#Fungal Medicine
Text
#Maitake Mushrooms#Health Benefits#Immune System Boost#Cholesterol Reduction#Mushroom Nutrition#Medicinal Mushrooms#Immunity Support#Dietary Supplements#Healthy Living#Fungal Medicine#Nutritional Benefits
0 notes
Text
Rhodotorula
“Rhodotorula mucilaginosa cells, methylene blue stain, magnification 400 x, notice the oval yeast cells as well as filamentous structures (pseudohyphae).” - via Wikimedia Commons
#fungi#fungus#microbiology#wikipedia#wikipedia pictures#wikimedia commons#nature#microbes#mycology#medical mycology#medical#medical microbiology#infectious diseases#medicine#methylene blue#methylene blue stain#specimen staining#fungal infection#fungicore#mycologycore#microscope#microscopy#yeast
9 notes
·
View notes
Note
Hii im recently hyperfixated with mushrooms and i want to know if you have information or good pages/authors to read about innovations in the uses of fungi in our everyday life, like for bioremediation.
Love your page! <3
i actually do not have extensive knowledge of fungi in bioremediation, so i unfortunately can't supply any sources for you to read about it. i'd love to learn more, so if any of my followers know of pages / authors that have written on this topic, please send it my way. ^^
#sorry if i am misunderstanding this ask - i have a killer headache. ^^"#if you'd like some information on another specific aspect of using fungi in our everyday life#i can offer knowledge on using them for dyes#food#medicine#fungicides#fuel#& more !!#for some reason i've just got no more knowledge on fungal bioremediation than a quick google search worth.#||#• askbox replies: •#(ask : isapolvorita)
17 notes
·
View notes
Text
i think it's really cool to like mycology as much as i do - it's such a vast field, with so many implications and outreaching effects (both good and bad), and it's very fun to say that I'm interested in EVERYTHING.
#likee yeah I know about fungal diseases and how they decimated the frog population (esp chytridiomycosis)#I know about mycotoxins and that mould scares a lot of people (understandably)#and yeast! Candida auris and its drug resistance#but I'm still interested in them!! all of it :)#it's really funny bc I can't “defend” them like animals - how they don't mean harm to humans‚ we're just there and disturbing their habitat#I admit fungi cause harm lol. no doubt about that: that's how they reproduce#doesn't mean I like them any less though! don't think “like” is the best word to use for this but you get my point#my posts#text#mycology#fungi#told my mum this and she said “you're crossing over to the dark side” well what if I welcome that 👀#isn't it so interesting that some fungal components have medicinal properties and others are the pathogens :]#(probably because some that harm bacteria harm us too)#fungi r like the delicious nuance of the natural world I think. rejecting the binaries. I love that shit
5 notes
·
View notes
Note
Resurrected sparrows learns the hard way that she no longer has the ability to digest uncooked meat like she could as tink.
i mean she used to eat the cleaning slugs raw, p sure that her low circle ass can handle uncooked meat better than a human, yanno
oh, on the way to the Root she would have to eat a shitton of meat cuz Boreas would constantly try to hurry them up and not stop to look for any fruit so when smth inevitably attacks them he'd generally just point at the corpse like "eat that and lets get a move on". they make it to the Root and she's starting to show signs of scurvy and stuff.... (she'd handle scurvy n such better than a human cuz yanno, anemones are carnivorous so she is set for this kinda stuff. the diet just got more rich once the Big Brains started developing, so veggies n fruits r still required)
Euros on his weak ass legs (cuz yes, the boy's puppet is rot infected) goes "h..hey are you hungry, we can go and... hunt?"
and she's like "goodness please that's- you'd get hurt, first of all. second of all, all i've seen since we met with Boreas has been meat, could we... go pick some fruit?"
Sporadic presents a blue fruit all joyfully
Sparrows not noticing her immediately "ideally some real fruit, not bug pupae"
Sporadic deflates defeated
Sparrows notices: "oh wait, no, don't be sad! i'd take the pupae over real meat anytime right now"
Sporadic proceeds to light up again
#Spot says stuff#rw#oc tag#Sporadic n Sparrow would work together often i think... cuz iterator medicine n shit- that fungal blorbo would prolly be Sparrows doctor
15 notes
·
View notes
Note
Hc about Demeter?
Or hm. Macavity
You get both <3
Demeter LOVES nice fabrics like silk, satin, and linen. Her friends and family are always keeping an eye out for scraps she can add to her nest.
Macavity has all sorts of bald spots from itching excessively. Not only is it because he's itchy (fleas, dirt, etc) but he also scratches himself when he's anxious or thinking.
#answering asks#ask games#cats the musical#demeter cats#macavity#macavity cats#yes macavity gets anxious. no he doesnt show it.#demeter learned all his anxious habits when she was with him#also one of my cats had the bald spot thing a while ago because he had a fungal infection:(#luckily he got some medicine and is no longer a fungus boy#headcanons
9 notes
·
View notes
Text
What Is a Fungal Infection?
Fungal Infection Best Treatment In Homeopathy
FunA fungal infection, also called mycosis, is a skin disease caused by a fungus.There are millions of species of fungi. They live in the dirt, on plants, on household surfaces, and on your skin.Sometimes, they can lead to skin problems like rashes or bumps.gal Infection Best Treatment In Homeopathy.
Fungal Infection Symptoms:
Irritation
Scaly skin
Redness
Itching
Swelling
Blisters
Types of skin fungal Infection:
Athlete’s foot: The most common type of fungal infection, this condition often spreads when people walk barefoot in public bathrooms or locker rooms.The skin between your toes turns white and starts to peel. Athlete’s foot can also affect the soles (bottoms) of the feet.
Nail fungus: This infection is a common foot problem.It usually affects the toenails, which become yellow and thick and break easily.
Jock itch: A rash of the groin area, jock itch affects more men than women.
Scalp ringworm: This rash occurs mostly in children. It causes hair loss, but with the right treatment, the hair usually grows back.
Ringworm: This “catch-all” term is what healthcare providers call a rash that doesn’t fit into any other category. The rash often forms a ring shape.

#brahmhomeo#homeopathy#health#patient#medicine#odhav#disease#treatment#ahmedabad#drpradeepkushwaha#fungal infection#fungal diseases
2 notes
·
View notes
Text
Empower Yourself with Ayurvedic Medicine for Fungal Infections

Ayurvedic therapy takes a holistic approach to treating fungal infections by correcting imbalances in the body's Doshas. Fungal infections are caused by a variety of fungi that can harm the skin, nails, and mucous membranes. Ayurvedic treatments aim to restore Dosha balance and eliminate underlying causes using a combination of herbal medicines, dietary changes, lifestyle changes, and detoxification therapies.
To address fungal infections, Ayurveda uses a variety of antifungal and antibacterial herbs. Neem, clove, turmeric, and tea tree oil are often used to eliminate fungus and restore bodily balance. Ayurvedic therapies for various fungal infections include a mixture of neem oil and turmeric for athlete's foot and a paste of crushed cloves and coconut oil for ringworm.
In addition to herbal therapies, Ayurveda emphasizes the importance of lifestyle changes in preventing and treating fungal infections. Good cleanliness practices, breathable clothing, and stress management approaches such as yoga and meditation are encouraged. The Ayurvedic diet also helps in the treatment of fungal diseases. Avoiding sugar and processed carbs is vital since fungi thrive on sugar, and increasing your consumption of antifungal foods can help starve the illness.
0 notes
Text
ASPERGILLOSIS IN DOGS
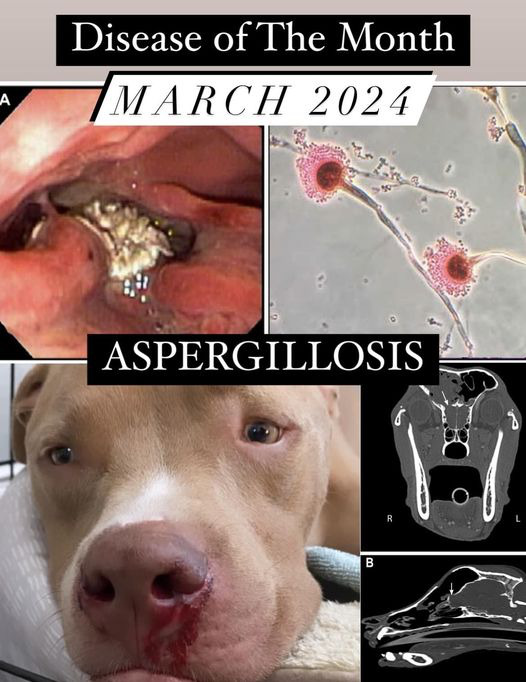
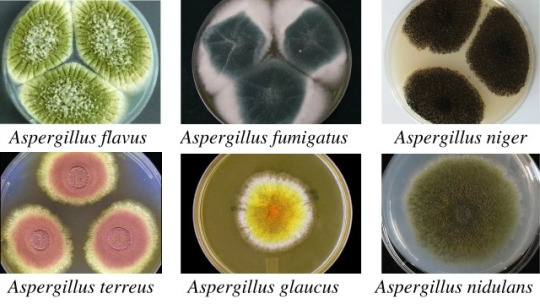
Aspergillosis is a fungal infection caused by a type of mold called Aspergillus. There are over 200 known species of Aspergillus fungi found worldwide that can grow either indoors or outdoors, and are commonly found in soil, dead or decaying vegetation, or spoiled food. They produce tiny asexual spores that can be easily inhaled or ingested, although do not generally lead to disease in humans or animals, unless the host has a compromised immune system or has significant exposure to the fungus.

SINONASAL ASPERGILLOSIS
In dogs, especially dolicocephalic (long-snout) breeds such as the Greyhound, Collie, and Dachshund, aspergillosis is typically localized to the nasal cavity/sinuses. Symptoms of sinonasal aspergillosis include chronic sneezing and bloody nasal discharge, classically from one nostril, and sometimes depigmentation and/or ulceration of the nares.

Mucous will eventually build up into a "fungal ball", or aspillergoma, which can be detected under advanced imaging.
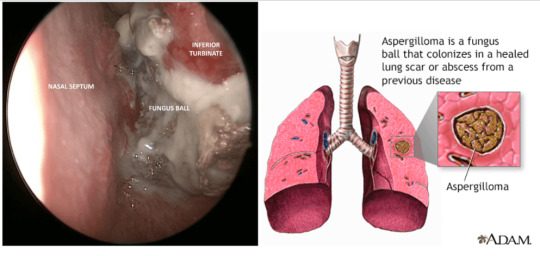
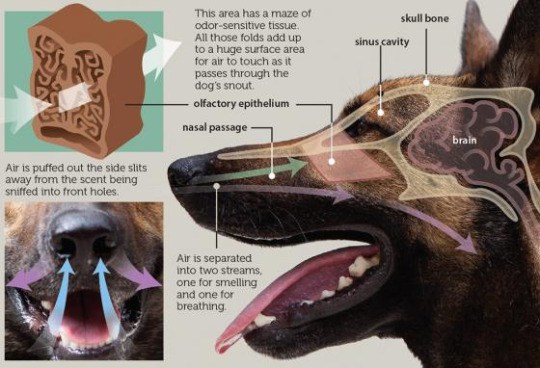
In severe cases, there will be marked damage of the nasal turbinates and the infection spreads from within the sinus cavity through the frontal bone of the skull, invading into the brain and central nervous system. For this reason, CT scan is highly recommended along with a rhinoscopy.
youtube
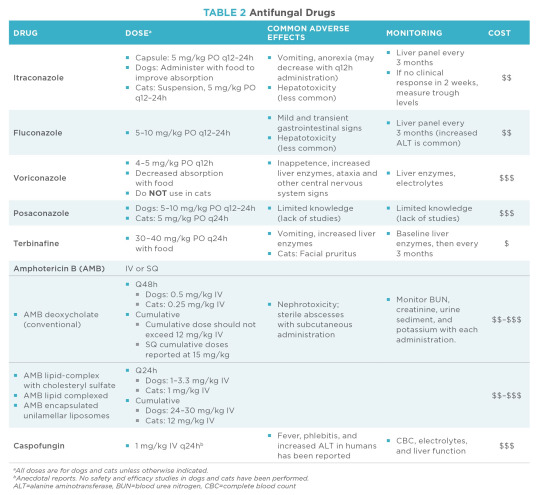
Historically, treating fungal infections with oral medications are very challenging, as the infections are often very slow to clear, and many anti-fungals available on the market are not only expensive, but may have severe side effects including liver damage and neurological symptoms. Because of this, the debridement of fungal lesions followed by topical infusion have become the gold standard treatment, as long as the cribriform plate of the skull is intact.
youtube
While under anesthesia, fungal plaque is removed with the guidance of a scope in the nasal cavity. In some cases, however, fungal plaque may be located in the sinuses but not in the nasal cavity - in which case trephination may be performed. An incision is made along the forehead to remove a layer of bone to create access.

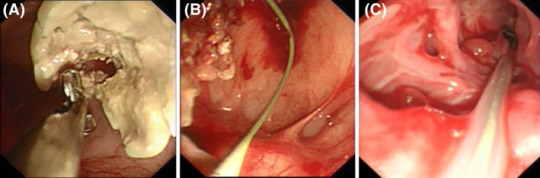
Once the aspergilloma is debrided, a clotrimazole (anti-fungal) solution is infused into the nose and frontal sinuses while the the back of the patient's throat is closed off with gauze and foley catheters. (The patient is able to breathe through an endotracheal tube.) Cotton swabs are used to plug the nostrils, and the clovtrimazole solution incubates for 30 minutes to 1 hour, as the patient is periodically rotated to allow even distribution throughout the sinuses and maximize penetration.



The clotrimazole solution is then drained out the nostrils and suctioned out. While this treatment has been shown to be highly effective, about 1/3 of patients may need repeat infusions.
If there is evidence that the infection has already eroded through the sinus bones and penetrated the brain, then the treatment described above may not be used, and oral medication would be recommended instead. Several months of treatment would be required, with a reported 60-70% success rate, compared to 86% observed in fungicide infusions.
DISSEMINATED ASPERGILLOSIS
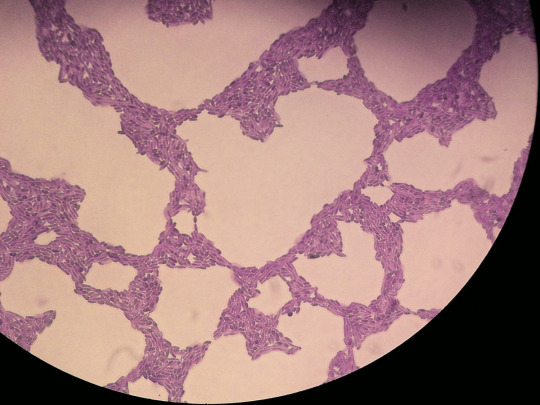
Systemic aspergillosis occurs in dogs when the fungal spores diffuse past the respiratory system and enter the bloodstream, spreading to other sites within the body, including bone, spine, muscles, kidneys, as well as the eyes. A bronchopulmonary form of aspergillosis also forms in dogs, although rare.

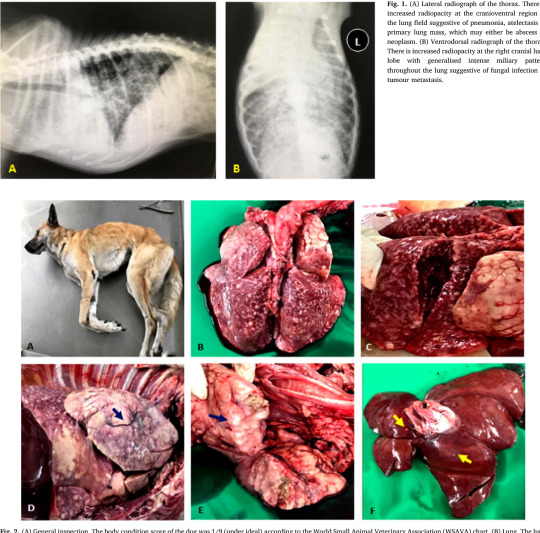

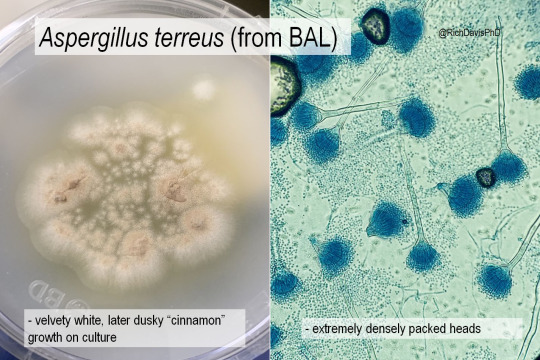
Although less commonly diagnosed, disseminated aspergillosis is most often observed in young-middle aged female German Shepherds and most commonly associated with the A. terreus species. Many patients may also have underlying immunocompromise, such as diabetes mellitus or concurrent bacterial infections, or are receiving immunosuppressive medications, such as glucocorticoids or chemotherapeutics.
Clinical signs of disseminated aspergillosis are dependent on which organ(s) are involved, although many dogs may also show nonspecific signs such as anorexia, lethargy, and fever. Other symptoms of systemic involvement include weight loss, muscle wasting, hematuria, urinary incontinence, uveitis, and neurological deficits such as head tilt and ataxia. There are also often draining tracts (holes with pus or bloody discharge oozing out) in areas of infection.
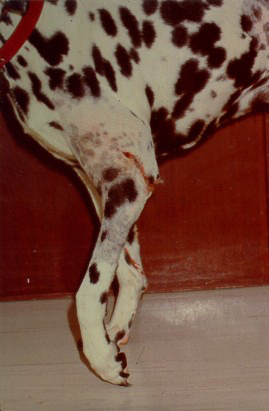

Diagnosing disseminated aspergillosis can actually be quite difficult and invasive. Unfortunately, many dogs are often terminal by the time aspergillosis is suspected, and have an extensive history of failed antimicrobial treatment before diagnosis.
Treatment is also particularly frustrating for these cases, either requiring years - or even lifelong - administration of anti-fungal drugs, and regular follow-ups to monitor for any side effects. While some anti-fungals like iconazole and fluconazole are more cost-effective than others, they are not as effective clinically. On the other hand, the ones that are more effective, like voriconazole, are also more expensive and more toxic over time.
Often times, surgery may also be required to remove the source of the fungal infection (i.e. limb amputation, osteotomy, lung lobectomy, enucleation, etc.). Although surgery may sometimes be curative, prognosis is generally very guarded to poor, as many dogs will often die of their disease before medication can begin to control their condition, or if the surgery required is out of reach.
However, treatment should still be considered in dogs with less severe clinical signs. While treatment of an opportunistic fungal infection is very challenging, early recognition and aggressive treatment can enhance the chance for success.


Sources/Further Reading:
Ballber, Clara, et al. “Minimally invasive treatment of sino‐nasal aspergillosis in dogs.” Journal of Veterinary Internal Medicine, vol. 32, no. 6, 16 Oct. 2018, pp. 2069–2073, https://doi.org/10.1111/jvim.15311.
Bennett, Peter F., et al. “Long term survival of a dog with disseminated Aspergillus deflectus infection without definitive treatment.” Medical Mycology Case Reports, vol. 22, Dec. 2018, pp. 1–3, https://doi.org/10.1016/j.mmcr.2018.07.002.
Brooks, Wendy. “Aspergillosis in Dogs.” Veterinary Partner, VIN (Veterinary Information Network), 1 Nov. 2023, veterinarypartner.vin.com/default.aspx?pid=19239&id=4952634.
Gull, Tamara. “Aspergillosis in Animals.” Merck Veterinary Manual, Merck & Co., Inc., Apr. 2023, www.merckvetmanual.com/generalized-conditions/fungal-infections/aspergillosis-in-animals.
Nelson, Whitney, and Audrey K. Cook. “When to Consider Aspergillosis in Dogs.” DVM 360, MJH Life Sciences, 1 Aug. 2010, www.dvm360.com/view/when-consider-aspergillosis-dogs.
Pascutti, Kristina, and Stuart A. Walton. “Approaches to Opportunistic Fungal Infections in Small Animals.” Today’s Veterinary Practice, 7 Apr. 2021, https://todaysveterinarypractice.com/internal-medicine/approaches-to-opportunistic-fungal-infections-in-small-animals/.
Renchler, J.S. “A Review of Systemic Aspergillosis in Dogs.” Clinical Reviews, Mira Vista Veterinary Diagnostics, Oct. 2020, miravistavets.com/fungal-diseases/aspergillus/review-systemic-aspergillosis-in-dogs/.
#aspergillosis#canine health#veterinary medicine#small animal internal medicine#fungal infection#sinonasal aspergillosis#disseminated aspergillosis#canine disease#dogs
1 note
·
View note
Text
Title: Understanding and Managing Nail Fungal Infections: A Comprehensive Guide to Antifungal Treatments
Introduction:

Nail fungal infections, also known as onychomycosis, are a common condition affecting millions of people worldwide. Characterized by the invasion of fungi into the nail bed, these infections can lead to discolored, brittle, and thickened nails, causing discomfort and embarrassment for those affected. In recent years, various antifungal treatments have been developed to combat this prevalent ailment, offering relief and restoration to afflicted individuals. This comprehensive guide aims to explore the nature of nail fungal infections, delve into the mechanisms of antifungal treatments, and provide insights into their efficacy and side effects.
Understanding Nail Fungal Infections:
Nail fungal infections are primarily caused by dermatophytes, fungi that thrive in warm, moist environments such as sweaty shoes or damp socks. Other fungi, including yeasts and molds, may also contribute to the development of onychomycosis. These pathogens invade the nail bed through tiny cracks or cuts in the skin, establishing a foothold and proliferating within the keratinous tissue of the nail.
Symptoms of nail fungal infections vary but often include:
- Discoloration of the nail, ranging from yellowish to brown or black.
- Thickening and distortion of the nail structure, leading to brittleness and crumbling.
- Separation of the nail from the nail bed, accompanied by pain or discomfort.
- Foul odor emanating from the infected nail.
Risk factors for nail fungal infections encompass a wide range of predisposing conditions, including:
- Advanced age, as circulation decreases and nails become thicker with age.
- Diabetes and other systemic illnesses that compromise the immune system.
- Trauma to the nail, such as repetitive microtrauma or injury.
- Poor foot hygiene and wearing tight-fitting shoes or non-breathable footwear.
- Prolonged exposure to moist environments, such as swimming pools or communal showers.
Diagnosis of nail fungal infections typically involves clinical evaluation and may require laboratory tests, such as microscopy or fungal culture, to confirm the presence of fungal pathogens. Once diagnosed, treatment strategies can be initiated to address the infection and promote nail health.
Antifungal Treatments for Nail Infections:
Antifungal treatments for nail infections encompass a variety of topical and systemic agents, each with its own mechanism of action and efficacy profile. These treatments aim to eradicate fungal pathogens, inhibit their growth, and restore the normal appearance and integrity of the affected nails.
1. Topical Antifungal Agents:
Topical antifungal agents are often the first line of defense against mild to moderate nail fungal infections. These formulations include creams, lotions, solutions, and nail lacquers containing active ingredients such as:
- Azoles (e.g., clotrimazole, miconazole): Azole antifungals inhibit the synthesis of ergosterol, a crucial component of fungal cell membranes, disrupting fungal growth and viability.
- Allylamines (e.g., terbinafine): Allylamines exert their antifungal effects by inhibiting the enzyme squalene epoxidase, disrupting fungal cell membrane integrity and leading to cell death.
- Ciclopirox: Ciclopirox functions by interfering with multiple cellular processes in fungi, including the synthesis of essential biomolecules, ultimately leading to fungal death.
Topical antifungal agents are typically applied directly to the affected nails once or twice daily for several weeks to months, depending on the severity of the infection and the product used. While these treatments are generally safe and well-tolerated, they may require prolonged use to achieve optimal results, and efficacy can vary among individuals.
2. Systemic Antifungal Medications:
For more severe or refractory nail fungal infections, systemic antifungal medications may be prescribed. These medications are taken orally, allowing them to circulate throughout the body and reach the site of infection via the bloodstream. Common systemic antifungal agents for nail infections include:
- Terbinafine: This oral antifungal medication is highly effective against dermatophyte fungi and is often prescribed as a first-line treatment for nail infections. Terbinafine works by inhibiting fungal cell wall synthesis, leading to fungal cell death and clearance of the infection.
- Itraconazole: Another oral antifungal agent, itraconazole, belongs to the azole class of antifungals and exerts its effects by disrupting fungal cell membrane function. It is often used as an alternative or adjunctive therapy for nail fungal infections.
Systemic antifungal medications are typically taken daily for several weeks to months, depending on the severity and extent of the infection. While these treatments can be highly effective, they may carry a risk of systemic side effects, including gastrointestinal upset, liver toxicity, and drug interactions. Regular monitoring of liver function and other relevant parameters may be necessary during systemic antifungal therapy.
3. Combination Therapies:
In some cases, combination therapies involving both topical and systemic antifungal agents may be employed to enhance efficacy and accelerate the resolution of nail fungal infections. These approaches may include:
- Using topical antifungal agents in conjunction with oral antifungal medications to target the infection from both external and internal perspectives.
- Employing adjunctive treatments such as nail debridement (removal of infected nail material) or laser therapy to augment the effects of antifungal therapy and improve nail appearance and function.
Combination therapies should be tailored to the individual patient's needs and may require close monitoring by a healthcare professional to optimize outcomes and minimize side effects.
4. Emerging Therapies:
In addition to traditional antifungal treatments, ongoing research is exploring novel therapeutic approaches for nail fungal infections. These include:
- Photodynamic therapy: Photodynamic therapy involves the use of photosensitizing agents and light activation to selectively target and destroy fungal pathogens within the nail bed.
- Nanoformulations: Nanotechnology-based formulations may enhance the delivery and penetration of antifungal agents into the nail matrix, improving treatment efficacy and minimizing systemic exposure.
While these emerging therapies show promise in preclinical studies, further research is needed to evaluate their safety, efficacy, and long-term outcomes in clinical settings.
Buy Anti Fungal Supplement from Here
Conclusion:
Nail fungal infections represent a common and challenging dermatological condition, affecting individuals of all ages and backgrounds. Effective management of these infections requires a multifaceted approach, including patient education, proper foot hygiene, and timely initiation of appropriate antifungal treatments. Topical and systemic antifungal agents, along with adjunctive therapies and emerging treatment modalities, offer hope for those afflicted with nail fungal infections, providing relief, restoration, and improved quality of life. By understanding the nature of nail fungal infections and the mechanisms of antifungal treatments, healthcare providers and patients alike can work together to combat this pervasive condition and promote healthy, beautiful nails for years to come.
Disclaimer:
This Content has affiliate links
#fungal infection#deadly infections#nails#nail fungus#feetish#méditation#fungalore#medicine#buynow#wishlist#ordernow
0 notes
Text

7 Amazing Home Remedies For Jock Itch at Livlong
Check out the home remedies for jock itch treatment that spreads through skin-to-skin contact. Know more about the jock itch treatment at home at Livlong.
#ringworm treatments#jock itch treatment#jock itch cream#treating skin fungal infection#itch medicine
0 notes
Text
Are homeopathic medicines helpful in fungal infection?
Fungal Infection is a disease that is caused by fungus. A fungus infects the tissues and can cause a disease that influences the skin, disperses into tissues, bones, and organs, or can impact the entire body. This infection can occur anywhere in the body. This fungal infection is also called mycosis and is commonly known as jock itch, ringworm, yeast infection, and athlete's foot. This happens when fungi or fungus insert into your body through inhalation or any other way and reproduces affecting your skin and lungs. It easily affects those who have a lessened immune system where the fungus grows rapidly causing infection. But not to worry much about it as you can prevent this infection by Doctor Bhargava homeopathic medicine for fungal infections in an easy way that works effectively.

Symptoms you should know:
It has some common symptoms that you may be aware of where skin infection is common that can occur in any part of your body. Rest symptoms depend on the kind of infection that you are suffering and those are following as:
It can be itchy and it can make you itch frequently.
It gives you redness on the affected area.
It may give you a burning sensation if it's a ringworm. Other skin infections can also give you a burning feeling.
Skin starts cracking or flaking or you may get blisters when it starts drying.
You may also feel swelling in the affected area of the infection.
Best Treatment for Fungal Infection:
Most people prefer and use cream or lotion for fungal infections that may recover your function but not completely. There may be chances of recurrence of the infection on your skin as creams can recover only the external layer of the skin. But you can get rid of fungal infections completely by a fungal infection treatment in homeopathy. Homeopathy deals with the best treatment for fungal infection where it focuses on recovery or cures completely not just externally but also internally by providing antifungal doses to the body. This homeopathy treatment helps to remove fungal infections from the skin simply and easily.
Homeopathic Medicine for Fungal Infections:
Choose always best and homeopathic medicines are the best for treating your disease including fungal infections. There are two major medicines for fungal infections that homeopathy deals with.
Skedin Drop:This drop contains all the goodness that not just cures fungal infections but also gives relief from other skin issues like rashes, eczema, boils, Urticaria, pimples, Psoriasis, etc. Bhargava Skedin Drop is known as the best homeopathic drop for fungal infections as it contains Juglans Regia, Berberis aquifolium, Azadirachta indica, Sarsaparilla, and Echinacea Angustifolia that prevents the infections completely.

Marhamdad cream: Another great solution for getting rid of fungal infection is Cutica cream popularly known for fungal infection homeopathic medicine. Applying Marhamdad cream regularly after cleaning the affected area can recover the fungal infection on the skin. It also helps in recovering other skin issues. It contains Zinc oxide, Calendula officinalis, Curcuma longa Q, Oleum Santali, Berberis aquifolium, Acid boricua, Hydrastis Canadensis, etc.
The prevention you should take care of:
Always wear neat and clean clothes, mainly underwear and socks to avoid rashes and so do the infections.
Avoid sharing your intimate items including towels and clothing with the person having an infection.
It is suggested to stay away from the animals having indications of fungal infections such as frequent scratching or missing fur.
Always make sure to clear off your body after bathing, swimming, or showering with a dry and clean towel. Keeping the body wet for a long time can cause infection on your skin.
Always wear slippers or flip flop on the wet floor to avoid the fungus.
#fungal infection treatment fungal infection cream Antifungal cream homeopathy treatment#ringworm medicine#fungus cream#skin infection cream
0 notes
Text
*Dr. Smita Goel Homeopathy Clinic*
Your immune system is your body’s defense against infections and other harmful invaders. Without it, you would constantly get sick from germs such as bacteria or viruses.
Your immune system is made up of special cells, tissues, and organs that work together to protect you.
The lymphatic system is a major part of the immune system. It's a network of lymph nodes and vessels. Lymphatic vessels are thin tubes that spread, like blood vessels, all over the body. They carry a clear fluid called lymph. Lymph contains tissue fluid, waste products, and immune system cells. Lymph nodes are small, bean-shaped clumps of immune system cells. They are connected by lymphatic vessels. They contain white blood cells that trap viruses, bacteria, and other invaders, including cancer cells.
White blood cells are the cells of the immune system. They are made in one of your lymph organs such as the spleen or thymus, and in the bone marrow.
When your immune system doesn't work the way it should, it is called an immune system disorder. You may:
• Be born with a weak immune system. This is called primary immune deficiency.
• Get a disease that weakens your immune system. This is called acquired immune deficiency.
• Have an immune system that is too active. This may happen with an allergic reaction.
• Have an immune system that turns against you. This is called autoimmune disease.
Immune system disorders
Here are some common examples:
• Severe combined immunodeficiency (SCID). This is an example of an immune deficiency that is present at birth. Children are in constant danger of infections from bacteria, viruses, and fungi. This disorder is sometimes called “bubble boy disease.” In the 1970s, a boy had to live in a sterile environment inside a plastic bubble. Children with SCID are missing important white blood cells. This disease is deadly without treatment.
• Temporary acquired immune deficiencies. Your immune system can be weakened by certain medicines, for example. This can happen to people on chemotherapy or other medicines used to treat cancer. It can also happen to people after organ transplants who take medicine to prevent organ rejection. Also, infections such as the flu virus, mono (mononucleosis), and measles can weaken the immune system for a short time. Your immune system can also be weakened by smoking, alcohol, and poor nutrition.
• AIDS. HIV, which causes AIDS, is an acquired viral infection that destroys important white blood cells and weakens the immune system. People with HIV/AIDS can become seriously ill with infections that most people can fight off. These infections are called “opportunistic infections” because they take advantage of weak immune systems.
An overactive immune system
If you are born with certain genes, your immune system may react to substances in the environment that are normally harmless. These substances are called allergens. Having an allergic reaction is the most common example of an overactive immune system. Dust, mold, pollen, and foods are examples of allergens.
Some conditions caused by an overactive immune system are:
• Asthma. The response in your lungs can cause coughing, wheezing, and trouble breathing. Asthma can be triggered by common allergens like dust or pollen or by an irritant like tobacco smoke.
• Eczema. An allergen causes an itchy rash known as atopic dermatitis.
• Hay fever (allergic rhinitis). Sneezing, a runny nose, sniffling, and swelling of your nasal passages from indoor allergens such as dust and pets or outdoor allergens such as pollens or molds.
• Food allergy. Severe allergic reactions that are caused by foods.
Autoimmune disease
In autoimmune diseases, the body attacks normal, healthy tissues. Experts don't know why. It is likely a combination of a person’s genes and something in the environment that triggers those genes.
Three common autoimmune diseases are:
• Type 1 diabetes. The immune system attacks the cells in the pancreas that make insulin. Insulin removes sugar from the blood to use as energy.
• Rheumatoid arthritis. This type of arthritis causes swelling and deformities of the joints. An auto-antibody called rheumatoid factor is in the blood of some people with rheumatoid arthritis.
• Lupus. This disease attacks body tissues, including the lungs, kidneys, and skin. Many types of auto-antibodies are found in the blood of people with lupus.
Experts don't know what causes autoimmune diseases. But many factors seem to be involved. If you have an immune system disorder, learn as much as you can about it. And work closely with your healthcare providers to manage it.
#best homeo clinic in indirapuram#ghaziabad#health & fitness#healthy eating#homeopathy#homeopathy clinics#homeopathy cold treatment in indirapuram#homeopathy doctor#homeopathy for ibs#homeopathy medicine#child specialist in noida#greater noida#homeopathy skin allergies treatment in noida#noida news#dentist in noida#anxitey#best skin doctor in ghaziabad#homeopathy skin allergies treatment in indirapuram#chronic illness#fungal
0 notes
Text
#Fungal Pneumonia market#Fungal Pneumonia market research#Fungal Pneumonia market insight#Fungal Pneumonia market trends#Fungal Pneumonia market forecast#Fungal Pneumonia market share#Fungal Pneumonia pipeline#Fungal Pneumonia treatment#Fungal Pneumonia drugs and medicine
0 notes
Note
i hope it’s okay to ask, what is the damage being done by neuralink to quadriplegics and people with ALS?
Any procedure that involves cutting into cavities of the body has inherent risk. And they are cutting into brains and spinal cords, the central nervous system and your body’s control panel, to implant these devices. These are tissues that once damaged, can never become completely whole again. You cannot grow more spinal cord or brain. When your literal nervous system gets damaged, your body has to work AROUND the damaged tissue and scarring. And sometimes you cannot win, and you do not recover, and you die.
And that’s what happened to a lot of the lab macaques that they put neuralink in.
I’m trying to say that the number of potential complications is immeasurable. UC Davis veterinary records showed macaque (monkeys) implanted with neuralink had complications including bloody diarrhea, fungal and bacteria infections, brain bleeding, partial paralysis, and brain swelling. Every single one had to be euthanized because of these complications. And every single one had a damaged cortex from the neuralink implant
Whoever has neuralink in their body now , I seriously hope they are okay and they recover and don’t have long term complications. But the realist in me feels nothing but dread for them because I know their future is full of invasive surgeries and potential death. Neuralink in humans is what happens when people care more about investors and capital and stock buybacks than they do about concrete medicine and ethics
404 notes
·
View notes
Note
is the horses eat birds thing true? What are other weird things about horses we don’t know every fact I learn about them is weird
Like many other herbivores, horses are not as strict about the “only plants” thing as you might think. Though it’s exceedingly rare (but not unheard of) for horses to purposefully hunt and kill birds, they’re not above opportunistically munching on a little bird here and there if it gets in the way of grazing. Calories are calories!
There are so many weird things about horses. My favorites are going to be related to anatomy and physiology because equine medicine is crazy. Here are my top picks
- Horses (like rabbits) are obligate nasal breathers and cannot breathe through their mouth. This means a super congested nose can kill them, and nasal surgery on horses is really scary because post op swelling can become fatal if you’re not careful
- Horses have a callus thing about halfway up the leg called a chestnut or night eye (everything in horse anatomy has several weird names like that). This callus is believed to be a vestigial toe
-Horses have a structure called the guttural pouch that is basically paired sacs of air nestled inside the head likely to help with thermoregulation. Only problem is that pretty much every vital structure in the head (veins, arteries, nerves) pass through these sacs, so if something like a fungal infection gets in there it can cause huge problems very quickly
- Every vet student hates the word laminitis. This is a condition involving inflammation of the inner parts of the hoof and if it gets bad enough the hoof actually starts to detach from the bone. Laminitis can be caused by everything from retained placenta to eating particularly lush grass. That’s right- if you allow your horse to feast on a pasture too green, it’s feet might start falling apart 🙃
Despite their rep as horribly designed animals I actually love horses and find their physiology fascinating. Any animal that has evolved to do one specific thing really, really well (in their case running) will have some little quirks of their biology as a result.
862 notes
·
View notes