#Internal Medicine
Photo
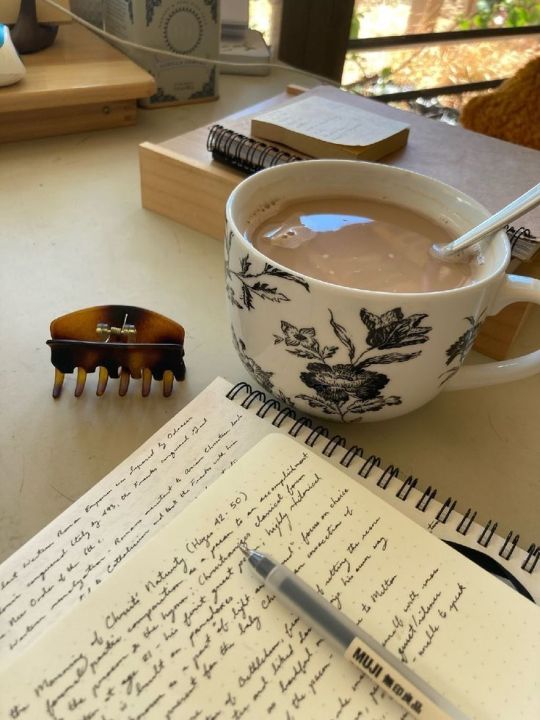

Samedi 11 février 2023
Hello there how are you doing ?
4 months left until graduation. 4 months before becoming a doctor :)) Life is rough and exhausting. Everyone is so stressed out and suspicious since they aren’t enough places for all of the students. I might chose internal medicine.
I try to stay out of this toxic environnement. I hate competition.
I hope you guys are doing good. May we all be walking safely and peacefully towards our goals.
Take care.
#medical school#academia#dark academia#classic academia#soon to be#physician#internal medicine#graduation#study inspo#studyblr#study with me#France#café#study hard#residency
2K notes
·
View notes
Text




internal medicine has been an uphill battle so far 😵💫
managed to catch some snow these past two weekends tho 🙌🏻
#medblr#medblog#junior doctors#medicine#internal medicine#junior doctor diaries#junior doctor#resident
49 notes
·
View notes
Text
Doctor: What lab parameters would you ask for?
Intern 1: To the patient or to the pleural effusion?
Intern 2: The pleural effusion is part of the patient, you dumbass.
35 notes
·
View notes
Text

Tuesday, 28 November 2023
I went put and studied with my friends today. I also found an amazing way to actually retain info in residency; it’s doing what i did in med school but with a twist (wow shocker). I’m going to be making anki decks. No surprise there.
#medstudyblr#medicine#productivity#being productive#internal medicine#internalmedicine#residency#medstudlife#medstudent#med student#100 days of productivity#productive#coffeeshop#study time#study notes
49 notes
·
View notes
Text
Random thoughts while rounding
Always have to swipe ourselves into the internal medicine wards. Swipe access in, swipe access out. It's to prevent patients with dementia from escaping.
One comes up to us, as we're discussing a case in the hallway. Some of them will just randomly join the walking part to rounds. He patiently waits for us to finish then asks if we can open the door for him, he needs to go home. Ask him where his nurse is, best to ask them, he goes, 'bloody useless" and walks off.
It's not entirely uncommon to get a call from families sometimes (usually disgruntled and frustrated) to go, so Mum or Dad's just escaped from hospital or the ED. Shall I ring the ambulance to bring them back? At the extreme, I've had patients barricade themselves in random rooms.
Mr H is still making his laps around the wards with his walker, if he bumps into something, he some how manages to troubleshoot it or wait for a staff member to move it. Usually a Wow (Workstation on wheels).
Another patient confidently walks past us to an alcohol hand wash/purell/hand sani. Picks up and tries to drink it, when her bedside nurse runs up and stops her. She goes, aww I was only going to take a sip.

Reminiscent of the woman who drank the perfume sample on tiktok. Addiction is hard.
12 notes
·
View notes
Text

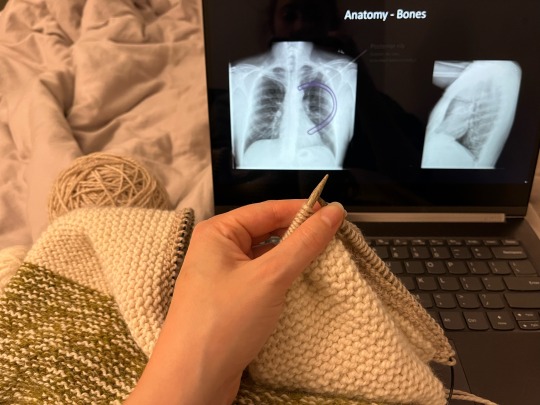
10/27/2022
Tranquil study challenge day 14
13. What was the most productive thing you did today? Why do you consider this action to be productive?
I went for a 5k run and took my time enjoying some self-care home spa activities. Today was day 6 of my 7 day stretch at the hospital and I have been very tired, not sleeping well, and struggling to stay engaged and complete tasks. Taking the time to exercise, be outside, and relax is important to break out of that cycle.
14. What passions do you have that led you to studying what you're studying in school now?
This is the super cheesy answer that I feel like everyone says but it's still true for me: life long learning and getting to help people on a daily basis.
Today, I am grateful for coffee and crisp fall air.
Today, I choose to give myself a chance to relax.
Today, my goals are
40 Uworld questions
200-300 anki cards
watch video on ECG interpretation
write reflection post on professionalism
complete slides for group practice questions session
workout
#emgoesmed#tranquilfallbuddies#studyblr#studyspo#med student#med studyblr#med school#medicine#ms3#clinical rotations#internal medicine#radiology#knitblr#knitting#self care#spa day#relax#cozy
114 notes
·
View notes
Text

GOLD 2023
Previous treatment categories C and D have been combined into a new category, named E (for
exacerbations). GOLD provides new guidance based on blood eosinophil level. Initial therapy for
categories A, B, and E is as follows:
– A: Long-acting β-agonist (LABA) or long-acting muscarinic antagonist (LAMA)
– B: LABA + LAMA (change from monotherapy)
– E: LABA + LAMA; if blood eosinophils are ≥300 cells/μL, consider LABA + LAMA + inhaled corticosteroid (ICS). No recommendation is made (at any eosinophil level) for ICS without
combined LABA + LAMA.
– For patients with persistent exacerbations despite LABA + LAMA + ICS or for those who have
100 eosinophils/μL, roflumilast (for patients with chronic bronchitis and FEV1 <50% of predicted)
or azithromycin (in nonsmokers) can be considered.
13 notes
·
View notes
Text
One day you’re an intern and the next you’re a PGY-4 chief resident teaching interns. Life comes at you fast!
11 notes
·
View notes
Text
Someone’s sodium was 128 and nobody even mentioned it. On medicine someone would have pulled out a whole-ass flow chart and gone to through every possible cause.
#medblr#internal medicine#i mean it was a chronic issue but still#i found my people and they have flow charts#let’s pull up that recent meta analysis in the middle of rounds to discuss which antihypertensive would be better for this one specific case#my favorite part of surgery was clinic…#like having your hands inside someone’s abdomen is cool and all but how about getting to know someone and forming longitudinal relationships
20 notes
·
View notes
Text
Highlights of the internship - Week 18:
• The last two days of paediatrics — FINALLY. And the start of internal medicine.
• When I said goodbye to the small surgical procedures room’s staff, they were like, “oh nooo. But we were so used to seeing you. We can gather signatures for you to keep you here ahaha.” 🥹🥹
• Going to miss only ob/gyn part of this hospital.
• At general medicine, I started in endocrinology clinic. We were supposed to get there 30 minutes earlier than the doctor and start admitting the patients, taking their history and getting them ready for the doctor. When she comes, we start admitting them together. This will be the sum of my two weeks here.
• I had the night shift of the first day. I don’t like the first day night shifts!! Nothing requiring an intern really happened so it was calm, at least.
• I got a text from my friend about our gynaecologic oncology attending. He told the nurses she and I are his favourites and firsts, the ob/gyn doctors of the future 🥹🥹🥹 stoppp 🥹🥹🥹
#medical student#medical stuff#medical school#medblr#6th year#internship#paediatrics#internal medicine#night shift memories#ob/gyn#endocrinology
4 notes
·
View notes
Text
Doc: You know it's bad when you got 17 VIN tabs open O.O
#she also had 2 textbooks and her whole desk was scribbled over with white board marker#veterinary#lol#my coworkers#internal medicine#tough case#rural GP#rural veterinary medicine
19 notes
·
View notes
Photo
Vendredi 24 février 2023
Writing cover letters and updating my CV & cat sitting for my friend.
So funny how they expect you to come with an amazing personal statement but nobody taught you how to write a proper one. Hopefully I have great company !
Hope you guys are doing good !
#med school#study with me#personal statement#studyinspo#study blog#cover letter#physician#application#internal medicine#classic academia#hospital#soon to be#doctor
26 notes
·
View notes
Text




work's hard but life has its moments 🫶🏻🍦
got myself a pair of crocs! look how cute they are!
#junior doctors#medicine#junior doctor#aesthetic#junior doctor diaries#residency#internal medicine#medblr
5 notes
·
View notes
Text
ICU Resident *evil smile*: Damn, looks like your are having a very quiet shift…
Night shift Med-Surg Resident: NOOO, LAST TIME YOU SAID THAT I HAD TWO PATIENTS BECOME SEPTIC, FUCK YOU
#medicine#medblr#internal medicine#hospital#superstition#mind you that medsurg resident is in charge of 72 patients during the shift#i meant to sent this to the queue#oh well
45 notes
·
View notes
Text
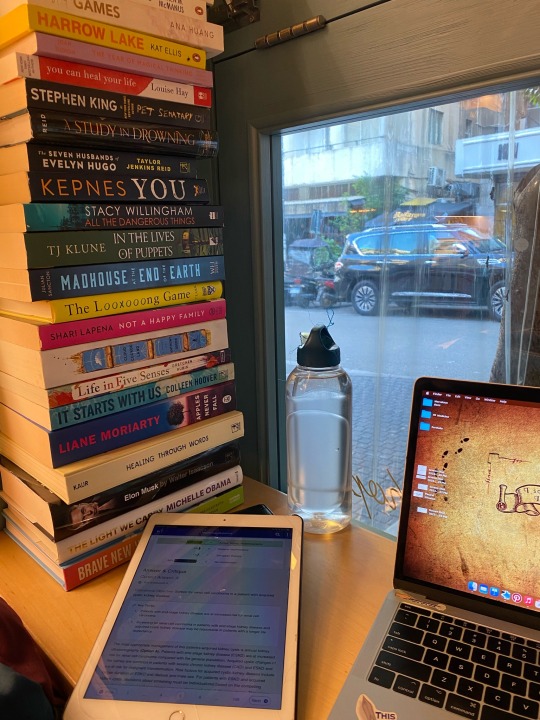

Monday, 4th of December 2023
I went to a coffee shop to study. It was hella productive. Did 30 MKSAP nephrology questions AND made anki cards. Love that.
#medstudyblr#medicine#medstudlife#medstudent#med student#productivity#being productive#productive#study notes#study time#internalmedicine#internal medicine#nephrology#coffeeshop
14 notes
·
View notes
Text
Enterococcus faecalis
As per wiki, "not to be confused with enterococcus faecium."
why in god's name are they so similarly named. I do not know. but it does change management.
Faecalis is more susceptible to penicillin and ampicillin. Faecalis is more virulent and more likely to cause IE than faecium. Faecium is also more likely to be resistant to ampicillin and vancomycin --> in the US: 80% to vanc, and 90% resistant to ampicillin.
It's a nosocomial common bug, so there aren't any cool case reports. If you walk into a ward, odds are you'll find someone with this. Not as common as staph or strep though.
Image source: bacteria under the microscope

E. Faecalis is gram positive cocci, (purple spheres), previously part of the streptococcus umbrella - if it makes it easier to remember - both appear in chains or pairs (rather than clusters like staph). Similar to strep it is catalase negative. Facultative anaerobe, so it will grow in both bottles. Faecalis is far more common than faecium, both live in the gut (think faeces). They grow at high salt concentrations, 6% (normal saline on the wards is 0.9%) and are usually non haemolytic.
Key thing to be aware of is that it can be a healthy part of your gut or genital tract but under the right circumstances for it - it can become pathogenic/disease causing. Further key thing: intrinsically resistant to bactericidal antibiotics hence they require synergism between a combination or prolonged duration in severe cases. like IE.
It's considered an opportunistic infection (for the lay public, it means when you're unwell or immunosuppressed, it becomes a problem). Increasingly it is a nosocomial infection (hospital acquired), 60% of cases in the US were acquired in hospital. They survive very harsh environments, including ethanol and can survive 10 mins at 60 degrees celsius and on surfaces from days to months. They are killed at 80 degrees or with 70% ethanol.

Similar to staph and strep, it can cause a variety of infections, including:
Infective endocarditis --> 3rd most common cause, 90% are faecalis other 5% are faecium (after staph aureus and strep viridans), subacute course, now more associated with TAVIs (elderly/frail/multimorbid patients). high mortality, 10-35%
UTIs - cause up to 20% of UTIs, but usually associated in hospital setting and with catheters/devices etc.
wound infections & OM (rarely)
line associated --> always replace lines if you can in sepsis, one cause of bacteraemia is the line
2nd or 3rd most common cause of nosocomial Utis, sepsis and wound infections (less often: diabetic ulcers, prosthetic joints)
less common: meningitis - and usually associated with shunts and neurosurgical procedures --> anything to do with devices and hospital. Mortality risk of 20%
odd association: strongyloides hyperinfection (remember this increases risk for bacteraemia), as post earlier.
sepsis/bacteraemia mortality risk is 25%
bottom line: high mortality in severe disease
Epidemio:
more likely to be found in the elderly populations who are multi-morbid and less independent in their activities of daily living.
Special powers:

No toxins (like staph or strep), but have inherent antibiotic resistance or are amenable to this and are very durable/hardy. Ability to form biofilms - hence attraction to lines and devices and staying there. This limits abx penetration allows them to persist. They gain resistance by their ability to pick up and transfer mobile gene elements like plasmids via conjugation etc. Abx including: cephalosporin, clinda, TMP-SMX, aminoglycosides like gent.
It is becoming more notorious for resistance particularly vancomycin resistant enterococcus faecalis (also not to be confused with VRE - Patients who were recently hospitalised or institutionalized are often swabbed for this, but this is actually E. faecium they're referring to). increased risk for this include previous antibiotics use (eg cephalosporins, vancomycin), due to disrupted gut biome, and exposure risk - more likely to occur if you've been recently hospitalised, require routine access to the wards (i.e. dialysis) etc. Also increased association with devices (like pacemakers), diabetics and stomach acid suppression from PPIs.
Investigations
Relevant imaging i.e. CT for abdominal collections, and culture/staining. sensitivities are an absolute must including aminoglycoside resistance, pencillin and vanco, which most labs will automatically do anyway when it's identified, teams just gotta remember to chase. other possibilities include PCR or 16s rRNA sequencing
Interesting additional work up: Colonoscopies. Some reports are starting to recommending doing this routinely if no source is found in cases of bacteraemia or IE. As there is an increasing association with neoplasms from the gut. Similar to guidelines for strep bovis.
Management
in general UTIs, wound infections etc, most are susceptible to penicillins and ampicillin, so you can treat with either.
Management of beta lactam resistant enterococcus:
- resistant against beta lactams --> refer to immunology for desensitisation, vanco is not as effective against enterococci, duration is 6 weeks in severe infection
Vanco resistant (your local infectious diseases team will be involved)
daptomycin, linezolid --> equally effective, tigecycline (last resort/salvage)
Treatment in IE --> synergism is key for bacteriocidal effect (durability)
in case of bacteraemia, try the denova calculator to determine risk of IE - Duration of symptoms, Embolizations, Number of positive cultures, Origin, valve disease, and Auscultation murmurs
if susceptible, it's intermittent doses of benzylpenicillin or continuous infusion at 2.4 g IV plus gentamicin (if concerning for kidneys, shorten the duration to 2 weeks) for approx 4-6 weeks
--> unless there's high level resistance to aminoglycosides
or if resistant as above options
issue with aminoglycosides -> ototoxicity and nephrotoxicity, requires frequent monitoring and caution in elderly
Resources:
Pathogen data sheet - Canadian government
StatPearls
Australian therapeutic guidelines - paywall, unless you're at an Australian hospital/medical school
Uptodate - always the gold standard, but is behind a paywall unless you have institutional access
Wikipaedia
#infectious diseases#internal medicine#medblrs#medblr#microbiology#infectious disease#enterococcus#enterococci#e faecalis#enterococcus faecalis
3 notes
·
View notes