#simple squamous epithelial tissue
Text
i woke up from a dead sleep fever dream with this very important pre-med intrusive thought:
new tag yourself, assign you and the homies epithelial tissue (with or without cilia/microvilli)
tag yourself i'm simple squamous epithelial tissue
[I'm assigning my roommate ciliated pseudostratified columnar epithelial tissue]
#tag yourself#tag urself#meme#memes#medical memes#medical meme#medical tag yourself#medical tag urself#premed#pre-med#premedical#medical#tw medical#simple squamous epithelial tissue
3 notes
·
View notes
Text
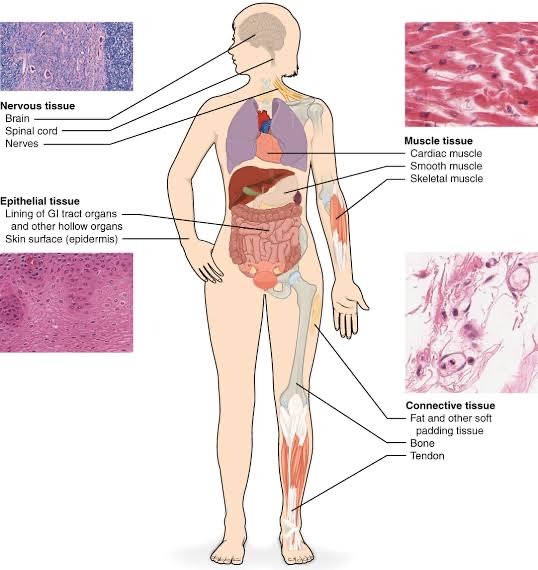
Human Tissues: An Anatomy and Physiology Exploration
In the captivating realm of human anatomy and physiology, tissues are the cornerstone, weaving the intricate tapestry of our bodily functions. Let's embark on a journey to uncover the different types of tissues, delving into their unique characteristics and significance.
1. Epithelial Tissue: The Body's Protective Shield
Epithelial tissue lines surfaces, cavities, and glands, acting as our first line of defense. Stratified, simple, squamous, cuboidal, and columnar epithelia all serve distinct functions in various bodily structures.
2. Connective Tissue: The Structural Framework
Connective tissues serve as the architectural scaffolding, binding and supporting other tissues. Dense, loose, cartilage, bone, and blood, each with its specialized properties, contribute to the body's structural integrity.
3. Muscle Tissue: The Engine of Movement
Muscle tissues are the driving force behind movement and force generation. Skeletal, smooth, and cardiac muscles exhibit unique characteristics and play crucial roles in our mobility and vital functions.
4. Nervous Tissue: The Information Superhighway
Nervous tissue conducts electrical impulses, facilitating rapid communication within the body. Neurons and neuroglia work in harmony to transmit and process vital information.
Diverse and specialized, these tissue types ensure the harmonious functioning of our body systems. Join us in this captivating journey through the pages of OpenStax Anatomy and Physiology to explore the intricacies of human biology. 📚🧬
Prepare to be captivated by the precise design and functionality of human tissues as we navigate the intricate world of anatomy and physiology! 📖🔬
References
OpenStax Anatomy and Physiology, Section 4.1
OpenStax Anatomy and Physiology, Section 4.2
OpenStax Anatomy and Physiology, Section 4.3
OpenStax Anatomy and Physiology, Section 4.4
OpenStax Anatomy and Physiology, available at https://openstax.org/details/books/anatomy-and-physiology.

#science#biology#college#education#school#student#medicine#doctors#healthcare#health#human physiology#humanphysiologynotes#human anatomy#anatomy#nursing#medical stuff
12 notes
·
View notes
Text
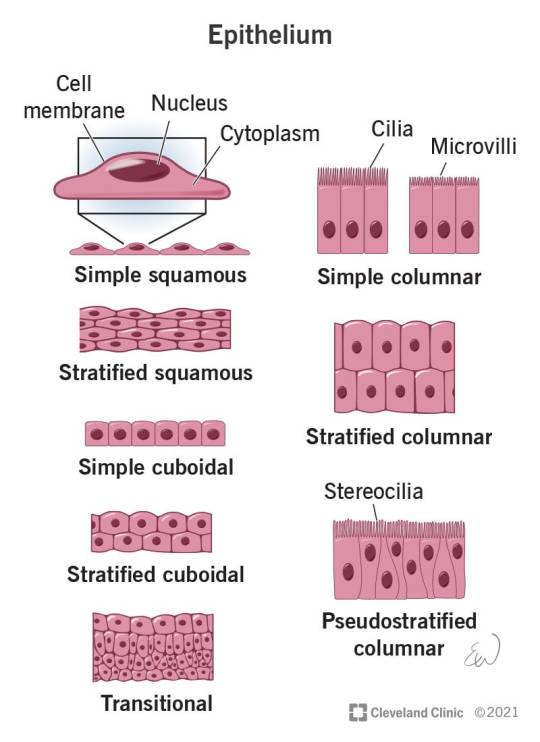
The Different Types of Epithelial Tissue
Epithelial tissue can be classified into several types based on its structure and function. Here are some of the different kinds of epithelial tissue:
Simple Squamous Epithelium:
Features a single layer of flattened cells.
Found in areas where diffusion and filtration occur, such as the lining of blood vessels (endothelium) and air sacs of the lungs (alveoli).
Simple Cuboidal Epithelium:
Consists of a single layer of cube-shaped cells.
Found in areas involved in secretion and absorption, such as kidney tubules and glands.
Simple Columnar Epithelium:
Composed of a single layer of column-shaped cells.
May contain specialized cells, such as goblet cells that secrete mucus.
Found in the lining of the digestive tract, where it aids in absorption and secretion.
Pseudostratified Columnar Epithelium:
Appears stratified but is actually a single layer of cells of varying heights.
Often contains cilia and goblet cells.
Found in the respiratory tract, where it helps in moving mucus and trapping foreign particles.
Stratified Squamous Epithelium:
Comprises multiple layers of flattened cells.
Provides protection against abrasion and forms the outer layer of the skin (epidermis) and lines the oral cavity, esophagus, vagina, and anal canal.
Transitional Epithelium:
Features multiple layers of cells that change shape when stretched.
Found in organs that undergo stretching, such as the urinary bladder, allowing it to accommodate varying volumes of fluid.
Stratified Cuboidal and Stratified Columnar Epithelium:
Less common types of epithelium.
Stratified cuboidal epithelium consists of two or more layers of cuboidal cells and is found in some ducts.
Stratified columnar epithelium consists of two or more layers of columnar cells and can be found in certain parts of the male urethra and large ducts of some glands.
These are just a few examples of the diverse epithelial tissues in the body. Each type is specialized for specific functions and locations within various organs and tissues.
2 notes
·
View notes
Text
Crash Course Anatomy & Physiology Notes, Tissues, Part 2
the body needs order to be able to function
epithelial tissue lines, covers, and organizes the body, creating order
proper epithelium - covers and lines the outer and inner body
glandular epithelium - forms your glands and secretes hormones and other substances
primary epithelium - protects the entire body, inside and out -covers the surface of the body when it combines with connective tissues to create skin -also lines the body cavities (pericardial, vertebral, cranial, thoracic, abdominal, and pelvic) and coats the internal and external walls of the organs
membranes covering the lungs are actually invaginations (the action or process being turned inside out or folded in on itself to form a cavity or pouch) of the epithelium
the epithelium does all this to protect your deeper layers of tissue from injury or infection
all epithelial tissues are avascular (not associated with or supplies by blood vessels), they rely on the blood supply of the supporting connective tissues around them or the materials they need
the three basic shapes of epithelial cells are the squamous, cuboidal, and columnar -squamous cells are flat, name means scale, the nucleus is flattened and easy to see, and they provide fast absorption and diffusion, and make thin membranes -cuboidal cells are cube-ish shaped, as tall as they are wide, the nucleus is circular, and they absorb nutrients and produce secretions like sweat -columnar cells are tall and thick and look like columns, the nuclei are stretched into an ellipse, and they cushion underlying tissues -the shape of each kind of epithelial cell correlates with its function
the tissue's first name is its number of layers, and its last name is the shape of the cells
layering of the cell also determines functions -simple epithelium has only one layer of cells -stratified epithelium has multiple layers set on top of each other -pseudo stratified epithelium is mostly just one layer, but the cells can be different shapes and sizes, and the nuclei can be at different levels
epithelial tissue regenerates really quickly
all of the epithelial cells are polar, meaning they have distinct sides -the apical (upper) side is exposed to either the outside of the body, or whatever internal cavity its lining -the basal (inner) side is tightly attached to the base membrane, a thin layer of mostly collagen fibers that helps hold the epithelium together, and anchors it to the connective tissue
many of the boundaries that the cells form aren't absolute, but instead selectively permeable, allowing for some form of absorption, filtration, and excretion of substances
glandular epithelium forms two different types of glands - the endocrine glands (secrete hormones right into your bloodstream or to nearby cells), and exocrine glands (secrete their juices into tubes or ducts that lead to the outside of the body or the inside of the tube)
#crash course#anatomy notes#anatomy#anatomy and physiology#crash course anatomy and physiology#crash course notes#hank green#science#science notes#tissues notes#tissues
15 notes
·
View notes
Text
Type 2 cells.
Alveoli are first located in the respiratory bronchioles that mark the beginning of the respiratory zone. They are located sparsely in these bronchioles, line the walls of the alveolar ducts, and are more numerous in the blind-ended alveolar sacs.[5] The acini are the basic units of respiration, with gas exchange taking place in all the alveoli present.[6] The alveolar membrane is the gas exchange surface, surrounded by a network of capillaries. Oxygen is diffused across the membrane into the capillaries and carbon dioxide is released from the capillaries into the alveoli to be breathed out.[7][8]
Alveoli are particular to mammalian lungs. Different structures are involved in gas exchange in other vertebrates.[9]
Structure
Bronchial anatomy showing terminal bronchioles (BT) leading to respiratory bronchioles (BR) and alveolar ducts (DA) that open into alveolar sacs containing out pockets of alveoli (A) separated by alveolar septa (AS).
The alveoli are first located in the respiratory bronchioles as scattered outpockets, extending from their lumens. The respiratory bronchioles run for considerable lengths and become increasingly alveolated with side branches of alveolar ducts that become deeply lined with alveoli. The ducts number between two and eleven from each bronchiole.[10] Each duct opens into five or six alveolar sacs into which clusters of alveoli open.
Each terminal respiratory unit is called an acinus and consists of the respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli. New alveoli continue to form until the age of eight years.[5]
A typical pair of human lungs contains about 480 million alveoli,[11] providing a total surface area for gas exchange of between 70 and 80 square metres.[10] Each alveolus is wrapped in a fine mesh of capillaries covering about 70% of its area.[12] The diameter of an alveolus is between 200 and 500 μm.[12]
Microanatomy
An alveolus consists of an epithelial layer of simple squamous epithelium (very thin, flattened cells),[13] and an extracellular matrix surrounded by capillaries. The epithelial lining is part of the alveolar membrane, also known as the respiratory membrane, that allows the exchange of gases. The membrane has several layers – a layer of alveolar lining fluid that contains surfactant, the epithelial layer and its basement membrane; a thin interstitial space between the epithelial lining and the capillary membrane; a capillary basement membrane that often fuses with the alveolar basement membrane, and the capillary endothelial membrane. The whole membrane however is only between 0.2 μm at its thinnest part and 0.6 μm at its thickest.[14]
In the alveolar walls there are interconnecting air passages between the alveoli known as the pores of Kohn. The alveolar septum that separates the alveoli in the alveolar sac contains some collagen fibers and elastic fibers. The septa also house the enmeshed capillary network that surrounds each alveolus.[3] The elastic fibres allow the alveoli to stretch when they fill with air during inhalation. They then spring back during exhalation in order to expel the carbon dioxide-rich air. A histologic slide of a human alveolar sac
There are three major types of alveolar cell. Two types are pneumocytes or pneumonocytes known as type I and type II cells found in the alveolar wall, and a large phagocytic cell known as an alveolar macrophage that moves about in the lumens of the alveoli, and in the connective tissue between them. Type I cells, also called type I pneumocytes, or type I alveolar cells, are squamous, thin and flat and form the structure of the alveoli. Type II cells, also called type II pneumocytes or type II alveolar cells, release pulmonary surfactant to lower surface tension, and can also differentiate to replace damaged type I cells.[12][15]
Development
Development of the earliest structures that will contain alveoli begins on day 22 and is divided into five stages: embryonic, pseudoglandular, canalicular, saccular, and alveolar stage.[16] The alveolar stage begins approximately 36 weeks into development. Immature alveoli appear as bulges from the sacculi which invade the primary septa. As the sacculi develop, the protrusions in the primary septa become larger; new septations are longer and thinner and are known as secondary septa.[16] Secondary septa are responsible for the final division of the sacculi into alveoli. Majority of alveolar division occurs within the first 6 months but continue to develop until 3 years of age. To create a thinner diffusion barrier, the double-layer capillary network fuse into one network, each one closely associated with two alveoli as they develop.[16]
In the first three years of life, the enlargement of lungs is a consequence of the increasing number of alveoli; after this point, both the number and size of alveoli increases until the development of lungs finishes at approximately 8 years of age.[16]
Function
An annotated diagram of the alveolus
Type I cells
The cross section of an alveolus with capillaries is shown. Part of the cross section is magnified to show diffusion of oxygen gas and carbon dioxide through type I cells and capillary cells. Gas exchange in the alveolus.
Type I cells are the larger of the two cell types; they are thin, flat epithelial lining cells (membranous pneumocytes), that form the structure of the alveoli.[3] They are squamous (giving more surface area to each cell) and have long cytoplasmic extensions that cover more than 95% of the alveolar surface.[12][17]
Type I cells are involved in the process of gas exchange between the alveoli and blood. These cells are extremely thin – sometimes only 25 nm – the electron microscope was needed to prove that all alveoli are lined with epithelium. This thin lining enables a fast diffusion of gas exchange between the air in the alveoli and the blood in the surrounding capillaries.
The nucleus of a type I cell occupies a large area of free cytoplasm and its organelles are clustered around it reducing the thickness of the cell. This also keeps the thickness of the blood-air barrier reduced to a minimum.
The cytoplasm in the thin portion contains pinocytotic vesicles which may play a role in the removal of small particulate contaminants from the outer surface. In addition to desmosomes, all type I alveolar cells have occluding junctions that prevent the leakage of tissue fluid into the alveolar air space.
The relatively low solubility (and hence rate of diffusion) of oxygen, necessitates the large internal surface area (about 80 square m [96 square yards]) and very thin walls of the alveoli. Weaving between the capillaries and helping to support them is an extracellular matrix, a meshlike fabric of elastic and collagenous fibres. The collagen fibres, being more rigid, give the wall firmness, while the elastic fibres permit expansion and contraction of the walls during breathing.
Type I pneumocytes are unable to replicate and are susceptible to toxic insults. In the event of damage, type II cells can proliferate and differentiate into type I cells to compensate.[18]
Type II cells
External links
0 notes
Text
Epithelial Tissue: Structure with Diagram, Function, Types and Location
0 notes
Text
Epithelial Tissue: Structure with Diagram, Function, Types and Location
0 notes
Text
Epithelial Tissue: Structure with Diagram, Function, Types and Location
0 notes
Text
Three types of tissue shapes for epithelial tissues:
Squamous (flat fucks)
Cuboidal (stout fucks)
Columnar (tall fucks)
Usually, they are either simple (meaning single layer) or stratified (multiple layers)
In the diagram that ma'am showed us, pseudostratified (looks like it has multiple layers, but is actually single layer) is only in columnar tissues, but I have been curious if pseudostratified is also among cuboidal and squamous tissues
0 notes
Text
Class 9 Science Notes Chapter 6 Tissues

Tissues Class9 Notes - Here are the summary and revision notes to Class 9 Science Chapter 6. This CBSE notes includes CBSE Key Notes and CBSE Revision Notices. It also contains images and diagrams of the complete Chapter 6 titled Tissues of Science. The Chapter 6 Tissues is for students in class 9. Once you have completed a lesson, you will want to look for notes to help you remember it. You can find complete Chapter 6 Tissues class 9 notes here. You should also see, Gravitation class 11 notes.
Tissues
Tissues are defined as a group of cells with a common origin and similar functions.
A. Plant tissues:
Meristematic tissues
Permanent tissues
1. Meristematic tissue: These tissues consist of actively-dividing cells. Three types of Meristematic tissues exist:
Apical Meristem: Found at the growth tips of stems or roots. Important function: To increase length of roots and stems.
Intercalary meristem is found at the base of internodes or leaves. Important function: Responsible for the growth of plants in a longitudinal direction.
Lateral Meristem: Found on the lateral sides and ends of the roots and stems. Important function: To increase stem and root thickness.
2. Permanent tissues: These tissues are made from meristematic materials and the cells have lost the ability of division. Permanent tissues are classified into two groups:
Only one type of cells make up the simple permanent tissue.
Types of simple permanent tissues:
Parenchyma: composed of unspecialised living cells, with thin cell walls and intercellular space. It is found in soft parts. Their primary function is storage.
Collenchyma: Collenchyma consists of living, elongated cell bodies with irregularly thickened cell walls at the comers. No intercellular space. It provides mechanical support to plants and elasticity. It assists in the bend of stems.
Sclerenchyma: A collection of thick-walled, long-walled cells. This tissue is comprised of dead cells. Intercellular spaces are absent. Sclerenchyma cells, which are found in seeds, nuts, husks of coconuts, fibers of hemp, etc., are dead.
Complex permanent tissue (Conducting tissue): Comprised of multiple types cells.
Types of complex permanent tissue:
Also read, Magnetic Effects of Electric Current Notes.
Xylem is a conductor of water and minerals between the roots and the different parts.
It is made up of four types cells: vessels (tracheids), vessels (xylem parenchyma), and xylem fibers (xylem fibres).
Phloem is a method of transporting food material from the leaves to various parts of the plant.
It is made up of four types cells, sive tubes, companion cells and phloem fibers.
Protective tissue: It is composed of a single layer. E.g., epidermis. The epidermis of a leaf bears stomata.
B. Animal tissues: Animal tissues are classified into four types based on the functions they perform:
Epithelial
Connective
Muscular
Nervous
Epithelial tissue: Covers the exterior surfaces, internal cavities, and organs in the animal's body. There are several types of epithelial tissues:
Simple squamous epithelium - Single layer of flat cells.
Localization in the human body : Lining of mouth, oesophagus or lung.
Cuboidal epithelium: Consists of cube-like cells.
The location of the human body: Lining the kidney tubules, and the ducts of salivary glands. Its function is secretion or absorption.
Columnar epithelium - Consists of column-shaped cells or elongated cells.
The location of the human body: The inner lining of the gut and intestine. Its function includes secretion, absorption.
Connective tissues are those that connect to various organs. There are several types of connective tissues available:
Areolar tissue is found in the skin and around the blood vessels.
Adipose tissues: Stores fats between the organs and the skin. They also act as insulation.
Dense regular connective tissues: Main components are the tendons and ligaments. Tendons connect bones to bones while ligaments link two bones together.
Skeletal tissue - The two main components of skeletal tissues include cartilage and bone.
Fluid tissue: This is the vascular tissue found in animals.
Muscular tissues: Muscular tissues are responsible for providing movement to the body. Three types of muscle tissues exist:
Striated muscles, skeletal muscle or voluntary muscles: Cells have a cylindrical shape and are unbranched and multinucleate.
Smooth muscles or involuntary ones: Cells can be long, spindle-shaped, and have a single nucleus.
Cardiac muscles, or involuntary muscular: Cells are cylindrical and branched.
Nervous tissues are found in the brain and spinal cord.
Neuron: Nervous tissue cells.
A neuron: It is composed of a cell, an axon, and a dendrite.
0 notes
Text
Anatomy stresses me out thank you gn
#if youve taken anatomy youd understand#idc about tissues#simple squamous epithelial my ass#statified columnar bs#idc#let me just enjoy the cardiovascular system#pls and thank you
2 notes
·
View notes
Video
This sqadia.com short video clip is a brief explanation of Epithelium.
Epithelium is one of the four basic tissues of the body and is derived from all three germ layers.
It is composed of very closely packed, contiguous cells, with very little or no extracellular material in the extracellular spaces.
Epithelial membranes can be: Simple squamous epithelium, Simple cuboidal epithelium, Simple columnar epithelium, and Pseudostratified epithelium.
When there are two or more layers of cells epithelia is referred to as stratified, hence can be stratified squamous, stratified cuboidal and stratified columnar.
#medical school#medical#medical video#medical animation#human anatomy#anatomy#histology anatomy#histology online lecture#histology video#histology video education#Histology#medical student#medical students#medical study#medical student education#medical histology
1 note
·
View note
Text
The Four Primary Tissue Types
The four primary tissue types in the human body are epithelial tissue, connective tissue, muscle tissue, and nervous tissue. Each tissue type has distinct features and functions. Here's an overview of each tissue type and its characteristics:
Epithelial Tissue:
Location: Covers the body surfaces, lines body cavities, and forms glands.
Features:
Composed of tightly packed cells arranged in continuous sheets.
Cells are closely joined together with little extracellular matrix.
Forms protective barriers, absorbs nutrients, and secretes substances.
Exhibits different cell shapes (squamous, cuboidal, columnar) and layering arrangements (simple, stratified, pseudostratified).
Connective Tissue:
Location: Found throughout the body, supporting and connecting other tissues.
Features:
Consists of cells scattered within abundant extracellular matrix.
Matrix can be solid, semisolid, or fluid, depending on the type of connective tissue.
Provides structural support, connects and binds tissues/organs, stores energy, and transports materials.
Includes various types like loose connective tissue, dense connective tissue, adipose tissue, cartilage, bone, blood, and more.
Muscle Tissue:
Location: Found in muscles throughout the body.
Features:
Composed of specialized cells called muscle fibers.
Exhibits contractility, allowing for movement and force generation.
Three types: skeletal muscle (attached to bones, voluntary control), smooth muscle (involuntary, found in organs and blood vessels), and cardiac muscle (involuntary, found in the heart).
Possesses a highly organized arrangement of actin and myosin filaments responsible for muscle contractions.
Nervous Tissue:
Location: Found in the brain, spinal cord, and peripheral nerves.
Features:
Composed of specialized cells called neurons and supporting cells called neuroglia.
Neurons transmit electrical impulses, allowing for rapid communication.
Neuroglia support and protect neurons.
Forms complex networks and controls functions such as sensation, movement, and cognition.
These tissue types work together to form organs and carry out various physiological functions within the body.
0 notes
Text
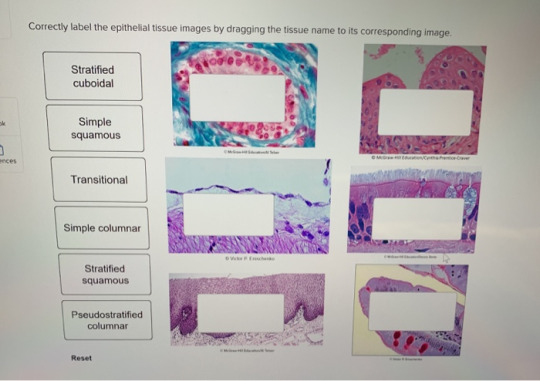
Correctly label the epithelial tissue images by dragging the tissue name to its corresponding image
Correctly label the epithelial tissue images by dragging the tissue name to its corresponding image
Correctly label the epithelial tissue images by dragging the tissue name to its corresponding image. Stratified cuboidal Simple squamous ences Transitional 000 Simple columnar Stratified squamous Pseudostratified columnar Reset
View On WordPress
0 notes
Text
Circumcision or Preputialplasty in Children with Phimosis: What is the Evidence? by Pan P in International Journal of Clinical Studies & Medical Case Reports

Short Communication
Circumcision is one of the oldest and undoubtedly one of the world's most common surgical procedures. The circumcision is done for religious, ritual and cultural reasons. The common medical indications for circumcision include phimosis, paraphimosis, trauma, recurrent skin infections and lesions. Embryologically the prepuce appears as a ring of thickened epidermis within the fetus penis at eight weeks, which develops from the coronal sulcus and proceed towards the tip of the glans by 16 weeks [1]. At this stage, the epidermis of the deep surface of the prepuce and the epidermis of the glans is fused. The preputial space is formed by process of desquamation [2]. The squamous cells assemble into whorls, creating nests of epithelial cells. The centres of these degenerate, thereby forming a sequence of spaces. Progressively they join up, as they increase in size until a continuous preputial space is finally created. At the time of birth, the prepuce is still forming and incomplete separation renders it non-retractable. This natural tightness of prepuce is misdiagnosed as phimosis. It is merely a typical evolutionary period. Some boys present with preputial ballooning. It is due to collection of urine between prepuce and glans where prepuce's inner layer has separated from the glans but the prepuce is not completely retractable. Ballooning is a temporary phenomenon. Babu et al found no interference in voiding due to ballooning and is not an indication for circumcision [3]. Physiologic phimosis is the rule in newborn males due to flimsy adhesions between glans and prepuce. The adhesion to glans and prepuce separates over time reducing to 50% at the age of two and to 8 % by seven years. This incidence is reduced to 1% by eighteen years [1, 4]. According to Wright, in infancy and early childhood, the prepuce is intended to be non-retractable when developing glans need protection from mechanical injury due to clothing and chemical trauma of ammonic urine [5]. The physiological role of a foreskin is being acknowledged progressively bringing several alternative techniques in use to treat phimosis. It undoubtedly protects the sensitive glans, provides lubrication and allows greater freedom of movement during sexual intercourse [6]. Enthusiastic efforts to retract the foreskin in physiological phimosis causes micro tears, infection, and bleeding with secondary scarring. Poor hygiene and recurrent balanoposthitis lead to the development of true phimosis [7]. Pathological phimosis is a quite rare condition marked a whitish ring of hardened tissue on the tip of prepuce. Currently, surgery of phimosis is conducted through two types of procedures: a) circumcision and b) preputialplasty. In children with phimosis, preputialplasty represents a surgical alternative to time honoured circumcision, which is associated with many functional and physiologic complications, trouble, and risks [8, 9]. Complications like hemorrhage, edema, infection, meatal stenosis, urethral fistulae, unsightly scars, penile curvature, shortness of shaft skin, and partial, or total penile loss all being noted after circumcision [10]. Preputialplasty is a conservative surgical technique as compared to classical circumcision for the treatment of phimosis. Preputialplasty broadens the preputial meatus to permit its simple withdrawal and better cleanliness while maintaining the typical cosmetic appearance of the penis. In subsequent years, different varieties of preputialplasty, such as V-flap and Z-flap repair, triple incision plasty, and multiple YV plasty, limited dorsal slit preputialplasty have been proposed with good functional results [11]. The results of previously reported studies in children undergoing preputialplasty showed a functional and cosmetic satisfaction rate of 77%-97.6% [12, 13]. Cuckow et al compared with circumcision and reported preputialplasty is associated with few complications and good functional and cosmetic results, provided the prepuce is mobilized regularly after surgery [14]. Circumcision occurs to be the most regularly performed procedure globally but there are reasonable reasons to avoid circumcision given the evidence available today. The preputialplasty is a safe surgical treatment for phimosis in children. It preserves the prepuce and has low complication rate. It expresses a good alternative to circumcision.
Message
Overenthusiastic preputial retraction is not advised in children.
Preputialplasty is safe, day care surgical procedure.
It preserves the prepuce and has an excellent cosmetic and functional outcome.
For more information about Journal :
https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/pdf/IJCMCR.SC.ID.00007.pdf
https://ijclinmedcasereports.com/ijcmcr-sc-id-00007/
0 notes
Text
Quiz Review #2: The PAS/PASD Stain
bout that time again ay chaps. right oh. big ol wall of text under the cut, let’s get at it
Alright so sometimes in the course of a patient’s disease, they’re either going to have carbohydrates end up in tissues that aren’t meant to store them or have too few carbohydrates in places where they ought to be. A handy test for this is the Periodic Acid-Schiff test and/or the Periodic Acid Schiff with Diastase digestion. This isn’t to say that the PAS/D is a strict presence/absence test but it gets used that way fairly often depending on the case.
First things first: What’s a carbohydrate? Well that’s a big chemistry question and if we wanted to deal with that mess we’d have gone to grad school. For the purposes of the HTL this post, carbohydrates are organic compounds such as sugars, starches, cellulose and polymers that are typically bound to proteins found in tissue. When we eat food, we break the complex sugars down into simple sugars such as glucose. What we don’t immediately use we store as glycogen. This glycogen *generally* should be found within liver and skeletal muscle tissue, specifically within the cytoplasm of those cells.
Disease and uses- A healthy liver should be able to store glycogen up and release it as the body’s demand for it changes. We can use the PAS/D to look at how much glycogen the liver has and where that glycogen is within the liver. Most of the disease you’ll see in medical histology regarding glycogen storage disorders are congenital and fatal. A good example is Pompe’s disease, in which the patient has a mutation that causes them to be unable to convert glycogen back into glucose, causing an over-accumulation of glycogen within the skeletal muscle, cardiac muscle and liver; most people born with Pompe’s disease will die in less than a year. Other illnesses that effect glycogen storage are diabetes (low glycogen in the liver) and certain wasting disease. There are also some applications for differentiating tumor types on the oncology end of things; for instance you can use the PAS to differentiate secreting adenocarcinomas (should be PAS positive) from undifferentiated squamous cell carcinomas (should be PAS negative). I am told that these days we would use an immuno stain to answer this question but, you know, half of histology is actually Arcane Medical History so whatever. My favorite application of the PAS, however- one that could have saved my undergrad research project had I known what the hell I was doing but that’s another topic for another day- is its ability to stain for fungal cell walls. Fungal cell walls are made of chitin, a complex carbohydrate that stains nicely with PAS. Some of the techs in my current lab will automatically order PAS along with any silver stains they get on a suspected fungal case, just because it’s a nice way of double checking (especially if you’re looking at tissues with lots of argentaffin/argyrophil structures where the fungi could be obscured other things).
Fixation- now if you’re in a hospital, chances are you’re just going to throw the tissue in question into a bucket for formalin and be done with it. And that’s not necessarily bad; tissue slated for PAS can be fixed in either aqueous or alcoholic solutions. Just remember that structurally, the carbohydrates you’re testing for are bound to the tissue proteins, so the faster you preserve those proteins the more honest and indicative the results of your PAS will be. If you know that this tissue is going to have to wait a while before going to processing, go for alcohol if you can. Formalin and most other aqueous fixatives will slowly leach glycogen from tissue because glycogen is water soluble. Of some note to pathologists, glycogen degrades rapidly postmortem, so get that liver out of there and into some sort of fixative asap of you’ll be missing that particular piece of the puzzle. The only real fixatives to avoid are those containing chromate, since these may over oxidize the tissue and result in a weak stain or cause resistance the diastase digestion in the PASD.
Reagents and their purposes- Fairly straight forward.
Periodic acid, aqueous, 0.5%. This will act as your oxidizer. It opens up ‘certain tissue elements’ (nice dodge, Frieda) and exposes aldehydes such as 1,2 glycol groups. At this concentration periodic acid probably will not burn you to death if you spill it on yourself but you should be extremely careful when preparing it from concentrate (under a hood, wearing goggles and gloves, full weenie regalia required, this is not fun stuff to get in your eyes). Remember: acid into water is the way that you oughta. Dispose of with lots of water down the sink.
Schiff Reagent. This stuff is N A S T Y but you gotta use it. It binds to the aldehyde groups exposed by the periodic acid and forms an intermediate colorless compound known as leucofuchsin. Schiff’s contains sodium metabisulfite, hydrochloric acid and basic fuchsin. Basic fuchsin is classified as a known carcinogen by OSHA so you need to make and use schiff’s under a fume hood whenever possible; most labs i have been in are not good about this and some even heat their shiff’s in a microwave, which causes techs to breath in even more vapors. Most labs need to dispose of used solution via a licensed waste hauler; do not flush down the sink.
Sodium metabisulfite, aqueous, 10%. This will remove any excess schiff’s that’s hanging onto the tissue and prevent overstaining. At 10% it’s not horribly dangerous but it is a strong reducing agent and if you’re preparing it from powder you should do your mixing under the hood. dispose of down the sink with lots of water.
Alum hematoxylin (counterstain). This is just hematoxylin that contains alcohol. Normal alcohol precautions apply (ie it’s slightly flammable and skin/eye irritant; normal ppe is fine). Dispose of down the sink.
How it works, step by step:
First- are you doing a PAS or a PASD? If you’re doing a PAS, start at step 2. For a PASD, start here. You need some way to chop up the glycogen in your section, and that’s a job for an enzyme. Once upon a time we used malt disatase to do this, which is a mix of a bunch of different amylases. If possible, you should use alpha amylase because it’s the most specific enzyme for glycogen, aka your target. Now, if you’re anything like my lab, you have chill pathologists and cheap administrators, so what you gotta do is think real hard about sour candy and go ahead and just spit on the slide. I’m dead serious. You have perfectly good amylase in your spit, and on the off chance that you have free cells in your mouth the pathologist should be able to figure out what doesn’t belong to the patient tissue; it’s a thing that’s done. The first time I saw my instructor do it I almost walked out of the lab but. you know. When in Rome. We usually let ours digest for about 20 minutes, rinse real well in DI and then add the slides to the PAS group for the rest of the procedure.
oxidize your tissue with periodic acid. We use periodic acid because it’s not going to over-oxidize the aldehyde groups it creates when it opens the c-c bonds in the sugars.
add schiff reagent. it will bind to the aldehyde groups creating an unstable, colorless compound (leucofuchsin) that resembles a partially opened ring. When you run warm water over the slide, the ring will close and this creates the colored reaction product (pink).
rinse in sodium metabisulfate. some labs omit this step to save time/money and some labs do get good results just by rinsing for extra time in water but you’re better safe than sorry. Sodium metabisulfate should remove any excess schiff reagent.
counterstain with hematoxylin. My instructor told me that some labs use fast green instead. I’ve never seen it done before but it strikes me as a good idea (who wants to look at a bunch of pink/purple on top of the schiff reaction? not me).
Other important details:
Controls should be kidney (specifically the golmeruli and basement membranes) if you’re doing PAS and Liver if you’re doing PASD.
Good results should show glycogen, neutral mucosubstances, epithelial sulfomucin and sialomucins, colloid, basment membranes and fungal cell walls. They will appear ‘bright rose’ (aka pink).
A PAS and a PASD of the same tissue slides run in the same batch should be loose negative images of eachother; this is to say, the PAS will show the presence of glycogen in the section, while the PASD will show what the tissue looks like once that glycogen is digested away. This is not to say that a PASD is necesarily PAS negative, but rather that a PASD will show any PAS positive substances that are NOT glycogen.
Before you use your schiff reagent you want to test it for freshness. Do this by pouring a small beaker (10ml should do) of formalin. Drip a few drops of schiff into the beaker. If it’s good to use, you’ll see a red to purple color. If it’s degraded, you’ll get a delayed reaction and an eventual dark purple to deep blue color. This a good test but remember: when it doubt, throw it out. It’s not worth having to repeat a day’s worth of PAS/Ds just because you don’t want to take ten minutes to make your reagents properly.
Calling back to last week’s quiz on water quality, PAS procedures have been known to fail if the water you’re using to rinse is heavily chlorinated, since the chlorine can oxidize the schiff reagent and turn it back into basic fuchsin, giving you a false negative. I’m not sure what constitutes ‘heavily chlorinated’ but I figure you’d probably smell it and say, you know, maybe i shouldn’t put this precious sample into this nasty water and go talk to my supervisor before i ruin this poor sick person’s life.
What-if list:
no PAS/D reaction occurs at all, including control- check your periodic acid. If oxidation fails, so does everything after it.
faint of pale staining-you probably cut the tissue too thin. This is a little counter-intuitive but the thicker the section is, the less time you will need to stain it for in PAS/D. My theory is that staining time is strictly is a function of quantity of glycogen, and quantity of glycogen should go up with section thickness. There’s biochemistry afoot here but my ochem-failing-self is ill-equipped to suss this one out. have at it, you nerds.
you still see glycogen on a PASD- give it more time in amylase and keep it around 37C. If you’re heating your slide too high you can degrade your enzymes (remember, most enzymes used in the clinical setting work at body temperature. Don’t go above that if you can help it).
you have weird glycogen looking artifacts in places where glycogen 100% can’t be-should have used some kind of sulfurous rinse. this is what you get for cutting corners and being a cheapskate. are you happy now. look at your life, look at your choices.
Alright that’s all for now. My instructor is traveling this week so I don’t know if I’ll have a quiz next monday but I’ll keep you posted.
Peace!
-Reby
#this has been an Apology Original#Quiz review#special stains series#periodic acid schiff#PAS#PASD#histology#special stains
3 notes
·
View notes