#monocytosis
Text
Blasts shouldn't be seen in peripheral blood.
Rule out leukemia, myelodysplastic syndrome, chronic myeloid leukemia.
Blasts may be other immature hematopoeitic cells. High monocyte count might actually be blasts, not monocytes.
If auto differential is abnormal, get a manual one.
Blasts newly elevated is more suggestive of acute leukemia. Pancytopenia suggests bone marrow failure. Febrile neutropenia is also concerning.
Make sure pt is stable with vitals, oxygen if needed, fluids.
Rule out emergencies and then contact heme/once.
APL is a subtype of AML. AML has 7 morphological categories using a system called fab. APL is the third subtype, M3. It has unique history and treatment. It presents with DIC and has early mortality. People hemorrhage and die. You can prevent it by giving all trans retinoic acid (ATRA). It helps APL cells differentiate into normal cells. APL is curable. Give all trans retinoic acid (ATRA). Diagnose by looking at source of the tumor cells. Look at peripheral blood smear. It separates ALL from AML. Auer rods are seen in AML. APL cells have multiple auer rods and folded nuclei that are very granulated.
CML has maturation of all the white cells, mature granulocytes, basophilia.
MDS (myelodysplastic syndrome) = elderly pts; hypogranular neutrophils, bilobed neutrophils, red cell shape/size changes (anisopoikilocytosis)*.
Do the peripheral blood smear first. Next do a peripheral blood flow cytometry or cell markers. It classifies cells based on the markers they express. Blasts express CD34. If CD34 is elevated, then the pt has increased blasts.
The definitive test to diagnose acute leukemia is a bone marrow biopsy. AML = more than 20% myeloblasts on bone marrow biopsy. ALL = more than 20% lymphoblasts on bone marrow biopsy.
APL has a characteristic genetic translocation--chromosome 15 and 17.
Before talking to heme/onc, also get bloodwork to rule out DIC (fibrinogen level, INR, PTT, d-dimer). If pt is febrile, work up includes blood culture, chest X-ray, urine culture for febrile neutropenia.
Also get CMP, phosphorus, magnesium, calcium, uric acid level to look for tumor lysis syndrome.
Transfuse platelets if platelets less than 10,000 and bleeding. If symptomatic anemia, transfuse RBCs.
Leukostasis = elevated WBCs such that blood flow to organs is impeded. Immature cells clog up the vasculature. Causes hypoxia, pulm infiltrates, SOB, AMS, HA, dizziness. WBC can be 50 to 100 or even less than that in leukostasis.
Other hematologic emergencies: cauda equina (spinal cord compression) is seen in lymphoproliferative disorders (lymphoma-> mass effect on spinal cord); myeloma (alters bone integrity-> compression fractures). Sometimes myeloma deposits can compress the spinal cord. So assess lower extremity reflexes, tone, Babinski sign, saddle anesthesia, rectal tone, bowel or bladder incontinence.
Top 5 clinical pearls
1) blasts are worrisome in peripheral blood, should not be in peripheral blood. Get heme/onc on board fast.
2) get a manual differential, review the film manually
3) acute leukemia can present with pancytopenia and no circulating blasts, OR with just circulating blasts. So either of those should be explored.
4) if you think the pt has acute leukemia, suspect APL, which is a medical emergency that can be treated with all trans retinoic acid immediately.
5) hematologic emergencies: severe cytopenia, febrile neutropenia, DIC, tumor lysis syndrome, leukostasis, cord compression. So screen for these.
*Anisopoikilocytosis is when you have red blood cells that are of different sizes and shapes.
The term anisopoikilocytosis is actually made up of two different terms: anisocytosis and poikilocytosis. Anisocytosis means that there are red blood cells of varying sizes on your blood smear. Poikilocytosis means that there are red blood cells of varying shapes on your blood smear.
So basically: get a peripheral blood smear, which let's you look at the cells. Flow cytometry can further differentiate the specific cell type that is elevated. Bone marrow biopsy is the definitive way to diagnose.
#heme#AML#APL#CML#febrile neutropenia#blasts#leukostasis#monocytosis#M3#leukemia#all trans retinoic acid#ATRA#Auer rods#Auer rod#hemeonc
3 notes
·
View notes
Text
Infantile cortical hyperostosis – Caffey’s disease
Children under 1 year of age
Etiology: AD or sporadic form – osseous growth spurt during development.Common sites:
Mandible
Clavicle
Scapula
Frontal bone
Ulna
Radiology: Mandibular enlargement, cortical redundancy
Lab:
Anemia
Leukocytosis
↑ ESR
↑Serum alkaline phosphatase.
Monocytosis
Management: Symptomatic
Picture
View On WordPress
0 notes
Photo
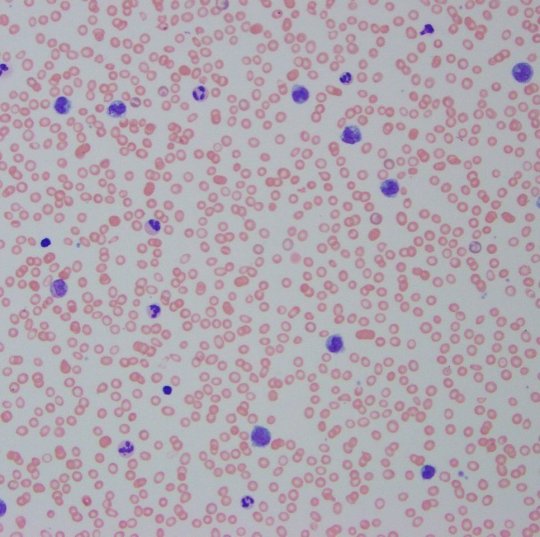
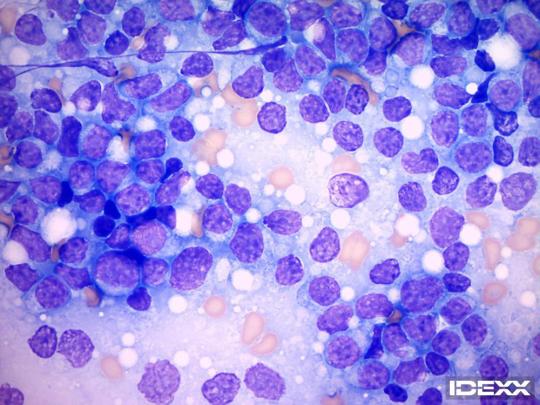
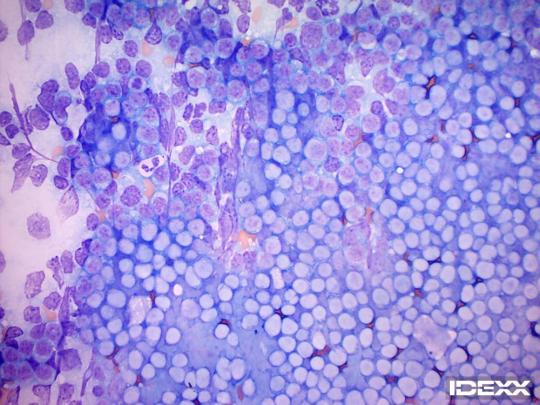
A day in a haemopathologist’s life: CMML In the loving memory of Genesis Breyer P-Orridge - here is a peripheral smear with chronic myelomonocytic leukemia. CMML is defined by the WHO using 5 main criteria: 1. Absolute monocytosis >1000/uL and should be at least 10% of the differential - persistent 2. No evidence of a defined myeloproliferative neoplasm 3. No rearrangement of PDGFRA, PDGFRB, or FGFR1, and no PCM1-JAK rearrangement 4. Blasts less than 20% of differential 5. Dysplasia in at least 1 lineage and/or evidence a clonal genetic abnormality Marrows are usually hypercellular. Blast can lack CD34 and CD117 so immunohistochemistry isn’t always as helpful in looking for blasts in bone marrow biopsies. Need careful morphological assessment. Graded CMML-0 (<2% blasts in blood and <5% in BM), CMML-1 (2-4% blasts in blood and 5-9% blasts in marrow), and CMML-2 (5-19% blasts in blood and 10-19% blasts in marrow) #porridgewitheverything #genesisbreyerporridge I am selling myself here: https://doi.org/10.1182/blood-2003-06-2124 https://www.instagram.com/p/CZfxjdUD1AX6zJuzP3tSjpSEu5MFZ5iE4YDhtw0/?utm_medium=tumblr
4 notes
·
View notes
Text
Monocytes
Monocytes typically make up 2-8% of white blood cells. Monocytopenia can be seen, for instance, if a patient is being immunosuppressed with glucocorticoids. Monocytosis can be seen with inflammatory states such as during viral illness or other stressors like sepsis or surgery, granulomatous disease like sarcoidosis. The rest of this week will be about a condition called Juvenile Myelomonocytic Leukemia (JMML).
3 notes
·
View notes
Text

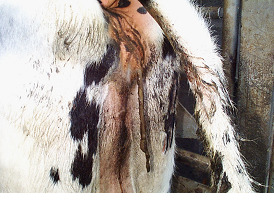
Hey everyone. My dog, Destiny, has been diagnosed with lymphoma 😢 I'm sharing her case study to help future vets/techs and also to help myself process the news. I apologise in advance for the long post since mobile doesn't have a read more options.
• Signalment: 11yo SF mixed breed canine
[Most patients are 4-9 years old at diagnosis; high-risk breeds include boxer, basset hound, golden retriever, Saint Bernard, Scottish terrier, Airedale terrier, and bulldog]
• History: History of roundworms and whipworms as a young puppy. HBC without serious injuries at 5mo. Spayed at 6m. Had a benign skin growth removed a few years ago. Tooth root abscess dx'd on May 27, 2020 and treated with Carprofen and Ciprofloxacin, responded well to tx. Finished medications on 6/3/20. UTD on vaccines and parasite prevention.
Starting 6/4/20, Mom noticed Destiny having a decreased appetite and increased thirst. She had 1 instance each of vomiting and diarrhea. Otherwise she was behaving normally.
On 6/6/20 Destiny woke her up very early with an episode of dyspnea and anxious vocalizing. While trying to calm her down, Mom felt a hard lump under her neck. Mom immediately called me and sent me video of her breathing. After she'd been awake for a few minutes, the episode subsided, but it returned whenever she tried to sleep. Her MM stayed pink. I called Doc and forwarded the video, and she decided Destiny needed seen right away.
When I picked her up from Mom's, I felt under her neck and my heart sank. Her submandibular lymph nodes were the same size and hardness as a baseball. I've only had 2 cases where the lymph nodes felt like that and it was *not* lymphoma (one was a severe erhlichiosis and the other was an autoimmune condition).
• Physical Exam: Moderate POD present. She had bilateral enlargement of her submandibular, prescapular, and politeal lymph nodes [I'm bad at palpating lymph nodes; if I can feel them, it's Not Good]. Otherwise PE was unremarkable. After returning to her kennel, she vomited water and stomach fluid.
• Diagnostics: We ran an Idexx 4dx SNAP test, which was negative. We also drew blood for a CBC and Chemistry panel, and I did a FNA of 3 different lymph nodes. We sent the samples out to Idexx for analysis.
• Treatment plan: Since an oncologist referral isn't in the cards for us, we started her on the palliative prednisone dose recommended by the oncologist, doxycycline in case it was a tick disease not covered by the 4dx, and Cerenia for the vomiting and diarrhea. We also put her on a bland diet.
• Diagnostic results:
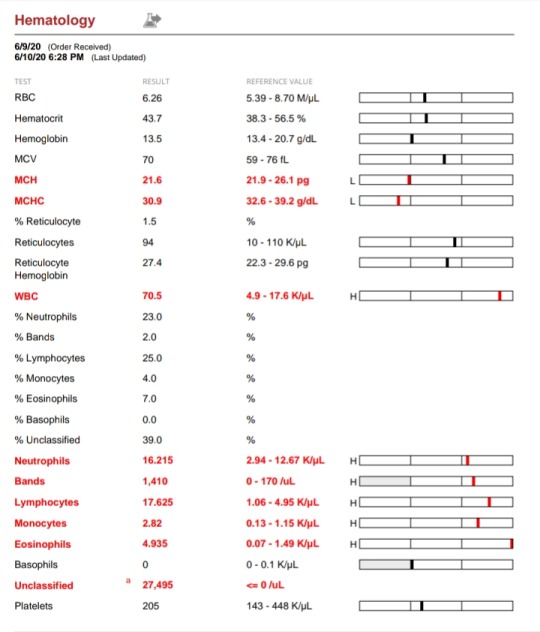
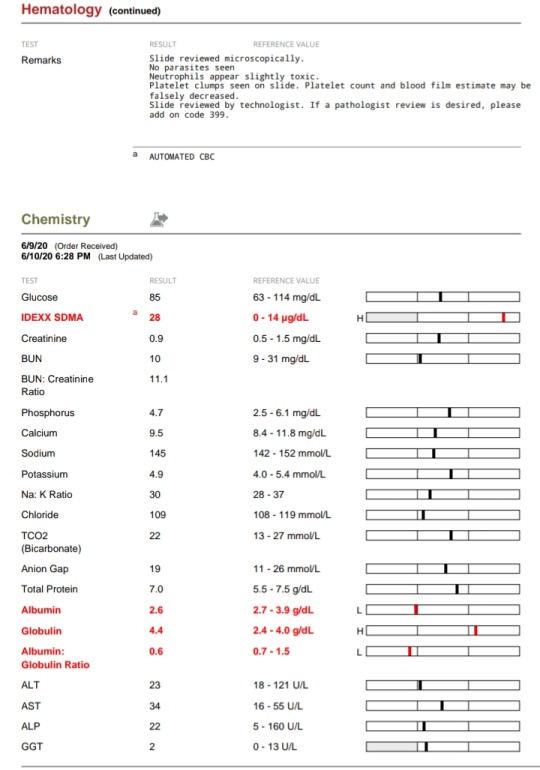
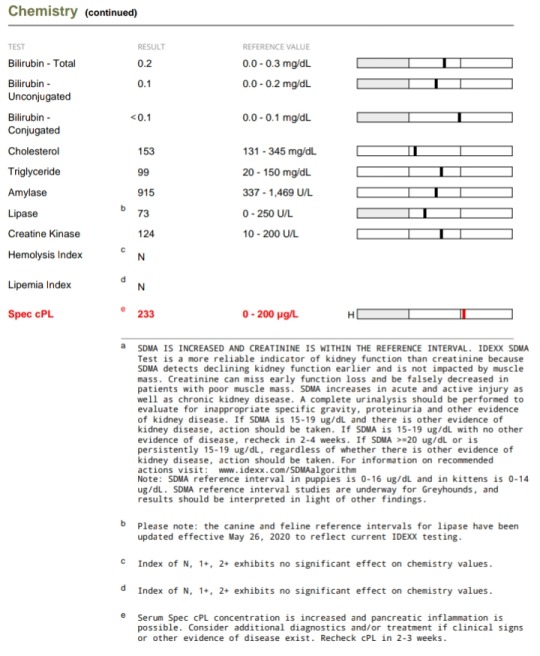
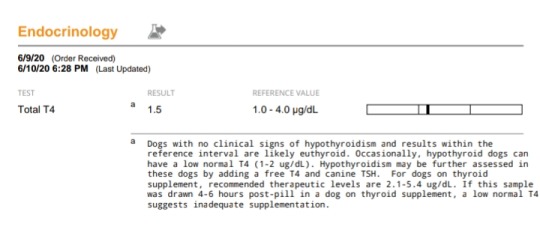
Taken together, especially in light of her clinical signs, her bloodwork abnormalities point further toward a diagnosis of lymphoma:
- A very high WBC count
- Neutrophilia
- Large #s of band cells, indicating an increased demand for neutrophils
- Lymphocytosis
- Monocytosis
- Eosinophilia
- Hyperglobulinemia (can be caused by lymphoma or by chronic infection, like POD)
- decreased albumin:globulin ratio (due to decreased albumin with an increase in globulins)
- The increased SDMA could also be due to lymphoma, or it could just be a response to the course of NSAIDs she recently finished, as well as a few other causes that are less likely in her case.
- Hypoalbuminemia can be due to increased losses through the intestines or into tissue, or due to inappetence
- MCH and MCHC can decrease due to low albumin
- High specCPL indicates something has upset the pancreas; it could be a low-level pancreatitis due to table scraps or it could be a secondary result of inflammation caused by a primary disease.
However, the FNA results provided the definitive diagnosis of lymphoma:
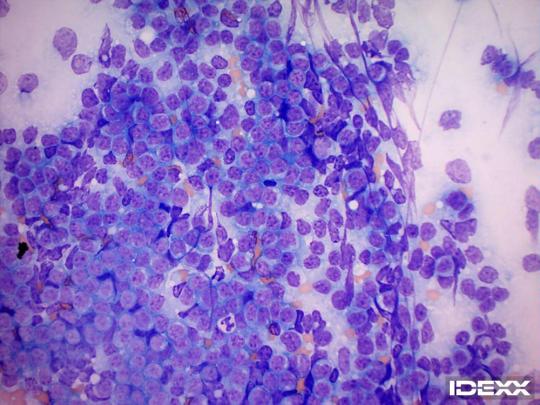
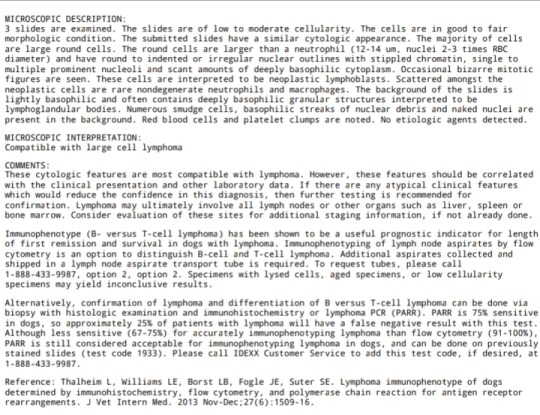
We are going to continue Destiny on palliative care until her quality of life diminishes, and then we'll put her to sleep. Because it depends on the type of lymphoma and her response to the disease and palliative medication, it may only be a week, or it may be a few months. Doc has seen 1 dog go into remission with pred alone, but it's very unlikely. We're preparing for the worst and will just be grateful if we get more good time with her 💔
#Destiny#my pets#dog#lymphoma#cancer#canine lymphoma#sad#emotions#veterinary#vet tech#diagnostic testing#FNA#personal#palliative care
26 notes
·
View notes
Photo
Children, Click, and Dogs: JASMINE IDH 46109 11 vr old Sweet Senior has lots of love to give! Playful and Affectionate & out of time ...57 lbs TO BE KILLED 11/10/18 Meet Jasmine! This gorgeous older lady needs a forever home @MACC - Sweet Seniorgirl has lots of love to give Playful, Affentionate & Out of time...please watch Jasmine's Video and step up before its to late. A volunteer writes: Jasmine is a very enjoyable dog to spend time with. She is so pretty, foxy like, an 11 year old golden gal so happy to be with a friend and play ball in the yard. Jasmine is full of good energy, running, jumping and catching tennis balls. She sits for treats or a toy, bright eyed and tail wagging, her face full of anticipation. After a while going back and forth after a ball, Jasmine comes to rest by my feet for caresses. She is a good walker, likely house trained and seems fine with dogs neared in the street. In our playgroups, she appears to prefer calm dogs. Jasmine is waiting at the Manhattan Care Center for a new leash on life. Will you be the one opening your door and your heart to this lovely and spunky senior? VIDEOS : <3 Spry Jasmine https://www.youtube.com/watch?v=QhPn96kUMHs Playgroup https://www.youtube.com/watch?v=-PQwrKIScdY Jasmine ID# 46109 MANHATTAN ANIMAL CARE CENTER Age: 11 years old Female, Is Vaccinated: Yes, Brown /Black , Weight: 57 lbs. , Intake Date: 10-31-2018 SHELTER ASSESSMENT ~ ADULT ONLY HOME No children (under 13) BEHAVIOR NOTES: Means of surrender (length of time in previous home): Owner Surrender (In home for 11 years) Previously lived with: An adult and a dog Behavior toward strangers: Friendly Behavior toward children: Pulls towards them, owner stated she was dangerous around them but did not detail why Behavior toward dogs: Friendly Resource guarding: None reported Bite history: None reported Housetrained: Yes Energy level/descriptors: Jasmine is described as affectionate and playful with a high level of activity. Other Notes: Jasmine will snap at bikes that pass by. Jasmine is reported to have been destructive in her previous home, ripping up furniture. SAFER SCORES: Date of assessment: 1-Nov-2018 Look: 1. Dog's eyes are averted, with tail wagging and ears back. Allows head to be held loosely in Assessor's cupped hands. Sensitivity: 1. Dog leans into the Assessor, eyes soft or squinty, soft and loose body, open mouth. Tag: 1. Dog follows at the end of the leash, body soft. Paw squeeze 1: 1. Dog gently pulls back his/her paw. Paw squeeze 2: 1. Dog gently pulls back his/her paw. Flank squeeze 1: Item not conducted Flank squeeze 2: Item not conducted Toy: 1. Minimal interest in toy, dog may smell or lick, then turns away. Summary: Jasmine approached the assessor with a soft body. She was social throughout the assessment, allowed all handling, and displayed no concerning behaviors. Summary (1): 11/1: When introduced off lash to dogs Jasmine greets politely, engages in brief play. She offers correction for mounting. Summary (2): 11/2: Jasmine is anxious and paces the yard, ignoring the other dogs. Summary (3): 11/4: Jasmine rushes over to the helper dog with a stiff body and stands over his back. She then anxiously paces the pen and seeks exit. Date of intake: 31-Oct-2018 Summary: Tense, whining, pacing ENERGY LEVEL: Jasmine is described as having a high level of activity. We recommend long-lasting chews, food puzzles, and hide-and-seek games, in additional to physical exercise, to positively direct her energy and enthusiasm. BEHAVIOR DETERMINATION: ADULT ONLY HOME Recommendations: No children (under 13) Recommendations comments: No children: Jasmine's previous owner reported that she was "dangerous" with children, but gave no specifics as to what this meant. Out of an abundance of caution, we recommend an adult only home. Potential challenges: Destructive behavior On-leash reactivity/barrier frustration Potential challenges comments: Destructive behavior: Jasmine is reported to show destructive behavior in the home, such as chewing on furniture. We are unaware of what, if any, attempts were made to remedy this behavior but we suggest to future adopters that Jasmine will need to be provided with physical and mental stimulation and with a variety of appropriate and engaging chew toys so she can engage in necessary chewing behavior without damage to human objects. On-leash reactivity/barrier frustration: Jasmine is reported to lunge and snap at bike while on leash and to lunge at children. Jasmine may need positive reinforcement, reward based training to teach her to look at you rather than other dogs. We recommend a front clip harness or head halter to help manage this behavior. MEDICAL EXAM NOTES 4-Nov-2018 Blood Work Interpretation Vet Notes: 4:18 PM CBC - lymphopenia 0.85 (1.05-5.1), monocytosis 1.23 (0.16-1.12) - pattern suggestive of stress leukogram CHEM - All parameters were within the reference range. 4-Nov-2018 DVM Intake Exam Estimated age: 11 yo Microchip noted on Intake? Yes Microchip Number (If Applicable): 0A10657603 History : Owner surrender Subjective: Observed Behavior - Cat reactive Evidence of Cruelty seen - No Evidence of Trauma seen - No Objective T = NT P = 120 bpm R = eupneic BCS 6/9 EENT: corneas and anterior chambers OU, mild ceruminous AU, no nasal or ocular discharge noted Oral Exam: Limited oral exam due to muzzle, dental calculus and gingivitis noted, worn PLN: No enlargements noted H/L: Grade 4/6 left systolic heart murmur, NSR, CRT <2 sec , Lungs clear, eupnic ABD: Non painful, no masses palpated U/G: Grossly normal castrated female, no vaginal discharge. Spay scar noted on ventrum. MSI: Ambulatory x 4, skin free of parasites, no masses noted, healthy hair coat. Excoration noted on nasal planum. CNS: Mentation appropriate - no signs of neurologic abnormalities Rectal: Externally clean Assessment 11 yo FS MBD Grade 4/6 left systolic heart murmur Nasal excoriation - r/o: secondary to trauma (rubbing) vs. other Prognosis: Good Plan: Recommend 2-view chest rads and echocardiogram Recommend TAB topically on nasal planum SID x 7d Recheck nasal planum in 7d SURGERY: Already spayed * TO FOSTER OR ADOPT * HOW TO RESERVE A “TO BE KILLED” DOG ONLINE (only for those who can get to the shelter IN PERSON to complete the adoption process, and only for the dogs on the list NOT marked New Hope Rescue Only). Follow our Step by Step directions below! PLEASE NOTE – YOU MUST USE A PC OR TABLET – PHONE RESERVES WILL NOT WORK! * STEP 1: CLICK ON THIS RESERVE LINK: https://newhope.shelterbuddy.com/Animal/List Step 2: Go to the red menu button on the top right corner, click register and fill in your info. Step 3: Go to your email and verify account \ Step 4: Go back to the website, click the menu button and view available dogs Step 5: Scroll to the animal you are interested and click reserve STEP 6 ( MOST IMPORTANT STEP ): GO TO THE MENU AGAIN AND VIEW YOUR CART. THE ANIMAL SHOULD NOW BE IN YOUR CART! Step 7: Fill in your credit card info and complete transaction HOW TO FOSTER OR ADOPT IF YOU CANNOT GET TO THE SHELTER IN PERSON, OR IF THE DOG IS NEW HOPE RESCUE ONLY! You must live within 3 – 4 hours of NY, NJ, PA, CT, RI, DE, MD, MA, NH, VT, ME or Norther VA. Please PM our page for assistance. You will need to fill out applications with a New Hope Rescue Partner to foster or adopt a dog on the To Be Killed list, including those labelled Rescue Only. Hurry please, time is short, and the Rescues need time to process the applications.
1 note
·
View note
Video
TO BE KILLED SATURDAY DECEMBER 4, 2021 AT 12PM & MUST BE PULLED BY A NEW HOPE PARTNER RESCUE: Euthanasia Rate For Nikki: High: She Could Be Killed Before Noon On Saturday Depending On Her Health: Hello, my name is #Nikki. My animal id is #ID130805. I am a desexed #female orange tabby/ white #cat at the Staten Island Animal Care Center. The shelter thinks I am about 12 years 2 weeks old. I came into the shelter as a owner surrender on 11/18/2021, with the surrender reason stated as person circumstance- owner elderly. Sorry, this pet is for new hope partners only. #130805: Nikki is a declawed senior cat who is being placed on the Emergency Placement List for advanced medical conditions that need to be addressed quickly by anyone who is willing to pull her for placement. Nikki has kidney disease and severe anemia that is progressing. Nikki will need to be seen by a specialist upon placement. Behaviorally Nikki has lived in a home with older adults and is generally shy but has shown some fear in the care center. This has caused her to hiss, growl, lunge and charge. What my friends at ACC say about me: I have never lived with other animals or children. I would do best in a home with only adult humans. I have medical needs that staff will address with you when you meet me. I am finding the shelter a bit overwhelming. I can be slow to adjust to new environments. I prefer to take things at my own pace. I would appreciate slow introductions to new people and places to help me feel safe. I'm sensitive and shy. I'll need extra help from you. I will flourish in a calm environment and a low-traffic home. I am looking for a home with a patient person. Observed Behavior - hissing, growling, swatting, biting at glove severe anemia (hematocrit= 15.5)- R/O renal disease vs neoplasia vs other mild neutrophilia and monocytosis- R/O stress vs infection vs inflammation vs neoplasia vs other eosinophilia- R/O parasites vs allergies vs other #AllAboutSavingAnimals: #NYCACC: #catsofinstagram: #Rescue: #NewHopePartner: #Donate: #Pledges: #StatenIsland: #NY: #NYC: #Sponsor: #Foster: #Video: #Animation: #cats_of_instagram: #catsofig: #Brooklyn: #Manhattan: (at Staten Island, New York) https://www.instagram.com/p/CXAD6lhDJs7/?utm_medium=tumblr
#nikki#id130805#female#cat#130805#allaboutsavinganimals#nycacc#catsofinstagram#rescue#newhopepartner#donate#pledges#statenisland#ny#nyc#sponsor#foster#video#animation#cats_of_instagram#catsofig#brooklyn#manhattan
0 notes
Text
Juniper Publishers- Open Access Journal of Case Studies

Low Serum Ferritin Probably Independent Risk Factor for Gallstones Formation - Case Study
Authored by Walaa Fikry Elbossaty
Abstract
Iron deficiency anemia is one of the most popular types of anemia in the Middle East, which is characterized by a severe deficiency in the proportion of hemoglobin and ferritin. The prevalence of iron deficiency anemia in women increases more than men, as they are more likely to lose blood. It was found that there is a relationship between the rate of iron deficiency and the development of gallstones. This is due to many vital processes in which iron contributes as a catalyst for some vital enzymes or influences rates of liver enzymes that have an effective role in the process of stone formation.
In this study we tried to study the relationship between iron deficiency anemia and the formation of gallstones, in addition to the use of ferritin as a preliminary indicator to predict the possibility of forming gallstones and then take the necessary preventive measures. So, ferritin is independent risk factor for gallstones formation.
Keywords:Iron deficiency anemia; IDA; GS; NOS; Liver enzymes
Background
The gallstones (GB) are one of the most common diseases that affect the digestive system and cause many health problems. Women are more likely to be gallstones; in addition to that it may appear in men. Stones may appear as a large stone or a group of small stones that group together in groups. Stones consist of mixture of cholesterol, bilirubin with, or without calcium [1].
Researches indicated that there is relation between gallstones formation and iron deficiency anemia (IDA) [2].
Iron deficiency anemia result from the negative balance between iron requirements and iron intake. This decrease may be due to malabsorption, malnutrition, excessive blood loss, inflammation in digestive system. Here we present patient with iron deficient anemia then developed gallstones [3].
Objective
The aim of the study was to determine the relationship between iron deficiency and the formation of gallstones with the use of ferritin as an indicator for the determination of iron deficiency anemia.
Case Report
18 - Years old - gentle woman was diagnosed with iron deficiency anemia in 2019. She presented to hospital in March 2019 with 4-week history of left upper quadrant abdominal pain associated with anorexia and easy fatigability. Physical examination was positive for pallor. Lab tests on presentation showed: white blood cells (WBCs) of 10.43 with monocytosis.
Hemoglobin (Hb) was 6.9g/dL, with mean corpuscular volume (MCV) of 54, RDWc 21.1 and platelets of 187.S. ferritin level is 2.3ng/ml. Renal and liver function tests were within normal limits. She is suffering from cholelithiasis confirmed by ultrasonography (Figure 1).
Discussion
There are many factors that help in the formation of gallstones, including: the concentration of bilirubin, the superior saturation of the bile in the bile ducts, the change in the degree of pH, some electrolytic materials such as copper, zinc, iron, and calcium play an important role in the formation of stones, in addition to iron deficiency anemia [4].
Iron deficiency anemia plays an important role in changing liver enzymes and thus increases the rate of super saturation for the bile, and thus helps in the formation of gallstones in addition to that iron acts as a catalyst in relation to nitric oxide synthetases (NOS) and this helps in the formation of nitric oxide, which has an effective role in improving the function of the gallbladder and its relaxing [5].
Conclusion
It was found that there is a relationship between the iron deficiency rate and the rate of formation of gallstones. Ferritin plays an effective predictor in identifying iron deficiency anemia. Then ferritin can be used as a diagnostic device to predict the presence of gallstones.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php
#juniper publishers contact info#Juniper Publishers#Surgical case reports#Family medicine#Internal Medicine#Molecular Biology#Ophthalmology
0 notes
Text
Describe the pathophysiology, clinical manifestations, evaluation, and treatment of polycystic ovary syndrome (PCOS).
Describe the pathophysiology, clinical manifestations, evaluation, and treatment of polycystic ovary syndrome (PCOS).
Week 4 Prompt 2 • Describe the pathophysiology, clinical manifestations, evaluation, and treatment of polycystic ovary syndrome (PCOS).
Week 5 Prompt 1 • Describe the most common causes and provide examples for neutrophilia, neutropenia, eosinophilia (i.e., eosinophilia caused by asthma, hay fever, or parasitic infection), eosinopenia, basophilia, monocytosis, monocytopenia, lymphocytosis, and…
View On WordPress
0 notes
Text
Juvenile Myelomonocytic Leukemia
Juvenile Myelomonocytic Leukemia (JMML) occurs when monoblasts start overproducing monocytes (absolute monocyte count >5000/microL). Patients present with fever, hepatosplenomegaly, lymphadenopathy, rash, and/or bleeding from thrombocytopenia due to crowding out of megakaryoctes in the bone marrow. Lab abnormalities include monocytosis out of proportion to other cytopenias, and the WBC differential includes immature and/or dysplastic cells that have been prematurely pushed out of the bone marrow. The stereotypical patient is a neonate with Noonan Syndrome or a 2-year-old boy with an NF1 mutation.
Pro-Tip: JMML can be difficult to distinguish from viral or bacterial infections, or from acute leukemia.
Source: Sivan Kassiff, "JMML/Pancytopenia," Children's Hospital of Pittsburgh Senior Morning Report (9 April 2020).
2 notes
·
View notes
Photo




Leptospirosis
Other names: Weill’s disease (severe form in humans)
Cause: Leptospira spp (multiple serovars exist)
Species: Swine, dogs, horses, cattle, humans. Many other species are also affected and/or asymptomatic carriers.
Signs:
Swine – abortion (usually in last 3 weeks of pregnancy), stillbirths, weak piglets that die soon after birth or grow slowly. Other than reproductive losses affected swine often appear healthy; anorexia, lethargy, and mild scours of a few day duration is sometimes seen.
Dogs – Acute kidney injury that, if survived, may progress to chronic kidney disease. Acute liver disease. Icteris, increased bilirubin and alkaline phosphatase, lethargy, anorexia, vomiting, diarrhea, abdominal pain, polyuria/oliguria/anuria, cylindruria, proteinuria, or glycosuria; azotemia, hyperphosphatemia, acidosis, hyperkalemia, neutrophilia, lymphopenia, monocytosis, and mild anemia, muscle pain, stiffness, weakness, trembling, reluctance to move, weight loss, fever or hypothermia, oculonasal discharge lymphadenopathy, effusions, and edema. Rarely bleeding disorders, uveitis, cough, dyspnea. Commonly fatal.
Horses – recurrent uveitis, abortion (usually after 9 months gestation); occasionally, fever and acute renal failure
Cattle – Most commonly abortion, stillbirth, increased services per conception, prolonged calving intervals, agalactia/blood-tinged milk. Often a large portion of the herd is affected. Less commonly, high fever, hemolytic anemia, hemoglobinuria, jaundice, pulmonary congestion, meningitis, death.
Humans – high fever, headache, chills, vomiting, diarrhea, abdominal pain, myalgia, uveitis, jaundice, rash; may resolve and then relapse with greater severity; kidney failure (nonoliguric, hyponatremia, hypokalemia), liver failure, pulmonary hemorrhages, meningitis, death
Transmission: Bacteria is shed in infected animal’s urine and enters an uninfected animal through the the mucous membranes or skin wounds, often via contaminated water. Venereal transmission can occur in swine and cattle. Among dogs, hunting dogs, farm/herding dogs, and pet dogs that explore the outdoors are at greatest risk.
Diagnosis: PCR or antibody level testing required for definitive diagnosis
Treatment: Swine – Streptomycin injections, tetracycline feed additives
Cattle – tetracycline, oxytetracycline, penicillin, ceftiofur, tilmicosin, tulathromycin
Dogs – Doxycycline, supportive care (fluid therapy, antiemetics, GI protectants, phosphate binders, hepatic support diets and medications)
Humans – Penicillin, doxycycline, supportive care
Prevention: Vaccination is the best method of control in animals! Additional management practices help reduce risk – good facility sanitation and rodent control. Maintenance of pens to prevent injuries. Do not allow pigs contact with cattle, horses, dogs, or cats. Do not graze cattle with sheep. Do not allow pigs into the areas used to house other susceptible species. Avoid open drains and communal drinking troughs to limit spread between pens; limit mixing of pigs from different herds or pens as much as possible. Maintain closed herds, and do not share bulls or boars.
Humans – No vaccine available. Use PPE whenever working around pigs (especially when handling urine, afterbirth, aborted fetuses, performing artificial insemination, or assisting with dystocias) or any individuals of other species suspected to have leptospirosis. Avoid drinking or wading/swimming in contaminated water.
Sources: State of Queensland Department of Agriculture and Fisheries, Merck Veterinary Manual, MSD Animal Health (image of dog), horsesidevetguide.com (horse image), NADIS (cattle images), leptospirosis.org (human image), CDC
#Leptospirosis#Lepto#Weill’s disease#recurrent uveitis#Leptospira spp#swine#dog#cattle#horse#sheep#pig#hog#wildlife#One Health#zoonoses#vaccination#equine#livestock#preventative medicine#veterinary#animal husbandry#diseases#biosecurity
103 notes
·
View notes
Photo
Children, Click, and Dogs: JASMINE IDH 46109 11 vr old Sweet Senior has lots of love to give! Playful and Affectionate & out of time ...57 lbs TO BE KILLED 11/9/18 Meet Jasmine! This gorgeous older lady needs a forever home @MACC - Sweet Seniorgirl has lots of love to give Playful, Affentionate & Out of time...please watch Jasmine's Video and step up before its to late. A volunteer writes: Jasmine is a very enjoyable dog to spend time with. She is so pretty, foxy like, an 11 year old golden gal so happy to be with a friend and play ball in the yard. Jasmine is full of good energy, running, jumping and catching tennis balls. She sits for treats or a toy, bright eyed and tail wagging, her face full of anticipation. After a while going back and forth after a ball, Jasmine comes to rest by my feet for caresses. She is a good walker, likely house trained and seems fine with dogs neared in the street. In our playgroups, she appears to prefer calm dogs. Jasmine is waiting at the Manhattan Care Center for a new leash on life. Will you be the one opening your door and your heart to this lovely and spunky senior? VIDEOS : <3 Spry Jasmine https://www.youtube.com/watch?v=QhPn96kUMHs Playgroup https://www.youtube.com/watch?v=-PQwrKIScdY Jasmine ID# 46109 MANHATTAN ANIMAL CARE CENTER Age: 11 years old Female, Is Vaccinated: Yes, Brown /Black , Weight: 57 lbs. , Intake Date: 10-31-2018 SHELTER ASSESSMENT ~ ADULT ONLY HOME No children (under 13) BEHAVIOR NOTES: Means of surrender (length of time in previous home): Owner Surrender (In home for 11 years) Previously lived with: An adult and a dog Behavior toward strangers: Friendly Behavior toward children: Pulls towards them, owner stated she was dangerous around them but did not detail why Behavior toward dogs: Friendly Resource guarding: None reported Bite history: None reported Housetrained: Yes Energy level/descriptors: Jasmine is described as affectionate and playful with a high level of activity. Other Notes: Jasmine will snap at bikes that pass by. Jasmine is reported to have been destructive in her previous home, ripping up furniture. SAFER SCORES: Date of assessment: 1-Nov-2018 Look: 1. Dog's eyes are averted, with tail wagging and ears back. Allows head to be held loosely in Assessor's cupped hands. Sensitivity: 1. Dog leans into the Assessor, eyes soft or squinty, soft and loose body, open mouth. Tag: 1. Dog follows at the end of the leash, body soft. Paw squeeze 1: 1. Dog gently pulls back his/her paw. Paw squeeze 2: 1. Dog gently pulls back his/her paw. Flank squeeze 1: Item not conducted Flank squeeze 2: Item not conducted Toy: 1. Minimal interest in toy, dog may smell or lick, then turns away. Summary: Jasmine approached the assessor with a soft body. She was social throughout the assessment, allowed all handling, and displayed no concerning behaviors. Summary (1): 11/1: When introduced off lash to dogs Jasmine greets politely, engages in brief play. She offers correction for mounting. Summary (2): 11/2: Jasmine is anxious and paces the yard, ignoring the other dogs. Summary (3): 11/4: Jasmine rushes over to the helper dog with a stiff body and stands over his back. She then anxiously paces the pen and seeks exit. Date of intake: 31-Oct-2018 Summary: Tense, whining, pacing ENERGY LEVEL: Jasmine is described as having a high level of activity. We recommend long-lasting chews, food puzzles, and hide-and-seek games, in additional to physical exercise, to positively direct her energy and enthusiasm. BEHAVIOR DETERMINATION: ADULT ONLY HOME Recommendations: No children (under 13) Recommendations comments: No children: Jasmine's previous owner reported that she was "dangerous" with children, but gave no specifics as to what this meant. Out of an abundance of caution, we recommend an adult only home. Potential challenges: Destructive behavior On-leash reactivity/barrier frustration Potential challenges comments: Destructive behavior: Jasmine is reported to show destructive behavior in the home, such as chewing on furniture. We are unaware of what, if any, attempts were made to remedy this behavior but we suggest to future adopters that Jasmine will need to be provided with physical and mental stimulation and with a variety of appropriate and engaging chew toys so she can engage in necessary chewing behavior without damage to human objects. On-leash reactivity/barrier frustration: Jasmine is reported to lunge and snap at bike while on leash and to lunge at children. Jasmine may need positive reinforcement, reward based training to teach her to look at you rather than other dogs. We recommend a front clip harness or head halter to help manage this behavior. MEDICAL EXAM NOTES 4-Nov-2018 Blood Work Interpretation Vet Notes: 4:18 PM CBC - lymphopenia 0.85 (1.05-5.1), monocytosis 1.23 (0.16-1.12) - pattern suggestive of stress leukogram CHEM - All parameters were within the reference range. 4-Nov-2018 DVM Intake Exam Estimated age: 11 yo Microchip noted on Intake? Yes Microchip Number (If Applicable): 0A10657603 History : Owner surrender Subjective: Observed Behavior - Cat reactive Evidence of Cruelty seen - No Evidence of Trauma seen - No Objective T = NT P = 120 bpm R = eupneic BCS 6/9 EENT: corneas and anterior chambers OU, mild ceruminous AU, no nasal or ocular discharge noted Oral Exam: Limited oral exam due to muzzle, dental calculus and gingivitis noted, worn PLN: No enlargements noted H/L: Grade 4/6 left systolic heart murmur, NSR, CRT <2 sec , Lungs clear, eupnic ABD: Non painful, no masses palpated U/G: Grossly normal castrated female, no vaginal discharge. Spay scar noted on ventrum. MSI: Ambulatory x 4, skin free of parasites, no masses noted, healthy hair coat. Excoration noted on nasal planum. CNS: Mentation appropriate - no signs of neurologic abnormalities Rectal: Externally clean Assessment 11 yo FS MBD Grade 4/6 left systolic heart murmur Nasal excoriation - r/o: secondary to trauma (rubbing) vs. other Prognosis: Good Plan: Recommend 2-view chest rads and echocardiogram Recommend TAB topically on nasal planum SID x 7d Recheck nasal planum in 7d SURGERY: Already spayed * TO FOSTER OR ADOPT * HOW TO RESERVE A “TO BE KILLED” DOG ONLINE (only for those who can get to the shelter IN PERSON to complete the adoption process, and only for the dogs on the list NOT marked New Hope Rescue Only). Follow our Step by Step directions below! PLEASE NOTE – YOU MUST USE A PC OR TABLET – PHONE RESERVES WILL NOT WORK! * STEP 1: CLICK ON THIS RESERVE LINK: https://newhope.shelterbuddy.com/Animal/List Step 2: Go to the red menu button on the top right corner, click register and fill in your info. Step 3: Go to your email and verify account \ Step 4: Go back to the website, click the menu button and view available dogs Step 5: Scroll to the animal you are interested and click reserve STEP 6 ( MOST IMPORTANT STEP ): GO TO THE MENU AGAIN AND VIEW YOUR CART. THE ANIMAL SHOULD NOW BE IN YOUR CART! Step 7: Fill in your credit card info and complete transaction HOW TO FOSTER OR ADOPT IF YOU CANNOT GET TO THE SHELTER IN PERSON, OR IF THE DOG IS NEW HOPE RESCUE ONLY! You must live within 3 – 4 hours of NY, NJ, PA, CT, RI, DE, MD, MA, NH, VT, ME or Norther VA. Please PM our page for assistance. You will need to fill out applications with a New Hope Rescue Partner to foster or adopt a dog on the To Be Killed list, including those labelled Rescue Only. Hurry please, time is short, and the Rescues need time to process the applications.
1 note
·
View note
Text
Week 4 Prompt 2 • Describe the pathophysiology, clinical manifestations, evaluat
Week 4 Prompt 2 • Describe the pathophysiology, clinical manifestations, evaluat
Week 4 Prompt 2 • Describe the pathophysiology, clinical manifestations, evaluation, and treatment of polycystic ovary syndrome (PCOS).
Week 5 Prompt 1 • Describe the most common causes and provide examples for neutrophilia, neutropenia, eosinophilia (i.e., eosinophilia caused by asthma, hay fever, or parasitic infection), eosinopenia, basophilia, monocytosis, monocytopenia, lymphocytosis, and…
View On WordPress
0 notes
Text
Week 4 Prompt 2 • Describe the pathophysiology, clinical manifestations, evaluat
Week 4 Prompt 2 • Describe the pathophysiology, clinical manifestations, evaluat
Week 4 Prompt 2 • Describe the pathophysiology, clinical manifestations, evaluation, and treatment of polycystic ovary syndrome (PCOS).
Week 5 Prompt 1 • Describe the most common causes and provide examples for neutrophilia, neutropenia, eosinophilia (i.e., eosinophilia caused by asthma, hay fever, or parasitic infection), eosinopenia, basophilia, monocytosis, monocytopenia, lymphocytosis, and…
View On WordPress
0 notes
Text
Describe the most common causes and provide examples for neutrophilia, neutropen
Describe the most common causes and provide examples for neutrophilia, neutropen
Describe the most common causes and provide examples for neutrophilia, neutropenia, eosinophilia (i.e., eosinophilia caused by asthma, hay fever, or parasitic infection), eosinopenia, basophilia, monocytosis, monocytopenia, lymphocytosis, and lymphocytopenia.
Use at least one scholarly source other than your textbook to connect your response to national guidelines and evidence-based research in…
View On WordPress
0 notes
Text
Describe the most common causes and provide examples for neutrophilia, neutropen
Describe the most common causes and provide examples for neutrophilia, neutropen
Describe the most common causes and provide examples for neutrophilia, neutropenia, eosinophilia (i.e., eosinophilia caused by asthma, hay fever, or parasitic infection), eosinopenia, basophilia, monocytosis, monocytopenia, lymphocytosis, and lymphocytopenia.
Use at least one scholarly source other than your textbook to connect your response to national guidelines and evidence-based research in…
View On WordPress
0 notes