#pancreatitis liver enzymes
Text
Well Being: Is Keto Food Plan Safe For The Liver
Your healthcare supplier can use a big selection of enzyme and protein blood tests to check for certain health situations. For instance, elevated liver enzymes could probably be a sign of liver disease. If you have high levels of liver enzymes in your blood, you have elevated liver enzymes. High liver enzyme levels could additionally be temporary, or they might be an indication of a medical situation like hepatitis or liver illness. In cholangitis with incomplete extrahepatic obstruction, patients may have normal or barely raised serum bilirubin concentrations and high serum alkaline phosphatase exercise. Serum alkaline phosphatase is also produced in bone, and bone illness might complicate the interpretation of irregular alkaline phosphatase exercise.
The bile duct and pancreatic duct join on the duodenum, which is the primary part of the small gut. In situations where blood sugar supplies are low, the physique will preserve glucose for the mind, red blood cells, and kidneys. When this happens, the liver can produce an alternate gas supply from fat, often identified as ketones, by way of a course of referred to as ketogenesis. See your physician, however, should you experience unexplained weight loss, abdominal pain, jaundice, or different signs and signs that hassle you. Liver perform tests embody a quantity of different markers and should be interpreted with respect to every individual, together with their medical history, symptoms, and family historical past. If the liver is damaged or contaminated, it would release sure chemical compounds that can be detected throughout routine bloodwork.
If the liver values show elevations further diagnostics are often required to substantiate the liver disease and get a diagnosis. In some instances, veterinarians might recommend no additional investigation if the liver values are solely slightly elevated or there’s a known cause (e.g. rising dogs will usually have elevated ALP due to the B-ALP a serotype produced by bones). Elevation in ALT shows there has been injury to the hepatocytes but that doesn’t mean there's undoubtedly liver illness as diseases outdoors the liver may cause elevated ALT also (pre-liver). Examples include heart disease, intestinal irritation, and extreme dental illness.
elevated liver and pancreas enzymes
Some slow growing tumors may be surgically removed, because the liver is able to regenerate even if a big portion is removed. Your veterinarian will typically carry out an initial blood panel to get a baseline for their values, and proceed to check them on the hour mark. Your pup could additionally be positioned on IV fluids, receive fluid additives to restore any deficits, injectable drugs for any symptom management, and any other remedies which may be recommended for their current state of affairs. ALP is an enzyme that is found in highest concentration in the liver and the bone.
Side effects might include fainting, extreme bleeding and an infection, but these are rare. These are symptoms of your pancreatic functions beginning to interrupt down. If you lay your right hand across your stomach, that's roughly the size and form of your pancreas behind it.
#what cancers cause elevated liver enzymes#blood test for pancreatic cancer#pancreatic cancer blood test#blood tests pancreatic cancer#does pancreatic cancer show in blood tests#blood tests for pancreatic cancer#can elevated liver enzymes be cancer#does pancreatic cancer show up in blood work#pancreatic cancer labs#high liver enzymes cancer#blood test pancreatic cancer#blood work for pancreatic cancer#elevated liver enzymes in pancreatitis#pancreatic cancer diagnostic tests#elevated liver and pancreatic enzymes#what blood test shows pancreatic cancer#pancreatic cancer blood test results#pancreatitis elevated liver enzymes#labs for pancreatic cancer#pancreatitis liver enzymes#elevated liver enzymes pancreatitis#can pancreatitis cause elevated liver enzymes#pancreatic cancer bilirubin levels#can a blood test detect pancreatic cancer#can blood work detect pancreatic cancer#can blood test detect pancreatic cancer#pancreatic cancer bilirubin#pancreatic cancer blood test markers#does elevated pancreatic enzymes mean cancer#bilirubin pancreatic cancer
1 note
·
View note
Text
Carbohydrate Antigen Ca 19-9 Labcorp
After further evaluations, it was confirmed she had early-stage gallbladder cancer and was capable of take action. Lipase is a sort of digestive enzyme or "digestive juice." It helps your body digest fats. Most of your lipase is made in your pancreas, an organ situated behind the lower part of your stomach. Lipase can also be made in your salivary (spit) glands and in your stomach.
For most types of tumors, a biopsy is the one sure way for the doctor to know if an space of the physique has a tumor. In a biopsy, the physician takes a small sample of tissue for testing in a laboratory. If a biopsy just isn't attainable, the physician might recommend other tests that may assist make a diagnosis. About 15 percent to 20 p.c of patients with pancreatic cancer are identified early sufficient that their tumor could be eliminated surgically.
does elevated pancreatic enzymes mean cancer
A level lower than 40 mg/dL is considered low (and is a threat factor for coronary heart disease), while a level of 60 mg/dL or larger is considered protective in opposition to heart illness. Thyroid issues can have an effect on cholesterol levels, with hypothyroidism often causing a rise in cholesterol. Thus, a Lipid Panel test may be helpful in managing thyroid issues by monitoring cholesterol levels and adjusting treatment as needed. High LDL cholesterol and triglyceride levels, or low HDL cholesterol levels, can lead to the development of atherosclerosis, which might cause strokes if arteries supplying the mind are affected.
Further to this, the vast majority of research have assessed the utility of diagnostic biomarkers in sufferers with symptomatic illness, somewhat than as a surveillance or screening biomarker in the common inhabitants. Blood tests can consider the function of the gallbladder, liver, and pancreas. Levels of the pancreatic enzymes amylase and lipase can be measured. Blood tests can even check for signs of associated conditions, together with an infection, anemia (low blood count), and dehydration. A tumor marker referred to as CA 19-9 could also be checked if pancreatic cancer is suspected. Several attempts to improve the present diagnostic methods for pancreatic cancer and in flip its prognosis.
Elevated levels of ALT and AST, for example, could recommend liver cell injury or illness. High bilirubin levels might point to impaired liver operate or a blocked bile duct. These tests additionally assess albumin levels, which mirror the liver's ability to supply proteins, and alkaline phosphatase levels, which might point out bile duct or liver injury. Changes in the quantity or percentage of various varieties of white blood cells can present insights into numerous well being conditions. An increase in neutrophils, for instance, might point out an acute infection, whereas a rise in lymphocytes could also be seen in persistent infections or sure types of cancers. The secretin stimulation test is a sort of pancreatic operate test that’s somewhat extra invasive than a blood test or stool test.
#what cancers cause elevated liver enzymes#blood test for pancreatic cancer#pancreatic cancer blood test#blood tests pancreatic cancer#does pancreatic cancer show in blood tests#blood tests for pancreatic cancer#can elevated liver enzymes be cancer#does pancreatic cancer show up in blood work#pancreatic cancer labs#high liver enzymes cancer#blood test pancreatic cancer#blood work for pancreatic cancer#elevated liver enzymes in pancreatitis#pancreatic cancer diagnostic tests#elevated liver and pancreatic enzymes#what blood test shows pancreatic cancer#pancreatic cancer blood test results#pancreatitis elevated liver enzymes#labs for pancreatic cancer#pancreatitis liver enzymes#elevated liver enzymes pancreatitis#can pancreatitis cause elevated liver enzymes#pancreatic cancer bilirubin levels#can a blood test detect pancreatic cancer#can blood work detect pancreatic cancer#can blood test detect pancreatic cancer#pancreatic cancer bilirubin#pancreatic cancer blood test markers#does elevated pancreatic enzymes mean cancer#bilirubin pancreatic cancer
1 note
·
View note
Text
Acute Pancreatitis: Signs, Treatment, Causes, And Issues
My wife and I just bought a model new house and were in the strategy of decorating it and putting within the landscaping. When gallstones cause a severe attack of acute pancreatitis, the remedy plan may include attempts to remove the stone(s).
Unintended weight reduction is fairly common in individuals with pancreatic cancer. Veterinarians diagnose hepatic lipidosis based on a cat's history, bodily examination findings, blood tests, and abdominal ultrasonography. The diagnosis is confirmed by analyzing a sample of the liver taken with an ultrasound-guided needle. To diagnose some causes of hepatic lipidosis, a larger biopsy must be taken during surgery. This test is used to seek out out if you might have a condition that impacts your pancreas or salivary glands.
The alpha-2 adrenergic receptor is a G-protein coupled receptor (GPCR) current in all kinds of tissues, corresponding to vascular clean muscle, coronary arteries, salivary glands and the gastrointestinal tract. Its particular actions on the gastrointestinal tract embody contraction of sphincters and decreased motility of the graceful muscle inside the gastrointestinal tract [4, 5]. Activation of the alpha-2 receptor causes contraction of the hepato-pancreatic sphincter (sphincter of oddi), resulting in obstruction of pancreatic enzyme move through the pancreatic duct, resulting in acute pancreatitis.
Like IL-6, they're usually not utilized in clinical follow and are more expensive than sometimes used tests. Abdominal radiographs have a limited role in acute pancreatitis. In some circumstances, the inflammatory process might harm peripancreatic structures, resulting in a colon cut-off signal, a sentinel loop, or an ileus. The presence of calcifications within or across the pancreas might indicate persistent pancreatitis. Serum amylase and lipase levels are usually elevated in individuals with acute pancreatitis. In research research, amylase or lipase levels a minimal of 3 instances above the reference vary are typically considered diagnostic of acute pancreatitis.
Thus, this method appears to carry promise for the therapy of patients with ALD. Although alcoholic beverages comprise energy, analysis means that underneath sure conditions these energy wouldn't have as much worth for the physique as those derived from other nutrients. In addition, many alcoholics suffer from malnutrition, which might result in liver harm and impaired liver perform. Many drinkers take in lower than the really helpful day by day quantity of carbohydrates, proteins, fats, nutritional vitamins (A, C, and B, especially thiamine [B1]), and minerals (such as calcium and iron). Of the three enzymes, GGT is one of the best indicator of excessive alcohol consumption, but GGT is present in lots of organs and is elevated by different medicine as well, so high GGT levels do not necessarily mean the patient is abusing alcohol.
In addition, they could also have fever, loss of urge for food, weight loss, fatigue, night time sweats, joint pains and body aches. Celiac disease is a genetic autoimmune disorder that impacts both kids and grownup. If a child has celiac illness, consuming gluten will cause harm to finger-like projections, called villi, in the lining of the kid's small intestines. This, in flip, interferes with the small intestine’s capability to absorb vitamins in food, leading to malnutrition and a wide selection of different issues. The protein in wheat, barley, rye and oats collectively called “gluten” cause the immune system to form antibodies which then assault the villi. These youngsters with Celiac illness might undergo from symptoms corresponding to belly bloating, pain, gas, diarrhea, constipation, weight reduction, anemia, progress issues, and short stature.
high liver enzymes cancer
Many completely different tumours may occur inside the liver – some simply affecting the liver (primary liver tumours), some which have spread to the liver from elsewhere (secondary liver tumours). Unfortunately many liver tumours carry a poor prognosis, but this is not invariably the case and with some tumours (eg, lymphoma) chemotherapy could also be possible. Tumours confined to one lobe of the liver can also be amenable to surgical resection. Alcohol consumption and smoking cigarettes can improve the danger of pancreatitis. It is strongly really helpful quitting smoking cigarettes and drinking alcohol to stop pancreatitis.
Chronic pancreatitis is much less common and results in 86,000 hospital stays per year. In AP, the serum biochemical indexes of the liver often change, and adjustments in liver function will have an effect on the severity and prognosis of AP. Several drugs can elevate GGT levels, such as phenytoin, phenobarbital, carbamazepine, valproic acid, cimetidine, heparin, methotrexate, furosemide, isotretinoin, and acetaminophen. Likewise, oral contraceptives also can raise the enzyme’s serum level. The size of time you'll have the ability to successfully scale back GGT depends on your actions to deliver the degrees down. For example, if you hand over alcohol, you can see your GGT levels decrease considerably after a month.
#what cancers cause elevated liver enzymes#how is pancreatic cancer diagnosed#pancreatic cancer diagnosis#tests for pancreatic cancer#can elevated liver enzymes be cancer#does pancreatic cancer show in blood tests#high liver enzymes cancer#testing for pancreatic cancer#how do you diagnose pancreatic cancer#does pancreatic cancer show up in blood work#diagnosis of pancreatic cancer#most accurate test for pancreatic cancer#how do they test for pancreatitis#elevated liver and pancreatic enzymes#how do you check for pancreatic cancer#pancreatitis elevated liver enzymes#how is pancreatic cancer detected#pancreatic cancer diagnostic tests#pancreatic cancer blood test results#liver enzymes and pancreatitis#how to detect pancreatitis#pancreatitis liver enzymes#elevated liver enzymes pancreatitis#how do they diagnose pancreatic cancer#can pancreatitis cause elevated liver enzymes#pancreatic cancer bilirubin levels#what is the test for pancreatic cancer#diagnostic testing for pancreatic cancer#diagnose pancreatic cancer#pancreatic cancer how to diagnose
1 note
·
View note
Text

“According to Eastern medicine be it Indian, Chinese, Tibetan or Thai, the left side of the body is totally different from the right side. Even some Buddhist monastic traditions include within their precepts for monks to sleep on their left side. Although it sounds weird resting and sleeping on the left side has many health benefits.
The lymph drains to the left.
The left side of the body is the dominant side of the lymphatic system. Most of the lymph drains down to the thoracic duct which is located on the left side. In its path the lymph transports proteins, glucose metabolites and waste products that are purified by the lymph nodes to be drained to the left side.
Derived from the above it is common to deduct in Eastern medicine that the diseases of the left side of the body may be due to chronic congestion of the lymphatic system.
The priorities of the body.
According to ayurveda congestion occurs in the body following certain priorities. If the lymphatic system is digested, the liver and blood are subsequently saturated with toxic substances. Primary symptoms of congestion present on the left side of the body before moving to the right side where they make their later appearance.
Feeling bored after a meal?
The Indian suggestion is that if you take a break after eating, do it lying on your left side. The rest should not exceed 10 minutes and is different from the evening nap which is usually 20 minutes or more.
Stomach and pancreas hanging to the left side. When you lie on your left side both naturally hang allowing for optimal and efficient digestion. Food is driven to move naturally through the stomach and pancreatic enzymes are secreted in a paulatin way and not in a single stroke, which happens if you lie down on the right side.
Laying on your left side your liver and gallbladder hang from your right side. Resting on the left side allows them to hang and secret their precious enzymes into the digestive tract, emulsifying fats and neutralizing stomach acids.
When the digestive system is stimulated this way your digestive cycle is shorter and doesn't leave you stranded for the rest of the afternoon. Try resting 10 minutes on your left side after eating.
Feel energized and not tired after eating.
Try to eat in a relaxed way mid-day and don't forget to rest on your left side and check that you will feel more energized and with better digestion.
Sleeping magic from the left side.
Best elimination.
The small intestine flushes toxins through the ileocecal valve (VIC) on the right side of the body at the start of the large intestine. The large intestine travels down the right side of your body, crosses your stomach and descends down the left side.
Through the VIC, sleeping on the left side allows gravity to stimulate bodily waste into the large intestine from the small intestine more easily.
As the night passes and continue sleeping on your left side the debris moves more easily toward the downward column and morning removal will be easier.
Best cardiac function.
More than 80% of the heart is located on the left side of the body. If you sleep on the left side the lymph drained to the heart will be driven by gravity taking work out of your heart while you sleep.
The aorta, which is the largest artery in the body, comes out from the upper part of the heart and is arched left before going down to the abdomen. By sleeping on the left side, the heart pumps blood more easily into the downing aorta.
Sleeping on the left side allows the intestines to move away from the cava vein that brings blood back to the heart. Noticeably the cava vein rests on the right side of the thorn, so when you lie down on the left side the viscera move away from the cava veina. Again gravity makes the heart job easier.
The sparrow is on the left side.
The spleen is part of the lymphatic system and is also on the left side of the body. Its function is that of a large lymph node which filters the lymph and additionally filters the blood. When you lie on the left side the fluids return to the basin is easier and is more easily produced by gravity.
The lymphatic system drains all cells in the body through contractions and muscle movement and not by heart pumping. Helping the lymph drain into the pelvis and heart with gravity is a simple way to purify your body.
And while there are no scientific protocols on it, sleeping on the left side does make sense. Understanding ancestral wisdom based on knowledge of modern anatomy clears up many doubts about the reasons that exist in the east to sleep a certain way.”
Original article written by Dr. John Doull
[Leila L'Abate]
#sleep#Physiology#left side#Leila L'Abate#Dr. John Doull#quotes#articles#lymphatic system#Body Alive
24 notes
·
View notes
Note
I’M LATE BUT HAPPY VALENTINE’S DAY💜💜
Bio chem has been kicking my ass all day and I finally got a breather 😭
My Valentine’s Day gift to you

I can’t remember if I’ve sent this to you already but it’s okay because it’s ✨Rhys✨
Those thighs 🧎🏻♀️🧎🏻♀️
HIIIIIII!!!
Happy Valentines! OMGGG WHAT A HOTTIE!!!!
I'm sorry biochem is kicking ur booty! It is all about the pathways if I am being honest! Def make diagrams of the metabolic pathways and include the enzymes (and if they drive the reaction forward or backward or both) and you should be solid!
For some reason, we were also always tested on Vitamins and their deficiencies!
Vitamin C def = Scurvy = bleeding gums
Vitamin A def = night vision changes
Vitamin D def = rickets in kids; osteomalacia in adults
Vitamin B6 and B12 def = marcocytic anemia; methylmalonic acid increased in vitamin B12 def
Fat soluble vitamins = A, D, E, K = occurs with pancreatic insufficiency causing steatorrhea!
Vitamin K def = clotting disorder -> liver cant produce clotting factors: II, XII, IX, X - I remember as 1972 (10 - 9 - 7 - 2) AND protein C and S
Iron deficiency = microcytic hypochromic anemia + restless leg syndrome
Some med school factoids for you <3
Rhys would be very impressed with you for trying!!!
7 notes
·
View notes
Text
to the person who said i post ana content:
I am 90 lb because I have a deadly, dangerous, progressive, treatment and cureless disease called Chronic Pancreatitis Stage 2. I'm a nondiabetic hypoglucagonemic and have severe biliary dyskinesia and dyspepsia. My bilirubin, liver enzymes and trypsin are chronically high. This means I often live off an IV and may soon need an NG. I never drank, smoke or partied, my condition is considered unknown cause.
That is why I eat low fat, and weigh little. It is not because I find weighing little to be attractive or low fat recipes to be particularly endearing. I would very much like to take a pill that cures my pancreatitis and smash impossiwhoppers back to back, but there is no treatments or cures.
I hope that helps explain my behavior and relationship with food, to whomever was wondering.
5 notes
·
View notes
Text
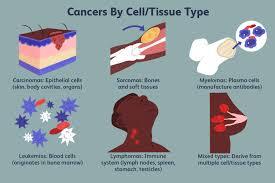
What are the common types of cancer?
There are numerous types of cancer, each affecting different organs and tissues in the body. Some of the most common types of cancer include:
Breast Cancer: Affects the breast tissue, most commonly in women but can also occur in men.
Lung Cancer: Arises in the lungs and is often associated with smoking but can also occur in non-smokers.
Prostate Cancer: Occurs in the prostate gland, which is part of the male reproductive system.
Colorectal Cancer: Develops in the colon or rectum and is often referred to as colon or rectal cancer.
Skin Cancer: Includes various types such as basal cell carcinoma, squamous cell carcinoma, and melanoma, which arise from different cells in the skin.
Bladder Cancer: Forms in the tissues of the bladder, which stores urine.
Non-Hodgkin Lymphoma: Affects the lymphatic system, which is part of the body's immune system.
Kidney Cancer: Develops in the kidneys, which filter waste from the blood to form urine.
Thyroid Cancer: Originates in the thyroid gland, which produces hormones that regulate metabolism.
Pancreatic Cancer: Occurs in the pancreas, an organ that produces enzymes for digestion and hormones that regulate blood sugar.
Ovarian Cancer: Affects the ovaries, which produce eggs and female hormones.
Leukemia: Cancer of the blood-forming tissues, including the bone marrow and lymphatic system, leading to abnormal production of white blood cells.
Liver Cancer: Arises in the liver, often in association with underlying liver disease such as cirrhosis or hepatitis.
Esophageal Cancer: Develops in the esophagus, the muscular tube that carries food from the throat to the stomach.
Brain Cancer: Can originate in the brain itself (primary brain cancer) or spread to the brain from other parts of the body (metastatic brain cancer).
These are just some of the common types of cancer, and there are many others that can affect various organs and tissues in the body. Each type of cancer has its own unique characteristics, risk factors, symptoms, and treatment options. Early detection and prompt treatment are crucial for improving outcomes and reducing the burden of cancer. Regular screenings, healthy lifestyle choices, and awareness of risk factors can help reduce the risk of developing cancer.
0 notes
Text
How is Alcohol-Induced Liver Disease Diagnosed?
Alcohol-induced liver disease (ALD) is a serious condition that results from excessive alcohol consumption. Diagnosing ALD requires a comprehensive approach involving clinical evaluation, laboratory tests, imaging studies, and sometimes a liver biopsy. If you are in Chennai and seeking the best gastroenterologist, Dr. Kumargurubaran is renowned for his expertise in diagnosing and treating liver diseases. This guide will walk you through the diagnostic process for ALD.
Clinical Evaluation
The first step in diagnosing alcohol-induced liver disease is a detailed clinical evaluation by a gastro specialist. The doctor will review your medical history, focusing on alcohol consumption patterns and any symptoms of liver disease, such as jaundice, fatigue, or abdominal pain. A physical examination is also crucial, during which the gastroenterologist will look for signs of liver enlargement or tenderness.
Laboratory Tests
Laboratory tests are essential in diagnosing ALD. Blood tests help assess liver function and detect markers of liver damage. The most common tests include:
Liver function tests (LFTs) to measure levels of liver enzymes, bilirubin, and proteins.
Complete blood count (CBC) to identify any blood abnormalities.
Tests for viral hepatitis to rule out other causes of liver disease.
These tests provide valuable information about the liver’s health and functionality, aiding the best gastroenterologist in Chennai in forming an accurate diagnosis.
Imaging Studies
Imaging studies, such as ultrasound, CT scan, or MRI, offer detailed views of the liver and can detect structural changes. An ultrasound is typically the first imaging test performed. It can reveal liver enlargement, fatty liver, or the presence of cirrhosis. Advanced imaging techniques like CT scans and MRIs provide more detailed images and can help assess the extent of liver damage.
Liver Biopsy
In some cases, a liver biopsy may be necessary to confirm the diagnosis of ALD. During this procedure, a small tissue sample is taken from the liver and examined under a microscope. This helps determine the severity of liver damage and identify specific changes associated with alcohol-induced liver disease. The best gastro surgeon in Chennai, such as Dr. Kumargurubaran, will perform this procedure with utmost precision to ensure accurate results.
Additional Diagnostic Tools
Endoscopy and ERCP (Endoscopic Retrograde Cholangiopancreatography) are additional diagnostic tools that might be used to evaluate complications related to ALD. These procedures allow for direct visualization of the gastrointestinal tract and bile ducts, helping to identify any blockages or abnormalities.
Seeking the Best Gastroenterologist in Chennai
If you suspect you have alcohol-induced liver disease, it’s crucial to seek medical attention from a qualified gastroenterologist. Chennai is home to some of the best gastroenterologists and gastro surgeons, such as Dr. Kumargurubaran. His extensive experience in treating liver diseases, gallbladder stones, pancreatitis, and performing advanced procedures like laparoscopic surgery and colonoscopy makes him a top choice for patients seeking comprehensive gastrointestinal care.
Whether you need a consultation for obesity awareness, colorectal surgery, or management of conditions like fistula in ano or constipation, Dr. Kumargurubaran and his team offer expert care tailored to your needs. Their expertise in hernia surgery, including complex cases like incisional, inguinal, umbilical, and ventral hernias, ensures that you receive the best treatment in Chennai.
For those dealing with gastrointestinal issues, from bile duct stones to pancreatitis, finding the best gastro specialist in Chennai is key to effective management and treatment. Dr. Kumargurubaran’s commitment to patient care and advanced medical techniques makes him a trusted name in the field of gastroenterology.
DrKumaragurubaran Best Gastroenterologist Surgeon in Chennai/Hernia/Gallbladder/Fistula/Laparoscopic Surgeon.
Address: Billroth Hospitals, B, block 43, Lakshmi Talkies Rd, Shenoy Nagar, Chennai, Tamil Nadu 600030
Phone: 093603 91740
#best gastro doctor chennai#best gastroenterologist in chennai#best gastro surgeon in chennai#gastro specialist in chennai#best laparoscopic surgeon chennai#best gastro surgeon chennai#best gastroenterologist chennai#gastro specialist chennai
0 notes
Text
Unraveling the Complexity: Exploring Pancreatic and Biliary Diseases
Introduction:
The pancreas and biliary system are integral components of the digestive system, playing crucial roles in digestion, nutrient absorption, and waste elimination. However, diseases affecting these organs can lead to significant morbidity and mortality if left untreated. In this blog, we will delve into the intricacies of pancreatic and biliary diseases, their causes, symptoms, diagnosis, and treatment modalities.
Pancreatitis:
Pancreatitis, inflammation of the pancreas, can be acute or chronic and is often triggered by factors such as gallstones, alcohol consumption, medications, or genetic predisposition. Acute pancreatitis manifests with sudden onset severe abdominal pain, nausea, vomiting, and elevated pancreatic enzymes. Chronic pancreatitis is characterized by recurrent episodes of abdominal pain, weight loss, and pancreatic insufficiency. Diagnosis involves clinical evaluation, imaging studies such as CT scans, and laboratory tests. Treatment aims to relieve symptoms, prevent complications, and address underlying causes through pain management, dietary modifications, enzyme replacement therapy, and, in severe cases, surgery.
Gallstone Disease:
Gallstone disease, one of the most common biliary disorders, occurs when gallstones form in the gallbladder or bile ducts. These stones can obstruct the flow of bile, leading to symptoms such as abdominal pain (biliary colic), nausea, vomiting, and jaundice. Diagnosis is typically made through imaging studies such as ultrasound or CT scans. Treatment options include lifestyle modifications, medications to dissolve stones, and surgical removal of the gallbladder (cholecystectomy) in symptomatic cases.
Biliary Obstruction:
Biliary obstruction occurs when the flow of bile from the liver to the small intestine is impaired, leading to jaundice, dark urine, pale stools, abdominal pain, and itching. Common causes of biliary obstruction include gallstones, tumors (benign or malignant), strictures, or inflammation of the bile ducts. Diagnosis involves imaging studies such as MRCP (magnetic resonance cholangiopancreatography) or ERCP (endoscopic retrograde cholangiopancreatography) to visualize the biliary tract. Treatment depends on the underlying cause and may include endoscopic interventions, surgical procedures, or palliative measures to relieve symptoms.
Pancreatic Cancer:
Pancreatic cancer is a highly aggressive malignancy with a poor prognosis, often diagnosed at an advanced stage due to nonspecific symptoms and lack of effective screening tools. Common symptoms include abdominal pain, jaundice, weight loss, and new-onset diabetes. Diagnosis involves imaging studies such as CT scans, MRI, and endoscopic ultrasound (EUS), followed by tissue biopsy for confirmation. Treatment options may include surgery, chemotherapy, radiation therapy, and targeted therapies, depending on the stage and extent of the disease.
Pancreatic and biliary diseases encompass a range of conditions affecting the pancreas and the biliary system, including the gallbladder, bile ducts, and associated structures. These diseases can be complex and challenging to diagnose and manage due to their often nonspecific symptoms and potential for severe complications.
Pancreatic Diseases
Acute Pancreatitis:
Definition: A sudden inflammation of the pancreas that can be mild or life-threatening.
Causes: Gallstones, chronic alcohol use, certain medications, and high triglyceride levels.
Symptoms: Severe abdominal pain, nausea, vomiting, fever, and a swollen abdomen.
Diagnosis: Elevated serum amylase and lipase levels, abdominal ultrasound, CT scan.
Treatment: Hospitalization for fasting, IV fluids, pain management, and treating the underlying cause (MDLinx) (MGMA Homepage).
Chronic Pancreatitis:
Definition: Long-term inflammation of the pancreas that leads to permanent damage.
Causes: Chronic alcohol consumption, genetic predisposition, and autoimmune conditions.
Symptoms: Chronic abdominal pain, malabsorption, weight loss, and diabetes.
Diagnosis: Imaging studies (CT, MRI), pancreatic function tests, and endoscopic ultrasound.
Treatment: Pain management, enzyme supplements, dietary changes, and addressing complications like diabetes (MDLinx) (MGMA Homepage).
Pancreatic Cancer:
Definition: Malignant tumor of the pancreas, often with poor prognosis.
Symptoms: Jaundice, weight loss, diabetes, and upper abdominal pain.
Diagnosis: Imaging (CT, MRI, endoscopic ultrasound), biopsy, and blood tests (CA 19-9).
Treatment: Surgery (Whipple procedure), chemotherapy, radiation therapy, and palliative care (MDLinx) (MGMA Homepage).
Biliary Diseases
Cholelithiasis (Gallstones):
Definition: Formation of stones within the gallbladder.
Symptoms: Often asymptomatic; can cause biliary colic, nausea, and vomiting if stones block ducts.
Diagnosis: Ultrasound, CT scan, and sometimes MRCP (magnetic resonance cholangiopancreatography).
Treatment: Dietary changes, pain management, and possibly cholecystectomy (surgical removal of the gallbladder) (MDLinx) (MGMA Homepage).
Cholecystitis:
Definition: Inflammation of the gallbladder, often due to gallstones blocking the cystic duct.
Symptoms: Severe right upper abdominal pain, fever, nausea, and vomiting.
Diagnosis: Ultrasound, HIDA scan, and blood tests showing elevated white blood cells.
Treatment: Hospitalization, antibiotics, fasting, IV fluids, and cholecystectomy (MDLinx) (MGMA Homepage).
Choledocholithiasis:
Definition: Presence of gallstones in the common bile duct.
Symptoms: Jaundice, dark urine, pale stools, and biliary colic.
Diagnosis: MRCP, ERCP (endoscopic retrograde cholangiopancreatography), and ultrasound.
Treatment: ERCP to remove stones, and possibly cholecystectomy to prevent recurrence (MDLinx) (MGMA Homepage).
Primary Sclerosing Cholangitis (PSC):
Definition: Chronic disease causing inflammation and scarring of the bile ducts.
Symptoms: Jaundice, itching, fatigue, and episodes of cholangitis.
Diagnosis: MRCP, ERCP, liver biopsy, and blood tests showing elevated liver enzymes.
Treatment: Symptom management, bile acid therapy, and eventually liver transplantation in advanced cases (MDLinx) (MGMA Homepage).
Diagnostic Techniques
Imaging: Ultrasound, CT scan, MRI, MRCP, and ERCP are crucial for visualizing the pancreas and biliary system.
Laboratory Tests: Blood tests to check liver function, pancreatic enzymes (amylase, lipase), and tumor markers (e.g., CA 19-9).
Biopsy: Fine-needle aspiration or surgical biopsy for histological examination.
Conclusion:
Understanding pancreatic and biliary diseases requires a multidisciplinary approach involving gastroenterologists, radiologists, and surgeons. Timely diagnosis and appropriate treatment are crucial to manage these conditions effectively and prevent complications.
For further reading and detailed information, you can explore the following resources:
MDLinx on Gastroenterology
Gastroenterology & Hepatology Journal
Medical Group Management Association (MGMA)
Pancreatic and biliary diseases pose significant challenges in clinical practice, requiring a multidisciplinary approach for effective management. Early recognition of symptoms, timely diagnosis, and appropriate treatment interventions are essential for improving outcomes and quality of life for patients affected by these conditions. Through ongoing research, advances in diagnostic techniques, and therapeutic innovations, healthcare providers continue to strive towards better understanding, prevention, and treatment of pancreatic and biliary diseases, offering hope to patients and their families facing these complex challenges.
Important Information:
Conference Name: 14th World Gastroenterology, IBD & Hepatology Conference
Short Name: 14GHUCG2024
Dates: December 17-19, 2024
Venue: Dubai, UAE
Email: [email protected]
Visit: https://gastroenterology.universeconferences.com/
Call for Papers: https://gastroenterology.universeconferences.com/submit-abstract/
Register here: https://gastroenterology.universeconferences.com/registration/
Exhibitor/Sponsor: https://gastroenterology.universeconferences.com/exhibit-sponsor-opportunities/
Call Us: +12073070027
WhatsApp Us: +442033222718

0 notes
Text
How does cystic fibrosis impact adults?
Impact of Cystic Fibrosis on Adults
Cystic Fibrosis (CF) is a genetic disorder that primarily affects the respiratory and digestive systems, but it can also have implications for other parts of the body. With advancements in treatment and care, more people with CF are living into adulthood. However, managing the condition in adults involves dealing with a range of challenges and complications.
Respiratory System
Chronic Lung Infections: Adults with CF often experience recurrent lung infections due to thick, sticky mucus that traps bacteria. Common pathogens include Pseudomonas aeruginosa and Staphylococcus aureus.
Reduced Lung Function: Over time, repeated infections and inflammation can lead to a decline in lung function, making breathing more difficult.
Bronchiectasis: The airways become permanently widened, leading to persistent cough, mucus production, and further infections.
Respiratory Failure: In severe cases, lung damage can progress to the point where the lungs cannot provide adequate oxygen to the body, requiring advanced interventions like oxygen therapy or lung transplantation.
Digestive System
Pancreatic Insufficiency: Thick mucus can block the ducts of the pancreas, preventing digestive enzymes from reaching the intestines. This leads to malabsorption of nutrients, malnutrition, and vitamin deficiencies.
Diabetes: CF-related diabetes (CFRD) is common in adults due to the damage to the pancreas. It shares characteristics of both Type 1 and Type 2 diabetes.
Liver Disease: Blockages in the bile ducts can lead to liver damage, cirrhosis, and portal hypertension.
Intestinal Issues: CF can cause intestinal blockages, gastroesophageal reflux disease (GERD), and distal intestinal obstructive syndrome (DIOS).
Reproductive System
Infertility: Most men with CF are infertile due to congenital absence of the vas deferens, which carries sperm from the testes. However, assisted reproductive technologies can help achieve pregnancy.
Reduced Fertility in Women: Thick cervical mucus can make it harder for sperm to reach the egg, but many women with CF can still conceive naturally or with assistance.
Musculoskeletal System
Osteoporosis: Due to malabsorption of calcium and vitamin D, adults with CF are at higher risk for osteoporosis and fractures.
Arthritis: Some adults may develop CF-related arthritis or musculoskeletal pain.
Psychosocial Impact
Mental Health: The chronic nature of CF can lead to anxiety, depression, and stress. The need for continuous treatment and hospitalizations can impact quality of life.
Social and Work Life: Managing CF often requires time-consuming treatments and frequent medical appointments, which can interfere with work and social activities.
Treatment and Management
Medications:
Bronchodilators: To open the airways.
Mucolytics: To thin mucus.
Antibiotics: To treat and prevent infections.
Pancreatic Enzymes: To aid digestion.
CFTR Modulators: Target the defective protein in CF and improve its function.
Airway Clearance Techniques: Daily physiotherapy to clear mucus from the lungs.
Nutritional Support: High-calorie diet, vitamin supplements, and enzyme replacements.
Exercise: Regular physical activity to maintain lung function and overall health.
Psychological Support: Counseling or therapy to help manage the emotional aspects of living with CF.
Advanced Therapies: Lung transplantation may be an option for those with severe lung disease.
Conclusion
While cystic fibrosis poses significant challenges for adults, ongoing advancements in medical care and treatment strategies are helping many individuals manage their condition more effectively and lead fuller lives. Comprehensive, multidisciplinary care is essential to address the complex needs of adults with CF, including respiratory, digestive, reproductive, and psychosocial aspects. Regular follow-up with healthcare providers specialized in CF care is crucial for optimizing health outcomes and maintaining quality of life.
0 notes
Text
Navigating the Digestive Maze: Exploring Gastroenterology
Introduction:
The human digestive system is a marvel of complexity, comprising a series of organs and processes that work together to break down food, absorb nutrients, and eliminate waste. From the moment food enters the mouth to its journey through the esophagus, stomach, intestines, and beyond, the digestive tract plays a crucial role in maintaining our overall health and well-being. However, when problems arise within this intricate system, the field of gastroenterology steps in to unravel the mysteries and provide solutions. In this blog, we'll embark on a journey through the digestive maze, exploring the fascinating world of gastroenterology and its significance in healthcare.
UCJournals provide a platform for , We cordially extend an invitation to researchers from all around the globe to submit their research work for publishing in our Global Journal Of Gastroenterology & Hepatology Research.
To know more, visit here: https://www.ucjournals.com/journals/global-journal-of-gastroenterology-hepatology-research/

Understanding the Digestive System:
Before delving into the realm of gastroenterology, it's essential to have a basic understanding of the digestive system's anatomy and function. The process begins in the mouth, where enzymes in saliva start breaking down food as it's chewed. The food then travels down the esophagus and into the stomach, where gastric juices further break it down into a semi-liquid substance known as chyme. From there, chyme enters the small intestine, where the majority of nutrient absorption occurs, facilitated by specialized structures called villi and microvilli. Finally, any remaining waste passes into the large intestine, where water is absorbed, and feces are formed before being expelled from the body.
The Role of Gastroenterology:
Gastroenterology is the branch of medicine focused on the digestive system and its disorders. Gastroenterologists are highly trained specialists who diagnose and treat a wide range of conditions affecting the esophagus, stomach, intestines, liver, gallbladder, and pancreas. They utilize various diagnostic tools and procedures, such as endoscopy, colonoscopy, imaging studies, and laboratory tests, to identify gastrointestinal (GI) issues accurately. From common ailments like acid reflux and irritable bowel syndrome (IBS) to more complex conditions such as Crohn's disease and liver cirrhosis, gastroenterologists play a vital role in managing digestive health and improving patients' quality of life.
UCJournals provide a platform for , We cordially extend an invitation to researchers from all around the globe to submit their research work for publishing in our Global Journal Of Gastroenterology & Hepatology Research.
To know more, visit here: https://www.ucjournals.com/journals/global-journal-of-gastroenterology-hepatology-research/

Common Gastrointestinal Disorders:
Let's take a closer look at some of the most prevalent gastrointestinal disorders that gastroenterologists encounter:
Gastroesophageal Reflux Disease (GERD): Characterized by chronic acid reflux, GERD can lead to heartburn, regurgitation, chest pain, and complications like esophagitis and Barrett's esophagus.
Inflammatory Bowel Disease (IBD): Including Crohn's disease and ulcerative colitis, IBD involves chronic inflammation of the digestive tract, causing symptoms such as abdominal pain, diarrhea, rectal bleeding, and weight loss.
Irritable Bowel Syndrome (IBS): A functional disorder of the intestines, IBS manifests as abdominal pain or discomfort, bloating, and changes in bowel habits without any evidence of structural damage.
Gallstones: Hardened deposits in the gallbladder, gallstones can cause abdominal pain, nausea, vomiting, and complications such as cholecystitis and pancreatitis.
Celiac Disease: An autoimmune disorder triggered by gluten consumption, celiac disease damages the small intestine and leads to symptoms like diarrhea, abdominal pain, fatigue, and malnutrition.
The Importance of Seeking Professional Care:
While some gastrointestinal symptoms may resolve on their own or with minor interventions, others require medical attention from a gastroenterologist. Ignoring persistent digestive issues or attempting to self-diagnose and treat can lead to complications and delayed recovery. Gastroenterologists have the expertise and resources to accurately diagnose GI disorders and develop personalized treatment plans tailored to each patient's needs. Whether it's lifestyle modifications, medications, endoscopic procedures, or surgery, their goal is to alleviate symptoms, promote healing, and improve overall digestive health.
UCJournals provide a platform for , We cordially extend an invitation to researchers from all around the globe to submit their research work for publishing in our Global Journal Of Gastroenterology & Hepatology Research.
To know more, visit here: https://www.ucjournals.com/journals/global-journal-of-gastroenterology-hepatology-research/

Conclusion:
Navigating the digestive maze can be challenging, but with the guidance of skilled gastroenterologists, patients can find their way to better gastrointestinal health. From routine screenings and preventive care to advanced treatments for complex conditions, gastroenterology offers a comprehensive approach to managing digestive disorders and optimizing well-being. By understanding the importance of digestive health and seeking timely medical care when needed, individuals can enjoy a higher quality of life and digestive comfort for years to come.
0 notes
Text
Exploring the Growth Trajectory of the Medium Chain Triglycerides Market: Trends, Opportunities, and Future Outlook
Medium Chain Triglycerides: An Essential Fat for Optimal Health
Introduction
Medium-chain triglycerides, commonly known as MCTs, are a type of saturated fatty acid that has many unique health benefits. MCTs are derived mainly from coconut and palm kernel oils and contain fatty acids that are 6-12 carbon atoms in length.
Chemical Composition of MCTs
The two most abundant MCTs are caprylic acid (C8) and capric acid (C10). Compared to other fats, MCTs are more easily digested and absorbed. When consumed, MCTs are sent directly to the liver from the digestive tract where they are used as a quick source of energy or converted into ketones to be used as fuel by the body. They do not require bile or pancreatic enzymes for breakdown and absorption like other fats.
Health Benefits of MCTs
Due to their unique properties, MCTs offer a variety of health benefits. Some key benefits include:
Weight Management: Medium chain triglycerides have been shown to increase feelings of fullness and reduce calorie intake. Several studies have found MCT oil supplementation to promote weight loss and reduce body fat when compared to other fats.
Energy and Endurance: As MCTs are rapidly absorbed and used for energy, they can boost physical and mental performance. MCTs have been used by athletes to increase stamina and endurance. They provide sustained energy without subsequent crash often seen with quick carbs.
Brain and Cognitive Function: MCTs are readily converted to ketones which are an efficient source of brain fuel. Higher ketone levels from MCTs may enhance memory, focus, and even help prevent neurodegenerative diseases. Supplementation has shown benefits for conditions like Alzheimer's and epilepsy.
Heart Health: Being saturated fats, MCTs do not negatively impact LDL cholesterol levels. They also raise HDL cholesterol and improve triglycerides. Studies even link MCTs to reduced risk of coronary heart disease.
Antimicrobial Properties: Caprylic acid, a major MCT, has potent antifungal and antibacterial properties. It supports digestive and immune health by inhibiting growth of pathogens.
Role in Mitochondrial Function: MCTs, when broken down into ketones, may positively impact mitochondrial functioning. This can boost overall energy levels, metabolism, and help prevent age-related damage and diseases.
Uses and Sources of Medium Chain Triglycerides
Some common uses and sources of MCTs include:
- MCT Oil: Primarily sourced from coconuts, MCT oil is colorless and relatively tasteless. It provides all the benefits of MCTs and is widely available as a dietary supplement.
- Palm Kernel Oil: Another plant source high in MCTs (about 65%), refined palm kernel oil supplies caprylic and capric acids. It is used in foods like chocolate.
- Coconut Products: Coconut meat/flakes and coconut milk naturally contain lauric acid (C12), the most abundant MCT. Coconut oil derived from mature coconuts supplies about 50% MCT content.
- Dietary Supplements: MCT powders are used in protein shakes, coffee creamers etc. while MCT oil softgels/capsules provide convenience as supplements.
- Specialty Foods: Products like MCT protein bars, MCT butter substitutes, and MCT-based ketogenic foods support ketogenic diets and lifestyles.
Recommendations for Use
For most benefits, 10-50 grams of medium chain triglycerides per day is recommended, depending on tolerance. Starting low at 1-2 tsp MCT oil per day and gradually increasing is advised. Consuming with foods helps tolerance. MCT supplements support weight loss, exercise performance, memory, and more when used regularly as part of a healthy lifestyle.
Conclusion
With so many health benefits and sources easily available, MCTs deserve recognition as an essential dietary fat. Their unique properties offer advantages over other fats and make them an excellent supplement for improving energy levels, weight control, brain health, and more. Including just small amounts of MCTs, whether from whole coconut products or purified supplements, can add value to one’s nutritional regimen.
0 notes
Text
How does Ponaxen 15mg work in the body?
Ponaxen 15mg, also known by its generic name Ponatinib, is a targeted therapy medication used primarily in the treatment of certain types of leukemia, particularly chronic myeloid leukemia (CML) and Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL). It belongs to a class of medications called tyrosine kinase inhibitors (TKIs).
The mechanism of action of Ponaxen 15mg (Ponatinib) revolves around its ability to inhibit the activity of certain enzymes called tyrosine kinases. These enzymes play a crucial role in cellular signaling pathways that regulate cell growth, division, and survival. In leukemia, abnormal activation of tyrosine kinases, particularly the BCR-ABL fusion protein in CML and Ph+ ALL, leads to uncontrolled proliferation of leukemia cells.
Ponaxen 15mg specifically targets and inhibits the activity of the BCR-ABL fusion protein, as well as other mutated forms of the ABL tyrosine kinase, including those with resistance mutations. By blocking the activity of these abnormal enzymes, Ponaxen 15mg helps to disrupt the signaling pathways that promote leukemia cell growth and survival.
In addition to its activity against BCR-ABL, Ponaxen 15mg also inhibits other tyrosine kinases such as FLT3, KIT, and FGFR, which may play a role in the growth and progression of certain types of leukemia.
By targeting specific molecular abnormalities driving the growth of leukemia cells, Ponaxen 15mg offers a targeted approach to treatment with the potential for improved efficacy and reduced toxicity compared to conventional chemotherapy.
It is important to note that while Ponaxen 15mg can be highly effective in many patients, it may also be associated with certain side effects, including cardiovascular events, liver toxicity, pancreatitis, and blood clotting disorders. Close monitoring by healthcare providers is essential to manage these side effects and optimize treatment outcomes.
0 notes
Text
Skin and supplements
I wrote a very long post earlier this morning discussing this.
Thankfully my skin is a lot better after using the steroids. Like I said I don't like using them and only use them when I have an emergency. I am hopeful they will remain this way for a while, now that it's warmer and less dry outside as well. I'm more hopeful now after seeing my skin heal. And even if my skin isn't perfect now, I'm still going to do microbial testing (both skin and gut) to find some solutions. I know this will be treated with gut supplements and a topical antibiotic if needed (I'll ask my dermatologist of an anti-inflammatory/anti-bacterial hand cream she can recommend because I'm sure she would know).
I also had pizza yesterday (with tomato sauce) and my hands did no flare up, yay! I did NOT take any anti-histamines and did not apply steroid creams until 12 hours later, and I would have had a flareup before 12 hours if I ate tomatoes. Tomatoes are NOT the problem, I've eaten tomatoes my whole life (with eczema) and never flared up after eating them. They're not the culprit. Though the fact that I'm reacting to a food in this manner means that I have a deeper root cause which is likely gut inflammation due to dysfunction and/or dysbiosis. Tomatoes are high in salicylates which are inflammatory and also high in histamine. I do have food allergies and mild eosinophilia, and I'm sure my eczema is linked to that.
I'm already taking a gut health supplement which is much better than taking nothing, though I still want to find a supplement more targeted to my personal gut issues (whether it be low HCl levels, not enough digestive enzyme, if I need l-glutamine for intestinal permeability, and which bacteria and yeast strains I can personally benefit from. But I have no ides what my issues are and I've never been officially tested. And I know the GI MAP test can help with identifying microbes and intestinal permeability, but I'm not sure how stomach acid and digestive enzyme levels can be identified. I'm sure enzymes can be measured on a pancreatic lab panel, and there is an online at home test where you can test your stomach acid levels by drinking 8 oz of water with 1 teaspoon of baking soda and waiting how long it takes until you burp. It sounds suspicious and maybe unsafe and I doubt it's that accurate. I can probably get similar results from drinking soda. I don't want to take risks, but I know HCl supplementation can be helpful because stomach acids can kill pathogens you swallow that can potentially infect your GI tract and cause inflammation if not killed. I'll speak to my functional medicine doctor about this.
And regarding my skin microbiome, in hopes I don't test positive for staph, I want to do a skin culture test at my dermatologist's office. I'm worried that my request may be denied, but I'll insist regardless. Everyone has microbes on their skin, but people with eczema have staph. aureus which can cause inflammation and disruption of the filaggrin protein which functions to promote skin barrier integrity.
I'm also happy I discovered Jennifer Fugo because I learned so much about the root causes of eczema, but in a scientific way that avoids all the pseudoscientific and wacky unsubstantiated stuff you see on the internet. She says detoxing isn't needed because your body already detoxes itself, which is true. I learned that I don't need to do a liver detox and the way I can protect my liver is to avoid consuming a lot of alcohol and fatty/sugary foods and be eating and supplementing with key nutrients, minerals and amino acids like magnesium, molybdenum, sulfur, vitamin B6, glycine, glutamine, and bioflavinoids which support its intrinsic detoxification biochemical pathways. I feel like regularly taking a multivitamin and magnesium glycinate as well as eating healthy foods rich in bioflavinoids can help here and I can avoid all the ciilantro, chlorella, milk thistle, and dandelion supplements because that can cause a headache and even some side effects I don't want to deal with (I got sick and nauseous last weekend and I believe it's from the liver supplement).
I also learned of the importance of healthy gut function and a microbiome balance. I know gut health is overhyped on the internet and gut issues are not the root cause of every condition out there. However there is definitely a heavy link between gut health and skin health. Skin health relies heavily on detoxification functions of your internal detoxing organs like the liver and gut and gut aspect of this process relies on proper gut function and microbiome balance.
So I'll speak to my functional medicine doctor about gut function and microbiome balance, and my dermatologist about a skin culture test.
The testing and healing process may take a while, but that's okay if I can manage my skin inflammation with topicals temporarily. So I'll definitely ask my dermatologist for some tacrolimus and any anti-inflammatory and anti-bacterial hand creams because I don't really know of any. But I should have both. After talking with my doctors and doing the testing, I will look for a hand cream (hopefully I don't test positive for staph) and a gut health supplement that will support my gut function and microbiome depending on where I have issues and that it can be targeted to my own gut issues. I'm taking one right now and I don't know if it's most compatible for me, but again it's better than nothing.
I will heal, I will become a healthier person and will prove people wrong. Just like how I proved my dentists wrong last year, I will prove dermatologists wrong this year. Eczema is not a skin disease, it has internal root causes.
0 notes
Text
Chronic Pancreatitis – All you need to know
Chronic Pancreatitis — All you need to know
Pancreatitis is inflammation of your pancreas. Pancreatitis can come and go quickly, or it can be a chronic problem. Treatment will depend on whether your pancreatitis is acute or chronic.
Chronic Pancreatitis:
Chronic pancreatitis is an inflammation of the pancreas that comes back consistently or occurs over a long period of time. People with chronic pancreatitis can have permanent damage to their pancreas and other complications. Scar tissue develops from this continuing inflammation. When pancreatitis damages these cells, it leads to diabetes in about 45 percent of people with chronic pancreatitis. Long-term heavy alcohol use can cause pancreatitis in adults. Dr. Srivatsan Gurumurthy Surgical Gastroenterologist in Chennai unravels the complexity of this condition, shedding light on its causes, symptoms, and long-term implications in a language that is both simple and engaging for everyone.
What causes Chronic Pancreatitis?
Although chronic pancreatitis is caused due to several reasons, 70% of cases are due
Alcohol
Tobacoo chewing
Smoking
Cystic fibrosis
Genetic factors
Hereditary
Symptoms:
Pain in your upper abdomen
Diarrhea
Fatty stools, which are loose, pale, and don’t flush away easily
Nausea and vomiting
Unexplained weight loss
Diabetes mellitus
Fatty and oily stools
Painful episodes can last for hours or even days. Some people find that eating or drinking can make their pain worse. As the disease progresses, the pain may become constant.
How Is Chronic Pancreatitis Diagnosed?
During the early stages of chronic pancreatitis, changes in your pancreas are difficult to see in blood tests. For this reason, blood tests typically aren’t used to diagnose the disease. However, they may be used to determine the amount of pancreatic enzymes in your blood. Blood tests may also be used to check blood cell counts along with kidney and liver function. Your doctor might ask you for a stool sample to test for levels of fat. Fatty stools could be a sign that your body isn’t absorbing nutrients correctly.
Treatment:
Treatment for chronic pancreatitis focuses on reducing pain and improving digestive function. The damage to pancreas can’t be undone, but with the proper care, the symptoms can be managed well. Treatment for pancreatitis can include medication, endoscopic therapies, or surgery.
Surgery For Chronic Pancreatitis:
Surgery is the primary treatment and helps relieving pain by decompressing the pancreatic duct. Sometimes a reasonable amount of pancreatic parenchyma is cored out to alleviate pain originating from the head of the pancreas. If there is severe pain that isn’t responding to medication, removing part of the pancreas can provide relief. Surgery may also be used to unblock the pancreatic duct, drain cysts, or to widen the duct if it’s too narrow. Avoidance of alcohol is mandatory, even if alcohol wasn’t the cause of pancreatitis. Avoid smoking because it can increase your risk of developing pancreatic cancer.
Have queries or concern?
Then Consult Dr. Srivatsan Gurumurthy for the proper consultation and treatment.
0 notes
Text
Dr. Karthik Mathivanan: Pioneering Pancreas Transplant Specialist in Chennai
Introduction: With a stellar career spanning over 15 years, Dr. Karthik Mathivanan stands as a distinguished multi-organ transplant surgery specialist in Chennai. His expertise encompasses liver, small bowel, kidney, and pancreatic transplantation and rehabilitation, making him renowned as one of the best liver doctors in the city. Currently serving as the Associate Director of Liver and Multi-organ Transplantation, as well as HPB surgery, at MGM Healthcare, Dr. Mathivanan is a founding member of India’s prestigious Liver Transplant Society. His wealth of experience equips him to address the myths, misinformation, and anxieties surrounding liver diseases, contributing to transformative healthcare in Chennai.
Liverindia’s Mission for Organ Health: Under the guidance of Dr. Mathivanan, Liverindia actively pursues key objectives to enhance organ health, particularly in the realm of pancreas transplantation:
Disseminating Awareness: Liverindia is dedicated to spreading accurate information about various liver diseases. Dr. Mathivanan utilizes his vast experience to debunk myths and provide clarity, not only about liver health but also about the intricacies of pancreas transplantation.
Promoting Health Practices: The initiative advocates for healthy practices, emphasizing the importance of early liver screenings. Dr. Mathivanan ensures the public receives timely and valuable health advice to maintain optimal organ health, including pre-transplant considerations for pancreas transplantation.
Guiding Life-saving Treatment: Liverindia serves as a guiding force for patients, offering essential information to direct them toward necessary life-saving treatments, with a specific focus on pancreas transplantation as a viable option.
Understanding Pancreas Transplantation: Pancreas transplantation is a surgical procedure aimed at replacing a malfunctioning pancreas with a healthy one from a deceased donor. Dr. Mathivanan's expertise in this intricate field ensures patients receive state-of-the-art care, with a focus on successful transplantation and post-operative recovery.
Conclusion: Dr. Karthik Mathivanan's role in pioneering pancreas transplants in Chennai reflects his commitment to transformative healthcare. His expertise, coupled with Liverindia's dedication, underscores a holistic approach to organ health. As a founding member of the Liver Transplant Society, Dr. Mathivanan continues to shape the narrative of transplantation in Chennai, offering hope and comprehensive care to those in need of pancreas transplantation. His contributions stand as a testament to the advancement of medical science and the improvement of lives affected by complex organ conditions in the vibrant city of Chennai.
0 notes