#coronavirus mucormycosis
Quote
Exactly a year ago, the second wave affected many people with mucormycosis fungal infection, and the actual cause is still not known. As per official data, there are 1,006 mucormycosis survivors in Karnataka who are still under treatment. While some survived the infection, normalcy is yet to be restored for most of them. Having lost parts of the mouth cavity (removed to take off the fungal debris), chewing food has been impossible for some senior citizens, while a few have also lost vision.
Sunitha Rao, ‘One Year On, Many Mucor Survivors Can’t Chew & See’, Times of India
1 note
·
View note
Text
Mucormycosis (Black Fungus) And COVID 19.
Catastrophic second wave of COVID 19 has left millions of people infected and dead. India is experiencing the world’s worst outbreak with not only rising COVID cases but also an alarming upsurge in a rare and potentially life-threatening fungal infection, Mucormycosis.
What is Mucormycosis?
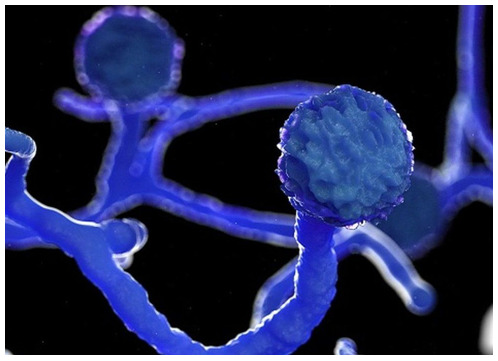
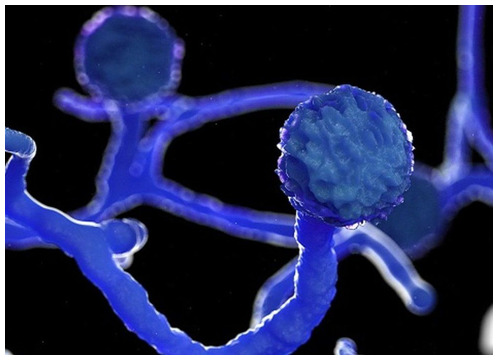
According to CDC, Mucormycosis (black fungus) is a serious and rare fungal infection caused by a group of molds called mucormycetes. These fungi live in the environment, particularly in soil and in decaying organic matter, such as fruits, vegetables, leaves, compost piles, or rotten wood.People can contract mucormycosis by coming in contact with the fungal spores in the environment. For example, by inhalation of spores, by swallowing spores. Additionally, mucormycosisis likely to develop on the skin when fungus enters the skin via scrape, cut, burn, or any other type of skin trauma or injury.
How is mucormycosis related to COVID 19?
This rare fungal infection usually affects people who suffer from long-term health issues and/or take medications that lower immunity. Mucormyosis can be life-threatening in diabetics and immunocompromised individuals, such as recipients of organ or stem transplants, long-term usage of steroids, post-surgery, and cancer.
When diabetes is poorly controlled, and blood sugar is high the tissues become relatively acidic, it creates a suitable condition for Mucorales fungi to grow. This has been identified as a risk factor for mucormycosis in India. People with diabetes and obesity are expected to develop more severe Covid-19 infections. This means they’re more likely to receive corticosteroids, which are frequently used to treat Covid-19. But corticosteroids together with diabetes increase the risk of mucormycosis. Meanwhile, coronavirus can damage airway tissue and blood vessels, which could also increase susceptibility to fungal infection.
Moreover, damaged lungs and suppressed immune system as seen in the case of COVID-positive patients make sinuses and nose the most common site of mucormycosis manifestation. From there it can spread to the eyes, leading to blindness, or the brain, causing headaches, seizures, stroke, and even death in certain cases. A recent study showed 94% of people infected with mucormycosis had diabetes and poorly controlled diabetes in 67% people.
Furthermore, long-term ventilation reduces immunity and there are speculations of the fungus being transmitted by the humidifier water being given along with oxygen.
Is it contagious?
No, it’s not. It does not spread from one person to another.
Image: Twitter/@drharshvardhan
What are the symptoms?
You must visit your doctor if you experience the following symptoms;
Cough
Shortness of breath
fever
headache
nasal congestion, discharge.
sinus pain
blackened skin tissue
blisters
redness and swelling
ulcers
one side facial pain
loosening of teeth
blackish discoloration over the bridge of the nose
How is mucormycosis treated?
This includes antifungal medication, controlling blood sugar, urgent removal of dead tissue.
The outcome is poor in many patients affected with mucormyosis. Nearly half of the patients affected will die and many will sustain permanent damage to their health.
Can we prevent mucormycosis?
Yes, mucormycosis can be prevented. Vaccination can help, it will protect from infection, which in turn will protect immunity. A strong immunity system can keep mucrmycosis at bay. Awareness must be created regarding fungal infections, diagnose them early, along with a focus on controlling diabetes and using corticosteroids wisely.
Dr. Rahul Sawant is one of the Best Cardiologist in Pune. He is Interventional Cardiologist, MBBS, MD (Med) Pune, MRCP London, CCT Cardiology Cambridge UK. He is Director of Hridaymitra Cardia Clinic, Pune. Hridaymitra Cardia Clinic of excellence in Pune for heart care and you will discover well trained, and topmost best cardiologist in Pune.
0 notes
Link
Several opportunistic infections were reported in COVID-19 patients, including Aspergillus spp., Candida spp., Cryptococcus neoformans, Pneumocystis jiroveci (carinii), mucormycosis, Cytomegalovirus (CMV), Herpes simplex virus (HSV), Strongyloides stercoralis, Mycobacterium tuberculosis, and Toxoplasma gondii.
...[these] have been reported from patients who received immunosuppressive therapy for their underlying diseases, such as IBD, systemic lupus erythematosus (SLE), and rheumatoid arthritis (RA)
Among the opportunistic infections, fungal infections account for the most case reports in COVID-19 patients. Other reported pathogens were related to viral, bacterial, protozoa, and helminth infections
Candida spp. is the second most numerous fungal infection worldwide [23]. The fungi are normally living on the skin, as well as inside the body, such as the throat, mouth, gut, and vagina. Oropharyngeal candidiasis is one of the most common infections in immunocompromised people, such as HIV/AIDS. Invasive candidiasis and candidemia are a serious and common infection in hospitalized patients
C. albicans is the most common Candida species; however, the emerging species such as C. auris is a highly invasive and multidrug-resistant yeast causing complicated conditions [43, 44]. COVID-19-associated candidiasis (CAC) has been reported in a number of cases until now [43], and C. auris was the most reported species [43, 45,46,47,48]. Other reported Candida species were C. albicans, C. tropicalis, C. parapsilosis, C. orthopsilosis, and C. glabrata among COVID-19 patients
The diagnosis of invasive candidiasis remains challenging, mainly due to the low number of Candida in infected tissues or circulation [43]. Serologic tests with β-D-Glucan (BDG) and mannan antigen as well as molecular platforms are recommended tests for diagnosis of candidiasis [52,53,54]. In COVID-19 patients, the treatment of invasive candidiasis is similar to that of non-COVID-19 patients [43]. Echinocandins that are usually well tolerated are the choice drugs for invasive candidiasis, while voriconazole, fluconazole, liposomal amphotericin B, posaconazolem, and isavuconazole are the second line of treatment [43]. Early diagnosis and treatment of CAC are important for management of the disease; however, multidrug-resistant species are a major challenge for CAC management.
Cryptococcus neoformans is an encapsulated yeast that causes subclinical infection in immunocompetent individuals. Humans can become infected by breathing fungal spores, and so, pulmonary infection is the major form of the disease.
Pneumocystis jirovecii is another common respiratory opportunistic pathogen in individuals with immunocompromising conditions, which causes pneumocystis pneumonia (PCP). PCP spreads from person to person through the air. Some healthy adults have the fungus in their lungs asymptomatically, and they can spread the infection to other individuals. The choice treatment for PCP is trimethoprim/sulfamethoxazole (TMP/SMX), which also known as co-trimoxazole
The results have shown that the most common pathogens causing respiratory coinfections were Staphylococcus aureus and Haemophilus influenzae
Respiratory viral pathogens, including Influenza, Parainfluenza, Metapneumovirus, and Rhinovirus, were reported among COVID-19 patients in different studies [120,121,122]. However, some infections such as CMV and HSV are opportunistic pathogens that could reactivate after immunosuppression.
CMV is a latent infection in immunocompetent individuals. The seroprevalence rate of CMV accounts about 80% in the elderly. CMV has been shown to manipulate the immune system by affecting T cell proliferation, decreasing in naïve T cell diversity, and increasing inflammatory cytokines (e.g., IL-6), leading to aging of the immune system (also called immunosenescence) [123, 124]. CMV infection has several sequels, mainly retinitis, pneumonitis, encephalitis/myelitis, neuropsychiatric disorder, and intrauterine infection [125,126,127]. Ganciclovir is an effective treatment option for CMV infection, especially for immunosuppressed individuals
Parasitic protozoa are a large group of unicellular pathogens, including blood and tissue protozoa (e.g., malaria, Leishmania, Toxoplasma, Trypanosoma, etc.) and intestinal and luminal protozoa (e.g., Entamoeba, Giardia, Cryptosporidium, Cyclospora, Blastocystis, Trichomonas vaginalis, etc.) [147]. However, intestinal protozoa and toxoplasmosis are an important opportunistic infections because their infections are usually latent or asymptomatic in healthy individuals, but severe infections could occur in immunocompromised patients
Intestinal protozoa can modulate immune responses through their direct interaction with host cells or by changing the gut microbiome composition [147]. To date, scarce information is available regarding the interaction of intestinal protozoa and COVID-19. Hence, there is an opportunity for researchers to investigate about the interaction of intestinal protozoa and COVID-19 in the clinical setting and experimental models. Nevertheless, opportunistic protozoa infection should not be neglected among COVID-19 patients.
Like the latent CMV infection, toxoplasmosis is a latent infection in immunocompetent individuals, but reactivation of latent toxoplasmosis or acquired toxoplasmosis among immunocompromised patients can cause severe infections with various sequels, such as toxoplasmic encephalitis, disseminated infections, and death [150,151,152,153]. Combination of pyrimethamine and sulfadiazine is the choice drug for toxoplasmosis treatment among nonpregnant women
0 notes
Text
Mucormycosis (Black Fungus) And COVID 19.
Catastrophic second wave of COVID 19 has left millions of people infected and dead. India is experiencing the world’s worst outbreak with not only rising COVID cases but also an alarming upsurge in a rare and potentially life-threatening fungal infection, Mucormycosis.
What is Mucormycosis ?
According to CDC, Mucormycosis (black fungus) is a serious and rare fungal infection caused by a group of molds called mucormycetes. These fungi live in the environment, particularly in soil and in decaying organic matter, such as fruits, vegetables, leaves, compost piles, or rotten wood. People can contract mucormycosis by coming in contact with the fungal spores in the environment. For example, by inhalation of spores, by swallowing spores. Additionally, mucormycosisis likely to develop on the skin when fungus enters the skin via scrape, cut, burn, or any other type of skin trauma or injury.
How is mucormycosis related to COVID 19 ?
This rare fungal infection usually affects people who suffer from long-term health issues and/or take medications that lower immunity. Mucormyosis can be life-threatening in diabetics and immunocompromised individuals, such as recipients of organ or stem transplants, long-term usage of steroids, post-surgery, cancer.
When diabetes is poorly controlled, and blood sugar is high the tissues become relatively acidic, it creates a suitable condition for Mucorales fungi to grow. This has been identified as a risk factor for mucormycosis in India. People with diabetes and obesity are expected to develop more severe Covid-19 infections. This means they’re more likely to receive corticosteroids, which are frequently used to treat Covid-19. But corticosteroids together with diabetes increase the risk of mucormycosis. Meanwhile, coronavirus can damage airway tissue and blood vessels, which could also increase susceptibility to fungal infection.
Moreover, damaged lungs and suppressed immune system as seen in the case of COVID-positive patients make sinuses and nose the most common site of mucormycosis manifestation. From there it can spread to the eyes, leading to blindness, or the brain, causing headaches, seizures, stroke, and even death in certain cases. A recent study showed 94% of people infected with mucormycosis had diabetes and poorly controlled diabetes in 67% people.
Furthermore, long-term ventilation reduces immunity and there are speculations of the fungus being transmitted by the humidifier water being given along with oxygen.
Note - Dr. Rahul Sawant is one of the Best Cardiologist in Pune. He is Interventional Cardiologist, MBBS, MD (Med) Pune, MRCP London, CCT Cardiology Cambridge UK. He is Director of Hridaymitra Cardia Clinic, Pune. He has rich experience with cardiology procedures and has performed around in excess of 5000 angiographies and in excess of 3,000 angioplasties.
Is it contagious ?
No, it’s not. It does not spread from one person to another.

What are the symptoms ?
You must visit your doctor if you experience the following symptoms; Cough Shortness of breath fever headache nasal congestion, discharge. sinus pain blackened skin tissue blisters redness and swelling ulcers one side facial pain loosening of teeth blackish discoloration over the bridge of the nose
How is mucormycosis treated ?
This includes antifungal medication, controlling blood sugar, urgent removal of dead tissue. The outcome is poor in many patients affected with mucormyosis. Nearly half of the patients affected will die and many will sustain permanent damage to their health.
Can we prevent mucormycosis ?
Yes, mucormycosis can be prevented. Vaccination can help, it will protect from infection, which in turn will protect immunity. A strong immunity system can keep mucrmycosis at bay. Awareness must be created regarding fungal infections, diagnose them early, along with a focus on controlling diabetes and using corticosteroids wisely.
#bestcardiologistinpune#cardiologistinpune#interventionalcardiologistinpune#cardiacclinicinpune#heartclinicinpune
0 notes
Text
Coronavirus black fungus infection symptoms | Mucormycosis: Early Signs, symptoms and everything we know about the deadly fungal infection
Coronavirus black fungus infection symptoms | Mucormycosis: Early Signs, symptoms and everything we know about the deadly fungal infection
Black fungus infection has officially been declared an epidemic in Rajasthan and several other states are recording an unproportionate number of cases, most of them linked to COVID complications.
Now, while fungal infections aren’t exactly rare or new like COVID-19, the precedence of cases has gone high in recent times. The infection seems to be most impactful for those suffering from severe…
View On WordPress
#Black Fungus#black fungus infection#black fungus symptoms#coronavirus black fungus#coronavirus black fungus infection#coronavirus mucormycosis#deadly fungal infection#Mucormycosis#mucormycosis symptoms
0 notes
Video
youtube
You all need to get vaccinated before some new variant comes along. The US is currently awash in vaccines. But that won’t do a lot of good unless those vaccines are inside us fending off the virus.
And unvaccinated people are still getting critically ill and dying in the US; on Saturday, 617 Americans died of COVID-19. I was just reading about a well-liked food vendor in Chicago’s Rogers Park neighborhood who had plans to get the vaccine but was five days away from his appointment. He’s currently in a coma in an intensive care unit.
Beloved Rogers Park elotero in coma with COVID-19; diagnosed 5 days before vaccination
In India doctors are seeing an upsurge in COVID-19 patients who have been afflicted by a dangerous fungal infection called mucormycosis.
Mucormycosis: The 'black fungus' maiming Covid patients in India
Mumbai's busy Sion Hospital has reported 24 cases of the fungal infection in the past two months, up from six cases a year, according to Dr Renuka Bradoo, head of the hospital's ear, nose and throat wing.
Eleven of them had to lose an eye, and six of them died. Most of her patients are middle-aged diabetics who were struck down by the fungus two weeks after recovering from Covid-19. "We are already seeing two to three cases a week here. It's a nightmare inside a pandemic," she told me.
In the southern city of Bengaluru, Dr Raghuraj Hegde, an eye surgeon, tells a similar story. He has seen 19 cases of mucormycosis in the past two weeks, most of them young patients. "Some were so sick that we couldn't even operate on them."
Don’t delay your vaccination. Yes, it’s a bit uncomfortable, I know that from my own two injections. 💉💉 But it’s a tiny price* to pay for the peace of mind of knowing that your chances of ending up in an ICU are close to zero and that you won’t come down with a disfiguring fungus.
And if you avoid getting COVID-19 then you’ll never have to worry about Long COVID.
Post-COVID Conditions
_____________________________________________
* As for the price of the vaccinations, they’re FREE. Get a small taste of Medicare for all.
#vaccinations#vaccines#covid-19#coronavirus#pandemic#public health#mucormycosis#felipe vallarta#long covid
4 notes
·
View notes
Photo

https://drfarooqeliteclinic.blogspot.com/2021/06/yellow-fungus.html
The second wave of coronavirus is finally slowing down with daily cases in India dipping to below 2 lakhs, but new fungal infections have followed in its aftermath, the most recently reported one being the deadly "Yellow Fungus".
#covid-19#black fungus#white fungus#yellow fungus#coronavirus india#second wave#coronavirus#fungal infection#infection#mucor septic#Mucormycosis#Aspergillus Flavus
1 note
·
View note
Photo

***Cow dung is likely behind an epidemic of ''Black Fungus' (Mucormycosis) that killed or maimed thousands of petients of COVID-19,*** says medical researchers. India recorded 51,755 cases of Mucormycosis as of November-2021. India accounted 71% of black fungus cases during the devastating second wave of Covid-19. #cowdung #CoronaUpdate #pendamic #cowshit #coronavirus #cowdungcakes #cattledung #COVID19 #CoronaVirusUpdate #blackfungus #mucormycosis #CoronavirusUpdates #covid19deaths https://www.instagram.com/p/CcDDE-lLZzI/?utm_medium=tumblr
#cowdung#coronaupdate#pendamic#cowshit#coronavirus#cowdungcakes#cattledung#covid19#coronavirusupdate#blackfungus#mucormycosis#coronavirusupdates#covid19deaths
0 notes
Quote
Two widely prescribed steroids - dexamethasone and methylprednisolone - are used for Covid patients in India to reduce the inflammation caused by the body's immune response. However, with hospitals and doctors overwhelmed by a growing numbers of cases, there's evidence that these steroids are being taken without medical supervision. The Indian authorities have recently warned against such self-medication, which can have seriously harmful consequences including, says Dr Denning, such as an increased the risk of developing mucormycosis. However, some states in India are reported to have distributed dexamethasone to the public along with home isolation kits.
Shruti Menon, ‘Black fungus: Is diabetes behind India's high number of cases?’, BBC
#BBC#Shruti Menon#India#Covid-19#coronavirus#mucormycosis#black fungus#dexamethasone#methylprednisolone#steroids#self-medication#David Denning#isolation kits
8 notes
·
View notes
Text
Kaun Banega Crorepati 13: Host Amitabh Bachchan fumbles while pronouncing 'mucormycosis' quite a few times; jokes 'isko bolte bolte insaan he bimar pad jaaye' - Times of India
Kaun Banega Crorepati 13: Host Amitabh Bachchan fumbles while pronouncing ‘mucormycosis’ quite a few times; jokes ‘isko bolte bolte insaan he bimar pad jaaye’ – Times of India
The latest episode of Kaun Banega Crorepati 13 started with host Amitabh Bachchan talking about how the week has been dominated by women players and that the last 3 players have been female contestants. He then resumed the game with roll-over contestant Sub Inspector Nimesha Ahirwar, who had won Rs 1,60,000 in the previous episode. Big B started talking with Nimisha and asked her if she slept…
View On WordPress
#amitabh bachchan#Big B#coronavirus#kaun banega crorepati 13#KBC 13#mucormycosis#nadeem-shravan#sub inspector nimesha ahirwar
0 notes
Link
#cases of mucormycosis#brihanmumbai municipal corporation#coronavirus#mucormycosis disease#mumbai#black fungus disease
0 notes
Text

#covid#covidvaccine#coronavirus#vaccine#india#coronavirusvaccine#coronavaccine#mucormycosis#deltapluscovid#deltaplus#deltaplusvarient#feku#googlekafeku
0 notes
Text
Black Fungus: इन राज्यों में अब आंख और दिमाग के बाद जबड़े में भी हो रहा है ब्लैक फंगस, क्या कहते हैं एक्सपर्ट
Black Fungus: इन राज्यों में अब आंख और दिमाग के बाद जबड़े में भी हो रहा है ब्लैक फंगस, क्या कहते हैं एक्सपर्ट
नई दिल्ली. भारत के सभी 28 राज्यों और तकरीबन 5 केंद्रशासित प्रदेशों में अभी भी ब्लैक फंगस (Black Fungus) यानी म्यूकोरमाइकोसिस (Mucormycosis) के मामले आने बंद नहीं हुए हैं. हालांकि, दिल्ली-एनसीआर सहित देश के दूसरे कुछ हिस्सों में बीते कुछ दिनों में ब्लैक फंगस के मामले में कुछ कमी आई है. एम्स के रिसर्च में दावा किया गया है कि कोरोना से उबरे मरीज ही ब्लैक फंगस के चपेट में ज्यादा आए हैं. बता दें कि…

View On WordPress
#Avascular necrosis#black fungus#Bone Death#CM Yogi#Corona patients#coronavirus in india#COVID recovery diet plan#diarrhea coronavirus#digetsive issues coronavrius#Ghaziabad#how long does long COVID last#Long Covid Symptoms#mucormycosis#nausea coronavirus#post COVID health#UP News#कोरोना वायरस#गाजियाबाद#पोस्ट कोविड कंप्लीकेशन ब्लैक फंगस#बोन डेथ#ब्लैक फंगस#ब्लैक फंगस एवैस्कुलर नेक्रोसिस#म्यूकोरमाइकोसिस#व्हाइट फंगस
0 notes