#mucormycetes
Text
Mucormycosis (research post)

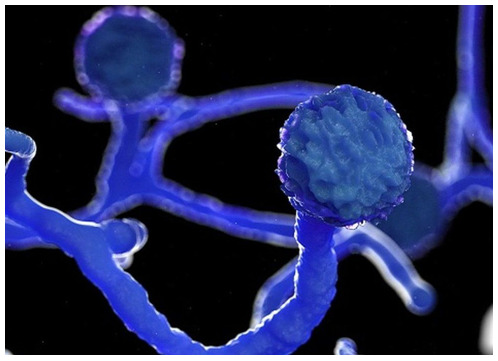
Mucormycosis is also known as ‘black fungus’ and it is a very serious and rare fungal infection
How is it caused?:
Mucormycetes are a type of mold that is present in our environment, usually in soil and organic matter in the process of decay (i.e compost).
Usually coming into contact with this type of mold is harmless, however mucormycosis typically presents in people with compromised immune systems.
There are five different types of mucormycosis:
Pulmonary mucormycosis (Infection of the lung)
Gastrointestinal mucormycosis (Infection of the GI tract)
Cutaneous mucormycosis (Infection of the skin)
Disseminated mucormycosis (Infection spread through the bloodstream)
Symptoms: The symptoms may vary for each type of mucormycosis however it generally presents as a respiratory or skin infection
Fever
Headache
Cough
Nasal congestion
Sinus pain
Swelling
Redness
Blisters
Ulcers
Blackened skin tissue
Treatment:
Mucormycosis is treated with a prescription antifungal medication, and is usually given intravenously or orally. The primary medication given is isavuconazole. However amphotericin B or posaconazole can also be administered depending on the patient's requirements.
___
Note: Second post and all I can say is....wow. This was a bit scary to think about how doing something as normal as like hanging around in a park or playing in the grass and soil could lead to something so detrimental, stay safe everyone. Here's another badly made meme that I couldn't stop laughing at for some reason- and I hope you all have an amazing day!

0 notes
Text
Mucormycosis, also known as black fungus, is a rare but serious fungal infection that has recently emerged as a post-COVID complication in some patients. Proper mucormycosis treatment is crucial given its high mortality rates and the limited timeline...
#Mirari #MirariDoctor #MirariColdPlasma #ColdPlasma
0 notes
Text
Mucormycosis Treatment in homeopathy
A group of moulds known as mucormycetes are the source of the deadly but uncommon fungal infection known as mucormycosis (formerly known as zygomycosis). These moulds are present everywhere in the environment. People with health issues or those who take medications that reduce the body's capacity to fight infection and disease are more likely to develop mucormycosis.
youtube
TREATMENT PLAN OF BRAHM HOMEOPATHIC HEALING & RESEARCH CENTRE
Brahm research based, clinically proved, scientific treatment module is very effective in curing this disease. We have a team of well qualified doctors who observe and analysis your case systematically, record all the signs and symptoms along with progress of disease, understand its stages of progression, prognosis and its complications. After that they clear you about your disease in details, provide you proper diet chart [what to eat or what not to eat], exercise plan, life style plan and guide you about many more factors that can improve your general health condition with systematic management of your disease with homeopathic medicines till it get cured.
0 notes
Text
Black Fungus: All You Need To Know
Commonly referred to as the Black Fungus, Mucormycosis is a rare fungal disease that comes from a mold that grows on decaying and rotting organic matter. Mucormycetes is the fungal mold that causes the infection and when a person is exposed to this, it affects the sinus and the eye region. The infection mainly affects those whose immune system is already weak or are under medication. The infection spreads when the body is not strong enough to fight the illness on its own.
0 notes
Text
Mucormycosis (Black Fungus) And COVID 19.
Catastrophic second wave of COVID 19 has left millions of people infected and dead. India is experiencing the world’s worst outbreak with not only rising COVID cases but also an alarming upsurge in a rare and potentially life-threatening fungal infection, Mucormycosis.
What is Mucormycosis?
According to CDC, Mucormycosis (black fungus) is a serious and rare fungal infection caused by a group of molds called mucormycetes. These fungi live in the environment, particularly in soil and in decaying organic matter, such as fruits, vegetables, leaves, compost piles, or rotten wood.People can contract mucormycosis by coming in contact with the fungal spores in the environment. For example, by inhalation of spores, by swallowing spores. Additionally, mucormycosisis likely to develop on the skin when fungus enters the skin via scrape, cut, burn, or any other type of skin trauma or injury.
How is mucormycosis related to COVID 19?
This rare fungal infection usually affects people who suffer from long-term health issues and/or take medications that lower immunity. Mucormyosis can be life-threatening in diabetics and immunocompromised individuals, such as recipients of organ or stem transplants, long-term usage of steroids, post-surgery, and cancer.
When diabetes is poorly controlled, and blood sugar is high the tissues become relatively acidic, it creates a suitable condition for Mucorales fungi to grow. This has been identified as a risk factor for mucormycosis in India. People with diabetes and obesity are expected to develop more severe Covid-19 infections. This means they’re more likely to receive corticosteroids, which are frequently used to treat Covid-19. But corticosteroids together with diabetes increase the risk of mucormycosis. Meanwhile, coronavirus can damage airway tissue and blood vessels, which could also increase susceptibility to fungal infection.
Moreover, damaged lungs and suppressed immune system as seen in the case of COVID-positive patients make sinuses and nose the most common site of mucormycosis manifestation. From there it can spread to the eyes, leading to blindness, or the brain, causing headaches, seizures, stroke, and even death in certain cases. A recent study showed 94% of people infected with mucormycosis had diabetes and poorly controlled diabetes in 67% people.
Furthermore, long-term ventilation reduces immunity and there are speculations of the fungus being transmitted by the humidifier water being given along with oxygen.
Is it contagious?
No, it’s not. It does not spread from one person to another.
Image: Twitter/@drharshvardhan
What are the symptoms?
You must visit your doctor if you experience the following symptoms;
Cough
Shortness of breath
fever
headache
nasal congestion, discharge.
sinus pain
blackened skin tissue
blisters
redness and swelling
ulcers
one side facial pain
loosening of teeth
blackish discoloration over the bridge of the nose
How is mucormycosis treated?
This includes antifungal medication, controlling blood sugar, urgent removal of dead tissue.
The outcome is poor in many patients affected with mucormyosis. Nearly half of the patients affected will die and many will sustain permanent damage to their health.
Can we prevent mucormycosis?
Yes, mucormycosis can be prevented. Vaccination can help, it will protect from infection, which in turn will protect immunity. A strong immunity system can keep mucrmycosis at bay. Awareness must be created regarding fungal infections, diagnose them early, along with a focus on controlling diabetes and using corticosteroids wisely.
Dr. Rahul Sawant is one of the Best Cardiologist in Pune. He is Interventional Cardiologist, MBBS, MD (Med) Pune, MRCP London, CCT Cardiology Cambridge UK. He is Director of Hridaymitra Cardia Clinic, Pune. Hridaymitra Cardia Clinic of excellence in Pune for heart care and you will discover well trained, and topmost best cardiologist in Pune.
0 notes
Text
Black Fungus; Definition, Symptoms and Causes
Black Fungus or Mucormycosis is a disease that is caused by a Fungus called Mucormycetes. This fungus is commonly found in our environment. Although the incidence of this disease is not new, it is a challenge that the Fungus attack is common to COVID-19 Patients. And it is a serious fungal infection that can affect our eyesight and even the brain.
Symptoms
According to the United States Center…

View On WordPress
0 notes
Text
Mucormycosis (Black Fungus) And COVID 19.
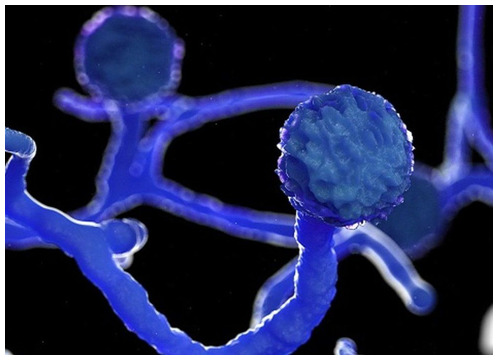
Catastrophic second wave of COVID 19 has left millions of people infected and dead. India is experiencing the world’s worst outbreak with not only rising COVID cases but also an alarming upsurge in a rare and potentially life-threatening fungal infection, Mucormycosis.
What is Mucormycosis ?
According to CDC, Mucormycosis (black fungus) is a serious and rare fungal infection caused by a group of molds called mucormycetes. These fungi live in the environment, particularly in soil and in decaying organic matter, such as fruits, vegetables, leaves, compost piles, or rotten wood. People can contract mucormycosis by coming in contact with the fungal spores in the environment. For example, by inhalation of spores, by swallowing spores. Additionally, mucormycosisis likely to develop on the skin when fungus enters the skin via scrape, cut, burn, or any other type of skin trauma or injury.
How is mucormycosis related to COVID 19 ?
This rare fungal infection usually affects people who suffer from long-term health issues and/or take medications that lower immunity. Mucormyosis can be life-threatening in diabetics and immunocompromised individuals, such as recipients of organ or stem transplants, long-term usage of steroids, post-surgery, cancer.
When diabetes is poorly controlled, and blood sugar is high the tissues become relatively acidic, it creates a suitable condition for Mucorales fungi to grow. This has been identified as a risk factor for mucormycosis in India. People with diabetes and obesity are expected to develop more severe Covid-19 infections. This means they’re more likely to receive corticosteroids, which are frequently used to treat Covid-19. But corticosteroids together with diabetes increase the risk of mucormycosis. Meanwhile, coronavirus can damage airway tissue and blood vessels, which could also increase susceptibility to fungal infection.
Moreover, damaged lungs and suppressed immune system as seen in the case of COVID-positive patients make sinuses and nose the most common site of mucormycosis manifestation. From there it can spread to the eyes, leading to blindness, or the brain, causing headaches, seizures, stroke, and even death in certain cases. A recent study showed 94% of people infected with mucormycosis had diabetes and poorly controlled diabetes in 67% people.
Furthermore, long-term ventilation reduces immunity and there are speculations of the fungus being transmitted by the humidifier water being given along with oxygen.
Note - Dr. Rahul Sawant is one of the Best Cardiologist in Pune. He is Interventional Cardiologist, MBBS, MD (Med) Pune, MRCP London, CCT Cardiology Cambridge UK. He is Director of Hridaymitra Cardia Clinic, Pune. He has rich experience with cardiology procedures and has performed around in excess of 5000 angiographies and in excess of 3,000 angioplasties.
Is it contagious ?
No, it’s not. It does not spread from one person to another.

What are the symptoms ?
You must visit your doctor if you experience the following symptoms; Cough Shortness of breath fever headache nasal congestion, discharge. sinus pain blackened skin tissue blisters redness and swelling ulcers one side facial pain loosening of teeth blackish discoloration over the bridge of the nose
How is mucormycosis treated ?
This includes antifungal medication, controlling blood sugar, urgent removal of dead tissue. The outcome is poor in many patients affected with mucormyosis. Nearly half of the patients affected will die and many will sustain permanent damage to their health.
Can we prevent mucormycosis ?
Yes, mucormycosis can be prevented. Vaccination can help, it will protect from infection, which in turn will protect immunity. A strong immunity system can keep mucrmycosis at bay. Awareness must be created regarding fungal infections, diagnose them early, along with a focus on controlling diabetes and using corticosteroids wisely.
#bestcardiologistinpune#cardiologistinpune#interventionalcardiologistinpune#cardiacclinicinpune#heartclinicinpune
0 notes
Text
Been hearing all about Black Fungus lately and feeling a little worried?
Well, DON’T FRET!
I have you covered with this “ultra” short YouTube video (only 50 seconds) containing all you need to know about the recent Black Fungus, or Mucormycosis, outbreaks in India and elsewhere.
Happy Watching!
#black fungus#covid#covid black fungus infection#covid back fungus#black fungus in covid patients#black fungus in humans#mucormycosis#mucormicose#mucormycetes#infectious disease#medicine#science
1 note
·
View note
Text
0 notes
Link
#health#health things#health tips#health news#health news in hindi#health tips in hindi#corona infection#corona positive#corona pandemic#corona symptoms#mucormycosis#mucormycetes#mucormycosis symptoms#covid19#blackfangus#white fungal infection#white fungus#black fungus#reporter17#trendzplay
0 notes
Text
Black Fungus Infection: Symptoms, Treatment, and Causes
Black fungus is a severe invasive fungal infection caused by RHIZOPUS typically seen in immunocompromised individuals.
There has been an increased incidence of this fungal infection in patients suffering from COVID 19 disease.
Several factors including underlying diabetes, immunosuppressives, host factors, pancreatic endocrine dysfunction by COVID 19 have been proposed as the putative causative mechanisms for Mucormycosis.
However, the judicious use of steroids and/or other immunosuppressants should not be withheld in patients with severe COVID 19, as they can be life-saving.
Treatment is long term and involves a combination of drugs and surgical measures.
What Black Fungus/Mucormycosis?
Mucormycosis, popularly termed “Black fungus” by the media and public, is a disease caused by ubiquitously occurring mold found in decaying vegetation and soil. It leads to necrotic black tissue at the infected sites, hence the name. In the Indian setting, it was more commonly seen in uncontrolled diabetics or people on extensive immunosuppression. We have seen the surge in cases of Mucormycosis during this COVID pandemic. We have also published such an initial series of patients (http://dx.doi.org/10.18203/issn.2454-5929.ijohns20211583). There have been several reasons proposed for this sudden surge in the deadly fungus.
These include:
Uncontrolled diabetes
Prolonged use of steroids and other immunosuppressives
Inborn errors of immunity
COVID19 could affect the pancreas which in turn can disturb the glycemic balance leading to prolonged periods of increased sugar levels in these patients. Thus, Mucormycosis can also be seen among COVID affected patients who were not treated with steroids or other immune-suppressing drugs.
Mucormycosis is caused by Rhizopus oryzae, the most common fungus responsible for the disease which causes about 70% of the cases. Despite advanced treatment and aggressive therapy, the mortality rate of the black fungus disease is over 50%. Further, the mortality rate in disseminated disease or with persistent neutropenia is even higher. The condition requires urgent and aggressive medical intervention; else it may result in debilitating or fatal consequences.
Who is Affected?
People with the following conditions/procedures are at increased risk for developing black fungus disease:
Compromised immunity
Uncontrolled diabetes mellitus in ketoacidosis
Organ or bone marrow transplantation
Malignant hematologic disorders
Other forms of metabolic acidosis
HIV/AIDS
Surgery
Treatment with corticosteroids
Trauma and burns
Neutropenia
Deferoxamine therapy in patients receiving hemodialysis
How Can They Get It?
The cause of black fungus is due to exposure to mucormycetes mold. The fungus is present in the soil, rotting wood, a pile of compost, and leaves.
You may contract black fungus infection through the skin. If you have any cut or scratch on the skin and comes in contact with the fungus, you may get black fungus disease.
Another way of developing this condition is through pulmonary exposure via inhaling the mould spores. Through inhalation, you may have an infection in your lungs and sinuses that may progress to the brain, eyes, and face.
However, not all people exposed to these moulds develop this disease. People with low immunity are at high risk for developing black fungus disease.
Does It Spread Through The Air?
Black fungus is not a contagious disease and does not spread from animals to the human. The fungal spores are present in the environment, including air. In most cases, when the person inhales these spores, they are attacked and destroyed by the immune system. However, in immunocompromised patients, the moulds survive and cause infection.
What Are The Black Fungus Infection Symptoms?
Some of the black fungal symptoms are:
Sinus and respiratory: Sinus, oral cavity and nasal involvement with extension to the eye is the commonest type of presentation.
Skin Infections: Due to cut, scratches or burnt skin, there is an exposure of the inner tissue to the black fungus. It may result in symptoms, such as ulcers, redness, swelling, tenderness, blisters, and blackened skin tissue.
Brain Infection: Disseminated black fungus infection in the brain may result in coma or altered mental status.
Ocular infection: Infection of black fungus in the eyes may result in eye pain, redness, swelling, blurred vision, and blindness. In some cases, there is a need to remove the eyes to prevent the progression of infection.
Gastrointestinal Infection: Black fungus infection in the gastrointestinal tract may result in Nausea and vomiting, abdominal pain, and gastrointestinal bleeding.
How The Doctor Diagnoses Black Fungus Disease?
There are various methods to diagnose black fungal disease. Some of them are:
Clinical diagnosis: Headache is the most common presenting feature. Tissue necrosis is the evident clinical sign and looking out for eschar (black scab) in the oral or nasal cavity helps in diagnosing the same. Redness and protrusion of the eye with swelling along with the loss of vision, severe facial pain and focal numbness should raise the suspicion of the disease
Imaging Techniques: CT Scan of paranasal sinuses and brain helps in picking up the rhino- orbital disease. CT lungs can help in looking for pulmonary nodule and effusion helps in diagnosing pulmonary disease.
Histopathological and microbiological examination: Identifying the fungus on the microscopic examination of the tissue and looking for uptake of special attains to identify the fungus is the most important step in diagnoses
Molecular assays: Molecular assays, such as restriction fragment length polymorphism analyses (RFLP), conventional polymerase chain reaction (PCR), melt curve analysis of PCR products, and DNA sequencing of defined gene regions, helps in determining the presence of Mucorales (pathogen responsible for black fungus disease). These tests are not commonly carried out as usually microscopic examination suffices
What Are The Treatment Options?
Management of black fungus disease requires a comprehensive approach. It includes managing the underlying predisposing factors, removing the necrotic tissues, initiating antifungal treatment, and adjunctive therapy. Following are the methods to manage black fungus disease.
Antifungal medications: The doctor may prescribe various antifungal medications. Some of them are liposomal amphotericin B, isavuconazole, and posaconazole.
Surgical debridement: Several infection specialists believe that surgical debridement of the infected part is required to save the patient's life. It helps in preventing the progression of the disease. After the successful outcome of treatment, the patient may undergo plastic surgery.
Problems
This disease usually has prolonged treatment duration and the drugs used are toxic, expensive and requires a long-term hospital stay. Apart from this, procurement of these lifesaving drugs has become problematic due to a sudden spike in the demand.
It can lead to severe comorbidities such as vision loss, focal deficits and even death at times particularly when the disease is not adequately treated at the early stages.
How to Prevent Mucormycosis Infection?
Having a high index of suspicion helps!!
If diagnosed early it can be treated better with improved outcomes.
Taking care of diabetes and having well-controlled sugars are the most important factor to prevent the invasion. Staying in touch with your endocrinologist and the ID physician post-COVID is also critical.
Following hygienic measures and frequent hand wash with minimizing the exposure of the fungal spores to the mucosal surface is also important.
You must take good care of yourself if you have compromised immunity. You should bandage all your wounds and use a mask while working in the yard. One must understand that steroid can be a lifesaving drug while managing COVID and shouldn’t shy away from its optimal use.
1 note
·
View note
Text
2021-05-15
Health
How to combat hormonal adult acne for women
India seeing surge in rare fungal infection - “Mucormycosis is a highly fatal disease caused by a group of moulds called mucormycetes that are commonly found in the environment, such as in soil or decaying organic material. Most people have the immunity necessary to fight it off, but the fungus can find easy entry into those who are immunosuppressed, most commonly through inhalation, with its spores spreading rapidly from sinuses and infecting other body tissues.” Those getting infected are those who have recovered from COVID-19.
Art

^ I could do that... and I won’t charge you US$9,500 for it!
Singapore
2 new COVID-19 clusters here
1 note
·
View note
Text
The treatment for India Mucormycosis Treatment (Black Fungus Drugs) involves prescription antifungal medication, such as isavuconazole, posaconazole, or amphotericin B

Mucormycosis is a rapidly progressive and potentially fatal invasive fungal disease with a high morbidity and mortality rate despite treatment. It primarily affects immunocompromised patients, such as those undergoing organ and bone marrow transplantation, those suffering from haematological malignancy, and those suffering from diabetes, cancer, neutropenia, and skin trauma.
It can also affect immunocompetent patients in rare cases. India Mucormycosis Treatment (Black Fungus Drugs) Market is caused by a type of mould known as a mucormycete. Mold spores can affect the lungs and sinuses when inhaled, and the fungus can also enter the skin through wounds such as cuts, burns, scrapes, or other types of skin trauma.
Read more @ https://digitalgrowinfo.blogspot.com/2022/04/the-outbreak-of-covid-19-has-increased.html
#India Mucormycosis Treatment (Black Fungus Drugs)#India Mucormycosis Treatment (Black Fungus Drugs) Market#Pharmaceutical
0 notes
Text
Black Fungus

Understanding Black Fungus
Mucormycosis, popularly known as ‘Black Fungus’ is a very rare fungal infection that infects one in ten lakh people. It affects the person when Mucor Mold (mucormycetes), which is naturally found in decayed or spoiled food, manure, and in the soil, enters the body. It is also found in the mucus of healthy people and is also present in the air. If the fungus contacts the skin and enters the body through cuts, it causes local infections, but if it enters through the sinus it can cause severe damages to the brain, lungs, and sinus. The infection can be fatal with a mortality rate that can be as high as 50%.

It can be severely life-threatening for diabetes, cancer, HIV/AIDS-affected people, people who have undergone transplants, or are on immunosuppressants.
Currently, the reason for the increase of black fungus among people is the excess use of steroids, especially in severely ill Covid19 patients. In Covid patients, steroids are used to lower the inflammation in the lungs of the affected patient overriding the immune system. The use of steroids has proven to cure many Covid positive patients. But, the use of steroids reduces the patient’s immunity and increases the blood sugar levels in diabetic and non-diabetic Covid patients. The low immune system increases the risk of getting infected with black fungus in most of the cases after recovering from Covid19. Many doctors mentioned that wearing face masks without washing them for a longer period and poorly ventilated rooms may also cause black fungus.
According to an article published by The Hindustan Times on 21st May 2021, India has recorded 7,205 reported cases of black fungus among which at least 219 people have died. The majority of cases are in Maharashtra, Gujarat, Madhya Pradesh, Haryana, Delhi, Uttar Pradesh, Bihar, Chhattisgarh, Karnataka, and Telangana. The state of Rajasthan has already declared black fungus an Epidemic under the Rajasthan Epidemic Act, 2020 on 19th May 2021 followed by Telangana, Tamil Nadu, Odisha, Gujrat, and Chandigarh, and other affected states.
Cure
The way of holding back the fungal infection is by keeping a regular check on the sugar levels and provisioning the right amount of steroid doses to the Covid patients especially diabetic patients even after recovery.
The most disturbing fact about this infection is that it is currently targeting the youth. In most cases, the infection causes blindness and can further cause the death of the patient, and to stop the spread of the infection in the eye sometimes the eyes of patients have to be removed. In a few cases, even the jaw bone, if infected, has to be removed. If the fungus infects the tissues, a team of microbiologists, ENT specialists, surgeons, internal medicine specialists along with other doctors have to remove the infected tissues.
If the infection is diagnosed before severe damage, an antifungal injection known as Amphotericin B costing Rs.3,500 per dose has to be injected into the patient’s body every day for 8 weeks. The injection is administered even to the patients who have undergone an operation for the removal of infected tissues. This antifungal injection is the only effective drug against black fungus. Only 6 companies are manufacturing the drug which has resulted in a shortage of doses. Taking into consideration the hike in the number of cases, the Ministry of Chemicals and fertilizers has approved five more pharma companies for the manufacture of Amphotericin.

Currently, in absence of Amphotericin B, Posaconazole, an alternative medicine used for curing yeast and throat infections is now being used by doctors against black fungus. Unlike during Covid19, people are not supposed to self-medicate after being infected by black fungus.
Symptoms
The symptoms on the affected patients can be
Stuffy/bleeding/green colored secretion from the nose
Swelling or pain in the eyes/ droopy eyelids
Black patches on the nose
Blurry/ loss of vision
Numbness or swelling on one side of the face especially cheekbones
Toothache/ falling of teeth
Chest pain
Thrombosis (appearance of blood clots).
If the doctor is consulted before the spread of the infection becomes severe, the patient can be saved, but most of the patients consult the doctor after complete blindness, because of which the affected eye(s) has to be completely removed. If the infection severely affects the jaw, it also may end up in the removal of the jaw bone.

Precautions
The safety measures for Covid19 of
maintaining 6 feet distance
wearing masks
staying home
sanitizing hands
washing hands
Inhaling steam
avoiding touching nose and mouth
maintaining hygienic lifestyle
should be followed for the prevention of black fungus too.
The additional measures are
staying away from garbage, rotting food, and construction sites.
controlling glucose levels especially if one has recovered from Covid19.
regularly checking diabetes levels
ingestion of steroids should be consulted by doctors and monitored regularly.
not missing the warning signs and symptoms of black fungus.
Crowdfunding
Crowdfunding platforms have proved to be of great help during the Covid19 Pandemic. Many crowdfunding platforms raised funds to donate essential kits to the needy as well as helped people raise campaigns on their platforms to save their loved ones. Donors came forward in large numbers and helped the people in distress as there was a lot of helplessness looming around.
“Black Fungus has been declared as an Epidemic and we should hope that it does not turn into a Pandemic.”
0 notes
Text
📰 ஓமிக்ரான் அலை: கருப்பு பூஞ்சை மீண்டும் வருமா? நிபுணர்கள் கூறுவது இதோ | ஆரோக்கியம்
📰 ஓமிக்ரான் அலை: கருப்பு பூஞ்சை மீண்டும் வருமா? நிபுணர்கள் கூறுவது இதோ | ஆரோக்கியம்
இந்தியா முழுவதும் ஓமிக்ரான் வழக்குகள் அதிகரித்து வருவதால், மியூகோர்மைகோசிஸ் அல்லது கருப்பு பூஞ்சை மீண்டும் வருவதற்கு பலர் பயப்படுகிறார்கள். கடந்த ஆண்டு, இரண்டாவது அலையின் போது, Mucormycete எனப்படும் அச்சுகளின் குழுவால் ஏற்பட்ட அரிதான மற்றும் ஆபத்தான பூஞ்சை தொற்று, பிந்தைய கோவிட் நோயாளிகளில் பல இறப்புகளுக்கு வழிவகுத்தது.
ம்யூகோர்மைகோசிஸ் குருட்டுத்தன்மை, உறுப்பு செயலிழப்பு, உடல் திசுக்களின்…
View On WordPress
0 notes
Text
ओमाइक्रोन तरंग: क्या काले कवक की वापसी होगी? यहां जानिए विशेषज्ञ क्या कहते हैं
ओमाइक्रोन तरंग: क्या काले कवक की वापसी होगी? यहां जानिए विशेषज्ञ क्या कहते हैं
जैसा ऑमिक्रॉन भारत भर में मामलों में वृद्धि, म्यूकोर्मिकोसिस या काले कवक की वापसी से कई लोगों को डर लग रहा है। पिछले साल, दूसरी लहर के दौरान, Mucormycete नामक मोल्ड के एक समूह के कारण होने वाले दुर्लभ लेकिन घातक फंगल संक्रमण के कारण कई मौतें हुईं। कोविड रोगियों को पोस्ट करें।
Mucormycosis अंधापन, अंग की शिथिलता, शरीर के ऊतकों की हानि और यहां तक कि समय पर इलाज न करने पर मृत्यु का कारण बन सकता…
View On WordPress
#ऑमिक्रॉन#ओमाइक्रोन तरंग#काला कवक और दूसरी लहर#काला कवक क्या है?#काले फंगस के लक्षण#क्या म्यूकोर्मिकोसिस वापस आ जाएगा#नैक फंगस ओमाइक्रोन वेव#म्यूकोर्मिकोसिस की वापसी#श्लेष्मा रोग
0 notes