#centralized monitoring clinical trials
Text
Clinical Research Monitoring: A Guide to Clinical Monitoring
Clinical research monitoring is a vital part of clinical trials and it involves various activities to ensure the safety and accuracy of the data collected. It is important that the clinical trial is conducted in a way that meets regulatory standards, protects human studies participants, and minimizes potential risks to their health and well-being. Clinical trial monitoring can include activities such as auditing study sites, evaluating data for accuracy and completeness, review of protocols and amendments, reviewing case report forms (CRFs), identifying any deviations from the standard operating procedures (SOPs) or protocols, managing corrective action plans (CAPs), following up on safety reports, tracking progress against enrollment goals and much more. Apart from evaluating data quality, clinical research monitoring also ensures compliance with all regulatory standards like GCP (Good Clinical Practices) ICH (International Conference on Harmonization), FDA regulations and local laws. In addition to this ongoing monitoring throughout a study's duration, there may be audits conducted by sponsors or regulatory authorities at any time during or after completion of a clinical trial. All these efforts are dedicated towards ensuring that the results obtained from a clinical trial are accurate, reliable and applicable for use in making medical decisions.
Steps to Clinical Monitoring
1. Establish an Effective Monitoring Plan: Ensure that the plan is comprehensive and contains all applicable elements, such as the types of monitoring activities to be conducted, frequency of monitoring visits, data collection methods, and specific criteria for acceptable performance.
2. Develop Appropriate Documentation: Design protocol-specific monitoring tools and forms to document information from site visits including source documents, data collection instruments, case report forms (CRF). In addition, develop a Monitoring Log or Tracking System which will enable better accountability for study activities.
3. Execute Monitors’ Visits: Depending on the complexity of the trial and regulatory requirements, conduct pre-study qualification visits (PSQV), pre-initiation visits (PIV), initiation visits (IVs), periodic monitoring visits (PMV) and close out visits (COV). During each visit, ensure that good clinical practice is followed at all times by reviewing source documents and data collection instruments. Review patient enrollment logs to ensure accuracy and record any discrepancies in the visit report.
4. Report Findings: Generate detailed yet concise reports per each monitor's visit with clear recommendations for corrective actions if required; provide professional feedback to investigators regarding their performance; identify any areas of noncompliance with protocol requirements or applicable regulations; recommend training or educational sessions when appropriate; track all follow up activities related to corrective actions taken in response to findings from monitors' visits; ensure that essential documentation is complete before closing out a particular study site.
5. Quality Assurance: Validate accuracy of tracking systems used by monitors during their visits; assess risk associated with various deficiencies identified during monitoring process; carry out periodic internal audits/assessments to ensure compliance with established SOPs/guidelines related to clinical research monitoring activities; take preventive measures based on audit/assessment results in order to strengthen internal quality system processes.
Types of Clinical Trial Monitoring
1. Types of Clinical Research Monitoring: Clinical research monitoring is the process to assess the quality and integrity of clinical trial data and ensure compliance with applicable regulatory requirements. It can be done through three primary methods: onsite monitoring, centralized or remote monitoring, and risk-based approaches.
2. Onsite Monitoring: Onsite monitoring is considered the "gold standard" for clinical research monitoring, as it requires the presence of a monitor at a study site during the entire duration of a trial. The monitor will typically review source documentation such as patient records, lab results, and investigational product dispensing logs to assess accuracy and conformance with study protocols and good clinical practices (GCP). The monitor also interviews staff members responsible for conducting the trial to verify that procedures are being followed properly.
3. Centralized or Remote Monitoring in Clinical Trials: Centralized or remote monitoring enables sponsors to conduct clinical research monitoring without needing to send someone onsite to each study location. This is accomplished by using technology such as web portals, video conferencing, and virtual meetings that allow monitors to remotely review data from various sites simultaneously and quickly flag any issues that arise. Additionally, centralized/remote monitoring allows sponsors to be more proactive in identifying potential risks associated with a trial prior to sending monitors onsite for an assessment.
4. Risk-Based Approaches: Risk-based approaches use data analytics tools such as descriptive statistics and predictive algorithms to identify potential trends or outliers in clinical trial data that may represent heightened risk of noncompliance with GCPs or other regulations. By leveraging technology, these approaches can help sponsors identify issues earlier in the course of a trial so they can take corrective action before something goes wrong.
5. Benefits of Clinical Research Monitoring: Utilizing effective clinical research monitoring strategies helps ensure that trials are conducted ethically, safely, correctly according to protocol standards, within timelines agreed upon with regulatory authorities, and within budget constraints set out by sponsors/CROs/investigators/other stakeholders involved in a study’s execution.. Clinical research monitors act as an independent third party who are able to provide objective insight into how studies are being conducted across multiple sites which helps minimize errors due to bias from investigators or other personnel who may have vested interests in outcomes associated with their studies.. In addition, effective clinical research monitoring helps ensure patient safety by providing oversight about how drugs or medical devices used in trials are administered as well as ensuring patient confidentiality is maintained throughout the course of a study.. Lastly, robust clinical research monitoring protocols help reduce costs associated with delays caused by errors made during trials which can add up significantly over time if not avoided through proper oversight methods both pre-study start up until closeout occurs after all enrolled patients have completed their participation in a given trial
Clinical Research Monitoring Guide
1. Understand the Basics of Clinical Research Monitoring: Clinical research monitoring is a key part of the clinical research process, ensuring the safety and accuracy of results. It involves periodically assessing study sites to confirm that data is being collected properly, according to ethical and legal requirements, as per Good Clinical Practice (GCP) guidelines.
2. Know What Types of Studies are Monitored: Clinical research monitoring can be used for a variety of studies, including clinical trials, observational studies, epidemiologic studies, and public health surveys. It is important to know what type of study you are monitoring in order to ensure that the appropriate procedures are followed.
3. Understand How to Monitor a Study Site: The primary goal of clinical research monitoring is to confirm that the protocol and informed consent form have been followed properly at each site. This requires a thorough review of all relevant documents such as case report forms (CRFs), source documentation (e.g., physician notes), internal audit reports (audit trails), and external quality assurance reports. Additionally, it involves evaluating compliance with GCP guidelines during study visits or remote reviews, as well as conducting interviews with staff members to assess how they are handling data collection and reporting processes.
4. Become Familiar With Regulatory Requirements: In addition to GCP guidelines, there may be applicable regulations from local governments or other institutions that must be adhered to when conducting clinical research monitoring activities. Understanding these regulations is essential for ensuring compliance with applicable laws and regulations related to clinical research activities.
5. Develop an Effective Monitoring Plan: An effective monitoring plan should include a detailed timeline for visiting sites, information about any specific areas where focused attention is required (e.g., enrolling/randomizing patients or managing adverse events), and plans for auditing/reviewing data generated by the study site(s). Additionally, it should incorporate measures for controlling risk associated with data collection processes so that issues can be identified early on in the study process before they become problematic later on down the line.
Clinical Research Monitor Job
The job of a Clinical Research Monitor is to ensure that clinical trials are conducted ethically, safely and in compliance with established standards. The primary responsibility of the monitor is to protect the rights, safety and well-being of the human subjects enrolled in the trial. Duties typically include developing protocols for clinical studies; coordinating study start up activities; conducting site visits; monitoring data for timeliness, accuracy and completeness; auditing files for regulatory compliance; managing investigator queries/issues; preparing visit reports; reviewing update protocols related to study operations; resolving issues raised through audit reports or other sources; providing technical guidance to sites regarding protocol implementation or study conduct; and escalating complex issues or potential risks as needed.
Clinical Research Monitor Salary
Salaries for this position tend to vary depending on education level, experience and geographical location but can range from $60,000 per year for entry level positions up to around $90,000 per year for more experienced professionals. In addition to salary many employers also offer benefits such as paid vacation days, health insurance plans and retirement packages.
Resources for Clinical Research Monitoring
1. National Institutes of Health (NIH): Clinical Research Monitoring
This link provides information on NIH's guidelines for monitoring clinical research, which include topics such as the roles and responsibilities of the investigator, data safety monitoring boards, and protocols for reporting unanticipated problems and adverse events.
2. National Institutes of Health (NIH): Guide to Clinical Research Monitoring
This comprehensive guide walks readers through all aspects of clinical research monitoring, including topics such as study design, randomization strategies, regulatory compliance requirements, data management, monitoring plans and reports, quality improvement initiatives, and safety assessments.
3. US Food and Drug Administration (FDA): Guidelines for Clinical Trials Monitoring
This resource from the FDA outlines the importance of effective monitoring in clinical trials and provides an overview of the different roles within a clinical trial as well as details about essential elements for implementation of an effective monitoring strategy such as risk assessments and adverse event tracking.
4. International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH)
ICH has developed standards that provide a set of harmonized technical requirements for clinical trials conducted across countries in the European Union (EU), Japan, and US with an emphasis on quality assurance and safety monitoring during trials.
5. Association of Clinical Research Professionals (ACRP)
ACRP's guidelines provide best practice recommendations for conducting clinical research studies in accordance with applicable regulations and standards to ensure patient safety monitoring during studies as well as data integrity throughout the process from start to finish.
6. Pharmaceutical Research & Manufacturers of America (PhRMA)
The PhRMA guidelines provide an overview of expectations around clinical research activities with respect to ethics, data integrity, safety reporting, resource allocation and more. It defines roles and responsibilities of all those involved in overseeing a clinical trial such as a Clinical Research Monitor or CRA who has primary responsibility for ensuring that the protocol is implemented correctly throughout a study’s duration
Clinical Research Monitoring Review
1. What is the main purpose of clinical research monitoring?
A) To ensure that a research study is conducted in accordance with applicable regulations and ethical standards
B) To ensure that data collected during a research study is accurate and reliable
C) To evaluate the safety of participants enrolled in a research trial
D) To oversee the financial management of a research project
Answer: A) To ensure that a research study is conducted in accordance with applicable regulations and ethical standards. Clinical Research Monitors are responsible for ensuring compliance with Good Clinical Practice guidelines, protecting participant privacy, verifying data accuracy, and evaluating protocol deviations. In addition, they may also be involved in reviewing participant eligibility requirements, conducting site assessments, providing training to investigators and staff on proper study procedures, as well as monitoring progress towards completion of all requirements of the study.
2. What type of individuals typically serve as clinical research monitors?
A) Physicians
B) Nurses
C) Regulatory specialists
D) All of the above
Answer: D) All of the above. Clinical Research Monitors can come from various backgrounds such as medical doctors (MDs), nurses (RNs), pharmacists (RPhs), regulatory specialists (e.g., Regulatory Affairs Professionals or Paralegals), or biostatisticians/data analysts who have experience in clinical trials and understand local regulations related to human subject protection. Each monitor has specific job duties depending on their education and experience, such as assessing compliance with regulatory guidance or analyzing data sets for accuracy, completeness, integrity, or validity.
3. What kind of activities do clinical research monitors need to perform?
A) Protocol reviews or verifications
B) Ensuring appropriate documentation completion
C) Site visits to observe investigator conduct
D )All of the above
Answer: D )All of the above. Clinical Research Monitors need to perform several activities including protocol reviews or verifications; ensuring appropriate documentation completion; site visits to observe investigator conduct; liaising between sponsors and sites; assisting with resolving issues associated with adverse events; reviewing case report forms for completeness, accuracy, consistency and correctness; evaluating subject safety throughout enrollment process;and writing reports detailing their findings at each visit.
4. What is one benefit gained from having an effective Clinical Research Monitor on-site? A) Reduced risk for legal liability stemming from negligence
B) Improved protocol adherence by investigators
C) Increased patient engagement during trial period
D )All of the above
Answer: D) All of the above . An effective Clinical Research Monitor encompasses several benefits such as reduced risk for legal liability stemming from negligence due to thorough oversight and accurate record keeping; improved protocol adherence by investigators through continued communication between sponsor representatives and researchers on-site regarding best practices; increased patient engagement during trial period due to more detailed explanations about potential risks/benefits offered by having monitor on-site ; and improved efficiency when dealing with complex protocols that require multiple levelsof oversight due to familiarity with protocol specifics which decreases time spent troubleshooting errors or unclear instructions..
5. How often should Clinical Research Monitors visit a particular site?
A) Weekly B) Biweekly C) Monthly D) Quarterly
Answer: C) Monthly . It is recommended that Clinical Research Monitors visit sites at least once per month in order to maintain active surveillance over ongoing studies at each location while also providing timely feedback regarding any issues discovered while on-site visits are taking place within a shorter timeframe if needed based upon changes made midstream or other unanticipated circumstances which might require immediate attention by sponsor personnel.
#clinical monitoring#clinical trial monitoring#remote monitoring clinical trials#clinical research monitor#clinical research monitor salary#risk based monitoring in clinical trials#clinical trial monitor#clinical trial monitor salary#monitoring of clinical trials by industry sponsors#centralized monitoring clinical trials#clinical research monitoring#clinical site monitoring#clinical trial monitoring services#clinical trial remote monitoring#clinical trials monitor#medical monitor clinical trial#risk based monitoring clinical trials#clinical monitor#clinical research monitor jobs#clinical trials monitoring#clinically validated blood pressure monitors for home use#monitoring in clinical trials#clinical monitoring services#clinical trial monitor jobs#journal of clinical monitoring and computing#monitoring clinical trials#remote monitoring in clinical trials#central monitoring clinical trials#clinical data monitoring#clinical monitoring jobs
0 notes
Text
Researchers have previously studied ibogaine as a potential treatment for opioid or cocaine dependence. While the recent study is one of the earliest to investigate ibogaine in relation to PTSD, the psychedelic compounds MDMA and psilocybin are in late-stage trials for PTSD treatment.
Alan Davis, a clinical researcher at Ohio State University who is unaffiliated with the study, tells Nature News that he agrees the data support launching trials to further test ibogaine. However, he says that MDMA and psilocybin may currently be better candidates for veterans’ PTSD treatment. He is not the only researcher looking at the study’s results with caution.
“Although the results have large effect sizes, most psychological studies will show improvement with any intervention,” says Amy Badura Brack, a psychologist at Creighton University who was not involved with the study, to Wired.
Though its results appear promising, the study did have some drawbacks. It was limited to a small sample size, lacking both participant diversity and a placebo arm. Researchers plan to continue monitoring study participants, publish the results and launch future research to better understand ibogaine and TBI treatment. {read}
#article#ptsd recovery#complex ptsd#PTSD#ibogaine#iboga#africa#medicine#science#medical study#smithsonian
12 notes
·
View notes
Text
Unveiling the Latest Breakthroughs: ASCO, Oncology, and Respiratory Conference Coverage
Introduction
Medical conferences serve as vital platforms where researchers, clinicians, and industry professionals converge to share groundbreaking discoveries, novel treatments, and innovative strategies.
Among the most anticipated gatherings are those focusing on oncology and respiratory health. In this comprehensive coverage, we delve into the highlights and key takeaways from the American Society of Clinical Oncology (ASCO) conference, alongside insights from recent oncology and respiratory conferences.

ASCO Conference Coverage: Pioneering Advances in Oncology
The ASCO Annual Meeting stands as a cornerstone event in the realm of oncology, offering a glimpse into the forefront of cancer research and treatment.
This prestigious gathering draws oncologists, researchers, and advocates from across the globe to Chicago, where they exchange knowledge, present findings, and explore collaborative opportunities.
Key presentations at ASCO often revolve around landmark clinical trials and breakthrough therapies. For instance, recent years have seen remarkable progress in the field of immunotherapy, particularly in checkpoint inhibitors and CAR-T cell therapy.
These modalities, designed to harness the body's immune system to combat cancer, have shown unprecedented efficacy across various malignancies, ushering in a new era of cancer treatment.
Moreover, discussions at ASCO extend beyond treatment strategies to encompass supportive care, survivorship, and healthcare disparities.
In summary, the ASCO conference serves as a catalyst for innovation and collaboration in oncology, driving progress towards improved outcomes and enhanced quality of life for cancer patients worldwide.
Oncology Conference Coverage & Insights: Navigating the Complexities of Cancer Care
Beyond ASCO, numerous oncology conferences around the globe offer valuable insights into the evolving landscape of cancer care. From the European Society for Medical Oncology (ESMO) to the American Association for Cancer Research (AACR), these gatherings provide platforms for networking, education, and scientific exchange.
At these conferences, researchers present findings across a spectrum of topics, ranging from early-phase clinical trials to translational research and epidemiology. Of particular interest are discussions surrounding novel therapeutic modalities, biomarker-driven approaches, and emerging trends in cancer biology.
In recent years, the advent of liquid biopsy has revolutionized the field of oncology by enabling non-invasive detection of tumor-derived genetic material in bodily fluids such as blood.
This technology holds immense promise for early cancer detection, monitoring treatment response, and detecting resistance mechanisms, thereby shaping the future of precision oncology.
Furthermore, oncology conferences shed light on the importance of interdisciplinary collaboration and patient-centered care. From molecular tumor boards to survivorship programs, healthcare professionals are embracing a team-based approach that prioritizes individualized treatment plans and holistic support services.
In essence, oncology conferences serve as crucibles of innovation and collaboration, driving progress towards more effective cancer prevention, diagnosis, and treatment strategies.
Respiratory Conference Perspectives: Navigating Challenges in Pulmonary Health
In parallel with advancements in oncology, conferences focusing on respiratory health play a crucial role in addressing the growing burden of lung diseases worldwide. From chronic obstructive pulmonary disease (COPD) to asthma and lung cancer, these gatherings convene experts to discuss cutting-edge research, clinical insights, and public health initiatives.
One of the central themes in respiratory conferences is the impact of environmental factors on lung health. With air pollution, smoking, and occupational exposures posing significant risks, researchers are striving to elucidate the underlying mechanisms and develop targeted interventions to mitigate these hazards.
Moreover, breakthroughs in the diagnosis and management of respiratory conditions are garnering attention within the medical community. Advances in imaging modalities, such as high-resolution computed tomography (HRCT) and positron emission tomography (PET), have revolutionized the early detection and staging of lung cancer, leading to more timely interventions and improved outcomes.
Furthermore, discussions at respiratory conferences often delve into the intersection of lung health and comorbidities, such as cardiovascular disease and diabetes. Recognizing the interconnected nature of these conditions, healthcare providers are adopting holistic approaches that address underlying risk factors and optimize overall health outcomes.
In addition, the emergence of novel therapeutics, including biologics and gene therapies, holds promise for patients with severe asthma, cystic fibrosis, and other refractory respiratory disorders. By targeting specific molecular pathways, these interventions aim to alleviate symptoms, reduce exacerbations, and improve long-term prognosis.
In summary, respiratory conferences serve as vital forums for knowledge exchange and collaboration, driving progress towards a future where lung diseases are better understood, preventable, and effectively managed.
Conclusion: A Tapestry of Innovation and Collaboration
In conclusion, conferences such as ASCO, alongside oncology and respiratory gatherings, represent beacons of hope in the ongoing battle against cancer and lung diseases. Through rigorous research, interdisciplinary collaboration, and patient-centered care, healthcare professionals are transforming the landscape of oncology and respiratory medicine, paving the way for improved outcomes and enhanced quality of life for patients worldwide. As we continue to navigate the complexities of these diseases, the insights gleaned from these conferences will undoubtedly shape the future of healthcare for generations to come.
0 notes
Text
Streamlining Clinical Data Management in Drug Development with Electronic Data Capture Systems
In the dynamic landscape of pharmaceutical research and development, the role of Clinical Data Management (CDM) is paramount. CDM encompasses a set of processes aimed at ensuring the quality, reliability, and integrity of clinical trial data collected throughout the drug development lifecycle. At the heart of efficient CDM lies the utilization of Electronic Data Capture (EDC) systems, which have revolutionized the way clinical data is collected, managed, and analyzed. In this blog post, we delve into the significance of EDC systems in CDM and their impact on expediting drug development processes.

Enhanced Data Accuracy and Quality
Traditional paper-based data collection methods are not only time-consuming but also prone to errors arising from manual entry and transcription. EDC systems eliminate these pitfalls by providing a digital platform for real-time data capture directly from study sites. By incorporating validation checks and edit checks, EDC systems ensure data accuracy and integrity, thus enhancing the overall quality of clinical trial data. This heightened accuracy minimizes the likelihood of data discrepancies and facilitates more reliable analysis, contributing to robust decision-making in drug development services.
Efficient Data Collection and Monitoring
One of the key advantages of EDC systems is their ability to streamline the data collection process. With built-in features such as electronic case report forms (eCRFs) and automated data entry, EDC systems enable researchers to efficiently capture and manage large volumes of clinical data. Moreover, real-time data monitoring functionalities empower study monitors and investigators to promptly identify and address data discrepancies or protocol deviations, thereby enhancing data quality and compliance with regulatory requirements.
Centralized Data Management and Accessibility
EDC systems facilitate centralized data management by consolidating all study-related information into a single, secure database. This centralized approach allows for seamless data integration across multiple sites and study phases, eliminating the need for manual data consolidation and reconciliation. Additionally, EDC systems offer secure access controls and audit trails, ensuring data confidentiality and traceability throughout the study lifecycle. Centralized data accessibility enhances collaboration among study stakeholders, promotes data transparency, and expedites regulatory submissions.
Real-time Data Insights and Decision-making
Timely access to accurate and reliable clinical trial data is critical for informed decision-making in drug development. EDC systems provide researchers and sponsors with real-time access to study data, enabling them to monitor trial progress, identify trends, and make timely adjustments to study protocols. By facilitating data-driven decision-making, EDC systems accelerate the pace of drug development, reduce development costs, and enhance the probability of regulatory approval.
Conclusion
In today's drug development landscape, Clinical Data Management is crucial for ensuring the reliability of trial data. Electronic Data Capture (EDC) systems have become indispensable, offering enhanced accuracy, simplified collection, centralized management, and real-time insights. Leveraging EDC systems accelerates trial processes, helping bring safe therapies to market faster. Partnering with Global Pharma Tek adds expertise to optimize these processes with comprehensive Clinical Data Management services.
0 notes
Text
Exploring the Vital Role of Dermatology Clinical Trials in Advancing Skin Health 🌟
In the realm of medical research, dermatology clinical trials stand as pillars of innovation and progress, driving advancements in the treatment and management of various skin conditions. These trials serve as critical pathways for evaluating new therapies, techniques, and medications aimed at addressing dermatological disorders. Within this landscape of discovery and healing, Cahaba Clinical Research plays a pivotal role, facilitating trials that offer hope and solutions to individuals grappling with skin-related concerns.

Understanding Dermatology Clinical Trials:🧪:
Dermatology clinical trials are meticulously designed studies conducted to assess the safety, efficacy, and potential side effects of interventions targeting skin disorders. These trials encompass a wide array of conditions, ranging from common ailments like acne and eczema to more complex diseases such as psoriasis and melanoma. Each trial follows a structured protocol, outlining the objectives, participant criteria, treatment regimen, and outcome measures, all under the oversight of qualified medical professionals and regulatory authorities.
The Significance of Participation:
Participation in dermatology clinical trials is not only an opportunity for patients to access cutting-edge treatments but also a vital contribution to scientific knowledge and medical progress. By enrolling in these trials, individuals play a crucial role in the development and refinement of therapies that could benefit millions worldwide. Furthermore, participants receive close monitoring and personalized care throughout the trial, ensuring their safety and well-being under the supervision of experienced dermatologists and research staff.
Advancing Treatment Options: 🚀
One of the primary goals 🎯 of dermatology clinical trials is to expand the arsenal of treatment options available to patients. Whether it involves testing novel medications, innovative procedures, or advanced technologies, these trials pave the way for breakthroughs that enhance therapeutic outcomes and quality of life for individuals affected by skin conditions. Through rigorous evaluation and evidence-based research, promising interventions are identified, leading to regulatory approval and eventual integration into clinical practice.

Addressing Unmet Needs:🎯
Many dermatological conditions pose significant challenges for patients and healthcare providers, often characterized by limited treatment efficacy or intolerable side effects. Dermatology clinical trials offer hope for addressing these unmet needs by exploring alternative approaches and refining existing therapies. By targeting specific disease mechanisms or developing targeted treatments, researchers strive to improve outcomes, minimize adverse reactions, and tailor interventions to individual patient profiles.
Embracing Innovation: 🌟
Innovation lies at the heart 💖 of dermatology clinical trials, driving progress in diagnosis, treatment, and prevention strategies. From groundbreaking discoveries in molecular biology to advancements in precision medicine and immunotherapy, these trials harness the latest scientific advancements to combat skin diseases with greater precision and efficacy. By embracing innovation and collaboration, researchers push the boundaries of medical knowledge, opening new avenues for combating dermatological disorders.
Ensuring Safety and Compliance: ⚖️
Central to the conduct of dermatology clinical trials is a commitment to ensuring participant safety and adherence to ethical standards. Rigorous protocols, informed consent procedures, and stringent regulatory oversight help safeguard the rights and well-being of trial participants. Cahaba Clinical Research adheres to strict guidelines and quality assurance measures, maintaining the highest standards of integrity and compliance throughout the research process.
Collaboration and Partnership: 🤝
Dermatology clinical trials thrive on collaboration between various stakeholders, including researchers, healthcare providers, pharmaceutical companies, and patient advocacy groups. These partnerships foster interdisciplinary approaches to research, facilitate resource sharing, and accelerate the translation of scientific discoveries into clinical practice. By fostering a collaborative ecosystem, Cahaba Clinical Research fosters synergy and collective efforts towards advancing dermatological care.
Looking Ahead: 🔮
As we venture into the future, the landscape of dermatology clinical trials holds promise for further innovation and progress. With emerging technologies, personalized medicine approaches, and a deeper understanding of skin biology, the potential for transformative breakthroughs is vast. Through continued investment in research infrastructure, community engagement, and scientific excellence, Cahaba Clinical Research remains dedicated to driving advancements in dermatological care and improving outcomes for generations to come.

Conclusion:
Dermatology clinical trials represent beacons of hope and progress in the journey towards healthier skin and improved quality of life. Through these trials, individuals gain access to cutting-edge treatments, while researchers work tirelessly to uncover new insights and solutions. With a steadfast commitment to excellence and collaboration, Cahaba Clinical Research continues to champion innovation and advance the frontiers of dermatological care, bringing us closer to a future where skin health knows no bounds. 🌈
1 note
·
View note
Text
Defying Limits: Rivaroxaban's Journey to Health
Introduction to Xarrlto
Rivaroxaban is an oral anticoagulant that works by selectively inhibiting factor Xa in the coagulation cascade. It was first approved by the FDA in 2011 for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation. Since then, its indications have expanded to also include treatment and secondary prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE).
Mechanism of Action
Factor Xa plays a central role in the coagulation pathway by acting as a link between the intrinsic and extrinsic pathways. Inhibiting factor Xa prevents the conversion of prothrombin to thrombin, thereby stopping the development of a blood clot. Xarrlto selectively and directly binds to the active site of factor Xa, inhibiting both free and prothrombinase-bound forms of the enzyme. It does not require a cofactor such as antithrombin III for its action. The drug forms a tight noncovalent binding interaction with factor Xa that is difficult to reverse.
Pharmacokinetics
Rivaroxaban has almost complete oral bioavailability and reaches maximum plasma concentration 2-4 hours after dosing on an empty stomach. The drug is approximately 92% protein bound and has a half-life of 5 to 9 hours in healthy individuals and 11-13 hours in the elderly population or those with renal impairment. Around one-third of the administered dose undergoes metabolism in the liver by CYP3A4, CYP2J2, and CYP-independent mechanisms. The rest is eliminated renally as inactive metabolites, with two-thirds excreted in the urine and one-third in the feces.
Clinical Efficacy
Xarrlto has shown excellent efficacy compared to warfarin across various disease states and patient populations in numerous Phase III clinical trials. Some key findings from these trials are discussed below:
Atrial Fibrillation
In the ROCKET AF trial involving over 14,000 patients with nonvalvular atrial fibrillation, Xarrlto demonstrated noninferiority to warfarin for the prevention of stroke or systemic embolism. The rates of major bleeding were also similar between the two groups, but intracranial and fatal bleeding events occurred less frequently with Xarrlto.
DVT/PE Treatment
The EINSTEIN-DVT and EINSTEIN-PE studies evaluated Xarrlto versus standard therapy with enoxaparin/warfarin for treating acute DVT and PE. Xarrlto was found to be noninferior to standard therapy in preventing recurrent VTE or death from all causes, while having significant reductions in major bleeding.
DVT/PE Secondary Prevention
The EINSTEIN-Extension trial showed that extending Xarrlto therapy for another 6-12 months after initial standard therapy reduced the risk of recurrent VTE by over 50% compared to placebo, without a significant rise in bleeding risk.
Orthopedic Surgery
Two trials, RECORD1-4, evaluated extended thromboprophylaxis with Xarrlto after hip or knee replacement surgery and found it significantly reduced VTE risks versus enoxaparin alone, with similar or lower bleeding rates.
Clinical Usage and Monitoring
Based on its efficacy and safety demonstrated in clinical trials, Xarrlto has become an attractive alternative to warfarin for certain indications. Some advantages over warfarin include its predictable pharmacokinetics, lack of required coagulation monitoring, fewer drug-drug and drug-food interactions, and rapid onset and offset of anticoagulant activity.
The usual dose of Xarrlto for atrial fibrillation and VTE treatment is 20mg daily, while extended VTE prevention and orthopedic thromboprophylaxis use 15mg daily. No drug level monitoring or dose adjustments are needed based on factors like age, weight or renal function. However, modifications may be required in certain patients with severe renal impairment.
Adverse Effects and Drug Interactions
Overall, Xarrlto is well-tolerated with a good safety profile. The most commonly reported side effects include bleeding events at injection sites, contusions, hematomas, and gastrointestinal hemorrhage. Rare side effects involving the liver, skin or nerves have also been seen.
Since Xarrlto is partly metabolized by CYP3A4 enzymes, strong inhibitors or inducers of this pathway can impact drug levels and require dosage adjustments. Drugs like azole antifungals, macrolide antibiotics, anti-HIV meds and St John's Wort commonly interact. Xarrlto also exhibits drug-drug interactions with antiplatelets like aspirin and NSAIDs, increasing bleeding risks when combined. Food or supplements containing cranberry or grapefruit may also raise Xarrlto levels.
Precautions are recommended in certain high-risk groups such as the elderly, those with renal or hepatic dysfunction, low body weight, or history of bleeding disorders or gastrointestinal diseases. Temporary discontinuation before surgeries or invasive procedures should be discussed with a healthcare provider.
In summary, Rivaroxaban is an important oral anticoagulant option that has revolutionized anticoagulation management due to its convenient dosing schedule and lack of coagulation monitoring. Numerous clinical trials provide strong evidence of its efficacy and safety in thromboprophylaxis and treatment of VTE, as well as stroke prevention in atrial fibrillation. Continued post-marketing monitoring will further elucidate its long-term risks and benefits in real-world populations. Overall, Xarrlto presents a suitable alternative to warfarin for appropriate patients.
0 notes
Text
Clinical Trial Management Systems Market Set to Reach US$ 4.6 Billion Surge in Demand by 2032
By 2022, the clinical trial management systems market is expected to be valued at approximately US$ 1.3 billion.
Clinical trial management system deployment is expected to grow at a rapid rate of 13.6% CAGR to reach US$ 4.6 billion by 2032. It is anticipated that the market for web-based clinical trial management systems will grow at a 13.9% compound annual growth rate.
Download a Sample Copy Of Report:
In the realm of healthcare and pharmaceuticals, the efficient management of clinical trials stands as a cornerstone for innovation and progress. With the advent of advanced technologies, the landscape of clinical trial management is undergoing a profound transformation, propelled by the emergence of Clinical Trial Management Systems (CTMS). This article delves into the pivotal role of CTMS in shaping the future of clinical research and the burgeoning market surrounding it.
Competitive Landscape:
The majority of businesses are concentrated on brand development, delivery, portfolio expansion, investments, and acquisitions. Important firms also enjoy a dominant position in the worldwide market and a sizable consumer base, giving them a competitive advantage over rivals.
In addition, developers fully engage in marketing activities to increase their exposure in the industry. Large companies are shifting their attention to smart service platforms that let patients use their products from a distance.
Kyoto University Hospital and Parexel, a preeminent worldwide clinical research organization, formed a strategic partnership in October 2021 with the goal of improving clinical research prospects and developing effective means of supporting clinical investigations.
Revolutionizing Clinical Research
Clinical Trial Management Systems (CTMS) serve as comprehensive software solutions designed to streamline and optimize the entire lifecycle of clinical trials. From study planning and participant recruitment to data collection and analysis, CTMS platforms provide researchers, sponsors, and regulatory authorities with the tools and capabilities necessary to conduct trials efficiently, accurately, and compliantly.
Enhancing Efficiency and Compliance
One of the primary drivers behind the adoption of CTMS is the pressing need for increased efficiency and compliance in clinical research. By centralizing study protocols, documents, and data within a unified platform, CTMS eliminates redundancies, minimizes errors, and accelerates trial timelines. Moreover, CTMS facilitates compliance with regulatory requirements and industry standards, ensuring that trials adhere to ethical guidelines and data integrity principles.
Optimizing Resource Management
CTMS platforms enable researchers to manage critical resources such as personnel, equipment, and funding more effectively. By automating workflows, tracking study progress, and monitoring resource utilization in real-time, CTMS enhances resource allocation and budget management, leading to cost savings and improved operational efficiency. Additionally, CTMS provides stakeholders with actionable insights and analytics, enabling data-driven decision-making and strategic planning.
Driving Market Growth
The Clinical Trial Management Systems market is experiencing rapid growth and expansion, driven by several key factors. The increasing complexity and scale of clinical trials, coupled with the growing demand for personalized medicine and innovative therapies, underscore the need for robust CTMS solutions. Furthermore, advancements in technology, such as artificial intelligence, machine learning, and cloud computing, are fueling innovation within the CTMS market, driving the development of more sophisticated and user-friendly platforms.
Read More: https://www.factmr.com/report/832/clinical-trial-management-systems-market
Future Outlook
Looking ahead, the future of the Clinical Trial Management Systems market appears exceptionally promising. Analysts project sustained growth and continued innovation as the demand for CTMS solutions continues to rise. With the global clinical trials market expected to expand further in response to emerging healthcare challenges and therapeutic advancements, CTMS will play an increasingly vital role in facilitating efficient, compliant, and successful clinical research endeavors.
Key Segments Covered in Clinical Trial Management System Industry Survey:
By Mode of Deployment :
Cloud-based Clinical Trial Management Systems
Web-based
On-premise
By Component :
Hardware
Services
Software
By Product Type :
Enterprise-based
Site-based
By End User :
Pharmaceuticals
Clinical Research Organizations (CROs)
Healthcare Providers
In conclusion, the Clinical Trial Management Systems market stands as a beacon of innovation and progress in the realm of healthcare and pharmaceuticals. By providing researchers, sponsors, and regulatory authorities with advanced tools and capabilities for managing clinical trials, CTMS is revolutionizing the way research is conducted, accelerating the pace of discovery, and ultimately improving patient outcomes. As the healthcare landscape continues to evolve, CTMS will remain at the forefront of clinical research, guiding stakeholders towards a future marked by innovation, efficiency, and excellence.
0 notes
Text
Enhancing Compliance with CTMS Software
CTMS (Clinical Trial Management System) software can significantly enhance compliance with regulatory requirements and best practices in clinical research. Here's how CTMS software can help enhance compliance:
Protocol Compliance: CTMS software helps ensure that clinical trials are conducted in accordance with the study protocol. It provides tools for protocol development, review, and approval, as well as for tracking protocol deviations and amendments.
Regulatory Compliance: CTMS software helps manage regulatory documents and requirements, such as informed consent forms, IRB approvals, and regulatory submissions. It provides reminders and alerts for upcoming deadlines and ensures that all regulatory requirements are met.
Data Integrity: CTMS software helps maintain data integrity by providing tools for data collection, validation, and management. It ensures that data is entered accurately and is consistent with the protocol and regulatory requirements.
Adverse Event Reporting: CTMS software facilitates adverse event reporting by providing standardized forms and workflows. It ensures that adverse events are reported promptly and accurately to regulatory authorities and ethics committees.
Site Monitoring: CTMS software helps monitor site performance and compliance with the protocol and regulatory requirements. It provides tools for remote monitoring, data review, and site visit planning, ensuring that sites are following the protocol and meeting quality standards.
Audits and Inspections: CTMS software helps prepare for audits and inspections by providing access to study documentation, reports, and data. It ensures that all required documents are up-to-date and easily accessible for regulatory authorities.
Training and Certification: CTMS software helps manage training and certification requirements for study staff. It tracks training completion and certification status, ensuring that staff are qualified to perform their roles in the clinical trial.
Documentation and Record Keeping: CTMS software helps maintain accurate and up-to-date documentation for the clinical trial. It provides a centralized repository for study documents, correspondence, and other records, ensuring easy access and retrieval.
By using CTMS software, organizations can enhance compliance with regulatory requirements and best practices in clinical research. CTMS software provides a comprehensive solution for managing all aspects of clinical trials, ensuring that studies are conducted ethically, safely, and in compliance with applicable regulations.
0 notes
Text
Understanding the Dynamics of the Dry Age-related Macular Degeneration Market: Drivers, Barriers, and Future Outlook
Dry age-related macular degeneration (AMD) is a chronic eye condition characterized by the gradual deterioration of the macula, a small area near the center of the retina responsible for sharp, central vision. Dry AMD is the most common form of AMD, accounting for approximately 85-90% of all cases. Unlike wet AMD, which involves abnormal blood vessel growth beneath the macula, dry AMD typically progresses more slowly and is characterized by the accumulation of yellow deposits called drusen in the macula.
Dry Age-related Macular Degeneration Market Drivers
Aging Population: The aging population is a significant driver of the dry AMD market, as AMD primarily affects individuals over the age of 50. With demographic trends indicating a growing proportion of elderly individuals worldwide, the prevalence of dry AMD is expected to increase, driving demand for diagnostic services, treatments, and supportive care products.
Rising Disease Burden: Dry AMD is a leading cause of vision loss and blindness in older adults, contributing to a substantial disease burden and socioeconomic impact. As the prevalence of dry AMD continues to rise, particularly in developed countries with aging populations, there is an increasing need for effective management strategies to prevent disease progression and preserve vision.
Advancements in Diagnostic Technologies: Technological advancements in imaging modalities, such as optical coherence tomography (OCT), fundus autofluorescence (FAF), and adaptive optics imaging, have improved the early detection and monitoring of dry AMD. These non-invasive imaging techniques enable more accurate assessment of retinal changes, drusen morphology, and disease progression, facilitating timely intervention and personalized treatment approaches.
Research and Innovation: Ongoing research efforts aimed at elucidating the pathogenesis of dry AMD, identifying novel therapeutic targets, and developing innovative treatment modalities drive innovation in the dry AMD market. Research areas of interest include anti-inflammatory agents, neuroprotective compounds, stem cell therapy, gene therapy, and drug delivery systems designed to target specific pathways implicated in AMD pathophysiology.
Clinical Trial Activity: The increasing prevalence of dry AMD and the need for effective treatment options have led to a surge in clinical trial activity focused on evaluating investigational therapies for dry AMD. Pharmaceutical companies, biotechnology firms, academic institutions, and government agencies are conducting clinical trials to assess the safety, efficacy, and tolerability of novel drugs, biologics, gene therapies, and cell-based interventions for dry AMD.
Regulatory Support and Incentives: Regulatory agencies provide support and incentives to expedite the development and approval of new treatments for dry AMD. Designations such as orphan drug status, fast track designation, breakthrough therapy designation, and priority review designation streamline the regulatory review process and accelerate market access for promising therapies targeting unmet medical needs in dry AMD.
Patient Advocacy and Awareness: Patient advocacy organizations and support groups play a crucial role in raising awareness about dry AMD, educating patients and caregivers, and advocating for improved access to treatment and supportive care services. Increased awareness of the importance of early detection, regular eye exams, and adherence to treatment regimens promotes proactive management of dry AMD and enhances patient outcomes.
Healthcare Infrastructure and Access to Care: Access to comprehensive eye care services, including retinal specialists, low vision rehabilitation programs, and low vision aids, is essential for effectively managing dry AMD and optimizing visual function. Investments in healthcare infrastructure, telemedicine platforms, and community-based outreach programs expand access to eye care services, particularly in underserved areas with limited access to specialty care.
Market Competition and Collaboration: Competition among pharmaceutical companies, biotechnology firms, and medical device manufacturers drives innovation and investment in the dry AMD market. Collaborations, partnerships, and licensing agreements between industry players facilitate the development and commercialization of novel therapies, diagnostic technologies, and supportive care products, enhancing market competitiveness and diversifying treatment options for patients.
Reimbursement Landscape: Reimbursement policies, coverage decisions, and pricing strategies influence market dynamics and access to dry AMD treatments. Payer reimbursement for diagnostic tests, treatments, and supportive care services impacts patient access and affordability, driving market adoption and utilization of approved therapies.
Dry Age-related Macular Degeneration Market Barriers
Despite the significant progress in understanding dry age-related macular degeneration (AMD) and developing treatments, several barriers impede the effective management and commercialization of therapies in the dry AMD market. Here are some of the key barriers:
Limited Treatment Options: Compared to wet AMD, there are fewer approved treatment options for dry AMD. Currently, there is no cure for dry AMD, and available treatments mainly focus on slowing disease progression rather than reversing vision loss. The lack of effective pharmacological interventions targeting the underlying mechanisms of dry AMD represents a significant barrier to addressing unmet medical needs in this patient population.
Complexity of Disease Pathophysiology: Dry AMD is a multifactorial disease with complex pathophysiology involving interactions between genetic, environmental, and lifestyle factors. The heterogeneous nature of dry AMD presents challenges for developing targeted therapies that address the diverse underlying mechanisms contributing to disease progression. Understanding the underlying pathophysiological processes and identifying effective therapeutic targets require further research and preclinical validation.
Difficulty in Early Detection and Diagnosis: Early detection and diagnosis of dry AMD are crucial for implementing timely interventions and preserving vision. However, early-stage dry AMD may be asymptomatic or present with subtle visual changes that are challenging to detect using conventional screening methods. Limited access to advanced diagnostic technologies, such as optical coherence tomography (OCT) and fundus autofluorescence (FAF), in primary care settings may delay diagnosis and initiation of treatment.
Lack of Biomarkers for Disease Progression: Biomarkers that reliably predict disease progression and treatment response in dry AMD are currently lacking. The absence of validated biomarkers hinders risk stratification, patient selection for clinical trials, and monitoring of treatment efficacy. Biomarker discovery efforts focusing on identifying molecular, genetic, and imaging-based markers associated with disease progression and treatment response are ongoing but face challenges in reproducibility and validation.
High Development Costs and Long Regulatory Pathways: Developing novel therapies for dry AMD involves substantial investment in research and development, preclinical studies, clinical trials, and regulatory approval processes. The high development costs and lengthy regulatory pathways associated with bringing new drugs to market pose financial barriers for small biotechnology firms and academic researchers. Additionally, uncertainties regarding regulatory requirements and endpoints for clinical trials in dry AMD may prolong the development timeline and increase the risk of clinical trial failure.
Limited Patient Access to Care and Treatment: Access to specialized eye care services, retinal specialists, and advanced treatments for dry AMD may be limited, particularly in rural or underserved areas. Geographic disparities in access to care, socioeconomic barriers, and lack of insurance coverage may prevent some patients from receiving timely diagnosis, treatment, and follow-up care. Improving access to eye care services through telemedicine, community outreach programs, and collaborative care models is essential for addressing disparities in patient outcomes.
Challenges in Patient Recruitment for Clinical Trials: Recruiting and retaining participants for clinical trials in dry AMD can be challenging due to the relatively low prevalence of the disease, stringent eligibility criteria, and competition among clinical trial sponsors. Enrolling a diverse patient population that reflects the heterogeneity of dry AMD and ensuring adequate representation of underrepresented groups (e.g., minorities, older adults) are critical for generalizing trial results and advancing evidence-based practice.
Regulatory and Reimbursement Challenges: Navigating complex regulatory pathways and securing reimbursement for novel therapies in dry AMD pose significant challenges for drug developers and manufacturers. Variability in regulatory requirements across jurisdictions, evolving evidentiary standards, and uncertainty regarding reimbursement coverage and pricing may deter investment in dry AMD drug development. Addressing regulatory and reimbursement challenges requires collaboration among industry stakeholders, regulatory agencies, payers, and patient advocacy groups to streamline approval processes and ensure timely access to innovative therapies.
Future Dry Age-related Macular Degeneration Market Analysis
Analyzing the future of the dry age-related macular degeneration (AMD) market involves considering emerging trends, technological advancements, regulatory developments, and evolving healthcare landscapes. Here's a prospective analysis of the future dry AMD market:
Growing Disease Burden: With the aging population and increasing life expectancy, the prevalence of dry AMD is expected to rise, leading to a growing disease burden and greater demand for effective management strategies. As a result, there will be an increased focus on research, diagnosis, and treatment options to address the needs of individuals with dry AMD.
Advancements in Diagnostic Technologies: Technological innovations in imaging modalities, such as optical coherence tomography (OCT), fundus autofluorescence (FAF), and adaptive optics imaging, will continue to improve the early detection, diagnosis, and monitoring of dry AMD. These advancements will enable more accurate assessment of disease progression, facilitate personalized treatment approaches, and support clinical decision-making.
Precision Medicine Approaches: Advances in genetics, molecular profiling, and precision medicine will enable personalized approaches to dry AMD management. Biomarker discovery efforts and genetic testing may identify individuals at higher risk of disease progression or with specific genetic subtypes of dry AMD, guiding treatment selection and prognosis prediction.
Emerging Therapeutic Modalities: Research into novel therapeutic modalities for dry AMD, including gene therapy, cell-based therapies, and regenerative medicine approaches, will continue to advance. Preclinical and clinical studies exploring the potential of gene editing technologies, stem cell transplantation, and neuroprotective agents aim to address the underlying mechanisms of dry AMD and provide disease-modifying treatments.
Combination Therapies: Combination therapies targeting multiple pathways involved in dry AMD pathogenesis may offer synergistic effects and improved treatment outcomes. Combinations of anti-inflammatory agents, neuroprotective compounds, angiogenesis inhibitors, and immunomodulatory drugs could provide additive or complementary effects, slowing disease progression and preserving vision in patients with dry AMD.
Digital Health Solutions: Digital health solutions, including telemedicine platforms, remote monitoring devices, and mobile applications, will play an increasingly important role in dry AMD management. These technologies enable remote patient monitoring, facilitate home-based vision testing, support patient education and self-management, and enhance communication between patients and healthcare providers.
Regulatory Support for Innovation: Regulatory agencies will continue to provide support and incentives to expedite the development and approval of innovative therapies for dry AMD. Designations such as orphan drug status, fast track designation, breakthrough therapy designation, and priority review designation will accelerate the regulatory review process for promising therapies targeting unmet medical needs in dry AMD.
Healthcare Integration and Access to Care: Integration of eye care services into primary care settings, multidisciplinary care teams, and collaborative care models will improve access to comprehensive care for individuals with dry AMD. Coordinated efforts among ophthalmologists, optometrists, retinal specialists, and primary care providers will optimize patient outcomes and ensure timely diagnosis and treatment.
Patient-Centered Care and Advocacy: Patient advocacy organizations and support groups will continue to play a vital role in raising awareness, promoting education, and advocating for the needs of individuals with dry AMD. Empowering patients, caregivers, and families through education, peer support networks, and access to resources will enhance patient-centered care and improve quality of life.
Economic and Market Dynamics: Economic factors, market competition, and healthcare policies will influence the commercialization and adoption of new treatments for dry AMD. Pricing strategies, reimbursement policies, and market access considerations will impact the availability and affordability of innovative therapies, shaping market dynamics and patient access to care.
Evolving Dry Age-related Macular Degeneration Treatment Outlook
The evolving treatment outlook for dry age-related macular degeneration (AMD) involves a multifaceted approach encompassing advancements in diagnostics, pharmacotherapy, regenerative medicine, and supportive care. Here's an overview of the evolving landscape of dry AMD treatment:
Diagnostics and Early Intervention: Advances in diagnostic imaging technologies, such as optical coherence tomography (OCT), fundus autofluorescence (FAF), and adaptive optics imaging, enable earlier detection and more precise monitoring of dry AMD. Early intervention strategies aim to identify high-risk individuals, detect disease progression, and initiate treatment before irreversible vision loss occurs.
Nutritional Supplements: Dietary supplementation with specific vitamins and minerals, such as vitamins C and E, zinc, copper, lutein, zeaxanthin, and omega-3 fatty acids, has been shown to slow the progression of dry AMD in certain patient populations. Research continues to explore the optimal formulation, dosing regimen, and long-term efficacy of nutritional supplements in preserving vision and reducing the risk of advanced AMD.
Anti-inflammatory Agents: Chronic inflammation plays a key role in the pathogenesis of dry AMD, making anti-inflammatory agents potential therapeutic targets. Drugs targeting inflammatory mediators, such as complement inhibitors, corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), and immunomodulators, aim to suppress retinal inflammation, reduce drusen formation, and prevent disease progression.
Neuroprotective and Anti-oxidant Therapies: Neuroprotective agents and antioxidants may help preserve retinal function and mitigate oxidative stress-induced damage in dry AMD. Compounds such as ciliary neurotrophic factor (CNTF), pigment epithelium-derived factor (PEDF), resveratrol, and coenzyme Q10 have shown neuroprotective effects in preclinical studies and clinical trials, offering potential therapeutic benefits for preserving photoreceptor and retinal pigment epithelial (RPE) cell function.
Angiogenesis Inhibitors: While abnormal blood vessel growth (neovascularization) is characteristic of wet AMD, emerging evidence suggests that angiogenic factors may also contribute to the pathogenesis of dry AMD. Anti-angiogenic agents targeting vascular endothelial growth factor (VEGF), such as aflibercept and ranibizumab, have shown promise in slowing disease progression and reducing geographic atrophy (GA) growth in certain subtypes of dry AMD.
Cell-Based Therapies: Regenerative medicine approaches using cell-based therapies, including stem cell transplantation, retinal pigment epithelial (RPE) cell replacement, and induced pluripotent stem cells (iPSCs), hold promise for repairing damaged retinal tissue and restoring vision in dry AMD. Clinical trials investigating the safety and efficacy of cell-based therapies are underway, with the goal of developing regenerative treatments for advanced dry AMD.
Gene Therapy and Genetic Targeting: Gene therapy strategies aim to correct genetic mutations associated with dry AMD, modulate gene expression, and restore normal cellular function in the retina. Techniques such as gene editing, RNA interference (RNAi), and viral vector delivery systems enable targeted delivery of therapeutic genes to retinal cells, offering potential disease-modifying effects and long-term benefits for individuals with genetic forms of dry AMD.
Drug Delivery Systems: Innovative drug delivery systems, such as sustained-release implants, nanoparticles, microparticles, and hydrogels, enhance the localized delivery of therapeutic agents to the retina, prolonging drug release and reducing treatment frequency. These drug delivery platforms improve treatment efficacy, minimize side effects, and optimize patient compliance in dry AMD management.
Combination Therapies and Multimodal Approaches: Combining multiple therapeutic modalities, such as anti-inflammatory agents, neuroprotective agents, and nutritional supplements, may offer synergistic effects and improved outcomes in dry AMD treatment. Multimodal approaches integrating pharmacotherapy, regenerative medicine, and supportive care aim to address the complex pathophysiology of dry AMD and optimize visual function.
Patient-Centered Care and Supportive Services: Patient-centered care models, low vision rehabilitation programs, and supportive services play a critical role in addressing the psychosocial impact of vision loss and optimizing patient outcomes in dry AMD. Low vision aids, adaptive technologies, vision rehabilitation therapy, and psychosocial support programs help individuals with dry AMD maximize their remaining vision, maintain independence, and improve quality of life.
Role of Companies in the Dry Age-related Macular Degeneration Market
In the Dry Age-related Macular Degeneration market, companies such as Alkeus Pharmaceuticals, Novartis, Molecular Partners, Stealth BioTherapeutics, Regenerative Patch Technologies, Aevitas Therapeutics, NGM Biopharmaceuticals, InflammX Therapeutics, Lineage Cell Therapeutics, Alexion AstraZeneca Rare Disease, Belite Bio, Katairo, Cognition Therapeutics, Apellis Pharmaceuticals, Galimedix Therapeutics, Amarna Therapeutics, 4D Molecular Therapeutics, Aviceda Therapeutics, Isarna Therapeutics, and others play a pivotal role in driving innovation, research, development, and the provision of treatments and therapies for individuals suffering from this chronic inflammatory skin condition. These companies encompass pharmaceutical giants, biotechnology firms, medical device manufacturers, and healthcare service providers, each contributing uniquely to the advancement of Dry Age-related Macular Degeneration management. Pharmaceutical companies lead the charge in developing novel drugs, ranging from topical corticosteroids to biologics targeting specific immune pathways implicated in Dry Age-related Macular Degeneration pathogenesis.
Dry Age-related Macular Degeneration Market Outlook - Key Conclusion and Analysis
The Dry Age-related Macular Degeneration market is undergoing a transformative period, driven by advances in research, innovation in therapeutic approaches, and shifting treatment paradigms. While significant progress has been made in improving outcomes for patients with Dry Age-related Macular Degeneration, several barriers continue to challenge the market's expansion, including high treatment costs, safety concerns, and regulatory hurdles. Looking ahead, personalized medicine, novel therapeutic targets, and digital health solutions are poised to shape the future of Dry Age-related Macular Degeneration management, offering new hope for patients and caregivers alike. Efforts to address these challenges and capitalize on emerging opportunities will be critical in advancing the field and ultimately improving the lives of individuals living with Dry Age-related Macular Degeneration.
Get a more detailed overview, at: Dry Age-related Macular Degeneration Market Outlook and Forecast
#Dry Age-related Macular Degeneration market#Dry Age-related Macular Degeneration#Dry Age-related Macular Degeneration market share#Dry Age-related Macular Degeneration treatment market#Dry Age-related Macular Degeneration market size
0 notes
Text
Clinical Trial Supply Management: Ensuring Seamless Operations

Clinical trials are vital components of the pharmaceutical and healthcare industries, providing valuable insights into the safety and efficacy of new treatments and medications. Behind the scenes of these trials lies a complex and intricate process known as clinical trial supply management. In this blog post, we'll delve into the essential aspects of clinical trial supply management, its significance in the research process, and the challenges it entails.
At its core, clinical trial supply management involves the coordination and oversight of all materials and resources required to conduct a clinical trial effectively. This includes not only the investigational drug or treatment being tested but also ancillary supplies such as placebos, medical devices, and laboratory equipment. The goal of supply management is to ensure that all necessary resources are available in the right quantities and at the right time, facilitating the smooth execution of the trial.
One of the primary challenges in clinical trial supply management is forecasting and planning for demand. Unlike traditional supply chains, where demand can be relatively stable and predictable, clinical trials are inherently dynamic and subject to numerous uncertainties. Factors such as patient recruitment rates, regulatory requirements, and unforeseen protocol changes can all impact demand for trial supplies, making accurate forecasting a challenging task.
To address this challenge, clinical trial supply managers rely on sophisticated forecasting models and algorithms that take into account various factors affecting demand. These models analyze historical data, patient enrollment projections, and other relevant variables to generate forecasts that guide procurement and inventory management decisions. By leveraging data-driven insights, supply managers can optimize inventory levels, minimize wastage, and ensure that sufficient supplies are available throughout the duration of the trial.
Another critical aspect of clinical trial supply management is ensuring compliance with regulatory requirements and quality standards. As clinical trials are subject to rigorous oversight by regulatory authorities such as the FDA and EMA, it is essential to adhere to strict guidelines regarding the handling, storage, and distribution of trial supplies. Failure to comply with these regulations can result in delays, fines, or even the suspension of the trial, highlighting the importance of robust supply management processes.
In addition to regulatory compliance, supply managers must also address logistical challenges related to supply chain logistics. This includes coordinating the transportation of trial supplies from manufacturers to clinical sites, managing temperature-sensitive products, and ensuring timely delivery to meet study timelines. In some cases, trials may involve multi-site or international collaborations, further complicating logistics and requiring careful coordination among stakeholders.
To overcome these challenges, many organizations are turning to advanced technologies and solutions to streamline their clinical trial supply management processes. This includes the adoption of cloud-based supply chain management platforms, automated inventory tracking systems, and real-time monitoring tools that provide visibility into supply chain performance. By embracing digital innovations, supply managers can enhance efficiency, reduce costs, and mitigate risks associated with clinical trial supply management.
In conclusion, clinical trial supply management is a critical function that plays a central role in the success of clinical trials. By effectively managing the procurement, distribution, and inventory of trial supplies, supply managers ensure that trials are conducted smoothly, safely, and in compliance with regulatory requirements. While the challenges associated with supply management are significant, the adoption of advanced technologies and best practices can help organizations overcome these hurdles and drive innovation in the field of clinical research.
0 notes
Text
Tagrix 80 mg (Osimertinib) - A Comprehensive Guide to Generic Osimertinib by IEB Pharma
Osimertinib, marketed under the brand name Tagrix 80 mg, is a revolutionary medication used in the treatment of non-small cell lung cancer (NSCLC). Developed and manufactured by IEB Pharma, this drug has garnered significant attention for its efficacy and safety profile in combating NSCLC, particularly in patients with specific mutations. This comprehensive guide explores the pharmacology, indications, dosage, side effects, and other pertinent information about Tagrix 80 mg, providing insight into its role in cancer therapy.
1. Understanding Osimertinib: Osimertinib belongs to a class of medications known as epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs). Unlike traditional EGFR-TKIs, osimertinib has demonstrated effectiveness in targeting tumors with specific EGFR mutations, such as the T790M mutation, making it a valuable therapeutic option for patients with advanced NSCLC.
2. Pharmacology and Mechanism of Action: The mechanism of action of osimertinib involves selective inhibition of EGFR tyrosine kinase activity, thereby blocking signaling pathways responsible for tumor growth and proliferation. Moreover, its high affinity for mutated EGFR variants, including T790M, enhances its potency against resistant cancer cells, making it a formidable weapon in the fight against NSCLC.
3. Indications and Usage: Tagrix 80 mg is primarily indicated for the treatment of metastatic NSCLC in patients with EGFR mutations, including those with the T790M resistance mutation. It is typically prescribed after the failure of previous EGFR-TKI therapy or as a first-line treatment in patients harboring specific mutations.
4. Dosage and Administration: The recommended dosage of Tagrix 80 mg is typically administered orally once daily, with or without food. Dosage adjustments may be necessary based on individual patient factors and tolerability. It is essential to adhere to the prescribed dosage and administration schedule to optimize treatment outcomes and minimize the risk of adverse effects.
5. Adverse Reactions and Side Effects: While osimertinib is generally well-tolerated, it may cause certain adverse reactions in some patients. Common side effects include diarrhea, rash, nausea, fatigue, and decreased appetite. Serious adverse reactions such as interstitial lung disease and cardiomyopathy may occur rarely but require prompt medical attention if experienced.
6. Precautions and Warnings: Before initiating treatment with Tagrix 80 mg, healthcare providers should assess patients for pre-existing conditions and potential drug interactions. Patients with a history of lung disease, cardiovascular disorders, or hepatic impairment may require close monitoring during therapy. Additionally, caution should be exercised when co-administering osimertinib with other medications that may affect its metabolism or QT interval.
7. Clinical Efficacy and Safety Profile: Clinical trials have demonstrated the efficacy and safety of osimertinib in various settings, including as a first-line treatment and in patients with central nervous system metastases. Its ability to penetrate the blood-brain barrier and target CNS lesions makes it particularly valuable in managing NSCLC with brain metastases. Furthermore, the favorable safety profile of osimertinib has made it a preferred option for many patients and healthcare providers.
8. Cost and Accessibility: As a generic alternative to branded osimertinib, Tagrix 80 mg by IEB Pharma offers a cost-effective option for patients without compromising quality or efficacy. The availability of generic osimertinib enhances accessibility to this essential medication, ensuring that more patients can benefit from its therapeutic effects.
Conclusion: In summary, Tagrix 80 mg (Osimertinib) by IEB Pharma represents a significant advancement in the treatment of NSCLC, offering a potent and well-tolerated therapeutic option for patients with EGFR mutations. With its demonstrated efficacy, favorable safety profile, and cost-effectiveness as a generic alternative, osimertinib has transformed the landscape of lung cancer therapy, providing hope for improved outcomes and quality of life for patients worldwide.
0 notes
Text
PRISM MarketView Spotlights Lipella Pharmaceuticals as it Seizes Opportunities in Rare Disease

New York, N.Y., March 07, 2024 - PRISM MarketView announces the release of an insightful interview with Lipella Pharmaceuticals’ CEO, Dr. Jonathan Kaufman, discussing the company's recent regulatory accomplishments and how investors stand to benefit.
Lipella Pharmaceuticals was recently granted Orphan Drug Designation by the FDA for LP-410, its drug candidate for oral Graft-versus-Host Disease (GvHD) and previously received Orphan Drug Designation for LP-10 in 2023. With these nods from the FDA, the company is on track to deliver two safe and effective treatments to cancer survivors, with a third therapeutic in its pipeline.
Dr. Kaufman remarked, “Orphan drug development can often be more profitable, entail lower risk and result in faster time to approval than non-orphan therapeutics. Our strategy involves leveraging the 505(b)(2) pathway which we believe will lower cost and allow for a faster approval process by allowing us to bypass Phase 1 trials and immediately initiate Phase 2 clinical trials. It also potentially mitigates risk from a CMC, safety and clinical development standpoint, and offers greater flexibility from the FDA.”
In conversation with PRISM MarketView, Dr. Kaufman discusses the strength of the company’s clinical pipeline, which has expanded significantly over the past 12 months. “We are excited to have been granted Orphan Drug Designation for two candidates targeting serious rare diseases that have a significant impact on patients’ lives and currently have no approved treatment. Our goal is to deliver safe and effective treatments as quickly as possible to the patients who need them most,” said Dr. Kaufman.
The full interview can be found at https://prismmarketview.com/lipella-pharmaceuticals-expanded-clinical-pipeline-targets-significant-unmet-need/
About Lipella Pharmaceuticals
Lipella is a clinical-stage biotechnology company focused on developing new drugs by reformulating the active agents in existing generic drugs and optimizing these reformulations for new applications. Additionally, Lipella maintains a therapeutic focus on diseases with significant, unaddressed morbidity and mortality where no approved drug therapy currently exists. Lipella completed its initial public offering in December 2022. For more information, please visit www.lipella.com or LinkedIn.
About PRISM MarketView:
Established in 2020, PRISM MarketView is dedicated to the monitoring and analysis of small cap stocks in burgeoning sectors. We deliver up-to-the-minute financial market news, provide comprehensive investor tools and foster a dynamic investor community. Central to our offerings are proprietary indexes that observe emerging sectors, including biotech, clean energy, next-generation tech, medical devices and beyond. Visit us at prismmarketview.com and follow us on Twitter.
PRISM MarketView does not provide investment advice.
Disclaimer:
This communication was produced by PRISM MarketView, an affiliate of PCG Advisory Inc., (together "PCG"). PCG is not a registered or licensed broker-dealer nor investment adviser. No information contained in this communication constitutes an offer to sell, a solicitation of an offer to buy, or a recommendation of any security. PCG may be compensated by respective clients for publicizing information relating to its clients’ securities. See www.pcgadvisory.com/disclosures
Media Contact
Company Name: Prism MarketView
Email: [email protected]
Phone: 646-863-6341
Website: https://prismmarketview.com
#press release#prism mediawire#stock market#investing#prismdigitalmedia#prismmarketview#healthcare#nasdaq#pharmaceutical#biopharma#lipo#Lipella Pharmaceuticals
0 notes
Text
Unveiling the Power of Beta Pack 150mg Injection: A Comprehensive Overview
In the ever-evolving landscape of medical advancements, Beta Pack 150mg Injection emerges as a noteworthy player, showcasing its potential in the field of healthcare. This comprehensive overview delves into the intricacies of Beta Pack 150mg Injection, shedding light on its composition, therapeutic uses, benefits, and potential impact on patient care.
Composition and Mechanism of Action:
Beta Pack 150mg Injection is a pharmaceutical formulation containing beta-1a interferon as its active ingredient. Interferons are proteins that play a crucial role in the body's immune response. Beta-1a interferon, specifically, is a type of protein that helps regulate the immune system, reducing inflammation and modifying the way the immune system responds to certain conditions.
The mechanism of action involves the modulation of immune responses, particularly in conditions where the immune system mistakenly attacks healthy cells. Beta Pack 150mg Injection aims to bring about a balance in the immune system, preventing excessive inflammation and damage to tissues.
Therapeutic Uses:
The primary therapeutic use of Beta Pack 150mg Injection is in the management of certain autoimmune disorders, including multiple sclerosis (MS). Multiple sclerosis is a chronic inflammatory condition of the central nervous system, where the immune system erroneously attacks the protective covering of nerve fibers.
By administering Beta Pack 150mg Injection, healthcare professionals aim to slow down the progression of the disease, reduce the frequency and severity of relapses, and alleviate symptoms associated with multiple sclerosis. The injection is designed to offer a targeted and systemic approach to managing the underlying immune dysregulation.
Benefits and Efficacy:
One of the notable benefits of Beta Pack 150mg Injection is its ability to provide a therapeutic intervention for conditions with limited treatment options. Its efficacy in managing multiple sclerosis has been established through rigorous clinical trials, where patients experienced a reduction in relapse rates and a slowing of disease progression.
The convenience of administration is another advantage, as the injection can be administered by healthcare professionals or self-administered by patients under proper guidance. This offers flexibility in treatment and empowers patients to take an active role in their healthcare.
Considerations and Precautions:
While Beta Pack 150mg Injection holds promise in the management of autoimmune disorders, it is essential to consider individual patient factors and potential side effects. Like any medication, it may have contraindications and precautions that healthcare providers need to evaluate before prescribing.
Close monitoring of patients during the course of treatment, along with regular check-ups, helps in identifying any adverse reactions and adjusting the treatment plan accordingly. Additionally, healthcare professionals should educate patients about the proper administration technique, potential side effects, and the importance of adherence to the prescribed treatment regimen.
Conclusion:
Beta Pack 150mg Injection represents a significant milestone in the realm of autoimmune disorder management, particularly in the context of multiple sclerosis. Its unique mechanism of action and demonstrated efficacy in clinical trials underscore its potential to make a positive impact on patient outcomes.
As ongoing research continues to unravel the intricacies of autoimmune disorders, Beta Pack 150mg Injection stands as a testament to the relentless pursuit of innovative solutions in the quest for improved patient care and quality of life. As with any medical advancement, ongoing vigilance, research, and collaboration between healthcare professionals and the pharmaceutical industry will pave the way for further developments and refinements in the field.
0 notes
Text
eClinical Solutions Market Size To Reach $22.7 Billion By 2030
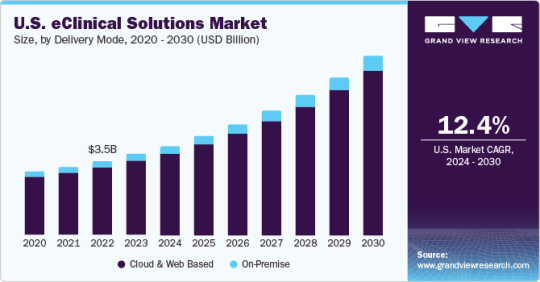
The global eClinical solutions market size is expected to reach USD 22.7 billion by 2030, growing at a CAGR of 14.1% from 2024 to 2030, according to a new report by Grand View Research, Inc. Increasing R&D activities by biopharma and pharma companies, application of software solutions in clinical trials, and expanding customer base are anticipated to fuel market growth. During COVID-19, clinical laboratories experienced high demand for COVID-19 tests. Clinical data management systems assisted these laboratories to seamlessly manage the huge influx of specimens daily. Technological advancements such as electronic data capture and Wi-Fi connectivity are projected to drive the market in the forthcoming years.
As the demand for tracking and analyzing clinical data increases, the need for effective clinical solutions rises. Unmet needs to manage efficient clinical development processes are poised to boost market growth over the forecast period. Moreover, digital transformation in the field of clinical trials and preference for data-centric approaches are providing a tremendous push to the market. Demand for integrated clinical IT solutions is increasing due to the massive volume of data generated during clinical development processes. eClinical solutions offer a single source of information that helps optimize the cost by eliminating redundant data entry and by reducing on-site verification and source data verification. Rising awareness regarding these advantages is projected to propel the market.
Increasing adoption of eClinical workflows in trials offers enormous potential in clinical development processes. These solutions can facilitate decision-making in each stage of development. It helps reduce cost and time between the development phase by utilizing seamless designs and identifying failing compounds. It offers rapid access to data and patient safety information, which helps make quick decisions. Market players engage in new product development and strategic alliances including partnership, agreement, promotional activities, etc. to keep market rivalry high. In August 2023, Sitero acquired Clarios eClinical technology suite to enhance clinical trial delivery. This acquisition demonstrates Sitero's dedication to remain at the forefront of innovation and offering its clients the best possible support and services.
Request a free sample copy or view report summary: https://www.grandviewresearch.com/industry-analysis/eclinical-solutions-market
eClinical Solutions Market Report Highlights
Based on product, the CTMS segment led the market in 2023 and accounted for a revenue share of around 20.2% owing to benefits such as centralized end-to-end management of clinical trial activities, elimination of reliance on manual processes, real-time status tracking, and maintenance of multiple databases, which cumulatively improve the overall efficiency of clinical trials
Web and cloud-based systems are anticipated to exhibit an exponential CAGR during the forecast period owing to integrated features such as flexibility, high accessibility, negligible handling costs, and easy data backup. Real-time data is available through these systems, which enables users to take quick decisions and provide high-quality information for risk-based monitoring
Based on development phase, the phase III segment held the largest market share of 53.3% in 2023. Phase I segment is expected to grow at the fastest CAGR over the forecast period
Based on end-use, the CRO segment held the largest revenue share in 2023. The segment is projected to rise at a remarkable CAGR during the forecast period owing to the growing inclination of pharmaceutical companies to reduce overall expenditure.
eClinical Solutions Market Segmentation
Grand View Research has segmented the global eClinical solutions market based on product, delivery mode, development phase, end-use, and region:
eClinical Solutions Product Outlook (Revenue, USD Million, 2018 - 2030)
Electronic Data Capture (EDC) and Clinical Data Management Systems (CDMS)
Clinical Trial Management Systems (CTMS)
Clinical Analytics Platforms
Randomization and Trial Supply Management (RTSM)
Clinical Data Integration Platforms
Electronic Clinical Outcome Assessment (eCOA)
Safety Solutions
Electronic Trial Master File (eTMF)
Electronic Consent (eConsent)
eClinical Solutions Delivery Mode Outlook (Revenue, USD Million, 2018 - 2030)
Web and Cloud based
On-premise
eClinical Solutions Development Phase Outlook (Revenue, USD Million, 2018 - 2030)
Phase I
Phase II
Phase III
Phase IV
eClinical Solutions End-use Outlook (Revenue, USD Million, 2018 - 2030)
Hospitals/Healthcare providers
CROs
Academic Institutes
Pharma & Biotech Organizations
Medical Device Manufacturers
eClinical Solutions Regional Outlook (Revenue, USD Million, 2018 - 2030)
North America
S.
Canada
Mexico
Europe
K.
Germany
France
Italy
Spain
Netherlands
Sweden
Denmark
Rest of Europe (EU) {RoE}
Asia Pacific
Japan
China
India
South Korea
Australia
New Zealand
Taiwan
Hong Kong
Singapore
Thailand
Vietnam
Rest of Asia Pacific (RoAPAC)
Central & South America
Brazil
Argentina
Chile
Rest of Latin America (RoLA)
Middle East & Africa
South Africa
Saudi Arabia
UAE
Egypt
Qatar
Rest of Middle East & Africa (RoMEA)
List of Key Players in the eClinical Solutions Market
Fountayn, formerly known as Datatrak International, Inc.
Oracle
Calyx, formerly part of Parexel International Corporation
Medidata (Dassault Systemes)
CRF Health (Signant Health)
Clario (ERT and Bioclinica)
eClinicalWorks
Merative (IBM Watson Health)
Anju Software
eClinical Solutions
MaxisIT
IQVIA
Castor
Veeva Systems
Browse Full Report: https://www.grandviewresearch.com/industry-analysis/eclinical-solutions-market
#eClinical Solutions Market#eClinical Solutions Market Trends#eClinical Solutions Market Size#eClinical Solutions Market Share
0 notes
Text
Advancements in Clinical Trials
Advancements in Clinical Trials: Perspectives from Europe
Clinical trials represent a frontier of medical progress, evolving swiftly with innovative methodologies and technologies. This article delves into the latest developments in clinical trials, specifically examining the European standpoint and how these advancements are shaping the future of medical research.
Introduction
The landscape of clinical trials is undergoing a profound transformation, driven by technological progress, evolving regulations, and a growing focus on patient-centric approaches. In Europe, a significant hub for clinical research, these innovations are reshaping trial methodologies, execution, and analysis.
Decentralized and Hybrid Trials
1. Patient-Centric Focus
A notable trend in Europe is the shift towards decentralized and hybrid trials, placing patients at the core of the research endeavor. Through the utilization of telemedicine, wearable devices, and remote monitoring, researchers can actively engage participants and gather real-world data, thereby fostering a more holistic comprehension of treatment outcomes.
2. Enhanced Accessibility
Decentralized trials broaden accessibility to a wider spectrum of participants, including those in remote or underserved regions. This inclusivity is pivotal in ensuring diverse and representative study cohorts, thus enhancing the generalizability of research findings.
Digitalization and Data Management
1. Utilization of Electronic Health Records (EHRs)
The integration of Electronic Health Records into clinical trials streamlines data capture and management processes. EHRs serve as a centralized repository of patient information, facilitating researchers' access to comprehensive, real-time data and augmenting the efficiency of trial operations.
2. Adoption of Blockchain Technology
In Europe, the uptake of blockchain technology is gaining momentum for ensuring the security and integrity of clinical trial data. Blockchain offers transparent and immutable data storage, mitigating the risk of fraudulent activities and bolstering trust in the research ecosystem.
Artificial Intelligence (AI) and Machine Learning (ML)
1. Predictive Analytics
AI and ML algorithms are harnessed to analyze vast datasets, foreseeing patient responses to treatments and identifying potential risks. This predictive analytics approach aids in optimizing trial designs, reducing costs, and expediting the identification of promising therapeutic interventions.
2. Implementation of Risk-Based Monitoring
AI-powered risk-based monitoring is revolutionizing the oversight of clinical trials for compliance and data quality. By scrutinizing data in real-time, AI algorithms can flag anomalies and deviations, enabling a targeted and efficient monitoring process.
Regulatory Progression
1. Embrace of Adaptive Trial Designs
European regulatory bodies are increasingly receptive to adaptive trial designs, enabling researchers to adapt study parameters based on accumulating data. This flexibility facilitates prompt identification of efficacious treatments, thus enhancing the overall efficacy of the clinical trial process.
2. Recognition of Real-World Evidence (RWE)
The acknowledgment of Real-World Evidence as a supplementary data source is expanding. Derived from routine healthcare data, RWE furnishes insights into the long-term effectiveness and safety of treatments, complementing traditional clinical trial data.
Collaborative Endeavors
1. Promotion of Public-Private Partnerships
Collaborations spanning academia, industry, and regulatory entities foster innovation in clinical trials. Public-private partnerships facilitate knowledge-sharing, resource pooling, and expertise exchange, thereby catalyzing more efficient and impactful research endeavors.
2. Establishment of Cross-Border Research Networks
The creation of cross-border research networks facilitates the amalgamation of data and expertise across European nations. These networks promote large-scale, multinational trials, accelerating the pace of discoveries and contributing to global medical progress.
Conclusion
The European outlook on innovations in clinical trials epitomizes a dynamic and forward-thinking approach to medical research. Decentralized trials, digitalization, AI, regulatory advancements, and collaborative initiatives collectively redefine the landscape, ensuring that clinical trials remain agile, patient-centered, and scientifically rigorous. As these trends evolve, Europe remains at the forefront of pioneering methodologies that will shape the future of clinical research.

1 note
·
View note
Text
Optimizing Trial Processes: How Clinical Trial Management Systems Drive Success
Clinical trials are intricate endeavors that demand meticulous organization and management. Clinical Trial Management Systems (CTMS) play a pivotal role in streamlining trial processes, enhancing efficiency, and driving success. This article explores how CTMS optimizes trial processes to facilitate successful clinical research endeavors.
Centralized Trial Management: CTMS serves as a centralized hub for managing all aspects of clinical trials. It consolidates trial-related information, including protocols, participant data, regulatory documents, and study progress updates, into a single, accessible platform. This centralization eliminates data silos and facilitates seamless collaboration among research teams, sponsors, and study sites.
Automated Workflows: One of the primary benefits of CTMS is its ability to automate repetitive and time-consuming trial processes. From participant recruitment and enrollment to data collection and reporting, CTMS automates workflows, reducing manual errors and accelerating trial timelines. Automated reminders and notifications ensure that tasks are completed promptly, keeping the trial on track.
Real-Time Data Capture and Analysis: CTMS enables real-time data capture and analysis, allowing researchers to monitor trial progress and make informed decisions on-the-fly. Electronic Case Report Forms (eCRFs) facilitate data collection at the point of care, eliminating the need for manual data entry and reducing transcription errors. Real-time analytics provide insights into participant recruitment, enrollment rates, and protocol adherence, empowering researchers to optimize trial strategies as needed.
Participant Management and Engagement: CTMS offers comprehensive tools for managing trial participants throughout the study lifecycle. From initial screening and consent to follow-up visits and retention efforts, CTMS streamlines participant management, ensuring a positive participant experience. Features such as automated appointment scheduling, reminders, and secure messaging portals enhance participant engagement and adherence to study protocols.
Regulatory Compliance: Compliance with regulatory requirements is paramount in clinical research. CTMS helps research organizations maintain compliance by providing robust regulatory features, including document management, audit trails, and protocol deviation tracking. Built-in compliance checks ensure that all trial activities adhere to applicable regulations, mitigating the risk of non-compliance and regulatory scrutiny.
Collaboration and Communication: CTMS fosters collaboration and communication among research teams, sponsors, and study sites, regardless of geographical location. Secure document sharing, messaging, and task assignment functionalities facilitate seamless communication and information exchange. By promoting collaboration, CTMS enhances transparency, accountability, and teamwork, driving success in clinical trials.
Scalability and Flexibility: CTMS solutions are scalable and flexible, capable of adapting to the evolving needs and complexities of clinical trials. Whether managing a single-site trial or a large-scale, multi-center study, CTMS can accommodate various trial designs, protocols, and workflows. Its scalability ensures that research organizations can scale up or down as needed, without compromising performance or usability.
Cost Savings and Resource Optimization: By automating processes, improving efficiency, and enhancing collaboration, CTMS helps research organizations save time and resources. The cost savings associated with CTMS implementation are substantial, reducing the overall cost of conducting clinical trials and maximizing return on investment. Additionally, resource optimization ensures that research teams can allocate resources effectively, maximizing productivity and driving success.
Conclusion: ctms play a critical role in optimizing trial processes and driving success in clinical research. By centralizing trial management, automating workflows, facilitating real-time data capture and analysis, enhancing participant management and engagement, ensuring regulatory compliance, fostering collaboration and communication, and offering scalability and flexibility, CTMS empowers research organizations to conduct trials more efficiently, cost-effectively, and with higher quality outcomes. As the demand for clinical research continues to grow, CTMS will remain indispensable tools for advancing medical science and improving patient care.
0 notes