#haematology
Photo


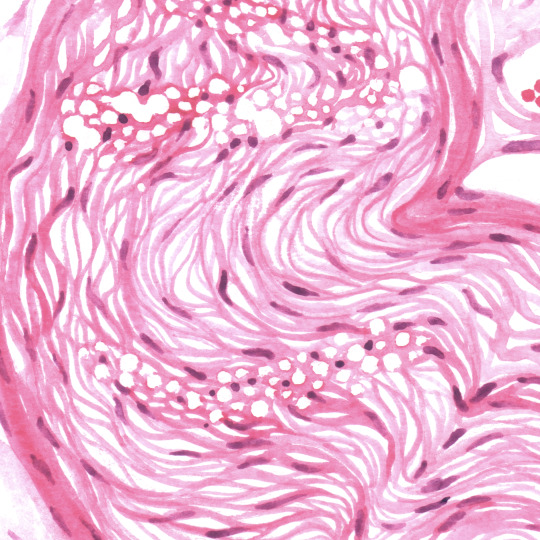

Histology ! Notes about each illustration on @celluloscope
#medblr#medecine#watercolor#histology#haematology#neurology#science#biology#cell#celluloscope#tw : trypophobia
670 notes
·
View notes
Text
Helpful free webinar coming up on transfusions!
16 notes
·
View notes
Text
I will be your blood loss consultant
Hey IWTV fic writers - want to ensure your character's blood loss feels realistic? Got a situation where a petit coup has gone too far, or a character got gravely injured? I've got a unique perspective to offer to the fandom - I've lived for extended periods of time with extremely low blood counts* and I'm happy for you to send me WIP snippets or to ask for advice on blood loss storylines.
To break it down a bit further, from my experience, how being low on the different types of blood feels/affects you:
Red blood cells - Red blood cells carry oxygen around the body, so if you're low on these, you're effectively low on oxygen in the blood. This is the most obvious, but you feel really sluggish, tired, and will be breathing heavily at the slightest physical exertion. Physically, it kinda feels like you're moving underwater, and your limbs feel heavy, and even short walks feel hard. (I went from running 10km 3x a week to getting out of breath just walking up stairs, for example). Cognition is fine, but frequent naps are a requirement.
Platelets - Platelets are what allow your blood to clot and heal cuts, so a lack of these means you bleed and bleed for a long time. But also you bruise super easily, and bruises last a really long time (weeks/months). You can also have spontaneous burst blood vessels in the whites of your eyes. Parts of your body that wouldn't normally bleed also do - like waking up to blood on the pillow because your gums bled overnight. The most unexpected part for me was having a constant background rushing sound in my ears - kinda like holding a seashell up, but all the time (until a transfusion).
White blood cells / neutrophils - A lack of these doesn't make you feel that different, tbh, but a lack of WBC means you can't fight off viruses so you pick up every single cough and cold, and have it for twice as long as normal people. A lack of neutrophils means you can't fight off bacteria, so your body's normal bacterial cohabitors cause problems that can really mess you up. So you've got to be insanely conscientious about what you eat (no runny eggs, unpasteurised cheeses, raw vegetables!), and brush your teeth and mouthwash after you ingest anything. You'll really only need to worry about these symptoms though if you've got low blood levels for an extended period of time (several weeks+).
Overall though, I've described the extreme examples. If your character is young and healthy, they will probably only experience the red blood loss symptoms (and possibly minor platelet symptoms) for a few days, depending on how much blood was lost. If they're in a situation where a hospital would give transfusions, be aware that you'll only ever be given enough to get you out of the dangerously low territory, never so much that you'd be "back to normal" counts after the transfusion(s). But transfusions do make you feel better almost instantly (better, but not good).
But again, feel free to message me with any specific questions (I can also tell you how chemo, meningitis, spinal taps, surgery w/o anaesthetic feels if that's of use!), I'm happy to talk about all this and I want to give back to this fandom and IWTV fanfic writers in particular to say thanks for the hundreds of hours of enjoyment you all have given me!
* I'm absolutely fine now! Over my lifetime, though, I've survived off the blood of literally hundreds of people. A bone marrow transplant saved my life 14 years ago and I run marathons now and am probably healthier than most 40-somethings, except I'm still Clinically Extremely Vulnerable to Covid and can't go into crowded places or unmask indoors. But my bloods have been fine for over a decade and this is in no way traumatic for me to talk about!
Please consider joining your country's bone marrow donor registry and/or donating blood regularly if you're able to! Both saved my life.
#interview with the vampire#iwtv#iwtv fanfiction#iwtv fic#iwtv fanfic#iwtv fandom#the vampire chronicles#anne rice#blood loss consultant#haematology#bone marrow transplantee#blood loss
37 notes
·
View notes
Text
The crisis the haematologist is in when the orthopaedist consults a patient because the patient’s hemoglobin level is 9.6 but no ferritin level has been investigated for a week.
“Reconsultation after the investigation of common causes of anemia (iron deficiency, B12 deficiency, folate deficiency) and the presence of a bleeding source will be convenient.”
11 notes
·
View notes
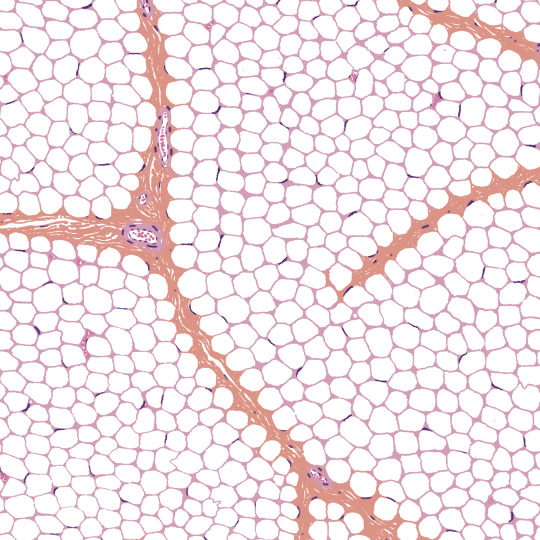
Photo

A couple of fun (not so fun) cases that I’ve had recently;
1. This cell was found within the peripheral blood smear of a dog with multicentric lymphoma affecting several lymph nodes. Unfortunately, this is a medium to large lymphocyte with a prominent, abnormally shaped nucleolus in the nucleus (lymphocytes do not usually have visible nucleoli!) which insinuates the lymphoma has reached Stage V, and has entered circulation or the bone marrow.
2. This picture depicts the exact area where a squamous cell carcinoma (a tumour of epithelial cells) has broken through the basement membrane of the epidermis and invaded into the dermis, in a skin sample from a toe.
30 notes
·
View notes
Photo

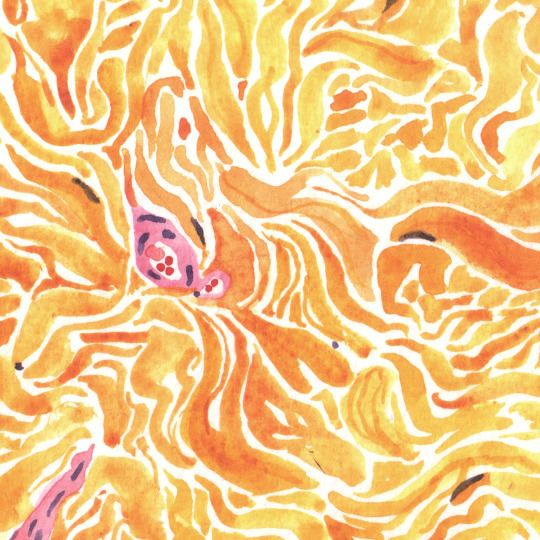
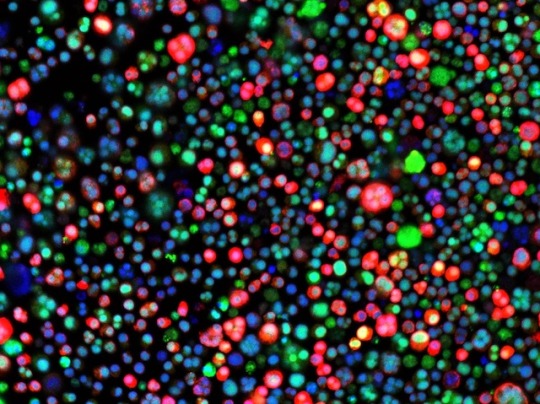
Blast Zone
An aggressive blood cancer, acute myeloid leukaemia (AML) occurs when abnormal developing white blood cells, known as blasts, start to multiply rapidly, filling up the bone marrow and disrupting the development of other blood cells. Pictured here are blasts (in purple) surrounded by red blood cells, from the bone marrow of a patient with Down syndrome; children with Down’s, a genetic condition caused by carrying a third copy of chromosome 21, are at much greater risk of developing AML. To understand why, researchers used gene editing tools to investigate all 218 genes on this extra chromosome. They homed in on RUNX1, which encodes a transcription factor, a protein that regulates other genes. RUNX1 can be expressed in several forms, and balance between them is key: these recent experiments suggest that AML is linked to an excess of a form called RUNX1A, opening up new avenues for research into potential treatments.
Written by Emmanuelle Briolat
Image by Jan Klusmann, University Hospital Frankfurt
Department of Pediatrics, Goethe University Frankfurt, Frankfurt am Main, Germany
Image copyright held by the original authors
Research published in Blood, March 2023
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#haemopoiesis#leukaemia#hemato oncology testing#hematooncology#oncology#haematology#Blood#bone marrow#may grunwald giemsa#runx1#down syndrome#chromosome 21#acute myeloid leukemia
17 notes
·
View notes
Text
Study: Sickle cell disease 11 times deadlier than previously recorded

- By Nuadox Crew -
A new study published in The Lancet Haematology journal reveals that the number of deaths caused by sickle cell disease is significantly higher than previously estimated.
The study found that the mortality rate attributed solely to sickle cell disease is 11 times lower than the actual number of deaths when considering various risk factors and associated conditions. Sickle cell disease not only leads to underdiagnosis but also increases the risk of infections and death from conditions such as stroke, heart problems, kidney problems, and pregnancy complications. As a result, doctors may overlook the connection between sickle cell disease and the cause of death when listing it on death certificates.
By combining data on prevalence, birth incidence, and mortality, the study estimated that the total mortality burden of sickle cell disease in 2021 was 373,000 deaths worldwide, compared to the previously reported figure of 34,600 deaths solely attributed to sickle cell disease. The increase in mortality was particularly significant in South Asia and sub-Saharan Africa, where the fatality rates were 67 times and nine times higher, respectively, than previously believed.
The research analyzed global health data from 2000 to 2021 and was part of the Global Burden of Disease 2021 study, led by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington's School of Medicine. The study highlights the rising number of babies born with sickle cell disease and the need for early detection and treatment due to the increased susceptibility to severe conditions and infections.
In 2021, approximately half a million babies were born with sickle cell disease, with over three-quarters of these births occurring in sub-Saharan Africa. When considering the total mortality burden, sickle cell disease was the 12th leading cause of death globally for children under the age of 5. However, it ranked among the top three causes of death in countries such as Portugal, Jamaica, Libya, Oman, and San Marino.
The study emphasizes the importance of improving data collection to track progress on sickle cell disease. Instead of relying solely on mortality data, the researchers used a mathematical algorithm that incorporated data on birth incidence, survival rates, and prevalence to estimate total deaths due to sickle cell disease. This approach provided a more comprehensive understanding of the true burden of the disease and its comparison to other leading causes of death.
The research highlights the urgent need for policymakers and public health advocates to address the underestimated burden of sickle cell disease. The implementation of universal newborn screening, the establishment of public registries for case monitoring, and early intervention treatments can significantly alleviate suffering for the approximately 8 million people living with sickle cell disease.
The study also stresses the importance of universal newborn screening for early diagnosis and management of sickle cell disease. While newborn screening is universal in the United States, many low- and middle-income countries lack a comprehensive screening process. Increasing global awareness and adopting health policies that expand neonatal screening and improve treatment accessibility are crucial for improving health outcomes for individuals with sickle cell disease.
--
Source: Institute for Health Metrics and Evaluation
Full study: Global, regional and national prevalence and mortality burden of sickle cell disease, 2000-2021: a systematic analysis from the Global Burden of Disease Study 2021, The Lancet Haematology (2023) DOI: https://doi.org/10.1016/S2352-3026(23)00118-7
Read Also
Yaw Ansong Jnr speaks on technologies for sickle cell disease patients
#sickle cell disease#sickle cell anemia#sicklecell#blood#health#pediatrics#africa#population health#public health#medicine#haematology#sickle cell#health informatics
6 notes
·
View notes
Text

One has to appreciate the work of fine subtlety, the grace of the ever-flourishing subslangs of scientific latin, because who else could ever bless the terraqueous globe with pearls such as qw (quaque week) and its worthy cousin, tiw (tris in week)?
#the spelling of alfa has reached a point where it's not even worth mentioning#sorry for the vent im not in my best mood today#pharmacology#pharmblr#cardio#tagamemnon#haematology
3 notes
·
View notes
Text
Student 1: Is anyone writing down what [Haematologist] is saying?
Student 2: I’m trying, but the God of Blood is a being a bit disorganized right now.
14 notes
·
View notes
Video
youtube
Turning an illness into art
2 notes
·
View notes
Note
Hey 🙂 How did you come up with becoming a haematologist ? What do you find fascinating about this field of medicine?
I just sort of slowly realised it would be the best fit for me! It took a while though - through most of medical school I sortof assumed I'd be a GP. It's the most common specialty and I didn't really have much calling to anything else, plus I was a below average med student and sort of assumed I'd have to go for one of the 'easier' options (not that the actual job of being a GP is easy in the slightest, but it's less competitive to get into).
Then I got more confident in myself when I did really well in my gastroenterology exams and thought maybe I could do gastro. So I did my whole Masters on pancreatic cancer and tried to get a gastro placement for my medical placement in final year. However, I got a haem placement instead! Which I really enjoyed, in fact out of the whole of med school it was the placement I enjoyed the most. I loved the fact that you got to know the patients on the wards as they'd often be in for weeks at a time, and found all the medicines and stem cell transplant stuff fascinating.
So then I was like, hmm it'll be haem or gastro, so I got myself a F1 job with both of them as rotations. I started with haem and LOVED it, again loving the rapport with the patients, finding the conditions and the new treatments fascinating (CAR-T was just coming on the scene and the registrars would teach me about it), although it was incredibly sad at times. And then... Covid hit, so I never got to do my gastro job. Maybe it was the universe telling me to do haem? I also realised when working as a doctor that I don't like procedures, so that ruled out gastro and a few other things like cardio, anaesthetics.
I think another good fit for me would be oncology, and I'm sure some others as well, but I just never had the exposure like I did with haem. I think that's sort of how it goes really! You can't experience and work in every specialty, so you get drawn into what you know.
12 notes
·
View notes
Text
Fresh hope
Today’s ICU consultant finally condescended to speak to me @ 6pm & I’m not convinced that I was much wiser afterwards but at 6.30pm along came a knight in shining armour – our very own lovely haematology consultant who has been off since last Thursday.
He proceeded to spend a half an hour with me having a full & frank two way conversation. As the Docs are now inclined to think that Leah’s lung…
View On WordPress
0 notes
Text
Want to be Lab Technician or Medicial Technician etc. Enroll in Bachelor in Medical Lab Science For more details speak to our education counselor at 8055 330 550 or visit https://tinyurl.com/57zkzyjj Currently working in PGI Chandigarh #studentreview #studenttestimonial #labtechnician #medicaltechnician #bloodbanking #essentialbiology #generalmicrobiology #haematology #hematologicaltechniques #biochemistry #mycology #immunology #clinicalbiochemistry #virology #cytology #analyticalbiochemistry #medicallaboratoryscience #cytology #ivyhospital #amcarehospital #srldiagnostics #indushospital
0 notes
Text
Happy Diwali 🪔🎇
#india#biochemistry#festival#hospital#hospitality#haematology#generalsurgery#dopplerstudies#chestphysician#love
0 notes
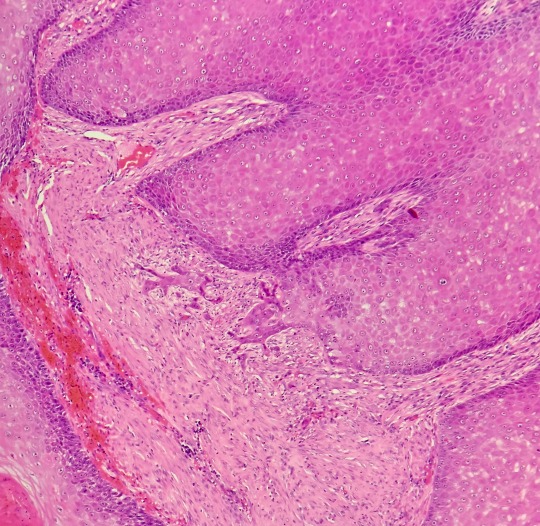
Photo
In a Bind
Multiple myeloma is a blood cancer affecting plasma cells, white blood cells that produce antibodies, causing them to multiply abnormally in the bone marrow. Right now, only half of patients can expect to survive five years after diagnosis, so better treatments are sorely needed. Promising targets include fatty acid-binding proteins (FABPs), a multi-functional family of proteins that can pick up lipids, involved in a variety of processes. A recent study found that cultured myeloma cells (pictured, their nuclei in blue) expressed high levels of one member in particular, FABP5 (in red); blocking it reduced cell proliferation, while patients with higher FABP5 levels tended to experience worse outcomes. Inhibiting FABPs more broadly appeared even more effective, improving survival in some mice with myeloma. To build on these results, further research needs to investigate why not all mice responded so well, and whether inhibiting FABPs would be safe and effective in humans.
Written by Emmanuelle Briolat
Image from work by Mariah Farrell and colleagues
Center for Molecular Medicine, Maine Health Institute for Research, Scarborough, ME, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in eLife, March 2023
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#myeloma#haemato-oncology#haematology#bone marrow#oncology#white blood cells#fatty acid binding proteins#cancer#blood cancer#immunofluorescence
10 notes
·
View notes
Text
Choosing a Specialty
One of the most difficult decision for any clinician to make is choosing a specialty. It is a very daunting decision for a lot of doctors because you get exposed to so many aspects of medicine during training and each one has its advantage over the other. So how do you choose?
You go through an extensive training that gives you in-depth knowledge on a lot of topics from anatomy, physiology,…

View On WordPress
#Emergency Medicine#Gynaecology#Haematology#Health#Medical school#Medicine#Obstetrics#Oncology#Paediatrics#Psychiatry#Radiology#Surgery
1 note
·
View note