#osteomyelitis symptoms
Text
Condensing Osteitis: Symptoms, Diagnosis and Management
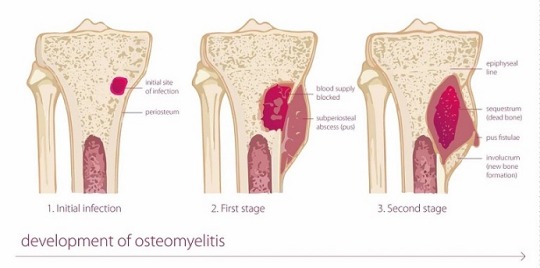
Focal sclerosing Osteomyelitis, also known as Condensing Osteitis, is an infection of the tissues around the root, or a periapical inflammatory disease. This is not a usual situation.
Here's some vital information to help you understand the fundamental features, symptoms, diagnosis, and treatment of this unusual tooth issue.

What is it?
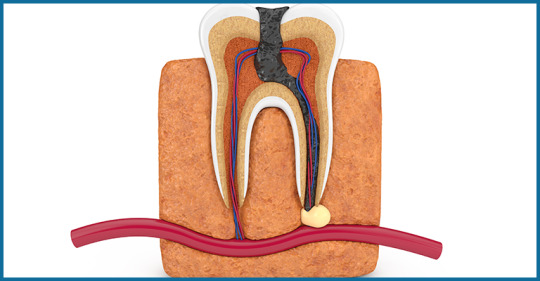
The tooth consists of two parts: the crown and the root. The crown is the visible component of the tooth inside the mouth, whereas the root is lodged inside the jaw bone. The periapical area refers to the area surrounding the apex or root tips. Condensing osteitis is an inflammatory illness affecting the periapical area. It is typically regarded as an inflammatory trigger.
Symptoms
It is usually symptomless with only intermittent episodes of discomfort, therefore your endodontist can identify it via an x-ray.
Condensing osteitis is most common in young people, however it can also occur in other age groups.
This disorder is more common in the molar region, but it can also occur in other tooth regions.
Diagnosis and Management
When condensing osteitis is detected, the first and most important action is to consult an endodontist. The care begins with a thorough evaluation of the affected tooth.
The endodontist will examine the pulp tissue of the tooth for vitality. The pulp tissue is the tooth's internal soft tissue, which contains nerves and blood vessels and helps to keep the tooth alive by providing sustenance.
This can be accomplished using a variety of pulp vitality testing procedures. The choice of test is determined on the patient's major complaint.
If the pulp contains necrosis or dead tissue, or if the inflammation is severe, the tooth must be extracted as it cannot be saved.
Prognosis
To your surprise, if the bone produced as a result of infection is not producing symptoms or discomfort, there is no need for treatment and the tooth can be left as is.
It has been discovered that such teeth remain normal and can work normally for years without any problems.
However, remember that a periodic checkup is required so that your endodontist can check for changes using x-rays. If necessary, the treatment can be performed. When the problematic tooth is taken, the socket left behind is the area of condensing osteitis of the jaw, and it can be left that way. It is painless and referred to as osteosclerosis of the bone scar.
For more information read the full blog here : https://www.orisdentalcenter.ae/blog/condensing-osteitis-symptoms-diagnosis-and-management/
#condensing osteitis#sclerosing osteitis#garre osteomyelitis#garre's sclerosing osteomyelitis#Osteomyelitis#osteomyelitis disease#osteomyelitis symptoms#Periodontitis#tooth psin#tooth infection#dental
0 notes
Note
Saw your post about Salem and it got me wondering if the oral mass in conjunction with the stomatitis is something that would be seen in other species as well?
One of my rescue bearded dragons came to me with osteomyelitis in his jaw (now treated) and has a small oral mass that was shown to be inflammatory and I do suspect the mass is linked to his osteo (secondary symptom?)
I've also seen it in dogs secondary to severe dental disease, but I don't know enough about bearded dragons to say one way or another. I recommend getting any growths evaluated by a vet as soon as possible. Even if benign oral growths do occur in that species, cancer is also always a possibility, and the sooner it's diagnosed and treatment (even if it's just palliative) started the better the outcome.
5 notes
·
View notes
Text
What are the Common Reasons for Sinus Surgery?
Sinus surgery, also known as sinusitis surgery or sinus surgery, is a medical procedure aimed at addressing various conditions affecting the sinuses. While sinusitis is often treated with medications and other conservative approaches, surgery becomes necessary in certain cases where these methods fail to provide relief or complications arise.

This comprehensive guide aims to delve into common ENT treatments like sinus and the reasons for sinus surgery, exploring the underlying conditions and indications for surgical intervention.
What is Sinus Anatomy and Function?
Before delving into the reasons for sinus surgery, it’s crucial to grasp the anatomy and function of the sinuses. The sinuses are air-filled cavities located within the skull bones, lined with mucous membranes. They play a vital role in humidifying and filtering the air we breathe, as well as producing mucus to trap bacteria and other harmful particles. However, when the sinuses become inflamed or infected, it can lead to various symptoms collectively known as sinusitis.
Common Causes of Sinusitis:
Sinusitis, characterized by inflammation of the sinuses, can be acute or chronic and may result from various underlying causes. Some common triggers of sinusitis include:
Viral Infections: The common cold and influenza viruses can lead to acute sinusitis by causing inflammation and swelling of the sinus linings.
Bacterial Infections: Bacterial sinusitis may develop as a complication of a viral infection or due to other factors such as anatomical abnormalities or impaired immune function.
Allergies: Allergic rhinitis, triggered by allergens such as pollen, dust mites, or pet dander, can inflame the sinus linings and contribute to chronic sinusitis.
Nasal Polyps: These benign growths arising from the nasal mucosa can obstruct the nasal passages and sinuses, leading to recurrent infections and inflammation.
Anatomical Abnormalities: Deviated nasal septum, nasal bone spurs, or narrow sinus openings (ostia) can predispose individuals to sinusitis by impairing sinus drainage and ventilation.
Treatment Approaches for Sinusitis:
The management of sinusitis typically involves a combination of medical therapies and lifestyle modifications. These may include:
Nasal Irrigation: Saline nasal irrigation helps flush out mucus and allergens from the nasal passages, promoting sinus drainage and relieving congestion.
Nasal Corticosteroids: Topical nasal corticosteroid sprays reduce inflammation and swelling in the nasal passages, improving symptoms and preventing recurrence.
Antibiotics: In cases of bacterial sinusitis, antibiotics may be prescribed to eradicate the infection and alleviate symptoms.
Decongestants: Oral or nasal decongestants can provide temporary relief from nasal congestion by shrinking swollen nasal tissues.
Allergy Management: Avoiding allergens and using antihistamines or allergy shots can help control allergic rhinitis and prevent sinusitis exacerbations.
Indications for Sinus Surgery:
Despite optimal medical management, some individuals may experience persistent or recurrent sinusitis symptoms that significantly impair their quality of life. In such cases, sinus surgery may be recommended to address underlying anatomical issues or to improve sinus drainage and ventilation. Common indications for sinus surgery include:
Chronic Sinusitis: When sinusitis symptoms persist for more than 12 weeks despite medical treatment, surgery may be considered to alleviate symptoms and prevent complications.
Recurrent Acute Sinusitis: Individuals experiencing frequent episodes of acute sinusitis (four or more episodes per year) may benefit from surgery to reduce the frequency and severity of recurrences.
Sinus Complications: Severe or complicated sinusitis, such as sinus abscess, osteomyelitis (bone infection), or orbital cellulitis (eye socket infection), may require surgical intervention to drain the affected sinuses and prevent further spread of infection.
Nasal Polyps: Large or recurrent nasal polyps that obstruct the nasal passages and sinuses despite medical therapy may necessitate surgical removal (polypectomy) to improve breathing and reduce the risk of recurrence.
Anatomical Abnormalities: Structural issues such as deviated septum, nasal bone spurs, or concha bullosa (enlarged nasal turbinates) that obstruct sinus drainage or ventilation may be corrected surgically to restore normal sinus function.
Types of Sinus Surgery:
Several surgical procedures may be performed to address sinusitis and related complications. These include:
Functional Endoscopic Sinus Surgery (FESS): FESS is the most common type of sinus surgery, performed using an endoscope inserted through the nostrils to access and remove obstructive tissues, polyps, or diseased sinus linings while preserving healthy tissue.
Balloon Sinuplasty: This minimally invasive procedure involves inserting a small balloon catheter into the sinus ostia and inflating it to widen the narrowed openings, promoting drainage and ventilation.
Septoplasty: Septoplasty is a surgical procedure to correct a deviated nasal septum, which may contribute to sinusitis by obstructing sinus drainage pathways.
Turbinoplasty: Turbinoplasty aims to reduce the size of enlarged nasal turbinates (concha bullosa) to improve nasal airflow and sinus drainage.
Sinus Ostial Dilation: In this procedure, specialized instruments or balloons are used to dilate and enlarge the sinus ostia, facilitating drainage and ventilation.
Conclusion
Sinus surgery is a valuable treatment option for individuals with chronic or recurrent sinusitis, nasal polyps, or anatomical abnormalities that impair sinus function. By addressing underlying issues and improving sinus drainage and ventilation, surgery can alleviate symptoms, reduce the frequency of recurrences, and enhance the quality of life for affected individuals. However, surgery is typically reserved for cases where conservative therapies have been ineffective, and the benefits outweigh the risks. A thorough evaluation by our otolaryngologist (Ent Specialist) at our ENT department provided the most appropriate treatment approach for each individual
Thangam Hospital, the best ENT hospital in Palakkad provides the ultimate care for sinus issues. We ensure world-class care with the most advanced technology support
Schedule a consultation with us to know more about the best sinus surgery treatments and procedures in managing sinusitis and related conditions.
0 notes
Text
Differentiating Between Bone and Muscle Pain

Pain is the body’s way of signaling that something isn’t quite right. However, not all pain is the same, and understanding the source of your discomfort is crucial for effective treatment. Two common types of pain that people often confuse are bone pain and muscle pain. While they can feel similar at times, they originate from different sources and require different approaches for management. In this blog, we’ll delve into the nuances of bone pain and muscle pain, helping you decipher the code to differentiate between them.
Understanding Bone Pain:
Bone pain typically originates from the bones themselves or the connective tissues surrounding them. It can be dull, achy, or sharp, depending on the underlying cause. Common causes of bone pain include fractures, osteoporosis, osteoarthritis, bone infections (such as osteomyelitis), and bone cancer.
When you experience bone pain, it often feels deep and localized to a specific area. You might notice tenderness, swelling, or redness around the affected area. Bone pain may worsen with movement or weight-bearing activities and can sometimes be accompanied by stiffness or limited range of motion.
Differentiating Muscle Pain:
On the other hand, muscle pain originates from the muscles or the soft tissues surrounding them. It can range from mild discomfort to severe, debilitating pain. Muscle pain can be caused by overuse, injury, tension, inflammation, or conditions such as fibromyalgia or muscular dystrophy.
Muscle pain tends to feel more superficial compared to bone pain. It may present as soreness, tightness, cramping, or aching sensations in the affected muscles. Unlike bone pain, muscle pain often improves with rest and worsens with activity. You may also notice swelling, bruising, or knots (trigger points) in the muscles experiencing pain.
Distinguishing Factors:
While bone pain and muscle pain share some similarities, several key differences can help you differentiate between them:
Location: Bone pain tends to be localized to a specific area overlying the bone, whereas muscle pain may affect a broader area surrounding the muscles.
Nature of pain: Bone pain is often described as deep, dull, or throbbing, while muscle pain is more likely to feel achy, sore, or cramp-like.
Aggravating factors: Bone pain typically worsens with movement or weight-bearing activities, whereas muscle pain may improve with rest and worsen with activity.
Associated symptoms: Bone pain may be accompanied by tenderness, swelling, or redness around the affected area, whereas muscle pain may present with swelling, bruising, or knots in the muscles.
Treatment Approaches:
Once you’ve identified whether your pain stems from bones or muscles, you can implement appropriate treatment strategies:
Bone Pain:
Rest: Limit activities that exacerbate bone pain and allow adequate time for healing.
Pain management: Over-the-counter pain relievers or prescription medications may help alleviate discomfort.
Physical therapy: Gentle exercises and stretches can improve mobility and strengthen surrounding muscles.
Medical interventions: Depending on the underlying cause, treatments such as immobilization, orthotics, or surgical procedures may be necessary.
Read more
0 notes
Text
Spinal infections are typically caused by bacteria or fungi. These microorganisms can enter the spine through various means, including bloodstream infections, surgical procedures, or infections in nearby tissues.
Conditions like diabetes, immunosuppression, or intravenous drug use can increase the risk of developing spinal infections. In some cases, the specific cause may be challenging to identify.
Diagnosis of spinal infections involves a combination of medical history review, physical examination, and diagnostic tests. Imaging studies such as MRI or CT scans are often crucial for identifying abscesses, osteomyelitis, or discitis in the spine. Blood cultures and other laboratory tests help determine the causative microorganism.
A biopsy may be performed in certain cases to confirm the diagnosis and guide appropriate treatment.
While routine health checkups can identify some general health issues, they may not always specifically detect spinal infections early. Spinal infections often present with symptoms such as back pain, fever, and neurological changes, which may prompt further investigation.
However, including spine-related assessments or imaging studies as part of comprehensive health checkups can contribute to the early detection of certain spinal conditions. Get full body health checkup at the best hospitals in India, for early detection and better treatment for various spinal conditions.
#health#full body checkups#surgery#healthcare#spine injury#spine infections#spinal cord injury#spinal surgery
1 note
·
View note
Text
Understanding Diabetic Ulcers: Causes, Symptoms, and Treatment
Diabetes is a chronic condition that affects millions of people worldwide, and one of its potential complications is the development of diabetic ulcers. These ulcers pose a significant threat to the well-being of individuals with diabetes, leading to complications that can have severe consequences if not addressed promptly. In this blog post, we will delve into the intricacies of diabetic ulcers, exploring their causes, symptoms, and available treatment options.
What Are Diabetic Ulcers?
Diabetic ulcers are open sores or wounds that commonly develop on the feet or lower extremities of individuals with diabetes. They result from a combination of factors, including poor circulation, nerve damage (neuropathy), and impaired immune function. Diabetes can lead to reduced blood flow to the extremities, making it harder for the body to heal wounds and fight off infections.
Causes of Diabetic Ulcers:
Peripheral Neuropathy: Diabetes can damage the nerves, particularly those in the feet, leading to loss of sensation. This lack of feeling makes individuals less aware of injuries or pressure on their feet, increasing the risk of developing ulcers.
Poor Circulation: Diabetes can cause blood vessels to narrow and harden, reducing blood flow to the extremities. Inadequate blood supply hinders the healing process and makes it easier for infections to take hold.
Foot Deformities: Individuals with diabetes may experience changes in the shape of their feet, such as hammertoes or Charcot foot, increasing the likelihood of developing pressure points and ulcers.
Symptoms of Diabetic Ulcers:
Recognizing the symptoms of diabetic ulcers is crucial for early intervention and prevention of complications. Common signs include:
Persistent redness or swelling
Open sores or wounds that are slow to heal
Drainage or pus from the ulcer
Increased warmth in the affected area
Foul odor
Complications:
If left untreated, diabetic ulcers can lead to severe complications, including cellulitis (a bacterial skin infection), osteomyelitis (bone infection), and, in extreme cases, amputation. The combination of compromised immune function and poor blood circulation creates an environment conducive to infections that can quickly escalate if not addressed promptly.
Treatment Options:
Wound Care: Proper wound care is essential for diabetic ulcers. This involves cleaning the wound, applying topical medications, and using dressings to promote healing and prevent infection.
Offloading Pressure: Offloading pressure from the affected foot or area is crucial to allow the ulcer to heal. This may involve the use of special footwear, casts, or braces.
Antibiotics: If an infection is present, antibiotics may be prescribed to combat bacterial growth. It's important to complete the full course of antibiotics as directed by a healthcare professional.
Surgical Intervention: In more severe cases, surgical procedures may be necessary to remove infected tissue or correct underlying issues contributing to ulcer development.
Prevention:
Preventing diabetic ulcers is key to minimizing the associated risks. Some preventive measures include:
Regular foot inspections
Proper foot hygiene
Choosing appropriate footwear
Managing blood sugar levels
Seeking prompt medical attention for any foot issues
Conclusion:
Diabetic ulcers are a serious complication of diabetes that require vigilant management. Individuals with diabetes must prioritize foot care, and healthcare professionals play a crucial role in educating patients about the risks and preventive measures. By understanding the causes, recognizing symptoms early, and implementing effective treatment strategies, it is possible to mitigate the impact of diabetic ulcers and improve overall quality of life for those affected.
0 notes
Text
What are the potential complications of untreated peripheral neuropathy?

Untreated peripheral neuropathy can lead to various complications, including:
Loss of Sensation: Persistent numbness and tingling can result in injuries that go unnoticed, leading to burns, cuts, or other wounds that may become infected.
Foot Ulcers: Reduced sensation and poor circulation in the feet can increase the risk of developing ulcers, which can be slow to heal and may become infected.
Falls and Injuries: Balance problems and muscle weakness associated with peripheral neuropathy can increase the likelihood of falls and injuries.
Muscle Atrophy: Over time, untreated neuropathy can lead to muscle wasting or atrophy, further reducing strength and mobility.
Chronic Pain: Untreated neuropathic pain can become chronic and debilitating, negatively impacting an individual's quality of life.
Decreased Mobility: As symptoms progress, individuals may experience difficulty walking and performing everyday activities, reducing their overall mobility and independence.
Autonomic Nervous System Dysfunction: Some forms of peripheral neuropathy can affect the autonomic nervous system, leading to issues like digestive problems, irregular heart rate, and blood pressure fluctuations.
Charcot Joint: In severe cases, untreated neuropathy can cause Charcot joint, a condition where the bones in the foot or ankle break down, leading to deformities and joint instability.
Infections: Foot ulcers and injuries that go unnoticed due to decreased sensation can become infected, potentially leading to serious infections, including cellulitis or osteomyelitis.
Reduced Quality of Life: The chronic pain, loss of mobility, and other complications associated with untreated peripheral neuropathy can significantly diminish a person's overall quality of life.
It's essential to seek medical attention and follow a treatment plan if you are diagnosed with peripheral neuropathy to help prevent or manage these potential complications. Early intervention and proper management can often improve symptoms and reduce the risk of complications.
It's essential to consult with Dr. Amit Shah, a healthcare professional or Neurologist in Mumbai practicing at Dr. Amit Shah Neurology Clinic for a proper diagnosis and individualized care.
0 notes
Text
Spinal infections can be the result of microorganisms invading any part of your spine. This can happen through a number of symptoms. While symptoms vary with the type of infection, vertebral osteomyelitis and discitis are common types of infection. Consider each in detail and if you see any symptoms then contact spine infection specialist doctor in Ahmedabad.
1 note
·
View note
Text
condensing osteitis : Symptoms and Treatments

What is Condensing Osteitis?
Focal Sclerosing Osteomyelitis, also known as Condensing Osteitis, represents a rare yet intriguing condition affecting the periapical region of teeth. While encountering this ailment is uncommon, it can manifest even in individuals adhering to diligent oral hygiene practices. Understanding its fundamental aspects, symptoms, diagnosis, and management is pivotal for dental practitioners and patients alike.
At its core, Condensing Osteitis perturbs the periapical area surrounding a tooth's root. Unlike typical inflammatory responses leading to bone degradation, this condition prompts bone deposition, rendering the affected area radiopaque on X-rays, contrasting with the usual radiolucency associated with bone destruction.
Symptoms of Condensing Osteitis are typically subtle, often presenting as sporadic episodes of discomfort rather than persistent pain. Although prevalent among young adults, it can manifest across different age groups, with a notable predilection for the molar region, albeit occurrences in other dental regions are not unheard of.
When suspecting Condensing Osteitis, prompt referral to an endodontist is imperative. Diagnosis commences with a comprehensive examination of the afflicted tooth. Pulp vitality testing, tailored to the patient's symptoms, aids in assessing the condition of the tooth's innermost tissues. In cases of severe inflammation or necrosis, extraction may be the only viable recourse to prevent further complications.
Remarkably, if the bone deposition remains asymptomatic, intervention may not be necessary, and the affected tooth can be left untreated. Long-term prognosis suggests that such teeth can maintain normal function for extended periods, although regular monitoring through X-rays is advisable to detect any changes necessitating intervention.
In instances where extraction is deemed necessary, the resultant socket represents an area of jaw osteosclerosis, devoid of pain and commonly known as a bone scar. Monitoring these sites for any developments is prudent, although intervention may not be warranted if they remain asymptomatic.
Final Thoughts
While condensing Osteitis may be rare, its impact on dental health merits attention. Understanding its nuances empowers dental professionals to provide timely and effective management, ensuring optimal outcomes for patients. Vigilance through regular check-ups enables early detection of any changes, facilitating appropriate interventions when needed.
FOR MORE INFO VISIT OUR BLOG ON CONDENSING OSTEITIS
0 notes
Text
Diabetic Foot Care: Understanding the Importance of Preventive Measures

According to the National Institutes of Healthcare, 7% of the world’s population is living with diabetes as of 2021, and is set to increase to 8.3% by 2030. And 80% of the diabetic population lives in developing countries. One of the crucial topics to discuss in diabetes is foot care since the extremity of a Diabetic foot ulcer (DFU) can get the patient’s leg amputated.
In this article let us dive deep into understanding diabetic foot care and a few insights on upcoming diabetes conferences and why you should attend them.
The Impact of Diabetes on Foot Health.
The patients with this condition are mostly elder people with a prolonged history of diabetes Mellitus and poor health conditions.DFU is caused by two important contributing factors which are neuropathy and peripheral artery disease.
Neuropathy can cause insensitivity towards any pain and pressure sensed in the foot, which is a threat because it alters the healing process, And with the peripheral vascular disease it would become even worse because the wound becomes ischemic and develops into a nonhealing ulcer.
Neglecting diabetic foot care can have serious repercussions. Sensation loss can result in unrecognized foot injuries, which can escalate to ulcers and infections if left untreated. In severe situations, these infections can extend to the bone and cause osteomyelitis, which can be fatal. Without prompt treatment, amputation may become the only choice to keep the illness from spreading. Upcoming Diabetes Conference 2023 is an insight ocean about diabetology and metabolic functions with 10+ workshops on diabetology and cardiology.
Importance of Preventive Measures in Diabetic Foot Care.
Daily Foot Inspection: Examining the feet daily is critical for spotting any problems early on. Diabetics should inspect their feet every day for wounds, blisters, redness, swelling, or symptoms of infection.
Foot Hygiene: It is critical to keep the feet clean and dry to avoid infections. Infections can be reduced by washing the feet with mild soap and warm water, followed by thorough drying (particularly between the toes).
Proper Nail Care: Diabetics should trim their toenails gently, avoiding cutting them too short or at an angle. Ingrown toenails, which can lead to infections, can be avoided with proper nail care.
Wear Proper Footwear: Foot health must wear comfortable, well-fitting shoes. Shoes should have enough room for the toes, and a cushioned sole, and should protect the foot from damage. Individuals should also avoid walking barefoot, especially at home, to reduce the chance of injury.
Regular Podiatry Check-ups: Individuals with diabetes must see a podiatrist, a healthcare expert who specializes in foot care, regularly. A podiatrist can detect any foot problems early on and treat them effectively.
Regulating Blood Sugar Levels: Properly regulating blood sugar levels can lower the incidence of foot problems. Consistent blood sugar regulation aids in nerve function and circulation, all of which are favorable to foot health.
Avoid smoking: Smoking can impair blood circulation, increasing the risk of foot issues in diabetics. Quitting smoking has been shown to improve foot health and general well-being.
Diabetic foot care is a key component of overall health maintenance and is not an optional aspect of diabetes management. Neuropathy and peripheral vascular disease can hurt foot health, leading to major problems if not treated properly. Preventive interventions are critical in lowering the incidence of diabetic foot ulcers, infections, and amputations. The cardiology conference discusses more on diabetic care in general and it has an exclusive workshop on foot care for Diabetes.
Individuals with diabetes can actively prevent foot-related issues by performing daily foot inspections, keeping correct sanitation, regulating blood sugar levels, wearing appropriate footwear, and getting frequent podiatrist check-ups. Implementing these preventive actions allows people to take control of their foot health and improve their overall quality of life.
To summarize, diabetic foot care is a proactive approach that can make a huge difference in the lives of people living with diabetes, allowing them to live healthy, meaningful lives while avoiding preventable foot-related issues.
Attend our 2nd Cardio Metabolic Congress an International Cardiology Conference and network with expert cardiologists and diabetologists.
Visit Now - https://bioleagues.com/cardio-metabolic-conference.php
#Upcoming Diabetes Conference#Diabetes Conference#International Diabetes Conference#Cardiology Conference
0 notes
Text
Mandibular Osteomyelitis Treatment Market Growth, Segments, Demand and Forecast to 2028
Global Mandibular Osteomyelitis Treatment Market, By Types (cute and secondary chronic osteomyelitis and primary chronic osteomyelitis.), Symptoms (fever, fatigue, pain, swelling and redness over the area of infection), ,Treatment (steroids, chemotherapeutic agents, bisphosphonates, Surgery), Cause (staphylococcus bacteria) End-Users (Clinics, Hospitals, Diagnostic centres, Home healthcare, others), Distribution Channel (Hospital Pharmacy, Retail Pharmacy, Online Pharmacy), Country (U.S., Canada, Mexico, Brazil, Argentina, Peru, Rest of South America, Germany, France, U.K., Netherlands, Switzerland, Belgium, Russia, Italy, Spain, Turkey, Hungary, Lithuania, Austria, Ireland, Norway, Poland, Rest of Europe, China, Japan, India, South Korea, Singapore, Malaysia, Australia, Thailand, Indonesia, Philippines, Vietnam, Rest of Asia-Pacific, Saudi Arabia, U.A.E, Egypt, Israel, Kuwait, South Africa, Rest of Middle East and Africa) Industry Trends and Forecast to 2028.
An expert team performs systematic, object-oriented and complete market research study to provide the facts associated with any subject in the field of marketing via Mandibular Osteomyelitis Treatment marketing report. The report has a lot to offer to both established and new players in the Mandibular Osteomyelitis Treatment industry with which they can completely understand the market. SWOT analysis and Porter’s Five Forces analysis methods are used wherever applicable, while generating this report. One of the most important parts of an international Mandibular Osteomyelitis Treatment market report is competitor analysis with which businesses can estimate or analyse the strengths and weaknesses of the competitors.
Key Players
The major players covered in the Global Mandibular Osteomyelitis Treatment Market are Pfizer Inc., Akorn, Sandoz International GmbH, Merck Sharp & Dohme Corp., Novartis AG, Cipla Inc., Sun Pharmaceutical Industries Ltd., Apotex Inc., among other domestic and global players. Market share data is available for Global, North America, Europe, Asia-Pacific (APAC), Middle East and Africa (MEA), and South America separately. DBMR analysts understand competitive strengths and provide competitive analysis for each competitor separately.
Browse More Info @ https://www.databridgemarketresearch.com/reports/global-mandibular-osteomyelitis-treatment-market
With the help of credible Mandibular Osteomyelitis Treatment market analysis report, businesses can make out the reaction of the consumers to an already existing product in the market. The report includes estimations of recent state of the market, CAGR values, market size and market share, revenue generation, and necessary changes required in the future products. A wide-ranging competitor analysis helps build superior strategies of production, improvement in certain product, its advertising or marketing and promotion for the business. Exhaustive and comprehensive market study performed in the wide ranging Mandibular Osteomyelitis Treatment market report offers current and forthcoming opportunities that put light on the future market investment.
Key questions answered in the report:
Which product segment will grab a lion’s share?
Which regional market will emerge as a frontrunner in coming years?
Which application segment will grow at a robust rate?
Report provides insights on the following pointers:
Market Penetration: Comprehensive information on the product portfolios of the top players in the Mandibular Osteomyelitis Treatment Market.
Product Development/Innovation: Detailed insights on the upcoming technologies, R&D activities, and product launches in the market.
Competitive Assessment: In-depth assessment of the market strategies, geographic and business segments of the leading players in the market.
Table Of Content
Part 01: Executive Summary
Part 02: Scope Of The Report
Part 03: Global Market
Part 04: Global Market Size
Part 05: Global Market Segmentation By Product
Part 06: Five Forces Analysis
More Reports:
Diuretic Drugs Market
Patient Engagement Technology Market
Healthcare Business Intelligence Market
Chinese Hamster Ovary cells (CHO) Market
Anti-cancer Drug Market
About Us:
Data Bridge Market Research set forth itself as an unconventional and neoteric Market research and consulting firm with unparalleled level of resilience and integrated approaches. We are determined to unearth the best market opportunities and foster efficient information for your business to thrive in the market
Contact:
Data Bridge Market Research
Tel: +1-888-387-2818
Email: [email protected]
0 notes
Text
Exploring Osteomyelitis: Causes, Symptoms, and Available Treatments
1. Osteomyelitis
2. Bone and Marrow Inflammation
3. Bone Marrow Infection
4. Bone and Joint Inflammation
5. Infectious Bone Marrow Disease
Introduction:
Inflammation of the bone marrow and adjacent bone is a condition that can affect the body's overall health. The bone marrow is responsible for producing red blood cells, white blood cells, and platelets that help the body fight infections and maintain healthy blood flow. Inflammation of the bone marrow and adjacent bone can cause pain, discomfort, and may lead to complicati...
Read More.
https://statesandcounties.com/2023/06/22/an-inflammation-of-the-bone-marrow-and-adjacent-bone-inflammation-of-bone-marrow-and-adjacent-bone-symptoms/?feed_id=5249&_unique_id=649b22c3a39d8
0 notes
Text
Osteomyelitis: A How to Guide to Management and Treatment
Osteomyelitis: A How to Guide to Management and Treatment
Learn how to effectively manage and treat osteomyelitis with this comprehensive guide. Understand the causes, symptoms, and treatment options.
Read the full article
0 notes
Text
Back Pain Treatment in Pune | Back Pain Specialist in Pune - Dr. Sachin Mahajan
Back pain is one of the most popular common problems and potentially serious disease. It can turn out to be so debilitating for certain patients that it obstructs their capacity to take participate in regular activities. Dr. Sachin Mahajan is a renowned back pain specialist and spine specialist in Pune, gives Best Back Pain Treatment in Pune at Sahyadri Hospital Pune.
The Maximum majority of the general people have encountered back pain eventually in their lives. The treatment of this back main may vary with the different causes of the reason for the pain. Many examples of back pain are the aftereffect of a muscle strain. Fortunately, such back pain, for the most part, mends rapidly in half a month or months. Depending upon the reasons for back pain treatments in Pune can vary from person to person, so it is commonly advisable to recover a back pain diagnosis from an accomplished medicinal expert.

What are the types of Back Pain?
Back pain is a pain in any area of the back. It is separated into neck pain (cervical), center back pain (thoracic), lower back pain(lumbar) or coccydynia (tailbone or sacral pain) in light of the section affected. The lumbar area is the most widely recognized region for Pain, as it supports the vast majority of the weight in the upper area.
Most instances of the intense back as well as leg pain may not require any examinations and will recuperate with initial treatment. Contingent upon the presumed getting an x-ray, blood examinations and an MRI scan might be asked. Tests that might be requested incorporate an x-ray, CT scan of the lower spine, or MRI of the lower spine.
What are the causes of Back Pain?
Strained muscles and ligaments.
Disc Injuries.
Herniated discs causing nerve compression resulting in Sciatica.
Piriformis syndrome.
Causes due to infection and Autoimmune disorders.
Spinal Canal Stenosis, Scoliosis, Spondylosis, Spondylolisthesis, Sacro-iliac Joint Dysfunction.
In some cases caused by metastatic cancers, Spinal Osteomyelitis, and Epidural Abscess.
What are the symptoms of Back Pain?
Low back pain might begin as acute due to an injury but can become chronic.
Dull aching pain in lower back accompanied by mild or severe muscles spasms &decreased range of motion
Sometimes low back pain includes a sharp, tingling, shooting pain that can radiate down the thighs to the leg and feet
Pain worsens during sitting
Pain that feels better while changing positions
Inability to stand up straight without pain
What are the Back Pain Treatment options in Pune?
How Lower Back Pain is Diagnosed
The first step for successfully treating lower back pain is to record an appointment with your primary care doctor. Before the appointment, take note of your symptoms. Back pain doctors may ask specific questions to gain better perceptivity into the sustaining cause of your pain.
Questions may include:
The spot of your pain
The intensity of your pain
Quality of your pain
Your medical history including any prior treatments or studies you’ve shared and how you’ve responded to the treatment.
The primary purpose behind Upper Back, Mid Back and Low Back pain is musculoskeletal imbalances. Hip misalignment causes serious musculoskeletal pain and compensation resulting in Disc prolapse, Spinal stenosis, Sacro-iliac joint dysfunction resulting in Pain. Dr. Sachin Mahajan is the best spine surgeon at Sahyadri hospital Pune providing all treatments regarding spine surgery and neurosurgery.
Generally, the current medical methods focus on reducing the pain, however, these back pain treatments don’t eliminate the underlying source of pain. The exact reason for back pain is never found in up to 85% of cases and often the diagnosed “cause” of back pain is the clearest structural harm that can be seen on an X-ray or MRI, yet is frequently not the real reason for the pain and can lead to unnecessary and possibly hurtful medical procedures and different interventions.
0 notes
Text
What is the importance of hyperbaric medicine?

Hyperbaric medicine is a branch of medicine that uses high-pressure oxygen chambers to treat a variety of illnesses. The value of hyperbaric medicine resides in its capacity to quicken the healing of a variety of illnesses, including decompression sickness, carbon monoxide poisoning, and wounds.
The capacity of hyperbaric therapy to speed up wound healing is one of its main advantages. Hyperbaric treatment can increase the quantity of oxygen given to tissues and encourage the creation of new blood vessels by subjecting the body to high-pressure oxygen. For this therapy, a special chamber is used where the air pressure is 1.5 to 3 times higher than usual, allowing a person to breathe only pure oxygen. The objective is to provide the blood with adequate oxygen to heal tissues and return the body to its natural state. This improved oxygenation can aid in hastening the healing of a number of wounds, including those brought on by radiation, surgery, and burns.
Carbon monoxide poisoning can be effectively treated using hyperbaric treatment. A poisonous gas called carbon monoxide binds to hemoglobin in the blood, preventing oxygen from reaching the body's tissues. By increasing the quantity of oxygen available to tissues and removing carbon monoxide from the body, hyperbaric therapy can help avoid long-term brain damage and other consequences.
The treatment of decompression sickness is a significant additional use of hyperbaric medicine. This ailment, commonly referred to as "the bends," happens when nitrogen bubbles develop in the blood and tissues as a result of abrupt pressure shifts, like those experienced by scuba divers. By reducing the size of these bubbles and increasing the oxygen available to tissues, hyperbaric therapy can help treat symptoms and avoid long-term consequences.
Other medical diseases like traumatic brain injury, stroke, and multiple sclerosis are among the ailments that hyperbaric medicine may be able to cure. It is still used today to treat people suffering from carbon monoxide poisoning, such as firefighters and miners. Additionally, it has received approval for more than a dozen ailments, from bone disease to burns, including:
poisoning by carbon monoxide
Crush wounds
Cyanide toxicity
A type of gangrene known as "gas gangrene" occurs when gas builds up in tissues.
a sudden or traumatic reduction in artery blood flow
Decompression sickness
Insecure skin flaps and grafts
damage from delayed radiation
Osteomyelitis is an infection of the bone that is unresponsive to other treatments.
(Air or gas embolism) A blood vessel that has a trapped air or gas bubble
Necrotizing soft tissue infection, often known as flesh-eating disease
Diabetes lesions that are not adequately healing.
A persistent infection known as actinomycosis
While more studies are required to determine whether hyperbaric therapy is effective for these conditions, preliminary findings are encouraging.
Hyperbaric medicine offers therapeutic advantages in addition to being reasonably safe and non-invasive. While there are some potential side effects of hyperbaric therapy, such as ear and sinus pain, these side effects are usually minor and manageable with the right precautions.
Hyperbaric medicine is significant because it may accelerate healing and enhance results in a range of medical disorders. It is conceivable that as hyperbaric therapy research advances, we will find even more applications for this ground-breaking therapy.
0 notes
Text
Hyperbaric Oxygen Therapy for Wound Healing: Benefits, Risks, and Effectiveness

Hyperbaric Oxygen Therapy (HBOT) is a medical treatment that involves breathing pure oxygen in a pressurized chamber. Hyperbaric Oxygen Therapy (HBOT) is a non-invasive medical treatment that uses pure oxygen at high pressure to promote wound healing. It has been gaining popularity in recent years as a safe and effective way to treat a wide range of conditions.
At Aadicura Superspeciality Hospital, which is considered as one of the best superspeciality hospital in Vadodara, we are proud to bring this advanced technology to our city, which can treat a wide range of serious conditions, including radiation injuries, non-healing wounds like diabetic foot ulcers, infections that destroy tissue in the skin or bone, burns, crushing injuries, at-risk skin grafts or flaps, brain abscesses, carbon monoxide poisoning, arterial gas embolism, decompression sickness, and many more.
The team at Aadicura Superspeciality Hospital is composed of highly trained medical professionals and some of the best vascular surgeons in Vadodara.
How does HBOT work?
Hyperbaric oxygen therapy (HBOT) involves breathing pure oxygen while inside a pressurized chamber. The purpose of this therapy is to increase the amount of oxygen that is delivered to the body’s tissues, which can promote healing and improve various medical conditions.
During a hyperbaric oxygen therapy session, the patient enters a chamber that is pressurized to a level higher than the normal atmospheric pressure. This pressure forces more oxygen into the patient’s blood plasma, allowing it to reach areas of the body that may have low oxygen levels due to injury or disease.
The high levels of oxygen in the body promote the growth of new blood vessels, stimulate the release of growth factors, and enhance the body’s natural healing processes. Additionally, the increased oxygen levels can help to reduce inflammation and swelling, which can improve the symptoms of many medical conditions.
Which conditions can be treated by HBOT?
Many Endovascular Hospitals in Vadodara use HBOT to treat a variety of conditions, including:
● Carbon monoxide poisoning
● Decompression sickness
● Non-healing wounds, such as diabetic foot ulcers
● Radiation injury
● Skin flaps and grafts that failed
● Gangrene
● Necrotizing soft tissue infections (which happen when the majority or all of the cells in a specific area of the body die from illness, trauma, or a lack of blood flow)
● Osteomyelitis (a bone infection and/or inflammatory condition)
● tissue damage brought on by radiation
● extreme burns
● Traumatic ischemia (a condition wherein only a portion of the body receives blood flow)
and many more.
The therapy is typically administered in a series of sessions, and the number of sessions required will depend on the individual patient and their specific condition.
Benefits of HBOT
There are several benefits to using HBOT for wound healing:
It can significantly speed up the healing process, reducing the time it takes for wounds to close and heal.
It can reduce the risk of infection by promoting the growth of healthy tissue and killing harmful bacteria.
It can help to reduce pain and discomfort associated with chronic wounds, promoting better mobility, thus improving the patient’s quality of life.
It increases blood flow.
Reduces swelling and inflammation
It enhances the body’s defences against free radicals, which can accumulate in cells and harm them.
It encourages the development of fresh blood vessels.
Are there any risks involved in treatment through HBOT?
As with any medical treatment, there are some risks associated with HBOT. The most common side-effects include ear pain, sinus pain, and/or changes in vision. These side effects are usually mild and temporary. It is not necessary that all patients undergoing HBOT experience these symptoms.
In rare cases, more serious complications such as lung damage or seizures can occur due to oxygen toxicity. It is important to discuss the risks and benefits of HBOT with a qualified healthcare professional before undergoing treatment.
How Does HBOT Work for Wound Healing?
HBOT works by increasing the amount of oxygen in the body, which helps to promote healing. When the body receives more oxygen, it can enhance its natural healing abilities and stimulate the growth of new blood vessels, allowing for better circulation to the affected area.
Effectiveness of HBOT for Wound Healing
HBOT has been shown to be effective for wound healing in numerous studies. HBOT significantly improves the healing rate of chronic wounds when used in combination with other standard wound care treatments.
HBOT can be an effective treatment for a wide range of conditions, particularly those that are difficult to heal using traditional therapies. Our team of one of the best vascular surgeons in Vadodara have treated conditions such as diabetic foot ulcers, failed grafts, burn injury cases and many more using HBOT, with most patients experiencing complete healing within six weeks of treatment.
Are the Benefits of HBOT Permanent?
The benefits of HBOT are not necessarily permanent, as wound healing can be affected by various factors such as underlying health conditions, lifestyle choices, and environmental factors. However, with proper wound care and management, the effects of HBOT can be long-lasting.
How Many HBOT Sessions are Needed?
The number of HBOT sessions needed for wound healing can vary depending on the severity of the wound and the individual patient. Typically, patients receive between 10–30 HBOT sessions, each lasting between 60–90 minutes. It is important to note that HBOT should be performed under the supervision of a trained medical professional.
Conclusion:
HBOT promotes healing by helping grow new skin along with forming new blood vessels and their connective tissues. Along with being highly effective and safe, it can also significantly improve the healing rate of chronic wounds and promote better overall quality of life for patients. If you are considering undergoing HBOT for wound healing, be sure to discuss the risks and benefits at Aadicura Multispeciality Hospital which is considered one of the best vascular surgery hospitals in Vadodara.
0 notes