#Ast Alt Medical Abbreviation
Text
TERMURAH Telp/WA 0821-2767-2598 Peralatan Klinik Gigi Kendal Jawa Tengah PT. JMM
Pterygota Alata Medicinal Uses, Terminalia Alata Medicinal Uses, Hyptis Alata Medicinal Uses, Passiflora Alata Medicinal Uses, Senna Alata Medicinal Uses
10 Peralatan Dokter,Online Shop Alat Kesehatan,Alat Kesehatan Radiologi
TIPS MENCEGAH URID ACID
Asam urat adalah kondisi kesehatan yang dapat menyebabkan nyeri dan pembengkakan pada sendi. Berikut adalah beberapa tips untuk mencegah asam…

View On WordPress
#Alat Lab Test#Alt Medical Abbreviation#Alt Medical Abbreviation Normal#Ast Alt Medical Abbreviation#Left Alt Medical Abbreviation
0 notes
Text
Case of Necrotizing Pancreatitis following COVID-19 Infection by Faezeh Sehatpour in Journal of Clinical Case Reports Medical Images and Health Sciences

ABSTRACT
New aspects of COVID-19 are increasingly being recognized. Although the virus is mainly known to affect the lungs, involvement of other organs including the heart, liver, gastrointestinal, renal and pancreas is also detected. Acute pancreatitis is detected as one of both the early and late presentations of COVID -19. Cytokine storm or the presence of angiotensin-converting enzyme 2 (ACE2) receptor in pancreatic cells, are both two causes of pancreatic injury in COVID-19 infection. In this study, we reported a 25-year-old man admitted to our department with the impression of necrotizing pancreatitis concomitant with COVID-19 infection. Patient's lab data, imaging and outcomes were documented in full detail.
Abbreviations:
WBC, white blood cell;HB, hemoglobin; MCV, mean corpuscular volume; PLT, platelet; BUN, blood urea nitrogen; Na, sodium; K, potassium; ; AST, aspartate aminotransferase; ALT, alanine aminotransferase; ALK.P, alkaline phosphatase; ALB, albumin; LDH, Lactate dehydrogenase ; CPK, creatine phosphokinase; CRP,c-reactive protein; AFP,alpha-fetoprotein; CEA,carcinoembryonic antigen; CA19-9,cancer antigen 19-9; Immunoglobulin G4.
INTRODUCTION
The Covid-19 pandemic is an ongoing pandemic that started in December 2019 and spread rapidly around the word. COVID-19 was caused by severe acute respiratory syndrome corona virus 2 (SARS-CoV-2), first identified in Wuhan, China. So far, more than 200 countries have been affected by the pandemic. (1)
New aspects of COVID-19 are increasingly being recognized. Although the virus is mainly known to affect the lungs, involvement of other organs including the heart, liver, gastrointestinal, renal and pancreas is increasingly being reported. (2)
The involvement of the gastrointestinal system is maybe due to the expression of the angiotensin-converting enzyme2 (ACE2) on the hepatocyte, cholangiocyte and other parts of the GI tract. (3) In a recent survey, acute pancreatitis was detected as one of both early and late presentations of COVID -19. (4-6) However, it is still unclear whether SARS-COV-2 directly affects pancreatic cells because of ACE2, if it is a cytokine storm which causes pancreatic injury. (7)
We reported a case of COVID-19 with subsequent acute necrotizing pancreatitis.
CASE REPORT
A 25-year-old man without any known medical disease presented to our emergency department with progressive epigastric pain, nausea and vomiting and anorexia one week prior to admission. He has no history of alcohol consumption. He also had a history of admission to another hospital about two weeks ago with a diagnosis of COVID-19 pneumonia. On admission, he has a blood pressure of 115/75 mm HG, a heart rate of 100 beats per minute, a temperature of 37.1 ⁰C and oxygen saturation of 95% while the patient is breathing in the room air. Primary investigations summarized in Table-1. Amylase and lipase were 146 IU/L and 82 IU/L respectively. Nasal swab test for COVID-19 (RT-PCR for SARS-CoV-2) was positive. Abdominal sonography showed markedly prominent pancreas with in homogeneous parenchymal echogenicity and large cystic lesion arising from the pancreas, in favor of acute complicated pancreatitis with pseudo cyst. The gall bladder has a normal size and wall thickness without any gall stones. The pancreatic duct was not dilated. Due to the finding of abdominal ultra sound, CT scan of abdomen was done on him which revealed an enlarged pancreas with necrosis of the main portion of pancreatic parenchyma. Large cystic lesion measuring 15×7×11 cm in size arising from the pancreatic neck with extension to the right and left side of the abdomen suggestive of large pancreatic pseudo cyst (figure1). Lung HRCT (low dose) also showed bilateral peripheral ground glass opacities in favor of COVID-19 pneumonia (figure2). According to the findings of a physical exam, laboratory data and clues in imaging immediate management of acute necrotizing pancreatitis (invasive intravenous hydration and pain control) was started for him. He was finally discharged from the hospital with a full recovery.
Table 1: laboratory data
Figure 1: Abdominal CT scan: large loculated pseudo cystic structure measuring about 158mm*100mm in lesser sac due to post pancreatitis pseudo cyst formation.
Figure 2: lung HRCT: multiple ground glass and bilateral pleural effusion
DISCUSSION
Acute pancreatitis is an acute inflammation of the pancreas characterized by abdominal pain, nausea, vomiting and elevated exocrine pancreatic enzymes; amylase and lipase. Gallstones and chronic alcohol abuse are the most common causes of acute pancreatitis. Viruses are uncommon causes of acute pancreatitis. Pancreatitis has been reported with several viruses, including mumps,
coxsackievirus, hepatitis A and B virus, cytomegalovirus, varicella-zoster, herpes simplex and human immunodeficiency virus. (8)
Although we have not conclusively proven the presence of the virus in the pancreas, the causes of COVID-19 and acute pancreatitis and the lack of other clear causes for pancreatitis strengthen the relationship between the two diseases. In this study, the patient presented with necrotizing COVID-19in 19 in the early post period of COVID-19 infection.
In Fan Wang and colleagues' survey, 52 COVID-19 cases followed and showed that 17% of COVID-19 patients developed pancreatic injury and presented with mild elevated pancreatic enzymes; serum amylase and lipase without clinically severe pancreatitis. The possibility of drug induced acute pancreatitis in patients who have received medication due to COVID-19 is also expressed as one of the reasons for acute pancreatitis in COVID-for19 infection. (9) Saffa Saeed Al Mazrouei and his teammates reported a 24-year-old patient with acute non-necrotizing pancreatitis with concurrent COVID-19. No evidence of pseudo cyst or abscess was detected in his imaging. (10)
Pancreatic damage can be due to the direct effect of the virus on pancreatic cells or indirectly secondary to the immune system. In another study in Wuhan, it showed that ACE2 was expressed in the pancreas higher than the lung in the normal population, indicating that SARS-CoV-2 can bind to ACE2 in the pancreas and cause pancreatic cell damage. (7, 11)
Acute pancreatitis is one of the presentations or complications of COVID-19 infection. Further investigation with samples is needed to reveal the pathophysiology, presentation, treatment and prognosis of acute pancreatitis in COVID-19 infection.
For more information: https://jmedcasereportsimages.org/about-us/
For more submission : https://jmedcasereportsimages.org/
#COVID-19#Cytokine storm#blood cell;HB#aminotransferase#CRP#c-reactive protein#carcinoembryonic antigen#alpha-fetoprotein#anorexia#RT-PCR for SARS-CoV-2#HRCT#Faezeh Sehatpour#jcrmhs
0 notes
Photo


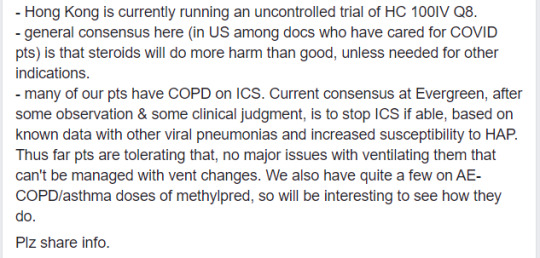
[Current as of March 13, 2020]
Dr. Shahed (screenshot above) is an emergency department physician in Ohio who shared this post on Facebook. It’s an account of COVID-19 from the perspective of an ICU doc working on the frontlines in Seattle. Some of my laypeople-friends were sharing it around (and I’ve seen it floating around on twitter and various internet forums], but I noticed that it’s really dense and contains a lot of medical abbreviations and jargon, like it was meant more for other physicians and isn’t really useful for the average reader. So I thought I’d provide a translation for my non-medblr followers who are looking to stay informed. (If you want further clarification, feel free to drop me an ask)
***
This is from a front-line ICU physician in a Seattle hospital
This is his personal account:
We have 21 patients and 11 deaths since 2/28.
We are seeing patients who are young (20s), fit, no comorbidities, critically ill. It does happen.
US has been past containment since January
Currently, all of ICU is for critically ill COVID patients, all of med-surg [medical-surgical] floors are for stable COVID patients and end-of-life care, half of PCU [progressive care unit], half of ER. New Pulmonary Clinic offshoot is open for patients with respiratory symptoms
CDC is no longer imposing home quarantine on providers who were wearing only droplet-isolation PPE when intubating, suctioning, bronching, and in one case doing bloody neurosurgery. Expect when it comes to your place you may initially have staff home-quarantined. Plan for this NOW. Consider wearing airborne-isolation PPE for aerosol-generating procedures in ANY patient in whom you suspect COVID, just to prevent the mass quarantines.
We ran out of N95s (thanks, Costco hoarders) and are bleaching and re-using PAPRs [powered air purifying respirators], which is not the manufacturer’s recommendation. Not surprised on N95s as we use mostly CAPRs [controlled air purifying respirators] anyway, but still.
Terminal cleans (including UV light) for ER COVID rooms are taking forever, Environmental Services is overwhelmed. This is bad, as patients are stuck coughing in the waiting room. Recommend planning now for Environmental Service upstaffing, or having a plan for sick patients to wait in their cars (that is not legal here, sadly).
CLINICAL INFO (based on our cases and info from CDC conference call today with other COVID providers in US):
The Chinese data on 80% mildly ill, 14% hospital-ill, 6-8% critically ill are generally on the mark. Data [in the US] very skewed by late and very limited testing, and the number of our elderly patients going to comfort care.
Being young & healthy (zero medical problems) does not rule out becoming vented or dead
Probably the time course to developing significant lower respiratory symptoms is about a week or longer (which also fits with timing of sick cases we started seeing here, after we all assumed it was endemic as of late Jan/early Feb).
Based on our hospitalized cases (including the not-formally-diagnosed ones who are obviously COVID – it is quite clinically unique), about 1/3 of patients have mild lower respiratory symptoms and need 1-5L NC [1-5 liters of oxygen per minute, via nasal cannula]. 1/3 are sicker, need face mask or non-rebreather. 1/3 are intubated with ARDS [acute respiratory distress syndrome].
Thus far, everyone is seeing:
normal WBC [white blood cell] count. Almost always lymphopenic, occasionally poly [neutrophil]-predominant but with normal total WBC count. Doesn’t change, even 10 days in.
Bronchoalveolar lavage: lymphocytic despite blood being lymphopenic. (Try not to bronch these patients; this data is from pre-testing time when we had several idiopathic ARDS cases)
Fevers, often high, may be intermittent; persistently febrile, often for >10 days. It isn’t the dexmed, it’s the SARS2.
Low procalcitonin; may be useful to check initially for later trending if you are concerned later for VAP [ventilator-associated pneumonia], etc.
Elevated AST/ALT, sometimes alkaline phosphatase. Usually in 70-100 range. No fulminant hepatitis. Notably, in our small sample, higher transaminitis [elevated AST/ALT] (150-200) on admission correlates with clinical deterioration and progression to ARDS. LFTs [liver function tests] typically begin to bump in 2nd week of clinical course.
Mild AKI [acute kidney injury] (creatinine <2). Uncertain if direct viral effect, but notably SARS2 RNA fragments have been identified in liver, kidneys, heart, and blood.</li>
Characteristic chest x-ray: always bilateral patchy or reticular infiltrates, sometimes peri-hilar despite normal ejection fraction and volume down at presentation. At time of presentation may be subtle, but always present, even in our patients on chronic high dose steroids. NO effusions.
CT is as expected, rarely mild mediastinal lymphadenopathy, occasional small effusions late in course, which might be related to volume status/cap leak.
Note - China is CT'ing everyone, even outpatients, as a primarily diagnostic modality. However, in US/Europe, CT is rare, since findings are nonspecific, would not change management, and the ENTIRE scanner and room have to be terminal-cleaned, which is just impossible in a busy hospital. Also, transport in PAPRs, etc.
2 of our patients had CTs for idiopathic ARDS in the pre-test era; they looked like the CTs in the journal articles. Not more helpful than chest x-ray.
When respiratory failure occurs, it is RAPID (likely 7-10 days out from symptom onset, but rapid progression from hospital admission). Common scenario for our patients is: admit on 1L/min oxygen via nasal cannula. Next 12 hrs escalate to NPPV [non-invasive positive pressure ventilation]. Next 12-24 hrs → vent/proned/Flolan.
Interestingly, despite some needing Flolan, the hypoxia is not as refractory as with H1N1. Quite different, and quite unique. Odd enough that you’d notice and say hmmm.
Thus far many are dying of cardiac arrest rather than inability to ventilate/oxygenate.
Given the inevitable rapid progression to ETT [endotracheal tube, aka intubation] once respiratory decompensation begins, we and other hospitals, including Wuhan, are doing early intubation. Face mask is fine, but if patients are needing HFNC [high-flow nasal cannula] or NPPV [non-invasive positive pressure ventilation], just tube them. They definitely will need a tube anyway, and no point risking the aerosols.
No MOSF [multi-organ system failure]. There’s the mild AST/ALT elevation, maybe a small creatinine bump, but no florid failure. Exception is cardiomyopathy.
Multiple patients here have had normal EF [ejection fraction] on formal Echo or POCUS [point-of-care ultrasound] at time of admission (or in a couple of cases, EF 40ish, chronically). Also normal troponins from emergency department. Then they get the horrible respiratory failure, sans sepsis or shock. Then they turn the corner, come off Flolan, supined, vent weaning, looking good, never any pressor requirement. Then over 12 hrs, newly cold, clamped, multiple-pressor shock that looks cardiogenic, EF 10% or less. Then either VT [ventricular tachycardia, aka V-tach] → VF [ventricular fibrillation, aka V-fib] → dead, or PEA [pulseless electrical activity] → asystole in less than a day. Needless to say, this is awful for families who had started to have hope.
We have actually had more asystole than VT. Other facilities report more VT/VF, but same time course, a few days or a week after admission, around the time they’re turning the corner. This occurs on med-surg patients too. One today, who is elderly and chronically ill but with baseline EF preserved, became newly hypotensive overnight, EF <10. Already no escalation, has since passed. So presumably there is a viral cardiomyopathy aspect, which presents later in the course of disease.
Of note, no wall motion abnormalities on Echo, right ventricular function preserved, troponins don’t bump. Could be unrelated, but I’ve never seen anything like it before, especially in a patient who had been hemodynamically stable without sepsis.
TREATMENT:
Remdesivir might work, some hospitals have seen improvement with it quite rapidly, marked improvement in 1-3 days. ARDS trajectory is impressive with it, patients improve much more rapidly than expected in usual ARDS.
Recommended course is 10 days, but due to scarcity, all hospitals have stopped it when the patient is clinically out of the woods. None have continued >5 days. It might cause LFT bump, but interestingly seem to bump (200s-ish) for a day or 2 after starting, then rapidly back to normal, suggests this is not a primary toxic hepatitis.
Unfortunately, the Gilead compassionate use and trial programs require AST/ALT <5x normal, which is pretty much almost no actual COVID patients. Also CrCl [creatinine clearance] >30, which is fine. CDC is working with Gilead to get LFT requirements changed now that we know this is a mild viral hepatitis.
Currently the Gilead trial is wrapping up, NIH trial still enrolling, some new trial soon to begin, can’t remember where.
Steroids are up in the air. In China, usual clinical practice for all ARDS is high dose methylprednisolone. Thus, ALL of their patients have had high dose methylprednisolone. Some question whether this practice increases mortality.
It is likely that it increases secondary VAP/HAP [ventilator-associated pneumonia/hospital-acquired pneumonia]. China has had a high rate of drug-resistant GNR [Gram-negative rod] HAP/VAP and fungal pneumonia in these patients, with resulting increases in mortality. We have seen none, even in the earlier patients who were vented for >10 days before being bronch’ed (prior to test availability. Again, it is not a great idea to bronch these patients now).
Unclear whether VAP-prevention strategies are also different [in China vs US], but wouldn’t think so?
Hong Kong is currently running an uncontrolled trial of HC 100IV Q8 [hydrocortisone 100 mg IV every 8 hours].
General consensus here (in US among doctors who have cared for COVID patients) is that steroids will do more harm than good, unless needed for other indications.
Many of our patients have COPD on ICS [inhaled corticosteroids]. Current consensus at Evergreen, after some observation & some clinical judgment, is to stop ICS if able, based on known data with other viral pneumonias and increased susceptibility to HAP. Thus far patients are tolerating that, no major issues with ventilating them that can’t be managed with vent changes. We also have quite a few on AE-COPD [acute exacerbation of COPD]/asthma doses of methylprednisolone, so will be interesting to see how they do.
8 notes
·
View notes
Text
300+ TOP DOCTOR Interview Questions and Answers
DOCTOR Interview Questions for freshers experienced :-
1) Explain who is Doctor?
A physician is someone who practices medicine to treat illnesses and injuries.
Physicians go to medical school to be trained. They typically hold a college degree in medicine. Physicians once made house calls to treat patients at home, but now mostly see patients in their offices or in hospitals. Physicians may also work for schools, companies, sports teams, or the military. Physicians are often assisted by nurses or other staff.
2) How doctor treat patients?
Physicians treat patients by diagnosing them, or figuring out what is wrong. When Physicians diagnose a patient, they begin by asking questions about the patient's symptoms such as fever, headache, or stomach ache. They may ask other questions about things like past illnesses or family members who have been sick. They will then examine the patient, often looking at different parts of the body and listening to the heart and lungs with a stethoscope. Sometimes they may need to collect blood, use an x-ray machine, or use other tools to look for things they cannot see when examining the patient. Usually, when they have gathered enough information, a doctor can make a diagnosis and then prescribe a treatment. Often they prescribe .
3) Who is a specialists doctor?
Some doctors specialise in a certain kind of medicine. These physicians are called specialists. They may only treat injuries to a certain part of the body, or only treat patients who have certain diseases. For example, there are physicians who specialise in diseases of the stomach or intestines. Other physicians are "general practitioners" or "family practitioners". This means that they do a little bit of everything. They try to deal with as much of a patient's health problems as they can without sending them to a specialist. A doctor who performs surgery is called a surgeon.
4) How communication skills help patient?
Once a patient begins developing trust in a doctor, the chances of him/her recovering increases as his/her confidence in the doctor goes up and s/he begins to believe that s/he can recover.
5) Why doctors should learn communication skills?
Communication skills play a major role in developing patient-doctor relationship. And miscommunication could lead to clashes with relatives/friends of patients over care given to the latter.
6) What is Venous thrombosis?
There are numerous extra-gastrointestinal manifestations of inflammatory bowel disease that occur in both ulcerative colitis and Crohn's disease, such as uveitis, conjunctivitis, arthritis, pyoderma gangrenosum and erythema nodosum. Some occur primarily in Crohn's, such as gallstones and renal stones due to the area of bowel affected, while patients with ulcerative colitis are more likely to develop primary sclerosing cholangitis and venous thromboses.
7) What is Azathioprine?
Azathioprine takes a number of months to exert its anti-inflammatory effect and therefore has a limited role in the acute management of Crohn's disease, though it can be started at the time of an acute flare of Crohn's.
8) What is Bendroflumethiazide?
Treatment of hypercalcaemia can include fluid rehydration, loop diuretics, bisphosphonates, steroids, salmon calcitonin and chemotherapy.
In clinical practice intravenous fluids are the first-line agent used to treat hypercalcaemia, both rehydrating the patient and helping to lower the calcium levels. This is combined with the co-administration of bisphosphonates such as pamidronate, which exert their maximal effect 5-7 days after administration.
9) What is Ceftriaxone?
A cephalosporin such as ceftriaxone is first-line treatment in patients with streptococcal meningitis. Benzylpenicillin would be more appropriate if Neisseria meningitidis was suspected.
10) What is Anti-Histone antibody?
In induced SLE anti-histone antibody is present in 90% of patients, although this is not specific for the condition. Anti-nuclear antibody is positive in 50% of patients as opposed to 95% of patients with idiopathic SLE.

DOCTOR Interview Questions
11) What is C-reactive protein?
In SLE the erythrocyte sedimentation rate is classically raised while C-reactive protein levels can stay normal and therefore CRP is also not as useful as the other investigations to monitor disease activity and progression.
12) What are the parameters of life-threatening asthma?
Peak expiratory flow rate of Tachycardia: heart rate > 100 beats per minute
Inability to complete sentences with one breath
14) What is terbutaline 10 mg nebulised
In the management of asthma, patients should be sitting upright in bed and receiving 100% oxygen. Salbutamol is given at a dose of 5 mg nebulised, not 500 micrograms. Ipratropium bromide and steroids should then be considered.
15) Medical Abbreviations part 19:
TFTs - thyroid function tests
U - units
UC - ulcerative colitis
V/Q - ventilation/perfusion
WCC - white cell count
16) Medical Abbreviations part 18:
RBBB - right bundle branch block
SIADH - syndrome of inappropriate ADH secretion
SLE - systemic lupus erythematosus
STEMI - ST-elevation myocardial infarction
STD
17) Medical Abbreviations part 17:
p.r.n. - pro re nata
PSA - prostate-specific antigen
PSC - primary sclerosing cholangitis
PSGN - post-streptococcal glomerulonephritis
RAS - renal artery stenosis
18) Medical Abbreviations part 16:
PaO2 - partial pressure of oxygen
PCA - patient-controlled analgesia
PCI - primary coronary intervention
PCP - Pneumocystis carinii pneumonia
PCR - polymerase chain reaction
19) Medical Abbreviations part 15:
--> NICE
1) Formerly: National Institute for Clinical Excellence
2) Currently: National Institute for Health and Clinical Excellence
--> NMDA - N-methyl-D-aspartate
--> NSAIDs - non-steroidal anti-inflammatory
--> NSTEMI - non-ST-elevation myocardial infarction
--> PaCO2 - partial pressure of carbon dioxide
20) Medical Abbreviations part 14:
MRI - magnetic resonance imaging
MRSA - methicillin-resistant Staphylococcus aureus
MSH - melanocyte-stimulating hormone
NAC - N-acetylcysteine
NG - nasogastric
21) Medical Abbreviations part 13:
LFT - liver function test
LTOT - long-term oxygen therapy
MCV - mean cell volume
MHC - major histocompatibility complex
MMSE - mini mental state examination
22) Medical Abbreviations part 12:
J - joules
JVP - jugular venous pressure
LBBB - left bundle branch block
LDH - lactate dehydrogenase
LDL - low-density lipoprotein
23) Medical Abbreviations part 11:
HONKC - hyper-osmolar non-ketotic coma
HSP - Henoch-Schnlein purpura
HUS - haemolytic uraemic syndrome
IV - intravenous
IVDU - intravenous user
24) Medical Abbreviations part 10:
HAART - highly active antiretroviral treatment
hCG - human chorionic gonadotrophin
HDL - high-density lipoprotein
HDU - High-Dependency Unit
HLA - human leukocyte antigen
25) Medical Abbreviations part 9:
G6PD - glucose-6-phosphate dehydrogenase
GCS - Glasgow coma scale
GFR - glomerular filtration rate
GORD - gastro-oesophageal reflux disease
GTN - glyceryl trinitrate
26) Medical Abbreviations part 8:
FEV1 - forced expiratory volume in 1 second
FFP - fresh frozen plasma
FH - familial hypercholesterolaemia
Fi(O)2 - fraction of inspired oxygen
FVC - forced vital capacity
27) Medical Abbreviations part 7:
DVT - deep vein thrombosis
ERCP - endoscopic retrograde cholangiopancreatography
ESR - erythrocyte sedimentation rate
F1 - Foundation year 1 doctor
F2 - Foundation year 2 doctor
28) Medical Abbreviations part 6:
CPAP - continuous positive airway pressure (ventilation)
CPR - cardiopulmonary resuscitation
CRP - C-reactive protein
CSF - cerebrospinal fluid
dsDNA - double-stranded DNA
29) Medical Abbreviations part 5:
CDT - Clostridium difficile toxin
CIN - cervical intraepithelial neoplasia
CLL - chronic lymphocytic leukaemia
COMT - catechol-O-methyltransferase
COPD - chronic obstructive pulmonary disease
30) Medical Abbreviations part 4:
BCG - bacille Calmette-Guerin
BHL - bilateral hilar lymphadenopathy
BMI - body mass index
BNP - B-type natriuretic peptide
CEA - carcinoembryonic antigen
31) Medical Abbreviations part 3:
AMT - abbreviated mental test
ANA - antinuclear antibody
ANCA - anti-neutrophil cytoplasmic antibody
APACHE - acute physiology and chronic health evaluation
AST - aspartate aminotransferase
32) Medical Abbreviations part 2:
ADH - antidiuretic hormone
AFB - acid-fast bacilli
AIDS - acquired immunodeficiency syndrome
ALP - alkaline phosphatase
ALT - alanine aminotransferase
33) Medical Abbreviations part 1:
AF - atrial fibrillation
aFP - alpha-fetoprotein
ABG - arterial blood gas
ACE - angiotensin-converting enzyme
ACTH - adrenocorticotrophic hormone
34) How many childrens affected with asthma in UK?
Asthma affects over 5 million individuals in the UK. Approximately 1 million children are affected.
35) Can medication is known to cause hypokalaemia?
The medication is most likely to be a selective 2-agonist such as salbutamol, which leads to a tremor, palpitations, headaches and hypokalaemia at high doses. Washing the mouth after administration of inhaled steroids is recommended, no matter what dose is given. Atrovent is the trade name for ipratropium bromide, which is more useful in chronic obstructive pulmonary disease than in asthma, although it can be used in an acute asthma attack.
36) Patient feeling randomly sick with headaches. What could it be?
Persistent headaches are not something that can be ignored, as this could be your body trying to send you a signal that there is something wrong. Often, the history and description of the headache can be quite helpful as you attempt to determine what is the cause of your headaches so that you can know how to get better. If your headaches are associated with certain movements, activities, foods, or other triggers, than this can serve as a clue to you and your doctor to help you feel better. If, on the other hand, your symptoms are somewhat predictable and come on in the same way, then it is also possible to use this information to diagnose the type of headache, which then gets you closer to getting some help with your pain and other symptoms. Migraines are classically associated with light sensitivity, nausea and vomiting, and intractable and incapacitating pain. People with migraines may have a family history of them, and they may have an aura, or symptoms that routinely come before the headache and let them know it is coming.
37) Why should be pain in neck?
There are times that infections can happen in the neck, and these infections can be very serious because of the number of important structures that run through the neck. Some of these include nerves that are relevant to moving some of the muscles of your upper extremities, and others are the very important arteries and veins that run through your neck to and from your head. Often, if people have an infection, they will also have symptoms of an infection, such as a high fever, swelling, redness, etc. These can be more common in those with a history of injecting, as this allows serious and dangerous bacteria direct access to the rest of the body through the arteries and veins. If it has been a while since your last injection, then it may make an infection less likely. Swelling and pain can also happen from muscle spasms that come with poor posture or increased exertion out of the norm. There are also some other possible explanations.
38) Why do in some cases patients feel chest, neck and hands flush?
Certainly the thought of carcinoid syndrome is something that crosses the mind in hearing about your symptoms. That is, however, a rather rare process that would be unusual for most people to have. In such a situation, it is good to describe your symptoms and your concerns to your doctor so that he or she can test for the possibility of something as serious or as rare as that condition. There are many other possible explanations, however, many of which are much more common. It is not unusual for some people to have changes of flushing and some of the other feelings that you describe when they are in stressful or unusual situations. Some of this can sometimes be understood in context of the response that some people have to loud noises or fright, ie, they can faint. This reaction is one extreme on the spectrum of a vagal reaction that can occur in some. On a less extreme note, other can have some of the same symptoms you describe without having something as notable as a syncopal episode. There are often things that can be done to help.
39) Suppose if a patient have abnormal blood on his underwear how you deal?
Abnormal bleeding can have many different causes, but you have provided some valuable information. First, we have to clarify where exactly the bleeding is coming from. While vaginal bleeding is perhaps the most likely, both the urinary tract and the GI tract can also be a source of bleeding. Either of those would have different causes and explanations, with infections and small sources of bleeding such as hemorrhoids being among the most common reasons for abnormal or untimely bleeding. With regards to vaginal bleeding, there is a clue that is suggested by the fact that the blood is bright red in color. In general, this can reflect fresher blood that has not started to be broken down. It may also suggest blood that is coming from a source further down the vaginal tract, although that is not necessarily true. There are different conditions that can affect the vaginal or uterine lining and are common explanations for symptoms such as you describe. There are also tumors that can result in abnormal bleeding, and these tumors can be both benign and malignant.
40) Suppose if patient have unbearable neck to shoulder pain only while on his period. What could it be?
This is a somewhat interesting phenomenon that will take more visits to your doctor to help explain. Your OB/GYN is likely a good place to start, as he or she will be best positioned to help sort out the hormonal element to your symptoms. Another option might be a neurologist or spine surgeon, either of which may be able to help with your symptoms at the level of your neck. An ear nose and throat surgeon may offer some other insight that could be helpful. Whichever you choose, the approach to your problem will likely be different. Primary care and medical doctors are more likely to use lab work and your symptoms to help arrive at an answer, and may use medications empirically to see what helps to make you better. A surgeon, on the other hand, is more likely to listen to your symptoms, complete an exam, and recommend imaging and other anatomic studies that can help to determine what is causing your symptoms. The pain may have a component of something that changes on a monthly basis with your menstrual cycle. This could be a swelling, or even something as simple as a change in the blood flow.
41) Suppose if patient having chronic neck pain for 4 days. Medication and RMT massage have done nothing, pain is 10/10 now. What could it be?
It is not normal for pain to become so severe and fail to respond in any way to conservative therapy, and so your doctor should discuss this with you in more detail to make sure that there is nothing serious that is causing your symptoms. Neck and muscle spasms can be common in some people with a history of c spine injury or trauma, and can be severe and debilitating. They should not be a new onset symptom for most people, however, unless you have had some precipitating event. Massage and things to help the muscles relax is often a great idea to help with some of the mild aches and pains that we can have from time to time, and the fact that you had no improvement is worrisome. Your doctor may entertain other possible explanations for this pain in addition to trauma and misuse injuries. He or she may decide it is important to get some imaging and complete a physical exam looking for things that might be amiss. Shooting pain can be a concern for nerve injury.
42) Suppose if I am patient of acid reflux, how can I get rid off?
Fortunately, there are things that can be done to help with reflux. The most obvious answer is some of the many medications that are available to help reduce stomach acid. Some of the least expensive and most effective are even available over the counter, but should be used after discussing your symptoms with your doctor. There are some medications, such as ranitidine and other anti histamine medications (H2 blockers as they are sometimes called), that can be very effective for many people and have a very mild side effect profile. They are most effective when taken as directed, and the efficacy does tend to decrease if they are not timed appropriately with regards to the meals. Other excellent medications are those that are known as proton pump inhibitors, or PPIs, which can be even more effective. The over the counter doses are effective for most people, but in severe cases prescription strength doses can also be used. These medications also have relatively mild side effects, but should be discussed with your doctor. In addition to these medications, lifestyle changes should be tried before any medications. These can be found suggested in many places. Please speak with your doctor.
DOCTOR Questions and Answers pdf Download
Read the full article
0 notes
Link
Blood Tests
Normal test result values are expressed as a reference range, which is based on the average values in a healthy population, 95% of healthy people have values within this range. These values vary somewhat among laboratories, due to methodology and even geography. Tests and testing vary widely in different parts of the world, and in different parts of most countries, due to characteristics in the population, as well as other factors.
American Blood laboratories use a different version of the metric system (mass per volume). The rest of the world uses the Systeme Internationale (SI). In some cases translation between the two systems is easy, but the difference between the two is most pronounced in the measurement of chemical concentration. The American system generally uses mass per unit volume, while SI uses moles per unit volume. Since mass per mole varies with the molecular weight of the substance being analyzed, conversion between American and SI units requires many different conversion factors.
Most Blood tests fall within one of two categories: Screening or Diagnostic.
Screening Blood tests are used to try to detect a disease when there is little or no evidence that a person has a suspected disease. For example, measuring cholesterol levels helps to identify one of the risks of heart disease. These screening tests are performed on people who may show no symptoms of a disease or illness, they are used as a tool for the physician to detect a potentially harmful and evolving condition.
Diagnostic Blood tests which are utilized when a specific disease is suspected to verify the presence and the severity of that disease.
Because most Blood test reference ranges (often referred to as 'normal' ranges of Blood test results) are typically defined as the range of values of the median 95% of the healthy population, it is unlikely that a given Blood sample, even from a healthy patient, will show "normal" values for every Blood test taken. Therefore, caution should be exercised to prevent over-reaction to mild abnormalities without the interpretation of those tests by your examining physician. Again, a Blood test, though important, is only a part of the final diagnosis of a potential health problem.
Here is a sample of what a "normal" blood test looks like. Keep in mind that your test might turn out slightly different from this one. Slight differences are to be expected.
BLOOD TEST REFERENCE RANGE CHART
Test: Reference Range (conventional units)
Acidity (pH) 7.35 - 7.45
Alcohol 0 mg/dL (more than 0.1 mg/dL normally indicates intoxication) (ethanol)
Ammonia 15 - 50 µg of nitrogen/dL
Amylase 53 - 123 units/L
Ascorbic Acid 0.4 - 1.5 mg/dL
Bicarbonate 18 - 23 mEq/L (carbon dioxide content)
Bilirubin Direct: up to 0.4 mg/dL
Total: up to 1.0 mg/dL
Blood Volume 8.5 - 9.1% of total body weight
Calcium 8.5 - 10.5 mg/dL (normally slightly higher in children)
Carbon Dioxide Pressure 35 - 45 mm Hg
Carbon Monoxide Less than 5% of total hemoglobin
CD4 Cell Count 500 - 1500 cells/µL
Ceruloplasmin 15 - 60 mg/dL
Chloride 98 - 106 mEq/L
Complete Blood Cell Count (CBC) Tests include: hemoglobin, hematocrit, mean corpuscular hemoglobin, mean corpuscular hemoglobin concentration, mean corpuscular volume, platelet count, and white Blood cell count.
Copper Total: 70 - 150 µg/dL
Creatine Kinase (CK or CPK) Male: 38 - 174 units/L
Female: 96 - 140 units/L
Creatine Kinase Isoenzymes 5% MB or less
Creatinine 0.6 - 1.2 mg/dL
Electrolytes Test includes: calcium, chloride, magnesium, potassium, sodium.
Erythrocyte Sedimentation Rate (ESR or Sed-Rate) Male: 1 - 13 mm/hr
Female: 1 - 20 mm/hr
Glucose Tested after fasting: 70 - 110 mg/dL
Hematocrit Male: 45 - 62%
Female: 37 - 48%
Hemoglobin Male: 13 - 18 gm/dL
Female: 12 - 16 gm/dL
Iron 60 - 160 µg/dL (normally higher in males)
Iron-binding Capacity 250 - 460 µg/dL
Lactate (lactic acid) Venous: 4.5 - 19.8 mg/dL
Arterial: 4.5 - 14.4 mg/dL
Lactic Dehydrogenase 50 - 150 units/L
Lead 40 µg/dL or less (normally much lower in children)
Lipase 10 - 150 units/L
Zinc B-Zn 70 - 102 µmol/L
Lipids: Cholesterol Less than 225 mg/dL (for age 40-49 yr; increases with age)
Triglycerides
10 - 29 years 53 - 104 mg/dL
30 - 39 years 55 - 115 mg/dL
40 - 49 years 66 - 139 mg/dL
50 - 59 years 75 - 163 mg/dL
60 - 69 years 78 - 158 mg/dL
> 70 years 83 - 141 mg/dL
Liver Function Tests Tests include bilirubin (total), phosphatase (alkaline), protein (total and albumin), transaminases (alanine and aspartate), prothrombin (PTT)
Magnesium 1.5 - 2.0 mEq/L
Mean Corpuscular Hemoglobin (MCH) 27 - 32 pg/cell
Mean Corpuscular Hemoglobin Concentration (MCHC) 32 - 36% hemoglobin/cell
Mean Corpuscular Volume (MCV) 76 - 100 cu µm
Osmolality 280 - 296 mOsm/kg water
Oxygen Pressure 83 - 100 mm Hg
Oxygen Saturation (arterial) 96 - 100%
Phosphatase, Prostatic 0 - 3 units/dL (Bodansky units) (acid)
Phosphatase 50 - 160 units/L (normally higher in infants and adolescents) (alkaline)
Phosphorus 3.0 - 4.5 mg/dL (inorganic)
Platelet Count 150,000 - 350,000/mL
Potassium 3.5 - 5.0 mEq/L
Prostate-Specific Antigen (PSA) 0 - 4 ng/mL (likely higher with age)
Proteins:
Total 6.0 - 8.4 gm/dL
Albumin 3.5 - 5.0 gm/dL
Globulin 2.3 - 3.5 gm/dL
Prothrombin (PTT) 25 - 41 sec
Pyruvic Acid 0.3 - 0.9 mg/dL
Red Blood Cell Count (RBC) 4.2 - 6.9 million/µL/cu mm
Sodium 135 - 145 mEq/L
Thyroid-Stimulating Hormone (TSH) 0.5 - 6.0 µ units/mL
Transaminase:
Alanine (ALT) 1 - 21 units/L
Aspartate (AST) 7 - 27 units/L
Urea Nitrogen (BUN) 7 - 18 mg/dL
BUN/Creatinine Ratio 5 - 35
Uric Acid Male 2.1 to 8.5 mg/dL (likely higher with age)
Female 2.0 to 7.0 mg/dL (likely higher with age)
Vitamin A 30 - 65 µg/dL
White Blood Cell Count (WBC) 4,300 - 10,800 cells/µL/cu mm
Below is an example of how to read the results of a Blood Test.
Glucose - This is a measure of the sugar level in your blood. High values are associated with eating before the test, and diabetes.
The normal range for a fasting glucose is 60 -109 mg/dl. According the the 1999 ADA criteria, diabetes is diagnosed with a *fasting* plasma glucose of 126 or more. A precursor, Impaired Fasting Glucose (IFG) is defined as reading of fasting glucose levels of 110 - 125. Sometimes a glucose tolerance test, which involves giving you a sugary drink followed by several blood glucose tests, is necessary to properly sort out normal from IFG from diabetes.
Electrolytes: These are your potassium, sodium, chloride, and CO2 levels.
Potassium is controlled very carefully by the kidneys. It is important for the proper functioning of the nerves and muscles, particularly the heart. Any value outside the expected range, high or low, requires medical evaluation. This is especially important if you are taking a diuretic (water pill) or heart pill (Digitalis, Lanoxin, etc.).
Sodium is also regulated by the kidneys and adrenal glands. There are numerous causes of high and low sodium levels, but the most common causes of low sodium are diuretic usage, diabetes drugs like chlorpropamide, and excessive water intake in patients with heart or liver disease.
CO2 reflects the acid status of your blood. Low CO2 levels can be due to either to increased acidity from uncontrolled diabetes, kidney disease, metabolic disorders, or low CO2 can be due to chronic hyperventilation.
Waste products:
Blood Urea Nitrogen (BUN) is a waste product produced in the liver and excreted by the kidneys. High values may mean that the kidneys are not working as well as they should. BUN is also affected by high protein diets and/or strenuous exercise which raise levels, and by pregnancy which lowers it.
Creatinine is a waste product largely from muscle breakdown. High values, especially with high BUN levels, may indicate problems with the kidneys..
Uric Acid is normally excreted in urine. High values are associated with gout, arthritis, kidney problems and the use of some diuretics.
Enzymes
AST, ALT, SGOT, SGPT, and GGT and Alkaline Phosphatase are abbreviations for proteins called enzymes which help all the chemical activities within cells to take place. Injury to cells release these enzymes into the blood. They are found in muscles, the liver and heart. Damage from alcohol and a number of diseases are reflected in high values.
Alkaline phosphatase is an enzyme found primarily in bones and the liver. Expected values are higher for those who are growing (children and pregnant women) or when damage to bones or liver has occurred or with gallstones. Low values are probably not significant.
GGT is also elevated in liver disease, particularly with obstruction of bile ducts. Unlike the alkaline phosphatase it is not elevated with bone growth or damage.
AST/SGOT , ALT/ SGPT are also liver and muscle enzymes. They may be elevated from liver problems, hepatitis, excess alcohol ingestion, muscle injury and recent heart attack.
LDH is the enzyme present in all the cells in the body. Anything which damages cells, including blood drawing itself, will raise amounts in the blood. If blood is not processed promptly and properly, high levels may occur. If all values except LDH are within expected ranges, it is probably a processing error and does not require further evaluation.
Bilirubin is a pigment removed from the blood by the liver. Low values are of no concern. If slightly elevated above the expected ranges, but with all other enzymes (LDH, GOT, GPT, GGT) within expected values, it is probably a condition known as Gilbert’s syndrome and is not significant
CPK is an enzyme which is very useful for diagnosing diseases of the heart and skeletal muscle. This enzyme is the first to be elevated after a heart attack (3 to 4 hours). If CPK is high in the absence of heart muscle injury, this is a strong indication of skeletal muscle disease.
Proteins
Albumin and Globulin measure the amount and type of protein in your blood. They are a general index of overall health and nutrition. Globulin is the "antibody" protein important for fighting disease.
A/G Ratio is the mathematical relationship between the above.
Blood Fats
Cholesterol is a fat-like substance in the blood which, if elevated has been associated with heart disease.
Total Cholesterol - A high cholesterol in the blood is a major risk factor for heart and blood vessel disease. Cholesterol in itself is not all bad, in fact, our bodies need a certain amount of this substance to function properly. However, when the level gets too high, vascular disease can result. A total cholesterol of less than 200, and an LDL Cholesterol of 100 or less is considered optimal by the National Heart, Lung, and Blood Institute. The levels that your doctor will recommend depend upon whether you are at high risk for cardiovascular disease.
As the level of blood cholesterol increases, so does the possibility of plugging the arteries due to cholesterol plaque build-up. Such a disease process is called "hardening of the arteries" or atherosclerosis. When the arteries feeding the heart become plugged, a heart attack may occur. If the arteries that go to the brain are affected, then the result is a stroke.
There are three major kinds of cholesterol, High Density Lipoprotein (HDL) , Low Density Lipoprotein (LDL), and Very Low Density Lipoprotein (VLDL).
LDL Cholesterol is considered "bad cholesterol" because cholesterol deposits form in the arteries when LDL levels are high. An LDL level of less than 130 is recommended, 100 is optimal, values greater than 160 are considered high risk and should be followed up by your physician. Those persons who have established coronary or vascular disease may be instructed by their doctor to get their LDL Cholesterol well below 100. You should ask your doctor which LDL target he or she wants for you. There are two ways to report LDL. The most common is simply an estimate calculated from the Total Cholesterol, HDL, and triglycerides results. This may say "LDL Calc" . A directly measured LDL Cholesterol is usually more accurate, but more expensive and may require that your doctor specify the direct LDL.
HDL cholesterol is a ‘good cholesterol’ as it protects against heart disease by helping remove excess cholesterol deposited in the arteries. High levels seem to be associated with low incidence of coronary heart disease.
Triglyceride is fat in the blood which, if elevated, has been associated with heart disease, especially if over 500 mg. High triglycerides are also associated with pancreatitis. Triglyceride levels over 150 mg/dl may be associated with problems other than heart disease. Ways to lower triglycerides: 1) weight reduction, if overweight; 2) reduce animal fats in the diet: eat more fish; 3) take certain medications your physician can prescribe; 4) get regular aerobic exercise; 5) decrease alcohol and sugar consumption—alcohol and sugar are not fats, but the body can convert them into fats then dump those fats into your blood stream 6) restrict calories - carbohydrates are converted to triglycerides when eaten to excess.
VLDL (very low density lipoprotein) is another carrier of fat in the blood.
Cardiac Risk Factors
C Reactive Protein (CRP) - This is a marker for inflammation. Traditionally it has been used to assess inflammation in response to infection. However we use a highly sensitive C Reactive Protein which is useful in predicting vascular disease, heart attack or stroke.. The best treatment for a high C reactive protein level has not yet been defined, however statin drugs, niacin, weight loss, quitting smoking, and exercise all appear to improve C- Reactive Protein
Homocysteine - Homocysteine is an amino acid that is normally found in small amounts in the blood. Higher levels are associated with increased risk of heart attack and other vascular diseases. Homocysteine levels may be high due to a deficiency of folic acid or Vitamin B12, due to heredity, older age, kidney disease, or certain medications. Men tend to have higher levels. Our lab normals are 4 - 15 micromole/l , but if you have had previous vascular disease we may recommend medications to reduce it below 10. You can reduce your homocysteine level by eating more green leafy vegetables and fortified grain products or cereals. The usual treatment is folic acid with or without Vitamin B-12.
Lipoprotein (a) or Lp(a) - Elevated lipoprotein(a) (Lp) concentrations are associated with premature coronary heart disease (CHD). The exact mechanism is not yet clear, but it appears that there is a strong genetic component to elevated Lp(a) levels that correlates with coronary disease. Persons with diabetes and a high Lp(a) level appear to be at increased risk of asymptomatic coronary disease.
Minerals
Calcium is controlled in the blood by the parathyroid glands and the kidneys. Calcium is found mostly in bone and is important for proper blood clotting, nerve, and cell activity. An elevated calcium can be due to medications such as thiazide type diuretics, inherited disorders of calcium handling in the kidneys, or excess parathyroid gland activity or vitamin D. Low calcium can be due to certain metabolic disorders such as insufficient parathyroid hormone; or drugs like Fosamax or furosemide type diuretics.
Calcium is bound to albumin in the blood, so a low albumin level will cause the total calcium level in the blood to drop. You doctor can easily determine if this is significant or not.
Phosphorus is also largely stored in the bone. It is regulated by the kidneys, and high levels may be due to kidney disease. When low levels are seen with high calcium levels it suggests parathyroid disease, however there are other causes. A low phosphorus, in combination with a high calcium, may suggest an overactive parathyroid gland.
Thyroid
There are 2 types of thyroid hormones easily measurable in the blood, thyroxine (T4) and triiodothyronine (t3). For technical reasons, it is easier and less expensive to measure the T4 level, so T3 is usually not measured on screening tests.
Thyroxine (T4) - This shows the total amount of the T4. High levels may be due to hyperthyroidism, however technical artifact occurs when estrogen levels are higher from pregnancy, birth control pills or estrogen replacement therapy. A Free T4 (see below) can avoid this interference.
T3 Resin Uptake or Thyroid Uptake - This is a test that confuses doctors, nurses, and patients. First, this is not a thyroid test, but a test on the proteins that carry thyroid around in your blood stream. Not only that, a high test number may indicate a low level of the protein! The method of reporting varies from lab to lab. The proper use of the test is to compute the free thyroxine index.
Free Thyroxine Index (FTI or T7) - A mathematical computation allows the lab to estimate the free thyroxine index from the T4 and T3 Uptake tests. The results tell us how much thyroid hormone is free in the blood stream to work on the body. Unlike the T4 alone, it is not affected by estrogen levels.
Free T4 - This test directly measures the free T4 in the blood rather than estimating it like the FTI. It is a more reliable , but a little more expensive test. Some labs now do the Free T4 routinely rather than the Total T4.
Total T3 - This is usually not ordered as a screening test, but rather when thyroid disease is being evaluated. T3 is the more potent and shorter lived version of thyroid hormone. Some people with high thyroid levels secrete more T3 than T4. In these (overactive) hyperthyroid cases the T4 can be normal, the T3 high, and the TSH low. The Total T3 reports the total amount of T3 in the bloodstream, including T3 bound to carrier proteins plus freely circulating T3.
Free T3 - This test measures only the portion of thyroid hormone T3 that is "free", that is, not bound to carrier proteins.
Thyroid Stimulating Hormone (TSH) - This protein hormone is secreted by the pituitary gland and regulates the thyroid gland. A high level suggests your thyroid is underactive, and a low level suggests your thyroid is overactive.
Glycohemoglobin (Hemoglobin A1 or A1c, HbA1c) - Glycohemoglobin measures the amount of glucose chemically attached to your red blood cells. Since blood cells live about 3 months, it tells us your average glucose for the last 6 - 8 weeks. A high level suggests poor diabetes control. Standardization for glycohemoglobin from lab to lab is poor, and you cannot compare a test from different labs unless you can verify the technique for measuring glycohemoglobin is the same. The only exception is if your lab is standardized to the national DCCT referenced method. You can ask your lab if they use a DCCT referenced method.
Hormones
Insulin - Insulin is secreted by the pancreas in response to eating or elevated blood sugar. It is deficient in persons with type 1 diabetes, and present at insufficient levels in persons with type 2 diabetes. The natural evolution of type 2 diabetes causes insulin levels to fall from high levels to low levels over a course of years. Thus insulin levels in persons with type 1 and type 2 diabetes overlap significantly, and insulin levels are not very useful in determining type 1 vs type 2. Insulin levels vary widely from person to person depending upon an individuals insulin sensitivity (or conversely, their insulin resistance.) Insulin levels also vary widely according to when the last meal occurred. Insulin resistance is a risk factor for coronary disease, thus assessing an individual's insulin resistance may have some value using the HOMA-IR calculation. Insulin levels are also elevated in patients with true hypoglycemia, however the interpretation of these levels is difficult. Insulin levels, when measured by itself at a random time is rarely useful.
C-peptide - This is a fragment cleaved off of the precursor of insulin (pro-insulin) when insulin is manufactured in the pancreas. C-peptide levels usually correlate with the insulin levels, except when people take insulin injections. When a patient is hypoglycemic, this test may be useful to determine whether high insulin levels are due to excessive pancreatic release of insulin, or from an injection of insulin.
Estradiol - This is the most commonly measured type of estrogen measured. In women it varies according to their age, and whether they are having normal menstrual cycles. Hormone levels are also changed when taking birth control pills or estrogen replacement.
Complete Blood Count (CBC) - The CBC typically has several parameters that are created from an automated cell counter. These are the most relevant:
White Blood Count (WBC) - This is the number of white cells. High WBC can be a sign of infection. WBC is also increased in certain types of leukemia. Low white counts can be a sign of bone marrow diseases or an enlarged spleen. Low WBC is also found in HIV infection in some cases. (ed. note: The vast majority of low WBC counts in our population is NOT HIV related.)
Hemoglobin (Hgb) and Hematocrit (Hct) - The hemoglobin is the amount of oxygen carrying protein contained within the red blood cells. The hematocrit is the percentage of the blood volume occupied by red blood cells. In most labs the Hgb is actually measured, while the Hct is computed using the RBC measurement and the MCV measurement. Thus purists prefer to use the Hgb measurement as more reliable. Low Hgb or Hct suggest an anemia. Anemia can be due to nutritional deficiencies, blood loss, destruction of blood cells internally, or failure to produce blood in the bone marrow. High Hgb can occur due to lung disease, living at high altitude, or excessive bone marrow production of blood cells.
Mean Corpuscular Volume (MCV) - This helps diagnose a cause of an anemia. Low values suggest iron deficiency, high values suggest either deficiencies of B12 or Folate, ineffective production in the bone marrow, or recent blood loss with replacement by newer (and larger) cells from the bone marrow.
Platelet Count (PLT) - This is the number of cells that plug up holes in your blood vessels and prevent bleeding. High values can occur with bleeding, cigarette smoking or excess production by the bone marrow. Low values can occur from premature destruction states such as Immune Thrombocytopenia (ITP), acute blood loss, drug effects (such as heparin) , infections with sepsis, entrapment of platelets in an enlarged spleen, or bone marrow failure from diseases such as myelofibrosis or leukemia. Low platelets also can occur from clumping of the platelets in a lavender colored tube. You may need to repeat the test with a green top tube in that case.
Urinalysis - Urine tests are typically evaluated with a reagent strip that is briefly dipped into your urine sample. The technician reads the colors of each test and compares them with a reference chart. These tests are semi-quantitative; there can be some variation from one sample to another on how the tests are scored.
pH : This is a measure of acidity for your urine.
Specific Gravity (SG) : This measures how dilute your urine is. Water would have a SG of 1.000 . Most urine is around 1.010, but it can vary greatly depending on when you drank fluids last, or if you are dehydrated.
Glucose: Normally there is no glucose in urine. A positive glucose occurs in diabetes. There are a small number of people that have glucose in their urine with normal blood glucose levels, however any glucose in the urine would raise the possibility of diabetes or glucose intolerance.
Protein: Normally there is no protein detectable on a urinalysis strip. Protein can indicate kidney damage, blood in the urine, or an infection. Up to 10% of children can have protein in their urine. Certain diseases require the use of a special, more sensitive (and more expensive) test for protein called a microalbumin test. A microalbumin test is very useful in screening for early damage to the kidneys from diabetes, for instance.
Blood: Normally there is no blood in the urine. Blood can indicate an infection, kidney stones, trauma, or bleeding from a bladder or kidney tumor. The technician may indicate whether it is hemolyzed (dissolved blood) or non-hemolyzed (intact red blood cells). Rarely, muscle injury can cause myoglobin to appear in the urine which also causes the reagent pad to falsely indicate blood.
Bilirubin: Normally there is no bilirubin or urobilinogen in the urine. These are pigments that are cleared by the liver. In liver or gallbladder disease they may appear in the urine as well.
Nitrate: Normally negative, this usually indicates a urinary tract infection.
Leukocyte esterase: Normally negative. Leukocytes are the white blood cells (or pus cells). This looks for white blood cells by reacting with an enzyme in the white cells. White blood cells in the urine suggests a urinary tract infection.
Sediment: Here the lab tech looks under a microscope at a portion of your urine that has been spun in a centrifuge. Items such as mucous and squamous cells are commonly seen. Abnormal findings would include more than 0-2 red blood cells, more than 0-2 white blood cells, crystals, casts , renal tubular cells or bacteria. (Bacteria can be present if there was contamination at the time of collection.)
0 notes
Text
New onset acute promyelocytic Leukemia during pregnancy: report of 2 cases.
Related Articles
New onset acute promyelocytic Leukemia during pregnancy: report of 2 cases.
Cancer Biol Ther. 2018 Nov 19;:1-5
Authors: Li H, Han C, Li K, Li J, Wang Y, Xue F
Abstract
Acute promyelocytic leukemia (APL) is one of the most fatal hematological malignancies. APL during pregnancy is a rare comorbidity and can lead to adverse outcomes, such as maternal and/or fetal death, without timely and appropriate management. Medical management for APL during pregnancy remains challenging. We reported 2 patients with no regular prenatal visits who were diagnosed with APL during pregnancy. One presented with typical hematological abnormalities related to infection, while the other presented with intracranial hemorrhage, which is rare. Although supportive measures and chemotherapy were administered after APL was diagnosed, these two patients had completely different outcomes. The pregnancy outcomes of APL patients depend greatly on the timely diagnosis and appropriate management of the disease. Physicians should pay more attention to APL during pregnancy and thus may save more maternal and fetal lives. Further study of the management of APL during pregnancy is warranted. Abbreviations: AML: acute myeloid leukemia; APL: acute promyelocytic leukemia; WBC: white blood cell; RBC: red blood cell; Hb: hemoglobin; PT: prothrombin time; TT: thrombin time; APTT: activated partial thromboplastin time; TP: total protein; ALB: albumin; AST: aspartate transaminase; ALT: alanine aminotransferase; LDH: lactate dehydrogenase; ATRA: all-trans retinoic acid; ICH: intracranial hemorrhage; DIC: disseminated intravascular coagulation.
PMID: 30453810 [PubMed - as supplied by publisher]
https://ift.tt/2Fx1vDZ
0 notes
Text
Non-Operatively Managed Primary Small Bowel Volvulus: A Case Report by Ewnte B*

Abstract
Background: Primary small intestinal volvulus is one of the common causes of intestinal obstruction in various localities of the developing world. Although operative intervention has been the usual mode of treatment; this case report depicts meticulous follow-up & care, there is a possibility for relief of obstruction with non-operative management.
Case presentation: this is a case report of a 20-year-old male patient presented with crampy abdominal pain and frequent bilious vomiting. Plain abdominal film showed multiple distended small bowel loops with air fluid level, consistent with small bowel obstruction. Ruling out other etiologies primary small bowel volvulus was entertained and naso-gastric tube inserted, patient catheterized and kept nil per oral. After 48 hours of admission all symptoms resolved the patient resumed feeding and was discharged home.
Conclusions: The reported case shows evidence in which the patient’s primary small bowel volvulus was relieved non-operatively with insertion of naso gastric tube keeping nil per oral.
Key words: Small bowel volvulus; Primary volvulus; Non-operative management
Abbreviations: BPM: Beats Per Minute; WBC: White Blood Cells; RBC: Red Blood Cells; HGB: Hemoglobin; HCT: Hematocrit; MCV: Mean Corpuscular Volume; BUN: Blood Urea Nitrogen; ALT: Alanine Aminotransferase; AST: Aspartate Aminotransferase; ALP: Alkaline Phosphatase
Introduction
Small bowel volvulus is a condition in which there is a torsion of all or a segment of the small bowel and its mesentery: this can lead to bowel obstruction, ischemia, infarction, or perforation. The typical patient with the primary volvulus of the small intestine was found to be a young adult, male, muscular, farmer, from a rural area whose diet was bulky and mainly made of cereals [1,2].
Case Presentation
A 20-year-old male patient presented to Nefas Mewcha primary hospital Emergency department in January 2020 with the main complaint of crampy abdominal pain and distention of 14 hours duration. Associated with this, he also had nausea and frequent bilious vomiting eight times. He had passed feces 24 hours ago. He had no fever, cough, chest pain or night sweating. He had no history of similar illness before, no history of previous abdominal surgery.
He is not married and claims to be not sexually active. Lives with his parents and has three sisters and two brothers. He makes a living as a farmer. There are no medical illnesses that run in the family. There was no history of tobacco smoking or substance abuse. He consumes a local alcohol made of sorghum occasionally.
At presentation, his blood pressure was 105/60 mm Hg, pulse rate was 68 Beats Per Minute (BPM), respiratory rate was 18 per minute and temperature was 36.2 oC axillary. Physical examination of the patient at presentation, the patient was acutely sick looking in pain; not in cardio respiratory distress. He had a dry tongue and buccal mucosa. No palpable lymph adenopathy in all accessible areas. Chest was clear and resonant. S1 and S2 cardiac sounds were well heard and there were no added cardiac sounds. Abdomen was slightly distended, moves with respiration, flanks were full, there were no scars, no distended veins and hernia sites were free. Palpation revealed a tense abdomen with no area of tenderness, no shifting dullness, hyperactive tympanic percussion note, bowel sounds were 35 per minute. There is scanty stool on the examining finger, with no blood on it from digital rectal examination, no palpable mass was detected. The patient was conscious and neurological examination was intact.
A complete blood count of our patient showed: White Blood Cells (WBC) 12500 mcL, Red Blood Cells (RBC) 4.6 mcL, Hemoglobin (HGB) 16 gm/dL, Hematocrit (HCT) 48%, Mean Corpuscular Volume (MCV) 89.1fL, platelets 470×103, creatinine 0.6, Blood Urea Nitrogen (BUN) 30, Alanine Aminotransferase (ALT) 28, Aspartate Aminotransferase (AST) 24, Alkaline Phosphatase (ALP) 48, albumin 4.3, total bilirubin 1.1 and direct bilirubin 0.4.
Plain abdominal X-Ray showed centrally distributed, distended small bowel loops and rectal gas shadow (Figure 1). CT scan is not available at this setup so it was not possible to do one.
Management and Outcomes
The diagnosis of acute abdomen secondary to small bowel obstruction secondary to primary small bowel volvulus plus stage I shock was entertained, Double intravenous line was inserted and Trans-urethral catheter inserted, Naso-gastric tube was inserted. Three Liters of normal saline was given over a course of 2 hours, at emergency department. The patient was admitted to the ward and was advised on the possible options of management, consented on conservative management, associated risks and the possibility of surgical intervention at any time in the course of the management. The patient was kept Nil per oral, put on maintenance fluid and replacement of ongoing losses. Nasogastric tubes produced 600 ml of bilious content during the first 6 hours; which was replaced with an equal amount of ringer lactate. The abdominal cramp subsided after 4 hours of inpatient admission. After 12 hours of admission, the Blood pressure was 100/70 mmHg, pulse rate 68 per minute and the abdominal distension decreased significantly and the bowel sounds were 26 per minute, there was no area of tenderness and the patient passed flatus.
Following 24 hours of admission, the patient passed feces and vital signs were within normal range. Naso-gastric was removed and the patient was initiated with sips. The patient tolerated sips very well and was observed for 24 more hours and discharged on the next day. He was appointed to the surgical referral clinic after a week.
In subsequent weeks, the patient was seen at a referral clinic; he had no change in bowel habit or any other complaint. His vital signs were stable and physical examination was detected with no abnormality. He has been followed every month for 3 consecutive months and has reported no recurrence of symptoms.
Discussion
Volvulus is the Latin word for rolled up or twisted and is derived from the verb ‘volvere’, meaning to roll or turnabout. By definition, volvulus is an abnormal twisting of the intestine, which can impair the blood flow to the intestine. Volvulus can lead to gangrene and death of that segment of the gastrointestinal tract, intestinal obstruction, perforation of the intestine and peritonitis [3]. Small intestinal volvulus in adults can be classified as primary or secondary. In the former there is no obvious anatomical cause involving the mesentery or the small bowel, whereas in the latter there is an abnormal fixation due to adhesions or bands leading to the twisting of the mesentery. The primary type is often seen in Africa and Asia [4]. It is a significant cause of primary bowel obstruction in sub-Saharan Africa [5]. It is the leading cause of small bowel obstruction in Ethiopia [6].It is a rare entity in Western adults [7].
Clinical signs & symptoms were unspecific & resembled intestinal obstruction [8]. The most frequent symptom was observed to be sudden abdominal pain [9]. Vomiting was also observed in most of the patients while abdominal distention and constipation were reported less frequently [10]. Clinical examination reveals abdominal distension and/or diffuse tenderness with or without signs of peritonitis [8]. Small bowel volvulus is a rare but life-threatening surgical emergency. Owing to its rarity, it is seldom entertained as a differential for small bowel obstruction [11].
One of the challenges in managing primary small bowel volvulus operatively has been the risk of subsequent adhesion obstructions. The risk of occurrence of adhesion obstructions among patients that underwent laparotomy in general was reported to be 4.6% [12]. This gives rise to the endless circle of obstruction and subsequent operation, which further increase the risk more.
This case report presents a case of primary small bowel volvulus causing small bowel obstruction; which was managed non-operatively. Treatment of primary volvulus has mostly been via surgical intervention. This report depicts with close follow-up and Naso-gastric tube decompression, primary small bowel volvulus can also be treated without surgical intervention.
In the course of managing patients with primary small bowel volvulus, spontaneous resolutions has been observed [3]. This is because of natural de-rotation of the volvulus segment and relief of the obstruction. The case reported presented with symptoms and signs of small bowel obstruction. The patient has frequent vomiting with severe abdominal cramp associated with mild abdominal distension. The vital signs were within normal range supporting the diagnosis of non-ischemic obstruction. Abdominal x-ray showed multiple air fluid levels, which confirmed the diagnosis of small bowel obstruction. Ruling out other causes and considering the epidemiological prevalence, primary small bowel volvulus was entertained as a cause of obstruction.
As per the request of the patient to be followed conservatively, the patient was managed non-operatively with insertion of naso gastric tube and keeping nil per oral. The patient responded well for the management and were discharged subsequently. Showed no recurrence during the follow-up period.
Conclusion
Primary Small bowel volvulus is a rare cause of small bowel obstruction. The reported case shows evidence in which the patient’s primary small bowel volvulus was relieved non-operatively with insertion of naso gastric tube keeping nil per oral.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00131/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00131.pdf
#Beats Per Minute#White Blood Cells#Red Blood Cells#Hemoglobin#Hematocrit#Mean Corpuscular Volume#Blood Urea Nitrogen#Alanine Aminotransferase#Aspartate Aminotransferase#Alkaline Phosphatase#Ewnte B*#IJCMCR#clinical studies
0 notes
Text
New onset acute promyelocytic Leukemia during pregnancy: report of 2 cases.
Related Articles
New onset acute promyelocytic Leukemia during pregnancy: report of 2 cases.
Cancer Biol Ther. 2018 Nov 19;:1-5
Authors: Li H, Han C, Li K, Li J, Wang Y, Xue F
Abstract
Acute promyelocytic leukemia (APL) is one of the most fatal hematological malignancies. APL during pregnancy is a rare comorbidity and can lead to adverse outcomes, such as maternal and/or fetal death, without timely and appropriate management. Medical management for APL during pregnancy remains challenging. We reported 2 patients with no regular prenatal visits who were diagnosed with APL during pregnancy. One presented with typical hematological abnormalities related to infection, while the other presented with intracranial hemorrhage, which is rare. Although supportive measures and chemotherapy were administered after APL was diagnosed, these two patients had completely different outcomes. The pregnancy outcomes of APL patients depend greatly on the timely diagnosis and appropriate management of the disease. Physicians should pay more attention to APL during pregnancy and thus may save more maternal and fetal lives. Further study of the management of APL during pregnancy is warranted. Abbreviations: AML: acute myeloid leukemia; APL: acute promyelocytic leukemia; WBC: white blood cell; RBC: red blood cell; Hb: hemoglobin; PT: prothrombin time; TT: thrombin time; APTT: activated partial thromboplastin time; TP: total protein; ALB: albumin; AST: aspartate transaminase; ALT: alanine aminotransferase; LDH: lactate dehydrogenase; ATRA: all-trans retinoic acid; ICH: intracranial hemorrhage; DIC: disseminated intravascular coagulation.
PMID: 30453810 [PubMed - as supplied by publisher]
https://ift.tt/2Fx1vDZ
0 notes