Link
0 notes
Link
0 notes
Link

#caleidoscoop#TRTC#CPTSS#Complex Trauma#Dissociatie#Dissociatieve stoornis#Celevt#Hart College#TopReferent Trauma Centrum#lotgenoten dissociatie#DIS#DSnos#VCT#Vroegkinderlijke Chronische Traumatisering
1 note
·
View note
Text
The Horror of a Psychologically-Trauma
THE HORROR OF A PSYCHOLOGICALLY-TRAUMA
(c) Nique, 22-10-2014
Is it just Fear ?

Fear is just one of the unbearable sensation which tortures the body and mind of a psychologically-traumatized daily life handling-system of once personality (the self and ego states). Fear can make you Run away, fear can make you Freeze, fear can make you Cry, fear can make you suffer without you even knowing ‘why’. Nobody will disagree that fear can cause all that, but does it mean you suffer a psychologically-trauma if you suffer or suffered only Fear: NO !
The word 'pain' barely used . . .
But the definition of suffering pain says a lot:. “an unpleasant sensory and emotional experience associated with acute or potential tissue damage or described in terms of such damage”. Suffering physical pain, mental pain, emotional pain and psychologically pain all at once, will cause an ‘injury’ - psychologically and or physically. And (Child) sexual and or physical abuse causes such an ‘injury’ because it’s an horrific event.
A psychologically-injury
An horrific event triggers bodily responses, sensations, feelings and emotions all at once. Horror overloads your daily life handling-system (ego- and self-states), your mental state and common sense with extreme stress. Even by witnessing a 'horrific event' you can get emotionally and bodily over-stressed and it can even cause a phobia for experiencing (witnessing or remembering) it ever again.
Horrific events or a horrific experiences can make us lose our common sense, activate unwanted bodily responses, can cause uncontrollable sensations, feelings and emotions or can even cause an unimaginable strength which can lead us to do the unthinkable as if we are in a hypnotic state. .
Ever heard of:
Blind madness?
Blind sadness?
Blind fear?
Or over excitement – uncontrollable joy which make one scream and or sideling ?
Read full Column .....
#Complex Trauma#cptsd#did#Trauma and Dissociation#traumatology#DIS#dissociatieve identiteitsstoornis#dissociative identity disorder#structural dissociation#ptsd#PTSS#cptss
0 notes
Link
Let op dit is GEEN GRAP: Pnt 2 DIS-zorg heeft totaal NIETS te maken met Dissociatie of de Dissociatieve Identiteitsstoornis !
0 notes
Link
0 notes
Photo

25-sep-14
©Nique EU Disja - www.complex-trauma.eu
Psychologically-Trauma & Dissociation
Because I noticed some people have still problems to understand the meaning of a personality Handling-System: I made a schema to help out in getting a sober understanding of ‘what do we mean by naming the total Handling system of a traumatize-Personality: the ANP-EP handling system.
The understanding of
Structural dissociation of the personality
THE ANP - EP handling SYSTEM (the personality)
The Self states (SS's - ANP parts of the ANP-EP handling system): Are task oriented personality parts which function automatically and recognize (remember) what to do at that moment or to which task oriented needs. They function present time task oriented and know automatically what to do on that moment or during that task (they memorize).
Ego States (alter states)
Those parts of our personality react emotion oriented and are fully controlled by emotions. They answer to emotionally daily live needs or events.
Those parts of our personality can provide personality reactions which we call emotional healthy reactions (normal), but they also can develop a pathologically behavior. Borderline, Narcissistic personality disorder, (pathological) psychopathic behavior and other mental pathological behavior, etc..
Dissociated Emotional Personality Parts (EP’s of the ANP-EP handling system)
A psychologically traumatized dissociated personality part – we call it an EP !!
Within the structural dissociation of the personality (theory) we call those parts 'Emotional personality Parts' which cause dissociative behavior. These parts hold a memory of a traumatic event or a part of a traumatic event of the past (physical and emotional memories)
Those parts can be:
1. totally dissociated by the personality (full dissociation)
2. partial dissociated by the personality (partial dissociation)
How to understand the meaning of an ANP-EP Handling system?
There I made a schema to give a better understanding of the different personality states we own and or all can develop.
Read full document .pdf
http://www.complex-trauma.eu/pdf/140925-ANP-EP-handlingsystem.pdf
#PTSD#Complex PTSD#CPTSD#Trauma and Dissociation#Dissociation#Structural dissociation#Ellert Nijenhuis#kathy steele#Onno van het Hart#dissociative identity disorder#dissociatieve identiteitsstoornis#DID#DIS#DisNique#Nique EU Disja
0 notes
Photo
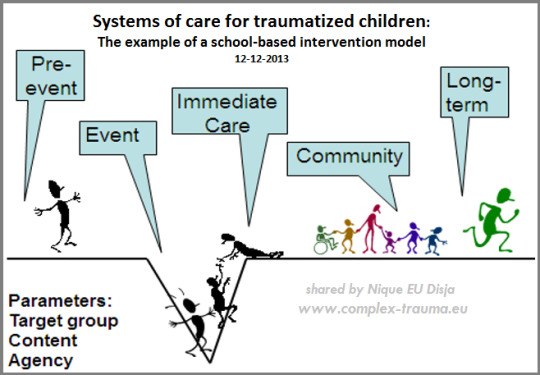
Systems of care for traumatized children:
The example of a school-based intervention model
Danny Brom, Naomi L. Baum & Ruth Pat-Horenczyk
The Israel Center for the Treatment of Psychotrauma,
Herzog Hospital, Jerusalem
12-12-2013
Introduction
Terrorism and war threaten not only law enforcement and the military, but also, and, in the case of terrorism, mainly the civilian population. The same is true for natural disasters and domestic violence. When disaster strikes, the immediate response is characterized by activities that have to ensure survival. Only when initial safety has been reached, there is room for emotional and cognitive processing of what happened. In a society, such as Israel, where war and terrorism are continuous, the threat to functioning, wellbeing and mental health of both adults and children is a pressing public health issue.
- - -
Traumatized children in society: A model of care
We present a comprehensive model for building resilience in school communities that have been exposed to the trauma of terrorism and war. We will describe the various levels of intervention beginning with the principal and the leading teams in the school, and then highlight our resilience building workshops for teachers. The guidelines for school- based screening for identifying post-traumatic distress will be clarified followed by three different modules of school-based treatment interventions. We conclude with challenges for implementation and future directions based on our experience.
Children exposed to mass trauma
In the aftermath of war and terrorism, children may downplay or deny their symptoms for fear of overtaxing their already over-burdened parents, and adolescents may avoid, ignore, or numb their symptoms either to assert their independence or simply to move on (Hoven, Duarte, & Mandell, 2003). After the Oklahoma bombing in 1995, Pfefferbaum, Pfefferbaum, Gurwitch, Nagumalli, Brandt and Robertson. (2003) found that only 5% of 2720 children surveyed after the Oklahoma bombing in 1995 received counseling. Further, after 9/11, a large school- based screening conducted by the NYC Board of Education 6 months after the attacks, reported that 2/3 of children identified with posttraumatic distress were not referred to any type of treatment (Hoven, Duarte & Mandell, 2003). Such findings highlight the need to actively reach out and provide screening and treatment resources for children and adolescents suffering in silence from war- and terrorism-related traumas.
Increasing evidence suggests that when students are directly asked to report their own reactions and behaviors, they tend to express their post-traumatic distress (Pat-Horenczyk, Abramovitz, et al., 2007). Similarly, adolescents clearly indicate when they feel they need help, and these reports have a strong correlation with their answers on questionnaires about symptoms (Schiff, Pat-Horenczyk, Benbenishty et al, 2010). This underscores the importance of simply asking the proper questions to elicit responses that can help identify child and adolescent post-war and post-terrorism syndromes.
Most individuals exposed to traumatic experiences seem to cope well or even thrive in the aftermath of traumatic events. There are various ways to conceptualize what constitutes resilience and what constitutes a "resilience factor." Such factors could include a combination of protective characteristics, such as competence or self-efficacy (Garmezy, 1991; Masten & Coatsworth, 1998), or the underlying processes of coping that an individual adopts in the face of adversity (Luthar, Cicchetti, & Becker, 2000). Discussions abound regarding what constitutes a resilient response to trauma. Most agree that resilient individuals can still experience some difficulty or distress in the course of coping with traumatic events, but they also must be able to draw on their resources to resume normal functioning.
Bonanno (2004) claims that resilient individuals maintain a degree of equilibrium during their traumatic experiences and "generally exhibit a stable trajectory of healthy functioning across time" ( p. 21), which separates them from individuals who "recover" from psychopathological episodes consequent to adversity. Our working definition of resilience is based on the formulation suggested by Masten (2001), which regards resilience as "ordinary magic," in contrast to extraordinary behavior in the face of adversity.
Read full document:
shared by
www.complex-trauma.eu
Nique
5 notes
·
View notes
Photo

ICD-11 (beta CPTSD) & DSM-5
By Nique:
After so many years and eventually a sub type PTSD categorized in the new DSM-5, the discussion to differentiate 5 different classes of a Complex trauma gets a global hearing.
We knew already 5 different classes of Trauma disorders
1. Acute Stress Disorder (acute short term Trauma disorder)
2. PTSD (trauma type I)
a. with Partial dissociation
b. with Full dissociation
3. Complex PTSD – with dissociation, now known as:
a. OSDD (trauma type II with comorbidity disorder . . . )
b. DID (trauma type III – per definition caused by Trauma – severe PTSD)
It’s a very good thing to see this discussion finds is way after so many years, and of course we will follow this development.
= = =
THE CO-OCCURRENCE OF PTSD AND DISSOCIATION
A dissociative-posttraumatic stress disorder (PTSD) subtype has been included in the DSM-5.
However
The LPA identified five classes:
one of which constituted a severe PTSD group (30.5 %), and one of which constituted a dissociative-PTSD group (13.7 %). None of the included, demographic, trauma, or clinical covariates were significantly predictive of membership in the dissociative-PTSD group compared to the severe PTSD group.
Conclusions:
a significant proportion of individuals report high levels of dissociation alongside their PTSD, which constitutes a dissociative-PTSD subtype. Further investigation is needed to identify which factors may increase or decrease the likelihood of membership in a dissociative-PTSD subtype group compared to a severe PTSD only group.
Article access due payment
ICD-11
Conceptualization ICD-11 (will be ready in 2015)
PTSD Posttraumatic stress disorder & CPTSD
An alternative conceptualization of PTSD is presented in the International Classification of Diseases, 11th version (ICD-11), which is due to be completed in 2015. In contrast to the DMS-5, the ICD-11’s guiding principle for classification development is clinical utility. As such the ICD-11 proposes two connected stress- and trauma related disorders: PTSD and complex PTSD (CPTSD; Maercker et al., 2013). The experience of any kind of stressful life event is viewed as a ‘‘gateway’’ for a consideration of a diagnosis of PTSD or CPTSD.
ICD-11 (Beta)
Disorders specifically associated with stress:
1 Post-traumatic stress disorder
2 Complex post-traumatic stress disorder
…..
Beta Draft ICD-11
Read full article:
www.complex-trauma.eu
+Nique EU Disja
Google+ share
#PTSD#cptsd#traumatology#trama center TRTC#Complex Trauma#Dissociation#trauma and dissociation#clinical trauma#dsm-5#ICD-11
0 notes
Text
Trauma disorders, Borderline- and Dissociative Disorders

I did receive the question:
Could you try to explain in your own words and average understandable language; the different types of Trauma disorders (diagnoses), versus a Borderline Personality Disorder and the relation of both with Dissociative Disorders – without the interference of the understanding of a Structural dissociation of the personality.
And my answer to it is: Yes I feel very honored to give it a try in my own words.
Read the column on . . . www.complex-trauma.eu

I. TRAUMA and Posttraumatic Stress Disorders – PTSD & CPTSD
Very simplified we know 3 main groups of diagnoses to a mental disturbance caused by Trauma:
1 an acute short term mentally disturbance (ASD)
2 a middle long term mentally disturbance (PTSD)
3 a long term e.g. chronically disturbance (CPTSD)
a bit more defined:
Acute Stress Disorder
an acute short term mentally disturbance / reaction to a one time experienced Traumatic event
for example: witnessing a very heavy train accident
PTSD
Post-Traumatic Stress disorder – middle long term mentally disturbance caused by experiencing a dead scary Traumatic event
for example: a kidnapping or a onetime rape experience, or other dead scary experiences
C-PTSD
Complex Post-Traumatic Stress disorder – a long term e.g. chronically mentally disturbance caused by experiencing more than one Traumatic event
a. Childhood trauma like sexually and or physically abuse
for example: incest or other repeated child molestation e.g. child abuse
b. War experiences (veteran care), etc.
To simplify: above we have mentioned the different types of Trauma disorders (diagnoses).
And keep in mind that those diagnoses can be given to everyone who experienced a Traumatic event. So also to people with Borderline, with Autism, with no mental disorder, etc.. From the policeman to the house wife – they can all experience a dead scary traumatic event which can lead to a post traumatic stress disorder.

II. DISSOCIATIVE DISORDERS – DD
The Second mental disorders I want you all to get acquainted with is the category
Dissociative Disorder – abbreviation = DD (watch out, it’s no DID)
Dissociative identity disorder – DID a trauma related polysymptomatic condition which is characterized by a hidden presentation
Other Specified Dissociative Disorder – OSDD
Dissociative Amnesia
Depersonalization/Derealization Disorder
sub group:
Unspecified Dissociative Disorder (DDnos)
Are dissociative disorders with switching behavior to different personality states always related or caused by TRAUMA and or a Dissociative Identity Disorder (DID)……… : NO
Switching between personality parts is not a phenomenon that only belongs to a Dissociative Identity Disorder (trauma related).There are other disorders that have symptoms of identity problems and switching behavior between personality states such as a theatrical personality disorder, a Borderline Personality disorder, a bipolar disorder or schizophrenia.
A Dissociative Disorder (DD) has a wider range of being a co-morbidity disorder.
PTSD and it’s relation to Dissociative Disorders (OSDD and DID):
Within the category Dissociative Disorders, we know two types of diagnoses which seems to be related to Trauma:
1. Otherwise Subscribed Dissociative Disorders (OSDD) and
2. the Dissociative identity Disorder (DID)
Those two Dissociative disorders are both categorized by Trauma specialists as Complex Trauma related disorders.
And both disorders are known with a wide range of dissociative problems. From Amnesia, Depersonalization to Derealization to somatic dissociation, etc.. The difference between a trauma related OSDD and DID is the comorbidity of disorders and the presentation of the Switching behavior. Both disorders are likewise severe and don’t tell a thing about more or more severe Trauma experiences – because both disorders are categorized as likewise very severe disorders ! they cause severe clinically distress and agony in life.
A Trauma related diagnose tells you only something about the complexity of the disorder(s).

III. BORDERLINE PERSONALITY DISORDER – BPD
not C-PTSD related – Abbreviation BPD
A Borderline personality disorder is a personality disorder which causes severe agony to life. It’s also a disorder which very often is misunderstood and stigmatized. People with a BPD suffer a lot, so please don’t judge them by the disorder but try to understand them.
BPD is a diagnose of a mental disorder which points out a list of ongoing disturbed, unstable and or harmful symptomatically behavior caused by a broad range of influences during childhood and a biologically given mental weakness. Examples of causes:
too less love and attention (negative child neglect)
too much negative love and attention (positive child neglect)
broth up by parents with harmful addictions
broth up by parents with social problems
broth up in a harmful e.g. stressful living environment
etc.
and the most upper handed cause to develop BPD:
is most likely a mental weakness given by biologically genes (Borderline structure).
A by nature given, not being able to handle or coupe well with stressful situations. A biological basis to develop a BPD.
Note: Not everyone born with the biologically genes will develop a Borderline Personality Disorder during life – A Borderline structure (is not a BPD) only tells something about the mental straight to coupe or handle with stressful situations.
Some psychologist e.g. mental clinicians like to call the causes to the development of a BPD – ‘childhood trauma’. But if you understand the clinical definition of Trauma you can’t place those causes in a direct line of Traumatic experiences. So I fully disagree with people who think and or declare that a Borderline Personality disorder is per definition caused by Trauma, and or is always trauma related, because it isn’t.
A Borderline Structure or a Borderline Personality Disorder by itself isn’t caused by Trauma, nor Trauma related!

And now we end up to the most spoken CLINICAL DISPUTE * * *

BPD and It’s relation with Dissociative Disorders (OSDD and or DDnos):
Of course it all needs research and a global acceptance to define the difference and or relation of causes and the influences of different comorbidity disorders, but I will give you a bit of an explanation in the line of both clinical streams which are still arguing about the cause and understanding of a BPD in combination with Dissociative Disorders and or a Trauma related dissociation:
A bit Freudiaans and a bit Janetiaans – I think; both theoretically streams do have a point
BPD + DDnos not Trauma related
BPD + Dissociative symptoms and switching behavior to different emotional personality states NOT Trauma related
(BPD + comorbidity DDnos)
People who suffer a Borderline Personality Disorder very often can’t coupe (independently) with stressful situation. They clamp on to addictive behavior to escape the inner stress and daily life stress, and or they clamp on to other people which can guide them through a stressful situation of life. If stress comes in to (such) a relation someone who suffers a BPD wants also to escape this relation (again) by clamping on to another person. They don’t attach on a healthy way and it’s not uncommon that someone with a BPD has a stormy history of different relationships or switches back and forward towards and between more than one relationship. They easily panic if they are left alone. And they show very often impulsive and or addictive behavior. It’s also not uncommon that someone who suffers a BPD seeks attention, I prefer to call it - they seek HELP because they are scared - they do this to escape the inner stress and the fear of being left alone. Life itself is sometimes even too much to handle and the fear of loneliness then also gets enormous, almost unbearable.
Graphed by this fear they sometimes develop different somatic problems with no physical cause, or they even start to develop their own internal family and play mates to escape the fear of being left alone. They start to Dissociate by the development of emotional personality parts.
BPD + (CPTSD) OSDD Trauma related
BPD + Dissociative symptoms and switching behavior under the influence of emotional personality parts:Trauma Related
(BPD + CPTSD + OSDD)
Like every human being also someone who suffers a BPD can experience a dead scary traumatic events or have suffered also Childhood sexual and or physical abuse which leads to the symptoms of a PTSD or a CPTSD with dissociative symptoms.
It’s also not oncoming that you see also severe Dissociative symptoms and dissociative Switching behavior in this category of a double mental disturbance and category of diagnosis.
But it’s also very difficult for diagnosticians to diagnose BPD + Dissociative Symptoms and the Switching behavior to other personality states of this category, because they need to determine if the Dissociative symptoms are caused by the BPD or by trauma related Dissociation (OSDD). And that is not an easy thing to do.
Fact or Factious:

Someone who suffers a BPD + Dissociative symptoms (DDnos and or OSDD) suffers severe agony in life. We know that this group is also the most difficult group to treat because of the underlying BPD and wide range of dissociative symptoms. Prognosis of treatment aren’t much positive because of the severity of the combinations of disorders. And although researches are doing their best to develop better diagnostically instruments (differential instruments) and treatment possibility’s, it’s still a group which gets to less global attention and understanding.
For the difference between a OSDD and DID dissociative disorder
I refer to the following link: The difference between OSDD and DID
(c) Nique
www.complex-trauma.eu
#complex trauma#PTSD#CPTSD#Borderline#BPD#dissociation#structural dissociation#DID#dissociative identity disorder#trama center TRTC#trtc#Disjanique#Disnique#trauma#psychology
1 note
·
View note
Photo

De 4 Google+ Communities of Complex Trauma and Dissociative Disorders.
A link share community of trauma related articles and research papers. - only link, informative en educative sharing.
A discussion Group of trauma related articles and research papers.
A 18+ (ANP) Support Group Complex-Trauma and Dissociative disorder sufferers.
A WERDID Dissociative Identity Disorder Support Group. EP child parts are also welcome
www.complex-trauma.eu
Nique
0 notes
Text
The difference between OSDD+ and DID
The difference between a secondary and tertiary SD
2-8-2014
Other Specified Dissociative Disorder (300.15) and the Dissociative Identity Disorder (300.14)

A Dissociative Disorder (DD) leads very rarely to a diagnose of a dissociative Identity disorder (DID), more common is a secondary SD. Read also my previous post and the notification I shared of Prof.Ph.D. Onno van der Hart and Ph.D. Ellert Nijenhuis.
And although a trauma related secondary Structural Dissociation, diagnoses OSDD+ in combination with another (personality) disorder such as BPD far more often occurs than a DID, you will find hardly websites that inform you about a OSDD+. It is also a very severe Trauma related disorder which presents itself with a wide range of dissociative symptoms and switching behavior under the influence of EP's (more than one). But its also very often mistaken with DID and diagnosed as a DID - but it isn't a DID.
That alone should ring a bell to the leg of understanding a Trauma related SD !!
Why are there so much websites and blogs about DID and nearly none about OSDD+ (DSM-5 code 300.15 - ICD F44.89 - ) And why are most of the DID related websites focused on, and explaining ANP-EP switching behavior and not ANP-ANP switching behavior which is more common to a DID?
I leave that answer to my readers who are willing to understand the theory of a trauma related structural dissociation of the personality (SD), but I will give you all some theoretically and educational stuff to think over in order to understand even better the difference between a OSDD+ and DID - e.g. the difference between a secondary and a tertiary structural dissociation of the personality.
Switching behavior caused and under the influence of Emotional personality parts ANP-EP’s switching is not a phenomenon that occurs most commonly as a symptom of a dissociative identity disorder (DID) - a Tertiary Structural Dissociation of the Personality. Indeed it is more common to a Secondary Structural Dissociation of the personality OSDD + very often in combination with a Borderline Personality disorder.
So there are also other disorders that have symptoms of identity problems, or which causes switching behavior, such as a theatrical personality disorder, a Borderline personality disorder (BPD), a Bipolar disorder, Schizophrenia etc.. A Dissociative Disorder (DD) has a wider range of being a co-morbidity disorder.
Take notice:
a tertiary Structural Dissociation - a trauma related Dissociative Identity disorder (DID) - is a poly-symptomatic condition which is characterized by a hidden presentation (Boon/Daijer). Diagnoses of a ‘trauma related’ structural dissociation of the personality can only be done by an experienced clinical trauma psychologist/psychotherapist which is specially taint to do so.
Read the full column . . . www.complex-trauma.eu
http://www.complex-trauma.eu/?p=836
#Dissociation#Dissociative Identity disorder#CPTSD#PTSD#structural dissociation#complex trauma#TRTC#Onno van der Hart#Ellert Nijenhuis#Caleidoscoop
2 notes
·
View notes
Text
The Diagnostically reality of a SD-DID sufferer

SD * Structural dissociation
MPD * Multiple Personality Disorder
DID * Dissociative Identity Disorder
BPD * Borderline Personality Disorder
Are all DID diagnoses a tertiary structural dissociation?
Technically and to SD diagnostically instruments: YES
Reality to the present time of a global diagnostically acceptance and understanding of a SD: NO
Until this moment level 2 and 3 are a diagnostically mess. Because there is still no suitable diagnostically DSM category to define a Complex Trauma (CPTSD) with severe dissociative symptoms.
Result: Level 2 and 3 of the SD are totally mixed up as a Dissociative Identity Disorder.
To this matter I want to share a personal note:
Last February I had a nice and also educative conversation with Professor Ph.D. Onno van der Hart. During this conversation we also spoke about the frequency DID is diagnosed. And that to my opinion to many people get diagnosed with a DID while they suffer more likely a level 2 of the Structural dissociation of the personality. And to this personal observation and conclusion I asked him some feedback and he answered to me:
"Nique, I agree with you that people much too quickly speak of a DID when in fact they talk about a secondary dissociation of the personality -- as it shows that though is more common than tertiary dissociation of personality. In short, I am very aware that the dissociative disorders (DD) include more than just DID, and that this often insufficiently is indicated.
I'm afraid that speaking in terms of primary, secondary and tertiary levels --- of a structural dissociation of the personality, as we do, not generally is accepted. Because then one must also accept our theory, and not everybody knows him or want to start thinking in those terms.". (Prof. Ph.D. Onno van der Hart, February 2014)
//
In may 2014, I also had a shared conversation with my own personal CPT and Ellert who both go in the same Dutch traumatology team and which also diagnosed my case. I spoke to them about the mixed up diagnoses to the personality disorders, SD and level 3 as a DID, and Ellert answered (Literal text translation):
"Sometimes the facts are more strongly than the theory. I mean: about 40% of the current DID population meets the criteria of BPS. An even larger group has a personality disorder (approximately 60%). BPS also develops in early childhood, sometimes BPS seems trauma-related, sometimes it seems not. You could also say that BPS is a sign of a certain imbalance of the personality.
Very general: on axis II diagnoses are not made out on the basis of a development, but on the basis of symptoms.(Ph.D. Ellert Nijenhuis, may 2014)".
//
My personal conclusion:
lots of info which you can find on the internet and which is carried out by people who were diagnosed with classical MPD in the past and now declare themselves as diagnosed with DID as a Trauma related tertiary structural dissociation of the personality;
lots of them don't even understand the theory of a Structural dissociation and inform you totally wrong about it. Until now I could not find one website who informs you right about the structural dissociation of the personality such as given by: Kathy Steele, Ellert Nijenhuis and Onno van der Hart.
My words are probably rough to take in and lots of people will hate me for saying so, but a diagnose is also not meant to please but to point out the reality of symptoms, behavior and a the mental disorder(s) someone is suffering. So again I answer to the question: is all the info on the net about DID - - related to a Tertiary Structural dissociation of the personality? NO !
Because to make such a statement we would need to re-diagnose all the MPD/DID sufferers which were diagnose for the 21st century and which aren't diagnosed by the diagnostically instruments (interviews and differential D instruments) which define a diagnose of a Trauma related Structural Dissociation of the personality.
Knowledge does change and has changed.
But in all those years they never adjusted diagnoses given in the past.
Read full Column on the website www.complex-trauma.eu
#CPTSD#DID#Dissociative Identity Disorder#Structural Dissociation#complex trauma#onno van der hart#kathy steele#ellert nijenhuis#trama center TRTC#DIS#Dissociatieve Identiteitsstoornis
0 notes
Text
Reboot your auto pilot
How to reboot our own auto pilot such as 'reacting by instinct or spontaneously' so that your auto pilot starts to functioning more in line with your own core values.
Dr. Manual Saint-Victor explains Video !
Complex-Trauma EU G+ Community Discussion !

#Complex Trauma#dissociatieve identiteitsstoornis#structural dissociation#Dr.Manual Saint-Victor#psychological trauma#DID#dissociative identity disorder#PTSD#CPTSD#PTSS#CPTSS#Nique Disja
3 notes
·
View notes
Text
What is Hypnosis
Paul Ramsay and Dr. Manual Saint-Victor explains
I enjoyed this interview so much ! I can advise everyone and certainly people who work with a Psychotherapeutically hypnotherapist to watch this video. It will give more understanding to Hypnosis and that it isn’t something to be afraid of.
What is Hypnosis?
http://www.youtube.com/watch?v=8NkjwdQ7xq4
#hypnotherapy#ptsd#cptss#structural dissociation#dissociation#dissociative identity disorder#dissociatieve identiteitsstoornis#Complex Trauma#trauma center
1 note
·
View note

