#hepatocellular adenoma
Text
Got my MRI results back, it's not terrible I guess but it's also...not great. I'm pretty unhappy actually. I was really, really hoping for more shrinking. But while the giant one in the left lobe has shrunk a little bit more, the biggest one in the right lobe has grown! It's now 8.4 cm x 6.7 x 7.1 cm, when before it was only 7.6 x 6.1 x 6.4. I'm really devastated that one has grown, I don't exactly know what that means for me but it's not good! And I remembered that I have a LOT of tumors, like, a lot, because when I looked at the scans last year honestly my liver looked like it was more tumor than liver. But I had kind of convinced myself that maybe I was exaggerating that in my head and actually only had like 6 or 8? But the report says "The lesions are too numerous to count [much greater than 10]." So it was how I remembered it, lots and lots of large tumors everywhere. Bc technically anything greater than 5cm is fairly high risk/often operated on, and I have several that are bigger than 5cm. But they can't operate because there are too many and so it's pointless/they can't remove enough of the liver safely. And now some are growing and even if some are shrinking they aren't shrinking much. The overall impression was that this scan was "similar to prior." Which is better than significantly worse but I was really really hoping for better news. I'll have to set up an appointment with a hepatologist to really discuss the results but...at first glance this kind of sucks.
#text post#my post#at least my unrelated blood work looked good. my cholesterol and vitamins and stuff is better#but yeah. this sucks.#i can't believe one of the big ones grew. idk what that means but i'm a bit freaked out about it#and it just. sucks that there are so so so many#the images really do look like my liver is at least 75% tumor when you see them it's wild :(#and by wild i mean kind of terrifying#medical cw#medical tw#hepatic adenoma#hepatocellular adenoma
15 notes
·
View notes
Text
Putting on Animations Printing within Preoperative Preparing.
The concentrate on civilized salivary sweat gland condition is extremely about result right after operation, and there have already been changes within operative strategy, specially in relation to its small dissection associated with salivary adenomas along with sialendoscopy. This post carries on a number of testimonials, which make an effort to present visitors with a quick introduction increase of latest publications inside the English Record regarding Dental and Maxillofacial Medical procedures (BJOMS) in just a certain subspecialty. (D) This year The particular Uk Association associated with Dental and Maxillofacial Doctors. Provided by Elsevier Limited. Just about all protection under the law earmarked.Objective: To test brand-new analysis standards for that splendour regarding early on hepatocellular carcinoma (HCC) from harmless hepatocellular nodules on gadoxetic acid-enhanced MRI (Gd-EOB-MRI). Methods: Many of us retrospectively analysed Thirty-four sufferers using Twenty nine surgically diagnosed early on HCCs as well as 31 operatively clinically determined not cancerous hepatocellular acne nodules. Two radiologists reviewed Gd-EOB-MRI, which includes diffusion-weighted imaging (Drunk driving), and the indication strength at each string, existence of arterial advancement along with washout had been noted. We all composed brand new diagnostic requirements in line with the patch measurement and also MRI results, therefore the analytical functionality this website ended up being compared with those of traditional imaging requirements with logistic regression as well as a generalised estimating picture strategy. Results: A dimensions cut-off price (>= A single.5cm diameter) along with MRI conclusions involving T-1 hypointensity, T-2 hyperintensity, Dui hyperintensity on both low and high b-value images (b=50 along with 800s mm(-2), respectively), arterial improvement, past due fail as well as hepatobiliary hypointensity ended up chosen as the analytic standards. Any time lesions on the skin ended up regarded as malignant whenever they pleased several of the aforementioned requirements, the particular level of responsiveness had been significantly above when coming up with a diagnosis determined by arterial development as well as washout by yourself (Fifty eight.6% vs 13.8%, respectively; p=0.0002), whilst the uniqueness had been 100.0% either way conditions. Conclusion: The brand-new analytic criteria about Gd-EOB-MRI may help to enhance the elegance involving early HCC through harmless hepatocellular acne nodules.Qualifications: Operative input is currently the very best modality with which to treat extreme being overweight. There is certainly too little non-invasive technological innovation with which we could successfully treat obesity along with reverse diabetes type 2 symptoms mellitus. Your EndoBarrier is really a fluoropolymer sleeved that is certainly reversibly fixated for the duodenal lamp and stretches 70 cm to the small bowel, typically ending inside the proximal jejunum. This particular endoscopically inserted unit aids weight reduction via malabsorption as well as triggering junk sparks. Methods: Many of us carried out any nonsystematic evaluation about throughout the world content released around the MEDLINE data source to establish progress from the development and make use of in the EndoBarrier. Results: Nearly all reports employed 12-week excess weight loss (EWL) like a principal final result calculate with results which range from 14.
#GDC-0941#BGB-3111#MTP-131#ITF2357#KU-57788#CB7630#GDC-0994#EPZ019997#NSC 2382#KY 12420#AG-014699#AZD6094#AP24534#ACP-196#MLN2238#CYC202#NVP-LDE225#Peptide 17#NSC 118218#LY3039478#BEZ235#CL-14377#NSC-26271#Caspase Inhibitor VI#AT406#VS-4718#RWJ 26251#CH5126766#BGB-290#GDC-0084
0 notes
Text
Laparoscopic Hepatobiliary Surgery In Delhi By Dr. Neeraj Goel
What Is Laparoscopic Hepatobiliary Surgery?
Laparoscopic hepatobiliary surgery is the minimally invasive surgery. These surgeries are done to treat the conditions related to liver, biliary system, and pancreas. The doctor advises these surgeries when the patients does not respond to medicines.
What Are The Various Diseases That Are Treated Thorugh Hepatobiliary Surgery In Delhi?
There are several diseases that can be treated with the laparoscopic hepatobiliary surgery. However, the doctor only recommends the surgery when the non-invasive methods of treatment are unable to treat the patients or hep in reducing their symptoms. Some of the disease treated with laparoscopic hepatobiliary surgery are:
Cholecystitis: Gall bladder is an organ generally considered as a part of digestive system. It is present just below the liver. It stores the bile synthesized by the liver. Any inflammation in the gall bladder is known as cholecystitis. Laparoscopic hepatobiliary surgery is used to treat this condition.
Cholelithiasis: Surgeons may also perform Laparoscopic hepatobiliary surgery for the management of cholelithiasis. This condition involves the presence of stones in the gall bladder.
Choledocholithiasis: It is also a disease of gall bladder and common bile duct. Laparoscopic hepatobiliary surgery is the procedural intervention for this disease. In this condition, the patient had gallstone in the common bile duct.
Choledochal cysts: This is a congenital condition. The patient with this condition have a cystic dilation of the bile ducts.
Biliary colic: Biliary colic is characterized by the presence of pain in the abdominal cavity. This pain is due to the blockage of bile duct due to gall stones. Doctors may perform Laparoscopic hepatobiliary surgery if the pain is not relieved through medicines and other treatments.
Biliary atresia: Biliary atresia is a congenital condition. Congenital conditions are present from the birth. In this condition, the patients have blockage in the bile ducts, i.e., the tubes that carry the bile from the liver to gall bladder. The exact cause of this condition is not known.
Liver cell carcinoma: Also known as hepatocellular carcinoma, this is the most common primary liver cancer. People with chronic liver diseases, such as hepatitis C, hepatitis B, and cirrhosis are at high risk for developing this condition. People who drink excessive alcohol and have fatty liver disease may develop hepatocellular carcinoma.
Gallbladder and bile duct cancers: Gallbladder cancers are now being treated laparoscopically in experienced centers with GI surgeons with high levels of skills.
Hydatid cysts: Echinococcus granulosismay also cause liver cysts. The cysts caused by this organism is known as hydatid cysts. The doctors may perform the Laparoscopic liver surgery to treat this condition.
Benign Liver lesions: Haemangiomas, focal nodular hyperplasia, and hepatocellular adenomas are the common benign liver tumours. Although in most cases the treatment is not required. However, the doctor may perform laparoscopic liver surgery in case the treatment is required.
What Are The Various Types Of Hepatobiliary Surgery In Delhi?
Various types of hepatobiliary surgery are available in Delhi. You should opt for the best laparoscopic GI surgeon in Delhi. Some of laparoscopic hepatobiliary surgery are:
Laparoscopic cholecystectomy: This is the procedure to remove the gallbladder. The doctor performs this surgery when the patients with gallstones have infection, pain, and inflammation. The doctor performs the minimally invasive surgery. The doctors discharge the patient on the day of surgery or the next day. The patients had fast recovery time.
Laparoscopic liver resection: Laparoscopic liver resection is the choice of treatment to remove the lesions of the liver. The lesions may be benign or cancerous. Before the liver resection surgery, the doctor advises the patients to limit the intake of alcohol and to maintain a healthy and active lifestyle.
Pancreatic Resection: The procedure of removing the complete pancreas or a part it is known as pancreatic resection. If the complete pancreas is removed, the procedure is known as pancreatectomy. The doctor performs the pancreatectomy in cases of sever pancreatitis or pancreatic cancer.
Laparoscopic Hepaticojejunostomy: The doctor performs this surgery in case of biliary strictures and injury to the biliary system. During this procedure, the surgeon creates a connection between the jejunum and hepatic duct. The doctor performs this surgery to ensure the smooth flow of bile from the hepatic system to the digestive system. This will serve multiple purposes. First, bile is required for digestion. Second, accumulation of bile in the hepatic system may cause damage to the organs, such as liver.
Laparoscopic Radical Cholecystectomy: Treatment of gallbladder cancer is now being done increasingly with minimally invasive means with good success. Laparoscopic surgery helps in faster recovery with good oncologic outcomes.
What Are The Advantages Of Laparoscopic Hepatobiliary Surgery?
Laparoscopic hepatobiliary system offers several advantages to the patient. It minimizes the post-operative complications and also reduces the risk of morbidity and mortality that may occur due to traditional open surgery. Further, only the small incisions are made during the surgery, thus there is a less scar formation. Due to minimal exposure of the internal tissues, there is low risk of infection. Laparoscopic surgery reduces the post-operative recovery time and reduces the length of stay at the hospital.
How The Doctor Performs Laparoscopic Heaptobiliary Surgery In Delhi?
The doctor makes one small incision in to the hepatobiliary system at the site where he wants to perform the surgery. The surgeon then inserts the laparoscope, a tube with the camera, to explore the internal diseases or abnormal organ. Once the site of surgery is evaluated, the doctor makes other incisions to insert the surgical instruments. The doctor then performs the surgery by viewing the internal organs on the external monitor.
What Are The Complications Of Hepatobiliary Surgery?
As compared to the traditional open surgery, the risk of complications with the laparoscopic hepatobiliary surgery is significantly lower. Some of the complications include infection, pain, bleeding, tissue damage, and damage to nearby organs.
Where Should I Get More Information About The Laparoscopic Hepatobiliary Surgery In Delhi?
You, as a patient, have the right to get detailed information about your diseases and the possible treatment options. Please contact to know more about the disease and treatment.
TAG- Laparoscopic Hepatobiliary Surgery in Delhi, GI Surgeon in Delhi, Robotic Surgeon in Delhi
0 notes
Text
Different Types Of Liver Cancer
The liver is considered to be the body's powerhouse. It is located beneath the diaphragm located on the right part of your abdomen. It is a key part of the metabolism of our body. It regulates blood sugar levels as well as filters blood. In the event of a malfunction, this organ could cause a variety of health issues.
The process of liver cancer starts with the formation of tumours. The tumour forms when liver cells known as hepatocytes, cells in the bile duct or the cells that line blood vessels within the liver expand in an uncontrolled way.
Liver cancer is classified as the secondary or primary cancer. Primary liver cancer develops from benign tumours such as Hemangiomas, hepatic adenomas and the focal hyperplasia of nodular origin. Cancer may be caused due to other ailments such as chronic kidney disease or viral infection and Hepatitis B or C as well as other liver toxins. Cancer can be further classified into:
* Hepatoma and hepatocellular Carcinoma: The reason is an uncontrolled increase in the number of hepatocyte cells from the liver. Adults, specifically those with liver cirrhosis are more vulnerable. This can happen to teenagers and children, too and is known as "hepatoblastoma". The condition is prevalent in a large number of Americans.
* Cholangiocarcinomas or cancers of the liver ducts: This type of cancer is prevalent in women.
*Hemangiosarcoma as well as Angiosarcoma The two forms of cancer are extremely rare. The former begins in blood vessels. It's more prevalent when children are younger than four years of age. The rate of survival is higher than the second kind of cancer because the rate of progression is slower. The latter is cancer that begins within blood vessels in the liver. Its rate of progress is quite quick, which makes survival rates less.
Secondary liver cancer happens when the cancerous cells within the liver begin to expand. This kind of tumour is known by the term metastatic tumour. Most often, primary cancer of the liver can cause secondary cancer. Other causes include colorectal cancer in advanced stages kidney cancer and lung cancer and other causes. Cancer starts from organs like the pancreas, stomach, or colon and eventually expands to the liver with the blood flow through these organs into the liver. Cancer can also propagate through the lymphatic system.
The symptoms in the beginning stage of cancer might not be obvious. In advanced stages, there are symptoms such as fatigue, fever, fatigue, weakness, or weight loss. When secondary cancer is present, the symptoms include enlarged spleens as well as lethargy and stomach discomfort or nausea.
Treatments for liver cancer may comprise chemotherapy, surgery radiotherapy, PDT and radiosurgery. There is also immunotherapy
For more details visit here: Liver Cancer Surgery in Jaipur
Liver Cancer Surgery in India
1 note
·
View note
Text
Laparoscopic Hepatobiliary Surgery In Delhi By Dr. Neeraj Goel, GI Surgeon In Delhi
Laparoscopic Hepatobiliary Surgery
What Is Laparoscopic Hepatobiliary Surgery?
Laparoscopic hepatobiliary surgery is the minimally invasive surgery. These surgeries are done to treat the conditions related to liver, biliary system, and pancreas. The doctor advises these surgeries when the patients does not respond to medicines.
What Are The Various Diseases That Are Treated Thorugh Hepatobiliary Surgery In Delhi?
There are several diseases that can be treated with the laparoscopic hepatobiliary surgery. However, the doctor only recommends the surgery when the non-invasive methods of treatment are unable to treat the patients or hep in reducing their symptoms. Some of the disease treated with laparoscopic hepatobiliary surgery are:
Cholecystitis: Gall bladder is an organ generally considered as a part of digestive system. It is present just below the liver. It stores the bile synthesized by the liver. Any inflammation in the gall bladder is known as cholecystitis. Laparoscopic hepatobiliary surgery is used to treat this condition.
Cholelithiasis: Surgeons may also perform Laparoscopic hepatobiliary surgery for the management of cholelithiasis. This condition involves the presence of stones in the gall bladder.
Choledocholithiasis: It is also a disease of gall bladder and common bile duct. Laparoscopic hepatobiliary surgery is the procedural intervention for this disease. In this condition, the patient had gallstone in the common bile duct.
Choledochal cysts: This is a congenital condition. The patient with this condition have a cystic dilation of the bile ducts.
Biliary colic: Biliary colic is characterized by the presence of pain in the abdominal cavity. This pain is due to the blockage of bile duct due to gall stones. Doctors may perform Laparoscopic hepatobiliary surgery if the pain is not relieved through medicines and other treatments.
Biliary atresia: Biliary atresia is a congenital condition. Congenital conditions are present from the birth. In this condition, the patients have blockage in the bile ducts, i.e., the tubes that carry the bile from the liver to gall bladder. The exact cause of this condition is not known.
Liver cell carcinoma: Also known as hepatocellular carcinoma, this is the most common primary liver cancer. People with chronic liver diseases, such as hepatitis C, hepatitis B, and cirrhosis are at high risk for developing this condition. People who drink excessive alcohol and have fatty liver disease may develop hepatocellular carcinoma.
Gallbladder and bile duct cancers: Gallbladder cancers are now being treated laparoscopically in experienced centers with GI surgeons with high levels of skills.
Hydatid cysts: Echinococcus granulosismay also cause liver cysts. The cysts caused by this organism is known as hydatid cysts. The doctors may perform the Laparoscopic liver surgery to treat this condition.
Benign Liver lesions: Haemangiomas, focal nodular hyperplasia, and hepatocellular adenomas are the common benign liver tumours. Although in most cases the treatment is not required. However, the doctor may perform laparoscopic liver surgery in case the treatment is required.
What Are The Various Types Of Hepatobiliary Surgery In Delhi?
Various types of hepatobiliary surgery are available in Delhi. You should opt for the best laparoscopic GI surgeon in Delhi. Some of laparoscopic hepatobiliary surgery are:
Laparoscopic cholecystectomy: This is the procedure to remove the gallbladder. The doctor performs this surgery when the patients with gallstones have infection, pain, and inflammation. The doctor performs the minimally invasive surgery. The doctors discharge the patient on the day of surgery or the next day. The patients had fast recovery time.
Laparoscopic liver resection: Laparoscopic liver resection is the choice of treatment to remove the lesions of the liver. The lesions may be benign or cancerous. Before the liver resection surgery, the doctor advises the patients to limit the intake of alcohol and to maintain a healthy and active lifestyle.
Pancreatic Resection: The procedure of removing the complete pancreas or a part it is known as pancreatic resection. If the complete pancreas is removed, the procedure is known as pancreatectomy. The doctor performs the pancreatectomy in cases of sever pancreatitis or pancreatic cancer.
Laparoscopic Hepaticojejunostomy: The doctor performs this surgery in case of biliary strictures and injury to the biliary system. During this procedure, the surgeon creates a connection between the jejunum and hepatic duct. The doctor performs this surgery to ensure the smooth flow of bile from the hepatic system to the digestive system. This will serve multiple purposes. First, bile is required for digestion. Second, accumulation of bile in the hepatic system may cause damage to the organs, such as liver.
Laparoscopic Radical Cholecystectomy: Treatment of gallbladder cancer is now being done increasingly with minimally invasive means with good success. Laparoscopic surgery helps in faster recovery with good oncologic outcomes.
What Are The Advantages Of Laparoscopic Hepatobiliary Surgery?
Laparoscopic hepatobiliary system offers several advantages to the patient. It minimizes the post-operative complications and also reduces the risk of morbidity and mortality that may occur due to traditional open surgery. Further, only the small incisions are made during the surgery, thus there is a less scar formation. Due to minimal exposure of the internal tissues, there is low risk of infection. Laparoscopic surgery reduces the post-operative recovery time and reduces the length of stay at the hospital.
How The Doctor Performs Laparoscopic Heaptobiliary Surgery In Delhi?
The doctor makes one small incision in to the hepatobiliary system at the site where he wants to perform the surgery. The surgeon then inserts the laparoscope, a tube with the camera, to explore the internal diseases or abnormal organ. Once the site of surgery is evaluated, the doctor makes other incisions to insert the surgical instruments. The doctor then performs the surgery by viewing the internal organs on the external monitor.
What Are The Complications Of Hepatobiliary Surgery?
As compared to the traditional open surgery, the risk of complications with the laparoscopic hepatobiliary surgery is significantly lower. Some of the complications include infection, pain, bleeding, tissue damage, and damage to nearby organs.
Where Should I Get More Information About The Laparoscopic Hepatobiliary Surgery In Delhi?
You, as a patient, have the right to get detailed information about your diseases and the possible treatment options. Please contact to know more about the disease and treatment.
Tags = Laparoscopic Hepatobiliary Surgery In Delhi, GI Surgeon in Delhi
For more information = https://www.gastrodelhi.com/
See more blogs = https://gisurgeonindelhi.blogspot.com/2022/06/colorectal-surgery-in-delhi-for.html
0 notes
Text
Life Update
Just a small real life update about what I’ve been doing lately. So, I’ll put it under a cut in case you don’t care to read that sort of thing. :)
First, the fun stuff:
I got another Grand-niece in November! <3 So, helping out with that where I can has kept me on my toes. She’s adorable! (and ginger!!!) I mostly help by spending time with my first grand-niece who is now a spitfire toddler. lol Still loves her some YB though!
I’ve been watching a lot of Kdrama. Finally finished Descendants of the Sun. Didn’t particularly like it. Followed that up with W, which was weird but quite good. And then I proceeded to take forever to watch Princess Hours. lol I think it was just too similar to Boys Over Flowers. (Or vice versa, I’m not sure which came out first.) But at least I can now say that I’ve seen GD’s fave drama. :p Currently, I’m IN LOVE with Touch Your Heart. It’s the best thing I’ve watched since Goblin, no lie. So adorable. <3 I’m 12 episodes in, so around halfway & I don’t want it to end!
Other than that, I’m just basically “momming”. Trying to keep up with one kid graduating this year & the other applying to go to the Academy next year. (Think of it as advanced High school. You graduate in 4 years with both a diploma and an associates degree.) Cross your fingers that he gets in please! They only take 20 kids per year in the program he applied for.
Now, the not so fun stuff:
I told you guys a while back that I had to have an MRI. The reason why is because I’ve been having problems with my blood pressure suddenly spiking. This has been happening for about a year and a half now. The first doctor I saw was totally useless for 6 months & the one I switched to has been amazing and spent a year helping me figure this out.
The short answer is that I have a benign tumor growing in my liver that’s occasionally pressing against my hepatic vein. They found it while doing a CT scan to see if I had a different type of tumor. (Thankfully, I don’t. That one would have been a whole lot worse.) And the MRI was to get a better look at it. Then I had a biopsy done just to make sure exactly what we were dealing with.
The technical term is Hepatocellular Adenoma. Most likely, it was caused by excess estrogen in my system, either from my birth control before I had kids, by my pregnancies themselves or just naturally. Either way, mine is currently 4.5 cm. I can’t have it removed unless it gets to 5cm. (Thank you, shitty American healthcare system.) So, I have to live with it for now. Luckily, my current medication regimen keeps my blood pressure mostly under control, with only the occasional spike.
I go back in April to see if the stupid thing has grown. If it has, then we start planning surgery, which would be major because they’d have to take a good chunk of liver along with it. But honestly, I’m to the point where I really want this thing out of me.
I hope this explains why my writing has been nonexistent for a while now. Juggling life and multiple doctor appointments has taken up a lot of my time. (Once I had to drive 2 hours just to see a specialist & all they did was draw blood. *sigh*)
I’m going to at least try my best and finish the Babysitting fic before April. I hate that I’ve left you guys hanging on that one. But it’s difficult to write when your body hates you.
If/when things change, I’ll keep you guys informed.
Love,
Sin
6 notes
·
View notes
Text
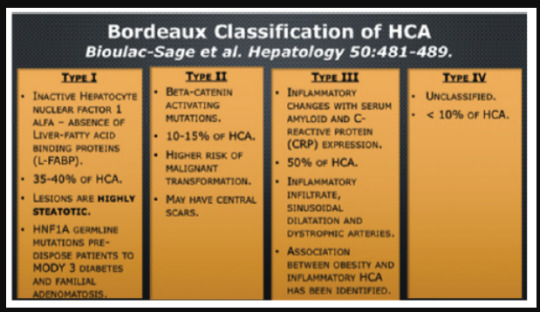
Biomed Grid | Hepatic Adenomas Challenges to their Diagnosis and Management with Emphasis on the Bordeaux Classification
Goals and Learning Objectives
a. To discuss the etiology and natural history of HA.
b. To detail the importance of the Bordeaux Classification.
c. To provide a comprehensive approach to their correct identification based on imaging and pathological features.
d. To present the risk factors associate with hepatic carcinogenesis.
e. To elaborate on the entity of hepatic adenomatosis.
f. To detail on the state-of-the-art management of HA and adenomatosis.
g. To emphasize their association to congenital cardiac conditions and other syndromes.
Disclosure Statement
Authors have nothing to disclose.
Etiology and Natural History of Hepatic Adenomas (Ha)
It has been postulated that disrupted hepatic vasculature results in the development of hepatic lesions including hepatic adenomas, FNH, and hemangiomas. The etiology of HA is that an altered hepatic circulation stimulates the evolution of hepatic adenomas, FNH and hemangiomas. The stimuli provided by estrogen and anabolic steroids in the genesis of HA is well established and first recognized by Edmundson. They can result from abnormal carbohydrate metabolism such as: in glycogen storage disease, mature onset diabetes mellitus of the young type 3 (MODY3), and metabolic syndrome.
Other factors include
Anabolic steroids exposure, Fanconi Anemia, glycogen storage disease types I, III and IV, and familial adenomatous polyposis.
Risk Factors Associated with Hepatic Carcinogenesis
Hepatocellular Carcinoma (HCC) in HA. Risk factors for malignant transformation of HA include: Male sex, glycogen storage disease and Anabolic steroid usage. B-catenin–mutated subtype (highest risk of malignancy) and tumors larger than 5 cm in maximum dimension. Teaching Point! B-catenin mutated hepatocellular adenomas are interpreted as borderline lesions between hepatocellular adenoma and hepatocellular carcinoma.
Hepatocellular Adenoma: Histology
Figure 1:
HA have dilated sinusoids which are thin-walled capillaries that are perfused by arterial pressure; adenomas lack a portal venous supply and are fed solely by peripheral arterial feeding vessels. Because a tumor capsule is usually absent or incomplete, hemorrhage may spread into the liver or abdominal cavity. Billiary ductules are notably absent from adenomas, a key histologic feature that helps distinguish hepatocellular adenoma from focal nodular hyperplasia [1, 4, 3, 4, 5, 6, 7] (Figure 1).
The Bordeaux Classification of Hepatic adenomas represents a multi-center series of 96 liver tumors with a firm or possible diagnosis of HA was reviewed by liver pathologists. This represents a collective experience from 13 French university hospitals encompassing from 1992-2004. All 96 cases were proven HA. Criteria of inclusion in the study had adequate sampling of frozen and fixed liver tissues following hepatectomy (95 cases) or transplantation (1 case). The HA were analyzed and classified according to their genetic profile, pathological and clinical manifestations
HA and Genetic Mutations
Activation of the B-catenin pathway has been found in HA (18-20) and is present in 20 to 34% of hepatocellular carcinomas (21-24). Beta Catenin is key in hepatic physiology: cell lineage and differentiation, stem cell renewal, epithelial-mesenchymal transition, proliferation and cell adhesion (25, 26). Twentytwo (4.5%) patients had HCC transformation. Predictors of HCC transformation, using both univariate and multivariate analyses, were male gender (odds ratio [OR]: 15.0; IC 95%: 5.4 – 44.0) and tumor size >10 cm (OR: 6.9; IC 95%: 2.5 – 20.1).
Bordeaux Classification of HCA
Type I
1. Inactive Hepatocyte nuclear factor 1 alfa – absence of Liver-fatty acid binding proteins (L-FABP).
2. 35-40% of HCA.
3. Lesions are highly steatotic.
4. HNF1A germline mutations pre-dispose patients to MODY 3 diabetes and familial adenomatosis.
5. Second most common (30-35%).
6. Associated with maturity-onset diabetes mellitus of the young (MODY3).
7. Predisposition for hepatic adenomatosis.
8. Develop exclusively in female with history of oral contraceptive use.
9. Intracellular fat results in signal loss on out-of-phase MRI– prevalence 86-100% Estrogens in OCP act as the genotoxic agent resulting in somatic mutations of the HNF 1 alpha resulting in lipogenesis and hepatocellular proliferation; the resulting silencing of hepatic fatty acid binding proteins in hepatocytes resulting in intracellular fat deposition (Figure 2).
Type II
1. Beta-catenin activating mutations.
2. 10-15% of HCA.
3. Higher risk of malignant transformation.
4. May have central scars.
5. Prevalence 10-15%.
6. No Specific MRI Patterns.
7. Occur More Frequently in Males, Associated with Hormone Administration, Glycogen Storage Disease and Familial Adenomatosis Polyposis Syndrome.
8. Β-Catenin is encoded in the beta catenin gene (ctnnb1) located in CHROMOSOME 3Q21.
9. It is the downstream effector of the WNT- β-catenin pathway which has a major role in liver embryogenesis [Figure 2].
Adenomas – Management
Surgical due to propensity for bleeding and malignancy.
Lesions > 5 cm; Liver adenomatosis – resection of largest and most vulnerable to hemorrhage (sub-capsular and/or pedunculated), pregnancy and increased risk of hemorrhage [8, 9, 10, 11, 12, 13, 14].
Hepatic Adenomatosis
a) Etiology is poorly understood; described in 1985 by Flejou et al. familial predisposition. Presence of 10 or more HA´s involving both hepatic lobes.
b) Females in their 4-5 decades of life with a 10-24% prevalence. (6). Associated with non-alcoholic fatty liver disease (NASH).
c) Presence of congenital or acquired hepatic vascular abnormalities.
d) All sub-types of HA may be found in hepatic adenomatosis.
e) Elevated serum alkaline phosphatase and gamma glutamyl transferase.
f) Do not respond to withdrawal of steroids.
g) Increased risk for HCC.
h) Monitoring with alfa feto-protein.
i) Resection of larger adenomas.
j) Imaging characteristics of adenomas similar to HA not associated to liver adenomatosis
Conclusion
I. Imaging characteristics play a key role in determine the surveillance and management of hepatocellular adenomas.
II. Inflammatory hepatocellular adenomas demonstrates peripheral dilated sinusoids (A toll sign), these are not associated with malignant differentiation.
III. Hepatocellular adenomas larger than 5 cm has greater risk for hemorrhage and rupture.
IV. Malignant transformation of hepatic adenoma is likely low and has a male predominance.
Read More About this Article: https://biomedgrid.com/fulltext/volume6/hepatic-adenomas-challenges-to-their-diagnosis-and-management-with-emphasis.001052.php
For more about: Journals on Biomedical Science :Biomed Grid | Current Issue
#biomedgrid#american journal of biomedical science & research#journals on biomedical science#top medical open access journal
0 notes
Text
Liver tumors
Liver tumors
Liver abnormalities appear to cause some abnormal increase in the liver They may be benign or malignant. There may be many different symptoms than lack of symptoms such as liver enlargement, abdominal pain, yellow skin and eyes, vomiting and sore throat.
Benign or mild tumors include hemangiomas, liver cysts, hepatic granulomas, and hepatocellular adenomas. Hepatic tumors can develop in the liver or spread from other parts of the body (metastasis). Hepatocellular carcinoma most often occurs in the liver, as well as gallbladder cancer and hepatoblastoma. They can be detected in medical imaging and confirmed by tissue biopsy.
Treatment depends on the type of tumor, which may or may not require chemotherapy, surgery, and liver transplantation. Hepatitis B is a relatively common liver disease Liver cancer is the most common metastatic disease. The first description of surgery for a liver tumor dates back to the late 1800s, and it was only after the 1970s that major advances were made.
0 notes
Link
Liver Tumor Treatment in Delhi
Liver tumor is abnormal mass growth in the cells of our liver; this growth can be both cancerous and non-cancerous. Most of the time the cancerous growth of tumor is cancer spread from other body parts. A secondary cancer is also called as metastatic cancer.
There are several types of non-cancerous types of liver tumors, which are often not life-threatening, but to know whether the tumor is cancerous or non-cancerous you should always consult with best gastro surgeon in Delhi
Some commonly find non-cancerous liver tumors are listed below:
Benign liver tumors are very common and often do not spread in any other body parts, these liver tumors have no visible symptoms, and often remain undiagnosed. Three types of benign liver tumors are mentioned below:
· Hemangiomas: this mass (lump) is usually not life-threatening, it’s a small cluster of blood vessels in liver which do not cause any pain, but in case of a larger lump it can be painful than only surgery from a liver specialist doctor can help.
· Hepatic adenomas: this tumor is also known as liver cell adenoma, this type of tumor is rare, and mostly seen in women who are on birth control (hormone induced liver tumor). This tumor can bleed causing severe stomach pain or abdominal bloat.
· Focal nodular hyperplasia: these are the 2nd most common kind of benign tumors, usually a single tumor is found in patient only in rare cases it multiplies, these tumors are also common in women than men and often misdiagnosed
Cancerous Liver Tumor
In rare cases a tumorous growth in liver can be cancerous, Hepatocellular carcinoma is one of the most common kind of primary liver cancer, only a timely treatment of liver cancer can save the life of patient, in case of metastatic liver cancer the chances of survival are very less. Liver specialist doctor in Delhi often suggest liver transplant surgery for end-stage liver diseases like liver cancer.
Symptoms of Liver Tumor:
· Weight-loss without any effort
· Fatigue or loss of appetite
· Yellowing of skin (jaundice)
· Abdominal bloating (ascites)
· Light colored or chalky stools
No matter whether your liver tumor is cancerous or non-cancerous both required medical attention, in many cases non-cancerous tumors can rupture or leak which can cause uncomfortable abdominal pain. On the other hand a cancerous tumor can spread without treatment.
Treatment
For the treatment of life-threatening diseases like tumors you should always consult with the best gastro surgeon in Delhi, only an expert gastro surgeon can provide you right guidance and treatment.
A gastro surgeon will first asses your current symptoms and medical history, based on that he will suggest some tests to rule out the cancer, he may suggest some tests like endoscopy, biopsy or some other imaging tests to determine the exact disease or condition of liver. In case of tumors only surgery provides the relief.
You can get consultation from liver specialist doctor in Delhi Dr. Sandeep Jha, he has more than 10 years of experience in treating various liver disorders including liver tumor.
0 notes
Text
Global Oxyfluorfen Market
Global Oxyfluorfen Market
Oxyfluorfen is also known as 2-Chloro-1-(3-ethoxy-4-nitrophenoxy)-4-(trifluoromethyl) benzene or a diphenyl-ether herbicide used for broad-spectrum post and pre-emergent control of grassy weeds and annual broadleafs such as in vine, tree fruit, nut, and field crops. Some of the common names of oxyfluorfen include Galligan, Oxygold, and RH-2915. The Oxyfluorfen has the largest market in the agricultural industry they are majorly used as an active ingredient such as in almonds and grapes. They are also majorly adopted in forestry, non-agricultural ornamental to control weeds in driveways, landscapes, patios, and similar areas in residential area sites. Oxyfluorfen products are available in emulsifiable concentrate and granular formulations.
The global agricultural market is expected to reach an xx% market share by 2027. Economies developments, increasing consumer’s awareness towards the protection of crop, increasing governments & FDI investments in the agricultural sector are the keys driving the market growth. Technological advancement in biotechnology and shift in farming practices are the other factors that are showing Northward trends towards the market growth of oxyfluorfen during the coming years.
However, the market growth may hamper by the factors such as, there is development in some weed species that are resistant to Oxyfluorfen also, inhalation of toxic chemicals causes low acute oral, dermal and alteration in blood parameters in the liver and anemia. In addition, Oxyfluorfen is classified as a possible human carcinogen based on combined hepatocellular adenomas/carcinomas in the mouse carcinogenicity.
The global oxyfluorfen market is anticipated to hit xx US $XX million by 2027. The report covers the in-depth analysis of market key players with their market share, primary and secondary forecast data analysis to 2027. The rationals behind the Covid-19 impact on various regions are mentioned in the report. The report focuses on market drivers and restrain, forecasting of the oxyfluorfen market, and concentrate on present opportunities in this sector. The global Oxyfluorfen market is growing in developing economies because of favorable government policies and market penetration of manufacturers, dealers, and suppliers of the Oxyfluorfen market.
For more information visit@ https://www.maximizemarketresearch.com/market-report/global-oxyfluorfen-market/81643/
Segment Analysis
Global Oxyfluorfen Market
The herbicides segment holds the largest market share of xx% in 2019 and is growing at a CAGR of xx% during the forecast period.
By application, the herbicides segment is projected to witness rapid growth with a CAGR of xx% during the forecast period. Extensive usages of oxyfluorfen in the agricultural sector across the globe, rising adoption of tending a lawn or home garden, and consumer awareness towards weeds also, products that are economically friendly to the environment has fueled the market growth.
Regional Insights:
Global Oxyfluorfen Market 1
Asia pacific was dominant in 2019 with a market share of xx% and expected to grow at a CAGR of xx% during the forecast period.
The Asia Pacific market is anticipated to be the fastest-growing market with a CAGR of xx% during the forecast period. In countries like India and China, with the growing populations, rapid urbanizations and shift in farming have to upsurge the market growth. The government has taken key initiatives by taking various agricultural programs to reduce crop losses by eliminating weed and pests which is further contributing the market growth. The crop losses due to insect pests were US$ 36 billion annually in 2018 and the total loss of food grains is around 1.3 billion tonnes per year according to the Food and Agricultural Organisation (FAO) of the United Nations (UN). Climate change makes pests hungrier as the warmer climate will increase the metabolic rate of insects making them devour more crops this has led to the adoption of oxyfluorfen.
North America is growth with a market share of xx% by 2019-2027
The market in North America is expected to grow at a CAGR of xx% during the forecast period. Increasing demand for cheaper herbicides, more effectiveness, and substitute of hand weeding in crop yielding or growing has fuelled the market growth. Extensive research & development in biological, physiological, and synthetic research of products to reduce the life of living organisms and to provide a better environment profile have made a positive impact on the market.
The objective of the report is to present a comprehensive analysis of the global Oxyfluorfen market including all the stakeholders of the industry. The past and current status of the industry with forecasted market size and trends are presented in the report with the analysis of complicated data in simple language. The report covers all the aspects of the industry with a dedicated study of key players that includes market leaders, followers, and new entrants. PORTER, SVOR, PESTEL analysis with the potential impact of micro-economic factors of the market have been presented in the report. External as well as internal factors that are supposed to affect the business positively or negatively have been analysed, which will give a clear futuristic view of the industry to the decision-makers. The report also helps in understanding global Oxyfluorfen market dynamics, structure by analyzing the market segments and project global Oxyfluorfen market clear representation of competitive analysis of key players by price, financial position, by detection and equipment portfolio, growth strategies, and regional presence in the global Oxyfluorfen market make the report investor’s guide.
This report submitted by Maximize market Research Company
Customization of the report:
Maximize Market Research provides free personalized of reports as per your demand. This report can be personalized to meet your requirements. Get in touch with us and our sales team will guarantee provide you to get a report that suits your necessities.
About Maximize Market Research:
Maximize Market Research provides B2B and B2C research on 20,000 high growth emerging opportunities & technologies as well as threats to the companies across the Healthcare, Pharmaceuticals, Electronics & Communications, Internet of Things, Food and Beverages, Aerospace and Defense and other manufacturing sectors.
Contact info:
Name: Lumawant Godage
Organization Address: MAXIMIZE MARKET RESEARCH PVT. LTD.
Email: [email protected]
Address: Omkar Heights, Sinhagad Road, Manik Baug, Vadgaon Bk,Pune, Maharashtra 411051, India.
Contact: +919607195908
0 notes
Text
Threat To People With Liver Disease, What You Should Know
Dr Piyush Ranjan is the best gastroenterologist in Delhi who successfully treats several kinds of liver diseases, some of which are life-threatening. Below are the various types of liver disorders that you may get.
Infections
Hepatitis A
You may acquire it by consuming anything tainted by faecal matter. Symptoms might not show. It generally subsides by itself within 6 months without future complications.
Hepatitis B
You may acquire it from another individual, for instance, via drugs with shared needles or unprotected sex. Remaining for more than 6 months, it can make you more vulnerable to liver cancer or other disorders.
Hepatitis C
You may get it from infected blood, which enters your blood by having drugs with shared noodles or via HIV. Healthcare workers may receive it from infected noodles which unintentionally stick them. Signs are not available for several years. For indistinct reasons, baby boomers are prone to this infection and must be tested for it.
Immune system disorders
Autoimmune hepatitis
It inflames the liver and might lead to other diseases, including liver failure. Female individuals more usually get it than males.
Primary biliary cholangitis
It attacks your bile ducts. With injured ducts, your bile gets accumulated inside the liver, thereby scarring it. Women acquire it more frequently than men.
Primary sclerosing cholangitis
It scars the bile ducts and might finally block them. Your bile gets collected inside the liver, disrupting the working of your liver. It may result in liver cancer or you may require liver transplantation, someday. Male individuals are more likely to get it than females.
Cancer and tumours
Liver cancer
It impacts men less often than women. Also called hepatocellular carcinoma, it more usually occurs if you drink a lot or have hepatitis. Dr Piyush Panjan is the best liver specialist doctor in Delhi.
Bile duct cancer
It attacks your bile ducts and significantly strikes people above 50 years of age. However, it is rare.
Liver cell adenoma
It is a tumour which is not cancerous. It is rare but women who use birth control pills for a long duration are more vulnerable to it than other individuals. As a minor possibility, the tumour might finally turn into cancer.
Genetic conditions
Hemochromatosis
It causes the body to accumulate excess iron from your food. The additional iron is collected in the heart, liver and/or other parts. It might cause life-threatening issues like liver disorders, diabetes, heart disease, etc.
Hyperoxaluria
It happens when the urine has an excess of a chemical named oxalate. With this issue, the liver produces much less oxalate, because of a genetic mutation. As such, kidney stones and/or kidney failure may occur. Due to kidney failure, oxalosis may take place with accumulated oxalate in other organs that leads to further complications.
Wilson’s disease
It causes copper to be stored up in the liver and other organs. Its primary signs generally appear between 6 and 35 years of age, especially in your teenage. It impacts the liver and also results in nervous and psychiatric issues.
Alpha-1 antitrypsin deficiency
It happens from a chemical (produced by your liver), which helps the lungs check infections. However, when the liver messes up the recipe, the troublesome chemical may accumulate, causing liver disease.
Other causes
Alcohol abuse
It may cause cirrhosis, long-term hepatitis B and/or C and non-alcoholic fatty liver.
Drug overdose
Consuming excess acetaminophen or other drugs may affect your liver. Following the dosing directions, check that acetaminophen may occur in your multiple medications.
NAFLD (non-alcoholic fatty liver disorder)
It happens from excess fat build-up in your liver, causing liver inflammation. One of its types is NASH (non-alcoholic steatohepatitis). It causes liver cell damage, inflammation and fat accumulation. It may also scar the liver, leading to other conditions, including cirrhosis. Dr Piyush Ranjan is also liver cirrhosis doctor in Delhi.
0 notes
Note
I just read you have a tumor? Are you ok...?
Don’t panic, dear anon! <3 I am, for the moment, okay.
My health has been really weird for almost 2 years now. My doctor has been doing everything he can to try and figure out what’s going on. I’ve been referred out to different specialists & had all sorts of tests. Most everything is normal, except they found that I have iron deficiency anemia.
As part of all the testing, I had a CT scan in September of last year to see if I had a rare type of tumor on my adrenal glands. (I did NOT, thank goodness!) In that process they found a “spot” on my liver. So, I had a follow up MRI and then a biopsy of the mass in October.
The good news is that it is a totally benign tumor called Hepatocellular Adenoma. (still very rare... about 1 per 1 million) Bad news is that it can spontaneously rupture & cause internal bleeding if it gets too big. Mine is in the left lobe of my liver, which makes it more likely to do that. Other bad news is that if it gets bigger, it could also turn cancerous.
As of now, I have restrictions on how much I can lift & certain strenuous exercises I can’t do. I’ll have a follow up scan at the end of April to see if it’s grown & we make a plan from there. My tumor is currently 4.5cm x 4.7cm. It only becomes a problem if it’s >5cm. If it’s grown, the plan is major surgery to remove it and a good chunk of my liver at the same time.
Unfortunately, the tumor also puts me in the “high risk” category to catch this stupid virus... so I’m pretty much on lock down.
I know a lot of people freak out when they hear the word tumor & I’m sorry if I caused you any panic. But I believe in calling the thing what it is. Somehow, the more I say it, the less scary it is for me. I’ll be sure to keep you guys updated on how things go. And, thank you so much for caring and asking if I’m okay. <3 That’s so sweet of you! This whole crazy process has been super stressful, but I’m learning to deal with it day by day.
2 notes
·
View notes
Photo
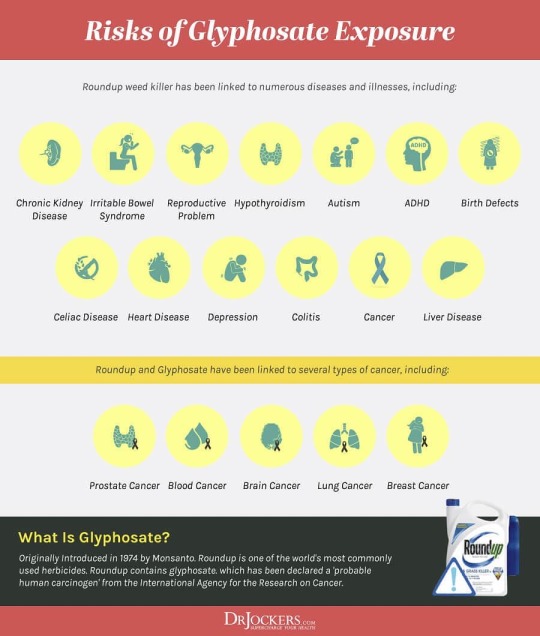
"Negative impact on the body is insidious and manifests slowly over time as inflammation damages cellular systems throughout the body." “Glyphosate, a synthetic herbicide patented in 1974 by the Monsanto Company and now manufactured and sold by many companies in hundreds of products, has been associated with cancer and other health concerns. A 2017 study found that Americans’ exposure to glyphosate increased approximately 500% since Roundup Ready GMO crops were introduced in the U.S in 1996” —> its a known carcinogen, and it wreaks havoc on your gut biome! In the United States alone, usage increased nearly sixteen-fold between 1992 and 2009. Most of this increase occurred after the introduction of genetically modified glyphosate-resistant "Roundup-ready" crops in 1996 Herbicide tolerance is the most prevalent GMO trait engineered into food crops, with some 90% of corn and 94% of soybeans in the U.S. engineered to tolerate herbicides, according to USDA data. The International Agency for Research on Cancer (IARC) classified glyphosate as Group 2A, "probably carcinogenic to humans." A test of surface areas inside homes: All surface wipe and dust samples collected from five farm households in Iowa contained detectable levels of glyphosate ranging from 0.0081-2.7 ng/cm2. In six non-farm households, 28 out of 33 samples collected contained detectable levels of glyphosate ranging from 0.0012-13 ng/cm2. Study shows: "Slight increases in pancreatic islet cell adenomas, hepatocellular adenomas, and thyroid C-cell adenomas were observed in some cases." "Kidney tissue examinations found chronic interstitial nephritis and tubular epithelial basophilia and hypertrophy in male rats." "Researchers noted increased DNA and micronuclei damage in the peripheral erythrocytes" glyphosate are “associated with a high risk of cutaneous melanoma” (skin cancer), “ the U.S. Food and Drug Administration (FDA) finds trace amounts of Roundup in various oatmeals, cereals, and baby foods. "birth defects of the heart, brain and intestines, even at doses 1,500 times lower than those used on soy crops. Other defects observed include head deformities & central nervous system problems" (at Happy Hippy Family) https://www.instagram.com/p/CAX00WxBFuz/?igshid=1kbgag6um1wrb
0 notes
Text
Lupine Publishers | The Current Approach to the Hepatocellular Carcinoma; A Mini Review of Etiology, Prognosis and Treatment
Lupine Publishers |Current Trends in Gastroenterology and Hepatology
Abstract
Hepatocellular carcinoma (HCC) is the most common liver malignancy worldwide and is one of the major causes of cancerrelated deaths. HCC is reported to be the second most fatal malignancy. The major risk factors for HCC are well known; the known risk factors include hepatitis C virus (HCV) and hepatitis B virus (HBV). Major advances have been reported in the treatment of HCC. Success of early diagnosis increases when these risk factors are identified, and the cases are followed up. It is reported that in the treatment of early-diagnosed HCC cases, ethanol injection or radiofrequency ablation methods as well as surgical resection should be preferred, particularly in cases without liver cirrhosis and in cases where the tumor is restricted. Similarly, liver transplantation may be an option for patients that meet specific criteria.
Keywords: Hepatocellular Carcinoma; Liver Carcinoma; Liver; Cirrhosis
Introduction
Hepatocellular carcinoma (HCC) is one of the leading causes of cancer-related deaths in the world. HCC is reported to be the second most fatal malignancy after pancreatic carcinoma [1-3]. In the United States of America, 5-year survival of patients with HCC is reported to be approximately 9% [4]. In contrast to several other malignancies, the major risk factors for HCC are well known. These risk factors include hepatitis C (HCV) and hepatitis B virus (HBV). Major advances have been reported in the treatment of HCC. Success of early diagnosis increases when these risk factors are identified, and the cases are followed up [1]. A glance at the epidemiology of HCC reveals that it is more common in developing regions [5,6]. A 2008 study reported extremely high mortality rates for HCC [7]. Owing to the high mortality rate, HCC is one of the most common causes of cancer-related deaths. There are several predisposing factors in the etiology and pathogenesis of HCC. Following are the few examples of these factors: Hepatotropic viruses, HBV and HCV, are the most common cause [8]. Cirrhosis: Considering its annual incidence, approximately 3% of the patients with cirrhosis are expected to develop HCC [9]. Liver cell dysplasia (Large cell dysplasia and small cell dysplasia): Although both large and small cell dysplasia’s are risk factors for HCC, some authors argue that the presence of small cell dysplasia is a more important risk factor for HCC [10,11]. Thorotrast: It has been reported to play a role in HCC development [12]. Alpha1 antitrypsin deficiency: It is reported that individuals born with this metabolic disorder have a predisposition for HCC [13]. Tyrosinemia: There is a high risk of HCC in individuals born with this metabolic problem [14]. Aflatoxin: Aflatoxin, derived from the metabolic wastes of the fungus Aspergillus flavus, is associated with HCC [15].
HCC can be radiographically diagnosed by computed tomography (CT) or magnetic resonance imaging (MRI). Moreover, dynamic imaging maintains contrast in the early arterial phase, which is then washed or released in the next portal phase. This imaging approach is 90% sensitive and 95% specific for HCC [16]. Ultrasound (US) findings are similar to those of CT and MRI. However, in recent years, contrast-enhanced US is no longer accepted as a diagnostic tool owing to the fact that cholangiocarcinoma cases cannot be distinguished from HCC and further investigation methods are recommended. In terms of laboratory findings, alpha fetoprotein (AFP) elevation in patients with HCC has been known for more than 40 years. AFP elevation can also be detected in pregnancy, normal fetal yolk sac, and fetal liver tissues. Other than HCC, it is also detected in the malignancies of the biliary tract, pancreas, and gastrointestinal system, as well as in nonseminamatous tumors. AFP level is expected to decrease in infants at 300 days after birth, and any AFP elevation detected after this period is a cause to suspect malignancy [17]. However, it has been reported that approximately one-third of the diagnosed cases may have normal AFP levels at the time of diagnosis [18]. Despite the advances in imaging systems and the support provided by laboratory findings, final diagnosis of HCC is still made on the basis of histopathological examination. US or CT-guided cytological fine-needle aspiration biopsy (FNAB) or histological tru-cut biopsy might be preferred in cases suspected with HCC. It has been reported that the diagnostic accuracy of concurrent FNAB and tru-cut biopsy is higher than that of either procedure on its own, with a sensitivity of 96% and specificity of 95% [19]. In microscopic examination of HCC, neoplastic hepatocytes mimic normal liver tissue depending on the degree of differentiation. Well-differentiated tumors that are almost similar to normal tissue are generally difficult to histopathologically distinguish from differentiated liver adenoma tissues. Less differentiated anaplastic tumors can be identified using certain additional immunohistochemical or histochemical analyses because their similarity with normal tissue is reduced.
The most common histological patterns in microscopy are trabecular (sinusoidal), solid, and pseudoglandular (acinar) patterns [20]. Most HCC cases are immunohistochemically positive for AFP, epithelial membrane antigen, alpha1 antitrypsin, fibrinogen, IgG, ferritin, Heppar 1, MOC 31, glypican-3, and polyclonal CEA [21]. HCC staging is generally dependent on many criteria such as tumor size, number of tumor nodules, and the presence/absence of vascular invasion [21]. There are various treatment approaches available for HCC cases. Considering the HCC stage, the functional status of liver and the accompanying medical problems, the treatment decision for HCC should be made with a multidisciplinary team comprising a surgeon, oncologist, pathologist, radiologist, and hepatologist [1]. The most effective treatment in HCC cases is surgical resection and liver transplantation (Figures 1 & 2) [22]. Ablative therapies such as radiofrequency ablation (RF), microwave ablation, or percutaneous ethanol injection are among the treatments that should be primarily used for masses smaller than 2 cm. However, ablative therapies are also preferred in patients with advanced age and poor clinical condition, and in whom surgical resection or transplantation cannot be employed [23]. In cases of HCC, many factors such as the number of tumors, tumor size, presence of cirrhosis, and surgical experience should be taken into account before performing resection and transplantation procedures. In case of partial resection of cirrhotic livers, patient’s condition may deteriorate owing to impaired function and low regeneration capacity. For this reason, liver functions should be comprehensively evaluated in patients with cirrhosis, and then decision regarding surgery should be taken [22]. In patients in whom surgery cannot be performed, neoadjuvant therapies such as transarterial embolization (TAE), transarterial chemoembolization (TACE), RF ablation, and percutaneous acid injection can be employed. In addition to these techniques, the use of microwave therapy, transarterial radioembolization, and cryotherapy applications has also been reported. Furthermore, sorafenib, a tyrosine kinase inhibitor used for molecular therapy, can be preferred in patients with advanced stage HCC [24].
Figure 1: Right Hepatectomy for Hepatocellular Carcinoma.
Figure 2: Liver Hiler dissection.
0 notes
Text
300+ TOP HEPATOBILIARY PANCREATIC SURGERY Objective Questions & Answers
HEPATOBILIARY PANCREATIC SURGERY Multiple Choice Questions :-
Liver and Pancreas MCQs :-
1. Which of the following statements about the segmental anatomy of the liver are not true?
A. Segments are subdivisions in both the French and American systems.
B. Segments are determined primarily by the hepatic venous drainage.
C. The French anatomic system is more applicable than the American system to clinical hepatic resection.
D. Segments are important to the understanding of the topographic anatomy of the liver.
Answer: D
2. Which of the following anatomic features of the biliary system are important considerations in operative cholangiography?
A. The left hepatic duct comes off farther anterior than the right one.
B. At the confluence there may be more than just a right and a left hepatic duct.
C. Dissection of the triangle of Calot is more important than cholangiography in preventing bile duct injury.
D. Segments V, VII, or VIII sometimes join the biliary system below the confluence.
Answer: ABCD
3. The hepatic artery:
A. Supplies the same amount of blood to the liver as the portal vein.
B. Provides more blood to the bile ducts than the portal vein.
C. Is autoregulated just as the portal vein is.
D. Supplies most of the blood to hepatic metastases.
Answer: BD
4. Bile formation is:
A. An active secretory process.
B. Determined at two sites principally.
C. Regulated physiologically by hormones.
D. Largely determined by the intactness of the enterohepatic circulation (EHC).
Answer: ABCD
5. Generally, the two most important hepatic functions to consider after hepatic resection are:
A. Hepatic synthetic function.
B. Glucose metabolism.
C. The liver's role in lipid metabolism.
D. The liver's role in vitamin metabolism.
Answer: AB
6. Which of the following statements about pyogenic abscess of the liver are true?
A. The right lobe is more commonly involved than the left lobe.
B. Appendicitis with perforation and abscess is the most common underlying cause of hepatic abscess.
C. Mortality is largely determined by the underlying disease.
D. Mortality from hepatic abscess is currently greater than 40%.
Answer: AC
7. Which of the following statements most accurately describes the current therapy for pyogenic hepatic abscess?
A. Antibiotics alone are adequate for the treatment of most cases.
B. All patients require open surgical drainage for optimal management.
C. Optimal treatment involves treatment of not only the abscess but the underlying source as well.
D. Percutaneous drainage is more successful for multiple lesions than for solitary ones.
Answer: C
8. Which of the following statements characterize amebic abscess?
A. Mortality is higher than that for similarly located pyogenic abscesses.
B. The diagnosis of amebic abscess may be based on serologic tests and resolution of symptoms.
C. In contrast to pyogenic abscess, the treatment of amebic abscess is primarily medical.
D. Patients with amebic abscess tend to be older than those with pyogenic abscess.
BC
9. Which of the following statement(s) is/are true about benign lesions of the liver?
A. Adenomas are true neoplasms with a predisposition for complications and should usually be resected.
B. Focal nodular hyperplasia (FNH) is a neoplasm related to birth control pills (BCPs) and usually requires resection.
C. Hemangiomas are the most common benign lesions of the liver that come to the surgeon's attention.
D. Nodular regenerative hyperplasia does not usually accompany cirrhosis.
Answer: A
10. Which of the following statement(s) about malignant neoplasms of the liver is/are true?
A. Hepatocellular carcinoma is probably the number 1 cause of death from cancers worldwide.
B. The most common resectable hepatic malignant neoplasm in the United States is colorectal metastasis.
C. Hepatoma has at least one variant that has a much more benign course than hepatomas in general.
D. Hepatomas are generally slower growing than was formerly believed.
Answer: ABCD

HEPATOBILIARY PANCREATIC SURGERY MCQs
11. Which of the following statement(s) is/are true about bile duct cancers?
A. If resected, proximal lesions are usually curable.
B. The more proximal the lesion, the more likely is resection to be curative.
C. Radiation clearly prolongs survival.
D. Transplantation is usually successful if the lesion seems confined to the liver.
E. None of the above is true.
Answer: E
12. Echinococcosis liver disease caused by Echinococcus granulosus:
A. Is not a neoplasm.
B. Is endemic to parts of Europe, but not the United States.
C. Is usually curable by resection.
D. Is more deadly than in its Echinococcus multilocularis form.
Answer: ABC
13. Which of the following statements about hemobilia are true?
A. Tumors are the most common cause.
B. The primary treatment of severe hemobilia is an operation.
C. Percutaneous cholangiographic hemobilia is usually minor.
D. Ultrasonography usually reveals a specific diagnosis.
Answer: C
14. Ligation of all of the following arteries usually causes significant hepatic enzyme abnormalities except:
A. Ligation of the right hepatic artery.
B. Ligation of the left hepatic artery.
C. Ligation of the hepatic artery distal to the gastroduodenal branch.
D. Ligation of the hepatic artery proximal to the gastroduodenal artery.
Answer: D
15. Which of the following is the most common acid-base disturbance in patients with cirrhosis and portal hypertension?
A. Metabolic acidosis.
B. Respiratory alkalosis.
C. Metabolic alkalosis.
D. Respiratory acidosis.
Answer: C
16. A portal venous pressure of 30 mm. Hg (elevated) and a hepatic venous wedge pressure of 5 mm. Hg (normal) may be associated with which of the following causes of portal hypertension?
A. Portal vein thrombosis.
B. Alcoholic cirrhosis.
C. Schistosomiasis.
D. Alcoholic hepatitis.
Answer: AC
17. Which of the following is the most effective definitive therapy for both prevention of recurrent variceal hemorrhage and control of ascites?
A. Endoscopic sclerotherapy.
B. Distal splenorenal shunt.
C. Esophagogastric devascularization (Sugiura procedure).
D. Side-to-side portacaval shunt.
E. End-to-side portacaval shunt.
Answer: D
18. Which of the following treatments most effectively preserves hepatic portal perfusion?
A. Distal splenorenal shunt.
B. Conventional splenorenal shunt.
C. Endoscopic sclerotherapy.
D. Side-to-side portacaval shunt.
Answer: C
19. Which of the following veins is preserved in performing the extensive esophagogastric devascularization procedure described by Sugiura?
A. Left gastric (coronary) vein.
B. Short gastric vein.
C. Splenic vein.
D. Left gastroepiploic vein.
Answer: A
20. Which of the following complications of portal hypertension often require surgical intervention (for more than 25% of patients)?
A. Hypersplenism.
B. Variceal hemorrhage.
C. Ascites.
D. Encephalopathy.
Answer: B
21. Which of the following effects are advantages of combined vasopressin and nitroglycerin intravenous infusion, as compared with vasopressin infusion alone, in controlling acute variceal bleeding?
A. Lower frequency of encephalopathy.
B. Lower incidence of vasopressin side effects.
C. More effective control of bleeding.
D. Less “rebound effect” when discontinuing the infusion.
Answer: BC
22. Which of the following statements about the peritoneovenous shunt (PVS) is/are correct?
A. For cirrhotic patients with intractable ascites, the LeVeen shunt is an effective “bridge” to liver transplantation.
B. Replacement of ascites with saline or lactated Ringer's solution reduces the coagulopathy following PVS.
C. For patients with cirrhotic ascites, the survival using repeated paracentesis with 5% albumin infusion is equivalent to that with the PVS.
D. Oliguria (less than 25 ml. per hour) in the immediate postoperative period following PVS should be treated with a 5% albumin infusion.
E. The transjugular intrahepatic portacaval shunt with stent (TIPSS) works on the same principle as the PVS.
Answer: BC
23. Which of the following clinical situations are considered good indications for PVS?
A. A 50-year-old cirrhotic man had an emergency portacaval shunt for bleeding varices and postoperatively had an ascites leak and mild superficial wound infection.
B. A 57-year-old woman with primary biliary cirrhosis (PBC) has difficult to control ascites and diuretic-induced encephalopathy.
C. A 46-year-old resistant alcoholic has chronic ascites uncontrolled by diuretics combined with repeat paracentesis.
D. A 34-year-old woman taking BCPs had rapid onset of ascites and is found to have hepatic vein thrombosis causing the Budd-Chiari syndrome.
Answer: C
24. Which of the following explanations account(s) for the fact that hepatitis C is the most common cause of posttransfusion hepatitis?
A. There are more carriers of hepatitis C virus (HCV) in the normal population who serve as blood donors.
B. Blood infected with hepatitis B virus (HBV) is eliminated through routine testing, leaving only HCV as the other blood-borne pathogen.
C. Current serologic tests for HCV antigen do not exclude carriers.
D. Questions designed to eliminate risk groups for HCV from the normal donor population may not be as specific as would be desirable.
E. Hepatitis C is a more virulent form of viral hepatitis, so it is expected that more cases of posttransfusion hepatitis would occur.
Answer: BD
25. True or false: HBV infections:
A. Are usually asymptomatic.
B. May not be clinically recognized but may lead to chronic hepatitis.
C. Reliably protect against subsequent HBV infection regardless of the measured antibody titer to hepatitis B surface antigen (HBsAg).
D. Are completely prevented by postexposure administration of HBIg hepatitis B immunoglobulin (HBIg).
E. Preclude subsequent infection with HDV.
Answer: TRUE: BC, FALSE ADE
26. Which of the following statements about choledocholithiasis are correct?
A. Common duct stones can originate in the gallbladder and migrate to the common duct, and stones can form de novo in the duct system.
B. Calcium bilirubinate stones are associated with the presence of bacteria in the duct system.
C. Common duct stones discovered at laparoscopic cholecystectomy should be treated by postoperative endoscopic extraction.
D. The serum bilirubin value is usually greater than 15 mg. per dl. in the patient with a symptomatic common duct stone.
Answer: ABC
27. A benign biliary duct stricture:
A. Need not be treated unless it causes clinical jaundice.
B. Should always be treated by percutaneous balloon drainage.
C. Is prone to recur after treatment with biliary-enteric anastomosis.
D. When due to chronic pancreatitis should be treated by side-to-side choledochoduodenostomy.
Answer: CD
28. Which statements about extrahepatic bile duct cancer are correct?
A. Cholangiography is essential in evaluating patients for resectability.
B. The prognosis is excellent when appropriate surgical and adjuvant therapy are given.
C. The location of the tumor determines the type of surgical procedure.
D. The disease usually becomes manifest by moderate to severe right-side upper quadrant pain.
Answer: AC
29. Which of the following statements about biliary tract problems are correct?
A. Choledochal cyst should be treated by Roux-en-Y cystojejunostomy.
B. Sclerosing cholangitis is characterized by long, narrow strictures in the extrahepatic biliary duct system.
C. Operative (needle) cholangiography is indicated in patients who at operation appear to have no gallbladder.
D. The long cystic duct, which appears to be fused with the common duct and enters it distally, should be dissected free and ligated at its entrance into the common duct.
Answer: C
30. Which of the following statements about the diagnosis of acute calculous cholecystitis are true?
A. Pain is so frequent that its absence almost precludes the diagnosis.
B. Jaundice is present in a majority of patients.
C. Ultrasonography is the definitive diagnostic test.
D. Cholescintigraphy is the definitive diagnostic test.
Answer: AD
31. Which statements about acute acalculous cholecystitis are correct?
A. The disease is often accompanied by or associated with other conditions.
B. The diagnosis is often difficult.
C. The mortality rate is higher than that for acute calculous cholecystitis.
D. The disease has been treated successfully by percutaneous cholecystostomy.
Answer: ABCD
32. True statements about the surgical management of patients with acute calculous cholecystitis include:
A. Operation should be performed in all patients as soon as the diagnosis is made.
B. Antibiotic therapy should be initiated as soon as the diagnosis is made.
C. Dissection of the gallbladder is facilitated by decompression of the organ with the use of a trocar.
D. An operative cholangiogram should be done in every patient.
Answer: BC
33. Which of the following are indications for cholecystectomy?
A. The presence of gallstones in a patient with intermittent episodes of right-side upper quadrant pain.
B. The presence of gallstones in an asymptomatic patient.
C. The presence of symptomatic gallstones in a patient with angina pectoris.
D. The presence of asymptomatic gallstones in a patient who has insulin-dependent diabetes.
Answer: A
34. Which of the following statements about laparoscopic cholecystectomy are correct?
A. The procedure is associated with less postoperative pain and earlier return to normal activity.
B. The incidence of bile duct injury is higher than for open cholecystectomy.
C. Laparoscopic cholecystectomy should be used in asymptomatic patients because it is safer than open cholecystectomy.
D. Pregnancy is a contraindication.
Answer: AB
35. Which of the following statements about cholangitis are correct?
A. Charcot's triad is always present.
B. Associated biliary tract disease is always present.
C. Chills and fever are due to the presence of bacteria in the bile duct system.
D. The most common cause of cholangitis is choledocholithiasis.
Answer: BCD
36. Recurrent episodes of cholangitis:
A. Suggest the presence of undetected or overlooked bile duct pathology.
B. Occur frequently in patients who have indwelling biliary tubes or stents.
C. May be ameliorated by long-term administration of antibiotics.
D. May be associated with the development of secondary biliary cirrhosis.
Answer: ABCD
37. The initial goal of therapy for acute toxic cholangitis is to:
A. Prevent cholangiovenous reflux by decompressing the duct system.
B. Remove the obstructing stone, if one is present.
C. Alleviate jaundice and prevent permanent liver damage.
D. Prevent the development of gallstone pancreatitis.
Answer: A
38. The clinical picture of gallstone ileus includes which of the following?
A. Air in the biliary tree.
B. Small bowel obstruction.
C. A stone at the site of obstruction.
D. Acholic stools.
E. Associated bouts of cholangitis.
Answer: ABCE
39. Which of the following statement(s) about gallstone ileus is/are not true?
A. The condition is seen most frequently in women older than 70.
B. Concomitant with the bowel obstruction, air is seen in the biliary tree.
C. The usual fistula underlying the problem is between the gallbladder and the ileum.
D. When possible, relief of small bowel obstruction should be accompanied by definitive repair of the fistula since there is a significant incidence of recurrence if the fistula is left in place.
E. Ultrasound studies may be of help in identifying a gallstone as the obstructing agent.
Answer: C
40. Which of the following lesions are believed to be associated with the development of carcinoma of the gallbladder?
A. Cholecystoenteric fistula.
B. A calcified gallbladder.
C. Adenoma of the gallbladder.
D. Xanthogranulomatous cholecystitis.
E. All of the above.
Answer: E
41. The preferred treatment for carcinoma of the gallbladder is:
A. Radical resection that includes gallbladder in continuity with the right hepatic lobe and regional lymph node dissection.
B. Radiation therapy.
C. Chemotherapy.
D. Combined treatment involving surgical therapy, chemotherapy, and radiation.
E. None of the above.
Answer: E
42. Which of the following statement(s) about pancreatic embryonic malformations is/are correct?
A. Pancreas divisum can be a cause of gastrointestinal bleeding.
B. Heterotopic pancreatic tissue predisposes to pancreatic adenocarcinoma.
C. Annular pancreas may cause gastrointestinal obstruction in children or in adults.
D. Relative obstruction to the flow of pancreatic juice through the minor papilla appears to be the cause of pancreatitis in some patients with pancreas divisum.
Answer: CD
43. The pancreas occupies a retroperitoneal position in the upper abdomen. Which statement(s) is/are correct?
A. The superior mesenteric vein and the splenic vein join to form the portal vein posterior to the neck of the pancreas.
B. The uncinate process of the pancreas extends posterior to the inferior vena cava.
C. The tail of the pancreas extends to the left of the aorta, toward the splenic hilum.
D. The head of the pancreas is jointly supplied by arterial blood from the celiac axis and the superior mesenteric artery.
Answer: ACD
44. Both endocrine and exocrine tissue comprise the pancreas. Which statement(s) is/are true?
A. The islets of Langerhans total 1 million per gland and drain their secretions via intercalated duct cells through the ampulla of Vater.
B. Islet alpha cells produce glucagon.
C. Islet sigma cells produce somatostatin.
D. The acini and ductal systems constitute the exocrine portion of the pancreas.
Answer: BD
45. Pancreatic exocrine secretory products include a bicarbonate-rich electrolyte solution as well as digestive enzymes. Which of the following statement(s) is/are true?
A. Cholecystokinin (CCK) is the most potent endogenous stimulant of pancreatic enzyme secretion.
B. The chloride and bicarbonate concentrations of pancreatic juice vary and depend on the secretory flow rate.
C. Secretin is the most potent endogenous stimulant of pancreatic water and electrolyte secretion.
D. The peptidases synthesized by acinar cells are released into the pancreatic duct system in active form.
Answer: ABC
46. Which of the following parameters is/are not included in the Ranson's prognostic signs useful in the early evaluation of a patient with acute pancreatitis?
A. Elevated blood glucose.
B. Leukocytosis.
C. Amylase value greater than 1000 U per dl.
D. Serum lactic dehydrogenase (LDH) greater than 350 IU per dl.
E. Alanine aminotransferase greater than 250 U per dl.
Answer: CE
47. Standard supportive measures for patients with mild pancreatitis include the following:
A. Intravenous fluid and electrolyte therapy.
B. Withholding of analgesics to allow serial abdominal examinations.
C. Subcutaneous octreotide therapy.
D. Nasogastric decompression.
E. Prophylactic antibiotics.
Answer: A
48. Which of the following statements about chronic pancreatitis is/are correct?
A. Chronic pancreatitis is the inevitable result after repeated episodes of acute pancreatitis.
B. Patients with chronic pancreatitis commonly present with jaundice, pruritus, and fever.
C. Mesenteric angiography is useful in the evaluation of many patients with chronic pancreatitis.
D. Total pancreatectomy usually offers the best outcome in patients with chronic pancreatitis.
E. For patients with disabling chronic pancreatitis and a dilated pancreatic duct with associated stricture formation, a longitudinal pancreaticojejunostomy (Peustow procedure) is an appropriate surgical option.
Answer: E
49. Which of the following statements about pancreatic ascites is/are correct?
A. Patients typically present with painful ascites, reflecting the release of toxic pancreatic enzymes into the peritoneal cavity.
B. The standard evaluation of a patient with new-onset ascites includes abdominal paracentesis. In cases of pancreatic ascites, the peritoneal fluid contains high concentrations of both amylase and protein.
C. Pancreatic ascites can follow an episode of acute pancreatitis.
D. Patients with pancreatic ascites may fail to improve with nonoperative therapy and require surgical procedures. At abdominal exploration an acceptable approach to the pancreatic duct disruption involves suture ligation with omental patching.
Answer: BC
50. Which of the following statements about adenocarcinoma of the pancreas is/are correct?
A. It is the fifth most common cause of cancer death in the U.S.
B. Most cases occur in the body and tail of the pancreas, making distal pancreatectomy the most commonly performed resectional therapy.
C. For cancers of the head of the pancreas resected by pancreaticoduodenectomy, prognosis appears to be independent of nodal status, margin status, or tumor diameter.
D. The most accurate screening test involves surveillance of stool for carbohydrate antigen (CA 19–9).
Answer: A
51. A 35-year-old woman presents with episodes of obtundation, somnolence, and tachycardia. An insulinoma is suspected based on a random serum glucose test value of 38 mg. per dl. Which of the following statements is/are true?
A. The most important diagnostic study for insulinoma is an oral glucose tolerance test.
B. It may be helpful to perform ERCP in an effort to localize the tumor.
C. Most patients with insulinoma present with extensive disease, rendering them only rarely resectable or curable.
D. An important component of the preoperative evaluation in patients with presumed insulinoma involves confirming elevated C-peptide or proinsulin levels and screening for anti-insulin antibodies.
Answer: D
52. Which of the following statements about gastrinoma (Zollinger-Ellison syndrome) is/are correct?
A. As many as 75% of gastrinoma patients have sporadic disease; 25% have gastrinoma associated with multiple endocrine neoplasia type 1 (MEN 1).
B. Extrapancreatic gastrinomas are common, and exploration should include careful assessment of the duodenum and peripancreatic lymph nodes.
C. Diarrhea may be a prominent presenting feature of some patients with gastrinoma.
D. Before elective operation acid-reducing medications such as omeprazole should be administered.
Answer: ABCD
53. With regard to the control of pancreatic exocrine function, which of the following statement(s) is/are correct?
a. Cholecystokinin, a hormone released from the duodenal mucosa, is the predominant stimulus for pancreatic enzyme secretion
b. Gastrin is a major stimulant for pancreatic bicarbonate secretion
c. Secretin is released from the duodenum upon mucosal acidification and stimulates pancreatic bicarbonate secretion
d. Acetylcholine, released from pancreatic nerves, stimulates enzyme secretion
Answer: a, c, d
54. In the performance of a pancreaticoduodenectomy (Whipple procedure), the superior mesenteric vein is an important landmark. Which of the following statements is/are true with regard to the superior mesenteric vein?
a. Small venous branches enter the superior mesenteric vein anteriorly as it courses beneath the neck of the pancreas
b. The superior mesenteric vein joins the splenic vein at the superior border of the pancreas to form the portal vein
c. Small venous branches enter the superior mesenteric vein laterally as it courses beneath the neck of the pancreas
d. The superior mesenteric vein courses anterior to the neck of the pancreas
Answer: b, c
55. Pancreas divisum results from incomplete fusion of the ventral pancreatic duct with the dorsal pancreatic duct during embryologic development. Which of the following statements correctly describes pancreas divisum?
a. The body and tail of the pancreas drain via an accessory ampulla distal to the ampulla of Vater. The uncinate process drains via the ampulla of Vater
b. The entire pancreatic ductal system drains via the ampulla of Vater
c. The entire pancreatic ductal system drains via an accessory ampulla proximal to the ampulla of Vater
d. The body and tail of the pancreas are absent. The uncinate process drains via the ampulla of Vater
Answer: c
56. Which of the following statements is/are correct with regard to the blood supply of the pancreas?
a. The inferior pancreaticoduodenal artery, a branch of the celiac artery, divides into anterior and posterior branches to supply the pancreatic head
b. The body and tail of the pancreas are supplied by branches of the splenic artery
c. The superior pancreaticoduodenal artery is a branch of the gastroduodenal artery
d. The body and tail of the pancreas are supplied by branches derived from the left renal artery
Answer: b, c
57. Orally administered glucose provokes a greater insulin response than an equivalent amount of intravenously administered glucose. The incremental response to ingested glucose is due to the effects of which of the following hormones?
a. Gastric inhibitory peptide
b. Somatostatin
c. Pancreatic polypeptide
d. Secretin
Answer: a
58. The islets of Langerhans contain four major endocrine cell types that secrete which of the following hormones?
a. Insulin, somatostatin, glucagon, secretin
b. Insulin, somatostatin, cholecystokinin, pancreatic polypeptide
c. Insulin, somatostatin, glucagon, pancreatic polypeptide
d. Insulin, secretin, glucagon, cholecystokinin
Answer: c
59. A 50-year-old man develops acute pancreatitis due to alcohol abuse. Hyperamylasemia resolves by the third day after admission. By the eighth hospital day, the patient is noted to have recurrent fever (38.5°C), progressive leukocytosis (18,500 WBC/mm3), and tachypnea. The most appropriate management includes which as the next step?
a. Laparotomy with pancreatic debridement
b. CT guided aspiration of peripancreatic fluid collections
c. ERCP with sphincterotomy and placement of biliary stent
d. Intravenous amphotericin B
Answer: b
60. The patient in the above question is treated by observation for 8 weeks. He continues to be symptomatic with epigastric pain. A repeat abdominal CT scan reveals a persistent 6 cm pseudocyst in the region of the body of the pancreas. The pseudocyst is unilocular and demonstrates a well-defined rim of fibrous tissue. The gastric antrum is displaced anteriorly. Using CT guidance, 300 ml of fluid is aspirated from the lesion which is shown to be collapsed radiographically. No further intervention is performed. What is the risk of pseudocyst recurrence after simple aspiration?
a. 80–85%
b. 60–65%
c. 40–45%
d. 20–25%
Answer: d
61. In prospective, randomized trials which of the following agents or therapeutic measures has/have been demonstrated to accelerate recovery from acute pancreatitis?
a. Peritoneal lavage
b. Anticholinergic blockade
c. Octreotide
d. H2 receptor blockade
e. None of the above
Answer: e
62. Which of the following medical procedures has/have been associated with an increased risk of post-procedure acute pancreatitis?
a. Common bile duct exploration
b. Endoscopic retrograde cholangiopancreatography
c. Coronary bypass grafting
d. Distal gastrectomy
Answer: a, b, c, d
63. A 42-year-old male develops acute pancreatitis in the setting of acute alcohol abuse. One week after onset of symptoms, computed tomography of the abdomen reveals a pancreatic phlegmon and associated pseudocyst. Which of the following factors, if present, would decrease the likelihood of spontaneous resolution of the pseudocyst?
a. Size greater than 5 cm
b. Diffuse calcification of the pancreatic gland
c. Multilocularity
d. Location in the pancreatic tail
Answer: a, b, c
64. Which of the following is/are prognostic signs reported by Ranson to predict outcomes associated with acute pancreatitis?
a. Age greater than 60 years
b. Hematocrit decrease of 105 within 48 hours of hospital admission
c. Serum amylase value greater than 4 times upper limit of normal
d. Serum glucose greater than 200 mg/dL on admission
e. Ca2+ level less than 8 mg/dL within 48 hours of hospital admission
Answer: b, d, e
65. A 36-year-old woman is admitted to a the hospital with upper abdominal pain, hyperamylasemia, elevation of serum alkaline phosphatase and ultrasound evidence of cholelithiasis. With intravenous hydration and analgesia, symptoms rapidly resolved. After 48 hours, serum amylase and alkaline phosphatase values had returned to normal and physical examination revealed lessening tenderness in the right upper quadrant of the abdomen. Appropriate management consists of which of the following as the next step?
a. Cholecystectomy and intraoperative cholangiography before hospital discharge
b. Elective cholecystectomy at approximately 8 weeks
c. Endoscopic sphincterotomy before discharge followed by cholecystectomy at approximately 8 weeks
d. Observation
Answer: a
66. For the patient in the preceding question, symptomatic recurrence at 3 weeks after aspiration is confirmed ultrasonographically. Endoscopic retrograde pancreatography does not demonstrate communication of a major pancreatic duct with the pseudocyst. Appropriate management includes which of the following?
a. Pancreatectomy to include the pseudocyst
b. Cystgastrostomy
c. Repeat aspiration followed by injection of sodium morrhuate into the pseudocyst cavity
d. Pancreatic debridement followed by external drainage
Answer: b
67. With regard to acute pancreatitis: which of the following statements is/are correct?
a. The majority of patients presenting with acute pancreatitis of biliary type are female
b. The majority of patients presenting with acute pancreatitis of alcoholic type are female
c. The most common cause of acute pancreatitis in the United States is alcohol use
d. Patients with alcohol-induced pancreatitis tend to be older than those with biliary-induced disease
Answer: a, c
68. Which of the following statement(s) relating to chronic pancreatitis is/are correct?
a. In the United States, the most common cause of chronic pancreatitis is alcohol abuse
b. Approximately 50% of chronic alcoholics develop chronic pancreatitis
c. Clinically significant chronic pancreatitis develops on average after five years of alcohol abuse in men
d. The risk of alcohol-induced chronic pancreatitis can be decreased by consumption of a high-protein diet
Answer: a
69. The most appropriate test to confirm a clinical diagnosis of early chronic pancreatitis is which of the following?
a. Serum amylase determination
b. Calculation of urinary amylase clearance
c. Measurement of para-aminobenzoic acid absorption
d. Endoscopic retrograde cholangiopancreatography
Answer: d
70. A 52-year-old male, known to be alcoholic, is evaluated because of chronic abdominal pain. The clinical diagnosis of chronic pancreatitis is supported by ERCP findings of pancreatic ductal ectasia with alternating areas of stricture and dilatation. Several pancreatic ductal stones are also noted. With chronic pain as the operative indication, the most appropriate procedure would be:
a. 80% distal pancreatectomy with splenectomy
b. Longitudinal pancreaticojejunostomy
c. Distal pancreatectomy with end pancreaticojejunostomy
d. Total pancreatectomy
Answer: b
71. For the patient in the preceding question, the most appropriate long-term management is which of the following?
a. Endoscopic stenting of the distal common bile duct
b. Choledochoduodenostomy
c. Pancreaticoduodenectomy (Whipple procedure)
d. Percutaneous transhepatic drainage of the common hepatic duct
Answer: b
72. Which of the following is the most common cause of obstructive jaundice in patients with chronic pancreatitis?
a. Adenocarcinoma of the head of the pancreas
b. Choledocholithiasis
c. Fibrotic stricture of the common bile duct
d. Pancreatic pseudocyst formation
Answer: c
73. Alcohol-induced and hereditary chronic pancreatitis are the two most common etiologies observed in North American patients. Most of the remaining patients fall into which of the following categories?
a. Chronic pancreatitis secondary to hyperparathyroidism
b. Chronic pancreatitis caused by protein-calorie malnutrition
c. Chronic pancreatitis secondary to congenital pancreatic ductal obstruction
d. Idiopathic chronic pancreatitis
Answer: d
74. Which of the following statements regarding prognosis in chronic pancreatitis is/are correct?
a. Patients with chronic pancreatitis have decreased long-term survival compared with the general population
b. Patients with chronic pancreatitis exhibit no excess mortality relative to the general population
c. Excess mortality in patients with chronic pancreatitis is related to cancers of the aerodigestive system, complications of diabetes, and complications of cirrhosis
d. Excess mortality in patients with chronic pancreatitis is due to development of adenocarcinoma of the pancreas and to the complications of recurrent pancreatitis
Answer: a, c
75. Which of the following is the most common clinical manifestation of chronic pancreatitis?
a. Epigastric pain with radiation to the hypogastrium
b. Diabetes mellitus
c. Steatorrhea
d. Epigastric pain with radiation to the upper lumbar vertebrae
Answer: d
76. For the patient in the preceding question, appropriate management includes which of the following?
a. Distal pancreatectomy
b. Cystjejunostomy
c. Percutaneous drainage
d. Primary radiotherapy and chemotherapy
Answer: a
77. A 72-year-old man develops jaundice and is demonstrated to have a 2.5 mass in the pancreatic head by computed tomography. There are no signs of unresectability on CT examination. Fine needle aspiration cytology is positive for adenocarcinoma. Which of the following intraoperative findings would indicate unresectability?
a. Fibrotic reaction in the body and tail of the pancreas
b. Microscopic tumor cells in perigastric lymph nodes on frozen section
c. Inability to develop an avascular plane anterior to the superior mesenteric vein
d. Cholelithiasis
Answer: b, c
78. A 67-year-old male presents with complaints of itching, dark urine, and epigastric pain. Physical examination reveals jaundice. Initial laboratory tests show total bilirubin of 6.5 mg/dL, alkaline phosphatase elevated at 3 the upper limit of normal, and mild elevations in serum transaminases. Appropriate management includes which diagnostic test next?
a. Abdominal ultrasonography
b. Computed tomography of the abdomen
c. Magnetic resonance imaging of the abdomen
d. Endoscopic retrograde cholangiography
Answer: a
79. Which of the following statements regarding ductal adenocarcinoma of the pancreas is/are correct?
a. For ductal adenocarcinoma, 60–70% of tumors arise in the head of the gland, 15% in the body, and 10% in the tail, the remainder are diffuse
b. Fifty percent of pancreatic adenocarcinomas involve the gland diffusely at the time of diagnosis
c. For ductal adenocarcinomas, tumors of the body and tail are usually larger at the time of diagnosis than those arising in the head of the gland
d. Pancreatic adenocarcinomas occur with equal frequency within the head, body, and tail of the gland
Answer: a, c
80. The most common cause of death in the postoperative period following pancreaticoduodenectomy is which of the following?
a. Myocardial infarction
b. Intraperitoneal hemorrhage
c. Pulmonary embolism
d. Pneumonia
Answer: b
HEPATOBILIARY & PANCREATIC SURGERY Objective Type Questions with Answers ::
81. For the above patient, ultrasonography reveals dilated extrahepatic and intrahepatic bile ducts and the absence of gallstones within the gallbladder. A 2 cm mass within the pancreatic head is visualized. Computed tomography of the abdomen is performed. Which of following CT findings indicate probable unresectability?
a. Common bile duct diameter of 2 cm
b. Ascites
c. Infiltration of the transverse colonic mesentery
d. Dilatation of the main pancreatic duct to 1.5 cm
Answer: b, c
82. Which of the following have been shown to be risk factors for development of adenocarcinoma of the pancreas?
a. Cigarette smoking
b. Coffee drinking
c. Adult-onset diabetes mellitus
d. Chronic coumadin usage
e. Prior gastrectomy
Answer: a, e
83. Which of the following surgical procedures has the lowest incidence of recurrent jaundice when used in the context of unresectable carcinoma of the head of the pancreas?
a. Choledochoduodenostomy
b. Cholecystojejunostomy
c. Cholecystoduodenostomy
d. Choledochojejunostomy
Answer: d
84. A 45-year-old woman is evaluated for epigastric and back pain. Physical examination is normal. Computed tomography of the abdomen reveals a 8 cm cystic lesion in the region of the tail of the pancreas. The cyst demonstrates internal septations and papillary projections from its walls. Which of the following diagnoses is most likely in this patient?
a. Pancreatic lymphoma
b. Retroperitoneal liposarcoma
c. Pancreatic pseudocyst
d. Pancreatic mucinous cystadenoma
Answer: d
85. A 45-year-old woman develops upper gastrointestinal hemorrhage. Evaluation by upper endoscopy reveals three ulcers in the second portion of the duodenum. Bleeding is controlled using an endoscopic heat probe. Further investigation reveals a serum gastrin value of 240 pg/mL. Which of the following would support the presumptive diagnosis of gastrinoma?
a. An increase of 320 pg/mL in serum gastrin upon intravenous infusion of secretin
b. Gastric acid analysis demonstrating fasting acid secretion of 3 mEq/h
c. Enlarged gastric rugae on upper gastrointestinal contrast study
d. An increase of 150 pg/mL in serum gastrin upon intravenous infusion of cholecystokinin
Answer: a, c
86. For the patient in the preceding question, an insulin/glucose ratio of 0.5 was documented at 28 hours of fasting. Symptoms of mental obtundation developed concurrently and were reversed by oral glucose administration. Endoscopic ultrasonography demonstrated a 1.2 cm mass in the head of the pancreas. Appropriate management consists of which of the following?
a. Surgical enucleation of the tumor
b. Total pancreatectomy
c. Long-term octreotide administration
d. Primary radiotherapy
Answer: a
87. A 35-year-old woman is evaluated for seizure disorder, mental obtundation, and personality change. Physical examination is normal. Fasting serum glucose is 44 mg/dL. Other serum values are normal. Subsequent investigations should include which of the following?
a. Oral glucose tolerance test
b. Determination of fasting insulin/glucose ratios
c. Assay of serum C-peptide levels
d. Determination of serum prolactin levels
Answer: b, c
88. The most common location(s) for development of gastrinoma is/are which of the following?
a. Pancreas to the right of the superior mesenteric vein
b. Pancreatic body and tail
c. Gastric antrum
d. Duodenum
Answer: a, d
89. Neoplastic hypersecretion of the hormone vasoactive intestinal peptide is associated with which of the following features?
a. Hypokalemia, hypochlorhydria, diarrhea
b. Hyperglycemia, necrolytic rash, hypoaminoacidemia
c. Constipation, gallstones, hyperglycemia
d. Hyperkalemia, necrolytic rash, diarrhea
Answer: a
90. A patient with biochemically confirmed gastrinoma undergoes computed tomography for tumor localization. CT reveals a 2 cm mass in the head of the pancreas and multiple nodules within right and left lobes of the liver. Appropriate management includes which of the following?
a. Omeprazole administration
b. Radiotherapy
c. Pancreaticoduodenectomy
d. Proximal gastric vagotomy
Answer: a
91. The following statement(s) is/are true concerning the widely accepted French or Couinaud’s nomenclature for liver anatomy.
a. The liver is divided into eight discrete segments based on portal pedicle branches and hepatic venous drainage
b. This anatomy is particularly useful in allowing less than lobar segmental anatomical resections that minimize blood loss and loss of hepatic reserve
c. Enumeration of the system begins from right to left
d. Segments II and III are synonymous with the left lateral segment based on English nomenclature
Answer: a, b, d
92. In the patient described above, which of the following are important operative steps in the performance of a right hepatic lobectomy?
a. The use of an ultrasonic dissector is essential for division of the hepatic parenchyma
b. If temporary portal inflow occlusion is used (Pringle maneuver), it is not necessary to reestablish blood flow during the course of the parenchymal division
c. The greater omentum may be used to buttress the transected liver edge
d. Control of the main right hepatic vein should eliminate all forms of venous drainage
Answer: c
93. Intraoperative ultrasound is now commonly used by the hepatic surgeon. Which of the following statement(s) is/are true concerning intraoperative ultrasound and hepatic surgery?
a. An intraoperative ultrasound offers no advantage to conventional transcorporial ultrasound in detection of hepatic lesions
b. Portal structures can be differentiated from hepatic veins by the extension of Glisson’s capsule surrounding these structures
c. It is difficult on ultrasound to differentiate a vascular structure from a mass
d. The short hepatic veins are difficult to detect with intraoperative ultrasound
Answer: b
94. The following statement(s) is/are true concerning hepatic anatomical nomenclature.
a. In the traditional English system, the right lobe is divided into anterior and posterior segments by an intersegmental line with no topographic landmarks or interparenchymal septi
b. The caudate lobe in the French or Couinaud’s nomenclature is referred to as segment I
c. The right lobe of the liver by English nomenclature is subdivided in the French system into segments V–VIII
d. In the English system, the left lobe of the liver is divided into the medial segment and lateral segment by the falciform ligament
Answer: a, b, c, d
95. A 57-year-old man with a history of Duke’s C colon cancer is being evaluated for a rising CEA. Which of the following statement(s) is/are correct concerning the use of CT scanning for this indication?
a. Conventional CT scanning will detect lesions well below 1 cm in size
b. CT arterio-portography involves immediate CT scanning after direct injection into both the common hepatic artery and superior mesenteric artery
c. A double helical (spiral) CT scan may eliminate the need for invasive angiography
d. Magnetic resonance imaging of the liver will add little to the workup of this patient
Answer: b, c, d
96. A solitary 6 cm lesion is identified in the right hepatic lobe in the patient described above. Which of the following statement(s) is/are true concerning the initial operative management?
a. To facilitate mobilization and assessment with intraoperative ultrasound, complete mobilization including dividing the left and right triangular ligaments would be necessary
b. In dividing the right triangular ligament, care must be taken to avoid injury to accessory right hepatic veins draining directly into the vena cava
c. Unless a considerable length of hepatic vein is found outside the hepatic parenchyma, early hepatic vein ligation should be avoided
d. Ligation of the portal arterial structures is always necessary before proceeding with hepatic lobectomy
Answer: a, b, c
97. Which of the following statement(s) is/are true concerning the arterial venous anatomy of the liver?
a. Most commonly, the right, left, and middle hepatic veins join the inferior vena cava as a separate trunk
b. Most frequently, the entire length of each hepatic vein is within the parenchyma of the liver
c. A replaced right hepatic artery may be placed in jeopardy during performance of a pancreaticoduodenectomy
d. There is little collateral arterial circulation between the right and left hepatic lobes
Answer: b, c
98. The liver plays a vital role in carbohydrate metabolism and regulation of blood glucose. The following statement(s) is/are true concerning carbohydrate metabolism by the liver.
a. Glycogen, a complex polymer of glucose, is synthesized by the hepatocyte in a remarkably energy efficient process
b. Glucagon stimulates glycogenesis
c. Glycolysis, the process by which glucose is converted to two molecules of pyruvate, occurs in the liver mitochondria
d. If glycogen stores become depleted, the liver is capable of synthesizing new glucose by the process of gluconeogenesis, which is stimulated by insulin
Answer: a
99. Transport of substances from the blood into the hepatocyte occurs through the sinusoidal membrane. The following statement(s) is/are true concerning this plasma membrane.
a. The high lipid content of this phospholipid bilayer allows lipid-soluble molecules to enter the cell by simple diffusion
b. Carrier proteins within the phospholipid bilayer bind to a solute in blood and by conformational change allow it to be transported into the cell
c. Large glycoprotein molecules of the sinusoidal membrane known as receptors always transport the binding ligand into the cell
d. The transmission of a signal to the interior of the cell by receptor-ligand binding which generates intracellular second messengers is known as signal transduction
Answer: a, b, d
100. The liver is an important site of protein metabolism. Which of the following statement(s) is/are true concerning protein metabolism by the liver?
a. Amino acids are taken up by hepatocytes by active transport mechanisms and are generally stored long-term for later synthetic activity
b. Under certain conditions the amine group is removed from the amino acids in the liver and the carbon chain used for carbohydrate, lipid, or nonessential amino acid synthesis
c. The most important route of detoxification of ammonia formed as the result of deamination of amino acids is via excretion of ammonia into the urine
d. Proteins synthesized by the liver include albumin, transferrin, fibrinogen, and apolipoproteins
e. Albumin is a sensitive indicator of hepatic synthetic function
Answer: b, d
101. The following statement(s) is/are true concerning hepatic blood flow.
a. Although constituting only 2.5% of total body weight, the liver receives 25% of the cardiac output
b. Hepatic blood flow is equally derived from the portal vein and hepatic artery
c. The liver serves as a physiologic blood reservoir either releasing blood back into the systemic circulation at times of acute blood loss or in situations of volume overload serving as a site of extra blood storage
d. An important function of the liver is to filter particulate debris which is performed by phagocytic Kupffer cells which line the hepatic sinusoidal endothelium
Answer: a, c, d
102. The liver synthesizes key metabolites essential for the production of fuel substrates for other organs. These key metabolites include:
a. Glucose-6-phosphate (G6P)
b. Acetyl CoA
c. Pyruvate
d. Oxaloacetate
Answer: a, b, c
103. The following statement(s) concerning hepatic bile formation/secretion is/are true.
a. The adult human liver secretes less than 1000 cc of bile daily
b. Most bile is secreted by hepatocytes (canalicular bile)
c. Primary bile acids include cholic acid, chenodeoxycholic acid, and deoxycholic acid
d. The enterohepatic circulation is tremendously efficient in reabsorption of intestinal bile acids
e. Bile acids are the primary determinant of bile flow
Answer: b, d, e
104. The following statement(s) is/are true containing lipid metabolism in the liver.
a. Hepatic mitochondrial hydrolysis of fatty acids is a tremendous source of ATP
b. Significant hepatic storage of triglyceride or fatty infiltration can cause hepatic fibrosis or necrosis
c. Approximately 90% of cholesterol synthesis occurs in the liver
d. Most cells in the body are capable of phospholipid synthesis, therefore the liver plays a minimal role in this process
Answer: a, c
105. Hepatic biotransformation is defined as the intracellular metabolism of endogenous and exogenous organic compounds. Which of the following is/are enzyme families responsible for hepatic bile transformation?
a. Cytochromes P-450
b. UDB-glucuronyl transferases
c. Glutathione-transferases
d. Sulfotransferases
Answer: a, b, c, d
106. The following statement(s) is/are true concerning the differential diagnosis between an amoebic and a pyogenic liver abscess.
a. The clinical presentation is often clearly distinguishable
b. A history of travel or origin from a high risk area might suggest an amebic liver abscess
c. Routine liver chemistries frequently can distinguish pyogenic from amoebic liver abscess
d. Serologic testing for the presence of antibody to entamoeba histolyctica is the only specific and sensitive way to confirm the diagnosis of amoebic liver abscess
e. Distinguishing pyogenic from hepatic abscesses preoperatively is not important since surgical drainage is imperative for both
Answer: b, d
107. A patient is found to develop evidence of hepatitis approximately eight weeks after receiving blood transfusions during a surgical procedure. Which of the following statement(s) is/are true?
a. The virus responsible is most likely hepatitis C
b. A chronic carrier state will ultimately develop in most patients
c. There is no role for interferon in the treatment of chronic hepatitis C viral infection
d. Chronic infection with hepatitis C is not associated with an increased risk of developing hepatocellular carcinoma
Answer: a, b
108. A surgeon is suspected of having contacted hepatitis B virus via needle stick. Which of the following statement(s) is/are true concerning his diagnosis and outcome?
a. Incubation of hepatitis B virus is about two weeks
b. Jaundice is the first serologic indicator of hepatitis B infection
c. The patient has about a 10% chance of developing a chronic carrier state
d. All susceptible household of the surgeon should receive hepatitis B viral vaccine
e. The surgeon should receive hepatitis B immunoglobulin as soon as possible after the accidental needle stick
Answer: c, d, e
109. The following statement(s) is/are true concerning the diagnosis and treatment of hydatid cysts.
a. Percutaneous aspiration is an important aspect of diagnosis and treatment of a hydatid cyst
b. CT scan will oftentimes show the classic findings of a cystic liver lesion with a calcific rim
c. At operation, care must be taken to protect the operative field from spillage of the cyst fluid
d. The use of a scoleocide has become obsolete with current surgical techniques
Answer: b, c
110. Which of the following statement(s) is/are true concerning treatment of pyogenic liver abscess?
a. Antibiotic therapy alone may be advisable in patients with multiple small abscesses
b. Percutaneous drainage provides comparable results to surgical drainage in patients with unilocular large abscesses
c. Sufficient antibiotic coverage for most hepatic abscesses includes coverage for gram-positive aerobic bacteria only
d. In patients with a primary biliary origin for the hepatic abscess, treatment must also be addressed at underlying biliary pathology such as choledocholithiasis or biliary ductal obstruction
Answer: a, b, d
111. Which of the following statement(s) is/are true concerning acute, fulminant hepatic failure?
a. The most frequent cause of acute hepatic failure world-wide is hepatitis B infection
b. Higher grades of encephalopathy are associated with a worse prognosis
c. Hypoglycemia is a common complication of all liver diseases
d. Liver transplantation would appear indicated in all patients with hepatic coma secondary to acute liver failure
Answer: b
112. Which of the following statement(s) is/are true concerning the natural history and clinical features of alcoholic cirrhosis?
a. In patients with compensated cirrhosis, the probability of survival at 10 years approaches 50%
b. The development of clinical evidence of hepatic decompensation reduces five year survival to less than 20%
c. Continued consumption of alcohol worsens prognosis
d. The risk of death after variceal hemorrhage depends more on the severity of underlying liver disease than the type of therapy
Answer: a, b, c, d
113. Which of the following statement(s) is/are true concerning the morphologic and histologic findings of cirrhosis?
a. Micronodular cirrhosis is a pattern typical of chronic alcoholic liver disease
b. Mallory bodies and megamitochondria are typical findings of alcoholic cirrhosis
c. Bile leaks caused by rupture of bile ducts with extravasation of bile into portal triads is a common finding in post-necrotic cirrhosis secondary to hepatitis
d. Large regenerating nodules separated by coarse irregular scars in piecemeal parenchyma necrosis is common in liver disease secondary to chronic active hepatitis
Answer: a, b, d
114. The following statement(s) is/are true concerning the management of ascites associated with chronic liver disease.
a. Spontaneous bacterial peritonitis is an insignificant complication
b. Large volume paracentesis is unsafe due to excessive volume loss from the intervascular space
c. Peritoneovenous shunting is a trivial surgical procedure with minimal perioperative morbidity and mortality
d. Transjugular intrahepatic portosystemic shunts (TIPS) can effectively treat ascites in patients refractory to conventional medical therapy
Answer: d
115. Which of these statement(s) is/are true concerning the etiologic factors in the development of cirrhosis?
a. Viral hepatitis of any type (A, B, or non-A, non-B) can all progress to cirrhosis
b. Acetaminophen can cause acute liver failure and necrosis but will not lead to cirrhosis
c. Alcohol exerts toxic effects on the liver via reactive intermediates such as acetaldehyde
d. Long-standing congestive heart failure can lead to cirrhosis secondary to centrilobular congestion, hemorrhage, and necrosis
Answer: c, d
116. Important spontaneous portosystemic collaterals which develop in the face of portal hypertension include:
a. The hemorrhoidal veins
b. Left renal vein
c. The paraumbilical venous plexus
d. The coronary, short gastric, and paraesophageal veins
Answer: a, b, c, d
117. Which of the following statement(s) is/are true concerning the pathophysiology of variceal hemorrhage?
a. All patients with portal hypertension will develop esophageal varices
b. All patients with esophageal varices eventually bleed
c. Variceal size can predict the incidence of variceal hemorrhage
d. Control of acid secretion by H2 blockade can decrease the incidence of rebleeding after esophageal hemorrhage
e. None of the above
Answer: e
118. Which of the following statement(s) is/are true concerning the use of transjugular intrahepatic portosystemic shunts (TIPS) in the treatment of variceal bleeding?
a. This procedure effectively creates an end-to-side portocaval shunt
b. Procedure-related mortality is generally in excess of 20%
c. TIPS has been used successfully as a pretransplant procedure to reduce portal pressure
d. The placement of a TIPS is not associated with the development of encephalopathy
Answer: c
119. Hepatic encephalopathy is a common systemic manifestation of chronic liver disease. Which of the following statement(s) is/are true concerning this condition?
a. Blood ammonia levels correlate well with the stage of hepatic encephalopathy
b. Alterations in central nervous system neurotransmitters such as the neurotransmitter g- aminobutyric acid (GABA) have been proposed in the pathogenesis of hepatic encephalopathy
c. Lactulose can be used to decrease intestinal ammonia absorption
d. Patients can be expected to have an increased sensitivity to benzodiazepines
Answer: b, c, d
120. Which of the following statement(s) is/are true concerning the management of gastroesophageal variceal hemorrhage?
a. Vasopressin decreases portal pressure through the process of splanchnic vasoconstriction
b. Somatostatin is as effective as vasopressin but without the cardiac side effects
c. Balloon tamponade provides good long-term control of bleeding esophageal varices
d. Endoscopic sclerotherapy is more effective than conservative medical therapy in the treatment of bleeding esophageal varices
e. Sclerotherapy, although excellent for the control of bleeding short-term, does not prolong overall survival
Answer: a, b, d
121. Which of the following statement(s) is/are true concerning the surgical management of bleeding esophageal varices.
a. A side-to-side portacaval shunt may be associated with the development of hepatofugal blood flow
b. Selective shunts preserve prograde (hepatopedal) blood flow while decompressing esophageal varices or reducing portal pressure
c. The presence of intractable ascites is a contraindication to the Warren shunt
d. If the patient is considered a liver transplant patient, an interposition mesocaval shunt is a suitable alternative
Answer: a, b, c, d
122. Which of the following statement(s) is/are true concerning the results of portosystemic shunting?
a. When comparing shunts with nonshunting procedures, only minor differences in long-term survival are reported, but the mode of death usually changes
b. Distal splenorenal shunts are associated with the development of less hepatic encephalopathy
c. Survival statistics following distal splenorenal shunt in good risk patients (Child’s Class A) are in excess of 80%
d. None of the above
Answer: a, b, c
123. Which of the following statement(s) is/are true concerning radiologic examinations used for the assessment of hepatic neoplasms?
a. Magnetic resonance imaging is considered the test of choice for distinguishing hemangiomas from other mass lesions
b. Dynamic CT scanning is the dominant imaging modality for routine screening and diagnosis
c. Radionucleotide imaging plays an important role in modern screening and detection for liver lesions
d. CT angio-portography (CTAP) is the gold standard for early detection of metastatic hepatic lesions
Answer: a, b, d
124. A 45-year-old woman undergoes an ultrasound because of vague right upper quadrant pain and epigastric fullness. A 7 cm cystic lesion is detected. Which of the following statement(s) is/are true concerning the patient’s diagnosis and management?
a. Simple aspiration is indicated for treatment and diagnosis
b. Bile stained fluid suggests underlying biliary pathology
c. The cyst is likely lined by cuboidal epithelium
d. Laparoscopic unroofing of the cyst can provide satisfactory treatment
Answer: c, d
125. Which of the following statement(s) is/are true concerning biopsy techniques for hepatic masses?
a. A fine needle aspiration (FNA for cytology is contraindicated for patients with hypervascular masses)
b. Percutaneous biopsy should be performed only if results may obviate the need for exploratory laparotomy
c. Needle track seeding of tumor is not a risk associated with percutaneous biopsy
d. Laparoscopy and biopsy play little role in the management of liver lesions
Answer: b
126. A 55-year-old woman presents with vague right upper quadrant pain and a palpable liver. Laboratory tests are normal and a noncontrast CT scan (patient has a history of contrast allergy) reveals an 8 cm right hepatic mass. Which of the following statement(s) is/are correct concerning the patient’s diagnosis and management.
a. A gadilinium-enhanced MRI would be indicated to define the extent of the lesion and confirm the diagnosis of hemangioma
b. A fine needle aspiration should be performed regardless of radiographic workup
c. Hepatic embolization is the treatment of choice
d. The lesion should be resected because of concern for malignant degeneration
Answer: a
127. Which of the following statement(s) is/are true concerning the pathogenesis of hepatocelluar carcinoma?
a. Hepatocellular carcinoma is associated with infection with hepatitis A, hepatitis B, and hepatitis C
b. The risk of developing hepatocellular carcinoma related to hepatitis B viral infection is related to the chronicity of the infection
c. Hepatocellular carcinoma only develops in cirrhosis associated with hepatitis
d. Alfatoxin B1 is a potent carcinogen in the development of hepatocellular carcinoma
Answer: b, d
128. A 38-year-old woman with a 17 year history of oral contraceptive use presents with right upper quadrant pain. A CT scan demonstrates a 4 cm lesion in the right lobe of the liver. Which of the following statement(s) is/are true concerning the patient’s diagnosis and management?
a. The lesion is likely premalignant
b. A 99mTc sulfur colloid scan will distinguish this benign lesion from a malignant hepatoma
c. The lesion, although benign, may be associated with life-threatening hemorrhage
d. The lesion would be expected to be hypervascular on angiographic study
Answer: c, d
129. Which of the following statement(s) is/are true concerning focal nodular hyperplasia (FNH)?
a. The lesion predominantly affects young women
b. The lesion is associated with the use of oral contraceptives and other estrogens
c. Radionucleotide scanning can be useful in the specific diagnosis of FNH
d. Excisional biopsy is indicated in almost all cases because of the risk of bleeding
Answer: a, c
130. Which of the following statement(s) is/are true concerning the prognosis of patients with hepatic metastases and colorectal carcinoma?
a. Over half of these patients will survive one year without treatment
b. Five year survivals following hepatic resection for an isolated metastasis is in excess of 25%
c. Survival beyond five years after resection suggests a high probability of cure
d. Survival rates are improved with a margin of resection greater than 1 cm
e. The size of a liver metastasis is not a significant factor in predicting recurrence if adequate margins can be obtained
Answer: b, c, d, e
131. Which of the following statement(s) is/are true concerning the treatment and prognosis of hepatocellular carcinoma?
a. The fibrolamellar variant of hepatocellular carcinoma has a distinctly better prognosis than other forms of the disease
b. Patients with untreated hepatocellular carcinoma rarely survive a year
c. Multiagent chemotherapy is extremely effective in hepatocellular carcinoma and should be considered for the treatment for most patients
d. Hepatic artery ligation or embolization has been demonstrated to be highly effective for hepatocellular carcinoma
Answer: a, b
132. The following statement(s) is/are true concerning the relationship of the biliary tree and the hepatic artery and portal vein.
a. The common hepatic and common bile duct lie immediately anterior to the portal vein
b. The cystic artery, which usually arises from the right hepatic artery, crosses behind the hepatic duct in most cases
c. A replaced right hepatic artery arising from the superior mesenteric artery system will run to the right of the common bile duct
d. The arterial supply of the extrahepatic biliary ducts is derived from major trunks running along the medial and lateral walls of the common duct at the 3 o’clock and 9 o’clock position
Answer: a, b, c, d
133. An understanding of the anatomy of the extrahepatic biliary tree is essential in performing biliary tract surgery. Which of the following statement(s) is/are true concerning biliary ductal anatomy?
a. The majority of patients have the "classic" anatomical description
b. The common hepatic duct unites with the cystic duct to form the common bile duct
c. An accessory right hepatic duct occurs in 5% of patients
d. A common channel or "Y" configuration of the distal bile duct and pancreatic ducts occur in approximately 70% of patients
Answer: b, c, d
134. A 35-year-old female presents with typical biliary colic symptoms, however her sonogram shows no gallstones. Which of the following statement(s) is/are true concerning her diagnoses?
a. Chronic acalculous cholecystitis or gallbladder dyskinesia is seldom associated with classic biliary colic symptoms
b. The most specific test for diagnosing gallbladder dyskinesia is CCK-enhanced cholescintigraphy with assessment of gallbladder ejection fraction
c. An ejection fraction greater than 75% is considered abnormal and indicative of gallbladder dyskinesia
d. Cholecystectomy is not indicated for chronic acalculous cholecystitis
Answer: b
135. The following statement(s) is/are true concerning the embryology of the biliary tree.
a. The primordial anlagen of the liver and biliary tract arises from the entoderm
b. Superior and inferior caudal buds form as the hepatic diverticulum develops
c. The development of the liver is a separate process from that of the gallbladder and distal biliary tree
d. The biliary tree develops in association with the dorsal pancreas
Answer: a, b
136. The following statement(s) is/are true concerning biliary motor function.
a. The contracted sphincter of Oddi impairs bile flow into the duodenum and directs it into the gallbladder
b. In the postprandial state about 70% of hepatic bile flows into the gallbladder before reaching the duodenum
c. During the interdigestive period, only a small fraction of gallbladder bile enters the duodenum
d. Gallbladder emptying during fasting is associated with phase III of the interdigestive migrating motor complex (MMC)
e. After a meal, the gallbladder empties by a steady tonic contraction thought to be due to release of endogenous motilin from the mucosa of the small intestine
Answer: a, b, c
137. The following statement(s) is/are true concerning the anatomy of the gallbladder.
a. The gallbladder lies between the right, left, and quadrate hepatic lobes or hepatic segments IV and V
b. The cystic duct contains the spiral valve of Heister which serves an important valvular function for the gallbladder
c. The cystic artery arises from the right hepatic artery in 95% of cases
d. The cystic artery crosses anterior to the hepatic duct in the majority of cases
Answer: a, c
138. The gallbladder plays an important role in altering bile composition by absorption and secretion. Which of the following statement(s) is/are true concerning this mucosal function?
a. The absorption of water by the gallbladder can result in concentration of the solute components of bile from 2-to 10-fold
b. Gallbladder mucosal absorption can occur by both active and passive mechanisms
c. Cyclic adenosine monophosphate (cAMP) stimulates NaCl-coupled transport and may also influence tight junction permeability
d. Secretory products of the gallbladder include bicarbonate and glycoproteins
Answer: a, b, d
139. Abnormalities of the sphincter of Oddi have been recently recognized to cause symptoms which are referable to the biliary tree or pancreas. The following statement(s) is/are true concerning sphincter of Oddi motor function.
a. The sphincter’s basal resting pressure is 10 to 15 mm Hg above duodenal pressure
b. Contraction of the sphincter occurs with CCK stimulation
c. Vagal stimulation results in relaxation of the sphincter
d. Manometry of the sphincter of Oddi may be performed at the time of ERCP to characterize basal pressure, amplitude, frequency of contraction, and direction of propagation of contractile waves
e. Stenosis of the sphincter of Oddi is characterized by abnormally elevated basal pressure on sphincter of Oddi manometrics
Answer: a, c, d, e
140. A 32-year-old woman with symptomatic gallstones wishes to discuss nonsurgical options for her gallstones. Which of the following statement(s) are true?
a. The best commercially available oral dissolution agent, ursodeoxycholic acid, is associated with a complete dissolution rate of less than 50%
b. If the gallstones dissolve, there is minimal risk of gallstone recurrence
c. Contact dissolution is applicable regardless of stone type
d. Extracorporial shock wave lithotripsy (ESWL) in combination with oral dissolution agents is an appropriate technique for most patients and can result in complete stone fragment clearance in over 90% of patients by one year
Answer: a
141. A 48-year-old woman presents with several hours of acute right upper quadrant pain, low grade fever, and nausea and vomiting. Which of the following statement(s) is/are true concerning her diagnosis and management?
a. A mild elevation of her bilirubin ( b. A positive bile culture can be expected in virtually 100% of patients with this scenario
c. Laparoscopic cholecystectomy is clearly contraindicated
d. Appropriate antibiotic coverage should include coverage for gram-negative aerobes
Answer: d
142. Laparoscopic cholecystectomy has become the procedure of choice for the management of symptomatic gallstones. Which of the following statement(s) is/are true concerning laparoscopic cholecystectomy?
a. Injury to biliary tree occurs more frequently with laparoscopic cholecystectomy than open cholecystectomy
b. Laparoscopic cholecystectomy is contraindicated in patients with acute cholecystitis
c. Bile duct injuries are more likely to occur during the surgeon’s early operative experience with the procedure
d. Previous upper abdominal surgery is an absolute contraindication to laparoscopic cholecystectomy
Answer: a, c
143. Which of the following statement(s) is/are true concerning gallstone ileus?
a. The diagnosis may be suggested by plain abdominal radiograph
b. Primary surgical management consists of relief of obstruction and cholecystectomy
c. Gallstone ileus accounts for less than 5% of all causes of intestinal obstruction
d. Typical patients are elderly with long-standing gallstone disease
Answer: a, c, d
144. The pathogenesis of cholesterol gallstones is multifactorial. A number of key processes, however, appear to interact closely in the formation of cholesterol gallstones. These include:
a. Cholesterol supersaturation
b. Gallbladder stasis
c. Accelerated nucleation
d. High bilirubin concentration
Answer: a, b, c
145. Which of the following statement(s). is/are true concerning the diagnosis of biliary tract disease?
a. Nonvisualization of the gallbladder on oral cholecystogram is diagnostic of biliary calculous disease
b. Ultrasonography has a diagnostic accuracy and sensitivity for cholelithiasis in excess of 95%
c. Ultrasonography is the preferred test to distinguish chronic from acute cholecystitis
d. Hepatobiliary scintigraphy is primarily indicated to confirm the clinical diagnosis of acute cholecystitis
Answer: b, d
146. Which of the following statement(s) is/are true concerning the solubilization of cholesterol in bile?
a. Cholesterol is highly soluble in both serum and bile
b. Mixed micelles are the primary transport mechanism for biliary cholesterol
c. Most cholesterol found in bile is the result of excretion from serum
d. Biliary vesicles are composed primarily of biliary phospholipid
Answer: d
147. Appropriate options for management of common bile duct stones identified at laparoscopic cholecystectomy include:
a. Conversion to open cholecystectomy and common duct exploration
b. Transcystic duct dilatation and exploration
c. Laparoscopic choledochotomy
d. Complete the laparoscopic cholecystectomy with postoperative ERCP and stone removal
Answer: a, b, d
148. Risk factors associated with development of gallstones include:
a. Increasing age
b. Obesity
c. Rapid weight loss
d. Cirrhosis
e. Diabetes mellitus
Answer: a, b, c, d, e
149. Which of the following statement(s) is/are true concerning a 35-year-old woman found to have asymptomatic gallstones?
a. The patient should undergo attempts at medical dissolution
b. Cholecystectomy should only be performed if the laparoscopic technique is an available option
c. The patient has less than 10% chance of developing significant symptoms over the next five years
d. The risk of gallbladder cancer with stones detected at such a young age, warrants cholecystectomy
Answer: c
150. In which of the following clinical situations is pigment rather than cholesterol gallstones a more common problem?
a. Alcoholic cirrhosis
b. Morbid obesity
c. Diabetes mellitus
d. Hereditary spherocytosis
e. Biliary tract infection
Answer: a, d, e
151. The following statement(s) is/are true concerning the mode of spread of gallbladder cancer.
a. The most common mode of spread for gallbladder cancer is to the liver by hematogenous spread
b. Lymphatic drainage of the gallbladder can extend from the cystic duct lymph node to periportal lymph nodes and the celiac and superior mesenteric lymph nodes
c. Gallbladder cancers rarely extend past the cystic duct
d. Direct extension to the liver, particularly liver segments IV and V, is the most common mode of spread for gallbladder cancer
e. Most patients with gallbladder cancer present with a very limited extent of disease
Answer: b, d
152. A 55-year-old woman undergoes cholecystectomy for symptomatic gallstones. The final pathology returns one week after the operation showing gallbladder carcinoma. Which of the following statement(s) is/are true concerning this patient’s prognosis and management?
a. If the gallbladder carcinoma is limited to the mucosa and/or submucosa, cholecystectomy alone is adequate treatment
b. If the carcinoma involves deeper layers of the gallbladder wall, the prognosis will be significantly worse
c. If reoperation is performed, the chance of finding residual disease will be low
d. If a full thickness tumor had been recognized at the time of cholecystectomy, an "extended cholecystectomy" may have been appropriate
Answer: a, b, d
153. Gallbladder cancer accounts for 3% to 4% of all gastrointestinal tumors. Which of the following statement(s) is/are true concerning the incidence of gallbladder cancer?
a. Gallbladder cancer is much more frequent in men
b. Southwest Native Americans, Alaskans, Mexicans, and Hispanics have a greater incidence of gallbladder cancer than the general population
c. The majority of patients with gallbladder cancer have gallstones
d. The association of gallstones with gallbladder cancer is greater in patients with multiple small stones
Answer: b, c
154. The following statement(s) is/are true concerning the prognosis for gallbladder cancer.
a. Average survival is in the range of one year
b. Five year survival rates approach 50%
c. The combination of postoperative adjuvant radiation and chemotherapy have been associated with overall improved survival
d. For most patients, the goal of treatment is palliation
Answer: d
155. Which of the following statement(s) is/are true concerning gallbladder polyps?
a. Sonographic findings of a gallbladder polyp include a filling defect which does not move with change in position
b. Benign gallbladder polyps can cause symptoms similar to those caused by gallstones
c. Ultrasonography can readily distinguish benign from malignant gallbladder lesions
d. An asymptomatic gallbladder polyp 1 cm in size can usually be followed with serial ultrasounds and does not require cholecystectomy
Answer: a, b
156. The following statement(s) is/are true concerning the surgical therapy of cholangiocarcinomas.
a. A resectable distal bile duct carcinoma is best treated by a Whipple procedure
b. Klatskin tumors may require hepatic resection in attempt for potential cure
c. Regardless of the surgical resection for proximal biliary tumors, stenting of the biliary anastomosis is important
d. Complete hepatic resection with hepatic transplantation has been associated with overall good results
Answer: a, b, c
157. The following statement(s) is/are true concerning carcinoma of the bile ducts.
a. Carcinoma of the bile ducts is more common than gallbladder carcinoma
b. Similar to gallbladder cancer, bile duct cancer is more common in females
c. Unlike gallbladder cancer, there is no association of bile duct cancer and gallstones
d. Ulcerative colitis is associated with an increased incidence of bile duct cancer
e. Choledochal cysts may be associated with the development of bile duct cancer
Answer: d, e
158. Which of the following statement(s) is/are true concerning the association of gallstones with gallbladder cancer?
a. The association of gallbladder cancer with gallstones is such that young patients with asymptomatic gallstones should undergo routine cholecystectomy
b. Calcification of the wall of the gallbladder is associated with an increased incidence of gallbladder cancer
c. Larger gallstones are associated with a greater risk of gallbladder cancer than smaller gallstones
d. The 20 year risk of developing gallbladder carcinoma in patients in the general population with gallstones is approximately 1%
Answer: b, c
159. A 65-year-old man presents with obstructive jaundice. The patient’s workup begins with a CT scan. Which of the following statement(s) is/are true concerning his diagnosis?
a. A CT scan demonstrating intrahepatic biliary obstruction with a decompressed gallbladder and a nondilated extrahepatic biliary tree will be consistent with a Klatskin tumor
b. The presence of biliary obstruction seen on the CT scan requires further evaluation with invasive cholangiography either percutaneously or endoscopically
c. Percutaneous transhepatic cholangiography would be the preferred technique for a suspected proximal cholangiocarcinoma in that it will better visualize the proximal extent of the tumor in the biliary tree
d. The placement of a transhepatic biliary catheter can prove useful in surgical management of proximal bile duct cancers
e. There is little role for angiography in the evaluation of a patient with suspected cholangiocarcinoma
Answer: a, b, c, d
160. Benign gallbladder and bile duct tumors are extremely rare. Which of the following statement(s) is/are true concerning benign biliary tumors?
a. Cholesterol polyps are due to foamy macrophages filled with cholesterol
b. Inflammatory polyps and cholesterol polyps are not considered to be premalignant
c. Gallbladder adenomas, like adenomas in other gastrointestinal organs, are considered premalignant
d. Most gallbladder adenomas are associated with gallstones
e. An adenomyoma is a mucosal lesion of the gallbladder not considered to be premalignant
Answer: a, b, c
161. Which of the following statement(s) concerning bile duct strictures due to chronic pancreatitis is/are true?
a. Most patients present with progressive jaundice
b. Strictures are classically long and tapered involving the entire intrapancreatic bile duct
c. Patients may be asymptomatic and diagnosed only by persistent elevation of serum alkaline phosphatase
d. An excellent option for surgical management is choledochoduodenostomy
Answer: b, c, d
162. If a bile duct injury is suspected at laparoscopic cholecystectomy, appropriate management includes which of the following?
a. Conversion to open cholecystectomy and intraoperative cholangiography
b. Small ducts ( c. If the injured segment is greater than 1 cm. in length an end-to-end ductal anastomosis is the procedure of choice
d. Postoperative external drainage should be avoided
Answer: a, b
163. Which of the following statement(s) is/are true concerning the incidence of bile duct injury following cholecystectomy?
a. Data from the pre-laparoscopic cholecystectomy era would suggest the incidence of bile duct injury during open cholecystectomy to be 0.1–0.2%
b. The current incidence of bile duct injury during laparoscopic cholecystectomy is greater than 1%
c. The experience of the surgeon performing laparoscopic cholecystectomy can be correlated with the incidence of bile duct injury
d. Intraoperative cholangiography during laparoscopic cholecystectomy will prevent bile duct injury in virtually all cases
Answer: a, c
164. Primary sclerosing cholangitis has a number of treatment options—both medical and surgical. Which of the following statement(s) is/are true?
a. A number of immunosuppressive oral agents can provide specific effective treatment for primary sclerosing cholangitis
b. Biliary reconstruction with long-term transanastomotic stents can be useful in selected patients with focal strictures at the hepatic duct bifurcation
c. Biliary reconstruction should be reserved only for patients with established biliary cirrhosis
d. Hepatic transplantation for primary sclerosing cholangitis can be associated with survival rates similar to other indications for transplantation
Answer: b, d
165. The following statement(s) regarding the elective repair of a bile duct stricture is/are true:
a. A transanastomotic stent is necessary for a successful result
b. Long-term stenting for approximately one year is necessary for an anastomosis performed at the distal common hepatic duct
c. A Roux-en-Y hepaticojejunostomy provides the best route for restoring biliary-enteric continuity
d. Preoperatively-placed biliary catheters facilitate dissection and identification of the stricture and are useful in placement of transanastomotic stents when employed
Answer: c, d
166. The vast majority of benign bile duct strictures occur following operations in or near the right upper quadrant. Other causes of benign bile duct strictures include:
a. Chronic pancreatitis
b. Ulcerative colitis
c. Primary sclerosing cholangitis
d. Intrahepatic arterial infusion of 5-fluorouracil
Answer: a, c, d
167. A 37-year-old female presents with obstructive jaundice due to a mid-bile duct stricture four months after laparoscopic cholecystectomy. Which of the following statement(s) are true:
a. Surgical reconstruction is the only option for management of this patient
b. Excellent long-term results can be expected in approximately 80% of patients following surgical biliary reconstruction
c. One year follow-up after successful repair is satisfactory regardless of the method of management
d. Surgical reconstruction offers a better chance of long-term success than either percutaneous or endoscopic dilatation
Answer: b, d
168. Most patients with postoperative bile duct strictures after cholecystectomy present early after their initial operation. Patients may present in which of the following manner(s)?
a. Obstructive jaundice
b. An external biliary fistula
c. Progressive accumulation of bile in the peritoneal cavity (bile ascites)
d. Biliary cirrhosis
Answer: a, b, c
169. Nonoperative dilatation, performed either endoscopically or percutaneously, can be successfully employed in which of the following etiologies of bile duct strictures?
a. Postoperative bile duct strictures following a hepaticojejunostomy used for reconstruction during a Whipple procedure
b. Complete transection of the bile duct during laparoscopic cholecystectomy (the so-called "classic laparoscopic cholecystectomy injury")
c. Primary sclerosing cholangitis
d. Oriental cholangiohepatitis
Answer: a, c
170. The gold standard for evaluation of patients with bile duct strictures is cholangiography. The two routes for cholangiography are percutaneous transhepatic cholangiography (PTC) or endoscopic retrograde cholangiography (ERC). Which of the following statement(s) is/are true?
a. PTC is generally more valuable than ERC in defining the proximal biliary tree to be used in reconstruction
b. ERC is technically easier in patients with bile leaks because the biliary tree is usually not dilated
c. Parenteral antibiotics should be administered prior to either procedure to prevent cholangitis
d. Biliary stents can be placed via either technique to control biliary leaks
Answer: a, b, c, d
171. The management of a suspected bile duct injury depends on a number of factors, most importantly the mode and timing of presentation. Which of the following statement(s) is/are true concerning a patient presenting with a suspected bile leak after laparoscopic cholecystectomy?
a. Laparotomy should be performed immediately
b. Cholangiography should be performed to determine the nature of the injury
c. Operatively-placed drains should be removed to allow the fistula to close
d. The patient should be discharged to home to allow the leak to close spontaneously
Answer: b
HEPATOBILIARY PANCREATIC SURGERY Questions and Answers pdf Download
Read the full article
0 notes
Text
Lowering Your Risk For Liver Cancer
Introduction
Various factors increase the risk of liver cancer. These factors include underlying medical conditions, such as cirrhosis and hepatitis, exposure to harmful chemicals, exposure to aflatoxins, and use of anabolic steroids. There are various ways to reduce the risk of liver cancer.
Risks For Liver Cancer
Although the exact cause of liver cancer remains unknown, however, various factors increase its risk. Underlying medical conditions as well as a sedentary lifestyle increases the risk of liver cancer. The liver is the organ that metabolizes the food we eat, the drugs we take, the toxins we are exposed to, and performs various other functions. Age and gender are also factors determining the risk of cancer. People above the age of 60 years are at high risk for developing liver cancer. Males are more prone to hepatocellular carcinoma as compared to females. Thus, you should take good care of your liver and lower the risk of liver cancer.
Viral Hepatitis
People with hepatitis B and hepatitis viral infections are at high risk of developing liver cancer. If the infection is not treated, it may lead to liver cirrhosis and chronic hepatitis. Unprotected sexual intercourse, exposure to infected fluid or blood, and needle contamination while drug usage results in the transmission of hepatitis.
The timely treatment of hepatitis infections helps in the recovery of the patients. The adults with a chronic infection or its carrier are at high risk of developing liver cancer. Infants and children with hepatitis are significant carriers of hepatitis infection.
Liver Cirrhosis
Liver cirrhosis increases the risk of liver cancer. In liver cirrhosis, there are scars in the liver that reduces the functional capacity of the liver. There are various causes of liver cirrhosis, such as fatty liver disease, hepatitis, diabetes, high cholesterol, and obesity.
Other causes for liver cirrhosis are the autoimmune diseases that cause primary biliary cirrhosis. In this condition, then there is damage to the bile ducts leading to cirrhosis. In advanced stages of primary biliary cirrhosis, the risk of liver cancer is high. Some patients have hemochromatosis. In this condition, the body absorbs excess iron resulting in its accumulation in the liver leading to cirrhosis.
If you are obese, you are at high risk of developing fatty liver disease. Fatty liver disease progress to cause liver cirrhosis, which is a high-risk factor for liver cancer. You may have alcoholic and non-alcoholic fatty liver disease.
If you are smoking for a few years and consuming alcohol, you can develop liver inflammation. The inflammation in the liver may result in liver cirrhosis that may lead to liver cancer.
Harmful Chemical Exposure
Exposure to harmful chemicals also increases the risk of liver cancer. The person may be exposed to these chemicals during the course of work. Vinyl chloride and thorium dioxide increase the risk of angiosarcoma and hepatocellular cancer. Vinyl chloride is generally used in the plastic industry, while thorium dioxide is used during the radiological examination.
Aflatoxins
Aflatoxin is a poisonous substance produced by mold which is found on crops that are not properly stored. Exposure to aflatoxin increases the risk of cancer.
Anabolic Steroids
Anabolic steroids also increase the risk of liver cancer. These steroids also transform the hepatocellular adenoma to carcinoma.
How To Lower Your Risk For Liver Cancer
Following are the tips through which a person may reduce the risk for liver cancer:
Maintain a healthy weight.
Avoid smoking and drinking excessive alcohol.
Get a vaccination for hepatitis B.
Practice hygiene to avoid hepatitis C infection.
Keep your blood sugar level under control.
Maintain a low sugar diet and exercise regularly.
Tags: Fatty liver disease, Liver Cancer Treatment in India, Liver cirrhosis
#Liver Cancer Treatment in India#Liver Transplantation In India#Liver Transplant in Delhi#Liver transplant cost in india#Best liver transplant surgeon in india#Liver cancer treatment in delhi
0 notes