#COVID impairs immunity
Text
I don't know what to do
in the longer term
month-to-month
it's been day-to-day
and systemic changes;
these need to happen, but,
what are feasible,
what can be brought about?
it can seem so insurmountable
regardless
I endeavor to hold on, here,
metaphorical waters rising
as the plague is spreading
and hope you are hanging on as well
a person I may never meet
is still someone I can care about
all the best,
lots of love,
and wishing you strength
and wellness
may we
remember the reality of the pandemic
now and in the future
<3
COVID floats like smoke
COVID is airborne
COVID is ongoing
COVID is NOT "mild"
COVID is NOT over
COVID impairs immunity
#COVID floats like smoke#COVID is airborne#COVID is ongoing#COVID is not mild#COVID is not over#COVID impairs immunity
2 notes
·
View notes
Text

Cat in the Hat:
"The German Health Minister gave an important update on the Covid situation yesterday.
I’ve written up the section of his speech from the video below for easy reading.
It’s immensely refreshing to see a government minister warning of the harms of Covid in such a transparent way."
https://x.com/_catinthehat/status/1732092683508678954
Prof. Karl Lauterbach
Health Minister, Germany
4 December 2023
"This second (long Covid) round table was very interesting, lasting three and a half hours. It serves as a unique forum for dialogue among scientists, researchers and those affected by long Covid, facilitating the exchange of ideas.
There are many new findings about long Covid. Not all of them are good news. One piece of not-so-good news concerns the fact that long Covid is actually still a problem for those who are newly infected. One estimate that has been put forward is that the risk of contracting long Covid now, even after vaccination, is around 3%. Now you may say, "that's not such a big risk" , but there are tens of thousands of people who are repeatedly affected in a short period of time. And so, the long Covid problem has not yet been solved.
We have also established that there really are many subgroups of long Covid and that we do not yet have a cure. And it was clearly pointed out that we are also dealing with problems here that will challenge society as a whole, because vascular diseases often occur after long Covid. Throughout Europe, we are currently seeing an increased incidence of cardiovascular disease in the middle-age group - from 25 to 50. This is associated with the consequences of Covid infections.
We also very often find cognitive impairment in older people. And one participant pointed out that it may well be like the Spanish flu, where 20 years after the Spanish flu there was a significant increase in Parkinson's disease and probably also dementia.
This is something we must pay attention to, as the past infection afiects how the immune system in the brain functions, as well as the brain's blood vessels, potentially increasing the long-term risk of these major neurodegenerative diseases. This is why we need to conduct very intensive research. This research has played a major role.
What is the overall assessment of the situation now?
We have to be careful. Long Covid is not curable at the moment. We also know that over 40% of those who have several manifestations of long Covid, for example, five or more, still have symptoms after 2 years, so it doesn't seem to heal spontaneously. We also know that those whose symptoms are more pronounced at the beginning are less likely to heal.
So some of what we know from the demographics of long Covid has been confirmed, and we now know more precisely which mechanisms in the brain, but also in the blood vessels and the immune system, are responsible for this. Professor Scheibenbogan will explain this briefly later.
At this point, I can only say the following - this is particularly important to me:
First of all, long Covid is a disease that stays with us and that we cannot yet cure. And we are seeing an increasing number of cases as the waves of infection continue to affect us.
Secondly, Covid is not a cold - with a cold, you don't usually see any long-term effects. You don't see any changes in the blood vessels. You don't usually see an autoimmune disease developing. You also don't usually see neurological inflammation - these are all things that we see with long Covid. Therefore, one should not assume that Covid infection is just a common cold. It can affect brain tissue and the vascular system, and we still lack an effective treatment, making these studies crucial.
Significantly, we know that the risk of long Covid decreases when you're infected but have been vaccinated. That's why it's concerning that only 3 million people have been vaccinated with the new, adapted vaccine. That is a very bad result.
Please protect yourself from severe infections.
Please protect yourself from long Covid.
Currently, the danger posed by Covid is indeed being underestimated. Nothing is worse than infecting someone at Christmas who then becomes seriously ill and may not fully recover."
Alt text is included in all images of this post.
#covid#not a cold#please wear a mask#pandemic#pandemic not over#long covid#Karl Lauterbach#Germany#German health minister
10K notes
·
View notes
Text
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Text
Although many Canadians act as though the pandemic has ended, the airborne virus that causes COVID-19 continues to evolve at an amazing pace with devastating consequences for both individuals and the public at large.
The pandemic may no longer be a major conflagration but it still kills about 140 Canadians a week while morphing into a steady viral blaze sustained by dirty air, waning immunity and overt political indifference.
What was once a giant wave of acute illness has become a series of often unpredictable wavelets driven by ever-changing variants that can cause chronic illness. Long COVID, a disabling health event that can affect multiple organs and destabilize the immune system, now affects millions and continues to claim new victims.
A 2023 Danish study recently confirmed that about 50 per cent of those diagnosed with long COVID fail to improve 18 months after infection regardless of the variant.
Long COVID has taken a huge toll among health-care workers. Anywhere from six to 10 per cent of Quebec’s health-care workforce, for example, has been derailed by long COVID.
Seventy-one per cent of health-care workers impaired by long COVID reported that their state of health now interferes with their ability to function. Another 16 per cent said that they are often unable to work. Multiply this data across the country and then ask: How sustainable is this trend?
Continue reading
423 notes
·
View notes
Text
January 12, 2024
“Five years, 10 years, 20 years from now, what are we going to see in terms of cardiac impairment, pulmonary impairment, neurologic impairment? It’s year five in the pandemic, but there’s still a lot we don’t know about it.”
212 notes
·
View notes
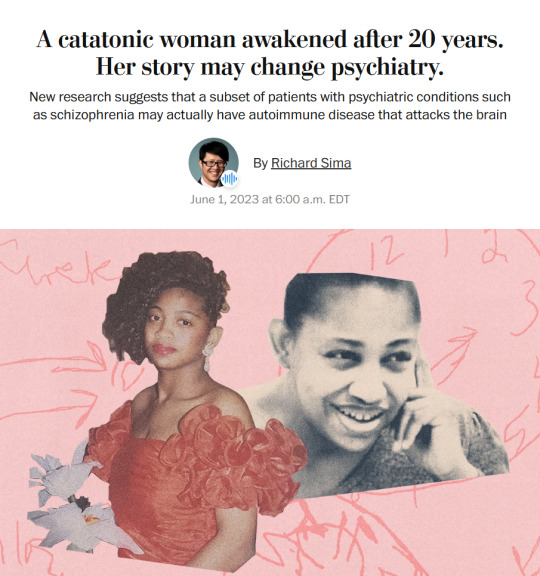
Photo

[image id: two screenshots of four tweets by user lisa_iannattone on Twitter, posted on 19 December 2022 at 1:14 p.m., reading sequentially: "It's absolutely wild to me that we're pretending that the higher than average number of respiratory tract infections and the pandemic of adults with pneumonia this year is not a warning sign of immune impairment. This is literally how immunodeficiency would present.In clinical practice, we we want to screen for the possibility of an undiagnosed underlying immunodeficiency syndrome, "how many respiratory infections do you get in an average year?" and "have you had pneumonia more than once?" are the 2 first questions we ask.There's been more pneumonias among my healthy adult friends & acquaintances in the last 6 months than among my immunosuppressed patients in the last 6 years. Something is clearly off. And healthy adults with pneumonia is not a viral transmission dynamics issue.This thread blew up and some people aren't sure if I'm suggesting immunity debt. Definitely not. Staying healthy doesn't make you sick, pathogens do. As for the immunity "gap", it's likely a contributing factor but doesn't explain adults with pneumonia. It's SARS2 I'm worried about.
end image id]
hey, the pandemic is not over. wear a mask.
in case this is unclear, immunocompromised, immunosuppressed, and other disabled people are not getting sick the same way as healthy adults because they are masking the fuck up and/or still largely being forced to isolate, while many many “healthy” adults are not. just because you are healthy doesn’t mean you are immune to long-term effects from covid. anyone can become disabled at any time. immunity debt is not real.
do your part to protect yourself and others. not wearing a mask is worse than ableism. It’s disablist.
Please at least wear masks in public indoor, and crowded outdoor spaces. Make public spaces safe and accessible for everyone.
#immunity debt#immunity debt is not real#ableism#wear a fucking mask#wear a mask#pneumonia#immunodeficiency#immunocompromised#disability#pretending the pandemic is over doesn't make it true#disablism#described#like disabled people are largely still isolating because of people who don't give a shit if they catch or spread covid
1K notes
·
View notes
Text

https://onlinelibrary.wiley.com/doi/10.1002/brx2.58
Published April 16, 2024
Abstract
Caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), coronavirus disease 2019 (COVID-19) primarily manifests as respiratory dysfunction. However, emerging evidence suggests SARS-CoV-2 can invade the brain, leading to cognitive impairment (CI). It may spread to other brain regions through transsynaptic neurons, including the olfactory, optic, and vagus nerves. Moreover, it may invade the central nervous system through blood transmission or the lymphatic system. This review summarizes the neuroimaging evidence from clinical and imaging studies of COVID-19-associated CIs, including magnetic resonance imaging and 18F-fluorodeoxyglucose positron emission tomography-computed tomography. The mechanisms underlying COVID-19-associated CIs are currently being actively investigated. They include nonimmune effects, such as viral proteins, tissue hypoxia, hypercoagulability, and pathological changes in neuronal cells, and immune effects, such as microglia and astrocyte activation, peripheral immune cell infiltration, blood-brain barrier impairment, cytokine network dysregulation, and intestinal microbiota. Inflammation is the central feature. Both central and systemic inflammation may cause acute and persistent neurological changes, and existing evidence indicates that inflammation underlies the elevated risk of Alzheimer's disease. Finally, potential therapeutic options for COVID-19-associated CIs are discussed. In-depth research into the pathological mechanisms is still needed to help develop new therapies.
#mask up#covid#covid 19#covid isn't over#pandemic#covid conscious#long covid#covid is airborne#wear a mask#coronavirus
57 notes
·
View notes
Text

“‘Five years, 10 years, 20 years from now, what are we going to see in terms of cardiac impairment, pulmonary impairment, neurologic impairment? It’s year five in the pandemic, but there’s still a lot we don’t know about it.’
“As of Dec. 31, the pandemic’s official death count sat at 7 million. But the true total is likely at least three times higher, she said.”
(Source)
[ID: “COVID levels are up to 19 times higher than reported, WHO says as it warns of the potential dangers of repeat reinfection: ‘We don’t know everything about this virus’ Because most people have some immunity to COVID, “we don’t necessarily know how often we’re getting infected,” a WHO spokesperson said. BY ERIN PRATER, January 12, 2024 3:45 PM EST”]
75 notes
·
View notes
Text
The Cause of Depression Is Probably Not What You Think (Joanna Thompson, Quanta Magazine, Jan 26 2023)
"A literature review that appeared in Molecular Psychiatry in July was the latest and perhaps loudest death knell for the serotonin hypothesis, at least in its simplest form.
An international team of scientists led by Joanna Moncrieff of University College London screened 361 papers from six areas of research and carefully evaluated 17 of them.
They found no convincing evidence that lower levels of serotonin caused or were even associated with depression.
People with depression didn’t reliably seem to have less serotonin activity than people without the disorder.
Experiments in which researchers artificially lowered the serotonin levels of volunteers didn’t consistently cause depression. (…)
Although serotonin levels don’t seem to be the primary driver of depression, SSRIs show a modest improvement over placebos in clinical trials.
But the mechanism behind that improvement remains elusive.
“Just because aspirin relieves a headache, [it] doesn’t mean that aspirin deficits in the body are causing headaches,” said John Krystal, a neuropharmacologist and chair of the psychiatry department at Yale University.
“Fully understanding how SSRIs produce clinical change is still a work in progress.”
Speculation about the source of that benefit has spawned alternative theories about the origins of depression. (…)
Repple warns, however, that another explanation for the effects his team observed is also possible: Perhaps the depressed patients’ brain connections were impaired by inflammation.
Chronic inflammation impedes the body’s ability to heal, and in neural tissue it can gradually degrade synaptic connections.
The loss of such connections is thought to contribute to mood disorders.
Good evidence supports this theory.
When psychiatrists have evaluated populations of patients who have chronic inflammatory diseases like lupus and rheumatoid arthritis, they’ve found that “all of them have higher-than-average rates of depression,” said Charles Nemeroff, a neuropsychiatrist at the University of Texas, Austin.
Of course, knowing that they have an incurable, degenerative condition may contribute to a patient’s depressed feelings, but the researchers suspect that the inflammation itself is also a factor.
Medical researchers have found that inducing inflammation in certain patients can trigger depression.
Interferon alpha, which is sometimes used to treat chronic hepatitis C and other conditions, causes a major inflammatory response throughout the body by flooding the immune system with proteins known as cytokines — molecules that facilitate reactions ranging from mild swelling to septic shock.
The sudden influx of inflammatory cytokines leads to appetite loss, fatigue and a slowdown in mental and physical activity — all symptoms of major depression.
Patients taking interferon often report feeling suddenly, sometimes severely, depressed.
If overlooked chronic inflammation is causing many people’s depression, researchers still need to determine the source of that inflammation.
Autoimmune disorders, bacterial infections, high stress and certain viruses, including the virus that causes Covid-19, can all induce persistent inflammatory responses.
Viral inflammation can extend directly to tissues in the brain. Devising an effective anti-inflammatory treatment for depression may depend on knowing which of these causes is at work.
It’s also unclear whether simply treating inflammation could be enough to alleviate depression.
Clinicians are still trying to parse whether depression causes inflammation or inflammation leads to depression. “It’s a sort of chicken-and-egg phenomenon,” Nemeroff said.
Increasingly, some scientists are pushing to reframe “depression” as an umbrella term for a suite of related conditions, much as oncologists now think of “cancer” as referring to a legion of distinct but similar malignancies.
"And just as each cancer needs to be prevented or treated in ways relevant to its origin, treatments for depression may need to be tailored to the individual."
82 notes
·
View notes
Note
Hey, I noticed that you tag all your posts with long covid, and I was wondering if you've read the study where they found the cause of long covid brain fog. file:///C:/Users/12406/Downloads/s41593-024-01576-9.pdf
I also made a translation that puts the abstract into easier terms, and I'm working on the rest of the study.
Vascular disruption has been implicated as a symptom of COVID and might predispose the neurological symptoms of long covid, yet it is unclear how blood–brain barrier (BBB) function is afected in these conditions. Here we show that BBB disruption is evident during acute infection and in patients with long COVID with cognitive impairment, commonly referred to as brain fog. Using advanced brain imaging, we show BBB disruption in patients with long COVID-associated brain fog. RNA analysis of peripheral blood mononuclear cells* revealed dysregulation of the coagulation system and dampened adaptive immune response in individuals with brain fog. Accordingly, blood cells showed increased adhesion to human brain endothelial cells** in test tubes. Together, our data suggest that sustained systemic infammation and persistent localized BBB dysfunction is a key feature of long COVID-associated brain fog.
*mononuclear blood cells refer to blood cells that have one nucleus. They make up most of your immune system.
**The cells that make up the walls of your blood vessels. Specifically designed to be slippery because when blood cells adhere to them it causes clotting - this is the dysregulation of the coagulation system they were talking about.
Let me know what you think! Or if you have questions
I find it very interesting that many people with long covid land up getting many autoimmune disorders. I have a few autoimmune disorders and have many, if not most, of the symptoms that people with long covid have. For example, I can not read what you wrote, just parts of it. I have cognitive issues, sometimes severe.
9 notes
·
View notes
Text
WHO: "Five years, 10 years, 20 years from now, what are we going to see in terms of cardiac impairment, pulmonary impairment, neurologic impairment? It’s year five in the pandemic, but there’s still a lot we don’t know about it."
https://www.reddit.com/r/HermanCainAward/
#world health organization#world health organisation (who)#who#long covid#covid19#covid isn't over#covid 19#covid#coronavirus#corona virus#viruses#virus#ausgov#politas#auspol#tasgov#taspol#australia#fuck neoliberals#neoliberal capitalism#anthony albanese#albanese government#infectious diseases#infection#health#healthcare#health & fitness#health and wellness#occupationalhealth#plague doctor
14 notes
·
View notes
Text
Although many Canadians act as though the pandemic has ended, the airborne virus that causes COVID-19 continues to evolve at an amazing pace with devastating consequences for both individuals and the public at large.
The pandemic may no longer be a major conflagration but it still kills about 140 Canadians a week while morphing into a steady viral blaze sustained by dirty air, waning immunity and overt political indifference.
What was once a giant wave of acute illness has become a series of often unpredictable wavelets driven by ever-changing variants that can cause chronic illness. Long COVID, a disabling health event that can affect multiple organs and destabilize the immune system, now affects millions and continues to claim new victims.
A 2023 Danish study recently confirmed that about 50 per cent of those diagnosed with long COVID fail to improve 18 months after infection regardless of the variant.
Long COVID has taken a huge toll among health-care workers. Anywhere from six to 10 per cent of Quebec’s health-care workforce, for example, has been derailed by long COVID.
Seventy-one per cent of health-care workers impaired by long COVID reported that their state of health now interferes with their ability to function. Another 16 per cent said that they are often unable to work. Multiply this data across the country and then ask: How sustainable is this trend?
The cost of living in a ‘viral soup’
While the media focus concern on the potential next big nasty viral wave, evolutionary biologist T. Ryan Gregory says that threat seems less likely than before, but the current reality is nothing like normal.
“We are not dealing with Omicron-like waves but a viral soup,” Gregory told The Tyee. “We are seeing a near-constant high level of hospitalizations that falls just below overwhelming them but is nonetheless unsustainable. More health-care workers are getting sick and that just adds to the strain on the whole system.”
What worries Gregory, an expert on the evolution of COVID variants at the University of Guelph, “are the long-term effects of multiple infections and the sustained pressure on the health-care system and well-being.”
Yet the current impact of COVID — measurably higher than at some previous points during the pandemic — remains largely ignored or poorly reported.
Tara Moriarty, a University of Toronto infectious disease expert and co-founder of COVID 19 Resources Canada, recently tallied the imperfect data, and it is bracing. She calculates that about one in every 23 Canadians is now infected with COVID. We are not at the low point of the pandemic in Canada. To the contrary, compared with a previous time during the pandemic, infections are 25 times higher and the rate of long COVID is 19 times higher. Meanwhile the hospitalization rate is 13 times higher and deaths are 25 times higher.
In the middle of October, Moriarty calculated that COVID patients occupied about nine per cent of intensive care beds and 21 per cent of hospital beds across the country. (The average hospitalization rate during the pandemic has been seven per cent.) The estimated cost of this sustained viral assault is $274 million a week.
Governments peddling denial
Most governments seem intent on diminishing or hiding these realities. They avoid any talk about the effectiveness of masking in public places or the value of improved ventilation and filtration in schools and workplaces. It’s a demonstrated fact that the virus travels through the air in tiny smoke-like aerosols that can infect people at much greater distances than six feet, but the natural responses to this reality are not encouraged by our leaders.
Alberta, for example, now pretends that COVID is just another mild respiratory disease and reports its doings along with influenza and RSV activity.
Despite this push for “normalization,” only one disease stands out as a routine killer and dominant occupant of hospital beds on the province’s “respiratory virus dashboard.” And that’s COVID. COVID also dominates outbreaks in Alberta’s hospitals and long-term care facilities where masking and attention to ventilation have become haphazard practices.
Lumping COVID in with other respiratory diseases is also patently misleading. A recent Swiss study compared hospitalized patients infected with COVID and those infected with the flu. Those with COVID had a 1.5-fold higher risk of dying in hospital up to 30 days after infection than patients infected by influenza A. The death rate was even higher for unvaccinated people.
A 2023 Swedish study also found the death rate from Omicron greatly surpassed that of influenza patients.
And next comes the increased risk of cardiovascular problems. Medical researchers have long observed strokes and acute myocardial infarctions in patients after respiratory infections, such as influenza. But COVID breaks the mould here. Compared with patients with the flu, the risk of stroke is more than sevenfold higher in COVID-19 patients.
This is likely tied to the fact that COVID can inflame the vascular system through which the body’s blood travels. New non-peer-reviewed evidence suggests that even a mild infection can temporarily damage endothelial cells that line the interior of blood vessels.
COVID may begin with the symptoms of a cold or flu for most people, but it often ends as thrombotic or vascular disease in a small percentage for reasons researchers don’t clearly understand. The virus can therefore infect multiple organs from the brain to the kidneys.
Immune systems and long COVID
COVID can also unsettle the immune system by damaging T-cell response, as recent studies have illustrated.
These findings make all the more illogical the current, widespread blasé attitude towards the ever-evolving virus.
Let’s begin with diabetes, which itself stresses the immune system and makes it less effective.
Early in the pandemic, researchers suspected there might be a connection between having COVID and later developing diabetes. Now it’s confirmed. Earlier this year the Smidt Heart Institute at Cedars-Sinai organization in Los Angeles found that a COVID infection dramatically increases the risk for developing Type 2 diabetes and that this risk continues with Omicron variants.
“The trends and patterns that we see in the data suggest that COVID-19 infection could be acting in certain settings like a disease accelerator, amplifying risk for a diagnosis that individuals might have otherwise received later in life,” noted Susan Cheng, a senior author of the study and a professor of cardiology.
Another study found that the incidence of diabetes in Black and Hispanic youth has increased by 62 per cent since the pandemic. The authors noted that COVID can bind to receptors in the pancreas, resulting in damaged cells.
A Canadian study also found steep increases in diabetes after COVID infections. University of British Columbia researchers examined a large population of British Columbians (more than 600,000) and discovered that people infected with COVID had a 17 to 22 per cent higher risk of developing diabetes within a year compared with uninfected people.
Concluded the researchers: “SARS-CoV-2 infection was associated with a higher risk of diabetes and may have contributed to a three per cent to five per cent excess burden of diabetes at a population level.”
Related research has also demonstrated that COVID infection can trigger or lead to a variety of autoimmune disorders.
One recent Lancet study that looked at nearly a million people who were unvaccinated between 2020 and 2021 found that COVID cases experienced much higher incidence of autoimmune disease than non-infected people.
These autoimmune conditions included rheumatoid arthritis, systemic lupus erythematosus, vasculitis (inflamed and swollen blood vessels), inflammatory bowel disease and Type 1 diabetes mellitus.
A similar German study, which has not yet been peer reviewed, evaluated a cohort of 640,701 unvaccinated individuals with PCR-confirmed COVID infection during 2020 for the risk of autoimmune conditions. The researchers identified “a 42.6 per cent higher likelihood of acquiring an autoimmune condition three to 15 months after infection” compared with a group of 1,560,357 individuals who weren’t infected.
The researchers also found that a COVID infection “increased the risk of developing another autoimmune disease by 23 per cent” in individuals with pre-existing immune conditions.
The autoimmune studies confirm that COVID can be a significant immune deregulator. The Yale University immunologist Akiko Iwasaki, who has dedicated her lab to studying long COVID, notes that “there's misfiring of the immune response happening in the severe COVID patients that lead to pathology and lethality.” Even a mild infection can lead to this misfiring and long COVID, and this group tends to be women between the ages of 30 and 50.
Reinfection is no trifle
The autoimmune studies, of course, don’t tell us anything about the current crop of variants and what autoimmune or cardiovascular diseases they might trigger in the future. But the precautionary principle would suggest avoiding infection.
The highly regarded U.S. epidemiologist Ziyad Al-Aly, who also studies long COVID, has been very clear about the hazardous consequences of reinfection in terms of chronic disease such as diabetes, brain inflammation and heart disease: “Two infections are worse than one and three are worse than two.”
His most recent research shows that people with mild infections are still at risk for chronic disease two years after the fact. Patients who were hospitalized with COVID were at even greater risk for chronic complications.
“The concern here is that this pandemic will generate a wave of chronic disease that we did not have before the pandemic,” Al-Aly, chief of research and development at Veterans Affairs St. Louis Health Care System, recently told Euronews Next.
“Even when the pandemic abates and is in the rear-view mirror, we will be left with it after the fact in the form of a chronic disease that for some people may last for a long time or even a lifetime,” added Al-Aly.
The Tyee has repeatedly reported evidence that immunity to COVID from natural infection or vaccination is not long-lasting because of the nature of the virus.
The research now confirms that infections can even leave some people more vulnerable to reinfection. A startling Canadian study published this year looked at 750 vaccinated elders at long-term care facilities where COVID deaths continue to be high. They found infection with Omicron in its first wave actually made these inmates more susceptible to reinfection in subsequent waves. Counterintuitively, these people were more prone to reinfection than patients who had never experienced COVID.
“Our current vaccine schedules are based on the assumption that having had an infection provides some level of protection to future infections, but our study shows that may not be true for all variants in all people,” noted Dawn Bowdish, an immunologist and one of the study’s authors.
What our health leaders should be saying
The implications of these findings are plain enough. The pandemic has a long tail, and it can be found in a growing population of people experiencing chronic disease. Therefore, limiting transmission is still the most important public health goal.
We know how to do that but are reluctant to employ the tools. Masking in crowded public spaces or poorly ventilated buildings during periods of high infection is a proven viral risk reducer. Cleaning dirty air in workplaces and schools removes the virus and other pollutants such as wildfire smoke and should be an urgent public health crusade.
We might all take inspiration from what happened at one Australian school. Concerned parents studied airflow and then installed HEPA filters with the result that improved air circulation stopped COVID transmission dead.
Rigorous surveillance testing is also essential to inform citizens of the advancing or retreating COVID risks.
Vaccinations play a role because they can significantly reduce the risk of hospitalization, death and long COVID. But current vaccines will not stop transmission. Or end the pandemic.
In a recent study a group of U.S. researchers modelled a variety of paths that COVID might take in the future.
If repeat infections and vaccinations actually work to improve immunity and dent the pandemic over time, then models suggest infections and the incidence of long COVID should decline too.
But as Omicron demonstrated, community immunity is unlikely to be achieved via existing vaccines and especially at a time when vaccine hesitancy is rising.
In one pessimistic scenario the researchers posited that “a first infection may provide partial protection against a second infection” but the combination of new variants and complexities surrounding immune responses “could then increase the susceptibility to tertiary and quaternary infections.”
That means a good proportion of the population could end up with long COVID in the absence of effective public health measures and the development of a durable, transmission-blocking vaccine.
“More pessimistic assumptions on host adaptive immune responses illustrate that the longer-term burden of COVID-19 may be elevated for years to come,” added the researchers.
17 notes
·
View notes
Text
I have been thinking: COVID consciousness is like climate crisis consciousness.
People can pretend it isn't real (e.g. "climate change isn't happening," or, "COVID is over," fallacies such as this).
Others can acknowledge it is real, but be despairing, choosing to focus on "the futility of things" (e.g. "maybe we could have changed CO2 emissions in the seventies, but we're past the point of no return, and the Earth is going to burn and there is nothing we can do; DAMN YOU ALL TO HELL etc." or, "humanity brought it upon itself, there's no point in trying to prevent the spread of COVID; now everyone is going to get sick," defeatist attitudes such as this…)
But one can come to appreciate the interconnectedness of everything, and, that while one might not have the ability to control one's destiny, let alone the destiny of future generations, one does have the ability to keep trying to make things as… good as possible? As beneficial to as many as possible? Most heartening? Most loving? Even when it is difficult!
Because:
We are all interconnected!
Caring about you makes sense because you caring about me makes sense because we inhabit a common reality! Caring about one another makes our mutual reality better for ALL of us, instead of being caught up in whatever this ridiculous pretense is that everything is fine, this weird attitude that the "immune compromised don't matter, because they'd be dying anyway,"
And even though I think you should care about others
I also keep thinking
like
do some people
not
realise
that
COVID infection has been documented to reduce immune function
for like
like
PRETTY MUCH ANYONE
so
THAT MEANS COVID IS A RISK FOR PRETTY MUCH EVERYONE
and
you do not have a better immune system because of moral superiority! A virus does not care about that kind of thing when it's floating through the air in tiny bits of airborne moisture!!!
And even those with previously of the most robust health do not have the assurance that their immune system will prevent long term impairment because of COVID infection; those who were previously athletes have found themselves sidelined by COVID infection.
Like…
COVID is BAD
AND
COVID is NOT over
And
Some people could be brought around to taking more careful measures if they knew the actual reality of things:
COVID floats like smoke, meaning that to prevent infection whenever one is indoors with strangers (e.g. public places!) one should be wearing an effective, well-fitting mask,
COVID hampers one's immune system
It's bad to spread it to others!
Why is this a controversial opinion?!
Like, let's stop the spread of disease!
This seems like a good idea!
And some people would agree with this, but for whatever reason they're isolated/cut off from the truth, and the trick is finding ways to inform these folks…
But then…
For whatever reason…
It seems like some other people somehow cannot acknowledge reality…
And I find it the weirdest thing!
And I mean, I've been around the internet ("I've seen things you people wouldn't believe…")
I've seen how people can get into echo chambers, affirming realities they want to be true…
But...
In the spring of 2020, I would not have imagined that things would be like this, in 2023…
I don't know what else to say?!
Care about other people?!
Take care of yourself?!
Take care of the biosphere and consider how the output of human activity impacts climactic cycles and the way the living situation will be for coming generations!?!?!?!
Avoid spreading disease because it can impair and kill yourself and/or others?!?!?!
Getting beyond the
"Yes"-
Because the "Yes" can mean
Despair
"Yes it is irreparably bad so there is no point in caring,"
And
Maybe everything will fry! Maybe the next meteorite will come and wipe us out as one did the dinosaurs, and the next species to evolve will have no idea we ever existed! And caring about climate change was pointless?
OK?!
So I should be the-right-amount-of-despairing?! It was better to be hopeless instead of hopeful?! No hope is the appropriate response? What if I hope, anyway?
What if somehow I make things better for someone three generations from now, even if I never meet them, even if humanity dies in five generations? Even if the world is hit by a meteorite tomorrow, why is it cringe if I try to make things better on what turns out to be the last day on the Earth?!
What if you cared about others, even if these others are coming generations and you will never meet them?
Why give into despair?
Even if things are REDONK.
There is PLAGUE; should we not be avoiding it?!
We could get beyond Yes- to but!
"Yes- there is a terrible situation!"
"...BUT this does not have to lead to despair…!"
"…BUT what we do now makes a difference, and cooperation is integral!"
Danged if I've got all the answers, but I'm pretty sure that caring about one another is a good place to start.
I may never meet you, but I can care about you.
<3
And not saying it isn't hard. Like. It can be hard not to despair.
Keep on keepin' on!!! <3
#COVID#COVID is BAD#COVID is NOT over#COVID is ongoing#covid is airborne#pandemic#mask up#long covid#masks#sars-cov-2#covid-19
24 notes
·
View notes
Text
Some commentators have described this situation — the crashing of wave after wave of COVID-19, a steady drip, drip, drip of death and mounting chronic illness — as the "new normal". But other experts insist it doesn't have to be, and that continuing on the current trajectory is unsustainable — especially in light of data showing that COVID has decreased life expectancy, will cost the global economy an estimated $US13.8 trillion by 2024, and is decimating the lives of millions of people who have developed long COVID.
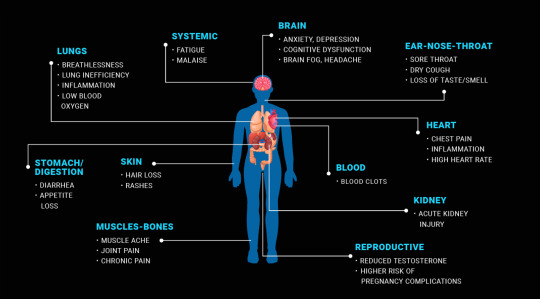
Meanwhile, studies continue to pile up showing COVID-19 can cause serious illness affecting every organ system in the body, even in vaccinated people with seemingly mild infections. It can cause cognitive decline and dysfunction consistent with brain injury; trigger immune damage and dysfunction; impair liver, kidney and lung function; and significantly increases the risk of cardiovascular disease and diabetes. Then there's long COVID, a debilitating disease that robs fit and high-functioning people of their ability to think, work and exercise.
16 notes
·
View notes
Text
Apparently Madeline Miller, of Song of Achilles fame, also still has Long Covid 3 years after catching Covid-19 in early 2020. Her op-ed is copied below (mostly under a Keep Reading link) for those who can't get past WaPo's paywall.
https://www.washingtonpost.com/opinions/2023/08/09/madeline-miller-long-covid-post-pandemic/
In 2019, I was in high gear. I had two young children, a busy social life, a book tour and a novel in progress. I spent my days racing between airports, juggling to-do lists and child care. Yes, I felt tired, but I come from a family of high-energy women. I was proud to be keeping the sacred flame of Productivity burning.
Then I got covid.
I didn’t know it was covid at the time. This was early February 2020, before the government was acknowledging SARS-CoV-2’s spread in the United States.
In the weeks after infection, my body went haywire. My ears rang. My heart would start galloping at random times. I developed violent new food allergies overnight. When I walked upstairs, I gasped alarmingly.
I reached out to doctors. One told me I was “deconditioned” and needed to exercise more. But my usual jog left me doubled over, and when I tried to lift weights, I ended up in the ER with chest pains and tachycardia. My tests were normal, which alarmed me further. How could they be normal? Every morning, I woke breathless, leaden, utterly depleted.
Worst of all, I couldn’t concentrate enough to compose sentences. Writing had been my haven since I was 6. Now, it was my family’s livelihood. I kept looking through my pre-covid novel drafts, desperately trying to prod my sticky, limp brain forward. But I was too tired to answer email, let alone grapple with my book.
When people asked how I was, I gave an airy answer. Inside, I was in a cold sweat. My whole future was dropping away. Looking at old photos, I was overwhelmed with grief and bitterness. I didn’t recognize myself. On my best days, I was 30 percent of that person.
I turned to the internet and discovered others with similar experiences. In fact, my symptoms were textbook — a textbook being written in real time by “first wavers” like me, comparing notes and giving our condition a name: long covid.
In those communities, everyone had stories like mine — life-altering symptoms, demoralizing doctor visits, loss of jobs, loss of identity. The virus can produce a bewildering buffet of long-term conditions, including cognitive impairment and cardiac failure, tinnitus, loss of taste, immune dysfunction, migraines and stroke, any one of which could tank quality of life.
For me, one of the worst was post-exertional malaise (PEM), a Victorian-sounding name for a very real and debilitating condition in which exertion causes your body to crash. In my new post-covid life, exertion could include washing dishes, carrying my children, even just talking with too much animation. Whenever I exceeded my invisible allowance, I would pay for it with hours, or days, of migraines and misery.
There was no more worshiping productivity. I gave my best hours to my children, but it was crushing to realize just how few hours there were. Nothing was more painful than hearing my kids delightedly laughing and being too sick to join them.
Doctors looked at me askance. They offered me antidepressants and pointed anecdotes about their friends who’d just had covid and were running marathons again.
I didn’t say I’d love to be able to run. I didn’t say what really made me depressed was dragging myself to appointments to be patronized. I didn’t say that post-viral illness was nothing new, nor was PEM — which for decades had been documented by people with myalgic encephalomyelitis/chronic fatigue syndrome — so if they didn’t know what I was talking about, they should stop sneering and get caught up. I was too sick for that, and too worried.
I began scouring medical journals the way I used to close-read ancient Greek poetry. I burned through horrifying amounts of money on vitamins and supplements. At night, my fears chased themselves. Would I ever get relief? Would I ever finish another book? Was long covid progressive?
It was a bad moment when I realized that any answer to that last question would come from my own body. I was in the first cohort of an unwilling experiment.
When vaccines rolled out, many people rushed back to “normal.” My world, already small, constricted further.
Friends who invited me out to eat were surprised when I declined. I couldn’t risk reinfection, I said, and suggested a masked, outdoor stroll. Sure, they said, we’ll be in touch. Zoom events dried up. Masks began disappearing. I tried to warn the people I loved. Covid is airborne. Keep wearing an N95. Vaccines protect you but don’t stop transmission.
Few wanted to listen. During the omicron wave, politicians tweeted about how quickly they’d recovered. I was glad for everyone who was fine, but a nasty implication hovered over those of us who weren’t: What’s your problem?
Friends who did struggle often seemed embarrassed by their symptoms. I’m just tired. My memory’s never been good. I gave them the resources I had, but there were few to give. There is no cure for long covid. Two of my friends went on to have strokes. A third developed diabetes, a fourth dementia. One died.
I’ve watched in horror as our public institutions have turned their back on containment. The virus is still very much with us, but the Centers for Disease Control and Prevention has stopped reporting on cases. States have shut down testing. Corporations, rather than improving ventilation in their buildings, have pushed for shield laws indemnifying them against lawsuits.
Despite the crystal-clear science on the damage covid-19 does to our bodies, medical settings have dropped mask requirements, so patients now gamble their health to receive care. Those of us who are high-risk or immunocompromised, or who just don’t want to roll the dice on death and misery, have not only been left behind — we’re being actively mocked and pathologized.
I’ve personally been ridiculed, heckled and coughed on for wearing my N95. Acquaintances who were understanding in the beginning are now irritated, even offended. One demanded: How long are you going to do this? As if trying to avoid covid was an attack on her, rather than an attempt to keep myself from sliding further into an abyss that threatens to swallow my family.
The United States has always been a terrible place to be sick and disabled. Ableism is baked into our myths of bootstrapping and self-reliance, in which health is virtue and illness is degeneracy. It is long past time for a bedrock shift, for all of us.
We desperately need access to informed care, new treatments, fast-tracked research, safe spaces and disability protections. We also need a basic grasp of the facts of long covid. How it can follow anywhere from 10 to 30 percent of infections. How infections accumulate risk. How it’s not anxiety or depression, though its punishing nature can contribute to both those things. How children can get it; a recent review puts it at 12 to 16 percent of cases. How long-haulers who are reinfected usually get worse. How as many as 23 million Americans have post-covid symptoms, with that number increasing daily.
Over three years later, I still have long covid. I still give my best hours to my children, and I still wear my N95. Thanks to relentless experimentation with treatments, I can write again, but my fatigue is worse. I recognize how fortunate I am: to have a caring partner and community, health insurance, good doctors (at last), a job I can do from home, a supportive publishing team, and wonderful readers who recommend my books. I’m grateful to all those who have accepted the new me without making me beg.
Some days, long covid feels manageable. Others, it feels like a crushing mountain on my chest. I yearn for the casual spontaneity and scope of my old life. I miss the friends and family who have moved on. I grieve those lost forever.
So how long am I going to do this? Until indoor air is safe for all, until vaccines prevent transmission, until there’s a cure for long covid. Until I’m not risking my family’s future on a grocery run. Because the truth is that however immortal we feel, we are all just one infection away from a new life.
21 notes
·
View notes
Text
#thewaronyou
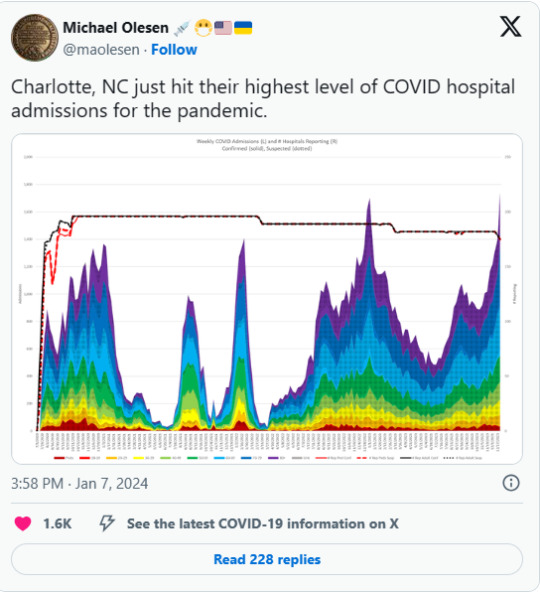
Another winter of death is now unfolding in the United States and across the Northern Hemisphere as the JN.1 variant of the coronavirus continues to surge globally. Wastewater data from the United States released Tuesday indicate that upwards of 2 million people are now being infected with COVID-19 each day, amid the second-biggest wave of mass infection since the pandemic began, eclipsed only by the initial wave of the Omicron variant during the winter of 2021-22.
There are now reports on social media of hospitals being slammed with COVID patients across the US, Canada and Europe. At a growing number of hospitals, waiting rooms are overflowing, emergency rooms and ICUs are at or near capacity, and ambulances are being turned away or forced to wait for hours to drop off their patients.
According to official figures, COVID-19 hospitalizations in Charlotte, North Carolina are now at their highest levels of the entire pandemic. In Toronto, Dr. Michael Howlett, president of the Canadian Association of Emergency Physicians, told City News, “I’ve worked in emergency departments since 1987, and it’s by far the worst it’s ever been. It’s not even close.” He added, “We’ve got people dying in waiting rooms because we don’t have a place to put them. People being resuscitated on an ambulance stretcher or a floor.”
Dr. Joseph Khabbaza, a pulmonary and critical care specialist at the Cleveland Clinic, told the Today Show website: “The current strain right now seems to be packing a meaner punch than the prior strains. Some features of the current circulating strain probably (make it) a little bit more virulent and pathogenic, making people sicker than prior (variants).”
Indeed, two recent studies indicate that JN.1 more efficiently infects cells in the lower lung, a trait that existed in pre-Omicron strains which were considered more deadly. One study from researchers in Germany and France noted that BA.2.86, the variant nicknamed “Pirola” from which JN.1 evolved, “has regained a trait characteristic of early SARS-CoV-2 lineages: robust lung cell entry. The variant might constitute an elevated health threat as compared to previous Omicron sublineages.”https://www.youtube-nocookie.com/embed/1MGIQxPf0Ig?rel=0An appeal from David North: Donate to the WSWS todayWatch the video message from WSWS International Editorial Board Chairman David North.DONATE TODAY
The toll on human life from the ongoing wave of mass infection is enormous. It is estimated that one-third of the American population, or over 100 million human beings, will contract COVID-19 during just the current wave. This will likely result in tens of thousands of deaths, many of which will not be properly logged due to the dismantling of COVID-19 testing and data reporting systems in the US. When The Economist last updated its tracker of excess deaths on November 18—before the JN.1 wave began—the cumulative death toll stood at 27.4 million, and nearly 5,000 people were continuing to die each day worldwide.
The current wave will also induce further mass suffering from Long COVID, which has been well known since 2020 to cause a multitude of lingering and often debilitating effects. Just last week, a pre-print study was published in Nature Portfolio showing that COVID-19 infection can cause brain damage akin to aging 20 years. The consequences are mental deficits that induce depression, reduced ability to handle intense emotions, lowered attention span, and impaired ability to retain information.
Other research indicates that the virus can attack the heart, the immune system, digestion and essentially every other critical bodily function. The initial symptoms of COVID-19 might resemble those of the flu, but the reality is that the virus can affect nearly every organ in the body and can do so for years after the initial infection. While vaccination slightly reduces the risks of Long COVID, the full impact of the virus will be felt for generations.
The latest winter wave of infections and hospitalizations takes place just eight months after the World Health Organization (WHO) and the Biden administration ended their COVID-19 public health emergency (PHE) declarations without any scientific justification. This initiated the wholesale scrapping of all official response to the pandemic, giving the virus free rein to infect the entire global population ad infinitum.
A virtual blackout of any mention of the coronavirus in the corporate media accompanied the swan song of official reporting. From then on, if illnesses at hospitals or among public figures were referenced at all, it was always with the euphemism “respiratory illness.” The words COVID, coronavirus and pandemic have been all but blacklisted, and the facts about the dangers of the disease have been actively suppressed.
Summarizing the cumulative results of this global assault on public health, the WSWS International Editorial Board wrote in its New Year 2024 statement:
All facts and data surrounding the present state of the pandemic are concealed from the global population, which has instead been subjected to unending lies, gaslighting and propaganda, now shrouded in a veil of silence. There is a systematic cover-up of the real gravity of the crisis, enforced by the government, the corporations, the media and the trade union bureaucracies. Official policy has devolved into simply ignoring, denying and falsifying the reality of the pandemic, no matter what the consequences, as millions are sickened and thousands die globally every day.
In response to the latest wastewater data, there have only been a handful of news articles, most of which have sought to downplay the severity of the current wave and largely ignored the deepening crisis in hospitals.
The official blackout has given rise to an extraordinary contradiction in social life. The reality of mass infection means that everyone knows a friend, neighbor, family member or coworker who is currently or was recently sick, or even hospitalized or killed, by COVID-19. Yet the unrelenting pressure to dismiss the danger of the pandemic means that shopping centers, supermarkets, workplaces and even doctor’s offices and hospitals are full of people not taking the basic and simple precaution of masking to protect themselves. Every visit outside one’s home carries the risk of being infected, with unknown long-term consequences.
As the pandemic enters its fifth year, it is critical to draw the lessons of this world historical experience. The past four years have demonstrated unequivocally that capitalist governments are both unwilling and incapable of fighting this disease. Their primary concern has always been to ensure the unabated accumulation of profits by corporations, no matter the cost in human lives and health.
The real solution to the coronavirus is not to ignore it, but to develop a campaign of elimination and eradication of the virus worldwide. To do so requires the implementation of mask mandates, mass testing and contact tracing, as well as the installation of updated ventilation systems and the safe deployment of Far-UVC technology to halt the spread of the virus. The resources for this global public health program must be expropriated from the banks and financial institutions, which are responsible for the mass suffering wrought by the pandemic.
All of these measures cut directly across the profit motive and the real disease of society: capitalism. As such, the struggle against the coronavirus is not primarily medical or scientific, but political and social. The international working class must be educated on the real dangers of the pandemic and mobilized to simultaneously stop the spread of the disease and put an end to the underlying social order that propagates mass death. This must be developed as a revolutionary struggle to establish world socialism.
7 notes
·
View notes