#medicineresidency
Photo
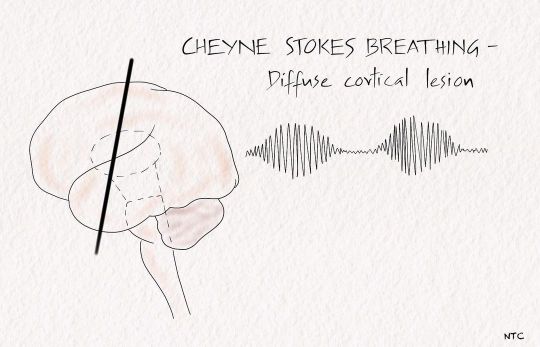
Respiratory abnormalities in coma. The full details are available in episode 13 of ‘Clinical neurology with KD’ podcast. Cheyne -stokes breathing. There are brief periods of hyperpnoea regularly alternating with an even shorter duration of apnoea. After the apneic phase, respiratory movement's amplitude increases to a peak before slowly waning off to the following apnea. It represents a more severe degree of normal post-hyperventilation apnea due to bilateral cortical dysfunction. Brainstem hyperventilation Patients with midbrain and pontine lesions can have rapid and prolonged hyperventilation. Lowering the local CSF pH and stimulating the respiratory centre of the medulla is one of the postulated mechanisms. Kussmaul's breathing is deep, rapid breathing seen in metabolic acidosis. Apneustic breathing In apneustic breathing, there is a prolonged inspiratory time followed by a long inspiratory pause. The air is retained for several seconds and released. The expiratory time is short, and a pontine lesion usually causes it. Cluster breathing It is a cluster of breaths following each other in an irregular sequence. It results from low pontine or high medullary lesions. Ataxic breathing The breathing pattern is entirely irregular. It is called the atrial fibrillation of breathing. The inspiration is of different amplitudes and lengths and intermixed with variable periods of apnea. It is often seen in terminally ill patients and suggests impending respiratory failure. The site of the lesion is the dorsomedial medulla. A paramedian medullary infarct, bleed, or tumour can produce it. The classical breathing described by Biot in severe meningitis is ataxic. Central hypoventilation The pathway of voluntary respiration from the cortex descends via the corticospinal tract. The automatic respiration fibres from the medulla descend in the ventrolateral cord, with anatomic separation of inspiratory and expiratory pathways. #neurology #neuroscience #coma #emergencymedicine #criticalcare #internalmedicine #neuro #neurologyteachingclub #clinicalneurology #respiration #respiratorymedicine #neurocriticalcare #neuroresident #medicineresidency #neetss https://www.instagram.com/p/ChEkwNAvGSl/?igshid=NGJjMDIxMWI=
#neurology#neuroscience#coma#emergencymedicine#criticalcare#internalmedicine#neuro#neurologyteachingclub#clinicalneurology#respiration#respiratorymedicine#neurocriticalcare#neuroresident#medicineresidency#neetss
0 notes
Photo

Sheldon M. Hoxie, MD comes to EliteCare Health Centers from completing his internal medicineresidency at HCA USF Morsani College of Medicine’s GME program at Citrus Memorial Hospital.
0 notes
Photo

Today Facebook reminded me of something: 7 years ago to the day, I began my med school journey and the commitment to my eventual profession. I didn’t know what this road would involve, the stress, the sacrifice, and the tears. I also couldn’t have anticipated the joy, excitement, knowledge, friendships, and the satisfaction of caring for others I would gain. It’s not easy, but as residency draws to an end and hematology/oncology fellowship draws near, I’m stand without regrets. #CantStopWontStop

#medicalschool#fellowship#hematologyoncology#womeninmedicine#thisiswhatyoudoctorlookslike#issathrowback#medicineresidency#doctor#medschool#medicine
1 note
·
View note
Text
Watch "#Doctor reacts: the pay gap" on YouTube
😂😂😂😂
1 note
·
View note
Text
HCSM Resource
Social Media Responses to the Annals of Emergency MedicineResidents’ Perspective Article on Multiple Mini-… https://t.co/OogVAaSPGf #hcsmR http://pic.twitter.com/IBq0TRUejm
— Symplur (@symplur) June 16, 2017
0 notes
Photo
Neurology teaching club case presentation on clubhouse at 8 PM IST on 03/07/2022. A patient who could not recognise faces. #prosopagnosia #neurology #neuroscience #neurologyresident #neuroeducation #medicalstudent #medicaleducation #dementia #internalmedicineresidency #internalmedicine #bedsideteaching #clinicalcasediscussion #neurosurgery #medico #medicineresidency #medicineresidents https://www.instagram.com/p/CfijPGzLfPI/?igshid=NGJjMDIxMWI=
#prosopagnosia#neurology#neuroscience#neurologyresident#neuroeducation#medicalstudent#medicaleducation#dementia#internalmedicineresidency#internalmedicine#bedsideteaching#clinicalcasediscussion#neurosurgery#medico#medicineresidency#medicineresidents
0 notes
Photo
In this episode, we will discuss the anatomy and physiology of the basal ganglia. We will learn how to approach a patient with parkinsonism, one of the most common movement disorders. For notes and images of the episode, visit neurologyteachingclub.com. #neurology #neuroscience #neuro #internal medicine #medicalpodcast #emergencymedicine #emergencymedicineresidency #criticalcaremedicine #criticalcarenurse #movementdisorder #basalganglia #parkinsonism #ntc #neurologyteachingclub #neuroanatomy #neurophysiology #physiotherapy #physiatry #neuronurse #mbbs #medicos #generalpractitioner #medicineresidency #neurorehabilitacion #neuroresidency https://www.instagram.com/p/CeQQXhoLwm-/?igshid=NGJjMDIxMWI=
#neurology#neuroscience#neuro#internal#medicalpodcast#emergencymedicine#emergencymedicineresidency#criticalcaremedicine#criticalcarenurse#movementdisorder#basalganglia#parkinsonism#ntc#neurologyteachingclub#neuroanatomy#neurophysiology#physiotherapy#physiatry#neuronurse#mbbs#medicos#generalpractitioner#medicineresidency#neurorehabilitacion#neuroresidency
0 notes
Photo
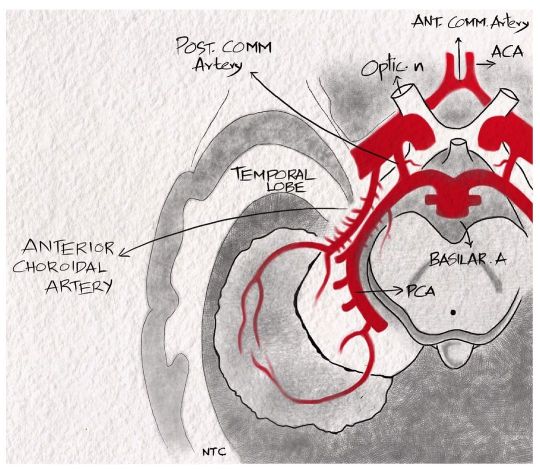
Anterior choroidal artery For discussion of this image, follow episode seven of ‘Clinical neurology with KD’ in Apple podcast, Spotify or Google podcast. The anterior choroidal artery is a branch of distal internal carotid artery. It passes posterolaterally and supplies the posterior two-thirds of the posterior limb of the internal capsule, optic tract, lateral geniculate body, optic radiation, amygdala, uncus, adjacent medial temporal lobe, posterior paraventricular corona radiata and a small supply to the thalamus. The symptoms produced by the anterior choroidal artery infarct include hemiparesis due to the posterior limb of internal capsule involvement, hemianopia due to the lateral geniculate body involvement and hemianesthesia due to thalamic supply. A middle cerebral artery infarct can cause the same triad, but the patient will be sicker and have cortical features like aphasia or neglect. There are no cortical features with an anterior choroidal artery infarct. #neurologyteachingclub #clinicalneurology #mbbs #medicineresidency #dnbmedicine #neetpg #neetsuperspeciality #finalmbbs #anteriorchoroidalartery #internalcarotidartery #circleofwillis #neuroanatomy #neurologypodcast #teachingneuroimages #nejm #lancet https://www.instagram.com/p/CZeKb58Pdub/?utm_medium=tumblr
#neurologyteachingclub#clinicalneurology#mbbs#medicineresidency#dnbmedicine#neetpg#neetsuperspeciality#finalmbbs#anteriorchoroidalartery#internalcarotidartery#circleofwillis#neuroanatomy#neurologypodcast#teachingneuroimages#nejm#lancet
1 note
·
View note
Photo
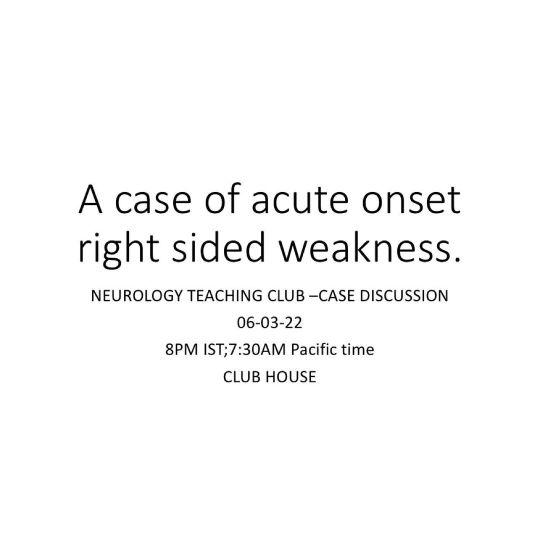
Today(06-03-2022) in Clubhouse at 8 PM IST(7:30 AM Pacific time), we will have a case discussion of a patient presenting with acute onset right-sided weakness, paresthesia, and visual deficits. We will revise the approach to a patient with hemiplegia and arterial localization of stroke while discussing this case. Hearing episodes 3 and 7 of the 'Clinical neurology with KD' podcast https://t.co/wxlIdYdPO9 before the discussion will be helpful. #clinicalneurologywithkd #neurologyteachingclub #stroke #NTC #neurology #neurosciences #neuro #clinicalneurology #medicine #clinicalmedicine #kdpodcast #mbbs #medicos #doctors #neuroanatomy #casediscussion #medicineresidents #residency #medschool #futureneurologist #neuroimages #NEET #finalmbbs #neetpg #neetsuperspeciality #neetmedicine #eanneurology #nejm https://www.instagram.com/p/Cav_aZwrVhB/?utm_medium=tumblr
#clinicalneurologywithkd#neurologyteachingclub#stroke#ntc#neurology#neurosciences#neuro#clinicalneurology#medicine#clinicalmedicine#kdpodcast#mbbs#medicos#doctors#neuroanatomy#casediscussion#medicineresidents#residency#medschool#futureneurologist#neuroimages#neet#finalmbbs#neetpg#neetsuperspeciality#neetmedicine#eanneurology#nejm
2 notes
·
View notes
Photo

Extra medullary compression of the spinal cord. For discussion of these images, follow episode five and six of podcast ‘Clinical neurology with KD’ in Apple podcast, Spotify or Google podcast. An extramedullary compressive lesion goes through three stages, according to Oppenheim. An initial stage of radicular pain and segmental motor and sensory symptoms. The initial phase is followed by a Brown-Sequard syndrome and finally a complete transection of the cord. The rapidity of development of these stages depends on the aetiology and can be acute or chronic. Some of the cardinal features of extramedullary compression include Radicular or root pain, which is a unilateral lancinating pain down the dermatome on coughing, straining, or Valsalva. The patient will have early corticospinal tract involvement with lower limb spasticity more than the upper limb. The leg is more involved as leg fibres are laterally placed in the corticospinal tract than arm fibres. The LMN findings are rare and, if present, occur at the segmental level at the site of compression. The patient will have only late bladder involvement. They have ascending paresthesia as sacral fibres are laterally placed in the spinothalamic tract. Funicular or tract pain is less common. The patient can have vertebral pain and tenderness, which suggest extramedullary extradural lesion. #clinicalneurologywithkd #neurologyteachingclub #paediatricneurology #NTC #neurology #neurosciences #neuro #clinicalneurology #medicine #clinicalmedicine #criticalcaremedicine #mbbs #medicos #doctors #neuroanatomy #casediscussion #medicineresidents #residency #medschool #futureneurologist #neuroimages #NEET #finalmbbs #neetpg #neetsuperspeciality #neetmedicine #eanneurology #nejm #emergencymedicine #spinalcord https://www.instagram.com/p/Cds4asLpst1/?igshid=NGJjMDIxMWI=
#clinicalneurologywithkd#neurologyteachingclub#paediatricneurology#ntc#neurology#neurosciences#neuro#clinicalneurology#medicine#clinicalmedicine#criticalcaremedicine#mbbs#medicos#doctors#neuroanatomy#casediscussion#medicineresidents#residency#medschool#futureneurologist#neuroimages#neet#finalmbbs#neetpg#neetsuperspeciality#neetmedicine#eanneurology#nejm#emergencymedicine#spinalcord
0 notes
Photo

🚨Spotter🚨Five year old boy came with episodes of stare of few seconds. He won’t respond to call at that time. Diagnosis was made from general examination. Please DM me the answers. Follow Clinical neurology with KD podcast at Apple podcast, Google Podcast and Spotify. #clinicalneurologywithkd #neurologyteachingclub #neurologypodcast #NTC #neurology #neurosciences #neuro #clinicalneurology #medicine #clinicalmedicine #kdpodcast #mbbs #medicos #doctors #neuroanatomy #casediscussion #medicineresidents #residency #medschool #futureneurologist #neuroimages #NEET #finalmbbs #neetpg #neetsuperspeciality #neetmedicine #eanneurology #nejm #seizure #epilepsy. https://www.instagram.com/p/CdJKLJOvxO8/?igshid=NGJjMDIxMWI=
#clinicalneurologywithkd#neurologyteachingclub#neurologypodcast#ntc#neurology#neurosciences#neuro#clinicalneurology#medicine#clinicalmedicine#kdpodcast#mbbs#medicos#doctors#neuroanatomy#casediscussion#medicineresidents#residency#medschool#futureneurologist#neuroimages#neet#finalmbbs#neetpg#neetsuperspeciality#neetmedicine#eanneurology#nejm#seizure#epilepsy
0 notes
Photo
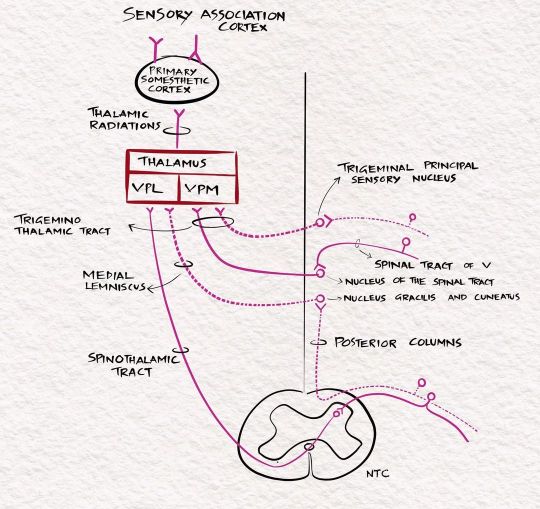
The sensory pathways. For full discussion of this image, follow 'Clinical neurology with KD' podcast episode 10 in Apple podcast, Spotify or Google podcast. Full notes are available on the neurologyteachingclub.com website. The primary modalities of sensation, including touch, pain, temperature, JPS, and vibration, are recognised at the level of the opposite thalamus. So all these sensations are carried to the opposite thalamus by the sensory pathways. The fine touch, vibration and JPS ascend in the posterior column- medial lemniscus pathway, while the pain and temperature through the lateral spinothalamic tract. From the thalamus, they are then projected to the sensory cortex in the postcentral gyrus through the posterior limb of the internal capsule. The sensory cortex helps identify the cortical sensations, namely tactile localisation, two-point discrimination, graphesthesia, stereognosis and sensory attention. #clinicalneurologywithkd #neurologyteachingclub #neurologypodcast #NTC #neurology #neurosciences #neuro #clinicalneurology #medicine #clinicalmedicine #kdpodcast #mbbs #medicos #doctors #neuroanatomy #casediscussion #medicineresidents #residency #medschool #futureneurologist #neuroimages #NEET #finalmbbs #neetpg #neetsuperspeciality #neetmedicine #eanneurology #nejm #aanbrain #neuroimage https://www.instagram.com/p/CdI1u4oP9cY/?igshid=NGJjMDIxMWI=
#clinicalneurologywithkd#neurologyteachingclub#neurologypodcast#ntc#neurology#neurosciences#neuro#clinicalneurology#medicine#clinicalmedicine#kdpodcast#mbbs#medicos#doctors#neuroanatomy#casediscussion#medicineresidents#residency#medschool#futureneurologist#neuroimages#neet#finalmbbs#neetpg#neetsuperspeciality#neetmedicine#eanneurology#nejm#aanbrain#neuroimage
1 note
·
View note
Photo
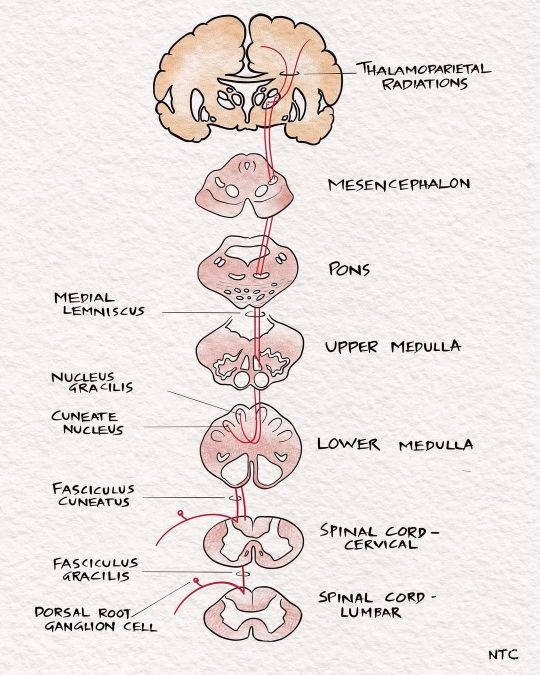
Light touch pathway For discussion of these image, follow 'Clinical neurology with KD' podcast episode ten in Apple podcast, Spotify or Google podcast. Full notes are available on the neurologyteachingclub.com website. The receptors for touch sensation include free nerve endings, Merkel cell endings, and encapsulated nerve endings such as Meissner's corpuscles, Pacinian corpuscles and Ruffini endings. The Pacinian corpuscles act as rapidly adapting mechanoreceptors and are especially sensitive to high-frequency vibration. Others are slowly adapting mechanoreceptors. Light touch sensation is conveyed over large myelinated peripheral nerve fibres to unipolar DRG cells. Tactile sensation follows several different pathways within the central nervous system. The central processes of DRG enter the spinal cord via the medial division of the posterior roots. It then projects through the ipsilateral posterior column to reach the cervicomedullary junction. The fibres from the sacral area will be arranged most medially in the posterior column. The lumbar will be just lateral, followed by the thoracic. The cervical fibres are lateral most as they are the last to enter while going up. The second-order neuron lies in the cuneatus and gracillis nucleus at the cervicomedullary junction. All the fibres below T8 are grouped in the fasciculus gracilis; fibres above T8 form the fasciculus cuneatus. The second-order neurons in the nucleus cuneatus and gracillis project to the opposite thalamus. They immediately sweep anteriorly as the internal arcuate fibres and cross over to the opposite side at the cervicomedullay junction. It ascends in the brainstem as the medial lemniscus to reach the thalamus. The Third-order neuron lies in the ventral posterolateral nucleus of the thalamus and project to the sensory cortex. #sensory #touchpathway #neuro#neurologyteachingclub #neurologypodcast #NTC #neurology #neurosciences #neuro #clinicalneurology #medicine #clinicalmedicine #kdpodcast #mbbs #medicos #doctors #neuroanatomy #casediscussion #medicineresidents #residency #medschool #futureneurologist #neuroimages #NEET #finalmbbs #neetpg https://www.instagram.com/p/CdDx2tIvefO/?igshid=NGJjMDIxMWI=
#sensory#touchpathway#neuro#neurologyteachingclub#neurologypodcast#ntc#neurology#neurosciences#clinicalneurology#medicine#clinicalmedicine#kdpodcast#mbbs#medicos#doctors#neuroanatomy#casediscussion#medicineresidents#residency#medschool#futureneurologist#neuroimages#neet#finalmbbs#neetpg
1 note
·
View note
Photo
New episode of the podcast’Clinical neurology with KD’ released. In this episode, we will discuss the clinical localisation of sensory symptoms. We will learn the sensory pathways and study the clinical features of lesions involving these pathways. You can hear it at Apple podcast, Spotify or wherever you get your podcast #clinicalneurologywithkd #neurologyteachingclub #neurologypodcast #NTC #neurology #neurosciences #neuro #clinicalneurology #medicine #clinicalmedicine #kdpodcast #mbbs #medicos #doctors #neuroanatomy #casediscussion #medicineresidents #residency #medschool #futureneurologist #neuroimages #NEET #finalmbbs #neetpg #neetsuperspeciality #neetmedicine #eanneurology https://www.instagram.com/p/CdACTF5PaTR/?igshid=NGJjMDIxMWI=
#clinicalneurologywithkd#neurologyteachingclub#neurologypodcast#ntc#neurology#neurosciences#neuro#clinicalneurology#medicine#clinicalmedicine#kdpodcast#mbbs#medicos#doctors#neuroanatomy#casediscussion#medicineresidents#residency#medschool#futureneurologist#neuroimages#neet#finalmbbs#neetpg#neetsuperspeciality#neetmedicine#eanneurology
0 notes
Photo
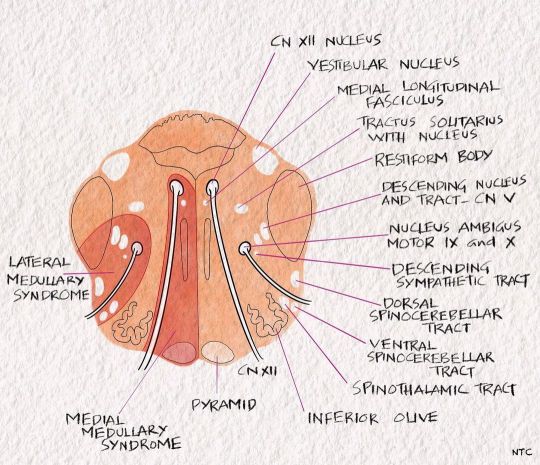
Medial medullary syndrome of Dejerine The 'rule of four' tells us that the 4M lies medially in the brainstem, including the motor pathway or pyramidal tract, motor nuclei of hypoglossal, medial lemniscus and medial longitudinal fasciculus. So a medial medullary syndrome produces opposite side weakness with loss of posterior column sensation and ipsilateral hypoglossal nerve palsy. The MLF involvement can cause upbeat nystagmus occasionally. #clinicalneurologywithkd #neurologyteachingclub #neurologypodcast #NTC #neurology #neurosciences #neuro #clinicalneurology #medicine #clinicalmedicine #kdpodcast #mbbs #medicos #doctors #neuroanatomy #casediscussion #medicineresidents #residency #medschool #futureneurologist #neuroimages #NEET #finalmbbs #neetpg #neetsuperspeciality #neetmedicine #eanneurology #nejm #aanam #medulla https://www.instagram.com/p/Cc2uhA7PxCd/?igshid=NGJjMDIxMWI=
#clinicalneurologywithkd#neurologyteachingclub#neurologypodcast#ntc#neurology#neurosciences#neuro#clinicalneurology#medicine#clinicalmedicine#kdpodcast#mbbs#medicos#doctors#neuroanatomy#casediscussion#medicineresidents#residency#medschool#futureneurologist#neuroimages#neet#finalmbbs#neetpg#neetsuperspeciality#neetmedicine#eanneurology#nejm#aanam#medulla
0 notes