Text
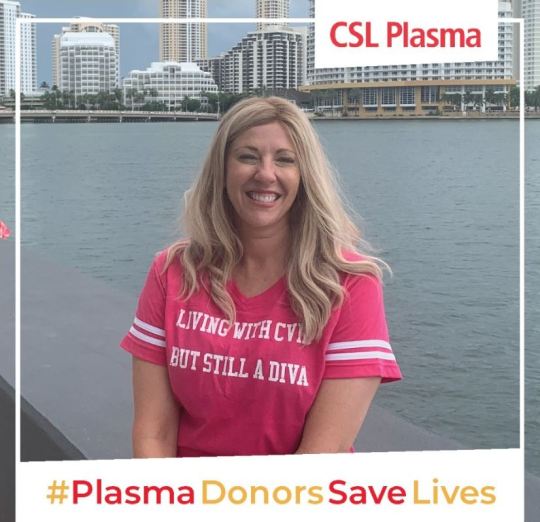
Jessica’s PI Story

It’s World PI Week and I’ve got PI! Private Investigator? Nope! Primary Immunodeficiency. Still not getting it? Well, there are different types of immunodeficiencies, but I have Common Variable Immunodeficiency / Hypogammaglobulinemia. This means I don’t have enough Immunoglobulins in my blood to fight off germs or form immunity to illness. The paranoia everyone has been experiencing with COVID is the everyday reality of Common Variable Immunodeficiency patients. We’re also very susceptible to cancer.
Everyone who has CVID is born with it, although many of us do not get severe until later in life. My disease got very bad when I was around 30 and getting constant infections. Other related autoimmune diseases started showing up at about the same time. I knew something was terribly wrong.
For five years I was a hopeless wanderer, going from doctor to doctor pleading for help. Their reactions varied; some said there was no underlying disease causing my body to implode. Yeah. Okay. Most, on the other hand, wanted to help but didn’t know how because they’d never seen a case like me. We’re few and far between.
The day I was diagnosed was one of the best days of my life. Sounds crazy, but it’s true. Although there’s no cure, the disease does have a treatment. People sell their plasma, and immunoglobulins are extracted from that plasma. So I get some immunoglobulins from other people (indirectly) every week. I have my own infusion pump and have been trained to do infusions subcutaneously at home. That way I don’t have to go and wait at a hospital, exposing myself even further to germs.

I have a lot to be grateful for: excellent specialists, my Freedom60 pump, and good insurance. Many don’t have it as good as I do, so I don’t dare complain. Why am I telling you all this? Well, now you know my story and maybe it will save someone you know from being a hopeless wanderer. Maybe you sell your plasma and I want to say THANK YOU for allowing me to live something akin to a normal life.
- Jessica S.
1 note
·
View note
Text
Louis’ PI Story

From infancy, Louis struggled with infections. From six months on he was sick all the time. His older brother was also getting sick often. Louis was about 1 year old when we had his older brother tested for allergy/immunity to see if that was the root cause of his illnesses. Allergies were not the cause, but it turned out that he had very little to no pneumococcal antibodies. The immunologist recommended a vaccine challenge, so we did it. He produced antibodies and with that, he stopped getting sick so frequently.
Fast forward about 2 years to Louis who was not quite 3 years old. We were one ear infection away from needing tubes when he was tested just as his brother was. We thought it would be the same story, he would make the antibodies and then the frequency of illnesses would decrease. He did not make antibodies with his vaccine challenge and was diagnosed with Specific Antibody Deficiency at the time. He did eventually need to get tubes placed, but that only helped with ear infections. He kept getting other infections, fortunately not too severe, but consistently needed to be put on antibiotics.
His illnesses were managed for about two years and then he became allergic to Augmentin. He was on and off antibiotics at least 6-7 times in a four-month period just as he was turning 5. His stomach was a mess, and he was missing out on so many activities and pre-k because he was sick so often.

We finally decided that we needed to start treatment. We chose to do subcutaneous infusions for him because his levels would stay more stable through the month and there would be fewer side effects. He started just after he turned 5 years old, and we have not looked back since. When he was around 7 years old, he was diagnosed with CVID (Common Variable Immune Deficiency).
He is now 10 years old and is in the healthiest stretch of his life these past two years during a global pandemic. He truly amazes us every day. He does not let anything stop him from doing the things that he loves to do. He is a very active and athletic boy who is growing like crazy. He loves all sports from playing to statistics, but his true love is lacrosse. He plays very competitively and thanks to his treatments he is healthy enough to do it. He is either at practices, training or out playing with his brother almost every day. He has recently been accepted to a National Team and we are beyond proud. His treatments were a game-changer for him, no pun intended! We are so thankful for our team of doctors and nurses.

- Gina G.
0 notes
Text
Susan’s PI Story
I was diagnosed November 1, 2017 by my son's asthma doctor, who also specializes in allergies and immunology. I had quite literally drug myself out of bed that afternoon to take my son to his appointment. It wasn't until I mentioned something about myself (I don't remember exactly what) in an attempt to help the doctor treat my son, that the doctor froze, turned and looked directly into my eyes and started firing questions one after another at me.
Then, an army of nurses entered the room at his beckoning and began drawing blood, taking vitals and writing furiously fast. Soon, the doctor began telling me what he thought the blood test would prove I had - a Primary Immunodeficiency called Common Variable Immunodeficiency (CVID). I began IVIG immediately and unfortunately suffered from numerous side effects.

After three years, I was stable enough to try SCIg. Of course, it was intimidating at first, but I immediately knew it would be a better treatment option for me with less side effects and the freedom to receive my medicine in smaller doses each week at home. I even crafted a zebra-themed rolling cart that houses all my SCIg supplies, including my Koru Freedom Pump! One tip: I use a lidocaine patch to numb my infusion area before inserting the needles. Lidocaine cream also works well!
- Susan D.
Follow Susan for more great CVID and infusion tips on her blog, CVIDiva!
1 note
·
View note
Text
Aeisha’s PI Story

My story began just before my 30th when I was planning my big birthday party. I was experiencing strange bloating symptoms where my stomach would go from flat and toned to large and distended for no reason at all. It wasn't triggered by food or anything, just spontaneous bloating. I generally stay fit and lean, so looking like I was 6 months pregnant was an issue for me, especially because my clothes were no longer fitting. It took me many visits to many doctors for them to tell me "it's just hormonal" and "it's no big deal", but I KNEW something was wrong. I know they thought I was just some crazy person coming to their office, but I had to find the answers to my issues.
After visiting primary care doctors and gynecologists who decided they couldn't find anything wrong, I went to a gastroenterologist. Upon seeing him, I broke down in tears letting him know that I wasn't crazy, that I have a great and fulfilling life, that I am not here for attention, but HE NEEDED to take me seriously. After months of tests and consulting with him about my own research and tests I wanted him to perform, we finally did an endoscopy and colonoscopy.

The first thing this doctor said to me was, "You are NOT crazy" since my results showed that my intestines expressed nodular lymphoid hyperplasia (NLH) which simply means they are lined with lumps which prohibits proper absorption of fats and nutrients as well. Though the NLH was seen, no one knew the reason for its existence. It took one of his colleagues to remember seeing this is in a medical book in medical school for him to remember it was linked to a type of blood deficiency.
From there I was sent to get my immunoglobulin levels checked (and a lot of other blood tests) and that is when it was noticed that my IgG and IgM levels presented just outside of the normal range, but my IgA was non-detectable. I was then sent to one of the few specialists in the United States to Mt. Sinai hospital in NY for diagnosis of my condition. She diagnosed me in 2010 with a "Selective IgA Deficiency" and for the next 10 years I managed my gastrointestinal issues by eating clean and removing processed foods. She mentioned that my condition could progress to CVID if my other immunoglobulin levels continue to decline and that I'd have to monitor them over the coming years.
In late 2019, I started to experience spontaneous weight gain in the abdominal area, though I was working out 5 days per week. I was gaining weight so fast that it was uncomfortable to eat or sit up in a chair and breathe. Additionally, I started having strange skin infections on my face and chest. Physically, I felt extremely fatigued and had hardly any energy past 12 noon every day. As someone who works full-time and lives a pretty active life, it was torture. I was too tired to do my normal tasks, I felt awful, and I looked terrible.
I decided to reach out to my gastroenterologist because it had been years since I saw him and I wanted to let him know of the newest issues. My food was no longer digesting, so days of food would sit without leaving my body along with the weight gain and fatigue. He repeated the immunoglobulin tests and repeated the endoscopy and colonoscopy. When my tests came back, the NLH still presented, but all my immunoglobulin levels were drastically low. In addition to treating the gastrointestinal issues, he advised me to find an immunologist who could focus on my condition and decide on my next course of action.
There are very few physicians who are familiar with immunoglobulin issues or physicians who are willing to take on patients with those issues, however, I was lucky enough to find one who was motivated to do extensive research and work with me on finding out what to do. I shared with her my medical files from all the previous years and equipped her with tests and lab results from all my physicians to get her started.
After months of seeing her and doing various tests, she confirmed my diagnosis of CVID and recommended I started immunoglobulin therapy. I went on Instagram and started talking to a few patients who have been using immunoglobulin therapy for CVID and knew what questions to ask her about treatment and the experience overall. Though she seemed sad to break the news, I was ecstatic to know there were options to explore. She set me up with the medication she felt was best for me and the nurses started training me at home in August 2021.

“It has been 7 months since my first infusion and I couldn't be happier with the progress of my treatment and the ease of the pump to do my infusions.”
I quickly learned how to inject my needles and get my infusion going by myself. After the first visit, I was able to do all the steps myself with the nurse on standby for assistance if needed. The first month or so was a bit rough since the infusions seemed to wipe out my energy completely, so when I infused on Thursday, I was in bed the entire weekend in recovery. But after that, I started to feel like Superwoman after my injections. My energy was back and I felt like a brand new me! It has been 7 months since my first infusion and I couldn't be happier with the progress of my treatment and the ease of the pump to do my infusions. Though I still have gastrointestinal issues, I do have more than enough energy to work and workout at the pace that I am used to. I feel as though my quality of life has been restored and I look forward to better days ahead!
- Aeisha W. - CVID Patient
0 notes
Text
How to Cultivate a Hopeful Mindset using Maybe
by Susan Alynne Day

A diagnosis of Common Variable Immune Deficiency (CVID) can take down a once hopeful mindset in one fell swoop. However, you can use this easy Maybe Technique to cultivate hope once again.
Recently, a CVID Zebra I mentor was sharing with me that she was having some anxious feelings about going to a social event. She used to attend this event annually before her diagnosis (and COVID) and she knew most of the people who would be in attendance. Before the event, she was noticing self-critical thoughts such as “I am not very interesting anymore…they might not like me anymore…and what if they act awkward around me now that I have CVID?”
Now, what I know to be true about this Zebra is that she is super interesting and everyone seems to like her. While some of her friends she hasn’t seen in a while may act a little awkward at first, my bet was that she could put them at ease with her humorous personality.
I encouraged her to try something new before the event and it really helped her re-frame her thinking – she said to herself “maybe I am interesting….maybe they will like me…maybe they will feel awkward at first but I can help them feel at ease.” She noticed the anxious feelings lessen and she enjoyed the event more than she thought she would.
There is Power in the Word Maybe
Try adding the word “maybe” to your thoughts this week:
I’m not going to do very well because I’m not at my best – maybe I will.
I’m not strong enough to do SCIG every week for the rest of my life – maybe I am.
This IVIG infusion is going to be miserable – maybe it won’t be.
I have no value to add now that I have CVID – maybe I do.
That was a horrible decision to attend that event – maybe it wasn’t.
I can’t figure out my purpose now that I have CVID – maybe I can.
I’m not a good friend because I’m always ill – maybe I am.
I’m going to fail because I can’t perform like I used to before my diagnosis – maybe I won’t.
I’m not the right size anymore because I’ve lost/gained weight since my diagnosis – maybe I am.
It is too late for me to succeed in my life – maybe it isn’t.
I can barely cope, how can I help anyone else – maybe I can.
My dreams aren’t going to happen now – maybe they will.
I won’t be chosen for that job I want now that I have CVID – maybe I will.
I am afraid I get even more sick – maybe my treatment(s) will make me feel better than I ever have before.
IVIG or SCIG will hurt – maybe it won’t hurt that much and I’ll learn methods to make it hurt less.
I can’t – maybe I can.
The Science Behind Maybe
The neuroscience behind this tool is that we feel a dose of hope in our brain when we use the word “maybe.” It brings a sense of possibility and potential. Hope has been widely researched as a feeling that results in a release of dopamine which leads to healing, optimism, and happiness in our psyches.
“Hope is the belief that the future will be better than the present, along with the belief that you have the power to make it so” - Dr. Shane Lopez, senior scientist at Gallup
Dr. Lopez is uncovering amazing new research showing that not only is hope good for your wellbeing, but it’s a measurable quality that can be increased with practice. His new book, Making Hope Happen, discusses the science behind hope and describes practical ways to improve your wellbeing by nurturing a positive, active approach to live. Click here to watch an interview with Dr. Lopez about his new research on hope.
Practice challenging yourself to flip your thoughts into a “maybe….” statement of the opposite sentiment. Challenge your brain when it tries to tell you something negative. Instead, use Maybe to change your mindset and cope with CVID.
Hope matters. Hope is a choice. Hope can be learned. Hope is contagious.
Here’s to Maybe…

ABOUT THE AUTHOR
Though DIVA as she may be, her path to success was not easy and is always evolving. Go here to read about her journey in “Becoming the CVIDiva.” If you want to send Susan Alynne a quick message, then visit her contact page here.
0 notes
Text
How to Move Through the Guilt of Being Chronically Ill
Blog by Laura Mazzotta, LCSW-R

Photo by Kat Smith from Pexels
For the majority of my life, I was what you could call “Type A”. I was organized, efficient, and a hard worker. I was also a chronic people pleaser and overachiever. This all changed when I contracted sepsis 5 years ago, and then later diagnosed with chronic illness. Suddenly, I was in bed for most of the day, unable to move, think, or even speak at times. As a mom of 3, a wife, and a business owner, it felt like everything I had worked so hard for was being put on hold without my permission.
My husband, also working full time, now had to become the head of the household, along with becoming my full-time caretaker. It was a difficult concept to process. My inner dialogue as I moved through the stages of guilt surrounding my husband’s role in my recovery from chronic illness (keep in mind this was a process of unfolding and did not happen overnight) looked something like this:
Me: OMG why do I have to lie down again?! I feel so useless.
Also Me: He just wants me to be healthy.
Me: But he is doing everything!
Also Me: His desire is for me to be happy.
Me: Poor guy did not sign up for this.
Also Me: He signed up for me. All of me.
Me: He doesn’t have room to do his own thing.
Also Me: He gets to make that choice for himself. He gets to ask for other help if he needs it.
Me: It’s not fair he has to experience this illness as well.
Also Me: Our souls contracted to do this life together. We both knew exactly how it would unfold. We are helping each other fulfill our life’s purpose.
Me: He is so tired and run down. I wish I could be a better wife.
Also Me: He can choose to rest. His happiness is not my responsibility. My happiness is my responsibility…
So I chose to be happy. I chose to go within and release the shame I was projecting onto him, so I can stand sovereign in my own experience. And now…?

He is so happy. He is so open. He is so full of energy. He is so resilient. We are so connected. We are more in love than ever before. Oh, and funny enough, I feel better. I have more energy. I can do more around the house…and most importantly, I am PROUD of myself. For healing, for deciding, and for being fully and unabashedly ME, in all my splendor.
Get support if you don’t know where to start with this process. There are so many who have gone before you and mastered this concept, and they’re soaring. Allow them to help you so you have a solid foundation as you heal.
Want to connect with Laura? You can set up an appointment HERE if you want to connect for a free 10-min Power of Connection Call, to clarify your current personal or professional goals.
1 note
·
View note
Text
A Lack of Awareness Prolongs CVID Diagnosis
by Susan Alynne
Among the CVID patient community and advocacy organizations, many agree that a lack of awareness prolongs CVID diagnosis. In 2017 I found out that I was born with Common Variable Immunodeficiency. CVID is a genetic Immune system disorder in which there are low levels of antibodies to fight off infections.

The “variable” in its name refers to the wide variety of symptoms and their severity found in patients. This makes it extremely difficult for doctors to diagnose and potential patients to recognize. Although awareness is on the rise in part because of the efforts of organizations like The Immune Deficiency Foundation and The Jeffrey Modell Foundation, there are still many doctors and people in general who are unfamiliar with Primary Immunodeficiencies and CVID in particular.
My Own Prolonged CVID Diagnosis Despite Numerous Warning Signs
For example, I wasn’t diagnosed until I was 41 even though I was often sick, seemingly without explanation, throughout my life. (You can read my diagnosis story here!) Case in point, I had never heard of CVID when I was diagnosed (neither had any of my friends or family!).
Below were some of the CVID symptoms I experienced:
Unexplained failure to thrive and hospitalization at just a few months old
Frequent Colds
Recurrent Tonsillitis
Repeated Swollen Lymph Nodes in my neck
Stomach Pain and digestion issues
Headaches
Recurrent Strep Throat
Numerous Urinary Tract and Bladder Infections which eventually required a nerve stimulator implanted in my back to allow the bladder to fully empty
Unexplained internal infection of C-section incision
Closer to my diagnosis, I experienced extreme fatigue, weight loss and body pain that confined me to my bed most days.
Why did the many, many doctors I saw throughout my childhood and the ones I consulted as an adult miss the underlying cause of so much illness?
Probably for numerous reasons.
Maybe my parents (and later I) did not provide a comprehensive enough look at my health history. Perhaps each doctor focused on doing what they could to treat my symptoms and provide quick relief. It could have been that the doctors I saw were not familiar with CVID. Whatever the reasons, we (i.e. me, my doctors) missed the clues.
Spreading Awareness Can Prevent a Prolonged CVID Diagnosis
Now that I know about and have CVID, I feel a great responsibility to spread awareness. With awareness, doctors can provide faster diagnosis of CVID and those with similar symptoms might recognize their story in mine.
Now it’s your turn!
Click here to download the Jeffrey Modell Foundation’s 10 Warning Signs of Primary Immunodeficiency and post to spread the word!
ABOUT THE AUTHOR
Though DIVA as she may be, her path to success was not easy and is always evolving. Go here to read about her journey in “Becoming the CVIDiva.” If you want to send Susan Alynne a quick message, then visit her contact page here.
0 notes
Text
6 Ways to Support Someone With Primary Immunodeficiency
by Joanna Tierno

I live with a primary immunodeficiency. Here are some ways you can support a friend who lives with this condition.
1) Learn all you can about primary immune deficiency.
Research, ask questions or even ask to tag along on a medical visit. Primary immunodeficiency foundations, such as the Immune Deficiency Foundation or Jeffrey Modell Foundation, provide a wealth of knowledge for family members as well. It’d be good to know the basics about the condition. I have to say, it’s upsetting when people I have known for decades still can’t name or describe what I have. Primary immunodeficiency diseases can also run in families, so knowing your loved one’s medical history could one day be important to your own health.
2) Respect the patient’s restrictions.
Just as you shouldn’t force ice cream cake on someone with diabetes, don’t try to force a high-risk situation on an immune compromised patient. Unfortunately, primary immunodeficiency diseases are not preventable. We did not choose or cause our disease. It’s easy to get frustrated when there are so many rules about our disease, but in order to stay well, we need to respect them.
3) Think before you post.
During the coronavirus pandemic, it has become fairly commonplace for people to post or say things like “Don’t worry, only people with weak immune systems will die from COVID-19.” As you may imagine, that isn’t very well received by someone living with a chronic illness. We want and deserve to survive just as much as everyone else.
4) Trust our experience.
When part of your body does not work properly, it forces you to learn more about it than you ever would if you were healthy. Most of the time, we are more than happy to share what our experience has taught us.
5) Sometimes we need you to speak up for us.
It is so hard always being the “bad guy” who has to remind people about the facts of infectious disease or of the reality of our condition. It can be a huge relief when someone else does the explaining for us, or when you can help us avoid a stressful or awkward situation altogether.
6) Just listen.
It’s one of the greatest acts of friendship any of us can do. Just be there for us and offer an ear. Have the uncomfortable conversations. Unfortunately, we can’t escape our own health issues, but knowing that we have the support and ability to talk about it really does help.
4 notes
·
View notes
Text
8 Things Immune Deficient Patients Can Teach the World in a Pandemic
by Joanna Tierno

I have lived with primary immune deficiency disease for nearly five decades and have worked at trying to stay well most of my life. I have picked up many tips along the way that I hope can help others during this pandemic. Here are lessons immunosuppressed patients have learned about staying safe and well.
1. We have learned ways to prevent infection.
Not touching our faces, avoiding crowded places, not accepting invitations that sound high risk, and noticing when others are sick and keeping a distance. I am on high alert with things like coughing, or a voice that sounds hoarse, which often goes unnoticed by others. I am also pretty good at visiting places without touching a thing. For years, I have been taking many of the precautions that people are being told to do right now — just not to this degree. Some tips for you: clean all your high-touch surfaces every morning with a proper disinfectant before it slips your mind. I also wash my hands and reusable face mask upon arriving home.
2. We are experts at dealing with isolation.
Like most people, this pandemic is the most isolation I have ever had to deal with, but it’s not my first rodeo. As a child with primary immune deficiency, I missed a lot of school due to illness. My mom worked and I was an only child, so I learned to care for and entertain myself. Luckily, that skill set has stayed with me. As a child, and even now I was never one to get bored. I always have things to do. To prepare for a potential quarantine or lockdown this winter, I have stocked up on books and videos. Many people throughout history have used times of isolation to their advantage. It is a great time to learn something new, develop ideas and work on projects.

3. We understand disappointment.
I have missed many important things throughout my journey with immune deficiency, and that is not at all uncommon. Illness has struck before parties, events and holidays. Someone else being sick has also kept me home many times. It’s disappointing, stressful and not at all fun, but sometimes health matters do come first. I know many things have been canceled in 2020, but the health of our country is invaluable. It’s hard to not celebrate holidays and milestones in our usual way, but it is important to retain perspective on it. We will enjoy better times ahead with those we love if we remain careful now. Instead of only focusing on the negative, try finding things in each day you can be grateful for.
4. We’ve learned about responsibility and discipline.
Being born healthy is something that shouldn’t be taken for granted. It’s not easy when you are born with an illness that can make it hard to survive. Part of my immune system is missing. It takes hard work and discipline for me to stay healthy. I have often wished I could bottle the chronic illness experience to share with healthy people who do not take care of their health. What if they could feel the fatigue, the pain or the respiratory issues of an immune deficient patient? Could they learn to value health and live in a more disciplined way? I have been frustrated watching many people take unnecessary chances during this pandemic. Even if you feel assured of your survival, what if you have long-term damage or effects? If you are not the self-disciplined type, know that any of us can change if we want to. Being responsible and showing self-restraint is like muscle building. The more you work out, the easier it will get.
5. From physical suffering and loss comes strength.
I’ve been paralyzed. I’ve been in so much pain that I have gone into shock. There have been a number of times I thought I was dying. I also experience migraines, so I understand the misery that chronic illness and pain can cause. All these experiences, if you get through them, can build strength. If you can manage even simple tasks while in agony, you have conquered. Every time you get back up and keep trying, keep moving forward and do not give up, you have built resilience. With COVID-19, everyone is going through something — loneliness, loss of income, illness, etc. Know that while 2020 has not exactly been anyone’s year, surviving the hardship of it can make you stronger and more confident in your ability to get through other difficulties in life.

6. We learn to cope with uncertainty.
I have three rare diseases. Rare disease patients are like pioneers. Most of us do not have a single FDA-approved treatment for our conditions - I am in the lucky percentage that does. Rare disease patients know that sometimes we will not get answers or help even from world experts because they simply do not yet know. It’s a very different experience than when you are diagnosed with something relatively common. And in many ways, the uncertainty of living with a rare disease somewhat prepares one for living in uncertain times that we are finding ourselves in today. Accepting what is and making the best of every situation is often the healthiest way to cope with all the unknowns. “Control the controllables” is a great mantra.
7. With love, much is possible.
While my mom didn't fully understand my diagnosis, she did her best to keep me safe from infections. Now, during this pandemic, I see my husband taking precautions he would not if I were healthy. With love, my mother helped me grow up and learn to thrive. With love, my husband is doing his best to keep me safe from this pandemic until effective treatments or vaccines are available. The fact that I made it this far is a testament to what is possible when people love and care for each other. Love is a miracle that we often take for granted. Cherish those who are showing you love and respect during this most difficult time.

8. Respect for experts.
Immunocompromised patients, like myself, know a lot about the immune system and infectious diseases thanks to our access to immunologists, infectious disease specialists and researchers. This knowledge makes it easier to spot misinformation regarding COVID-19. Unfortunately, conspiracy theories, lack of trust in science, and political and social divisions have hampered our response to the pandemic in the United States. I urge everyone to try to unite and not view this pandemic through a political lens. Get your news from multiple and diverse sources, and please listen to and respect our experts. They are our best way through this pandemic.
4 notes
·
View notes
Text
The Hidden Sacrifices of Chronic Illness
by Jennifer Landry

Chronic illness comes with the somewhat expected sacrifices: things like cancelling plans when you aren’t well, financial costs, lost job opportunities, etc. The sacrifices often permeate so much deeper into your life though when you have a serious chronic illness, especially one that is difficult and expensive to treat.
My illness has put a distance in my romantic relationship - a literal physical distance. My significant other is a physician. He just graduated from his fellowship training in June of this year. After his graduation, he took a job in an area at the opposite side of the country. We talked about it a lot, and that job was the best option for him at the time. Here’s the thing though: I couldn’t go with him. We are in the middle of a pandemic, and by nature of primary immunodeficiency, I am HIGH RISK for infection and serious complications. Moving across the country with him right now, a 30 hour drive, is dangerous in the current public health crisis. In addition to that, healthcare coverage and access is…extremely intricate and complicated at best.

I would have lost my health plan by leaving my job and moving cross country. I would have been in a bind to find a job in order to obtain health insurance asap. Then, I would have had to find a new specialist in a city that does not have a great selection of immunologists. I would have had to fight insurance all over again for coverage for the very expensive immunoglobulin infusions that my life and wellness basically depend on. In this entire process, I would have had a ton of exposure during a pandemic, and I would have likely missed several doses, if not months’ worth of infusions, making me HIGHLY susceptible to an infections.
Why does this all matter? My significant other and I have been doing long distance since early July (almost 3 months now with no end in sight), all because of my primary immunodeficiency. While my disease is currently well-controlled, a single thing like a job in a new city can create an absolute mess of a decision for someone with a chronic illness. It is an aspect of illness that we and our loved ones experience and is both deeply painful and often incredibly secretive. We don’t talk about it, because it feels too personal, even in this space, because of the way that my illness has directly impacted my relationship.

I want to scream about how unfair it is. Trust me, I know all too well that life usually isn’t fair, but it still makes me want to scream.
I want to scream about how my partner shouldn’t be forced into sacrifices, because of my illness. We both understand why it is necessary, but that doesn’t make it stink any less.
I want to scream about how if the general public pulled their weight to end the pandemic, it would lessen the time that my partner and I spend apart.
I want to scream about how much my life is tied to the actions of others right now. I like being solely responsible for the things that happen in my life, so having to rely on others to do their part is not in my nature.
I want to scream every time someone says that those of us who are high risk “should just stay home so the rest of the world can get on with their lives,” - what they are saying is that they expect me to continue making all the sacrifices indefinitely so that they can go on living their fun lives.
I want to scream about how I deserve to get to enjoy my life too and live in the same city as my partner again.
We sacrifice more than just health and money and lost job opportunities due to our illnesses. The term “we” doesn’t just include patients, either. It also includes those most closely around us: partners, parents, children, friends, etc. We all sacrifice pieces of ourselves that are so hard to quantify. I feel like revealing this part of me right now is just a rambling rant, but if this rambling rant makes one person feel less alone, then it has served its purpose. Please know that I see your hidden sacrifices, even when you can’t find the words to talk about them yourself. I know how much those hurt your heart, and I am here alongside you for the journey.
Chronically yours,
Jen

Chronic illness isn’t always obvious. Some of us look “normal” but struggle with symptoms that you would never know about if you didn’t know us.
>> To read more, check out Jen’s blog: a space about learning to live a full life with chronic illness
#invisibleillnessawareness#chronicillness#primaryimmunedeficiency#invisibleillness#potssyndrome#livingwithpi#chronicillnessblogger#zebrastrong
5 notes
·
View notes
Text
Who am I?
by Julieann Hartley

I am a brave person who has advocated nonstop for my health.
I am a strong person who can find a way to persevere through this medical journey and re-balance my health.
I am a vulnerable person who can admit I wouldn't be alive today without my community support systems and partner.
I am an empathetic person who now understands what living with a brain injury and chronic infection really means.
I am a passionate music therapist who genuinely cares about my clients and will find creative ways to help and advocate for them. I will get though this so I can continue to help them.
I am a children's music composer who writes music children actually listen to because it's neurologically appropriate for them. My last album (which won a national award!) was written and recorded entirely while I was fighting off multiple chronic infections at a time due to my immune disorder, which prevents my body from being able to fight off an infection.
I am enough and I am worth it.
Who are you?

Julieann’s Story
I have been on a journey to find health my whole life. I'm a classic "textbook" case of immune deficiency, spending my lifetime fighting off infection after infection. I never get a "normal" immune response to illness to signal to a doctor that I may actually be very sick. I'm the kind of person who gets strep, but because I may not get a fever, the strep will linger and linger until suddenly I break out in hives from having the infection for so long. I will then be able to subdue the infection with antibiotics, but almost always, it comes back for a second or third round.
For the past decade, I've been trying to explain to doctors that something was wrong. I couldn't digest food, every joint in my body hurt, I was slowly losing cognitive abilities and I was struggling with my sensory processing. For years, my primary doctor suggested I was depressed and never opted to do more testing. The fact that I was made to feel like it was all in my head, and like I was a hypochondriac was so disheartening.
Finally, when I decided to see another doctor who actually ran more tests, it turned out I had an advance neurological Lyme disease infection, severe autoimmunity, lead poisoning, a brain injury and an immune deficiency. Over the years, I've been picking up the pieces of my shattered health, slowly but surely addressing the root causes of my illness.
Throughout all this, I had managed to graduate as valedictorian of my college, hike the Appalachian trail, run a full time music therapy practice and write a national award winning children's album. For so long, when I asked for more testing from my original doctor, he reminded me that "Sick people don't smile". I think to him, I was too successful, too determined to be seen as seriously ill.
News flash: You can be severely sick and be smiling and successful at the same time.
Recently, I had to leave my music therapy practice after a neurologist told me, "Your brain is turning into stew. You need to rest and we need to treat this seriously." At this point, I could no longer drive, the world was spinning constantly, and I was losing cognitive abilities and strength at an alarming rate. It was terrifying, and a vulnerable process. I had always defined my self worth by my ability to work and support myself and others. For the first time, I had to redefine what made me worthy and let others begin tending to me.
I just had a PICC line placed so we can begin IV antibiotics and IV immunoglobulins through home infusion. This is amazing and allows me to continue writing music for children. I know in my heart that I'll be OK, I'm worthy and that I will heal.

#chronicillness#primary immunodeficiency#lymedisease#music therapy#autoimmunity#immunoglobulin#ivig#chronic infection
6 notes
·
View notes
Text
How Does Hate for my Illness Call for Unconditional Love?
by Laura Mazzotta, LCSW-R

I hate being sick. I’m so tired of:
Having to cancel plans
Not making plans because my health is too unpredictable
Saying no when my kids ask to play
Staying inside when it’s a gorgeous fall day because I have to lay down and need just the right temperature
Having to take my supplements, medications, and eat meals and snacks at exactly the same time each day so I remain marginally stable
Having to regulate how long I can stand up so I don’t collapse
Asking my husband for help, once again, when he is taking care of the kids, working, and doing all the cooking, cleaning and shopping
Canceling on my clients, again, without knowing when I can reschedule
Having to wait on visiting family or taking vacations because I don’t know if I’ll be healthy enough to go
Spending tons of time and money on supplements, appointments and meds, all while I’m working less.
IT SUCKS…OR DOES IT?
I’m tired and angry. Sitting in this vibration doesn’t serve me; it only adds to my dis-ease.
I’m also relieved. Of a lot of responsibility, obligation, our fast-paced lives, and expectations.
There’s something freeing in that. My body is offering me the choice to invest my energy into what is truly in my best interest, versus weighing all the other factors.
It’s simplifying life and decisions for me. No explanation or justification is needed, to myself or others, because I’m sick. Everyone understands when you’re sick.
But then you look at the underpinnings of this. What purpose is this serving me right now? Because there is a purpose.
EXPLORING THE PURPOSE
Inspired by the four questions of Byron Katie (The Work), I chose to explore this idea by turning the statement around that’s come to define me. My statement: I hate my illness.
The turn around? I unconditionally love my illness. Hence the blog title. This sentence scares the crap out of me because I have resisted consciously identifying with being ill.
My classic statement when I first got sick was, “I will not let this define me.” Guess what? When you actively resist something like that statement, it persists. So…
Since the illness has come to define me so much, the question becomes, for what or where do I need to learn and apply unconditional love toward myself? Does it involve my loved ones? Those I need to forgive?
Ultimately, in any of the above scenarios, it comes down to me. Everything and everyone else I come into contact with is reflecting back qualities within myself. The world is a mirror.
So what does unconditional love of self mean? Where does it come from? How do I even start this process?

UNCONDITIONAL SELF-LOVE
Unconditional love of self is acceptance and awe of your current state of being (physically, energetically, emotionally, cognitively and spiritually), without judgment or agenda.
It is a glowing warmth that is always extending from your Higher Self to your physical form. Casting healing, compassion and forgiveness upon you at all times.
There is an endless supply of this love flowing through each one of us. We need to take the time in stillness to witness it.
To call it in. Embrace and inhale the glow. Imagine its immersion into all of our cells. And elevate ourselves to meet this golden vibration. The air is lighter up there, and carries a stream of unconditional love and simplicity that cannot be matched here on Earth.
In this space, we are untouchable. Our physical bodies don’t matter. They’re vehicles that we choose and can choose to embody.
When we choose to return to and remember who we are at a spiritual level, the significance of external reality washes away. We are timeless. Our mission and purpose has existed for longer than we may ever know (at least in human form).
This timelessness erases the pressure felt in this life for achievement and measured progress. Who gives a shit about all the expectations? These details aren’t even on the radar of those in the spiritual realm.
Rise up, my friends. Beyond the scope of where we are. Spiritually, we are nourished. We are healthy. We are thriving. That’s the truth of who we are, where we came from and will return to. All of this 3D world is just temporary. Spend a little more time with your head in the spiritual clouds and this reality will become palpable.
Once you taste it, mmmm, you will be continuously called to go back. Allow yourself to feast from this limitless table and you will always feel fulfilled.
_
Laura Mazzotta, The Akashic Therapist
Laura Mazzotta, LCSW-R, is an expert therapist, Certified Akashic Records Practitioner and Reiki Healer with over 15 years of experience. She serves women ready to explore holistic, alternative methods of healing and transformation, to address their chronic or complex pain, illness and disease. Laura knows true healing occurs much more powerfully when all components (physical, mental, energetic and spiritual) of a person’s issue are addressed. She’s here to guide her clients in all steps on that journey. You can find Laura at www.theakashictherapist.com and join her free group for healing tools at Room for Healing.
0 notes
Text
7 ‘Hidden’ Things About My Life With Primary Immune Deficiency
by Joanna Tierno

Since primary immune deficiencies (PI) are an “invisible” disability, it’s hard to see what I go through on a daily basis. So here’s a glimpse of what you can’t see about my life as I manage my chronic illness.
1. It’s exhausting.
It’s hard to describe fatigue that comes from a systemic disease. But if you think of the last time you were sick — that is what it can feel like to live with a disease like PI where your immune system is always struggling and never exactly “normal.” Imagine feeling like that every day. Then imagine you have more – not less to do – than everyone else to maintain your health. This includes infusions, medications, treatments, appointments, insurance issues and research. And I am never actually ever “done” with these things.
2. I am usually in pain.
I do a lot to manage my pain so I can stay functional, including using a Quell device numerous times a day. I do not sit or stand too long, and I avoid muscle strain. I take medications to prevent migraines. I use ice every day to reduce inflammation. Still, I always have some level of pain. Sometimes before my infusions, if my levels are low, my knees hurt really bad.
3. It takes a lot of discipline.
I eat what I am supposed to, when I am supposed to. I separate the medications that need to be separated throughout the day. I apply my topical medications twice a day and avoid the sun. I get my infusions every week on time. I avoid crowded indoor places during flu season. My day is structured around my illnesses and it takes a lot of discipline to follow all the rules all the time. Sometimes I want some dairy with my medication, or some high noon sunlight. I would love to go wherever I wanted without fear of getting sick.
4. My body doesn’t always cooperate.
It’s not uncommon for me to end a sentence involving any plans I make with: “As long as I am feeling OK.” Actually, most plans I make with anyone do end this way. I never actually know how I will feel or what I can or can’t do until the actual day of the event. With any plan I make, I am secretly hoping I can keep my word. I never really know when a migraine, illness or just plain fatigue will kick in.
5. It can be lonely, scary and frustrating.
The winters are the worst. I spend a lot more time home alone afraid of catching a cold or flu. I want to get out and do things, and it can be super frustrating to pass up important opportunities or events I would like to attend because I am immune compromised and there are too many infections going around. It’s hard to always feel like you are missing out, or in some cases, missing friends and loved ones very much. You also don’t know fear until you have a rare disease. Just imagine not trusting that anyone, anywhere actually knows how to help you. Imagine there is little to no research for what you have. It is a lonely and scary situation to be in. I am so lucky to have a treatment for my primary immune deficiency disease; most rare conditions do not have an FDA-approved treatment. Mine is plasma derived, so there are shortages sometimes. It’s also extremely expensive. Indeed, there is a lot you can worry about.
6. It takes extraordinary courage to do “normal” everyday things.
Attending a function, or not running for the door when someone is sick is not easy for me. Even going to a doctor’s visit can take courage when you don’t know what germs are lurking in the waiting room and whether or not the appointment is going to get you sick. Visiting a school or hospital is another simple act that takes courage because of all the germs that can be there.
7. I carry with me the story of every friend I have lost to this disease.
I can’t even give you a number on how many brave and amazing friends I have lost. It’s that many. While I don’t share the details of their stories, theirs have undoubtedly shaped mine. It’s made me want to raise awareness and make things better for other patients. At the same time, I am struck with my own limitations and my own mortality. If only I could be a healthy person raising awareness. Instead, I am always one step forward and two steps back. My only hope is that my efforts make some small difference.
0 notes
Text
I Couldn’t Do it Without My Freedom Pump!
by Jessica Slade
I was diagnosed with CVID about five years ago. It was one of the happiest days of my life! Yep, you read that right. For the five previous years, from the time I turned thirty, my health had been declining rapidly...you know the drill...constant infections, then one disease diagnosis after another - Diabetes, Asthma, Cushing's Syndrome, Cholelithiasis, Interstitial Cystitis, crazy allergic reactions all of the sudden - you get the picture. I knew there was some underlying problem causing these other issues; doctors pretty much thought I was crazy when I told them that though. Or the few that believed me told me they couldn't help me. I was just too difficult a case for them.
The ironic thing is that after going to pretty much every kind of specialist you can imagine, a family doctor who practices just a few miles from my home is the one who listened to me, ran the proper tests, and figured things out.
I was immensely relieved and felt incredibly validated the day I was finally diagnosed! Not only that, but I also knew that help was on the way, in the form of immunoglobulin therapy! I had identified my enemy and I was strategizing against it.
When I was pregnant with my youngest, I had Hyperemesis Gravidarum. I was hooked up to an IV, confined to the sofa or the bed, basically miserable; but it's relevant to this story because I had a Zofran pump in my thigh for about six months, which gave me a point of comparison for the Freedom Pump.
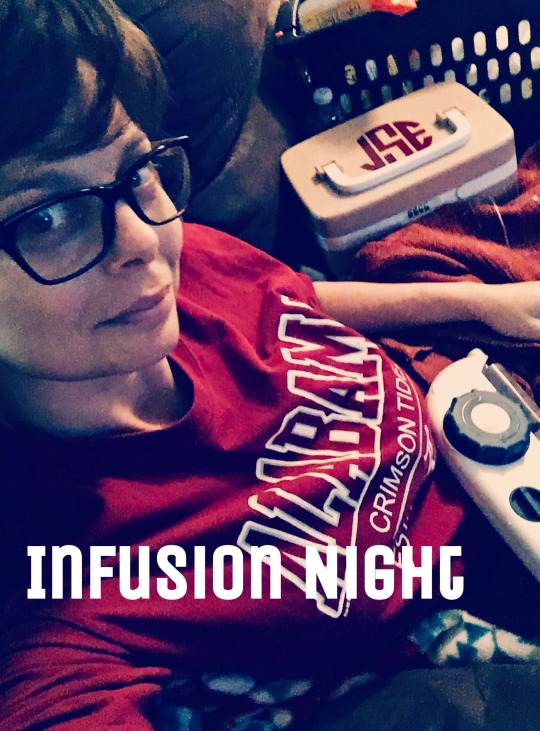
Here are the three main points I want to mention about the Freedom:
1. When I heard I could be trained to do the infusions myself, I was elated! I live all the way across the country from my extended family. And looking back on it, I am ever so grateful because it allowed me to get to spend precious time with my mother during the last two years of her life as she bravely fought Pancreatic Cancer. I wasn't restricted to a treatment schedule in Arizona; I could go to Atlanta and be with her when she needed me.
2. The pump I had when I was pregnant, as well as the chemo pump my mother had, may have been shorter than my Freedom Pump, but they were boxy and heavy, and they beeped all the time about something. I never got a good night's sleep with those pumps in the room. They were just a lot more upkeep.
3. My mother was also my RN and my best friend, and I was utterly devastated by her passing. I have always loved to travel, and now I use travel as therapy. I like to keep a trip on the horizon to look forward to so that I don't get depressed. I couldn't do that without my Freedom Pump.


The pump is so slim and easy to slip into a backpack or a carry on. Because there's no metal or batteries, there's no problem when sending it through a security checkpoint...in any airport. It's simple and easy to inspect.

A year ago, my two teenage daughters and I decided to go on an epic adventure. My friends were already living in Portugal, so that was our main area of concentration. We also went to Iceland (twice), Italy, and France.
To make a long story short, I brought everything else for my infusion, but somehow managed to set aside my Freedom Pump when packing and leave it at home. The memories of how I felt before I started immunoglobulin therapy began flooding back. I tried not to panic, and I started making phone calls to hospitals and pharmacies.

I was able to locate a pump, for which I was very grateful. The pump in Portugal was quite the dinosaur compared to my Freedom Pump though! I'm guessing it was about fifty years old and it weighed a little more than your average American house brick. We turned it on and it worked like the dinosaur it was, slow and sluggish, and stopped when there was one gram left in the syringe. But it got the job done, and I was able to carry on with the trip. I haven't forgotten my Freedom Pump since though, and won't again. It'll be with me at the Grand Canyon this summer!
Thanks for reading this tale of caution and woe,
Beware! Take your Freedom with you where'er you go!
-Jessica in Phoenix
0 notes
Text
With Freedom, Anything is Possible
Based on an interview with Cody Cowart; a CVID Patient using the RMS Freedom Infusion System.

Situated in Rocky Mountain National Park is Moraine Park, a unique valley formed by an ancient glacial lake that offers panoramic views of the surrounding mountain range and its snow-capped mountains. The air here is a crisp 38 degrees Fahrenheit and the silence of the meadow is broken only by the sound of Elk in the distance.

Venturing deeper inside Moraine Park is the campground where Cody, a 27 year old CVID patient, sits in front of a campfire infusing his medication, a cup of hot coffee in his hand, and his eyes fixed on the natural wonder before him. About halfway through his infusion, it starts to snow.

Cody was diagnosed with Common Variable Immune Deficiency (CVID) in August 2016. When asked whether his diagnosis had any effect on the way he approaches challenges, he said, “Absolutely not.” Although being diagnosed with CVID was a “gut punch” and took some adapting, Cody says, “CVID is just something I have to deal with once a week, and I keep moving forward.” Using RMS’ Freedom Infusion products, he infuses once a week, encounters zero site reactions, and “goes about [his] day as normal.”
Cody advises patients, “to not think of it as something you have to do. Think of it as something you get to do. I’m thankful I have the ability to infuse. It’s given me a much better quality of life.”

Cody started with SCIg infusions, using the RMS Freedom Infusion System, once he was diagnosed with CVID. “It’s super simple and user-friendly. The products are good quality and I haven’t had a single problem.”

RMS’ consistent patient-focused approach to primary immune disease maintains the highest quality of life standards. RMS supports and celebrates each and every patient, such as Cody, who epitomizes the courage and the vitality central to the slogan, “With Freedom, anything is possible.”
CLICK HERE for full interview.
0 notes
Text
“CVID Hasn’t Stopped Me from Doing Anything”
An Interview with Cody Cowart, a CVID Patient Using the RMS Freedom Infusion System.

1. Can you give us a short bio?
Hi, my name is Cody Cowart and I am 27 years old. I live in Central Florida. I’ve been married for almost 2 years and my wife has been a huge support through the whole process of being diagnosed with CVID. I love the outdoors and traveling. I am currently going to school to become a firefighter/emt and my goal is to get hired on with a department in 2019.
2. When were you diagnosed with CVID? Were you sick for a while before diagnosis? What was the process like?
I was diagnosed with CVID in August of 2016. For about a year leading up to diagnosis, I felt sick all the time. I was always extremely tired, and my knees and other joints would hurt for no reason. My workouts weren’t like they used to be and I would be extremely sore for longer than normal. I had no idea why or what was going on. It wasn’t until I was diagnosed that it all made sense. That explained why I was feeling sick, tired, grumpy, and just not 100% myself for so long.
3. Did you start with IV infusions? If so, what made you switch to subcutaneous immunoglobulin (SCIg)? Would you recommend SCIg to newly diagnosed patients over IVIg?
I did not start with IV. I have been infusing via (SCIg) from the beginning. I obviously don’t know how I would like IVIg, but I can tell you that after you get a good routine in place, SCIg goes very smoothly. I would recommend SCIg to new patients because it is a very simple process and easily administered to yourself.
4. What was your experience like with your infusion nurse?
My infusion nurse was great!! She was very knowledgeable and lived close by. She made the whole experience a lot easier. In the four visits I had with her, she taught me everything I needed to know, and I have been fine since then.
5. Have you always used RMS Freedom Infusion products or have you tried other brands?
I’ve always used RMS Freedom Infusion products and I’ve been happy with them.
6. Have you experienced any adverse events from infusions? (i.e. site irritation, drug leakage, itching?)
I have not experienced any adverse events. Each week I infuse early in the morning, then I go about my day like normal.
7. What is your experience with the Freedom Infusion System? Do you find it easy to use?
I like the Freedom Infusion System. It’s super simple and use friendly. The products are good quality and I haven’t had a single problem.
8. How often do you infuse?
I infuse once a week. Usually early Saturday or Sunday morning.
9. Do you travel? Where are some unique places you’ve infused?
I definitely travel as far and as often as possible. One of the coolest places I’ve infused would have to be Moraine Park inside the Rocky Mountain National Park located in Estes Park, Colorado. It was early, about 38 degrees outside and I was sitting in a camp chair next to the fire. I had amazing views of the Rocky Mountains and could hear the elk in the valley next to camp. About half way through my infusion, it started to snow. It didn’t bother me because I had hot coffee, and my wife & I planned to go hiking when I was finished. The following week, we were in Glacier National Park, and I did my infusions while sitting in our jeep watching the sun come up.
10. Do you have any tips for patients traveling with their Freedom system?
One tip I would suggest for patients traveling with their Freedom system is to make sure they keep their meds in a hard container so the glass doesn’t break and just keep it in your cooler. To warm mine up before infusing, I would get up an hour early, take the meds out of the cooler, and put them back in my sleeping bag with me. In my opinion, there’s no reason why you couldn’t travel anywhere and infuse along the way. I know I will be infusing on many more trips.
11. How has being diagnosed with CVID changed your perspective on life?
Being diagnosed with CVID was definitely a gut punch and a hard pill to swallow. After learning about it and starting treatment, it got a lot easier to deal with. Honestly, I’m glad CVID is all I have. I know it could be much worse. I still go about life just the same as I did before and that’s a blessing. CVID really showed me how fast life can change. I don’t take anything for granted anymore.
12. Do you think living with CVID has changed the way you approach or deal with challenges?
Absolutely not. To me, CVID is just something I have to deal with once a week, and I keep moving forward. I’m currently going to EMT school and will go right into Fire school after this. CVID can’t slow me down.
13. What advice would you give fellow PI patients?
My advice would be to not think of it as something you “have” to do. Think of it as something you “get” to do. I’m thankful I have the ability to infuse. It’s given me a much better quality of life. Also, get into a routine. Something you do every time you infuse. That way it just becomes habit.
14. What is your take on “With Freedom, Anything is Possible”
I agree 100%. CVID hasn’t stopped me from doing anything since I started my infusions with the Freedom Infusion system. I travel, hike, mountain bike, camp, and still do everything I want to do.
0 notes
Text
Questions for a PI Patient, from a PI Patient
by Joanna Tierno

Q. How can you become an active member of a PI Patient Community, as a way to help yourself and others?
A. There are so many ways to be an active part of the primary immune deficiency community. You can become a volunteer for the Immune Deficiency Foundation (IDF), attend events, participate in action alerts or simply join online groups. I am in over a dozen groups on Facebook and IDF has its own, so I can reach out to patients anytime. I also enjoy writing blogs and articles that I hope will help PI patients and their loved ones.

Q. As a patient, do you feel alone in this battle? Do you feel you should be doing more before and/or after treatment? What do you do with feelings of inadequacy and failure?
A. I have to say, early-on in my journey with primary immune deficiency disease I did feel very alone. For some time I literally felt like I was just about the only person in the world with this disease and all the problems that can come along with it. Then a shortage of immune globulin, which I was also experiencing, made the news and I realized there were many others like me. My feelings of being alone and that no one cared actually energized me to stand up a little for ALL primary immune deficiency patients. Slowly, I began to meet other patients online until I was finally introduced to the Immune Deficiency Foundation (IDF). I don't think I have felt alone since!
As for how I feel before and after treatment - I really take it on a day-to-day basis. I have days with a good amount of energy and I have days with next to none, where I can barely get out of bed. I have grown to accept it and to use my good days as best as I can. I try not to be hard on myself when I am having a difficult time. I am fighting a lot, after all! Getting others to understand continues to be a challenge.
As far as feeling inadequate, I try to appreciate all that I can do and all I have done. I have come a long way considering I was born with a disease that could kill me. I know you can achieve specific goals too. They may take you longer than you would like and you may have to modify them, but I feel that everyone can lead a life of purpose and achieve their goals. It’s a matter of prioritizing and taking it step-by-step until you get there. Oh, and don't let detours throw you off! Few roads to success are perfectly straight and we learn and grow from our mistakes and from our hardest times.

Q. What’s the best way to face life experiences such as school, physical activity, etc? Can you give advice on how to lead a better lifestyle?
A. One of the things that has helped me in school and in life has been to do my best to get ahead of everything possible while feeling well. Back in college, it meant reading all my assigned books sometimes even before the course began. On a daily level it may mean having my clothes planned out and medications packed and ready to go. Anything that can make your life easier when you inevitably will lose precious time because you are not feeling well. Procrastination and lack of preparedness is your enemy. Do what you can when you can.
On physical activity - I have always loved being active. If you haven't been active in a long time due to pain, injuries, fatigue or whatever, the best advise I have is to seek professional help, such as that of a physical therapist. They can help you safely get moving and set goals.
As for lifestyle, I believe in doing all you can to stay healthy. Eating nutritious foods is a great place to start. You can gradually replace one junk food item with a healthy treat. Learn new recipes, read ingredients and be mindful of what you are putting in your body. For long lasting improvement, your new lifestyle should to be sensible and one you enjoy. So no crash or fad diets - just better food choices that you can stick with long term.

Q. How can I be as "normal" as possible for my age, but still take care of myself? For example: I can never do things on Sundays, my one day off a week, because that's my infusion day. And during the week, I'm so run down, all I do is go to work, come home and crash. Then I wake up and do it all over again. What's the best way to take care of your mental health when your physical health is bad?
A. It’s not really “normal” to have a chronic illness when you are young. You are supposed to be healthy and full of energy when young, then slowly lose that vitality as you age. That is what our culture tells us, anyway.
If you are trying to keep up with your peers, you may not be able to without feeling too run down to take care of yourself. Is there anything in your schedule you can cut back on such as work hours? Or any way you can get more rest and free time? Will your boss allow you to do some of your work at home?
My best mental health tip is to accept yourself for who you are - health conditions and all. Then try to create a schedule that allows you the free time and rest you need to be feeling your best. I know this is easier said than done. You may lose some income or have to find a job closer to home or cut down on hours. You may need more support from family and friends. Talk with your doctor about how you are feeling. Maybe your medications can be tweaked so you are feeling a bit better.
Just remember this: DON’T blame yourself if you can't keep up with people your age who are not fighting a disease. Primary immune deficiency is not your fault or any reflection of your character or work ethic. It is part of you and you have to respect that - don't push yourself to do things you cannot handle.

0 notes