#Gait ataxia
Text
अटैक्सिआ तेलंगिएक्टेसिअ इनहेरिटेंस क्या है?, कारण, लक्षण, इलाज
अटैक्सिआ तेलंगिएक्टेसिअ एक दुर्लभ बीमारी है जो की मस्तिष्क के अंगो को प्राभावित करती है। यह बीमारी मुख्या रूप से छोटी उम्र के बच्चो में पायी जाती है। ऐसा ज़रूरी नहीं की यह बीमारी बस मस्तिष्क तक ही सीमित रहे, कई मामले ऐसे भी है जिनमे यह बीमारी शरीर के विभिन्न अंगो पर भी असर करती है।
अटैक्सिआ में हाथ पैर के चलन और संगठन बनाये रखने में बेहद ही कठिनाई होती है। यदि कोई व्यक्ति अटैक्सिआ से जूझ रहा हो तो उसे चलने फिरने व् अन्य रोजमर्रा के काम करने में कठिनाई होने की अत्यधिक सम्भावना होती है। अटैक्सिआ तेलंगिएक्टेसिअ का मरीज़ो को विरासत में मिलती या आसान भाषा में कहे तो यह बीमारी जेनेटिक होती है।

अटैक्सिआ तेलंगिएक्टेसिअ के कारण
अटैक्सिआ तेलंगिएक्टेसिअ का एक मात्र कारण जेनेटिक्स है। मतलब की यह बीमारी मरीज़ को अपने माँ बाप से विरासत में मिलती है ।
यह एक जेनेटिक बीमारी है जो की इन्हेरिटेंस से आती है । यह बीमारी मनुष्य की एक विशेष प्रकार की जीन्स के गड़बड़ी से होती है जिसका नाम अटैक्सिआ तेलंगिएक्टेसिअ म्यूटेट है।
अटैक्सिआ तेलंगिएक्टेसिअ के लक्षण
अटैक्सिआ तेलंगिएक्टेसिअ के लक्षण कुछ इस प्रकार है:
छोटे बच्चे या जिनकी उम्र 10 से 12 साल के बीच है उनका सही तरीके से मानसिक विकास न हो पाना।
आँखों के सफ़ेद हिस्से में लाल रेखाएं जो की ब्लड की रेखाएं होती है उनका बोहोत ज़्यादा बढ़ना।
सांस सम्बन्धी बीमारियों की बार बार होना। सांस लेने में अदिकतर दिक्कत महसूस करन।
अधिक जानकारी प्राप्त करें"अटैक्सिआ" से संबंधित,
और संपर्क करें 9111234529
#अटैक्सिआ#अटैक्सिआ तेलंगिएक्टेसिअ#अटैक्सिआ तेलंगिएक्टेसिअ के कारण#अटैक्सिआ तेलंगिएक्टेसिअ के लक्षण#Main Cause of Ataxia#Ataxia#Ataxia in hindi#What is Ataxia?#Spinocerebellar ataxia#Vestibular ataxia#Gait ataxia
0 notes
Text
anyway um. shoutout to disabled people who move their bodies in ways that are considered "wrong" or "abnormal" regardless of the cause or how it's classified. and this isn't limited to just ambulation.
paralysis. dystonia. gait abnormalities. people with muscle weakness and/or atrophy. people with brain damage. rotational differences. clubfoot. knocked knees. other limb and bodily differences. functional deformities that affect movement. tissue contracture. muscular dystrophies. spasticity. impaired proprioception, balance, and/or coordination. chronic pain. spinal disorders. dyspraxia/DCD. apraxia. ataxia. dystaxia. tourette's syndrome and other tic disorders. conversion symptoms. tremors. neurodegenerative disease. degenerative bone diseases. joint instability. myoclonus. parkinsonism. tardive dyskenisia. various other neurological problems.
...and the list goes on.
personally i feel a bit surreal when my body not doesn't always move in the ways i want it to because that straightforward connection that's there for abled people has been disrupted in a myriad of ways. but no one is gross, ugly, or scary for being unable to move their body in ways that society considers "normal" and "healthy." no one deserves to be gawked/stared at or treated like they're subhuman because of the way their body moves.
it's okay for us to exist.
#cripple punk#cripplepunk#cpunk#neurodivergence#disabled positivity#j#idk a better term for 'functional deformity' bc afaik deformity is a term w/ negative associations#affirmations
6K notes
·
View notes
Text








21 April 2024
Ivan and I visited Ribsby's dog park today (named after Beverly Cleary's dog character) and did a slow meander through the trail. This place is basically heaven for an old dog like Ivan. There's rarely anyone else here and the trail is all soft surfaces. This time of year there's the sound of meadowlarks and camas is blooming all over. Ivan took his time and enjoyed his slow sniffies. I'm starting to see what looks like ataxia in his gait and it really worries me. I'm not sure if its weakness (although to me he seems to have enough muscle that this shouldn't be the case) or if it's the new pain control regimen (Gabapentin can cause some wobbliness but I only give it to him in the evening) or if there's something else going on. His parents are both DM clear so I doubt it's that but I guess there are many diseases that can cause similar symptoms. Yet again I'm trying to just be okay with seeing him get older and slower and weaker but man it's hard. It hit me today that his days of playing chuck-it or doing competitive obedience are long behind him. It happened so much faster than I could have imagined. But, a slow walk through a grassy, sunny path with birds singing and flowers blooming is certainly still nice and definitely more relaxing.
19 notes
·
View notes
Text
I ended up cancelling the Friday appointment and making an appointment with Kero's old vet that I already trusted, I got nervous about going to a vca because of their shit reputation even if it means waiting an extra couple days since the mass hasn't changed any.
And it's a good thing I did reschedule because he had some kind of neurological event last night around 11pm, that I believe was most likely a focal seizure. First time, no history of seizures, had one vet theorize his weird gait was neurological in nature (but his proprioceptive positioning reflexes have always been normal and as he ages it really does seem to be associated just with poor structure) but no other history of neuro issues. Idk anything about his littermates or parents at all. It lasted just under 2 minutes, I timed it but wasn't able to video record. Ataxia, confusion, dilated pupils with absent pupillary light reflex, weirdly hunched back and hind limb tremors followed by postictal lethargy.
It hasn't happened again and I have not left him alone a single second, I stayed up with him all last night and today he's been pretty normal
Between that and the mass I'm nervous ): I'm trying really hard to keep things in perspective and not borrow any grief from the future, when there's a decent possibility that the mass is harmless and/or easily treatable (but I'm worried about the location because I know from experience paw stuff is a pain in the ASS to heal) and that the seizure was a fluke or it's easily controlled IE (not uncommon in poodles). But I'm also trying to brace myself and be prepared for the possibility of more sinister news. All while trying to stay present with him first and foremost and vigilant without being afraid because regardless of the outcome worrying about it will steal time away with him
Good vibes our way please ... he's my everything
4 notes
·
View notes
Text
Have A Merry Christmas 🎄
Happy Holidays 🍹🍸🍷🥃🥂🍼
Happy New Year 🎊
I will be back in January 2024 until then enjoy this short clip of me almost taking out a rack of costumes at New York Comic Con because of "Chucky" 🔪

Why do people with Multiple Sclerosis can't walk?
If you have Multiple Sclerosis and have difficulty walking then you know the struggle is real.
Difficulty in walking is known as gait disorders and is one of the more common symptoms of MS.
Problems with BALANCE can result in an unsteady swaying from side to side or referred to as the "drunk walk".
The actor David L. Lander that played Squiggly on the Laverne and Shirley show,when he was diagnosed with MS during the peak of his career and instead of telling the studios he had the disease,he let them think he was coming to work drunk so they would not drop him because of the disease.
Sensory deficits results from severe numbness in the feet and can be referred to as sensory ataxia which can cause hard stomping,heavy,delivery gait.
*Fatigue is generally reported with walking difficulties and causing weakness,drop foot, impaired balance with sensory deficits.
This is what happened to me in this video after five hours at NYCC which included standing on the autograph line for three hours and walking the show floor for two (10am-3pm) on Thursday, Day One.*

Friday
12.22.2023
L.George
#chucky#chuckypeacock#chucky syfy#multiple sclerosis#walking difficulties#walking disaster#gaitproblems#nycc#medicalstickers#new york comic con#merry christmas#happy holidays#happynewyear2024#blamechucky
5 notes
·
View notes
Text
I'm going to make this a separate post itself so its not one honkin huge thing attached to the poll when I reblog it.
Regarding Vic's health primarily (he's mainly okay from what we know atm) and comm money in general
I referenced this but cavaliers can have a lot of neurological issues. Apparently this stems from their skulls being too small for their brains often?
I took him to the vet on 10/19 because he was having an issue with what I thought was his ear. What has been happening, since the day I got him back in june, is that he would occasionally scratch at his left ear and start yelping a lot. The place i got him at checked it and said he was fine, the vet I took him to just a couple of days after also checked it and said he was fine. They said that it was likely an anxious thing, so it was dismissed.
And to be blunt, for a while, he only had that yelping scratch occasionally. But within the past monthish it started getting more frequent. And then when it hit too often (4-7 times a week), I called the vet after the first long run of it happening persistently and got an appt a week later. I got worried he had an ear infection even though he was showing no actual signs of an infection of any sort.
And they did the full gambit of an exam, even cleaned his ears, and verified again: no ear infection. No seeming issue with the ear itself. But, she explained she noticed he had a weird gait, which she later called a hypermetric gait, and said shes very worried he has ataxia and/or some issue with his cerebellum. She immediately worked on a referral and told me the neurologist is likely going to want an MRI and to expect it, and that I needed to get him checked out Soon as she was worried the ear thing would get worse. Which. When I explained again how often it was occurring, she seemed more concerned and ran to get pain meds for Vic.
Neurologist was closed friday, so I spent the whole weekend googling what I could. Ataxia is not a illness, but its a symptom. I have no idea of what, and thats what I gotta get checked out. Googling it was uhhhhh. Not fun. Google scared me with talking about how bad cases of conditions that ataxia is connected to usually require the pet to be put down.
Looking on reddit made me feel a bit better. Specifically cavalier talk reddit. Sometimes this thing leads to surgery, but it also seems very likely that (in a good case scenario), Vic may just have a life of pain management. Hopefully minimal pain!!!!
The neurologist called me today and scheduled an appt for nov 2nd. Apparently its an exam and, if needed, MRI same day. Exam is $180 (wheeze), and an MRI can be anywhere between 3k-4k (wheezes louder).
As long as talks with bank go well, if they push for an MRI, I'm going to do it. Even if the diagnosis is that Vic is just a silly lil dude with anxiety, it'll be worth it, you know? For the peace of mind, to know there isn't anything scary with his noggin.
The MRI can be rescheduled, so that will be my next option if bank talk does not go well, but. Thats the info I got. Please keep in mind what the vet said verses what I googled, as google is not a vet.
When it comes to commissions, the funds will likely not go to this. This is why:
Every time I get paychecks, I look on my Bill Schedule and deduct all the stuff that will be coming out that paycheck and work with whatever is leftover. Usually thats not a crazy amount left. If I succeed with regular comms, the money would be going towards any bills I may be struggling with that paycheck/month, or small things to help like. Yaknow. Live outside of bills. Like money towards a cheap haircut. Some energy drinks that week. Getting a couple of extra things when grocery shopping instead of what I count as absolutely needed only.
I wanna be transparent, so I am. It'd likely go towards treats for me to make living not unbearable. That is that. It wouodnt be going towards Me commissioning others, though I will be transparent Still and state I did pay for a small comm before vet visit and so if yall see that, that was smth i paid for already.
3 notes
·
View notes
Text
Learned that the way I limp besides ataxia is called "antalgic gait" aka "pain-avoiding gait" and the reason is "to avoid putting weight on one leg because that leg hurts"
Check and mate, you got me there, neurologists, my left leg always fucking hurts lmao
7 notes
·
View notes
Text
some ways that congenital hypotonia affects me personally in my everyday life
disclaimer: this is a "i want to see hypotonia talked about more"/vent-post adjacent thing rather than something that should be used as some kind of diagnostic reference. hypotonia is more of a symptom than a condition on its own & is associated with a wide variety of diagnoses, i personally don't have a label or explanation for what i experience other than "congenital hypotonia" (and my case is not "self-diagnosed," this was identified when i was still a child.)
generalized hypermobility and painful joint instability either caused by hypotonia or at least contributed to by it if not; no frequent dislocations but joints still tracking badly (especially my knees) and causing pain, ankle instability once gave me an injury
related to above, knees have occasionally buckled/threatened to give out, usually when i'm tired or when i've stood from a sitting position in a chair
unfixable bad posture putting unnecessary strain on a lot of things (reason why my hamstring muscles are so tight)
sitting or standing up easily causing fatigue and pain unless something else is adquately supporting my body (normal chairs usually don't suffice because that still requires adequate posture)
related to above, persistent need to lean on things for support; this is the primary reason why i own a cane
staying in bed a lot due to the above because it's the only time my body doesn't have to support itself
tendency to drool, usually when laying down
dysphagia (things feel "stuck" in my throat a lot, swallowing capsules is becoming more and more uncomfortable), aspirating food/water, acid reflux making these issues worse
may or may not be part of the reason i'm a bit of a loud breather
sometimes chewing hurts or is tiring (or talking)
related to above, mild speech issues mainly affecting articulation (e.g. mouth making a "v" sound rather than "th" sometimes), makes speech physically feel weird or forced, or something even painful; sometimes "talking out of the side of my mouth"
poor grip = poor handwriting, also often makes writing or gripping things painful, including holding/typing on my phone
related to above, makes drawing hard because i don't have proper grip/as much control over my hands as i should
doesn't happen too often but almost randomly losing my balance; i'll just be standing minding my own business and then i'll start tipping over
related to above, can't just stand still and be still, i start tipping in different directions and i think i've subconsciously learned to counteract this when i'n required to stand in place
walking/moving slowly because it feels like my muscles don't have the capacity to move any faster, even if i'm not really "tired" per-se (decreased state of readiness for movement)
have a very hard time holding my head up spine even remotely straight when i am actually tired/worn out
legs/arms start shaking if i hold them out against gravity
also, legs shake if i sit on the floor/a flat surface with my knees bent upward, or arms quickly start to give out if i lay on my stomach and prop myself up on my elbows
walking feels awkward/uncomfortable and wrong most of the time; anything wrong with my gait is probably only recognizable to a PT or someone else who knows what they're looking for, but things just feel too loose/floppy when i walk; probably the reason why i'm prone to tripping and accidentally kicking stuff (POTS-induced ataxia - or w/e it is - makes this much worse)
also probably contributes to constipation and maybe other digestive problems
there's probably more but that's all i can think of for now. this is not universal hypotonia experience as hypotonia is a symptom that varies in its severity and my case seems fairly mild, but i thought i'd talk a little bit about what it's like since it's an under-discussed thing (especially pertaining to disabled adulthood.)
this is okay to reblog.
65 notes
·
View notes
Text
Why is it preferable to obtain a skin turgor over the caudal abdomen or the dorsal skull rather than over the neck? Skin over dorsal neck is too pliable to be accurate
What do we do if the patient is panting and we are unable to obtain an accurate respiratory rate? Panting dogs, gently hold muzzle closed – if still can’t get it – note that the patient is panting
When the temperature of the body exceeds the normal range it is referred to as…..?
Hypothermia - low body temperature <37.5C
Pyrexia- fever condition
Hyperthermia - > 40C
What are the 7 parameters of a complete history?
Date of examination
Signalment – the name, age, breed and sex of the patient
Presenting complaint - what are the clinical signs of the illness, onset and duration of symptoms
Past history – vaccinations, medications, previous surgeries
Family history – if known ( hip dysplasia etc…)
Environment – indoor vs outdoor kitties, recent travel?
Diet – what food, how often fed, appetite, vomiting? Diarrhea?
What information are we looking for with following?
Temperament – Are they Calm? Aggressive? Nervous?
Mental alertness/attitude – Depressed? Bright and alert?, Confused?
General Condition – Body condition score, Hair coat quality, Observable lumps or bumps.
Gait and Posture – Limping?, Have a Head tilt?, Arched back?, Ataxic?
Know your vital signs – what are the “normals” for both cats and dogs
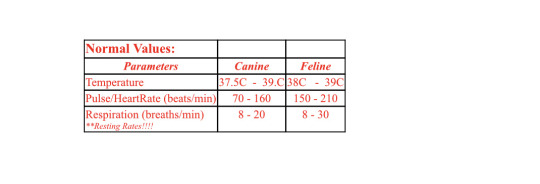
What might cause errors when taking a temperature?
In a fecal ball, or not in the rectum long enough
Where is the easiest location to palpate a pulse rate?Femoral artery up high in the groin
If we count 5 breaths taken by a patient in 15 seconds, what is respiratory rate? Is this a normal rate? 20, yes
What are the 3 ways in which we can assess our patient’s hydration status?
Skin Turgor - refers to the pliability of the skin, or its’ ability to spring back into shape when stretched.
Method Of Hydration
Grasp the skin over the dorsal midline of the lumbar region while the animal is in a standing position
Skin over the neck region is has too much play to be an accurate assessment!
Gently extend the skin up until it forms a “tent”, twist and release
Normal – skin bounces back in less than 2 seconds
Abnormal – skin is prolonged returning to position
Eyes should be well placed, forward in the eye socket and bright.
Eyes that are dull or dry and exhibiting a slight to obvious depression in the eye socket may represent dehydration
Mucous Membranes
gums in the mouth are the easiest to utilize for hydration assessment.
gums should be warm and moist. Gums that are cool, dry and/or sticky indicate a dehydrated patient
How many pounds per kilogram are there? 2.2
What do we mean by capillary refill time? What is normal? This is different from just assessing the mucous membranes – how?
parameter is an indicator the efficiency of the patient’s blood flow or blood pressure.
The gums or gingiva overlaying the canine teeth is a good site to do a CRT. This may be difficult in dogs with pigmented or dark gums.
METHOD
Press down on the area indicated until you can see the area around your finger blanch or whiten
Release the pressure and count in seconds how long it takes for the gum to return to it’s pink color
Normal is less than 2 seconds
How do we know where to place the stethoscope in order to auscultate the heart and obtain a heart rate?
placement of the stethoscope on the chest of the patient is at the level of the space between the 4th and 6th rib
partially flex the elbow so the point lies over the ventral 1/3rd of the chest.
What comprises patient signalment
That part of the veterinary medical history dealing with the animal's age, sex and breed. Including reproductive status
What does the term “Ataxia” mean?
Neurological sign and symptom consisting of gross lack of coordination of muscle movements
When trimming black dog nails, what is one method or indicator that we can use to determine when we are approaching the quick?
Watch the cut end for a lightening of the center may indicate that you are getting close to the quick

0 notes
Text
Navigating life on wheels
In the middle of July 2014, after forty-two years of cruising through life, I got hit with a heatstroke , induced coma , finishing with acquired ataxia.
Waking up in the hospital, I was scared and bewildered, facing a whole new reality outside those walls.
Dealing with sudden issues like speech problems, balance issues, and wonky movements can really throw you for a loop.
It took me ages to wrap my head around this new normal and figure out how to tackle these hurdles day in and day out.
Thankfully, I had my family, medical pros, who still supporting me to this day through this daily wild ride.
It's all about finding and acknowledging your own limitations, adapting so you can maintain your independence and own (proven) safety protocols in order to boost your quality of life.
Yeah, it's tough as nails, but it's also where you find your grit and guts to push through.
Don’t ever forgetting of GOD , who has the upper hand, never ever
1 note
·
View note
Text

In Baltimore City, MD: 4-month-old very sweet and curious kitten with suspected CH is looking for rescue - BARCS, Baltimore MD
- Rescue Needed -
Flamenco- 4 months, unaltered female, 4.3lbs
Sweet 4-month-old Flamenco was brought to the shelter by Animal Control after being left behind during an eviction. She's a bit unsure of her new surroundings, but is easily handled, sweet, and curious.
Upon examination, our vets noted that Flamenco was covered in fleas (which we've treated for), and has signs consistent with Cerebellar Hypoplasia (ataxia, uncoordinated gait, intention tremors). She also has abrasions on her nose, likely from falling over.
Flamenco will be available for rescue pick-up close of business 12/15, and due to her medical, we would love to find placement for her placement.
Please let us know if your organization can help!
Thank you,
The BARCS Rescue Team
Baltimore Animal Rescue & Care Shelter (BARCS)
New Address! 2490 Giles Rd, Baltimore, MD 21225
[email protected]| (410) 396-4695
Rescue pick-up hours:
Monday-Friday: 10:30 a.m.-6:30 p.m.
Saturday and Sunday: 8:30 a.m.-4:30 p.m
Adoption hours:
Monday-Friday: 2 p.m.-6 p.m.
Saturday and Sunday: 11 a.m.-4 p.m.
Baltimore Animal Rescue and Care Shelter, Inc. (BARCS) | 2490 Giles Rd, Baltimore, MD 21225
0 notes
Text
A family named Ulas, in Turkey, has astounded scientists with their unique mode of mobility—walking on all fours.

Check The Video Here
In Southeastern Turkey, the Ulas family has captured worldwide fascination due to their unique ability to walk on all fours, a phenomenon previously undocumented in modern humans. This extraordinary form of locomotion, reminiscent of a bear crawl, has not only baffled scientists but also prompted extensive research into its origins, implications, and potential insights into human evolution.
The Ulas family's remarkable journey into the spotlight began with a scientific paper authored by Turkish researchers, shedding light on this uncommon condition that affects multiple members of their family. Among Resit and Hatice Ulas' 19 children, 12 displayed a distinctive way of moving, walking on all fours. This condition was identified as non-progressive congenital cerebellar ataxia, accompanied by mild intellectual disabilities. Those affected encountered challenges when attempting to maintain balance while walking upright on two legs, leading them to adopt a quadrupedal gait that utilized both their feet and palms.
This phenomenon challenges the traditional understanding of human evolution. According to Professor Nicholas Humphrey, an evolutionary psychologist from the London School of Economics, who spoke with 60 Minutes Australia, "What sets us apart from the rest of the animal world is the fact that we're the species that walks on two legs and holds our heads high in the air... of course, it's language and many other things too, but it's crucial to our self-perception as different from other creatures in the animal kingdom. These individuals blur that distinction."
Professor Humphrey suggests that the Ulas family might provide a glimpse into a transitional phase in human evolution. While walking on all fours resembles the gait of chimpanzees, it could represent an intermediate stage that preceded upright walking. This perspective challenges the linear narrative of human evolution, proposing a more intricate process influenced by adaptation, environment, and genetic factors.
The idea of "backward evolution," raised by some scientists, has faced criticism, including from Professor Humphrey himself, who labeled it as "deeply insulting" and "scientifically irresponsible." This concept contradicts the notion that evolution is a progressive process primarily guided by adaptation to shifting environments.
While scientists persist in uncovering the enigma surrounding the unique gait of the Ulas family, we are prompted to recognize that the tale of human evolution is intricate and ever-evolving. As we delve deeper into our past, the narrative of our evolution remains a dynamic and evolving story.
For more such articles and viral news, click here
1 note
·
View note
Text
What is Ataxia?
Ataxia is a degenerative disease of the nervous system. Many symptoms of Ataxia mimic those of being drunk, such as slurred speech, stumbling, falling, and incoordination. These symptoms are caused by damage to the cerebellum, the part of the brain that is responsible for coordinating movement. Ataxia treatment involves a combination of medication to treat symptoms and therapy to improve quality of life.
People affected by Ataxia may experience problems with using their fingers and hands, arms, legs, walking, speaking or moving their eyes. Ataxia affects people of all ages. Age of symptom-onset can vary widely, from childhood to late-adulthood. Complications from the disease are serious and oftentimes debilitating. Some types of Ataxia can lead to an early death.
Symptoms
Ataxia symptoms vary by person and type of Ataxia. Rate of progression varies as well. Symptoms may worsen slowly, over decades – or quickly, over mere months. Common symptoms of Ataxia are:
Lack of coordination
Slurred speech
Trouble eating and swallowing
Deterioration of fine motor skills
Difficulty walking
Gait abnormalities
Eye movement abnormalities
Tremors
Heart problems
Individuals with Ataxia often require the use of wheelchairs, walkers, and/or scooters to aid in their mobility.
1 note
·
View note
Text
Ataxia
Ataxia is a neurological sign consisting of lack of voluntary coordination of muscle movements that includes gait abnormality.
0 notes
Text
Medical Knowledge
1. The sympathetic postganglionic fibers, called adrenergic fibers, release norepinephrine.
Yes, that statement is correct. Sympathetic postganglionic fibers, also known as adrenergic fibers, release norepinephrine (also known as noradrenaline) as their primary neurotransmitter. Norepinephrine is a catecholamine and belongs to a class of compounds known as adrenergic agonists. It plays a crucial role in the sympathetic nervous system's response, commonly known as the "fight or flight" response.
When a sympathetic nerve impulse reaches the terminal end of a postganglionic fiber, norepinephrine is released into the synaptic cleft. Norepinephrine then binds to adrenergic receptors on target tissues, including organs, blood vessels, and smooth muscle cells. The binding of norepinephrine to these receptors initiates a series of physiological responses, such as increased heart rate, vasoconstriction (narrowing of blood vessels), and increased blood pressure. These effects help prepare the body for action in response to stress or danger.
It's worth noting that some sympathetic postganglionic fibers release a different neurotransmitter called acetylcholine. These fibers are called cholinergic fibers and typically innervate sweat glands and certain blood vessels. However, the majority of sympathetic postganglionic fibers are adrenergic and release norepinephrine as their primary neurotransmitter.
2. Hyperopia is corrected by convex lens.
Yes, that is correct. Hyperopia, also known as farsightedness, is a common refractive error of the eye. In hyperopia, the eyeball is shorter than normal or the cornea has a flatter curvature, causing light to focus behind the retina instead of directly on it. This results in blurred vision, especially when looking at close objects.
To correct hyperopia, a convex lens is used. A convex lens is thicker at the center and thinner at the edges, causing light rays to converge before reaching the eye's lens. When a person with hyperopia wears a convex lens, it helps to refract incoming light rays and bend them slightly inward before they reach the eye's lens. This additional bending of light compensates for the decreased focusing power of the eye and allows the light to focus correctly on the retina, resulting in clearer vision.
By using a convex lens, the lens refracts incoming light in a way that brings the focal point closer to the retina, enabling a person with hyperopia to see both near and distant objects more clearly. The specific power of the convex lens prescribed for a person with hyperopia depends on the individual's refractive error and the degree of correction required.
3. Romberg’s test is a test for balance or gait.
Yes, that is correct. Romberg's test is a neurological test used to assess a person's balance and proprioception (awareness of body position) during standing. It is named after the German neurologist Moritz Romberg.
During the Romberg's test, the individual is instructed to stand with their feet together, arms at their sides, and their eyes closed. The healthcare provider or examiner observes the person for any signs of balance impairment. If the person sways or loses balance significantly while their eyes are closed but maintains balance with their eyes open, it suggests a positive Romberg's sign, indicating a sensory ataxia or impairment of proprioception.
The test is based on the concept of proprioception and the integration of sensory input from the visual, vestibular (inner ear), and somatosensory systems. By closing the eyes, visual input is eliminated, and the reliance on the vestibular and somatosensory systems increases. If there is a sensory deficit or impairment, such as damage to the vestibular system or peripheral neuropathy, the individual may have difficulty maintaining balance during the test.
Romberg's test is commonly used in clinical settings to assess balance and detect neurological conditions that may affect proprioception, such as peripheral neuropathy, sensory ataxia, and certain neurological disorders. It is one of several tests that healthcare providers use to evaluate a person's overall neurological function and help diagnose or monitor certain conditions affecting balance or gait.
4. Hypothalamus controls vital bodily functions such as hunger, thirst, body temperature, and hormone secretion.
Yes, that is correct. The hypothalamus is a small but vital part of the brain located at the base of the brain, below the thalamus. It plays a crucial role in regulating various essential bodily functions, including hunger, thirst, body temperature, and hormone secretion.
The hypothalamus serves as a key link between the nervous system and the endocrine system, which is responsible for the production and regulation of hormones. It controls the release of hormones from the pituitary gland, often referred to as the "master gland," which influences the function of other endocrine glands throughout the body.
The hypothalamus also regulates hunger and satiety (feeling full) through the integration of signals from the digestive system, blood sugar levels, and adipose tissue. It stimulates or inhibits appetite based on these signals, helping to maintain energy balance and regulate body weight.
Thirst regulation is another important function of the hypothalamus. It detects changes in blood osmolality (concentration) and stimulates the sensation of thirst to ensure proper hydration and fluid balance in the body.
Furthermore, the hypothalamus plays a crucial role in maintaining body temperature. It receives input from temperature-sensitive neurons throughout the body and initiates appropriate responses to maintain the body's core temperature within a narrow range. These responses include shivering, sweating, and adjustments in blood flow.
In summary, the hypothalamus controls and regulates several vital bodily functions, including hunger, thirst, body temperature, and hormone secretion, making it a critical part of maintaining overall homeostasis and ensuring the proper functioning of the body.
5. Dura mater is the outermost layer of the meninges.❌
The dura mater is not the outermost layer of the meninges. Instead, it is the toughest and most external layer of the meninges, which are the protective membranes that surround the brain and spinal cord.
The meninges consist of three layers: the dura mater, the arachnoid mater, and the pia mater. The dura mater is the outermost layer, located closest to the skull and vertebrae. It is a thick, strong, fibrous membrane that provides mechanical support and protection to the underlying nervous tissue.
Beneath the dura mater is the arachnoid mater, which is a delicate and web-like layer. It is situated between the dura mater and the innermost layer, the pia mater. The arachnoid mater is responsible for cushioning the brain and spinal cord and contains cerebrospinal fluid (CSF) within the subarachnoid space.
The pia mater is the innermost layer of the meninges and is closely attached to the surface of the brain and spinal cord. It is a thin and delicate membrane that follows the contours of the brain and provides vital nourishment to the underlying neural tissue.
So, to correct the statement, the dura mater is the toughest and most external layer of the meninges, but it is not the outermost layer.
6. The arachnoid or arachnoid mater is the middle layer of the meninges.
Yes, that statement is correct. The arachnoid mater, also known as the arachnoid, is the middle layer of the meninges. It is located between the outermost layer, the dura mater, and the innermost layer, the pia mater.
The arachnoid mater is a delicate, avascular membrane that forms a loose sac around the brain and spinal cord. It is named for its spiderweb-like appearance due to the fine, web-like trabeculae that extend across the subarachnoid space, which is the space between the arachnoid mater and the pia mater.
The subarachnoid space contains cerebrospinal fluid (CSF), a clear fluid that acts as a protective cushion for the brain and spinal cord. The arachnoid mater helps circulate and contain the CSF within this space. It also contains blood vessels that supply nutrients to the brain and spinal cord.
The arachnoid mater is separate from the pia mater by the subarachnoid space, and it does not closely adhere to the underlying neural tissue like the pia mater does. The space between the arachnoid and pia mater is traversed by blood vessels and CSF-filled cisterns, which contribute to the overall support, protection, and nourishment of the central nervous system.
Therefore, the arachnoid mater is indeed the middle layer of the meninges, situated between the dura mater and the pia mater.
7. The innermost layer that contours closely to the many folds and crevices of the brain is called the pia mater.
Yes, that statement is correct. The pia mater is the innermost layer of the meninges, and it closely adheres to the surface of the brain and spinal cord. It follows the many folds, crevices, and contours of the brain, providing a direct covering for the neural tissue.
The pia mater is a thin and delicate membrane composed of a network of blood vessels and connective tissue. It is highly vascularized and supplies nutrients and oxygen to the underlying brain and spinal cord.
Due to its close adherence to the brain's surface, the pia mater is the layer that comes into direct contact with the cerebral cortex and other structures of the central nervous system. It envelops the brain's gyri (convolutions) and dips into the sulci (grooves) and fissures, ensuring that every contour of the brain is covered and protected.
In addition to its protective function, the pia mater also helps to anchor and stabilize the brain within the cranial cavity. It connects with the arachnoid mater, the middle layer of the meninges, via delicate connective tissue trabeculae that span the subarachnoid space.
8. The corpus luteum secretes large quantities of progesterone.
Yes, that statement is correct. The corpus luteum is a temporary endocrine structure that forms in the ovary after the release of an egg during ovulation. It plays a crucial role in the female reproductive system, particularly in the menstrual cycle and early pregnancy.
After ovulation, the ruptured follicle transforms into the corpus luteum. The corpus luteum consists of luteal cells that produce and secrete hormones, primarily progesterone. Progesterone is a steroid hormone that prepares the uterus for pregnancy and helps maintain the early stages of pregnancy if fertilization occurs.
The corpus luteum secretes large quantities of progesterone, which is important for several functions. Progesterone helps to prepare the endometrium (lining of the uterus) for implantation of a fertilized egg. It promotes the growth and development of blood vessels in the uterine lining, making it more receptive to a potential embryo.
If fertilization occurs, the corpus luteum continues to produce progesterone, which supports the maintenance of the uterine lining, inhibits further ovulation, and helps prevent contractions of the uterus that could lead to miscarriage. Progesterone also plays a role in suppressing the immune response to prevent rejection of the embryo.
However, if fertilization does not occur, the corpus luteum undergoes degeneration, leading to a decrease in progesterone production. This drop in progesterone levels triggers the shedding of the uterine lining, resulting in menstruation and the start of a new menstrual cycle.
9. Astrocytes serve as the major supporting tissue in the CNS and contribute to the blood-brain barrier.
Yes, that statement is correct. Astrocytes are a type of glial cell that serves as the major supporting tissue in the central nervous system (CNS). They play important roles in maintaining the structural integrity of the CNS and providing support to neurons.
Astrocytes have numerous functions, and one of their key roles is in the formation and maintenance of the blood-brain barrier (BBB). The BBB is a highly specialized barrier formed by the tight junctions between the cells lining the blood vessels in the CNS. It restricts the passage of substances from the bloodstream into the brain, protecting the brain from potentially harmful substances and maintaining a stable environment for proper neuronal function.
Astrocytes contribute to the formation and regulation of the BBB. They extend their endfeet processes to wrap around blood vessels in the brain, forming a structural and functional association with the endothelial cells of the blood vessels. Astrocytes release specific chemical signals and molecular factors that help establish and maintain the integrity of the tight junctions between endothelial cells, thus contributing to the selective permeability of the BBB.
In addition to their role in the BBB, astrocytes have many other functions in the CNS. They provide physical and metabolic support to neurons, help regulate the extracellular ion balance and neurotransmitter levels, assist in the repair of neural tissue after injury, and play a role in the regulation of cerebral blood flow.
10. Thermoreceptors respond to temperature changes.
Yes, that statement is correct. Thermoreceptors are sensory receptors specialized to detect changes in temperature. They are responsible for the perception of temperature by the nervous system.
Thermoreceptors are found in various locations throughout the body, including the skin, internal organs, and hypothalamus (the region of the brain responsible for regulating body temperature). They respond to temperature stimuli and generate electrical signals that are transmitted to the central nervous system.
There are two types of thermoreceptors: cold receptors and warm receptors. Cold receptors are more sensitive to lower temperatures, while warm receptors are more sensitive to higher temperatures. These receptors provide information to the brain about changes in the external or internal temperature, allowing the body to respond and regulate its temperature accordingly.
When thermoreceptors detect a temperature change, they generate nerve impulses that are transmitted to the brain. This information is then processed, and appropriate responses are initiated to maintain homeostasis. For example, if the body is exposed to cold temperatures, thermoreceptors send signals to the brain, which triggers physiological responses such as shivering and vasoconstriction to conserve heat. Conversely, if the body is exposed to high temperatures, thermoreceptors send signals that initiate sweating and vasodilation to release heat and cool down the body.
0 notes
Text
Dushyant Verma - Ataxia: What It Is, Causes, Symptoms, Treatment & Types
Dushyant Verma Shillong - Ataxia is a neurological disorder that affects the body’s ability to coordinate movement. It can cause difficulty in walking, standing, and speaking. It can also affect the eyes and other parts of the body. The severity of ataxia varies from person to person and is usually caused by damage to the cerebellum or spinal cord. While there is no cure for ataxia, there are treatments that can help manage symptoms and improve quality of life. In this blog dushyant verma southern avenue will explain what ataxia is, its causes, symptoms, types, and treatment options available.
Types of Ataxia
Cerebellar ataxia: This type of ataxia is caused by damage to the cerebellum, which is responsible for controlling movement and balance. Symptoms can include difficulty with coordination and balance, slurred speech, and tremors.
Spinocerebellar ataxia: This is a group of genetic conditions that cause progressive damage to the cerebellum and other parts of the nervous system. Symptoms can include difficulty with coordination and balance, muscle stiffness and spasms, and difficulty with speech.
Friedreich's ataxia: This is a rare genetic condition that affects the nervous system, leading to progressive damage to the cerebellum, spinal cord, and peripheral nerves. Symptoms can include difficulty with coordination and balance, muscle weakness, vision problems, and heart problems.
Vestibular ataxia: Vestibular ataxia is a type of ataxia that is caused by damage to the vestibular system, which is responsible for maintaining balance and spatial orientation. Symptoms of vestibular ataxia can include difficulty with balance and coordination, dizziness or vertigo, and a feeling of unsteadiness or disorientation.
Sensory ataxia: Sensory ataxia is a type of ataxia that is caused by damage to the sensory nerves that transmit information about the body's position, movement, and balance to the brain. This damage can occur due to various underlying conditions, such as vitamin deficiencies, diabetes, or nerve damage caused by alcoholism.
Causes of Ataxia
According to dushyant verma maharani bagh, ataxia can be caused by a variety of underlying conditions, including stroke, multiple sclerosis, alcohol abuse, brain tumors, and vitamin deficiencies.
Stroke: Ataxia can occur as a result of a stroke, which happens when blood flow to the brain is interrupted, causing brain damage.
Multiple sclerosis: This is a condition where the immune system attacks the protective covering of the nerves, causing damage to the nerves and leading to ataxia.
Alcohol abuse: Long-term excessive alcohol consumption can cause damage to the cerebellum, the part of the brain responsible for controlling movement, leading to ataxia.
Brain tumors: Tumors in the brain can affect the areas responsible for controlling movement, leading to ataxia.
Vitamin deficiencies: Deficiencies in certain vitamins, such as vitamin B12 and vitamin E, can lead to ataxia.
Symptoms of Ataxia
Dushyant verma says, the symptoms of ataxia can vary depending on the underlying cause of the condition. Some common symptoms include:
Difficulty with coordination and balance: People with ataxia may have trouble maintaining their balance, standing or walking without stumbling, and may have a wide-based gait.
Slurred speech: Ataxia can affect the muscles used for speaking, resulting in slurred or slowed speech.
Tremors: Some people with ataxia may experience tremors, which are involuntary movements of the limbs or other parts of the body.
Vision problems: Ataxia can affect eye movements, leading to vision problems such as double vision or difficulty tracking moving objects.
Fatigue: People with ataxia may experience fatigue or weakness, particularly if their condition affects their ability to perform daily activities.
Treatment of Ataxia
There is no cure for ataxia, but treatment options are available to help manage symptoms and improve quality of life. The type of treatment recommended will depend on the underlying cause of the ataxia.
Some common treatment options include:
Physical therapy: Physical therapy can help improve balance and coordination, and may include exercises to strengthen muscles and improve flexibility.
Speech therapy: Speech therapy can help improve communication skills for people with ataxia who experience slurred speech or other speech difficulties.
Occupational therapy: Occupational therapy can help people with ataxia improve their ability to perform daily activities, such as dressing and grooming.
Medications: Depending on the underlying cause of the ataxia, medications may be prescribed to help manage symptoms or slow the progression of the condition. For example, people with ataxia caused by multiple sclerosis may benefit from medications that suppress the immune system.
1 note
·
View note