#fertility care
Text
My Infertility Journey: Part 4
Yeah, future me needs to go in the past and tell past me to not be crazy. Well, they have not arrived yet-part four starts. The sooner I get in the drivers seat the sooner I park my car in the winners circle I hope....Just hopping on late? Here is Part 1, Part 2, and Part 3.

August 2022:
A week after the ERA comes a cycle. This is highly unusual as it does not normally come that soon. Second half of the month is the start of round 4. Initial ultrasound and bloodwork scheduled to see if the body is on the starting line. Now let’s talk about the definition of insanity, it is doing the same thing over and over again expecting different results. Based on the ERA, I am perfectly fine and we have been doing this with proper timing-so initially they said we are going to move forward with no changes. At consultation, they mentioned adding Intralipids-IV injected twice during the process. I am open to this idea, more than the anti-coagulants, because I think my body can only handle so many injections. I only have two more embryos at this point, and while I want to make sure they have the best odds of sucess-there are physical limitations of being...ya know...human?
The results from the blood work came back, my hormones were too high. So they are having me wait and we will reassess on next cycle. I am happy that this news came from the doctor, I felt like it was better to wait and give the body a break. But for some reason, it felt like it would not have as much credence as it does coming from the doctor backed by “data”. I am looking forward to my break and plan on getting a family trip to Havasu in before my next cycle. PARTAY! No but otherwise this is a great time to hunker down and see if I can’t get some good training in for game day. Using muscle stims, heat, massage, and exercise to promote healing of the area. Maintaining diet and exercise to see if I can’t lose anymore weight before then.
September 2022:
Have I ever mentioned how much of this process is PLAYING THE WAITING GAME? But waiting has its own perks. So far just waiting for a cycle to come, estimated to come around the middle of the month according to P Tracker, and see if hormone levels are good enough to move forward. Also, I am (heavily) playing with the idea of implanting two instead of just one. My own doctor says the odds are better with just one, but I have heard a lot of other doctors/patients have success with 2. Part of me really likes the idea of implanting both and having this be the last round, for better or for worse. We will see what the doctor says.
So my body decided to get stuck in “period limbo” this cycle. I get all the feels but none of the results. Doctor did a “wellness check” on me and decided to reset my cycle with a week’s worth of Birth Control. Then we are going to move on the next cycle. I picked up my prescription and then took them, one a day, for a week. My doctor puts me on Enskyce, and man I usually get all of the side effects: migraines, nausea, and lack of energy.
October 2022:
Body goes into cycle and then on Cycle Day 5, we went in for an appointment. Ultrasound and bloodwork looked good, we updated my thyroid panel as well. Now starts injections and the new element this time-intralipids. They are to be done at a third party facility, Oso Home Care in Irvine, in week 4 (before transfer) and after transfer. I am (attempting) to schedule an appointment with Oso Home Care after my next Ultrasound/Bloodwork appointment with Fertility Care in Brea. Ya know the one appointment(s) before implant. It is kind of crazy how much happens in a month.
Drugs: EV (Estradiol Valerate), Dex (Dexamethasone), P4 (Progesterone), hCG, Valium, Doxy (Doxycycline Hyclate), Medrol (methylprednisolone),
Vitamins: Baby Aspirin, Prenatal vitamins (NAC, Prenatal, Omega 3, L Arginine, Coq10, Myo Inositol, D3)
Suggestions: Keto diet/Fasting, Exercise, Proper Injection Guidelines.
Price: $5,000+ (Fertility Care), $100+ (MDR Pharmacy), $550 (Oso Home Care),
Here are some Injection Guidelines:
Before: Ice the area
During: Inject the right area, Massage it after
After: Walk it off a bit, Use a heating pad
In Between: Arnica, Massaging to promote healing
Check: Infection (red, raised/bumpy, burning, itchy)
Note: Injections are intramuscular, and depending on the injection, there are only so many spots you can inject. Just because there are other muscles, does not mean you can use them even if your areas are “out of commission”. You just gotta keep them in commission!
The phone tag that was had was fun by all? Honestly as much as this is not my first rodeo and this should not worry me, the intralipids worry me a bit. Really the scheduling process being the slowest thing ever doesn’t help anything either. Be careful when doing research too, it is not always as helpful as you would think to know what you are signing up for. Also, the slow time between the first and second appointment where there is only an injection every 3 days is lovely. So I barely got my appointment for the intralipid place, if I did not call, that might not have happened. Then went in for the next ultrasound, the last one before implant. Ultrasound was good and blood work was TBD.
This starts the next phase of the process. From here we add 4 hCG shots, add 2 times a day of p4, and continue with EV every 3 days. Also, for the hCG...the first injection has to be in the back area, but the smaller ones can go in the stomach to give the back a bit of a break. Round one of the Intralipids happens. The dexamethasone comes off the schedule just before implant-a couple of meds get added for a couple days around implant. Implant happens, this time it will be a boy (currently between the names Roland and Kai). After implant it is suggested for up to 3 days of rest. Then we move into November (after playing the waiting game) to confirm the pregnancy.
Oso Home Care...Intralipids: Its a cute little place in Irvine. Kind of disorganized and busy but it would seem a lot people go to a facility like this. I got there early. I spent 2.5 hours in the chair. Yeah, kind of a long time. The gals that work there are sweet, but I don’t like how they had to prick both my arms to get it to work. I felt strange after? I am not sure how I was supposed to feel. Based on when I left and where home is, it took an hour to get home. But I hope in the future that since I am already in the system that booking is easier, and I kind of have a better idea of what to expect. Dress comfortable, don’t bring a book.
Ovation Fertility...Implant: I always forget COVID never stopped being a reality for hospital establishments. I always forget to bring a mask to these things. Arrive 15 minutes early in Newport Beach, take a Valium an hour before. Implant goes well-go home and rest. Also, if they let your partner in-film the implant.
Implant day is a day of rest, and this time I am trying to take two more days of rest after. I am an awful patient and this is hard for me to do. Post transfer we ran low on p4 so we transitioned to 1/2 crinone and 1/2 p4 for the every 12 hour injections. There are enough drugs on hand to get through to the pregnancy test and once confirmed, we stick with this or go all crinone. I don’t remember my last boys’ implant well but this time around, my left uterus feels like a battle zone a bit.
Trimester Breakdown:
Part 1: 10/7-1/8
Part 2: 1/9-4/12
Part 3: 4/13-7/15
November 2022:
An appointment was set up to have a blood draw/pregnancy test on 11/7. What was the time like before? I felt most, if not all, the symptoms. Pray tell, what are the symptoms of the first trimester?
First Trimester Signs: Nausea, Metallic Taste, Foggy Brain, Cramps, Tiredness, Breast Tenderness,
For me, and according to old wives tales, boys are supposed to be worse. This round definitely felt different as I felt very sore for up to a week after implant. Google says this is ok but man, it was kind of odd. The first blood test of Week 4/5 happened and TBD. If this goes well, I go two more times-two days apart. In theory the HCG a pregnant body produces should double every day. The first time you are able to view anything on an ultrasound is week 6. The next, and final, intralipid appointment would also happen that week.
The first blood test was good and positive, the next blood test the values should of doubled...and they did not. They increased but did not double. The office wants me to see the third test before jumping to any conclusions. The second blood draw was a 15% rise. The third blood draw was a 66% rise, so they kept us on the schedule and we scheduled the first ultrasound at 6 weeks 4 days. They also had me schedule my second, and last, intralipid appointment for that same day. Prior to going to going into the first ultrasound, there were 50/50 odds that this is a viable pregnancy.
We went in for an ultrasound and there was a gestational sac, but nothing that could be seen in the sac. They did a blood draw, to confirm the hCG is rising as a pregnant body should be. I had an intralipid appointment but they wanted me to move it, and wait for the results. The beta was rising, so we stay in the game another week. Order more drugs from MDR Pharmacy and scheduled another ultrasound for the end of the week. The intralipid appointment was moved to the same day as the next ultrasound.
Oso Home Care...Intralipids: This trip was shorter, already in the system and they have an idea of how quickly you take the liquids and what not. I believe this time was about 3 hours?
Also, I am keeping track of my weight, as women who are overweight before need to be careful how much weight they put on. When I checked on it, I actually had lost weight. Between my keto diet, morning sickness, and other pregnancy symptoms. In the first trimester one can lose a bit, but should this trend keep up in the second trimester...we got problems. Went in for the next appointment and while it was still not where it was supposed to be, there was improvement in both Beta (blood draw) and ultrasound findings. By this time I am almost 8 weeks along and there should be some major organs created, like the heart.
December 2022:
The next ultrasound would be interesting as it was kind of the determined trip to “call it”. Why would I want to call it? Because since implant, it has been very “we don’t have good news but we have not bad news so keep injecting”. And the body can only take so much for something that they said was most likely to end in bad news? But the doctor makes a good point that while certain things should be in place by this appointment, babies can be “past their due date” so if they are slow to grow, as long as they grow, it is fine? As the train carrying the passenger, the “limbo” is annoying as hell.
The Week 8 Ultrasound: Yeah, so that went about as good as that was going to. The doctor finally called it. It is sad, bumming, annoying, frustrating, relieving yet unwantedly so. They are three options to resolve this round: to let it happen naturally, use drugs to help “speed things along”, or get a D&C. For now, we are going to cancel medications and assess in another couple of days. Did a blood draw to see where the beta is, and establish a comparison point for declines in the future.
For the next blood draw, I could of gone to my Fertility Care office-but with us at the sad end of the process-and them not being part of our insurance-we decided to finish the process in slightly more complicated insured way. They ordered the blood draw at Quest Diagnostics. I made an appointment and the results were sent to Fertility Care. I have seen some insurance that covers infertility, but for the most part that is a sad joke. Some jobs cover that too. If you need that as an option, it’s worth looking into.
Pay attention to your body. I had sharp pains on my lower left abdomen area the day before the blood draw. Like, bad enough to make me basically pointless the rest of the night. The next day they continued, and I called it in. I am now on the alert for heavy bleeding and those pains, as the combination means bad news. But should be signs the body is starting the miscarriage process. To speed things up, they put me on Letrozole and Acetaminophen-COD. This will be my first time having a drug induced natural miscarriage.
Four pills at night for 7 nights, bleeding can last up to a week. Blood was being drawn at Quest Diagnostics and the beta hcg was going down. I used pads for a week to “measure” how much I was bleeding, more than two pads in two hours was bad news. Blood draw to see where we were at, luckily enough for all involved-there was no hemorrhaging. The second week of miscarriage recovery-less blood, less medications, but no less feels? Research shows it could take up to 6 weeks for my body to get back to “normal”. There are some herbs and vitamins I can take to help, but mostly it was rest and food and relaxation.
So, what happened? While there are no answers, there is a scientific name for this. Funny how that works out huh? Here is what I think happened:
“ A blighted ovum, also called an anembryonic pregnancy, occurs when an early embryo never develops or stops developing, is resorbed and leaves an empty gestational sac. The reason this occurs is often unknown, but it may be due to chromosomal abnormalities in the fertilized egg.” (Source: https://www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/expert-answers/blighted-ovum/faq-20057783)
Because this is an IVF process, and everything is tested and in some ways controlled, I doubt it is because of any chromosomal abnormalities. But it is crazy how many variations of miscarriages are out there. And really, even in the same person’s journey-no two are the same. Oh to know so much yet so little.
Honestly, this is a very tough process. I am not sure what to think. Doctor thinks we should implant (IN ME) the last embryo, possibly changing nothing, and see if it works when I am mentally and emotionally ready. For now, the only thing for sure is its BREAK TIME. Is it too soon for a surrogate? I don’t understand how I can be such a medical mystery. It is a very strange feeling.
#my infertility journey#IVF#in vetro fertilzation#round 4#pixabay#ERA#intralipids#rant#cvs pharmacy#birth control#enskyce#fertility care#oso home care#ovation fertility#surrogate#quest diagnostics#anembryonic pregnancy#miscarriage#blighted ovum
2 notes
·
View notes
Text
Demystifying Fertility Options: A Patients Guide To IUI IVF And FET At Healix Hospitals

Navigating fertility treatment options can feel overwhelming for many individuals and couples. At Healix Hospitals, we understand the importance of providing clear guidance and support to patients embarking on their fertility journey. In this comprehensive guide, we will demystify three common fertility treatments: Intrauterine Insemination (IUI), In Vitro Fertilization (IVF), and Frozen Embryo Transfer (FET). Let's explore each option and understand how they can help you achieve your dream of parenthood.
1. Intrauterine Insemination : Quick Overview!
Intrauterine Insemination, commonly known as IUI, is a fertility treatment where sperm is directly placed into the uterus during the woman's ovulation period. Here's what you need to know about IUI:
Process: During IUI, carefully prepared sperm is inserted directly into the uterus using a thin catheter, timed to coincide with ovulation.
Who it's for: IUI is often recommended for couples with unexplained infertility, mild male factor infertility, or cervical issues.
Success rates: Success rates for IUI vary depending on factors such as age, fertility diagnosis, and the woman's ovarian reserve. Our experienced fertility specialists at Healix Hospitals will provide personalized guidance based on your specific circumstances.
2. Decoding In Vitro Fertilization (IVF)
In Vitro Fertilization, or IVF, is a more advanced fertility treatment that involves fertilizing eggs with sperm outside the body. Here's a closer look at IVF:
Procedure: IVF involves stimulating the ovaries to produce multiple eggs, retrieving the eggs surgically, fertilizing them in a laboratory, and transferring the resulting embryos into the uterus.
Candidates: IVF is recommended for individuals or couples with more complex fertility issues, such as tubal factor infertility, severe male factor infertility, or advanced maternal age.
Success rates: While IVF success rates can vary, advancements in technology and protocols have significantly improved outcomes over the years. Our dedicated team at Healix Hospitals is committed to maximizing your chances of success through personalized care and state-of-the-art techniques.
3. Navigating Frozen Embryo Transfer (FET)
Frozen Embryo Transfer, or FET, is a procedure where embryos that were previously frozen during an IVF cycle are thawed and transferred into the uterus. Here's what you should know about FET:
Process: After undergoing an IVF cycle, any excess embryos can be cryopreserved (frozen) for future use. When the time is right, these frozen embryos can be thawed and transferred into the uterus during a FET cycle.
Benefits: FET offers patients the flexibility to undergo multiple embryo transfer attempts without the need for additional ovarian stimulation and egg retrieval procedures.
Success rates: FET success rates are comparable to fresh embryo transfers, and in some cases, may even be higher. Our experienced fertility team will work closely with you to optimize your chances of a successful pregnancy through FET.
Read More: https://www.healixhospitals.com/blogs/demystifying-fertility-options:-a-patients-guide-to-iui-ivf-and-fet-at-healix-hospitals
#Frozen Embryo Transfer#Fertility Treatment#Assisted Reproduction#Intrauterine Insemination (IUI)#In Vitro Fertilization (IVF)#Frozen Embryo Transfer (FET)#Reproductive Options#Infertility Solutions#Family Planning#Fertility Clinic#Conception Assistance#Fertility Procedures#Reproductive Health#IVF Process#Fertility Care#Fertility Services#Pregnancy Planning#Assisted Conception#Reproductive Medicine#Fertility Support#Fertility Specialists
1 note
·
View note
Text
Embracing Motherhood: Finding the gynecologist and fertility specialist in patna with Dr. Monalisa Singh

The road of becoming a parent is a deep one, full of expectation, hope, and occasionally difficulties. For people dealing with fertility issues, choosing the best gynecologist and fertility specialist in patna is essential. Dr. Monalisa Singh stands out as a shining example of knowledge and kindness, providing individualized treatment and creative solutions catered to your particular requirements.
It is crucial that you develop an alliance with a healthcare provider who is knowledgeable about the intricacies of reproductive health as you embark on this life-changing journey. When it comes to treating reproductive difficulties, Dr. Monalisa Singh provides a depth of experience and a dedication to excellence. Throughout their reproductive journey, patients receive personalized attention and support at her practice, which is tucked away in the heart of Patna.
The patient-centered, comprehensive approach to reproductive care taken by Dr. Monalisa Singh includes extensive assessments and treatments that are supported by research. Dr. Singh uses the most recent developments in reproductive medicine, from first consultations to complex treatments like intrauterine insemination (IUI) and in vitro fertilization (IVF), to maximize your chances of becoming pregnant.
In addition to her professional expertise, Dr. Monalisa Singh stands out for her steadfast commitment to her patients' wellbeing. She understands that infertility issues can have a negative emotional impact and works to provide a supportive atmosphere where patients feel empowered and understood. You are more than just a patient with Dr. Singh; you are a partner on your path to motherhood.
In addition to her medical background, Dr. Monalisa Singh has a strong desire to lead the way in innovative reproductive healthcare. In order to provide her patients with the most cutting-edge and efficient treatment options possible, she consistently upgrades her knowledge and abilities. Whether you're considering fertility preservation or looking for answers for repeated miscarriages, Dr. Singh offers compassionate, all-encompassing care.
On your journey to fatherhood, selecting the best gynecologist and fertility specialist in patna is crucial. You're choosing more than just a physician when you work with Dr. Monalisa Singh; you're choosing a reliable ally who will walk by you, providing knowledge, encouragement, and hope. Make an appointment with Dr. Singh now to begin the process of fulfilling your dream of becoming a parent.
0 notes
Text
Fertility Care Journey ReproMed Fertility

ReproMed Fertility: Fertility Care Journey There are foundations of care and pillars of support that can guide your fertility journey. ReproMed is well-grounded in understanding the entire range of fertility needs; our team’s commitment is to guide you through the plan that’s right for you with compassion and encouragement.
0 notes
Text
Find the Best Fertility Specialist in Thane West for Effective Treatment

Dr. Manjushri Kothekar: Your Trusted Fertility Specialist
At Chembur Fertility Clinic, Dr. Manjushri Kothekar, the leading fertility specialist in Thane West, offers personalized care and cutting-edge treatments to help couples achieve their dream of parenthood.
Tailored Treatment Plans
Dr. Kothekar designs customized fertility plans, utilizing advanced assisted reproductive technology (ART) such as IVF, IUI, and more, ensuring the highest chances of success.
Empathetic Support
Beyond medical expertise, Dr. Kothekar provides compassionate support, easing the emotional burden of infertility and empowering patients to navigate their journey with confidence.
Trusted Guidance
Couples seeking the best fertility specialist in Thane West trust Dr. Kothekar's unwavering commitment to their well-being and dreams of starting a family.
Excellence in Fertility Care
Under Dr. Kothekar's stewardship, Chembur Fertility Clinic stands as a beacon of excellence, offering a nurturing environment where patients receive comprehensive and compassionate fertility care.
Ready to start your journey towards parenthood?
For expert fertility care, contact Dr. Manjushri Kothekar, the best fertility specialist in Thane West, at Chembur Fertility Clinic. Call now at 976937593 to schedule your consultation and take the first step towards parenthood.
#ivf clinic in chembur#ivf clinic in mumbai.#dr. manjushri kothekar#ivf specialist in chembur#fertility clinic in chembur#ivf specialist in mumbai#ivf specialities in chembur#best fertility specialist in Thane West#fertility specialist in Thane West#best fertility specialist#fertility specialist#Chembur Fertility Clinic#healthcare#fertility care
0 notes
Text
Best IVF specialist in Lucknow - Dr Radhika Bajpai
Meet the exceptional Dr. Radhika Bajpai, leading the way as the Best IVF Specialist in Lucknow. Serving as the Head of the Department and Consultant in Infertility & IVF at Apollomedics Super Speciality Hospital, Dr. Bajpai brings unparalleled expertise and compassion to her role. Trust Dr. Radhika Bajpai for personalized, comprehensive care on your journey to parenthood.
Address: Kanpur - Lucknow Rd, Sector B, Bargawan, LDA Colony, Lucknow, Uttar Pradesh 226012
Phone Number: 08429021960
Contact Now
0 notes
Text

Audubon Fertility is committed to expanding access to comprehensive Fertility Care. Explore our strategies for making fertility treatment more accessible and attainable.
0 notes
Text
Tailored Care for Optimal Conception and Pregnancy
Utilizing personalized fertility care involves tailoring individualized approaches to support individuals and couples throughout their fertility journey. By taking into account distinct medical histories and preferences, this approach strives to enhance the effectiveness of fertility treatments, encompassing methods like the advantageous fallopian tube flushing procedure. This customized strategy further bolsters the potential for successful conception and improved pregnancy chances through fallopian tube flushing.
0 notes
Text
5 Tips To Improve Sleep

Discover five expert-recommended tips to enhance your sleep quality, from establishing a calming bedtime routine to optimizing your sleep environment. Implementing these strategies can promote better rest, ensuring you wake up refreshed and ready to take on the day, whether you're trying to conceive or seeking expert guidance at a fertility clinic.
0 notes
Text

SCI IVF Hospital is the best fertility treatment centre in Delhi. A fertility clinic that brings transparency, simplicity & lots of love to fertility care.
𝗧𝗼 𝗗𝗶𝘀𝗰𝘂𝘀𝘀 𝘄𝗶𝘁𝗵 𝗜𝗩𝗙 𝗘𝘅𝗽𝗲𝗿𝘁𝘀, 𝗰𝗼𝗻𝘁𝗮𝗰𝘁 𝘂𝘀 𝘁𝗵𝗿𝗼𝘂𝗴𝗵 𝗳𝗼𝗹𝗹𝗼𝘄𝗶𝗻𝗴 𝗼𝗽𝘁𝗶𝗼𝗻𝘀
0 notes
Text
preterm delivery | lifespring maternity Hospital
What Are the Symptoms & Risk Factors of Preterm Delivery &How to Prevent It?
It's difficult to predict when a baby will be born. Most people have a plan for labor and delivery, assuming that the pregnancy will last the standard 40 weeks. However, when it comes to delivery, the baby sometimes has its own idea and decides to come out early. Some hazards can be attributed to a variety of factors, including a previous premature baby.
What is Preterm Delivery?
Preterm labor is defined as giving birth at least three weeks before the due date. This signifies that a preterm birth occurs before the 37th week of pregnancy. Preterm babies are born before the 40th week of a normal pregnancy. However, they frequently have problems, which vary in severity. It can potentially endanger the mother's and baby's health.

Preterm Delivery Symptoms and Causes
Premature birth can occur unexpectedly and for no apparent reason.
For medical reasons, the healthcare provider may induce preterm birth. However, the following are some of the most common causes of premature birth:
Diabetes and other infections in pregnant women are examples of chronic health disorders.
Excessive alcohol consumption or drug misuse
Having previously had numerous pregnancies, such as triplets or twins,
Having several pregnancies
Preeclampsia is characterized by high blood pressure while pregnant.
There were less than 18 months between pregnancies.
Problems with the cervix or the uterus
Infections or vaginal bleeding during pregnancy
Risk factors for premature birth
The exact cause of preterm pregnancy is unknown.
However, several risk factors enhance the likelihood of premature birth.
They are as follows:
expecting triplets, twins, or other multiples
Having fewer gaps between pregnancies
Being overweight or underweight prior to pregnancy
Domestic abuse or the death of a loved one is both stressful circumstances.
Multiple miscarriages or abortions
Physical harm or injury
having high blood pressure that is not managed by drugs, as well as a low-lying placenta
Premature birth prevention
Although the reason for preterm birth is unknown, there are a few things women can do to lower their chances of having a young baby.
It includes the following:
Progesterone supplementation:
Women who have a history of preterm birth or have a short cervix can minimize their risk by taking this supplement.
Cervical cerclage is a surgical treatment used to treat women with a short cervix or a history of preterm labor.
The cervix is sewn with sutures in this technique to provide extra support to the uterus. When the time comes to give birth, the sutures will be removed.
Other activities include: While pregnant, avoid smoking, drugs, and alcohol.
LifeSpring Maternity Hospital is one of the best gynecology hospitals in Hyderabad, with an excellent team of gynecologists providing comprehensive treatments.
0 notes
Text
My Infertility Journey: Part 3
If you read part 1, and followed all the way to part 2, I know what you are thinking. What are you thinking? Based on two miscarriages, RIP Luella and Damien, this “possible” next round is a whole different ball game. Different risks, more knowledge, more pain, less hope. There are still options, and yes always hope, but we are into some different territory.

June 2022
This will pick up in part 3 where we left off in part 2. I can imagine your thoughts, did you take any time at all? My recovery time was shorter, as my body came back into normal mode way faster round 2 versus round 1. Mentally, emotionally, yeah I am still a wreck. To a certain degree I don’t think that is going away. Next step was to have a consultation about next steps. Next steps don’t necessarily mean let’s implant again. It might mean tests, but are there any tests I haven’t done? Will the tests be worth it? How invasive are the tests going to be? Should we start considering the “S” word yet?
We had a pow wow with our doctor. There is not a lot of tests I have not done, so we took a look at the file and figured out what we had done, and what we had not. They want me to go back on the fasting/keto diet and there we might have some disagreements, as I am not sure that it is working for me anymore but I am keeping an open mind. They want to do an ERA with the next cycle and do cancer testing, and possibly add anticoagulants / intralipids into the 3rd implant. Let’s break this down a little bit more.
ERA/Cancer: This is a mock cycle in which instead of implanting after going on all the drugs “like normal” you take a skin scrape for Endometrial Receptivity Analysis. Based on my research, one should take a valium before the procedure, and while the actual pain of the procedure is short, it is supposed to suck. Day of the procedure one should have some spotting and have less than a day of recovery, and it will take 2-3 weeks to get the results back. The results will tell you if you need more or less or the same amount of preparation for implant. This is highly suggested for anyone with at least one loss to increase odds of sucess for the next implant. My doctor wants to take part of the skin scrape and have it tested for cancer. The only cancer I could find was endometrial cancer. If it is that we will get more into that, but I will tell you right now, it would make a lot of sense if I did have it. We are looking to see if this explains not only the losses but the unexplained bleeding that has happened since we started our fertility journey. The test for this is called EMB (Endometrial Biopsy).
Anticoagulants/intralipids: So intralipids are extra nutrients that get delivered to your system by IV to make sure your body has everything it needs to make sure baby makes it. Diet should do so, but between pregnancy restrictions and fasting/keto diet, some doctors add this. I don’t know much more than that about it, once I know more I will update this section. Anticoagulants are blood thinners that are injected. I believe they are injected into ones stomach and it is supposed to help not have blood problems while on an IVF cycle.
July 2022
In July, we are waiting for the body to have its first cycle since the miscarriage. Now there are two trains of thought, some people start the count down clock when the body comes to 0 beta results OR when the miscarriage happened. For me, the miscarriage happened in May/June 2022 and 0 beta happened in June 2022. At first the doctor said to call him by 7/15 if I did not have a cycle by then, but then he adjusted it to 8/1. 8/1 makes more sense, as it could take up to 3 months for the body to come back to normal with a cycle after a miscarriage. 3 months would be either: May June July OR June July August. So this month we play the waiting game.
While we “wait in july” (god that feels like a wannabe twilight reference) let’s talk about how important it is to listen to your body. Coming out of miscarriage, I had “fever weekend” with rigors and really I was not ok even after I felt better. I was talking to doctors on the phone, but not going in to see one in person. Urine and blood testing were ordered and it showed my body was fighting some sort of infection, because I was feeling better they did not prescribe any medications. They arranged another urine/blood test to see what future results said. The second round of tests showed that there was still something not ok. They gave me antibiotics. They did confirm it was a UTI, but not much else.
My theory: I had the miscarriage and with the changes I got a UTI, but it got lost in the shuffle. UTI’s that go unnoticed can turn into a kidney infection and the body could try to “fever it out” to fix itself. This combination is called Septic Shock.
I took the antibiotics, and (as far as I know) I am all better now. The doctor doesn’t think the miscarriage has anything to do with it since the infection appeared in the second result. But it does not explain anything else that happened. Regardless of what happened, or happens, listen to your body and don’t be as stubborn as me in not going to get help. I am grateful that I am ok enough to pull myself through that, but luck will only get one so far.
August 2022
This month my body would of had a natural cycle, or I will call my doctor and we will force a cycle with medication. My body was kind of coming in and out of cycle towards the end of month, so I called it and made an appointment to start the process again. Last week of July we had an appointment to have an ultrasound and blood work to see if we are good to start the ERA round, and if we are, we order more drugs from MDR.
Went in for the appointment, and we are good to go. Schedule received, drugs ordered, and anxiety enters stage right. Let’s go over some of the basics in this cycle:
Drugs: EV (Estradiol Valerate), Dex (Dexamethasone), P4 (Progesterone), hCG, Valium
Vitamins: Baby Aspirin, Prenatal vitamins (NAC, Prenatal, Omega 3, L Arginine, Coq10, Myo Inositol, D3)
Suggestions: Keto diet/Fasting, Exercise, Proper Injection Guidelines.
Price: $2000 for the ERA, $500 for drugs from MDR, $325 for the EMB
Here are some Injection Guidelines:
Before: Ice the area
During: Inject the right area, Massage it after
After: Walk it off a bit, Use a heating pad
In Between: Arnica, Massaging to promote healing
Check: Infection (red, raised/bumpy, burning, itchy)
Note: Injections are intramuscular, and depending on the injection, there are only so many spots you can inject. Just because there are other muscles, does not mean you can use them even if your areas are “out of commission”. You just gotta keep them in comission!
Also, my Oscar insurance covered some of the drugs! Who would of guessed! We had one appointment today, we have another 10 days later to check the lining, and 6 days later is the ERA. I have heard the ERA is painful for not very long, but painful none the less. I will update this with those updates. Next appointment came, and I asked about Cancer testing prices and a Valium for the procedure. Next time we see the doctor, it is ERA time.
ERA: Day of the test has arrived. I asked for a valium and received one, with instructions to take it an hour before the procedure. Also to not drive myself to the office. I will oblige. My procedure was at 11 am on a Thursday in August, and I took the valium at 10 am. Got to the office by 11 am. Procedure was prepped for and once started, very short. Dear god, just because that pain is only for a minute or less-does not mean that it is not the most excruciating and violating pain there really could be, with some complimentary cramps to go with it. I signed some paperwork and then left. Feeling wise after, it is sore and cramping and emotionally I am done. Plan for the rest of the day is to rest and recover from not only the procedure but from all the drugs in general. Day of was cramping and some spotting. Next day was better but not like myself yet.
The “need for mental breakdown” came, as this is my second round IN THE SAME YEAR. It was my first panic attack, and it was a pretty scary thing. I tried to meditate, walk, sit, and finally exhaustion and ice cream lead to sleep. Update, I ran the numbers and based on the cycle that comes in August-its 21 days from day 1 to implant day, in theory the test results come just in time (if ontime) to know when to implant (early-normal-late). At this point, I have to decide a couple of things: do I go back so soon? I only have two more embryos left, am I ready to risk life or death for it? Holiday season is coming up, do I really want up to 12 weeks of injections starting pre halloween?
ERA Results: If there is a “before” “normal” and “later” window for timing, I am the normal timing. WHICH I THOUGHT I WAS BASED ON THE LAST TWO IMPLANTS. But I guess I am glad I know for sure?
EMB Results: No infections and no cancer. Yay?
Results came early, which I think is funny because I wanted to know the results before going into another cycle. Be careful what you wish for, the universe will grant it. I knew I was facing either “nothing is wrong with you” or “here is what is wrong/what you should of done before” when going into this. I am glad to be healthy but it leaves me answerless still.
Highly Suggested: it is so important to have enough people you can count on, so that if your spouse who normally does the injections can’t, you can still keep on schedule. I almost missed one of my injections because I misread/missed it on the schedule and he had work. It is also a great idea to not be the only one reading the paperwork. Both should read, and ideally, the person giving the injections should understand and prep and clean them more than the partner being injected. It takes something off the injected’s shoulders and allows them to focus on getting through to the end line. Also, this is being added to this note as I was told by my spouse that I messed up the preparation of one of the injections, and we might have used the wrong needle one time. If you miss an injection, that is generally not good, but I am also on a lot of hormones right now and If I make a mistake, well its not that shocking.
It is kind of crazy to me to think I could do three rounds of IVF in a year. But then the year before it took me a year to come out of my first miscarriage. Crazy stuff. Let’s say for shits and giggles, we implanted again in 2022, that means by christmas I am over the moon and sailing through my first trimester or sadder than puppy dog eyes. The bigger picture is an important thing to look at when going through this process. I can not believe I am considering a fourth part but stay tuned.
#rant#pixabay#my infertility journey#part 3#miscarriage#ivf#in vetro fertilization#fertility care#brea#surrogate#surrogacy#ERA#endometrial receptivity analysis#cancer#endometrial cancer#intralipids#anticoagulant#septic shock#antibiotics#estradiol valerate#dexamethasone#progesterone#hcg#valium#baby aspirin#prenatal#nac#omega3#larginine#coq10
0 notes
Text
Fertility doctors, IVF families, Post-Roe: 'We are anxious'
Fertility doctors, IVF families, Post-Roe: ‘We are anxious’
Shelly Battista, 36, mother and IVF patient, Chicago.
Barbara Collura, president and CEO, Resolve, The National Fertility Association, McLean, VA.
Sean Tipton, chief policy and advocacy officer, American Society for Reproductive Medicine, Washington, DC
Contemporary OB/GYN Diary: “Not Just Abortion: How the Demise of Roe v. Wade May Affect Fertility Care.”
Eli Reshef, MD, reproductive…
View On WordPress
0 notes
Text
By: Christina Buttons
Published: Apr 4, 2024
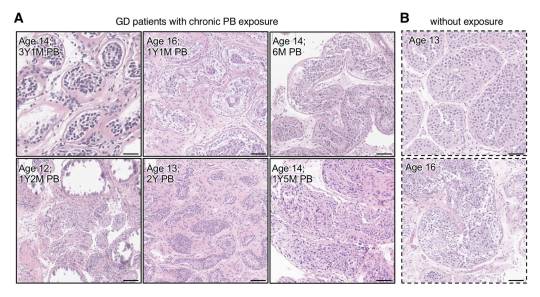
[ Figure 2: Representative images of Hematoxylin and Eosin-stained sections of testicular tissue biopsied from the testis from GD patients (A) with and (B) without PB exposure. ]
In a groundbreaking study from the Mayo Clinic, a globally recognized leader in medical research and patient care, researchers examined the effects of puberty blockers on testicular development in gender dysphoric male children. Their investigation revealed evidence of mild to severe atrophy in the sex glands of these children, leading the authors to express doubt in the claims of “reversibility” often made about puberty blockers.
The authors assert, “We provide unprecedented histological evidence revealing detrimental pediatric testicular sex gland responses to [puberty blockers].”
This preprint study, not yet peer-reviewed, presents evidence that puberty blockers induce significant cellular changes, impacting testicular development and sperm production in ways that are not fully reversible, with potentially permanent effects on testicular function and fertility. It challenges the longstanding view of puberty blockers as a reversible "pause button" on puberty.
As noted by the researchers of this study, no long-term studies exist for the use of puberty blockers in the context of stopping puberty for gender dysphoric children, and many potential health consequences remain unknown. In particular, the long-term impact on reproductive health is uncertain, making this study critical for filling this knowledge gap.
To address these unknowns, the Mayo Clinic has established the largest collection of testicular samples for patients aged 0-17 years, including those with gender dysphoria who have and have not yet received puberty blocker treatment, creating a database of over 130,000 individual cells for analysis.
Using a novel approach, the research team meticulously analyzed testicular tissue samples from youths undergoing puberty blocker treatment, with those not on puberty blocker treatment serving as controls. This comparison provides important insights into the potential cellular and molecular changes induced by these drugs.
Key Findings
The study utilized the Mayo Clinic's Pediatric Testicular Biobank for Fertility Preservation, which has been recruiting patients primarily from pediatric urology departments since 2015. Researchers analyzed testicular specimens from 87 young individuals (ages 0-17) undergoing fertility preservation surgery for various health reasons. Among these, 16 were gender dysphoric boys between the ages of 10 and 16, all of whom began identifying as transgender girls between the ages of 2 and 15. At the time of surgery, 9 patients (56%) were already on puberty blockers, with exposure ranging from 3 to 52 months. The authors noted that 100% of the 16 children would eventually go on to take them, highlighting “the widespread nature of PB intervention in this demographic.”
Among nine patients treated with puberty blockers, two exhibited unusual features in their testicles upon physical examination. One patient had abnormalities in both testicles, including incomplete development of the tunica albuginea, which is a protective covering around the testicles. The other patient had a right testicle that was difficult to detect.
In one part of the tissue-level analysis, over 400 testicular biopsy samples were analyzed and stained to examine the differences between those treated with puberty blockers and those who were not. Comparisons showed that testicular development in those treated with puberty blockers was abnormal compared to non-treated individuals. There was variability in how individuals responded to puberty blockers, leading to different outcomes in testicular development, including the degeneration of testicular tissues.
The study authors presented a case of a 12-year-old patient who underwent treatment with puberty blockers for 14 months. In this individual, 59% of the sex glands showed complete atrophy, along with the presence of microlithiasis—a condition where small clusters of calcium form in the testicles. This insight suggests that puberty blockers could lead to lasting structural changes. Additionally, research has shown a link between testicular microlithiasis and testicular cancer.

[ D) Representative images of normal (top) and fully atrophied sex gland (bottom). ]
This study also utilized single-cell analysis to investigate the effects of puberty blockers and aging on testicular cell composition. It took a very detailed look at individual cells from the testicles of a 14-year-old who had been on puberty blockers for over 4 years. The study analyzed a total of 130,100 cells, including 11,199 cells from the juvenile puberty blocker-treated patient.
The study observed that over 90% of the cells responsible for sperm production in this patient were stunted at an early developmental stage, unable to progress further. Additionally, it found "pathologically" higher and lower levels of two types of support cells (Sertoli cells) necessary for healthy sperm development. These findings suggest that puberty blockers can disrupt the normal maturation process of cells critical for sperm production.
In another part of the analysis, the authors found distinct cell-specific changes, including altered expression patterns of puberty-associated genes in endothelial cells, due to puberty blocker treatment. The authors believe that these drugs might induce juvenile testicular atrophy in part by disrupting the normal function of testicular endothelial cells.
Another aspect of the study focused on examining the effects of puberty blockers on the genetic activity of early-stage sperm cells, revealing significant changes that could potentially influence their development and fertility. By analyzing the activity of specific genes within these cells, the researchers found that puberty blockers may have caused alterations in gene expression, affecting processes crucial for the normal growth and function of these cells. This analysis suggests that the use of puberty blockers in gender dysphoric youth could have lasting implications for their reproductive health, particularly by impacting the ability of these early-stage sperm cells to mature properly.
Study Impact
Puberty blockers are increasingly used as a treatment for gender dysphoric youth to halt the development of secondary sex characteristics, such as breast development and widening of hips in females, or the growth of facial hair and deepening of the voice in males. Thousands of children in the United States are placed on this medical pathway as part of the gender-affirming model of care, under the presumption that these drugs are safe and fully reversible.
However, many aspects of the long-term consequences of puberty blockers, which have been administered to children off-label in an experimental manner, remain unknown. This study contributes valuable insights into the potential irreversible harm these treatments can cause to bodily and reproductive functions.
Arguably, the most critical finding is the evidence of mild to severe sex gland atrophy in children treated with puberty blockers. This atrophy signifies potential damage or impairment to the structures essential for sperm production, raising serious concerns about the long-term fertility impacts of these drugs for these individuals.
Given the Mayo Clinic's esteemed reputation in the medical and research communities, should the study pass peer review without any issues, its findings will carry significant weight.
Broader Implications
Puberty blockers belong to a group of synthetic gonadotropin-releasing hormone (GnRH) analogues. These drugs act on the pituitary gland to hinder the release of chemical signals that typically trigger the production of estrogen and testosterone. Historically GnRH analogues were used to treat conditions such as prostate cancer, fibroids, and endometriosis and, in some cases, as a measure to chemically castrate sex offenders.
In children, puberty blockers prevent the natural changes of puberty driven by sex hormones and have been used to treat central precocious puberty, a condition where a child begins to sexually mature much earlier than usual. In gender dysphoria, puberty blockers are administered experimentally, lacking long-term testing.
Notably, the U.S. Food and Drug Administration (FDA) has not approved puberty blockers and sex hormones for use in pediatric gender care. No clinical trials have substantiated the safety of these drugs for such non-approved applications and manufacturers of puberty blockers have repeatedly declined to conduct safety trials for their use on this cohort.
While puberty-blocking drugs are often promoted as “safe,” "reversible" and a "pause button" on puberty, these characterizations seem to stem from their approved use for treating central precocious puberty in younger children, not their burgeoning off-label use for managing gender dysphoria in adolescents.
Past studies have indicated possible negative effects on bone density and brain health. There is also a concern that these drugs might solidify gender dysphoria in adolescents, potentially leading them down a lifelong road of biomedical interventions. Following reports in 2016 of suicidal ideation in children administered puberty blockers, the FDA instructed drug manufacturers to include a warning about potential psychiatric issues on the drugs' labels.
Puberty blockers are increasingly administered to adolescents at Tanner Stage 2, the first signs of puberty. Research shows administering puberty blockers at this stage, followed by cross-sex hormones, may result in infertility, sterility, and sexual dysfunction. Furthermore, they inhibit the development of mature male genitalia, making it difficult to create a pseudovagina in the event of a later vaginoplasty due to a lack of sufficient tissue.
The National Health Service England recently announced it would no longer prescribe puberty blockers to youth outside of research settings and closed down its only national clinical service for pediatric gender medicine, following a review that deemed the service "not safe.”
Several European countries, including Sweden, Finland, the UK, Denmark, and Norway have updated their guidelines for youth transition to align with systematic evidence reviews, the gold standard in evidence-based medicine. These reviews concluded that the risks associated with youth transition outweigh any purported benefits. Consequently, these countries have implemented restrictions on medical interventions, prioritizing psychotherapy as a first-line response for minors experiencing gender-related distress.
==
They're sterilizing boys and giving them cancer. When "god" does it, we call him evil. When humans do it, we call it "gender affirming care."
#Christina Buttons#puberty blockers#atrophy#medical scandal#medical malpractice#medical corruption#sterilization#fertility#irreversible#gender affirming care#gender affirming healthcare#gender affirmation#queer theory#gender ideology#gender identity ideology#intersectional feminism#religion is a mental illness
188 notes
·
View notes