#but now sunny has a pa who’s safe and warm and will take care of her even when she’s dirty
Text
Sunny coming to the island and not wanting to touch dirt or get her hands dirty because it’s a reminder of the stress and fear from egg island where sunny was constantly dirty, tired and scared. The sight of dirt and the feeling grit making contact with her skin reminds her of falling asleep with Empanada and Pepito hoping that they’ll make it another day.
Sunny now asking when they can start building. Sunny asking when she can get her hands covered in dirt, grease and oil because it’s a reminder of her dad and the way he smells and feels when they hug after a long day of work. It reminds her of the way that he smiles when they finish a build and how his eyes light up when she gets something right with a machine. The feeling of grease on her face and hands is familiar and comforting in a way Sunny never thought it would be.
Dirt and grime no longer mean something bad to Sunny. Instead, it means she’s home safe and sound
#i keep thinking about how sunny asked tubbo when they were going start building today#so different from the first time tubbo asked sunny to help him and sunny immediately said no and dirt was gross#also the fact that they came from egg island and had no one to take care of them#but now sunny has a pa who’s safe and warm and will take care of her even when she’s dirty#tubbo#qsmp tubbo#qsmp sunny#qsmp
185 notes
·
View notes
Note
(tw: death) Hey doc! What are the common reasons children will be in A&E needing CPR? Is it usually due to an allergic reaction or a cardiac arrest? (this question was based on one of your last posts), hope you have had a nice day!
Hello! I did indeed have a nice day today. It was sunny, warm, and I left work at a reasonable time, having had adequate staffing not to be running around like a headless chicken. OK, first the warning: this post is going to discuss child death, suicide, non-accidental injury/abuse. It’s a very sad topic for obvious reasons. That’s why I’m putting it behind the cut…
Firstly, we need to think about the way we think of death. Cardiac arrest means when your heart stops. But technically all death involves that. What we mean when we say ‘cardiac arrest’ is an unexpected stopping of the heart. Children are more likely to suffer respiratory arrest as opposed to cardiac arrest so our focus and our causes can be different in paediatrics. Just like in adult medicine, when the heart stops, and we start doing CPR, this may not ‘fix’ the problem, it is usually buying time whilst we try to figure out if we try to identify if there are any reversible causes for this. We can only ‘fix’ things if we can find a cause that we can reverse. I have seen no better example of human cooperation, ingenuity and love than what I’ve witnessed taking part in crash calls.
Compared to adults, children experience respiratory or cardiac arrest more rarely; I didn’t see it very often when I worked in paeds, and some of my registrars (with 4+ years of paeds training) hadn’t seen one at all. That’s not to say that children don’t die; unfortunately sometimes it is unavoidable. Incurable childhood cancers and inherited diseases are not common, but they happen. When most of these children die, it is heartbreaking, but not unexpected. In these instances, the children, like adults, will have been not for resuscitation, because it was expected for them to die from their illness, and that could not be reversed. Or they would be unable to deal with the intensive support their body would need if they were rescuscitated. So some children who die will never be treated as a crash call, because it was expected and there was nothing that could be done to reverse the cause of their death. And the last thing any of us would want, would be to subject a dead child and their family to CPR if we knew it would be futile. Children with severe or chronic disorders can still come in with cardiac arrest; however, often their condition may be a complicating factor, or even the reason that they come in. To keep things simple, we won’t focus on rare diseases and how those children can present very, very unwell, but that’s something to consider if you are an on-call paediatrician. There’s always a first time for a rare condition to present, and that might be when your patient comes in very, very sick. Going back to more common causes, some of the kinds of things that might bring a child in are:
choking (for example on toys)
drowning
asthma
severe respiratory infections
sepsis or meningitis
allergic reactions.
electrocution
severe accidents
drugs/poisoningI’ve found a couple of good explanations here and here.
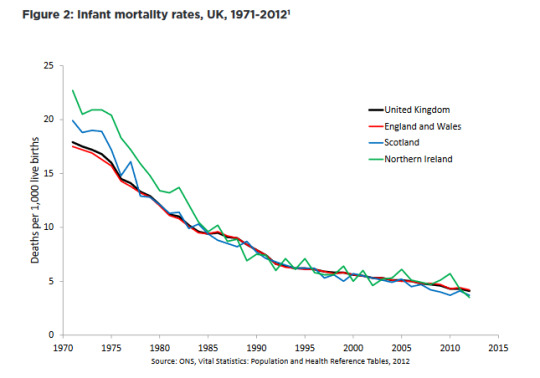
Kids are more likely to get into accidents or choke on things or drown, or accidentally electrocute themselves. They can accidentally take mum’s medicines, or poison themselves with whatever is lying around at home. Looking after children is a minefield. Injuries are the third most common cause of child death in the UK after the age of 1. Car accidents are a leading cause. I’m also going to mention the thing nobody wants to talk about; non-accidental injury can lead to child death. Most injuries, whether they cause death or cardiac arrest, are fortunately accidental, but we can’t ignore non-accidental injury, because in paeds that must always be at the back of your mind. You are always on the lookout for warning signs that any trauma could be non-accidental. I want to mention, too, that street violence (like stabbings) cannot be ignored, though it may not be a major cause, it is nevertheless a senseless, unnecessary and horrific thing to go through, and underprivileged children and minorities, particularly black boys are at increased risk of gang violence and knife crime. Any society in which children feel their only recourse is carrying knives or joining gangs is failing those children. I also want to mention, that equally horrifically, that for older children and teenagers, suicide is a considerable cause of death. The RCPCH figures make for grim reading. The youngest (likely) suicide I’ve seen was 19 years old. Though admittedly not a paeds patient it is still a case I remember clearly; I wish she could have seen how hard we tried to save her, how many people cared so much for her. One thing we don’t like is SIDS; sudden infant death syndrome. We don’t like it because we unfortunately still don’t 100% know what causes it, though the ‘back to back’ initiative has made lots of progress. We also don’t like it because on a paediatric night shift, there’s a distinct nervousness in the air when it gets too quiet in the morning. They call it ‘SIDS o’clock for a reason, because it’s the time of day when parents go to wake their baby for a feed and find them not breathing; unclear how long they had been that way. There are few more horrific things than seeing chest compressions being done on a lifeless baby. Sudden cardiac death in children who aren’t babies is relatively rare, but it can still happen, and the causes are different than in older people. Younger people may have an underlying heart condition, and this can be genetic. In families where there has been any sudden death of a young person, genetically transmitted cardiac conditions should be investigated for; these things are rare but they can be prevented once the warning signs have been seen.Before we get too despondent about it, it’s worth pointing out that overall, child mortality is decreasing, and has gone down significantly (figure from the RCPCH report):
That report is really interesting, because it breaks things down into pie charts like this:
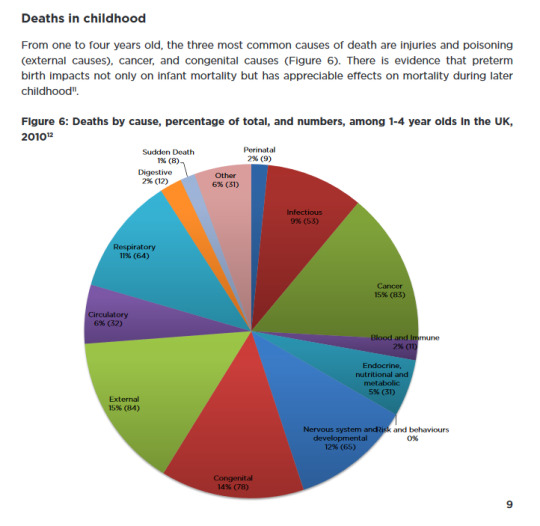
And it actually has different pie charts for different ages, so you can chart that for example, babies re more likely to die of some things, and teenagers are more likely to die of other things.
That’s just data from the UK. On an international level, it’s a bit different. If we look at this chart from the WHO regarding child mortality from the ages of 1-5, it’s quite useful:
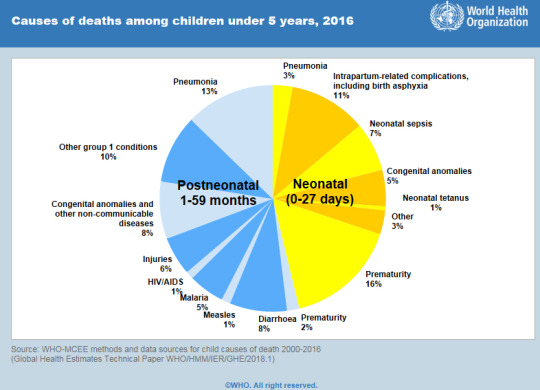
Now, this is a little different, because it’s all the causes of death around the world. For example, children rarely die of diarrhoea in the UK, but it is much more common in countries where there are particular endemic pathogens, or where there are large numbers of children in poverty unable to have basic sanitation, safe drinking water or medical help. The yellow and blue bits are to scale, by the way, Neonatal deaths accounted for 46% of under-five deaths in 2016. Being a newborn baby is a particularly hazardous time, and in paeds we have a very low threshold for admitting babies if they are at all sick. You’ll note I shifted from ‘cardiac arrests’ and ‘CPR’ to deaths; obviously not all respiratory or cardiac arrests lead to death, though the mortality rate is high, even in children. Unfortunately, the figures for mortality are easier to dig out than those for arrests, but I think they are nevertheless useful. I hope this helps, even if it is rather a downer. After reading this, you’ll probably need to go off and do something you enjoy, because it’s truly depressing reading, and I’m sorry that it’s an upsetting topic, but an important one; we cannot save children if we don’t know what they are facing.
22 notes
·
View notes
Photo

Beautiful, Cats, and Children: Sweet special beloved & beautiful- Sunny ld 62509, 2 Yrs, 50 Lbs. of Perfection, at Staten Island ACC INTAKE DATE – 5/11/2019 With eyes as the color of caramel, and just as soft and sweet, SUNNY is a gem of a dog who is stunning in every way. Just a youngster and puppy playful, she flashes her beautiful smile and wins the hearts of everyone around her. She is incredibly friendly and social, and she so deserves a long and happy life with a family who will love and cherish her. Just read all the accolades from volunteers below who all adore this amazing girl, then rush to foster or adopt her now. Message our page or email us at [email protected] for assistance. A staff member writes: “Some people start the day with coffee, some start it with tea, but why not start your day with a large helping of Sunny D! Sunny D is a friendly girl who likes to solicit attention at the front of her kennel to all who pass by. She likes to play in the yard and run around, she surely is full of vibrant energy. She is a mere two years old, so you will still get lots of that playful "puppy prowess". Why not come down and start the next day of your life by picking up our Sunny D and taking her home to cherish!” Volunteer Sandra McDonald writes: “Sunny D has the perfect name !!! She so cheerful and fun shes sure to brighten even the gloomiest day. Sunny loved every person she met and was happy to meet Max thru the fence. She’s a great dog.” Another staff member writes: “Sunny D was found as a stray and is looking for a new home. She's really sweet, and so full of life! She's in adoptions now at SIACC.” MY MOVIE: Hazel Eyed Honey http://bit.ly/2JSamkg SUNNY D, ID# 62509, 2 yrs old, 50.6 lbs, Unaltered Female Staten Island ACC, Large Mixed Breed, Tan / White Surrender Reason: Found Stray Shelter Assessment Rating: LEVEL 3 No children (under 13) Medical Behavior Rating: BEHAVIOR NOTES Means of surrender (length of time in previous home): Stray, no known history SHELTER ASSESSMENT SUMMARIES - Date of assessment: 15-May-2019 Summary: Leash Walking Strength and pulling: Moderate Reactivity to humans: None Reactivity to dogs: None Leash walking comments: Sociability Loose in room (15-20 seconds): Fearful, avoids Call over: Approaches with coaxing, wary, tense, whale-eyeing Sociability comments: Handling Soft handling: Tolerates contact, tense Exuberant handling: Tolerates contact, tense Handling comments: Arousal Jog: Follows, a bit fearful, low body Arousal comments: Knock Knock Comments: No response Toy Toy comments: Freezes, growls MEDICAL BEHAVIOR - Date of initial: 15-May-2019 Summary: Tense, growling ENERGY LEVEL: Sunny D displays a high energy level in the care center. We recommend daily mental and physical stimulation as a way to direct her energy and enthusiasm. IN SHELTER OBSERVATIONS: During her stay in the care center, Sunny D has displayed social behavior with familiar handlers, seeking attention and accepting pets. When newer handlers approach to interact with Sunny D, she appears timid and moves away and avoids (whale eyeing). She has been observed to warm up with the use of treats, however. BEHAVIOR DETERMINATION: Level 3 Behavior Asilomar TM - Treatable-Manageable Recommendations: No children (under 13) Recommendations comments: No children (under 13): Due to Sunny D's overall level of fear and discomfort combined with her resource guarding concerns, we feel she would be best set up to succeed in an adult only home environment. Potential challenges: Resource guarding Fearful/potential for defensive aggression Potential challenges comments: Sunny D was observed to freeze and growl while approached while engaged with a toy item, please see handout on Resource guarding. Sunny D appears fearful of strangers initially and will avoid contact. She has displayed appropriate warning signals (lip licking, whale-eyeing, moving away). When she has been highly uncomfortable though she has escalated to growling and snapping. Please see handout on Fearful and defensive aggression as well as Decompression period. MEDICAL EXAM NOTES 15-May-2019 DVM Intake Exam Estimated age: 2 years History : stray Subjective: Observed Behavior - tense, growling and snapping during exam Evidence of Cruelty seen - no Evidence of Trauma seen - no Objective BCS 5/9 EENT: Eyes clear, no nasal or ocular discharge noted Oral Exam: muzzled, no oral exam PLN: No enlargements noted H/L: NSR, NMA, CRT < 2, Lungs clear, eupneic ABD: Non painful, no masses palpated U/G: Female, no spay scar seen MSI: Ambulatory x 4, skin free of parasites, no masses noted, superficial abrasion at nares CNS: Mentation appropriate - no signs of neurologic abnormalities Assessment appears healthy Prognosis: good Plan: gave 0.46 mls morphine and 0.14 mls dexdomitor IM after giving premedication, elected to postpone surgery until after behavior evaluation SURGERY: Okay for surgery 11-May-2019 LVT Intake Exam Microchip Scan: negative Evidence of Cruelty: no Observed Behavior: relaxed body, mouth open, ears forward, tail wagging low. Allowed all treatments with minimal restraint. Sex:FI Estimated Age:2 years Subjective: stray Ears: minimal waxy debris Eyes: clear, no discharge noted Nose: no discharge noted Teeth: patient did not allow full mouth exam, minimla tartar on cranial teeth, some food debris present on canines Heart: NSR, no murmurs auscultated Lungs: clear Abdomen: soft, non-painful Musculoskeletal: Ambx4, BCS 4/9 Integument: healthy coat and skin, free of external parasites Urogenital: FI- no spay scar noted Mentation: BAR Preliminary Assessment: Healthy Plan: DVM Exam...spay...RV *** TO FOSTER OR ADOPT *** If you would like to adopt a NYC ACC dog, and can get to the shelter in person to complete the adoption process, you can contact the shelter directly. We have provided the Brooklyn, Staten Island and Manhattan information below. Adoption hours at these facilities is Noon – 8:00 p.m. (6:30 on weekends) If you CANNOT get to the shelter in person and you want to FOSTER OR ADOPT a NYC ACC Dog, you can PRIVATE MESSAGE our Must Love Dogs page for assistance. PLEASE NOTE: You MUST live in NY, NJ, PA, CT, RI, DE, MD, MA, NH, VT, ME or Northern VA. You will need to fill out applications with a New Hope Rescue Partner to foster or adopt a NYC ACC dog. Transport is available if you live within the prescribed range of states. Shelter contact information: Phone number (212) 788-4000 Email [email protected] Shelter Addresses: Brooklyn Shelter: 2336 Linden Boulevard Brooklyn, NY 11208 Manhattan Shelter: 326 East 110 St. New York, NY 10029 Staten Island Shelter: 3139 Veterans Road West Staten Island, NY 10309 *** NEW NYC ACC RATING SYSTEM *** Level 1 Dogs with Level 1 determinations are suitable for the majority of homes. These dogs are not displaying concerning behaviors in shelter, and the owner surrender profile (where available) is positive. Some dogs with Level 1 determinations may still have potential challenges, but these are challenges that the behavior team believe can be handled by the majority of adopters. The potential challenges could include no young children, prefers to be the only dog, no dog parks, no cats, kennel presence, basic manners, low level fear and mild anxiety. Level 2 Dogs with Level 2 determinations will be suitable for adopters with some previous dog experience. They will have displayed behavior in the shelter (or have owner reported behavior) that requires some training, or is simply not suitable for an adopter with minimal experience. Dogs with a Level 2 determination may have multiple potential challenges and these may be presenting at differing levels of intensity, so careful consideration of the behavior notes will be required for counselling. Potential challenges at Level 2 include no young children, single pet home, resource guarding, on-leash reactivity, mouthiness, fear with potential for escalation, impulse control/arousal, anxiety and separation anxiety. Level 3 Dogs with Level 3 determinations will need to go to homes with experienced adopters, and the ACC strongly suggest that the adopter have prior experience with the challenges described and/or an understanding of the challenge and how to manage it safely in a home environment. In many cases, a trainer will be needed to manage and work on the behaviors safely in a home environment. It is likely that every dog with a Level 3 determination will have a behavior modification or training plan available to them from the behavior department that will go home with the adopters and be made available to the New Hope Partners for their fosters and adopters. Some of the challenges seen at Level 3 are also seen at Level 1 and Level 2, but when seen alongside a Level 3 determination can be assumed to be more severe. The potential challenges for Level 3 determinations include adult only home (no children under the age of 13), single pet home, resource guarding, on-leash reactivity with potential for redirection, mouthiness with pressure, potential escalation to threatening behavior, impulse control, arousal, anxiety, separation anxiety, bite history (human), bite history (dog) and bite history (other).
0 notes