#pleural disease
Text
What Should I Know About Asbestos Removal in Ottawa?

Asbestos is a scary word to hear as a homeowner. If your home in Ottawa was built in 1990 or earlier, it’s possible that asbestos was used in its construction. At one point in time, asbestos was a popular building material used for weather insulation, fireproofing, and noise proofing. However, its many construction benefits were too good to be true. Asbestos is now known to be an agent that can cause various forms of cancer and lung issues if the fibrous materials are inhaled. If you believe you may have asbestos in your home and want to learn more about how you should take care of it, read on. Trust experienced professionals for asbestos removal in your Ottawa home.
FREQUENTLY ASKED QUESTIONS ABOUT ASBESTOS REMOVAL
1. What Are the Most Common Signs That Asbestos May Be Present In My Home?
Asbestos is a silent roommate and may not be recognized right away. However, there are some indicators that you may need to have asbestos removed from your Ottawa home; it is always best to test certain materials to confirm if it contains asbestos. Here are some common signs that may indicate it’s hiding place:
Your home was built in the 1990s or earlier.
Your home has vinyl flooring from the 1990s or earlier.
You have an older, popcorn ceiling.
Your registers or duct work are wrapped in material.
You have older blown insulation in the attic, walls or floors.
2. How Can Asbestos Harm My Health?
Asbestos is a fibrous mineral that is a known carcinogen. It is linked to several diseases that can inhibit lung function, cause immune system distress, and even lead to death. The diseases caused by asbestos inhalation include:
Lung cancer – This disease is typically caused by smoking, but it is also linked to asbestos. Its symptoms include persistent coughing, shortness of breath, fatigue, wheezing, and respiratory infection.
Asbestosis – This illness is the result of scarring of the lungs from breathing in asbestos over a long period of time. Affected individuals experience shortness of breath, wheezing, and chest pain.
Mesothelioma – A rare disease linked to asbestos; mesothelioma is a cancer that creates tumors that block lung function. This illness is characterized by chest pain, extreme fatigue, and difficulty breathing.
Pleural disease – This disease known as pleural disease is non-cancerous but still affects lung function and can cause issues in the chest cavity. Pleural disease can cause fluid in the lungs, collagen deposits, folding of the lung, and thickening of lung tissue. It can lead to respiratory failure, chest pain, and coughing.
3. What Are The Risks Associated With Asbestos Removal?
There are significant risk factors involved when removing and disposing of asbestos. In the process of removal, asbestos fibers can easily become airborne and be inhaled by individuals occupying a space. Breathing in asbestos fibres can lead to the significant health problems described above. Therefore, it’s important to take the necessary precautions to avoid this from happening. If the area is disturbed and removed without safety equipment, trained specialists, and proper disposal, it can lead to dangerous consequences. If you think you may have asbestos in your home, your best option is to contact professional asbestos removal specialists in Ottawa.
4. Can I Remove Asbestos From My House By Myself?
No, regulations in Ontario prevent you from removing, transporting or disposing of asbestos on your own. Attempting this on your own can result in disturbance of the fibers and may cause disease from inhalation. If you suspect you may have asbestos in your home, you should always contact a professional to assess the situation and complete the removal process. Trained professionals will have years of experience, proven testing procedures, and specialty equipment to remedy your asbestos concerns.
5. Why Was Asbestos Used In The Past In Ottawa Homes?
Asbestos is a naturally occurring mineral that was used as a building material and considered suitable for several types of construction. Asbestos was commonly used in drywall and popcorn ceilings, as well as for vinyl flooring, siding, cement, and heating systems. This material was found to be useful for fireproofing, weathering, and sound insulation. Not only was this material useful for multiple building needs, but it was also inexpensive, strong, and resistant to water, electricity, and chemicals.
Originally Posted on Go Pro Restoration
#Asbestos#asbestos removal in your Ottawa#lung cancer#asbestosis#mesothelioma#pleural disease#asbestos removal specialists
0 notes
Text
Global Pleural Diseases Market is Estimated To Witness High Growth Owing To Growing Prevalence of Pleural Diseases
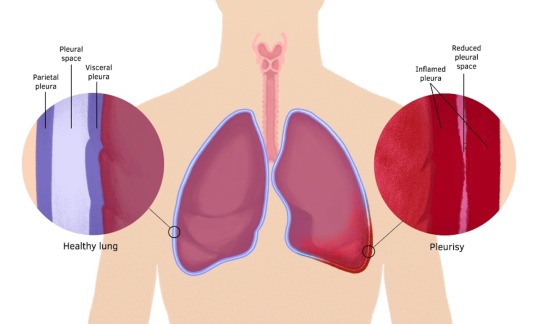
The global Pleural Diseases Market is estimated to be valued at US$ 3.84 billion in 2023 and is expected to exhibit a CAGR of 6.8% over the forecast period 2023-2030, as highlighted in a new report published by Coherent Market Insights. Market Overview: The Pleural Diseases Market refers to the market for the diagnosis, treatment, and management of diseases affecting the pleura, the thin membrane surrounding the lungs. Pleural diseases include conditions such as pleurisy, pleural effusion, pneumothorax, and mesothelioma. Pleural diseases often cause symptoms such as chest pain, breathlessness, cough, and fever. The market for pleural diseases is driven by the increasing prevalence of these conditions, which can be attributed to factors such as aging population, rising pollution levels, and high prevalence of respiratory diseases such as tuberculosis and lung cancer. The main products associated with the Pleural Diseases Market include diagnostic tests, imaging techniques, surgical procedures, and medications. These products play a crucial role in the timely diagnosis and effective management of pleural diseases, which can significantly improve patient outcomes and quality of life. Market Key Trends: One key trend observed in the Pleural Diseases Market is the growing adoption of minimally invasive procedures for the diagnosis and treatment of pleural diseases. Minimally invasive procedures offer several advantages over traditional open surgeries, including reduced pain, shorter hospital stays, faster recovery times, and less scarring. For example, video-assisted thoracoscopic surgery (VATS) is now commonly used for diagnosing and treating pleural diseases, as it allows surgeons to access the pleural cavity through small incisions using a video camera and specialized instruments. PEST Analysis: Political: Government initiatives and policies aimed at improving healthcare
0 notes
Note
So what you want Kate to not get chemotherapy so that she gets even more worse and more unwell? Who even thinks like that and William doesn’t smoke

First off, it's well known that William smokes. Just because he hides it better than Harry doesn't mean he doesn't do it. He clearly has smoker skin. That's why his skin looks so terrible & dry. So dry that soon we might be able to grate cheese on it.
"You want Kate to not get chemotherapy so that she gets even more worse and more unwell?"
Your ignorance is clearly showing.
This is how people die from cancer:
Catabolism: the body breaks down on a cellular level; substances released by tumor cells are strong anorexics.
Secondary infection due to immune system suppression.
Blockage of vital structures: trachea/esophagus, superior vena cava (SVC) syndrome, impacts to the spinal cord, pericardial effusion, pleural effusion, etc.
Side effects of medication/treatment: immune suppression, pulmonary fibrosis, Graft-versus-Host-Disease (GvHD), etc.
You do not die from cancer just because you have "cancer."
I wrote a long post yesterday differentiating that different people have different physiology. Just because you have "cancer" does not mean that it poses a threat to your life or health. Plenty of people have "cancer" that does not progress at all or affect them in any way. Just because you have "cancer present" does not mean it will affect your life or health in any significant way.
The situation is really like the anon said:
"Catherine has a much more serious cancer than they are letting on, hence, the decision to have chemo is not even a discussion point,"
"she’s not having chemo and there’s another reason why she’s missing in action,"
"she and William are panicking and she’s receiving chemo regardless"
My bets are on numbers two or three.
Kensington Palace is clearly lying. Can't wait for it to be revealed! KP's strategy before Kate's cancer announcement was to release the news that her medical records had been breached and paint Kate as a victim. After the cancer announcement, it was those pesky conspiracy theorists and the axis of evil who was to blame for Kate's reputation being slagged around the world, not the utter incompetence of William and KP.
Let's not forget that William is an emotionally damaged, thin skinned, control freak with a privacy fetish.
Let's also not forget that next Monday, 01 April 2024, begins a new fiscal year for the BRF.
#ask#hate mail#medicine#smoking#William The Prince of OWN GOALS#William The Terrible#William The Weak#William The Prince of Wales#prince william#Prince & Princess OWN GOALS#kate middleton#Catherine The Princess of Wales#kensington palace#palace officials#lies lies lies#pr games#strategery#Wales fandom ARMAGEDDON
14 notes
·
View notes
Text
Entamoeba Histolytica
Moving on from Disseminated infections.
and back to parasites, we have this amoeba.
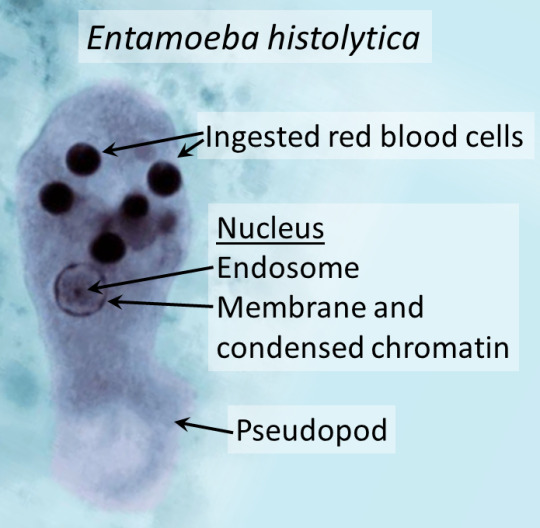
Courtesy of wikipaedia.
One complication is liver abscess.

Image from NEJM
Ring enhancing cysts were seen on CT (requested after the authors noted deranged liver function tests) and on percutaneous drainage (which radiology can do), they had brown cloudy fluid. Under the microscope they noted the pseudopods (leg like extensions).
Classically though, entamoeba causes amoebic dysentery or bloody diarrhoea that develops over 1-4 weeks. However, 90% are asymptomatic. Given the complications/extra-GI manifestations, it can be fatal in a very small minority.
Severe disease/Complications
- toxic megacolon (always makes me think of heavy metal bands, in sad actuality it's inflammation that affects more layers and causes the colon to wide. resembling balloon animals)
- fulminant colitis + perforation (from inflammation, ulceration etc. that the trophozoites induce, high mortality)
- liver abscess (more common, fevers/RUQ/hepatomegaly, transamnitis and jaundice, maybe months before this develops)
- rarely: pericarditis + tamponade (from liver rupture, rare but high mortality), pleural effusion & brain abscess (exceedingly rare - but acute confusion + fevers, rapid deterioration)
risk factors for severe diseases/complications: malignancy, pregnancy, immunosuppression in general.
Toxic megacolon:
Can actually rupture eventually.
Courtesy of wiki

Transmission: faecal oral routes (contaminated food/water sources) and it's widely distributed across the world. As with many infectious diseases, it has a higher prevalence in lower socioeconomic groups and regions of the world. Africa & South/Central AMerica have higher rates than other countries (poor sanitation areas, water sources like rivers have multiple purposes for households etc.). Generally, in western countries, it develops in returned travellers who went to endemic areas or immigrants.
Detection: EIA assay for entamoeba antigen in stool, serology (relies on antibodies, so undetectable the first week and last a life time, does not differentiate acute vs past infection), stool MCS for cysts and ova, PCR and colonoscopy (ulcer/erosions, biopsy will reveal cysts and trophozoites)
Treatment: metronidazole in active/acute disease, increased doses in severe/complicated disease or invasive. depending on where you are, also paromycin if asymptomatic or following active treatment to remove cysts.
Consider this in returned travellers with high fevers, abdo pain and bloody diarrhoea lasting > 2 weeks.
Avoids while travelling to endemic areas - uncooked foods, unbottled water/ice cubes, street vendors (what a shame), just anything raw. Practice good hand hygiene.

Sources:
StatPearls ON PubMed
Amoebiasis on CDC
#entamoeba histolytica#medblrs#medblr#infectious diseases#parasites#parasitology#infectious disease#microbiology
9 notes
·
View notes
Note
Can binding cause pleural effusion?
I've been feeling pressure in my rib and chest area for a while and recently it's gotten worse as well as my ability to breath, could it be from binding? I don't have any bruised or broken ribs
I do have an inflammatory disease but I don't think it's that
Lee says:
We are not medical professionals, which is why I would recommend that you speak to someone who is!
I can't tell you whether the symptoms that you are experiencing are caused by binding or worsened by binding because I'm not a medical professional who has taken your medical history and examined you, but I can tell you that it's important to get it checked out by someone who can diagnose the issue and recommend a plan to address it.
You should call your primary care provider/general practitioner/family doctor, and/or send a message to them through the patient portal if there is one.
If you don't have a doctor or other provider who you usually see for an annual check-up or sick visit, you could look to see if there are any urgent care clinics near you who accept your insurance.
And don't bind until you've been cleared to do so by a medical professional-- it sucks, but it's time to take a break from binding, just in case it could exacerbate the issue.
If you've been having unexplained issues breathing for a while, you should see a medical professional. That's always true. If you're worried about telling your parents about your concerns about binding because you're closeted or they don't approve of you binding, don't mention binding when you explain why you'd like to go to the doctor, just tell your parents about your symptoms.
If you think that your parents might not allow you to go to the doctor, start by going to the school nurse, explaining your symptoms, and see if they'd call your parents or write a note for your parents recommending that they take you to the doctor. That might make them more likely to take you if they tend to otherwise disregard your concerns.
But when you do go to the doctor, do mention your binding, as well as what symptoms you're experiencing and how long you've been experiencing them.
I've had two family members get pneumonia in the last year, and one had to be hospitalized and the other needed a CT scan to diagnose lung issues, and both needed antibiotics. There are a lot of illnesses and injuries that can cause issues with breathing (example one: COVID!) but some things don't always improve without treatment.
It seems like you've been having these issues for a while, so I'd encourage you to do whatever you have to be sure you get the care that you need instead of waiting it out and seeing if you get better.
I hope you feel better soon anon! And again, please do seek out medical attention IRL!
40 notes
·
View notes
Text
Liver transplantation.
The one time you might actually want cancer.
Why? Because having a primary liver cancer bumps you up on the liver transplant list. But it can't just be any cancer - there's a criteria for acceptable cancer burden for adult liver transplant, which is known as Milan Criteria. Essentially one big tumor smaller than 5 cm or 3 small tumors less than 3 cm each. The tumor can't have left the liver either aka metastasis. However if it's too small (<2 cm ), you don't get priority listing for having that cancer. Kind of like Goldilocks - the tumor has to be just right.
Now first off, you almost never get a primary liver tumor aka hepatocellular carcinoma (HCC) without something wrong in the liver in the first place.
This is usually Cirrhosis aka fibrosis of the liver, which can be caused by Hepatitis C or more commonly drinking too much alcohol too often. The liver fails cause its cells are dead or dying, and the resulting scarring prevents blood from your GI tract from returning properly to your systemic blood. This pseudo-blockage results in fluid backing up in your body, resulting in ascites (fluid in the belly) and pleural effusion (fluid in the lung space) and generalized soft tissue swelling.
The body tries to compensate for this by making alternate paths. Problem is the liver is also a filter, and bypassing the filter through an alternate path affects the brain - a common symptom is confusion and sometimes coma in these patients. Official term is hepatic encephalopathy.
Cirrhosis patients can also literally turn yellow because bilirubin, which occurs from the normal breakdown of red blood cells, can't be processed well by a dysfunctional liver. Liver does a lot of other important stuff too, but I'd go on forever with that - so I'll end that here.
In any case, the only treatment for cirrhosis is getting a new liver - once cirrhosis occurs, it cannot reverse, only worsen. The liver transplant list uses its own criteria known as MELD which I also won't get into here, but generally the sicker you are, the higher you are on the transplant list.
Cirrhosis is essentially a breeding ground for primary liver cancer because cirrhosis is essentially repeated constant inflammation - and all it takes is one cell to heal in the absolutely worst way - and then you have a cancer. This is why cirrhosis patients get yearly liver imaging screening to detect that.
Milan Criteria was created because a good number of liver transplants in cancer patients turned out to have recurrent liver cancer in the new liver. After Milan was implemented, long-term recurrence-free survival improved from 30% to 75%. I believe the sizes used in Milan acts as a surrogate for the likelihood of microscopic metastasis, cancer that's left the liver but too small to be seen in imaging, but don't quote me on that.
Now why did I bring this up? One of the residents asked out loud about why we don't just cut out the cancer.
For one, cirrhosis ensures another one will pop up eventually, and for two, cutting a cancer out also means cutting out good tissue (or semi-okay in a cirrhotic's case) to create the disease-free margin. You don't have much good tissue left in a cirrhosis liver.
You could ablate the cancer by frying it with heat or freezing it, but you again have the issues of damaging normal tissue. Typically excision or ablation is done when there's no chance patient will get a donor liver.
There's also TACE (transarterial chemoembolization) which can be used to shrink tumors, usually back into the limits imposed by Milan criteria. Because if your cancer is too big for Milan, you don't get a liver. There are strict rules for that, and if you break them, your liver transplant service is not getting donor livers.
4 notes
·
View notes
Text
Pleural diagnosis Delhi NCR|
Post Covid Pulmonary Rehabilitation Delhi|
tb specialist doctor in delhi|
Interstitial Lung Disease (ILD) Doctor in Delhi
Dr. Neetu Jain is a very renowned and highly experienced doctor in New Delhi who specializes in Critical care and Pulmonary medicine.
91-8287429854
2 notes
·
View notes
Text
we get some wild referrals...had a cat come in for abdominal effusion recently and the rDVM had given it Lasix and Convenia?
Lasix aka furosemide is a diuretic, so you give it when you're thinking right-sided heart failure, which can cause abdominal effusion. but cats almost never get right-sided heart failure, they get left-sided heart failure, which causes pulmonary edema & pleural effusion. aka they get fluid in their chest, not the abdomen. certainly heart disease is on the rule out list, but it shouldn't be anyone's first assumption.
Convenia is an injectable antibiotic, so I assume they were thinking about infectious disease as a possibility, which again isn't crazy. but Convenia is for, like...skin infections? small wounds and abscesses in cats that refuse to take oral medications? I've never seen anyone use it for anything more serious. certainly not for FIP, lol
but like...honestly, without an acute trauma history, in an indoor-only senior cat with relatively normal blood work, realistically this kind of thing is going to be cancer. carcinoma, sarcoma, IDEK what else, but definitely cancer. tumors were confirmed by ultrasound for this patient, although I don't think they went as far as biopsying anything.
it was just one of those head scratching "what were they thinking?" cases. up there on my list along with the place that once sent us an unblocked cat for hospitalization with his urinary catheter just...open. not attached to a collection set, not even capped off briefly for travel after the bladder was emptied, just...open. dribbling urine and exposing the patient to urinary tract infection. what on earth
3 notes
·
View notes
Text
Reviewing questions:
Blindness is a potentially devastating complication of sarcoidosis. Ocular sarcoid can develop in up to half of all cases and most commonly presents as anterior uveitis or keratoconjunctivitis. The most serious complication is optic neuritis.
A complete ophthalmologic examination at the time of diagnosis is recommended, as asymptomatic disease can result in permanent visual impairment. All patients with sarcoidosis should have a careful history and physical examination to identify other organ involvement before having further testing, including ECG, pulmonary-function testing, and baseline laboratory studies (calcium level, alkaline-phosphatase level, renal-function, and hepatic-function tests) to evaluate the extent of disease.
McConnell's sign is defined as right ventricular free wall akinesis with sparing of the apex. Typically this looks as if the apex of the RV is a trampoline. Echocardiogram shows right ventricular strain and a positive McConnell sign, which is indicative of pulmonary embolism (PE).
All patients who have known or suspected bronchiectasis and who are acutely ill with suspected lower respiratory tract infection should be empirically treated with an antipseudomonal antibiotic, such as cefepime until culture results are available to guide treatment decisions.
Heerfordt’s syndrome (uveoparotid fever) is another collection of clinical findings specific enough to diagnose sarcoidosis without a biopsy. These signs and symptoms include uveitis, parotid gland enlargement, and facial nerve palsy.
Lofgren’s syndrome is a form of acute sarcoidosis. Sarcoidosis is a multisystem disease characterized by the presence of noncaseating granulomas and although classically described in African Americans, it has one of its highest prevalences in the northern European population. Clinical variants exist with certain forms having diagnostic and prognostic value. Lofgren’s syndrome is the combination of erythema nodosum, bilateral hilar adenopathy, migratory polyarthralgias, and fever. This pattern is so consistent that it has 95% diagnostic specificity and allows diagnosis of sarcoidosis without a biopsy. Among European patients, the presence of Lofgren’s syndrome portends to a good prognosis. For mild disease symptomatic treatment with non-steroidal anti-inflammatory agents is reasonable or low dose prednisone may be added.
The optimal management of laryngotracheitis (croup) is determined by the severity of disease. There are numerous scoring systems for croup severity, with the Westley croup score being the most validated and most often used. The Westley croup severity scale includes evaluation for the presence of stridor at rest, retractions, and cyanosis as well as assessment of mental status and air entrance. Regardless of any official scoring system, most physicians would consider the presence of retractions and stridor at rest to be indications of moderate to severe disease that requires evaluation in the emergency department. The presence of cyanosis, confusion, depressed mentation, agitation, severe retractions, or absent breath sounds would indicate severe disease and/or the possibility of impending respiratory failure.
Mild cases of croup are treated on an outpatient basis with cool mist therapy and fluid replacement. Moderate cases may require supplemental oxygen, oral or intramuscular corticosteroids, or racemic epinephrine. Severe cases are best treated with hospitalization and racemic epinephrine.
Bottom Line: The most important step in initial management of laryngotracheitis includes nebulized epinephrine (racemic or L-epinephrine) and dexamethasone along with humidified oxygen, fever reduction, and hydration. Epinephrine acts almost immediately, while steroids have a delayed onset of action.
Pneumothorax is defined as a collection of air in the pleural space. The result is pleural separation of the visceral and parietal pleura. Spontaneous pneumothorax lacks an antecedent event (e.g. trauma). There are two types: primary and secondary. Primary spontaneous pneumothorax (PSP) occurs in patients without recognizable underlying lung disease. Secondary spontaneous pneumothorax (SSP) occurs in patients with visible underlying lung disease (e.g. COPD). The most common etiology of PSP is rupture of a subpleural bleb (which are usually not seen on imaging and are undiagnosed). Many cases initially diagnosed as PSP may eventually be diagnosed as SSP after further workup.
Management depends on the size of the pneumothorax. The spectrum of management includes watchful waiting, aspiration, chest tube insertion, and thoracoscopy with pleurodesis or lung resection.
Rhinosinusitis can be defined as either viral/bacterial and if bacterial, as complicated/uncomplicated. Complicated rhinosinusitis implies the extension of disease outside the nasal cavity/sinuses into adjacent structures, such as soft tissues, ophthalmologic tissues, and nervous system.
Current criteria for the presumptive (many of these cases may still be viral) diagnosis of acute bacterial rhinosinusitis (ABRS) include persistent symptoms lasting more than 10 days without any evidence of clinical improvement or a biphasic illness pattern which is also called double worsening, meaning the patient was sick, improved, and then became sicker a second time within a short time frame, usually within a 10 day period. The IDSA guidelines from 2012 also recommend the use of a high fever greater than 39C associated with severe symptoms for 3-4 days as being more consistent with bacterial rhinosinusitis. According to the guidelines by the American Academy of Otolaryngology-Head and Neck Surgery published in 2015, fever itself early in the course of illness is not sensitive or specific enough to warrant treatment based on this vital sign alone, and they do not recommend using this as criteria for the diagnosis of ABRS. They agree with the other criteria used by the IDSA and acknowledge that a "severe" presentation may warrant the use of antibiotics as recommended by the IDSA and the American Academy of Pediatrics which considers more than 3 days of high fever and purulent nasal discharge as a severe presentation of ABRS in children.
Summary Criteria for the Diagnosis of ABRS
Signs or symptoms of acute rhinosinusitis present for 10 days or more after symptom onset with no improvement
Acute worsening of improving rhinosinusitis within 4-6 days of symptom onset or "double-sickening."
Severe rhinosinusitis: onset of high fever greater than 39C and severe symptoms within 3-4 days of onset
Tx of ABRS: amoxicillin, amoxicillin-clavulanate, doxycycline if PCN allergic, or respiratory fluoroquinolone in kids who can't take doxycycline. I just had a pt in clinic who had bacterial rhinosinusitis and I gave him amoxicillin-clavulanate.
Bottom Line: In patients with ABRS who require antibiotic therapy, the initial therapy of choice is with amoxicillin with or without clavulanate.
One of the feared complications of acute bacterial rhinosinusitis (ABRS) is orbital cellulitis. This infection commonly develops in the setting of ABRS due to the direct extension of bacteria from the sinus cavity into the orbit. Commonly it can project through the roof of the maxillary sinus. Additionally, there can be extension through the adjacent soft tissues. The diagnosis of this condition is clinical and is confirmed with radiographic imaging (CT scan of the sinuses). The presence of pain/difficulty with eye movement, double vision, eye swelling, and erythema should be concerning for orbital infection. The initial imaging test of choice would be with a contrasted CT study of the face and orbits. An MRI could also be performed and has similar accuracy, but is generally slower and more expensive to obtain. Additionally, patients with suspected orbital cellulitis should be evaluated by ophthalmology in the emergency department and started on IV antibiotics with coverage for MRSA (vancomycin generally).
If the sinuses are the suspected source, ampicillin-sulbactam or piperacillin-tazobactam can be added to vancomycin as long as there is no concern for CNS involvement. If the CNS is involved, it should be noted that both ampicillin-sulbactam and piperacillin-tazobactam have relatively poor CNS penetration, and a 3rd generation cephalosporin (ceftriaxone) should be used with the addition of metronidazole for coverage of anaerobic organisms. General guidelines for sepsis and infection should be followed with the physician obtaining the regular laboratories including a complete blood count, metabolic profile, blood cultures, and lactate.
Symptoms of Complicated ABRS:
Proptosis or impaired extraocular movements
Painful eye movements
Diplopia or impaired vision
Periorbital edema or erythema
Cranial nerve palsies
Altered mental status
Neck stiffness/meningeal signs
Papilledema
Complications of ABRS:
Meningitis
Orbital cellulitis
Cavernous sinus thrombosis/thrombophlebitis
Preseptal cellulitis
Ruptured eardrum:
Tympanic membrane perforations are commonly caused by trauma or acute otitis media and are usually noted on otoscopic examination. Perforations with marked hearing loss or other concerning neurologic signs such as nystagmus, ataxia, or vomiting should receive a prompt evaluation by an otolaryngologist. Supportive care only is a perfectly reasonable treatment plan for patients with simple perforations with minimal hearing loss and no neurologic signs. Many perforations will heal spontaneously within 4 weeks and require no intervention.
#sarcoidosis#McConnell#Heerfordts syndrome#Lofgrens syndrome#Lofgren#croup#PTX#sinusitis#rhinosinusitis#ruptured ear drum
3 notes
·
View notes
Text
What may induce a pleural effusion?

A pleural effusion is a complication of many different conditions. The following are some of the more prevalent causes of pleural effusion.
Inflammation of the lung and pleura may be caused by lung infection (pneumonia), TB, and malignancy. This may result in the accumulation of fluid, resulting in a pleural effusion.
Some arthritic diseases may generate pleural inflammation in addition to joint inflammation. Pleural effusion, for example, is a rare consequence of rheumatoid arthritis and systemic lupus erythematosus (SLE).
Back pressure in the veins (blood vessels) that return blood to the heart is caused by heart failure. A small amount of fluid may leak from the blood vessels. Fluid swelling in the legs is common with heart failure, but a pleural effusion may also occur.
Low protein content in the blood also allows fluid to leak out of the blood vessels. Cirrhosis of the liver, for example, and certain renal diseases may result in a low quantity of blood protein, allowing a pleural effusion to form.
If you are facing this disorder, Consult Dr. Parthiv Shah one of the best Pulmonologist in Mumbai.
2 notes
·
View notes
Text
Purpose of Thoracoscopy in Pleural Mesothelioma
Purpose of Thoracoscopy in Pleural Mesothelioma
Diagnosis: Thoracoscopy is used to obtain tissue samples (biopsies) from the pleura for microscopic examination to confirm the presence of mesothelioma and determine its subtype.
Staging: The procedure helps assess the extent of tumor spread within the chest cavity and provides valuable information for staging the disease.
Therapeutic…
View On WordPress
0 notes
Text
Looking for the Best Chest Physician in Mumbai?

Lung Care with Mumbai's Premier Chest Physician, Dr. Parthiv Shah
Discover unparalleled lung care with Dr. Parthiv Shah, Mumbai's leading chest physician in Mumbai, at Sparsh Super Speciality Lung Clinic. With years of expertise in respiratory medicine, Dr. Parthiv ensures top-notch care for all lung-related concerns.
About Dr. Parthiv Shah - Chest Physician in Mumbai:
Dr. Parthiv Shah is a distinguished pulmonologist with extensive experience spanning over 8 years. Armed with qualifications including MBBS, MD (Pulmonary Medicine), and DNB (Pulmonary Medicine), along with a Fellowship in Pulmonary Diseases & Intensive Care, Dr. Parthiv is committed to excellence in patient care.
Why Choose Dr. Parthiv Shah?
Expertise: Benefit from Dr. Parthiv's profound understanding of pulmonary medicine, ensuring precise diagnoses and effective treatments.
Experience: With a wealth of experience, Dr. Parthiv has successfully treated countless patients with diverse lung conditions.
Personalized Care: Experience a compassionate and personalized approach to healthcare under Dr. Parthiv's expert guidance.
State-of-the-Art Facilities: Sparsh Super Speciality Lung Clinic boasts cutting-edge technology, guaranteeing the highest standards of care.
Services Offered:
Explore a comprehensive range of services tailored to meet your lung health needs:
Diagnosis and Treatment: From asthma and COPD to TB and pulmonary infections, Dr. Parthiv offers accurate diagnosis and effective treatment plans.
Procedures: Benefit from essential procedures including bronchoscopy, thoracoscopy, pleural tapping, allergy testing, and sleep studies, performed with precision.
Preventive Care: Receive invaluable guidance on maintaining optimal lung health and preventing respiratory issues.
Emergency Care: Rest assured, Dr. Parthiv is readily available for immediate assistance in emergencies.
Contact Us:
Your search ends here. Book an appointment today at Sparsh Super Speciality Lung Clinic with Dr. Parthiv Shah, chest physician in Mumbai. Call now at 93242 47349 | 90297 72904 for exceptional lung care tailored to your needs.
0 notes
Text
youtube
Star Hospitals, Financial District is proud to announce the inauguration of its state-of-the-art Interventional Pulmonology Suite. Take a virtual tour of this groundbreaking facility that marks a significant milestone in pulmonary medicine, offering a wide range of services, including the diagnosis and treatment of primary lung cancer, management of metastatic lung tumors, relief of airway obstructions, and treatment of pleural diseases. By prioritizing minimally invasive techniques and leveraging cutting-edge technologies, Star Hospitals aims to redefine pulmonary healthcare, ensuring better outcomes and enhanced quality of life for patients.
To book an appointment at Star Hospitals, Call: 07969250194
Visit: www.starhospitals.in/site/contactus
Follow Star Hospitals on Social Media for Daily Updates
#best hospital in hyderabad#best multispeciality hospital in hyderabad#best hospitals in nanakramguda#best hospital in banjara hills#hospitals in nanakramguda#best pulmonologist in hyderabad#Youtube
0 notes
Text
Top Uses of Chiba Needles in the Medical Field
Chiba needles, also known as Chiba biopsy needles, are thin and sharp medical instruments commonly used in various procedures within the medical field. These specialized needles have become an essential tool for physicians and healthcare professionals due to their versatility and effectiveness in a wide range of medical applications.
From diagnostic biopsies to therapeutic injections, Chiba needles have revolutionize the way medical procedures are perform, providing accurate and efficient results. In this article, we will discuss the top uses of Chiba needles in the medical field, highlighting their importance and impact on patient care.
What are chiba needles?
Chiba needles are thin, flexible needle that are use in various medical procedures to access specific areas of the body with precision. They are named after the Japanese radiologist who first introduced them, Dr. Chiba. These needles come in different lengths and gauges, making them versatile tools for healthcare professionals.
Top chiba needle applications in the medical field
1.Diagnostic Procedures
One of the primary use of Chiba needle is in diagnostic procedures such as biopsies and aspirations. These needles allow doctors to obtain tissue or fluid samples from deep within the body with minimal trauma to the patient. This is crucial in diagnosing conditions such as cancer or infections.
2.Pain Management
Chiba needle are also use in pain management procedures such as nerve blocks and epidural injections. By delivering medication directly to the source of pain, these needles can provide targeted relief for patients suffering from chronic pain conditions.
3.Biopsy Procedures
When it comes to performing biopsies, Chiba needle are essential tools for obtaining tissue samples from organs such as the liver, kidneys, or lungs. These needles are design to penetrate deep tissues safely and accurately, making them invaluable in the diagnosis of various diseases.
Read More : How to Choose the Right Biopsy Needle for Your Practice
4.Interventional Radiology
In the field of interventional radiology, chiba needle play a crucial role in procedures such as percutaneous drainage or ablation. These needles allow radiologists to access and treat tumors or fluid collections under imaging guidance, offering minimally invasive alternatives to traditional surgery.
5.Drainage Procedures
Chiba needles are commonly employ for various drainage procedures, including thoracentesis (draining fluid from the pleural space), paracentesis (draining fluid from the abdominal cavity), and pericardiocentesis (draining fluid from the pericardial sac). The sharpness and flexibility of Chiba needles facilitate smooth insertion and effective drainage, crucial for managing conditions such as pleural effusion and ascites.
6.Minimally Invasive Surgery
In minimally invasive surgical techniques such as laparoscopy and percutaneous procedures, Chiba needles find application in tasks such as tissue sampling, vessel cannulation, and suture placement. Their slender profile and precise control make them invaluable instruments for surgeons performing complex procedures through small incisions.
Conclusion: The Versatility of Chiba Needles
In conclusion, chiba needle are versatile instruments that have revolutionized the way medical procedures are performed. From diagnostic biopsies to pain management interventions, these needles continue to be indispensable tools in the medical field. So, the next time you hear about Chiba needle, remember their significant impact on patient care and the advancement of medical technology.
Source : Top Uses of Chiba Needles in the Medical Field
#Chiba Needles#Chiba biopsy needles#medical instruments#medical procedures#biopsies injections#Medical Device#Medication#Healthcare#Needle Manufacturers#Needle Suppliers
0 notes
Text
Revolutionize Recovery: Thoracic Drainage Catheters Unleashed
Technological developments in the medical field constantly change how patients are treated and allowed to heal. Thoracic drainage catheterization is one such innovation that is revolutionising the treatment of pulmonary diseases and thoracic surgery. These compact, yet mighty gadgets are transforming recuperation, providing patients with unprecedented ease, speed, and healing effectiveness.
The Thoracic Drainage Catheters: An Understanding
Chest tubes, sometimes called thoracic drainage catheters, are thin tubes that are put into the chest cavity to drain pus, fluid, or air to help the lungs return to normal. They are essential in the management of pleural effusion and pneumothorax, as well as in the post-operative care following thoracic procedures like lobectomy, pneumonectomy, or thoracotomy.
Changing the Course of Recovery:
In the past, receiving post-operative care meant longer hospital stays, more discomfort, and a higher chance of problems. But healing has changed dramatically since sophisticated thoracic drainage tube became available. These contemporary gadgets have a number of significant benefits:
Enhanced Comfort: Modern thoracic drainage catheters are made with the patient's comfort in mind, as opposed to previous types. Because of their smaller diameter, they cause less discomfort during the healing period and cause less tissue damage during insertion.
Quicker Recovery: Patients recover more quickly when they have better drainage capacities and a lower chance of problems. This enhances overall quality of life by resulting in shorter hospital stays and a quicker return to regular activities.
Minimised Complications: Modern thoracic drainage catheters are highly precise and successful in minimising the risk of complications, including bleeding, infection, and pneumothorax recurrence. This helps to ensure that patients have more comfortable recovery paths.
Tailored Solutions: With the wide range of sizes and configurations available for thoracic drainage catheters, medical professionals can customise treatment regimens to meet the specific requirements of each patient. Better results are encouraged and drainage efficiency is optimised by this customisation.
Case Studies:
In order to demonstrate the revolutionary nature of thoracic drainage catheters, let us examine two fictitious case studies:
A lobectomy is performed on 45-year-old Sarah in order to treat her early-stage lung cancer. In the past, difficulties from standard chest tube drainage would have meant a protracted hospital stay and recuperation period. But thanks to the use of contemporary thoracic drainage catheters, Sarah has very little pain, quick post-operative fluid drainage, and is sent home from the hospital a few days later, well on her road to a full recovery.
John, a 60-year-old male, has congestive heart failure and arrives with a massive pleural effusion. In the past, his condition would have needed to be managed with invasive surgeries and prolonged hospital stays. However, John has a minimally invasive thoracentesis operation with quick drainage and gets great symptomatic relief, allowing him to resume his daily activities sooner. This is made possible by the efficacy of modern thoracic drainage catheters.
A new era in patient treatment and recuperation has begun with the development of contemporary thoracic drainage catheter. These technologies are transforming the post-operative experience for patients having thoracic surgeries or treating pulmonary disorders by placing a high priority on comfort, efficiency, and customised solutions. Thoracic drainage catheters are expected to undergo additional developments and improvements as technology develops, leading to even better patient outcomes and quality of life.
0 notes
Text
Pleural Mesothelioma (Considerations for Biopsy)
Pleural Mesothelioma (Considerations for Biopsy)
Accuracy: Biopsies provide the most definitive way to diagnose pleural mesothelioma and distinguish it from other conditions, such as lung cancer or benign pleural diseases.
Risk and Recovery: Each biopsy method has its risks, including bleeding, infection, or pneumothorax (collapsed lung). The recovery time and potential complications depend on…
View On WordPress
0 notes