#Pregnancy Services
Text
A Whistle Stop Tour Of Birth
There are many unusual things you may experience during your pregnancy. The body goes through a lot of changes, which compels you to change your lifestyle. Butterbean covers the process of what actually happens during birth. From pregnancy to childbirth, learn everything here.
Website:
https://butterbean.uk/a-whistle-stop-tour-of-birth/

0 notes
Text
A personal update...
I've been quiet on here and with my WIPs for a while; it's a brief hiatus and nothing's abandoned -- I've just been settling in as a new mum with my baby girl ❤️💜❤️
#thank you fandom for being an unwitting outlet over the last 10 months#normal service will resume#when I've slept!#personal#tw pregnancy
11 notes
·
View notes
Text



What does everyone think of Nigel Forbes-Colbie ever getting pregnant? It doesn't matter how you interpret it: Omegaverse, males can get pregnant Au, Trans! Nigel. Just tell me your guys' headcanons of Nigel's pregnancy: The changes, the hardships, the softness, and the vulnerabilities.
#murderous intent#like minds 2006#like minds#alex forbes#nigel colbie#Alex Forbes X Nigel Colbie#Nigel Colbie x Alex Forbes#If you guys haven't noticed my recent posts I've been feeling way too soft for this fandom#Like#Too soft#And it's both Nigel and Alex's fault for making me too soft when all I want is to cause chaos and do crimes#To be honest I'd like to Imagine Nigel's pregnancy as an arduous one: Swollen feet . Sore back. Weird cravings. Mood swings. Everything.#And he isn't used to seeing himself get swollen with life each and every day. While Alex is so gullible first thing in the morning because#of the baby bump growing every single day. And Nigel getting rounder every week.#Sure. Nigel is enjoying being pampered by Alex with all these services and gifts but sometimes he thinks that he isn't that attractive#Anymore for Alex. And that while he's carrying his children he will leave him like a used toy.#He'd have instances where he'd feel conflicting feelings for their child and think of possibilities of removing her from his body#But he'd soon regret it. He just breaks down into tiny little pieces of ever thinking of their daughter that way. His and ALEX"S#He can never stomach killing her. He can never stomach ruining her beautiful life that he has yet witnessed.#He still has his self-harm tendencies but he avoids it. He avoids harming his angel. His miracle. His life.#He wants to be a good father to his child. He wants to nurture her. Feed her knowledge and love. Cater to her needs and be at her beck#and call: be a father.#Alex knows what's happening to Nigel. They talk. And they talk everyday. He knows how much it can be hard for Nigel during his pregnancy#And he will always be there to protect his spouse and his unborn child.#He will spite their original purpose in order to create their own purpose. Which Nigel had a hard time letting go of.#It was hard. Seeing the history that made them into the people they are today. But it had to#they had to change#change for their family.#For their miracle.#And Nigel seeing Alex being this doting makes him fall for him ten times more
9 notes
·
View notes
Text
one thing i truly do not know where i stand on is the ability 2 change legally documented gender. someone throw some opinions at me so i can figure out wtf i think abt that
#i know i do NOT support the ability 2 just up and change it based on self-id#but im like. ok obviously if someone looks totally male but it says female on their ID they are going 2 have some issues#and they can b put in very real dangerous situations there#but i also very much support the need for sex-specific services. so how does that figure in#and i ALSO think transmen should generally have a right to access most female-specific services so how does THAT figure in#and u get issues w medical treatment w certain things being/not being covered or available depending on if ur male or female#transmen being refused pregnancy care or gyno care bc their documentation says male#i think w medical stuff the issue is pretty much solved by adding extra options on documentation - male/female/ftm/mtf#but that wouldn't solve the issue in other areas#like u cant just make someone walk around with an ID declaring that theyre transgender thats so scary thats none of anyones business
26 notes
·
View notes
Text
Babies are not props to be used to validate gender feelz. And unfortunately this is just the start of a long list of why this guy should not be around kids
By Genevieve Gluck February 26, 2024
A trans-identified male residing in Canada who claims to be HIV positive and inserts progesterone rectally has been allegedly “breastfeeding” his child with the support of established medical clinics. Former men’s rights activist Murray Pearson, 52, who uses the name Margaret (Margie) Fancypants on social media, has been criticized after he shared an image of himself at a lactation clinic holding a young infant.
The photo was first posted three months ago on Reddit community titled r/TransLater, a board dedicated to males who transition later in life. In a post titled, “Milk, baby, milk! MTF 52,” wherein Pearson appears ecstatic that one “benefit of being transfemme” includes “that you can be pregnant and get drunk” with no undue problems.
“I have a baby almost 9 months old… I cannot wait to connect through feeding. And yes, I will stop drinking before it negatively affects anything they drink!” said Pearson

“This is a wish I have had for decades. My egg cracked a year ago on December 12 and I realized I could nurse my baby already on the way. That lit a fire under me, and I have gone from having lean pectoral muscle in March to full B-cups now and growing fast,” he added.
Pearson continues on to claim to have the assistance of “medical expertise,” including “five physicians in three clinics in two world class hospitals,” with one of the clinics named as the Goldfarb Clinic in Montreal.
“Two endocrinologists, Newman and Goldfarb, created a protocol to induce lactation in adoptive mothers,” Pearson explained in the comments. “It works for trans women as well, it works best when breast growth is mature but I am taking domperidone while my primary breast growth is underway. By an astonishing coincidence, I live right next to their breastfeeding institute!”
According to statements Pearson has made on social media, he began identifying as transgender in December 2022, and the following year, began taking progesterone. Approximately eight months ago, Pearson announced that he had found his “true self” as a result of performing in a drag show for a friend’s birthday celebration.
Earlier this month, Pearson described the first moment he believed he was a woman after trying on used women’s clothing at a thrift store. “I realized that the beautiful curvy woman in the mirror was the real me and I could be her every day… after more than two decades of stealth resistance. 87 days later I started spiro, 14 days after that estradiol, and now I am looooooving my boobs. Having curves without fakery is AMAZING.”
In a post made to the TransLater community last week, Pearson described how to insert the female hormone progesterone rectally, as a suppository, rather than swallowing it as a tablet.
“My breasts get a wonderful plumpness and pleasing jiggliness when I have had progesterone the night before…. You’ll need some lubricant (personal lube such as K-Y jelly or similar, or silicone personal lube which may be overkill, or some sort of non-irritating oil; I use my own mixture of cocoa butter and shea butter) to allow free clearance for the capsule… Some people simply pop the capsule in their mouth to use saliva, but I like a more effective lube,” he commented.
Pearson has also shared images of himself in a blue and pink wig attempting to eat ice cream containing the hormone in a seductive manner.

Disturbingly, Pearson has also revealed that he is HIV positive and is aware that the deadly virus can be transmitted through breastfeeding.
“I am HIV+, continuously controlled for 18.5 years now,” said Pearson in a Reddit post six months ago. “The viral suppression into undetectability [sic] makes sexual transmission impossible. But transmission through milk IS possible if viral load becomes detectable so I will test viral load monthly (opposed to semiannually) to keep a VERY close eye on that.”
In a shocking display of further disregard for the child’s health, Pearson speculated as to whether his experiment would qualify him as a candidate for the participation in academic research.
“Fortunately, Dr Lenore Goldfarb, creator of the protocol, has her clinic at the same hospital we birthed our baby in. I may even end up in the medical literature.” While again discussing his HIV status in relation to ‘breastfeeding’ a child, Pearson alleges that his case is being documented by infectious diseases researcher Dr. Marina Klein, who is affiliated with McGill University.

Pearson in a “before” picture posted to Reddit tracking his transitioning progress.
Reduxx reached out to Dr. Klein to request information on her involvement in Pearson’s experimental lactation, and she confirmed that she had been monitoring Pearson for his HIV infection at the Chronic Viral Illness Service of the McGill University Health Centre. However, she stated she had not been involved in his transition nor had she been consulted on his induction of lactation.
“It’s important to emphasize that we do not recommend breast feeding for people with HIV as this is the only way to be certain that no HIV transmission will occur after a baby is born,” Dr. Klein said in her response. “However, guidelines have evolved over time with the recognition that the risk of transmission is very low when HIV infection is undetectable with effective therapy … If, after informed discussion, a person expresses a wish to breastfeed they may chose to do so provided they are willing to follow a close protocol of viral monitoring and have their baby followed closely with pediatric specialists who would generally recommend that they receive preventive medication.”
Dr. Klein further states that Pearson had expressed a desire to breastfeed and then had been referred to an endocrinologist.
Prior to identifying as transgender, Pearson was involved in politically advocating for the US-based, anti-feminist men’s rights non-profit A Voice for Men (AVFM).
The organization was founded in 2009 by Paul Elam, who has said that there would no longer be “any place to hide on the internet” for “lying bitches,” and members associated with the group have previously published personal information about women who opposed their activities.
Pearson has linked to the organization’s website on his YouTube channel biography, where he has uploaded videos of himself advocating positions held by AVFM, such as accusing women of lying about sexual violence.

In one video shared in July 2013, titled “Rape, Posters, Traffic Lights and Consent,” Pearson claims that he was previously drugged and raped by a woman on the University of Alberta campus.
He also encourages discussion of posters produced by Men’s Rights Edmonton which featured the headline, ‘Don’t Be That Girl’, created with the intention of parodying an anti-rape campaign designed by a women’s rape crisis shelter, Sexual Assault Voices of Edmonton (SAVE), which used the slogan, ‘Don’t Be That Guy.’
Pearson has also been active in a Facebook group for “trans lesbians,” a term which labels men who call themselves transgender as same-sex attracted women.

Criticism of Pearson’s claims to be “lactating” and “breastfeeding” have focused on concerns that he is “motivated… to experience sexual arousal from lactation,” as one X user, Lulu Solomon, said.
“Because it is not motivated by what is best for the baby it’s automatically risky because the baby becomes a prop in the fantasy,” she stated, alongside a photo of Pearson at the Goldfarb clinic.
This is not the first controversy that has involved trans-identified males breastfeeding babies, with a number of recent examples triggering concern over the past year.
Last year, a lactation professional in Australia along with a women’s rights campaigner were warned that they had broken the law after criticizing a trans-identified male who had boasted of breastfeeding his infant. Shortly after, a trans-identified male in the UK dismissed critics of the practice as “transphobes” after he posted images of himself with a baby latched to his nipple.
UPDATE 02/26/24: The article has been updated to include comment received from Dr. Klein.
#Canada#Margaret (Margie) Fancypants is Murray Pearson#A men's rights activist turned TIM#Reddit#TransLater#Hospitals used to give new mothers the option to have a beer to induce lactation until they encouraged actual mothers to not drink at all#Narcissists just hate it when the attention is on other people#Even when the attention is on their wife or girlfriend due to pregnancy#Another man transitioning while his wife is pregnant#The Goldfarb Clinic#montreal#Another man who transed due to autogynephilia#Dr Lenore Goldfarb#Dr. Marina Klein#Chronic Viral Illness Service of the McGill University Health Centre#A Voice for Men (AVFM)#Another abusive man claiming to be the victim of the family court system#Transbian
11 notes
·
View notes
Text
A ‘twisted’ experience: How KY’s abortion bans are depriving pregnant patients of health care
BY ALEX ACQUISTO
On the way to her 20 week ultrasound, Amy English texted her family group chat inviting guesses on her baby’s biological sex.
“Baby boy English muffin!” her father in-in-law texted.
“I thought boy at first but I’m thinking girl now,” her sister-in-law said. “My official guess is a girl :).”
It was December 28. Earlier that morning, Amy, 31, her husband David, and their 20-month-old daughter Annie had celebrated a belated Christmas at their house in Louisville with family visiting from out of state.
Amy and David had planned this pregnancy, and it was, in a way, perfectly timed. Their baby’s due date was five days after Annie’s birthday. Her children would be two years apart almost exactly to the day — a reality Amy was “ecstatic about.”
Sitting in a fluorescent-lit room inside Baptist Health Louisville, Amy looked for familiar shapes on the screen as an ultrasound tech probed her abdomen. Familiar with radiology in her career as a physical therapist, she has a baseline understanding of how to read ultrasounds: gray shapes usually indicate fluid, and bone shows up as white.
Amy remembers seeing her baby’s arms, legs and the curve of its back. But there was no recognizable outline where the skull should be.
“I couldn’t see the top of my baby’s head,” Amy said in an interview with the Herald-Leader. “I kept waiting for the tech to move the probe in a way where we could see what we should be seeing. I could tell she was searching for it, too.”
Amy had also learned in school about anencephaly, a severe fetal birth defect impacting the brain and skull. A lack of folic acid early in pregnancy increases the likelihood of this happening. This possibility flashed in her mind but she quickly batted it down; she’d been taking her prenatal vitamins, rich in folic acid, for months even before discovering she was pregnant.
The tech paused, then spoke.
“What we’re looking for here is an outline of the baby’s head, and right now I’m not really seeing that,” the woman explained before calling in Amy’s longtime OBGYN.
Over the next few minutes, Amy remembers the room blurring as she heard her doctor use the word “acrania,” which is when a fetus matures through pregnancy without ever developing parts of its skull. It can spur anencephaly, when the brain, too, is underdeveloped and partially missing. Pregnancies with either of these conditions are nonviable.
Amy’s baby, which they learned was a boy, had both. He would not survive into childhood, likely not beyond a few minutes after birth.
This, alone, was devastating news. Her dismay was compounded the next day when she learned that terminating her nonviable pregnancy, even by way of an early induction — a commonplace and provider-recommended method of treatment for such a diagnosis — couldn’t happen.
Even though Amy’s baby would never survive outside her womb, the pregnancy still had a fetal heartbeat — a technicality, considering the diagnosis. Coupled with the lack of immediate threat to her health, her doctors explained they couldn’t induce labor, much less give her an abortion. Kentucky laws forbade it, they said.
“I don’t know what was more shocking: to find out the baby had anencephaly, or that I would have to go out of state to get this care,” Amy said.
Kentucky’s abortion bans do not legally permit the standard of care treatment for a nonviable pregnancy like Amy’s. As a result, doctors must refer patients needing otherwise medically-recommended terminations out of state in droves, along with people desiring elective abortions, according to interviews with seven providers across four hospital systems. Providers who terminate pregnancies in violation of the trigger law can be charged with a felony in Kentucky.
Though this scenario is increasingly common statewide, it’s one arbiters of the state’s laws have yet to remedy, and one lawmakers are not publicly working to resolve.
Kentucky’s trigger law, enacted in late June 2022, criminalizes abortion except to prevent a “substantial risk of death,” or to “prevent the serious, permanent impairment of a life-sustaining organ of a pregnant woman.” The fetal heartbeat law also includes these exceptions but otherwise bans abortion except in a “medical emergency” once fetal cardiac activity begins, usually around six weeks.
Any time a pregnancy is terminated, each law requires a provider to document in writing why it was necessary to, in the case of the six-week ban, “prevent the death of the pregnant woman or to prevent a serious risk of the substantial and irreversible impairment of a major bodily function of the pregnant woman.”
The law permits the Cabinet for Health and Family Services to audit any licensed health care facility to make sure its abortion reporting requirements are “in compliance” with the law.
Both bans allow physicians to use their “reasonable medical judgment” when deciding whether pregnancy terminations are medically necessary. But providers interviewed for this story said that guidance is antithetical with the rest of the law’s limits, which only permit terminations in medical emergencies. There are no exceptions for fetal anomalies, or for the gamut of conditions that may make a pregnancy nonviable but don’t pose an immediate or emergent health risk to a pregnant person.
Moreover, the lack of uniform guidance from the state on what’s considered an emergency means definitions across hospitals sometimes vary, the Herald-Leader found. This has created a legal thicket for health care institutions. As a result, the final say on some critical medical decisions affecting pregnant patients is falling not to medical experts, but to hospital attorneys and administrators, who are worried about legality, liability and reputation.
The Herald-Leader asked the University of Kentucky, UofL Health and Baptist Health for insight into how their respective risk management teams and providers are navigating the laws. None responded to multiple questions about respective protocols for deciding when terminations are legally defensible, or how risk management teams, administrators and providers go about deciding.
“Clinicians have a responsibility to provide compassionate, evidence-based care and counsel to their patients, and also comply with the law,” Baptist said in a statement.
“UofL Health is committed to provide comprehensive health care to all its patients and their families,” UofL said in a statement. “In the case of a nonviable pregnancy that poses a health risk to the mother, we explain options for care while complying with all state and federal laws.”
“Although we cannot discuss when or how our legal counsel gives advice,” UK HealthCare said, “in Kentucky, state law prohibits the University’s physicians and staff from performing abortions except when the mother’s life is in danger. In the case of a nonviable pregnancy, our health care staff work with patients to determine the best course of care for the patient that is consistent with state and federal law.”
‘WE COULD NOT PROVIDE THIS SERVICE HERE’
The morning after Amy learned her baby likely had a fatal birth defect, the diagnosis was confirmed at a second ultrasound with a high-risk specialist. The buoyancy and excitement of the prior day was replaced with dread and grief. Amy remembers the quietness of the room during the second ultrasound, the hollow clicking of the keyboard keys and the intermittent clicking of the computer mouse.
Baptist Health refused to make Amy’s doctor available for an interview. But their conversation was outlined in Amy’s medical records, which were provided to the Herald-Leader.
“I discussed this finding with the patient and offered my sincerest condolences — that this was not compatible with life and that I am so sorry she and her husband are in this situation,” the doctor wrote in her notes. “She was understandably tearful.”
Amy listened as her provider explained her two options: Amy could carry her son to term and deliver him via C-section. He would immediately be taken to palliative care, where he would live a few minutes, maybe hours. Grief counselors would be on standby.
Her second option was to terminate the pregnancy early by way of an abortion or preterm induction. “Choosing not to continue the pregnancy: we discussed that this is also a loving choice for a baby that will certainly not survive,” her doctor wrote.
Pre-trigger law, termination under these circumstances would’ve happened in a hospital, and Amy’s health insurance likely would’ve covered it.
“No part of me wanted to be pregnant anymore,” Amy said. “Every flutter and kick he gave felt like a literal gut punch reminder that I would never get to take him home.”
Strangers were already approaching her at the grocery to ask to touch her stomach. Her patients at work often asked how far along she was. It seemed emotionally unthinkable to continue subjecting herself to a life where, at any moment, she would be forced to repeat that her growing body was nurturing a baby that wouldn’t live, she said.
Termination was what Amy wanted. She erupted into sobs when her doctor told her that under her current circumstances (her life wasn’t immediately threatened, and there was still a fetal heartbeat) it wasn’t an option.
“We discussed that due to our current Kentucky laws, we could not provide this service here,” her doctor wrote in her records.
“I’m sorry, I’m sorry, I’m so sorry,” Amy remembers the specialist saying.
She gave Amy a list of hospitals and clinics in surrounding states that might be able to terminate her pregnancy. Her doctor recommended calling Northwestern Memorial Hospital in Chicago, or another clinic in Illinois, where abortion is widely available.
“Am I just supposed to Google the number, call the front desk and ask, ‘How do I get an abortion at your hospital?’” Amy remembered thinking.
Over the next few days, she, her husband and sister-in-law cold-called a handful of clinics to request a dilation and evacuation abortion, common in the second trimester. But a combination of abortion restrictions in Indiana and Ohio, including gestational limits on when abortion is legal — Amy was 21 weeks along at this point — left her with few options.
Then, Amy’s sister, a nurse anesthetist at Northwestern Medicine Kishwaukee Hospital in Dekalb, west of Chicago, stepped in. Her hospital lacked the equipment for a D&E, but they agreed to induce Amy.
On January 4, after driving close to 400 miles, Amy was induced and gave birth to a son she and her husband named Solomon Matthew. He didn’t cry. His heart beat for about two minutes before it stopped.
‘NOT KNOWING WHAT TO DO’
The Republican-led General Assembly has made no moves to amend or further clarify either abortion ban since both took effect seven months ago, even though the combined impact has harmed patients, doctors have told lawmakers.
The Kentucky Supreme Court still hasn’t issued a preliminary opinion on whether either law infringes on a person’s constitutional right to bodily autonomy and self-determination. Deciding so would temporarily block one or both bans from being enforced. Convened for a regular session through March, the Republican supermajority has yet to file any bills related to reproductive health care access and likely won’t until the high court weighs in.
In the meantime, there’s disagreement about whether or not either ban infringes on providers’ ability to dole out the standard level of care to pregnant patients.
Kentucky Supreme Court Justice Michelle Keller and former Deputy Chief Justice Lisabeth Hughes raised this point during November oral arguments in the pending court case from the state’s two outpatient abortion clinics challenging the constitutionality of both laws.
The trigger law “doesn’t recognize an exception for women who are under the care of a physician who tells them that the standard of care would be to terminate the pregnancy,” Hughes told Solicitor General Matt Kuhn, arguing on behalf of the Attorney General’s office.
As a result, “What’s really happening is physicians in (hospitals) all over the commonwealth are calling the risk managers and attorneys for the hospitals not knowing what to do,” Keller added. “You’re obfuscating what this trigger statute says. There isn’t a strict life of the mother exception.”
The law’s proponents, including Republican Attorney General Daniel Cameron, have cited the provision in the law that allows for use of “reasonable medical judgment” as protecting doctors’ autonomy, and that any challenge to that fact is overblown.
“The law has an explicit health exception, (which) depends on a ‘reasonable medical judgment’ from physicians,” Kuhn told Kentucky Supreme Court Justices that day. There’s been “a lot of misinformation” suggesting the law doesn’t adequately protect a pregnant person’s health, he said, citing two advisories Cameron’s office has issued since both measures took effect. Both clarify that in vitro fertilization, and abortions as treatment of miscarriages, preeclampsia and ectopic pregnancies don’t violate the law.
As for the host of other conditions not mentioned, “we are continuing to work with Kentucky doctors giving guidance on that,” Kuhn said.
But no written evidence of that guidance appears to exist. In response to an open records request from the Herald-Leader, Cameron’s office said this week it had no written or electronic records of communication between the Attorney General’s office and licensed health care facilities or providers regarding the trigger law or six week ban.
‘AN UNNECESSARY PHYSICAL AND PSYCHOLOGICAL RISK’
It was mid June when Leah Martin, 35, discovered she was pregnant with her second child.
Pregnancy at ages 35 and above is considered geriatric. Aware that her age meant she faced a heightened risk, she opted for genetic testing early on to gauge any abnormalities.
Her first ultrasound didn’t raise any alarm. At just over nine weeks, Leah took a prenatal genetic test. The results a week later showed “low fetal fractal numbers,” she said in an interview.
That result, her OBGYN told her, could mean there hadn’t been enough material collected to show a clearer result. It could also signal an abnormality.
Leah, wanting to be judicious, got a more exact genetic test just before 12 weeks. She quickly learned her fetus had triploidy, a rare condition that causes the development of 69 chromosomes per cell instead of the regular 46. It causes not only severe physical deformities, but triploidy stunts development of crucial organs, like the lungs and heart. It means a fetus, if it even survives to birth, will likely not live beyond a few days.
What’s more, Leah was also diagnosed with a partial molar pregnancy, which causes atypical cells to grow in the uterus and, as Leah’s doctors told her, could lead to cancer.
It was mid-July, and Kentucky’s trigger law and six week ban had been in effect for barely two weeks. Leah was familiar enough with what both laws restricted and assumed that because her pregnancy could cause her cancer and was nonviable, she would lawfully qualify as an exception.
So, she weighed her options with her doctors at Baptist Health Lexington, who included Dr. Blake Bradley, her longtime OBGYN.
Similar to Amy’s diagnosis, Leah’s doctors told her that even if she opted to carry the pregnancy to term, her baby “would live a short life in palliative care, most likely never leaving the hospital. It would really be a quite painful existence,” she said.
“I have a 2-year-old at home, and I’m 35, weighing how I would like to expand my family. It seemed like the safest option for me and the compassionate choice for my unborn child was to terminate the pregnancy,” she said.
Like Amy’s, a medically-necessary abortion under these circumstances would typically take place at a hospital, doctors interviewed for this story said. Leah’s health insurance had already agreed to cover it. It was also the quickest way to help Leah to her end goal: getting pregnant again in order to birth a child that would survive.
It was July 21 and Leah was just over 12 weeks pregnant when she learned that Baptist’s legal counsel had blocked her doctors from giving her a dilation and curettage abortion.
“I was told the hospital refused to perform the procedure while the case was being litigated. I was dumbfounded,” Leah said. Hospital lawyers cited an ongoing lawsuit from Kentucky’s two outpatient abortion providers that’s pending before the Kentucky Supreme Court.
According to Leah, hospital providers, relaying the message from administration and risk management, reportedly said if her fetus died on its own, doctors would be able to terminate her pregnancy. But their hands were tied as long as it had a heartbeat.
“People minimize that pregnancy, even under its best circumstances, is associated with life-threatening risks, life-altering risks and emotional impacts,” Bradley told the Herald-Leader. “So, to compel a woman to continue a pregnancy that is by everyone’s assessment, doomed, by definition places that woman at an unreasonable and unnecessary physical and psychological risk, period.”
Baptist Health refused to make Leah’s high-risk doctor available for an interview.
The following Monday, July 25, Leah had an ultrasound at the hospital to confirm what she already knew. As an ultrasound tech probed her abdomen, a wheel of dizzying emotions spun in her head: she desperately wanted a baby, but she didn’t want to birth a child into a painful existence.
Already faced with a gutting dilemma, she felt further burdened by having such an intimate choice ripped from her. And she was furious at now being forced to remain pregnant despite there being no chance for survival, despite the risks continuing such a pregnancy posed to her own body.
She remembers staring at the ultrasound screen waiting to hear the muffled heartbeat of her fetus, racked with guilt because she hoped she wouldn’t.
“It was such a twisted experience being pregnant with a baby I desperately wanted, lying there hoping its heart had stopped,” she said shakily. “It was horrible to have to wish for that in order to receive care. It just felt so unsafe and cruel.”
Leah had already arranged to drive to Chicago to get an abortion when a Jefferson Circuit judge issued a preliminary injunction on July 22, temporarily blocking the state from enforcing both bans. She immediately called EMW Women’s Surgical Center in Louisville — one of the plaintiffs in the lawsuit against the state — and made an appointment.
On Wednesday, July 27, almost 13 weeks pregnant, Leah paid $950 out of pocket for her abortion. Her insurance wouldn’t cover it, since it was considered elective. The following Monday, the Kentucky Court of Appeals overturned the circuit court injunction, reinstating both abortion bans.
After Leah’s abortion, she sent a message to her high-risk doctor. Her doctor responded the following day. Leah shared that correspondence with the Herald-Leader.
“You’ve been on my thoughts a lot,” her doctor wrote. “Words cannot express the dismay I feel right now. I’ve spent my whole adult life learning how to care for mothers in heart wrenching or dangerous situations like yours, and the politics now make it not only impossible, but to work to take care of patients like they deserve — with compassion and science — in these horrible situations is wrong and immoral.”
“I hope your procedure yesterday was smooth, though I know it was hard,” her doctor wrote. “I’m so sorry we could not (were not allowed, rather) to take care of you here.”
#us politics#news#Kentucky Herald-Leader#2023#abortions#Abortion bans#anencephaly#acrania#nonviable pregnancies#kentucky#fetal heartbeat laws#Cabinet for Health and Family Services#dilation and evacuation abortions#Kentucky Supreme Court#Daniel Cameron#triploidy#palliative care#dilation and curettage abortions#Kentucky Court of Appeals#reproductive rights#bodily autonomy
68 notes
·
View notes
Text


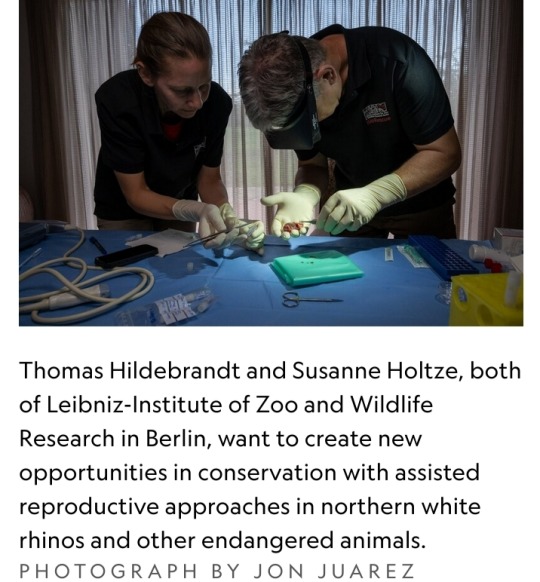
By Dina Fine Maron
January 24, 2024
Scientists have cleared a significant hurdle in the years-long effort to save Africa’s northern white rhinoceros from extinction with the first-ever rhino pregnancy using in vitro fertilization.
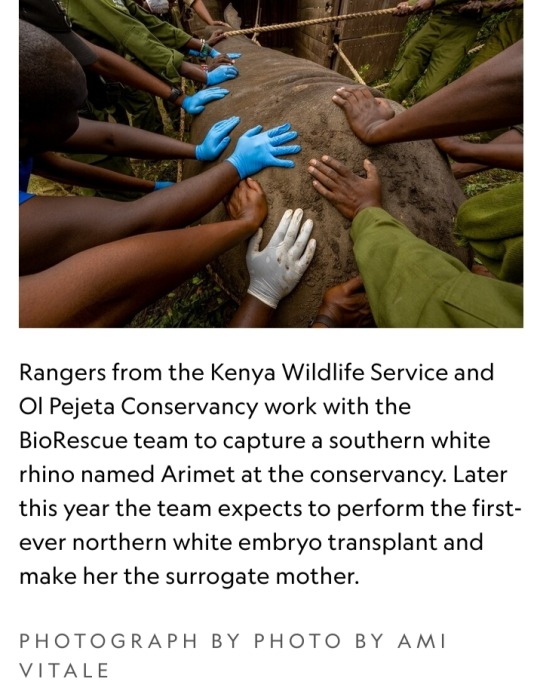
The lab-assisted pregnancy, which researchers will announce today, involved implanting a southern white rhino embryo in a surrogate mother named Curra.
The advance provides the essential “proof of concept” that this strategy could help other rhinos, says Jan Stejskal of the BioRescue project, the international group of scientists leading this research.
Curra died just a couple months into her 16-month pregnancy from an unrelated bacterial infection, Stejskal says.
However, the successful embryo transfer and early stages of pregnancy pave the way for next applying the technique to the critically endangered northern white rhino.
The process was documented exclusively by National Geographic for an upcoming Explorer special currently slated to air in 2025 on Nat Geo and Disney+.
BioRescue expects to soon implant a northern white rhino embryo into a southern white rhino surrogate mother.
The two subspecies are similar enough, according to the researchers, that the embryo will be likely to develop.
Eventually, this approach may also help other critically endangered rhinos, including the Asian Javan rhinoceros and the Sumatran rhinoceros, which each now number under 100 individuals, Stejskal says.
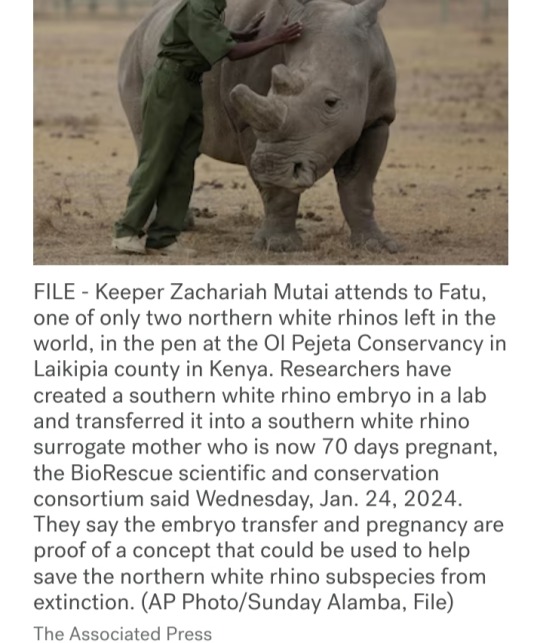
But the northern white rhino’s current situation is the most pressing by far.
There are no males left, and the only two remaining animals are both elderly females that live under armed guard on a reserve in a 700-acre enclosure in Kenya called Ol Pejeta Conservancy.
The boxy-jawed animals once roamed across central Africa, but in recent decades, their numbers have plummeted due to the overwhelming international demand for their horn, a substance used for unproved medicinal applications and carvings.
Made from the same substance as fingernails, rhino horn is in demand from all species, yet the northern white rhino has been particularly hard-hit.
"These rhinos look prehistoric, and they had survived for millions of years, but they couldn’t survive us,” says Ami Vitale, a National Geographic Explorer and photographer who has been documenting scientists’ efforts to help the animals since 2009.
“If there is some hope of recovery within the northern white rhino gene pool — even though it’s a substantially smaller sample of what there was — we haven’t lost them,” says conservation ecologist David Balfour, who chairs the International Union for the Conservation of Nature’s African rhino specialist group.
Blueprints for rhino babies

To stave off the animal’s disappearance, BioRescue has used preserved sperm from northern white rhinos and eggs removed from the younger of the two remaining females.
So far, they’ve created about 30 preserved embryos, says Thomas Hildebrandt, the head scientist of BioRescue and an expert in wildlife reproduction based at the Leibniz-Institute of Zoo and Wildlife Research in Berlin.
Eventually, the team plans to reintroduce northern white rhinos into the wild within their range countries.
“That’d be fantastic, but really, really far from now—decades from now,” says Stejskal.
Worldwide, there are five species of rhinoceros, and many are in trouble.
Across all of Africa, there are now only about 23,000 of the animals, and almost 17,000 of them are southern whites.
Then there are more than 6,000 black rhinos, which are slightly smaller animals whose three subspecies are critically endangered.
In Asia, beyond the critically endangered Javan and Sumatran rhinos, there’s also the greater one-horned rhino, whose numbers are increasing and currently are estimated to be around 2,000.
The BioRescue effort has experienced many setbacks, and even though the team now has frozen embryos, the clock is ticking.
The researchers intend to use southern white rhinos as surrogate moms for the northern white rhino embryos.
However, scientists want any northern white rhino calves to meet and learn from others of their kind, which means they need to be born before the two remaining females die.
“These animals learn behaviors — they don’t have them genetically hard-wired,” says Balfour, who’s not involved with the BioRescue work.
But birthing new animals in time will be a challenge.
“We’re really skating on the edge of what’s possible,” he says, “but it’s worth trying.”
Najin, the older female, will be 35 this year, and Fatu will be 24.
The animals, which were born in a zoo in the Czech Republic, are expected to live to about 40, says Stejskal, who also serves as director of international projects at the Safari Park Dvůr Králové, the zoo where the animals lived until they were brought to Kenya in 2009.
Impregnating a rhino
The next phase of BioRescue’s plan involves implanting one of their limited number of northern white rhino embryos into a southern white rhino surrogate mother — which the group plans to do within the next six months, Stejskal says.
They’ve identified the next surrogate mother and set up precautions to protect her from bacterial infections, including a new enclosure and protocols about disinfecting workers’ boots.
But now, they must wait until the female rhino is in estrus — the period when the animal is ready to mate — to implant the egg.
To identify that prime fertile time, they can’t readily perform regular ultrasounds at the conservancy as they might do in a zoo.
Instead, they have enlisted a rhino bull that has been sterilized to act as a “teaser” for the female, Hildebrandt says, adding that they must wait a few months to make sure that their recently sterilized male is truly free of residual sperm.
Once the animals are brought together, their couplings will alert conservancy staff that the timing is right for reproductive success.
The sex act is also important because it sets off an essential chain of events in the female’s body that boosts the chances of success when they surgically implant the embryo about a week later.
"There’s little chance the conservancy staff will miss the act. White rhinos typically mate for 90 minutes," Hildebrandt says.
What’s more, while mounted on the females, the males often use their temporary height to reach tasty plant snacks that are generally out of reach.
Boosting genetic diversity
With so few northern white rhinos left, their genetic viability may seem uncertain.
But the BioRescue team points to southern white rhinos, whose numbers likely dropped to less than 100, and perhaps even as few as 20, due to hunting in the late 1800s.
Government protections and intense conservation strategies allowed them to bounce back, and now there are almost 17,000.
“They have sufficient diversity to cope with a wide range of conditions,” says Balfour.
Researchers don’t know exactly how many southern white rhinos existed a century ago, he says, but it’s clear that the animals came back from an incredibly low population count and that they now appear healthy.
Beyond their small collection of embryos, the BioRescue team hopes to expand the northern white rhino’s gene pool by drawing from an unconventional source — skin cells extracted from preserved tissue samples that are currently stored at zoos.
They aim to use stem cell techniques to reengineer those cells and develop them into sex cells, building off similar work in lab mice.
According to their plan, those lab-engineered sex cells would then be combined with natural sperm and eggs to make embryos, and from there, the embryos would be implanted into southern white rhino surrogate mothers.
Such stem cell reprogramming work has previously led to healthy offspring in lab mice, Hildebrandt says, but rhinos aren’t as well-studied and understood as mice, making this work significantly challenging.
A global effort
The northern white rhino revitalization venture has cost millions of dollars, supported by a range of public and private donors, including the German Federal Ministry of Education and Research.
Other partners on the effort include the Leibniz Institute for Zoo and Wildlife Research, the Czech Republic’s Safari Park, Kenya Wildlife Service, Ol Pejeta Conservancy, and also Katsuhiko Hayashi, a professor of genome biology at Osaka University in Japan who conducted the mouse stem cell research.
Building upon Hayashi’s stem cell techniques could ultimately bring the northern white rhino gene pool up to 12 animals — including eggs from eight females and the semen of four bulls, according to Stejskal.
An alternative approach to making more babies, like crossbreeding northern and southern white rhinos, would mean the resulting calves wouldn’t be genetically pure northern white rhinos, Hildebrandt notes.
The two subspecies look quite similar, but the northern version has subtle physical differences, including hairier ears and feet that are better suited to its swampy habitat.
The two animals also have different genes that may provide disease resiliency or other benefits, Hildebrandt says.
There are unknown potential differences in behavior and ecological impact when populating the area with southern white rhinos or cross-bred animals.
"The northern white rhino is on the brink of extinction really only due to human greed,” Stejskal says.
“We are in a situation where saving them is at our fingertips, so I think we have a responsibility to try.”
🩶🦏🩶
#northern white rhinoceros#rhino embryo transfer#in vitro fertilization#IVF#southern white rhinoceros#critically endangered animals#National Geographic#BioRescue#rhino horn#International Union for the Conservation of Nature#African rhino specialist group#Thomas Hildebrandt#German Federal Ministry of Education and Research#Leibniz Institute for Zoo and Wildlife Research#Kenya Wildlife Service#Ol Pejeta Conservancy#Katsuhiko Hayashi#genome biology#IVF rhino pregnancy
8 notes
·
View notes
Note
hello coming in here after some time and curious about what your favorite fantasy to think about is right now. pregnancy related, expansion related, or whatever little thing brings you kinky joy to think about August i must know
Aw heck thank you Gabe! Oh my gosh one that has me in an absolute chokehold lately is Friars and priests getting ridiculously knocked up by demons. I love the idea of the being like, tempted and seduced by demons to the point where they willingly let the demons knock them up. Then coupling that up with them trying to conceal a pregnancy among their community, ooh, or maybe doing a thing where nobody can see it but them. Either way, love the idea of the demon occasionally visiting them to taunt them with what their own "sinful lust" has gotten them into, and to fuck them silly
Double bonus points if the friar starts exhibiting lil demonic attributes like tiny horns or a forked tail as their pregnancy progresses!
#pregnancy kink#preg kink#mpreg#mpreg kink#demon voice what if you went into labor during service wouldnt that be hot
24 notes
·
View notes
Text
atsumus the type of menace to insist on doing it raw, flee during the pregnancy scare… come back and insist on it raw again
#rinse and repeat#tw pregnancy#remi.rambles#oh ur late ? how convenient that he’s going on a two week camping trip w no cell service
71 notes
·
View notes
Text
11 Ways To Manage Pain in Childbirth
Are you scared of childbirth? Worried about how your body will manage? Well, our bodies are built to give birth, and if we follow the right steps, we can significantly minimize the pain during labour. Butterbean brings you 11 highly effective ways to manage pain in childbirth and welcomes your little one into this beautiful world.

1 note
·
View note
Text
me, elbow deep in a commercial bag of mozzarella cheese bc we ran out halfway through the dinner rush: call that an emergency cheese section
the customer waiting on their pizza:

#pov the gayest person you’ve seen all day says this#90% sure my manager heard me say this#but he didnt say anything lol#if yall cant tell i think im funny#pregnancy cw#i think idk really know#work life#food service
14 notes
·
View notes
Text
Birth Doulas: Empowering Support for Expectant Families
Shaina Tranquilino
December 12, 2023

Bringing a new life into the world is an incredible journey filled with joy, anticipation, and sometimes, uncertainty. During this transformative time, many women seek additional support to ensure a positive birth experience. Enter birth doulas – compassionate professionals who provide continuous physical, emotional, and informational assistance before, during, and after childbirth. In this blog post, we will delve into what birth doulas are and explore their invaluable role in empowering expectant mothers.
Understanding Birth Doulas:
A birth doula is a trained individual who offers non-medical support to expectant mothers throughout the entire childbirth process. These dedicated individuals are typically experienced in various birthing techniques and possess extensive knowledge of the physiological and emotional aspects of labour and delivery.
Their Role:
1. Emotional Support:
Birth doulas provide unwavering emotional support during pregnancy, labour, and postpartum periods. They assist expectant mothers by actively listening to their concerns, fears, hopes, and dreams surrounding childbirth. By offering empathy and reassurance, these caring professionals help alleviate anxieties while fostering confidence.
2. Continuous Physical Comfort:
Doulas employ an array of comfort measures to ease discomforts associated with labour pains such as massage techniques, breathing exercises, relaxation techniques, positioning suggestions, and more. Their presence ensures that the mother's physical needs are addressed consistently throughout the birthing process.
3. Advocacy & Communication:
One significant aspect of a birth doula's role is to act as an advocate for the mother's preferences and desires when communicating with healthcare providers or medical staff. This may include discussing pain management options or ensuring the mother has access to accurate information about procedures being performed.
4. Informational Support:
Birth doulas empower expectant mothers by providing evidence-based information on various aspects of childbirth like different birthing positions or breastfeeding techniques. They ensure that the mother is well-informed, enabling her to make educated decisions regarding her birth plan.
5. Partner Support:
Birth doulas also extend their support to partners or other family members involved in the birthing process. By guiding them on how best to assist and comfort the labouring mother, doulas help create a harmonious environment where everyone feels included and informed.
Benefits of Hiring a Birth Doula:
The advantages of having a birth doula during childbirth are numerous:
1. Increased Satisfaction: Studies have shown that women who receive continuous support from a birth doula report higher levels of satisfaction with their birthing experience.
2. Reduced Interventions: Research indicates that with the presence of a doula, there is often a decrease in interventions like cesarean sections and epidurals, leading to more positive outcomes for both mother and baby.
3. Emotional Well-being: The emotional support provided by birth doulas significantly reduces stress levels for expectant mothers, promoting overall emotional well-being throughout pregnancy and beyond.
4. Lowered Risk of Postpartum Depression: Women supported by birth doulas tend to have lower rates of postpartum depression due to the consistent guidance and nurturing they receive during the vulnerable post-birth period.
Birth doulas play an essential role in ensuring positive experiences for expectant mothers during childbirth. Their unwavering support, knowledge, and advocacy empower women to navigate this transformative journey confidently. By providing physical comfort, emotional reassurance, informational assistance, and acting as an advocate, these dedicated professionals contribute significantly to creating fulfilling and empowering birthing experiences for all involved.
#birth doulas#doula#doula support#pregnancy companion#empowered birth#maternal care#birth journey#supportive doula#birth preparation#labour and delivery#holistic birth#childbirth support#doula services#pregnancy wellness#labour coach#empowered motherhood#maternal health#birth experience#doula love#birth advocate
4 notes
·
View notes
Text
confidently Perform Accurate, Efficient, and Effective Physical Examinations. Master the techniques for successful physical examinations with the #1 choice for complete, authoritative guidance. This highly regarded text includes fully illustrated, step-by-step techniques that outline the correct performance of the physical examination and an easy-to-follow two-column format that correlates examination techniques on the left and abnormalities (clearly indicated in red) with differential diagnoses on the right. NEW! Expanded Unit 1 provides an overview of the components of the patient encounter and helps you ensure the most effective information-gathering and decision-making approaches. NEW! Key terms are bolded in chapters and correspond to an online glossary with definitions. UPDATED! Expanded coverage of special populations familiarizes you with important approaches for persons who identify as LGBTQ, persons with physical disabilities, and diverse populations throughout the life cycle. UPDATED! Restructured Regional Exam chapters enhance your understanding of overview material, examination techniques, and health promotion and counseling considerations. UPDATED! Photographs, illustrations, and references reinforce key content based on the latest evidence-based information. UPDATED! Text boxes are numbered to provide quick access to important summaries of clinical conditions and tips for challenging examination techniques. Clinical pearls, printed in blue, highlight key points at a glance. Detailed, highly illustrated tables of abnormal conditions display examination and clinical information in an easy-to-find, quick-reference format at the end of each chapter. eBook available. Fast, smart, and convenient, today s eBooks can transform learning. These interactive, fully searchable tools offer 24/7 access on multiple devices, the ability to highlight and share notes, and much more.35 MB
#testing#syndrome#pulmonary#preventive services#prevention#pregnancy#posterior#peripheral#palpation#ora#nodes#nerve#murmurs#medical#live#lateral#infection#infants#hypertension#guidelines#factors#diagnostic#diagnosis#diabetes#counseling#clinicians#chronic#cervical#cardiovascular#associated
2 notes
·
View notes
Text

I enjoy being knocked up pregnant way too much
#personal#living my best cottagecore life#my dress and apron are giving me ghibli vibes#my husband is a baker irl#I’m totally the bakers wife in Kiki’s delivery service#👀#pregnant#pregnancy#cottagecore#24 weeks pregnant#6 months pregnant
9 notes
·
View notes
Text
“One looked at non-masculinizing dose of testosterone given for depressive symptoms, and two involved masculinizing doses of testosterone given to trans-identifying females as a part of ‘gender affirming’ regimen. In all these studies, either the sex and age of the infant wasn’t noted, or the age of infant was over one years old, or the sex of the infant was male. Therefore we have no long-term data on how this practice would specifically effect female infants, and the evidence of safety in male infants cannot be said to be adequate.”
By Reduxx Team. October 12, 2023
The National Health Service of the United Kingdom is advising “transgender” females who take testosterone to continue doing so even while breastfeeding a baby despite acknowledging the unknown risks the hormone may have to the child.
The worrying guidance was first called to attention by users on social media, prompting a wave of backlash from advocates concerned with women’s rights and child safeguarding.
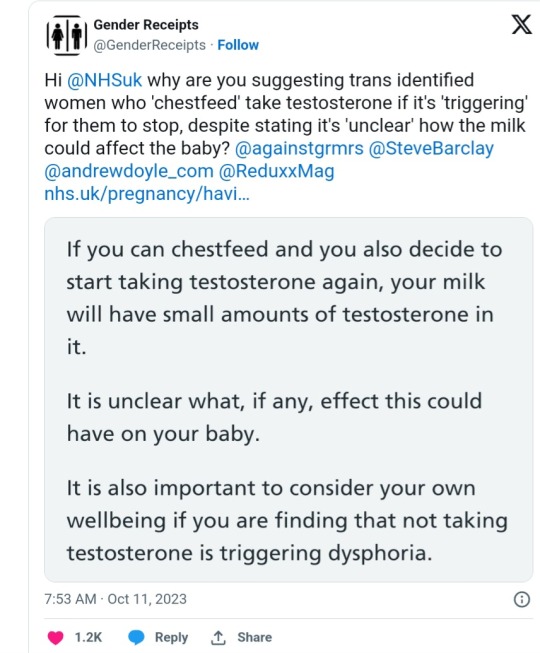
In a screenshot from the page posted by @GenderReceipts to X (formerly Twitter), the NHS states: “If you have taken testosterone in the past then your milk supply may be affected. So you may not be able to chestfeed your baby,” but continues that if “chestfeeding” is possible while on testosterone, the milk may have trace amounts of the hormone in it.
@GenderReceipts also posted a link to the page, titled Testosterone and Pregnancy, and asked why the NHS would suggest “trans-identified women who ‘chestfeed’ take testosterone” if the impacts on the child’s health were unknown.
“It is unclear what, if any, effect this could have on your baby,” the guidance read. “It is also important to consider your own wellbeing if you are finding that not taking testosterone is triggering dysphoria.”
Speaking to Reduxx, retired family physician Dr. Maja Bowen condemned the NHS for what she labeled an “alarming” guidance.
“There’s a paucity of research into the effects of elevated maternal testosterone on breast milk and breastfed infants,” Dr. Bowen said, noting the existence of three available studies which analyzed the issue of maternal testosterone usage.
“One looked at non-masculinizing dose of testosterone given for depressive symptoms, and two involved masculinizing doses of testosterone given to trans-identifying females as a part of ‘gender affirming’ regimen. In all these studies, either the sex and age of the infant wasn’t noted, or the age of infant was over one years old, or the sex of the infant was male. Therefore we have no long-term data on how this practice would specifically effect female infants, and the evidence of safety in male infants cannot be said to be adequate.”
Dr. Bowen also points out the apparent contrast between the guidance given to trans-identified females, noting how pregnant women and nursing mothers are often inundated with warnings about avoiding certain medication, food, and drink deemed risky.
“In medicine, we always err on the side of caution when we are advising mothers about which medicines are safe to take during pregnancy or lactation. However, the evidence for safety of masculinizing doses of testosterone on breastfed babies of trans-identifying females is inadequate. Therefore, I am alarmed that the NHS is putting the wishes of trans-identifying adults to be ‘affirmed in their chosen gender’ above the safety of children.”
This is not the first time concerns have been raised about official guidance on transgender adults breastfeeding children, though many previous issues have surrounded the phenomenon of trans-identified males inducing lactation for the purposes of “gender affirmation.”
As early as 2018, an endocrinologist from Boston Medical Center claimed that breastfeeding was an important method of validating a trans-identified male’s gender identity.
In an interview with The New Scientist, Dr. Joshua Safer said: “Many transgender women are looking to have as many of the experiences of non-transgender women as they can, so I can see this will be extremely popular.”
Since then, reports of trans-identified males seeking support from lactation consultants have increased. On social media, many new and breast feeding mothers have also stated they’ve noticed an increase in men attending breast-feeding groups.
As previously reported by Reduxx, two women in Australia received notices from X informing them that they had broken Australian law after posting about a trans-identified male who had been breastfeeding a child.
Issues have also emerged regarding the adoption of “inclusive” language in maternity care, such as utilizing “chestfeeding” in place of “breastfeeding.”
Last year, a collaborative research paper led by Australian academic Karlene Gribble concluded that the adoption of “desexed” language in female-specific healthcare had “serious implications” for women and children.
“Desexing the language of female reproduction has been done with a view to being sensitive to individual needs and as beneficial, kind, and inclusive,” they wrote in the paper. “Yet, this kindness has delivered unintended consequences that have serious implications for women and children.”
Gribble and her team assert that neutralizing the language around motherhood, including “disembodying and undermining breastfeeding,” would result in “reducing protection of the mother-infant [bond]” and the dehumanization of women.
#UK#The National Health Service#Breastfeeding#Breastfeeding and maternal use of drugs#The gender feels of adults are not more important than a babies health#GenderReceipts#Testosterone and pregnancy#This is while normal mothers are hounded with warnings about what to and what not to do during pregnancy and Breastfeeding
2 notes
·
View notes
Text
(also, since im disgruntled, maybe we dont use adoption as a "solution" and pretend that kids arent verrrrrryyy aware when theyre unwanted. and also still makes the issue about 'the children' vs. what its actually about which is bodily autonomy. two things!
greys anatomy does alot of things wrong but one thing it got very right was an argument btween cristina yang and owen. And hunt says " a relationship is about compromise. Cant you just give a little?" And cristina says "you dont give a little on a baby. you dont compromise on a baby.")
#cw: unwanted pregnancy#cw: roe v wade#cw: abortion#we could talk about new wave of mental health crises#or maybe about FEDERAL FUNDING and where money goes because its not towards agencies#nor towards counseling services#or trauma associated with forced birth#but we wont because yall arent ready#we could also talk about how this is a disability rights issue as well#but since were not even being inclusive in our language and using PERSONS instead of women/girls#were not ready to add another layer#also you know. risks associated with pregnancy.
29 notes
·
View notes