#cognitiveimpairment
Photo

Unlocking Insights: Long COVID Cognitive Symptoms Under the Microscope | CeBoz.com
A clinical trial investigates potential therapies for brain fog and cognitive aftereffects in long COVID patients.
0 notes
Text
Unleashing the Power of Play: The Numerous Benefits of Play-Based Pediatric Occupational Therapy
As pediatric occupational therapists, we know that children learn and develop through play. Play not only allows children to have fun, but it also helps them develop the skills they need for daily activities and function. This is why play-based Occupational Therapy (OT) has become a popular approach among therapists and parents alike as it offers a range of benefits for children. Let’s dive in deeper to explore some of the key benefits of play-based OT.
1. Improves Motor Skills
Play-based OT is a great way to improve a child's motor skills, including both gross and fine motor skills. By incorporating various activities into therapy sessions, such as building blocks, playing with playdough, catching and throwing a ball, or crawling under an obstacle course, children can improve their coordination, balance, and strength. This can help them with daily activities such as dressing, feeding, and writing.
2. Enhances Cognitive Skills
Play-based OT can also help children improve their cognitive skills such as problem-solving, planning, and organization. By engaging children in activities such as puzzles, memory games, and board games, children can improve their attention, memory, and processing skills. This can help them with school-related tasks like reading, writing, and math.
3. Boosts Self-Esteem
Play-based therapy can be an excellent way to boost a child's self-esteem and confidence. By providing a safe and supportive environment where they can be creative and explore different materials and activities, children can experience success and accomplishment. This can help them feel more confident in their abilities and encourage them to try new things.
4. Facilitates Socialization
Play-based therapy sessions also offer children the opportunity to socialize and interact with others, which is an essential aspect of their development. In group sessions, for example, children can learn how to share, take turns, and collaborate with others while engaging in different activities. This can also help children improve their communication skills and develop relationships with peers.
5. Customizable to Individual Needs
Play-based therapy is customizable to each child's unique needs. Play-based sessions can be tailored to target specific skills and areas of weakness, whether it's fine motor skills, sensory processing, or social skills. This way, each child can receive a personalized approach that meets their specific needs and goals.
#pediatricoccupationaltherapy#OTforchildren#sensoryprocessing#fineandgrossmotor#handwriting#feedingtherapy#autism#developmentaldelay#cognitiveimpairment#behavioraldisorders#ADHD#learningdisabilities#earlyintervention#sensoryintegration#visualperception#socialskills#motorplanning#selfregulation#assistivetechnology#schoolbasedOT#playtherapy#therapeuticinterventions#balanceandcoordination#mentalhealth#occupationaltherapygoals
1 note
·
View note
Link
🧠 Neurobehavioral symptoms can be challenging to understand and manage. They are complex and can arise from a variety of conditions, including brain injury, neurological disorders, and mental illnesses. 🤔 It can be difficult to differentiate between neurobehavioral symptoms and other types of behavioral problems. Understanding the underlying causes is key to developing effective treatment plans. 💡 This article will explore the various types of neurobehavioral symptoms, their causes, and potential treatment options. By gaining a better understanding of these symptoms, individuals and caregivers can improve their quality of life and overall well-being.1. The Basics of Neurobehavioral Symptoms: Understanding the Brain's Response to Injury or IllnessNeurobehavioral symptoms are common after brain injury or illness. They affect how a person thinks, feels, and acts. Understanding the brain's response is key to treating these symptoms. Common neurobehavioral symptoms include depression, anxiety, irritability, and impulsivity. These symptoms can be caused by a variety of factors, including damage to the brain's structure or chemical imbalances. Neurobehavioral symptoms can also be influenced by environmental factors, such as stress or lack of sleep. Treatment for neurobehavioral symptoms may include medication, therapy, or a combination of both. It's important to work with a healthcare professional to find the best treatment plan. Medications can help regulate mood and behavior, but they may also have side effects. Therapy can help individuals learn coping strategies and improve communication skills. Support from family and friends can also play a crucial role in managing neurobehavioral symptoms. It's important to remember that recovery from neurobehavioral symptoms takes time and patience. With the right treatment and support, individuals can regain control of their lives and improve their quality of life. 🧠💪2. Common Neurobehavioral Symptoms: Identifying and Managing Changes in Behavior, Emotions, and CognitionNeurobehavioral symptoms can be challenging to identify and manage. Here are some common symptoms: Agitation Depression Anxiety Impulsivity Disinhibition Memory loss Identifying and managing these symptoms can be done through: Behavioral therapy Medication Environmental modifications Exercise and physical activity Supportive care It's important to involve the patient and their caregivers in the management plan. This ensures compliance and better outcomes. It's also important to monitor for side effects of medications and adjust the treatment plan accordingly. Managing neurobehavioral symptoms can improve quality of life for patients and their caregivers. 🌟3. Neurobehavioral Symptoms in Traumatic Brain Injury: Causes, Diagnosis, and Treatment OptionsNeurobehavioral symptoms in TBI can be caused by physical damage to the brain. Diagnosis involves a thorough evaluation of symptoms. Treatment options include medication, therapy, and lifestyle changes. 🧠 Common symptoms include irritability, aggression, depression, and anxiety. These can impact daily life and relationships. 🙁 TBI can also cause cognitive issues like memory loss and difficulty concentrating. These can be treated with cognitive rehabilitation therapy. 💻 Medications can help manage symptoms like mood swings and sleep disturbances. Therapy can also help patients and families adjust to life after TBI. 🏥 Lifestyle changes like exercise, healthy diet, and stress management can also improve symptoms. It's important to seek help from medical professionals for proper diagnosis and treatment. 💪4. Neurobehavioral Symptoms in Neurodegenerative Diseases: Recognizing and Addressing Cognitive and Behavioral ChangesNeurodegenerative diseases can cause cognitive and behavioral changes. Recognizing these symptoms is crucial for early intervention. Symptoms include depression, anxiety, apathy, and irritability. Addressing these symptoms can improve quality of life. Treatment options include medication, therapy, and lifestyle changes. 🧠💊💆♀️ Early intervention can slow the progression of neurodegenerative diseases. Caregivers should monitor for changes in behavior and cognition. Support groups can provide emotional support and practical advice. 💪👥 Cognitive changes can include memory loss, difficulty with language, and impaired judgment. Behavioral changes can include impulsivity, aggression, and social withdrawal. Treatment should be tailored to the individual's needs. 🤔😠👥 Medication can help manage symptoms such as depression and anxiety. Therapy can help with communication and coping strategies. Lifestyle changes such as exercise and a healthy diet can improve overall well-being. 💊💬🏃♀️🍎 Caregivers should also take care of their own mental and physical health. Self-care can prevent burnout and improve the quality of care provided. 💆♀️💪🧘♀️5. The Role of Neuropsychological Testing in Understanding Neurobehavioral Symptoms🧠 Neuropsychological testing helps identify cognitive and behavioral changes in individuals with neurological conditions. 📝 These tests assess memory, attention, language, and executive functioning. 🔍 They provide insight into brain-behavior relationships, aiding in diagnosis and treatment planning. 💊 Results can guide medication selection and monitor treatment effectiveness. 🌟 Neuropsychological testing also helps identify strengths to maximize functioning and improve quality of life.6. Neurobehavioral Symptoms in Children: Recognizing and Addressing Behavioral and Emotional Changes🧒 Children can experience behavioral and emotional changes due to neurological conditions. 🧠 Neurobehavioral symptoms can include anxiety, aggression, and impulsivity. 💡 Recognizing these symptoms early can lead to better outcomes. 👩⚕️ Consult with a healthcare professional for proper diagnosis and treatment. 🏫 Teachers and parents can work together to create a supportive environment for children with neurobehavioral symptoms. 🧩 Behavioral therapy and medication can be effective treatments for these symptoms. 🌟 With proper support and treatment, children with neurobehavioral symptoms can thrive.7. Strategies for Coping with Neurobehavioral Symptoms: Supportive Care and Rehabilitation TechniquesSupportive care and rehabilitation techniques can help individuals cope with neurobehavioral symptoms. Encourage a healthy lifestyle, including regular exercise and a balanced diet. Provide a structured daily routine and consistent environment. Use visual aids and reminders to help with memory and organization. Practice relaxation techniques, such as deep breathing and meditation. Encourage social support and participation in meaningful activities. Provide cognitive and behavioral therapy to address specific symptoms. Use assistive technology, such as communication devices and mobility aids. It's important to tailor supportive care and rehabilitation techniques to the individual's needs and goals. With the right strategies, individuals with neurobehavioral symptoms can improve their quality of life and achieve their full potential. 🌟 In conclusion, understanding neurobehavioral symptoms is crucial for individuals and their loved ones. Recognizing the signs and seeking professional help can lead to a better quality of life. 🧠💪 It's important to remember that neurobehavioral symptoms can be caused by a variety of factors, including brain injury, mental illness, and neurological disorders. Early intervention and treatment can make a significant difference. 🏥🩺 By educating ourselves and others about neurobehavioral symptoms, we can reduce stigma and promote understanding. Let's work together to support those who may be struggling with these symptoms and encourage them to seek help. 🤝❤️ https://symptomfinder.com/understanding-neurobehavioral-symptoms/?_unique_id=64858bf03126b
#Uncategorised#BehavioralChanges#brainfunction#cognitiveimpairment#mentalhealth#neurobehavioraldisorders#aiomatic_0
0 notes
Text
Exercise for Better Sleep
Exercise is excellent for our body and mind and it can also help us get a good night’s sleep.
There is evidence that exercise does help you fall asleep more quickly and improves sleep quality, based on existing studies, but there’s some debate as to what time of day you should exercise.
How exercise helps us sleep
The research doesn't fully explain how physical activity improves sleep and some studies conclude that we may never be able to establish the mechanism that explains how the two are related.
However, we do know that moderate aerobic exercise increases the amount of slow wave sleep you get. Slow wave sleep refers to deep sleep, where the brain and body have a chance to rejuvenate. Exercise can also help to stabilise your mood and decompress the mind.
Why the timing of exercise matters?
Some people may find that exercising close to bedtime seems to keep them up at night.
Aerobic exercise causes the body to release endorphins. These chemicals can create a level of activity in the brain that keeps some people awake. If you experience this, you should exercise at least 1 to 2 hours before going to bed, giving endorphin levels time to reduce and the brain time to 'wind down'.
Exercise raises your core body temperature. The effect of exercise in some people is like taking a hot shower that wakes you up in the morning and this elevation in core body temperature signals the body clock that it’s time to be awake. But after about 30 to 90 minutes, the core body temperature starts to fall and this fall helps to facilitate sleepiness.
Despite these biological responses to exercise, other people find that the time of day they exercise doesn’t make a difference and whether it’s in the early morning or close to bedtime, they’ll see a benefit to their sleep.
How Much Exercise Do You Need for Better Sleep?
The good news is people who participate in at least 30 minutes of moderate aerobic exercise may see a difference in sleep quality that same night.
So, while we should all be encouraged to exercise, just be mindful of timing and whether it seems to affect your ability to get optimal sleep quality. You know your body the best.
Source: https://www.hopkinsmedicine.org
For more inspirational, life-changing blogs, please check out my site https://www.thecpdiary.com
#thecpdiary#blog#Exercising#for#BetterHealth#BetterImmunity#SleepingPatterns#SleepHabits#QualitySleep#BetterMentalHealth#BetterMemory#CognitiveImpairments#SleepHealth
0 notes
Text
Can You Fix Your Foggy Brain After Cancer Treatment? https://copingmag.com/can-you-fix-your-foggy-brain-after-cancer-treatment/ via @coping_cancer
#brainfog #chemobrain #cognitiveimpairment #cancer
0 notes
Text
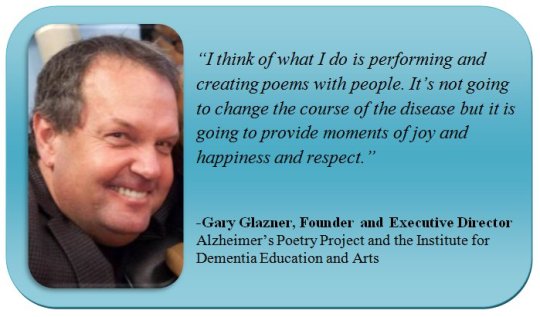
POETRY, PASTRIES & PIES PODCAST: Participatory Arts with Gary Glazner, Founder of the Alzheimer’s Poetry Project
POETRY, PASTRIES & PIES PODCAST: Participatory Arts with Gary Glazner, Founder of the Alzheimer’s Poetry Project
#Dementia #CognitiveImpairment #MemoryLoss
When you hear the words dementia and Alzheimer’s Disease, how does that make you feel? Typically you associate sadness, agitation, forgetfulness, helplessness, confusion, and exhaustion with those words, especially if you have a family member or know someone who experiences these conditions.
But what if you flip those emotions by turning them into joy and engaging fun? Now I know this may sound…
View On WordPress
#ALZHEIMER&039;S DISEASE#Cognitive Impairment#DEMENTIA#Gary Glazner#Memory Loss#Mental Health#Podcast Community#Poetry#Poetry Community#Poetry Pastries & Pies
1 note
·
View note
Text
#cognitiveimpairment UT Southwestern Medical Center researchers found that AI-powered voice analysis can help diagnose Alzheimer’s and cognitive impairment in early stages, potentially providing an efficient screening tool for primary care providers if confirmed by larger studies. https://scitechdaily.com/ai-can-detect-early-signs-of-alzheimers-in-speech-patterns-before-symptoms-begin-to-show/
0 notes
Photo
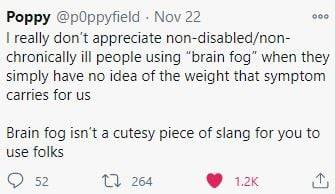
https://twitter.com/p0ppyfield/status/1330562011873374213?s=20
24 notes
·
View notes
Photo
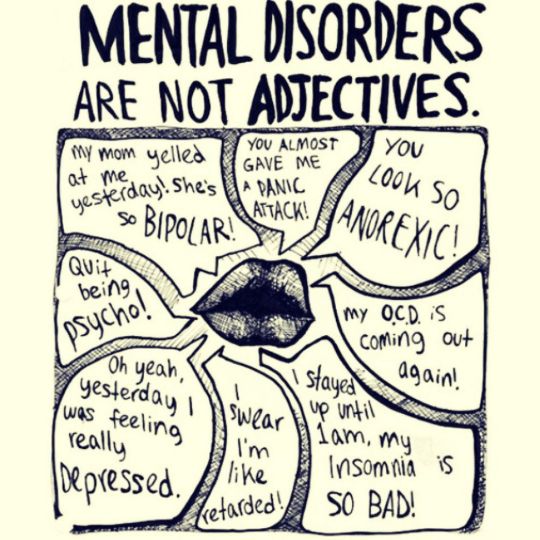
Wow❣️ What we say does matter… fight the stigma and join the conversation 😘💪🏼 #reducethestigma #fightthegoodfight #fightthestigma #fightthenoise #watchwhatyousay #chooseyourself #chooseyourwordswisely #speakyourtruth #speakyourmind #speakyourheart #powerinwords #changethenarrative #mentalillnesssupport #cognitiveimpairment #yourwordshavepower #giveyourselfabreak #peoplematter #ifightforyou #advocacy #advocacymatters #advocateforyourself #advocateforchange #changeispossible #changeiscoming #changeisconstant #steadfast #loveforothers #rachaelsroadtorecovery #mentaldisorders #mentaldisorder https://www.instagram.com/p/CW2ZhZeLADb/?utm_medium=tumblr
#reducethestigma#fightthegoodfight#fightthestigma#fightthenoise#watchwhatyousay#chooseyourself#chooseyourwordswisely#speakyourtruth#speakyourmind#speakyourheart#powerinwords#changethenarrative#mentalillnesssupport#cognitiveimpairment#yourwordshavepower#giveyourselfabreak#peoplematter#ifightforyou#advocacy#advocacymatters#advocateforyourself#advocateforchange#changeispossible#changeiscoming#changeisconstant#steadfast#loveforothers#rachaelsroadtorecovery#mentaldisorders#mentaldisorder
0 notes
Text
Untangling Life as a Millennial Caregiver with Lauren Dykovitz
#alzauthors#alzauthorspodcast#alzheimers#alzheimersblogs#alzheimersbooks#alzheimersdaughter#caregiver#caregiving#cognitiveimpairment#dementia#earlyonsetalzheimers#laurendykovitz#lifeloveandalzheimers#mariannesciucco#memory#memoryloss#millennialcaregiver#untanglingalzheimers&dementia#wholecarenetowrk#youngonsetalzheimers
0 notes
Text
Amyloid and Tau Biomarkers Help Distinguish Alzheimer's from Other Forms of Mild Cognitive Impairment
MedicalResearch.com Interview with:

Lauren McCollum, MD
Cognitive and Behavioral Neurology Fellow
Penn Memory Center / Cognitive Neurology Division
MedicalResearch.com: What is the background for this study?
Response: Alzheimer’s Disease (AD) is a heterogenous condition, with considerable variability in cognitive symptoms and progression rates.
One major reason for this heterogeneity is “mixed pathology,” – i.e., both AD- and non-AD pathology. Examples of non-AD pathology include cerebrovascular disease (CVD), Lewy Bodies, and TDP-43. Pathologically, Alzheimer’s Disease is defined by characteristic amyloid plaques and neurofibrillary tangles, which can be assessed for in living patients with CSF- or PET-based biomarkers for amyloid and tau, respectively. Classically, amyloid deposition begins years or even decades before pathologic tau accumulation, which is in turn associated with brain atrophy and cognitive decline.
The recently developed NIA-AA “ATN” research framework allows for the classification of individuals with regard to 3 binary biomarkers: Amyloid (A), Tau (T), and Neurodegeneration (N). An individual’s ATN biomarker status indicates where along the “Alzheimer’s Disease continuum” they lie. Additionally, some ATN statuses are on the “typical AD” continuum, while others are not. Research has shown that 15-30% of cognitively normal older adults have elevated amyloid. It stands to reason that some portion of cognitively impaired individuals with elevated amyloid and neurodegeneration have something other than AD driving their neuronal injury. Within the context of the ATN research framework, this subset of people is the A+T-N+ group (i.e., people who have elevated amyloid and neurodegeneration, but are tau-negative), as amyloid alone (that is, amyloid without tau) is not thought to cause significant cognitive impairment or brain atrophy. Our hypothesis was that, compared to A+T+N+ (a set of typical-AD biomarkers), A+T-N+ have cognitive and neuroimaging profiles that deviate from a typical Alzheimer’s Disease pattern – i.e., with less memory loss and less atrophy in AD-signature regions – and may have biomarkers suggestive of alternate non-AD pathologies .
MedicalResearch.com: What are the main findings?
Response: We performed two analyses using data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI). The first analysis used a PET-based approach to compare amyloid-positive people with mild cognitive impairment (MCI) or AD based on tau status (i.e., A+T- vs A+T+). Amyloid status was determined based on a composite SUVR of 1.11 with florbetapir PET. Tau status was assessed using the tau PET tracer AV-1451, and a cut-off of 1.22 SUVR in the bilateral extrahippocampal mesial temporal lobes was determined based on analysis of amyloid-negative cognitively normal controls. 13 A+T- and 30 A+T+ individuals were identified and compared. (In this analysis, cognitive impairment was used as a proxy for neurodegeneration as the sample size was small.)
The main findings in this analysis were that verbal memory was less impaired in A+T- compared to A+T+ (5-minute delayed recall score 5.3 vs 2.7, p=0.024), while the groups were similarly impaired on executive function as assessed by Trails B time (146 vs 131 seconds, p=0.628).
In a second, larger analysis, amyloid and tau positivity were determined based on CSF using cut-off values for the Roche Elecsys platform (A-beta-4224), and the neurodegeneration cut-off was set at the 90th percentile for mean ICV-and-age-adjusted hippocampal volume of 113 amyloid-positive individuals with dementia-level impairment. 29 A+T-N+ MCI, 87 A+T+N+ MCI, and 165 amyloid-negative cognitively normal controls were compared. The cognitive findings were similar to the first analysis, with A+T-N+ having less severe memory impairment compared to A+T+N+ (30-minute delayed recall score of 3.2 vs 1.6, p=0.004) and similar impairment in other domains, including executive function (Trails B time of 126 vs 124 seconds, p=0.899). Additionally, A+T-N+ had less severe posterior hippocampal atrophy compared to A+T+N+, and both MCI groups had similarly substantial burdens of WMHs.
MedicalResearch.com: What should readers take away from your report?
Response: Compared to the typical-AD biomarkers groups, both A+T- MCI/AD (from the first analysis) and A+T-N+ MCI (from the second analysis) displayed relative sparing of memory compared to executive functioning. Relative posterior hippocampal sparing in A+T-N+ MCI compared to A+T+N+ MCI may suggest non-AD pathology, as along the “hippocampal longitudinal axis” AD pathology (specifically, tau) preferentially affects the posterior hippocampus (while still involving the whole axis) and suspected TDP-43-opathies preferentially affect the anterior hippocampus.Both MCI groups had greater WMH burden than controls, suggesting CVD may contribute to symptoms in both.
Taken together, symptomatic patients who have elevated amyloid but not tau had features suggestive of alternative non-Alzheimer’s disease pathologies, including a less “Alzheimer’s-like” cognitive profile (i.e., with less memory loss), abnormal burden of WMHs, and relative sparing of the posterior hippocampus.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: Future directions for this research will include cortical thickness analyses to assess for additional neuroimaging correlates of these distinct cognitive profiles. We will also be further assessing our hypothesis with longitudinal analyses.
Any disclosures?
I (Dr. McCollum) have no disclosures. Dr. Wolk has received personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities with Merck, Jannsen, Eli Lilly and GE.
AAN 2019 abstract:
Cognitive Profiles in Amyloid-Positive Mild Cognitive Impairment and Alzheimer’s Disease with and without Tau (P2.1-030)
Lauren McCollum, Laura Wisse, Sandhitsu Das, Robin de Flores, Paul Yushkevich, David Wolk
First published April 9, 2019,
https://n.neurology.org/content/92/15_Supplement/P2.1-030#
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Read the full article
0 notes
Photo

#Repost @migraineinspiredart ・・・ Migraine disease is one of the leading causes of disability worldwide. Migraine that can severely impact every aspect of your life. But, it’s not just the severe pain that makes living with chronic migraine disease disabling. In addition to unpredictable and relentless pain, cognitive symptoms such as brain fog, problems communicating (aphasia) and chronic fatigue also make functioning “normally” very difficult. These cognitive impairments make comprehension, memory and communication very slow and sometimes impossible for those living with chronic migraine. It can be, at the least, embarrassing. At the most, it can be dangerous in certain situations. What do you do to cope with your cognitive deficits caused by chronic migraine disease? 💜❤️💜#migraineawareness #chronicmigrainedisease #chronicmigraineawareness #migrainesymptoms #migraine #cognitiveimpairments https://www.instagram.com/p/COfpqmKB4bN/?igshid=86r1yztrbokd
#repost#migraineawareness#chronicmigrainedisease#chronicmigraineawareness#migrainesymptoms#migraine#cognitiveimpairments
0 notes
Link
🧠 Schizophrenia is a mental disorder that affects how a person thinks, feels, and behaves. It's a severe illness that can cause delusions, hallucinations, and disordered thinking. Schizophrenia symptoms can be very distressing for both the person experiencing them and their loved ones. 👥 One of the most common symptoms of schizophrenia is social withdrawal. People with schizophrenia may find it difficult to interact with others, and they may become isolated and withdrawn. They may also experience changes in their mood and behavior, such as becoming more irritable or agitated. 🤔 However, there is one symptom of schizophrenia that is often overlooked: lack of insight. This means that people with schizophrenia may not be aware that they have a mental illness. They may not recognize that their thoughts and behaviors are abnormal, and they may resist treatment. Lack of insight can make it challenging for people with schizophrenia to get the help they need.1. Understanding Schizophrenia Symptoms: An OverviewSchizophrenia is a chronic mental disorder that affects how a person thinks, feels, and behaves. Symptoms can vary but often include hallucinations, delusions, disorganized thinking, and abnormal behavior. It usually develops in the late teens or early adulthood. Symptoms can be divided into positive, negative, and cognitive categories. Positive symptoms include hallucinations, delusions, and disorganized thinking. Negative symptoms include lack of motivation, emotional expression, and social interaction. Cognitive symptoms include difficulty with memory, attention, and decision-making. Hallucinations can involve hearing, seeing, feeling, or smelling things that are not there. Delusions can involve false beliefs, such as being persecuted or having special powers. Disorganized thinking can involve jumping from one topic to another or making up words. Treatment usually involves a combination of medication and therapy. Antipsychotic medications can help reduce symptoms, while therapy can help with coping skills and social interaction. It's important to seek help early and stick to a treatment plan. Living with schizophrenia can be challenging, but with proper treatment and support, many people with the disorder can lead fulfilling lives. It's important to educate yourself and others about the disorder to reduce stigma and promote understanding. 🧠📚💚2. Common Schizophrenia Symptoms and Their ImpactSchizophrenia symptoms vary, but some common ones include delusions, hallucinations, disorganized speech, and behavior. These symptoms can significantly impact a person's life, making it difficult to work, socialize, and care for themselves. 😔 Delusions are false beliefs that are not based on reality, such as believing that someone is trying to harm them. Hallucinations involve seeing, hearing, or feeling things that aren't there. Disorganized speech can make it hard to communicate, while disorganized behavior can make it challenging to complete tasks. 😞 Negative symptoms of schizophrenia can also occur, such as a lack of motivation, social withdrawal, and difficulty experiencing pleasure. These symptoms can make it challenging to maintain relationships and participate in activities. Treatment can help manage symptoms and improve quality of life. 💊 It's essential to seek help if you or a loved one is experiencing symptoms of schizophrenia. Early intervention can improve outcomes and prevent complications. Treatment options include medication, therapy, and support groups. With the right treatment, people with schizophrenia can lead fulfilling lives. 🙌3. Excluding One: Unique Schizophrenia Symptoms to Watch Out ForAs schizophrenia symptoms vary, some are unique to certain individuals. Here are some to watch out for: Catatonia: A state of unresponsiveness to the environment, including lack of movement or speech. Delusions of control: Believing that one's thoughts or actions are controlled by an external force. Thought broadcasting: Believing that one's thoughts are being broadcasted to the world. Thought insertion: Believing that someone else is inserting thoughts into one's mind. Visual hallucinations: Seeing things that are not there, such as people or objects. It's important to note that these symptoms are not exclusive to schizophrenia and can occur in other mental health conditions. If you or someone you know is experiencing any of these symptoms, seek professional help immediately. Early intervention and treatment can improve outcomes and quality of life. 👀🧠🏥4. How to Recognize Schizophrenia Symptoms in Loved OnesRecognizing schizophrenia symptoms in loved ones can be challenging. Here are some signs to look out for: Delusions or false beliefs Hallucinations, hearing or seeing things that aren't there Disorganized speech or behavior Difficulty concentrating or following conversations If you notice any of these symptoms, encourage your loved one to seek professional help. Early intervention is key. Other symptoms may include: Withdrawal from social activities Difficulty sleeping or changes in sleep patterns Lack of motivation or interest in activities Flat affect or lack of emotional expression It's important to remember that schizophrenia is a treatable condition. With proper medication and therapy, many individuals with schizophrenia can lead fulfilling lives. Be patient and supportive of your loved one. Educate yourself about the condition and seek support from mental health professionals and support groups. Remember, early recognition and treatment can make a significant difference in the long-term outcome for individuals with schizophrenia. 🧠💚5. The Importance of Early Intervention for Schizophrenia SymptomsEarly intervention for schizophrenia symptoms is crucial for better outcomes. Early detection can prevent the worsening of symptoms. It can also reduce the risk of hospitalization and improve quality of life. Research shows that early intervention can lead to better long-term outcomes. Patients have a higher chance of achieving remission and recovery. They may also experience fewer relapses and hospitalizations. Early intervention involves a combination of medication, therapy, and support. Antipsychotic medication can help reduce symptoms like hallucinations and delusions. Therapy can help patients manage their symptoms and improve their social skills. Support from family and friends can also be beneficial. Unfortunately, many people with schizophrenia don't receive early intervention. Stigma surrounding mental illness can prevent people from seeking help. Lack of access to healthcare can also be a barrier. It's important to raise awareness about the importance of early intervention for schizophrenia. Education can help reduce stigma and encourage people to seek help. Improving access to healthcare can also make early intervention more accessible. Overall, early intervention for schizophrenia symptoms is crucial for better outcomes. 🧠💊🧑🤝🧑🌟6. Managing Schizophrenia Symptoms: Treatment Options and StrategiesSchizophrenia treatment options include medication, therapy, and lifestyle changes. Antipsychotic medication can reduce symptoms, but side effects may occur. Therapy can help manage symptoms and improve quality of life. Lifestyle changes, like exercise and a healthy diet, can also be beneficial. Cognitive Behavioral Therapy (CBT) can help manage symptoms like delusions and hallucinations. Family therapy can help loved ones understand and support the person with schizophrenia. Support groups can provide a sense of community and understanding. It's important to work with a healthcare professional to find the right treatment plan. Medication may need to be adjusted over time. It's also important to communicate any side effects or concerns. Other strategies for managing symptoms include stress reduction techniques, like mindfulness and relaxation exercises. Avoiding drugs and alcohol can also help. It's important to have a support system and to stay engaged in activities that bring joy and fulfillment. Recovery is possible with the right treatment and support. 🙌🏼7. Supporting Individuals with Schizophrenia Symptoms: Tips for Family and FriendsSupporting someone with schizophrenia can be challenging, but it's essential to provide care and understanding. Here are some tips for family and friends: Be patient and listen actively to their concerns. Encourage them to seek professional help and attend therapy sessions. Learn about the condition and its symptoms to understand their experiences better. Help them maintain a healthy lifestyle with a balanced diet, exercise, and sleep. Offer emotional support and reassurance, but avoid being overprotective. It's crucial to understand that schizophrenia is a complex condition that affects individuals differently. Therefore, it's essential to tailor your support to their specific needs. Encourage them to participate in social activities and hobbies they enjoy. Help them set achievable goals and celebrate their successes. Be aware of potential triggers and help them avoid stressful situations. Be patient and understanding during periods of relapse or medication changes. Encourage them to stay on their medication and attend appointments regularly. Remember, supporting someone with schizophrenia requires patience, empathy, and understanding. It's essential to prioritize self-care and seek support for yourself if needed. Join a support group or seek counseling to manage your emotions and stress. Take breaks when needed and prioritize your own mental health. Communicate openly and honestly with your loved one about your concerns and feelings. Be aware of your own biases and avoid stigmatizing language or behavior. Celebrate progress and small victories along the way. Supporting someone with schizophrenia can be challenging, but with patience, understanding, and support, individuals with the condition can lead fulfilling lives. In conclusion, it's important to recognize that not all individuals with schizophrenia experience the same symptoms. While delusions, hallucinations, and disorganized thinking are common, some may not experience all three. It's crucial to seek professional help if you or a loved one is experiencing any symptoms of schizophrenia. Remember, early intervention and treatment can greatly improve outcomes for those with schizophrenia. Don't hesitate to reach out for help and support. 🙏🏼💙 #mentalhealthawareness #endthestigma https://symptomfinder.com/schizophrenia-symptoms-excluding-one/?_unique_id=64850d0e03740
#Uncategorised#cognitiveimpairment#delusionsandhallucinations#earlywarningsigns#negativesymptoms#schizophreniadiagnosis#aiomatic_0
0 notes
Photo
#cognitiveimpairment #shorttermmemoryissues #brainfog #vestibulardisorder #superiorcanaldehiscence #topamax #ptsdsucks #ptsd #migrainedisorder #vertigosucks #dizzy #stillfighting #domesticwintersoldier #fullmetalblunt #credittoartist #mybrainishangingupsidedown #motivation
#brainfog#cognitiveimpairment#credittoartist#dizzy#domesticwintersoldier#fullmetalblunt#migrainedisorder#Motivation#mybrainishangingupsidedown#ptsd#ptsdsucks#shorttermmemoryissues#stillfighting#superiorcanaldehiscence#topamax#vertigosucks#vestibulardisorder
0 notes
Text
POETRY, PASTRIES & PIES PODCAST: Remembering What's Forgotten through Poetry
POETRY, PASTRIES & PIES PODCAST: Remembering What's Forgotten through Poetry
#CognitiveImpairment #MemoryLoss #AlzheimersDiseaseAwarenessMonth #MentalHealth #PoetryCommunity
Image Credit: Matthias Zomer
How do you feel when you can’t remember something you know you should remember? How do you remember when you don’t know you can’t remember? You know, we used to call older people who were forgetful back in the day as senile. But what if “what” we think is simple forgetfulness, but leads to something deeper, like dementia and Alzheimer’s disease?
Throughout the month…

View On WordPress
#Alzheimer&039;s Disease Awareness Month#Behavioral Sciences#Cognitive Impairment#DEMENTIA#Geriatric Medicine#Memory Loss#Mental Health#Poetry#Poetry Community#Psychiatry#Senility
1 note
·
View note