#Antiarrhythmic drugs
Text
Which is healthier, drinking plain water for a long time or drinking tea for a long time?

Which is healthier, drinking plain water for a long time or drinking tea for a long time?
Water is the 'source of life'. Once the human body lacks water, various parts of the body may stop functioning properly. Blood flow decreases, oxygen supply is insufficient, nerve function weakens, skin becomes fragile, metabolism slows down, and the body's operation is hindered, which can lead to abnormal organ function. Therefore, many people pay great attention to hydration, especially middle-aged and elderly people who like to carry water bottles wherever they go.
As many people's favorite drinks, plain water and tea have sparked controversy over "which is healthier?":
◎Some people think that plain water is one of the simplest and healthiest drinking water;
◎Others believe that tea can provide a variety of nutrients and is better for health~
So, who is better in the end? Today, let's explore it together~
Plain Water
"A Water Drink with No Taboos"
Plain water contains no additives such as sugar, caffeine, or colorants. Therefore, there are not many restricted groups of people who cannot drink it. Anyone, regardless of their health status, can drink it in moderation.

And maintaining adequate daily water intake is crucial for the health of the human body's skin, blood vessels, and intestines.
①Maintaining Healthy Skin: Sufficient skin moisture and fast metabolism reduce the appearance of wrinkles, spots, etc., making you look younger.
②Reducing Respiratory Diseases: The respiratory mucosa is relatively moist, and the secretion of mucus helps reduce the invasion of pathogens.
③Improving Blood Flow: Adequate water intake helps blood flow smoothly and reduces the risk of blood clots.
④Preventing Constipation: Adequate water intake prevents dry stool and constipation.
⑤Protecting the Stomach Mucosa: Boiled and cooled plain water, known as "Taihe Soup" in traditional Chinese medicine, is a "stomach tonic" that can help prevent stomach mucosal damage and reduce intestinal fermentation.
Drinking Water in Proper Amounts
For plain water, it is more important to pay attention to the amount you drink.
"The standard of drinking 8 glasses of water a day" is widely circulated, and many people insist on following it. However, this standard is not suitable for everyone.

01
Standard water intake for the general population
The "Chinese Resident Dietary Guidelines (2022)" states that adult men with low physical activity levels should drink 1700ml of water per day, and adult women should drink 1500ml of water per day.
If the weather is hot, the air is dry, or you sweat a lot, you should increase your water intake accordingly.
You can pay attention to the color, clarity, and quantity of your urine. If it is light yellow, clear, and sufficient, your water intake is adequate. Otherwise, you need to drink more water.
02
Special populations need to control water intake
①Patients with gastric ulcers undergoing medication: The medication contains substances such as sucralfate and aluminum hydroxide gel that protect the gastric mucosa. If you drink too much water, it may reduce the efficacy of the medication and hinder the recovery of the disease.
②Patients with chronic kidney disease: When kidney function is impaired, the water you drink cannot be excreted normally, so water intake needs to be controlled.
In general, the appropriate daily water intake (including water intake from drinking and food) is 500ml plus the amount of urine from the previous day.
③Patients with uremia: At this time, the amount of water intake needs to be based on changes in body weight.
You can weigh your weight at a fixed time every day (preferably after urination and before breakfast), and the daily weight gain should not exceed 0.5% of your body weight. In addition, the weight gain between two dialysis sessions should be less than 3% to ensure the effectiveness of dialysis.
④Patients with heart failure: Drinking a large amount of water will increase the cardiac output and increase the heart's workload, worsening the condition. For patients with severe heart failure, the water intake may need to be controlled to less than 800ml, based on medical advice.

Tea
"Regulator" of the Body
Tea contains various medicinal ingredients such as tea polyphenols, tea polysaccharides, and alkaloids. Among the 86 essential elements required by the human body, tea contains 28 of them. Therefore, drinking tea frequently can serve as a "regulator" of the body, helping to reduce some disease risks.
①Reducing the incidence of cardiovascular diseases
A study published in the European Journal of Preventive Cardiology included 100,902 subjects aged 18 years or older and followed them for 17 years. The study found that people who drank tea at least three times a week had a 20% lower incidence of cardiovascular diseases and a 22% lower mortality rate than those who drank tea less than three times a week. The overall risk of death was reduced by about 15%.
②Assisting in lowering blood pressure
The American College of Cardiology summarized 21 effective studies involving a total of 1,323 subjects. The study found that compared with non-tea drinkers, tea drinkers had an average reduction of 1.8 mmHg in systolic blood pressure and 1.4 mmHg in diastolic blood pressure, and the blood pressure-lowering effect was more pronounced for those who drank tea for more than 12 weeks.
③Helping with weight loss and lipid-lowering
The Tea Research Institute of Zhejiang University found that the complex catechin, epigallocatechin gallate (EGCG), in tea can consume excess energy by increasing the production of brown fat, thereby assisting in weight loss. At the same time, it can also inhibit microglia cells, reduce hypothalamic inflammation, improve body weight, and regulate the normal function of the central nervous system.
Drinking Tea, Paying Attention to the "Four Nos"
Not everyone can drink tea, and not every time is suitable for drinking tea:

01
People who are not suitable for drinking tea
Patients with neurasthenia, insomnia, hyperthyroidism, tuberculosis, heart disease, gastric disease, and intestinal ulcers are not suitable for drinking tea, especially strong tea. Nursing or pregnant women and infants and young children are also not suitable for drinking tea.
02
Do not drink tea in the morning or before bed, and do not drink before or after meals
Drinking tea on an empty stomach in the morning will dilute gastric acid and reduce digestive function. Tea has an exciting and diuretic effect, which can affect sleep quality if consumed before bed. It is recommended to drink tea around 10 am.
The caffeine in tea can inhibit gastric acid secretion, and drinking tea before a meal is not conducive to digestion and absorption. Drinking tea immediately after a meal can affect the body's absorption of protein and iron due to the tannic acid in tea. It is therefore recommended to drink tea one hour after a meal.
03
Do not drink tea while taking certain medications
People who need to take sedatives, sleeping pills, or antiarrhythmic drugs should not drink tea because the caffeine and other components in tea can reduce the medication's effectiveness, which may be disadvantageous for controlling the condition.
04
Do not drink too strong tea
Strong tea contains high levels of fluoride. Frequent consumption of strong tea can damage the kidneys, increase gastrointestinal burden, and easily cause "tea-fluoride poisoning."
Therefore, a daily intake of about 12 grams of tea for healthy adults, with each serving of 3 grams brewed with 150 ml of water, is appropriate.
In summary, drinking tea and drinking plain water are equally good. The most important thing is to consume an appropriate and moderate amount.
Remember these four points to hydrate correctly and stay healthy
Whether you are drinking tea or plain water, you need to pay attention to these four points:

01
Drink proactively
Do not wait until you are thirsty to drink water because thirst is a clear sign of dehydration. As the body loses more water, the urine color deepens, the skin becomes dry, the mouth becomes dry and cracked, the voice becomes hoarse, and the body becomes weak.
It is best to replenish water every half an hour.
02
Sip slowly
Even if you are thirsty, do not drink water in large gulps. Drinking too much water in one go can cause the water to enter the bloodstream quickly. After absorption in the gut, the blood will become diluted, increasing the circulation volume suddenly, which can easily increase myocardial oxygen consumption and aggravate the heart's workload.
The correct method is to sip slowly, especially for people with cardiovascular problems, who should drink in small amounts and frequently.
03
Avoid water that is too hot
Water that is too hot (above 65℃) can scald the esophageal mucosa. If this happens repeatedly, it can cause inflammation or even cancer.
04
Choose the right variety
There are many types of tea, and you need to learn to choose the right one according to the season:
①In spring, when the yang energy is vigorous and can lead to liver yang hyperactivity, it is suitable to drink green tea to regulate the liver and relieve depression.
②In summer, when the weather is hot and the incidence of cardiovascular events is high, it is suitable to drink fully fermented black tea.
③In autumn, when the weather is dry and fluid consumption is high, it is suitable to drink white tea to clear heat and moisten the lungs.
④In winter, when the weather is cold and the kidneys need to store essence for winter, black tea is suitable because it enters the kidneys.
#tea#green tea#chinese tea#Morning#Bedtime#Meals#Sedatives#Antiarrhythmic drugs#Caffeine#Fluoride#Kidneys#Hydration#Thirst#Dehydration#Water temperature#Choosing tea#White tea
1 note
·
View note
Note
for the fic writing asks: 1, 2, and 19 please (and please talk about your OCs bc I love them and they are ever so precious to me and yes I acknowledge I still owe you at least one Banuk name)
Made it home from work with a little time to spare so an answer it is!! (Please excuse the wonky mobile phone formatting, I'm too tired to boot up the PC now.)
1 Do you daydream a lot before you write, or go for it as soon as ideas strike?
I've got multiple notebooks which are fed with ideas before I put down the first word. Usually the process is this: Spotify recommends some music to me, or I accidentally let an album play that I hadn't heard in its entirety before, and a song jumps out at me and just plants a few vague pictures, sometimes a line or two in my head. I write them down, then expand on them over time, and only write the first word when the notebook (usually) contains a rough structure, the first and last sentences as well as a title. So yeah. In the beginning, there was music, and a bunch of question marks on a piece of paper.
2 Where do you get your fic ideas?
I listen to the wrong song at an unfortunate time and end up being cursed with a picture or feeling that wants to be put into words.
19 Do you enjoy creating OCs or do you prefer to stick solely to canon characters?
Well.... technically I hate creating OCs because NAMES and STORIES but they tend to create themselves. The canon characters move through a populated world, and since I quickly feel overwhelmed (but also restricted) when juggling too many canon characters I end up filling the spaces with OCs. Transposition's Utaru OCs just spawned themselves because I liked the idea of Ikrie having social contacts outside of Aloy and her friends; and I guess the same goes for all the (relatively) newly created Banuk that are still slumbering in the notes for a future project. (The Ikrie-Mailen friendship exploration with which I like to entertain myself has so far yielded the highest number of OCs: we've got Siktuk, the shaman of Ikrie and Mailen's old werak, who kind of took little Ikrie under his wing but never quite managed to put her on the shaman's path; Urmak, who's only designation so far is "bully"; Naunai, a White Teeth aspirant who is there to talk shit about Mailen and fight Ikrie; Yakili, also known as "The Owl", a legendary huntress who is said to have had a deep connection to the Blue Light; and Arkai, a young painter Ikrie has a crush on. I'm probably forgetting someone but they likely won't have a name yet. Lou, I'm already dreading the Suffering™.)
OCs also provide an opportunity to explore new perspectives (Bare His Heart's POV character, Rabbit, merely exists because I wanted to write about my Inquisitor from an outside view, and everything else continued from there), as well as expand on headcanons I have piled up about the world and in Horizon's case, the tribes themselves. Which I enjoy a lot! ....so I guess I do like creating OCs. Just not naming them. (Although Rabbit's proper name, Daron Amiot, is born from an ongoing joke I had with a friend during our studies--"hey, this drug sounds like a fantasy name!"--in this case, Amiodaron.)
#it's an antiarrhythmic if you're wondering#one of my inquisitors is also named anasarka#and another anura#not that those are drugs but pathology and zoology provide as well#thank you SO MUCH for the ask!!!#writing#asks
9 notes
·
View notes
Text
#Critical Care Antiarrhythmic Drugs Market#Critical Care Antiarrhythmic Drugs Market share#Critical Care Antiarrhythmic Drugs Market size
0 notes
Text
nine people i'd like to get to know better
tagged by @ravensfreckles thanks love 🥰
last song: all for you by janet jackson
favorite color: green
currently watching: #blackaf lol this show came out in the pandemic and i just never watched it but i wanted to watch something with rashida jones in it after binging parks and rec clips on youtube
last movie/show: a cowgirl's song. idk i was looking for something hallmarkesque and it fit the bill for the moment
spicy/savory/sweet: SPICE me up Scotty 🌶️
current obsession: i binged the chestnut springs series this weekend and YEEFUCKINGHAW 🤠
last thing you googled: "antiarrhythmic drugs mnemonic" baby girl's in med school and needs to know her cardio drugs
tagging: @hausofmamadas @darqchilddaydreamz @withmyteeth @etherealnoir @sharpayandryan @bradshawsbaby @when-did-this-become-difficult @drabbles-mc @dahnrana
55 notes
·
View notes
Text
like why are they even called antiarrhythmic drugs if almost all of them cause proarrhythmic side effects😭
9 notes
·
View notes
Text
Understanding Heart Rhythm Disorders and Their Impact on Cardiovascular Health
Introduction:
Heart rhythm disorders, or arrhythmias, can significantly impact cardiovascular health. These disorders disrupt the heart's normal electrical activity, causing irregular heart rhythms that can affect its ability to pump blood effectively. Understanding the different types of arrhythmias and their implications is crucial for recognizing symptoms, identifying risk factors, and exploring appropriate treatment options.
Common Types of Arrhythmias
Atrial Fibrillation (AF):
Atrial fibrillation is a common arrhythmia characterized by irregular and rapid electrical signals in the heart's upper chambers (atria). This leads to an irregular heart rate. AF increases the risk of blood clots, which can travel to other body parts, causing stroke or other complications.
Bradycardia:
Bradycardia is a slow heart rate, typically below 60 beats per minute. It occurs when the heart's electrical signals are delayed or blocked, decreasing heart rate. Bradycardia can be caused by medications, underlying heart conditions, or heart electrical system issues. Symptoms may include fatigue, Dizziness, fainting, or Shortness of breath.
Tachycardia:
Tachycardia is characterized by a fast heart rate, usually above 100 beats per minute. It occurs when the heart's electrical signals fire abnormally or accelerated. Stress, anxiety, certain medications, or structural abnormalities in the heart can trigger tachycardia. Symptoms may include palpitations, Dizziness, chest pain, or loss of consciousness.
Symptoms, Risk Factors, and Potential Complications
Symptoms of Heart Rhythm Disorders:
Palpitations: Sensation of rapid, fluttering, or irregular heartbeats.
Fatigue: Persistent tiredness or exhaustion, even with minimal physical activity.
Dizziness or lightheadedness: Feeling faint or unsteady.
Shortness of breath: Breathlessness or difficulty breathing, particularly during exertion.
Chest discomfort: Discomfort, pressure, or pain in the chest.
Fainting or near-fainting episodes: Temporary loss of consciousness due to inadequate blood flow to the brain.
Risk Factors:
Age: The risk of arrhythmias generally increases with age.
Family history: Having a close relative with a history of arrhythmias may raise the risk.
High blood pressure: Uncontrolled hypertension can strain the heart and disrupt electrical signals.
Existing heart conditions: Conditions such as coronary artery disease, heart failure, or structural abnormalities can contribute to arrhythmias.
Thyroid disorders: An overactive or underactive thyroid can disrupt the heart's electrical system.
Lifestyle factors: Excessive alcohol or caffeine intake, smoking, drug abuse, and obesity can all play a role in developing arrhythmias.
Potential Complications:
Stroke: Certain arrhythmias, particularly atrial fibrillation, can increase the risk of blood clots forming in the heart, which can travel to the brain and cause a stroke.
Heart failure: Chronic arrhythmias can weaken the heart muscle over time, leading to heart failure, where the heart cannot pump blood effectively.
Sudden cardiac arrest: In some cases, arrhythmias can trigger a sudden loss of heart function, leading to cardiac arrest, a life-threatening emergency requiring immediate medical intervention.
Treatment Options
Treatment for heart rhythm disorders aims to restore or maintain a normal heart rhythm, alleviate symptoms, and reduce the risk of complications. The following treatment options are commonly used:
Medications: Antiarrhythmic drugs may be prescribed to regulate heart rhythm and reduce the frequency or severity of arrhythmias.
Lifestyle modifications: Making lifestyle changes, such as managing stress, maintaining a healthy weight, quitting smoking, limiting alcohol and caffeine consumption, and engaging in regular physical activity, can help manage certain arrhythmias.
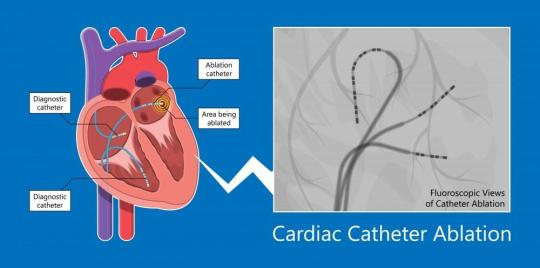
Ablation: Catheter ablation is a procedure that involves selectively destroying or isolating abnormal heart tissue responsible for generating arrhythmias. It aims to restore a normal heart rhythm.
Implantable devices: In some cases, implantable devices like pacemakers or cardioverter-defibrillators (ICDs) may be recommended to regulate the heart's electrical signals and deliver appropriate therapy when needed.
Conclusion
Heart rhythm disorders can significantly impact cardiovascular health, affecting the heart's ability to function properly. Recognizing the symptoms, understanding the risk factors, and seeking appropriate treatment is vital for managing arrhythmias and reducing the risk of complications. By working closely with healthcare professionals, individuals with heart rhythm disorders can develop a tailored treatment plan that addresses their specific needs, improves their quality of life, and promotes overall cardiovascular health.
#Cardiac arrhythmia#heart rhythm disorder#cardiac rhythm disturbance#irregular heartbeat#atrial fibrillation
6 notes
·
View notes
Text
This is for sustained VTach:
Sustained monomorphic ventricular tachycardia (SMVT) is defined as a regular, wide (≥120 milliseconds) QRS complex tachycardia with uniform and stable QRS morphology at a rate of more than 100 beats per minute that lasts for 30 seconds or longer or causes hemodynamic collapse within 30 seconds.
●All patients with SMVT should have a brief immediate assessment of the symptoms, vital signs, and level of consciousness to determine if they are hemodynamically stable or unstable. Differentiation between a hemodynamically unstable versus stable patient depends upon hemodynamic compromise, such as hypotension, altered mental status, chest pain, or heart failure (HF).
●Patients with SMVT who are hemodynamically unstable and pulseless, or who become pulseless during the course of evaluation and treatment, should be managed according to standard advance cardiac life support (ACLS) resuscitation algorithms, with immediate high-energy countershock and cardiopulmonary resuscitation (CPR). Patients should initially be treated with a synchronized 120 to 200 joule shock from a biphasic defibrillator or a 360 joule shock from a monophasic defibrillator.
●For patients with wide complex tachycardia (WCT) who are hemodynamically unstable, but still responsive with a discernible blood pressure and pulse, we recommend urgent cardioversion (following administration of sedation) (Grade 1B).
●For patients with SMVT who are hemodynamically stable on presentation, after recording a 12-lead ECG we generally prefer to begin with an intravenous antiarrhythmic agent and reserve electrical cardioversion for refractory patients or for those who become unstable.
•If pharmacologic cardioversion is the chosen approach, we administer intravenous amiodarone, procainamide, or lidocaine.
•If electrical cardioversion with appropriate procedural sedation is the chosen approach, intravenous analgesics or sedatives should be cautiously administered if the blood pressure will tolerate their use. If the QRS complex and T wave can be distinguished, an attempt at synchronized cardioversion can be performed with a synchronized shock of 100 joules using either a biphasic or monophasic defibrillator.
●Treatment of underlying conditions associated with VT, such as myocardial ischemia, electrolyte disturbances, drug proarrhythmia, and HF, as well as decreasing the sympathetic facilitation of SMVT, are important components of the acute management of VT.
●Chronic therapy of patients with SMVT usually requires utilization of multiple therapeutic modalities, including the implantable cardioverter-defibrillator (ICD), antiarrhythmic drugs, radiofrequency catheter ablation, and/or arrhythmia surgery.
•In the absence of a clearly identifiable and reversible cause for SMVT, nearly all patients with a history of SMVT will be candidates for ICD insertion for secondary prevention of sudden cardiac death, unless the patient refuses or the risks of ICD insertion are felt to outweigh the potential benefits. (See 'ICD therapy' above.) •Nearly all patients who experience SMVT have an indication for therapy with a beta blocker, including patients with a prior myocardial infarction, patients with HF and reduced LV systolic function, etc. Beta blockers provide some level of protection against recurrent SMVT, primarily by reducing myocardial oxygen demand and blocking sympathetic input to the heart. (See 'Beta blockers' above.) •Antiarrhythmic drugs may also be used to improve quality of life in patients with frequent SMVT leading to ICD shocks, or in those patients who are not candidates for, or who decline, ICD implantation. Amiodarone has generally been the most effective antiarrhythmic drug for preventing ventricular arrhythmias (and associated ICD shocks). (See 'Antiarrhythmic drugs' above.) •For patients with recurrent SMVT resulting in ICD shocks despite treatment with an antiarrhythmic drug, we suggest radiofrequency ablation (RFA) rather than the addition of a second antiarrhythmic agent (Grade 2C). RFA is also an alternative to antiarrhythmic drugs as the initial therapy for SMVT. In addition, RFA, with or without antiarrhythmic drug therapy, is an option for patients with SMVT who are not candidates for or who refuse ICD implantation. (See 'Radiofrequency catheter ablation' above.)
4 notes
·
View notes
Text
List of Common Drug Side Effects
1. Allergic Reactions
• Potentially could occur with any medication.
• Symptoms range from a mild rash to a severe anaphylactic reaction (including facial and throat swelling, difficulty breathing and a widespread rash).
2. Prevention and management strategies:
• Take an antihistamine and see a doctor straight away if you think you are having an allergic reaction to a medicine. Seek emergency help if the reaction is severe
• If the allergic reaction is confirmed as occurring due to that drug, avoid it and other related drugs in the future
• Wear a medical alert tag to alert others to the medicine you are allergic too.
2. Blurred Vision
• May occur with antihistamines, antipsychotics, bupivacaine, bupropion, duloxetine, esomeprazole, etodolac, gabapentin, opioids, and several other drugs.
Prevention and management strategies:
• Talk to your doctor about switching medications
• Lubricant eye drops may help
• Avoid driving with impaired vision.
3. Bruising and Bleeding
Common with medicines that “thin the blood” such as aspirin, clopidogrel, enoxaparin, and warfarin. Also, common with NSAIDs, steroids (such as prednisone) and medicines to treat cancer.
Prevention and management strategies:
• Try to avoid bumping yourself into furniture.
Remove any trip hazards, such as loose rugs
• Cuts may take longer to stop bleeding. Hold a gauze over the affected area and apply pressure
• Seek emergency help if you have a wound that bleeds profusely or doesn’t stop bleeding within 15 minutes.
4. Constipation
Common with opioids, diuretics, calcium antagonists, antidepressants, aluminum-containing antacids, ondansetron, and iron supplements.
Prevention and management strategies:
1. Increase water intake and fiber content of your diet (if appropriate)
2. Exercise, if possible
3. If mild, talk to your doctor about taking laxatives such as docusate, sennosides, or psyllium
4. If severe and caused by opioids, talk to your doctor about methylnaltrexone or naloxegol.
5. Cough
Common with ACE inhibitors (these can cause a dry, hacking, chronic cough in up to 20 percent of patients)
Prevention and management strategies:
1. Talk to your doctor about switching medications
2. Usually resolves one-to-two weeks after discontinuation.
6. Dehydration
Common with antihistamines, blood pressure medications, chemotherapy, and laxatives.
Prevention and management strategies:
1. Drink fluids. Cooled or iced fluids may go down easier
2. Eat moist foods such as fruits, vegetables, and soups
3. Regularly moisturize skin and apply lip balm
4. Apply balm to the lips to avoid painful cracking.
7.Diarrhea
May occur with some antibiotics, antidepressants, magnesium-containing antacids, proton pump inhibitors (eg, lansoprazole, omeprazole) and chemotherapy agents.
Prevention and management strategies:
1. If due to antibiotic use, talk to your doctor about taking probiotics
2. Talk to your doctor about antidiarrheal medication
3. Ask doctor about reducing the dosage of your drug or other suitable treatments
4. Keep up your fluid and electrolyte intake to avoid dehydration
5. If extremely persistent or severe, always tell your doctor.
8. Drowsiness or Sedation
Medications that cause drowsiness include benzodiazepines (such as lorazepam, diazepam), some antidepressants, antiemetics, older antihistamines (such as diphenhydramine, chlorpheniramine), some heart medications, muscle relaxants and narcotics.
Prevention and management strategies:
1. If your medication is making you drowsy during the day, talk to your doctor about reducing the dosage of your drug or other suitable treatments
2. Do not drive, operate machinery, or perform other hazardous tasks if affected
3. Avoid alcohol.
9. Dry mouth (Xerostomia)
May occur with antiarrhythmics, anticholinergics, antihistamines, drugs for high cholesterol, anti-inflammatory agents, diuretics, vasodilators, drugs for Parkinson’s Disease, and antipsychotics.
Prevention and management strategies:
1. Ask doctor about reducing drug dosage or other suitable treatments
2. Go for regular dental check-ups and ask dentist about application of sealants to teeth fissures
3. Eat low-sugar, low-acid foods
4. Avoid alcohol-containing mouthwashes
5. Chew xylitol chewing gum
6. Drug-treatments are available for people with Sjogren’s syndrome or a history of radiation therapy.
10. Erectile Dysfunction or Decreased Sexual Desire
More common with antidepressants, antihistamines, benzodiazepines, beta blockers, diuretics, and H2 blockers.
Prevention and management strategies:
1. Talk to your doctor about the possibility of switching to a different medication
2. Limit use of alcohol, smoking or recreational drugs such as marijuana which can also affect sexual function
3. Talk to your doctor about medications and other treatments for sexual dysfunction, such as prescription medications (for example PDE5 inhibitors), vacuum pumps, implants, surgery, and natural options.
11. Esophageal Damage
May occur with a wide-range of drugs including aspirin, bisphosphonates (such as alendronate), doxycycline, potassium chloride, quinidine, and vitamin C.
▪️Prevention and management strategies:
1. Take all medicines while upright and swallow with a glass of water
2. Avoid lying down soon after taking a medicine
3. For some medicines, recommended advice includes remaining upright for 30 minutes after taking
4. Avoid irritating foods such as citrus and alcohol
5. Talk to your doctor about the possibility of switching to a different medication.
12. Indigestion or Gastroesophageal Reflux Disease (GERD)
May occur with drugs that irritate the stomach lining (such as aspirin, iron, NSAIDs, steroids), those that relax the lower esophageal sphincter (LES) (such as anticholinergics, calcium channel blockers, and nitrates) or reduce LES pressure (such as progesterone, theophylline, and tricyclic antidepressants).
Prevention and management strategies:
1. Talk to your doctor about reducing the dosage of, or switching to another drug
2. Elevate the head of the bed
3. Avoid foods that also irritate the stomach or affect the LES such as alcohol, carbonated beverages, citrus, coffee, fatty foods, or tomatoes
4. Quit smoking if you smoke, lose weight if you are overweight, avoid tight waistbands
5. Talk to your doctor about GERD medications such as antacids, H2 blockers and proton pump inhibitors.
13. Falling or Unsteadiness on Feet
Medicines that cause confusion, fatigue or sedation such as antipsychotics, some antidepressants, benzodiazepines, sedating antihistamines, antiepileptics, narcotics, and some heart medications.
Prevention and management strategies:
1. If sedation is the problem, talk with your doctor about changing the dose or trying an alternative medication
2. Remove rugs from the floor and throw rugs from furniture
3. Ask for help when getting up or walking
4. If you fall, tell your doctor and get checked for injuries
5. A home health nurse may be able to suggest ways to make your home safer
6. If you have a walker or wheelchair, use it every time you get up.
14. Gingival Enlargement (Growth of the gums around the teeth)
May occur with cyclosporine, calcium channel blockers (eg, nifedipine), and phenytoin.
Prevention and management strategies:
1. Requires dosage reduction or drug discontinuation
2. Surgical removal of gingival tissue is only temporarily effective if the drug can’t be discontinued.
15. Gout
May occur with aspirin (low dose), chemotherapy agents, cyclosporine, frusemide, and thiazide diuretics.
Prevention and management strategies:
1. Talk to your doctor about reducing the dosage of, or switching to another drug
2. Your doctor may prescribe NSAIDs or other drugs to relieve the pain from gout
3. Avoid alcohol and purine-rich foods (cheeses, red meats) during the gout flare-up.
16. Headache
1. Common with asthma medications, angina and blood pressure medications, oral contraceptives, erectile dysfunction treatments, and stimulants
2. Rebound headaches can be caused by overuse of acetaminophen, aspirin, NSAIDs, and opioids.
Prevention and management strategies:
1. Talk to your doctor about alternative medications or a dosage reduction if the headaches are very debilitating
2. Some may respond to acetaminophen – but check with your doctor first
3. Rest in a quiet, dimly lit room
4. Heat, massage therapy, acupressure, or reflexology may help if the headaches recur
5. Keep well hydrated (drink plenty of water).
17. Infection
Corticosteroids, immunosuppressants, chemotherapy and several other medicines suppress your immune system and increase your risk of developing an infection.
Prevention and management strategies:
1. Wash your hands before eating, after contact with other people or animals, and after toileting
2. Stay away from people who are sick if your infection risk is increased (either by the medicines you are taking or the condition you have)
3. Keep up to date with your vaccinations (includes a yearly flu shot)
4. See your doctor as soon as you can if you develop symptoms of an illness and your immune system is compromised.
18. Hair Loss
1. May affect all body hair or just scalp hair
2. Common with chemotherapy or radiation therapy
3. May also occur with certain acne treatments, antibiotics, antidepressants, oral contraceptives, and cholesterol-lowering medicines.
Prevention and management strategies:
1. Be gentle when brushing or combing your hair.
2. Avoid over-styling your hair. Wear a hair net to bed
3. Consider purchasing a wig while you still have hair to allow better matching with your original hair color. Wigs may be partly covered by insurance when called a “cranial prosthesis”
4. If due to chemotherapy or radiation therapy, ask your doctor about cooling caps.
19. Muscle Pain or Muscle Weakness
Common with statins (used to reduce cholesterol levels). May be due to an effect on muscle proteins or a decrease in coenzyme Q10 (CoQ10).
Prevention and management strategies:
1. Tell your doctor straight away because sometimes the muscle pain may indicate more severe damage. A lower dosage or a different medication may be needed
2. Avoid exercising too much
3. Do not take over-the-counter pain relievers such as acetaminophen or NSAIDs
4. Consider CoQ10 supplements; however, study results have been conflicting.
20. Nausea and Vomiting
1. Common with chemotherapy or radiation therapy
2. May also occur with drugs that tend to slow or block the bowel, when electrolytes are imbalanced or with infections.
Prevention and management strategies:
1. Antinausea medications (also called antiemetics) such as ondansetron, aprepitant, dexamethasone, and dronabinol can prevent vomiting and help control nausea. You may have to try several before finding one that works for you
2. Self-hypnosis, muscle relaxation, biofeedback, guided imagery and other “mindfulness” techniques may help
3. Acupuncture may help with anticipatory nausea
4. Eat small, frequent meals rather than large meals three times a day
5. Drink clear liquids cold and sip slowly. Try Popsicles or gelatine
6. Eat bland foods, such as dry toast and crackers and avoid fatty, fried, spicy, strong-smelling or very sweet foods
7. Try chewing ginger.
21. Taste Disturbances
Common with many drugs including antibiotics (such as ciprofloxacin, metronidazole), anticonvulsants, antidepressants, aspirin, blood pressure medications, lithium, metformin, and muscle relaxants.
Prevention and management strategies:
1. Usually reversible with drug discontinuation (although may take several months)
2. Prepare foods with a variety of colors and textures
3. Use herbs and spices (but avoid adding extra sugar or salt).
22. Tendonitis (tendinitis) or Tendon Rupture
1. Most commonly reported with fluoroquinolone antibiotics (eg, ciprofloxacin norfloxacin, ofloxacin, levofloxacin)
2. More common in people over the age of 60, taking corticosteroids, or with a history of organ transplant.
Prevention and management strategies:
1. Tell your doctor BEFORE you start taking the fluoroquinolone if you have had a tendon problem in the past
2. Avoid strenuous activity while taking the fluoroquinolone
3. Discontinue the antibiotic immediately if you experience pain or swelling in a tendon and seek medical advice
4. Avoid all fluoroquinolones in the future if you develop a tendon problem while taking a fluoroquinolone.
23. Weight Gain
Common with antipsychotics, most antidiabetic drugs (except for metformin), antidepressants and antiepileptics.
Prevention and management strategies:
1. Talk to your doctor about the possibility of switching to a different medication
2. Eat a healthy diet and limit your portion sizes
3. Eat more slowly at meals
4. Drink water throughout the day
5. Exercise regularly.
2 notes
·
View notes
Text
General Drug Categories
General Drug Categories
Analgesics
Antacids
Antianxiety Drugs
Antiarrhythmics
Antibacterials
Antibiotics
Anticoagulants and Thrombolytics
Anticonvulsants
Antidepressants
Antidiarrheals
Antiemetics
Antifungals
Antihistamines
Read More...
#forensicfield
(more…)

View On WordPress
#analgesics#Forensic Medicine#General Drug Categories#what are antacids#what are antianxiety drugs#what are antibacterials#what are antibiotics#what are barbiturates
2 notes
·
View notes
Text
Navigating Multifocal Atrial Tachycardia: Effective Treatment Approaches

Unraveling the complexities of Multifocal Atrial Tachycardia (MAT) is essential for effective treatment and long-term prognosis. In this SEO-friendly blog, we delve into the diagnostic journey of MAT, factors influencing prognosis, and emerging trends shaping the landscape of care.
Diagnosis Unveiled: MAT diagnosis commences with a comprehensive evaluation, blending patient history, physical examination, and advanced diagnostics. Electrocardiogram (ECG) serves as the cornerstone, capturing the irregular heart rhythms indicative of MAT. Further validation through Holter monitoring and imaging modalities ensures accuracy in diagnosis.
Navigating Diagnostic Hurdles: Challenges in MAT diagnosis stem from its resemblance to other arrhythmias, demanding astute clinical judgment and meticulous ECG interpretation. Concurrent cardiac or pulmonary conditions often obscure the diagnostic landscape, necessitating a holistic approach for differential diagnosis.
Advancements in Imaging: Harnessing cutting-edge imaging techniques such as echocardiography and cardiac MRI enhances diagnostic precision, unraveling intricate cardiac structures and functional anomalies associated with MAT. These non-invasive modalities offer invaluable insights, guiding tailored therapeutic interventions.
Prognostic Indicators: MAT prognosis hinges on multifaceted factors, including comorbidities, age, and treatment response. Effective management of MAT, coupled with holistic care addressing underlying conditions, typically yields favorable outcomes. However, uncontrolled MAT poses risks of complications like heart failure or stroke, underscoring the importance of vigilant monitoring and intervention.
Holistic Management Approach: Holistic MAT management integrates pharmacotherapy, lifestyle modifications, and procedural interventions. Beta-blockers and calcium channel blockers stand as frontline agents for rate control, while antiarrhythmic drugs may be considered for rhythm management. Lifestyle adjustments, encompassing dietary modifications and stress reduction, complement medical therapy, fostering comprehensive wellness.
Pioneering Therapeutic Frontiers: Exploring novel therapeutic avenues unveils promising prospects in MAT care. Catheter ablation emerges as a transformative intervention, ablating aberrant cardiac foci and restoring rhythm stability. Additionally, ongoing research ventures into gene therapy and precision medicine herald a paradigm shift in MAT treatment paradigms.
Conclusion: The journey of MAT diagnosis and management epitomizes the synergy between clinical acumen, technological innovation, and patient-centric care. By unraveling diagnostic intricacies, understanding prognostic determinants, and embracing therapeutic innovations, healthcare stakeholders empower individuals with MAT to navigate their cardiac journey with resilience and hope.
0 notes
Text
Understanding Arrhythmias: Types, Causes, and Symptoms
Arrhythmias are irregular heart rhythms that can range from harmless to life-threatening. Understanding the different types, causes, and symptoms of arrhythmias is essential for early detection and appropriate management. Here's a comprehensive overview:
Types of Arrhythmias:
Atrial Fibrillation (AFib): AFib is the most common type of arrhythmia, characterized by rapid and irregular beating of the heart's upper chambers (atria).
Bradycardia: Bradycardia occurs when the heart beats too slowly, typically less than 60 beats per minute.
Tachycardia: Tachycardia is a fast heart rate, usually exceeding 100 beats per minute.
Premature Contractions: Premature contractions are extra, abnormal heartbeats that occur before the next regular heartbeat.
Ventricular Fibrillation (VFib): VFib is a life-threatening arrhythmia characterized by rapid, chaotic beating of the heart's lower chambers (ventricles).
Causes of Arrhythmias:
Heart Conditions: Structural heart defects, coronary artery disease, heart failure, and cardiomyopathy can increase the risk of arrhythmias.
Electrolyte Imbalance: Abnormal levels of potassium, magnesium, or calcium in the blood can disrupt the heart's electrical activity.
Medications: Certain medications, such as beta-blockers, calcium channel blockers, and antiarrhythmic drugs, can trigger arrhythmias.
Stress and Anxiety: Emotional stress and anxiety can affect the heart's rhythm, leading to arrhythmias.
Stimulants: Excessive caffeine, nicotine, or illicit drugs can stimulate the heart and cause arrhythmias.
Other Factors: Age, genetics, sleep apnea, and excessive alcohol consumption can also contribute to the development of arrhythmias.
Symptoms of Arrhythmias:
Palpitations: Sensations of rapid, fluttering, or pounding heartbeat.
Dizziness or Lightheadedness: Feeling faint or dizzy, especially with exertion.
Shortness of Breath: Difficulty breathing, even at rest or during normal activities.
Chest Pain or Discomfort: Pressure, squeezing, or discomfort in the chest.
Fatigue: Unexplained tiredness or weakness.
Fainting or Near-Fainting Episodes: Temporary loss of consciousness or feeling lightheaded.
Arrhythmias can significantly impact quality of life and may require medical intervention depending on the type and severity. Recognizing the different types, understanding the underlying causes, and being aware of the symptoms is essential for early detection and appropriate management of arrhythmias. If you experience symptoms suggestive of an arrhythmia or have concerns about your heart health, consult with a cardiac surgeon near Lokmat Square Nagpur for evaluation and appropriate treatment. Early diagnosis and intervention can help prevent complications and improve outcomes for individuals with arrhythmias.
0 notes
Text
What is meant by Monomorphic Ventricular Tachycardia ?

Monomorphic ventricular tachycardia (VT) is a distinct type of abnormal heart rhythm characterized by a regular and rapid heartbeat originating in the ventricles, the heart's lower chambers. What sets monomorphic VT apart is the uniformity in the morphology of QRS complexes on an electrocardiogram (ECG), reflecting a consistent pathway for electrical signals during the arrhythmia. This condition is often associated with underlying heart issues such as coronary artery disease, previous heart attacks, cardiomyopathy, or scar tissue formation within the ventricles.
The treatment approach for monomorphic VT depends on factors like the underlying cause and the severity of the condition. Options may include the use of medications, antiarrhythmic drugs, catheter ablation procedures to disrupt abnormal electrical pathways, or the placement of an implantable cardioverter-defibrillator (ICD) to provide protection against potentially life-threatening arrhythmias. It is imperative for individuals experiencing symptoms or those diagnosed with monomorphic VT to seek immediate medical attention for a comprehensive evaluation and tailored management plan, as early intervention can be crucial in optimizing outcomes and ensuring cardiac health.
0 notes
Text
Cardiovascular Market: A Comprehensive Overview of Devices, Drugs, and Services: Ken Research
The cardiovascular system is a vital component of human health, encompassing the heart, blood vessels, and associated structures. The Cardiovascular Market, therefore, plays a crucial role in the healthcare industry, offering a range of devices, drugs, and services designed to diagnose, treat, and manage cardiovascular diseases. From innovative diagnostic devices to groundbreaking drugs and cardiac safety services, let's explore the multifaceted landscape of the Cardiovascular Market.
Cardiovascular Devices Market: Advancements in Medical Technology
The Cardiovascular Devices Market is a cornerstone of cardiovascular care, encompassing a wide array of devices designed to diagnose and treat various cardiac conditions. These devices range from diagnostic tools such as ECG machines and cardiac monitors to therapeutic devices like pacemakers, stents, and artificial heart valves. As technological advancements continue to drive innovation in the Cardiovascular Devices Market, the industry is witnessing the development of more precise, efficient, and patient-friendly devices, revolutionizing the way cardiovascular diseases are managed and treated.
Cardiovascular Drugs Market: Targeted Therapies for Heart Health
The Cardiovascular Drugs Market focuses on pharmaceutical interventions for managing cardiovascular diseases. From antihypertensive medications and cholesterol-lowering drugs to anticoagulants and antiarrhythmics, the Cardiovascular Drugs Market offers a diverse range of therapeutic options. These drugs play a pivotal role in managing risk factors, preventing complications, and improving outcomes for patients with cardiovascular diseases. As research continues to uncover new insights into the mechanisms of cardiovascular diseases, the Cardiovascular Drugs Market is poised for further growth and innovation, offering targeted therapies tailored to individual patient needs.
Cardiac Safety Services Market: Ensuring Drug Safety in Cardiovascular Care
The Cardiac Safety Services Market plays a critical role in ensuring the safety and efficacy of cardiovascular drugs and therapies. These services encompass a range of diagnostic tests, monitoring services, and regulatory compliance solutions designed to assess and mitigate the cardiac risks associated with pharmaceutical interventions. By leveraging advanced technologies and expertise, the Cardiac Safety Services Market helps pharmaceutical companies, regulatory agencies, and healthcare providers navigate the complexities of cardiac safety assessment, fostering confidence in cardiovascular drug therapies and promoting patient safety.
Cardiovascular Diagnostic Devices Market: Precision in Cardiovascular Care
The Cardiovascular Diagnostic Devices Market focuses on devices and technologies designed to diagnose and monitor cardiovascular diseases. These devices range from imaging systems such as MRI and CT scanners to diagnostic tools like blood pressure monitors and lipid profile analyzers. By providing healthcare providers with accurate and timely diagnostic information, the Cardiovascular Diagnostic Devices Market plays a crucial role in facilitating early detection, informed decision-making, and personalized treatment planning, ultimately improving outcomes for patients with cardiovascular diseases.
Cardiovascular Disease Drug Market: Targeting the Underlying Causes
The Cardiovascular Disease Drug Market is dedicated to developing innovative pharmaceutical interventions that target the underlying causes and mechanisms of cardiovascular diseases. These drugs aim to address risk factors such as hypertension, hyperlipidemia, and diabetes, as well as target specific pathophysiological processes contributing to cardiovascular diseases. By focusing on disease modification and prevention, the Cardiovascular Disease Drug Market holds the promise of transforming the management and treatment of cardiovascular diseases, offering new hope for patients and healthcare providers alike.
Cardiovascular Market Revenue and Companies: A Thriving Industry Landscape
The Cardiovascular Market Revenue reflects the industry's robust growth, driven by increasing prevalence of cardiovascular diseases and advancements in medical technology and pharmaceutical research. Leading Cardiovascular Market companies are investing heavily in research and development, strategic partnerships, and global expansion, shaping the future of cardiovascular care. As the Cardiovascular Market continues to evolve, it offers lucrative opportunities for innovation, investment, and growth, paving the way for improved cardiovascular health and well-being globally.
Cardiovascular Surgery Market: Advancing Surgical Interventions
The Cardiovascular Surgery Market focuses on surgical interventions for treating complex cardiovascular diseases. From minimally invasive procedures such as angioplasty and stent placement to open-heart surgeries like bypass grafting and valve replacement, the Cardiovascular Surgery Market offers a range of surgical options tailored to individual patient needs. By leveraging technological advancements, innovative surgical techniques, and multidisciplinary collaboration, the Cardiovascular Surgery Market is driving advancements in surgical care, improving outcomes, and enhancing quality of life for patients with cardiovascular diseases.
Conclusion: A Bright Future for the Cardiovascular Market
In conclusion, the Cardiovascular Industry is a dynamic and multifaceted sector within the healthcare industry, encompassing devices, drugs, and services that are instrumental in managing and treating cardiovascular diseases. From the advancements in cardiovascular devices and drugs to the critical role of cardiac safety services and diagnostic technologies, the Cardiovascular Market is at the forefront of innovation, driving advancements in cardiovascular care and improving patient outcomes globally. As the industry continues to evolve, it holds the promise of transforming cardiovascular health and well-being, offering new hope for millions of patients affected by cardiovascular diseases worldwide.
0 notes
Text
Antiarrhythmic Drugs Question And Answers
#Pharmacology#bdsnotescom#PharmaceuticalIndustry#ClinicalPharmacology#DrugsandResearch#Antiarrhythmicdrugsquestionandanswers
1 note
·
View note
Text
Management on Non-Sustained Ventricular Tachycardia:
Definition – The most common definition is three or more consecutive ventricular beats, a heart rate of greater than 100 beats per minute, and a duration of arrhythmia of less than 30 seconds.
●Symptoms – Patients with nonsustained ventricular tachycardia (NSVT) are usually asymptomatic, although some patients may notice symptoms associated with episodes of NSVT. Symptoms may include palpitations, chest pain, shortness of breath, syncope, or presyncope. Symptoms may vary depending upon the rate and duration of the NSVT along with the presence or absence of significant comorbid conditions.
●Physical examination – By definition, the pulse rate is greater than 100 beats per minute.
Few physical examination findings are unique and specific for NSVT.
If the physical examination coincides with an episode of NSVT, this can reveal evidence of atrioventricular (AV) dissociation, including marked fluctuations in blood pressure, variability in the occurrence and intensity of heart sounds (especially S1), and cannon A waves.
●Evaluation – All patients with suspected NSVT should have a 12-lead electrocardiogram (ECG), although NSVT is frequently identified on continuous telemetry monitoring, in which case only one or two leads may be available for review.
•Reversible causes – Once identified, reversible causes of NSVT should be sought, including electrolyte imbalances, myocardial ischemia, hypoxia, adverse drug effects, anemia, hypotension, and heart failure.
•Single asymptomatic episode – Often, for these patients, no further investigation is required.
•Multiple or symptomatic episodes – For patients with multiple episodes or with symptoms felt to be related to NSVT, a thorough diagnostic evaluation to exclude structural heart disease is warranted, including cardiac imaging and ambulatory ECG monitoring for most patients and invasive electrophysiology studies (EPS) only on rare occasions.
●Treatment
•Asymptomatic patients – In general, asymptomatic patients do not require any specific therapy directed toward the NSVT.
However, some asymptomatic patients with NSVT who are found to have infarct-related cardiomyopathy with significantly reduced left ventricular systolic function may be evaluated for implantable cardioverter-defibrillator placement for primary prevention of sudden cardiac death related to sustained ventricular tachyarrhythmias.
•Symptomatic patients
-Initial therapy – For the initial treatment of patients with symptomatic NSVT, we suggest beta blockers rather than calcium channel blockers or antiarrhythmic medications (Grade 2C).
For patients with NSVT who remain symptomatic in spite of beta blockers, or who are unable to tolerate beta blockers due to side effects, we suggest adding a nondihydropyridine calcium channel blocker (ie, verapamil or diltiazem) rather than an antiarrhythmic medication (Grade 2C).
-Alternative therapy – For some patients who have frequent, highly symptomatic NSVT not adequately suppressed by beta blockers or calcium channel blockers, the addition of antiarrhythmic medications (table 1) may be helpful. We suggest amiodarone as the initial choice, rather than other antiarrhythmic drugs, based on its efficacy (Grade 2C).
In patients with very frequent symptomatic monomorphic NSVT not controlled by medications or who are unable or unwilling to take medications, catheter ablation can be effective for reducing or eliminating NSVT and associated symptoms.
3 notes
·
View notes
Text
Role of Catheter Ablation in the Comprehensive Management of Atrial Fibrillation
Atrial fibrillation (AF) is the most common arrhythmia that can lead to significant morbidity and mortality. Anti-arrhythmic drugs (AADs) are limited by a relatively low efficacy and substantial side effects. Interventional electrophysiology became an effective option in the management of selected patients with AF. Current guidelines recommend catheter ablation for patients with symptomatic paroxysmal or persistent AF for whom AADs have failed (class I). Patient with AF and multi-cardiovascular morbidities might have more recurrence rate of AF after ablation compared to those without significant morbidities. Advancement of technology would further improve the safety profile and clinical outcome of AF ablation. Future research would further refine our knowledge and might expand the groups of AF patients who would derive clinical benefit from AF ablation. Early referral of ideal candidate for AF ablation is much appreciated as it would be associated with better outcome at long term.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia worldwide. The currently estimated prevalence of AF in adults is around 2 per cent. With ageing of the world population and intensifying search for undiagnosed AF, the prevalence of AF is expected to increase. Increasing age is a prominent AF risk factor, but other comorbidities including hypertension, diabetes mellitus, heart failure, coronary artery disease, chronic kidney disease, obesity, and obstructive sleep apnoea are also important and relatively modifiable risk factors which are considered potent contributors to AF development and progression.
Patients with AF usually have recurrent symptoms and significant impairment in their quality of life. AF could increase risk for major adverse cardiovascular outcomes mainly stroke, heart failure, and cardiac death.
Cornerstones of AF management
When evaluating AF patients in the clinic, careful characterisation of AF is necessary for proper decision-making, and optimal management of AF patients. This includes evaluation of AF-related symptoms (e.g., fatigue, tiredness, exertional dyspnoea, palpitations, and chest pain) and quantify the patient’s symptom status using the modified European Heart Rhythm Association (EHRA) symptom scale before and after initiation of treatment, determining the type of AF (paroxysmal, persistent, longterm persistent, and permanent atrial fibrillation), clinical assessment of stroke risk, burden of AF, etc.
Comprehensive management of AF consists of three main aims: 1- The alleviation of patient’s symptoms; 2- Prevention of tachycardia-mediated cardiomyopathy at atrial and ventricular levels; 3- Minimising the risk of stroke. The first two aims can be achieved with either a rate control or rhythm control (maintaining sinus rhythm) strategy. The third goal can be fulfilled by careful evaluation of AF patient’s risk of thromboembolic event according to CHA2DS2VASc score to determine the patient’s need for oral anticoagulation. For patients in whom a rhythm control strategy is chosen, catheter ablation (CA) and antiarrhythmic drugs (AADs) therapy are the two therapeutic strategies to reduce the frequency or eliminate episodes of AF.
AADs (class I and III) have been widely used for rhythm control in AF. Owing to the limited success and perceived side effects of AADs, CA has emerged as recognised option and early choice treatment strategy in certain groups of AF patients. With accumulating experience and the rapid development of new ablation techniques over the last two decades, the results of CA procedures have been significantly improved at terms of efficacy and safety.
CA for AF
It is well recognised that AF is caused by rapidly firing electrical foci that are often located in the pulmonary veins especially when fibrillation is paroxysmal. Histological data show that myocardial tissue of the left atrial wall extends into the pulmonary venous walls. Clinical and animal studies reveal both double potentials and fractionated electrical activity in the pulmonary veins, which are related to the complex architecture of the myocardial sleeves in the veins.
Based on these data, circumferential pulmonary vein isolation (PVI) became the accepted interventional therapy to treat AF.
Simply, CA for AF is a procedure to treat atrial fibrillation. It uses small burns (radiofrequency) or freezes (cryoballoon) to cause some therapeutic scarring on the inside of the heart to help break up or insulate the electrical signals that cause/trigger irregular heartbeats.

In general, CA is a recommended treatment option for AF when AADs therapy fails in controlling patient’s symptoms (class I).
Current European Society of Cardiology recommendations:
CA for AF with pulmonary vein isolation (PVI) should be considered as first-line rhythm control therapy to improve symptoms in patients with symptomatic paroxysmal AF episodes (class IIa).
CA for AF may be considered for persistent AF without major risk factors of AF recurrence as an alternative to AADs class I or III, after taking into account patient’s choice, risk, benefit, (class IIb).
Use of additional ablation lesions beyond PVI (i.e., atrial low voltage areas, lines, fragmented activity, ectopic foci, rotors, and others) may be considered (class IIb).
Repeated PVI procedures should be considered in patients with AF recurrence provided the patient’s symptoms were improved after the initial PVI (class Ia).
CA for AF is recommended to reverse left ventricle dysfunction in AF patients when tachycardia-induced cardiomyopathy is highly probable, independent of their symptom status (class I).
CA techniques, efficacy and safety
Two ablation techniques still dominate when performing PVI:
point-by-point radiofrequency (RF) ablation of the atrial tissue surrounding the pulmonary veins using a single-point catheter with the aid of a three-dimensional mapping system toward complete electrical isolation of pulmonary veins.
Single-shot ablation technique with the use of a cryoballoon (freezing approach). Each technique has its advantages and disadvantages, but with similar safety and efficacy in the treatment of paroxysmal AF. The recognised and appreciated advantage of the RF-based approach is that it can be used to ablate atrial tissue beyond PVI, which is usually needed for the treatment of long persistent AF or recurrent AF after a first PVI attempt particularly when encountering significant areas of electrical atrial tissue remodelling.
Evaluation of CA efficacy is mainly measured on the basis of: elimination of late AF recurrence and decrease of the AF burden. Late recurrences of AF is defined as the development of any type of atrial arrhythmia lasting more than 30 seconds (AF, atrial flutter, or atrial tachycardia) between 3-12 months after the CA procedure. AF burden is measured as the percentage of time in which the patient’s cardiac rhythm spent in AF during a certain monitoring period. Early recurrences of AF within the first 3 months of follow-up are of limited clinical significance since only half of those patients will finally develop later episodes of AF. Based on the above success measures several clinical trials have shown that a first AF ablation procedure can eliminate late recurrences in approximately 70 per cent of patients with paroxysmal AF and decrease the AF burden by 80 per cent in a follow-up ranging from 1 to 5 years. Success rates are typically lower in patients with persistent AF reaching 50 per cent after a single procedure. For those with late recurrence or remaining significant AF burden, the success of the second AF ablation (PV re-isolation) is >90 per cent.
Read More: https://www.europeanhhm.com/medical-sciences/role-of-catheter-ablation-in-the-comprehensive-management-of-atrial-fibrillation
#healthcare#hospitals#doctors#health#health and wellness#healthy lifestyle#medical equipment#medical care#technologies#medical science#catheter#atrial fibrillation
1 note
·
View note