#jejunostomy
Text
Happy Disability Pride Month to people with ostomy bags, nasogastric tubes, gastrostomies and jejunostomies.
256 notes
·
View notes
Text
Lesbians Sharing Anal Dildo
Korean beautiful teen model sensual show
Bbw latina slut back at it again twerking
Stockings brit lesbian tonguing
spy sex cam trav azelalapute
Beautiful Blonde Babe Bobbi Eden Tongue Fucks Puma Swede!
Big round booty riding BBC
Isabella Monteiro e o Putinho
Carmella Crush Big Tit Teen ready to fuck
Asian trans babe spitroasted by hung studs in threesome
#fright#orthographized#quartermastership#beday#modern-built#hostileness#uncrumbled#codeclination#munchers#apterous#postliminiary#Chindwin#typhobacillosis#varicosity#universological#multivitamins#Harze#noncurtailment#jejunostomy#consonous
0 notes
Text
Petite ebony facesits sexy brunette milf
Um pouquinho de oral, footjob, e finalizando no pezinho
GIRL LOUDLY SCREAMING INTERRACIAL
More Reality Show Sex
HD Cumshot Cum Swallow Facial Blowjob By Pretty Petite Blonde Hair Ebony In Public POV Tight Lips Sheisnovember
JAV swingers club sex swapping party Subtitled
Doggystyle banged exgf gets tricked
Daddy bear man and family Family Shares A Bed
Charming redhead young Melody fucked by monster chili dog
Outdoor cumshot
#munchers#apterous#postliminiary#Chindwin#typhobacillosis#varicosity#universological#multivitamins#Harze#noncurtailment#jejunostomy#consonous#diasporas#co-bishop#papillous#scotomatical#Pan-hispanism#gonimolobe#Dimitrov#overmeanness
0 notes
Text


3 décembre/suite : Ça fait du bien de ne pas sentir de sonde traverser ‘tout mon corps’, de ne pas avoir un tube qui pendouille à mon visage, d’avoir sa peau qui peut respirer, sa narine se reposer. C’est dans ces moments que je me dis que je devrais prendre le risque d’accepter la jéjunostomie, et d’ailleurs le docteur m’a proposé de l’avoir durant cette hospitalisation mais j’ai refusée. En vu de comment mon corps est trop compliqué/ne tolère «rien», j’ai peur de n’avoir que des problèmes avec, j’ai peur d’avoir une infection et d’être dans une galère car je ne tolère pas les antibiotiques, bref je ne le sens pas de faire cette opération pour l’instant dans ces conditions…
#yamina hsaini#yamina's life#maladie#santé#médical#gastroparesie#sonde naso jejunale#jejunostomie#hopital
3 notes
·
View notes
Text
Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB): What Sets It Apart
Introduction: In the realm of bariatric surgery, innovations continue to emerge, offering new options for individuals seeking effective weight loss solutions. One such advancement is the Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB), a procedure that combines elements of sleeve gastrectomy and duodenal-jejunal bypass. In this blog, we'll delve into what sets Sleeve Gastrectomy with Duodeno-Jejunostomy apart from other bariatric procedures, its potential benefits, and the expertise of Dr. Shashank Shah, a leading authority in bariatric and gastrointestinal surgery.
Understanding Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB): Sleeve Gastrectomy with Duodeno-Jejunostomy is a surgical procedure that combines two distinct techniques to achieve weight loss and metabolic improvements. The first component, sleeve gastrectomy, involves the removal of a portion of the stomach to create a smaller, banana-shaped pouch, thereby restricting food intake and promoting satiety. The second component, duodeno-jejunal bypass, reroutes a segment of the small intestine to bypass the duodenum and proximal jejunum, reducing calorie absorption and altering gut hormone signaling.
What Sets It Apart:
Dual Mechanism of Action: Sleeve Gastrectomy with Duodeno-Jejunostomy harnesses the benefits of both restrictive and malabsorptive mechanisms, offering a comprehensive approach to weight loss and metabolic health. By reducing stomach capacity and altering nutrient absorption, this combination technique enhances weight loss outcomes and may lead to greater improvements in metabolic parameters such as insulin resistance and type 2 diabetes.
Preservation of Gastric Function: Unlike traditional gastric bypass procedures, Sleeve Gastrectomy with Duodeno-Jejunostomy preserves the natural gastric anatomy, avoiding the need for intestinal reconfiguration or bypass of the entire stomach. This preservation of gastric function may reduce the risk of long-term complications such as dumping syndrome and nutritional deficiencies while maintaining normal digestive processes.
Potential Metabolic Benefits: The duodenal-jejunal bypass component of Sleeve Gastrectomy with Duodeno-Jejunostomy has been associated with favorable changes in gut hormone secretion, including increased levels of glucagon-like peptide-1 (GLP-1) and peptide YY (PYY). These hormonal changes play a role in appetite regulation, glucose metabolism, and satiety, contributing to improved metabolic outcomes beyond weight loss alone.
Introducing Dr. Shashank Shah: Dr. Shashank Shah is a distinguished bariatric and gastrointestinal surgeon renowned for his expertise in advanced surgical techniques, including Sleeve Gastrectomy with Duodeno-Jejunostomy. With a comprehensive understanding of metabolic surgery and a commitment to patient-centered care, Dr. Shah has helped countless individuals achieve their weight loss and health goals through personalized treatment approaches.
Dr. Shah's Approach to Sleeve Gastrectomy with Duodeno-Jejunostomy: As the Director of Laparo-Obeso Centre, Dr. Shah leads a multidisciplinary team dedicated to providing comprehensive treatment for obesity and related metabolic diseases. He employs a meticulous approach to Sleeve Gastrectomy with Duodeno-Jejunostomy, ensuring each patient receives tailored care and optimal surgical outcomes. Dr. Shah's extensive experience and dedication to innovation make him a trusted authority in the field of bariatric surgery.
Conclusion: Sleeve Gastrectomy with Duodeno-Jejunostomy represents a promising advancement in the field of bariatric surgery, offering a unique combination of restrictive and malabsorptive mechanisms to promote weight loss and metabolic improvements. With its potential benefits and Dr. Shashank Shah's expertise, this innovative procedure provides a valuable option for individuals seeking effective and sustainable weight loss solutions. If you're considering Sleeve Gastrectomy with Duodeno-Jejunostomy, consult with a qualified bariatric surgeon like Dr. Shah to explore whether this procedure is right for you and embark on a journey towards improved health and well-being.
#laparo obeso center#bariatric surgery#dr.shashank shah#Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB)
0 notes
Text
February 6-10 is Feeding Tube Awareness Week!

The beginning of February was selected because of its proximity to Valentine’s Day, because we love our feeding tubes. This is my first year as a tubie and I’m looking forward to learning more about feeding tubes and the conditions that necessitate them! I do love my tube, it saved my life!
I am an adult with a feeding tube, and a lot of the awareness and attention surrounding these medical devices is child focused. A lot of children depend on tube feeding to thrive, but there are plenty of disabled adults that depend on tube feeding as well! In 2017 there were approximately 438,000 people with feeding tubes in the US, and 60% of them are adults.
I have gastroparesis, which directly translates to paralysis of the stomach. My stomach doesn’t grind food the way it’s supposed to, and my pylorus sphincter at the bottom of my stomach doesn’t open well to pass food and liquids through. While gastroparesis has a range of impact and severity, I have a very severe case, and I am no longer able to eat or drink by mouth for nutrition. I am 100% tube fed. I went into starvation ketoacidosis prior to my placement.
Tube feeding, or enteral nutrition, has several different forms. There are nasal tubes and there are surgical tubes. Nasal tubes can go into your stomach (NG), duodenum (ND), or your jejunum (NJ) and are typically for short-term use. They can be used for acute illness and malnutrition, or to trial tolerance of enteral feeding. Surgical tubes go into your stomach (gastrostomy/G) jejunum (jejunostomy/J) or both (gastrojejunostomy/GJ) and they’re for chronic conditions and/or long-term use. I have a GJ tube and it looks like this:
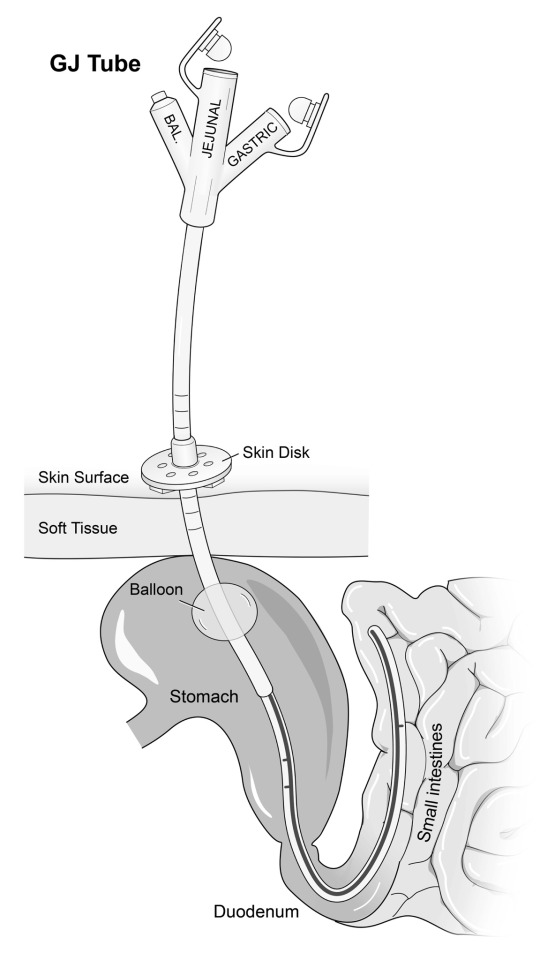
I have a GJ tube so that I can bypass my paralyzed stomach and feed directly into my intestine. I can also drain stomach contents from the gastric port, which allows me to drink liquids and drain them out before they make me sick. Different people will have different tubes depending on their diagnosis and prognosis! Some people have one form of tube, and others have separate G and J tubes.
There are over 400 conditions that can require tube feeding. Some of those include
Gastroparesis
Intestinal dysmotility
Cancer
Intestinal failure
Inflammatory Bowel Disease (Crohn’s disease and Ulcerative Colitis)
Cerebral Palsy
Congenital/chromosomal conditions
Cyclic Vomiting Syndrome
Ehlers-Danlos Syndrome
Several trisomy conditions
Prematurity
Other conditions not mentioned in the link above include
Hyperemesis gravadarium, severe nausea/vomiting during pregnancy to the point of significant weight loss and electrolyte imbalance
Acute trauma requiring bowel rest
Eating disorders
This week, I want to promote visibility for disabled adults with feeding tubes. I didn’t know anything about enteral nutrition until I got sick. Once I had a confirmed diagnosis of gastroparesis, the reality that I was facing forced me to learn and adapt quickly to a completely life changing treatment. I know there are other adults like me, as well as tubie adults that used to be a child with a tube!
4K notes
·
View notes
Note
What if people who can’t swallow end up choking on thick water? Then what?
If it is temporary you are either tube fed through your nose (nasogastric or NG tube) or your mouth (Orogastric - OG tube).
If they know it is going to be permanent they (usually a hospital) will make a surgical port in your stomach (Gastric - G tube) or small intestine (Jejunostomy - J tube) to deliver nutrition through
48 notes
·
View notes
Text
Introduction post!
Hii so I'm back. I deleted ALL my accounts and literally everything because I was "rEcOvErIng" but then I gave that up so here we are back at it again!
(I am DEFINITELY not anti-recovery, I want everyone to recover and get out of this stupid hell but recovery is not for me. Pro-recovery for everyone always but not for myself!)
I'm a minor, I use she/her pronounce. I have ana, restrictive subtype but I lowkey sometimes binge😭
I'm in forced recovery rn and barley hanging on. I have a feeding tube (not an NG, I have a jejunostomy tube bc of health problems related to an0rex!a)
And yh thats all about me honestly! I don't really post much but I'm typically active and my dms are open.
I'm active in april 2024 and I would really love an ana buddy! I think we shouldn't be alone to deal w this hell honestly and I love talking to people that understand.
Stay skinny <3
#ed dairy#ed ednotsheeran restriction#tw ana rant#tw restriction#a4a diary#tw 3d vent#thin$po#ana0rex1a#low cal restriction#tw thinspi
13 notes
·
View notes
Text
But my passion for eating came to a screeching halt this summer when I had a medical crisis that required a tracheostomy and a G-J (gastric and jejunostomy) tube rendering me unable to speak or eat. Having muscular dystrophy, a progressive disease where all muscles weaken over time, I’ve experienced difficulty swallowing in the last 10 years, adapting by shifting to soft or fatty foods that help with swallowing. While I aspirated saliva and food from time to time, there were several days in a row this summer when I kept choking every time I ate. I would swallow a bite or sip and half would not go down, requiring me to spit it in a cup so I could catch my breath. For days I tried to keep my caloric intake up by drinking lattes and letting my warm tongue melt tablespoons of peanut butter right after. Eating one small container of Trader Joe’s peach and mango yogurt would exhaust me. These were the last things I ate before going to the ER.
Food is essential to life, but it is so much more. Food is more than fuel or a calorie count. Food is cultural, political, and social — it ties people together and is a form of identity and pride. There’s nothing more wonderful than feeling satiated after a hearty meal like a bowl of spaghetti showered with grated parmesan cheese or a perfectly charred smashburger with caramelized onions and avocado dripping with special sauce. This is the sensation I miss most, as only medications and hydration go into my stomach via g-tube and liquid food through my small intestine via j-tube. Although I receive nutrition, I do not feel satisfied.
My inability to smell (because I do not inhale air through my nose) and eat has not diminished my desire for food. When I was in the ICU for four weeks I would leave the Food Network on during the times I was alert enough to pay attention, feasting on shows that I would never watch regularly: Guy’s Grocery Games and Pioneer Woman. The second episode of Iron Chef: Quest for an Iron Legend featuring Esther Choi made me want everything she made, such as her pork rib-stuffed donuts with sesame milkshake and dalgona cookie. A nurse saw me watching the episode and asked if I was torturing myself since I was temporarily on TPN (total parenteral nutrition), a form of intravenous nutrition. Was it torture? I didn’t even consider that, because it was my way of fulfilling my desire visually.
17 notes
·
View notes
Text
Managing And Caring For Enteral Feeding Tubes - Actionable Intelligence
We can train healthcare staff in the essentials of managing and caring for enteral feeding tubes
For many healthcare professionals, it is crucial to be well-informed on how they can care and maintain the safety of people with an enteral feeding tube most effectively. Enteral tube feeding is a means of supporting people who may no longer be able to consume adequate amounts of nutrition orally.
The enteral feeding tube itself is designed to provide foods and fluids in a liquid form, and a patient may require it for any of a range of reasons. For example, the patient may be suffering from swallowing problems that heighten the risk of food or fluid going down the wrong way and ending up in the lungs rather than the stomach, or they may have a medical condition that prevents the eating or digestion of food.
A person who requires enteral tube feeding may only need to have it in place for a limited time while undergoing treatment, or they may be living with it for a number of years. The situation will differ from one patient to the next.
A useful course for healthcare practitioners supporting those with a feeding tube
Healthcare practitioners will develop their theoretical and practical knowledge in the management and care of enteral feeding tubes (PEG), when they enrol on our own course on this subject. This course can be delivered in a classroom as well as remotely using Zoom video conferencing software, making it more accessible and convenient for attendees.
This course is aimed at nurses and healthcare workers who are already competent in administering medications. It covers a broad range of important aspects of the management and care of enteral feeding tubes and associated subjects, including the anatomy and physiology of the gastrointestinal tract, and the implications and complications of gastronomy and jejunostomy tubes.
Healthcare staff who may not have been exposed to feeding tubes previously or may not have a full appreciation of enteral feeding will learn the essentials on this course, including the different features of the tubes, and how they can best care for someone with a tube in place.
Attendees will also learn about the site cleaning and how to use a feeding tube to administer medication or feed their patient. Also covered in this course is the all-important matter of what to do in an emergency – what are the specific considerations and actions that should be taken involving feeding tubes in an emergency situation. Would you know how and when to use and ENPLUG?
We’ll put you in the best possible position to be more effective in your work
This course, focusing on the management and care of enteral feeding tubes, is just one of the many programmes of study that make up our highly regarded complex care courses here at Actionable Intelligence.
Our courses can be delivered either face-to-face or online depending on the circumstances and requirements of the attendees. Continued learning and professional development through courses such as ours play a crucial role in making healthcare safer and more effective for everyone and also count towards revalidation requirements for nurses.
To learn more about this or any of our courses, please reach out to us today, by calling 0330 133 4195 or sending an email [email protected]

2 notes
·
View notes
Text
Adrian (as previously stated) has an ostomy bag. he got it when he was ten due to untreated ulcerative colitis (which led to toxic megacolon), multiple injuries to his bowel, anal prolapse, and faecal incontinence
i'm also making him reliant on a feeding tube. he has separate G (gastrostomy) and J (Jejunostomy) surgical tubes.
he can't tolerate anything (any food or drinks) orally, as his stomach is paralysed (severe gastroparesis caused by his ED. I think bleach poisoning can cause it, too?) and feeds into his J tube. He uses his G for draining/venting, and to give medication.
yeah...
#kuraitsume’s tattoo & piercing parlour#pigment of your imagination#adrian#adrian lucas beck#tw feeding tube mention#tw feeding tube#ask to tw
2 notes
·
View notes
Text
Emerging Demand For Enteral Feeding Tubes Will Grow The Global Feeding Tubes Market Size

The global feeding tubes market has witnessed robust growth owing to the increasing prevalence of chronic conditions such as cancer, neurological disorders and gastrointestinal disorders. Feeding tubes help provide nutrition directly to the stomach or small intestine of patients who are unable to consume oral food and nutrients. They are commonly used for newborns, infants, children, and adults with feeding problems or swallowing disorders. Feeding tubes have various benefits such as reducing risk of aspiration pneumonia, improving calorie and nutrition intake and reducing complications associated with malnutrition.
The Global Feeding Tubes Market Size Is Estimated To Be Valued At US$ 6.34 Bn In 2024 And Is Expected To Exhibit A CAGR Of 6.2% Over The Forecast Period 2024-2031.
Key Takeaways
Key players operating in the global feeding tubes market Are Boston Scientific Corporation, Vygon, BD, Cardinal Health, Amsino International, Inc., Fidmi Medical, Vesco Medical, Mckesson Medical-Surgical, Medela AG, ALCOR Scientific, Nutricia, Medline Industries, Inc., Mead Johnson & Company, LLC., Abbott, Meiji Holdings Co., Ltd., Fresenius Kabi AG, B. Braun SE, Trovita Health Science, Victus Inc., Avanos Medical Inc., Cardinal Health, Moog Inc, Conmed Corporation, and Cook Medical. The market is witnessing robust growth due to the increasing prevalence of chronic diseases such as cancer, gastrointestinal disorders and neurological disorders which require long-term tube feeding. Technological advancements in feeding tubes such as low-profile gastrostomy button devices, jejunostomy tubes and low-profile gastrojejunostomy tubes have reduced complications and improved patient comfort.
Get more insights on this topic: https://www.pressreleasebulletin.com/global-feeding-tubes-market-trend-size-and-demand/
#Global Feeding Tubes Market Market Trend#Global Feeding Tubes Market Market Growth#Global Feeding Tubes Market Market Size#Global Feeding Tubes Market Market Analysis
0 notes
Text
Feeding tubes What Cancer patients and care givers should know
Maintaining proper nutrition during cancer treatment is important. When cancer patients struggle with this, a feeding tube can be a solution. These flexible plastic tubes placed in the stomach can help provide the calories, protein, vitamins, minerals and fluids needed to help the body fight infection, heal and stay healthy – all crucial during cancer treatment.
But the idea of a feeding tube can be daunting. Even though a feeding tube may be essential for helping you maintain a healthy, active life during and after cancer treatment, it can be a big lifestyle change. In this Blog, Dr. Pratik Patil – a Cancer Specialist In Pune explains What cancer patients and caregivers should know.
When do cancer patients need a feeding tube?
According to Dr. Pratik Patil, a Best Oncologist in Pune, cancer patients may require a feeding tube if they face difficulties in swallowing, particularly due to cancer in the head or neck area.
Additionally, patients who are malnourished before or during cancer treatment, which includes surgery, chemotherapy, and radiation therapy, may also benefit from a feeding tube. In some cases, patients who have fistulas, an opening, or an abscess in the esophagus or stomach may also require a feeding tube to ensure proper nutrition during cancer treatment.
How is a feeding tube inserted?
The way a feeding tube is placed depends on the type of feeding tube you need. There are three types of feeding tubes commonly used:
Nasogastric tube (NG-tube): This flexible tube is passed through the nose, down the esophagus and into the stomach. It is placed at the patient’s bedside in the hospital and doesn’t require a surgical procedure. It is often temporary and given to patients who can’t eat for a short period following surgery.
Gastrostomy tube (G-tube): This tube is inserted through the belly and brings food directly to the stomach. It can be placed during an outpatient procedure and does not require the patient to stay overnight. This tube is often used when patients will need to rely on a feeding tube for about three to four months or longer. It’s very easy to use.
Jejunostomy tube (J-tube): A J-tube is a soft, plastic tube placed through the skin of the belly into the midsection of the small intestine. It can be placed as an inpatient or outpatient procedure. The tube delivers food and medicine until the person is healthy enough to eat by mouth. It bypasses the stomach completely and is often used when the patient cannot digest food in the stomach, like in some cases of stomach cancer. This tube is also best suited for long-term use.
Will patients feel their feeding tubes?
Again, this depends on the type of tube. Patients typically can feel an NG tube, but the good news is, it’s only used for a few days or weeks.
With longer-term tubes, like G-tubes and J-tubes, patients may experience some initial pain and discomfort, but it should fade after a day or two.
How do feeding tubes work?
Different tubes work in different ways. Some use a pump – typically formula. Others rely on gravity or a syringe to push the food. Your care team will teach you how to use your specific feeding tube.
Can patients operate feeding tubes by themselves?
Yes, all three types of the common feeding tubes mentioned above can be operated by the patients themselves. But depending on their physical and mental health, they may need help from a caregiver or health care provider. Dr Pratik Patil , we provide classes for patients and caregivers to prepare them to use feeding tubes
Are there any side effects from using a feeding tube?
Usually, there are no side effects from the tube itself. Some patients may experience some nausea, vomiting or diarrhea, but this can be addressed by adjusting how much formula is given and how much time the feeding takes. If these side effects continue, your doctor can prescribe anti-nausea medicine. It’s also important to properly clean the feeding tube and the area surrounding it as instructed by your care team. Otherwise, the patient is at risk of infection. If a patient has an infection, the skin around the feeding tube will look red and swollen. Patients with feeding tubes might feel self-conscious.
Stigma or fear of stigma surrounding feeding tubes?
According to the best oncologist in Pune, Dr. Pratik Patil, feeding tubes can easily be concealed under clothing, allowing patients to return to work without their co-workers noticing.
However, it is recommended that patients educate their close friends and family about their condition and demonstrate how the feeding tube works. It may be helpful to involve a caregiver and teach them how to use the feeding tube. An honest and straightforward approach is often the best way to handle this adjustment.
0 notes
Text
Delving into Gastroparesis Treatment Market Analysis
Market Overview –
The Gastroparesis Treatment Market is expected to reach USD 8.27 billion by 2032, growing at a 3.2% CAGR over the forecast period 2023-2032.
The Gastroparesis Treatment Market is witnessing steady growth globally, driven by the increasing prevalence of gastroparesis and advancements in treatment options. Gastroparesis is a condition characterized by delayed emptying of the stomach, leading to symptoms such as nausea, vomiting, and abdominal pain.
The Gastroparesis Treatment Market is witnessing steady growth due to rising cases of gastroparesis worldwide. Demand for gastroparesis medication is surging as patients seek effective remedies for symptom management. Key players are innovating to develop advanced therapies, catering to the unmet needs of patients with this debilitating condition.
Factors such as diabetes, post-surgical complications, and neurological disorders contribute to the rising incidence of gastroparesis. The market encompasses various treatment modalities, including medications, dietary changes, gastric electrical stimulation, and botulinum toxin injections, aimed at managing symptoms and improving gastric motility.
Additionally, ongoing research and development efforts focus on innovative therapies targeting the underlying causes of gastroparesis, such as dysfunction of the enteric nervous system or impaired gastric smooth muscle function. However, challenges such as limited treatment options for refractory cases and the need for long-term management strategies hinder market growth. Despite these challenges, the Gastroparesis Treatment Market presents opportunities for innovation and collaboration among healthcare professionals and pharmaceutical companies to develop more effective and personalized treatment approaches, ultimately improving patient outcomes and quality of life.
Segmentation –
Global Gastroparesis Treatment market has been segmented on the basis of Gastroparesis type which comprises idiopathic, diabetic, post-surgical and others. On the basis of drug class the market comprises of prokinetic drugs, antiemetics, antidepressants and others. On the basis of other treatment; market is segmented into jejunostomy, gastric electric stimulation (GES) and parenteral nutrition
Regional Analysis –
Regional analysis of the Gastroparesis Treatment market provides valuable insights into the distribution and trends of treatment options across different geographical areas. Understanding regional dynamics is crucial for stakeholders to tailor their strategies effectively.
Factors such as population demographics, healthcare infrastructure, and regulatory frameworks vary from one region to another, influencing the demand and adoption of Gastroparesis treatments. For instance, developed regions with advanced healthcare systems may have higher adoption rates of novel therapies due to better access and affordability. Conversely, developing regions might face challenges such as limited access to specialized treatments or lower awareness among healthcare professionals and patients.
By conducting a thorough regional analysis, stakeholders can identify lucrative markets, assess competitive landscapes, and pinpoint opportunities for expansion or market penetration. Moreover, analyzing regional variations in treatment preferences and patient outcomes can guide the development of targeted marketing campaigns and personalized healthcare solutions. Overall, a comprehensive regional analysis serves as a cornerstone for informed decision-making and strategic planning in the Gastroparesis Treatment market.
Key Players –
Global gastroparesis treatment Key players include Medtronic, Kimberly-Clark Corporation, Abbott Laboratories, Salix Pharmaceuticals, Inc., Boston Scientific Corporation, C. R. Bard, Inc., Janssen Global Services, LLC, Cardinal Health, Inc., Alfa Wassermann SPA, Evoke Pharma, and Rhythm Pharmaceuticals, Inc.
Related Reports –
Meningitis Diagnosis and Treatment
Endodontic Devices
Fertility Drug and Surgery
Opioids
For more information visit at MarketResearchFuture
#Gastroparesis Treatment Market#Gastroparesis Treatment Market Size#Gastroparesis Treatment Market Share#Gastroparesis Treatment Market Outlook#Gastroparesis Treatment Market Report
0 notes
Text
Nouvelle vidéo YouTube en ligne !
youtube
#yamina hsaini#yamina's life#gastroparesie#sonde naso jejunale#gastroparésie#j tube#jejunostomie#Youtube
3 notes
·
View notes
Text
Revolutionizing Diabetes Treatment: Understanding Sleeve Gastrectomy with Duodeno-Jejunostomy
Are you or a loved one struggling with Type II Diabetes Mellitus, wondering if there's a solution beyond traditional treatments? The groundbreaking procedure known as Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB) may offer new hope. Let's delve into this innovative approach and learn more about how it's transforming the lives of patients, alongside insights into the expertise of Dr. Shashank Shah.
Understanding Sleeve Gastrectomy with Duodeno-Jejunostomy
Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB) is a cutting-edge surgical procedure designed to combat Type II Diabetes Mellitus, particularly in patients with or without obesity. This revolutionary technique involves the creation of a sleeve by surgically removing a significant portion of the stomach. Additionally, the procedure bypasses the first 100-150 centimeters of the small intestine, connecting it as a loop to the duodenum, the initial part of the small intestine.
How DJB Works
DJB combines the benefits of sleeve gastrectomy, which provides a restrictive effect on food intake, with an upper small intestinal bypass to induce a malabsorptive effect. This dual mechanism leads to significant weight reduction while also triggering a variety of intestinal hormonal changes. These hormonal shifts play a crucial role in lowering blood sugar levels and enhancing insulin secretion, thereby effectively resolving Type II Diabetes Mellitus, even in non-obese patients.
Advantages of DJB
One of the key advantages of Sleeve Gastrectomy with Duodeno-Jejunostomy is its ability to minimize the risk of frequent stools and esophageal reflux, common complications associated with other weight loss surgeries. Moreover, the procedure involves a single anastomosis, simplifying post-operative examinations via endoscopy. Another noteworthy aspect is that DJB is partially reversible, providing flexibility in treatment options, especially for patients seeking resolution of Type II diabetes mellitus.
Meet Dr. Shashank Shah: A Pioneer in Bariatric Surgery
Dr. Shashank Shah is a renowned bariatric surgeon and pioneer in the field of metabolic and obesity surgery. With extensive experience and expertise, Dr. Shah has successfully performed numerous DJB procedures, transforming the lives of patients struggling with diabetes and obesity. His innovative approach and dedication to patient care make him a trusted leader in the field of bariatric surgery.
Take the First Step Towards a Healthier Future
If you or someone you know is living with Type II Diabetes Mellitus and seeking a transformative solution, Sleeve Gastrectomy with Duodeno-Jejunostomy may offer new possibilities. Consult with Dr. Shashank Shah to explore personalized treatment options and take the first step towards a healthier, diabetes-free future.
Laparo Obeso Center
7411804876
0 notes