#symposiumgo
Text
The Recent Changes In Medical Coding And Its Effect In Your Practice
Introduction
As technology became more reliant in the healthcare industry, medical coding has developed into a crucial part of it. Medical practitioners as well as insurance companies have grown contingent to medical coding with each passing improvement.
The coding process originated in the 17th century England has today advanced into a systematic procedure in the industry.

What is Medical Coding?
Medical coding principally translates healthcare record, diagnosis, reports, medical services and systems into specific alphanumeric codes.
It is centrally the process of translating extensive medical data and services into efficient and uncomplicated codes. Daily, numerous patients visit the hospital, and with each visit the data multiplies several folds, making it a lengthy process for medical practitioners to evaluate.
Medical coding helps in the assessment of records by generating appropriate codes and labels mitigating the daily burden of billers and coders. It is essential for medical coders to translate and update the codes correctly to make the billing procedure free of any errors.
These codes, later on, help in claiming reimbursements during billing by the hospitals which benefits both the patient and the doctor. Therefore, due to the recent overhaul in the industry, every hospital is in acute need of a medical coder.
Medical Coders- The new foundation in Healthcare
Translating all the patient records into codes is not an easy job in healthcare. A certified Medical coder must work well with numbers, computer systems, and various software programs. He can work in hospitals, clinics, urgent care facilities, nursing homes, treatment centers, etc.
The coder first takes the medical charts and records from the doctors and read the patients' reports. After reading and understanding the procedures, they assign codes, feed data in the computer and finally translate the records for an enhanced coding and billing system. It is important to decipher the data accurately as any change in a minuscule code can result in an erroneous judgment during a medical procedure.
A medical coder plays a vital role in the reimbursement process. After giving required services to a patient, medical practitioners or hospitals need to be reimbursed by the insurance companies. The codes of services and facilities provided by medical coders help the doctors claim their reimbursements.
Why is medical coding the next best thing?
With each patient visit, there exist at least 2-3 set of records and documentation. These records can get as descriptive as the visits increase. And to decode such intricate reports, certified medical coders are a must.
In the years to come, the rate of hospital visits will cross over 6 billion visits a year which directly indicates a hike in the proportion of patient data. These complex data need to be converted into simple terms for medical practitioners, billers and insurance companies to understand. Medical coding helps the practitioners to follow the previous visit's data. It includes the necessary treatment, kinds of symptoms a patient has or any other detailed analysis helpful in the diagnosis of a patient.
These codes make communication with the doctor easy by providing the documentation and comprehensive patient data into an easy to understand the coding system.
Commercial payers like insurance companies, Medicare and Medicaid use these codes while paying a claim.
It is indispensable to submit and communicate appropriate codes because these organizations can even refuse to pay if these codes are in any way inappropriate or erroneous. The common language is too vague for the insurance companies to know what type of reimbursement they have to pay.
The coding and billing system helps the companies segment their payment options easily. The insurance companies use these codes in eliminating the fraudulent claims or any other errors in payments.
Big changes ahead in medical coding
CMS administrator, Seema Verma, in the proposed rule has manifested the patient over paperwork initiative. The recent changes in the various codes and modifiers only corroborate with what the CMS's agenda was.
1. E/M changes
a- The key change made in the E/M visits is the use of time basis or the decision making capability of the practitioner rather than the 1995 or 1997 guidelines. This change has made the E/M visits less papery and strenuous for the coders.
b- E/M codes are part of the CPT codes which holds a prominent position while translating the records in the codes.
2. Additions in CPT codes
a- From 1st, January 2019 the new CPT (Current Procedural Terminology) codes have come into effect. CMS has deleted 72 codes, added 164 new codes and revised 49 codes in the latest rule.
b- Category II codes, under surgery –Integumentary, Pathology and the Medicine section has testified the highest revisions in the updated codes.
c- In the 2019 updates, CPTs 99446, 99447, 99448 and 99449 are now covered for Medicare patients.
3. Latest ICD-10 CM revisions
a- ICD-10 CM codes are effective from October 1, 2018, through September 31, 2019, with various revisions, additions, and deletions.
b- The latest updates include 279 new codes, 51 deleted codes, and 143 revised codes. A total of 71,932 active codes have been recorded with the most recent CMS revisions.
c- Chapters 1, 3 and 8 witnessed no new changes whereas chapter 2,7,11,14,15,16 and 19 went through the highest changes.
4. HCPCS codes overhaul
a- CMS has also changed HCPCS codes Q9994, effective December 3, 2018.
b- The HCPCS code B4105 is changed from D "Special Coverage Instructions Apply" to C "Contractor Discretion. Code B4105 replaces code Q9994 effective for claims with dates of service on or after January 1, 2019.
With the latest live Healthcare Webinar, SymposiumGo is bringing you all the latest updates related to the latest changes in the coding environment as well as other healthcare topics.
#coding and billing#coders and billers#medical coding and billing#healthcare compliance webinars#healthcare live webinars#hipaa compliance#symposiumgo
1 note
·
View note
Text
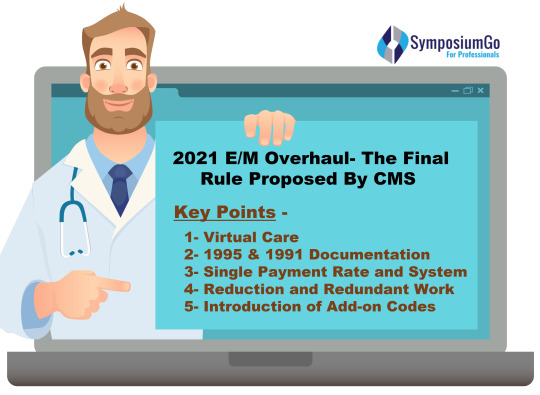
Final Rule on E/M Services - What CMS Changes Mean for your practice?
On July 27, 2018, the Centers for Medicare & Medicaid Services (CMS) released a proposed Rule ‘CMS-1693-P’ with an aim to lower the cost of American Healthcare System. The reformed guidelines modified the documentation timing by using the latest Current Procedural Terminology (CPT) code requirements by the American Medical Association (AMA).
The most imperative refurbishments have been made to the Evaluation and Management (E&M) services as well as telemedicine reimbursement.
Evaluation and management services are used by various healthcare providers for medical coding in support of medical billing. In the healthcare industry, reimbursement by Medicare, Medicaid programs, or private insurance for patient encounters is done by using these guidelines only.
CMS is proposing various changes in the coding and billing process of E/M Guidelines. In the healthcare industry, these guidelines have not been updated since the last 20 years. But preceding July, CMS proposed a dramatic overhaul in the system.
The reformation done will make the payment system in the industry more transparent with an undertaking to make it easier for patients as well as physicians. The recommended implementations by CMS will chiefly update Medical Decision-Making (MDM), Physician Fee Schedule (PFS) and calendar-year 2019 Quality Payment Program (QPP).
Although a two-year window has been given for 2019-20, the proposed final rule has already started to reduce the burden of patients as well as the physician. The aim is to replace the existing 5 tier system into one single uncomplicated payment system and to lower the complex documentation procedure.
Pre-CMS Overhaul And The Reasons Behind The Proposed Refurbishment
For more than two decades, physicians have struggled with unnecessary paperwork and overcomplicated regulatory requirements. With each patient visit, the Evaluation and management documentation process had become a burdensome process for the billers and coders. The necessity of a change in the recording of E/M visits was simmering for a long time in the healthcare industry.
Multiple visits of patients in a day were re-documented which created redundant paperwork and deviated decision-making process of medical practitioners. It was hard for physicians to focus on the patient and give them the proper time they needed.
The Quality Payment Program (QPP) has also faced excessive regulations with minimal technology-based service evaluation. High-Quality patient care was much needed in the virtual care of the patient. Restructuring both Merit-based Incentive Payment System (MIPS) and Average Sales Price (ASP) was required to reduce provider reimbursement rates for new drugs under Medicare.
Post CMS Overhaul
On November 1st of 2018, CMS published the final rule reforming important guidelines followed during EM visits. The 2379 pages overhaul has taken a giant leap forward in the following topics:-
1. Virtual Care
CMS has made a colossal change in the method of “check-ins” with doctors. With the introduction of virtual care, they have made the interaction between doctors and patients less time-taking. The new rule will provide technology-based communication services in exchange of classified videos/images. This will save patients the time to travel and visits doctors’ office. CMS is taking the services to next level by proposing telemedicine services with online payments and communication.
2. 1995 &1997 Documentation
A long-awaited change also took place in the previous year’s final rule. The Medicare billing of the E/M office and outpatient visits either uses the 1995 or 1997 E/M guidelines documentation. But after the overhaul, regardless of the level of history, physicians could choose the documentation of an E/M visit by time or their decision making authority.
3. Single Payment Rate And System
After the refurbishment, CMS has reduced the payment variation by proposing a single payment rate system. The proposed method includes both new patients’ visits (99202-99205) as well as established patients’ visit (99212-99215). The decision affirms one rate for payment of level one patients and a different payment rate for level 2-5.
The documentation requirements for level 2 will cover the documentation for all the levels from 2 through 5. Unless the time factor is used to document the services, the documentation requirements (history, examination, and medical decision-making) will be the same.
4. Reduction In Redundant Work
From 2021, the rule of two separate billing of E/M visits of a minor procedure scheduled at the same day will be eliminated. E/M payment will be reduced by 50% of the least expensive procedure. This will reduce the revenue of the practitioners but will benefit patients. CMS is proposing telemedicine services with online payments and communication to alleviate the burden of patients.
5. Introduction of Add-on codes
In office and outpatient E/M levels 2-4 where a patient requires complex care, the rule has introduced add-on HCPCS Level II codes. This will eliminate the new per visit document requirements in providers’ reimbursement. For complex care patients, a new add-on G code will be billed with the primary code to adjust the additional costs used in level 2-5.
For primary care, the add-on amount would be $5, and for approved specialties above the E&M level 2-5, $14 would be accepted.
These E/M changes are going to impact the healthcare industry at large. And to help you update your practice with these changes, our healthcare webinar will assist you in becoming versed in all the upcoming revisions. SymposiumGo will provide you with numerous essential webinars which will aid you to achieve the next level in your practice.
#emguidelinesupdates2021#emguidelines-updates-2019#lynn-anderanin#symposiumgo#hipaa-compliance#healthcare-compliance-webinars#healthcare-webinars#healthcare-live-webinars
0 notes
Link
A vast majority of patients use online reviews to either find a doctor or get assured about the same before initiating the treatment with them in the healthcare domain. Consumer reviews are one of the most distinguishing factors which entice new patient's decision about the doctor and the healthcare system.
0 notes
Link
At SymposiumGo, we have various reputed speakers to cover a range of healthcare topics including case management, HIPAA, coding & billing, CPT code update and more. We focus on delivering high-quality content to support your professional development. Please check the calendar and register for upcoming and recorded webinars.
1 note
·
View note
Link
Here at SymposiumGo, you will get insightful blog posts from the healthcare industry. Choose the topic relevant to your medical fields such as case management, HIPAA, Acute Care Case etc and update your practice with time. If you need any assistance while using our website, please contact us at [email protected]
1 note
·
View note
Link
SymposiumGo provides live webinars for professionals working in the healthcare industry. Stay updated with us and learn more in the different areas of healthcare. Check the schedule of live webinars and book accordingly. You can visit the website for more details.
1 note
·
View note
Link
At SymposiumGo, learn online with our high-quality healthcare webinars. Check out our website for the various viewpoints to examine in the healthcare sector like reimbursement, Healthcare HIPAA compliance, coding and billing updates, CPT updates and many more.
1 note
·
View note
Link
At SymposiumGo, check out the latest Live webinar - HCPCS Coding ABC’s, the key points are HCPCS, DME, Drugs, Braces, and S-codes. For more details, visit our website and attend this webinar on Aug 07, 2019. Use LI30 code to get $30 Off.
0 notes
Link
Read our blog to learn about the new medical coding 2019 changes. Topic included are - CPT and HCPCS changes, latest updates on new codes, E/M changes and a lot more about medical coding. Come and check out the latest Live Webinars on medical billing and coding at SymposiumGo.
0 notes
Link
Check out our latest blog on the buzzing topic of 3D printing in the Healthcare Industry. Read the blog to know how 3D printing has reformed the industry in its various facets. Also, learn how changing technology is changing your medical practice with each passing year. Come and enhance your professional knowledge and medical practice with SymposiumGo.
0 notes
Link
SymposiumGo blogs are updated regularly and encompass a wide range of topics in the healthcare industry. This blog focuses on the 6 Stages of Revenue Cycle Management to Make Your Hospital Financially Sound. Visit our website and read the full blog and learn how a perfect revenue cycle can make the hospital financially fit!
0 notes
Link
The recent breakthrough In CoP by CMS is all the industry is talking about. Know all the latest inside reforms for 2019 and all the outdated and updated changes in your medical practice. Visit SymposiumGo to read the full blog.
0 notes
Link
At SymposiumGo, we have prominent speakers like Lynn Anderanin. Lynn, CPPM, CPMA, CPC-I, COSC, is the Senior Director of Coding Education for Healthcare Information Services. She has over 36 years of experience in all areas of the physician practice and particularizes in Orthopedics. Lynn is currently a Workshop and Audio Presenter. She is also the founder of her Local Chapter of the AAPC. Hope to see your participation there!
0 notes
Link
Jim Sheldon-Dean, Speaker at SymposiumGo is a frequent speaker regarding HIPAA, including speaking engagements at numerous regional and national healthcare association conferences and conventions and the annual NIST/OCR HIPAA Security Conference. Read more about our speaker and his webinars.
0 notes
Link
SymposiumGo is an online training site which provides educative and constructive content filled with the latest updates, educational modules, and recent trends in the healthcare industry. Our online training program consists of Live/Recorded Webinars in the form of Transcripts and DVDs so that you manage your schedule and never miss an update. Email us at [email protected]
0 notes
Text
Why CMS Updates Are Important? Learn The Latest Changes Made In CoP Standards?
The Centers for Medicare and Medicaid updates for the new CoP standards which will come into effect in January of 2019.
Recently, there were numerous updates made by CMS in the healthcare industry. The Medicare program has updated and eliminated various reforms for a better patient care atmosphere in a hospital. Consequently, Conditions of Participation (CoP) has also been updated by CMS. The published finalized plan for the CY 2019-20 was in the limelight as Centers for Medicare and Medicaid reformed several CoP standards and regulations.
Why the CoP updates are important in healthcare?
In order to receive financial backing from the Medicare and Medicaid programs, the healthcare organizations must follow and include themselves in the CoP standards. The hospital and other associations are requisite to be in compliance with CMS and for that it mandatory for them to meet the CoP requirements.
Cop Background
CoP was first established from the consideration that various hospitals and healthcare organizations were out of reach of the Joint Commission accredited program. Therefore the Medicare legislation created a program under the federal law where hospitals and other healthcare providers can volunteer consequently. This was done to include those facilities which were still deprived of the benefits of the Medicare program.
The OCR initiates to publish the updated CoP in the federal register and then CMS publishes it in the interpretive guidelines. These changes are made in respect to the Hospital Improvement Rule, plans of care and staff policy changes by the CMS.
Conditions of Participation (CoP) standards are chiefly the rules within which an entity is governed for participating in the activities of the Medicare and Medicaid program. CoP standards are first published in the federal register, and then CMS publishes the interpretive guidelines. CMS updates CoP a few times a year regarding various alterations in surveys and certification memos. The updates are mandatory to be followed by all the nurse practitioners and other medical staff of every organization.
Over the revision, CoP has updated various steps and margins within which a registered nurse can act. The new standards also determine the detailed contributions of the nursing staff in patient care. CMS has changed the way nurses interact with the patients and it has also impacted the patient-nurse relationship profoundly.

Recent updates by CMS
The new changes in the CoP are currently affecting more than 13,000 home health agencies (HHA) under the Medicare program. If the healthcare agencies want to get reimbursed for treating Medicaid and Medicare patients, then they must consider and comprehend the new changes stated below:-
1- Updates in the facilities accredited by the Joint Commission, Health Care Facility Accreditation Program, CIHQ, and DNV Healthcare.
2- CMS has also issued the revised memos related to privacy and confidentiality, humidity, insulin pen, and practice memo.
3- Various changes have also been made to IV medications, safe injection practices, restraint reporting, soft wrist restraints as well as standing reports.
4- The proposed changes also include discharge planning, infection control worksheet, and the final worksheet on QAPI.
5- The modernized lists illustrate that Quality Assessment and Performance Improvement (QAPI) must create and follow system to plan, assess, scrutinize and regularly report the outcome data.
6- The biggest change made was in regards with the significance of updating the care plan assessment system. Earlier, the nurse practitioners would only consult the physicians and then modify the documents. But after the 2019 updates by CMS, it is a mandatory step for hospitals to update the patients’ records and the documents, whether good or bad, regularly and systematically.
The Outdated and Updated changes in Condition of Participations
1. Bulging out exhausted systems
The last time CMS updated the guidelines of CoP was more than 30 years ago. It was a much-awaited change in the healthcare industry; the reason being an exalting increase in the percentage of patients' receiving home healthcare. Therefore, the changes in the policies and regulations were implemented to serve patients with the latest medical care plan requirements and to eliminate the used-up policies from the hospital environment.
2. Incompetent use of paper-based HHA system
CMS has made it impractical today to use the paper-based system in the hospitals which were being incessantly used from the last 30 years. The efficient use of electronic health record (EHR) in the organization will be beneficial for the Nurse Practitioners together with the members of the interdisciplinary care team.
The updated alterations by CoP will help the practitioners to document, allocate, and capture the assessment information of the patients as well as the relevant drugs.
3. Need for refinement in the Patient Driven Groupings Model (PDGM)
PGDM is not new in the industry but a reformed model of Home Health Groupings Model (HHGS) which was proposed and then dropped by CMS in 2017. The latest proposed model is subjected to cut down and halves the 60-day unit program to a 30-day program which is a remarkable change made by CMS.
The object behind it was to curb the cost of care and amplify the value of care. The Medicare program has reformed interpretive guidelines for CoP by making significant changes in the model.
4. Required removal of two Outcomes and Assessment Information Set (OASIS) based measures
The program has decided to remove “influenza Immunization Received for Current Flu Season” measure and the “Pneumococcal Polysaccharide Vaccine Ever Received” measure from the Home Health Value-Based Purchasing Model.
5. Inadequate nurse staff
The main agenda behind updating cop standards besides serving patients was to ease up the burden of nurse practitioners and other medical practitioners through organized and efficient regulatory rules. A new study revealed that the shortage in nurse staffing has directly increased the patient mortality rate by 7%. Therefore, it has been estimated that by 2020, there will be increased by 80% to balance the nurse-patient ratio.
To summarize it all, the latest updates are vital for the medical practitioners as well as the related hospitals to meticulously follow and inculcate the latest CoP standards to be in compliance with the Medicare program and HIPAA.
At SymposiumGo, we cover various other topics on healthcare and also provide webinars on the subject matter. Our webinars are conducted by eminent Healthcare Speakers of the industry with decades of experience in their respective fields.
#CMS CoP Standards 2019 Nurse Practitioners Hipaa Compliance Healthcare Speakers Director of Nursing
0 notes