#treatments for endometrial cancer
Text
Cancer is a severe illness that has inflicted millions of individuals worldwide. Women are susceptible to developing various forms of cancer, and among the most common ones are pancreatic cancer and endometrial cancer.
#Pancreatic cancer#endometrial cancer#Symptoms of pancreatic cancer#Pancreatic cancer treatment alternatives#treatments for endometrial cancer
0 notes
Text
My mom is definitely getting chemo and she already is so tired from cancer she can barely function
What kind of things can I get or ask for to help make her more comfortable?
Or just any tips?
#i don't think she has the energy to do this#she is so tired a shower a day is an achievement for her#but i know there is stuff people swear helped by for chemo people but I can't remember them#personal#chemo#cancer#cancer treatment#endometrial cancer#my mom has cancer
4 notes
·
View notes
Text
Empowering Women: Endometrial Cancer Treatment at Dr. Chandrakanta’s Gynae-Oncology Center in Jaipur
Endometrial cancer, though less commonly discussed, is a significant health concern among women, necessitating specialized care and treatment. At Dr. Chandrakanta’s Gynae-Oncology Center in Jaipur, we are committed to providing comprehensive and personalized treatment for endometrial cancer, empowering women to navgate their cancer journey with confidence and resilience.
Understanding Endometrial Cancer:
Endometrial cancer, also known as uterine cancer, originates in the lining of the uterus (endometrium) and is the most common type of gynaecological cancer in women. While the exact causes of endometrial cancer remain unclear, certain risk factors may increase the likelihood of developing this condition, including:
- Hormonal imbalances, such as excess estrogen relative to progesterone
- Obesity
- Diabetes
- Older age
- History of endometrial hyperplasia
- Family history of endometrial or colorectal cancer
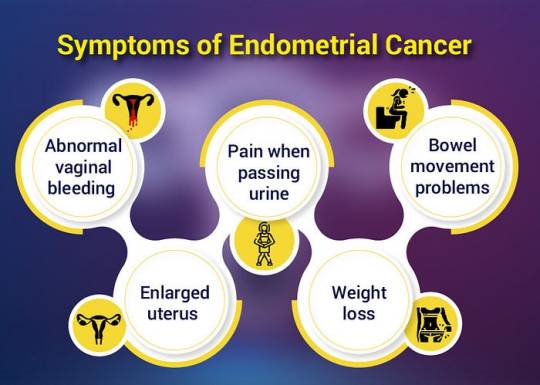
Endometrial cancer may present with various symptoms, which should prompt further evaluation by a healthcare professional. Common signs and symptoms may include:
1. Abnormal vaginal bleeding, such as bleeding between periods, after menopause, or unusually heavy menstrual bleeding
2. Pelvic pain or discomfort
3. Pain during intercourse
4. Unintended weight loss
5. Fatigue
6. Changes in bowel or urinary habits
Treatment:
The treatment approach for endometrial cancer depends on several factors, including the stage of the disease, the patient’s overall health, and personal preferences. At Dr. Chandrakanta’s Gynae-Oncology Center, we offer a multidisciplinary approach to endometrial cancer treatment, incorporating the following modalities:
1. Surgery: The primary treatment for early-stage endometrial cancer involves surgical removal of the uterus (hysterectomy) and may include removal of surrounding tissues or lymph nodes for staging purposes.
2. Radiation Therapy: Radiation therapy may be used as adjuvant treatment following surgery to target any remaining cancer cells or as primary treatment for advanced or unresectable tumors.
3. Chemotherapy: Chemotherapy drugs may be administered to kill cancer cells or prevent them from multiplying, either alone or in combination with surgery and/or radiation therapy.
4. Hormone Therapy: For certain types of endometrial cancer, hormone therapy may be prescribed to block the effects of estrogen or lower estrogen levels in the body.
Comprehensive Care and Support:
At our center, we understand the physical and emotional challenges that accompany a diagnosis of endometrial cancer. That’s why we offer comprehensive care and support services to address the holistic needs of our patients, including counseling, nutritional support, pain management, and survivorship care.
Conclusion:
Endometrial cancer may present significant challenges, but with early detection and expert treatment, women can achieve favorable outcomes and regain their health and well-being. At Dr. Chandrakanta’s Gynae-Oncology Center in Jaipur, we are dedicated to providing compassionate and cutting-edge care that empowers women to face endometrial cancer with strength and resilience. With our multidisciplinary approach and personalized treatment plans, we offer hope and healing to women affected by this condition, guiding them towards a brighter and healthier future.
#choriocarcinomatreatment in jaipur#dr chandrakanta gynae oncology in jaipur#cervical cancer treatment in jaipur#gynae oncologist in jaipur#endometrial cancer treatment in jaipur#gynae cancer doctor in jaipur#gynaecological cancer in jaipur#gynaecological surgeries in jaipur#gynaecological oncologist near me
0 notes
Text
Innovating Lung Cancer Care: Antibody-Drug Conjugates Lead the Way
The ENHERTU Effect: A Closer Look at the Dynamic Duo Daiichi Sankyo and AstraZeneca Taking on HER2-mutant NSCLC
Lung cancer remains one of the most challenging and prevalent forms of cancer. Within this landscape, innovative treatments are offering new hope. One such breakthrough is the collaboration between Daiichi Sankyo and AstraZeneca, which brings forth ENHERTU, an Antibody-Drug Conjugate…
View On WordPress
#ADC#ADCs#Antibody-Drug Conjugates#CEACAM5#Endometrial Cancer - Pipeline Insights#Enhertu#Her2#HER3#Keytruda#Lung Cancer#Lung Cancer Treatmen#Non-Small Cell Lung Cancer#Non-Small Cell Lung Cancer Market#NSCLC#NSCLC Market#NSCLC Treatment#TROP-2
0 notes
Text
Endometrial cancer Treatment in Mumbai | SSO Hospital
Introduction
Endometrial cancer is a type of cancer that affects the lining of the uterus. Early detection and proper treatment are crucial for a successful outcome. Here's what you need to know about endometrial cancer, its symptoms, risk factors, causes, and treatment options at SSO Hospital in Mumbai.

Symptoms
Abnormal vaginal bleeding, especially post-menopause.
Pelvic pain
Difficult or painful urination
Pain during sexual intercourse
Unexpected and rapid weight loss
Risk Factors
Obesity.
Hormone therapy without progestin.
Early onset of menstruation.
Late onset of menopause.
Never having been pregnant.
Family history of endometrial or colorectal cancer.
High blood pressure.
Diabetes.
Polycystic ovary syndrome (PCOS)
Causes
Endometrial cancer usually starts when cells in the inner lining of the uterus (endometrium) mutate and multiply uncontrollably.
The exact cause is not always known, but hormonal imbalances, obesity, and genetic factors may contribute.
As the patient gets older the risk of getting endometrial cancer increases.
Treatment Options-
Surgery: Removal of the uterus (hysterectomy) may be recommended in early stages. Lymph node removal may also be necessary.
Radiation Therapy: Targeted radiation to destroy cancer cells.
Chemotherapy: Medications to kill cancer cells or stop their growth.
Hormone Therapy: Certain hormonal medications can slow cancer growth.
Targeted Therapy: Drugs targeting specific molecules involved in cancer growth.
Take control of your health and explore our comprehensive endometrial cancer treatment in Mumbai. at SSO Hospital Schedule a consultation today. know more our expert endometrial cancer Surgeon will guide you toward a brighter, cancer-free future.
SSO Hospital Expertise-
SSO Hospital in Mumbai is renowned for its comprehensive cancer care. They have a dedicated team of oncologists, surgeons, and support staff specializing in endometrial cancer treatment.
They offer state-of-the-art diagnostic facilities, personalized treatment plans, and ongoing support for patients and their families.
Conclusion
Endometrial cancer is a serious condition, but with early detection and advanced treatments available at SSO Hospital in Mumbai, there is hope for a successful outcome. If you or a loved one is experiencing symptoms or have risk factors, don't hesitate to seek medical advice and explore treatment options. Your health is a top priority.
#endometrial cancer treatment in Mumbai#endometrial cancer Hospital in Mumbai#best cancer hospital in mumbai#cancer hospital#top cancer hospital in mumbai
0 notes
Text
Best Doctor for Endometrial Cancer Treatment in Gurugram
Dr. Archit Pandit is a best doctor for endometriosis in delhi and providing advanced level treatment to the patient who has endometrial cancer; find more about best doctor for endometrial cancer treatment in gurugram.
#best doctor for endometrial cancer treatment in gurugram#endometrial cancer specialist in delhi#best doctor for endometriosis in delhi
0 notes
Link
Dr. Ajay Sharma is a best medical oncologist in north delhi, provides hormonal therapy for cancer treatment in delhi to give complete cure to the patients; find more about hormone therapy for endometrial cancer in delhi.
#hormone specialist doctor in delhi#hormonal therapy for breast cancer in delhi#hormonal therapy for cancer in delhi#hormonal therapy for cancer treatment in delhi#hormone therapy for breast cancer treatment in delhi#hormone therapy for endometrial cancer in delhi#best medical oncologist in delhi#best medical oncologist in north delhi#best medical oncologist in rohini
1 note
·
View note
Text
Pathohistological and Immunohistochemical Characteristics of Locally Advanced Papillary Serous Endometrial Carcinoma - Differential Diagnosis, Prognosis and Complex Treatment by Marinova Lena*

Abstract
We present a clinical case of a rarely diagnosed serous endometrial carcinoma (SEC) with infiltration of the cervix, left parametrium, right fallopian tube, with bilateral ovarian metastases and tumor cells in the peritoneal lavage. After extensive pathohistological and immunohistochemical examinatoin, it was proved to be a locally advanced serous endometrial carcinoma - pT3b N0 M0. The publication discusses the importance of immunohistochemical (IHC) differential diagnosis for determining the histogenesis of papillary serous adenocarcinoma. The main pathohistological dilemma is the determination of the histological subtype of this locally aggressive endometrial carcinoma. Another problem is the definition of the primary origin of the tumor, due to the difference between the pathohistological classification in cervical, uterine and tubo-ovarian adenocarcinomas, as well as the radically different postoperative adjuvant treatment. Incorrect differential diagnosis leads to misdefinition of the necessary complex oncological treatment.
Keywords: Endometrial Serous Carcinoma; Papillary Serous Uterine Cancer; Immunohistochemistry; Differential Diagnosis; Prognosis; Complex Treatment
Introduction
Uterine Serous Cancer (USC), although rare, is the most lethal type of uterine cancer. It has distinct molecular features and pathogenetic pathways compared with other uterine cancer types [1]. According to Bokhman’s 1983 model, Endometrial Carcinoma (EC) is broadly classified based on histopathologic features into two categories, type I and type II, which differ in incidence, prognosis, epidemiology, molecular pathology, and clinical behavior [2]. Type II tumors (nonendometrioid carcinomas), such as serous carcinoma, clear cell carcinoma, carcinosarcoma/malignant-mixed Müllerian tumor, are characterized by poorly differentiated histology and deep migration/invasion [1]. Among the most common problems encountered in practice is the distinction between primary endometrial and primary endocervical adenocarcinomas, and the determination of the tumor origin when there is synchronous, multifocal involvement of gynecologic tract sites, for example the endometrium and the ovary [3]. In this article we present a clinical case of locally advanced serous uterine cancer with difficult differential diagnosis both in terms of histogenesis and histological features, as well as in terms of its primary origin, which is extremely important for complex treatment.
Clinical Case
It concerns 51-year-old woman with pain and bloating. After three peritoneal punctures, a metastatic effusion from adenocarcinoma with probable ovarian origin was found. After CT scan of the abdomen and pelvis, bilateral ovarian formations were found. A total class II laparohysterectomy with bilateral adnexectomy, omentectomy and appendectomy was performed. Intraoperatively - In situ- Ascites- 6 liters of clear liquid. Uterus of normal size. Bilateral ovarian formations with a maximum diameter of about 9 and 8 cm. There were no enlarged iliac and paraaortic lymph nodes. Liver - smooth surface without pathological changes. There were no peritoneal metastases. Radical hysterectomy with bilaterally adnexectomy, omentectomy and lymphadenectomy of the iliac lymph nodes were performed.
Histological Result
In the uterus a polypoid tumor mass was found with complex papillary and glandular architecture, infiltrating the myometrium up to 5 mm; the gland-like spaces were without sharp luminal borders, necrotic material was present in the lumens (Figure 2B). In the isthmus (Figure 3A) and in the cervix (Figure 1, Figure 2A) the histological findings were similar - tumor, composed of merging papillary and gland-like structures was observed, infiltrating over ½ of the muscular layer and reaching the orificium externum canalis cervicalis. In the right ovary (Figure 2C) and in the right fallopian tube (Figure 3B,3C), the same tumor, composed of complex papillary and gland-like structures was discovered, papillary structures were found on the outer surface of both ovaries, as well. Among the tumor cells in the uterus, isthmus, cervical canal, and right fallopian tube, psammoma bodies were found, as well as necrotic debris in the lumens of the tumor glands. In the left ovary cysts lined by stratified collumnar epithelium were found. The left fallopian tube was with fibro-sclerotic changes and paratubal cysts. The right parameter was with preserved architecture. The left parameter was invaded by the tumor. Five right pelvic lymph nodes have reactive changes. Seven left pelvic lymph nodes have reactive changes. Omentum - with hyperemia and mesothelial proliferation. The ascites fluid analysis reports erythrocytes, mesothelial cells, tumor cells with large nuclei - single and in small complexes of 3-4 cells. It is about metastatic effusion.
Histological Diagnosis
Рapillary serous endometrial carcinoma (рТ3b N0 M0) with predominantly exophytic growth, infiltrating the myometrium up to 5 mm., with local invasion of the right fallopian tube and left parametrium. Рapillary serous endometrial carcinoma infiltration in the cervical canal with papillary and glandular architecture reaching the orificium externum canalis cervicalis with infiltration above ½ of the muscle layer. Metastases in both ovaries. Metastatic peritoneal effusion.
Discussion
Uterine papillary serous carcinoma (UPSC) is an uncommon form of endometrial cancer that typically arises in postmenopausal women. UPSC is staged like other forms of endometrial carcinoma at time of surgery using the FIGO cancer staging system. In case of infiltration of serosa or adnexa and / or tumor cells into ascites or peritoneal lavage, the carcinoma is classified as stage 3A. The tumor spread in the vagina and/or parametrium (direct extension or metastases) is staged as stage 3B according to the modified FIGO classification on 1/1/2010 and “Pathologic TNM staging of carcinoma and carcinosarcoma of the corpus uteri, AJCC 8th edition and FIGO 2018 update“[4,5]. For patients who undergo surgical staging—consisting of open abdominal exploration, hysterectomy, bilateral adnexal removal, and pelvic and para-aortic lymphadenectomy in the modified FIGO classification, peritoneal lavage cytology is no longer considered in tumor staging. In the presented clinical case, despite the metastases in the ovaries, the tumor is stage 3B.
Pathohistological characteristics of serous carcinoma adenocarcinoma: Complex papillary, solid or glandular architecture; The architecture is papillary with or without appreciable fibrovascular cores; slit-like spaces; gland-like spaces may be observed (but luminal borders are not sharp as seen in endometrioid carcinoma); solid growth. Psammoma bodies may be present in up to 33% of cases. Cytoplasm is usually scant but can be abundant with eosinophilia or clearing. Nuclei are typically high grade with pleomorphism, hyperchromasia, prominent nucleoli and frequent mitotic figures (including atypical mitotic figures) [6-8]. Most type II endometrial carcinomas, especially UPSC, have a complex papillary or glandular architecture, which is similar to serous papillary ovarian carcinomas. In general, densely fibrotic papillae fronds and slit-like spaces are common [1] [Figure 2,3]. Huge, round, undifferentiated tumor cells with a high number of mitotic figures, increased nuclear-to-cytoplasmic ratios, and prominent nuclear atypia are detached and present in the blank spaces. Hobnail cells, clear cells, and polygonal cells are frequently observed. Cilia are also observed in some cases, as in papillary serous ovarian carcinomas [9,10]. Serous carcinoma cells are arranged in true papillae lined with many cells with overlapping nuclei; cells are large, better preserved and with indistinct cell borders; nuclear chromatin is coarse with large prominent nucleoli [11] (Figure 2, Figure 3).
Immunohistochemical stains in papillary serous endometrial carcinoma show that the tumor is positive for p53 (strong and diffuse expression, mutated) and p16 (strong and diffuse expression) (Figure 4), focally positive for ER (Figure 5C) and negative for PR [6]. In the presented case all tumors (in the different parts of the genital tract) demonstrated diffuse/moderate-strong p16 expression (Figure 4), with percentage of positive tumor cells ranging from 90% to 100%. In contrast, endometrial endometrioid carcinomas exhibit less diffuse and less intense expression, with percentage of positive tumor cells ranging from 10% to 90% [12]. In endometrial endometrioid carcinoma, ER and PR are strongly positive; p53 and p16 are weak and patchy [6]. Highly expressed EMA by most adenocarcinomas is associated with poor prognosis [13,14].
Differential diagnosis (DD): Non-endometrioid carcinomas, which account for about 10% of endometrial carcinomas, may pose a great array of problems in differential diagnosis, including their distinction not only from benign lesions but also from endometrioid carcinoma and various tumors that may secondarily involve the uterine corpus [15]. The complex papillary architecture of serous uterine carcinoma causes a number of diagnostic difficulties. The differential diagnosis includes Villoglandular Variant Of Endometrial Carcinoma. Papillary endometrioid or villoglandular adenocarcinoma (VGAC) is a relatively common type of well-differentiated endometrial adenocarcinoma [16,17]. VGAC is characterized by a papillary architecture with delicate fibrovascular stalks lined by cuboidal to columnar cells with minimal cellular stratification and mild nuclear pleomorphism [16]. VGAC only superficially invades the myometrium, being diagnosed at an early stage and thereby having a better prognosis than typical endometrioid carcinoma. To avoid confusion with papillary serous carcinoma, some authors refer to this entity as endometrioid adenocarcinoma with papillary architecture(16). In mixed endometrial adenocarcinomas the tumor has microscopic features intermediate between serous and endometrioid; for example, papillary architecture typical of serous but without classical cytologic features or glandular architecture with epithelial features suggestive of serous (11). Villoglandular Cervical Adenocarcinoma (VGCA) is a rare well-differentiated subtype of endocervical mucinous adenocarcinoma that usually occurs in young women in early clinical stage I-II [18-24]. VGCA is associated with a better prognosis than other adenocarcinomas [18-20,23,25-27] аnd accounts for 5% of cervical adenocarcinomas [28,29]. It is characterized as superficially infiltrative and shows infrequent lymph node invasion and lymphovascular space invasion [30,31]. Serous Carcinoma of the Uterine Cervix (SCUC) is a very rare malignant tumor, while this histological subtype is common in the ovary, fallopian tube, uterine corpus and peritoneum. Because of its rarity, details of the clinicopathological features of SCUC are largely unknown [32]. SCUC has a complex papillary pattern with epithelial stratification. The tumor is characterized by >10 mitotic figures per 10 high-power fields. An intense acute and chronic inflammatory infiltrate is typically present within the cores of the papillae and in areas of stromal invasion [33]. Pleomorphic and macronucleated atypical cells are observed [32]. Occasional psammoma bodies are present, like in the presented clinical case (Figure 1). The tumor cells in SCUC are positive for p16, focally positive for p53 and ER, and negative for progesteron receptor. Age <65 years, stage >I, tumor size >2 cm, tumor invasion >10 mm, the presence of lymph node metastases, and elevation of serum CA-125 were associated with a poor prognosis [33].
Important for the DD between endometrial and endocervical carcinoma is the study which notes that p16 reactivity is mainly limited to areas with endometrioid or nonspecific cell type differentiation and does not occur in areas with normal endocervical mucinous morphology [34]. It is important to recognize special variants such as uterine serous carcinoma and clear cell carcinoma, as these can show extensive staining for p16 [34]. Univariate analysis on the training set identified 6 markers—p16, ProExC, ER, PR, vimentin, and HPV ISH—as performing well in distinguishing between endocervical and endometrial origin. Positive results for vimentin, ER, and PR support endometrial origin whereas p16, ProExC, and HPV ISH support endocervical origin [34,35]. Primary endocervical adenocarcinomas are characterized by CEA positivity, which is usually, but not always diffuse, negativity for vimentin, and negativity or focal weak positivity for ER [35]. Similar to serous carcinomas, all endocervical adenocarcinomas exhibited diffuse/moderate-strong p16 expression, with percentage of positive tumor cells ranging from 90% to 100% [12]. In the distinction between a high-risk HPV-related (usual type) endocervical adenocarcinoma and a low-grade endometrial endometrioid adenocarcinoma, the most useful immunohistochemical markers are p16 and ER and PR hormone receptors [36]. Given the limits of immunohistochemical stains in distinguishing between endocervical and endometrial origin, individual cases should be evaluated in the context of standard clinical, radiographic, gross, and morphologic findings [34]. In the presented clinical case, DD is required between synchronous serous adenocarcinomas, i.e. primary endometrial with infiltration in the uterine cervix and primary tubo-ovarian carcinoma, or serous endometrial carcinoma with metastases in both ovaries. Multifocal tumor distribution is relatively common in carcinomas arising in the female genital tract. Accurate designation of tumor origin is not always straightforward but is important for staging, prognosis and management [36]. In the context of endometrial carcinoma, the most common dilemmas occur in the setting of concurrent endometrial and adnexal/peritoneal high-grade serous adenocarcinoma [3]. High grade serous tubo-ovarian adenocarcinomas are characterized by complex papillary, solid or glandular architecture [6]; Significant nuclear atypia; significant nuclear pleomorphism (>3 x variation in size) with large, bizarre and multinucleated forms [37]. Prominent nucleoli, often large and eosinophilic; High mitotic index: ≥ 12 mitotic figures per 10 high power fields, often atypical; Necrosis is frequent [13]. Positive stains: p16 (~60%), ER (80%), PR (30%), high Ki67 proliferation index (> 75%) [38]. Usually they present as unilateral tubo-ovarian tumor in 80-90% of cases, no tumor infiltration on the surface of the ovary; without invasion into the lumen of the tube; without vascular invasion - 71.4%; without or presence of ovarian endometriosis [39,40]. IHC analysis of ER and PR of endometrioid endometrial and ovarian tumors distinguishes primary tumor synchronicity from hematogenous metastasis. The same levels of ER and PR are found in metastatic endometrial or ovarian cancer (Figure 5C,5D) and different in synchronous primary endometrial and ovarian neoplasms [41,42]. One general principle used in determining tumor origin in pathology is the identification of intraepithelial carcinoma because the presence of such a lesion is considered a strong evidence of tumor development at a particular anatomic site. Occasionally metastases can colonize preexisting mucosal structures and replace the native epithelium, for example, endometrial serous adenocarcinoma may involve the mucosa of the fallopian tube and closely mimic serous tubal intraepithelial carcinoma [3]. Simultaneous endometrioid carcinomas of the uterus and of the fallopian tube are unusual and occur primarily in obese perimenopausal women. These tumors are predominantly well or moderately differentiated with dissimilar endometrial and fallopian tube grades. The carcinoma of the fallopian tube is usually unilateral and located at the distal end of the tube [36]. It is well established that high-grade endometrial carcinomas may present with metastases even when there is minimal myometrial invasion [3].
Conclusions from the IHC panel of the presented clinical case: 1/The positive expression of ER and PR receptors in the tumor cells of the tumor in the cervix proves the primary endometrial origin of the carcinoma with infiltration of the cervical canal (Figure 5A,5B,5D,5E). 2/ Diffuse positive expression of p16 in the tumor cells of the endometrial tumor mass and in the cervical tumor is typical for serous carcinomas (Figure 4). 3 / Positive expression for Vimentin in the tumor cells in the cervical and the ovarian tumors is typical for primary endometrial carcinoma, negative - is observed in primary viloglandular endocervical adenocarcinoma and primary endometrioid ovarian carcinomas. The positive expression of Vimentin in both tumors of the cervix and the ovary proves the local growth of serous endometrial carcinoma to the cervix with bilateral metastases in the ovaries (Figure 6). 4/ IHC analysis of ER and PR of the endometrial and the ovarian tumors distinguishes primary tumor synchronicity from hematogenous metastasis. The same levels of ER and PR in the endometrial and ovarian tumors report bilateral metastatic tumor spread in the ovaries (Figure 5). 5/ Positive EMA expression in cervical tumor cells determines a poor prognosis (Figure 7). 6/ Psammoma bodies are observed on histological examination of the tumors of the cervix, uterine body, fallopian tube (Figure 1,3A,3B,5A,5B). They are typical for malignancies such as serous carcinoma of the ovaries and serous carcinomas of the cervix, endometrium, fallopian tube, peritoneum [43].
By the above immunohistochemical characteristics primary locally advanced serous endometrial carcinoma/ III B class stage is evidenced. Despite the initial tumor infiltration in the myometrium, as well as the superficial invasion of the cervix in the presented clinical case, the typical tumor spread of locally advanced serous carcinoma with unilateral infiltration into the right fallopian tube and left parametrium and bilateral ovarian metastases are observed.
Prognosis
Uterine Papillary Serous Carcinoma (UPSC) is a rare aggressive variant of type II endometrial cancer [44]. The prognosis is unfavorable, as it is an extremely aggressive tumor with a high potential for local recurrences and distant metastases. The recurrence rate of UPSC is high, estimated to be 31%–80% even in its early stages (stage I–II) [45]. Frequent recurrences in UPSC have led to the induction of adjuvant treatment, including systemic chemotherapy or radiation therapy [46]. Prognosis of the UPSC is affected by age, stage, and histology as well as treatment [47]. UPSC accounts for 10% of all endometrial cancer; however, it carries the poorest prognosis, with 5-year survival rates as low as 55% [48,49].
Complex Treatment
With such a dismal prognosis, these patients should be treated aggressively [48]. The primary treatment is surgical. FIGO-cancer staging is done at the time of surgery which consists of peritoneal cytology, total hysterectomy, bilateral salpingo-oophorectomy, pelvic/para-aortic lymphadenectomy, and omentectomy. After staging and surgery, radiation therapy and/or chemotherapy is recommended to treat patients at high risk for recurrence [50]. Analyses of Gynecologic Oncology Group (GOG) protocol 209 (a noninferiority trial in advanced/recurrent endometrial cancer patients comparing carboplatin and paclitaxel vs paclitaxel, adriamycin and cisplatin) support the favorable side effect profile of six cycles of carboplatin (AUC 6) and paclitaxel (175 mg/m2) [51]. Those who are identified to have residual UPSC in the uterus at the time of surgery, should receive adjuvant carboplatin and paclitaxel chemotherapy, and a strong consideration should be given for vaginal cuff brachytherapy [48]. UPSC’s aggressive features, resistance to chemotherapy, poor prognosis, and extremely high recurrence rate (50% to 80%) contribute to the increase in endometrial cancer-related deaths every year. Currently, surgery together with chemotherapy and radiotherapy (vaginal cuff brachytherapy or external pelvis radiotherapy) remains the dominant treatment option for UPSC [1].
Conclusion
We present a rare clinical case of locally advanced uterine papillary serous carcinoma with difficult differential diagnosis both in terms of histogenesis and histological features, as well as in terms of its primary origin, which is extremely important for complex treatment. Strict pathohistological and immunohistochemical analysis is required for the differential diagnosis of this rare aggressive variant of type II endometrial carcinoma. The prognosis is unfavorable, as it is an extremely aggressive tumor with a high potential for local recurrences and distant metastases. The primary treatment is surgical. FIGO-cancer staging is done at the time of surgery which consists of peritoneal cytology, total hysterectomy, bilateral salpingo-oophorectomy, pelvic/para-aortic lymphadenectomy and omentectomy. Locally advanced uterine serous carcinomas require adjuvant treatment, including concominant radiochemotherapy followed by systemic chemotherapy.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00140/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00140.pdf
#Endometrial Serous Carcinoma#Papillary Serous Uterine Cancer#Immunohistochemistry#Differential Diagnosis#Prognosis#Complex Treatment#Marinova Lena*#IJCMCR#clinical studies
0 notes
Text
Hello my moots and anyone who sees this. I’m trying my best on all avenues to get this cancer treated and fully done with. I was found to have endometrial cancer at 28. I have to have a full hysterectomy and insurance is not great in America as we know!
More info on the donation page!
Any donation or share helps!
#disability#cancer#treatment#donations#please help I just want to go back to living life and working#anything helps#ehlers danlos syndrome#gofundme
77 notes
·
View notes
Text
It's endometriosis awareness month! Here's some general knowledge on my condition, as misinformation is constantly spread about it.
Endometriosis is a disease affecting 1 in 10 people with uteruses. A tissue similar to the endometrial lining, of period blood, grows and sheds on the outside of the uterus. As the menstrual cycle comes, the blood has nowhere to go. This causes intense pain and irritation to surrounding organs. It is one of the most painful diseases recorded.
Endometriosis was first discovered in 1860, though it was recognized in the Hippocratic Corpus around 4,000 years ago. Treatments have varied through the years, starting out with bloodletting, leeches, hanging upside down, exorcisms, genital mutilation, and chemical douches. During the Middle ages, the perception of chronic pelvic pain shifted from a recognized condition to something caused by hysteria, promiscuity, or it was made up. In the hayday of Hippocratic practice, Endometriosis was more common than it is today, likely due to the inaccessibility of diagnosis compared to 4,000 years ago. Somehow.
Today, treatments include birth control, surgery, hysterectomy, and pain relief. There is no cure.
It takes an average of 7-12 years for someone to receive a diagnosis.
Anyone can get endometriosis, including cis men
A hysterectomy is not a cure, as endometriosis will continue to grow and spread to other organs
The pain one experiences due to endometriosis does not correlate with staging. Staging reveals how extensive endometriosis lesions are, not pain. Someone with stage 1 could experience excruciating pain, while someone with stage 4 and frozen pelvis can experience no pain.
Endometriosis lesions are not endometrial lining. The tissue is similar, but not the same. Thus, no one actually knows what endometriosis actually is.
It is only diagnosable through laparoscopic surgery. It can be detected via imaging such as ultrasound or MRI, but more often than not, it isn't seen. You can have completely clear tests up until your surgery and still have even the higher stages of Endo (like me!) (this one was for all you undiagnosed people, you're not crazy!)
Endometriosis is comorbid with many things, including pelvic floor dysfunction, adenomyosis, vulvodynia, uterine cancer and fibroids, ovarian cancer, many autoimmune and inflammatory conditions (rheumatoid arthritis, MS, IBD), and cardiovascular disease.
I've provided links in each point and I deeply encourage you to read my sources, whether you have endo or not. Not enough people understand endometriosis so a lot of us who deal with it don't get grace or compassion, be it in our work lives, relationships, friendships, or family. People with endo, happy endometriosis awareness month.
#endometriosis#endo#endometriosis awareness#chronic illness#disability#cripple punk#chronic pain#chronically ill#disability awareness#cpunk#endometriosis awareness month
63 notes
·
View notes
Text
i'd like to talk about grieving, a little bit. as in the past, discussions of death and cancer below the cut, don't read if this will hurt you, etc....i'm having a bad day and i just need to stream of consciousness for a little bit. sorry.
so my mom died. if you've read my personal posts before or whatever, you probably figured that out. it happened on thursday february 15th around noon. luckily we had a bit of notice that it was coming, so i was able to drive down the saturday prior and spend time with her—three full days where she was pretty much still herself, and part of a fourth.
it's been a really hard month. like, obviously. but i think a part of me still wasn't quite ready for it. i don't know how.
my mom was first diagnosed with breast cancer in fall 2011. she had a mastectomy and went through chemo, and that was hard and scary, but it was i think technically considered stage one—a tumor that was definitely growing fast, but it hadn't spread out of the area, like not to her lymph nodes or anything, and with the treatment she went almost ten years totally symptom-free. right at the start of the pandemic, the cancer came back, but this time it was already stage four, and it was in her abdomen and uterus and intestines.
there was a time when we weren't sure she'd live more than a year. endometrial and other reproductive cancers aren't 'sexy' like breast cancer is, they're not widely studied and there aren't a lot of treatment options. when she had breast cancer i hated 'save the boobies' campaigns (and please never donate to susan komen), but now that my family has lived with another type of cancer that doesn't have tits as a draw, i hate them even more.
my mom made it four years, pretty much, since the first diagnosis. she did chemo, and radiation, and went on medication trials, and put her body through hell to try and fight it. she lived longer than i think any of us thought she would.
the problem with that is how long i've been existing in a state of grief.
i've had years to prepare for this. i've thought about it literally thousands of times—how i'd feel, how i'd tell people, what i'd do after. i pictured it, because i was trying to plan. i was trying to get myself ready.
turns out pre-grieving isn't real. turns out you can't get this pain out of the way by experiencing it in advance. much to my chagrin. i'm not sure there was a way to avoid it, though. so here i am, with four years of grief behind me, and not one second of it has made what's going on now any easier.
some days i forget. every time i'm on twitter or instagram, there are posts i want to send her, and then i don't know what to do with myself. for all that my relationship with her had its hard times, she was my mom, she was my best friend. i love her more than anything and i don't know what to do with myself now that she's gone.
i've been sort of just surviving for the last four weeks. my apartment is a mess, i'm barely leaving, i haven't been good at responding to people. so today i thought i'd at least clean up a little. i'd gone to target a day or two before i drove down to my parents', and i figured i would start with those bags, because they were just sitting there.
i'd forgotten that i bought valentine's day cards for my whole family that i wanted to send. one for each of my brothers, one for my dad, one for my mom. i never sent them, obviously, i didn't even bring them with me. i burst into tears when i pulled them out of the bag, and i've been crying pretty much all day since then. i'm never going to pick out a card for my mom ever again.
i also have a notes app file sitting on my phone. she wrote each of us letters, and my dad sent them out to us, but i haven't been able to open mine yet. it's the last new thing she'll ever say to me. how could i possibly be ready for that? how do i know when the right time to read that will be?
one thing my mom wanted was to die at home. she didn't want it to be in a hospital, and i get it. she spent a month in the hospital after christmas, and god knows how much time cumulatively over the last four years. the fact that she was able to push to get home is something i don't understand, because she was so sick—but she did it somehow. she was able to die in her bed.
and i was with her. like. i wasn't just at home, i was with her.
something they don't tell you about having someone die is you have to start arranging stuff before it actually happens. when we woke up on the 15th, we knew it was only a matter of time—her eyes weren't all the way open and her breath was labored, and she couldn't talk, although at first she still tried to say stuff. we sat there with her and kept her company and talked to her. hospice came by around 11 or 11:30, i don't even remember, and said that based on whatever measurements or readings they take (pupils? breathing? i don't know), it would be between 4-8 hours, and he recommended that my dad call the funeral home. because you have to do that first.
so my youngest brother was driving down from where he lives, my middle brother was in his room, my dad was in his room on the phone, and i stayed with her, because....well, of course, right? and i was just kind of talking, and crying, but trying not to...i don't know, beg her to stay? ask for more time? the nurse said she could still hear, they're pretty sure that hearing and understanding what's being said is the last thing to go, and i didn't want her to feel bad or guilty, or to hurt herself in an effort to stay longer even though there's nothing more that i've ever wanted in my life.
so i told her, you know, we'll be okay. it's going to be unbearably sad, and it's going to suck, but all the stuff we did as a family with her—we'll still do it. and we'll be okay. and there's nothing more important to us than her not hurting anymore, not being miserable and stuck and just...not herself. all that matters to us right now is her, and she didn't have to worry about us, because we'd be okay.
and she took in a breath. there was a pause. she took in another one. and she stopped. that was it.
i didn't even realize at first, not right the second it happened. the hospice booklet had talked about a 'death rattle', about how it happens almost all the time, but that it's more distressing for the people with the person dying than them, that they're not in pain. how the fuck would they know that, i'm not sure i believe it, but...it's what i was expecting. that didn't happen, though. she just stopped breathing.
the amount of guilt i felt for my dad being out of the room...i don't know if that will ever leave me. he said it was ok, because he was having to deal with stuff, and he'd spent a lot of time with her and it was fine, but jesus. how do i not feel like i stole that from him?
i've felt like a shell ever since. i'm back where i live, and i'm getting up and going to work and taking care of my dog and trying to stay connected to life, but...i don't know.
how is it that she's gone? how is this possible? how am i supposed to go the rest of my life without her?
i had four years to get ready for this, and i wasn't. i don't think there's any way i really could have been, but still. it doesn't seem fair that it was so hard for so long, and for NOTHING. nothing is easier now.
i'm sick of feeling sad, and hurt. i feel like i should be over it or something? i don't know, maybe just less actively affected? it's been a month. people's parents die all the time, right?
what am i supposed to do?
35 notes
·
View notes
Text
Just as an FYI for my Gumshoes~
March 15, I may be completely offline or making some rather unusual posts, depending on if I am allowed my phone or not.
My Artist/IRL me is going into surgery that day for a lung nodule biopsy with a DaVinci Robot in Boston. They want to see if the constantly growing nodule is benign or malignant.
This is not my first run in with cancer. I have had Endometrial cancer about 7-8 years back and is in 5years remission currently. The cancer was a Stage 1, Grade 1A meaning it was tight-clustered and tiny. It never grew past 50% of my lining.
Even if it did grow past 50% past my uterus lining, there was still a chance that particular cancer jumped to my lungs, apparently thats common for that cancer. BUT with the multiple CT Scans and PET Scans I have been put through, the wonderful Doctors at Dana Farber say the nodules are not acting like cancer so they need to figure out why they are sticking around and growing instead of shrinking and disappearing like regular nodules do.
The only risks they foresee in this surgery is a 1.5% chance of my lung collapsing. Then I’ll stay overnight so they can “fix it”. Otherwise if it does not collapse, I can go home the same day, just be very out of it due to the anesthesia.
Now, I’m hoping the results will be good. I do NOT want a repeat of the past 7/8 years of wrestling my mental health with the depression of having cancer and dealing with possible chemo treatments. (Not that I had much treatment before, it was so small I was just given a pill and IUD and that made it fuck off pretty much) Which that depression was the reason I stepped away in the first place.
I just got this all back, I do NOT want to abandon it again.
So thats my Ides of March, how will you spend yours?? XD ❤️
8 notes
·
View notes
Text
understand that this medication's side effects includes an increased risk of endometrial cancer
understand that this medication's side effects includes an altered libido
understand that this medication should not be used for the prevention of cardiovascular disease
understand that this medication is not a replacement for distinction treatment, nor will it prevent a prognostic event
understand that the user accepts all risks associated
9 notes
·
View notes
Text
The sheer number of people I have had to tell they have cancer in the last like 3 weeks. I hate it. I've done it probably a couple dozen times in my career now and it hasn't gotten easier, and listening to people cry, trying to describe the kind of cancer and their prognosis despite not being Onc--look, don't go into rural medicine if you can't stomach turning someone's day into the worst day of their life, because it's going to happen. I've diagnosed cancer. I've diagnosed miscarriages. I've told people I don't think they'll ever be able to leave the hospital. I've yelled--I don't like yelling!--to get more pain medication for my terminal patients.
My poor patient with a very obvious and profound learning disability who's managed to cling to functionality in his life, now learning that despite having gotten complete treatment for his HepC he still has developed hepatocellular carcinoma with what look like mets on the imaging. Me reaching out to one of the three local oncologists, one I went to school with as kids, to find out if I need to try to expedite a liver biopsy. The young mother with breast cancer who found out because Epic releases results directly to patients now, so I didn't find out until hours after she'd found out and called us screaming. The woman who asked me right after her biopsy how many endometrial biopsies I've done that turned out to be cancer and I had to say, all of them.
Cancer sucks.
35 notes
·
View notes
Text
lkjdfhakljfdas my parents are so upset by my weight that i told them last week "they're the ones who have to deal with it" and i meant emotionally, but they apparently took this as a challenge and are going to pay $500 a month for treatment
We are not rich and i was the opposite of spoiled, just btw. Imagine hating that your kid who is in post-surgical menopause due to endometrial cancer is fat that much that you spend that chunk of change out of your retirement.
Fine by me, I guess.
7 notes
·
View notes
Link
Dr. Ajay Sharma is a best chemotherapy doctor in delhi, providing chemotherapy treatment for cancer in delhi; find more about chemotherapy treatment for breast cancer in delhi, cervical cancer, stomach cancer, lung cancer, colon cancer etc.
#best chemotherapy doctor in delhi#chemotherapy treatment for cancer in delhi#chemotherapy treatment for breast cancer in delhi#chemotherapy treatment for cervical cancer in delhi#chemotherapy treatment for stomach cancer in delhi#chemotherapy treatment for lung cancer in delhi#chemotherapy treatment for colon cancer in delhi#chemotherapy treatment for esophageal cancer in delhi#chemotherapy treatment for endometrial cancer in delhi#chemotherapy treatment for brain tumor in delhi#chemotherapy drugs for gynecological cancer in delhi#chemotherapy treatment for uterine cancer in delhi#chemotherapy drugs for gallbladder cancer in delhi#chemotherapy drugs for pancreatic cancer in delhi
0 notes