidi grassi presenti nell'organismo, con l'intenzione di collegare il risultato di questa analisi a un'interpretazione in chiave antinfiammatoria (più grassi saturi, pochi omega-3, più omega-6, significa più infiammazione)
Personalmente, non ho mai voluto appoggiarmi a questa metodica, perché pur ritenendo l'analisi in sé decisamente interessante, non ne capisco l'applicazione pratica: alla fine, la dieta sarà per forza di cose con le giuste proporzioni dei grassi; quindi, analisi o meno, quei valori si risistemeranno se viene seguita. So di colleghi che la consigliano, e tra le analisi "alternative" è, insieme a quella nutrigenomica, un'analisi interessante. Ma non credo sia utile. Sempre meglio dell'analisi delle intolleranze, comunque.
Infine, ti ricordo che per legge il biologo (dici "nutrizionista", immagino sia una biologa) non può prescrivere analisi né fare diagnosi. Parlando col paziente mi è capitato di chiedere se potesse fare questo o quell'accertamento, ma la mia richiesta è sempre "chieda al medico se anche secondo lui sarebbe utile analizzare X". Perché, appunto, prescrivere analisi come biologo è abuso di professione medica.
Non lo scrivo per farmi pubblicità... anzi sì: dalla prossima settimana partirò ufficialmente con le consulenze online. Così, tanto per dire.
4 notes
·
View notes
Text
Introduction
Poisoning by medical agents refers to the harmful effects caused by the ingestion, inhalation, or injection of medications or other medical substances. This condition can range from mild to severe, depending on the type and amount of ag...
#Mirari #MirariDoctor #MirariColdPlasma #ColdPlasma
0 notes