#papillary layer
Text
Dermis
Layers Of The Dermis
The dermis layer is located inferior to the epidermis layer in the cutaneous layer. This layer is made of connective tissue and can be divided into two layers:
Papillary LayerReticular Layer
https://www.researchgate.net/figure/Adult-human-skin-is-a-layered-organ-consisting-of-an-epidermis-and-a-dermis-The_fig1_233976352
The papillary layer of the dermis is the most…

View On WordPress
#aging#anatomy#animals#biology#blog#collagen#college#cutaneous#cutaneous membrane#epidermis#facts#fibers#follow#human anatomy#hypodermis#nature#Nerves#neurons#papillary layer#photography#plexus#reticular layer#science#skin#stretch marks#subscribe#tension lines
3 notes
·
View notes
Text
Chemical Peels for Melasma(Pigmentation) in Dark-Skinned Patients
Individuals with melasma, a skin disorder marked by dark or gray spots that appear on the skin's surface, may experience severe emotional distress. It is true that chemical peels are an advanced treatment option for reducing pigmentation. However, individuals with dark skin tone, wonder if chemical peels help with dark skin tone. Chemical peels slough off dead surface skin, they must be used with caution. A frequent myth is that persons with dark skin cannot have chemical peels. It's understandable given that some people have damaged skin and a condition known as post-inflammatory hyperpigmentation (dark patches). Nevertheless these are the exception, not the rule.

It all comes down to the sort of peel used and your doctor's experience with dark skin. So, in this article, we'll go over the many types of chemical peels and how they can affect skin of colour. The information is gathered from the insights shared by the expert dermatologists of Skination Clinic. The clinic that is renowned for providing the best pigmentation treatment in Faridabad. This skin facility is known for conducting advanced chemical peels on dark skin. In this post we'll also give you some pointers on how to make the procedure go as smoothly as possible.
Types of Chemical Peels
Before getting a chemical peel, it's important to understand both the different types of peels and what's in them. This knowledge will assist you in understanding what is happening during your peel and determining whether what your doctor is recommending is appropriate for you. Chemical peels are divided into three types: superficial peels, medium-depth peels, and deep peels.
Superficial Peels- They target your skin's stratum corneum, also known as the epidermis. These peels might reach all the way to the top of the papillary dermis.
Medium-Depth Peels- It affects the dermis, or middle layer of your skin. This layer extends from the papillary dermis to the middle of the reticular dermis. Medium-depth peels are far more effective in removing dead skin cells and dissolving scars.
Deep Peels- They penetrate deep into the skin's inner layer, breaking up severe acne scars and hyperpigmentation. Deep peels are only performed under the guidance of a skilled dermatologist. These peels have lengthy healing durations and should be performed with prudence.
The chemical peel will contain either alpha-hydroxy acid (AHAs) or beta-hydroxy acid (BHAs). AHAs are plant and animal-derived acids. These, in various quantities, can exfoliate your skin, lighten it, stimulate blood flow, and collagen synthesis. BHAs are oil-based organic compounds that can unclog pores, reduce oil, clear acne, and do a variety of other things.
Why is Dark Skin Such a Source of Concern?
People of color, with dark complexion or the many gorgeous colors of brown, account for nearly one-third of our population. While skin seems different on the exterior, its genetic makeup is nearly identical on the inside. We all have the same melanocytes, or melanin-producing cells.
People of color, on the other hand, create significantly more melanin at the surface level. The pigment called melanin is what gives our skin and hair their color. However, it also shields the skin from the sun's damaging ultraviolet radiation. One notable benefit is that darker skin tones are significantly more shielded from UV rays than lighter skin tones.
Dark skin, on the other hand, is more likely to react poorly to skin injury, resulting in conditions such as melasma, hyperpigmentation, textural changes, and more. Furthermore, because chemical peels purposely damage and remove layers of skin, there is a risk of an adverse reaction.
There is also concern that persons of color are under-represented in dermatology. Many skin specialists would choose to avoid certain treatments owing to a lack of experience, believing that it is better to be safe than sorry. Nonetheless, a lot of progress has been made in solving this problem. More and more doctors and aestheticians are learning how to aid people with darker skin tones. Furthermore, there is an increasing number of dermatologists of color.
Consider Consulting The Experts
One such expert is the skilled team of doctors of Skination Clinic. The leading doctors, Dr. Swati Agarwal and Dr. Rajat Gupta who are known for providing advanced medical and aesthetic treatments for all skin types and skin color. In addition to general dermatology, the experts specialize in aesthetic services, lasers, and hair loss treatments. They are certified in injectables, such as anti-wrinkle injections and fillers, as well as lasers. While providing any skincare service, they take extra care to assure the skin's safety, integrity, and beautiful appearance.
Having been treated by such skilled dermatologists can help you select the best peel for your skin condition. To learn more, one can consult them.
Best Chemical Peels for Melasma
Chemical peels used to cure melasma that contain a number of different chemicals with various modes of action are:
Azelaic Acid is a bleaching chemical that is used to lighten skin tone and treat pigmentation problems such as melasma. Azelaic acid inhibits melanin production in overactive melanocyte cells and is suitable for all skin types.
Glycolic Acid peels are a typical type of alpha hydroxy acid peel that is excellent for melasma treatment.
Kojic Acid is a tyrosinase inhibitor, which means it works to prevent pigmentation in the skin. Kojic acid is utilized in the composition of the Cosmelan peel to remove melasma and is safe to use on all skin types.
Lactic Acid is another alpha hydroxy acid that is used in the formulation of chemical peels like the Jessner peel. Lactic acid is suitable for every type of skin.
Salicylic Acid is a beta hydroxy acid that is often used in chemical peels to treat acne and acne scars. Salicylic acid, lactic acid, and resorcinol are commonly utilized in the composition of Jessner's solution. Jessner's peel is a popular superficial chemical peel that works on all skin tones. Salicylic acid is also anti-inflammatory, which lowers the risk of developing post-inflammatory hyperpigmentation.
Tretinoin (retinoic acid) can be used to treat acne and sun-damaged skin. Tretinoin is frequently used to address wrinkles, fine lines, and dark spots on the skin.
Trichloroacetic Acid, found in a trichloroacetic acid or TCA peel, is more typically utilized for patients with lighter skin because those with darker skin are slightly at risk of major side effects. TCA peels are also ineffective for treating non-surface level melasma, which is melasma present in the dermis.
How To Begin with a Chemical Peel Treatment?
One can consult the skilled skin doctor in Faridabad, Dr. Rajat Gupta or Dr. Swati Agarwal of Skination Clinic. They are expert dermatologists who are chemical peel experts, treating patients of all skin types, including those with dark skin tones.

The expert doctors can help you whether your hyperpigmentation or melasma is the result of laser treatment, sun exposure, or acne breakouts. The doctors treat patients with various skin types and will advise you on the finest skin care products, sunscreens, and chemical peels to improve discolouration and rejuvenate your skin tone and texture. Please visit at Skination Clinic to find out which chemical peel treatment is ideal for you. Start your journey towards a new you now!
Original Source:- https://www.hashtap.com/@skinationclinic/chemical-peels-for-melasma-pigmentation-in-dark-skinned-patients-NVlQL9AXJ9l8
#skin doctor in Faridabad#Best Chemical Peels For Melasma#Types Of Chemical Peels#Chemical Peels For Melasma#Pigmentation Treatment#pigmentation treatment in Faridabad
0 notes
Text
Skin
The skin is actually the largest organ and it actually makes up 15 per cent of your bodyweight. The average person roughly 10kg covering two square metres. Your skin does many things. It:
Contains nerve receptors that allow you to feel touch, pain, and pressure
Helps control fluid and electrolyte balance
Helps control your body temperature
Protects you from the environment
This system acts as a protective barrier between the external environment and the inside of the body, shielding the internal organs against heat, light, injury and infection. In addition, skin plays an important role in regulating body temperature, preventing water loss, producing vitamin D and detecting sensations caused by mechanical stimuli that make contact with or put pressure on the skin.
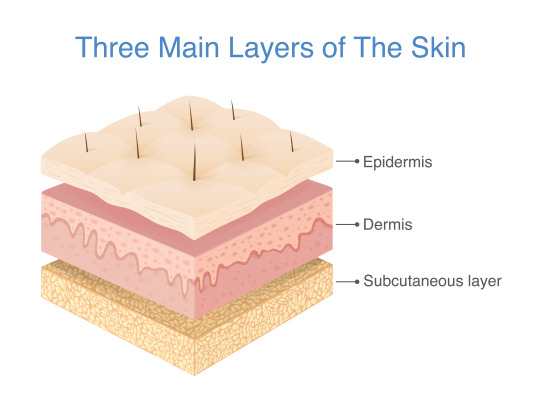
Our outer organ is made up of two main layers. The outer ‘epidermis’ is as thin as a sheet of paper, yet it accounts for most of the skin’s barrier functions. The ‘dermis’ beneath is thicker and carries out a diverse range of roles: collagen and elastin give skin its shape, plumpness and elasticity, over 17 kilometres of blood vessels – enough to bridge the Strait of Gibraltar – and millions of sweat glands regulate body temperature by retaining or releasing heat, exquisitely sensitive nerve receptors enable us to feel our way through life and a standing army of immune cells waits for any foreign intruder.
Your paper-thin epidermis is scratched, squashed and stretched thousands of times a day, but it doesn’t break – at least not easily– or wear out. This is because the wall of the skin is constantly being supplied with new, living bricks: keratinocytes. These cells are made up of the tough protein keratin, which is unbelievably strong: it also forms our hair and nails, as well as the unbreakable claws and horns found in the animal kingdom.
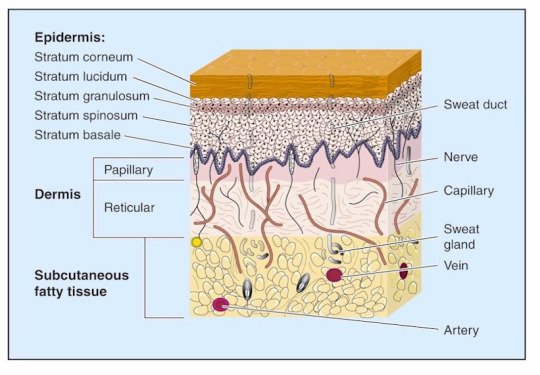
Epidermis
The epidermis is a complex ‘brick wall’ made of cells called keratinocytes, which produce a protein called keratin. The epidermis also contains pigment cells called melanocytes, which produce melanin, Langerhans cells, which present antigens to the immune system, and Merkel cells, which have a sensory function.
Basal layer — the columnar or rectangular cells at the bottom of the epidermis from which new cells are continuously produced. Scattered melanocytes are normally found in this layer.
Squamous cells — flat epithelial cells found on the skin surface. The structure of the skin is described as a stratified squamous epithelium, referring to the way the cells are built up in layers.
Granular layer — flattened cells filled with dark granules containing keratohyaline protein.
Horny layer — stacks of dead cells without nuclei make up the dry or keratinised stratum corneum. The top layer of cells loosens and falls off.
Desmosomes — the structures that stick adjacent keratinocytes tightly together, rather like cement between bricks.
Epidermal appendages include:
Eccrine glands, which produce sweat
Apocrine glands, scent glands found in armpits and groins
Pilosebaceous structures containing hair and sebaceous glands
The dermis
The dermis is made up of connective tissue that supports the epidermis, providing nutrients and protecting it. The papillary dermis is the upper portion beneath the epidermis, and the lower portion is the reticular dermis.
Collagen — a structural protein making up the bulk of the dermis. It is produced by fibroblasts. It is composed of a triple helix of strong fibres.
Elastin — the protein that makes up thin elastic fibres. These are produced by fibroblasts. They return deformed skin to its resting position.
Ground substance — the gel component of the dermis. It contains hyaluronic acid, dermatan sulphate, and chondroitin-6-sulphate (these are anionic polysaccharides or glycosaminoglycans).
Fibroblasts — cells found in the dermis that produce collagen, elastin, ground substance and fibronectin (a glycoprotein).
Nerves — sensory and autonomic fibres with distinct nerve endings for touch, heat, cold, pressure and pain.
Blood vessels — arteries, arterioles, capillaries, venules and veins carrying blood to and from the skin.
Lymphatics — an extensive network of thin-walled vessels that nourish and drain the skin.
Arrector pili muscles — these are attached to hair follicles. Contraction results in goosebumps.
Cellular infiltrations — immune cells around blood vessels, and recruited in great numbers to heal wounds and fight infection. Many skin diseases are characterised by specific patterns of these cells.

Dr Monty, Lyman (2019) 10 remarkable facts about skin. https://www.sciencefocus.com/the-human-body/10-remarkable-facts-about-skin (Accessed: November 10, 2023).
0 notes
Text
Unlock Youthful Skin with Fibroblast Plasma Blushing at Estrella Collective
Are you seeking a cutting-edge solution to combat the signs of aging and rejuvenate your skin? Look no further than Estrella Collective in Santa Cruz, California, where Fibroblast Plasma technology is revolutionizing the way we approach aging. In this article, we'll delve into the world of Fibroblast Plasma Blushing, exploring what it is, how it works, and what you can expect from this innovative cosmetic procedure.
What is Fibroblast Plasma Blushing?
Fibroblast Plasma Blushing is a groundbreaking cosmetic procedure that harnesses the power of plasma arc energy to rejuvenate and tighten your skin. Using a specialized pen-like device, this non-surgical treatment creates controlled micro-abrasions on the skin's surface, resulting in the appearance of tiny dots. These dots are strategically placed to enhance your unique facial features. More importantly, they stimulate the fibroblast cells in the dermal and papillary layers of your skin, kickstarting the collagen production process and ultimately leading to skin tightening.
The Science Behind Plasma Pen Therapy
Plasma fibroblast therapy employs a pen-like device that emits a high-frequency electric current precisely above the skin, without direct contact. This current generates small, controlled injuries or micro-injuries on the skin's surface. These micro-injuries target the fibroblast cells in the dermal layers, breaking down proteins within the skin. This process initiates tissue regeneration, stimulates fibroblast activity, and triggers tissue contraction, effectively tightening the skin.
The Transformative Power of Fibroblast Plasma Pen Therapy
Wondering what Fibroblast Plasma Pen therapy can do for you? This innovative treatment offers remarkable results, with the effects lasting for up to three years. It is particularly effective for addressing loose and wrinkled skin, particularly in areas such as the face and neck. In the past, these concerns were often addressed with surgical procedures or dermal fillers. However, with the advent of Plasma Pen therapy, you can achieve a more youthful appearance without going under the knife.
What to Expect During the Healing Process
The healing process following Fibroblast Plasma Pen therapy can vary from person to person. However, here's a general timeline to help you understand what to expect:
Dot Removal: Typically, the tiny dots created during the procedure will naturally fall off within 8 to 10 days. However, this timeframe can vary, with some individuals experiencing quicker or slightly longer healing periods. It's important not to scratch or scrape off the dots, as this can interfere with the healing process.
Swelling: Swelling is a common side effect, particularly around the eyes, in the days immediately following the treatment. This swelling should begin to subside around the 3rd or 4th day.
For more detailed information on the healing process and aftercare, we invite you to explore our Before/After Care blog posts.
Conclusion
Fibroblast Plasma Blushing at Estrella Collective in Santa Cruz, California, offers a cutting-edge solution for achieving youthful, rejuvenated skin. This non-surgical procedure utilizes the power of plasma arc energy to stimulate collagen production and tighten your skin, with results that can last up to three years. If you're ready to take control of your aging and enhance your natural beauty, consider the transformative benefits of Fibroblast Plasma Pen therapy. Say goodbye to wrinkles and hello to radiant, youthful skin at Estrella Collective.
#Fibroblast Plasma Blushing#Fibroblast Plasma santa cruz#fibroblast plasma treatment#plasma fibroblast near me#Fibroblast Plasma
0 notes
Text
7 Ways To Reduce Acne Scars

The most uncomfortable aspect of having acne is the appearance of acne scars. Scars from acne are fairly common, so one should not feel self-conscious about them. Acne scars are temporary, though. There are some available therapies. While some treatments use the skin's own collagen to help the skin recover, some therapies virtually eliminate the scars.
One in five people between the ages of 11 and 30 will have scarring, while 80% of people will have acne. The social life of individuals may be impacted by acne scars, which can also lower their self-esteem and lead to psychological anguish.
Acne breakouts frequently result in indentation scars known as pitted acne scars. People frequently struggle to get rid of acne scars, and they do not disappear rapidly. However, various treatment methods may help minimise the look of acne scars. But are they safe? This blog will try to answer all the related concerns and questions and will include a discussion on different treatment options for acne scars.
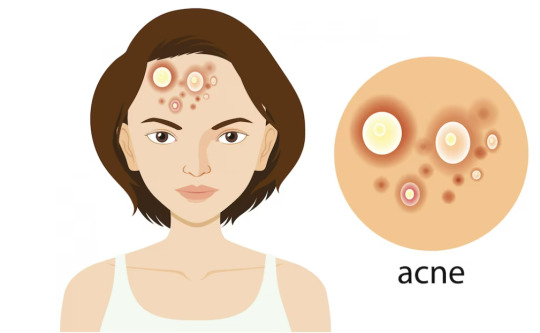
What Causes Acne Scars?
Before treating acne scars, one should understand the reason for their occurrence. One should remember that prevention is preferable to treatment; therefore, if individuals take care of their skin, they will not have to worry about scars. Here are some of the causes of breakouts and scars:
Breakouts caused by puberty.
Inflammation and cystic acne.
Acne popping.
Direct exposure to sun rays.
Pollution
Use of harsh skincare products and medications.
Visit a top dermatology hospital as soon as possible to get skin treatment in Mangalore before your acne scars become deeper.
Types of Acne Scars
Treatment solutions may differ slightly based on the type of scarring caused by acne. There are three major kinds:
Atrophic Scars
Small indentations in the skin appear as scars. They happen when the skin doesn't produce enough fibroblasts during the healing process. Fibroblasts are cells that help with wound healing and collagen formation.
Hypertrophic Scars
These develop when the skin produces more fibroblasts while the acne area heals, resulting in a raised scar.
Keloid Scars
These scars resemble hypertrophic scars but are thicker than the original acne area. Hyperpigmentation occurs frequently, making them darker than the surrounding skin. They can be either red or brown. Itching or pain may also occur.
How are Acne Scars Reduced?
The methods for reducing acne scars vary depending on the types of scars the individual is suffering from and their severity. Hence, it is recommended not to start the treatment immediately until the acne is completely cured. Some of the common ways of reducing acne scars include some dermatological treatments, which are discussed below:
Resurfacing Procedures
Laser therapy, dermabrasion, microdermabrasion, and chemical peels can all help improve the appearance of shallow acne scars. They all entail removing layers of skin cells in order to stimulate the skin's production of new cells. If someone has darker skin, they should avoid dermabrasion, which can cause scarring and discolouration. Some laser therapies may also achieve this; however, Nd: YAG lasers are often safer for darker skin.
There are two types of laser resurfacing: ablative and non-ablative. The ablative laser eliminates a small amount of skin to reveal a smoother texture. The non-ablative laser produces heat and collagen. The laser induces damage to trigger the wound-healing process. It also encourages dermal fibroblasts to replenish depleted collagen and elastin. Laser resurfacing is a non-invasive, rapid procedure that requires 6 to 8 treatments.
Dermabrasion involves the removal of the epidermis to modify the skin's structural proteins in the reticular dermis (the thick bottom layer of the dermis). This procedure reorganises the papillary dermal collagen without harming the reticular dermis. It is the best treatment for healing rolling scars or boxcar scars. However, this treatment may raise the risk of sun sensitivity and photodamage. Hence, one should always protect their skin after treatment to avoid hyperpigmentation.
Fillers
Shallower scars can be filled in by the dermatologist with substances such as hyaluronic acid, collagen, or the body’s fat. Although some fillers are permanent, the effects usually last a few months. There is no downtime, and it adds volume to the scar. However, it is only a temporary remedy because the body's enzymes gradually break down the fillers.
Micro Needling
If someone has a lot of depressed acne scars, they should consider collagen induction therapy. A motorised micro needling pen with rotating needles is used. The pen is used to stimulate collagen formation in depressed acne scars.
Micro-needling involves healing the skin by causing injuries to stimulate collagen formation. When paired with radiofrequency, the energy is released deeper into the skin. It increases the inflammatory response and remodels the dermal collagen. This is one of the most successful methods for reducing indented scarring with few adverse effects.
Radiofrequency Skin Tightening
Deep ice pick and boxcar scars can sometimes be efficiently treated with this treatment. A doctor will use radio frequency to tighten skin and conceal depressed acne scars.
Subscision
A sterile needle is inserted under the skin and used to rupture fibrous scar tissue and "loosen" depressed scars. Multiple sessions are required to attain the desired outcomes. The technique is more effective in treating rolling scars. Combining subcision with other scar repair treatments may yield superior results.
Injections
A series of corticosteroid injections may flatten and soften elevated and thick scars.
Surgery
Surgery involves elevating or splitting up tissue to minimise the look of depressed acne scars. Cryosurgery removes elevated acne scars, but it is not suggested for individuals with darker skin.
Consult a skin specialist in Mangalore to get best treatment and care for acne scars.
0 notes
Text
Never have I ever heard the phrase 'nipple shaped' used to describe something as much as I have today when learning about the papillary layer
0 notes
Text
What Causes Retinal Detachment Most Frequently?
If you can recognize the warning signs and act quickly, the likelihood of a positive outcome is significantly increased.
The retina is frequently compared to camera film. The retina is a thin layer of nerve tissue that borders the back of the eye. Via our pupils, the retina collects light rays, which the retina then uses to convey electrical signals to our brain via the optic nerve. This makes it possible for our brain to process and understand the visual data around us.
As the vitreous, a material that fills the interior of the eye and resembles gel, shrinks, it causes a hazardous condition called retinal detachment. As a result, the retina could be pulled or torn. When vitreous fluid leaks into the tear and pulls the retina away from the back of the eye, it causes retinal detachment. If left untreated, retinal detachment can result in permanent vision loss.
Although it can also be brought on by injury, myopia, eye surgery, and ocular inflammations, age-related vitreous shrinkage is a disease. There are a lot of warning signs and symptoms for retinal detachment. These include:
Sudden appearance of dark spots (floaters)
Unexpected light flashes
Foggy vision or vision with dark shadows
In Singapore, there are several retinal detachment therapies available, including:
Laser photocoagulation with a thermal barrier
When a patient has very little detachment and is diagnosed very early, thermal barrier laser photocoagulation may be used.
Papillary retinopexy
Pneumatic retinopexy is a possibility for patients who suffer retinal fractures at the top of the retina. A gas bubble is injected into the eye's rear to flatten the damaged retina. After that, laser photocoagulation is used to seal the retinal cracks.
The scleral buckle
To indent the sclera over the site of the retinal break, the white of the eye is sutured with a silicone band. Cryopexy is then used to seal the fractures (freezing). This band cannot be seen from the outside of the eye.
Vitrectomy
During a vitrectomy, the vitreous is removed to relieve pressure on the retina, the retinal breaks are encircled with laser photocoagulation, and gas is injected into the eye while waiting for the laser to scar and close the cracks. Following surgery, a face-down position must be kept for two weeks.
One in every 300 persons with otherwise healthy eyes has a lifetime chance of retinal detachment. This risk increases to one in every twenty in people with severe myopia. If you've already experienced retinal detachment in one eye, your risk of having it in the other eye increases to 20%.
Please visit Eye Max Centre for further details on retinal tears and detachments as well as the treatment of retinal illnesses.
0 notes
Text
What is Sylfirm X?

Sylfirm X is the first FDA approved radio-frequency (RF) micro-needling treatment that uses dual wave (a combination of continuous-wave and pulsed wave) for the treatment of skin rejuvenation, scars, pigmented and vascular lesions like melasma, diffuse redness and rosacea.
Sylfirm X has 8 different modes which enables it to be customised to different treatment sites and conditions. Sylfirm X also has the widest depth range of 0.3 – 4.0mm compared to other micro-needling RF systems in the market.
Unlike its predecessor SYLFIRM, the new SYLFIRM X has the widest depth range of 0.3-4.0mm among other micro-needling RF systems. A depth of 0.3mm enables it to target the papillary dermis or the upper dermal layer that is located just below the basement membrane, where senescent fibroblasts and type III collagen are largely distributed and is an important place to interact with the epidermis as this is the ideal depth to target when trying to eradicate stubborn pigmentation.
Another unique feature of SYLFIRM X over older generation and other similar equipment is the option to choose between pulsed mode (which is not commonly available) and continuous mode, giving your doctor better control over the treatment, which is especially useful for difficult to treat conditions
0 notes
Text
Papillary cystadenoma lymphomatosum (Warthin’s tumor)
Affects men, positive correlation to smoking
Histology: Encapsulated tumor with numerous cystic spaces – containing papillae – lined byoncocytes (columnar eosinophilic cells) – and overlie a layer of cuboidal cells – whichoverlie lymphoid tissue – complete with germinal centers
Picture
View On WordPress
0 notes
Text
How To Treat Your Damaged Tissue And Week Heart?

A bovine pericardium tissue patch is a specialized patch that is designed for the repair of damaged organs. It is made from the outer layer of the pericardium of a calf and has a biocompatible material. It is typically used in the repair of the heart, lung, or liver. It is typically used in human medicine in the repair of the heart, lung, or liver.
The tricuspid and pulmonic valves are the main valves of the heart. They are located in the right atrium and left atrium, respectively. These valves are responsible for maintaining the flow of blood through the heart. Without these valves, blood would be pumped into the lungs instead of the rest of the body.
Tissue patch concept:
A bovine pericardium tissue patch is a biological valve leaflet replacement used in tricuspid and pulmonic valve repair or reconstruction. It is a collagenous membrane that covers the heart and limits the pericardial cavity.
The bovine pericardium has three layers: an epithelial layer, a connective tissue layer, and a serosal layer. The connective tissue layer is made up of collagen and elastin fibers, which gives the pericardium its strength and flexibility.
Benefits:
The bovine Pericardium Tissue patch is a biological valve repair tissue that is used to treat patients with tricuspid or pulmonic valve disease. There are many benefits of using a Bovine Pericardium Tissue patch to repair tricuspid or pulmonic valves. They are-
· The patches are strong and durable, and they provide long-term valve function
· They are an alternative to mechanical valves, which can wear out over time and require replacement surgery
· It is an alternative to mechanical valves, which can wear out over time and require replacement surgery
Tricuspid Valve and Pulmonic Valve:
The tricuspid and pulmonic valves are the main valves of the heart. These valves are responsible for maintaining the flow of blood through the heart. Without these valves, blood would be pumped into the lungs instead of the rest of the body.
These valves work together to make sure that the blood is pumped to the lungs. If one of the valves does not work properly different symptoms arise in your body.
Valve manufacturing process:
The tricuspid and pulmonic valves are made from a variety of materials. The Tricuspid & Pulmonic Valve contract manufacturing uses a variety of materials that are then placed on a steel wire frame. The frame is then placed on a metal mold.
Then the metal mold is filled with the material. Then the mold becomes cool after few minutes. The mold is then removed and the valve is taken out of the mold.
How are the tricuspid and pulmonic valves attached to the heart?
The tricuspid and pulmonic valves are attached to the heart by the chordae tendineae. The chordae tendineae are the tendons that attach to the leaflets of the valves, and they are attached to the papillary muscles. The papillary muscles are the muscle that encircles the heart.
The tricuspid and pulmonic valves are the two valves that are found in the heart of the human body. They are responsible for the proper circulation of blood throughout the body and the proper functioning of the heart.
0 notes
Text
Bogus Std Cures: Are You Taking One?
Often triggered by bronchial infections or an allergic response, asthma affects more than 22 million Americans. Nebulizing asthma with colloidal silver helps eliminate the issue, killing pathogens. Dr. Grune has a patented chelated silver oxide that's colloidal silver for hpv a hundred to a hundred,000 occasions more bioactive when used topically. This productbinds to a floor space for no less than two and a half hours; different forms of silver only bind for about 15 seconds.
The most typical complaints had been ache upon intralesional injection and pruritus throughout the first 24 hours. Warts completely resolved in 85% of the duct tape arm of the research versus solely 60% within the cryotherapy group.74 The mechanism by which duct tape acts remains speculative. Distant warts that were not handled with the duct tape also resolved, raising the possibility colloidal silver for hpv that the host’s immune system was stimulated by way of native irritation produced by the duct tape. There have been no reported side effects with utilizing the duct tape, and most warts resolved inside 1 month of remedy.seventy four This is an optimal method to treating youngsters with warts, as a end result of it is painless and value efficient.
They can appear wherever on the physique, however are most typical on the arms and ft. A particular person could have one wart or a cluster of warts. There are many types of warts, but all are brought on by human papillomavirus . For the examine, Smith handled cervical most cancers cells with AHCC and incubated them for 72 hours, sampling them each 24 hours.
These final clearance decreased to 71% and 48% at the 3-month follow-up, respectively. Total wart clearance was 94% with podophyllotoxin and 74% with podophyllin answer. Podophyllin cream came to as straightforward to apply and results significantly better than podophyllin answer. Local unwanted effects had been gentle to reasonable with erythema, and erosion gave the impression to be greater in the podophyllotoxin group however not so serious to discontinue therapy . It selectively impacts squamous cell and reticuloendothelial tissue . Bleomycin isn't thought to bind on to HPV.
A clearance price of 46–52% has been noticed in numerous research. Duct tape occlusion therapy involves placing a piece of duct tape over the wart. The mechanism of motion of this method still remains unknown. Computed tomography or magnetic resonance imaging can be used to determine the extent of unfold colloidal silver for hpv of cervical carcinoma and extensive anogenital papillomatosis that has unfold into the pelvis. Acanthosis, epidermal hyperplasia, papillomatosis, compact orthokeratosis, hypergranulosis, tortuous dermal papillary capillaries, and vertical tiers of parakeratotic cells are the everyday histological findings of warts. In the granular layer, cells have coarse keratohyalin granules and vacuoles surrounding wrinkled-appearing nuclei.
0 notes
Text
What You Should Know About Microblading
Microblading is a process that involves making fine incisions in the skin. The results are a very natural-looking semi-permanent tattoo. It differs from traditional tattoos, which are opaque and have blue or green edges as they fade. A microblader will use a specialised hand tool to create the design in the client's skin.
The procedure is usually painless, but residual stinging can occur. While the pain and stinging is minor, you should monitor the area closely to avoid infection or puffiness. If the area is excessively red or swollen, it may be an indication of an infection. If you are prone to infections, you should avoid having the procedure done.
Some people experience allergic contact dermatitis after microblading, resulting in an itchy, cracked rash. If this happens, you should visit a dermatologist to get the area treated. This will help prevent infection and help your new tattoo look as natural as possible. You can ask for before-and-after pictures of other people's microblading results to check for irregularities.
The results of microblading can last for up to two years, depending on the individual's lifestyle, skin type, and sun exposure. However, it may require a touch-up every six to eight months or a year, particularly if your skin is oily or has a tendency to get oily. This skin type also tends to fade faster, so you might need to go back for another session.
Before your first session, you should avoid taking blood thinners or caffeine for at least 48 hours before the appointment. After your appointment, you should avoid any medication containing anti-biotics. These medications will affect the color of the pigments and affect the healing process. In addition, it may be important to use sunscreen if you plan to spend a lot of time outdoors.
Microblading is an amazing cosmetic procedure that will drastically reduce the time you need to spend getting ready in the morning. In addition to looking naturally beautiful, it can also save you time when getting ready for work. You will no longer need to apply makeup in the morning! You can go out and do other things while the microblading technician does the work. It can be a life-saver if you don't have the time to apply makeup every day.
Prices for microblading vary widely. You can expect to pay anywhere from $300 to $450 for the procedure, depending on the location of the salon. The cost of the procedure is largely dependent on the artist's skill level and the materials used. The average cost in California is around $450. You may want to opt for a high-end salon if you want to get the best results.
You can choose from several types of pigments for your microblading. There are organic and inorganic pigments available. Afterward, the color fades to a lighter shade to give a more natural look. The ideal depth for microblading is the papillary dermis. During your treatment, your microblading artist will use a blade-like tool to draw individual hairs.
You should expect your microblading session to last up to two hours. During this time, the area will be numbed with a topical anesthetic. It will take about 10-14 days to heal completely, and it is important to follow the technician's instructions carefully. After the procedure, it is important to avoid touching your eyebrows to prevent the spread of bacteria. Additionally, you should avoid strenuous physical activity for the first week after your procedure.
After microblading, the pigment will fade to the final shade in about a month, depending on the artist and your individual skin's healing process. There may be slight redness or swelling for a few days afterward, but this is usually minimal. You should avoid picking at the scabs to ensure a faster recovery.
Microblading is similar to eyebrow tattooing, except that it uses fine needles instead of a tattoo gun. The technician will create lines similar to eyebrow hairs by drawing the pigment into the dermis, the inner layer of skin. This procedure will take about an hour to complete. This is a great option for people who have sparse eyebrows or thinning hair.
0 notes
Text
Dysplastic Nevus (BK mole)
++Dysplastic Nevi (BK mole): non-sun exposed area. Relatively large. Flat macules or slightly raised papules with darker center. Irregular borders.
++Usually compound (superficial dermis aka papillary layer)
++Lentiginous hyperplasia: proliferation of atypical melanocytes
++Cytotypical atypia
++Has some clinical features of melanoma, tend to be larger than a typical mole, variable pigmentation.
0 notes
Photo

From • @pathologeek Warthin's Tumor Warthin's tumor (WT), AKA papillary cystadenoma lymphomatosum, cystadenolymphoma or just simply adenolymphoma. It is a relatively frequent and benign neoplasm of the major salivary glands. The WT was first described by Dr. Hildebrand who reported it in 1895. But in 1929, the pathologist Dr. Aldred Scott Warthin (1866 − 1931) described extensively two cases, and it now bears his name. Dr. Warthin is regarded as "the father of cancer genetics". PEARLS: - Second most common benign salivary gland tumor after pleomorphic adenoma. - Usually in male smokers age 40+ years. - Subtype(s): Infarcted/metaplastic Warthin Tumor. - Localization: almost exclusively restricted to parotid glands. - Clinical features: painless, slow-growing, and fluctuant swellings. Pain or facial nerve palsy may occur in metaplastic / infarcted variants. - Pathogenesis: probably arises from salivary ductal inclusions in parotid lymph nodes. - Histopathology: A circumscribed mass with spaces lined by double layer of oncocytic epithelium with a papillary and cystic architectural pattern and lymphoid stroma including germinal centers. - Differential Diagnosis: The main differential diagnosis of the metaplastic WT subtype is Warthin-like mucoepidermoid carcinoma; however, Warthin tumors lack MAML2 gene rearrangement. - Cytology smears triad: Cohesive sheets of oncocytes, numerous lymphocytes and granular background debris. - The malignant transformation of Warthin's tumor is extremely rare and occurs in about 0.3%-1%, to lymphoma and less common epithelial neoplasms. https://www.instagram.com/p/ChUmzdyDx0dMExVRjUj6Di3EzUaEQMtrpQhatE0/?igshid=NGJjMDIxMWI=
0 notes
Text
Pathohistological and Immunohistochemical Characteristics of Locally Advanced Papillary Serous Endometrial Carcinoma - Differential Diagnosis, Prognosis and Complex Treatment by Marinova Lena*

Abstract
We present a clinical case of a rarely diagnosed serous endometrial carcinoma (SEC) with infiltration of the cervix, left parametrium, right fallopian tube, with bilateral ovarian metastases and tumor cells in the peritoneal lavage. After extensive pathohistological and immunohistochemical examinatoin, it was proved to be a locally advanced serous endometrial carcinoma - pT3b N0 M0. The publication discusses the importance of immunohistochemical (IHC) differential diagnosis for determining the histogenesis of papillary serous adenocarcinoma. The main pathohistological dilemma is the determination of the histological subtype of this locally aggressive endometrial carcinoma. Another problem is the definition of the primary origin of the tumor, due to the difference between the pathohistological classification in cervical, uterine and tubo-ovarian adenocarcinomas, as well as the radically different postoperative adjuvant treatment. Incorrect differential diagnosis leads to misdefinition of the necessary complex oncological treatment.
Keywords: Endometrial Serous Carcinoma; Papillary Serous Uterine Cancer; Immunohistochemistry; Differential Diagnosis; Prognosis; Complex Treatment
Introduction
Uterine Serous Cancer (USC), although rare, is the most lethal type of uterine cancer. It has distinct molecular features and pathogenetic pathways compared with other uterine cancer types [1]. According to Bokhman’s 1983 model, Endometrial Carcinoma (EC) is broadly classified based on histopathologic features into two categories, type I and type II, which differ in incidence, prognosis, epidemiology, molecular pathology, and clinical behavior [2]. Type II tumors (nonendometrioid carcinomas), such as serous carcinoma, clear cell carcinoma, carcinosarcoma/malignant-mixed Müllerian tumor, are characterized by poorly differentiated histology and deep migration/invasion [1]. Among the most common problems encountered in practice is the distinction between primary endometrial and primary endocervical adenocarcinomas, and the determination of the tumor origin when there is synchronous, multifocal involvement of gynecologic tract sites, for example the endometrium and the ovary [3]. In this article we present a clinical case of locally advanced serous uterine cancer with difficult differential diagnosis both in terms of histogenesis and histological features, as well as in terms of its primary origin, which is extremely important for complex treatment.
Clinical Case
It concerns 51-year-old woman with pain and bloating. After three peritoneal punctures, a metastatic effusion from adenocarcinoma with probable ovarian origin was found. After CT scan of the abdomen and pelvis, bilateral ovarian formations were found. A total class II laparohysterectomy with bilateral adnexectomy, omentectomy and appendectomy was performed. Intraoperatively - In situ- Ascites- 6 liters of clear liquid. Uterus of normal size. Bilateral ovarian formations with a maximum diameter of about 9 and 8 cm. There were no enlarged iliac and paraaortic lymph nodes. Liver - smooth surface without pathological changes. There were no peritoneal metastases. Radical hysterectomy with bilaterally adnexectomy, omentectomy and lymphadenectomy of the iliac lymph nodes were performed.
Histological Result
In the uterus a polypoid tumor mass was found with complex papillary and glandular architecture, infiltrating the myometrium up to 5 mm; the gland-like spaces were without sharp luminal borders, necrotic material was present in the lumens (Figure 2B). In the isthmus (Figure 3A) and in the cervix (Figure 1, Figure 2A) the histological findings were similar - tumor, composed of merging papillary and gland-like structures was observed, infiltrating over ½ of the muscular layer and reaching the orificium externum canalis cervicalis. In the right ovary (Figure 2C) and in the right fallopian tube (Figure 3B,3C), the same tumor, composed of complex papillary and gland-like structures was discovered, papillary structures were found on the outer surface of both ovaries, as well. Among the tumor cells in the uterus, isthmus, cervical canal, and right fallopian tube, psammoma bodies were found, as well as necrotic debris in the lumens of the tumor glands. In the left ovary cysts lined by stratified collumnar epithelium were found. The left fallopian tube was with fibro-sclerotic changes and paratubal cysts. The right parameter was with preserved architecture. The left parameter was invaded by the tumor. Five right pelvic lymph nodes have reactive changes. Seven left pelvic lymph nodes have reactive changes. Omentum - with hyperemia and mesothelial proliferation. The ascites fluid analysis reports erythrocytes, mesothelial cells, tumor cells with large nuclei - single and in small complexes of 3-4 cells. It is about metastatic effusion.
Histological Diagnosis
Рapillary serous endometrial carcinoma (рТ3b N0 M0) with predominantly exophytic growth, infiltrating the myometrium up to 5 mm., with local invasion of the right fallopian tube and left parametrium. Рapillary serous endometrial carcinoma infiltration in the cervical canal with papillary and glandular architecture reaching the orificium externum canalis cervicalis with infiltration above ½ of the muscle layer. Metastases in both ovaries. Metastatic peritoneal effusion.
Discussion
Uterine papillary serous carcinoma (UPSC) is an uncommon form of endometrial cancer that typically arises in postmenopausal women. UPSC is staged like other forms of endometrial carcinoma at time of surgery using the FIGO cancer staging system. In case of infiltration of serosa or adnexa and / or tumor cells into ascites or peritoneal lavage, the carcinoma is classified as stage 3A. The tumor spread in the vagina and/or parametrium (direct extension or metastases) is staged as stage 3B according to the modified FIGO classification on 1/1/2010 and “Pathologic TNM staging of carcinoma and carcinosarcoma of the corpus uteri, AJCC 8th edition and FIGO 2018 update“[4,5]. For patients who undergo surgical staging—consisting of open abdominal exploration, hysterectomy, bilateral adnexal removal, and pelvic and para-aortic lymphadenectomy in the modified FIGO classification, peritoneal lavage cytology is no longer considered in tumor staging. In the presented clinical case, despite the metastases in the ovaries, the tumor is stage 3B.
Pathohistological characteristics of serous carcinoma adenocarcinoma: Complex papillary, solid or glandular architecture; The architecture is papillary with or without appreciable fibrovascular cores; slit-like spaces; gland-like spaces may be observed (but luminal borders are not sharp as seen in endometrioid carcinoma); solid growth. Psammoma bodies may be present in up to 33% of cases. Cytoplasm is usually scant but can be abundant with eosinophilia or clearing. Nuclei are typically high grade with pleomorphism, hyperchromasia, prominent nucleoli and frequent mitotic figures (including atypical mitotic figures) [6-8]. Most type II endometrial carcinomas, especially UPSC, have a complex papillary or glandular architecture, which is similar to serous papillary ovarian carcinomas. In general, densely fibrotic papillae fronds and slit-like spaces are common [1] [Figure 2,3]. Huge, round, undifferentiated tumor cells with a high number of mitotic figures, increased nuclear-to-cytoplasmic ratios, and prominent nuclear atypia are detached and present in the blank spaces. Hobnail cells, clear cells, and polygonal cells are frequently observed. Cilia are also observed in some cases, as in papillary serous ovarian carcinomas [9,10]. Serous carcinoma cells are arranged in true papillae lined with many cells with overlapping nuclei; cells are large, better preserved and with indistinct cell borders; nuclear chromatin is coarse with large prominent nucleoli [11] (Figure 2, Figure 3).
Immunohistochemical stains in papillary serous endometrial carcinoma show that the tumor is positive for p53 (strong and diffuse expression, mutated) and p16 (strong and diffuse expression) (Figure 4), focally positive for ER (Figure 5C) and negative for PR [6]. In the presented case all tumors (in the different parts of the genital tract) demonstrated diffuse/moderate-strong p16 expression (Figure 4), with percentage of positive tumor cells ranging from 90% to 100%. In contrast, endometrial endometrioid carcinomas exhibit less diffuse and less intense expression, with percentage of positive tumor cells ranging from 10% to 90% [12]. In endometrial endometrioid carcinoma, ER and PR are strongly positive; p53 and p16 are weak and patchy [6]. Highly expressed EMA by most adenocarcinomas is associated with poor prognosis [13,14].
Differential diagnosis (DD): Non-endometrioid carcinomas, which account for about 10% of endometrial carcinomas, may pose a great array of problems in differential diagnosis, including their distinction not only from benign lesions but also from endometrioid carcinoma and various tumors that may secondarily involve the uterine corpus [15]. The complex papillary architecture of serous uterine carcinoma causes a number of diagnostic difficulties. The differential diagnosis includes Villoglandular Variant Of Endometrial Carcinoma. Papillary endometrioid or villoglandular adenocarcinoma (VGAC) is a relatively common type of well-differentiated endometrial adenocarcinoma [16,17]. VGAC is characterized by a papillary architecture with delicate fibrovascular stalks lined by cuboidal to columnar cells with minimal cellular stratification and mild nuclear pleomorphism [16]. VGAC only superficially invades the myometrium, being diagnosed at an early stage and thereby having a better prognosis than typical endometrioid carcinoma. To avoid confusion with papillary serous carcinoma, some authors refer to this entity as endometrioid adenocarcinoma with papillary architecture(16). In mixed endometrial adenocarcinomas the tumor has microscopic features intermediate between serous and endometrioid; for example, papillary architecture typical of serous but without classical cytologic features or glandular architecture with epithelial features suggestive of serous (11). Villoglandular Cervical Adenocarcinoma (VGCA) is a rare well-differentiated subtype of endocervical mucinous adenocarcinoma that usually occurs in young women in early clinical stage I-II [18-24]. VGCA is associated with a better prognosis than other adenocarcinomas [18-20,23,25-27] аnd accounts for 5% of cervical adenocarcinomas [28,29]. It is characterized as superficially infiltrative and shows infrequent lymph node invasion and lymphovascular space invasion [30,31]. Serous Carcinoma of the Uterine Cervix (SCUC) is a very rare malignant tumor, while this histological subtype is common in the ovary, fallopian tube, uterine corpus and peritoneum. Because of its rarity, details of the clinicopathological features of SCUC are largely unknown [32]. SCUC has a complex papillary pattern with epithelial stratification. The tumor is characterized by >10 mitotic figures per 10 high-power fields. An intense acute and chronic inflammatory infiltrate is typically present within the cores of the papillae and in areas of stromal invasion [33]. Pleomorphic and macronucleated atypical cells are observed [32]. Occasional psammoma bodies are present, like in the presented clinical case (Figure 1). The tumor cells in SCUC are positive for p16, focally positive for p53 and ER, and negative for progesteron receptor. Age <65 years, stage >I, tumor size >2 cm, tumor invasion >10 mm, the presence of lymph node metastases, and elevation of serum CA-125 were associated with a poor prognosis [33].
Important for the DD between endometrial and endocervical carcinoma is the study which notes that p16 reactivity is mainly limited to areas with endometrioid or nonspecific cell type differentiation and does not occur in areas with normal endocervical mucinous morphology [34]. It is important to recognize special variants such as uterine serous carcinoma and clear cell carcinoma, as these can show extensive staining for p16 [34]. Univariate analysis on the training set identified 6 markers—p16, ProExC, ER, PR, vimentin, and HPV ISH—as performing well in distinguishing between endocervical and endometrial origin. Positive results for vimentin, ER, and PR support endometrial origin whereas p16, ProExC, and HPV ISH support endocervical origin [34,35]. Primary endocervical adenocarcinomas are characterized by CEA positivity, which is usually, but not always diffuse, negativity for vimentin, and negativity or focal weak positivity for ER [35]. Similar to serous carcinomas, all endocervical adenocarcinomas exhibited diffuse/moderate-strong p16 expression, with percentage of positive tumor cells ranging from 90% to 100% [12]. In the distinction between a high-risk HPV-related (usual type) endocervical adenocarcinoma and a low-grade endometrial endometrioid adenocarcinoma, the most useful immunohistochemical markers are p16 and ER and PR hormone receptors [36]. Given the limits of immunohistochemical stains in distinguishing between endocervical and endometrial origin, individual cases should be evaluated in the context of standard clinical, radiographic, gross, and morphologic findings [34]. In the presented clinical case, DD is required between synchronous serous adenocarcinomas, i.e. primary endometrial with infiltration in the uterine cervix and primary tubo-ovarian carcinoma, or serous endometrial carcinoma with metastases in both ovaries. Multifocal tumor distribution is relatively common in carcinomas arising in the female genital tract. Accurate designation of tumor origin is not always straightforward but is important for staging, prognosis and management [36]. In the context of endometrial carcinoma, the most common dilemmas occur in the setting of concurrent endometrial and adnexal/peritoneal high-grade serous adenocarcinoma [3]. High grade serous tubo-ovarian adenocarcinomas are characterized by complex papillary, solid or glandular architecture [6]; Significant nuclear atypia; significant nuclear pleomorphism (>3 x variation in size) with large, bizarre and multinucleated forms [37]. Prominent nucleoli, often large and eosinophilic; High mitotic index: ≥ 12 mitotic figures per 10 high power fields, often atypical; Necrosis is frequent [13]. Positive stains: p16 (~60%), ER (80%), PR (30%), high Ki67 proliferation index (> 75%) [38]. Usually they present as unilateral tubo-ovarian tumor in 80-90% of cases, no tumor infiltration on the surface of the ovary; without invasion into the lumen of the tube; without vascular invasion - 71.4%; without or presence of ovarian endometriosis [39,40]. IHC analysis of ER and PR of endometrioid endometrial and ovarian tumors distinguishes primary tumor synchronicity from hematogenous metastasis. The same levels of ER and PR are found in metastatic endometrial or ovarian cancer (Figure 5C,5D) and different in synchronous primary endometrial and ovarian neoplasms [41,42]. One general principle used in determining tumor origin in pathology is the identification of intraepithelial carcinoma because the presence of such a lesion is considered a strong evidence of tumor development at a particular anatomic site. Occasionally metastases can colonize preexisting mucosal structures and replace the native epithelium, for example, endometrial serous adenocarcinoma may involve the mucosa of the fallopian tube and closely mimic serous tubal intraepithelial carcinoma [3]. Simultaneous endometrioid carcinomas of the uterus and of the fallopian tube are unusual and occur primarily in obese perimenopausal women. These tumors are predominantly well or moderately differentiated with dissimilar endometrial and fallopian tube grades. The carcinoma of the fallopian tube is usually unilateral and located at the distal end of the tube [36]. It is well established that high-grade endometrial carcinomas may present with metastases even when there is minimal myometrial invasion [3].
Conclusions from the IHC panel of the presented clinical case: 1/The positive expression of ER and PR receptors in the tumor cells of the tumor in the cervix proves the primary endometrial origin of the carcinoma with infiltration of the cervical canal (Figure 5A,5B,5D,5E). 2/ Diffuse positive expression of p16 in the tumor cells of the endometrial tumor mass and in the cervical tumor is typical for serous carcinomas (Figure 4). 3 / Positive expression for Vimentin in the tumor cells in the cervical and the ovarian tumors is typical for primary endometrial carcinoma, negative - is observed in primary viloglandular endocervical adenocarcinoma and primary endometrioid ovarian carcinomas. The positive expression of Vimentin in both tumors of the cervix and the ovary proves the local growth of serous endometrial carcinoma to the cervix with bilateral metastases in the ovaries (Figure 6). 4/ IHC analysis of ER and PR of the endometrial and the ovarian tumors distinguishes primary tumor synchronicity from hematogenous metastasis. The same levels of ER and PR in the endometrial and ovarian tumors report bilateral metastatic tumor spread in the ovaries (Figure 5). 5/ Positive EMA expression in cervical tumor cells determines a poor prognosis (Figure 7). 6/ Psammoma bodies are observed on histological examination of the tumors of the cervix, uterine body, fallopian tube (Figure 1,3A,3B,5A,5B). They are typical for malignancies such as serous carcinoma of the ovaries and serous carcinomas of the cervix, endometrium, fallopian tube, peritoneum [43].
By the above immunohistochemical characteristics primary locally advanced serous endometrial carcinoma/ III B class stage is evidenced. Despite the initial tumor infiltration in the myometrium, as well as the superficial invasion of the cervix in the presented clinical case, the typical tumor spread of locally advanced serous carcinoma with unilateral infiltration into the right fallopian tube and left parametrium and bilateral ovarian metastases are observed.
Prognosis
Uterine Papillary Serous Carcinoma (UPSC) is a rare aggressive variant of type II endometrial cancer [44]. The prognosis is unfavorable, as it is an extremely aggressive tumor with a high potential for local recurrences and distant metastases. The recurrence rate of UPSC is high, estimated to be 31%–80% even in its early stages (stage I–II) [45]. Frequent recurrences in UPSC have led to the induction of adjuvant treatment, including systemic chemotherapy or radiation therapy [46]. Prognosis of the UPSC is affected by age, stage, and histology as well as treatment [47]. UPSC accounts for 10% of all endometrial cancer; however, it carries the poorest prognosis, with 5-year survival rates as low as 55% [48,49].
Complex Treatment
With such a dismal prognosis, these patients should be treated aggressively [48]. The primary treatment is surgical. FIGO-cancer staging is done at the time of surgery which consists of peritoneal cytology, total hysterectomy, bilateral salpingo-oophorectomy, pelvic/para-aortic lymphadenectomy, and omentectomy. After staging and surgery, radiation therapy and/or chemotherapy is recommended to treat patients at high risk for recurrence [50]. Analyses of Gynecologic Oncology Group (GOG) protocol 209 (a noninferiority trial in advanced/recurrent endometrial cancer patients comparing carboplatin and paclitaxel vs paclitaxel, adriamycin and cisplatin) support the favorable side effect profile of six cycles of carboplatin (AUC 6) and paclitaxel (175 mg/m2) [51]. Those who are identified to have residual UPSC in the uterus at the time of surgery, should receive adjuvant carboplatin and paclitaxel chemotherapy, and a strong consideration should be given for vaginal cuff brachytherapy [48]. UPSC’s aggressive features, resistance to chemotherapy, poor prognosis, and extremely high recurrence rate (50% to 80%) contribute to the increase in endometrial cancer-related deaths every year. Currently, surgery together with chemotherapy and radiotherapy (vaginal cuff brachytherapy or external pelvis radiotherapy) remains the dominant treatment option for UPSC [1].
Conclusion
We present a rare clinical case of locally advanced uterine papillary serous carcinoma with difficult differential diagnosis both in terms of histogenesis and histological features, as well as in terms of its primary origin, which is extremely important for complex treatment. Strict pathohistological and immunohistochemical analysis is required for the differential diagnosis of this rare aggressive variant of type II endometrial carcinoma. The prognosis is unfavorable, as it is an extremely aggressive tumor with a high potential for local recurrences and distant metastases. The primary treatment is surgical. FIGO-cancer staging is done at the time of surgery which consists of peritoneal cytology, total hysterectomy, bilateral salpingo-oophorectomy, pelvic/para-aortic lymphadenectomy and omentectomy. Locally advanced uterine serous carcinomas require adjuvant treatment, including concominant radiochemotherapy followed by systemic chemotherapy.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00140/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00140.pdf
#Endometrial Serous Carcinoma#Papillary Serous Uterine Cancer#Immunohistochemistry#Differential Diagnosis#Prognosis#Complex Treatment#Marinova Lena*#IJCMCR#clinical studies
0 notes
Text

Historical research: sheepskin parchment to prevent fraud in historical juridical documents -new in history (3/?)
In a recent British research, historians Doherty, Henderson and Fiddyment proved the preferential use of sheepskin parchment. The use of sheepskin over those of other species was because it was abundantly available and cheaper than the skin of other species. But this new research proves sheepskin was also used because of the increased visibility of fraudulent text erasure and modification, which was a result of the unique structure of the sheepskin.
(photo: S. P. Doherty)
Research article: Doherty, S.P., Henderson, S., Fiddyment, S. et al. Scratching the surface: the use of sheepskin parchment to deter textual erasure in early modern legal deeds. Herit Sci 9, 29 (2021).
After a long oral tradition, English common law was predominantly text-based in the late sixteenth century. In this century, the use of paper took already hold in society. However, for legal documents such as deeds, they continued to use animal skin. While paper was cheaper, parchment was more durable.
By observing hair fibres and follicle patterns, it is possible to identify of which species the parchment was derived from. Research showed that between the thirteenth and nineteenth century, they preferred to use sheepskin for legal deeds.
But where did this preference for sheepskin comes from? This preference may stem from early efforts to impede the fraudulent modification of legal agreements after signing. This was because later erasures and alterations were visible on sheepskin.
Parchment consist of the dermis layer of skin. This layer is divided into the fine dermal fibres (upper papillary dermis) and larger fibres (lower reticular dermis). Because of the presence of cutaneous lipids, the intersection between these layers is weak in sheepskin. During the process to make the sheepskin suitable for writing, large quantities of lipids are removed, which causes voids that facilitate the detachment of the two layers. Sheepskin contains more lipid content than other species skins. This way, it is more likely to detach these layers using sheepskin (compared to the skin of other species). This makes textual manipulation (such as scraping) more visible using sheepskin.
Already in the twelfth century, it was noted in the Dialogus de Scaccario (attributed to the Lord Treasurer Richard FitzNeal during the reigns of Henry II and Richard I) that scribes must use sheepskin for they do not easily yield to erasure without the blemish being apparent.
#new in history#history#archeology#parchment#medieval times#medieval history#historiography#historical facts#early modern times#early modern history#england#english history
24 notes
·
View notes