#I see a lot of burnout amongst authors
Text
I want my mutuals to know—
I OBSESS over your work. I ain’t even playin’ around here. I’ll be balls deep in a fantasy world YOU created, in my own mind at all times of day, just frolicking around in the world YOU built.
Give yourself more credit. Give yourself more time. Give yourself more rest.
True fans give space, appreciation, and understanding for life happening outside.
#I see a lot of burnout amongst authors#they need the appreciation they deserve#and the rest and relaxation#sure as shit I can wait#I’ll still be here when you come back#take your time and enjoy yourself#I love y’all#Yan gets sappy
70 notes
·
View notes
Text
When we are talking about charity, there must exist a level of certain precaution to not let your emotional turmoil result in subpar actions. If empathy is a natural response to seeing people in pain, then it makes sense to liken it to a kneejerk response, much different from a graceful strike of a soccer player.
Very often, personal face-to-face ingroup charity is used to displace the actual efforts at improving people's conditions, and if your organization lacks political oversight or a certain analytical capacity, you might have serving the community replaced with individual help which eventually accumulates every bias and/or ends up being co-opted by some cult.
I am seeing especially egregorious horrific examples of that on Twitter right now, so I will use them to illistrate a point that is otherwise too global and deep-rooted.
In order to understand how this approach does its harm, you need to understand cause and effect, past and future.
THE CAUSE
We are talking about a clique that talks about investing in trans community by helping homeless and/or unemployed trans women by "paying their bills" for some months before they "get up on their own legs". Thankfully, it's a US based clique, so a lot of sociological studies exist to demonstrate the current situation with trans rights.
Let's investigate the causes of queer people being unemployed and/or homeless. The obvious systemic cause is trans-/homophobia, which results in people losing their capabilities immediately after leaving their parents/coming out to them (see e.g. https://doi.org/gq37kh), or otherwise follows the patterns of stigmatization, exclusion and victimization. If we address more widespread political economy of this vulnerability in the USA, topics of mental health, such as PTSD burnout, substance abuse and sexual abuse - including significantly from within queer community - emerge as vulnerability categories (https://doi.org/ggsjt6). As for how inventive abuse from within "community" is, one might refer themselves to the concepts of "hot allostatic load" and "identity abuse" (https://doi.org/ggmdcd).
Failures of t4t ethos and "community short-circuit" also have been described as sources of chronic homelessness among queer youth (https://doi.org/mpx8).
One must be especially mindful of the fact that level of education is an important - if not the most important - predictive factor of queer homelessness, effects were described in depth by Rachel M. Schmitz in the dissertation work "ON THE STREET AND ON CAMPUS".
While the effects identified the author ascribes to better socioeconomical standing of college students majorly, author both identified " experiences of homelessness" as
"uniting people through a shared sense of struggle and conflict", and notably gives credit to educational endeavor of academia as vastly superior to "street experience", and studies in countries with accessible education still identify low education level with risks of anxiety and depression. (https://doi.org/mpx3) (https://doi.org/mpx4)
As Negura notes, "Ultimately, the three concepts—‘social support’, ‘social capital’ and
‘social bonds’ — are complementary. These terms are used here to understand the same reality of mutual help amongst people, from different social perspectives."
CONSEQUENCES
The most recognized effect of homelessness is anxiety and depression. Recent works identify that both of these health effects are significantly resolved through providing housing, however meta-analysis of the works being done is very complicated by poor methodology of studies: short follow-up, making it impossible to judge the homelessness outcomes, and high group heterogeneity. (https://doi.org/mpxx)
Among the outcomes of homelessness specifically in queer people, "utopian thinking" is seen, in accordance with England, 2022, "an inevitable part of community responses: to improve the present it, it is necessary to look beyond the present and to an alternative in which queerness does not only survive, but is valued, celebrated and encouraged".
To a materialist that would mean death of the community as a utopianism-free endeavor, but it is not, however, it should be noted that imperfect solutions to the crisis provide fertile soil to these cognitive failures.
Actual observations of the long-lasting effects of experienced homelessness are, indeed, lacking, but so far there's no data that homelessness and unemployment actually have significant lasting damage in the queer population, nonetheless remaining the risk factor in their duration.
One, however, important effect of escaping and avoiding homelessness is resiliency. As Cronley, 2017 notes, "Rather than understanding how youth are surviving in extremely adverse environments, research applies
socially normative models of behavior to their actions such that conclusions of deviancy and
marginalization are inevitable" and "youth rely on informal social networks to survive on the street and that
spirituality, mental health, and creativity are associated with improved coping". Once again we are drawn to connections to education systems within this approach.
And therefore we must remember establishment of education systems during historical cases.
PAST
Expansion of educational processes has long been demonstrated to be a driver of establishing new or maintaining old hegemony.
One might remember Huguenots, who existed both in France and in Netherlands. Often, for example in Van der Lem's "Eighty Years War", Erasmus of Rotherdam is remembered to be as a reason for catholics' loss in the region - humanism, moderateness and church reforms were indeed the ideas of his. It's not easy for me to believe, considering how Netherlands were absolute leaders in amount of exterminated heretics during the 1520-1540, therefore you cannot imagine the humanism and spirit of mercantile freedom helping very much.
But comparing the historical evidence between French Huguenot fighting and Netherlands' Huguenot fighting, one stark difference is seen immediately without even examining the evidence - it's the material amount of Evidence piled up.
Netherlands of XVI century was ultimately a literature-centric country: rational argument, presented with necessary charisma and efficiency, put into the easy epistolary style allowing for open discussion - all that erased the differences between catholics and protestants.
And using this positional leveling, protestants spent 10-20 years before, well, protesting with continuous work of printing press, while catholics of Netherlands continued, thinking themselves safe, sat complacent, only satisfying the demands of the already intellectual public.
Indeed, you can not let a worldly peasant work with biology, err, theology, lest they will be mistaken and fall into the tenets of sin themselves. A good example of this "Don't give the North Korean kids iGEM distribution" was dutch translation of La Bouclier de la Foy by Nicole Grenier, which the translator prefaced with an easy explanation that you should never actually argue with heretics, the priestly class knows best.
In France, enjoying the closeness of Rome, literacy was synonymous with military industry, err, Raytheon, wait, wrong, Catholic Church.
Of course it was literacy ultimately sympathetic to the plight of the layman, and easily putting itself into their shoes - «Les disputes de Guillot le porcher et de la Bergère de S. Denis en France contre Jehan Calvin prédicant de Genesve» is exactly about the lower classes destroying Kalvin himself with facts and logic.
And, like this, simply by virtue of being able to work with higher reasoning in lower genres, you can win the Hegemony.
The ultimate victory of feminism in 1917 also answers a lot about where did soviet feminists come from - from the intermediate spaces where people of higher class can interact as equals with people of lower class, without financial or institutional power relationship between them. An example is, of course Pavlov teaching women's courses and creating a whole host of women physiologists, actual hymnasia and schools, such as in Sonya Yanovskaya case.
Masonic secret societies, where jews could freely talk to christians and nobles mingles with commoner bourgeois were this driver in bourgeois revolutions, universities drove February and October revolution, and even in the USA the connectedness to high-socioeconomic status, what is called "bridging social capital" remains a primary predictor of success of people from oppressed groups. (https://doi.org/gqmpxx)
FUTURE
As such, I cannot see a way for personal charity - bonding social capital, excising queer people from support networks and from solidarity with marginalized, destructive to both people outside of it and to attempts to build a queer community — to be excused in modern conditions.
Build new platforms to, instead of elevating select voices, sing together.
2 notes
·
View notes
Note
New-author-Anon here. Thank you so much, Pia. It just... It's so easy to see the "small" wordcount and think "oh, this is nothing." I'm pretty good at churning words out normally, but on top of this, I have a legal job that takes up 25-30 hours a week, and I teach Japanese 3 hours a week. I kept telling myself that it's not too much. The salary is good for my area (about 19k AUD a year), and that's the probationary one. Thank you. You're probably right it's burnout. Ill try to adjust my workload
It's so easy to see the "small" wordcount and think "oh, this is nothing."
Honestly I agree! I saw the 1,600-1,900 words and thought 'oh that's not too bad' and then I saw 'twice a week' and was like '....hang on' and then added up the numbers on my calculator and did a tiny little scream in my head about what you'd committed yourself to.
I'm just a little worried about you anon! You're obviously a superstar with everything you do, and I'm really really glad you're getting paid a decent amount for your area! I want this to be a good fit for what you're doing because you like the content and you like the work. But man, non-fiction takes a toll. It's harder to write than fiction, for the most part, because it requires more research every single time. You don't get to 'settle down' into characters, and those hours of research and editing aren't invisible.
One thing you can maybe consider doing while you figure this all out, is sit down and - if you aren't doing this already - work out the hours you spend realistically on the writing job. Not just the writing itself, but the editing, the researching, and also thinking about what to write re: the topic itself. It's sometimes easy to forget that these are also the hours of your new job, and they are all equally important.
Another thing you could do if you're very committed to keeping this job, or can't restructure easily, is seeing if you can try and get ahead on your schedule, so that you feel less like you're constantly at the mercy of your deadlines - I don't know if it's possible, but if you can even get a week ahead sometimes, it can help remove some of that dread. ADHD makes this very hard, and so this may not be possible with what you're already doing, so don't stress if you can't. It's okay.
Your feeling of helplessness may be your body or mind trying to communicate to you that you're just overwhelmed right now. And if it is writer's block - there will absolutely be different techniques that you can use to help you.
And 100% you need to look at scheduling some rest. One of my hardest earned skills personally is the ability to go - after staring at a chapter and hating myself for not writing anything - is 'Right! I'm not going to write for the next four hours! I'm clearly tired! I'm going to go lie down, and get some rest. Or I'm going to do something fun or relaxing. Or I'm going to go for a walk. But the thing I'm 100% not going to do is stare at this document. I'll come back later.' The hardest part of this skill is catching it before 3 hours have gone by, lmao. Sometimes I'll just do the 'endless scroll' and distract myself and feel guilty and stressed, and I have to actually just be like 'walk away and go do something else.' I may still worry about it, but at least I gave my brain a TV show, or a movie I love, or a book, or I ate something tasty, or I drank some water.
The fact is, people tend to write better when they're not exhausted all the time. I have to take days off because of chronic illness anyway, but taking actual rest time is vital to you actually being able to feel inspired and motivated enough to write. You obviously have discipline! And reaching out for help is great too. Give yourself some mercy and kindness in amongst feeling like you're not getting anything done, you're getting a lot done, and are maybe now needing to re-evaluate a little. I really hope it works out though, and it sounds like you're working damn hard to achieve it. I do wish you all the best, seriously.
(Oh, and random tip that isn't in my other writer's block links - if you can, consider hooking up with some Twitch stream 'write ins' or other writing groups. Sometimes the gentle pressure of other people who 'get it' all kind of figuring it out at the same time can actually help? I'm not one of those writers who benefits from this, but I know plenty who are, and it might end up being your thing too!)
#asks and answers#pia on writing#dodgy advice#please dismiss anything i say that doesn't work for you!!#<3333333
10 notes
·
View notes
Text
The Call
So much of my life has been marked by my struggle to find a home that sometimes I think that I don’t spend enough time thinking about my search for a calling. Maybe it’s because they’re so intertwined that it’s hard for me to separate one from the other. Admittedly, it’s a strange train of thought, but I’m a writer, and strange is my native milieu.
I bounced around from major to major in college... I probably looked like the ultimate commitment-phone with all of my major changes looking for the major that would be just right. There were a lot that were almost right. But, for various reasons (math requirements, boredom, burnout, too many gut feelings while looking at my degree audit trying to figure out how to graduate in four years...), they didn’t work out.
My interests are wide enough that often, I can see several options and feel that I could be happy with any of them, which makes figuring out My Calling even more difficult.
In high school, I thought that going to Stony Brook was what would make me happy, but I wasn’t any happier there than I was in high school. I was actually miserable. My boss knew I wanted to transfer, and one day when I showed up for work, he ordered me to his work truck. When I asked him where we were going, he reiterated that I was going to his work truck. He drove me out to a satellite campus on the East End, parked at the dock, and as I got out of his truck, a breeze kicked up over the Bay. I started crying. I blamed it on the sun. It wasn’t the sun. It was enough, for a while.
Over winter break my second year of college, I visited my godparents in Utah. God found me again in a mission church on the edge of the Navajo Nation, and I didn’t want to finish school without figuring out what God was asking of me. I wanted to take time off to do a certificate program through a seminary, but that didn’t go over well with my family. I decided to put all of my energy into getting out of college as fast as I possibly could so that I could pursue ordination and get myself back to the Navajo Nation. I even had a job offer waiting for me to sign on the dotted line. But it didn’t work out. And I was devastated.
I applied to grad school, went to Kenya, found a place that I loved, a place that needed help as much as I needed the feeling of wholeness I found there. I had little to offer, because what good is English language when there is no water? So, I went to Hawaii to learn how to farm sustainably and efficiently, and fell in love with a completely different environment, and somehow, I found myself, too. It wasn’t perfect. There were fights with the cook, conflicts amongst members of my Esky team, vastly different expectations of how our time would be spent and who we would answer directly to... It was different than we expected, but it was wonderful, too. I daydreamed about what I would do next. There was a Fulbright Fellowship on the slow food movement that I thought would compliment the farming bit well, but I didn’t want to leave Hawaii. I asked if I could apply for a second year. And then I broke my finger, got a sunburn, and got a rash. I knew what it meant; I just hoped I was wrong. I wasn’t.
Going back to Hawaii would be a fatal mistake.
I never understood how one sentence could shatter your life until that appointment. My plans to return to finish out my contract, my plans to go to Italy, my plans to go back to Kenya and spend my life there... They were all gone, only I knew they existed, and I couldn’t pretend they hadn’t for the sake of getting on with things. Still, life went on. I had to make calls.
I called my Esky Director. I felt horrible. I was offered the first contract on my team, and I was letting him and my team down. The reasons why didn’t matter. They were depending on me and I couldn’t follow through. He wasn’t surprised; I’d been gone long enough that he doubted there would be good news about what was making me so sick, but he had hoped, and I had, too. In every moment of fear before I’d left for Hawaii, and in every moment of fear I’d had before I had a diagnosis, I reminded myself that the will of God would never take me anywhere that the grace of God would not also protect me. And yet: everything I wanted to do, everything I felt called to do, every certainty I’d felt in my bones had been taken from me. It didn’t seem like there was a surplus of people who wanted to move to a remote, politically unstable region of the Horn of Africa. Why would I be taken out of the equation? What good could I do the world inside all of the limitations of my new life? How was that time better spent than it would have been going through the mystics with my Hawaiian spiritual director? What did the chronic pain teach me? My suffering was, for years, so intense that if I were a house pet, I would have been put down because it was inhumane to leave me in pain. But I had to endure it.
I knew that I would never know how or why, and that made it so much harder to endure it all.
For years, I could hardly dream any new dreams for my life. It felt useless; even if I loved something, it would probably be outside of my capabilities, or something else would happen to take it away from me. And I’d had my calling. I couldn’t do it. Nothing came to replace it. Nothing eased that ache. I started to believe that I would spend the rest of my life with the phantom pain of my lost calling.
I went back to Hawaii for a writers conference I’d been planning to attend before I got sick. It wasn’t painful. In fact, I felt happier than I had in years. When I swam in the Bay, it was like she remembered me. Like she was welcoming me home again. Slowly, the pain released its grip on me. And as it did, I waited for the day I would wake up and know that I had a new calling. A few years went by. No calling came.
Before I turned 30, I asked my Esky boss why there was no new calling. “It’s been 6 years.” I told him. Plenty of time for a Type A Perfectionist to decide that God’s missing the cues. In a surprising turn of events, I found a new calling, and made lists and worked towards my goals. In a more surprising turn of events, a worldwide pandemic hit, and all of my plans and all of my lists went up in smoke. In the most shocking turn of events of all, it’s been a year since that pandemic started, and I’ve moved from despair to productivity. I’ve done more continuing ed this last year than I’d done in the previous ten--by a lot!
Last spring--and I couldn’t even tell you how I found them--I came across a school and realized that I wanted to do every single degree they offered. I was in a panic about the future of my life, and decided that going back to grad school for housing security was a terrible idea. I had plenty to keep busy with without throwing grad school into the mix, so I moved on. I wrote, I learned, I meditated, I tentatively made new lists and new plans, but I still had terrible uncertainty hanging over my head. We moved. I came back to those programs, and read them all again. And in the unexpected and inexplicable way that it is when the Spirit moves, the path forward became clear. Joseph Campbell said, “Follow your bliss and the universe will open doors for you where there were only walls.”
I have struggled in the 8 years since I graduated to fully articulate how I see the interdisciplinary sustainability work of my BA working with my MFA in writing, beyond that I was interested in both fields, so I got a degree in each. The graduate certificate I’m taking now has bridged those fields in a way that feels exciting and natural. I feel like I got new glasses and now the fuzzy world has been rendered clear, sharp, and vivid.
It turns out that the questions I’ve been asking and the things I like do actually go together... I just needed to find a place that understood those questions, and I think I have. I also needed not only to be ready, but to feel ready to undertake the work. While I still struggle with my imposter syndrome some days, one of the liberating and wonderful surprises of my thirties is that after graduating with an MFA at 23 and deferring to others for years, I finally feel like I can speak with authority, and not only on matters of writing or text analysis. I know a lot! And people value my insights! (Crazy, right?)
I also know that no matter what I do, or where I go, all roads lead me back to Hawaii. That is where my heart is at home, and where my spirit feels settled.
5 notes
·
View notes
Text
RHR: How to Fight Practitioner Burnout with Dr. Akil Palanisamy
In this episode, we discuss:
Burnout among healthcare practitioners
How common the problem is
The results of widespread physician burnout
The difference between burnout and moral injury
How technology is contributing to the problem, not alleviating it
How to fight physician burnout
Show notes:
The Paleovedic Diet by Dr. Akil Palanisamy
The Sutter Health Institute for Health & Healing in San Francisco
Unconventional Medicine by Chris Kresser
1440 Multiversity retreat for healthcare professionals
Akil Palanisamy’s website, DoctorAkil.com
youtube
[smart_track_player url="https://ift.tt/2MsScI1" title="RHR - How to Fight Practitioner Burnout with Dr. Akil Palanisamy " artist="Chris Kresser" ]
Chris Kresser: Hey, everybody, Chris Kresser here. Welcome to another episode of Revolution Health Radio. This week we’re going to be talking to Dr. Akil Palanisamy, who is a friend and colleague in the Functional Medicine space. And I’ve known him for several years. He is the author of The Paleovedic Diet, a really interesting book combining Paleo and Ayurveda, a traditional Indian medicine which is an interest of his. And he also runs the Paleo Symposium that’s put on by the Institute for Health & Healing at UCSF every year, that I’ve been a featured speaker at since it started.
But today actually, we’re going to be talking about something different, which is burnout amongst healthcare practitioners. It’s a really important topic that has pretty significant implications not only in terms of the effect on individual clinicians, but on patients and their access to care, things like medical errors and just the healthcare system overall.
So if you’re not familiar with Akil, he’s an integrative medicine physician who blends his medical training with Functional Medicine in Ayurveda, the traditional medicine of India. He studied biochemistry at Harvard and received his medical degree from UCSF and completed his residency at Stanford. Dr. Akil also completed a fellowship in integrative medicine with Dr. Andrew Weil at the University of Arizona. He sees patients at the Sutter Health Institute for Health & Healing in San Francisco, where he also serves as physician director for community education. He’s been a consultant with the medical board of California for many years and as I mentioned, he’s the author of The Paleovedic Diet: A Complete Program to Burn Fat, Increase Energy, and Reverse Disease.
So I’m really excited to dive into this conversation with Akil. I think you’ll find it interesting, even if you’re not a healthcare practitioner that’s experiencing burnout, because we talk about a lot of issues that are relevant to anybody doing any kind of work, really. So I hope you enjoy the conversation. Let’s dive in. Akil, thank you so much for joining us. I’m so glad to have you here.
Akil Palanisamy: Thank you, Chris. Pleasure to be here.
Burnout among healthcare practitioners
Chris Kresser: So today we’re going to talk about a really important topic that I don't think gets enough attention, and this is physician burnout. So, and I would extend it to burnout for any healthcare practitioners. We might be focusing a little bit on physicians because this is where most of the statistics are available, but it’s certainly a problem across the entire healthcare world whether we’re talking about:
Nurses
Nurse practitioners
Occupational therapists
Chiropractors
Acupuncturists
Anybody working in the care profession
In my book Unconventional Medicine, I talked a lot about how this is one of the major challenges within medicine in general, not just conventional medicine, but also integrative medicine and Functional Medicine. And it's something that we need to develop a sensible approach to if we’re going to meet our goals in terms of preventing and reversing disease. So this is something that Akil has thought deeply about and has been involved in a number of different initiatives from his work at Sutter to working with medical students and other physicians to address this problem. So I'm really looking forward to having this conversation. So why don’t we start a little bit with the stats on burnout, Akil?
Ask yourself: Does medicine still feel like your calling? If daily stress and exhaustion are turning you away from the profession, you might be headed toward physician burnout. Find out what causes burnout and learn how to rediscover your sense of purpose.
How common the problem is
Akil Palanisamy: Sure, yeah, I think it's really rampant, and most studies report around 50 percent or higher of physicians report some significant burnout. And that's up from about 40 percent just five years ago. So, I think the numbers are really scary and also this is a global problem. So this is across the board. Many countries throughout the world and also regardless of the stage of training. So medical students, residents, physicians, even the number of years of practice has no impact.
Chris Kresser: Wow.
Akil Palanisamy: I will check on this number, so, I mean, I know because I did my medical training 20 years ago, and it was like, I would say, a soul-crushing and exhausting process.
Chris Kresser: Right, right.
Akil Palanisamy: So I started early in this topic, and that’s why I’m so passionate about it.
Chris Kresser: Yeah, yeah. That’s really revealing in some ways. If medical students are as burned out as people who've been in the profession for 10 or 20 years, that's an indication that something’s already going wrong, even at that very early stage.
Akil Palanisamy: Right. I came across a really fascinating study. They interviewed almost 3,000 medical students about burnout and 53 percent of them reported feeling burnt out. About 15 percent were depressed, about 5 percent had seriously considered suicide. But the interesting thing was 100 percent of the students, every single one reported feeling humiliated at some point, demeaned, disrespected as part of their training. And that had huge effects on their performance and judgment, and that was my experience too. It’s part of the culture of training doctors.
Chris Kresser: It really is, isn’t it? It’s almost like fraternity hazing or something. I've heard for residents that it's … and it seems to be perpetuated for some of the same reasons, like this, “I went through this, so you have to go through it,” type of mentality. And I've even read the studies that support that.
Akil Palanisamy: Yeah, right. When I started my residency, I was super thrilled because they had just passed a law limiting the work hours, continuous work hours to 24 hours in a row. That was like a huge drop.
Chris Kresser: That’s a big development.
Akil Palanisamy: And I was like, “Wow, this is fantastic. I only have to work 24 hours in a row, like, every week.” And people thought that would solve the problem of burnout. But it hasn’t because that’s just one of many factors.
The results of widespread physician burnout
Chris Kresser: Right, and so we know that there’s a huge problem with the shortage of primary care physicians. I don't remember the exact number from the study I shared in my book, but it's something like, predicted to be a shortage of around 50,000 primary care providers by the year 2025, which is not very far off in the future. And yet one of the costs of burnout, as you said, is that two-thirds of physicians know a doctor who is likely to stop practicing medicine or at least to reduce their access to patients, switch to concierge model, or something like that within the next five years as a result of burnout. So this is a real problem that's really kind of having an outsize effect on our healthcare system.
Akil Palanisamy: Yeah, absolutely. I mean, I think it is genuinely a public health crisis. And I think that that word is increasingly being used in the literature because this really does impact not just individual physicians but patients, healthcare organizations, the entire healthcare system in our country and other countries around the world. So I think the scope of the effects and the impact of burnout is being recognized now and it's huge in terms of not just the individual level, but medical errors as well. So, recent studies have shown that there’s a strong relationship between physician burnout and medical errors. And already medical errors are one of the major leading causes of death in the United States. And so I think as we get more burned out physicians and higher rates of medical errors, I think that's one of the big issues in terms of the costs of this problem.
Chris Kresser: Yeah, this is critical, and I highlighted this in my book. But if you go to a site like CDC or a general website and you search for the top 10 causes of death, let’s see what happens if we do that right now. Cardiovascular disease is still holding at number one, and then you’ve got lung cancer or you’ve got other diseases that come shortly after that. The data is often changing. Cancer continues to go up the list. But you’re not going to see medical errors on these lists, right?
Akil Palanisamy: Right.
Chris Kresser: There was a study published in the British Medical Journal in 2016, just a couple of years ago, and then another one by Barbara Starfield, who’s since passed away, back in 2000 in JAMA. And both of those found the same thing, that medical errors are actually the third-leading cause of death. And since only 5 to 15 percent of the atherogenic events are even reported, Dr. Starfield actually speculated that medical errors could be the number one cause of death if all of the atherogenic events were reported. So this is something you don't see on the typical list, but that doesn't mean it's not true.
Akil Palanisamy: Right, exactly. Yeah, because when you experience burnout, the impaired judgment, lack of attention to detail, communication breakdown, all the things, the depression, that just greatly increases the risk of medical errors.
Chris Kresser: Right. So this is a, it's a common problem, it's a problem that has not only effects on individual practitioners and their health and their lifespan, their feelings about their work, but also to patients and their safety and their ability to get the care that they need, and then to society as a whole. The healthcare crisis continues to deepen, and we need more doctors, rather than fewer. The fact that 50 … that two-thirds of physicians know a doctor who’s likely to stop practicing medicine in five years is exactly the opposite direction that we need to be going in here.
The difference between burnout and moral injury
So let's talk … so, we’ve been throwing this term “burnout” around, and I'm sure that means different things to different people. But you actually emailed me before the show with a really interesting distinction that I want to highlight—the difference between burnout and moral injury. So can you talk about that a little bit?
Akil Palanisamy: Yeah, absolutely. So traditionally, burnout is defined as a work-related syndrome characterized by emotional exhaustion, a cynical feeling, and feeling like you're ineffective on the job. But this concept of burnout really doesn't resonate with doctors. I can tell you from talking to many of them that they really don't connect with this concept of burnout because the problem is you're pointing the finger at doctors. And you’re saying, “You’re burned out, you need to start doing yoga and eat granola, and just like change your lifestyle.” But you know, these are some of the most resilient people out there.
Chris Kresser: Absolutely.
Akil Palanisamy: Medicine, I mean we’ve survived decades of intense training, sleep deprivation, the training process itself is incredibly stressful, the work demands. So these are some of the most resilient and resourceful people out there. And so I think the problem is really, a big part of it is the system. But the distinction that you mentioned between moral injury and burnout, the concept of moral injury actually was first used to describe how soldiers responded to what they did during war and when they came back, having to do things that went against their morals.
In healthcare, it refers to physicians being unable to provide the high-quality care that they would really like to, essentially, not being able to be true to themselves. So I think the problem is not that physicians are burned out and so we don't care. The problem is that we care very deeply.
Chris Kresser: Care too much.
Akil Palanisamy: Yeah.
Chris Kresser: Not too much, but it’s the care that’s causing the problem, yeah.
Akil Palanisamy: Right and then as a result, in our current healthcare system, it's so hard to consistently meet patients’ needs and provide the kind of care that we envisioned we would going into medicine. Because most doctors think of medicine as a calling, and so that failure and inability to meet needs of patients in the way that we really envision, that is hugely damaging, and I think that has a huge effect on physician well-being. And so that's the concept of moral injury. So I think that it's really much broader than just pointing the finger at doctors.
Chris Kresser: I think that’s really, really important to understand, and I've always made it clear that when I'm criticizing conventional medicine and its shortcomings, I'm not criticizing individual doctors. Of course, I might be criticizing some individual doctors, but not as a group because the vast majority of doctors that I have met are people that genuinely want to help their patients. They went into medicine for all the right reasons and they do recognize that they're not having the impact that they would like to have, and it's painful for them. But there's, they feel like their hands are tied because of the way that the system is set up. And they’re just as much victims of the system as the average patient is.
And I think this is a good example of how that plays out where we all want to have meaningful and rewarding work. We all want to get to the end of the day and feel like we really made a difference. And doctors, I think, especially. That's the path they chose. They didn't go into private equity. They didn't choose to go into a career that was really not about helping people, but more about making money or enriching their own lives. Not that there's necessarily anything wrong with that. They willingly chose to go through a very arduous path that involves many, many years of schooling and as you said, rigorous training with residency, working 24 hours straight, often graduating with hundreds of thousands of dollars of debt. I mean, it’s an enormous risk to take, an enormous amount of investment of money and time and energy to become a physician.
So you don't make it through that generally, unless you really have a guiding moral compass that is pushing you through it. And so it's really, I think, even more important and critical that we figure out a way to, where we create a path forward for doctors and other healthcare practitioners that really do want to have that feeling at the end of the day. Because that's the antidote to burnout, where when you really do feel like you're transforming the lives of the people that you're working with, and you're having a huge impact. Because in that situation it doesn't mean you won't get tired and it doesn't mean you won't occasionally feel, “Geez, I need a vacation.” But you're not going to have that moral injury, and that’s what makes all the difference in the world.
Akil Palanisamy: Yeah, I know, exactly. And I think that the rates of suicide among physicians is a real wake-up call because it’s twice that of I think active duty military, and then there was a report from the UK that there was a young junior doctor who, she took her own life by walking into the sea.
Chris Kresser: Yeah, that’s not, yeah.
Akil Palanisamy: Statistically, women physicians are a significantly higher risk of completed suicide than matched females in other professions. So it’s not uncommon, unfortunately, and I think that, yeah, exactly what you said about that moral compass that physicians have, I think being able to feel like you're true to yourself. That's a basic need that all of us have, and I think especially those who go into medicine, we feel that pretty intensely.
How technology is contributing to the problem, not alleviating it
Chris Kresser: Right. And there may be lots of choices every day that they have to make that are, don't feel true to themselves because of the way that the system is set up. And I know from my own research and I know you and I have talked about this, one of the influences in terms of burnout has been the rise of electronic medical records or electronic health records, EMRs and EHRs. Initially these were hailed as, that this is going to dramatically reduce the amount of paperwork that doctors would have to do and they were going to be great time-saving and productivity devices, and they were going to be doctors’ best friends. But the reality has not quite lived up to that, has it?
Akil Palanisamy: No, no. Yeah, I would, I think that studies show that about like half of the average physician’s workday is spent entering data or doing other clerical work in the EHR. So the amount of time actually spent with patients is less than a third, and for me I think it's a bit of a double-edged sword. Because it does make it easier to respond to patient messages rather than playing phone tag with patients. But on a typical day, I might get 50 to 60 electronic messages in addition to charting visit notes for each patient, and each of these questions or patient calls, etc., requires some thought.
And increasingly we’re being measured on how quickly we can respond to these messages because the priority is patient satisfaction, and that's eventually going to be tied to financial compensation and that kind of thing. So I think this EHR, it takes up so much time, and it really hasn’t translated to the reduced workload and that sort of thing. And when we deal with insurance in my practice, I think that's a huge benefit for patients because it improves access, and for Functional Medicine and integrative medicine, I think we need to move in that direction where insurance covers services. And so we offer that, but then it creates a whole universe of responsibilities in terms of the paperwork, the criteria for each progress note when we’re billing insurance, the forms, the prior authorizations, the other kind of paperwork. So it just adds another layer of paperwork to everything else that we’re dealing with in terms of the EHR every day.
Chris Kresser: Yes. And then there’s another issue of when you're actually in the room with the patient, that connection that you're trying to make with the patient is now being mediated by a computer screen and having to type into the computer. And we’ve all seen, I've heard many stories of people going to doctors and complaining that their doctor was hardly even looking at them because they were working on the computer the entire time, and this is especially true with younger doctors from what I've heard, who never operated without an EHR.
So they never had the experience of being in a visit with the patient without the computer being part of that. And I think with all the data that we now have in terms of how important the physician-patient relationship is to the outcomes in care and the research on the placebo effect, and just the, in Carl Rogers's words, the unconditional positive regard and the type of connection that is made just is therapeutic in its own right. And I think the EHR can compromise that in some ways.
Akil Palanisamy: Yeah, absolutely. And I'm always torn because I want to maintain good eye contact and really be present with each patient, but then if I don’t touch the EHR at all, then at the end of the day I’m like, this one’s like …
Chris Kresser: You’ve got eight more hours of work.
Akil Palanisamy: Exactly.
Chris Kresser: It’s really challenging, and, I mean, my solution to that, which is not possible for everybody because of the model I work independently, so I’m able to just kind of set things up how I want. But I have a nurse practitioner that's by my side at every appointment, and she takes the notes. So I'm able to just maintain eye contact with my patient and not really look at the computer. And I recognize that's not a viable solution for most practitioners, but it's something that I felt compelled to do because I, like you, didn't want to get home and do four hours of data entry into the EHR after a full day of seeing patients. And but I didn't also want to sacrifice the connection with the patient.
So I think the other thing that's also not always in an individual physician’s control is the quality of the EHR or the EMR system. So many of them are just completely bloated and full of functions that they'll never use, and just really difficult to navigate, and they’re a nightmare in terms of software development. They’ve been just sort of cobbled together and put on top of each other, and it’s, for anyone who likes software and technology, EMR software is not going to be particularly inspiring for the most part.
Akil Palanisamy: Yes, yeah. No, I think you’re right on that. And the point about having additional support for progress notes, I think, is a good one because studies show that having some type of help with the charting actually reduces burnout, and it's obvious, right? And I think at Sutter Health where I work, they really take burnout quite seriously. And so they’ve supported having scribes, which is the same thing. They take notes and they kind of do everything, and you just have to sign the note.
So I think it’s really, it’s a shared issue with burnout between individuals and healthcare systems and organizations. So I think it’s very important that all of these systems realize they have an important role to play, and I think Sutter Health is a really great example of that. They've supported a lot of these changes, and like this example of scribes and with our EHR, which is Epic, just helping us to use it in the most efficient way possible. So I think systemic changes are really a huge part of the solution as well.
Chris Kresser: Absolutely, and this is a recurring theme in this conversation. It's that individual physicians can only do so much when they're employed in a larger organization, and they’re not free to just do whatever they want. And so we have to continue to work to raise awareness institutionally about these issues so that the institutions themselves can make the changes, and then individual physicians will benefit from those.
Akil Palanisamy: Right.
How to fight physician burnout
Chris Kresser: So let's talk a little bit about some of the work you've done in the past with medical students and other doctors at Sutter on burnout. What kind of things have you done to approach this?
Akil Palanisamy: Yeah, I think for me during medical school, it was really a survival mechanism. Because I was pretty burned out and the training, yes, I absolutely had that being belittled and demeaned when I was on the wards in my rotations. And so I really got interested in the certain classes that were offered on finding meaning in medicine and really connecting with your purpose or actually reconnecting with why you went into medicine, and keeping that front and center. And also developing tools for maintaining well-being like mindfulness.
So mindfulness is one thing that has been studied. There’s actually been about 14 studies looking at physician burnout and mindfulness, and nine of them have shown positive outcome in terms of:
Reducing burnout
Improving well-being
Improving mood
Improving resiliency
So I think, I don't think that's the entire solution, but the more tools you have in your toolkit, the better. And we don't really get any training in general in terms of how to deal with stress and how to manage emotions during our healthcare training. And so I think I got into mindfulness very early, studied MBSR, developed a daily meditation practice, became involved in educational programs teaching people about mindfulness. And then since … then during residency and now practice, after that I've been very interested in workshops and events that kind of focus on that aspect of meaning and really reconnecting with a sense of purpose, a sense of direction. Kind of helping people be true to themselves.
And so I think small group exercises and workshops where people are getting out of their left brain and reconnecting with their right brain, using art and things like that, have been really effective. So for me, I've benefited as much as I’ve helped anybody in this work, and it's been just partly for my own gains, but I think you teach what you have to learn. And for me, being involved in burnout and teaching people about it has been a lifesaver.
Chris Kresser: That’s so great. I think all of those are fantastic tools for kind of exploring the causes of burnout on an individual level and helping people respond in a way that will reduce the risk of moral injury, if we will. And I know for me, one of the ways that I've approached this personally and also with people that I've worked with and that I’ve trained is just to make sure that I feel like the work I'm doing is having a big impact on my patient’s lives. Because that’s one of the reasons I really love that distinction that you make between burnout and moral injury. Because if I look at it that way, I think, “Okay, well, that's the biggest risk is just getting to the end of the day and feeling like I'm not making a difference. Feeling like all of my efforts are for naught really. Or they’re not really having the impact that I would like them to have.” And to me, that's the greatest risk in terms of burning out. When I know that my work is making a difference, my endurance and stamina are considerable.
Akil Palanisamy: Right.
Use Functional Medicine to prevent it
Chris Kresser: But when I don't feel that way, it doesn't take much to make me feel tired and like what I'm doing is not worth it. So this is, I think, where a Functional Medicine approach has a lot to offer, not just as a treatment modality, but as a means of really actually making a difference in the patients’ lives. Like getting to the root cause of the problem and actually addressing the problem and helping the patient to recover and feel better without the use of unnecessary drugs and surgery. For me that was one of the most appealing things about Functional Medicine, and I think it's one of the less talked about but most important gifts that it has to offer to individual physicians who shift their practice in that direction.
Akil Palanisamy: Yeah, I think that's what motivated me to go into Functional Medicine as well, just to get that sense of fulfillment and satisfaction when you help someone really get a permanent solution to something and by uncovering the root causes and taking that holistic approach. So I think that's what drew me to Functional Medicine as well.
Schedule a retreat
Chris Kresser: Absolutely. So another area where I know, or a kind of antidote to burnout that I know that you and I are both passionate about is a retreat. So I've been a big believer in retreat. I’ve done annual retreats myself for many years. I’ve done meditation retreats for about 25 years and I just can't really imagine my life without that opportunity to step away from my day-to-day life and experience and to get a different perspective, to slow down, to have more spacious existence for a few days were the busyness of life is not overtaking me and where I can just hear myself think and feel my body, and just look at things from a fresh perspective. It's just crucial for me. And I've always felt like my wish has been that others can experience this. That we can, because I really believe in its transformative power.
Connect with colleagues
Akil Palanisamy: Yeah, absolutely. I do as well, and I’ve had a number of retreats over the years in terms of individual retreats and also group retreats. And especially in the professional setting, I find that ability to connect with other colleagues and professionals in that informal, nonwork setting is so powerful because in healthcare there's so much isolation. There are so many individual silos.
Everybody's just doing their thing trying to get through the day, and you rarely have a chance to step back and step out of that situation to just really deeply connect with people who are in the same boat and really understand what they're going through, share their story, listen to their stories, and really deepen your connection and solve problems together.
So I think that sort of deep connection is so important because that's like a huge need for all human beings, and especially in such an isolating profession like in healthcare. I think it's essential.
Chris Kresser: Absolutely, yeah. So many clinicians can just spend, we spend most of our time in a room with patients and we’re interacting with patients, but we’re not, we’re interacting with them in a certain way. We’re playing a certain role. We’re the clinician, they’re the patient, and those can be rich and rewarding interactions. But it's not the same as connecting with other colleagues and being able to talk about the issues that we face professionally and share together. So yeah I think that group experience is really powerful. And I’ve been writing about this recently.
I’ve been sharing some book recommendations, and Akil and I have actually teamed up to offer a retreat for healthcare practitioners at 1440 Multiversity in October. It’s from October 5th to 7th this year. And so it starts on Friday afternoon, Friday evening, and it goes through Sunday midday. And the retreat’s called “From Burnout to Brilliance: Rediscover Your Passion and Purpose, Reclaim Your Health, and Create a Practice You Love.” So the intention of this retreat is to address the issues that we've been talking about in the show and to help healthcare professionals explore their own situation, help them rediscover their passion for medicine and healthcare, and reconnect with a sense of meaning and purpose in their work to take some practical steps. Break those down into really doable actionable steps that they can take to reclaim their health and well-being. Rediscover parts of themselves that are not typically expressed in the course of their day-to-day work and just kind of cultivate a sense of energy and vitality that they may have been missing for many years.
And I'm really excited about doing this. I’m excited about doing this with Akil, who I've known for several years now and I really respect, and I'm excited about doing it at 1440. It's an incredible new retreat center, which I think you did a retreat there with Michelle Tam with Nom Nom Paleo last year, Akil?
Akil Palanisamy: Yes, yes beautiful, beautiful place. Yeah.
Chris Kresser: So this is, and for those of you who are not familiar, it's in Santa Cruz Mountains, right?
Akil Palanisamy: Yeah, it’s surrounded by redwood trees and there's all these amazing hiking trails. And yeah, a beautiful place.
Chris Kresser: Yeah. I haven't actually been there yet, but I know several people who’ve taught there and who’ve been there. And if you go to 1440.org, click on the stay button and check out some of the pictures. It's an absolutely beautiful campus. Really nice accommodations, gorgeous dining hall with lots of different food options. They've got daily yoga classes and massage, and a spa and other health offerings there. And they’ve got, of course, gorgeous hiking trails because it's in the redwood forest there. It just looks to me like they're really doing it right. I've been to a lot of retreat centers. I actually lived at a retreat center in Big Sur called the Esalen Institute …
Akil Palanisamy: Oh. sure.
Chris Kresser: … and many people may be familiar with. When I was still really sick and dealing with my health issues, I got to a point where I just decided, I kind of reached the end of the line of supplements and diets, and medications, and I decided that I would explore the psychological, emotional, psycho-spiritual aspects of what was going on for me. So I moved to Esalen and lived there for a couple of years. So I'm very familiar with retreat centers. I've been to many others around the country, both for Buddhist meditation retreats and other retreats, and I have, they're all great in many ways. But they’re, I can see that 1440 is bringing it to a different level.
So I'm excited to be a part of that. I'm excited to get together with a group of professionals that are all wanting to cultivate more meaning in their work and to find that work/life balance that can be so elusive. And I just can't wait to get together and support each other and share because that's, I mean, we all have so much to offer, and I think when we come together with a similar purpose, it's really powerful.
Akil Palanisamy: Yeah. I am also really excited about the upcoming event, and I think for anyone who feels like they're not being true to themselves in their work or as to themselves as they would want to be, I think this is a great opportunity to really reflect. And I think our vision for that weekend is that it's going to be a very introspective weekend and really focused in small groups and interactive elements. So it’s not going to be just mostly didactic.
Chris Kresser: Yeah. It’s not going to be Akil and I standing in front of the room talking at you the whole time. Definitely going to be the opposite of that.
Akil Palanisamy: Right, exactly, yeah. Because I think that this work is really about looking within and then sharing and connecting with other people. And so that's the focus of the weekend, is really building that sense of community with whoever comes and really learning to deepen your own sense of meaning and purpose in work, and look within to reconnect with that vision for what drew you to this work initially. Because I think that's the ultimate goal is having that feeling like you're really being true to yourself at the end of the day and having the kind of practice that you envision.
Don’t be afraid to make changes
Chris Kresser: Absolutely. I shared the story of Sheri in my book Unconventional Medicine, who is a clinician that was working in the VA. And she's a doctor and was mostly seeing patients with diabetes. That's the most common health challenge for veterans. And it was, she was counting the days until retirement. It was just really a factory-medicine type of situation. She often didn’t even have time to go to the bathroom during the day because she was just that busy from appointment to appointment. And as we've discussed, there was a real risk of moral injury because she didn't feel like she was making a difference. She was just handing out medications to these people and she wasn't, she knew as an athlete herself who tried to pay attention to her diet, she knew that wasn’t the best way to go about it. But what else could she do in the amount of time that she had?
And she moved into kind of a more, started incorporating more of a functional approach in her work, and then eventually left and started her own Functional Medicine practice. But for her, it was just a total game changer. She went from counting the days to retirement, to not ever being able to imagine retiring. And that's the kind of shift that’s possible, I think, when you really address the root causes of burnout and take the opportunity to step out of your current system, your current day-to-day, and really give yourself the chance to discover something new. And even if that’s maybe moving in a different direction entirely, or maybe staying in your current situation but just making a series of small changes that collectively can have a big impact.
Akil Palanisamy: Yeah, I think for me, my whole approach has been in terms of incremental change because I know that for many people, they have gone out of the insurance model and set up their own Functional Medicine practice, and that can be fantastic. But my work is really just building change within the system. Because if the people within the system leave and do their own thing, then the system itself is going to not be changed. And so I think that a big part of this is also figuring out solutions within systems and incremental steps we can take, and I think that'll hopefully be part of what we talk about as well. Just if you do belong to a system, how you can take a leadership role and effect change within that system as well.
Chris Kresser: Absolutely. That's why Akil and I are a good team, because I’m outside the system and he’s inside of the system, and we have different perspectives. So that's another reason I'm happy to team up with him. I mentioned this in the beginning, but I'll throw it out there again. You need not be an MD to participate in this workshop. It's really for all healthcare practitioners and providers who are experiencing burnout. And so this could be anyone from a health coach to a nutritionist to a dietitian to an occupational therapist to a chiropractor, a naturopath in addition to MDs, and DOs, and MPs, and PAs, and all of the other abbreviations and acronyms. Anyone working in healthcare really would be welcome. And we’re not even limiting it to people working in healthcare. We don't want to exclude people here, so if you're not working in healthcare and the things we've been talking about resonate with you, maybe you work in emergency services or something else, you are absolutely welcome to come.
Akil Palanisamy: Yeah, and I would add that even if you're not feeling burned out, I think that prevention is really the best medicine.
Chris Kresser: That’s true.
Akil Palanisamy: So I think learning about the research and the science, because we know how to prevent it, and it's much better to prevent burnout than treat it once it happens.
Chris Kresser: That is a very good point. Yeah, and I guess if the statistics are any indication, we know that even if you’re not feeling burnout now, chances are statistically you will at some point.
Akil Palanisamy: Right.
Chris Kresser: Especially without any intervention. It’s kind of like the diabetes example I used before. If you’ve got high normal blood sugar, now’s the time to get it under control rather than waiting until it turns into diabetes.
Akil Palanisamy: Right.
Chris Kresser: Great, well, thank you so much, Akil, for being with us. It’s a fascinating and important topic, and I’m really looking forward to leading this workshop with you. Again, in the retreat, you can go to 1440, it’s 1-4-4-0 dot o-r-g, and when you get there on the website, you just hover over Learn, and then under programs click on Professional Development. And if you scroll down there, you’ll see our program, which, again, is on the first weekend of October, October 5th to 7th, it’s a Friday through a Sunday.
And there’s a tuition for the program, and then there’s several different accommodation options available there. It’s really neat. I like what they've done with that. Everything from a private room to a suite to a really cool bunk style, kind of modern bunk-style accommodation that's much more affordable. I don’t know if you saw those last time.
Akil Palanisamy: I did, yeah.
Chris Kresser: Check the pictures out, they look pretty cool. They call them pods.
Akil Palanisamy: Right, yeah, yeah. They’re pretty comfy. I’ve seen them.
Chris Kresser: Yeah, yeah, it looks great. So lots of different accommodation options. If you’ve never been to this part of the world, the Santa Cruz Mountains are a beautiful, beautiful area, gorgeous redwood forests. You can head down to the beach before or after in Santa Cruz there. It’s a funky, cool little town. Great, great part of the world. So I hope you can make it. Those of you who have been listening to this and resonating with it, we’d love to meet you in person and have a chance to explore these topics with you.
And then Akil, is also, we haven’t talked much about his other work, but he’s also an author in addition to being a clinician. And he organizes the Paleo Symposium every year that I've been fortunate enough to be a speaker at. So why don’t you tell everyone a little bit more about your work and where they can find out more about your work.
Akil Palanisamy: Oh sure, yeah. So I practice integrative medicine and I combine Functional Medicine with the Paleo approach and Ayurveda, which is the traditional medicine of India. And still that has led to my book which is called The Paleovedic Diet, combining Paleo and Ayurvedic medicine. And the best way to connect with me would be through my website, which is DoctorAkil.com. Just doctor spelled out, A-k-i-l dot com. And yeah, I wanted to thank you, as well, Chris, for having me on the podcast. I’m very excited to be working on this event with you, and it was really a pleasure to talk today.
Chris Kresser: Pleasure is mine, Akil. And I'm sure we’ll be in touch before October, but I look forward to seeing you then and anyone else who's listening, who wants to join us. So 1440.org, and thanks for listening, everybody. Keep sending your questions in. I know I haven’t answered many of them recently. We’ve been doing a lot more interviews lately. But I do see that I have a few Q&A episodes coming up, and we do read all of your questions, and we also consider them for writing articles or emails.
So even if we’re not able to answer them on the show, it helps me to understand what you're thinking about and what you want me to write about and talk about. So please do keep sending them in. That’s ChrisKresser.com/podcastquestion. And thanks, everyone, for listening. And thank you, Akil, and we’ll see you next time.
Akil Palanisamy: Thank you, Chris.
The post RHR: How to Fight Practitioner Burnout with Dr. Akil Palanisamy appeared first on Chris Kresser.
Source: http://chriskresser.com
August 23, 2018 at 02:07AM
2 notes
·
View notes
Video
youtube
professional writing services
About me
Taylor University'S Professional Writers' Conference Tickets, Thu, Jul 23, 2020 At 1
Taylor University'S Professional Writers' Conference Tickets, Thu, Jul 23, 2020 At 1 Custom essay service can help you write your essays for cheap. Professional writers of service provider possess all needed expertise to write down an effective essay which persuades the audiences. I keep in mind when I started working at a legislation firm that I was surprised at how a lot writing there was. “Why didn’t anybody inform me I was going to be doing a lot was writing? When the situation turns into too troublesome to deal with and deadlines for papers get dangerously shut, it’s time to turn to professionals. Don’t risk struggling burnout trying to do all of it by yourself. Our writing providers team is here, prepared to take a few of the strain off. Did you see what number of writers mentioned their battle to write down? Housseni stated that his first drafts are “troublesome” and “laborious” and “disappointing.” Russell referred to as her writing “unhealthy.” Kingsolver throws out 100 pages before she will get to the primary page of a e-book. ” If writing is a major a part of your job, you’re a professional writer. What good is it to get a well-written tutorial piece if it comes even simply an hour too late? Stellar writing quality has put us on the map, and excellence assure we provide for every written piece our team members provide is sure to fulfill even essentially the most demanding tutors. Every hardworking, devoted pupil is aware of how troublesome and overwhelming it is to steadiness college obligations and personal life. A strong want and sincere attempts to make it all work will sometimes convey the results you might be aiming for, however, sadly, that received’t be the case every time. Imagine writing within the nexus of creativity that is The Writers Room. You'll be amongst revealed authors and serious skilled writers, supported by different writers as dedicated to their craft as you might be. Writing essays could be robust for an individual, particularly when one doesn't have correct command of the English language. Exceptional writing is the primary and most necessary facet of our business, but it’s removed from the only factor we are able to provide our loyal prospects. Whether you want to order a paper right away or just wish to hear extra about our services, be at liberty to contact us at any time. Our research paper writing service is something PaperWritingPro became famend for. Even at first glance, it is possible for you to to recognize the quantity of care, time, and professionalism woven into each single sentence. You have each right to expect on-time content material delivery and also you shouldn’t accept anything lower than optimal. Teaming up with PaperWritingPro, the essay writing service supplier established as an business chief, ensures your essay will always be on time, regardless of how tight the deadline could also be. It’s a widely known fact that writers don’t suppose in a straight line. Their concepts are at all times jumbled up, and then ultimately, those ideas type an attractive and finalized piece. Keeping that in mind, Milanote has give you this writing software that’ll help you store all your ideas and unfinished content material into one place after which work on your last piece. As writers, we regularly get distracted by the tiniest things, and it affects the way we write. Unlike a printed piece, embedding hyperlinks to deeper content is also important online. Plus, writers want to consider how individuals are looking for content material associated to the subject at hand. Weaving in key words and phrases is essential for search engine marketing , however authors should keep away from key word stuffing on the similar time. Remember to add alt tags to the images on the page as nicely. Writers ought to aim to write for human readers in addition to Internet spiders. In order to probably avoid that, you can use iA Writer. It creates a full-display and plans writing house so that you can dedicate your time and give attention to it with out being distracted.
0 notes
Text
Does Time Tracking Really Boost Workplace Productivity?
We’re living in a time of endless distractions. Our attention is constantly divided amongst many different things. Even if we fight it, the majority of us still compulsively checks our phone messages and notifications, no matter if we’re hanging out with friends or at work.
We’re especially prone, understandably, to distractions at work. Discussing work with teammates, checking emails, or reading customer comments and reviews are of significance.
However, these tasks are the number one priority, yet we tend to spend a lot of time on them. Even though they’re all work-related, we can consider them being significant disturbances since they take your mind away from much more critical tasks and lead you to procrastination.
Not only do we achieve less due to problems with focusing, but we also get more and more overworked and burned out. Why is this the case? Well, expectations towards employees aren’t getting any lower. If you spend time procrastinating, you’ll have to work extra hours to meet deadlines.
What can you do as a team leads to maintain the balance between productivity and the well-being of your teammates? One of the most popular methods that are generally recommended to managers is to implement time tracking.
Time Tracking – What Impact Might it Have on a Company?
One way of combating employee procrastination is to keep track of the team’s progress by recording the time they devote to completing their project tasks. The most common method of time tracking is to use time tracking software – the most popular tools being Toggl, Clockify, and Timely.
Read more about different tools and their features in our article “12 Time Tracking Software To Improve Team Productivity” to find out more.
Let’s take a look at the advantages and disadvantages of scrupulous time and progress tracking.
Advantages of time tracking
i) Time on the Mind
Having thoughts on how one spends their time at work has an impact on overall progress and productivity. It can cut time spent on chatting with colleagues, having coffee and snacks, and checking social media.
It will result in less time spent procrastinating and more work to achieve goals faster.
ii) Having a Source of Knowledge for Team Leads
Data gathered through time tracking is an excellent source of information for the team leads on how to manage their team better.
It can be the case that a seemingly fast and easy task may take several hours to complete for inexperienced employees – so it is better to delegate it to another. It’s good to analyze this data and draw conclusions while distributing the tasks.
iii) Increasing Transparency
Sharing a workspace with your employees where everyone can see what everyone is working on, and for how long is a great way to increase transparency. In your company – if your aim is for ensuring transparency across team members, the use of project management tools is essential.
There are many project management tools out there, which also include time tracking, like, e.g., Asana or Monday. You can choose whatever suits your needs best.
It ensures that everyone is on the same page, and it also helps with a fair distribution of tasks.
iv) Increase in Business Profitability
By monitoring the time spent vs revenue gained, you’ll easily be able to compare your KPIs and see whether the amount of time and money invested in a project offers a return.
This data can be precious, especially for scale-ups, which cannot afford to incur any additional costs or losses.
Disadvantages of time tracking
a) It Requires Discipline and Consistency
The biggest con is the need for time tracking itself. It’s a real bother for employees to remember to enter the amount of time spent working on a task. Speaking from my own experience – it’s not as obvious to do so as it may seem. As a result, some people may ignore it and not enter any of their hours.
Some will think “ah, screw it, let’s just say I worked on this 3 hours” even though it was 5 in total – our perception of time can very much differ depending on many variables. One is the perception of a task’s complexity or whether it’s exciting for the employee or not. In such a case, the data that you receive may not be reliable.
b) Low Morale Among Employees
The thought of being controlled for many employees results in a negative ripple effect. As much as it may have a positive impact on efficiency, it may also cause general dissatisfaction among teammates. The key to success is to listen to your employees’ opinions because any savings that you make through an increase in productivity most likely will be incomparable with the losses you’ll incur if your employees decide to quit.
Cutting out on small pleasures like chatting with work colleagues or grabbing a cup of coffee together, and rushing/cutting down lunch breaks can impose unnecessary stress on the employees. If you want to take care of your teams’ wellbeing – think twice about how you approach the time tracking introduction.
Is it really about time?
Adam Grant, a professor of management and psychology at the Wharton School at the University of Pennsylvania and a book author, wrote an article for the New York Times entitled Productivity Isn’t About Time Management. It’s About Attention Management. The title sums up the author’s reluctance towards the idea of time management and measuring one’s progress through time spent on working towards something.
We’re living in a period where everyone and everything that surrounds us is fighting for our attention span.
Research on the topic of human focus shows that an average person is productive only for 2 hours and 53 minutes per 8 hours spent at work . The majority of us feel a constant urge to check email inbox, social media, news sites, have a snack or coffee break, while working.
You know those sayings,
“Procrastination is the thief of time”.
“Procrastination is the enemy of success”.
Today, procrastination has become the number one enemy in today’s world. We’re trying to fight it off, but sometimes it’s not only a waste of time. Taking a breather is essential to avoid getting burnt out. These small things help us to unwind and also strengthen the bonds between teammates – which results in better teamwork.
Try to Focus More on the Reasons Than the Time
People right now are so caught up in the idea of increasing one’s productivity that they lose focus on the reason why they are doing something.
How will completing this task help me or others? Does completing this task brings me closer to my goal? Should I be doing this or should I focus on something which will help me achieve my goals faster?
When you shift your mind from focusing on time efficiency to concentrating more on reasons and prioritizing your tasks, you’ll soon notice that you’re moving towards your goals competently.
Check out this article Why Time Management Does Not Work? to understand the most common myths surrounding time management and productivity effectiveness.
Switching to attention management is challenging, but it’s harder to instruct your teammates on how to adapt to this mindset. It’s not easy to change, mainly if teams are used to time tracking from previous structures and companies. Tracking progress won’t be as simple as it is in the case of time tracking as the data won’t be as quickly gatherable and accessible.
What Can Companies Offer to Boost Employee Productivity?
As mentioned above, there are at least a few ways of boosting your employees’ productivity. You can keep a finger on the pulse and monitor the progress in the project management tool but, at the same time, give your employees a bit of freedom to reset their minds. Encourage people to unwind and chat at the “water cooler” (focused on non-work related topics).
The key to success is to be a talented and observant team lead. Many managers do not understand that their responsibilities involve reaching KPI or sales goals and also to take care of their teams’ wellbeing. It’s the manager’s role to encourage someone to give more if they notice a lack of attention or energy or to tell when a team member is reaching breaking point. It’s a very accountable role.
As a manager or team leader, look for the signs that you may be missing, to prevent employee burnout. No matter how exciting a project is or how engaged and willing team members are, there can always be a breaking point if the workload isn’t managed appropriately.
Cases of obvious signs of exhaustion or fatigue as well as mood swings need to be nipped in the bud. Communicate with your team and ensure that you understand there can be issues outside of work that affect one’s mood. Giving employees a few days off or a much-needed vacation can recharge their batteries and safeguard productivity in the long term.
What can such a team lead do to make sure their team does not lose the will to work? One of the things is to introduce benefits like the opportunity to take a power nap at work or having a shorter workweek. They become more and more widespread. As an example, one of the top remote companies, Basecamp, allows its employees to work for 4 days per week during the summer months.
According to Basecamp’s Head of People Operations, Andrea LaRowe, it’s not humanly possible to give 100% all the time. They decided it’s better to shorten their working time and complete less. The only condition is delivering and maintaining tasks at the same high level as the work done during any other time of the year. Basecamp has done this for more than 10 years, and it has proven to be an excellent benefit for both employees and executive-tier.
What about remote work? We’re living in a time where companies, especially startups and scale-ups, compete with each other in creating and implementing new work trends and benefits. We’re quite accustomed to remote work, which has already proven to be quite handy, especially recently, during the recent coronavirus outbreak.
The research on telecommuting has shown that the employees who work from other places than the office tend to achieve better results compared to those who work onsite. As much as 77% of respondents stated they are more productive while working remotely, while 30% say they accomplish more in less time.
Remote work can also help to deal with career burnout. How? By giving employees more flexibility to decide how they work. Letting employees work from home and structuring the workloads that suit them will provide satisfied remote team members who are more willing to bring efforts to their projects.
However, with new benefits comes new challenges. Not all companies are ready to face them right away. Some business executives believe that incorporating such benefits will have a positive impact on their employees, and instead of a negative impact on their business development and revenue. If you want to learn more about how to incorporate remote work into your company and maintain its culture, check out the article Remote Work vs Company’s Culture How Can We Make It Work?
Conclusion
As an employer or team leader, you need to think about what will be the best solution for your team to increase productivity – this refers to time tracking. Before deciding whether to incorporate time tracking in your company, it’s essential to carefully consider and examine the cons, since they can make the whole undertaking not worth the hustle.
If your team is not disciplined enough or if you as a team lead won’t be able to communicate appropriately, why and what you require from them – then all the data and the whole point of time tracking will be just useless. If you decide that time tracking is not for your company, there are other methods of encouraging your employees to complete more.
It’s worth thinking about incorporating certain benefits to take care of your employees’ wellbeing. A happy employee achieves more than an employee who feels controlled all the time. Don’t be afraid to leap of faith and use an example of remote-first companies or companies that implement a 4-day workweek. Experiment and always remember to listen to your employees’ opinions!
The post Does Time Tracking Really Boost Workplace Productivity? appeared first on CareerMetis.com.
Does Time Tracking Really Boost Workplace Productivity? published first on https://skillsireweb.tumblr.com/
0 notes
Text
How TrapKing is Breaking Stereotypes and Changing the World
The post How TrapKing is Breaking Stereotypes and Changing the World by JaneA Kelley appeared first on Catster. Copying over entire articles infringes on copyright laws. You may not be aware of it, but all of these articles were assigned, contracted and paid for, so they aren't considered public domain. However, we appreciate that you like the article and would love it if you continued sharing just the first paragraph of an article, then linking out to the rest of the piece on Catster.com.
Sterling “TrapKing” Davis’ mission, as his website says, is “to change the stereotypes of not only men in cat rescue, but also bridge the gap in communication between black communities and animal rescue/local shelters.” Sterling brings the work of TNR to some of the poorest neighborhoods in Georgia’s cities, bringing together advocates from a variety of cat rescue and community cat advocacy groups, and even managing to wrangle a couple of cat haters into becoming TNR advocates.
The humble beginnings of TrapKing
Sterling Davis. Photography courtesy Andrea Weir/Devil Cat Studios.
How did Sterling become such a vocal and committed advocate for community cats? “I’ve been a vegetarian since I was 12 and a cat lover all my life, yet I never knew about shelters or TNR,” he says. “That made me think of how many other people loved animals and wanted to help as well but didn’t even know about TNR or rescue in general. Once I started working at a shelter just scooping litter, I realized how much of a void I could fill.”
One of Sterling’s top priorities is working with communities of color, which, he says, have long been overlooked by TNR advocates, and, he says, there’s a lot of poverty and lack of understanding. “A lot of black people have told me that they can’t take care of themselves so they can’t support someone else or donate. They never looked at it as helping or taking care of their communities and the animals in it, and they never knew they could help for free.”
And then sometimes there’s even just the matter of seeing someone like them being involved in TNR efforts. “Traditionally women have been the catalyst for rescue and community cat care, so it’s a matter of the black community being able to see someone like them doing this,” Sterling says.
That holds true even for Sterling himself. “Jackson Galaxy made it a little more possible from a visual standpoint that a man could be a force in rescue.”
How TrapKing Makes a Difference
The TrapKing logo.
Still, sometimes Sterling finds himself in situations where people don’t understand what he’s doing. “When I was returning some cats, a gentleman was filming me and very upset. He thought I was dumping random cats in his area,” he says. “I saw him recording me with his phone and told him to keep filming so I can explain what I’m doing and why.
“Once I explained, I watched this guy — a black man — change his whole outlook. He never even knew the benefits of having TNRd cats in the community. I came back a month or so later, and that same guy had a trap and was doing TNR. He still didn’t like cats, but he respected that there was a better way other than euthanasia or trying to get rid of them.” Beyond the number of cats Sterling has trapped, neutered and returned to their communities, the thing that makes him the most proud is actually the people.
“There can be so much competition or bickering amongst rescues; people take sides and go back and forth about who’s doing it right or who’s doing it wrong,” Sterling says. In the face of that, he has been able to build relationships with individual animal advocates like Samantha Martin of Acro-Cats fame, “Kitten Lady” Hannah Shaw, musician Adam Myatt, and with cat cafes in Chicago and in Savannah, Georgia. He’s even been able to convince some bird advocates of the benefits of TNR.
“Ultimately, it’s not the cats that are the issue, it’s not the cats causing compassion fatigue and burnout; it’s the people in rescue, lack of resources, and how we treat or talk to one another,” Sterling says. “So many people have come to me to say they were burnt out and ready to give up until they saw me living out of my van, catching cats with a big smile on my face. I really love that!”
More About TrapKing
Sterling is currently touring with Samantha Martin and her Amazing Acro-Cats to raise awareness of TNR across the nation. His newly adopted kitten, Damita Jo, is part of the show, too.
To find out more about TrapKing and the work he and his organization do, visit trapkinghumane.org.
Thumbnail: Photography courtesy Virgil Ocampo Photography for Show Your Soft Side.
About the author
JaneA Kelley is the author of the award-winning cat advice blog Paws and Effect. She is a professional member of the Cat Writers’ Association and an advocate for all cats, whether they live with people or in the community.
Read more about rescue on Catster.com:
How to Make an Outdoor Cat Shelter
You Found a Stray Kitten — Here’s What to Do
Shutting Down Black Cat Superstitions
The post How TrapKing is Breaking Stereotypes and Changing the World by JaneA Kelley appeared first on Catster. Copying over entire articles infringes on copyright laws. You may not be aware of it, but all of these articles were assigned, contracted and paid for, so they aren't considered public domain. However, we appreciate that you like the article and would love it if you continued sharing just the first paragraph of an article, then linking out to the rest of the piece on Catster.com.
from Catster https://www.catster.com/lifestyle/trapking-breaking-stereotypes-around-rescue-and-tnr
via IFTTT
0 notes
Text
How to select a psychologist
At some time in our lives, every of us could truly feel overwhelmed and may possibly need to have aid working with our issues. In accordance to the National Institute of Mental Wellness, much more than 30 million People in america require help working with inner thoughts and problems that seem to be beyond their manage — problems with a marriage or romantic relationship, a family members situation or working with getting rid of a task, the dying of a liked one, melancholy, pressure, burnout or substance abuse. Those losses and stresses of daily dwelling can at moments be significantly debilitating. Occasionally we need outside help from a qualified, certified specialist in get to work via these problems. By ΨΥΧΟΛΟΓΟΙ ΘΕΣΣΑΛΟΝΙΚΗ of remedy, psychologists aid millions of Individuals of all ages live healthier, much more effective life.
Contemplate treatment if...
You really feel an overwhelming and extended sense of helplessness and disappointment, and your issues do not appear to get much better in spite of your endeavours and assist from household and pals.
You are discovering it difficult to have out everyday activities: for example, you are not able to focus on assignments at perform, and your job efficiency is struggling as a consequence.
You fret excessively, anticipate the worst or are continuously on edge.
Your actions are harmful to oneself or to others: for occasion, you are ingesting also considerably liquor, abusing medicines or turning out to be overly argumentative and aggressive.
What is a psychologist and what is psychotherapy?
Psychologists who specialize in psychotherapy and other kinds of psychological therapy are hugely skilled pros with skills in the regions of human habits, psychological wellness evaluation, prognosis and treatment, and conduct adjust. Psychologists function with individuals to adjust their emotions and attitudes and support them create much healthier, much more powerful styles of behavior.
Psychologists apply scientifically validated procedures to support men and women change their ideas, emotions and behaviors. Psychotherapy is a collaborative hard work amongst an person and a psychologist. It gives a supportive setting to talk overtly and confidentially about concerns and thoughts. Psychologists consider keeping your confidentiality incredibly important and will reply your questions relating to these rare conditions when confidential info must be shared.
How do I discover a psychologist?
To locate a psychologist, inquire your doctor or another wellness skilled. Get in touch with your regional or point out psychological association. Consult a regional college or school office of psychology. Question family members and close friends. Speak to your area group psychological wellness heart. Inquire at your church or synagogue. Or, use APA's Psychologist Locator service.
What to consider when making the decision
Psychologists and clientele function with each other. The correct match is critical. Most psychologists concur that an critical issue in figuring out whether or not to function with a distinct psychologist, once that psychologist's qualifications and competence are proven, is your degree of private ease and comfort with that psychologist. A great rapport with your psychologist is critical. Pick 1 with whom you come to feel comfortable and at relieve.
Inquiries to ask
Are you a certified psychologist? How a lot of several years have you been practicing psychology?
I have been emotion (anxious, tense, depressed, etc.) and I'm getting difficulties (with my job, my marriage, ingesting, sleeping, and so forth.). What knowledge do you have helping men and women with these types of issues?
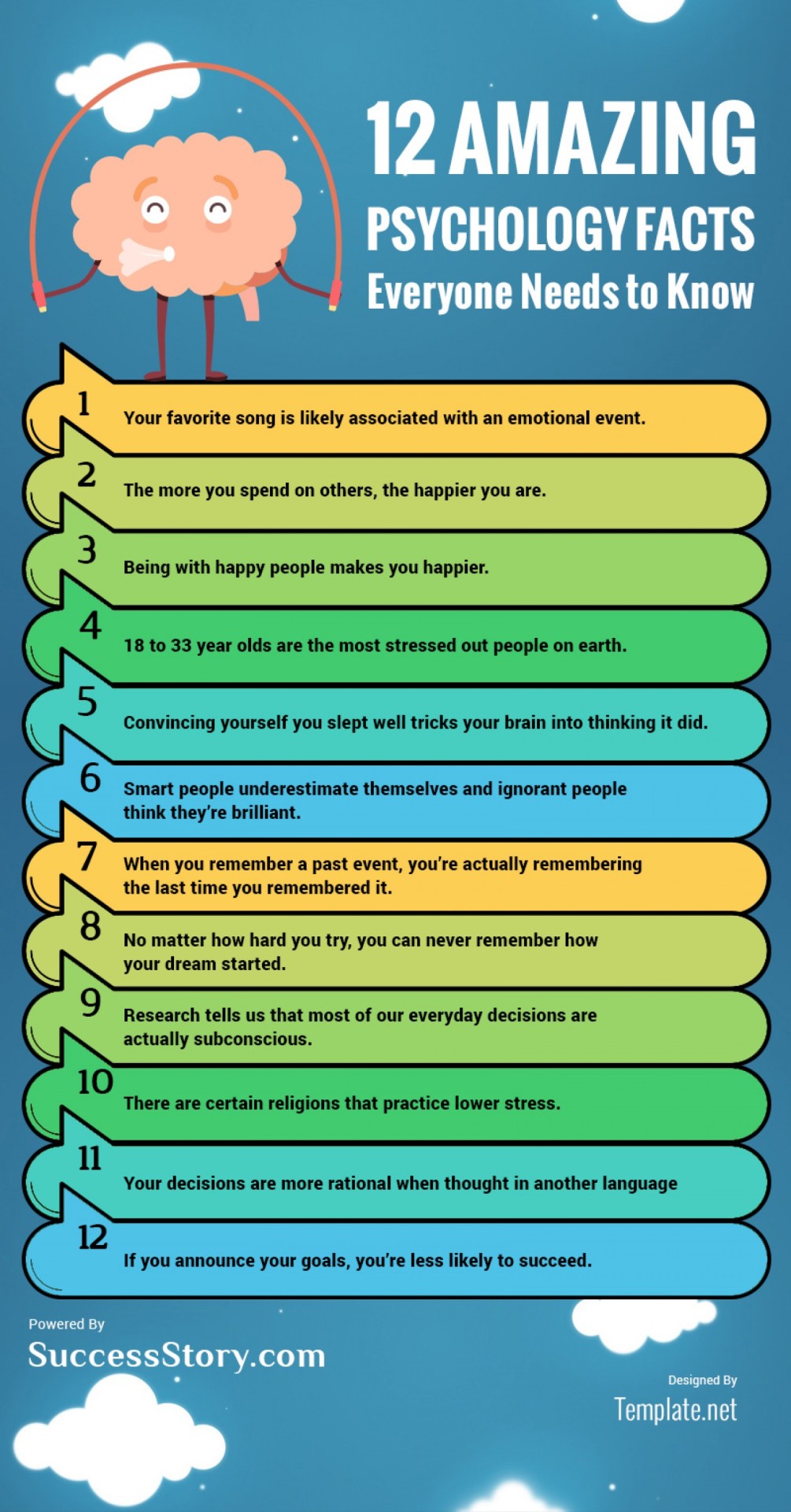
What are your regions of expertise — for example, operating with youngsters and people?
What varieties of treatments do you use, and have they been verified powerful for working with my kind of difficulty or problem?
What are your charges? (Charges are generally primarily based on a 45-minute to 50-minute session.) Do you have a sliding-scale charge policy?
What sorts of insurance do you settle for? Will you take immediate billing to or payment from my insurance policy firm? Are you affiliated with any managed treatment businesses? Do you settle for Medicare or Medicaid insurance coverage?
Funds
Many insurance policy organizations offer coverage for psychological wellness companies. If you have personal wellness insurance protection (normally by way of an employer), check out with your insurance organization to see if psychological wellness providers are protected and, if so, how you may acquire these rewards. This also applies to people enrolled in HMOs and other sorts of managed treatment plans. Find out how significantly the insurance policy organization will reimburse for psychological health solutions and what limitations on the use of rewards may utilize.
If you are not coated by a private health insurance policy strategy or worker help plan, you may possibly determine to shell out for psychological companies out-of-pocket. Some psychologists operate on a sliding-scale fee coverage, exactly where the quantity you shell out is dependent on your cash flow.
An additional prospective supply of psychological wellness providers includes govt-sponsored wellness treatment plans — which includes Medicare for people age sixty five or older, as well as health insurance ideas for authorities workers, military personnel and their dependents. Community psychological overall health facilities during the country are one more feasible substitute for acquiring psychological wellness services. Condition Medicaid plans might also offer for mental overall health providers from psychologists.
Qualifications to appear for
After graduation from university, psychologists spend an typical of 7 many years in graduate education instruction and investigation before obtaining a doctoral diploma. As part of their specialist education, they have to comprehensive a supervised clinical internship in a healthcare facility or arranged well being placing and at the very least one particular 12 months of put up-doctoral supervised knowledge before they can exercise independently in any overall health treatment arena. It is this mixture of doctoral-degree instruction and a scientific internship that distinguishes psychologists from several other mental overall health care suppliers.
Psychologists should be accredited by the state or jurisdiction in which they practice. Licensure regulations are intended to shield the general public by restricting licensure to individuals people qualified to apply psychology as described by condition law. In most states, renewal of this license depends on the demonstration of ongoing competence and needs continuing education. In addition, APA users adhere to a rigid code of expert ethics.
Will looking at a psychologist assist me?
According to a research summary from the Stanford University University of Medicine, some types of psychotherapy can effectively decrease patients' despair, stress and relevant indicators this sort of as soreness, exhaustion and nausea. Study progressively supports the notion that psychological and physical overall health are intently connected and that seeing a psychologist can boost a person's general overall health.
There is convincing proof that most people who have at least a number of sessions with a psychologist are significantly much better off than folks with psychological issues who are untreated. A single key research confirmed that 50 p.c of clients noticeably improved after 8 classes, while seventy five p.c of people in remedy improved by the end of 6 months.
How will I know if therapy is operating?
As you commence treatment, you ought to create very clear ambitions with your psychologist. You may well be attempting to defeat thoughts of hopelessness related with depression or manage a worry that is disrupting your everyday daily life. Keep in mind, particular ambitions require a lot more time to reach than other individuals. You and your psychologist need to decide at what point you might anticipate to begin to see development.
It is a excellent indication if you get started to feel a perception of relief, and a perception of hope. Individuals often really feel a wide assortment of feelings throughout treatment. Some qualms about remedy that folks may have end result from their getting trouble speaking about painful and troubling encounters. When you get started to come to feel relief or hope, it can be a good signal indicating that you are starting to explore your views and behavior.
0 notes
Text
RHR: How to Fight Practitioner Burnout with Dr. Akil Palanisamy
https://healthandfitnessrecipes.com/?p=9582
In this episode, we discuss:
Burnout among healthcare practitioners
How common the problem is
The results of widespread physician burnout
The difference between burnout and moral injury
How technology is contributing to the problem, not alleviating it
How to fight physician burnout
Show notes:
The Paleovedic Diet by Dr. Akil Palanisamy
The Sutter Health Institute for Health & Healing in San Francisco
Unconventional Medicine by Chris Kresser
1440 Multiversity retreat for healthcare professionals
Akil Palanisamy’s website, DoctorAkil.com
[smart_track_player url="http://traffic.libsyn.com/thehealthyskeptic/RHR_-_How_to_Fight_Practitioner_Burnout_with_Dr._Akil_Palanisamy.mp3" title="RHR - How to Fight Practitioner Burnout with Dr. Akil Palanisamy " artist="Chris Kresser" ]
Chris Kresser: Hey, everybody, Chris Kresser here. Welcome to another episode of Revolution Health Radio. This week we’re going to be talking to Dr. Akil Palanisamy, who is a friend and colleague in the Functional Medicine space. And I’ve known him for several years. He is the author of The Paleovedic Diet, a really interesting book combining Paleo and Ayurveda, a traditional Indian medicine which is an interest of his. And he also runs the Paleo Symposium that’s put on by the Institute for Health & Healing at UCSF every year, that I’ve been a featured speaker at since it started.
But today actually, we’re going to be talking about something different, which is burnout amongst healthcare practitioners. It’s a really important topic that has pretty significant implications not only in terms of the effect on individual clinicians, but on patients and their access to care, things like medical errors and just the healthcare system overall.
So if you’re not familiar with Akil, he’s an integrative medicine physician who blends his medical training with Functional Medicine in Ayurveda, the traditional medicine of India. He studied biochemistry at Harvard and received his medical degree from UCSF and completed his residency at Stanford. Dr. Akil also completed a fellowship in integrative medicine with Dr. Andrew Weil at the University of Arizona. He sees patients at the Sutter Health Institute for Health & Healing in San Francisco, where he also serves as physician director for community education. He’s been a consultant with the medical board of California for many years and as I mentioned, he’s the author of The Paleovedic Diet: A Complete Program to Burn Fat, Increase Energy, and Reverse Disease.
So I’m really excited to dive into this conversation with Akil. I think you’ll find it interesting, even if you’re not a healthcare practitioner that’s experiencing burnout, because we talk about a lot of issues that are relevant to anybody doing any kind of work, really. So I hope you enjoy the conversation. Let’s dive in. Akil, thank you so much for joining us. I’m so glad to have you here.
Akil Palanisamy: Thank you, Chris. Pleasure to be here.
Burnout among healthcare practitioners
Chris Kresser: So today we’re going to talk about a really important topic that I don't think gets enough attention, and this is physician burnout. So, and I would extend it to burnout for any healthcare practitioners. We might be focusing a little bit on physicians because this is where most of the statistics are available, but it’s certainly a problem across the entire healthcare world whether we’re talking about:
Nurses
Nurse practitioners
Occupational therapists
Chiropractors
Acupuncturists
Anybody working in the care profession
In my book Unconventional Medicine, I talked a lot about how this is one of the major challenges within medicine in general, not just conventional medicine, but also integrative medicine and Functional Medicine. And it's something that we need to develop a sensible approach to if we’re going to meet our goals in terms of preventing and reversing disease. So this is something that Akil has thought deeply about and has been involved in a number of different initiatives from his work at Sutter to working with medical students and other physicians to address this problem. So I'm really looking forward to having this conversation. So why don’t we start a little bit with the stats on burnout, Akil?
Ask yourself: Does medicine still feel like your calling? If daily stress and exhaustion are turning you away from the profession, you might be headed toward physician burnout. Find out what causes burnout and learn how to rediscover your sense of purpose.
How common the problem is
Akil Palanisamy: Sure, yeah, I think it's really rampant, and most studies report around 50 percent or higher of physicians report some significant burnout. And that's up from about 40 percent just five years ago. So, I think the numbers are really scary and also this is a global problem. So this is across the board. Many countries throughout the world and also regardless of the stage of training. So medical students, residents, physicians, even the number of years of practice has no impact.
Chris Kresser: Wow.
Akil Palanisamy: I will check on this number, so, I mean, I know because I did my medical training 20 years ago, and it was like, I would say, a soul-crushing and exhausting process.
Chris Kresser: Right, right.
Akil Palanisamy: So I started early in this topic, and that’s why I’m so passionate about it.
Chris Kresser: Yeah, yeah. That’s really revealing in some ways. If medical students are as burned out as people who've been in the profession for 10 or 20 years, that's an indication that something’s already going wrong, even at that very early stage.
Akil Palanisamy: Right. I came across a really fascinating study. They interviewed almost 3,000 medical students about burnout and 53 percent of them reported feeling burnt out. About 15 percent were depressed, about 5 percent had seriously considered suicide. But the interesting thing was 100 percent of the students, every single one reported feeling humiliated at some point, demeaned, disrespected as part of their training. And that had huge effects on their performance and judgment, and that was my experience too. It’s part of the culture of training doctors.
Chris Kresser: It really is, isn’t it? It’s almost like fraternity hazing or something. I've heard for residents that it's … and it seems to be perpetuated for some of the same reasons, like this, “I went through this, so you have to go through it,” type of mentality. And I've even read the studies that support that.
Akil Palanisamy: Yeah, right. When I started my residency, I was super thrilled because they had just passed a law limiting the work hours, continuous work hours to 24 hours in a row. That was like a huge drop.
Chris Kresser: That’s a big development.
Akil Palanisamy: And I was like, “Wow, this is fantastic. I only have to work 24 hours in a row, like, every week.” And people thought that would solve the problem of burnout. But it hasn’t because that’s just one of many factors.
The results of widespread physician burnout
Chris Kresser: Right, and so we know that there’s a huge problem with the shortage of primary care physicians. I don't remember the exact number from the study I shared in my book, but it's something like, predicted to be a shortage of around 50,000 primary care providers by the year 2025, which is not very far off in the future. And yet one of the costs of burnout, as you said, is that two-thirds of physicians know a doctor who is likely to stop practicing medicine or at least to reduce their access to patients, switch to concierge model, or something like that within the next five years as a result of burnout. So this is a real problem that's really kind of having an outsize effect on our healthcare system.
Akil Palanisamy: Yeah, absolutely. I mean, I think it is genuinely a public health crisis. And I think that that word is increasingly being used in the literature because this really does impact not just individual physicians but patients, healthcare organizations, the entire healthcare system in our country and other countries around the world. So I think the scope of the effects and the impact of burnout is being recognized now and it's huge in terms of not just the individual level, but medical errors as well. So, recent studies have shown that there’s a strong relationship between physician burnout and medical errors. And already medical errors are one of the major leading causes of death in the United States. And so I think as we get more burned out physicians and higher rates of medical errors, I think that's one of the big issues in terms of the costs of this problem.
Chris Kresser: Yeah, this is critical, and I highlighted this in my book. But if you go to a site like CDC or a general website and you search for the top 10 causes of death, let’s see what happens if we do that right now. Cardiovascular disease is still holding at number one, and then you’ve got lung cancer or you’ve got other diseases that come shortly after that. The data is often changing. Cancer continues to go up the list. But you’re not going to see medical errors on these lists, right?
Akil Palanisamy: Right.
Chris Kresser: There was a study published in the British Medical Journal in 2016, just a couple of years ago, and then another one by Barbara Starfield, who’s since passed away, back in 2000 in JAMA. And both of those found the same thing, that medical errors are actually the third-leading cause of death. And since only 5 to 15 percent of the atherogenic events are even reported, Dr. Starfield actually speculated that medical errors could be the number one cause of death if all of the atherogenic events were reported. So this is something you don't see on the typical list, but that doesn't mean it's not true.
Akil Palanisamy: Right, exactly. Yeah, because when you experience burnout, the impaired judgment, lack of attention to detail, communication breakdown, all the things, the depression, that just greatly increases the risk of medical errors.
Chris Kresser: Right. So this is a, it's a common problem, it's a problem that has not only effects on individual practitioners and their health and their lifespan, their feelings about their work, but also to patients and their safety and their ability to get the care that they need, and then to society as a whole. The healthcare crisis continues to deepen, and we need more doctors, rather than fewer. The fact that 50 … that two-thirds of physicians know a doctor who’s likely to stop practicing medicine in five years is exactly the opposite direction that we need to be going in here.
The difference between burnout and moral injury
So let's talk … so, we’ve been throwing this term “burnout” around, and I'm sure that means different things to different people. But you actually emailed me before the show with a really interesting distinction that I want to highlight—the difference between burnout and moral injury. So can you talk about that a little bit?
Akil Palanisamy: Yeah, absolutely. So traditionally, burnout is defined as a work-related syndrome characterized by emotional exhaustion, a cynical feeling, and feeling like you're ineffective on the job. But this concept of burnout really doesn't resonate with doctors. I can tell you from talking to many of them that they really don't connect with this concept of burnout because the problem is you're pointing the finger at doctors. And you’re saying, “You’re burned out, you need to start doing yoga and eat granola, and just like change your lifestyle.” But you know, these are some of the most resilient people out there.
Chris Kresser: Absolutely.
Akil Palanisamy: Medicine, I mean we’ve survived decades of intense training, sleep deprivation, the training process itself is incredibly stressful, the work demands. So these are some of the most resilient and resourceful people out there. And so I think the problem is really, a big part of it is the system. But the distinction that you mentioned between moral injury and burnout, the concept of moral injury actually was first used to describe how soldiers responded to what they did during war and when they came back, having to do things that went against their morals.
In healthcare, it refers to physicians being unable to provide the high-quality care that they would really like to, essentially, not being able to be true to themselves. So I think the problem is not that physicians are burned out and so we don't care. The problem is that we care very deeply.
Chris Kresser: Care too much.
Akil Palanisamy: Yeah.
Chris Kresser: Not too much, but it’s the care that’s causing the problem, yeah.
Akil Palanisamy: Right and then as a result, in our current healthcare system, it's so hard to consistently meet patients’ needs and provide the kind of care that we envisioned we would going into medicine. Because most doctors think of medicine as a calling, and so that failure and inability to meet needs of patients in the way that we really envision, that is hugely damaging, and I think that has a huge effect on physician well-being. And so that's the concept of moral injury. So I think that it's really much broader than just pointing the finger at doctors.
Chris Kresser: I think that’s really, really important to understand, and I've always made it clear that when I'm criticizing conventional medicine and its shortcomings, I'm not criticizing individual doctors. Of course, I might be criticizing some individual doctors, but not as a group because the vast majority of doctors that I have met are people that genuinely want to help their patients. They went into medicine for all the right reasons and they do recognize that they're not having the impact that they would like to have, and it's painful for them. But there's, they feel like their hands are tied because of the way that the system is set up. And they’re just as much victims of the system as the average patient is.
And I think this is a good example of how that plays out where we all want to have meaningful and rewarding work. We all want to get to the end of the day and feel like we really made a difference. And doctors, I think, especially. That's the path they chose. They didn't go into private equity. They didn't choose to go into a career that was really not about helping people, but more about making money or enriching their own lives. Not that there's necessarily anything wrong with that. They willingly chose to go through a very arduous path that involves many, many years of schooling and as you said, rigorous training with residency, working 24 hours straight, often graduating with hundreds of thousands of dollars of debt. I mean, it’s an enormous risk to take, an enormous amount of investment of money and time and energy to become a physician.
So you don't make it through that generally, unless you really have a guiding moral compass that is pushing you through it. And so it's really, I think, even more important and critical that we figure out a way to, where we create a path forward for doctors and other healthcare practitioners that really do want to have that feeling at the end of the day. Because that's the antidote to burnout, where when you really do feel like you're transforming the lives of the people that you're working with, and you're having a huge impact. Because in that situation it doesn't mean you won't get tired and it doesn't mean you won't occasionally feel, “Geez, I need a vacation.” But you're not going to have that moral injury, and that’s what makes all the difference in the world.
Akil Palanisamy: Yeah, I know, exactly. And I think that the rates of suicide among physicians is a real wake-up call because it’s twice that of I think active duty military, and then there was a report from the UK that there was a young junior doctor who, she took her own life by walking into the sea.
Chris Kresser: Yeah, that’s not, yeah.
Akil Palanisamy: Statistically, women physicians are a significantly higher risk of completed suicide than matched females in other professions. So it’s not uncommon, unfortunately, and I think that, yeah, exactly what you said about that moral compass that physicians have, I think being able to feel like you're true to yourself. That's a basic need that all of us have, and I think especially those who go into medicine, we feel that pretty intensely.
How technology is contributing to the problem, not alleviating it
Chris Kresser: Right. And there may be lots of choices every day that they have to make that are, don't feel true to themselves because of the way that the system is set up. And I know from my own research and I know you and I have talked about this, one of the influences in terms of burnout has been the rise of electronic medical records or electronic health records, EMRs and EHRs. Initially these were hailed as, that this is going to dramatically reduce the amount of paperwork that doctors would have to do and they were going to be great time-saving and productivity devices, and they were going to be doctors’ best friends. But the reality has not quite lived up to that, has it?
Akil Palanisamy: No, no. Yeah, I would, I think that studies show that about like half of the average physician’s workday is spent entering data or doing other clerical work in the EHR. So the amount of time actually spent with patients is less than a third, and for me I think it's a bit of a double-edged sword. Because it does make it easier to respond to patient messages rather than playing phone tag with patients. But on a typical day, I might get 50 to 60 electronic messages in addition to charting visit notes for each patient, and each of these questions or patient calls, etc., requires some thought.
And increasingly we’re being measured on how quickly we can respond to these messages because the priority is patient satisfaction, and that's eventually going to be tied to financial compensation and that kind of thing. So I think this EHR, it takes up so much time, and it really hasn’t translated to the reduced workload and that sort of thing. And when we deal with insurance in my practice, I think that's a huge benefit for patients because it improves access, and for Functional Medicine and integrative medicine, I think we need to move in that direction where insurance covers services. And so we offer that, but then it creates a whole universe of responsibilities in terms of the paperwork, the criteria for each progress note when we’re billing insurance, the forms, the prior authorizations, the other kind of paperwork. So it just adds another layer of paperwork to everything else that we’re dealing with in terms of the EHR every day.
Chris Kresser: Yes. And then there’s another issue of when you're actually in the room with the patient, that connection that you're trying to make with the patient is now being mediated by a computer screen and having to type into the computer. And we’ve all seen, I've heard many stories of people going to doctors and complaining that their doctor was hardly even looking at them because they were working on the computer the entire time, and this is especially true with younger doctors from what I've heard, who never operated without an EHR.
So they never had the experience of being in a visit with the patient without the computer being part of that. And I think with all the data that we now have in terms of how important the physician-patient relationship is to the outcomes in care and the research on the placebo effect, and just the, in Carl Rogers's words, the unconditional positive regard and the type of connection that is made just is therapeutic in its own right. And I think the EHR can compromise that in some ways.
Akil Palanisamy: Yeah, absolutely. And I'm always torn because I want to maintain good eye contact and really be present with each patient, but then if I don’t touch the EHR at all, then at the end of the day I’m like, this one’s like …
Chris Kresser: You’ve got eight more hours of work.
Akil Palanisamy: Exactly.
Chris Kresser: It’s really challenging, and, I mean, my solution to that, which is not possible for everybody because of the model I work independently, so I’m able to just kind of set things up how I want. But I have a nurse practitioner that's by my side at every appointment, and she takes the notes. So I'm able to just maintain eye contact with my patient and not really look at the computer. And I recognize that's not a viable solution for most practitioners, but it's something that I felt compelled to do because I, like you, didn't want to get home and do four hours of data entry into the EHR after a full day of seeing patients. And but I didn't also want to sacrifice the connection with the patient.
So I think the other thing that's also not always in an individual physician’s control is the quality of the EHR or the EMR system. So many of them are just completely bloated and full of functions that they'll never use, and just really difficult to navigate, and they’re a nightmare in terms of software development. They’ve been just sort of cobbled together and put on top of each other, and it’s, for anyone who likes software and technology, EMR software is not going to be particularly inspiring for the most part.
Akil Palanisamy: Yes, yeah. No, I think you’re right on that. And the point about having additional support for progress notes, I think, is a good one because studies show that having some type of help with the charting actually reduces burnout, and it's obvious, right? And I think at Sutter Health where I work, they really take burnout quite seriously. And so they’ve supported having scribes, which is the same thing. They take notes and they kind of do everything, and you just have to sign the note.
So I think it’s really, it’s a shared issue with burnout between individuals and healthcare systems and organizations. So I think it’s very important that all of these systems realize they have an important role to play, and I think Sutter Health is a really great example of that. They've supported a lot of these changes, and like this example of scribes and with our EHR, which is Epic, just helping us to use it in the most efficient way possible. So I think systemic changes are really a huge part of the solution as well.
Chris Kresser: Absolutely, and this is a recurring theme in this conversation. It's that individual physicians can only do so much when they're employed in a larger organization, and they’re not free to just do whatever they want. And so we have to continue to work to raise awareness institutionally about these issues so that the institutions themselves can make the changes, and then individual physicians will benefit from those.
Akil Palanisamy: Right.
How to fight physician burnout
Chris Kresser: So let's talk a little bit about some of the work you've done in the past with medical students and other doctors at Sutter on burnout. What kind of things have you done to approach this?
Akil Palanisamy: Yeah, I think for me during medical school, it was really a survival mechanism. Because I was pretty burned out and the training, yes, I absolutely had that being belittled and demeaned when I was on the wards in my rotations. And so I really got interested in the certain classes that were offered on finding meaning in medicine and really connecting with your purpose or actually reconnecting with why you went into medicine, and keeping that front and center. And also developing tools for maintaining well-being like mindfulness.
So mindfulness is one thing that has been studied. There’s actually been about 14 studies looking at physician burnout and mindfulness, and nine of them have shown positive outcome in terms of:
Reducing burnout
Improving well-being
Improving mood
Improving resiliency
So I think, I don't think that's the entire solution, but the more tools you have in your toolkit, the better. And we don't really get any training in general in terms of how to deal with stress and how to manage emotions during our healthcare training. And so I think I got into mindfulness very early, studied MBSR, developed a daily meditation practice, became involved in educational programs teaching people about mindfulness. And then since … then during residency and now practice, after that I've been very interested in workshops and events that kind of focus on that aspect of meaning and really reconnecting with a sense of purpose, a sense of direction. Kind of helping people be true to themselves.
And so I think small group exercises and workshops where people are getting out of their left brain and reconnecting with their right brain, using art and things like that, have been really effective. So for me, I've benefited as much as I’ve helped anybody in this work, and it's been just partly for my own gains, but I think you teach what you have to learn. And for me, being involved in burnout and teaching people about it has been a lifesaver.
Chris Kresser: That’s so great. I think all of those are fantastic tools for kind of exploring the causes of burnout on an individual level and helping people respond in a way that will reduce the risk of moral injury, if we will. And I know for me, one of the ways that I've approached this personally and also with people that I've worked with and that I’ve trained is just to make sure that I feel like the work I'm doing is having a big impact on my patient’s lives. Because that’s one of the reasons I really love that distinction that you make between burnout and moral injury. Because if I look at it that way, I think, “Okay, well, that's the biggest risk is just getting to the end of the day and feeling like I'm not making a difference. Feeling like all of my efforts are for naught really. Or they’re not really having the impact that I would like them to have.” And to me, that's the greatest risk in terms of burning out. When I know that my work is making a difference, my endurance and stamina are considerable.
Akil Palanisamy: Right.
Use Functional Medicine to prevent it
Chris Kresser: But when I don't feel that way, it doesn't take much to make me feel tired and like what I'm doing is not worth it. So this is, I think, where a Functional Medicine approach has a lot to offer, not just as a treatment modality, but as a means of really actually making a difference in the patients’ lives. Like getting to the root cause of the problem and actually addressing the problem and helping the patient to recover and feel better without the use of unnecessary drugs and surgery. For me that was one of the most appealing things about Functional Medicine, and I think it's one of the less talked about but most important gifts that it has to offer to individual physicians who shift their practice in that direction.
Akil Palanisamy: Yeah, I think that's what motivated me to go into Functional Medicine as well, just to get that sense of fulfillment and satisfaction when you help someone really get a permanent solution to something and by uncovering the root causes and taking that holistic approach. So I think that's what drew me to Functional Medicine as well.
Schedule a retreat
Chris Kresser: Absolutely. So another area where I know, or a kind of antidote to burnout that I know that you and I are both passionate about is a retreat. So I've been a big believer in retreat. I’ve done annual retreats myself for many years. I’ve done meditation retreats for about 25 years and I just can't really imagine my life without that opportunity to step away from my day-to-day life and experience and to get a different perspective, to slow down, to have more spacious existence for a few days were the busyness of life is not overtaking me and where I can just hear myself think and feel my body, and just look at things from a fresh perspective. It's just crucial for me. And I've always felt like my wish has been that others can experience this. That we can, because I really believe in its transformative power.
Connect with colleagues
Akil Palanisamy: Yeah, absolutely. I do as well, and I’ve had a number of retreats over the years in terms of individual retreats and also group retreats. And especially in the professional setting, I find that ability to connect with other colleagues and professionals in that informal, nonwork setting is so powerful because in healthcare there's so much isolation. There are so many individual silos.
Everybody's just doing their thing trying to get through the day, and you rarely have a chance to step back and step out of that situation to just really deeply connect with people who are in the same boat and really understand what they're going through, share their story, listen to their stories, and really deepen your connection and solve problems together.
So I think that sort of deep connection is so important because that's like a huge need for all human beings, and especially in such an isolating profession like in healthcare. I think it's essential.
Chris Kresser: Absolutely, yeah. So many clinicians can just spend, we spend most of our time in a room with patients and we’re interacting with patients, but we’re not, we’re interacting with them in a certain way. We’re playing a certain role. We’re the clinician, they’re the patient, and those can be rich and rewarding interactions. But it's not the same as connecting with other colleagues and being able to talk about the issues that we face professionally and share together. So yeah I think that group experience is really powerful. And I’ve been writing about this recently.
I’ve been sharing some book recommendations, and Akil and I have actually teamed up to offer a retreat for healthcare practitioners at 1440 Multiversity in October. It’s from October 5th to 7th this year. And so it starts on Friday afternoon, Friday evening, and it goes through Sunday midday. And the retreat’s called “From Burnout to Brilliance: Rediscover Your Passion and Purpose, Reclaim Your Health, and Create a Practice You Love.” So the intention of this retreat is to address the issues that we've been talking about in the show and to help healthcare professionals explore their own situation, help them rediscover their passion for medicine and healthcare, and reconnect with a sense of meaning and purpose in their work to take some practical steps. Break those down into really doable actionable steps that they can take to reclaim their health and well-being. Rediscover parts of themselves that are not typically expressed in the course of their day-to-day work and just kind of cultivate a sense of energy and vitality that they may have been missing for many years.
And I'm really excited about doing this. I’m excited about doing this with Akil, who I've known for several years now and I really respect, and I'm excited about doing it at 1440. It's an incredible new retreat center, which I think you did a retreat there with Michelle Tam with Nom Nom Paleo last year, Akil?
Akil Palanisamy: Yes, yes beautiful, beautiful place. Yeah.
Chris Kresser: So this is, and for those of you who are not familiar, it's in Santa Cruz Mountains, right?
Akil Palanisamy: Yeah, it’s surrounded by redwood trees and there's all these amazing hiking trails. And yeah, a beautiful place.
Chris Kresser: Yeah. I haven't actually been there yet, but I know several people who’ve taught there and who’ve been there. And if you go to 1440.org, click on the stay button and check out some of the pictures. It's an absolutely beautiful campus. Really nice accommodations, gorgeous dining hall with lots of different food options. They've got daily yoga classes and massage, and a spa and other health offerings there. And they’ve got, of course, gorgeous hiking trails because it's in the redwood forest there. It just looks to me like they're really doing it right. I've been to a lot of retreat centers. I actually lived at a retreat center in Big Sur called the Esalen Institute …
Akil Palanisamy: Oh. sure.
Chris Kresser: … and many people may be familiar with. When I was still really sick and dealing with my health issues, I got to a point where I just decided, I kind of reached the end of the line of supplements and diets, and medications, and I decided that I would explore the psychological, emotional, psycho-spiritual aspects of what was going on for me. So I moved to Esalen and lived there for a couple of years. So I'm very familiar with retreat centers. I've been to many others around the country, both for Buddhist meditation retreats and other retreats, and I have, they're all great in many ways. But they’re, I can see that 1440 is bringing it to a different level.
So I'm excited to be a part of that. I'm excited to get together with a group of professionals that are all wanting to cultivate more meaning in their work and to find that work/life balance that can be so elusive. And I just can't wait to get together and support each other and share because that's, I mean, we all have so much to offer, and I think when we come together with a similar purpose, it's really powerful.
Akil Palanisamy: Yeah. I am also really excited about the upcoming event, and I think for anyone who feels like they're not being true to themselves in their work or as to themselves as they would want to be, I think this is a great opportunity to really reflect. And I think our vision for that weekend is that it's going to be a very introspective weekend and really focused in small groups and interactive elements. So it’s not going to be just mostly didactic.
Chris Kresser: Yeah. It’s not going to be Akil and I standing in front of the room talking at you the whole time. Definitely going to be the opposite of that.
Akil Palanisamy: Right, exactly, yeah. Because I think that this work is really about looking within and then sharing and connecting with other people. And so that's the focus of the weekend, is really building that sense of community with whoever comes and really learning to deepen your own sense of meaning and purpose in work, and look within to reconnect with that vision for what drew you to this work initially. Because I think that's the ultimate goal is having that feeling like you're really being true to yourself at the end of the day and having the kind of practice that you envision.
Don’t be afraid to make changes
Chris Kresser: Absolutely. I shared the story of Sheri in my book Unconventional Medicine, who is a clinician that was working in the VA. And she's a doctor and was mostly seeing patients with diabetes. That's the most common health challenge for veterans. And it was, she was counting the days until retirement. It was just really a factory-medicine type of situation. She often didn’t even have time to go to the bathroom during the day because she was just that busy from appointment to appointment. And as we've discussed, there was a real risk of moral injury because she didn't feel like she was making a difference. She was just handing out medications to these people and she wasn't, she knew as an athlete herself who tried to pay attention to her diet, she knew that wasn’t the best way to go about it. But what else could she do in the amount of time that she had?
And she moved into kind of a more, started incorporating more of a functional approach in her work, and then eventually left and started her own Functional Medicine practice. But for her, it was just a total game changer. She went from counting the days to retirement, to not ever being able to imagine retiring. And that's the kind of shift that’s possible, I think, when you really address the root causes of burnout and take the opportunity to step out of your current system, your current day-to-day, and really give yourself the chance to discover something new. And even if that’s maybe moving in a different direction entirely, or maybe staying in your current situation but just making a series of small changes that collectively can have a big impact.
Akil Palanisamy: Yeah, I think for me, my whole approach has been in terms of incremental change because I know that for many people, they have gone out of the insurance model and set up their own Functional Medicine practice, and that can be fantastic. But my work is really just building change within the system. Because if the people within the system leave and do their own thing, then the system itself is going to not be changed. And so I think that a big part of this is also figuring out solutions within systems and incremental steps we can take, and I think that'll hopefully be part of what we talk about as well. Just if you do belong to a system, how you can take a leadership role and effect change within that system as well.
Chris Kresser: Absolutely. That's why Akil and I are a good team, because I’m outside the system and he’s inside of the system, and we have different perspectives. So that's another reason I'm happy to team up with him. I mentioned this in the beginning, but I'll throw it out there again. You need not be an MD to participate in this workshop. It's really for all healthcare practitioners and providers who are experiencing burnout. And so this could be anyone from a health coach to a nutritionist to a dietitian to an occupational therapist to a chiropractor, a naturopath in addition to MDs, and DOs, and MPs, and PAs, and all of the other abbreviations and acronyms. Anyone working in healthcare really would be welcome. And we’re not even limiting it to people working in healthcare. We don't want to exclude people here, so if you're not working in healthcare and the things we've been talking about resonate with you, maybe you work in emergency services or something else, you are absolutely welcome to come.
Akil Palanisamy: Yeah, and I would add that even if you're not feeling burned out, I think that prevention is really the best medicine.
Chris Kresser: That’s true.
Akil Palanisamy: So I think learning about the research and the science, because we know how to prevent it, and it's much better to prevent burnout than treat it once it happens.
Chris Kresser: That is a very good point. Yeah, and I guess if the statistics are any indication, we know that even if you’re not feeling burnout now, chances are statistically you will at some point.
Akil Palanisamy: Right.
Chris Kresser: Especially without any intervention. It’s kind of like the diabetes example I used before. If you’ve got high normal blood sugar, now’s the time to get it under control rather than waiting until it turns into diabetes.
Akil Palanisamy: Right.
Chris Kresser: Great, well, thank you so much, Akil, for being with us. It’s a fascinating and important topic, and I’m really looking forward to leading this workshop with you. Again, in the retreat, you can go to 1440, it’s 1-4-4-0 dot o-r-g, and when you get there on the website, you just hover over Learn, and then under programs click on Professional Development. And if you scroll down there, you’ll see our program, which, again, is on the first weekend of October, October 5th to 7th, it’s a Friday through a Sunday.
And there’s a tuition for the program, and then there’s several different accommodation options available there. It’s really neat. I like what they've done with that. Everything from a private room to a suite to a really cool bunk style, kind of modern bunk-style accommodation that's much more affordable. I don’t know if you saw those last time.
Akil Palanisamy: I did, yeah.
Chris Kresser: Check the pictures out, they look pretty cool. They call them pods.
Akil Palanisamy: Right, yeah, yeah. They’re pretty comfy. I’ve seen them.
Chris Kresser: Yeah, yeah, it looks great. So lots of different accommodation options. If you’ve never been to this part of the world, the Santa Cruz Mountains are a beautiful, beautiful area, gorgeous redwood forests. You can head down to the beach before or after in Santa Cruz there. It’s a funky, cool little town. Great, great part of the world. So I hope you can make it. Those of you who have been listening to this and resonating with it, we’d love to meet you in person and have a chance to explore these topics with you.
And then Akil, is also, we haven’t talked much about his other work, but he’s also an author in addition to being a clinician. And he organizes the Paleo Symposium every year that I've been fortunate enough to be a speaker at. So why don’t you tell everyone a little bit more about your work and where they can find out more about your work.
Akil Palanisamy: Oh sure, yeah. So I practice integrative medicine and I combine Functional Medicine with the Paleo approach and Ayurveda, which is the traditional medicine of India. And still that has led to my book which is called The Paleovedic Diet, combining Paleo and Ayurvedic medicine. And the best way to connect with me would be through my website, which is DoctorAkil.com. Just doctor spelled out, A-k-i-l dot com. And yeah, I wanted to thank you, as well, Chris, for having me on the podcast. I’m very excited to be working on this event with you, and it was really a pleasure to talk today.
Chris Kresser: Pleasure is mine, Akil. And I'm sure we’ll be in touch before October, but I look forward to seeing you then and anyone else who's listening, who wants to join us. So 1440.org, and thanks for listening, everybody. Keep sending your questions in. I know I haven’t answered many of them recently. We’ve been doing a lot more interviews lately. But I do see that I have a few Q&A episodes coming up, and we do read all of your questions, and we also consider them for writing articles or emails.
So even if we’re not able to answer them on the show, it helps me to understand what you're thinking about and what you want me to write about and talk about. So please do keep sending them in. That’s ChrisKresser.com/podcastquestion. And thanks, everyone, for listening. And thank you, Akil, and we’ll see you next time.
Akil Palanisamy: Thank you, Chris.
The post RHR: How to Fight Practitioner Burnout with Dr. Akil Palanisamy appeared first on Chris Kresser.
http://media.blubrry.com/thehealthyskeptic/traffic.libsyn.com/thehealthyskeptic/RHR_-_How_to_Fight_Practitioner_Burnout_with_Dr._Akil_Palanisamy.mp3
Credits:
Original Content Source
0 notes
Text
RHR: How to Fight Practitioner Burnout with Dr. Akil Palanisamy
In this episode, we discuss:
Burnout among healthcare practitioners
How common the problem is
The results of widespread physician burnout
The difference between burnout and moral injury
How technology is contributing to the problem, not alleviating it
How to fight physician burnout
Show notes:
The Paleovedic Diet by Dr. Akil Palanisamy
The Sutter Health Institute for Health & Healing in San Francisco
Unconventional Medicine by Chris Kresser
1440 Multiversity retreat for healthcare professionals
Akil Palanisamy’s website, DoctorAkil.com
youtube
[smart_track_player url="http://traffic.libsyn.com/thehealthyskeptic/RHR_-_How_to_Fight_Practitioner_Burnout_with_Dr._Akil_Palanisamy.mp3" title="RHR - How to Fight Practitioner Burnout with Dr. Akil Palanisamy " artist="Chris Kresser" ]
Chris Kresser: Hey, everybody, Chris Kresser here. Welcome to another episode of Revolution Health Radio. This week we’re going to be talking to Dr. Akil Palanisamy, who is a friend and colleague in the Functional Medicine space. And I’ve known him for several years. He is the author of The Paleovedic Diet, a really interesting book combining Paleo and Ayurveda, a traditional Indian medicine which is an interest of his. And he also runs the Paleo Symposium that’s put on by the Institute for Health & Healing at UCSF every year, that I’ve been a featured speaker at since it started.
But today actually, we’re going to be talking about something different, which is burnout amongst healthcare practitioners. It’s a really important topic that has pretty significant implications not only in terms of the effect on individual clinicians, but on patients and their access to care, things like medical errors and just the healthcare system overall.
So if you’re not familiar with Akil, he’s an integrative medicine physician who blends his medical training with Functional Medicine in Ayurveda, the traditional medicine of India. He studied biochemistry at Harvard and received his medical degree from UCSF and completed his residency at Stanford. Dr. Akil also completed a fellowship in integrative medicine with Dr. Andrew Weil at the University of Arizona. He sees patients at the Sutter Health Institute for Health & Healing in San Francisco, where he also serves as physician director for community education. He’s been a consultant with the medical board of California for many years and as I mentioned, he’s the author of The Paleovedic Diet: A Complete Program to Burn Fat, Increase Energy, and Reverse Disease.
So I’m really excited to dive into this conversation with Akil. I think you’ll find it interesting, even if you’re not a healthcare practitioner that’s experiencing burnout, because we talk about a lot of issues that are relevant to anybody doing any kind of work, really. So I hope you enjoy the conversation. Let’s dive in. Akil, thank you so much for joining us. I’m so glad to have you here.
Akil Palanisamy: Thank you, Chris. Pleasure to be here.
Burnout among healthcare practitioners
Chris Kresser: So today we’re going to talk about a really important topic that I don't think gets enough attention, and this is physician burnout. So, and I would extend it to burnout for any healthcare practitioners. We might be focusing a little bit on physicians because this is where most of the statistics are available, but it’s certainly a problem across the entire healthcare world whether we’re talking about:
Nurses
Nurse practitioners
Occupational therapists
Chiropractors
Acupuncturists
Anybody working in the care profession
In my book Unconventional Medicine, I talked a lot about how this is one of the major challenges within medicine in general, not just conventional medicine, but also integrative medicine and Functional Medicine. And it's something that we need to develop a sensible approach to if we’re going to meet our goals in terms of preventing and reversing disease. So this is something that Akil has thought deeply about and has been involved in a number of different initiatives from his work at Sutter to working with medical students and other physicians to address this problem. So I'm really looking forward to having this conversation. So why don’t we start a little bit with the stats on burnout, Akil?
Ask yourself: Does medicine still feel like your calling? If daily stress and exhaustion are turning you away from the profession, you might be headed toward physician burnout. Find out what causes burnout and learn how to rediscover your sense of purpose.
How common the problem is
Akil Palanisamy: Sure, yeah, I think it's really rampant, and most studies report around 50 percent or higher of physicians report some significant burnout. And that's up from about 40 percent just five years ago. So, I think the numbers are really scary and also this is a global problem. So this is across the board. Many countries throughout the world and also regardless of the stage of training. So medical students, residents, physicians, even the number of years of practice has no impact.
Chris Kresser: Wow.
Akil Palanisamy: I will check on this number, so, I mean, I know because I did my medical training 20 years ago, and it was like, I would say, a soul-crushing and exhausting process.
Chris Kresser: Right, right.
Akil Palanisamy: So I started early in this topic, and that’s why I’m so passionate about it.
Chris Kresser: Yeah, yeah. That’s really revealing in some ways. If medical students are as burned out as people who've been in the profession for 10 or 20 years, that's an indication that something’s already going wrong, even at that very early stage.
Akil Palanisamy: Right. I came across a really fascinating study. They interviewed almost 3,000 medical students about burnout and 53 percent of them reported feeling burnt out. About 15 percent were depressed, about 5 percent had seriously considered suicide. But the interesting thing was 100 percent of the students, every single one reported feeling humiliated at some point, demeaned, disrespected as part of their training. And that had huge effects on their performance and judgment, and that was my experience too. It’s part of the culture of training doctors.
Chris Kresser: It really is, isn’t it? It’s almost like fraternity hazing or something. I've heard for residents that it's … and it seems to be perpetuated for some of the same reasons, like this, “I went through this, so you have to go through it,” type of mentality. And I've even read the studies that support that.
Akil Palanisamy: Yeah, right. When I started my residency, I was super thrilled because they had just passed a law limiting the work hours, continuous work hours to 24 hours in a row. That was like a huge drop.
Chris Kresser: That’s a big development.
Akil Palanisamy: And I was like, “Wow, this is fantastic. I only have to work 24 hours in a row, like, every week.” And people thought that would solve the problem of burnout. But it hasn’t because that’s just one of many factors.
The results of widespread physician burnout
Chris Kresser: Right, and so we know that there’s a huge problem with the shortage of primary care physicians. I don't remember the exact number from the study I shared in my book, but it's something like, predicted to be a shortage of around 50,000 primary care providers by the year 2025, which is not very far off in the future. And yet one of the costs of burnout, as you said, is that two-thirds of physicians know a doctor who is likely to stop practicing medicine or at least to reduce their access to patients, switch to concierge model, or something like that within the next five years as a result of burnout. So this is a real problem that's really kind of having an outsize effect on our healthcare system.
Akil Palanisamy: Yeah, absolutely. I mean, I think it is genuinely a public health crisis. And I think that that word is increasingly being used in the literature because this really does impact not just individual physicians but patients, healthcare organizations, the entire healthcare system in our country and other countries around the world. So I think the scope of the effects and the impact of burnout is being recognized now and it's huge in terms of not just the individual level, but medical errors as well. So, recent studies have shown that there’s a strong relationship between physician burnout and medical errors. And already medical errors are one of the major leading causes of death in the United States. And so I think as we get more burned out physicians and higher rates of medical errors, I think that's one of the big issues in terms of the costs of this problem.
Chris Kresser: Yeah, this is critical, and I highlighted this in my book. But if you go to a site like CDC or a general website and you search for the top 10 causes of death, let’s see what happens if we do that right now. Cardiovascular disease is still holding at number one, and then you’ve got lung cancer or you’ve got other diseases that come shortly after that. The data is often changing. Cancer continues to go up the list. But you’re not going to see medical errors on these lists, right?
Akil Palanisamy: Right.
Chris Kresser: There was a study published in the British Medical Journal in 2016, just a couple of years ago, and then another one by Barbara Starfield, who’s since passed away, back in 2000 in JAMA. And both of those found the same thing, that medical errors are actually the third-leading cause of death. And since only 5 to 15 percent of the atherogenic events are even reported, Dr. Starfield actually speculated that medical errors could be the number one cause of death if all of the atherogenic events were reported. So this is something you don't see on the typical list, but that doesn't mean it's not true.
Akil Palanisamy: Right, exactly. Yeah, because when you experience burnout, the impaired judgment, lack of attention to detail, communication breakdown, all the things, the depression, that just greatly increases the risk of medical errors.
Chris Kresser: Right. So this is a, it's a common problem, it's a problem that has not only effects on individual practitioners and their health and their lifespan, their feelings about their work, but also to patients and their safety and their ability to get the care that they need, and then to society as a whole. The healthcare crisis continues to deepen, and we need more doctors, rather than fewer. The fact that 50 … that two-thirds of physicians know a doctor who’s likely to stop practicing medicine in five years is exactly the opposite direction that we need to be going in here.
The difference between burnout and moral injury
So let's talk … so, we’ve been throwing this term “burnout” around, and I'm sure that means different things to different people. But you actually emailed me before the show with a really interesting distinction that I want to highlight—the difference between burnout and moral injury. So can you talk about that a little bit?
Akil Palanisamy: Yeah, absolutely. So traditionally, burnout is defined as a work-related syndrome characterized by emotional exhaustion, a cynical feeling, and feeling like you're ineffective on the job. But this concept of burnout really doesn't resonate with doctors. I can tell you from talking to many of them that they really don't connect with this concept of burnout because the problem is you're pointing the finger at doctors. And you’re saying, “You’re burned out, you need to start doing yoga and eat granola, and just like change your lifestyle.” But you know, these are some of the most resilient people out there.
Chris Kresser: Absolutely.
Akil Palanisamy: Medicine, I mean we’ve survived decades of intense training, sleep deprivation, the training process itself is incredibly stressful, the work demands. So these are some of the most resilient and resourceful people out there. And so I think the problem is really, a big part of it is the system. But the distinction that you mentioned between moral injury and burnout, the concept of moral injury actually was first used to describe how soldiers responded to what they did during war and when they came back, having to do things that went against their morals.
In healthcare, it refers to physicians being unable to provide the high-quality care that they would really like to, essentially, not being able to be true to themselves. So I think the problem is not that physicians are burned out and so we don't care. The problem is that we care very deeply.
Chris Kresser: Care too much.
Akil Palanisamy: Yeah.
Chris Kresser: Not too much, but it’s the care that’s causing the problem, yeah.
Akil Palanisamy: Right and then as a result, in our current healthcare system, it's so hard to consistently meet patients’ needs and provide the kind of care that we envisioned we would going into medicine. Because most doctors think of medicine as a calling, and so that failure and inability to meet needs of patients in the way that we really envision, that is hugely damaging, and I think that has a huge effect on physician well-being. And so that's the concept of moral injury. So I think that it's really much broader than just pointing the finger at doctors.
Chris Kresser: I think that’s really, really important to understand, and I've always made it clear that when I'm criticizing conventional medicine and its shortcomings, I'm not criticizing individual doctors. Of course, I might be criticizing some individual doctors, but not as a group because the vast majority of doctors that I have met are people that genuinely want to help their patients. They went into medicine for all the right reasons and they do recognize that they're not having the impact that they would like to have, and it's painful for them. But there's, they feel like their hands are tied because of the way that the system is set up. And they’re just as much victims of the system as the average patient is.
And I think this is a good example of how that plays out where we all want to have meaningful and rewarding work. We all want to get to the end of the day and feel like we really made a difference. And doctors, I think, especially. That's the path they chose. They didn't go into private equity. They didn't choose to go into a career that was really not about helping people, but more about making money or enriching their own lives. Not that there's necessarily anything wrong with that. They willingly chose to go through a very arduous path that involves many, many years of schooling and as you said, rigorous training with residency, working 24 hours straight, often graduating with hundreds of thousands of dollars of debt. I mean, it’s an enormous risk to take, an enormous amount of investment of money and time and energy to become a physician.
So you don't make it through that generally, unless you really have a guiding moral compass that is pushing you through it. And so it's really, I think, even more important and critical that we figure out a way to, where we create a path forward for doctors and other healthcare practitioners that really do want to have that feeling at the end of the day. Because that's the antidote to burnout, where when you really do feel like you're transforming the lives of the people that you're working with, and you're having a huge impact. Because in that situation it doesn't mean you won't get tired and it doesn't mean you won't occasionally feel, “Geez, I need a vacation.” But you're not going to have that moral injury, and that’s what makes all the difference in the world.
Akil Palanisamy: Yeah, I know, exactly. And I think that the rates of suicide among physicians is a real wake-up call because it’s twice that of I think active duty military, and then there was a report from the UK that there was a young junior doctor who, she took her own life by walking into the sea.
Chris Kresser: Yeah, that’s not, yeah.
Akil Palanisamy: Statistically, women physicians are a significantly higher risk of completed suicide than matched females in other professions. So it’s not uncommon, unfortunately, and I think that, yeah, exactly what you said about that moral compass that physicians have, I think being able to feel like you're true to yourself. That's a basic need that all of us have, and I think especially those who go into medicine, we feel that pretty intensely.
How technology is contributing to the problem, not alleviating it
Chris Kresser: Right. And there may be lots of choices every day that they have to make that are, don't feel true to themselves because of the way that the system is set up. And I know from my own research and I know you and I have talked about this, one of the influences in terms of burnout has been the rise of electronic medical records or electronic health records, EMRs and EHRs. Initially these were hailed as, that this is going to dramatically reduce the amount of paperwork that doctors would have to do and they were going to be great time-saving and productivity devices, and they were going to be doctors’ best friends. But the reality has not quite lived up to that, has it?
Akil Palanisamy: No, no. Yeah, I would, I think that studies show that about like half of the average physician’s workday is spent entering data or doing other clerical work in the EHR. So the amount of time actually spent with patients is less than a third, and for me I think it's a bit of a double-edged sword. Because it does make it easier to respond to patient messages rather than playing phone tag with patients. But on a typical day, I might get 50 to 60 electronic messages in addition to charting visit notes for each patient, and each of these questions or patient calls, etc., requires some thought.
And increasingly we’re being measured on how quickly we can respond to these messages because the priority is patient satisfaction, and that's eventually going to be tied to financial compensation and that kind of thing. So I think this EHR, it takes up so much time, and it really hasn’t translated to the reduced workload and that sort of thing. And when we deal with insurance in my practice, I think that's a huge benefit for patients because it improves access, and for Functional Medicine and integrative medicine, I think we need to move in that direction where insurance covers services. And so we offer that, but then it creates a whole universe of responsibilities in terms of the paperwork, the criteria for each progress note when we’re billing insurance, the forms, the prior authorizations, the other kind of paperwork. So it just adds another layer of paperwork to everything else that we’re dealing with in terms of the EHR every day.
Chris Kresser: Yes. And then there’s another issue of when you're actually in the room with the patient, that connection that you're trying to make with the patient is now being mediated by a computer screen and having to type into the computer. And we’ve all seen, I've heard many stories of people going to doctors and complaining that their doctor was hardly even looking at them because they were working on the computer the entire time, and this is especially true with younger doctors from what I've heard, who never operated without an EHR.
So they never had the experience of being in a visit with the patient without the computer being part of that. And I think with all the data that we now have in terms of how important the physician-patient relationship is to the outcomes in care and the research on the placebo effect, and just the, in Carl Rogers's words, the unconditional positive regard and the type of connection that is made just is therapeutic in its own right. And I think the EHR can compromise that in some ways.
Akil Palanisamy: Yeah, absolutely. And I'm always torn because I want to maintain good eye contact and really be present with each patient, but then if I don’t touch the EHR at all, then at the end of the day I’m like, this one’s like …
Chris Kresser: You’ve got eight more hours of work.
Akil Palanisamy: Exactly.
Chris Kresser: It’s really challenging, and, I mean, my solution to that, which is not possible for everybody because of the model I work independently, so I’m able to just kind of set things up how I want. But I have a nurse practitioner that's by my side at every appointment, and she takes the notes. So I'm able to just maintain eye contact with my patient and not really look at the computer. And I recognize that's not a viable solution for most practitioners, but it's something that I felt compelled to do because I, like you, didn't want to get home and do four hours of data entry into the EHR after a full day of seeing patients. And but I didn't also want to sacrifice the connection with the patient.
So I think the other thing that's also not always in an individual physician’s control is the quality of the EHR or the EMR system. So many of them are just completely bloated and full of functions that they'll never use, and just really difficult to navigate, and they’re a nightmare in terms of software development. They’ve been just sort of cobbled together and put on top of each other, and it’s, for anyone who likes software and technology, EMR software is not going to be particularly inspiring for the most part.
Akil Palanisamy: Yes, yeah. No, I think you’re right on that. And the point about having additional support for progress notes, I think, is a good one because studies show that having some type of help with the charting actually reduces burnout, and it's obvious, right? And I think at Sutter Health where I work, they really take burnout quite seriously. And so they’ve supported having scribes, which is the same thing. They take notes and they kind of do everything, and you just have to sign the note.
So I think it’s really, it’s a shared issue with burnout between individuals and healthcare systems and organizations. So I think it’s very important that all of these systems realize they have an important role to play, and I think Sutter Health is a really great example of that. They've supported a lot of these changes, and like this example of scribes and with our EHR, which is Epic, just helping us to use it in the most efficient way possible. So I think systemic changes are really a huge part of the solution as well.
Chris Kresser: Absolutely, and this is a recurring theme in this conversation. It's that individual physicians can only do so much when they're employed in a larger organization, and they’re not free to just do whatever they want. And so we have to continue to work to raise awareness institutionally about these issues so that the institutions themselves can make the changes, and then individual physicians will benefit from those.
Akil Palanisamy: Right.
How to fight physician burnout
Chris Kresser: So let's talk a little bit about some of the work you've done in the past with medical students and other doctors at Sutter on burnout. What kind of things have you done to approach this?
Akil Palanisamy: Yeah, I think for me during medical school, it was really a survival mechanism. Because I was pretty burned out and the training, yes, I absolutely had that being belittled and demeaned when I was on the wards in my rotations. And so I really got interested in the certain classes that were offered on finding meaning in medicine and really connecting with your purpose or actually reconnecting with why you went into medicine, and keeping that front and center. And also developing tools for maintaining well-being like mindfulness.
So mindfulness is one thing that has been studied. There’s actually been about 14 studies looking at physician burnout and mindfulness, and nine of them have shown positive outcome in terms of:
Reducing burnout
Improving well-being
Improving mood
Improving resiliency
So I think, I don't think that's the entire solution, but the more tools you have in your toolkit, the better. And we don't really get any training in general in terms of how to deal with stress and how to manage emotions during our healthcare training. And so I think I got into mindfulness very early, studied MBSR, developed a daily meditation practice, became involved in educational programs teaching people about mindfulness. And then since … then during residency and now practice, after that I've been very interested in workshops and events that kind of focus on that aspect of meaning and really reconnecting with a sense of purpose, a sense of direction. Kind of helping people be true to themselves.
And so I think small group exercises and workshops where people are getting out of their left brain and reconnecting with their right brain, using art and things like that, have been really effective. So for me, I've benefited as much as I’ve helped anybody in this work, and it's been just partly for my own gains, but I think you teach what you have to learn. And for me, being involved in burnout and teaching people about it has been a lifesaver.
Chris Kresser: That’s so great. I think all of those are fantastic tools for kind of exploring the causes of burnout on an individual level and helping people respond in a way that will reduce the risk of moral injury, if we will. And I know for me, one of the ways that I've approached this personally and also with people that I've worked with and that I’ve trained is just to make sure that I feel like the work I'm doing is having a big impact on my patient’s lives. Because that’s one of the reasons I really love that distinction that you make between burnout and moral injury. Because if I look at it that way, I think, “Okay, well, that's the biggest risk is just getting to the end of the day and feeling like I'm not making a difference. Feeling like all of my efforts are for naught really. Or they’re not really having the impact that I would like them to have.” And to me, that's the greatest risk in terms of burning out. When I know that my work is making a difference, my endurance and stamina are considerable.
Akil Palanisamy: Right.
Use Functional Medicine to prevent it
Chris Kresser: But when I don't feel that way, it doesn't take much to make me feel tired and like what I'm doing is not worth it. So this is, I think, where a Functional Medicine approach has a lot to offer, not just as a treatment modality, but as a means of really actually making a difference in the patients’ lives. Like getting to the root cause of the problem and actually addressing the problem and helping the patient to recover and feel better without the use of unnecessary drugs and surgery. For me that was one of the most appealing things about Functional Medicine, and I think it's one of the less talked about but most important gifts that it has to offer to individual physicians who shift their practice in that direction.
Akil Palanisamy: Yeah, I think that's what motivated me to go into Functional Medicine as well, just to get that sense of fulfillment and satisfaction when you help someone really get a permanent solution to something and by uncovering the root causes and taking that holistic approach. So I think that's what drew me to Functional Medicine as well.
Schedule a retreat
Chris Kresser: Absolutely. So another area where I know, or a kind of antidote to burnout that I know that you and I are both passionate about is a retreat. So I've been a big believer in retreat. I’ve done annual retreats myself for many years. I’ve done meditation retreats for about 25 years and I just can't really imagine my life without that opportunity to step away from my day-to-day life and experience and to get a different perspective, to slow down, to have more spacious existence for a few days were the busyness of life is not overtaking me and where I can just hear myself think and feel my body, and just look at things from a fresh perspective. It's just crucial for me. And I've always felt like my wish has been that others can experience this. That we can, because I really believe in its transformative power.
Connect with colleagues
Akil Palanisamy: Yeah, absolutely. I do as well, and I’ve had a number of retreats over the years in terms of individual retreats and also group retreats. And especially in the professional setting, I find that ability to connect with other colleagues and professionals in that informal, nonwork setting is so powerful because in healthcare there's so much isolation. There are so many individual silos.
Everybody's just doing their thing trying to get through the day, and you rarely have a chance to step back and step out of that situation to just really deeply connect with people who are in the same boat and really understand what they're going through, share their story, listen to their stories, and really deepen your connection and solve problems together.
So I think that sort of deep connection is so important because that's like a huge need for all human beings, and especially in such an isolating profession like in healthcare. I think it's essential.
Chris Kresser: Absolutely, yeah. So many clinicians can just spend, we spend most of our time in a room with patients and we’re interacting with patients, but we’re not, we’re interacting with them in a certain way. We’re playing a certain role. We’re the clinician, they’re the patient, and those can be rich and rewarding interactions. But it's not the same as connecting with other colleagues and being able to talk about the issues that we face professionally and share together. So yeah I think that group experience is really powerful. And I’ve been writing about this recently.
I’ve been sharing some book recommendations, and Akil and I have actually teamed up to offer a retreat for healthcare practitioners at 1440 Multiversity in October. It’s from October 5th to 7th this year. And so it starts on Friday afternoon, Friday evening, and it goes through Sunday midday. And the retreat’s called “From Burnout to Brilliance: Rediscover Your Passion and Purpose, Reclaim Your Health, and Create a Practice You Love.” So the intention of this retreat is to address the issues that we've been talking about in the show and to help healthcare professionals explore their own situation, help them rediscover their passion for medicine and healthcare, and reconnect with a sense of meaning and purpose in their work to take some practical steps. Break those down into really doable actionable steps that they can take to reclaim their health and well-being. Rediscover parts of themselves that are not typically expressed in the course of their day-to-day work and just kind of cultivate a sense of energy and vitality that they may have been missing for many years.
And I'm really excited about doing this. I’m excited about doing this with Akil, who I've known for several years now and I really respect, and I'm excited about doing it at 1440. It's an incredible new retreat center, which I think you did a retreat there with Michelle Tam with Nom Nom Paleo last year, Akil?
Akil Palanisamy: Yes, yes beautiful, beautiful place. Yeah.
Chris Kresser: So this is, and for those of you who are not familiar, it's in Santa Cruz Mountains, right?
Akil Palanisamy: Yeah, it’s surrounded by redwood trees and there's all these amazing hiking trails. And yeah, a beautiful place.
Chris Kresser: Yeah. I haven't actually been there yet, but I know several people who’ve taught there and who’ve been there. And if you go to 1440.org, click on the stay button and check out some of the pictures. It's an absolutely beautiful campus. Really nice accommodations, gorgeous dining hall with lots of different food options. They've got daily yoga classes and massage, and a spa and other health offerings there. And they’ve got, of course, gorgeous hiking trails because it's in the redwood forest there. It just looks to me like they're really doing it right. I've been to a lot of retreat centers. I actually lived at a retreat center in Big Sur called the Esalen Institute …
Akil Palanisamy: Oh. sure.
Chris Kresser: … and many people may be familiar with. When I was still really sick and dealing with my health issues, I got to a point where I just decided, I kind of reached the end of the line of supplements and diets, and medications, and I decided that I would explore the psychological, emotional, psycho-spiritual aspects of what was going on for me. So I moved to Esalen and lived there for a couple of years. So I'm very familiar with retreat centers. I've been to many others around the country, both for Buddhist meditation retreats and other retreats, and I have, they're all great in many ways. But they’re, I can see that 1440 is bringing it to a different level.
So I'm excited to be a part of that. I'm excited to get together with a group of professionals that are all wanting to cultivate more meaning in their work and to find that work/life balance that can be so elusive. And I just can't wait to get together and support each other and share because that's, I mean, we all have so much to offer, and I think when we come together with a similar purpose, it's really powerful.
Akil Palanisamy: Yeah. I am also really excited about the upcoming event, and I think for anyone who feels like they're not being true to themselves in their work or as to themselves as they would want to be, I think this is a great opportunity to really reflect. And I think our vision for that weekend is that it's going to be a very introspective weekend and really focused in small groups and interactive elements. So it’s not going to be just mostly didactic.
Chris Kresser: Yeah. It’s not going to be Akil and I standing in front of the room talking at you the whole time. Definitely going to be the opposite of that.
Akil Palanisamy: Right, exactly, yeah. Because I think that this work is really about looking within and then sharing and connecting with other people. And so that's the focus of the weekend, is really building that sense of community with whoever comes and really learning to deepen your own sense of meaning and purpose in work, and look within to reconnect with that vision for what drew you to this work initially. Because I think that's the ultimate goal is having that feeling like you're really being true to yourself at the end of the day and having the kind of practice that you envision.
Don’t be afraid to make changes
Chris Kresser: Absolutely. I shared the story of Sheri in my book Unconventional Medicine, who is a clinician that was working in the VA. And she's a doctor and was mostly seeing patients with diabetes. That's the most common health challenge for veterans. And it was, she was counting the days until retirement. It was just really a factory-medicine type of situation. She often didn’t even have time to go to the bathroom during the day because she was just that busy from appointment to appointment. And as we've discussed, there was a real risk of moral injury because she didn't feel like she was making a difference. She was just handing out medications to these people and she wasn't, she knew as an athlete herself who tried to pay attention to her diet, she knew that wasn’t the best way to go about it. But what else could she do in the amount of time that she had?
And she moved into kind of a more, started incorporating more of a functional approach in her work, and then eventually left and started her own Functional Medicine practice. But for her, it was just a total game changer. She went from counting the days to retirement, to not ever being able to imagine retiring. And that's the kind of shift that’s possible, I think, when you really address the root causes of burnout and take the opportunity to step out of your current system, your current day-to-day, and really give yourself the chance to discover something new. And even if that’s maybe moving in a different direction entirely, or maybe staying in your current situation but just making a series of small changes that collectively can have a big impact.
Akil Palanisamy: Yeah, I think for me, my whole approach has been in terms of incremental change because I know that for many people, they have gone out of the insurance model and set up their own Functional Medicine practice, and that can be fantastic. But my work is really just building change within the system. Because if the people within the system leave and do their own thing, then the system itself is going to not be changed. And so I think that a big part of this is also figuring out solutions within systems and incremental steps we can take, and I think that'll hopefully be part of what we talk about as well. Just if you do belong to a system, how you can take a leadership role and effect change within that system as well.
Chris Kresser: Absolutely. That's why Akil and I are a good team, because I’m outside the system and he’s inside of the system, and we have different perspectives. So that's another reason I'm happy to team up with him. I mentioned this in the beginning, but I'll throw it out there again. You need not be an MD to participate in this workshop. It's really for all healthcare practitioners and providers who are experiencing burnout. And so this could be anyone from a health coach to a nutritionist to a dietitian to an occupational therapist to a chiropractor, a naturopath in addition to MDs, and DOs, and MPs, and PAs, and all of the other abbreviations and acronyms. Anyone working in healthcare really would be welcome. And we’re not even limiting it to people working in healthcare. We don't want to exclude people here, so if you're not working in healthcare and the things we've been talking about resonate with you, maybe you work in emergency services or something else, you are absolutely welcome to come.
Akil Palanisamy: Yeah, and I would add that even if you're not feeling burned out, I think that prevention is really the best medicine.
Chris Kresser: That’s true.
Akil Palanisamy: So I think learning about the research and the science, because we know how to prevent it, and it's much better to prevent burnout than treat it once it happens.
Chris Kresser: That is a very good point. Yeah, and I guess if the statistics are any indication, we know that even if you’re not feeling burnout now, chances are statistically you will at some point.
Akil Palanisamy: Right.
Chris Kresser: Especially without any intervention. It’s kind of like the diabetes example I used before. If you’ve got high normal blood sugar, now’s the time to get it under control rather than waiting until it turns into diabetes.
Akil Palanisamy: Right.
Chris Kresser: Great, well, thank you so much, Akil, for being with us. It’s a fascinating and important topic, and I’m really looking forward to leading this workshop with you. Again, in the retreat, you can go to 1440, it’s 1-4-4-0 dot o-r-g, and when you get there on the website, you just hover over Learn, and then under programs click on Professional Development. And if you scroll down there, you’ll see our program, which, again, is on the first weekend of October, October 5th to 7th, it’s a Friday through a Sunday.
And there’s a tuition for the program, and then there’s several different accommodation options available there. It’s really neat. I like what they've done with that. Everything from a private room to a suite to a really cool bunk style, kind of modern bunk-style accommodation that's much more affordable. I don’t know if you saw those last time.
Akil Palanisamy: I did, yeah.
Chris Kresser: Check the pictures out, they look pretty cool. They call them pods.
Akil Palanisamy: Right, yeah, yeah. They’re pretty comfy. I’ve seen them.
Chris Kresser: Yeah, yeah, it looks great. So lots of different accommodation options. If you’ve never been to this part of the world, the Santa Cruz Mountains are a beautiful, beautiful area, gorgeous redwood forests. You can head down to the beach before or after in Santa Cruz there. It’s a funky, cool little town. Great, great part of the world. So I hope you can make it. Those of you who have been listening to this and resonating with it, we’d love to meet you in person and have a chance to explore these topics with you.
And then Akil, is also, we haven’t talked much about his other work, but he’s also an author in addition to being a clinician. And he organizes the Paleo Symposium every year that I've been fortunate enough to be a speaker at. So why don’t you tell everyone a little bit more about your work and where they can find out more about your work.
Akil Palanisamy: Oh sure, yeah. So I practice integrative medicine and I combine Functional Medicine with the Paleo approach and Ayurveda, which is the traditional medicine of India. And still that has led to my book which is called The Paleovedic Diet, combining Paleo and Ayurvedic medicine. And the best way to connect with me would be through my website, which is DoctorAkil.com. Just doctor spelled out, A-k-i-l dot com. And yeah, I wanted to thank you, as well, Chris, for having me on the podcast. I’m very excited to be working on this event with you, and it was really a pleasure to talk today.
Chris Kresser: Pleasure is mine, Akil. And I'm sure we’ll be in touch before October, but I look forward to seeing you then and anyone else who's listening, who wants to join us. So 1440.org, and thanks for listening, everybody. Keep sending your questions in. I know I haven’t answered many of them recently. We’ve been doing a lot more interviews lately. But I do see that I have a few Q&A episodes coming up, and we do read all of your questions, and we also consider them for writing articles or emails.
So even if we’re not able to answer them on the show, it helps me to understand what you're thinking about and what you want me to write about and talk about. So please do keep sending them in. That’s ChrisKresser.com/podcastquestion. And thanks, everyone, for listening. And thank you, Akil, and we’ll see you next time.
Akil Palanisamy: Thank you, Chris.
The post RHR: How to Fight Practitioner Burnout with Dr. Akil Palanisamy appeared first on Chris Kresser.
0 notes
Text
RHR: How to Fight Practitioner Burnout with Dr. Akil Palanisamy
In this episode, we discuss:
Burnout among healthcare practitioners
How common the problem is
The results of widespread physician burnout
The difference between burnout and moral injury
How technology is contributing to the problem, not alleviating it
How to fight physician burnout
Show notes:
The Paleovedic Diet by Dr. Akil Palanisamy
The Sutter Health Institute for Health & Healing in San Francisco
Unconventional Medicine by Chris Kresser
1440 Multiversity retreat for healthcare professionals
Akil Palanisamy’s website, DoctorAkil.com
youtube
[smart_track_player url="http://traffic.libsyn.com/thehealthyskeptic/RHR_-_How_to_Fight_Practitioner_Burnout_with_Dr._Akil_Palanisamy.mp3" title="RHR - How to Fight Practitioner Burnout with Dr. Akil Palanisamy " artist="Chris Kresser" ]
Chris Kresser: Hey, everybody, Chris Kresser here. Welcome to another episode of Revolution Health Radio. This week we’re going to be talking to Dr. Akil Palanisamy, who is a friend and colleague in the Functional Medicine space. And I’ve known him for several years. He is the author of The Paleovedic Diet, a really interesting book combining Paleo and Ayurveda, a traditional Indian medicine which is an interest of his. And he also runs the Paleo Symposium that’s put on by the Institute for Health & Healing at UCSF every year, that I’ve been a featured speaker at since it started.
But today actually, we’re going to be talking about something different, which is burnout amongst healthcare practitioners. It’s a really important topic that has pretty significant implications not only in terms of the effect on individual clinicians, but on patients and their access to care, things like medical errors and just the healthcare system overall.
So if you’re not familiar with Akil, he’s an integrative medicine physician who blends his medical training with Functional Medicine in Ayurveda, the traditional medicine of India. He studied biochemistry at Harvard and received his medical degree from UCSF and completed his residency at Stanford. Dr. Akil also completed a fellowship in integrative medicine with Dr. Andrew Weil at the University of Arizona. He sees patients at the Sutter Health Institute for Health & Healing in San Francisco, where he also serves as physician director for community education. He’s been a consultant with the medical board of California for many years and as I mentioned, he’s the author of The Paleovedic Diet: A Complete Program to Burn Fat, Increase Energy, and Reverse Disease.
So I’m really excited to dive into this conversation with Akil. I think you’ll find it interesting, even if you’re not a healthcare practitioner that’s experiencing burnout, because we talk about a lot of issues that are relevant to anybody doing any kind of work, really. So I hope you enjoy the conversation. Let’s dive in. Akil, thank you so much for joining us. I’m so glad to have you here.
Akil Palanisamy: Thank you, Chris. Pleasure to be here.
Burnout among healthcare practitioners
Chris Kresser: So today we’re going to talk about a really important topic that I don't think gets enough attention, and this is physician burnout. So, and I would extend it to burnout for any healthcare practitioners. We might be focusing a little bit on physicians because this is where most of the statistics are available, but it’s certainly a problem across the entire healthcare world whether we’re talking about:
Nurses
Nurse practitioners
Occupational therapists
Chiropractors
Acupuncturists
Anybody working in the care profession
In my book Unconventional Medicine, I talked a lot about how this is one of the major challenges within medicine in general, not just conventional medicine, but also integrative medicine and Functional Medicine. And it's something that we need to develop a sensible approach to if we’re going to meet our goals in terms of preventing and reversing disease. So this is something that Akil has thought deeply about and has been involved in a number of different initiatives from his work at Sutter to working with medical students and other physicians to address this problem. So I'm really looking forward to having this conversation. So why don’t we start a little bit with the stats on burnout, Akil?
Ask yourself: Does medicine still feel like your calling? If daily stress and exhaustion are turning you away from the profession, you might be headed toward physician burnout. Find out what causes burnout and learn how to rediscover your sense of purpose.
How common the problem is
Akil Palanisamy: Sure, yeah, I think it's really rampant, and most studies report around 50 percent or higher of physicians report some significant burnout. And that's up from about 40 percent just five years ago. So, I think the numbers are really scary and also this is a global problem. So this is across the board. Many countries throughout the world and also regardless of the stage of training. So medical students, residents, physicians, even the number of years of practice has no impact.
Chris Kresser: Wow.
Akil Palanisamy: I will check on this number, so, I mean, I know because I did my medical training 20 years ago, and it was like, I would say, a soul-crushing and exhausting process.
Chris Kresser: Right, right.
Akil Palanisamy: So I started early in this topic, and that’s why I’m so passionate about it.
Chris Kresser: Yeah, yeah. That’s really revealing in some ways. If medical students are as burned out as people who've been in the profession for 10 or 20 years, that's an indication that something’s already going wrong, even at that very early stage.
Akil Palanisamy: Right. I came across a really fascinating study. They interviewed almost 3,000 medical students about burnout and 53 percent of them reported feeling burnt out. About 15 percent were depressed, about 5 percent had seriously considered suicide. But the interesting thing was 100 percent of the students, every single one reported feeling humiliated at some point, demeaned, disrespected as part of their training. And that had huge effects on their performance and judgment, and that was my experience too. It’s part of the culture of training doctors.
Chris Kresser: It really is, isn’t it? It’s almost like fraternity hazing or something. I've heard for residents that it's … and it seems to be perpetuated for some of the same reasons, like this, “I went through this, so you have to go through it,” type of mentality. And I've even read the studies that support that.
Akil Palanisamy: Yeah, right. When I started my residency, I was super thrilled because they had just passed a law limiting the work hours, continuous work hours to 24 hours in a row. That was like a huge drop.
Chris Kresser: That’s a big development.
Akil Palanisamy: And I was like, “Wow, this is fantastic. I only have to work 24 hours in a row, like, every week.” And people thought that would solve the problem of burnout. But it hasn’t because that’s just one of many factors.
The results of widespread physician burnout
Chris Kresser: Right, and so we know that there’s a huge problem with the shortage of primary care physicians. I don't remember the exact number from the study I shared in my book, but it's something like, predicted to be a shortage of around 50,000 primary care providers by the year 2025, which is not very far off in the future. And yet one of the costs of burnout, as you said, is that two-thirds of physicians know a doctor who is likely to stop practicing medicine or at least to reduce their access to patients, switch to concierge model, or something like that within the next five years as a result of burnout. So this is a real problem that's really kind of having an outsize effect on our healthcare system.
Akil Palanisamy: Yeah, absolutely. I mean, I think it is genuinely a public health crisis. And I think that that word is increasingly being used in the literature because this really does impact not just individual physicians but patients, healthcare organizations, the entire healthcare system in our country and other countries around the world. So I think the scope of the effects and the impact of burnout is being recognized now and it's huge in terms of not just the individual level, but medical errors as well. So, recent studies have shown that there’s a strong relationship between physician burnout and medical errors. And already medical errors are one of the major leading causes of death in the United States. And so I think as we get more burned out physicians and higher rates of medical errors, I think that's one of the big issues in terms of the costs of this problem.
Chris Kresser: Yeah, this is critical, and I highlighted this in my book. But if you go to a site like CDC or a general website and you search for the top 10 causes of death, let’s see what happens if we do that right now. Cardiovascular disease is still holding at number one, and then you’ve got lung cancer or you’ve got other diseases that come shortly after that. The data is often changing. Cancer continues to go up the list. But you’re not going to see medical errors on these lists, right?
Akil Palanisamy: Right.
Chris Kresser: There was a study published in the British Medical Journal in 2016, just a couple of years ago, and then another one by Barbara Starfield, who’s since passed away, back in 2000 in JAMA. And both of those found the same thing, that medical errors are actually the third-leading cause of death. And since only 5 to 15 percent of the atherogenic events are even reported, Dr. Starfield actually speculated that medical errors could be the number one cause of death if all of the atherogenic events were reported. So this is something you don't see on the typical list, but that doesn't mean it's not true.
Akil Palanisamy: Right, exactly. Yeah, because when you experience burnout, the impaired judgment, lack of attention to detail, communication breakdown, all the things, the depression, that just greatly increases the risk of medical errors.
Chris Kresser: Right. So this is a, it's a common problem, it's a problem that has not only effects on individual practitioners and their health and their lifespan, their feelings about their work, but also to patients and their safety and their ability to get the care that they need, and then to society as a whole. The healthcare crisis continues to deepen, and we need more doctors, rather than fewer. The fact that 50 … that two-thirds of physicians know a doctor who’s likely to stop practicing medicine in five years is exactly the opposite direction that we need to be going in here.
The difference between burnout and moral injury
So let's talk … so, we’ve been throwing this term “burnout” around, and I'm sure that means different things to different people. But you actually emailed me before the show with a really interesting distinction that I want to highlight—the difference between burnout and moral injury. So can you talk about that a little bit?
Akil Palanisamy: Yeah, absolutely. So traditionally, burnout is defined as a work-related syndrome characterized by emotional exhaustion, a cynical feeling, and feeling like you're ineffective on the job. But this concept of burnout really doesn't resonate with doctors. I can tell you from talking to many of them that they really don't connect with this concept of burnout because the problem is you're pointing the finger at doctors. And you’re saying, “You’re burned out, you need to start doing yoga and eat granola, and just like change your lifestyle.” But you know, these are some of the most resilient people out there.
Chris Kresser: Absolutely.
Akil Palanisamy: Medicine, I mean we’ve survived decades of intense training, sleep deprivation, the training process itself is incredibly stressful, the work demands. So these are some of the most resilient and resourceful people out there. And so I think the problem is really, a big part of it is the system. But the distinction that you mentioned between moral injury and burnout, the concept of moral injury actually was first used to describe how soldiers responded to what they did during war and when they came back, having to do things that went against their morals.
In healthcare, it refers to physicians being unable to provide the high-quality care that they would really like to, essentially, not being able to be true to themselves. So I think the problem is not that physicians are burned out and so we don't care. The problem is that we care very deeply.
Chris Kresser: Care too much.
Akil Palanisamy: Yeah.
Chris Kresser: Not too much, but it’s the care that’s causing the problem, yeah.
Akil Palanisamy: Right and then as a result, in our current healthcare system, it's so hard to consistently meet patients’ needs and provide the kind of care that we envisioned we would going into medicine. Because most doctors think of medicine as a calling, and so that failure and inability to meet needs of patients in the way that we really envision, that is hugely damaging, and I think that has a huge effect on physician well-being. And so that's the concept of moral injury. So I think that it's really much broader than just pointing the finger at doctors.
Chris Kresser: I think that’s really, really important to understand, and I've always made it clear that when I'm criticizing conventional medicine and its shortcomings, I'm not criticizing individual doctors. Of course, I might be criticizing some individual doctors, but not as a group because the vast majority of doctors that I have met are people that genuinely want to help their patients. They went into medicine for all the right reasons and they do recognize that they're not having the impact that they would like to have, and it's painful for them. But there's, they feel like their hands are tied because of the way that the system is set up. And they’re just as much victims of the system as the average patient is.
And I think this is a good example of how that plays out where we all want to have meaningful and rewarding work. We all want to get to the end of the day and feel like we really made a difference. And doctors, I think, especially. That's the path they chose. They didn't go into private equity. They didn't choose to go into a career that was really not about helping people, but more about making money or enriching their own lives. Not that there's necessarily anything wrong with that. They willingly chose to go through a very arduous path that involves many, many years of schooling and as you said, rigorous training with residency, working 24 hours straight, often graduating with hundreds of thousands of dollars of debt. I mean, it’s an enormous risk to take, an enormous amount of investment of money and time and energy to become a physician.
So you don't make it through that generally, unless you really have a guiding moral compass that is pushing you through it. And so it's really, I think, even more important and critical that we figure out a way to, where we create a path forward for doctors and other healthcare practitioners that really do want to have that feeling at the end of the day. Because that's the antidote to burnout, where when you really do feel like you're transforming the lives of the people that you're working with, and you're having a huge impact. Because in that situation it doesn't mean you won't get tired and it doesn't mean you won't occasionally feel, “Geez, I need a vacation.” But you're not going to have that moral injury, and that’s what makes all the difference in the world.
Akil Palanisamy: Yeah, I know, exactly. And I think that the rates of suicide among physicians is a real wake-up call because it’s twice that of I think active duty military, and then there was a report from the UK that there was a young junior doctor who, she took her own life by walking into the sea.
Chris Kresser: Yeah, that’s not, yeah.
Akil Palanisamy: Statistically, women physicians are a significantly higher risk of completed suicide than matched females in other professions. So it’s not uncommon, unfortunately, and I think that, yeah, exactly what you said about that moral compass that physicians have, I think being able to feel like you're true to yourself. That's a basic need that all of us have, and I think especially those who go into medicine, we feel that pretty intensely.
How technology is contributing to the problem, not alleviating it
Chris Kresser: Right. And there may be lots of choices every day that they have to make that are, don't feel true to themselves because of the way that the system is set up. And I know from my own research and I know you and I have talked about this, one of the influences in terms of burnout has been the rise of electronic medical records or electronic health records, EMRs and EHRs. Initially these were hailed as, that this is going to dramatically reduce the amount of paperwork that doctors would have to do and they were going to be great time-saving and productivity devices, and they were going to be doctors’ best friends. But the reality has not quite lived up to that, has it?
Akil Palanisamy: No, no. Yeah, I would, I think that studies show that about like half of the average physician’s workday is spent entering data or doing other clerical work in the EHR. So the amount of time actually spent with patients is less than a third, and for me I think it's a bit of a double-edged sword. Because it does make it easier to respond to patient messages rather than playing phone tag with patients. But on a typical day, I might get 50 to 60 electronic messages in addition to charting visit notes for each patient, and each of these questions or patient calls, etc., requires some thought.
And increasingly we’re being measured on how quickly we can respond to these messages because the priority is patient satisfaction, and that's eventually going to be tied to financial compensation and that kind of thing. So I think this EHR, it takes up so much time, and it really hasn’t translated to the reduced workload and that sort of thing. And when we deal with insurance in my practice, I think that's a huge benefit for patients because it improves access, and for Functional Medicine and integrative medicine, I think we need to move in that direction where insurance covers services. And so we offer that, but then it creates a whole universe of responsibilities in terms of the paperwork, the criteria for each progress note when we’re billing insurance, the forms, the prior authorizations, the other kind of paperwork. So it just adds another layer of paperwork to everything else that we’re dealing with in terms of the EHR every day.
Chris Kresser: Yes. And then there’s another issue of when you're actually in the room with the patient, that connection that you're trying to make with the patient is now being mediated by a computer screen and having to type into the computer. And we’ve all seen, I've heard many stories of people going to doctors and complaining that their doctor was hardly even looking at them because they were working on the computer the entire time, and this is especially true with younger doctors from what I've heard, who never operated without an EHR.
So they never had the experience of being in a visit with the patient without the computer being part of that. And I think with all the data that we now have in terms of how important the physician-patient relationship is to the outcomes in care and the research on the placebo effect, and just the, in Carl Rogers's words, the unconditional positive regard and the type of connection that is made just is therapeutic in its own right. And I think the EHR can compromise that in some ways.
Akil Palanisamy: Yeah, absolutely. And I'm always torn because I want to maintain good eye contact and really be present with each patient, but then if I don’t touch the EHR at all, then at the end of the day I’m like, this one’s like …
Chris Kresser: You’ve got eight more hours of work.
Akil Palanisamy: Exactly.
Chris Kresser: It’s really challenging, and, I mean, my solution to that, which is not possible for everybody because of the model I work independently, so I’m able to just kind of set things up how I want. But I have a nurse practitioner that's by my side at every appointment, and she takes the notes. So I'm able to just maintain eye contact with my patient and not really look at the computer. And I recognize that's not a viable solution for most practitioners, but it's something that I felt compelled to do because I, like you, didn't want to get home and do four hours of data entry into the EHR after a full day of seeing patients. And but I didn't also want to sacrifice the connection with the patient.
So I think the other thing that's also not always in an individual physician’s control is the quality of the EHR or the EMR system. So many of them are just completely bloated and full of functions that they'll never use, and just really difficult to navigate, and they’re a nightmare in terms of software development. They’ve been just sort of cobbled together and put on top of each other, and it’s, for anyone who likes software and technology, EMR software is not going to be particularly inspiring for the most part.
Akil Palanisamy: Yes, yeah. No, I think you’re right on that. And the point about having additional support for progress notes, I think, is a good one because studies show that having some type of help with the charting actually reduces burnout, and it's obvious, right? And I think at Sutter Health where I work, they really take burnout quite seriously. And so they’ve supported having scribes, which is the same thing. They take notes and they kind of do everything, and you just have to sign the note.
So I think it’s really, it’s a shared issue with burnout between individuals and healthcare systems and organizations. So I think it’s very important that all of these systems realize they have an important role to play, and I think Sutter Health is a really great example of that. They've supported a lot of these changes, and like this example of scribes and with our EHR, which is Epic, just helping us to use it in the most efficient way possible. So I think systemic changes are really a huge part of the solution as well.
Chris Kresser: Absolutely, and this is a recurring theme in this conversation. It's that individual physicians can only do so much when they're employed in a larger organization, and they’re not free to just do whatever they want. And so we have to continue to work to raise awareness institutionally about these issues so that the institutions themselves can make the changes, and then individual physicians will benefit from those.
Akil Palanisamy: Right.
How to fight physician burnout
Chris Kresser: So let's talk a little bit about some of the work you've done in the past with medical students and other doctors at Sutter on burnout. What kind of things have you done to approach this?
Akil Palanisamy: Yeah, I think for me during medical school, it was really a survival mechanism. Because I was pretty burned out and the training, yes, I absolutely had that being belittled and demeaned when I was on the wards in my rotations. And so I really got interested in the certain classes that were offered on finding meaning in medicine and really connecting with your purpose or actually reconnecting with why you went into medicine, and keeping that front and center. And also developing tools for maintaining well-being like mindfulness.
So mindfulness is one thing that has been studied. There’s actually been about 14 studies looking at physician burnout and mindfulness, and nine of them have shown positive outcome in terms of:
Reducing burnout
Improving well-being
Improving mood
Improving resiliency
So I think, I don't think that's the entire solution, but the more tools you have in your toolkit, the better. And we don't really get any training in general in terms of how to deal with stress and how to manage emotions during our healthcare training. And so I think I got into mindfulness very early, studied MBSR, developed a daily meditation practice, became involved in educational programs teaching people about mindfulness. And then since … then during residency and now practice, after that I've been very interested in workshops and events that kind of focus on that aspect of meaning and really reconnecting with a sense of purpose, a sense of direction. Kind of helping people be true to themselves.
And so I think small group exercises and workshops where people are getting out of their left brain and reconnecting with their right brain, using art and things like that, have been really effective. So for me, I've benefited as much as I’ve helped anybody in this work, and it's been just partly for my own gains, but I think you teach what you have to learn. And for me, being involved in burnout and teaching people about it has been a lifesaver.
Chris Kresser: That’s so great. I think all of those are fantastic tools for kind of exploring the causes of burnout on an individual level and helping people respond in a way that will reduce the risk of moral injury, if we will. And I know for me, one of the ways that I've approached this personally and also with people that I've worked with and that I’ve trained is just to make sure that I feel like the work I'm doing is having a big impact on my patient’s lives. Because that’s one of the reasons I really love that distinction that you make between burnout and moral injury. Because if I look at it that way, I think, “Okay, well, that's the biggest risk is just getting to the end of the day and feeling like I'm not making a difference. Feeling like all of my efforts are for naught really. Or they’re not really having the impact that I would like them to have.” And to me, that's the greatest risk in terms of burning out. When I know that my work is making a difference, my endurance and stamina are considerable.
Akil Palanisamy: Right.
Use Functional Medicine to prevent it
Chris Kresser: But when I don't feel that way, it doesn't take much to make me feel tired and like what I'm doing is not worth it. So this is, I think, where a Functional Medicine approach has a lot to offer, not just as a treatment modality, but as a means of really actually making a difference in the patients’ lives. Like getting to the root cause of the problem and actually addressing the problem and helping the patient to recover and feel better without the use of unnecessary drugs and surgery. For me that was one of the most appealing things about Functional Medicine, and I think it's one of the less talked about but most important gifts that it has to offer to individual physicians who shift their practice in that direction.
Akil Palanisamy: Yeah, I think that's what motivated me to go into Functional Medicine as well, just to get that sense of fulfillment and satisfaction when you help someone really get a permanent solution to something and by uncovering the root causes and taking that holistic approach. So I think that's what drew me to Functional Medicine as well.
Schedule a retreat
Chris Kresser: Absolutely. So another area where I know, or a kind of antidote to burnout that I know that you and I are both passionate about is a retreat. So I've been a big believer in retreat. I’ve done annual retreats myself for many years. I’ve done meditation retreats for about 25 years and I just can't really imagine my life without that opportunity to step away from my day-to-day life and experience and to get a different perspective, to slow down, to have more spacious existence for a few days were the busyness of life is not overtaking me and where I can just hear myself think and feel my body, and just look at things from a fresh perspective. It's just crucial for me. And I've always felt like my wish has been that others can experience this. That we can, because I really believe in its transformative power.
Connect with colleagues
Akil Palanisamy: Yeah, absolutely. I do as well, and I’ve had a number of retreats over the years in terms of individual retreats and also group retreats. And especially in the professional setting, I find that ability to connect with other colleagues and professionals in that informal, nonwork setting is so powerful because in healthcare there's so much isolation. There are so many individual silos.
Everybody's just doing their thing trying to get through the day, and you rarely have a chance to step back and step out of that situation to just really deeply connect with people who are in the same boat and really understand what they're going through, share their story, listen to their stories, and really deepen your connection and solve problems together.
So I think that sort of deep connection is so important because that's like a huge need for all human beings, and especially in such an isolating profession like in healthcare. I think it's essential.
Chris Kresser: Absolutely, yeah. So many clinicians can just spend, we spend most of our time in a room with patients and we’re interacting with patients, but we’re not, we’re interacting with them in a certain way. We’re playing a certain role. We’re the clinician, they’re the patient, and those can be rich and rewarding interactions. But it's not the same as connecting with other colleagues and being able to talk about the issues that we face professionally and share together. So yeah I think that group experience is really powerful. And I’ve been writing about this recently.
I’ve been sharing some book recommendations, and Akil and I have actually teamed up to offer a retreat for healthcare practitioners at 1440 Multiversity in October. It’s from October 5th to 7th this year. And so it starts on Friday afternoon, Friday evening, and it goes through Sunday midday. And the retreat’s called “From Burnout to Brilliance: Rediscover Your Passion and Purpose, Reclaim Your Health, and Create a Practice You Love.” So the intention of this retreat is to address the issues that we've been talking about in the show and to help healthcare professionals explore their own situation, help them rediscover their passion for medicine and healthcare, and reconnect with a sense of meaning and purpose in their work to take some practical steps. Break those down into really doable actionable steps that they can take to reclaim their health and well-being. Rediscover parts of themselves that are not typically expressed in the course of their day-to-day work and just kind of cultivate a sense of energy and vitality that they may have been missing for many years.
And I'm really excited about doing this. I’m excited about doing this with Akil, who I've known for several years now and I really respect, and I'm excited about doing it at 1440. It's an incredible new retreat center, which I think you did a retreat there with Michelle Tam with Nom Nom Paleo last year, Akil?
Akil Palanisamy: Yes, yes beautiful, beautiful place. Yeah.
Chris Kresser: So this is, and for those of you who are not familiar, it's in Santa Cruz Mountains, right?
Akil Palanisamy: Yeah, it’s surrounded by redwood trees and there's all these amazing hiking trails. And yeah, a beautiful place.
Chris Kresser: Yeah. I haven't actually been there yet, but I know several people who’ve taught there and who’ve been there. And if you go to 1440.org, click on the stay button and check out some of the pictures. It's an absolutely beautiful campus. Really nice accommodations, gorgeous dining hall with lots of different food options. They've got daily yoga classes and massage, and a spa and other health offerings there. And they’ve got, of course, gorgeous hiking trails because it's in the redwood forest there. It just looks to me like they're really doing it right. I've been to a lot of retreat centers. I actually lived at a retreat center in Big Sur called the Esalen Institute …
Akil Palanisamy: Oh. sure.
Chris Kresser: … and many people may be familiar with. When I was still really sick and dealing with my health issues, I got to a point where I just decided, I kind of reached the end of the line of supplements and diets, and medications, and I decided that I would explore the psychological, emotional, psycho-spiritual aspects of what was going on for me. So I moved to Esalen and lived there for a couple of years. So I'm very familiar with retreat centers. I've been to many others around the country, both for Buddhist meditation retreats and other retreats, and I have, they're all great in many ways. But they’re, I can see that 1440 is bringing it to a different level.
So I'm excited to be a part of that. I'm excited to get together with a group of professionals that are all wanting to cultivate more meaning in their work and to find that work/life balance that can be so elusive. And I just can't wait to get together and support each other and share because that's, I mean, we all have so much to offer, and I think when we come together with a similar purpose, it's really powerful.
Akil Palanisamy: Yeah. I am also really excited about the upcoming event, and I think for anyone who feels like they're not being true to themselves in their work or as to themselves as they would want to be, I think this is a great opportunity to really reflect. And I think our vision for that weekend is that it's going to be a very introspective weekend and really focused in small groups and interactive elements. So it’s not going to be just mostly didactic.
Chris Kresser: Yeah. It’s not going to be Akil and I standing in front of the room talking at you the whole time. Definitely going to be the opposite of that.
Akil Palanisamy: Right, exactly, yeah. Because I think that this work is really about looking within and then sharing and connecting with other people. And so that's the focus of the weekend, is really building that sense of community with whoever comes and really learning to deepen your own sense of meaning and purpose in work, and look within to reconnect with that vision for what drew you to this work initially. Because I think that's the ultimate goal is having that feeling like you're really being true to yourself at the end of the day and having the kind of practice that you envision.
Don’t be afraid to make changes
Chris Kresser: Absolutely. I shared the story of Sheri in my book Unconventional Medicine, who is a clinician that was working in the VA. And she's a doctor and was mostly seeing patients with diabetes. That's the most common health challenge for veterans. And it was, she was counting the days until retirement. It was just really a factory-medicine type of situation. She often didn’t even have time to go to the bathroom during the day because she was just that busy from appointment to appointment. And as we've discussed, there was a real risk of moral injury because she didn't feel like she was making a difference. She was just handing out medications to these people and she wasn't, she knew as an athlete herself who tried to pay attention to her diet, she knew that wasn’t the best way to go about it. But what else could she do in the amount of time that she had?
And she moved into kind of a more, started incorporating more of a functional approach in her work, and then eventually left and started her own Functional Medicine practice. But for her, it was just a total game changer. She went from counting the days to retirement, to not ever being able to imagine retiring. And that's the kind of shift that’s possible, I think, when you really address the root causes of burnout and take the opportunity to step out of your current system, your current day-to-day, and really give yourself the chance to discover something new. And even if that’s maybe moving in a different direction entirely, or maybe staying in your current situation but just making a series of small changes that collectively can have a big impact.
Akil Palanisamy: Yeah, I think for me, my whole approach has been in terms of incremental change because I know that for many people, they have gone out of the insurance model and set up their own Functional Medicine practice, and that can be fantastic. But my work is really just building change within the system. Because if the people within the system leave and do their own thing, then the system itself is going to not be changed. And so I think that a big part of this is also figuring out solutions within systems and incremental steps we can take, and I think that'll hopefully be part of what we talk about as well. Just if you do belong to a system, how you can take a leadership role and effect change within that system as well.
Chris Kresser: Absolutely. That's why Akil and I are a good team, because I’m outside the system and he’s inside of the system, and we have different perspectives. So that's another reason I'm happy to team up with him. I mentioned this in the beginning, but I'll throw it out there again. You need not be an MD to participate in this workshop. It's really for all healthcare practitioners and providers who are experiencing burnout. And so this could be anyone from a health coach to a nutritionist to a dietitian to an occupational therapist to a chiropractor, a naturopath in addition to MDs, and DOs, and MPs, and PAs, and all of the other abbreviations and acronyms. Anyone working in healthcare really would be welcome. And we’re not even limiting it to people working in healthcare. We don't want to exclude people here, so if you're not working in healthcare and the things we've been talking about resonate with you, maybe you work in emergency services or something else, you are absolutely welcome to come.
Akil Palanisamy: Yeah, and I would add that even if you're not feeling burned out, I think that prevention is really the best medicine.
Chris Kresser: That’s true.
Akil Palanisamy: So I think learning about the research and the science, because we know how to prevent it, and it's much better to prevent burnout than treat it once it happens.
Chris Kresser: That is a very good point. Yeah, and I guess if the statistics are any indication, we know that even if you’re not feeling burnout now, chances are statistically you will at some point.
Akil Palanisamy: Right.
Chris Kresser: Especially without any intervention. It’s kind of like the diabetes example I used before. If you’ve got high normal blood sugar, now’s the time to get it under control rather than waiting until it turns into diabetes.
Akil Palanisamy: Right.
Chris Kresser: Great, well, thank you so much, Akil, for being with us. It’s a fascinating and important topic, and I’m really looking forward to leading this workshop with you. Again, in the retreat, you can go to 1440, it’s 1-4-4-0 dot o-r-g, and when you get there on the website, you just hover over Learn, and then under programs click on Professional Development. And if you scroll down there, you’ll see our program, which, again, is on the first weekend of October, October 5th to 7th, it’s a Friday through a Sunday.
And there’s a tuition for the program, and then there’s several different accommodation options available there. It’s really neat. I like what they've done with that. Everything from a private room to a suite to a really cool bunk style, kind of modern bunk-style accommodation that's much more affordable. I don’t know if you saw those last time.
Akil Palanisamy: I did, yeah.
Chris Kresser: Check the pictures out, they look pretty cool. They call them pods.
Akil Palanisamy: Right, yeah, yeah. They’re pretty comfy. I’ve seen them.
Chris Kresser: Yeah, yeah, it looks great. So lots of different accommodation options. If you’ve never been to this part of the world, the Santa Cruz Mountains are a beautiful, beautiful area, gorgeous redwood forests. You can head down to the beach before or after in Santa Cruz there. It’s a funky, cool little town. Great, great part of the world. So I hope you can make it. Those of you who have been listening to this and resonating with it, we’d love to meet you in person and have a chance to explore these topics with you.
And then Akil, is also, we haven’t talked much about his other work, but he’s also an author in addition to being a clinician. And he organizes the Paleo Symposium every year that I've been fortunate enough to be a speaker at. So why don’t you tell everyone a little bit more about your work and where they can find out more about your work.
Akil Palanisamy: Oh sure, yeah. So I practice integrative medicine and I combine Functional Medicine with the Paleo approach and Ayurveda, which is the traditional medicine of India. And still that has led to my book which is called The Paleovedic Diet, combining Paleo and Ayurvedic medicine. And the best way to connect with me would be through my website, which is DoctorAkil.com. Just doctor spelled out, A-k-i-l dot com. And yeah, I wanted to thank you, as well, Chris, for having me on the podcast. I’m very excited to be working on this event with you, and it was really a pleasure to talk today.
Chris Kresser: Pleasure is mine, Akil. And I'm sure we’ll be in touch before October, but I look forward to seeing you then and anyone else who's listening, who wants to join us. So 1440.org, and thanks for listening, everybody. Keep sending your questions in. I know I haven’t answered many of them recently. We’ve been doing a lot more interviews lately. But I do see that I have a few Q&A episodes coming up, and we do read all of your questions, and we also consider them for writing articles or emails.
So even if we’re not able to answer them on the show, it helps me to understand what you're thinking about and what you want me to write about and talk about. So please do keep sending them in. That’s ChrisKresser.com/podcastquestion. And thanks, everyone, for listening. And thank you, Akil, and we’ll see you next time.
Akil Palanisamy: Thank you, Chris.
The post RHR: How to Fight Practitioner Burnout with Dr. Akil Palanisamy appeared first on Chris Kresser.
RHR: How to Fight Practitioner Burnout with Dr. Akil Palanisamy published first on https://chriskresser.com
0 notes
Text
2017-2(FEB)-26 & 27--a--Sunday & Monday.
2017-2(FEB)-26 & 27--a--Sunday & Monday
Sunday:---------
I had to get some painkillers (pain maskers) today as I'm practically almost all out. I saw a LOT of black tyre marks on the roads...burnouts.....
Returned, and saw a few mini criminals from the aboriginal CRIMINAL HOUSEHOLD roaming the streets.
I also saw late afternoon that a rubbish bin from a house THAT HAS NOBODY LIVING THERE (next to the aboriginal CRIMINAL HOUSEHOLD), that bin has highly suspiciously just appeared against the kerb ready for council rubbish collection.....but the rubbish truck won't be due for 3 days.......
Another rubbish bin situated just across the street from the aboriginal CRIMINAL HOUSEHOLD has been sitting there on the street kerb in the street for almost a solid week (5 days)........why do you think? Could it be that the crims have used it and can't be bothered to put it back and is used as a 'marker' to see if a household has returned from (wherever/holidays) and has taken back their own bin?
There's also some smashed glass on the road......
The criminals were 'hidden' and hiding away for a day or so, but today on Sunday afternoon they were visibly out and roaming the streets from-and-going-in-and-out-of the aboriginal CRIMINAL HOUSEHOLD.......darting in and out or just sitting on the front fence, as they nestled in amongst the overgrown foliage that they used to conceal themselves being seen from any passing POLICE or authorities........(any normal innocent resident who would live there would have long ago trimmed-up the deliberately heavily overgrown 'jungle' that the criminals have let be overgrown so they cannot be observed such as not having any of the criminal kids ones go to school..........
I heard a POLICE car siren close during Sunday afternoon on a couple of seperate ocassions.........
Everything criminal around is STILL existing. It's just being hidden more carefully and not made so 'apparent' to any and all. Hence the apparent 'success' of POLICE and authorities to reign in and control the criminals.........meanwhile the rubbish bins keep coming on the streets for many days at a time (or not ever being put away) whilst all other innocent residents have completely empty front verges where they don't even dare to park their cars upon lest they be a target for criminals.......
----------------------------------------------------------------------
I'm so utterly exhausted. Utterly been without any proper sleep for days now. I had about 4 hours in two batches overnight. First batch was 1.5 hours of terrible broken 'sleep', and the rest was afterwards and just as terrible and broken....not sleep at all.
Around 4-5pm on Sunday I was so exhausted that I almost physically collapsed from lack of sleep, and I had to lay down. Just as I was getting to sleep, Sam & Max demanded to go outside, so I had to let them out. Sleep gone again.
----------------------------------------------------------------------
Monday:--(very early am moring)-----
Later.....I managed to get to 'sleep' but kept waking up in pain. Still haven't had any proper 'sleep'. I am more than utterly exhausted.
I eventually had to get up and feed dear Sam & Max, then take them outside for their much needed ablutions session during the temporary cool-before-the-dawn period which is now very very short. (And which people mistakenly assume is going to last all day.)
----------------------------------------------------------------------
Every day starts the same.....and whilst the sun is not out (when it's darkness), the temperatures in this hellhole area is coolish and tolerable. But as soon as the sun gets up.....it gets HOT...too HOT. And it always goes up far more than the temperature forecasts predict. - Oh and of course, it's utterly dry, no rain or anything and so things are dying and so plants and stuff are going dry & 'crisp' as they're dying. -- And of course the weather department puts out stating in a few days time there 'might' be a small tiny chance of some precipitation coming....so you're advised not to use any water because there's 'rain' comong. The same 'rain' that (if it does come) just evaporates when it hits the ground because it's so hot and utterly dry. It just rearranges the dry dust.
Oh, by the way, everytime I go outside and it's dark, I do an impromptu air test by shining a flashligt up into the dark ('night') sky. -- And when I do, I almost always see ultra dust swirling about like smoke and falling down EVERY time.
I've been sneezing a LOT. On Sunday it was about 18 times, The day before was around 20-30 times. The only reason Sunday was less was because I took some pills to try to contain it. I hate going outside, coming back into this hove, laying down to rest, and then suddenly sneezing, or sneezing just as I'm getting tired to maybe get some 'sleepp. -- And I was not the only one sneezing a LOT.
P@4:46am---Monday--27-February-2017.....I love you Fliss and want to be with you. I dearly hope you are okay.
0 notes