#handbook of diagnosis and treatment of dsm-5 personality disorders
Text
Clinical Formulations of Histrionic PD
Clinical formulations and case conceptualisations are introduced in this post.
These are all generalisations and theories of how HPD develops, not something that is supposed to be true for everyone with HPD.
Psychodynamic model
Histrionics lack relationships with maternal caregivers so turn to paternal caregivers for love and attention
Learn that they can get attention through sexualised behaviours
Men with HPD may be hypomasculine (effeminate) or hypermasculine if their paternal caregiver is emotionally unavailable
Biosocial model
Mood swings, very emotional
Biggest influences are environmental: caregivers’ reinforcement of attention-seeking & manipulative behaviours and histrionic role models
Children learn they can use cuteness, charm, attractiveness & seductive behaviours to get what they want/need (attention from caregivers)
Histrionics are externally focused and largely ignore their internal worlds
Histrionic behaviours are self-perpetuating
Cognitive-Behavioural model
Two main underlying assumptions: “I am inadequate and unable to handle life by myself” and “I must be loved by everyone to be worthwhile.”
Need attention and approval from others, and in a similar way to DPD feel they are inadequate to look after themselves and need others
Hypersensitive to rejection & criticism (similar to DPD, NPD and AvPD)
Feel they must perform for others to gain approval and self-esteem
Thinking is “impressionistic, global, and unfocused” and leads to over-generalisation, emotional dysregulation, and splitting
Two subtypes:
The controlling type, who tries to gain control through dramatics and manipulation; they struggle with reading others’ emotions and are shallow, self-centred, and uncomfortable without immediate assurance; lack empathy.
The reactive type tries to gain approval and reassurance.
Interpersonal model
People with HPD learnt that their entertainment value and appearance was more important to others than their worth as a person
Learnt that physical appearance and charm can be used to manipulate others
Their childhood homes were unpredictable and probably involved substance abuse
The unpredictability was dramatic and interesting (unlike the “primitive” and life-threatening chaos associated with BPD)
Histrionics were likely rewarded (i.e. had their physical and emotional needs met) for their disabilities, illnesses and complaints
Histrionics “exhibit a strange fear of being ignored, together with a wish to be loved and taken care of by important others, who can be controlled through charm or guile.”
Integrative model
Histrionics experience reactive mood swings and have high levels of energy
They are hyper-responsive and externally oriented
“The self-view of the histrionic will be some variant of the theme “I am sensitive and everyone should admire and approve of me.” The world-view will be some variant of “Life makes me nervous so I am entitled to special care and consideration.” Life goal is some variant of the theme “Therefore, play to the audience, and live in the moment.””
Cargivers’ style based in reciprocity, i.e. “I’ll give you attention if you do what I want”, with minimal or inconsistent discipline and probable neglect
Internal experiences of HPD are “denial of one’s real or inner self; a preoccupation with externals; the need for excitement and attention-seeking, which leads to a superficial charm and interpersonal presence; and the need for external approval. This, in turn, further reinforces the dissociation and denial of the real or inner self from the public self, and the cycle continues.”
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#clinical formulations#case conceptualisations#case conceptualisation#hpd#hpd info#pd info#dogpost#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#this has been in my drafts for 10 months LOL#also re reading this its like 'people w hpd were neglected and so they try to get their needs met thru trying to get ppl to love them#which is OBVIOUSLY manipulative and selfish right?? /sarcasm#personality disorder concepts
35 notes
·
View notes
Text
Takahiro A. Kato et al., Multidimensional anatomy of ‘modern type depression’ in Japan: A proposal for a different diagnostic approach to depression beyond the DSM-5, 70 Psychiatry Clin Neurosci 7 (2016)
Abstract
Japan’s prototype of depression was traditionally a melancholic depression based on the premorbid personality known as shūchaku-kishitsu proposed by Mitsuzo Shimoda in the 1930s. However, since around 2000, a novel form of depression has emerged among Japanese youth. Called ‘modern type depression (MTD)’ by the mass media, the term has quickly gained popularity among the general public, though it has not been regarded as an official medical term. Likewise, lack of consensus guidelines for its diagnosis and treatment, and a dearth of scientific literature on MTD has led to confusion when dealing with it in clinical practice in Japan. In this review article, we summarize and discuss the present situation and issues regarding MTD by focusing on historical, diagnostic, psychosocial, and cultural perspectives. We also draw on international perspectives that begin to suggest that MTD is a phenomenon that may exist not only in Japan but also in many other countries with different sociocultural and historical backgrounds. It is therefore of interest to establish whether MTD is a culture-specific phenomenon in Japan or a syndrome that can be classified using international diagnostic criteria as contained in the ICD or the DSM. We propose a novel diagnostic approach for depression that addresses MTD in order to combat the current confusion about depression under the present diagnostic systems.
Clinical Picture
Case: male, 24 years old
Chief complaint: No desire to do anything
Medical history: No previous psychiatric disorder
Family history: Nothing of note
Developmental and social history: He is the first son, with an older sister. His father is a company employee, his mother a full-time homemaker. There was nothing particularly problematic during junior or senior high school, although apparently he sometimes deliberately did not apply himself to the subjects of teachers that he disliked. At university he took part in group activities and had a part-time job, just like other students. He was not terribly enthusiastic about searching for a job and aimed to become a civil servant. After graduation, he attended a vocational college for a year to prepare for the entrance exam to the civil service, and at the age of 23 started to work in the municipal government of a provincial city – he says he just happened to sit the exam and pass it.
History of present illness: He did not particularly dislike the work in the place he was assigned to after being hired, though he was not greatly interested in it either. However, he would occasionally be absent from work; he says this was because he had an annoying boss who he couldn’t stand the sight of. Nonetheless, it was not a case of being unable to go to work because he was depressed, and when he was absent from work he would play slot machines, go to the movies, or go shopping. In June 2010, a year after starting work, he married a female colleague from the same work-place with whom he had fallen in love. In May 2011, his first child was born. He was still halfhearted about his job, but also finding it hard to be at home, he would play slot machines or go to the movies. Raising the child proved to be very difficult, but his wife had stopped working and, together with both his mother and her own mother, managed the household very well.
In December 2011, his boss reprimanded him for his attitude toward his work. He had previously been given warnings on a number of occasions, but apparently this time the reprimand he received was very severe. He subsequently left work early, complaining of feeling unwell. He says that from that day on he was unable to sleep at night. He became easily irritated and tended to have feelings of desperation. Even though, he went to work properly every day. Whilst at work, he had no motivation to do anything and had no energy. He would become angry and did not feel like attending work social events, such as the year-end party or the New Year party. He would tend to stay out of his boss’s sight. He would feel a little more cheerful only when he played slot machines and when spending time in an Internet cafe, but when he went home he would again slip into gloom because, he says, he found it boring. His anger was not toward himself but others, such as his boss and his wife. He sometimes would feel valueless himself; however, he could alleviate such unpleasant feelings by his devotion toward his hobbies. His sleep was constantly mildly disturbed but not severely, and sometimes he would have trouble getting to sleep and fail to get up in the morning. Therefore, from around the middle of January he started to fail to go into his office once/twice a week and during this absence he would surf the net to relax or go out to play slot machines.
In March of 2012, he found a site on the Internet called ‘Mind medicine cures your Depression!!’ which contained a checklist for depression, and he quickly came to believe that he himself must have ‘depression.’ The following day, he decided to go to a local psychiatric clinic for a prescription of antidepressants. He entered the examination room, greeting the doctor politely, then he voluntarily read out his life history and medical history from a memo he had prepared. When he finished, he handed the psychiatrist in charge a depression checklist, which he had found on the Internet, and requested a particular medicine by himself: ‘Doctor, as I have just mentioned, these diagnostic criteria apply to me. I heard that selective serotonin re-uptake inhibitors are effective.’ Based on his examination, his score on the Hamilton Rating Scale for Depression1,2 was 17 (mild depressive level); he met the DSM-IV criteria for a major depressive episode (based on the handbook, entitled Quick Reference to the Diagnostic Criteria from DSM-IV-TR3) and was diagnosed as suffering from depression. He requested a medical certificate then and there. Additional clinical history revealed that he did not meet the diagnostic criteria for avoidant personality disorder, schizoid personality disorder, or narcissistic personality disorder. Also, according to information supplied by his wife, who was present when he was examined, there was nothing particular in the symptoms to suggest that the illness was feigned.
This clinical picture was originally used for the symposium during the 109th annual meeting of The Japanese Society of Psychiatry and Neurology in Fukuoka, 2013.
Introduction
Cases like the above have emerged in Japan since around 2000, and these cases have been called ‘modern type depression (MTD)’ – a novel form of depression. This catchy ‘modern’ name has quickly and widely spread to the public via Japan’s mass-media and Internet-related media, while the name itself has not been regarded as an official medical term, and there is no consensus guideline for its diagnosis and treatments, which has led to confusion when dealing with MTD in clinical practice. Scientific literature about MTD remains very limited. In this review paper, we summarize and discuss the present situation and issues regarding MTD – focusing on historical, diagnostic, sociocultural and international perspectives, by referring to our recent international survey.4 Is MTD a phenomenon limited to Japan? The pilot survey has indicated that MTD may exist not only in Japan but also in many other countries with different sociocultural and historical backgrounds. It is therefore of interest to establish whether MTD is a cultural phenomenon specific to Japan or a syndrome that can be classified using the present international diagnostic criteria of the ICD/DSM. Finally, we propose a novel diagnostic system of depression including MTD in order to combat current confusion regarding the diagnosis of depression under the present ICD/DSM diagnostic systems.
Historical Background
Just since the beginning of the 21st century, Japanese psychiatrists have increasingly reported patients with a type of depression that does not seem to fit the criteria of the ICD-10 and the DSM-IV, and which is widely denoted as MTD among Japanese psychiatrists. The Japanese psychiatrist/psychopathologist Shin Tarumi reported the increasing occurrence of MTD and he labeled MTD as Dysthymia-gata utsu-byo (dysthymic type of depression) in the Japanese literature.5,6 Tarumi described the associated premorbid personality as Typus dysthymicus (TD) and compared it with Japan’s traditional type of depression.5,6 Tarumi defined the characteristics of MTD with TD as follows: (i) younger generation; (ii) attachment to oneself with less loyalty for social structures; (iii) feeling distressed about rules/order; (iv) negative feelings about social order/models; (v) vague sense of omnipotence; and (vi) not hard-working by nature (Table 1).6–17 MTD is also characterized by (a) distress and reluctance to accept prevailing social norms; and (b) avoidance of effort and any strenuous work.4,18 Most sufferers of MTD are born after 1970, that is, the generation growing up with home video games in the era of Japan’s high economic growth. Youths with MTD tend to feel depressed only when they are at work; otherwise, they can enjoy the virtual world of the Internet, video games, and pachinko (Japanese pinball). Therefore, sufferers of MTD have difficulties in adapting to work/school and participating in the labor market.
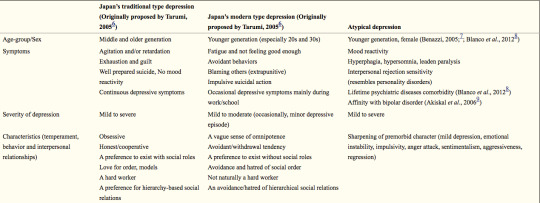
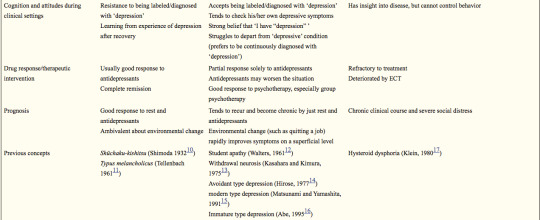
Table 1. Comparison between Japan’s traditional type depression, Tarumi’s Japan’s modern type depression and atypical depression
This table is a proposed comparison between Japan’s traditional type depression, Japan’s modern type depression and atypical depression according to Tarumi 2005,6 Tarumi & Kanba 2005,5 and Kato et al. 2011.4 Data, especially the section on ‘Drug response/Therapeutic intervention,’ has not yet been validated. ECT, electroconvulsive therapy.
Formerly, the melancholic type of depression had been regarded as a typical form of depression amongst the Japanese population, whose premorbid personality was defined as shūchaku-kishitsu (SK) by the Japanese psychiatrist Mitsuzo Shimoda.10,19 Shimoda characterized SK as: (i) middle aged; (ii) strong loyalty to society and community and one’s role within these structures; (iii) a preference for rules and order; (iv) positive feelings about social order/models; (v) attentive and diligent; and (vi) fundamentally hardworking.10,19,20 SK has been discussed in a similar context to Tellenbach’s Typus melancholicus (TM), which was identified amongst Germans after World War II.11 Tellenbach described the premorbid personality of patients with unipolar endogenous depression as orderly, devoted to duty and to family members, and scrupulous.11 Such types of depression based on SK and TM are considerably different from MTD. On the other hand, since the 1970s, different types of depression have been reported by Japanese psychiatrists and psychopathologists, such as taikyaku shinkei-sho (withdrawal neurosis);13 tohi-gata utsu-byo (avoidant type of depression);14 gendai-gata utsu-byo (modern type of depression);15 and mizyuku-gata utsu-byo (immature type of depression).16 Commonalities between the above types of depression and the currently emerging MTD have been pointed out. The former (taikyaku shinkei-sho, tohi-gata utsu-byo, gendai-gata utsu-byo and mizyuku-gata utsu-byo) was limited to highly educated youth, but MTD has been known to affect youth regardless of educational backgrounds.4
The 24-year-old man presented in the above clinical picture expressed moderate depressive symptoms just after a stressful event at his workplace. He came to regard himself as having severe depression, and finally he asked a doctor for sick leave in order to take a rest. His depressive symptoms mainly emerged during working time, and his symptoms were relieved in other situations. His characteristics, including behaviors and interpersonal relationships, contained the following features: not naturally a hard worker; an avoidance/hatred of hierarchical social relations; a preference to exist without social roles; extrapunitive type; and a vague sense of omnipotence. These features are exactly matched with MTD proposed by Tarumi.5,6
Diagnostic Issues of MTD
MTD has not been regarded as an official medical term, and various diagnoses have been applied based on ICD-10 and DSM-IV criteria. Our case vignette survey among Japanese psychiatrists suggests that MTD tends to be diagnosed as a variety of psychiatric disorders, such as mood disorder (296, code of DSM-IV; the same shall apply hereafter), dysthymic disorder (300.4), adjustment disorder (309) and adjustment disorder with depressed mood (309.0) by Japanese psychiatrists.4 Interestingly, some Japanese psychiatrists reported that categorical diagnostic systems, such as the ICD-10 and the DSM-IV, are not applicable to MTD. The case vignette survey was also administered to foreign psychiatrists at the same time, which revealed that they tend to diagnose the MTD case as mood disorder (296), dysthymic disorder (300.4), adjustment disorder (309), adjustment disorder with depressed mood (309.0) and adjustment disorder with mixed anxiety and depressed mood (309.28). Based on the reports and our clinical experiences in Japan, it is challenging to differentiate between MTD and other types of depression, such as atypical depression (AD) and dysthymia.
Atypical depression
It is often difficult to differentiate MTD from AD due to some overlap of their clinical features, including young onset, impulsivity, aggression toward others, behavioral symptoms similar to personality disorders, being refractory to treatment, and severe social disability caused by a chronic clinical course.7,8,21
Patients with MTD tend to have specific features of personality or characteristics, while patients with AD have no such features. However, it is also well known that the characteristics of AD patients would alter dramatically around the onset of AD, showing its aggressive and impulsive aspects. Around the onset of AD, the characteristics in patients with AD often sharpen, and their emotions become unstable. The features and alterations of characteristics in patients with both AD and MTD often lead to interpersonal rejection sensitivity and social disability. Formerly, Klein suggested the concept of ‘hysteroid dysphoria’ in regards to the disease concept related to AD,17 and recently, AD has been suggested to have the affinity of characteristics or symptoms with bipolar II disorder.9 In the present stage, there exists no specific markers to differentiate MTD from AD, but specific symptoms of AD (hyperphagia, hypersomnia, leaden paralysis, and mood reactivity) seem to be useful for the differentiation.
Dysthymia
Dysthymia is also on the differential diagnosis for MTD, because both show a chronic clinical course and less severe depressive symptoms. In regards to this differentiation, the Japanese psychiatrist Shin Tarumi did not refer to the distinct difference between the two diseases and just stated ‘MTD has not completely become dysthymia yet.’5,6
In DSM-5, dysthymia (dysthymic disorder) was combined with chronic major depressive disorder under the name of persistent depressive disorder.22 The DSM-5 diagnostic criteria for persistent depressive disorder still characteristically include subjective superior symptoms, but not some objective depressive symptoms, such as psychomotor agitation/inhibition and suicidal ideation. These would be common features of MTD. Needless to say, the concept of dysthymia itself has not been clearly defined, which makes the differentiation between MTD and dysthymia more difficult.
Previously, Akiskal developed a framework of soft bipolar from subaffective dysthymia to character-spectrum disorders by therapeutic reactions.23 Similar to soft bipolar, the present situation has suggested that MTD might be heterogeneous. Therefore, further studies are needed to clarify the syndrome of MTD, which has important implications for the selection of appropriate interventions.
Personality disorder
Tarumi did not include the comorbidity of personality disorders (avoidant personality disorder, schizoid personality disorder, or narcissistic personality disorder) in clinical case descriptions of MTD in his original paper.5 However, the international case vignette survey by Kato et al. in 2011 has suggested that personality problem is the most highly influential factor for MTD, and a variety of personality disorders are suggested to be comorbid with MTD.4 The underlying features of personality have yet to been clarified, while psychopathologists have highlighted the temperamental features of MTD syndrome as narcissism (omnipotence) and avoidance.5,6,24 In addition, immaturity may be an important factor.25 People who originally have a tendency toward an immature and narcissistic personality may easily develop depression and evasive behaviors when confronted with stressful situations at school and in the work-place (Fig. 1).
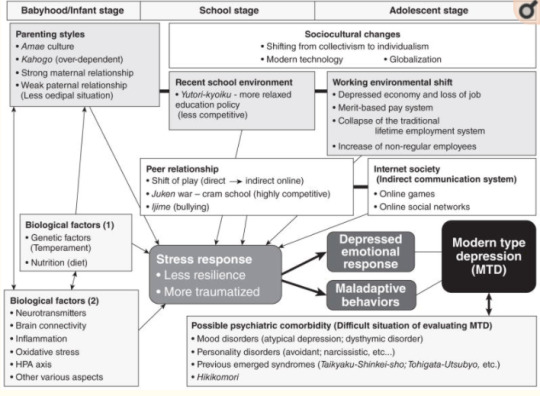
Figure 1. Multidimensional understandings of Japan’s modern type depression (MTD). A variety of psychosocial factors, from the early stages of life through to adolescence, have been suggested to contribute to the onset of MTD. Especially important are childrearing, school and later workplace environments. Within this, parent–child relationships, and how/whether good-enough relationships between peers and friends have been established is vital. The establishment of these bonds can facilitate smooth relationships with workplace colleagues and superiors later in life. However, in MTD, the establishment of such fundamental interpersonal skills during the early stages of life may be insufficient, which can induce vulnerability to stress, meaning that mental dysfunctions are more likely to develop. In other words, lower resilience and the greater possibility of experiencing stress traumatically. Regarding the sociocultural impact in Japan, along with modernization and globalization, there has been a continuing shift away from the hitherto respected and venerated ‘group mentality’ to an ‘individualism’ in which individual achievements are pursued and this shift has resulted in rapid changes in school and work environments. In addition, we suppose that such sociocultural factors are occurring along with an interrelated biological basis, and it is important not to ignore underlying biological factors. With regards to diagnosis and evaluation of MTD, we are in a transitional period and a differential method to distinguish from existing psychiatric diagnoses is warranted. HPA, hypothalamic–pituitary–adrenal.
On the other hand, in the case vignette survey, only Japanese psychiatrists disregarded the factor of personality – SK, that is, immodithymia – as a component cause of Japan’s traditional type of depression, while many psychiatrists in other countries believed that the SK personality strongly affects the onset of depression as a pathological factor. Generally speaking, the Japanese are regarded to be a diligent, scrupulous and hard-working people, and such personality traits have been positively accepted and moreover encouraged in Japanese society over a long period of history since the Samurai era.26 However, these personality traits are not always considered to be positive but as a cause of illness, such as obsessional personality, by experts, including psychiatrists, anthropologists and sociologists in Japan and other countries.27,28 Therefore, Japanese psychiatrists’ opinions in the case vignette survey indicate that not only lay people but also psychiatrists in Japan have been influenced by such Japanese cultural contexts.4
Interestingly, a Japanese clinical study, published in 1997, suggested that TM, which is similar to SK, is not the premorbid personality trait of unipolar (endogenous) depression in Japan.29 This result might have predicted the recently suggested prototype shift of depression in Japan from TM to TD.30
On the other hand, Kotov et al. performed a meta-analysis regarding the association between the personality traits in the Big Three model (negative emotionality, positive emotionality, and disinhibition vs constraint) and Big Five model (neuroticism, extraversion, conscientiousness, agreeableness, and openness), and common psychiatric disorders, such as depression, anxiety and substance abuse disorders.31 The meta-analysis revealed that these common psychiatric disorders are strongly connected to personality. Both major depressive disorder (MDD) and dysthymic disorder showed a similar tendency for high neuroticism and low conscientiousness. Dysthymic disorder showed the most pathological profile. Actually, more than other ailments, dysthymic disorder showed extremely negative extraversion, negative conscientiousness, and positive disinhibition. There is a fairly small number of studies but this outcome is consistent with the argument that dysthymic disorder may be best seen as a form of personality disorder.32 Indeed, dysthymic disorder tends to be chronic and is often lifelong.33 Hence, prominent personality disturbance can be expected to manifest in dysthymic disorder. Surprisingly, the connection between MDD and extraversion was unexpectedly weak. On the other hand, low extraversion was revealed to play an important role in dysthymic disorder. Prospective studies are extremely rare in this field and a causal relationship is yet to be elucidated. Moreover, there are only a few longitudinal studies, the problem of comorbidity, and other limitations (Japanese clinical data seem not to be included in this meta-analysis). In spite of these limitations, this meta-analysis is an important resource when considering the relationship between MTD and personality.
Further clinical, psychopathological and epidemiological studies are needed to clarify underlying personalities, temperaments and characteristics of depression and MTD among particular cultural groups.
Sociocultural Aspects
Psychiatric disorders are strongly influenced by culture, society, history and region.34,35 In any case, much attention should be paid to any medical culture that allows for an immediate diagnosis and the dispensation of medicines in such cases. Japan’s rapid socioeconomic and cultural changes have affected the lifestyle, behavior and mentality of people of all ages in Japan,36 and new types of psychiatric disorders or behavioral disorders have recently appeared in Japan. Tarumi suggested that MTD is caused by the unique Japanese cultural background and sociocultural changes in Japan.5,6 Tarumi regarded MTD as the byproduct of Japan’s historical socioeconomical shifts; beginning with World War II, the following period of high and rapid economic growth (1960–1980s), the economic crisis (1990s), and the diversity and complexity of modern society in the 21st century.5,6 Traditionally, Japanese society has greatly encouraged immodithymia, but modernization, globalization and the introduction of Western culture have led to a mixture of cultures and the celebration of individualism in Japan. The effects of changes in the education system and a move from its traditional disciplinarian base to Yutori education, a system that emphasizes the individual and freedom, may have been great. In the corporate world, the collapse of the traditional nenkō joretsu or seniority-based promotion system will also have had an effect. With the disintegration of the seniority system, there has been an evolution to an intensely competitive society and a distancing from the traditionally harmonious Japanese sense of group belonging.37 It has been suggested that a lack of a sense of belonging could be behind the increase in middle–older-age suicide.38,39 With regards to MTD, the problem of such a sense of belonging may be another major consideration. In the corporate world, younger employees who do not have such a sense of belonging and exhibit aspects of depression at work are often able to function normally and happily with such a sense on weekends, at places of leisure and/or online (Facebook, etc.), and this may reflect that very lack of a sense of belonging within the traditional Japanese organizations. According to the analysis by Takahashi et al.,40 the Japanese corporate organization gave a sense of belonging and community to workers because of its long-term-based relationship under the systems of seniority and permanent employment. After the burst of the bubble economy in the 1990s, however, these traditional systems collapsed and this organization no longer provides a sense of community or belonging.
Unfortunately, Japanese society had not prepared for the effects of this transition. Thus, patients with symptoms of MTD may have often been judged as lazy or ‘sloths’ because one of the most highlighted characteristics of MTD is the tendency to feel depressed only during work or at school.4,18
MTD and hikikomori based on amae
While the psychopathology of MTD is not well understood, it has been suggested that it is related to amae and other Japanese forms of mentality, a suggestion that raises the possibility of MTD as a cultural syndrome or form of psychopathology that predominates in Japan.28
Takeo Doi, a psychiatrist and psychoanalyst, described Japanese dependent behaviors with the word amae.28 The person who is acting amae may beg or plead, or alternatively act selfishly and indulgently, while secure in the knowledge that the caregiver will forgive this. The behavior of children towards their parents is the most typical example of amae. Doi argued that child-rearing practices in Western society seek to stop this kind of dependence in children, whereas in Japan it persists into adulthood in all kinds of social relationships.28 Even now, compared to Western societies, in Asian societies, including Japan, Korea and Taiwan, young people tend to be more economically dependent on their parents, and this phenomenon seems to be one of the expressed forms of amae.41 Hikikomori, a form of social withdrawal characterized by persistent isolation in one’s home for more than 6 months, may be indirectly promoted by amae to the extent that parents accept their child staying at home for prolonged periods of time.41 Even though the concept of amae was originally considered to be uniquely Japanese, contemporary opinions suggest that amae is actually more universal in nature.42 Thus, there is an interesting parallel to hikikomori that has been thought of as unique to Japan but, as our preliminary results show, is perceived by psychiatrists as occurring in a variety of other countries.41 In addition, our international clinical investigations have revealed real hikikomori persons in different countries, including the USA.43,44 These facts suggest that hikikomori and/or MTD could also be a universally observed psychiatric problem.
Cultural/social psychological understandings of MTD and hikikomori
The sociocultural background and tradition of amae is related to hikikomori and MTD. On the other hand, as another research stream, cultural psychologists and social psychologists have focused on the cultural uniqueness of inter-dependence with experiment and quantitative methods.45–49 A common argument being that East Asians are more collectivistic and/or more inter-dependent than Westerners.50–52 In a collectivist culture, inter-dependence is emphasized and in an individualist culture, independence has more value than inter-dependence. A common traditional assumption of these concepts is that collectivistic people tend to prefer harmonious inter-dependence to individual motivation or self-interest. This means that collectivists are ‘harmony seekers.’ On the other hand, Hashimoto and Yamagishi have claimed that the above assumption is not necessarily true, and have recently proposed a novel dimension, namely ‘dis-engaging inter-dependence.’53 They have claimed that the conventional distinction has focused only on dis-engaging independence and engaging interdependence, and relatively ignored the opposite (engaging independence and dis-engaging interdependence). Engaging independence is characterized as voluntary formation of interaction relationships with others to find desirable interaction partners and to prove to others that one is a desirable interaction partner. Hence, individualistic and harmonious. On the other hand, dis-engaging interdependence is characterized as ‘rejection avoidance’ to try to confirm qualification of informal membership in a given social group by following the group norm and informal rules. It is not voluntary adaptation for the group, but motivated to avoid being ostracized by other group members. Hence, collectivistic but not harmonious.
Of these categories, dis-engaging inter-dependence may be deeply related to MTD and also hikikomori. Patients with MTD tend to avoid many interpersonal relationships because they are so afraid of being hurt and humiliated by others. They are always scared of potential psychological attack from others. In particular, hikikomori persons do not want to leave their homes. For them, their family is the only group that they are convinced will not hurt them. This is consistent with the characteristics of dis-engaging interdependence. Although an empirical demonstration has yet to be carried out, it would be plausible to consider MTD patients as having much higher levels of dis-engaging inter-dependence than normal and healthy people. According to Hashimoto and Yamagishi,53,54 comparing student samples from the USA and Japan, the Japanese showed significantly higher scores on dis-engaging inter-dependence than Americans. This may be indirect evidence that it can be related to MTD because currently MTD is frequently observed among youth in Japan. Interestingly, a recent review article by Li and Wong has indicated the interaction between hikikomori and inter-dependence.55 It is necessary to conduct systematic empirical research to investigate the relationship (and/or causality) between MTD and dis-engaging inter-dependence.
Biological Factors
While the biological foundation of MTD is unknown, some specific biological mechanisms are worth speculation. The frequently observed clinical viewpoint that treatment with only the standard pharmacological therapies for depression is not successful for patients with MTD has strongly suggested that a different biological mechanism from traditional depression may exist in the biological features of MTD.
Abnormal function of the hypothalamic–pituitary–adrenal (HPA) axis has long been proposed as a candidate biological foundation of depression.56 A number of studies using the dexamethasone (DEX)/corticotrophin-releasing hormone (CRH) test have been conducted for the assessment of HPA axis function in patients with depression, while these outcomes have been inconsistent.57 The inconsistency may result from the heterogeneity of depression. Hori et al. have reported key findings in elucidating the heterogeneity of depression using the DEX/CRH test and the Temperament and Character Inventory in patients with MDD.58 MDD patients with high cooperativeness showed exaggerated cortisol reactivity; on the contrary, patients with low cooperativeness and high reward dependence showed blunted cortisol reactivity.58 In addition, Hori et al. revealed that MDD patients with escape-avoidance coping showed blunted cortisol reactivity.59 On the other hand, schizotypal personality traits60 and low novelty-seeking with harm avoidance61 in healthy adults are reported to be correlated with exaggerated cortisol reactivity, which proposes the possibility that functions of the HPA axis differ with character and temperament. Low cooperativeness and escape-avoidance coping coincide with the features of MTD, thus the biological foundation of MTD may, at least to some extent, result from abnormal functions of the HPA axis. While not MTD, abnormal function of the HPA axis (abnormal cortisol reactivity in DEX/CRH test) has also been observed in patients with borderline personality disorder62 and atypical depression.63 Based on the above data, Kunugi et al. has recently proposed a classification of depression focusing on the HPA axis functions.64
Interestingly, a recent clinical research regarding atypical depression has suggested a significantly higher comorbidity with metabolic syndrome.65 Metabolic syndrome has recently been suggested to be related to oxidative stress and inflammation.66 Our pilot study has indicated a correlation between serum proinflammatory cytokines and depressive symptoms/personality traits in Japanese university students (unpub. data). We propose an inflammation hypothesis of psychiatric diseases, including depression, via microglia, brain immune cells.67–71 These data may suggest that inflammation and oxidative stress may link to MTD. Further translational studies are needed to clarify the biological foundation of MTD.
Therapeutic Approach
No systematic data have been reported regarding therapeutic interventions of MTD. While our previous case vignette survey has suggested that both psychotherapy and pharmacotherapy were recommended to treat MTD, psychotherapy was especially preferred by psychiatrists in all countries.4 Interestingly, Japanese psychiatrists seemed to hesitate to recommend pharmacotherapy for MTD. In addition, some Japanese psychiatrists hesitated to treat MTD at all. These data have indicated that Japanese psychiatrists, at least to some extent, regard MTD as a non-medical condition. This was in contrast to most psychiatrists in other countries endorsing the need for active treatments to MTD.4 Why is there a discrepancy in psychiatrists’ attitudes toward MTD? These findings may suggest that Japanese psychiatrists themselves are bound to their own socio-cultural and historical contexts.4
The arrival of new antidepressants to Japan in 1999 has also been suggested to have influenced the public view toward depression,72 and may have led to a similar phenomenon occurring in Western countries.73 Previously, depressed persons had tended to hesitate to visit psychiatrists, and Japanese psychiatrists had tended to equate depression only with the traditional melancholic type. Perhaps with the introduction of public awareness campaigns for depression and antidepressants, people who considered themselves depressed began to feel less self-conscious about visiting psychiatrists. This may have been a contributing factor leading to increasing numbers of visits of depressed persons to psychiatrists in Japan.4 However, as the case vignette survey implies, this popular shift has not been accompanied by similar changes in the perception of Japanese psychiatrists, who have very much remained deeply bound to earlier, more traditional conceptions of depression. On the other hand, the results of the case vignette survey indicate that psychotherapy was regarded to be of importance for MTD patients with Japanese psychiatrists who did not see a role for pharmacotherapy.4 Therefore, public education about depression and psychotherapy as a treatment should also be considered as one of the possible solutions to alleviate this discrepancy between the general population and psychiatrists in Japan.
Therapeutic strategies regarding MTD based on pathophysiological understandings should be established. We hypothesize that child and adolescent development has been impacted by rapid environmental changes, which may cause the novel phenomenon. The ways of ‘playing’ among children and adolescents have dramatically shifted from ‘direct playing’ (direct communication in a physical space, such as outdoors or in parks) to ‘indirect playing’ (indirect virtual communication via video games and Internet-related materials) within the past decades.36 People who have grown up in such new environments may become confused and depressed when they enter the traditional workforce and encounter the need for real direct communication. Therefore, psychoeducation and (group) psychotherapy may be the recommended approaches in order to develop skills of direct communication, which may lead to a smoother adjustment to adult communication environments. In addition, pharmacological and social approaches may also be effective. Clinical research to measure therapeutic responses should be performed to dig up the appropriate intervention.
How to Solve the Issues Associated with MTD
Blind-spots of the DSM system
Recently, early-career psychiatrists in Japan have considered that it is possible to make diagnoses based solely on the abbreviated pocket-sized DSM-IV-TR. This book, entitled the Quick Reference to the Diagnostic Criteria from DSM-IV-TR,3 states that it is intended to be used in combination with the unabridged version of the DSM-IV-TR (which is 900+ pages in length).74 In fact, the DSM-IV-TR also states in an introductory section entitled ‘Cautionary Statement’ that ‘the proper use of these criteria requires specialized clinical training that provides both body of knowledge and clinical skills.’ Many early-career psychiatrists seem to be unaware of these facts. The DSM-IV-TR includes detailed explanations of diagnostic criteria, diagnostic features, and differential diagnoses for each disorder. However, even in the unabridged version, there is no mention of which examinations should be performed in the garnering of information for each disorder. This can only be achieved through not only reading of psychiatric textbooks but also the accumulation of real clinical experiences with supervisory psychiatrists involving the joint examination of patients in a hospital/clinic setting. However, in reality, early-career psychiatrists who are actually willing to accumulate such valuable experiences are on the decline. In addition, there are some problems based on the nature of operational diagnosis in DSM. Parker indicated that operational criteria of the depression dimensional model in DSM has made it easy to diagnose depression, and also resulted in loose diagnostic practice blunting clarification of causes and treatment specificity of depression.75
On the other hand, the Structured Clinical Interview for DSM-IV (SCID) is considered the best available method for diagnosis of psychiatric disorders, but in reality there are limitations to its applicability. When applying the systematic diagnostic criteria for MDD based on the DSM-IV (and also DSM-5), whilst being relevant, a difficulty arises when strictly applying the criteria. In particular, within the definition of MDD, a continuous depressed mood of more than 2 weeks is one of the criteria for diagnosis, and in reality it is difficult to judge whether this criteria has been met for this continuous period for almost every day for 2 weeks. Furthermore, ambiguity exists regarding the extent at which ‘continuous’ may be defined. In MTD, depressive symptoms are exhibited at work or at school but during weekend rest times or when at home these symptoms are not exhibited. In such cases, are the DSM criteria of ‘for more than 2 weeks’ met? Depending on the psychiatrist, there are those who would diagnose MDD and others who would not. In Japanese clinical settings, for such cases and similar cases where symptoms are even less frequent, there is still a high probability that a diagnosis of MDD will eventuate.
Proposing a novel diagnostic approach to depression
The greatest difficulty in the evaluation and diagnosis of depression is the gap between subjective patient symptoms and objective realities. It is a well-known given among experienced psychiatrists that information garnered from the individual only is not enough in the diagnosis of depression. Information regarding psychiatric symptoms from an individual is no more than ‘subjective symptoms’ and in many cases differs from objective realities. It is particularly difficult for inexperienced psychiatrists to reach a diagnosis for depression based on information garnered solely from the individual but it is also often the case that treatment is commenced without understanding this reality. Moreover, it is important to note that recently not only psychiatrists but also physicians are diagnosing depression and tend to prescribe antidepressants. In order to improve this situation, changes must be made to allow for a more detailed assessment of the individual’s situation. Along with the individual, the collection of information from family members and other third parties is incredibly important (Fig. 2). When an individual claims to be depressed, an objective assessment is required that cannot be limited to the individual. Because of this, when the only obtainable information is from the individual, a diagnosis of ‘possible’ depression may be preferable. This aspect has not been included in many guidelines of depression; however, it must be of great importance, especially in diagnosing MTD.
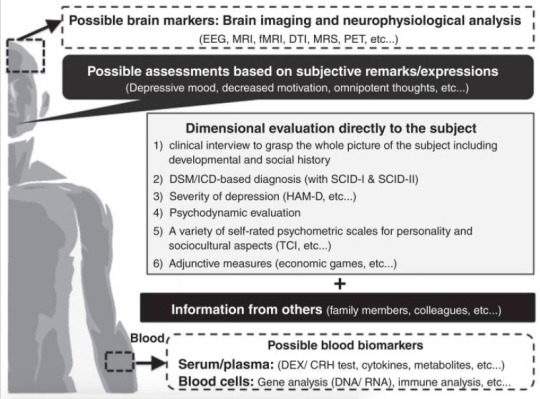
Figure 2. Multi-axial assessments of modern type depression (MTD). In order to evaluate MTD, we recommend utilizing the 1–6 assessment methods directly to depressed persons. In addition, information from others is essential to evaluate such persons. Objective biomarkers of MTD have not been developed until now. Some biomarkers of MTD may overlap with major depressive disorder and other psychiatric diagnosis/syndromes, while some data from brain imaging/neurophysiological analysis and peripheral blood analysis may help to distinguish MTD from other psychiatric conditions. Further investigations should be developed to dig up such biomarkers. CRH, corticotrophin-releasing hormone; DEX, dexamethasone; DTI, diffusion tensor imaging; EEG, electroencephalography; HAM-D, Hamilton Rating Scale for Depression; fMRI, functional magnetic resonance imaging; MRI, magnetic resonance imaging; MRS, magnetic resonance spectroscopy; PET, positron emission tomography; SCID, Structured Clinical Interview for DSM-IV; TCI, Temperament and Character Inventory.
Using a three-tier diagnostic system (possible/probable/definite)
Here, we propose a novel criteria that can make evaluation/diagnosis of depression understandable even for less experienced psychiatrists.76 Along the lines of a diagnostic system for many physical illnesses (cancer, etc ) and dementia, we propose that diagnosis of depression should be divided into the three tiers of ‘possible,’ ‘probable’ and ‘definite.’ The first tier (possible) would be ‘diagnosis based on information from the subject only,’ the second tier (probable) would be ‘diagnosis based on the information from the subject and other sources (family or colleagues, etc.),’ and the third tier (definite) would be ‘diagnosis based on information from the subject + (family, colleagues, etc.) + (intensive clinical examination during outpatient clinic and/or hospitalization).’ Furthermore, we believe that each tier should have a different treatment guideline.77 By utilizing this novel diagnostic system, we can avoid the tendency to overdiagnose depression in persons with MTD tendencies (Fig. 2).
Investigating research into adjunctive measures, such as economic games
In addition, economic games, such as the trust game, have been utilized to evaluate real-world interpersonal relationships as a novel candidate for psychiatric evaluations. Economic games have been developed in the field of social psychology and economics, and have been proposed as a novel tool for evaluating interpersonal psychiatric problems. Clinical studies using economic games (prisoner’s dilemma, the public goods game, the ultimatum game and the trust game) have revealed some difficulties of social decision-making in individuals with MDD and personality disorders.77–80 The trust game, an economic game, has been widely used to evaluate a person’s trust toward others.81 In this two-person game, the first player has to make a risky financial decision depending on how much s/he would trust the second player (partner). Recent studies have examined whether other factors, such as personality and psychiatric conditions, influence trusting behaviors and cooperation.79,80,82–84 As a pilot study, we recently conducted a trust game experiment with 81 Japanese university students.85 Clinical case reports have indicated that people with MTD and hikikomori have difficulties in developing trust among family members, and colleagues in schools and working places.86–88 Therefore, a common feature of modern psychiatric syndromes may be induced through difficulty in trusting others, and these features may not be limited to patients but also to the wider contemporary populations, especially the young. In the economic experiment, participants made a risky financial decision about whether to trust each of 40 photographed partners.85 Participants then answered a set of questionnaires, including the Patient Health Questionnaire (PHQ)-9. Regression analysis revealed that item 8 of the PHQ-9 (subjective agitation and/or retardation) for female participants was associated with participants’ trusting behaviors. Women with higher subjective agitation (and/or retardation) gave less money to men and highly attractive women, but more to less attractive women in interpersonal relationships. This indicates that women with high subjective agitation may tend to make more defensive and cautious decisions in daily life, which may cause difficulties in various social interactions. These data indicate the possible impact of economic games in psychiatric research and clinical practice, including MTD, and further validation should be investigated.
Conclusion
In this review paper, we introduced MTD, citing the few scientific reports available and offered our collective experiences and perspectives on its diagnosis and treatment. In Japan, MTD refers to a syndrome with predominant symptoms of depression and withdrawal that has rapidly increased among youth since around 2000. It is worth recalling that the phenotype of mental illness – be it the appearance of late-19th century hysteria, the appearance of post-1950 eating disorders, or post-1970 borderline personality disorders – is transforming along with society. Despite the lack of agreement upon diagnostic criteria of MTD, it may be considered that cultural, social, and biological factors are all involved in its development and Japanese cultural and social influences may be creating MTD (Fig. 1). In Japan, along with MTD, social withdrawal syndrome (i.e. hikikomori) is concurrently prevalent amongst youth and is considered a great social problem. We hypothesize that the onset of MTD and a prolonged maladaptive social situation may be one of the causal factors of hikikomori. As we may consider ‘withdrawal/avoidance’ to be a common factor in both syndromes, further research regarding shared psychopathology and risk factors in modern society is necessary. We believe that combating MTD may also rescue hikikomori. Differentiation of MTD from other psychiatric disorders has not been established under the present situation, while we have newly classified MTD and related psychiatric disorders (syndromes) from the following two aspects: maturation of personality and ability for social interaction (Fig. 3).
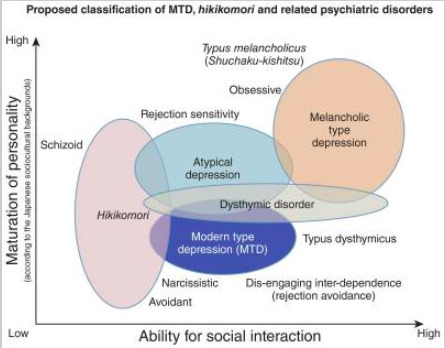
Figure 3. Proposed classification of modern type depression (MTD), hikikomori and related psychiatric disorders. Based on the maturation of personality and ability of social interaction, we have classified the five psychiatric disorders (syndromes), including MTD and hikikomori. The level of personality maturation in this figure is based on the Japanese sociocultural contexts. In Japan, melancholic personality (Typus melancholicus or Shūchaku-kishitsu) has long been regarded as matured personality, while this perspective may not be applied in other countries with different sociocultural backgrounds.
We have suggested the necessity for the introduction of novel methods of evaluation, not only limited to the diagnosis of MTD but to depressive disorders in general, as we consider the modern usage of psychiatric tools that rely on subjective claims by patients to be insufficient. In particular, we recommend the addition of: third-party evaluations to the diagnostic criteria; the usage of economic game experiments and the like; and the evaluation of actual behavioral characteristics. It is hoped that through the introduction of these tools, a more accurate diagnosis of depressive disorders will become possible. The development of a new multi-axial evaluation and diagnostic tool that incorporates such new tools is required (Fig. 2). As the nosology of MTD has not been validated, we need to keep in mind that the presented data shown in the ‘biological factors’ and ‘therapeutic approach’ sections does not directly provide the findings of MTD (mixed with issues regarding major depression in general). In order to advance MTD research, we have proposed research-based draft operational criteria for MTD (Table 2). The draft operational criteria are limited to research use at the present stage. We hope that in the near future, a breakthrough diagnostic and treatment methodology for MTD will be developed based on these draft criteria.
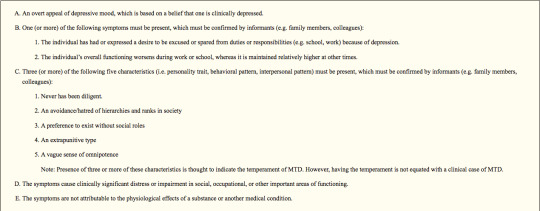
Table 2. Proposed research-based operational criteria and intervention for ‘modern type depression (MTD)’: Provisional –recommended only for research use.
In order to advance MTD research, MTD should be defined with more systematic methodology. Thus, we herein propose operational criteria for MTD based on the present knowledge of MTD. The draft operational criteria are for research use at the present stage. Based on research with the draft criteria, clinically useful operational criteria should be developed in the near future. Of note, five components are listed as representative of MTD in Item C. In order to evaluate the temperament of MTD, the person must be comprehensively assessed, including personality, development, life history and present status. In order to help conduct the assessment more efficiently, a self-report questionnaire (‘MTD-trait scale’) for evaluation of MTD temperament is being developed (Kato et al. unpub. material). HAM-D, Hamilton Rating Scale for Depression; MDD, major depressive disorder; MTD, modern type depression.
References
1. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960; 23:56–62. [PubMed: 14399272]
2. Furukawa TA, Streiner DL, Azuma H, et al. Cross-cultural equivalence in depression assessment: Japan-Europe-North American study. Acta Psychiatr Scand. 2005; 112:279–285. [PubMed: 16156835]
3. American Psychiatric Publishing. Quick Reference to the Diagnostic Criteria from DSM-IV-TR. American Psychiatric Publishing, Inc; Arlington, VA: 2000.
4. Kato TA, Shinfuku N, Fujisawa D, et al. Introducing the concept of modern depression in Japan: An international case vignette survey. J Affect Disord. 2011; 135:66–76. [PubMed: 21782250]
5. Tarumi S, Kanba S. Sociocultural approach toward depression – Dysthymic type depression. Jpn Bull Soc Psychiatr. 2005; 13:129–136. (in Japanese).
6. Tarumi S. The ‘new’ variant of depression: The dysthymic type. Jpn J Clin Psychiatr. 2005; 34:687– 694. (in Japanese).
7. Benazzi F. Testing atypical depression definitions. Int J Methods Psychiatr Res. 2005; 14:82–91. [PubMed: 16175877]
8. Blanco C, Vesga-Lopez O, Stewart JW, Liu SM, Grant BF, Hasin DS. Epidemiology of major depression with atypical features: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry. 2012; 73:224–232. [PubMed: 21939615]
9. Akiskal HS, Akiskal KK, Perugi G, Toni C, Ruffolo G, Tusini G. Bipolar II and anxious reactive ‘comorbidity’: Toward better phenotypic characterization suitable for genotyping. J Affect Disord. 2006; 96:239–247. [PubMed: 16973219]
10. Shimoda M. On the treatment of involutional depression in my department. Taiwan Igaku Zasshi. 1932; 31:113–115. (in Japanese).
11. Tellenbach, H. Melancholie. Springer; Berlin: 1961.
12. Walters, PA, Jr. Student apathy. In: Blame, GB., Jr, McArthur, CC., editors. Emotional problems of the student. Appleton-Century-Crofts; New York: 1961. p. 129-147.
13. Kasahara Y, Kimura B. Utsu-byo no rinshoteki-bunrui ni kansuru kenkyu. Seishin Shinkeigaku Zasshi. 1975; 77:715–735. (in Japanese). [PubMed: 1243687]
14. Hirose, T. Tohi-gata utsu-byo ni tsuite. In: Miyamoto, T., editor. Sou-utsu-byo no seishin-byori 2 [Psychopathology of Manic-Depressive Illness 2]. Kobundo, Tokyo: 1977. p. 61-86.
15. Matsunami K, Yamashita Y. Syakai-hendo to utsu-byo [Social changes and depression]. Jpn Bull Soc Psychiatr. 1991; 14:193–200. (in Japanese).
16. Abe T, Otsuka K, Nagano M, Kato S, Miyamoto T. A consideration on ‘Immature Type of Depression’: Premorbid personalities and clinical pictures of depression from the structural- dynamic viewpoint (W. Janzarik). Jpn Clin Psychopathol. 1995; 16:239–248. (in Japanese).
17. Klein DF, Liebowitz MR. Hysteroid dysphoria. Am J Psychiatry. 1982; 139:1520–1521. [PubMed: 7137409]
18. Kato TA, Shinfuku N, Sartorius N, Kanba S. Are Japan’s hikikomori and depression in young people spreading abroad? Lancet. 2011; 378:1070. [PubMed: 21924990]
19. Shimoda M. Shuchaku-kishitsu ni tsuite. Yonago Igaku Zasshi. 1950; 2:1–2. (in Japanese).
20. Kanba S. Modern interpretation of Shimoda’s shuchaku-kishitsu. Kyushu Neuro-Psychiatry. 2006; 52:79–88. (in Japanese).
21. Ohmae S. The modern concept of atypical depression: Four definitions. Seishin Shinkeigaku Zasshi. 2010; 112:3–22. (in Japanese). [PubMed: 20184236]
22. American Psychiatric Publishing. Diagnostic and Statistical Manual of Mental Disorders. 5. American Psychiatric Publishing; Arlington, VA: 2013.
Psychiatry Clin Neurosci. Author manuscript; available in PMC 2017 August 17.
VA Author Manuscript VA Author Manuscript VA Author Manuscript
Kato et al.
Page 16
23. Akiskal HS. Dysthymic disorder: Psychopathology of proposed chronic depressive subtypes. Am J Psychiatry. 1983; 140:11–20. [PubMed: 6336637]
24. Hirose T. Depression of avoidant type compared with depression of dysthymic type. Jpn J Clin Psychiatr. 2008; 37:1179–1182. (in Japanese).
25. Abe T. Depression from the viewpoint of life stage: Diagnosis and treatment. Jpn J Psychosom Med. 2009; 49:987–993. (in Japanese).
26. Nitobe, I. Bushido: The Soul of Japan. G. P. Putnam’s Sons; New York: 1906.
27. Benedict, RF. The Chrysanthemum and the Sword: Patterns of Japanese Culture. Houghton Mifflin; Boston, MA: 1946.
28. Doi, T. The Anatomy of Dependence. Kodensha International; Tokyo: 1973.
29. Furukawa T, Nakanishi M, Hamanaka T. Typus melancholicus is not the premorbid personality trait of unipolar (endogenous) depression. Psychiatry Clin Neurosci. 1997; 51:197–202. [PubMed: 9316163]
30. Kanba S, Kano R, Eguchi S, Utsumi T, Abe T. Has the prototype of depression been shifted? Jpn J Clin Psychiatr. 2008; 37:1091–1109. (in Japanese).
31. Kotov R, Gamez W, Schmidt F, Watson D. Linking ‘big’ personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychol Bull. 2010; 136:768–821. [PubMed: 20804236]
32. Watson D, Clark LA. Depression and the melancholic temperament. Eur J Pers. 1995; 9:351–366.
33. Klein DN, Shankman SA, Rose S. Ten-year prospective follow-up study of the naturalistic course of dysthymic disorder and double depression. Am J Psychiatry. 2006; 163:872–880. [PubMed: 16648329]
34. Tseng, WS. Handbook of Cultural Psychiatry. Academic Press; San Diego, CA: 2001.
35. Alarcon RD. Culture, cultural factors and psychiatric diagnosis: Review and projections. World Psychiatry. 2009; 8:131–139. [PubMed: 19812742]
36. Ogata Y, Izumi Y, Kitaike T. Mobile-phone e-mail use, social networks, and loneliness among Japanese high school students. Nippon Koshu Eisei Zasshi. 2006; 53:480–492. (in Japanese). [PubMed: 16944832]
37. Watabe, M. Social exchange; transition from ‘embedded long-term relationships’ to ‘voluntary short-term relationships’. In: Hibino, A.Watabe, M., Ishii, K., editors. Disconnected Society (Tsunagarenai Shakai). Nakanishiya, Kyoto: 2014.
38. Hatcher S, Stubbersfield O. Sense of belonging and suicide: A systematic review. Can J Psychiatry. 2013; 58:432–436. [PubMed: 23870726]
39. Kim SY, Kim MH, Kawachi I, Cho Y. Comparative epidemiology of suicide sin South Korea and Japan: Effects of age, gender and suicide methods. Crisis. 2011; 32:5–14. [PubMed: 21371965]
40. Takahashi, K., Kawai, D., Nagata, M., Watabe, M. Fukigen na shokuba [Unpleasant Workplace]. Kodansha, Tokyo: 2008.
41. Kato TA, Tateno M, Shinfuku N, et al. Does the ‘hikikomori’ syndrome of social withdrawal exist outside Japan? A preliminary international investigation. Soc Psychiatry Psychiatr Epidemiol. 2012; 47:1061–1075. [PubMed: 21706238]
42. Niiya Y, Ellsworth PC, Yamaguchi S. Amae in Japan and the United States: An exploration of a ‘culturally unique’ emotion. Emotion. 2006; 6:279–295. [PubMed: 16768560]
43. Teo AR, Stufflebam K, Saha S, et al. Psychopathology associated with social withdrawal: Idiopathic and comorbid presentations. Psychiatry Res. 2015; 228:182–183. [PubMed: 25977071]
44. Teo AR, Fetters MD, Stufflebam K, et al. Identification of the hikikomori syndrome of social withdrawal: Psychosocial features and treatment preferences in four countries. Int J Soc Psychiatry. 2015; 61:64–72. [PubMed: 24869848]
45. Heine, SJ. Cultural Psychology. W. W. Norton & Company; New York: 2011.
46. Yamagishi, T. Trust – The Evolutionary Game of Mind and Society. Springer Tokyo; Tokyo: 2011. 47. Yamagishi T, Cook KS, Watabe M. Uncertainty, trust, and commitment formation in the United
States and Japan. Am J Sociol. 1998; 104:165–194.
48. Cross SE, Hardin EE, Gercek-Swing B. The what, how, why, and where of self-construal. Pers Soc Psychol Rev. 2011; 15:142–179. [PubMed: 20716643]
49. Markus HR, Kitayama S. Culture and the self: Implications for cognition, emotion, and motivation. Psychol Rev. 1991; 98:224–253.
50. Oyserman D, Coon HM, Kemmelmeier M. Rethinking individualism and collectivism: Evaluation of theoretical assumptions and meta-analyses. Psychol Bull. 2002; 128:3–72. [PubMed: 11843547]
51. Matsumoto D. Culture and self: An empirical assessment of Markus and Kitayama’s theory of independent and interdependent self-construals. Asian J Soc Psychol. 1999; 2:289–310.
52. Levine TR, Bresnahan MJ, Park HS, et al. Self-construal scales lack validity. Hum Commun Res. 2003; 29:210–252.
53. Hashimoto, H., Yamagishi, T. Center for the Study of Cultural and Ecological Foundations of the Mind Working Paper Series. Hokkaido University; 2014. Engaging and disengaging aspects of independence and interdependence: An adaptationist perspective.
54. Hashimoto H, Yamagishi T. Two faces of interdependence: Harmony seeking and rejection avoidance. Asian J Soc Psychol. 2013; 16:142–151.
55. Li TM, Wong PW. Youth social withdrawal behavior (hikikomori): A systematic review of qualitative and quantitative studies. Aust N Z J Psychiatry. 2015; 49:595–609. [PubMed: 25861794]
56. Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000; 23:477–501. [PubMed: 11027914]
57. Holsboer F, von Bardeleben U, Wiedemann K, Muller OA, Stalla GK. Serial assessment of corticotropin-releasing hormone response after dexamethasone in depression. Implications for pathophysiology of DST nonsuppression. Biol Psychiatry. 1987; 22:228–234. [PubMed: 3028512]
58. Hori H, Teraishi T, Sasayama D, et al. Relationship of temperament and character with cortisol reactivity to the combined dexamethasone/CRH test in depressed outpatients. J Affect Disord. 2013; 147:128–136. [PubMed: 23178186]
59. Hori H, Teraishi T, Ota M, et al. Psychological coping in depressed outpatients: Association with cortisol response to the combined dexamethasone/CRH test. J Affect Disord. 2014; 152–154:441– 447.
60. Hori H, Teraishi T, Ozeki Y, et al. Schizotypal personality in healthy adults is related to blunted cortisol responses to the combined dexamethasone/corticotropin-releasing hormone test. Neuropsychobiology. 2011; 63:232–241. [PubMed: 21494051]
61. Tyrka AR, Wier LM, Price LH, et al. Cortisol and ACTH responses to the Dex/CRH test: Influence of temperament. Horm Behav. 2008; 53:518–525. [PubMed: 18294637]
62. Rinne T, de Kloet ER, Wouters L, Goekoop JG, DeRijk RH, van den Brink W. Hyperresponsiveness of hypothalamic-pituitary-adrenal axis to combined dexamethasone/ corticotropin-releasing hormone challenge in female borderline personality disorder subjects with a history of sustained childhood abuse. Biol Psychiatry. 2002; 52:1102–1112. [PubMed: 12460693]
63. Gold PW, Chrousos GP. The endocrinology of melancholic and atypical depression: Relation to neurocircuitry and somatic consequences. Proc Assoc Am Physicians. 1999; 111:22–34. [PubMed: 9893154]
64. Kunugi H, Hori H, Ogawa S. Biochemical markers subtyping major depressive disorder. Psychiatry Clin Neurosci. 2015; 69:597–608. [PubMed: 25825158]
65. Takeuchi T, Nakao M, Kachi Y, Yano E. Association of metabolic syndrome with atypical features of depression in Japanese people. Psychiatry Clin Neurosci. 2013; 67:532–539. [PubMed: 24152284]
66. Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006; 444:860–867. [PubMed: 17167474]
67. Horikawa H, Kato TA, Mizoguchi Y, et al. Inhibitory effects of SSRIs on IFN-gamma induced microglial activation through the regulation of intracellular calcium. Prog Neuropsychopharmacol Biol Psychiatry. 2010; 34:1306–1316. [PubMed: 20654672]
68. Kato TA, Monji A, Mizoguchi Y, et al. Anti-inflammatory properties of antipsychotics via microglia modulations: Are antipsychotics a ‘fire extinguisher’ in the brain of schizophrenia? Mini Rev Med Chem. 2011; 11:565–574. [PubMed: 21699487]
69. Kato TA, Yamauchi Y, Horikawa H, et al. Neurotransmitters, psychotropic drugs and microglia: Clinical implications for psychiatry. Curr Med Chem. 2013; 20:331–344. [PubMed: 23157624]
70. Mizoguchi Y, Kato TA, Seki Y, et al. Brain-derived neurotrophic factor (BDNF) induces sustained intracellular Ca2+ elevation through the up-regulation of surface transient receptor potential 3 (TRPC3) channels in rodent microglia. J Biol Chem. 2014; 289:18549–18555. [PubMed: 24811179]
71. Monji A, Kato T, Kanba S. Cytokines and schizophrenia: Microglia hypothesis of schizophrenia. Psychiatry Clin Neurosci. 2009; 63:257–265. [PubMed: 19579286]
72. Schulz, K. New York Times. 2004. Did antidepressants depress Japan?.
73. Healy, D. The Antidepressant Era. Harvard University Press; Cambridge, MA: 1997.
74. American Psychiatric Publishing. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Publishing; Arlington, VA: 2000. text rev
75. Parker G. Is depression overdiagnosed? Yes. BMJ. 2007; 335:328. [PubMed: 17703040]
76. Hashimoto R, Yasuda Y, Yamamori H, et al. Is it possible to make a diagnosis of major depression based solely on the medical interview of the patient? Seishinka. 2013; 22:243–249.
77. Wang Y, Zhou Y, Li S, Wang P, Wu GW, Liu ZN. Impaired social decision making in patients with major depressive disorder. BMC Psychiatry. 2014; 14:18. [PubMed: 24450703]
78. Zhang HJ, Sun D, Lee TM. Impaired social decision making in patients with major depressive disorder. Brain Behav. 2012; 2:415–423. [PubMed: 22950045]
79. Brendan Clark C, Thorne CB, Hardy S, Cropsey KL. Cooperation and depressive symptoms. J Affect Disord. 2013; 150:1184–1187. [PubMed: 23726777]
80. King-Casas B, Sharp C, Lomax-Bream L, Lohrenz T, Fonagy P, Montague PR. The rupture and repair of cooperation in borderline personality disorder. Science. 2008; 321:806–810. [PubMed: 18687957]
81. Berg J, Dickhaut J, McCabe K. Trust, reciprocity, and social history. Games Econ Behav. 1995; 10:122–142.
82. Chiu PH, Kayali MA, Kishida KT, et al. Self responses along cingulate cortex reveal quantitative neural phenotype for high-functioning autism. Neuron. 2008; 57:463–473. [PubMed: 18255038]
83. Kato TA, Watabe M, Tsuboi S, et al. Minocycline modulates human social decision-making: Possible impact of microglia on personality-oriented social behaviors. PLoS ONE. 2012; 7:e40461. [PubMed: 22808165]
84. Watabe M, Kato TA, Monji A, Horikawa H, Kanba S. Does minocycline, an antibiotic with inhibitory effects on microglial activation, sharpen a sense of trust in social interaction? Psychopharmacology. 2012; 220:551–557. [PubMed: 21956241]
85. Watabe M, Kato TA, Teo AR, et al. Relationship between trusting behaviors and psychometrics associated with social network and depression among young generation: A pilot study. PLoS ONE. 2015; 10:e0120183. [PubMed: 25836972]
86. Nakano M. How supervisors deal with subordinates who have characteristics of ‘new-type depression’. Rinsho-Shinrigaku. 2014; 14:235–243.
87. Tsujii H, Natsuhori K, Uozumi E. Nursing care for an adolescent hikikomori case with domestic violence: A case report. Nihon Seishinka Kangogaku Kaishi. 2010; 52:72–76.
88. Nakagama H. Integration of individual and family conjoint interview: A case study of a social withdrawal adolescent and his family members. Kazoku-Shinrigaku-Kenkyu. 2008; 22:28–41.
#psychiatry#global psychiatry#cross-cultural psychiatry#atypical depression#mental illness#DSM-5#depression#major depressive disorder#shūchaku-kishitsu#diagnosis#diagnostic symptoms#modern type depression#dysthymia#classification#hikikomori
1 note
·
View note
Text
a dissertation nobody asked for, ft. my dysphoric trans ass (on the subject of truscum, cisgender medicine, and stupid assholes)
BOY HOWDY DID THIS GET LONG
I know that nobody asked for this post, and definitely nobody needed it, but you know what? Fuck it. You’re getting this post anyway.
Very recently someone in the community outed himself (himself, because I’m aware that he uses he/him pronouns and am not a piece of shit who will misgender someone under guise of offering anonymity. Cough cough.) as a transmedicalist. A truscum, if you will, because we all know that they mean the same thing and anyone who tries to convince you otherwise is a bitchcoward and a bigot.
Very disappointing, yes, considering the amount of transgender people* I know exist in this community, myself included. Disappointing, frightening, and rage-inducing. Particularly because this revelation followed an encounter said truscum had with a close friend of mine. Which I admit might make me a little biased but shhh. Neither me nor my friend(s) started this. The contents of that conversation had between the truscum and my bro should have been handled privately like an adult but- hey, since we’re putting all this shit out there now, guess I get to put in my two cents! Awesome!
And because we apparently like to bring science into shit, let’s get a lil scientific up in this bitch.
*Note: transgender from here on will be used to refer to as the umbrella of non-cis gender identities just for context and ease of reference. And also because that’s what it is, fuck off.
So, guys. Let’s talk about dysphoria.
PART 1. SEMANTICS
Dysphoria. Most of you have heard of it, particularly those among us (both within and outside of the fantroll community) who happen to be transgender.
But what does it actually mean? Let’s look a little closer. Dysphoria, as defined by Merriam-Webster:
dysphoria (noun)
dys·pho·ria | \ dis-ˈfȯr-ē-ə \
Definition of dysphoria
: a state of feeling very unhappy, uneasy, or dissatisfied
— see GENDER DYSPHORIA
But this is just semantics. Let’s look at it, and gender oriented dysphoria in particular from a mental health perspective-
“Gender dysphoria is the feeling of discomfort or distress that might accompany a difference between gender identity, sex assigned at birth or sex-related physical characteristics. This type of distress doesn't affect everyone who is transgender.
Gender dysphoria is listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a manual published by the American Psychiatric Association to diagnose mental conditions. Gender dysphoria is a diagnosis that is given to individuals who are experiencing discomfort or distress due to the difference between gender identity, sex assigned at birth or sex-related physical characteristics.”
This is from the Mayo Clinic, a nonprofit academic medical center based in Rochester, Minnesota, lauded as the best hospital in the nation for 2018-2019 by the U.S News and World Report. Do with that information what you will, but most would consider the Mayo Clinic (while not a good replacement for proper doctor’s visits and medical treatment) a pretty credible health resource.
But we’ll come back to this.
For now, let’s look at another definition. That of the word ‘opinion.’
PART 2: FACTS VS. OPINIONS VS. BELIEFS VS. PREJUDICE
opinion (noun)
opin·ion | \ ə-ˈpin-yən \
Definition of opinion
1a : a view, judgment, or appraisal formed in the mind about a particular matter
We asked them for their opinions about the new stadium.
b : APPROVAL, ESTEEM
I have no great opinion of his work.
2a : belief stronger than impression and less strong than positive knowledge
a person of rigid opinions
Opinions are inherently biased. It may be influenced by facts, but opinions in and of themselves are not fact. To borrow and paraphrase from Fowler, H. Ramsey. The Little, Brown Handbook. Boston: Little, Brown, 1986.:
When forming personal convictions, we often interpret factual evidence through the filter of our values, feelings, tastes, and past experiences. Hence, most statements we make in speaking and writing are assertions of fact, opinion, belief, or prejudice. The usefulness and acceptability of an assertion can be improved or diminished by the nature of the assertion, depending on which of the following categories it falls into:
A fact is verifiable. [Determinable by] ...researching the evidence. This may involve numbers, dates, testimony, etc. (Ex.: "World War II ended in 1945.") The truth of the fact is beyond argument if one can assume that measuring devices or records or memories are correct. Facts provide crucial support for the assertion of an argument. However, facts by themselves are worthless unless we put them in context, draw conclusions, and, thus, give them meaning.
An opinion is a judgment based on facts, an honest attempt to draw a reasonable conclusion from factual evidence. [Opinions are] potentially changeable--depending on how the evidence is interpreted. By themselves, opinions have little power to convince. You must always let your reader know what your evidence is and how it led you to arrive at your opinion.
Unlike an opinion, a belief is a conviction based on cultural or personal faith, morality, or values. Statements such as "Capital punishment is legalized murder" are often called "opinions" because they express viewpoints, but they are not based on facts or other evidence. They cannot be disproved or even contested in a rational or logical manner. Since beliefs are inarguable, they cannot serve as the thesis of a formal argument. (Emotional appeals can, of course, be useful if you happen to know that your audience shares those beliefs.)
Y’all get what I’m getting at, right?
Oh, but one more thing I’d like to add- And I think this one is important.
“Another kind of assertion that has no place in serious argumentation is prejudice, a half-baked opinion based on insufficient or unexamined evidence. (Ex.: "Women are bad drivers.") Unlike a belief, a prejudice is testable: it can be contested and disproved on the basis of facts. We often form prejudices or accept them from others--family, friends, the media, etc.--without questioning their meaning or testing their truth. At best, prejudices are careless oversimplifications. At worst, they reflect a narrow-minded view of the world. Most of all, they are not likely to win the confidence or agreement of your readers.”
We’ve all encountered our fair share of these sorts of prejudices, disguised as “opinions.” Because isn’t that a much sweeter word for what it is? It’s not bigotry to delegitimize the experiences of other transgender people, it’s just an opinion. Like which is the best ice cream flavour, or something equally harmless.
But when your opinion involves the dehumanization, invalidation, exclusion and harm of other people… Well, that’s not so harmless, is it?
Racism is prejudice influenced by opinions and beliefs. Transphobia is prejudice influenced by opinions and beliefs. They are not fact, they are not based in rational thinking, and in many cases they cannot be argued because these prejudices are willingly cultivated and held.
‘But, Eli!’ I know at least one truscum who may or may not be reading this might cry, ‘It’s a scientifically proven fact that transgender people need to have dysphoria to be trans!’
To which I say fuck you, this is why that isn’t true.
Let’s go back to the definition of gender dysphoria, shall we?
“Gender dysphoria is the feeling of discomfort or distress that might accompany a difference between gender identity, sex assigned at birth or sex-related physical characteristics. This type of distress doesn't affect everyone who is transgender.”
MIGHT accompany a difference between those things, and DOESN’T affect everyone who is transgender. Interesting take coming from a scientific source, right? It’s almost like transmedicalist/truscum thinking is based off prejudice, rather than opinion; much less fact.
Especially considering dysphoria wasn’t even a word we (we meaning transgender people) chose for ourselves in the first place. It was picked by the American Psychiatric Association’s board of trustees to replace the term “Gender Identity Disorder” (GID)
Disorder. A sickness. Because Western medicine, practiced primarily by cisgender people (be they medical experts or not) has never been kind to transgender people. The word doesn’t mean what transmedicalists or truscum think it does. It doesn’t make you more valid than our fellow trans siblings just because the perceptions held by you or others of what your body and gender are worth make you miserable.
Wanna read up a little more on this? Check out these links:
THIS IS WHAT I WISH PEOPLE WHO IDENTIFY AS ‘TRUSCUM’ WOULD TRY TO UNDERSTAND.
Not All Transgender People Have Dysphoria – And Here Are 6 Reasons Why That Matters
Transgender People, Gender Identity and Gender Expression
PART 3: THE COMMUNITY (™)
If you’re dysphoric, my heart goes out to you. I’m dysphoric too. Dysphoric enough to transition despite the medical costs- because I was tired of feeling trapped in other people’s perceptions of me. But you know what? I love that there are transgender people who don’t feel defined by this persistent sensation of wrongness.
You shouldn’t be defined by that. Even dysphoric trans people know (or should, for the sake of their health) that your unhappiness isn’t the only thing that makes you transgender. In fact, in the least unhealthy cases, it’s only the smallest fraction of the gender experience. Being transgender and exploring your gender identity consist of a broad spectrum of emotions. The fact that some of us (US. WE are a community, and have to treat each other as such) get to snip that little fraction out of the spectrum is beautiful.
We’re made stronger by how different we all are, not weaker.
PART 4: IN CLOSING
Whether you’re dysphoric or not, whether you identify with a gender binary or not, you are worthy of celebration and validation and love. All of us have it rough- frankly speaking, cisgender people as a whole barely tolerate us even when our identities do follow the narrative most commonly accept us. It’s not our place to judge, or shun, or invalidate one another.
And as both a personal goodbye and a TL;DR to truscum who like to treat gender identity like a competition, like something you get to gatekeep and police, fuck you. Our identities are ours to decide, our experiences to forge, and if that happens to not include transitioning or dysphoria, no matter what your reasons are that doesn’t make you less valid.
Fuck you, for painting your bigotry as an opinion. Fuck you for hurting the feelings of other transgender people. And fuck you for making posts trying to paint yourself as anything other than an asshole so full of internalized transphobia and misery that you can’t look past it to respect other people and act like that’s only your opinion UWU
Anyway, trans rights.
#ooc#jesus this is so long#nobody's gonna read this#But I'm PISSED#trans rights#I hate terfs#And transmeds/truscums#All those motherfuckers#fuck that
38 notes
·
View notes
Text
Postpartum Anxiety: Symptoms, Causes, Treatment
New Post has been published on https://depression-md.com/postpartum-anxiety-symptoms-causes-treatment/
Postpartum Anxiety: Symptoms, Causes, Treatment

Postpartum anxiety is anxiety that occurs after giving birth. It is normal to be stressed and have anxious feelings after having a baby. After all, your life has undergone a huge change in taking on the responsibility of caring for your baby, often on little to no sleep.
While some amount of anxiety is completely normal during this period, postpartum anxiety refers to overwhelming anxiety and uncontrollable worry that inhibits your daily functioning. With postpartum anxiety, you may experience intrusive thoughts and physical symptoms, and find it difficult to take care of your baby and yourself.
Atipati Netiniyom / EyeEm / Getty Images
It is unclear exactly how many people experience postpartum anxiety—estimates of this condition range from 4.4% to 18%. One systematic review of 58 studies on postpartum anxiety found a prevalence rate of 8.5%.
Seeking diagnosis and treatment for postpartum anxiety will not only help you feel better, but it can support your baby’s development and keep you involved in your daily life, relationships, and the activities that are meaningful to you.
Postpartum Anxiety vs. Postpartum Depression
Unfortunately, postpartum anxiety is not as well-studied or publicized as its counterpart, postpartum depression, even though some research indicates that postpartum anxiety is actually more common than postpartum depression.
One study found that about 35% of people who experience postpartum anxiety will also have postpartum depression.
Definition of Postpartum Anxiety
There are no official diagnostic criteria for postpartum anxiety, but one definition is that it’s an anxiety disorder that occurs in the time period from immediately post-birth up to a year post-birth.
Most commonly, postpartum depression presents as generalized anxiety disorder (GAD), but other anxiety disorders such as obsessive-compulsive disorder (OCD) can also occur in the postpartum period.
Symptoms of Postpartum Anxiety
Symptoms of postpartum anxiety can include:
Intrusive or persistent thoughts
Excessive worry
Insomnia
Avoidant behaviors
Tension
Dry mouth
Nausea
Irregular heartbeat
Fatigue
Shakiness or trembling
Panic attacks
How these symptoms manifest will look different from person to person. You may find yourself constantly worrying that your baby is breathing and find it difficult to concentrate or focus on anything else as this worry consumes you.
You may avoid breastfeeding due to worry and anxiety about latching. Or you may be overwhelmed with physical symptoms like nausea or even chest pain.
If these symptoms are disproportionate to the situation and prevent you from functioning within your normal relationships, roles, and activities, it is important to have a conversation with your doctor.
If you are having suicidal thoughts, hallucinations, or are a risk to yourself, your baby, or others, there is help available. Contact the National Suicide Prevention Lifeline at 1-800-273-8255 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
For more mental health resources, see our National Helpline Database.
Diagnosis
Diagnosis of postpartum anxiety can be challenging or missed for multiple reasons. First, many anxiety symptoms may be considered “normal” in the postpartum period.
These symptoms include fatigue, irritability, insomnia, tension, and difficulty concentrating. As such, it may be difficult for physicians to identify a clinical anxiety disorder in the postpartum period.
Second, unlike postpartum depression, there is no official postpartum anxiety definition within the “Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition” (DSM-5), which is the handbook of the American Psychiatric Association used by healthcare professionals to diagnose mental health conditions.
Currently, the DSM-5 specifier (a diagnosis extension used to clarify a disorder) “with peripartum onset” can only be used for mood disorders, such as depression, and not for anxiety disorders.
The lack of criteria in the DSM-5 makes it difficult to categorize postpartum anxiety as generalized anxiety disorder (GAD), especially since a GAD diagnosis requires a history of six months of symptoms.
A person who develops anxiety in the postpartum period may not have this history. Therefore, some researchers encourage clinicians to diagnose postpartum anxiety if the criteria for GAD have been met over a one-month period instead.
Third, there has been an under-recognition of anxiety disorders within the peripartum and postpartum populations. This means that anxiety, specifically among people who are pregnant or who have recently given birth, is not well-researched. As a result, there are no anxiety screening tools available that are designed specifically for the postpartum population.
The State Trait Anxiety Inventory (STAI) is a general screening tool for anxiety that has been studied for use in the postpartum population. Research indicates that this tool can accurately diagnose postpartum anxiety with screening at both four and eight weeks postpartum.
A psychological interview, or conversation with your doctor, may also be used to diagnose postpartum anxiety. Your doctor will ask you questions to determine if your anxiety is causing significant distress or is functionally limiting (inhibiting your ability to perform normal activities) and meets the DSM-5 criteria for an anxiety disorder.
Causes
Like all anxiety disorders, there is not a clear cause and effect for postpartum anxiety. Additionally, there is a lack of research on the causes of postpartum anxiety.
Neurobiological research has found both similarities and differences in brain activity between postpartum anxiety and anxiety in the general population. This may indicate that there is a different set of causes for postpartum anxiety.
In some cases, the natural stressors of the perinatal period may contribute to developing postpartum anxiety. Normal worries and fears around the baby’s well-being, the mother’s well-being, the partner’s well-being, and more all have the potential to grow out of control.
When these worries become persistent and lead to functional impairment (the inability to carry out certain activities in your daily life), postpartum anxiety may be diagnosed.
Unlike anxiety among the general population, pregnancy-related hormonal changes may also contribute to postpartum anxiety. One theory is that postpartum estrogen withdrawal may lead to anxiety.
During pregnancy, estrogen levels increase significantly and then rapidly drop to below prepregnancy levels after childbirth and throughout the postpartum period.
This theory was supported by a 2016 study using mice and a 2020 study using hamsters. However, human studies still need to be performed to draw decisive conclusions.
Treatment
Despite postpartum anxiety’s potentially having different causes than anxiety in the general population, it typically is treated in the same way. However, in choosing a treatment plan that is right for you, your doctor should take into consideration your postpartum status, including whether you are breastfeeding.
Psychotherapy
Cognitive behavioral therapy (CBT) is the first-line treatment for mild and moderate postpartum anxiety. Mindfulness training and relaxation techniques also are effective treatments for lowering anxiety levels and symptoms in the postpartum population.
Medication
Medication typically is a second-line treatment for postpartum anxiety and is used in moderate to severe cases. This is due to the possibility of some drugs being transferred via breast milk to the baby.
Your physician will consider this when prescribing your medication and will usually start with the lowest possible dose before titrating up (raising the dosage gradually).
Medications used to treat postpartum anxiety include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), buspirone, benzodiazepines, or tricyclic antidepressants. Of these, SSRIs are the most studied and frequently used during the peripartum and postpartum periods.
Risk Factors
There are various factors that may make a person more likely to develop postpartum anxiety. Risk factors include:
High perceived stress
Low partner social support
History of pregnancy loss
History of multiple births
Diagnosis of other anxiety or mood disorders
Family history of anxiety disorders
Early breastfeeding cessation
One 2016 study found that people at highest risk of developing postpartum anxiety are those who are multiparous (have previously given birth) and have an existing psychiatric history and high levels of stress from diverse sources.
Having multiple risk factors increases your chances of having postpartum anxiety, and this can include taking care of multiple children, including your newborn, during the postpartum period. Notably, a different study found that childcare stress, maternal self-esteem, and depression did not play a significant role in postpartum anxiety.
Coping
Take comfort in knowing there are good reasons for experiencing feelings of postpartum anxiety. First, realize that caring for a new baby is hard, and there is nothing you did to cause your postpartum anxiety.
Here are some ways you can cope with your postpartum anxiety:
Talk to your partner, friends, and family about your worries and need for support.
Balance caregiving duties equally with your partner or a loved one.
Recruit family members or babysitters to help.
Join a support group of new parents, many of which can be found online.
Try to maintain a balanced diet, which is possible through batch cooking, meal delivery services, and more.
Engage in mindfulness and relaxation practices, such as clinical aromatherapy or yoga.
A Word From Verywell
Coping with caring for a new baby and all the life changes your baby brings can be worrisome. For some people, these worries may manifest in postpartum anxiety. If you are struggling with excessive fears, intrusive thoughts, insomnia, and physical symptoms such as muscle tension, dry mouth, nausea, and more, then you may have postpartum anxiety.
While it is normal to feel anxious after childbirth, it is not normal for these worries to take over your life. Talk to your doctor about postpartum anxiety and the treatments that are available to you.
Source link
0 notes
Text
Learn about service of Chemical Dependence
Identifying a medication dependency (" material use disorder") needs a thorough examination and also frequently includes an evaluation by a psychiatrist, psycho therapist or qualified alcohol as well as medication professional. Laboratory tests, such as blood or pee examinations, are utilized to evaluate substance abuse, but they can not detect dependency. Nevertheless, Chemical Dependency Treatment Near Me can be utilized to manage it.
Diagnosis
You certainly wish to know about What Is Nicotinamide Adenine Dinucleotide. For the medical diagnosis of a compound use disorder, many psychological wellness experts use the requirements of the Diagnostic as well as Statistical Handbook of Mental Illness DSM-5
Treatment
Although there is no remedy for drug dependency, the Chemical dependency treatment options described below can aid you get over a dependency and also keep you far from drugs. The therapy you receive will rely on the medications you take and the associated psychological or medical disorders you might have. Lasting follow-up is essential to prevent relapse.
Chemical dependency treatment programs
Therapy programs generally provide the following:
Household, group or individual treatment sessions
Concentrate on comprehending the nature of addiction, quit utilizing drugs and protect against relapse
Degrees of care as well as locations that differ according to your requirements, such as outpatient, domestic as well as inpatient programs
Detoxing
The objective of detoxing, additionally called "removal of contaminants" or "withdrawal therapy," is to permit you to stop using the addictive drug as rapidly and also safely as feasible. For some people, it may be safe to undergo Post Traumatic Stress Disorder Treatment. Others may need admission to a hospital or domestic treatment facility.
Abstinence from various categories of medicines, such as antidepressants, stimulants or opioids, produces different side effects and also requires different techniques. Detoxification may be composed in the gradual decrease of the dose of the drug or short-lived replacement by other materials, such as methadone, buprenorphine or a combination of buprenorphine and naloxone.
Opioid overdose
When a case of opioid overdose happens, the emergency group or, in some states, any person who witnesses an overdose can administer naloxone (an opioid villain). Naloxone turns around the results of opioids temporarily.
While naloxone has actually been on the market for many years, administration systems such as Narcan (a naloxone nasal spray) as well as Evzio (a naloxone injection gadget) are currently available, although they can be really costly.
Evzio is a little shot device that overviews the customer through voice instructions and immediately presents the needle into the thigh to use the naloxone shot. Regardless of the technique of administration, look for instant clinical attention after making use of naloxone.
Behavior modification
As part of a treatment program for medicine addiction, you can conduct behavioral therapy - a kind of psychiatric therapy - with a psycho therapist or psychoanalyst, or obtain mental counseling from an accredited alcohol and also medication therapist. Treatment and also psychological therapy can be private, group or family. The specialist or counselor can:
Assist you to get ways to face your compulsion to medications
Suggest methods to avoid medications and also avoid relapse
Offer pointers on just how to treat a regression, if it occurs
Speak about problems connected to your job, your legal issues and also your connections with family and friends
Include relative to aid them acquire better interaction skills as well as give assistance
Address other mental health problems
#Chemical Dependency Treatment Near Me#Chemical dependency treatment#Post Traumatic Stress Disorder Treatment
0 notes
Text
What Is PMDD – Symptoms and Treatments for Premenstrual Dysphoric Disorder
The (incredibly sexist) joke about premenstrual syndrome (colloquially PMS) is that it drives people to do mean, crazy things. But if you've ever had PMS yourself, you understand.
youtube
There are few things more disorienting than watching your body inflate every month with water retention, or having agonizing headaches for a week just because your period is coming. So yeah, maybe it makes you a little mean. But wouldn't anyone who feels like shit half of every month be mean, too? (Yes.)
A small percentage of people who menstruate feel this even more, and have something called premenstrual dysphoric disorder (PMDD), which is essentially an extreme version of PMS that comes with symptoms similar to clinical depression. Like PMS, PMDD is tied to the menstrual cycle. But unlike PMS, PMDD is severe enough that it has a negative effect on your school/work life, your personal life, and your general ability to function in the two weeks before your period starts.
Two specialists, Dr. Shari Lusskin, a clinical professor of psychiatry, obstetrics, gynecology and reproductive science at Mount Sinai's Icahn School of Medicine, and Dr. Alexandra Sacks, a reproductive psychiatrist in New York City, explained what makes PMDD so bad, and what a doctor looks for when diagnosing it.
What causes PMDD
Like most disorders related to women's health, doctors aren't yet totally sure what causes PMDD, though Sacks said it's certainly something researchers are interested in. The leading theory is that it's rooted in a sensitivity to the natural hormone fluctuations that occur during the menstrual cycle.
"In women who have PMDD, the hormone changes in their menstrual cycle may impact their serotonin levels, which is a chemical in the brain that your brain cells use to regulate all sorts of physical, emotional and behavioral experiences but includes mood, attention, sleep [and] pain," Sacks said.
Per the theory, your hormones and brain are connected by a system called the hypothalamic-pitutiary-gonadal axis, and through this system, hormonal fluctuations produced by the ovaries (part of a normal menstrual cycle) impact the hypothalamus and pituitary areas of the brain, which impacts mood. Sacks clarified that women with PMDD don't necessarily have high or low levels of hormones or any physical problems with their ovaries — it's more a matter of how sensitive your body is to the levels of hormones present.
PMDD vs. regular PMS
According to a 2018 study in Clinical Obstetrics and Gynecology, about three to eight percent of menstruating women meet the diagnostic criteria for PMDD. It was added to the DSM-5, a handbook used by medical professionals to diagnose mental health disorders, in 2013. "This gave it much greater legitimacy for the millions of women who were suffering worldwide," Sacks said. "And it just speaks to the importance of how much more research is needed in the field of women's mental health."
Lusskin said "up to 80 percent of women have premenstrual syndrome" and experience mood and body changes (like bloating and breast tenderness). "But they don't meet the criteria for PMDD, which is defined as having at least thirty percent worsening — you have to have a significant decrease in mood with a substantial impact on functioning."
The symptoms for PMDD are similar to those of PMS, but more severe. Sacks said to officially diagnose someone with PMDD, a doctor will look for five or more combined emotional, physical, and behavior symptoms. These are things like mood swings, anxiety, a feeling of hopelessness, trouble concentrating, change in appetite, trouble sleeping or oversleeping, breast tenderness or swelling, bloating, et cetera. And they should be severe enough that they impact your day-to-day function when you're experiencing them.
PMDD vs. clinical depression
If the symptoms of PMDD look familiar it's because they are. Part of what makes PMDD tricky to diagnose is that it so closely resembles other mental disorders, particularly clinical depression and anxiety. Lusskin said the key difference between PMDD and general mood disorders is that PMDD is linked to the menstrual cycle and symptoms don't persist all month long. For a PMDD diagnosis as opposed to clinical depression, doctors look for symptoms that start around the time of ovulation (about two weeks after the first day of your period) and subside shortly after your next period starts, according to Lusskin.
To identify a pattern, Lusskin said your doctor will ask you track your symptoms in real time instead of retrospectively, when it's easy to point at any symptoms you were having and blame them for the period that you know showed up three days later. What the doctor is looking to rule out is symptoms that last all month long but get worse around the time of your period, which would technically be something more like depression or panic disorder than PMDD.
Sacks said the doctor will look for symptoms that accompanied every menstrual cycle for the past year, but may only ask you track symptoms for two months in a row before making a diagnosis and starting treatment. They'll also ask about medical history (to rule out other mood disorders) and ask about any recent changes in birth control.
"You really want to see this as a pattern in your life not impacted by anything else — not other conditions or medications," Sacks said. If it seems that your symptoms only started showing up or got worse around the time you switched birth control medication, your doctor will offer the option of switching to a different contraceptive before diagnosing with PMDD.
Is it Normal to Feel Sad After Sex?
Treating PMDD
Even though the symptoms are similar, differentiating between PMDD and depression or PMS is important because the treatment options are subjective to each condition. Like depression, PMDD is also often treated with an SSRI. But unlike depression, a doctor might suggest you only take an SSRI during the two weeks of the month that your symptoms appear for PMDD, while someone with depression takes an SSRI continuously.
There's also a difference in how quickly the SSRI kicks into action. "SSRIs have a quick onset of action for PMDD, within one to two days," Lusskin said. "Whereas it takes up to six or eight weeks to get a response for depression." The research on this is still being conducted, but medical professionals believe this quick action has something to do with the fact that SSRIs can impact how progesterone and estrogen impact mood. Researchers believe PMDD is a hormonal sensitivity, so this would make sense.
It may also help to level out hormonal fluctuations. Another common treatment option is to prescribe the birth control pill Yaz, which has been shown in clinical studies to reduce symptoms of PMDD because, unlike most other contraceptives, it contains drospirenone (a synthetic version of the hormone progesterone). Yaz also targets another hormone that works as a diuretic and therefore helps to reduce some of the physical symptoms of PMDD, like water retention that causes bloating.
Sacks added that your doctor may also suggest talk therapy and lifestyle approaches, like increasing exercise, decreasing alcohol and drug use, decreasing caffeine and sugar intake, and just generally eating and acting healthfully (which feels incredibly counterintuitive when you're depressed, but c'est la vie).
The important thing to not about treatment for PMDD is that it's highly individualized. While there isn't a cure, per say, treatment can help some women feel much more "normal" leading up to their period, so to speak. Which is just to say that, if you think you're experiencing PMDD, you should absolutely bring it up with your doctor. Whether it's PMDD or something else (like depression or another mood disorder) there's almost certainly something that can be done to help you feel less "meh."
And if you ever experience severe thoughts of hopelessness or feel suicidal, whether it's in the two weeks before your period or at any time during the month, don't wait to set an appointment with your doctor. You can call 9-1-1 or the National Suicide Prevention Lifeline 24/7 at 1 (800) 273-8255. You can also text the Crisis Text Line anytime at 741741.
Source
http://cosmopolitan.com/sex-love/a18735059/pmdd-symptoms-treatment-facts/
0 notes
Text
Wait, what? (Vol. I)
One of the most confusing parts of parenthood is that we have to navigate several professional worlds outside our own to gain access to what our children may need: educational, medical, health, legal... it’s enough to make you go home and crack open a Bota Box.
Here’s a handy primer of jargon and acronyms (we special ed teachers especially LOVE jargon, and I apologize on my people’s behalf). Bookmark this one and remember that language should NEVER be a barrier in your involvement in decision making for your child. An additional rule of thumb: please never be afraid to ask what something means. You don’t look dumb and you aren’t bothering anyone; you sound mature and curious. Promise.

THE WELL INFORMED MAMA’S GLOSSARY, VOL. I (504 – A)
504 Plan: Section 504 is a federal law that prohibits discrimination and provides for accommodations for any documented disability which affects a life function. Sometimes this is a very good idea, indeed; sometimes, it’s a consolation prize when a Team decides against an IEP. It does not have the “specialized instruction required” piece of an IEP. As in: “Johnny’s 504 gives him extended time on assessments because of his processing speed.”
AAC: Augmentative and Alternative Communication – This includes any alternative means to oral communication, namely speech devices (aligning visuals to “speak” from a computer, often handheld) and PECS (picture communication – more to follow on that one for sure). We see this most often in autism and in apraxia. This is a huge topic but please remember that taking away someone’s “talker” (speech device) is the same as covering a speaking person’s mouth with tape. Not OK. As in: “My son used his AAC device to request he stay home from school and watch Octonauts.”
ABA: Applied Behavior Analysis - An evidence based, systematic, frequent therapy that individuals with autism (or anyone who wants to modify behavior or increase communication) may access. The “client” is exposed to programs that build tolerance, add desirable behaviors, or decrease unsafe or nonfunctional behaviors, for example. It’s the only recognized “treatment” for autism and is mandated by law to be covered by insurance (thanks, Autism Speaks). As in: “Sorry I can’t make it to playgroup, we have ABA today. And tomorrow. And the next day.”
ABS: Adaptive Behavior Scale - aka “The Vineland” - This is the assessment your Early Intervention specialist busts out to rank and file your baby; a necessary evil I suppose. They use observation, interaction using specifically mapped out questions/tasks, and talking to mom and dad to score your little one in four “domains” (skill areas): Communication, Daily Living Skills, Socialization, and Motor Skills. As in: “Bobby didn’t qualify for EI this year because her scores on the ABS were typical.”
Accommodations: A change in the way something is presented (presentation, time or setting, response) that does not change the intention of what is being taught. In other words, it changes how we teach, not what we teach. Good accommodations level the playing field and are NOT an advantage. Some are universal (or should be) and some need to be in an IEP or 504 plan. As in: “If these gen ed teachers don’t give Sally her accommodations on her quiz again, I’m going to lose my shit.”
Advocate: 1. One who does her homework in order to be the voice of someone she loves. 2. Someone we pay when we are too exhausted or enraged to carry on effectively. As in: “That girl advocates like a mother.”
ADHD: Attention Deficit Hyperactivity Disorder – this used to be either ADD or ADHD; now it’s all officially ADHD and then you get a “type” as a bonus prize – hyperactive, inattentive, or combined. In Massachusetts, for example, ADHD is actually listed under health impairment on the IEP as a disability category, and you really want a pediatrician or psychologist to deliver this diagnosis even with school-based testing (more on that later). Kids with ADHD are among my favorite humans: buzzy, busy, dreamy, kinetic, original. They need help. That’s fine, but you’ll often find they’re brilliant, too. As in: “That kid with ADHD in Sally’s class sits on a yoga ball instead of a chair.”
APE: Adapted Physical Education – Adapted or modified PE/gym, including the use of assistive equipment or a different curriculum, so that a student with a gross motor disability or a developmental delay can take PE. There are different levels of qualifications to teach APE and how it all works varies from state to state. I’m learning more about this myself right now. As in: “We may need to put APE in his IEP.”
Apraxia: Apraxia of Speech – This is a disorder in which the brain sends incomplete signals to the mechanical parts of the body that “do the talking.” Apraxia has no bearing on cognitive capacity (intelligence) so always assume competence when interacting with a person with apraxia. Some will move on from apraxia with intensive speech therapy; some will not. Many will end up seeking AAC. As in: “A child with apraxia still has something to say.”
Articulation: aka “artic” – The understandability or clarity of speech. Completely separate from receptive language. May include consonant confusion, dropped syllables, lisps, or mumbling. Many kids with speech delays who learn to speak later than is typical, and kids with frequent ear infections, have artic issues. As in: “Henry’s articulation is a mess, but his vocab is on point.”
ASD: Autism Spectrum Disorder(s) - This the formal name for an autism diagnosis in the official medical handbook DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), which saw big changes in 2013. (For the record, I take issue with “disorder,” but I’ll get into that later.) It covers a wide range of presentations of autism, a developmental and neurological difference, that used to be differentiated into categories like PDD-NOS (Pervasive Developmental Delay - Not Otherwise Specified in very young children) and Asperger’s (now classified as “high functioning autism” - also problematic, but that’s that). Side note – autistic is not a dirty word or dehumanizing descriptor, and one instance where people-first language is not a must. As in: “My ASD/autistic kiddo ate a vegetable this one time.” Now, importantly, in education, autism does not apply as a disability category if a child’s educational performance is adversely affected primarily because the child has an emotional disturbance, but a mental illness can be co-morbid with autism. (Confused? That’s OK. I got you. Stay tuned.)
ASL: American Sign Language - its own language and culture for a subset of deaf Americans; the signs are also used by some in the nonverbal community to communicate, and sometimes simplified for little ones. Signing in infancy and toddlerhood can help prompt language later on. As in: “Noah signs ‘more’ when we tickle him because he is an adorable baby-god.”
Asperger’s Syndrome: The name for a specific type of autism that medical professionals now call “high functioning autism.” This one is chock full of problematic assumptions about really cool, deeply neurodiverse and aware individuals. Many are verbal, but not all, and many feel challenged by social nuances or other communication demands. It may also encompass sensory sensitivities or executive functioning deficits. Or not. Many proudly call themselves “Aspies” and were diagnosed prior to the 2013 DSM-5 update. As in: “Will Big Bang Theory ever tell us outright if Sheldon has Asperger’s?”
AT: Assistive Technology - Any tool, electronic device or hardware, or any software, that helps a student access learning by removing barriers to access. Assistive tech includes communication devices, speech to text and text to speech programs, word prediction software, simply using a Chromebook to type, using an iPad or other tablet to submit work, audiobooks from Learning Ally, and much more. The possibilities are exciting, and can be a little tricky, too. You can request an AT evaluation from a public school just like any other assessment (tip: say eval and not consult). As in: “Hank’s plan has assistive tech. He needs to turn in his worksheets digitally or no one can read his handwriting.”
Auditory Processing Disorder: FYI, nobody really says “APD,” they say “auditory processing.” May also be called “Central Auditory Processing Disorder,” and then we do frequently use CAPD as an acronym. Anyhoo, this is a hearing issue that affects the way kids experience the world and learn, because it makes processing auditory information very challenging. They can hear, but have trouble telling the difference between sounds. Requires speech therapy and sometimes seeing an audiologist for medical intervention. Can frequently be mislabeled as ADHD. As in: “Billy’s not being fresh; he’s not following the conversation because he has auditory processing disorder.”
To be continued…
0 notes
Text
What every parent needs to know about 'gaming disorder'
yahoo
Video game addiction is a term that has been used for years by parents and mental health professionals who believe that it’s a real disorder. Now, there’s more weight behind their argument: The World Health Organization (WHO) has including “gaming disorder” as a new mental health condition listed in the 11th edition of its International Classification of Diseases.

Your child may love video games. But how do you know if he or she is addicted? Photo: Getty Images.
According to WHO, there are three major criteria for the diagnosis of gaming disorder: Gaming takes precedence over other activities so much that a person often stops doing other things, a person continues gaming even when it causes issues in their life or they feel that they can’t stop, and gaming causes significant distress and impairments in a person’s relationships with others, as well as their work or school life. If your child gets sucked into a game for a few days, but goes back to normal after that, they wouldn’t qualify: Instead, people must engage in this behavior for at least 12 months, WHO says.
It’s worth noting that WHO’s stance on gaming addiction is different from that of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the handbook used by health professionals in the U.S. and other countries to help diagnose mental health disorders. The DSM-5 calls out “Internet Gaming Disorder” but says it’s a condition that warrants more clinical research and experience before it can be classified in the book as a formal disorder.
WHO says on its website that all people who participate in gaming should be aware that gaming disorder is a real condition, and that it’s important to be mindful of how often they play video games. However, they also point out that gaming disorder only affects a small amount of people who game.
It’s only natural that the news would make you give your child’s gaming system the side-eye.
In general, parents should limit the amount of screen time their children have daily, and gaming is included in that, along with TV, computers, phones, and tablet use, Gina Posner, MD, a pediatrician at MemorialCare Orange Coast Medical Center in Fountain Valley, Calif., tells Yahoo Lifestyle.
Screen time isn’t recommended at all for kids who are 18 months or younger, but for children who are older than that up to five, it’s generally recommended that they have not more than one hour of screen time, she says. For those who are six and up, it’s more at the parents’ discretion. “The maximum amount of screen time should be two hours a day, but less is always better,” Posner says.
Posner says that it’s important to set clear limits for your child when it comes to screen time and gaming. For example, say that your child has to do their homework first and/or get out and play for an hour before they’re allowed to game. And even then, make it clear that they’re only allowed to do so for a set period of time.
If your child starts fussing when they’re not allowed to be gaming all day, it’s a clear sign that you need to cut back, Posner says.
Treatment for gaming disorder is generally based in cognitive behavioral therapy, which would generally be done in two phases, Simon Rego, PsyD, chief psychologist at Montefiore Medical Center/Albert Einstein College of Medicine, tells Yahoo Lifestyle. The first is raising awareness for your child that their gaming is a problem, and looking for triggers and cues that could make the gaming habit better or worse. A mental health professional would also address problematic thoughts associated with either stopping playing or the thoughts that keep them gaming, he says.
The goal then is to step down the behavior from something that’s pathological to problematic, and then being able to manage it in a “reasonable way,” Rego says. People don’t necessarily have to quit gaming altogether, but they do need to learn to better manage it with parameters, like only gaming with friends during select times during the day vs. doing it at night alone in their room.
If you suspect that your child has a gaming disorder, it’s important to seek help for it.
Just know that this is still a new diagnosis and you may need to do some sleuthing to find someone who specializes in this kind of behavior.
Read more from Yahoo Lifestyle:
Here’s what happens during a home birth, like the one of James Van Der Beek’s wife
Little boy grows hair long just so he can donate it, regardless of gender stereotypes
Shop 16 floral summer wedding dresses just like Meghan Markle’s
Follow us on Instagram, Facebook, and Twitter for nonstop inspiration delivered fresh to your feed, every day.
#news#_revsp:wp.yahoo.style.us#psychology#mental health#gaming disorder#_author:Korin Miller#health#_uuid:e033c674-445c-381a-b8be-c95a2233aa81#_lmsid:a0Vd000000AE7lXEAT#WHO#DSM#video games
0 notes
Text
Clinical Formulations of Narcissistic PD
Clinical formulations and case conceptualisations are introduced in this post.
These are all generalisations and theories of how NPD develops, not something that is supposed to be true for everyone with NPD.
Psychodynamic model
Freud suggests parents either overvaluing or neglecting (or both) a child can lead to NPD & especially inability to form healthy, lasting relationships and regulate self-esteem
"In other words, [NPD] is the outcome of insufficient gratification of the normal narcissistic needs of infancy and childhood."
Kohut theorises that narcissists' ability to form a cohesive sense of self and others was developmentally arrested in childhood, resulting in grandiosity & idealising others
"Narcissistic injury" = fragmentation of the self
Kernberg suggests grandiosity & exploitation result from maternal emotional abuse
Grandiosity is an "emotional escape valve"
Grandiosity & entitlement mask the "real self" that is "split off"
The real self unconsciously holds rage, fear, envy, deprivation
Defensive structure is same as BPD but difference is grandiosity
Biosocial model
NPD is primarily the result of environment, especially "parental indulgence and overvaluation, learned exploitive behavior, and only-child status"
Special treatment from caregivers leads children to believe that the "world revolves around them", and therefore they expect the same outside the home
When special treatment outside the home doesn't happen, they "experiment with demanding and exploitive tactics and subsequently develop considerable skill in manipulating others"
"At the same time they come to believe that most others are inferior, weak, and exploitable."
NPD is self-perpetuating through sense of superiority, lack of self control, sense of entitlement, and dismissing of those who reject their world / self-view
Cognitive-Behavioural model
Key feature of NPD is self-aggrandisement
Core beliefs:
> Deserving of special treatment
> Not bound by social norms and rules
Conditional beliefs:
> Others should be punished for not recognising their specialness
> To maintain that special status others should be subservient to them
Instrumental belief:
> Always strive to demonstrate their superiority
> See themselves as special, superior, entitled to special favors and treatment, and vulnerable to loss of status
> View others as inferior but potential admirers
Main pattern of behaviour is "seeking prestige, power, position, and wealth as a way of reinforcing their image of superiority", using "manipulation and guile" if necessary
The primary schema is superior & special (/ entitlement & grandiosity)
> Superior schema "shaped by flattery, indulgence, and favoritism"
> Special schema shaped by "rejection, limitations, exclusion, or deficits"
> Common denominator is the belief that the individual is different in some way
Three subtypes:
> Self-centered impulsive type
> Ruthless impression-management type
> Acceptance-oriented impression-management type
> Each type is centred around an impulse control deficit developed in childhood
> "Specifically, these individuals learned to seek reinforcers without having to work for them. This resulted in their development as self-indulgent, egocentric, and impulsive individuals."
> Ruthless & Acceptance-oriented types focus on creating favourable impressions with others, but struggle with long-lasting healthy relationships because of their empathy deficits
Interpersonal model
People with NPD were raised in an environment of "selfless not contingent" love, leading to insensitivity to others' needs
The caregiver was over-adoring, but there was also a constant threat of a "fall from grace", with pressure to be the perfect child
The constant overbearing love means that any criticism or disappointment hits very hard
"In short, there is extreme vulnerability to criticism or being ignored, together with a strong wish for love, support, and admiration from others. Noncontingent love and presumptive control of others is expected and even demanded. If support is withdrawn, or lack of perfection is evident, the self-concept degrades into severe self-criticism."
Integrative model
People with NPD are hypersensitive
Seen as exceptional children, leading to pressure to perform
As children likely had highly developed speech and interpersonal skills
Life purpose: "I’m special and unique, and I am entitled to extraordinary rights and privileges whether I have earned them or not."
World-view: "Life is a banquet table to be sampled at will. People owe me admiration and privilege."
Goal: "Therefore, I’ll expect and demand this specialness."
Defense mechanisms: rationalisation and projective identification
Parental injunction: "Grow up and be wonderful—for me."
"The illusion of specialness, disdain for others’ views, and a sense of entitlement lead to an underdeveloped sense of social interest and responsibility. This, in turn, leads to increased self-absorption and confirmation of narcissistic beliefs."
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#len sperry#handbook of diagnosis and treatment of dsm 5 personality disorders#personality disorder concepts#case conceptualisations#clinical formulations#pd info#npd#npd info#dogpost
142 notes
·
View notes
Note
hi! could you go a bit more into detail about how it's rarer for someone to have one PD rather than multiple? I tried searching it up but there were no helpful results. thanks!! :D
most of my info for that comes from @shitborderlinesdo, but unfortunately they don't cite that claim.
Sperry says that the average number of PD diagnosis for a person is 3-4. this chart uses DSM-III-R criteria so it’s pretty outdated, but it shows the likelihood of a particular PD being comorbid with other PDs.
Tasman says that “pure” SZPD & HPD are rare, and if you (general you) have one of those it’s more likely that you also have another PD (or more) (most likely STPD, PPD & AVPD in schizoids & NPD, BPD & DPD for histrionics).
1. Len Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorder (2016)
2. Allen Tasman, Psychiatry (2013)
27 notes
·
View notes
Note
Do you know of any psychology books that may be good to look into for someone who wants to learn more about personality disorders? I am looking for books that specialize in one specific personality disorder, which disorder does not matter to me but I am looking for books that don't demonize them, they're hard to stomach and I have trouble differentiating the biased from facts. (And don't want to spend money on books that do that)
Distancing: Avoidant Personality Disorder by Martin Kantor
The Essential Guide to Overcoming Avoidant Personality Disorder by Martin Kantor
Obsessive-Compulsive Personality Disorder by Grant et al.
Obsessive-Compulsive Personality Disorder: Understanding the Overly Rigid, Controlling Person by Martin Kantor
Schizoid Phenomena, Object Relations and the Self by Harry Guntrip (1969, so pretty old but referenced a lot in schizoid research)
Treatment of Schizoid Personality by Zachary Wheeler
The Divided Self by R.D. Laing (about SZPD)
Split Self and Split Object: Understanding and Treating Borderline, Narcissistic and Schizoid Disorders by Philip Manfield
Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders by Len Sperry
Borderline, Narcissistic, and Schizoid Adaptions: The Pursuit of Love, Admiration, and Safety by Elinor Greenberg
Cognitive Behavior Therapy of DSM-5 Personality Disorders: Assessment, Case Conceptualization, and Treatment by Len & Jon Sperry
Disorders of Personality: Introducing a DSM/ICD Spectrum from Normal to Abnormal by Theodore Millon
Handbook of Personality Disorders: Theory, Research, and Treatment by W. John Livesley & Roseann Larstone
Personality Disorders in Modern Live by Millon et al.
The Empty Core: An Object Relations Approach to Psychotherapy of the Schizoid Personality by Jeffrey Seinfeld
Disorders of the Self by Masterson et al.
The Borderline Personality Disorder Survival Guide: Everything You Need to Know About Living with BPD by Alexander L. Chapman & Kim L. Gratz
The Narcissistic and Borderline Disorders by James F. Masterson
Treating Dissociative and Personality Disorders: A Motivational System Approach to Theory and Treatment by Antonella Ivaldi
I haven't read all of these so I can't vouch for lack of ableism, but these are the books I have saved.
Kantor and Millon are ableist but also very knowledgeable, Wheeler seems good from the bits I've read, Sperry is good and not as [overtly] ableist as other writers, Masterson is seen as the absolute expert (along with Millon) but I haven't read him so I don't know if he's ableist or not, and Greenberg is the only non-ableist writer I've read on PDs (though even she is a bit ableist towards NPD at times).
I'll add all these to my drive (linked in my pinned post) so people can download them! (z-lib is a great site to find books if you're not opposed to 🏴☠️)
24 notes
·
View notes
Text
Personality Disorder Concepts: Defining Characteristics
These are the defining characteristics of PDs, each of which are different depending on the PD in question.
Triggering event(s).
The situations that trigger a maladaptive response that is reflected in the person’s behavioral, interpersonal, cognitive, and affective styles. Triggering events can be intrapersonal (e.g. failing an exam), or interpersonal (e.g. being criticised).
ASPD: Social standards and rules.
AVPD: Close relationships; being social/in public.
BPD: The expectation of meeting goals; maintaining close relationships; real or imagined abandonment.
DPD: The expectation that they can rely on themselves; being alone.
HPD: Relationships, particularly with those they're attracted to.
NPD: Self-evaluation, either by themselves or others.
OCPD: Unstructured situations; meeting other’s standards (in all aspects of life: work, family, etc).
PPD: Close relationships; personal questions.
STPD: Close relationships.
SZPD: Close relationships.
Behavioral style
The way in which the person reacts to a triggering event.
ASPD: Impulsive, irritable, aggressive; irresponsible and struggles to keep commitments; relies on themselves, uses cunning and force; risk-taking and thrill-seeking.
AVPD: Tense and self-conscious; controlled speech & behaviour; appear apprehensive and awkward; self-criticising and overly humble.
BPD: Self-damaging behaviours (self-harm, self-sabotage, suicidal ideation); aggression; achieve less than they could (e.g. in work or school); chronic insomnia & irregular circadian rhythms (”body clocks”); feel helpless & empty void.
DPD: Docile, passive, non-assertive, insecure, and submissive; doubts themselves & lacks self-confidence.
HPD: Charming, dramatic, expressive; demanding, self-indulgent, inconsiderate; attention-seeking, mood swings, impulsive, unpredictable, and superficial.
NPD: Self-centred, egotistical, self-assured; dominates conversations; seeks approval and attention; impatient, arrogant, hypersensitive.
OCPD: Perfectionists; workaholics; dependable, stubborn, possessive; indecisive, prone to procrastination.
PPD: Always tense and hypervigilant; defensive, argumentative, guarded.
STPD: Eccentric, bizarre; strange speech; struggles with work and school and often become drifters and wanderers; avoids long-term commitment and looses touch with society’s expectations; dissociative.
SZPD: Lethargic, inattentive, eccentric; slow and monotone speech; rarely spontaneous; indifferent.
Interpersonal style
The way they relate to others.
ASPD: Deceitful; irritable, antagonistic and aggressive; disregards their and other’s safety; distrustful; lacks empathy; competitive.
AVPD: Sensitive to rejection; want acceptance but are too scared; withdraw and avoid when afraid; test people to see if they’re safe to interact with.
BPD: “Paradoxical instability”; splitting (idealise & cling vs devalue & dismiss); sensitive to rejection; “abandonment depression” & separation anxiety; superficial yet quickly developed and intense relationships; “extraordinarily intolerant” of being alone.
DPD: People-pleasers, self-sacrificing, clingy & needs reassurance; over-compliant & over-reliant on others; want others to be in control of their lives; avoids arguments; puts themselves down so they can receive the support of others; urgently seeks a new relationship when one ends.
HPD: Needs attention; flirtatious, manipulative; lacks empathy; overestimates intimacy of relationships.
NPD: Exploitative; self-indulgent; charming, pleasant & endearing; lacks empathy; irresponsible; jealous; needs approval and admiration.
OCPD: Very aware of social hierarchy; deferential to superiors and haughty to subordinates; polite and loyal; insist that their way is the right way to do things, because they are anxious to ensure perfection; stubborn; devoted to work which interferes with relationships.
PPD: Distrustful, secretive, suspicious, tend to isolate themselves and avoid intimacy; hypersensitive to criticism; bears grudges and blames others; reluctant to open up for fear of vulnerability.
STPD: Loners; socially anxious, apprehensive, suspicious and paranoid, which doesn’t fade as they get to know people; tends to live on the margins of society and relationships; often choose jobs with minimal social interaction that are usually below their skill level; indifferent to social norms.
SZPD: Aloof, loners, reserved, solitary; socially awkward; tend to fade into the background; happy to remain alone.
Cognitive style
How the person perceives and thinks about a problem and its solution.
ASPD: Impulsive; realistic; very aware of social cues; prone to executive dysfunction.
AVPD: Hypervigilant; distracted and preoccupied with their fears of rejection.
BPD: Inflexible (splitting) & impulsive; difficulty learning from the past; external loss of control leads them to blame others to avoid feeling powerless; emotions fluctuate between hope and despair; unstable self-image and fragmented sense of self; unable to tolerate frustration; brief psychotic episodes; dissociation; intense rage; difficulty focusing & processing information.
DPD: Suggestible and persuadable; optimistic, sometimes to the point of naïveté; uncritical; minimises difficulties and are easily taken advantage of.
HPD: Impulsive, dramatic; vague; suggestible; relies on intuition; avoids reflection and introspection as so to avoid realising their dependency on others; needs approval from others; has separate real/inner/private & constructed/outer/public selves; tendency to mimic speech patterns.
NPD: Focuses on feelings rather than facts; compulsive lying (to themselves as well as others); inflexible, impatient, persistent; superiority; unrealistic goals of success, power, ideal love.
OCPD: Rule & detail oriented; difficulty with prioritising; inflexible, unimaginative; conflicted between assertiveness & defiance vs obedience & pleasing people.
PPD: Mistrustful; hypervigilant; focuses on feelings (of paranoia) rather than facts; brief psychotic episodes; their need to find evidence for their paranoid suspicions gives them a tendency for authoritarianism.
STPD: Scattered; obsessive and tends to ruminate; superstitious, bizarre fantasies; vague ideas of reference (thinking things are about them when they’re not, e.g. someone laughing is directed at them) and magical thinking (thinking they caused something to happen by thinking about it); dissociative.
SZPD: Distracted; difficulty organising their thoughts; vague and indecisive; difficulty with introspection and reflection.
Affective style
How the person expresses and experiences emotions.
ASPD: Superficially expresses emotions; avoids emotions that will make them vulnerable; rarely feels guilt, shame or remorse; unable to tolerate boredom, depression, & frustration and needs stimulation.
AVPD: Shy & apprehensive; feels empty, sad, lonely & tense; depersonalisation.
BPD: Mood swings; inappropriately intense anger; feelings of emptiness, boredom, a “void”; emotional dysregulation.
DPD: Insecure & anxious; lacks self-confidence & fears being alone; fears abandonment & rejection; often sad or somber.
HPD: Displays intense, extreme emotions but may only feel them shallowly; sensitive to rejection; mood swings; need reassurance that they are loved.
NPD: Presents as self-confident and nonchalant; when criticised or rejected (”narcissistic injury”) they experience extreme shame which is often redirected into anger (”narc rage”/shame redirect); splitting; lacks empathy and so has difficulty with commitments.
OCPD: Somber, difficulty expressing feelings; avoids emotions that will make them vulnerable; comes across as stiff and stilted.
PPD: Cold, aloof, humourless; difficulty expressing feelings; tendency for anger and jealousy.
STPD: Cold, humourless, aloof; difficult to engage with; suspicious and mistrustful; hypersensitive; may react inappropriately for the situation or not at all.
SZPD: Humourless, cold, aloof; indifferent; lacks empathy; emotionally and socially distant; difficulty responding to other people’s feelings.
Temperament
The response pattern that reflects the person’s energy level, emotions and intensity of emotions, and how quick they react.
ASPD: Irresponsible, aggressive and impulsive.
AVPD: Irritable.
BPD: Passive (dependent subtype); hyperreactive (histrionic subtype); irritable (passive-aggressive subtype).
DPD: Low energy; fearful, sad or withdrawn; melancholic.
HPD: Hyperresponsive; needs attention from others.
NPD: Active and responsive; has special talents and developed language early.
OCPD: Irritable, difficult, anxious.
PPD: Active and hyperresponsive (narcissistic subtype); irritable (obsessive-compulsive and passive-aggressive subtypes).
STPD: Passive (schizoid subtype); fearful (avoidant subtype).
SZPD: Passive, difficulty experiencing pleasure and motivation (anhedonia).
Attachment style
Discussed in this post.
ASPD: Fearful-dismissing.
AVPD: Preoccupied-fearful.
BPD: Disorganised.
DPD: Preoccupied.
HPD: Preoccupied.
NPD: Fearful-dismissing.
OCPD: Preoccupied.
PPD: Fearful.
STPD: Fearful-dismissing.
SZPD: Dismissing.
Parental injunction
The expectation (explicit or implied) from caregivers for how the child should be or act.
ASPD: “The end justifies the means.”
AVPD: “We don’t accept you, and probably nobody else will either.”
BPD: “If you grow up, bad things will happen to me [caregiver].”; overprotective, demanding or inconsistent parenting.
DPD: “You can’t do it by yourself.”
HPD: “I’ll give you attention when you do what I want.”
NPD: “Grow up and be wonderful, for me.”
OCPD: “You must do/be better to be worthwhile.”
PPD: “You’re different. Keep alert. Don’t make mistakes.”
STPD: “You’re a strange bird.”
SZPD: “Who are you, what do you want?”
Self view
The way they view and conceptualise themselves.
ASPD: Cunning & entitled.
AVPD: Inadequate & frightened of rejection.
BPD: Identity problems involving gender, career, loyalties, and values; self-esteem fluctuates with emotions.
DPD: Pleasant but inadequate, fragile.
HPD: Needs to be noticed.
NPD: Special, unique and entitled; relies on others for self-esteem.
OCPD: Responsible for anything that goes wrong, so they must be perfect.
PPD: They're alone and disliked because they're different and better than others.
STPD: Different than other people.
SZPD: Different from others; self-sufficient; indifferent to everything.
World view
The way they view the world, others, and life in general.
ASPD: Life is dangerous and rules get in the way of their needs. They won’t be controlled or degraded.
AVPD: Life is unfair; even though they want to be accepted, people will reject them, so they'll be vigilant & demand reassurance; escapes using fantasies and daydreams.
BPD: Splits between people and the world as either all-good or all-bad, resulting in commitment issues.
DPD: Other people need to take care of them because they are unable to.
HPD: Life makes them nervous, so they need attention and reassurance that they're loved.
NPD: Life is full of opportunities; they expect admiration and respect.
OCPD: Life is unpredictable and expects too much, so they manage this by being in control and being perfectionists.
PPD: Life is unfair, unpredictable, demanding, and dangerous; they need to be suspicious and on guard against others, who are to blame for failures.
STPD: Life is strange and unusual; others have special magic intentions, so they are curious but also cautious when interacting with the world.
SZPD: Life is difficult and dangerous; if they trust no one and keep their distance from others, they won’t get hurt.
Maladaptive schema
Discussed in this post.
ASPD: Mistrust/abuse; entitlement; insufficient self-control; defectiveness; emotional deprivation; abandonment; social isolation.
AVPD: Defectiveness; social isolation; approval-seeking; self-sacrifice.
BPD: Abandonment; defectiveness; abuse/mistrust; emotional deprivation; social isolation; insufficient self-control.
DPD: Defectiveness; self-sacrifice; approval-seeking.
HPD: Approval-seeking; emotional deprivation; defectiveness.
NPD: Entitlement; defectiveness; emotional deprivation; insufficient self-control; unrelenting standards.
OCPD: Unrelenting standards; punitiveness; emotional inhibition.
PPD: Abuse/mistrust; defectiveness.
STPD: Alienation; abandonment; dependence; vulnerability to harm.
SZPD: Social isolation; emotional deprivation; defectiveness; subjugation; undeveloped self.
Optimal diagnostic criterion
One key criterion for each personality disorder, based on its ability to summarise all criteria for that PD, accurate description of behaviour, and the predictive value (ability to predict if the person has the PD or not).
ASPD: Aggressive, impulsive, irresponsible behavior.
AVPD: Avoids activities that involve being social out of fear of criticism, disapproval, or rejection.
BPD: Frantic efforts to avoid real or imagined abandonment.
DPD: Needs other people to be responsible for most major parts of their lives.
HPD: Uncomfortable not being the centre of attention.
NPD: Grandiose sense of self-importance.
OCPD: Perfectionism that interferes with life.
PPD: Paranoia, without evidence, that others are trying to harm, exploit or deceive them.
STPD: Thinking, speech, behavior, or appearance that is odd, eccentric, or peculiar.
SZPD: Doesn’t want or enjoy close relationships.
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#dogpost#pd info#personality disorder concepts#cluster a#cluster b#cluster c#personality disorders#*reads this and is both reassured and hits home that im bpd & stpd*
539 notes
·
View notes
Text
Personality Disorder Concepts: Attachment Styles
Attachment is the “emotional bond” between a child and their caregiver. It’s relevant to personality disorders since it influences the child’s “capacity to form mature intimate relationships in adulthood”. It “influences and organizes motivational, emotional, and memory processes that involve caregivers”. Attachment is associated with “emotional regulation, social relatedness” and the “development of self-reflection and narrative”, all things that are impacted by personality disorders.
Attachment Styles
Attachment styles are made up of two dimensions:
the distinction between self and others
“valence”: positive vs. negative evaluation
Most people will exhibit more than one attachment style.
The five styles are:
secure: positive view of self and others
preoccupied: negative view of self, positive view of others
dismissing: positive view of self, negative view of others
fearful: negative view of self and others
disorganized: fluctuating positive and negative views of self and others
Preoccupied style: DPD, OCPD & HPD
Negative view of self (“a sense of personal unworthiness”)
Positive view of others
Tend to be very “externally oriented in their self-definitions”, i.e. look to others to define them
Dismissing style: SZPD
Positive view of self (“a sense of self that is worthy and positive”)
Negative view of others, which “typically manifests as mistrust”
See themselves as “emotionally self-sufficient”
See others as emotionally unresponsive
Therefore they “dismiss the need for friendship and contact with others”
Fearful style: PPD
Negative view of self and others
Expectation that others are untrustworthy & will reject them
Don’t trust themselves or others
Believe themselves to be “special and different”
Hypervigilant against threats and “unexpected circumstances”
Preoccupied-fearful style: AVPD
Negative view of self
Fluctuates between negative and positive view of others
Want to be liked and accepted but fear rejection and abandonment, so they avoid and withdraw
Fearful-dismissing style: ASPD, NPD, STPD
Fluctuates between negative and positive view of self
Negative view of others
See themselves as “special and entitled”
Acknowledge their need for others, as well as others’ potential to hurt them
Use others to meet their needs but are fearful and dismissing of them
Disorganized style: BPD
Fluctuates between negative and positive view of self and others
This style develops from trauma
Associated with dissociation & PTSD
Seems to shift among the other attachment styles
(More on disorganised attachment & dissociation)
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#pd info#attachment styles#disorganised attachment#its interesting that stpd is included with aspd & npd cuz i dont normally see those together but it makes sense#(esp as im stpd & considering if i have npd &/or aspd traits)#len sperry#dogpost#handbook of diagnosis and treatment of dsm-5 personality disorders#personality disorder concepts
245 notes
·
View notes
Photo
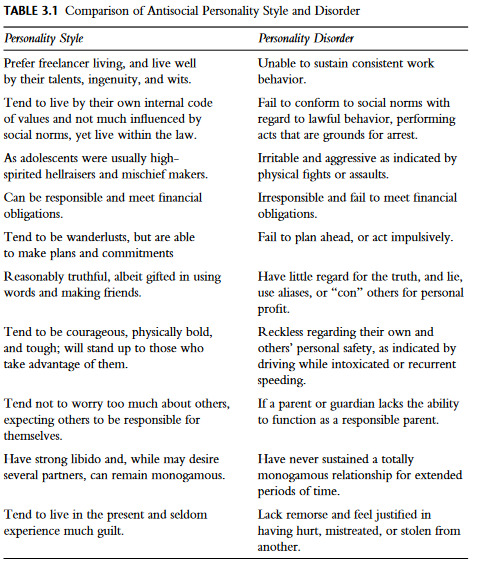
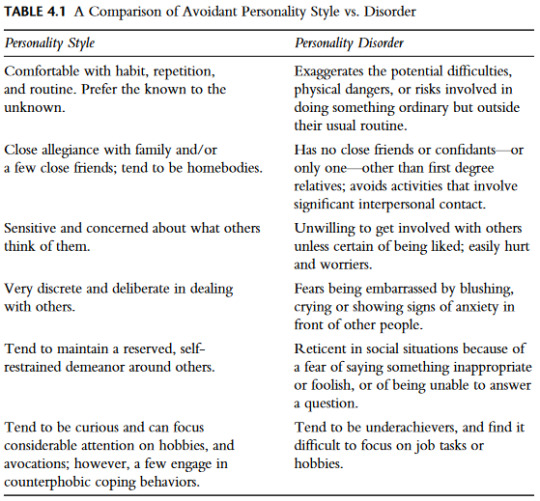
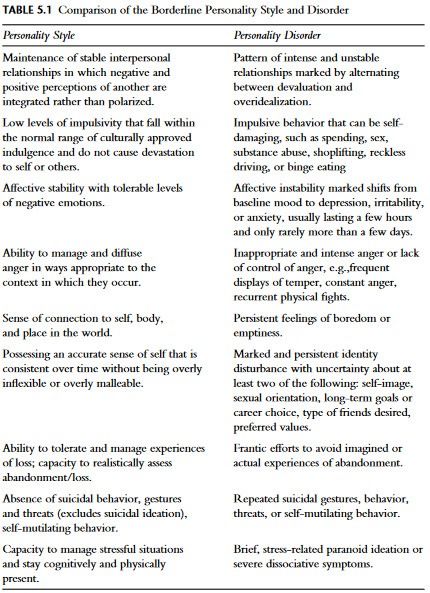
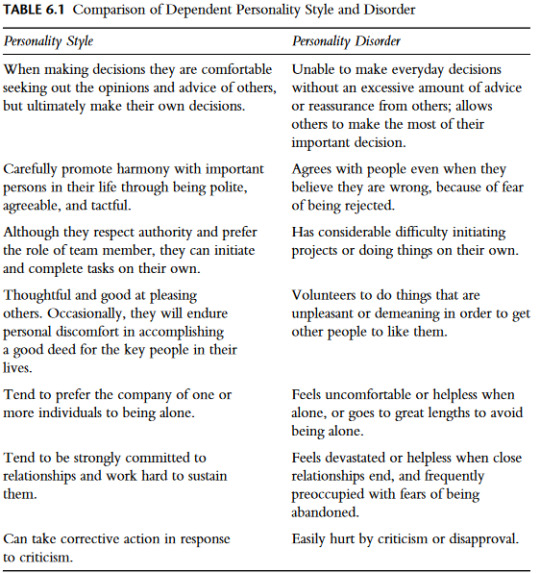
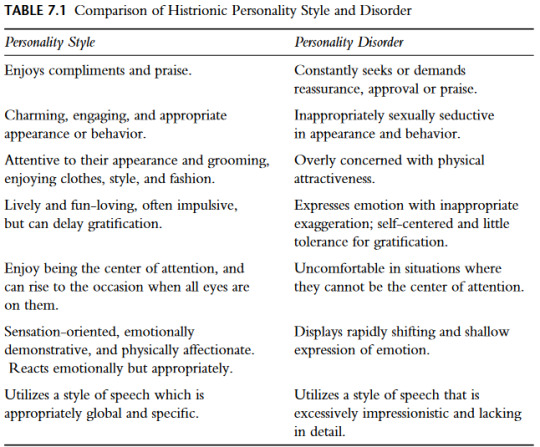
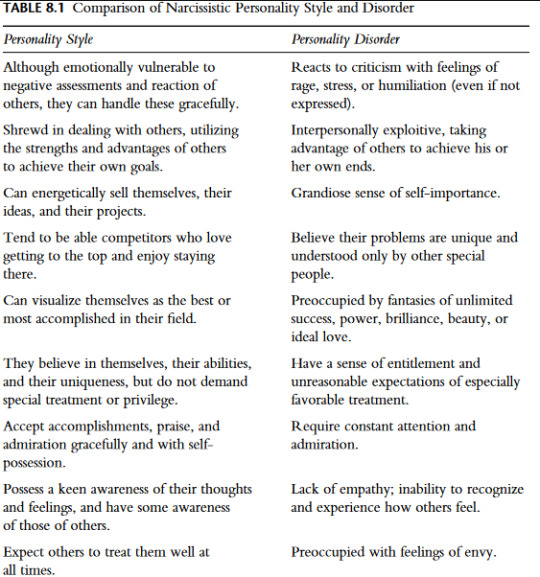
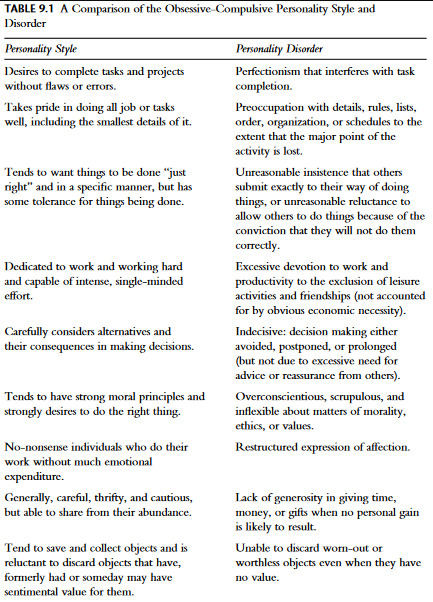
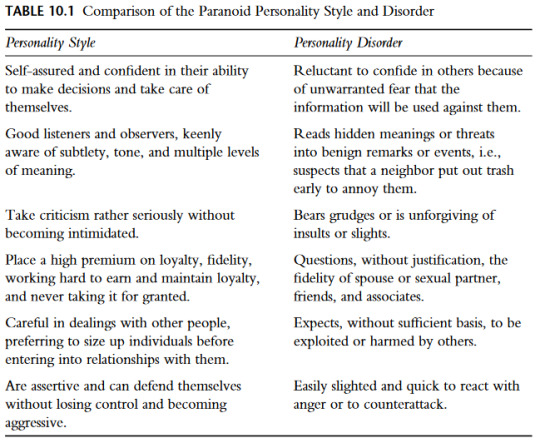
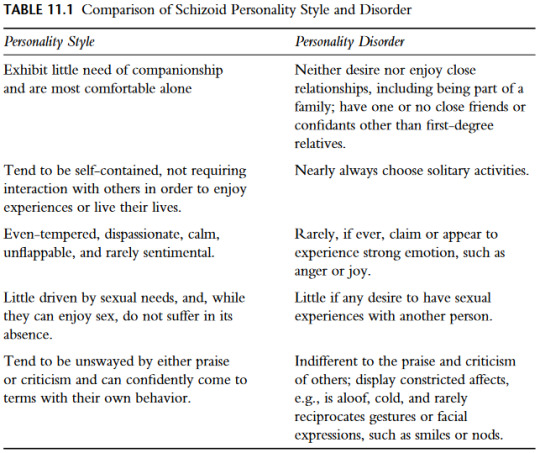
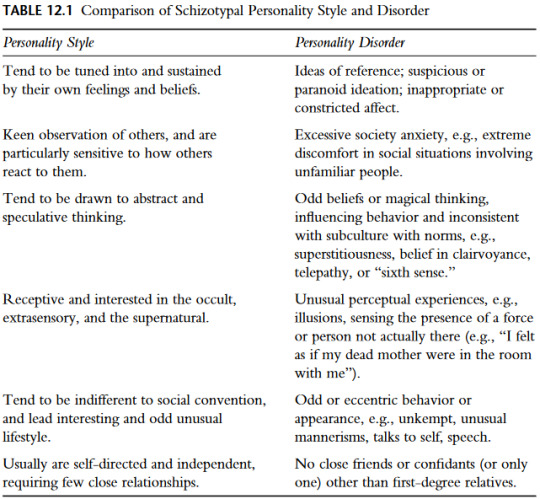
Comparison of Personality Styles vs Personality Disorders
- From Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders by Len Sperry (2016)
#putting them all in one post for ease#dogpost#pd info#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#aspd#aspd info#avpd#avpd info#bpd#bpd info#dpd#dpd info#hpd#hpd info#npd#npd info#ocpd#ocpd info#ppd#ppd info#stpd#stpd info#szpd#szpd info#personality disorders vs styles
177 notes
·
View notes
Text
Clinical formulations of Avoidant PD
Clinical formulations and case conceptualisations are introduced in this post.
These are all generalisations and theories of how AVPD develops, not something that is supposed to be true for everyone with AVPD.
Psychodynamic model
Shyness, shame, withdrawal & avoidance are defense mechanisms against embarrassment, rejection, humiliation and failure
Shame & fear of vulnerability/exposure of the self to others are interconnected
Avoidants feel ashamed about their perceptions of themselves as weak, incapable, defective
Shame a result of childhood experiences, and not living up to their ideal self
Shame is a defense mechanism designed to protect by perceiving others’ neutral or positive actions or words as negative, and by avoiding and withdrawing from social situations where they could be judged
Biosocial model
High sympathetic nervous system (flight & fight) vs low autonomic arousal (fawn & freeze)
Results in hypervigilance (fight) against threats (being judged), shyness, timidity and avoidance (flight)
AVPD results from caregivers and peer groups’ rejection
Caregiver rejection is frequent and/or intense
Peer rejection reinforces the caregiver rejection, and reduces self-worth and self-confidence, creating self-criticism
Results in avoidance, hypersensitivity and excessive introspection
Hypersensitivity means they interpret small criticisms or even positive or neutral statements as rejections, and this lowers their self-esteem even further
Cognitive-Behavioural model
Avoidants fear being rejected so they don��t initiate or accept relationships
The conflict between their need for connection and fear of rejection is unbearable, so they withdraw
They also withdraw cognitively and emotionally from things that would make them feel uneasy or dysphoric
View themselves as incompetent socially and in school & work, as inadequate and different from others
View others as criticising, judgemental and uncaring
View criticism as being based solely on their perceived inadequacies
Use strategies like distraction, rationalisation, and excuses for when they feel sad and anxious
Interpersonal model
Avoidants grew up with relatively normal attachment processes, but their caregivers were very controlling when it comes to social image and reputation
Noticeable flaws were seen as embarrassing and humiliating
They were expected to be seen as perfect, and they were mocked and degraded if they weren’t
Results in hypersensitivity to rejection and judgement
Integrative model
Avoidants were likely irritable and fearful as babies and were likely slow to warm up to caregivers
View themselves as inadequate and fear rejection
View the world as unfair and criticising, but they still want connection
They need reassurance, but stay hypervigilant for judgement, and use fantasies and daydreams as escape methods
Tendency for catastrophic thinking
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#personality disorder concepts#case conceptualisations#clinical formulations#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#pd info#avpd#avpd info#dogpost#*dysphoria here meaning unease; unsatisfied; unhappy etc
122 notes
·
View notes
Text
Personality Disorder Concepts: Prototypic Descriptions
Prototypic descriptions are brief descriptions that "capture the essence of how a particular disorder commonly presents", i.e., a summary of the key features of the disorder. The following are the protoypic descriptions of the DSM-5-TR personality disorders, summarised from Sperry:
ASPD
Antisocials displayed symptoms of Conduct Disorder from early childhood, and their manipulative and irresponsible behaviour continued into adulthood. They lack empathy and use others for their own gain. Because they can’t tolerate boredom, they are reckless, impulsive thrill-seekers and disregard their safety and others'. ASPD is over-diagnosed in prisons and detention centres.
AVPD
Avoidants are frightened and anxious, which makes them socially awkward. They are hypersensitive to criticism and rejection, and the fear of being embarrassed and humiliated causes them to withdraw and avoid social interaction. They crave connection with others, and may have trusted people with whom they can relax and feel safe.
BPD
Borderlines are terrified of being abandoned, which leads to intense relationships that often end in disappointment when they split on their favourite person. They are prone to self-damaging behaviours, and self-harm and suicide attempts are common. They have a fragmented, confused sense of self. They are often impulsive and prone to anger.
DPD
Dependents feel inadequate and fragile and need others to rely on. They struggle with being alone and find it nearly impossible to make their own decisions. They are submissive and are more than willing to put others’ needs and views above their own. They will do whatever it takes to get others to care for them, to give them affection, and give direction to their lives.
HPD
Histrionics are dramatic, charming and intense people. Their emotions are both intense and shallow at the same time. Their interests and attitudes are easily influenced by what others think and value. They need attention and reassurance that they are loved from others, so they often overestimate the intimacy of relationships.
NPD
Narcissists have a grandiose sense of self-importance, specialness and uniqueness that leads them to feel entitled and privileged. They expect and need admiration and respect from others to fuel their self-esteem. They lack empathy, so they have difficulty recognising the needs, concerns, or feelings of others. Criticism, rejection and failure leads to massive feelings of shame which is often redirected into anger.
OCPD
Obsessive-compulsives are perfectionists and need to get every detail right. As such, they are anxious and want to be in control of situations, so to avoid mistakes. They find comfort in schedules, rules and details, but their devotion to perfection interferes with their relationships and life outside of work or school. They have a tendency to hoard and are unusually tight with money, just in case.
PPD
Paranoids believe that the world is dangerous and that others will try to harm, exploit and deceive them if they open up. They are always on guard to any sign of threat. They hold on to grudges, never forget a slight, nor pass up a chance for revenge.
STPD
Schizotypals are eccentric, disorganised people whose emotions and speech are strange and blunted. Their strange beliefs are associated with ideas of reference and magical thinking, but don't extend to full-blown psychosis. It's not uncommon for schizotypals to be misdiagnosed as being autistic.
SZPD
Schizoids are uncomfortable being around others and just want to be left alone. Connection with others is scary and difficult, so they tend to keep to themselves. They come across as awkward, distant, and overly formal, and may be described as “cold fish”.
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#dogpost#pd info#personality disorders#personality disorder concepts#prototypic descriptions#i have no idea what cold fish means btw that just what sperry said
132 notes
·
View notes