#correct spinal curvature
Text
youtube
الحل السحري لعلاج تقوس وانحناء الظهر The magic solution to treat curvature and curvature of the back
#magic the gathering#back relaxation device#yoga to correct spinal curvature#back pain#back relaxation#back stretcher#curvature pen tool#photoshop curvature pen tool#curvature pen tool photoshop#new curvature pen tool#curvature tool#photoshop curvature tool#curvature pen tool in photoshop cc 2018#curvature pen photoshop#photoshop curvature pen#back pain relief#curvature#correct spinal curvature#learn magic the gathering#spinal curvature#gym body#gym bro#gym routine#gymlover#gymlife#gymfit#gym#home gym#tumblr milestone#gymwear
0 notes
Text
this summer we embrace my hunchback
#before any of you flat backed hoes with bad posture decide you can relate to this let me tell you#i have a spinal deformity that causes a spinal curvature no matter how i stand#and could only be corrected with surgery#so please understand my hump is intrinsicly more tortured and complicated than yours#unless you too are a kyphosis warrior in which case we're comrades
1 note
·
View note
Text
Freelancer scoliosis headcanons (+ a little bit of Gavin)
this is mostly just me self projecting btw
for those who dont know, scoliosis is an abnormal curvature of the spine that can be caused by genetics and a number of other factors 👍
they have a specific routine they do in the morning that prevents further curvature in their spine
they got spinal fusion surgery in order to correct the worst curve
they take vitamins out of habit, they dont really need to take them anymore
when Gavin first found out that they had scoliosis, he was scared that he would hurt Freelancer during sex (“I dont want to knock anything out of place :(“ “Gavin, these metal rods have been screwed into my spine for over ten years, you’ll be fine.”)
sometimes, before or after they shower, Freelancer just marvels at the incision scar (from the surgery) on their back (literally just going :O at it in the mirror)
Gavin loves to kiss said scar <3
they still gets the occasional stinging muscle pain due to the surgery
when they first got home from the surgery, they found out that their back was entirely numb (bc they had to cut through nerves and disturb some muscles) and they were really freaked out by it
the beginning of the incision scar is just below their neck, and sometimes they reach behind them in order to feel it (without realizing)
Gavin makes “i love your curves” jokes (haha get it because Freelancer’s spine used to be abnormally curved haha)
there’s a bit of a dip in Freelancer’s back due to the remaining curve, and Gavin loves placing his hands there. he doesnt even have a reason, he just likes the way it feels under his fingers
Freelancer used to shift around a lot when they were trying to fall asleep because no position was comfortable for them
while they dont shift around in bed anymore, they do still shift their sitting positions
Gavin has to remind them not to shrimp because it makes their back ache
they dont do sports, but they do do yoga
they like to say “there are ribs in places where there were no ribs before,” because their ribcage was also fucked up and it indeed feels like there are ribs in places where there were no ribs before
uhh thats all i have atm :3 👍
#i love self projecting onto my favorite characters#teehee#redacted asmr#redactedverse#redactedaudio#redacted freelancer#redacted gavin#vinn says fandom things#vinn headcanons things#vinn yapping#redacted headcanons
41 notes
·
View notes
Note
Hello, I apologize if this is a question you have answered before or just a dumb question, but I am curious. I think I have understood that before having to have spinal surgery and getting the metal vertebrae, you were pretty much without pain. Was the surgery something you didn’t have a choice in, or to treat some kind of underlying issue? It seems like you are in so much pain all the time and I guess I am just nosy and curious about what led to that
I had my fusion done to correct some pretty terrible scoliosis I had that was never properly treated, my parents were extremely medically neglectful and so by the time I got help, it was too late for a hard brace

here’s a picture of what it looked like when I was about 14. the curvature actually progressed about 15° more to a 70° curve on the upper curve and around 35° on the lower when I finally had my fusion done a few years later
the fusion was done for multiple reasons, pain was one of them (but it wasn’t nearly as bad as it got 10 years after the fusion) and function being another. there was a concern the curve would keep progressing or something and cosmetics was probably a factor as well


nowadays thankfully we have better surgical technology and more options besides a solid fusion. my disc replacement is a good example of this


it restored function and didn’t limit my mobility as much as the fusion did (I can still turn my head side to side). I’m not sure how long it will last at this rate but I’m glad I was able to get it. I had it done in mid 2022
26 notes
·
View notes
Text
Can I say something that might be outlandish?
Here goes: I have a headcanon that Midas had scoliosis (a curvature of the spine), and it was corrected with titanium. Spinal fusion surgery. He has chronic pain, and some nerve damage in his lower back and in one knee. When he was imprisoned, the pain flared up in his legs and back more than usual because he was forced to be stood (or sat (?)) in one position for so long.
16 notes
·
View notes
Text
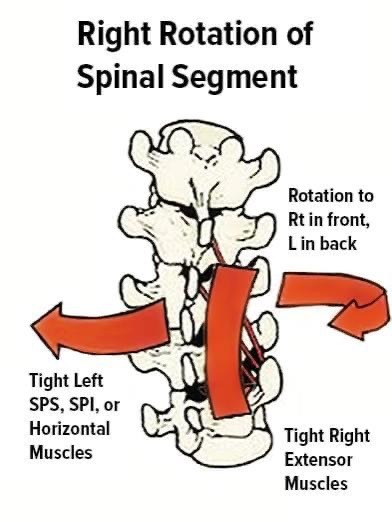
The Key Element in Scoliosis...
and Tension between the shoulder blades...
When one side of the spinal extensors gets tight, the opposite side will be inhibited and/or weak. This is a “C” curve in Scoliosis.
You already know to stretch the tight/concave side and condition the lengthened/weak side. What you may not already know is that tight extensors inhibit all rotations to the opposite side. If you do not cue and correct the extension to rotation coordination problems the problem will not resolve. This is why NMR is such a great addition to the management of Scoliosis.
It's not just Scoliosis that has tight one sided extensors. Lots of us have that pattern but don't have a dramatic curvature of the spine.
The key element is rebalancing the rotations to extensions. Then integrating the rotational segments to each other.
[Jocelyn Olivier]
[Neuromuscular Reprogramming]
3 notes
·
View notes
Text
The Rules of NMR
Recently a new student asked me “What are the Rules of NMR?”
I was flustered for a moment then my innovator/rebel answered, “There are no rules.” Since I did not follow a path in my studies that adopted someone else’s way of viewing the body, I’ve been able to innovate based on what the body tells me and I am seeing a HUGE IMPORTANCE for PRIORITIES in how we approach a problem to get the fastest possible results.
So yes, there are rules: the body’s rules = NMR’s Rules.
Here they are:
Correct the Sympathetic/Parasympathetic balance first. (Even that has Priorities)
1. Integration between R/L hemispheres of the Cortex. The fastest track to this starts with Brain Buttons http://www.neuromuscular-reprogramming.com/.../brain.../.
2. Space Buttons or CranioSacral Rebalancing or Polarity or Restorative Breathing can help the NS to deeply relax. The body’s ability to restore itself is optimized when we deeply relax. Hence periods of rest/relax are also good intertwined with your structural bodywork. Structural work is challenging to the NS, as we are pushing for change in a system that is committed to homeostasis. When there has been an accident or injury, this is paramount.
Reduce Torsions/Rotations in the Torso next:
Organize the base of the spine for reciprocal rotation in the waist/core pivot at T12/L1
Follow that with the Low Back and Hips Protocols for safely reprogramming the coordination sequencing of the hips and low back/core. (Detail of this to be found in the NMR Mod 1 Intro manual.)
Organize the Hips to Shoulders relationships before working on the shoulders and neck. This includes reducing torsions and insufficiencies in the diaphragm. Other than some general fact finding and massage warm up for the neck, changes will not be possible until the coordination issues in the torso are reduced. (Details on this can be found in the NMR Mod 2 manual)
Moving out from this basic level of organization one can begin to follow the client’s priorities.
The Thoraco/Cervical junction needs to be functional in order to change pain and dysfunction in the shoulders and neck.
Shoulders should be functionally rebalanced before working on elbow and wrist problems.
Hips should be functionally rebalanced on the way to working on knees and ankles and feet.
The Neck has its own priorities….Because of the complexity of neck issues the intricacies of reprogramming the neck in details are not explored until Mod 3 of the basic 72 hr, training and again in the NMR Advanced 30 hr in great detail.
Once big muscle support is available and relationships are functional one can start undoing the deep layers of detail in the soft tissue matrix of the body and even in the skeleton itself. The Reprogramming of the Spine is explored in Adv NMR also.
Contraindications:
Spot work. Too much in depth work in one area without a larger integration plan can be dangerous and leave clients in pain.
Releasing deep tension without an understanding of what it’s bracing for and strategy for providing the stability that requires it to be tight.
Digging to release spinal fixations. The spine responds best to support and movement instruction in the direction of its normal curvature and function.
(Neuromuscular Reprogramming)
#NMR#Jocelyn Olivier#bodywork#movement#movement work#exercise#Neuromuscular Reprogramming Network#technique#order of relative importances
21 notes
·
View notes
Text
The Disease Of Scheuermann: What You Should Know!
Did you know that Holger Scheuermann, a Danish orthopaedic surgeon who initially characterised the Scheuermann disease in the early 1900s, received his name from the condition? For more information, keep reading.
The musculoskeletal condition Scheuermann's disease, also called Scheuermann's kyphosis, mainly affects the spine. Atypical spinal growth, which causes kyphosis, or a rounded or stooping posture, distinguishes Scheuermann's disease.
It is unclear what causes Scheuermann's disease. It is thought to result from a combination of hereditary and environmental causes. Numerous study results suggest a genetic risk. Environmental elements like poor posture, spinal tension, or food limitations during periods of rapid growth may also impact how it develops.
What Is The Disease Kyphosis?
Kyphosis is the medical term describing an unnatural forward curve of the spine. It can refer to a particular ailment known as kyphosis or be used as a general term to indicate an excessive upper back rounding. Kyphosis can be structural or postural and can affect persons of all ages, from infants to older people.
Teenagers are prone to postural kyphosis, which is typically brought on by poor posture. It can be reversed and has nothing to do with spine structural issues. Postural kyphosis can be treated with exercises, postural correction, and back muscle strengthening.
An aberrant spine curvature is caused by structural deformities such as congenital anomalies, Scheuermann's disease, osteoporosis, or spinal fractures. A few illustrations of structural kyphosis are as follows:
1. Scheuermann's Kyphosis
Scheuermann's illness, as was previously mentioned, is a specific kind of kyphosis characterised by abnormal spinal growth during adolescence, resulting in a rounded upper back.
2. Inborn Kyphosis
This kyphosis begins at birth and grows abnormally as the spinal vertebrae develop.
3. Kyphosis Brought On By Osteoporosis
Osteoporosis deteriorates bone strength and increases the risk of compression fractures. Multiple compression fractures in the spine can cause an increase in forward curvature and kyphosis.
4. Kyphosis Caused By Trauma
This kind of kyphosis may occur due to spine fractures or other injuries, which could cause the vertebrae to collapse or misalign.
Scheuermann's Disease Symptoms
Some of the most typical Scheuermann's disease symptoms, also known as Scheuermann's kyphosis, are listed below:
1. Kyphosis
The characteristic feature of Scheuermann's disease is an abnormal forward curving of the upper back, which results in a rounded or slumped posture. It is readily apparent and can be mild to severe.
2. Pain In The Back
A lot of people, to varying degrees, are affected by Scheuermann's disease, which frequently manifests as upper back (thoracic) pain. The discomfort may be mild or even severe, and it may get worse with activity or after spending a lot of time sitting or standing.
3. Stagnancy And Less Flexibility
Scheuermann's illness can result in several symptoms due to aberrant spine curvature. It could be challenging to bend or twist the back as a result.
4. Tiredness
Due to spinal stress, people with Scheuermann's illness may grow tired or uncomfortable after exerting themselves physically for an extended amount of time or while maintaining an upright position.
5. Muscle Cramps
Muscle cramps in the back might occur infrequently and hurt or be uncomfortable.
6. Uneven Shoulders Or Prominent Shoulder Blades
Due to the curvature of the spine, the shoulders may appear unequal, with one being higher than the other. The shoulder blades can be seen if they are prominent.
In uncommon neurological situations, the spine's nerves may be compressed or irritated, resulting in symptoms including numbness, tingling, or weakness in the legs. These neurological symptoms are less frequent, though.
The Disease Of Scheuermann Treatment
Controlling symptoms, improving posture, and preventing the progression of the spine's curvature are the main objectives of treatment for Scheuermann's disease. Depending on the condition's severity and individual features, the course of therapy may alter. Here are some common medical remedies:
1. Monitoring And Observation
If symptoms are mild and the degree of spine curvature is not severe, a cautious observation strategy and routine checkups may be advocated in milder cases of Scheuermann's illness. This is particularly true if the individual's growth spurt has passed because the problem often stabilises with skeletal maturity.
2. Stretching And Exercise
Physical therapy exercises can benefit posture, the strength of the back and core muscles, flexibility, and pain management. A physical therapist can design a personalised exercise programme appropriate for the patient's needs and guide proper body mechanics and postural awareness.
3. Pain Control
Scheuermann's disease-related pain and inflammation can be managed with over-the-counter medications. Before using a medicine, visit a doctor.
The Final Say
Consider anti-inflammatory foods, consume enough calcium and vitamin D for healthy bones, and follow a nutrient-rich diet to promote general health. When offering tailored advice, dietary requirements, restrictions, and weight-control goals should be considered.
A diet specialist can help optimise nutrition and increase general well-being even though nutrition cannot treat Scheuermann's disease. For further information, speak with the orthopaedic department at Bansal Hospital.
About Bansal Hospital
Bansal Hospital is a multispeciality hospital and is one of the leading, reputable and reliable healthcare providers trusted by patients and their families across the region. It has all the major departments, including cardiology, neurology, oncology, orthopaedics, gastroenterology, urology, liver transplant, bone marrow transplantation, nephrology, gynaecology and more. The hospital is equipped with state-of-the-art facilities and technology and has a team of highly qualified and experienced doctors and medical staff who provide round-the-clock care to the patient.
Visit Our Website
3 notes
·
View notes
Text
Physical Therapy Clinic in New York City
What is Joint Stabilization?
Joint stabilization refers to the process of strengthening and supporting a joint to reduce excessive movement, prevent dislocation, and improve joint function. In the context of Ehlers-Danlos Syndrome (EDS) or other conditions associated with joint hypermobility or instability, joint stabilization techniques are often employed to address recurrent joint dislocations or subluxations.
There are different approaches to joint stabilization, depending on the specific joint involved and the severity of the instability. Here are some common methods used for joint stabilization:
Physical Therapy and Exercise: Physical therapy is crucial in joint stabilization. Therapeutic exercises are designed to strengthen the muscles surrounding the joint, providing additional support and stability. This may involve targeted strengthening exercises, proprioceptive training (improving joint position sense), and neuromuscular retraining.
Bracing and Orthotic Devices: Braces or orthotic devices can be used to stabilize and support joints that are prone to dislocation or excessive movement. These devices are designed to limit the range of motion in the affected joint while providing external support. Examples include ankle braces, knee braces, wrist splints, or custom-made orthoses for specific joints.
Ligament Reconstruction: In cases where ligament laxity or weakness is the primary cause of joint instability, surgical ligament reconstruction may be considered. This involves repairing or reconstructing damaged or stretched ligaments to restore stability and prevent recurrent dislocations. The surgical technique and specific approach depend on the joint involved and the individual's needs.
Tendon Transfers: In certain situations, tendon transfers may be performed to reinforce the stability of a joint. This involves transferring a tendon from a less important muscle group to a location where it can provide additional support to the joint. The goal is to improve joint stability and function.
Arthroscopic Stabilization: Arthroscopic stabilization is a minimally invasive surgical technique used to address joint instability. It involves using small incisions and specialized instruments to repair or tighten the structures surrounding the joint, such as ligaments or capsules, to enhance stability.
The choice of joint stabilization method depends on factors such as the specific joint involved, the severity of instability, the overall health of the individual, and their treatment goals. A comprehensive evaluation by healthcare professionals, including orthopedic specialists or physical therapists experienced in managing EDS or joint instability, is essential to determine the most appropriate approach for joint stabilization.
Ehlers-Danlos Syndrome Surgical
Surgical interventions may be considered in individuals with Ehlers-Danlos Syndrome (EDS) when conservative treatments have been ineffective or when there are specific complications that require surgical management. It's important to note that surgery in EDS patients can be challenging due to the increased risk of complications related to underlying connective tissue abnormalities. Therefore, careful evaluation and planning are crucial. Here are some surgical considerations for EDS:
Joint Stabilization: In some cases of EDS, individuals may experience recurrent joint dislocations or severe joint instability. Surgical procedures, such as ligament reconstruction or joint stabilization surgeries, may be considered to address the instability and provide additional support to the affected joints.
Spinal Surgery: EDS can be associated with spinal abnormalities, including spinal instability, spinal curvature (scoliosis or kyphosis), or Chiari malformation. Surgical interventions like spinal fusion, spinal decompression, or correction of spinal deformities may be required to alleviate symptoms and prevent further complications.
Skin and Wound Management: EDS can affect wound healing, leading to delayed healing, poor scar formation, and increased risk of wound complications. In cases where surgical incisions or wound closures are necessary, special techniques, such as careful suture selection and placement, may be employed to optimize wound healing and minimize the risk of dehiscence (opening of the wound).
Vascular Surgery: Some individuals with EDS, particularly those with vascular subtypes, may develop arterial or organ rupture or other vascular complications. In such cases, vascular surgical procedures may be necessary to repair or reinforce weakened blood vessels and prevent life-threatening complications.
Gastrointestinal Surgery: EDS can be associated with gastrointestinal abnormalities, such as hiatal hernias, gastrointestinal dysmotility, or bowel perforation. Surgical interventions may be considered to address these issues, such as hernia repair, bowel resection, or surgical management of intestinal strictures.
It's important to emphasize that surgical interventions in EDS require careful preoperative evaluation, appropriate surgical techniques, and close postoperative monitoring to minimize the risk of complications. A multidisciplinary approach involving experienced surgeons, anesthesiologists, and other healthcare professionals familiar
4 notes
·
View notes
Text
Swaybacks: Effective Solutions for Improved Posture
Swaybacks, also known as lordosis, is a medical condition characterized by an exaggerated inward curvature of the lower back, leading to a distinctive swayback appearance. The condition can result from various factors, such as poor posture, muscle imbalances, obesity, or certain medical conditions. Swaybacks may cause discomfort, reduced flexibility, and increased stress on the spine. Management typically involves physical therapy, exercises to strengthen core muscles, and lifestyle modifications. Early diagnosis and intervention are crucial to prevent further complications. Seeking medical advice and adopting corrective measures can improve posture, alleviate symptoms, and enhance overall spinal health.
#Swaybacks#Swaybacks Machine#swayback posture#swayback horse#swayback medical term#swayback exercises#sway bar 350z#swayback saddle pad#swayback adjustment#swayback bridge trail#swayback horse saddle pad#swayback lordosis#case swayback#sway bar 4runner#swayback dog#swayback knives#swayback posture fix#swayback spine#sway bar 370z#sway bar links for 6-inch lift#swayback pad#swayback campground#swayback cat#swayback correction#swayback horse pad#swayback in dogs#swayback is another word for#swayback meaning#swayback symptoms#swayback treatment
2 notes
·
View notes
Note
What are your thoughts about whether people should be able to say famous and historical figures had or have disabilities (without them or people close to them saying they had or have the disability)? For example, people sometimes say Albert Einstein had autism. Separately some people say FDR did not have Polio but had a different disability. Do you think we should be questioning what might have been known about someone like him even if the diagnosis we know for them might not be correct?
I think this is potentially less straightforward than assigning gender/sexual identities for people of the past. In that example, there's a blanket rule of not projecting modern cultural definitions onto people of the past.
With disabilities, sometimes we can objectively know what that person was experiencing. We know that Richard III had scoliosis because his skeleton showed a severe spinal curvature. That's not up to interpretation.
However, as a person with a disability, I think that the world has an unhelpful and unhealthy obsession with a diagnosis. People ask me all the time about what particular disability I have, when really it should be enough for them to know that I struggle to stand for long periods of time. To me, the most important thing about my disability is how it affects the way I interact with the world.
Let's go back to the Richard III example. It doesn't really matter that scoliosis was what was causing his back problems, just that he had them. And it is equally important to know that saddle and armor designs of his time would have acted as very effective back braces, allowing him to participate in horse and foot combat.
I don't necessarily mind when we know/are able to find out a specific diagnosis for a historical person, but I really don't think it's the most important thing.
Does it matter if FDR had polio or some other condition, or just that he had a limb difference? In terms of the way he existed in an able bodied world, the diagnosis means less than the challenges he faced as the result of his physical differences.
At the same time, I understand that it can be incredibly affirming to find out that a historical person had the same disability that you do. That is understandable, if that is something that helps you cope, go ahead. I would just encourage the sentiment of solidarity in experience over solidarity in diagnosis in your everyday interactions with the world.
-Reid
33 notes
·
View notes
Text
Understanding Humpback Neck: Causes, Symptoms, and Treatments
Humpback neck, clinically known as kyphosis or dowager's hump, refers to an exaggerated outward curvature of the upper back. This condition can lead to a noticeable rounding of the upper spine, causing discomfort, pain, and affecting overall posture. Understanding the causes, symptoms, and available treatments for humpback neck is crucial for effective management and prevention.
Causes of Humpback Neck
Several factors contribute to the development of humpback neck:
Poor Posture: Prolonged periods of slouching, hunching over desks, or improper sitting habits weaken the muscles and ligaments supporting the spine. Over time, this can lead to an abnormal curvature of the upper back.
Aging: As individuals age, spinal discs naturally degenerate and lose height, contributing to changes in spinal alignment and curvature. The aging process can also weaken muscles and decrease bone density, further exacerbating spinal curvature.
Osteoporosis: Weakening of bones due to osteoporosis increases the risk of vertebral compression fractures, which can lead to kyphosis. Fragile bones are more susceptible to deformities and changes in spinal structure.
Genetics: Some individuals may have a genetic predisposition to developing kyphosis. Certain genetic conditions affect bone and muscle development, potentially leading to abnormalities in spinal curvature.
Injury or Trauma: Severe injury to the spine, multiple vertebral fractures, or certain medical conditions like Scheuermann's disease can result in abnormal spinal curvature. Traumatic events can disrupt the natural alignment of the spine, causing structural changes over time.
Symptoms of Humpback Neck
The symptoms of humpback neck can vary depending on the severity and underlying cause but may include:
Noticeable rounding of the upper back, often described as a hump or curvature
Back pain, stiffness, or discomfort, especially in the upper back region
Limited mobility and flexibility in the spine, making it difficult to perform certain activities
Fatigue and muscle weakness in the back due to compromised spinal support
Changes in posture, such as a stooped appearance or difficulty maintaining an upright position
Treatment Options for Humpback Neck
Addressing humpback neck involves a multifaceted approach, and chiropractic care plays a pivotal role in its management:
Chiropractic Adjustments: Chiropractors use gentle spinal adjustments to realign the spine, reduce abnormal curvature, and alleviate pressure on affected vertebrae. These adjustments aim to restore proper spinal alignment and enhance mobility.
Therapeutic Exercises: Specific exercises are prescribed to strengthen the muscles supporting the spine, improve posture, and enhance spinal flexibility. Targeted exercises can help correct muscle imbalances and promote spinal stability.
Postural Education: Chiropractors provide guidance on ergonomic adjustments, proper sitting and standing posture, and lifestyle modifications to prevent further progression of humpback neck. Educating patients about optimal postural habits is essential for long-term management.
Nutritional Support: Nutrition counseling may be recommended to ensure optimal bone health and support the healing process. Adequate intake of calcium, vitamin D, and other nutrients is vital for maintaining strong bones and preventing bone-related disorders.
Prevention and Management of Humpback Neck
Preventing humpback neck involves maintaining good posture, staying physically active, and practicing ergonomic habits. Regular chiropractic care can significantly improve humpback neck and prevent its progression. Patients are encouraged to:
Maintain a healthy weight to reduce strain on the spine
Avoid prolonged periods of sitting or standing in one position
Perform regular stretching and strengthening exercises to support spinal health
Use supportive pillows and ergonomic chairs to maintain proper spinal alignment
Seek prompt medical attention for any signs of spinal discomfort or abnormal curvature
In summary, understanding the causes, symptoms, and treatments for humpback neck empowers individuals to take proactive steps toward spinal health and overall well-being. Chiropractic care offers effective and holistic solutions for managing this condition and promoting optimal posture and mobility. By addressing underlying factors and promoting spinal alignment, chiropractors help patients achieve long-term relief from humpback neck and associated symptoms.
0 notes
Text
Scoliosis treatment in Hyderabad - Dr.SureshCheekatla
Transforming Lives: Scoliosis treatment in Hyderabad with Dr. Suresh Cheekatla
Are you or a loved one struggling with scoliosis, a condition characterized by an abnormal curvature of the spine? Finding effective treatment is essential for managing symptoms and preventing progression. Dr. Suresh Cheekatla offers comprehensive Scoliosis treatment in Hyderabad, combining expertise, advanced techniques, and compassionate care to help patients regain mobility and improve their quality of life.
Understanding Scoliosis
Scoliosis is a spinal disorder that causes the spine to curve sideways in an "S" or "C" shape. While mild cases may not cause significant problems, severe curvature can lead to pain, difficulty breathing, and deformity. Early diagnosis and intervention are crucial for managing scoliosis and preventing complications.
Why Choose Dr. Suresh Cheekatla for Scoliosis treatment in Hyderabad?
Specialized Expertise: Dr. Suresh Cheekatla is a leading expert in spinal disorders, including scoliosis. With years of experience and specialized training, he offers comprehensive evaluation, diagnosis, and treatment for patients of all ages with scoliosis.
Advanced Treatment Options: Dr. Cheekatla utilizes the latest advancements in scoliosis treatment, including innovative surgical techniques and non-surgical interventions, to achieve optimal outcomes for his patients. He customizes treatment plans based on the severity of the curvature, the patient's age, and overall health.
Compassionate Care: Dr. Suresh Cheekatla understands the physical and emotional impact of scoliosis on patients and their families. He provides compassionate, patient-centered care, guiding individuals through every step of their treatment journey with empathy and support.
Multidisciplinary Approach: Dr. Cheekatla collaborates closely with a team of healthcare professionals, including physical therapists, pain management specialists, and orthotists, to provide comprehensive care for scoliosis patients. This multidisciplinary approach ensures that each patient receives personalized treatment tailored to their unique needs.
Treatment Options Offered
Observation and Monitoring: For mild cases of scoliosis, especially in children and adolescents, Dr. Cheekatla may recommend close observation and periodic monitoring to assess the progression of the curvature.
Bracing: In cases where scoliosis is still developing, especially in growing children and adolescents, Dr. Cheekatla may prescribe a brace to help prevent further curvature progression and provide support to the spine.
Surgical Intervention: For severe or progressive scoliosis, surgical intervention may be necessary to correct the curvature and stabilize the spine. Dr. Suresh Cheekatla performs a variety of surgical procedures, including spinal fusion, spinal instrumentation, and vertebral column resection, using advanced techniques to achieve optimal results.
Patient Testimonials
"Dr. Suresh Cheekatla's expertise and compassion transformed my life. Thanks to his skillful hands, I am now living without the pain and limitations caused by scoliosis."
"Dr. Cheekatla's personalized approach to scoliosis treatment gave me hope and confidence. He guided me through surgery with care and support, and I am grateful for the positive outcome."
Conclusion
If you or a loved one is seeking effective scoliosis treatment in Hyderabad, Dr. Suresh Cheekatla offers the expertise, advanced techniques, and compassionate care you need. Schedule a consultation today and take the first step towards a healthier, more active life free from the limitations of scoliosis.
0 notes
Text
Exploring Pediatric Orthopedics: Ensuring Strong Foundations for Growing Bodies🩺
Pediatric orthopedics is a specialized branch of medicine that focuses on the musculoskeletal system of children, from infancy through adolescence. 🩺
As young bodies grow and develop, they encounter a myriad of orthopedic conditions that require careful attention and treatment. You can also browse https://topdoc.com/ to get more information about the pediatric orthopedics.
Let's delve into the realm of pediatric orthopedics, understanding its significance, common conditions, and treatment approaches. 📚

Why Pediatric Orthopedics Matters:
Critical Developmental Phase: Childhood and adolescence are crucial stages of growth and development, during which bones, muscles, and joints undergo significant changes. Any abnormalities or injuries during this period can impact long-term health and mobility.🕵️♂️
Early Intervention: Addressing orthopedic issues in children early on can prevent or minimize complications in adulthood. Prompt diagnosis and treatment can help children achieve optimal musculoskeletal health and function. 🌱
Enhanced Quality of Life: Effective management of pediatric orthopedic conditions improves a child's overall quality of life by promoting physical activity, independence, and participation in daily activities. To get more information about the pediatric orthopedics, you can also navigate this site. ⏰
Common Pediatric Orthopedic Conditions:
Congenital Malformations: Conditions such as clubfoot, hip dysplasia, and limb length discrepancies are present at birth and require early intervention for correction. 🏃♂️
Developmental Disorders: Skeletal disorders like scoliosis (abnormal curvature of the spine), juvenile idiopathic arthritis, and osteogenesis imperfecta (brittle bone disease) can affect bone growth and alignment.
Fractures and Injuries: Children are prone to fractures due to their active lifestyles. Fractures may occur from falls, sports injuries, or accidents and require specialized care to ensure proper healing and alignment.🦴
Infections and Tumors: Infections of the bones and joints (osteomyelitis, septic arthritis) and benign or malignant bone tumors (osteosarcoma, Ewing sarcoma) are less common but require specialized treatment and management.
Neuromuscular Conditions: Conditions such as cerebral palsy, spina bifida, and muscular dystrophy affect muscle tone and coordination, often requiring multidisciplinary care involving orthopedic surgeons, neurologists, and physical therapists.🩹
Approaches to Treatment:
Non-Surgical Interventions: Conservative treatments such as bracing, physical therapy, and activity modification are often the first line of management for many pediatric orthopedic conditions, particularly in milder cases or when the child is still growing.🧠
Surgical Interventions: When conservative measures are insufficient, surgical interventions may be necessary. These can range from minimally invasive procedures to complex surgeries such as spinal fusion for scoliosis correction or limb lengthening procedures for discrepancies.
Multidisciplinary Care: Pediatric orthopedic care often involves collaboration with other specialists such as pediatricians, physical therapists, occupational therapists, and genetic counselors to provide comprehensive management tailored to the child's needs.

Long-term Follow-up: Many pediatric orthopedic conditions require ongoing monitoring and follow-up to ensure optimal outcomes as the child grows. Regular assessments of growth, development, and functional abilities are essential for detecting any recurrence or progression of the condition.🧘♀️
Conclusion:
Pediatric orthopedics plays a vital role in ensuring the musculoskeletal health and well-being of children as they grow and develop. 🌟
From congenital malformations to fractures and developmental disorders, early intervention and appropriate treatment are essential for minimizing long-term complications and maximizing quality of life.
By employing a multidisciplinary approach and staying abreast of advancements in pediatric orthopedic care, healthcare providers can help children thrive and reach their full potential.📈
1 note
·
View note
Text
Spine Specialist in Pune | Dr. Shrikant Dalal
Can a spinal deformity be corrected?
Spinal deformity refers to an abnormal curvature or alignment of the spine, which can result from various factors such as congenital conditions, degenerative diseases, trauma, or poor posture. These deformities can manifest in different regions of the spine and lead to discomfort, limited mobility, and, in severe cases, neurological complications.
Spinal deformities, such as scoliosis, can be life-altering conditions, but the advancements in medical science offer promising solutions for correction. From non-invasive approaches like physical therapy and bracing to surgical interventions, there are diverse methods available to address and correct spinal deformities. Understanding these deformities, their non-invasive treatment options, surgical interventions, post-surgical rehabilitation, and the latest advancements in medical science is crucial. Orthos Centre and Shrikant Dalal one of the best spine specialist in Pune provide comprehensive. Dr. Shrikant Dalal is best spine surgeon for all Spinal problems.
#bestspinespecialistinpune#bestspinecentreinpune#bestspinesurgeoninpune#dr.shrikantdalal#orthoscentre#bestjointreplacementsurgeoninpune#bestspinedoctorinpune
0 notes
Text
Difference between Scoliosis and Kyphosis
Scoliosis and kyphosis are both spinal disorders, yet they differ significantly in their presentation and impact on the body. Scoliosis is characterized by a sideways curvature of the spine, often resembling an "S" or a "C" shape, leading to asymmetry of the shoulders, hips, and waist. This curvature can result in back pain, breathing difficulties, and in severe cases, compression of internal organs. On the other hand, kyphosis involves an excessive outward curvature of the upper back, causing a rounded or hunched posture commonly known as "hunchback" or "roundback." Kyphosis can lead to stiffness, back pain, and in severe cases, compression fractures of the vertebrae, affecting mobility and quality of life.
While both conditions can arise from various causes, including congenital defects, neuromuscular disorders, or degenerative changes, they often manifest differently and require distinct treatment approaches. Scoliosis management may involve bracing, physical therapy, or in severe cases, surgery to straighten the spine. Kyphosis treatment focuses on exercises to improve posture, pain management, and in severe cases, surgical intervention to correct spinal alignment.
Understanding these distinctions is crucial for accurate diagnosis and tailored treatment plans, ensuring optimal outcomes and improved quality of life for individuals affected by these spinal disorders.
You can contact us by:
Phone: +91 9818776763
Email: at Dr. Nagesh Chandra, Top Neurologist in Delhi
Website: Best Brain & Spine Treatment in Delhi
Visit us: at Dr. Nagesh Chandra, Top Neurologist in Delhi
#SPINE DOCTOR IN DELHI#SPINE SURGERY IN DELHI#SCOLIOSIS TREATMENT IN DELHI#NEUROSURGEON IN DELHI#BEST NEUROSURGERY SPECIALIST IN DELHI
0 notes