#rhamnogalacturonan
Text
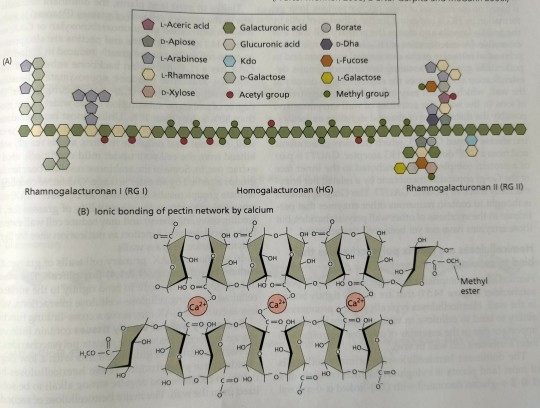
Figure 14.10 illustrates a hypothetical scheme for linkage of HG, RG I, and RG II.

"Plant Physiology and Development" int'l 6e - Taiz, L., Zeiger, E., Møller, I.M., Murphy, A.
#book quotes#plant physiology and development#nonfiction#textbook#linkage#homogalacturonan#rhamnogalacturonan#pectin#network#ionic bond#calcium#aceric acid#apiose#arabinose#rhamnose#xylose#galacturonic acid#glucuronic acid#kdo#galactose#acetyl#borate#dha#fucose#methyl
0 notes
Text
A ginseng-derived rhamnogalacturonan I (RG-I) pectin promotes longevity via TOR signalling in Caenorhabditis elegans
http://dlvr.it/SmX9Xz
0 notes
Text
10 Foods Which Will Help You To Maintain a Healthy Blood Sugar

1. Okra
Okra is a fruit that’s commonly utilized like a vegetable. It’s a rich source of blood-sugar-lowering compounds like polysaccharides and flavonoid antioxidants
In Turkey, okra seeds have long been used as a natural remedy to treat diabetes due to their potent blood-sugar-lowering properties (24Trusted Source).
Rhamnogalacturonan, the main polysaccharide in okra, has been identified as a powerful antidiabetic compound. Plus, okra contains the flavonoids isoquercitrin and quercetin 3-O-gentiobioside, which help reduce blood sugar by inhibiting certain enzymes
Although animal studies suggest that okra has powerful antidiabetic properties, human research studies are needed.
2. Chia Seeds
You might have heard that losing or managing weight is one of the best things you can do to improve your blood sugar. Chia seeds can help with that. In one study, people with diabetes who added about an ounce of chia seeds per 1,000 calories day to a calorie-controlled diet for six months shed four pounds and trimmed an inch-and-a-half from their waistlines. Aside from being packed with fiber, these gems also contain protein and provide 18 percent of your recommended daily intake of calcium.
3. Broccoli and broccoli sprouts
Sulforaphane is a type of isothiocyanate that has blood-sugar-reducing properties.
This plant chemical is produced when broccoli is chopped or chewed due to a reaction between a glucosinolate compound called glucoraphanin and the enzyme myrosinase, both of which are concentrated in broccoli (5).
Test-tube, animal, and human studies have shown that sulforaphane-rich broccoli extract has powerful antidiabetic effects, helping enhance insulin sensitivity and reduce blood sugar and markers of oxidative stress
Broccoli sprouts are concentrated sources of glucosinolates like glucoraphanin, and they’ve been shown to help promote insulin sensitivity and reduce blood sugar levels in people with type 2 diabetes when supplemented as a powder or extract
Additionally, eating cruciferous vegetables has been linked to a lower risk of type 2 diabetes
Keep in mind that the best way to enhance the availability of sulforaphane is to enjoy broccoli and broccoli sprouts raw or lightly steamed, or to add active sources of myrosinase like mustard seed powder to cooked broccoli
4. Apples
You might think that there’s no room in a diabetic meal plan for fruit, but apples are also low glycemic. Aiming for foods like apples that are low or medium on the glycemic index is one way to manage blood sugar levels. And eating an apple a day has its benefits — they are high in fiber, vitamin C as well as fat-free! Not to mention a portable and easy snack option.
5. Berries
Numerous studies have linked berry intake with improved blood sugar control. Berries are loaded with fiber, vitamins, minerals, and antioxidants, and they make an excellent choice for people with blood sugar management issues.
A 2019 study found that eating 2 cups (250 grams) of red raspberries with a high carb meal significantly reduced post-meal insulin and blood sugar in adults with prediabetes, compared with a control group
In addition to raspberries, studies have shown that strawberries, blueberries, and blackberries may benefit blood sugar management by enhancing insulin sensitivity and improving glucose clearance from the blood
6. Almonds
These crunchy nuts are rich in magnesium, a mineral that may help your body use its own insulin more effectively. Try adding more almonds into your diet to have your daily dose of this blood sugar-balancing mineral. Plus, nuts like almonds are high in monounsaturated fatty acids, protein, and fiber, which makes them a great way to help manage blood glucose levels.
7. Yogurt
Yoghurt is known because of its active and live cultures which help in the digestive issues by providing good bacteria. Whether you are eating unsweetened yoghurt or one with artificial sugars, it will still fall under low GI foods. However, low-fat yoghurt is recommended. Its glycemic index is 33. Also, it is advisable to consume natural flavoured yoghurt that is free of any type of artificial sweeteners.
8. Coconut
Coconut ranks highly in saturated fats, but if used sparingly, it is not a big threat to your blood glucose levels. Coconuts are used to flavour different types of dishes. Its different parts can be used, be it, coconut milk, coconut flour, its flesh and also coconut water. However, it’s important to know which part you are using to determine the glycemic index as well as nutritional benefits.
9. Apricots
Apricots are sweet and have a delicate flavour. They have a wide range of nutrients and this makes them worthwhile to be added to a diabetic diet. Apricots can help you satisfy your sweet tooth without worrying about your blood sugars due to their low glycemic index. Dried apricots are also a great alternative when eaten in small amounts.
10. Oranges
An orange is an excellent source of pectin, a soluble fiber that has been shown to lower LDL cholesterol levels, Smithson says. Although they’re sweet, oranges are actually low on the glycemic index (GI), according to the American Diabetes Association (ADA) and have a GL of 4, per Oregon State University.
Do factor in that one orange isn’t exactly a low-carb food, Smithson notes. It contains about 18 g of carbs, plus 72 calories, 1.45 g of protein, and less than 0.2 g of fat, according to the USDA.
Oranges provide other key nutrients, including vitamin C. Opt for the whole fruit instead of juice for more fiber and antioxidants that may help prevent cell damage, Smithson adds, as well as decrease any effect on blood sugar.
#blood sugar#blood sugar fix#how to fix blood sugar#blood sugar reduce#maintain blood sugar#healthy blood sugar
0 notes
Text
Adriamycin like a neoadjuvant adviser throughout preoperative chemoradiation with regard to rectal most cancers
This particular factor details a compressed activity to be able to ethyl trans-[(4S)-methoxy-(2S)-pyrrolidinylmethoxy]cyclohexanecarboxylate (2b) as a crucial advanced involving very past due antigen-4 (VLA-4) villain trans-4-[1-[[2,5-dichloro-4-(1-methyl-3-indolylcarboxyamide)phenyl]acetyl]-(4 spades)-methoxy-(2S)-pyrrolidinylmethoxy] cyclohexanecarboxylic acidity (A single). The actual functionality employs any reductive etherification as being a essential response making use of (2S,4S)-1-benzyloxycarbonyl-4-methoxypyrrolidine-2-carboxyaldehyde (14) and also trans-4-triethylsilyloxycyclohexanecarboxilic acid ethyl ester (13b). This kind of synthesis offers 2b inside Some steps using 38% all round produce from commercially available starting up materials.BH1115 is often a gene via Bacillus halodurans pressure C-125 which hypothetically encodes any rhamnogalacturonan acetyl esterase (RGAE) with the CE-12 family. Because verification, this kind of gene was duplicated, and the merchandise was indicated within Escherichia coli tension Rosetta (DE3) tissue and purified. The particular enzyme received had been monomeric, which has a molecular size associated with Forty-five kDa, along with shown alkaliphilic properties. Research of the inhibition in the activity by a few modulators established that this catalytic triad for that esterase exercise was Ser-His-Asp. This particular chemical in addition gifts broad substrate nature and it is productive in the direction of 7-aminocephalosporanic acid solution, cephalosporin C, p-nitrophenyl acetate, beta-naphthyl acetate, blood sugar #Link# pentaacetate, along with acetylated xylan. Furthermore, RGAE via T. halodurans achieves any synergistic impact together with xylanase The to acetylated xylan. Being a person in the particular SGNH loved ones, this doesn't take up the common alpha/beta hydrolase retract. Your homology relating to the folds involving RGAE from Aspergillus aculeatus and also the hypothetical YAM precursor from Bacillus subtilis, that the two are part of the actual SGNH family members, features the divergence of these protein from a typical ancestor. Additionally, the particular molecule carries a putative substrate holding area at the N terminus with the health proteins containing in no way already been referred to to date for any RGAE.Goals: To examine your opposition involving High-density lipoprotein contaminants for you to primary oxidation with respect towards the submitting regarding HDL allergens. Design and Methods: We researched HDL arrangement, subclass submission, as well as the kinetics associated with CuSO(4)-induced oxidation involving full High-density lipoprotein and HDL(3) within vitro in 36 low-HDL-C topics along with Forty-one manage topics using standard HDL-C. Results: Your level of resistance involving HDL3 for you to corrosion, since evaluated in the dissemination charge was significantly greater than that of complete High-density lipoprotein. The actual propagation rate along with diene creation through HDL oxidation throughout vitro was attenuated throughout HDL produced from low-HDL-C themes. Propagation price along with maximum diene creation during overall High-density lipoprotein oxidation related substantially together with HDL mean compound dimension. The reproduction rate involving overall HDL oxidation inside vitro shown an important beneficial association with HDL(Two) chemical muscle size and HDL imply chemical size simply by a number of regression studies. Conclusions: These findings spotlight that the distribution associated with High-density lipoprotein subpopulations offers #Link# essential significance for the possible of #Link# HDL being an anti-oxidant origin.
0 notes
Text
Identification of plant-parasitic nematode attractant
Scientists have purified and identified an attractant for crop-infecting root-knot nematodes from flaxseeds. Their experiments revealed that rhamnogalacturonan-I (RG-I), a flaxseed cell wall component, can attract root-knot nematodes. The linkages between rhamnose and L-galactose are essential for the attraction.
Latest Science News -- ScienceDaily https://www.sciencedaily.com/releases/2021/09/210903132639.htm
0 notes
Text
Best quinoa pasta brands
There are two or three things to pay special mind to when you're cooking sans gluten pasta. A few choices have a terrible soft surface, and others don't hold their shape and self-destruct during cooking (think: fusilli transforming into miserable worms, penne parting separated). To stay away from all that, ensure you cook utilizing a moving bubble and mix consistently to keep the pieces from remaining together. I likewise think that it’s supportive to utilize the cooking guidance time as a rule instead of a standard, and I begin tasting the pasta, in any event, three minutes sooner than prescribed to help forestall a soft result.
Visit Best quinoa pasta brands
Natural supergrain pasta made with quinoa
Taste and surface of conventional pasta
Without gluten
Low sodium and without cholesterol
Appreciate the rich nutty flavor
Old collect's natural supergrain pasta elbows - the solution to your quest for a legit pasta establishment to any dish. Our supergrain pasta draws out your innovative side with the wonderful taste, surface, and intrigue of conventional wheat noodles - without the wheat. This pasta is made from natural corn flour and quinoa flour. Every 8-ounce box of pasta is confirmed by the Non-GMO Project and altogether without gluten while being stacked with 4g of protein and dietary fiber per serving. Our pasta is Star-K fit confirmed and USDA natural, so you can be certain that what you get is the genuine article. As we've developed, antiquated grains like quinoa and heartbeats remain the establishment of all that we make. Regardless of whether you're searching for scrumptious plant-based nourishments, an organization that is established in uprightness, or a network of individuals who are attempting to change the way the world considers nourishment, you've gone to the opportune spot. Welcome to the old collect family.
Also, visit Quinoa Chips In India
Quinoa is the nourishment of high protein quality and is ordinarily viewed as a sufficient wellspring of all fundamental amino acids, including lysine and isoleucine. It gives an assortment of cancer prevention agent phytonutrients, including ferulic, coumaric, hydroxybenzoic, and vanillic corrosive. Cell reinforcement flavonoids including quercetin and kaempferol are likewise particularly copious in quinoa. Mitigating polysaccharides in quinoa incorporate arabinans and rhamnogalacturonan. Numerous individuals from the nutrient E tocopherol family are given by quinoa, including significant measures of gamma-tocopherol. Quinoa is a generally excellent wellspring of manganese. It is additionally a decent wellspring of phosphorus, copper, magnesium, dietary fiber, folate, and zinc.
Singular Concerns
Quinoa can't ordinarily allergenic nourishment and can't contain quantifiable measures of purines. Since quinoa doesn't have a place with the plant family containing wheat, oats, grain, and rye, it is likewise a sans gluten nourishment. A few investigations additionally show higher-than-anticipated edibility for quinoa, making it nourishment less inclined to deliver antagonistic responses. In any case, similar to all individuals from the Amaranthaceae-Chenopodiaceae plant family (counting spinach, chard, and beets), quinoa contains oxalates, and now and again in considerable sums. The oxalate substance of quinoa goes broadly, yet even the lower end of the oxalate run puts quinoa on the alert or evasion list for an oxalate-limited eating routine.
Developing locales
Quinoa is local to the Andes district of South America. It is developed in scope of elevations, atmospheres, and soil types. In 2013, 70 nations created quinoa.
The biggest maker of quinoa in Australia is situated in northern Tasmania. Fundamental editing preliminaries have been fruitful in the wheat-belt and Kununurra under the water system in Western Australia.
Quinoa creation is yet to be attempted in different regions of Australia.
Soil type
Quinoa flourishes in loamy soils with high natural substance and great seepage. Soils with an impartial pH are liked, be that as it may, plants can endure soluble (pH 8.5) and acidic soils (pH 4.8). The connection between soil types and harvest yield keeps on being inquired about.
#Quinoa Chia Seeds#Quinoa Grain#Quinoa Pasta#Quinoa Crisps#Quinoa Chips#Quinoa in India#quinoa Pasta in india#Quinoa Chips In india#quinoa pasta india#quinoa chips india#Quinoa Crisps In india
0 notes
Text
Structural characterization of blackberry wine polysaccharides and immunomodulatory effects on LPS-activated RAW 264.7 macrophages.
PMID: Food Chem. 2018 Aug 15 ;257:143-149. Epub 2018 Feb 24. PMID: 29622190 Abstract Title: Structural characterization of blackberry wine polysaccharides and immunomodulatory effects on LPS-activated RAW 264.7 macrophages. Abstract: Three polysaccharide fractions were isolated from blackberry wine. The crude extract BWPs was obtained with ethanol precipitation and freeze-thawing process, it was then submitted to Fehling treatment, giving soluble BWPFs and insoluble BWPFp fractions. These fractions were characterized by Gas Chromatography-Mass Spectrometry (GC-MS) and Nuclear Magnetic Resonance (NMR). Major polysaccharides were identified for each fraction: mannan, type II arabinogalactan and type I rhamnogalacturonan for BWPs, a mannan formed by a major chain ofα-Manp(1 → 6)-linked units, O-2 substituted with α-d-Manp(1 → 2)-linked side chains for BWPFp and a AG II formed by a major chain of β-d-Galp(1 → 3)-linked, substituted at O-6 by side chains of the β-d-Galp(1 → 6)-linked, which then are substituted at O-3 by non-reducingunits of α-l-Araf and a RG I, formed by [→4)-α-d-GalpA-(1 → 2)-α-l-Rhap-(1→]for BWPFs. Anti-inflammatory effects of polysaccharide fractions were evaluated in RAW 264.7 cells. Fractions markedly reduced nitric oxide (NO) and pro-inflammatory cytokine production (TNF-α and IL-1β) in LPS-treated cells.
read more
0 notes
Text
The three major pectic polysaccharides, sometimes called pectin domains, are homogalacturonan (HG), rhamnogalacturonan I (RG I), and rhamnogalacturonan II (RG II) (Figure 14.9).
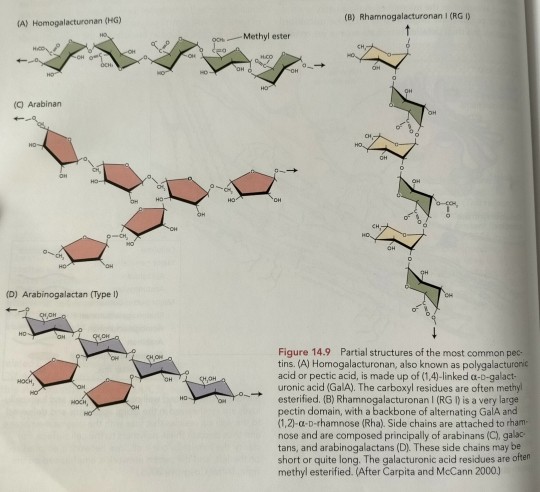
"Plant Physiology and Development" int'l 6e - Taiz, L., Zeiger, E., Møller, I.M., Murphy, A.
#book quotes#plant physiology and development#nonfiction#textbook#pectin#pectic#polysaccharides#homogalacturonan#rhamnogalacturonan#arabinan#arabinogalactan#galacturonic acid
0 notes
Text
Rhamnogalacturonan-I as a nematode chemoattractant from Lotus corniculatus L. super-growing root culture
http://dlvr.it/SjLsxr
0 notes
Text
Paleo, Resistant Starch, and TMAO: New Study Warning Worth Heeding
Paleo, Resistant Starch, and TMAO: New Study Warning Worth Heeding:
SCIENCE SIMPLIFIED:
A human study was published looking at how long-term adherence to a Paleo diet affects the gut microbiota and production of TMAO, which is linked to cardiovascular disease and some forms of cancer.
The study demonstrates that a low-carb Paleo diet increases TMAO, attributable to a decrease in probiotic bacteria from the Bifidobacterium and Roseburia genera and an increase in Hungatella species in the gut.
The dietary factors most strongly associated with the undesirable gut microbiome shift and TMAO production were total carbohydrate intake and resistant starch intake.
While the authors conclude that lack of grains are to blame, the study participants were eating mostly non-starchy vegetables (about 7 servings per day, averaging 28 grams of fiber but only 90 grams of total carbohydrates). Starchy roots and tubers are a healthy alternative to grains and would have increased the participant’s total carbohydrate intake (all slow-burning nutrient-dense carbs) as well as resistant starch intake.
The results of this study are relevant to our community and offer a stern warning against long-term low-carb implementations of the Paleo diet.
RELATED READING:
What Is the Gut Microbiome? And Why Should We Care About It?
The Case for More Carbs: Insulin’s Non-Metabolic Roles in the Human Body
Why Root Veggies Are Great for the Gut Microbiome
Whenever a new Paleo study comes out, it’s sure to stir up controversy—no matter what the findings are. “Good” findings are met with cheers from the Paleo community, while “bad” findings tend to explode in media headlines and send the Paleo community rushing to find reasons the study is poorly conducted, inaccurate, or otherwise worth dismissing.
As you know, I don’t believe in dismissing scientific findings (except for the rare occasion where flaws in how the study was designed or conducted result in retraction). Instead, I seek to understand the data in the context of the research field as a whole, seeking context and nuance while being open to adjusting my conclusions and recommendations. (I discuss the merits of different types of scientific studies as well as the problem with cherry-picking data in my Introduction to Nutritional Sciences online course.)
Recently, a human study was published looking at how long-term adherence to a Paleo diet affects the gut microbiota and TMAO. And, the headlines (both mainstream media and outlets targeting physicians) have not been flattering, for example: “Paleo Diet Increases Risk for Heart Disease”, “Paleo Diet Study Links ‘Caveman’ Regime to Heart Disease Biomarker”, and “Study Linking Paleo Diet to Increased Heart Disease Risk Strengthens Diet Industry Concerns”.
As you’re probably aware by now, I’m all about the gut microbiome, and believe it will continue to prove itself as a massive missing piece in our health puzzle! For that reason, this study is particularly interesting and important to look at (and not dismiss!).
Before we dive into the study itself, let’s review the things we need to know to make sense of the findings!
A Refresher on Fiber, Resistant Starch, and the Microbiome
The gut is a biological niche, home to a diverse array of microbes that influence nearly all aspects of human biology through their interactions with our bodies. We have a symbiotic relationship with these microbes, collectively referred to as our gut microbiome—in exchange for food and shelter, they contribute to our wellbeing by performing diverse functions essential to our health.
When we don’t have a healthy diversity of the right kinds of microbes in our gut, our entire body suffers. An unfavorable gut microbiome has been linked to conditions as wide-ranging as cancer, obesity and other metabolic problems, heart disease, anxiety, depression, autism, autoimmunity, ulcers, IBD, liver disease, systemic infections, and more. See What Is the Gut Microbiome? And Why Should We Care About It?.
I’m writing a book on the gut microbiome, so I could expound for days, but let’s focus on a few specifics that are particularly important to understanding this new paper.
Fiber Is Food for Our Gut Microbiome
If there’s one thing our gut microbes love, it’s fiber. In fact, out of all the dietary factors that can impact the gut, fiber may be the most important.
Carbohydrates, including fiber, are chains of monosaccharides (simple sugars) and of chemical derivatives of monosaccharides. Both the types of simple sugar (and their derivatives) in the chain and the ways they link together to form chains (both overall structure and the types of chemical bonds between sugar molecules) determine what type of carbohydrate it is. What separates fiber from other carbohydrates is that the way the sugars link together are not compatible with our digestive enzymes; our bodies just aren’t capable of breaking apart those types of molecular bonds. Instead, fiber passes through the digestive tract mainly intact. And once it reaches the colon, the magic begins: fiber serves as a substrate (food) for a wide range of bacteria, including some of the most important species we can harbor!
Why Different Fiber Types Feed Different Bacteria
The bacteria that live in our guts are collectively capable of producing over ten thousand different enzymes that can break down complex carbohydrates like fiber, which is pretty remarkable when you consider that we only produce about 17 different enzymes that digest carbohydrates! These enzymes belong to at least 206 different families of CAZymes (which stands for “Carbohydrate-Active enZymes”). Enzymes are typically highly specialized, breaking apart only specific molecular bonds, which is why different types of carbohydrates require different enzymes to break them apart (and why we can’t digest fiber but our gut bacteria can).
When it comes to carbohydrate degradation, some bacteria are highly specialized, producing only a few dozen CAZymes, whereas others are multitaskers, producing hundreds of CAZymes which allows them to grow on a variety of substrates and adapt to changing nutritional circumstances, thereby giving them a competitive advantage in the gut ecosystem.
Bacteria from the Bacteroides genus in general tend to be multitaskers, producing enzymes that can break down starch, pectin, hemicelluloses, and other plant carbohydrates (galactomannan, arabinogalactan, alginate, laminarin and xylans xyloglucan, rhamnogalacturonans I and II, β-glucans and glucomannan, to name a few!). Bacteroides thetaiotaomicron is an example of multitasker, considered a diet insensitive strain thanks to its ability to produce around 400 CAZymes (at least 260 of which are glycoside hydrolases) that help it thrive on pectins as well as complex carbohydrates that are produced by our own intestinal cells, such as mucin (a glycoprotein that is a major component of mucus).
In contrast, Bifidobacterium species are more specialized, producing an average of 45 CAZymes that make them highly effective at degrading high amylose starches, including resistant starch, as well as fructooligosaccharides, galactooligosaccharides, and inulin fiber. The critical consequence is that Bifidobacterium don’t survive if our diet doesn’t include sufficient amounts of these starches and fiber types.
Importance of Fiber Variety in the Diet
One of the consequences of this diversity in CAZyme production by various resident microbes is that different fermentable carbohydrates support different species in the gut. Therefore, consuming a variety of dietary fibers—various cellulose, hemicellulose, pectins, gums, fructans, glucans, mucilage, chitin, chitosan, and resistant starch fiber—best supports a diverse microbial community compared to a diet comprised of less varied fermentable carbohydrates like the Standard American Diet which is rich in refined carbohydrates.
Which foods are rich in which fiber sources?
Cellulose is found in all plants, but foods that contain particularly large amounts of cellulose include bran, legumes, nuts, peas, root vegetables, celery, broccoli, peppers, cabbage and other substantial leafy greens like collards, and apple skins. See The Fiber Manifesto-Part 2 of 5: The Many Types of Fiber
Hemicellulose is particularly high in bran, nuts, legumes, and whole grains, as well as many green and leafy vegetables.
Pectin is found in all fruits and vegetables but are particularly rich in certain fruits, including apples and citrus fruits, and are also found in legumes and nuts. See Why Fruit is a Good Source of Carbohydrates
Lignin is most commonly a component of wood, but food sources include root vegetables, vegetable filaments (like the stems of leafy greens and the strings in celery), many green, leafy vegetables, wheat, and the edible seeds of fruit (such as berry seeds and kiwi seeds). See Polyphenols: Magic Bullet or Health Hype?
Chitin is found not only in plants and fungi but also in the exoskeletons of insects and in the shells of crustaceans. See Elevating Mushrooms to Food Group Status and Why Crickets Are Great for the Gut Microbiome.
Chitosan is naturally found in the cell walls of fungi but are also produced as a functional fiber by treating shrimp and other crustacean shells with sodium hydroxide. See Elevating Mushrooms to Food Group Status.
Beta-glucans are found in some grains (mainly oats and barley, but also rye and wheat), fungi (yeast and mushrooms, particularly those mushrooms that are used medicinally like shiitake and maitake), and some types of seaweed (mainly algae). Beta-glucans are the fiber in oats that are largely responsible for their unique health benefits among grains. See Why Seaweed is Amazing! and Elevating Mushrooms to Food Group Status.
Fructans are naturally occurring in a variety of plants and are particularly high in chicory, Jerusalem artichoke and alliums (the onion family). Cruciferous vegetables contain modest amounts of fructans. See What about the Goitrogens in Cruciferous Veggies?.
Gums are a diverse group of fibers that plants secrete when they are damaged. Isolated versions are used in food manufacturing as thickening and gelling agents (like guar gum and xanthum gum). See Is It Paleo? Guar Gum, Xanthan Gum and Lecithin, Oh My!.
Mucilages are particularly concentrated in cacti and other succulents (like aloe), many types of seaweed (like agar agar algae), flax, chia and psyllium. They can also be found in relatively large amounts in a variety of fruits and vegetables, including plantains, bananas, taro root, cassava, and berries. See Mucilaginous Fiber: The Good, the Bad, and the Gooey and The Verdict on Psyllium Husks: Not Paleo!.
Resistant starch is divided into four subgroups: RS1 is rich in grains, legumes, and seeds; RS2 is found in most roots and tubers, and particularly high in green bananas, green plantains, and raw potatoes; RS3 is rich in cooked and cooled roots and tubers, particularly potatoes, as well as cooked and cooled rice; RS4 is the product of enzymatically or chemically modified starches sold under various brand names. See also Resistant Starch: It’s Not All Sunshine and Roses.
Because of their varying fiber types (and other food compounds that influence gut microbial composition like micronutrients, phytochemicals, proteins and fats), different families of fruits and vegetables are independently beneficial for the gut microbiome. See also The Fiber Manifesto-Part 2 of 5: The Many Types of Fiber
That means that beyond aiming for 8+ servings of fresh vegetables and fruits daily (see also The Importance of Vegetables), it’s important to hit as many of the different families of vegetables and fruits each day, ideally cycling through all of them every two days: cruciferous vegetables, leafy vegetables, roots and tubers, mushrooms, alliums, apple family, citrus, berries, nuts and seeds, etc.
Resistant Starch-Rich Foods as Microbiome Superfoods
Resistant starch is classified as a fiber because amylase, the enzyme that breaks starch into individual glucose units, doesn’t work on this type of starch.
Resistant starch is insoluble yet highly fermentable, and is divided into four subgroups: RS1, which is physically inaccessible due to being bound within cell walls; RS2, which is tightly packed ungelatinized granules found in certain raw starchy foods; RS3 (retrograded amylose), which is formed when certain starchy foods are cooked and then cooled down; and RS4, which is formed via a manmade chemical process. See also Resistant Starch: It’s Not All Sunshine and Roses
In general, resistant starch is famous for feeding short-chain-fatty-acid-producing bacteria and enhancing levels of butyric acid. In a human study, RS2 was shown to increase the abundance of Ruminococcus bromii and Eubacterium rectale, whereas RS4 increased Bifidobacterium adolescentis and Parabacteroides distasonis. Long-term feeding of RS1 and RS2 in rats showed that both types increased the abundance of anaerobes, the levels of Bifidobacteria, and total SCFAs in the cecum; meanwhile, RS2 (but not RS1) enhanced levels of Lactobacillus, Streptococci, and Enterobacteria. In pigs, RS3 has been shown to increase the abundance of Faecalibacterium prausnitzii while reducing levels of E. coli and Pseudomonas species. Interestingly, Ruminococcus bromii plays a keystone role in the degradation of resistant starch, releasing breakdown products that are then utilized by other microbes in the gut.
Two Important Probiotic Bacteria: Bifidobacteria and Roseburia
Hundreds of beneficial probiotic species of bacteria (as well as fungi like yeast and archaea, which we’ll come back to) have been well studied in terms of their roles in the gut microbiome and human health in general. I want to focus in on two genera of bacteria that are particularly relevant to this new paper.
The Bifidobacteria genus exerts a range of beneficial effects on human health, including producing vitamins, inhibiting pathogens from colonizing or infecting the gut mucosa, helping regulate the microbiome’s homeostasis, modulating local and systemic immune responses, repressing potentially carcinogenic enzymatic activities among different bacteria, and facilitating the bioconversion of various dietary compounds into bioactive forms. In a variety of studies, Bifidobacteria have been shown to improve the gut barrier function, suppress E. coli, improve glucose tolerance, reduce low-grade inflammation, and reduce endotoxemia induced by high-fat diets. As another benefit, because Bifidobacteria produce lactic acid instead of gas, people with higher levels tend to have less flatulence and digestive problems!
There are 39 identified species of Bifidobacteria, which represent 3-6% of health adult fecal flora. Their favorite foods are resistant starch 2, resistant starch 4, oligosaccharides from plants and milk, and hexose.
Let me emphasize: Bifidobacterium are critically important to human health. If you see an argument dismissing this paper because somehow low-carb diets or low-carb Paleo benefits make up for missing Bifidobacteria, that is unequivocally false.
The Roseburia genus are butyrate-producing bacteria that are implicated in maintaining gut barrier health and immune regulation, with strong anti-inflammatory properties. Reduced levels of Roseburia are associated with inflammatory bowel disease (Roseburia actually suppress the pathogenesis of Crohn’s disease), irritable bowel syndrome, obesity, type 2 diabetes, cardiovascular disease, neurological diseases, autoimmune disease, asthma and allergies—likely mediated through higher intestinal permeability and inflammation.
There are five known species of Roseburia (R. intestinalis, R. hominis, R. inulinivorans, R. faecis and R. cecicola) and their favorite foods are beta-glucans, fructans, pectin and resistant starch.
The Deal with TMAO
So, where does TMAO fit into the microbiome?
In recent years, trimethylamine-N-oxide (TMAO) has emerged as a possible new risk factor for cardiovascular disease, with potential to other conditions as well (such as chronic kidney disease, chronic heart failure, and colorectal cancer). For instance, a meta-analysis using 11 prospective studies found that higher circulating levels of TMAO were associated with a 23% increased risk of cardiovascular events and a 55% increased risk of all-cause mortality. This little molecule gets produced from the microbial metabolism of choline, lecithin, and carnitine (from our diet) into trimethylamine (TMA), which the liver then oxidizes into TMAO. Once it’s in our bodies, TMAO gets transported to different tissues and can potentially accumulate.
However, our levels of TMAO aren’t just a matter of how much free TMAO or TMAO precursors we ingest! Gut bacteria, especially the genus Prevotella, is a key mediator between diet and the amount of TMAO in our blood. In one study, researchers found that participants with gut microbiomes dominated by Prevotella were the ones who produced the most TMA (and therefore TMAO, after it reached the liver) from the carnitine they consumed. Those with microbiomes high in Bacteroides rather than Prevotella saw dramatically less conversion to TMA and TMAO.
So far, the list of TMAO-producing bacteria also includes multiple Clostridium species, Desulfovibrio desulfuricans, Providencia rettgeri, Edwardsiella targa, Escherichia fergusonii, Anaerococcus hydrogenalis, Proteus penneri, Firmicutes, and Proteobacteria. In other words, we can’t look at TMAO without also looking at the composition of our gut microbiota!
TMAO: Symptom or Cause of Heart Disease?
Despite some compelling associations with disease and mortality, there’s still a lot of controversy over whether TMAO has a causal relationship with the conditions it’s been associated with. On one hand, we have identified some plausible mechanisms for its role in disease, especially heart disease. For example, TMAO appears to increase the number of scavenger receptors in macrophages, resulting in greater binding to LDL particles and subsequent foam cell formation (foam cells play a major role in the progression of atherosclerotic plaque buildup!). TMAO also interferes with sterol transportation and bile acid metabolism, which can further contribute to the development of heart disease. And, TMAO may increase platelet activity, which can raise the risk of thrombosis by promoting excessive coagulation in the blood.
But despite these possible mechanisms, the literature is still mixed when it comes to how elevated TMAO plays out in real life! Along with studies showing a link between high TMAO levels and disease or mortality, many studies have failed to find any predictive value for TMAO on cardiovascular events, chronic kidney disease, or heart failure.
It’s possible that high TMAO occurs as a result of some of these diseases, rather than as a causative factor (high TMAO makes sense in the case of kidney failure, for instance, because the kidneys are the major site of circulating TMAO clearance, and their compromised function would naturally lead to a buildup of TMAO).
It’s also very possible that gut microbiota compositions that contribute to chronic disease also happen to result in more TMA and TMAO production, making TMAO a marker for disease states rather than a causal risk factor. Overall, the jury’s still out!
The Fish Paradox
One of the major monkey wrenches in the whole TMAO story is a fishy one (pun intended). Seafood—famously considered heart-healthy—is one of the most abundant sources of free TMAO, and also contains TMAO precursors. And we’d be hard pressed to find a study that shows seafood is bad for our cardiovascular health (indeed, the vast majority of research shows that fish is one of the best things we can eat for our hearts!). Physiologically, TMAO helps fish survive in their marine environments by increasing buoyancy, acting as a form of antifreeze (by increasing osmotic concentration), and protecting tissue proteins against destabilizing forces. The degradation of TMAO into TMA is also what gives seafood its characteristic fishy odor! TMAO levels can vary dramatically between different species of fish (and even vary within the same species depending on the season), but in general, deep-sea fish and shellfish tend to be higher in TMAO than shallow water fish and shellfish, likely because of the role TMAO plays in protecting against pressure-induced protein damage.
Research has shown that following the consumption of seafood, blood levels of TMAO levels rise to significantly higher levels than after the consumption of beef or eggs. In one study, 40 participants were fed meals containing cod fish, eggs, beef, or a fruit control in random order, with week-long washout periods between each intervention. After the fish meal, participants’ plasma TMAO rose up to 62 times higher than after the beef, eggs, or fruit meals. These levels peaked at 2 hours post-meal and remained elevated for the remainder of the 6-hour study period. The rise in TMAO levels started within 15 minutes following fish consumption, indicating the TMAO was being directly absorbed rather than undergoing conversion in the gut by bacteria. This same study found dramatic variations in TMAO response after eating eggs or beef. Compared to baseline, TMAO levels ranged anywhere from a 30% decrease to a 270% increase!
Food vs. Microbiome Sources of TMAO
So, why would we see such extreme variations in TMAO levels after eating the same foods? The answer is, not surprisingly, bacteria! Stool analysis showed that compared to low TMAO producers, high TMAO producers had some important microbiota differences, including lower alpha-diversity, different species compositions, and a higher ratio of Firmicutes to Bacteroidetes (about 2:1, versus a 1:1 ratio for the low producers). And very importantly, as we’ll see in a moment, the Archaea phylum was completely absent in the microbiota of the high TMAO producers, but was represented among the low TMAO producers.
This study provided some important pieces for the TMAO puzzle. Along with demonstrating that fish (at least in the form of cod) yields vastly higher levels of TMAO and TMAO metabolites than beef or eggs, the study demonstrated that TMAO can be absorbed intact from foods like fish without involvement of the gut microbiota. That means that the level of TMAO we have in our bodies isn’t just a result of our gut microbiota churning it out from precursors, but can also be influenced by the direct consumption of TMAO from food. And, that could mean that high circulating TMAO from seafood potentially indicates a much different (AKA lower!) risk profile than high TMAO produced by disease-associated microbes.
So, as much as is still up in the air about TMAO, one thing seems pretty likely: we don’t want a gut microbiome that produces a lot of it. Whether or not TMAO itself turns out to be a major risk factor or just a red herring, and whether or not our circulating levels are a cause or consequence of specific health conditions, a high-TMAO-generating microbiota seems to be consistent with greater disease risk.
Archaea: A Microbiome Missing Piece
Whenever we hear about the microbiota, it’s usually all about the bacteria, bacteria, and more bacteria! But, while bacteria might be numerically dominant among the microbes in our gut, they’re definitely not the only residents there. Another type of single-celled organism that call our GI tracts home are archaea. And, these little guys are incredibly important!
Archaea (sometimes called archaebacteria) are strict anaerobes that live in various mucosal sites throughout the body, including the intestinal mucosa. We aren’t born with archaea inside us, but we acquire them from the environment throughout life: by the time children are school-aged, archaea are almost universally present in the gut, and levels continue to increase with age (with the highest occurrence and diversity of archaea being found in older adults). Along with lacking lipopolysaccharide (meaning archaea won’t contribute to our endotoxin load), archaea is also the only domain of life that doesn’t include any known pathogens, which is pretty cool!
Archaea degrade TMA and TMAO
One important subtype of archaea are the methanogens, which produce methane gas as a byproduct of hydrogen reduction. Up to 95% of human guts harbor the methanogenic archaea Methanobrevibacter smithii and Methanosphaera stadtmanae, at varying levels. While the idea of producing methane might not sound very pleasant, some of these archaea (in particular, an order of methanogens called the Methanomassiliicoccales) actually play an integral role in reducing our TMAO production. Along with being able to use carbon dioxide, formate, and methanol (all released by bacteria breaking down food and other organic matter in the gut), these archaea can use methyl compounds like TMA and TMAO to generate methane. And that means that the archaea in our gut actually deplete the pool of TMA we have available to be converted into TMAO (along with any free TMAO from foods like seafood). So, all that TMA generated by Prevotella, or entering our body from fish consumption? Archaea can help wipe some of it out!
The TMAO-reducing effects of archaea is far from just speculative, too. In a study of ELDERMET subjects, the fecal TMA concentration in people with TMA-metabolizing archaea was significantly lower than in those without this archaea—and the difference was particularly dramatic when the abundance of Methanomassiliicoccales was greater than 10^8 cells per gram of stool. This role of archaea is so exciting that some scientists are proposing a new class of probiotics called archaeabiotics, which could help reduce our TMAO levels without us needing to cut back on choline and other important nutrients!
Importantly, methanogenic archaea have an important interactive relationship with bacteria in the gut, which often takes the form of what scientists call syntrophy (where two organisms participate in consuming a substance that neither one can catabolize on its own). And, it appears that archaea are particularly chummy with the important probiotic bacteria Bifidobacteria. For example, mixed cultures of M. smithii and Bifidobacteria bifidum have been shown to collectively produce methane from glucose, and in females with gut Methanobacteriales levels higher than 0.71%, there’s a significantly higher mean abundance of Bifidobacteriaceae. And as we’ve already seen, healthy levels of Bifidobacteria are super important!
Archaea Thrive When We Eat Carbs!
So, how do we keep our archaea happy and thriving? Scientists are just at the beginning stages of understanding how diet impacts our archaea colonies (after all, archaea are relative newcomers to the microbiota research scene compared to bacteria!), but here’s what we know so far. In children, organic dairy (especially organic yogurt and organic milk) has been associated with the initial colonization of M. smithii, due to organic dairy serving as a vehicle for delivering it to our guts. And, some methanogens degrade methanol, which gets produced when bacteria degrade pectin in fruits—thus suggesting that archaea might benefit from including fruit in our diets! In Chinese goats, eating a high-grain diet appears to suppress methanogenic archaea relative to a high-hay diet—possibly due to the pH-lowering effect of grains in the rumen (which can then suppress methanogenic archaea that are sensitive to low pH environments). Obviously, we’re not Chinese goats, but it would certainly be interesting if a high-grain diet in humans had a similar effect!
More broadly, though, in humans, Methanobrevibacter abundance is positively associated with higher carbohydrate consumption (both recent and long-term), and negatively associated with recent consumption of fat (especially vegetable fat and polyunsaturated fat intake) and amino acids. Although more research is definitely needed, the picture getting painted so far is that archaea benefit from a variety of plant polysaccharides, and not so much from animal-based diets.
However, this isn’t because the archaea themselves eat carbohydrate. In fact, methanogenic archaea have an almost complete lack of enzymes for breaking down complex carbohydrates into simple sugars. What does appear to be happening is that archaea thrive off the metabolic products of carbohydrate-loving bacteria, and therefore are still dependent on dietary carbohydrate for their own survival!
The Study: Long-term Paleolithic diet is associated with lower resistant starch intake, different gut microbiota composition and increased serum TMAO concentrations
Whew! Now that we’ve covered the necessary background, let’s take a look at what this study is all about!
Researchers recruited a total of 44 participants who self-reported following a Paleo diet for over a year, along with 47 controls who more or less followed the national dietary recommendations of Australia (where the study was conducted). Within the Paleo group, participants were further divided based on how strictly they followed the Paleo framework (as gauged by the exclusion of grain and dairy products): 22 people fell into the “strict Paleo” group (less than one serving of grains and/or dairy per day), and 22 people fell into the “pseudo-Paleo” group (more than one serving of grains and/or dairy per day). (This is important, because “real-world” Paleo includes a variety of interpretations about what Paleo actually means, including how strictly to adhere to the diet—so a pseudo-Paleo group might be closer to reality for a lot of people!)
The study excluded anyone who’d taken antibiotics within the past six months, who had any type of GI tract surgery, who had past or present digestive disorders, who used cholesterol or blood pressure lowering medications, or who had been diagnosed with cardiovascular disease. This helped make sure the results weren’t confounded by preexisting health conditions or drugs, and allowed the researchers to better isolate the effects of the participants’ diets.
To ensure accurate dietary data, the researchers had participants undergo three-day weighed diet records (including two weekdays and one weekend day), which were then validated using urine nitrogen tests (which could detect whether participants were over- or under-reporting their protein intake) and the Goldberg cut point (which can identify which participants were under-reporting their energy intake, through the ratio of energy intake to basal metabolic rate). Participants who appeared to inaccurately report both their protein and energy intake were deemed unreliable dietary reporters (this ended up being two people from the strict Paleo group and three people from the control group).
Paleo Diet Adherents Had Increased TMAO
Now, the headline-grabbing finding. In the strict Paleo group, serum TMAO was a whopping 9.53 µM, the pseudo-Paleo group averaged 5.47 µM, and the control group averaged 3.93 µM. Higher TMAO levels were associated positively with red meat intake and negatively with grain intake.
Whether TMAO is a causative agent for disease or a marker for a disease-associated microbiota, those are some scary numbers—especially for the strict Paleo group!
What Study Participants Were Actually Eating
So, what were the Paleo groups actually eating? Here’s what the data showed!
Not surprisingly, both Paleo groups ate more protein than the controls (118 and 102.7 grams per day for the strict Paleo group and pseudo-Paleo group, respectively, compared to 92 grams for the controls), less carbohydrate (99 and 81.4 grams per day for the strict Paleo group and pseudo-Paleo group, respectively, compared to 202.6 grams for the controls), less sugar (51.8 and 44 grams per day for the Paleo groups, and 75.6 grams for the controls), and more fat—with the increase mostly coming from saturated and monounsaturated forms (117.9 total fat grams per day for the strict Paleo group, 133.1 grams for the pseudo-Paleo group, and 82.5 grams for the controls).
Importantly, total dietary fiber was adequate (and very similar!) for both the control group and the strict Paleo group—29.7 grams and 27.4 grams daily, respectively, which falls within the recommended daily intake of 25-30 grams for adults. The pseudo-Paleo group averaged 20.8 grams of fiber each day, which is still more than most people consume! For the Paleo groups, much of their fiber came from vegetables, with the strict Paleo group eating 6.7 servings of veggies per day and the pseudo-Paleo group averaging 4.3, compared to the control group’s 3.93. (We could definitely argue that the official recommendations for fiber are still too low for optimal health, but the point here is, these study participants weren’t slacking on the non-starchy veggies!)
While the control group averaged 4.5 – 14.2 grams of resistant starch per day, largely from grains (those are estimated minimum and maximum amounts, since the same foods can vary in resistant starch content), the strict Paleo group averaged only 2.6 – 6.1 grams per day, and the pseudo-Paleo group got a mere 1.3 – 2.9 grams of resistant starch. That’s a significant drop off!
Low-Carb Paleo Effects on the Microbiome
Remember that one of the favorite foods of Bifidobacteria is resistant starch? And that Roseburia also likes to munch on carbohydrates like beta-glucans? Maybe we shouldn’t be surprised that this study showed a significant decrease in these important bacteria among both Paleo groups.
Likewise, the relative abundance of Hungatella was significantly higher among the Paleo subjects. After adjusting for age, gender, stool frequency, and body fat, Hungatella abundance was significantly negatively associated with grain intake among the study’s participants, and was also significantly negatively correlated with Bifidobacteria and Roseburia abundance. Although we don’t have a lot of information about Hungatella in relation to human health (not yet, anyway!), we do know that some species originating from the genus Hungatella are associated with choline consumption and TMA production, including at least one species identified in this study. The researchers speculated that some components of grains and/or whole grains either interfere with Hungatella’s TMA production or prevent it from dominating in the gut. And, these components might not be resistant starch, since neither Hungatella nor TMAO was significantly associated with resistant starch intake!
Resistant Starch and Total Carb Intake Are Important!
One of the things that makes this study so interesting (and important!) is the fact that fiber and vegetable intake was relatively high for both Paleo groups. Often, when we talk about how ketogenic diets or low-carb or low-starch Paleo might affect the gut microbiome, we’re given a false sense of security thinking we’ll be fine as long as we eat plenty of fiber from leafy greens; see also How Ketogenic Diet Wreaks Havoc on Your Gut. As this study indicates, low-starch veggies alone are not enough to maintain a robust, diverse gut microbiome! The Paleo subjects clearly weren’t ingesting a broad enough array of fibers and starches to support some very important bacterial populations.
Given all that, can we just add some supplemental resistant starch to otherwise low-carb diet and call it a day?
Actually, the answer here seems to be no! Consistent with my post Resistant Starch: It’s Not All Sunshine and Roses, the research shows that isolated resistant starch doesn’t bring the same range of benefits as resistant starch from whole-food sources. And what’s more, when it comes to TMAO, supplemental resistant starch may even be counterproductive in the context of a low-carb and/or high fat diet. In a human cross-over trial from 2016, for example, 52 adults consumed four different diets in random orders—a low resistant starch, higher carbohydrate diet; a low resistant starch, lower carbohydrate diet; a high resistant starch, higher carbohydrate diet; and a high resistant starch, lower carbohydrate diet (with resistant starch coming from Hi-Maize 260, supplying RS2). Intriguingly, the highest TMAO levels occurred when subjects were eating the high resistant starch, lower carbohydrate diet, despite dietary levels of carnitine and choline being less on that diet compared to the low resistant starch periods. The researchers proposed that a high isolated resistant starch intake, in the presence of an overall lower carbohydrate diet, shifted the microbiota towards greater TMAO generation. Likewise, studies in rodents have shown that high fat consumption (which often goes hand-in-hand with low-carbohydrate diets), in the amount of of 42% of total energy, partially counteracts the beneficial effects of RS2 by suppressing levels of beneficial bacteria. So, low-carb diets can be a double whammy against our gut microbiota, both by failing to supply a wide range of fiber and starch types and by overloading our guts with levels of fat that become harmful to bacteria. (Don’t worry; we aren’t calling fat bad here—but a balanced intake of macronutrients seems to be where the evidence is pointing for optimal health!)
Other studies support the idea that resistant starch is most health-promoting in conjunction with other dietary carbohydrates. In pigs, resistant starch alone (in the form of RS2) was shown to get rapidly fermented in the proximal (beginning part) of the colon, while failing to reach further down into the distal (lower) colon—resulting in only a small portion of the colon receiving fermentation benefits. But, when additional carbohydrate in the form of wheat bran (a soluble non-starch polysaccharide) was included in the pigs’ diets, the amount of resistant starch getting fermented between the lower colon and feces nearly doubled—indicating that the bulk from the wheat bran was helping spread fermentation further down through the colon, flooding a much greater area with cancer-protective butyrate. The addition of wheat seed (RS1) to supplemental green banana flour and high-amylose starch (RS2) has been shown to help spread fermentation throughout the entire colon, as indicated by a decrease in fecal pH (which is a good thing!).
When it comes to low-carb Paleo diets, it’s easy to see how a similar effect could occur. Cutting out sources of bulky fermentable carbohydrate (like root veggies and legumes) limits how far isolated resistant starch can spread, resulting in bacteria in the proximal colon gobbling it up and leaving none for microbes further down the colon. Likewise, given what we know about the role of methanogenic archaea in regulating TMAO levels and interacting with other microbes like Bifidobacteria (as well as how much methanogenic archaea likes carbohydrates and doesn’t like fat!), we might suspect that low-carb diets can also enhance TMAO production by suppressing archaea growth.
As further confirmation, the main study we’ve been discussing in this article found that TMAO levels were more strongly negatively associated with grain intake than with resistant starch intake. That doesn’t mean we all need to eat grains to be healthy, but it does imply that diverse components of starchy plant foods (such as the other forms of fiber and carbohydrate they contain) contribute to a healthy microbiome, even more so than resistant starch on its own.
Short-Term Vs. Long-Term Microbiome Shifts
We should also stress the importance of the long-term nature of this study! While shorter dietary trials can be very useful (and in some cases, are the only studies we have at our disposal), they can’t capture potential health issues that develop months or years down the line (such as gradual changes in the core gut microbiota composition). That’s particularly relevant here, because the same researchers who conducted this study previously published a similar one, randomizing 22 women to a Paleo diet for four weeks and 17 women to a diet in line with Australian health recommendations. In that study, there wasn’t a significant change in TMAO concentration compared to the control group, despite a lower intake of resistant starch and higher intake of meat and eggs among the Paleo dieters. While those findings could have been due to the small sample size and limited data for resistant starch content of foods (making it difficult to precisely calculate resistant starch intake), it’s also possible that the Paleo group hadn’t yet exhibited some longer-term microbiota shifts that lead to higher TMAO generation as seen in the more recent study.
Indeed, the field of microbiota research has shown us that while some microbial changes happen rapidly when we alter our diet, others can occur on a more gradual basis. So, only using participants who had been eating Paleo for over a year gives this study greater insight into the full effects that low-carb Paleo has on the gut microbiota.
The Bottom Line: Paleo Should Not Be Low-Carb
Some people have seen this paper as an attack on red meat, which, given the TMAO link, is a valid concern (see also The Link Between Meat and Cancer). But what this paper is actually making a case for is that starch-free diets are a problem. Don’t get me wrong: fibrous, low-starch veggies are fantastic, and we should be filling our plates with them on the daily—but not at the exclusion of Paleo starches! Root veggies rich in resistant starch are consistently showing up as a vital component of a nutrient-dense Paleo diet, and there are no real “hacks” to get around that (see also Why Root Veggies Are Great for the Gut Microbiome and Resistant Starch: It’s Not All Sunshine and Roses).
When we combine this information with an examination of the non-metabolic roles that insulin plays (another rationale for moderate [not low] carb intake, see The Case for More Carbs: Insulin’s NonMetabolic Roles in the Human Body and How Many Carbs Should We Eat?), the potential problems of too-high-fat intake (not that we wan’t to eat low-fat; see Saturated Fat: Healthful, Harmful, or Somewhere In Between?, Adverse Reactions to Ketogenic Diets: Caution Advised), and understanding that micronutrient sufficiency is most easily attained with a balanced macronutrient diet (see The Diet We’re Meant to Eat, Part 3: How Much Meat versus Veggies?, The Importance of Nutrient Density, and Carbs Vs. Protein Vs. Fat: Insight from Hunter-Gatherers), it’s becoming harder and harder to make a compelling case against moderate carbohydrate intake, 30 to 60% of total calories, from whole food sources.
Citations
Bergeron N, et al. “Diets high in resistant starch increase plasma levels of trimethylamine-N-oxide, a gut microbiome metabolite associated with CVD risk.” Br J Nutr. 2016 Dec;116(12):2020-2029. doi: 10.1017/S0007114516004165. Epub 2016 Dec 20.
Borrel G, et al. “Genomics and metagenomics of trimethylamine-utilizing Archaea in the human gut microbiome.” ISME J. 2017 Sep;11(9):2059-2074. doi: 10.1038/ismej.2017.72. Epub 2017 Jun 6.
Charrier JA, et al. “High fat diet partially attenuates fermentation responses in rats fed resistant starch from high-amylose maize.” Obesity (Silver Spring). 2013 Nov;21(11):2350-5. doi: 10.1002/oby.20362. Epub 2013 Jul 2.
Cho, CE, et al. “Trimethylamine‐N‐oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: A randomized controlled trial” M. A., Mol. Nutr. Food Res. 2016, 1600324. Doi: 10.1002/mnfr.201600324
Dridi B, et al. “High prevalence of Methanobrevibacter smithii and Methanosphaera stadtmanae detected in the human gut using an improved DNA detection protocol.” PLoS One. 2009 Sep 17;4(9):e7063. doi: 10.1371/journal.pone.0007063.
Dridi B, et al. “High prevalence of Methanobrevibacter smithii and Methanosphaera stadtmanae detected in the human gut using an improved DNA detection protocol.” PLoS One. 2009 Sep 17;4(9):e7063. doi: 10.1371/journal.pone.0007063.
Genoni, A, et al. “Long-term Paleolithic diet is associated with lower resistant starch intake, different gut microbiota composition and increased serum TMAO concentrations.” European Journal of Nutrition, 2019; DOI: 10.1007/s00394-019-02036-y
Genoni A, et al. “A Paleolithic diet lowers resistant starch intake but does not affect serum trimethylamine-N-oxide concentrations in healthy women.” Br J Nutr. 2019 Feb;121(3):322-329. doi: 10.1017/S000711451800329X. Epub 2018 Nov 13.
Govers MJ, et al. “Wheat bran affects the site of fermentation of resistant starch and luminal indexes related to colon cancer risk: a study in pigs.” Gut. 1999 Dec;45(6):840-7.
Hoffmann C, et al. “Archaea and fungi of the human gut microbiome: correlations with diet and bacterial residents.” PLoS One. 2013 Jun 17;8(6):e66019. doi: 10.1371/journal.pone.0066019.
Jin W, Cheng Y, Zhu W. “The community structure of Methanomassiliicoccales in the rumen of Chinese goats and its response to a high-grain diet.” J Anim Sci Biotechnol. 2017 Jun 1;8:47. doi: 10.1186/s40104-017-0178-0.
Qi J, et al. “Circulating trimethylamine N-oxide and the risk of cardiovascular diseases: a systematic review and meta-analysis of 11 prospective cohort studies.” J Cell Mol Med. 2018 Jan;22(1):185-194. doi: 10.1111/jcmm.13307. Epub 2017 Aug 7.
Raymann K, et al. “Unexplored Archaeal Diversity in the Great Ape Gut Microbiome.” mSphere. 2017 Feb 22;2(1). pii: e00026-17. doi: 10.1128/mSphere.00026-17.
Tamanai-Shacoori Z, et al. “Roseburia spp.: a marker of health?” Future Microbiol. 2017 Feb;12:157-170. doi: 10.2217/fmb-2016-0130.
van de Pol JA, et al. “Gut Colonization by Methanogenic Archaea Is Associated with Organic Dairy Consumption in Children.” Front Microbiol. 2017 Mar 10;8:355. doi: 10.3389/fmicb.2017.00355. eCollection 2017.
Vanderhaeghen S, Lacroix C, Schwab C. “Methanogen communities in stools of humans of different age and health status and co-occurrence with bacteria.” FEMS Microbiol Lett. 2015 Jul;362(13):fnv092. doi: 10.1093/femsle/fnv092.
Vanessa DN, et al. “Archaea: Essential inhabitants of the human digestive microbiota.” Human Microbiome Journal, 2017 3:1-8. doi.org: 10.1016/j.humic.2016.11.005.
from https://www.thepaleomom.com/paleo-resistant-starch-and-tmao-new-study-warning-worth-heeding/
from https://myfunweightloss.tumblr.com/post/186961759247
0 notes
Text
Paleo, Resistant Starch, and TMAO: New Study Warning Worth Heeding
SCIENCE SIMPLIFIED:
A human study was published looking at how long-term adherence to a Paleo diet affects the gut microbiota and production of TMAO, which is linked to cardiovascular disease and some forms of cancer.
The study demonstrates that a low-carb Paleo diet increases TMAO, attributable to a decrease in probiotic bacteria from the Bifidobacterium and Roseburia genera and an increase in Hungatella species in the gut.
The dietary factors most strongly associated with the undesirable gut microbiome shift and TMAO production were total carbohydrate intake and resistant starch intake.
While the authors conclude that lack of grains are to blame, the study participants were eating mostly non-starchy vegetables (about 7 servings per day, averaging 28 grams of fiber but only 90 grams of total carbohydrates). Starchy roots and tubers are a healthy alternative to grains and would have increased the participant’s total carbohydrate intake (all slow-burning nutrient-dense carbs) as well as resistant starch intake.
The results of this study are relevant to our community and offer a stern warning against long-term low-carb implementations of the Paleo diet.
RELATED READING:
What Is the Gut Microbiome? And Why Should We Care About It?
The Case for More Carbs: Insulin’s Non-Metabolic Roles in the Human Body
Why Root Veggies Are Great for the Gut Microbiome
Whenever a new Paleo study comes out, it’s sure to stir up controversy—no matter what the findings are. “Good” findings are met with cheers from the Paleo community, while “bad” findings tend to explode in media headlines and send the Paleo community rushing to find reasons the study is poorly conducted, inaccurate, or otherwise worth dismissing.
As you know, I don’t believe in dismissing scientific findings (except for the rare occasion where flaws in how the study was designed or conducted result in retraction). Instead, I seek to understand the data in the context of the research field as a whole, seeking context and nuance while being open to adjusting my conclusions and recommendations. (I discuss the merits of different types of scientific studies as well as the problem with cherry-picking data in my Introduction to Nutritional Sciences online course.)
Recently, a human study was published looking at how long-term adherence to a Paleo diet affects the gut microbiota and TMAO. And, the headlines (both mainstream media and outlets targeting physicians) have not been flattering, for example: “Paleo Diet Increases Risk for Heart Disease”, “Paleo Diet Study Links ‘Caveman’ Regime to Heart Disease Biomarker”, and “Study Linking Paleo Diet to Increased Heart Disease Risk Strengthens Diet Industry Concerns”.
As you’re probably aware by now, I’m all about the gut microbiome, and believe it will continue to prove itself as a massive missing piece in our health puzzle! For that reason, this study is particularly interesting and important to look at (and not dismiss!).
Before we dive into the study itself, let’s review the things we need to know to make sense of the findings!
A Refresher on Fiber, Resistant Starch, and the Microbiome
The gut is a biological niche, home to a diverse array of microbes that influence nearly all aspects of human biology through their interactions with our bodies. We have a symbiotic relationship with these microbes, collectively referred to as our gut microbiome—in exchange for food and shelter, they contribute to our wellbeing by performing diverse functions essential to our health.
When we don’t have a healthy diversity of the right kinds of microbes in our gut, our entire body suffers. An unfavorable gut microbiome has been linked to conditions as wide-ranging as cancer, obesity and other metabolic problems, heart disease, anxiety, depression, autism, autoimmunity, ulcers, IBD, liver disease, systemic infections, and more. See What Is the Gut Microbiome? And Why Should We Care About It?.
I’m writing a book on the gut microbiome, so I could expound for days, but let’s focus on a few specifics that are particularly important to understanding this new paper.
Fiber Is Food for Our Gut Microbiome
If there’s one thing our gut microbes love, it’s fiber. In fact, out of all the dietary factors that can impact the gut, fiber may be the most important.
Carbohydrates, including fiber, are chains of monosaccharides (simple sugars) and of chemical derivatives of monosaccharides. Both the types of simple sugar (and their derivatives) in the chain and the ways they link together to form chains (both overall structure and the types of chemical bonds between sugar molecules) determine what type of carbohydrate it is. What separates fiber from other carbohydrates is that the way the sugars link together are not compatible with our digestive enzymes; our bodies just aren’t capable of breaking apart those types of molecular bonds. Instead, fiber passes through the digestive tract mainly intact. And once it reaches the colon, the magic begins: fiber serves as a substrate (food) for a wide range of bacteria, including some of the most important species we can harbor!
Why Different Fiber Types Feed Different Bacteria
The bacteria that live in our guts are collectively capable of producing over ten thousand different enzymes that can break down complex carbohydrates like fiber, which is pretty remarkable when you consider that we only produce about 17 different enzymes that digest carbohydrates! These enzymes belong to at least 206 different families of CAZymes (which stands for “Carbohydrate-Active enZymes”). Enzymes are typically highly specialized, breaking apart only specific molecular bonds, which is why different types of carbohydrates require different enzymes to break them apart (and why we can’t digest fiber but our gut bacteria can).
When it comes to carbohydrate degradation, some bacteria are highly specialized, producing only a few dozen CAZymes, whereas others are multitaskers, producing hundreds of CAZymes which allows them to grow on a variety of substrates and adapt to changing nutritional circumstances, thereby giving them a competitive advantage in the gut ecosystem.
Bacteria from the Bacteroides genus in general tend to be multitaskers, producing enzymes that can break down starch, pectin, hemicelluloses, and other plant carbohydrates (galactomannan, arabinogalactan, alginate, laminarin and xylans xyloglucan, rhamnogalacturonans I and II, β-glucans and glucomannan, to name a few!). Bacteroides thetaiotaomicron is an example of multitasker, considered a diet insensitive strain thanks to its ability to produce around 400 CAZymes (at least 260 of which are glycoside hydrolases) that help it thrive on pectins as well as complex carbohydrates that are produced by our own intestinal cells, such as mucin (a glycoprotein that is a major component of mucus).
In contrast, Bifidobacterium species are more specialized, producing an average of 45 CAZymes that make them highly effective at degrading high amylose starches, including resistant starch, as well as fructooligosaccharides, galactooligosaccharides, and inulin fiber. The critical consequence is that Bifidobacterium don’t survive if our diet doesn’t include sufficient amounts of these starches and fiber types.
Importance of Fiber Variety in the Diet
One of the consequences of this diversity in CAZyme production by various resident microbes is that different fermentable carbohydrates support different species in the gut. Therefore, consuming a variety of dietary fibers—various cellulose, hemicellulose, pectins, gums, fructans, glucans, mucilage, chitin, chitosan, and resistant starch fiber—best supports a diverse microbial community compared to a diet comprised of less varied fermentable carbohydrates like the Standard American Diet which is rich in refined carbohydrates.
Which foods are rich in which fiber sources?
Cellulose is found in all plants, but foods that contain particularly large amounts of cellulose include bran, legumes, nuts, peas, root vegetables, celery, broccoli, peppers, cabbage and other substantial leafy greens like collards, and apple skins. See The Fiber Manifesto-Part 2 of 5: The Many Types of Fiber
Hemicellulose is particularly high in bran, nuts, legumes, and whole grains, as well as many green and leafy vegetables.
Pectin is found in all fruits and vegetables but are particularly rich in certain fruits, including apples and citrus fruits, and are also found in legumes and nuts. See Why Fruit is a Good Source of Carbohydrates
Lignin is most commonly a component of wood, but food sources include root vegetables, vegetable filaments (like the stems of leafy greens and the strings in celery), many green, leafy vegetables, wheat, and the edible seeds of fruit (such as berry seeds and kiwi seeds). See Polyphenols: Magic Bullet or Health Hype?
Chitin is found not only in plants and fungi but also in the exoskeletons of insects and in the shells of crustaceans. See Elevating Mushrooms to Food Group Status and Why Crickets Are Great for the Gut Microbiome.
Chitosan is naturally found in the cell walls of fungi but are also produced as a functional fiber by treating shrimp and other crustacean shells with sodium hydroxide. See Elevating Mushrooms to Food Group Status.
Beta-glucans are found in some grains (mainly oats and barley, but also rye and wheat), fungi (yeast and mushrooms, particularly those mushrooms that are used medicinally like shiitake and maitake), and some types of seaweed (mainly algae). Beta-glucans are the fiber in oats that are largely responsible for their unique health benefits among grains. See Why Seaweed is Amazing! and Elevating Mushrooms to Food Group Status.
Fructans are naturally occurring in a variety of plants and are particularly high in chicory, Jerusalem artichoke and alliums (the onion family). Cruciferous vegetables contain modest amounts of fructans. See What about the Goitrogens in Cruciferous Veggies?.
Gums are a diverse group of fibers that plants secrete when they are damaged. Isolated versions are used in food manufacturing as thickening and gelling agents (like guar gum and xanthum gum). See Is It Paleo? Guar Gum, Xanthan Gum and Lecithin, Oh My!.
Mucilages are particularly concentrated in cacti and other succulents (like aloe), many types of seaweed (like agar agar algae), flax, chia and psyllium. They can also be found in relatively large amounts in a variety of fruits and vegetables, including plantains, bananas, taro root, cassava, and berries. See Mucilaginous Fiber: The Good, the Bad, and the Gooey and The Verdict on Psyllium Husks: Not Paleo!.
Resistant starch is divided into four subgroups: RS1 is rich in grains, legumes, and seeds; RS2 is found in most roots and tubers, and particularly high in green bananas, green plantains, and raw potatoes; RS3 is rich in cooked and cooled roots and tubers, particularly potatoes, as well as cooked and cooled rice; RS4 is the product of enzymatically or chemically modified starches sold under various brand names. See also Resistant Starch: It’s Not All Sunshine and Roses.
Because of their varying fiber types (and other food compounds that influence gut microbial composition like micronutrients, phytochemicals, proteins and fats), different families of fruits and vegetables are independently beneficial for the gut microbiome. See also The Fiber Manifesto-Part 2 of 5: The Many Types of Fiber
That means that beyond aiming for 8+ servings of fresh vegetables and fruits daily (see also The Importance of Vegetables), it’s important to hit as many of the different families of vegetables and fruits each day, ideally cycling through all of them every two days: cruciferous vegetables, leafy vegetables, roots and tubers, mushrooms, alliums, apple family, citrus, berries, nuts and seeds, etc.
Resistant Starch-Rich Foods as Microbiome Superfoods
Resistant starch is classified as a fiber because amylase, the enzyme that breaks starch into individual glucose units, doesn’t work on this type of starch.
Resistant starch is insoluble yet highly fermentable, and is divided into four subgroups: RS1, which is physically inaccessible due to being bound within cell walls; RS2, which is tightly packed ungelatinized granules found in certain raw starchy foods; RS3 (retrograded amylose), which is formed when certain starchy foods are cooked and then cooled down; and RS4, which is formed via a manmade chemical process. See also Resistant Starch: It’s Not All Sunshine and Roses
In general, resistant starch is famous for feeding short-chain-fatty-acid-producing bacteria and enhancing levels of butyric acid. In a human study, RS2 was shown to increase the abundance of Ruminococcus bromii and Eubacterium rectale, whereas RS4 increased Bifidobacterium adolescentis and Parabacteroides distasonis. Long-term feeding of RS1 and RS2 in rats showed that both types increased the abundance of anaerobes, the levels of Bifidobacteria, and total SCFAs in the cecum; meanwhile, RS2 (but not RS1) enhanced levels of Lactobacillus, Streptococci, and Enterobacteria. In pigs, RS3 has been shown to increase the abundance of Faecalibacterium prausnitzii while reducing levels of E. coli and Pseudomonas species. Interestingly, Ruminococcus bromii plays a keystone role in the degradation of resistant starch, releasing breakdown products that are then utilized by other microbes in the gut.
Two Important Probiotic Bacteria: Bifidobacteria and Roseburia
Hundreds of beneficial probiotic species of bacteria (as well as fungi like yeast and archaea, which we’ll come back to) have been well studied in terms of their roles in the gut microbiome and human health in general. I want to focus in on two genera of bacteria that are particularly relevant to this new paper.
The Bifidobacteria genus exerts a range of beneficial effects on human health, including producing vitamins, inhibiting pathogens from colonizing or infecting the gut mucosa, helping regulate the microbiome’s homeostasis, modulating local and systemic immune responses, repressing potentially carcinogenic enzymatic activities among different bacteria, and facilitating the bioconversion of various dietary compounds into bioactive forms. In a variety of studies, Bifidobacteria have been shown to improve the gut barrier function, suppress E. coli, improve glucose tolerance, reduce low-grade inflammation, and reduce endotoxemia induced by high-fat diets. As another benefit, because Bifidobacteria produce lactic acid instead of gas, people with higher levels tend to have less flatulence and digestive problems!
There are 39 identified species of Bifidobacteria, which represent 3-6% of health adult fecal flora. Their favorite foods are resistant starch 2, resistant starch 4, oligosaccharides from plants and milk, and hexose.
Let me emphasize: Bifidobacterium are critically important to human health. If you see an argument dismissing this paper because somehow low-carb diets or low-carb Paleo benefits make up for missing Bifidobacteria, that is unequivocally false.
The Roseburia genus are butyrate-producing bacteria that are implicated in maintaining gut barrier health and immune regulation, with strong anti-inflammatory properties. Reduced levels of Roseburia are associated with inflammatory bowel disease (Roseburia actually suppress the pathogenesis of Crohn’s disease), irritable bowel syndrome, obesity, type 2 diabetes, cardiovascular disease, neurological diseases, autoimmune disease, asthma and allergies—likely mediated through higher intestinal permeability and inflammation.
There are five known species of Roseburia (R. intestinalis, R. hominis, R. inulinivorans, R. faecis and R. cecicola) and their favorite foods are beta-glucans, fructans, pectin and resistant starch.
The Deal with TMAO
So, where does TMAO fit into the microbiome?
In recent years, trimethylamine-N-oxide (TMAO) has emerged as a possible new risk factor for cardiovascular disease, with potential to other conditions as well (such as chronic kidney disease, chronic heart failure, and colorectal cancer). For instance, a meta-analysis using 11 prospective studies found that higher circulating levels of TMAO were associated with a 23% increased risk of cardiovascular events and a 55% increased risk of all-cause mortality. This little molecule gets produced from the microbial metabolism of choline, lecithin, and carnitine (from our diet) into trimethylamine (TMA), which the liver then oxidizes into TMAO. Once it’s in our bodies, TMAO gets transported to different tissues and can potentially accumulate.
However, our levels of TMAO aren’t just a matter of how much free TMAO or TMAO precursors we ingest! Gut bacteria, especially the genus Prevotella, is a key mediator between diet and the amount of TMAO in our blood. In one study, researchers found that participants with gut microbiomes dominated by Prevotella were the ones who produced the most TMA (and therefore TMAO, after it reached the liver) from the carnitine they consumed. Those with microbiomes high in Bacteroides rather than Prevotella saw dramatically less conversion to TMA and TMAO.
So far, the list of TMAO-producing bacteria also includes multiple Clostridium species, Desulfovibrio desulfuricans, Providencia rettgeri, Edwardsiella targa, Escherichia fergusonii, Anaerococcus hydrogenalis, Proteus penneri, Firmicutes, and Proteobacteria. In other words, we can’t look at TMAO without also looking at the composition of our gut microbiota!
TMAO: Symptom or Cause of Heart Disease?
Despite some compelling associations with disease and mortality, there’s still a lot of controversy over whether TMAO has a causal relationship with the conditions it’s been associated with. On one hand, we have identified some plausible mechanisms for its role in disease, especially heart disease. For example, TMAO appears to increase the number of scavenger receptors in macrophages, resulting in greater binding to LDL particles and subsequent foam cell formation (foam cells play a major role in the progression of atherosclerotic plaque buildup!). TMAO also interferes with sterol transportation and bile acid metabolism, which can further contribute to the development of heart disease. And, TMAO may increase platelet activity, which can raise the risk of thrombosis by promoting excessive coagulation in the blood.
But despite these possible mechanisms, the literature is still mixed when it comes to how elevated TMAO plays out in real life! Along with studies showing a link between high TMAO levels and disease or mortality, many studies have failed to find any predictive value for TMAO on cardiovascular events, chronic kidney disease, or heart failure.
It’s possible that high TMAO occurs as a result of some of these diseases, rather than as a causative factor (high TMAO makes sense in the case of kidney failure, for instance, because the kidneys are the major site of circulating TMAO clearance, and their compromised function would naturally lead to a buildup of TMAO).
It’s also very possible that gut microbiota compositions that contribute to chronic disease also happen to result in more TMA and TMAO production, making TMAO a marker for disease states rather than a causal risk factor. Overall, the jury’s still out!
The Fish Paradox
One of the major monkey wrenches in the whole TMAO story is a fishy one (pun intended). Seafood—famously considered heart-healthy—is one of the most abundant sources of free TMAO, and also contains TMAO precursors. And we’d be hard pressed to find a study that shows seafood is bad for our cardiovascular health (indeed, the vast majority of research shows that fish is one of the best things we can eat for our hearts!). Physiologically, TMAO helps fish survive in their marine environments by increasing buoyancy, acting as a form of antifreeze (by increasing osmotic concentration), and protecting tissue proteins against destabilizing forces. The degradation of TMAO into TMA is also what gives seafood its characteristic fishy odor! TMAO levels can vary dramatically between different species of fish (and even vary within the same species depending on the season), but in general, deep-sea fish and shellfish tend to be higher in TMAO than shallow water fish and shellfish, likely because of the role TMAO plays in protecting against pressure-induced protein damage.
Research has shown that following the consumption of seafood, blood levels of TMAO levels rise to significantly higher levels than after the consumption of beef or eggs. In one study, 40 participants were fed meals containing cod fish, eggs, beef, or a fruit control in random order, with week-long washout periods between each intervention. After the fish meal, participants’ plasma TMAO rose up to 62 times higher than after the beef, eggs, or fruit meals. These levels peaked at 2 hours post-meal and remained elevated for the remainder of the 6-hour study period. The rise in TMAO levels started within 15 minutes following fish consumption, indicating the TMAO was being directly absorbed rather than undergoing conversion in the gut by bacteria. This same study found dramatic variations in TMAO response after eating eggs or beef. Compared to baseline, TMAO levels ranged anywhere from a 30% decrease to a 270% increase!
Food vs. Microbiome Sources of TMAO
So, why would we see such extreme variations in TMAO levels after eating the same foods? The answer is, not surprisingly, bacteria! Stool analysis showed that compared to low TMAO producers, high TMAO producers had some important microbiota differences, including lower alpha-diversity, different species compositions, and a higher ratio of Firmicutes to Bacteroidetes (about 2:1, versus a 1:1 ratio for the low producers). And very importantly, as we’ll see in a moment, the Archaea phylum was completely absent in the microbiota of the high TMAO producers, but was represented among the low TMAO producers.
This study provided some important pieces for the TMAO puzzle. Along with demonstrating that fish (at least in the form of cod) yields vastly higher levels of TMAO and TMAO metabolites than beef or eggs, the study demonstrated that TMAO can be absorbed intact from foods like fish without involvement of the gut microbiota. That means that the level of TMAO we have in our bodies isn’t just a result of our gut microbiota churning it out from precursors, but can also be influenced by the direct consumption of TMAO from food. And, that could mean that high circulating TMAO from seafood potentially indicates a much different (AKA lower!) risk profile than high TMAO produced by disease-associated microbes.
So, as much as is still up in the air about TMAO, one thing seems pretty likely: we don’t want a gut microbiome that produces a lot of it. Whether or not TMAO itself turns out to be a major risk factor or just a red herring, and whether or not our circulating levels are a cause or consequence of specific health conditions, a high-TMAO-generating microbiota seems to be consistent with greater disease risk.
Archaea: A Microbiome Missing Piece
Whenever we hear about the microbiota, it’s usually all about the bacteria, bacteria, and more bacteria! But, while bacteria might be numerically dominant among the microbes in our gut, they’re definitely not the only residents there. Another type of single-celled organism that call our GI tracts home are archaea. And, these little guys are incredibly important!
Archaea (sometimes called archaebacteria) are strict anaerobes that live in various mucosal sites throughout the body, including the intestinal mucosa. We aren’t born with archaea inside us, but we acquire them from the environment throughout life: by the time children are school-aged, archaea are almost universally present in the gut, and levels continue to increase with age (with the highest occurrence and diversity of archaea being found in older adults). Along with lacking lipopolysaccharide (meaning archaea won’t contribute to our endotoxin load), archaea is also the only domain of life that doesn’t include any known pathogens, which is pretty cool!
Archaea degrade TMA and TMAO
One important subtype of archaea are the methanogens, which produce methane gas as a byproduct of hydrogen reduction. Up to 95% of human guts harbor the methanogenic archaea Methanobrevibacter smithii and Methanosphaera stadtmanae, at varying levels. While the idea of producing methane might not sound very pleasant, some of these archaea (in particular, an order of methanogens called the Methanomassiliicoccales) actually play an integral role in reducing our TMAO production. Along with being able to use carbon dioxide, formate, and methanol (all released by bacteria breaking down food and other organic matter in the gut), these archaea can use methyl compounds like TMA and TMAO to generate methane. And that means that the archaea in our gut actually deplete the pool of TMA we have available to be converted into TMAO (along with any free TMAO from foods like seafood). So, all that TMA generated by Prevotella, or entering our body from fish consumption? Archaea can help wipe some of it out!
The TMAO-reducing effects of archaea is far from just speculative, too. In a study of ELDERMET subjects, the fecal TMA concentration in people with TMA-metabolizing archaea was significantly lower than in those without this archaea—and the difference was particularly dramatic when the abundance of Methanomassiliicoccales was greater than 10^8 cells per gram of stool. This role of archaea is so exciting that some scientists are proposing a new class of probiotics called archaeabiotics, which could help reduce our TMAO levels without us needing to cut back on choline and other important nutrients!
Importantly, methanogenic archaea have an important interactive relationship with bacteria in the gut, which often takes the form of what scientists call syntrophy (where two organisms participate in consuming a substance that neither one can catabolize on its own). And, it appears that archaea are particularly chummy with the important probiotic bacteria Bifidobacteria. For example, mixed cultures of M. smithii and Bifidobacteria bifidum have been shown to collectively produce methane from glucose, and in females with gut Methanobacteriales levels higher than 0.71%, there’s a significantly higher mean abundance of Bifidobacteriaceae. And as we’ve already seen, healthy levels of Bifidobacteria are super important!
Archaea Thrive When We Eat Carbs!
So, how do we keep our archaea happy and thriving? Scientists are just at the beginning stages of understanding how diet impacts our archaea colonies (after all, archaea are relative newcomers to the microbiota research scene compared to bacteria!), but here’s what we know so far. In children, organic dairy (especially organic yogurt and organic milk) has been associated with the initial colonization of M. smithii, due to organic dairy serving as a vehicle for delivering it to our guts. And, some methanogens degrade methanol, which gets produced when bacteria degrade pectin in fruits—thus suggesting that archaea might benefit from including fruit in our diets! In Chinese goats, eating a high-grain diet appears to suppress methanogenic archaea relative to a high-hay diet—possibly due to the pH-lowering effect of grains in the rumen (which can then suppress methanogenic archaea that are sensitive to low pH environments). Obviously, we’re not Chinese goats, but it would certainly be interesting if a high-grain diet in humans had a similar effect!
More broadly, though, in humans, Methanobrevibacter abundance is positively associated with higher carbohydrate consumption (both recent and long-term), and negatively associated with recent consumption of fat (especially vegetable fat and polyunsaturated fat intake) and amino acids. Although more research is definitely needed, the picture getting painted so far is that archaea benefit from a variety of plant polysaccharides, and not so much from animal-based diets.
However, this isn’t because the archaea themselves eat carbohydrate. In fact, methanogenic archaea have an almost complete lack of enzymes for breaking down complex carbohydrates into simple sugars. What does appear to be happening is that archaea thrive off the metabolic products of carbohydrate-loving bacteria, and therefore are still dependent on dietary carbohydrate for their own survival!
The Study: Long-term Paleolithic diet is associated with lower resistant starch intake, different gut microbiota composition and increased serum TMAO concentrations
Whew! Now that we’ve covered the necessary background, let’s take a look at what this study is all about!
Researchers recruited a total of 44 participants who self-reported following a Paleo diet for over a year, along with 47 controls who more or less followed the national dietary recommendations of Australia (where the study was conducted). Within the Paleo group, participants were further divided based on how strictly they followed the Paleo framework (as gauged by the exclusion of grain and dairy products): 22 people fell into the “strict Paleo” group (less than one serving of grains and/or dairy per day), and 22 people fell into the “pseudo-Paleo” group (more than one serving of grains and/or dairy per day). (This is important, because “real-world” Paleo includes a variety of interpretations about what Paleo actually means, including how strictly to adhere to the diet—so a pseudo-Paleo group might be closer to reality for a lot of people!)
The study excluded anyone who’d taken antibiotics within the past six months, who had any type of GI tract surgery, who had past or present digestive disorders, who used cholesterol or blood pressure lowering medications, or who had been diagnosed with cardiovascular disease. This helped make sure the results weren’t confounded by preexisting health conditions or drugs, and allowed the researchers to better isolate the effects of the participants’ diets.
To ensure accurate dietary data, the researchers had participants undergo three-day weighed diet records (including two weekdays and one weekend day), which were then validated using urine nitrogen tests (which could detect whether participants were over- or under-reporting their protein intake) and the Goldberg cut point (which can identify which participants were under-reporting their energy intake, through the ratio of energy intake to basal metabolic rate). Participants who appeared to inaccurately report both their protein and energy intake were deemed unreliable dietary reporters (this ended up being two people from the strict Paleo group and three people from the control group).
Paleo Diet Adherents Had Increased TMAO
Now, the headline-grabbing finding. In the strict Paleo group, serum TMAO was a whopping 9.53 µM, the pseudo-Paleo group averaged 5.47 µM, and the control group averaged 3.93 µM. Higher TMAO levels were associated positively with red meat intake and negatively with grain intake.
Whether TMAO is a causative agent for disease or a marker for a disease-associated microbiota, those are some scary numbers—especially for the strict Paleo group!
What Study Participants Were Actually Eating
So, what were the Paleo groups actually eating? Here’s what the data showed!
Not surprisingly, both Paleo groups ate more protein than the controls (118 and 102.7 grams per day for the strict Paleo group and pseudo-Paleo group, respectively, compared to 92 grams for the controls), less carbohydrate (99 and 81.4 grams per day for the strict Paleo group and pseudo-Paleo group, respectively, compared to 202.6 grams for the controls), less sugar (51.8 and 44 grams per day for the Paleo groups, and 75.6 grams for the controls), and more fat—with the increase mostly coming from saturated and monounsaturated forms (117.9 total fat grams per day for the strict Paleo group, 133.1 grams for the pseudo-Paleo group, and 82.5 grams for the controls).
Importantly, total dietary fiber was adequate (and very similar!) for both the control group and the strict Paleo group—29.7 grams and 27.4 grams daily, respectively, which falls within the recommended daily intake of 25-30 grams for adults. The pseudo-Paleo group averaged 20.8 grams of fiber each day, which is still more than most people consume! For the Paleo groups, much of their fiber came from vegetables, with the strict Paleo group eating 6.7 servings of veggies per day and the pseudo-Paleo group averaging 4.3, compared to the control group’s 3.93. (We could definitely argue that the official recommendations for fiber are still too low for optimal health, but the point here is, these study participants weren’t slacking on the non-starchy veggies!)
While the control group averaged 4.5 – 14.2 grams of resistant starch per day, largely from grains (those are estimated minimum and maximum amounts, since the same foods can vary in resistant starch content), the strict Paleo group averaged only 2.6 – 6.1 grams per day, and the pseudo-Paleo group got a mere 1.3 – 2.9 grams of resistant starch. That’s a significant drop off!
Low-Carb Paleo Effects on the Microbiome
Remember that one of the favorite foods of Bifidobacteria is resistant starch? And that Roseburia also likes to munch on carbohydrates like beta-glucans? Maybe we shouldn’t be surprised that this study showed a significant decrease in these important bacteria among both Paleo groups.
Likewise, the relative abundance of Hungatella was significantly higher among the Paleo subjects. After adjusting for age, gender, stool frequency, and body fat, Hungatella abundance was significantly negatively associated with grain intake among the study’s participants, and was also significantly negatively correlated with Bifidobacteria and Roseburia abundance. Although we don’t have a lot of information about Hungatella in relation to human health (not yet, anyway!), we do know that some species originating from the genus Hungatella are associated with choline consumption and TMA production, including at least one species identified in this study. The researchers speculated that some components of grains and/or whole grains either interfere with Hungatella’s TMA production or prevent it from dominating in the gut. And, these components might not be resistant starch, since neither Hungatella nor TMAO was significantly associated with resistant starch intake!
Resistant Starch and Total Carb Intake Are Important!
One of the things that makes this study so interesting (and important!) is the fact that fiber and vegetable intake was relatively high for both Paleo groups. Often, when we talk about how ketogenic diets or low-carb or low-starch Paleo might affect the gut microbiome, we’re given a false sense of security thinking we’ll be fine as long as we eat plenty of fiber from leafy greens; see also How Ketogenic Diet Wreaks Havoc on Your Gut. As this study indicates, low-starch veggies alone are not enough to maintain a robust, diverse gut microbiome! The Paleo subjects clearly weren’t ingesting a broad enough array of fibers and starches to support some very important bacterial populations.
Given all that, can we just add some supplemental resistant starch to otherwise low-carb diet and call it a day?
Actually, the answer here seems to be no! Consistent with my post Resistant Starch: It’s Not All Sunshine and Roses, the research shows that isolated resistant starch doesn’t bring the same range of benefits as resistant starch from whole-food sources. And what’s more, when it comes to TMAO, supplemental resistant starch may even be counterproductive in the context of a low-carb and/or high fat diet. In a human cross-over trial from 2016, for example, 52 adults consumed four different diets in random orders—a low resistant starch, higher carbohydrate diet; a low resistant starch, lower carbohydrate diet; a high resistant starch, higher carbohydrate diet; and a high resistant starch, lower carbohydrate diet (with resistant starch coming from Hi-Maize 260, supplying RS2). Intriguingly, the highest TMAO levels occurred when subjects were eating the high resistant starch, lower carbohydrate diet, despite dietary levels of carnitine and choline being less on that diet compared to the low resistant starch periods. The researchers proposed that a high isolated resistant starch intake, in the presence of an overall lower carbohydrate diet, shifted the microbiota towards greater TMAO generation. Likewise, studies in rodents have shown that high fat consumption (which often goes hand-in-hand with low-carbohydrate diets), in the amount of of 42% of total energy, partially counteracts the beneficial effects of RS2 by suppressing levels of beneficial bacteria. So, low-carb diets can be a double whammy against our gut microbiota, both by failing to supply a wide range of fiber and starch types and by overloading our guts with levels of fat that become harmful to bacteria. (Don’t worry; we aren’t calling fat bad here—but a balanced intake of macronutrients seems to be where the evidence is pointing for optimal health!)
Other studies support the idea that resistant starch is most health-promoting in conjunction with other dietary carbohydrates. In pigs, resistant starch alone (in the form of RS2) was shown to get rapidly fermented in the proximal (beginning part) of the colon, while failing to reach further down into the distal (lower) colon—resulting in only a small portion of the colon receiving fermentation benefits. But, when additional carbohydrate in the form of wheat bran (a soluble non-starch polysaccharide) was included in the pigs’ diets, the amount of resistant starch getting fermented between the lower colon and feces nearly doubled—indicating that the bulk from the wheat bran was helping spread fermentation further down through the colon, flooding a much greater area with cancer-protective butyrate. The addition of wheat seed (RS1) to supplemental green banana flour and high-amylose starch (RS2) has been shown to help spread fermentation throughout the entire colon, as indicated by a decrease in fecal pH (which is a good thing!).
When it comes to low-carb Paleo diets, it’s easy to see how a similar effect could occur. Cutting out sources of bulky fermentable carbohydrate (like root veggies and legumes) limits how far isolated resistant starch can spread, resulting in bacteria in the proximal colon gobbling it up and leaving none for microbes further down the colon. Likewise, given what we know about the role of methanogenic archaea in regulating TMAO levels and interacting with other microbes like Bifidobacteria (as well as how much methanogenic archaea likes carbohydrates and doesn’t like fat!), we might suspect that low-carb diets can also enhance TMAO production by suppressing archaea growth.
As further confirmation, the main study we’ve been discussing in this article found that TMAO levels were more strongly negatively associated with grain intake than with resistant starch intake. That doesn’t mean we all need to eat grains to be healthy, but it does imply that diverse components of starchy plant foods (such as the other forms of fiber and carbohydrate they contain) contribute to a healthy microbiome, even more so than resistant starch on its own.
Short-Term Vs. Long-Term Microbiome Shifts
We should also stress the importance of the long-term nature of this study! While shorter dietary trials can be very useful (and in some cases, are the only studies we have at our disposal), they can’t capture potential health issues that develop months or years down the line (such as gradual changes in the core gut microbiota composition). That’s particularly relevant here, because the same researchers who conducted this study previously published a similar one, randomizing 22 women to a Paleo diet for four weeks and 17 women to a diet in line with Australian health recommendations. In that study, there wasn’t a significant change in TMAO concentration compared to the control group, despite a lower intake of resistant starch and higher intake of meat and eggs among the Paleo dieters. While those findings could have been due to the small sample size and limited data for resistant starch content of foods (making it difficult to precisely calculate resistant starch intake), it’s also possible that the Paleo group hadn’t yet exhibited some longer-term microbiota shifts that lead to higher TMAO generation as seen in the more recent study.
Indeed, the field of microbiota research has shown us that while some microbial changes happen rapidly when we alter our diet, others can occur on a more gradual basis. So, only using participants who had been eating Paleo for over a year gives this study greater insight into the full effects that low-carb Paleo has on the gut microbiota.
The Bottom Line: Paleo Should Not Be Low-Carb
Some people have seen this paper as an attack on red meat, which, given the TMAO link, is a valid concern (see also The Link Between Meat and Cancer). But what this paper is actually making a case for is that starch-free diets are a problem. Don’t get me wrong: fibrous, low-starch veggies are fantastic, and we should be filling our plates with them on the daily—but not at the exclusion of Paleo starches! Root veggies rich in resistant starch are consistently showing up as a vital component of a nutrient-dense Paleo diet, and there are no real “hacks” to get around that (see also Why Root Veggies Are Great for the Gut Microbiome and Resistant Starch: It’s Not All Sunshine and Roses).
When we combine this information with an examination of the non-metabolic roles that insulin plays (another rationale for moderate [not low] carb intake, see The Case for More Carbs: Insulin’s NonMetabolic Roles in the Human Body and How Many Carbs Should We Eat?), the potential problems of too-high-fat intake (not that we wan’t to eat low-fat; see Saturated Fat: Healthful, Harmful, or Somewhere In Between?, Adverse Reactions to Ketogenic Diets: Caution Advised), and understanding that micronutrient sufficiency is most easily attained with a balanced macronutrient diet (see The Diet We’re Meant to Eat, Part 3: How Much Meat versus Veggies?, The Importance of Nutrient Density, and Carbs Vs. Protein Vs. Fat: Insight from Hunter-Gatherers), it’s becoming harder and harder to make a compelling case against moderate carbohydrate intake, 30 to 60% of total calories, from whole food sources.
Citations
Bergeron N, et al. “Diets high in resistant starch increase plasma levels of trimethylamine-N-oxide, a gut microbiome metabolite associated with CVD risk.” Br J Nutr. 2016 Dec;116(12):2020-2029. doi: 10.1017/S0007114516004165. Epub 2016 Dec 20.
Borrel G, et al. “Genomics and metagenomics of trimethylamine-utilizing Archaea in the human gut microbiome.” ISME J. 2017 Sep;11(9):2059-2074. doi: 10.1038/ismej.2017.72. Epub 2017 Jun 6.
Charrier JA, et al. “High fat diet partially attenuates fermentation responses in rats fed resistant starch from high-amylose maize.” Obesity (Silver Spring). 2013 Nov;21(11):2350-5. doi: 10.1002/oby.20362. Epub 2013 Jul 2.
Cho, CE, et al. “Trimethylamine‐N‐oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: A randomized controlled trial” M. A., Mol. Nutr. Food Res. 2016, 1600324. Doi: 10.1002/mnfr.201600324
Dridi B, et al. “High prevalence of Methanobrevibacter smithii and Methanosphaera stadtmanae detected in the human gut using an improved DNA detection protocol.” PLoS One. 2009 Sep 17;4(9):e7063. doi: 10.1371/journal.pone.0007063.
Dridi B, et al. “High prevalence of Methanobrevibacter smithii and Methanosphaera stadtmanae detected in the human gut using an improved DNA detection protocol.” PLoS One. 2009 Sep 17;4(9):e7063. doi: 10.1371/journal.pone.0007063.
Genoni, A, et al. “Long-term Paleolithic diet is associated with lower resistant starch intake, different gut microbiota composition and increased serum TMAO concentrations.” European Journal of Nutrition, 2019; DOI: 10.1007/s00394-019-02036-y
Genoni A, et al. “A Paleolithic diet lowers resistant starch intake but does not affect serum trimethylamine-N-oxide concentrations in healthy women.” Br J Nutr. 2019 Feb;121(3):322-329. doi: 10.1017/S000711451800329X. Epub 2018 Nov 13.
Govers MJ, et al. “Wheat bran affects the site of fermentation of resistant starch and luminal indexes related to colon cancer risk: a study in pigs.” Gut. 1999 Dec;45(6):840-7.
Hoffmann C, et al. “Archaea and fungi of the human gut microbiome: correlations with diet and bacterial residents.” PLoS One. 2013 Jun 17;8(6):e66019. doi: 10.1371/journal.pone.0066019.
Jin W, Cheng Y, Zhu W. “The community structure of Methanomassiliicoccales in the rumen of Chinese goats and its response to a high-grain diet.” J Anim Sci Biotechnol. 2017 Jun 1;8:47. doi: 10.1186/s40104-017-0178-0.
Qi J, et al. “Circulating trimethylamine N-oxide and the risk of cardiovascular diseases: a systematic review and meta-analysis of 11 prospective cohort studies.” J Cell Mol Med. 2018 Jan;22(1):185-194. doi: 10.1111/jcmm.13307. Epub 2017 Aug 7.
Raymann K, et al. “Unexplored Archaeal Diversity in the Great Ape Gut Microbiome.” mSphere. 2017 Feb 22;2(1). pii: e00026-17. doi: 10.1128/mSphere.00026-17.
Tamanai-Shacoori Z, et al. “Roseburia spp.: a marker of health?” Future Microbiol. 2017 Feb;12:157-170. doi: 10.2217/fmb-2016-0130.
van de Pol JA, et al. “Gut Colonization by Methanogenic Archaea Is Associated with Organic Dairy Consumption in Children.” Front Microbiol. 2017 Mar 10;8:355. doi: 10.3389/fmicb.2017.00355. eCollection 2017.
Vanderhaeghen S, Lacroix C, Schwab C. “Methanogen communities in stools of humans of different age and health status and co-occurrence with bacteria.” FEMS Microbiol Lett. 2015 Jul;362(13):fnv092. doi: 10.1093/femsle/fnv092.
Vanessa DN, et al. “Archaea: Essential inhabitants of the human digestive microbiota.” Human Microbiome Journal, 2017 3:1-8. doi.org: 10.1016/j.humic.2016.11.005.
from
https://www.thepaleomom.com/paleo-resistant-starch-and-tmao-new-study-warning-worth-heeding/
from https://myfunweightloss.blogspot.com/2019/08/paleo-resistant-starch-and-tmao-new.html
0 notes
Link
SCIENCE SIMPLIFIED:
A human study was published looking at how long-term adherence to a Paleo diet affects the gut microbiota and production of TMAO, which is linked to cardiovascular disease and some forms of cancer.
The study demonstrates that a low-carb Paleo diet increases TMAO, attributable to a decrease in probiotic bacteria from the Bifidobacterium and Roseburia genera and an increase in Hungatella species in the gut.
The dietary factors most strongly associated with the undesirable gut microbiome shift and TMAO production were total carbohydrate intake and resistant starch intake.
While the authors conclude that lack of grains are to blame, the study participants were eating mostly non-starchy vegetables (about 7 servings per day, averaging 28 grams of fiber but only 90 grams of total carbohydrates). Starchy roots and tubers are a healthy alternative to grains and would have increased the participant’s total carbohydrate intake (all slow-burning nutrient-dense carbs) as well as resistant starch intake.
The results of this study are relevant to our community and offer a stern warning against long-term low-carb implementations of the Paleo diet.
RELATED READING:
What Is the Gut Microbiome? And Why Should We Care About It?
The Case for More Carbs: Insulin’s Non-Metabolic Roles in the Human Body
Why Root Veggies Are Great for the Gut Microbiome
Whenever a new Paleo study comes out, it’s sure to stir up controversy—no matter what the findings are. “Good” findings are met with cheers from the Paleo community, while “bad” findings tend to explode in media headlines and send the Paleo community rushing to find reasons the study is poorly conducted, inaccurate, or otherwise worth dismissing.
As you know, I don’t believe in dismissing scientific findings (except for the rare occasion where flaws in how the study was designed or conducted result in retraction). Instead, I seek to understand the data in the context of the research field as a whole, seeking context and nuance while being open to adjusting my conclusions and recommendations. (I discuss the merits of different types of scientific studies as well as the problem with cherry-picking data in my Introduction to Nutritional Sciences online course.)
Recently, a human study was published looking at how long-term adherence to a Paleo diet affects the gut microbiota and TMAO. And, the headlines (both mainstream media and outlets targeting physicians) have not been flattering, for example: “Paleo Diet Increases Risk for Heart Disease”, “Paleo Diet Study Links ‘Caveman’ Regime to Heart Disease Biomarker”, and “Study Linking Paleo Diet to Increased Heart Disease Risk Strengthens Diet Industry Concerns”.
As you’re probably aware by now, I’m all about the gut microbiome, and believe it will continue to prove itself as a massive missing piece in our health puzzle! For that reason, this study is particularly interesting and important to look at (and not dismiss!).
Before we dive into the study itself, let’s review the things we need to know to make sense of the findings!
A Refresher on Fiber, Resistant Starch, and the Microbiome
The gut is a biological niche, home to a diverse array of microbes that influence nearly all aspects of human biology through their interactions with our bodies. We have a symbiotic relationship with these microbes, collectively referred to as our gut microbiome—in exchange for food and shelter, they contribute to our wellbeing by performing diverse functions essential to our health.
When we don’t have a healthy diversity of the right kinds of microbes in our gut, our entire body suffers. An unfavorable gut microbiome has been linked to conditions as wide-ranging as cancer, obesity and other metabolic problems, heart disease, anxiety, depression, autism, autoimmunity, ulcers, IBD, liver disease, systemic infections, and more. See What Is the Gut Microbiome? And Why Should We Care About It?.
I’m writing a book on the gut microbiome, so I could expound for days, but let’s focus on a few specifics that are particularly important to understanding this new paper.
Fiber Is Food for Our Gut Microbiome
If there’s one thing our gut microbes love, it’s fiber. In fact, out of all the dietary factors that can impact the gut, fiber may be the most important.
Carbohydrates, including fiber, are chains of monosaccharides (simple sugars) and of chemical derivatives of monosaccharides. Both the types of simple sugar (and their derivatives) in the chain and the ways they link together to form chains (both overall structure and the types of chemical bonds between sugar molecules) determine what type of carbohydrate it is. What separates fiber from other carbohydrates is that the way the sugars link together are not compatible with our digestive enzymes; our bodies just aren’t capable of breaking apart those types of molecular bonds. Instead, fiber passes through the digestive tract mainly intact. And once it reaches the colon, the magic begins: fiber serves as a substrate (food) for a wide range of bacteria, including some of the most important species we can harbor!
Why Different Fiber Types Feed Different Bacteria
The bacteria that live in our guts are collectively capable of producing over ten thousand different enzymes that can break down complex carbohydrates like fiber, which is pretty remarkable when you consider that we only produce about 17 different enzymes that digest carbohydrates! These enzymes belong to at least 206 different families of CAZymes (which stands for “Carbohydrate-Active enZymes”). Enzymes are typically highly specialized, breaking apart only specific molecular bonds, which is why different types of carbohydrates require different enzymes to break them apart (and why we can’t digest fiber but our gut bacteria can).
When it comes to carbohydrate degradation, some bacteria are highly specialized, producing only a few dozen CAZymes, whereas others are multitaskers, producing hundreds of CAZymes which allows them to grow on a variety of substrates and adapt to changing nutritional circumstances, thereby giving them a competitive advantage in the gut ecosystem.
Bacteria from the Bacteroides genus in general tend to be multitaskers, producing enzymes that can break down starch, pectin, hemicelluloses, and other plant carbohydrates (galactomannan, arabinogalactan, alginate, laminarin and xylans xyloglucan, rhamnogalacturonans I and II, β-glucans and glucomannan, to name a few!). Bacteroides thetaiotaomicron is an example of multitasker, considered a diet insensitive strain thanks to its ability to produce around 400 CAZymes (at least 260 of which are glycoside hydrolases) that help it thrive on pectins as well as complex carbohydrates that are produced by our own intestinal cells, such as mucin (a glycoprotein that is a major component of mucus).
In contrast, Bifidobacterium species are more specialized, producing an average of 45 CAZymes that make them highly effective at degrading high amylose starches, including resistant starch, as well as fructooligosaccharides, galactooligosaccharides, and inulin fiber. The critical consequence is that Bifidobacterium don’t survive if our diet doesn’t include sufficient amounts of these starches and fiber types.
Importance of Fiber Variety in the Diet
One of the consequences of this diversity in CAZyme production by various resident microbes is that different fermentable carbohydrates support different species in the gut. Therefore, consuming a variety of dietary fibers—various cellulose, hemicellulose, pectins, gums, fructans, glucans, mucilage, chitin, chitosan, and resistant starch fiber—best supports a diverse microbial community compared to a diet comprised of less varied fermentable carbohydrates like the Standard American Diet which is rich in refined carbohydrates.
Which foods are rich in which fiber sources?
Cellulose is found in all plants, but foods that contain particularly large amounts of cellulose include bran, legumes, nuts, peas, root vegetables, celery, broccoli, peppers, cabbage and other substantial leafy greens like collards, and apple skins. See The Fiber Manifesto-Part 2 of 5: The Many Types of Fiber
Hemicellulose is particularly high in bran, nuts, legumes, and whole grains, as well as many green and leafy vegetables.
Pectin is found in all fruits and vegetables but are particularly rich in certain fruits, including apples and citrus fruits, and are also found in legumes and nuts. See Why Fruit is a Good Source of Carbohydrates
Lignin is most commonly a component of wood, but food sources include root vegetables, vegetable filaments (like the stems of leafy greens and the strings in celery), many green, leafy vegetables, wheat, and the edible seeds of fruit (such as berry seeds and kiwi seeds). See Polyphenols: Magic Bullet or Health Hype?
Chitin is found not only in plants and fungi but also in the exoskeletons of insects and in the shells of crustaceans. See Elevating Mushrooms to Food Group Status and Why Crickets Are Great for the Gut Microbiome.
Chitosan is naturally found in the cell walls of fungi but are also produced as a functional fiber by treating shrimp and other crustacean shells with sodium hydroxide. See Elevating Mushrooms to Food Group Status.
Beta-glucans are found in some grains (mainly oats and barley, but also rye and wheat), fungi (yeast and mushrooms, particularly those mushrooms that are used medicinally like shiitake and maitake), and some types of seaweed (mainly algae). Beta-glucans are the fiber in oats that are largely responsible for their unique health benefits among grains. See Why Seaweed is Amazing! and Elevating Mushrooms to Food Group Status.
Fructans are naturally occurring in a variety of plants and are particularly high in chicory, Jerusalem artichoke and alliums (the onion family). Cruciferous vegetables contain modest amounts of fructans. See What about the Goitrogens in Cruciferous Veggies?.
Gums are a diverse group of fibers that plants secrete when they are damaged. Isolated versions are used in food manufacturing as thickening and gelling agents (like guar gum and xanthum gum). See Is It Paleo? Guar Gum, Xanthan Gum and Lecithin, Oh My!.
Mucilages are particularly concentrated in cacti and other succulents (like aloe), many types of seaweed (like agar agar algae), flax, chia and psyllium. They can also be found in relatively large amounts in a variety of fruits and vegetables, including plantains, bananas, taro root, cassava, and berries. See Mucilaginous Fiber: The Good, the Bad, and the Gooey and The Verdict on Psyllium Husks: Not Paleo!.
Resistant starch is divided into four subgroups: RS1 is rich in grains, legumes, and seeds; RS2 is found in most roots and tubers, and particularly high in green bananas, green plantains, and raw potatoes; RS3 is rich in cooked and cooled roots and tubers, particularly potatoes, as well as cooked and cooled rice; RS4 is the product of enzymatically or chemically modified starches sold under various brand names. See also Resistant Starch: It’s Not All Sunshine and Roses.
Because of their varying fiber types (and other food compounds that influence gut microbial composition like micronutrients, phytochemicals, proteins and fats), different families of fruits and vegetables are independently beneficial for the gut microbiome. See also The Fiber Manifesto-Part 2 of 5: The Many Types of Fiber
That means that beyond aiming for 8+ servings of fresh vegetables and fruits daily (see also The Importance of Vegetables), it’s important to hit as many of the different families of vegetables and fruits each day, ideally cycling through all of them every two days: cruciferous vegetables, leafy vegetables, roots and tubers, mushrooms, alliums, apple family, citrus, berries, nuts and seeds, etc.
Resistant Starch-Rich Foods as Microbiome Superfoods
Resistant starch is classified as a fiber because amylase, the enzyme that breaks starch into individual glucose units, doesn’t work on this type of starch.
Resistant starch is insoluble yet highly fermentable, and is divided into four subgroups: RS1, which is physically inaccessible due to being bound within cell walls; RS2, which is tightly packed ungelatinized granules found in certain raw starchy foods; RS3 (retrograded amylose), which is formed when certain starchy foods are cooked and then cooled down; and RS4, which is formed via a manmade chemical process. See also Resistant Starch: It’s Not All Sunshine and Roses
In general, resistant starch is famous for feeding short-chain-fatty-acid-producing bacteria and enhancing levels of butyric acid. In a human study, RS2 was shown to increase the abundance of Ruminococcus bromii and Eubacterium rectale, whereas RS4 increased Bifidobacterium adolescentis and Parabacteroides distasonis. Long-term feeding of RS1 and RS2 in rats showed that both types increased the abundance of anaerobes, the levels of Bifidobacteria, and total SCFAs in the cecum; meanwhile, RS2 (but not RS1) enhanced levels of Lactobacillus, Streptococci, and Enterobacteria. In pigs, RS3 has been shown to increase the abundance of Faecalibacterium prausnitzii while reducing levels of E. coli and Pseudomonas species. Interestingly, Ruminococcus bromii plays a keystone role in the degradation of resistant starch, releasing breakdown products that are then utilized by other microbes in the gut.
Two Important Probiotic Bacteria: Bifidobacteria and Roseburia
Hundreds of beneficial probiotic species of bacteria (as well as fungi like yeast and archaea, which we’ll come back to) have been well studied in terms of their roles in the gut microbiome and human health in general. I want to focus in on two genera of bacteria that are particularly relevant to this new paper.
The Bifidobacteria genus exerts a range of beneficial effects on human health, including producing vitamins, inhibiting pathogens from colonizing or infecting the gut mucosa, helping regulate the microbiome’s homeostasis, modulating local and systemic immune responses, repressing potentially carcinogenic enzymatic activities among different bacteria, and facilitating the bioconversion of various dietary compounds into bioactive forms. In a variety of studies, Bifidobacteria have been shown to improve the gut barrier function, suppress E. coli, improve glucose tolerance, reduce low-grade inflammation, and reduce endotoxemia induced by high-fat diets. As another benefit, because Bifidobacteria produce lactic acid instead of gas, people with higher levels tend to have less flatulence and digestive problems!
There are 39 identified species of Bifidobacteria, which represent 3-6% of health adult fecal flora. Their favorite foods are resistant starch 2, resistant starch 4, oligosaccharides from plants and milk, and hexose.
Let me emphasize: Bifidobacterium are critically important to human health. If you see an argument dismissing this paper because somehow low-carb diets or low-carb Paleo benefits make up for missing Bifidobacteria, that is unequivocally false.
The Roseburia genus are butyrate-producing bacteria that are implicated in maintaining gut barrier health and immune regulation, with strong anti-inflammatory properties. Reduced levels of Roseburia are associated with inflammatory bowel disease (Roseburia actually suppress the pathogenesis of Crohn’s disease), irritable bowel syndrome, obesity, type 2 diabetes, cardiovascular disease, neurological diseases, autoimmune disease, asthma and allergies—likely mediated through higher intestinal permeability and inflammation.
There are five known species of Roseburia (R. intestinalis, R. hominis, R. inulinivorans, R. faecis and R. cecicola) and their favorite foods are beta-glucans, fructans, pectin and resistant starch.
The Deal with TMAO
So, where does TMAO fit into the microbiome?
In recent years, trimethylamine-N-oxide (TMAO) has emerged as a possible new risk factor for cardiovascular disease, with potential to other conditions as well (such as chronic kidney disease, chronic heart failure, and colorectal cancer). For instance, a meta-analysis using 11 prospective studies found that higher circulating levels of TMAO were associated with a 23% increased risk of cardiovascular events and a 55% increased risk of all-cause mortality. This little molecule gets produced from the microbial metabolism of choline, lecithin, and carnitine (from our diet) into trimethylamine (TMA), which the liver then oxidizes into TMAO. Once it’s in our bodies, TMAO gets transported to different tissues and can potentially accumulate.
However, our levels of TMAO aren’t just a matter of how much free TMAO or TMAO precursors we ingest! Gut bacteria, especially the genus Prevotella, is a key mediator between diet and the amount of TMAO in our blood. In one study, researchers found that participants with gut microbiomes dominated by Prevotella were the ones who produced the most TMA (and therefore TMAO, after it reached the liver) from the carnitine they consumed. Those with microbiomes high in Bacteroides rather than Prevotella saw dramatically less conversion to TMA and TMAO.
So far, the list of TMAO-producing bacteria also includes multiple Clostridium species, Desulfovibrio desulfuricans, Providencia rettgeri, Edwardsiella targa, Escherichia fergusonii, Anaerococcus hydrogenalis, Proteus penneri, Firmicutes, and Proteobacteria. In other words, we can’t look at TMAO without also looking at the composition of our gut microbiota!
TMAO: Symptom or Cause of Heart Disease?
Despite some compelling associations with disease and mortality, there’s still a lot of controversy over whether TMAO has a causal relationship with the conditions it’s been associated with. On one hand, we have identified some plausible mechanisms for its role in disease, especially heart disease. For example, TMAO appears to increase the number of scavenger receptors in macrophages, resulting in greater binding to LDL particles and subsequent foam cell formation (foam cells play a major role in the progression of atherosclerotic plaque buildup!). TMAO also interferes with sterol transportation and bile acid metabolism, which can further contribute to the development of heart disease. And, TMAO may increase platelet activity, which can raise the risk of thrombosis by promoting excessive coagulation in the blood.
But despite these possible mechanisms, the literature is still mixed when it comes to how elevated TMAO plays out in real life! Along with studies showing a link between high TMAO levels and disease or mortality, many studies have failed to find any predictive value for TMAO on cardiovascular events, chronic kidney disease, or heart failure.
It’s possible that high TMAO occurs as a result of some of these diseases, rather than as a causative factor (high TMAO makes sense in the case of kidney failure, for instance, because the kidneys are the major site of circulating TMAO clearance, and their compromised function would naturally lead to a buildup of TMAO).
It’s also very possible that gut microbiota compositions that contribute to chronic disease also happen to result in more TMA and TMAO production, making TMAO a marker for disease states rather than a causal risk factor. Overall, the jury’s still out!
The Fish Paradox
One of the major monkey wrenches in the whole TMAO story is a fishy one (pun intended). Seafood—famously considered heart-healthy—is one of the most abundant sources of free TMAO, and also contains TMAO precursors. And we’d be hard pressed to find a study that shows seafood is bad for our cardiovascular health (indeed, the vast majority of research shows that fish is one of the best things we can eat for our hearts!). Physiologically, TMAO helps fish survive in their marine environments by increasing buoyancy, acting as a form of antifreeze (by increasing osmotic concentration), and protecting tissue proteins against destabilizing forces. The degradation of TMAO into TMA is also what gives seafood its characteristic fishy odor! TMAO levels can vary dramatically between different species of fish (and even vary within the same species depending on the season), but in general, deep-sea fish and shellfish tend to be higher in TMAO than shallow water fish and shellfish, likely because of the role TMAO plays in protecting against pressure-induced protein damage.
Research has shown that following the consumption of seafood, blood levels of TMAO levels rise to significantly higher levels than after the consumption of beef or eggs. In one study, 40 participants were fed meals containing cod fish, eggs, beef, or a fruit control in random order, with week-long washout periods between each intervention. After the fish meal, participants’ plasma TMAO rose up to 62 times higher than after the beef, eggs, or fruit meals. These levels peaked at 2 hours post-meal and remained elevated for the remainder of the 6-hour study period. The rise in TMAO levels started within 15 minutes following fish consumption, indicating the TMAO was being directly absorbed rather than undergoing conversion in the gut by bacteria. This same study found dramatic variations in TMAO response after eating eggs or beef. Compared to baseline, TMAO levels ranged anywhere from a 30% decrease to a 270% increase!
Food vs. Microbiome Sources of TMAO
So, why would we see such extreme variations in TMAO levels after eating the same foods? The answer is, not surprisingly, bacteria! Stool analysis showed that compared to low TMAO producers, high TMAO producers had some important microbiota differences, including lower alpha-diversity, different species compositions, and a higher ratio of Firmicutes to Bacteroidetes (about 2:1, versus a 1:1 ratio for the low producers). And very importantly, as we’ll see in a moment, the Archaea phylum was completely absent in the microbiota of the high TMAO producers, but was represented among the low TMAO producers.
This study provided some important pieces for the TMAO puzzle. Along with demonstrating that fish (at least in the form of cod) yields vastly higher levels of TMAO and TMAO metabolites than beef or eggs, the study demonstrated that TMAO can be absorbed intact from foods like fish without involvement of the gut microbiota. That means that the level of TMAO we have in our bodies isn’t just a result of our gut microbiota churning it out from precursors, but can also be influenced by the direct consumption of TMAO from food. And, that could mean that high circulating TMAO from seafood potentially indicates a much different (AKA lower!) risk profile than high TMAO produced by disease-associated microbes.
So, as much as is still up in the air about TMAO, one thing seems pretty likely: we don’t want a gut microbiome that produces a lot of it. Whether or not TMAO itself turns out to be a major risk factor or just a red herring, and whether or not our circulating levels are a cause or consequence of specific health conditions, a high-TMAO-generating microbiota seems to be consistent with greater disease risk.
Archaea: A Microbiome Missing Piece
Whenever we hear about the microbiota, it’s usually all about the bacteria, bacteria, and more bacteria! But, while bacteria might be numerically dominant among the microbes in our gut, they’re definitely not the only residents there. Another type of single-celled organism that call our GI tracts home are archaea. And, these little guys are incredibly important!
Archaea (sometimes called archaebacteria) are strict anaerobes that live in various mucosal sites throughout the body, including the intestinal mucosa. We aren’t born with archaea inside us, but we acquire them from the environment throughout life: by the time children are school-aged, archaea are almost universally present in the gut, and levels continue to increase with age (with the highest occurrence and diversity of archaea being found in older adults). Along with lacking lipopolysaccharide (meaning archaea won’t contribute to our endotoxin load), archaea is also the only domain of life that doesn’t include any known pathogens, which is pretty cool!
Archaea degrade TMA and TMAO
One important subtype of archaea are the methanogens, which produce methane gas as a byproduct of hydrogen reduction. Up to 95% of human guts harbor the methanogenic archaea Methanobrevibacter smithii and Methanosphaera stadtmanae, at varying levels. While the idea of producing methane might not sound very pleasant, some of these archaea (in particular, an order of methanogens called the Methanomassiliicoccales) actually play an integral role in reducing our TMAO production. Along with being able to use carbon dioxide, formate, and methanol (all released by bacteria breaking down food and other organic matter in the gut), these archaea can use methyl compounds like TMA and TMAO to generate methane. And that means that the archaea in our gut actually deplete the pool of TMA we have available to be converted into TMAO (along with any free TMAO from foods like seafood). So, all that TMA generated by Prevotella, or entering our body from fish consumption? Archaea can help wipe some of it out!
The TMAO-reducing effects of archaea is far from just speculative, too. In a study of ELDERMET subjects, the fecal TMA concentration in people with TMA-metabolizing archaea was significantly lower than in those without this archaea—and the difference was particularly dramatic when the abundance of Methanomassiliicoccales was greater than 10^8 cells per gram of stool. This role of archaea is so exciting that some scientists are proposing a new class of probiotics called archaeabiotics, which could help reduce our TMAO levels without us needing to cut back on choline and other important nutrients!
Importantly, methanogenic archaea have an important interactive relationship with bacteria in the gut, which often takes the form of what scientists call syntrophy (where two organisms participate in consuming a substance that neither one can catabolize on its own). And, it appears that archaea are particularly chummy with the important probiotic bacteria Bifidobacteria. For example, mixed cultures of M. smithii and Bifidobacteria bifidum have been shown to collectively produce methane from glucose, and in females with gut Methanobacteriales levels higher than 0.71%, there’s a significantly higher mean abundance of Bifidobacteriaceae. And as we’ve already seen, healthy levels of Bifidobacteria are super important!
Archaea Thrive When We Eat Carbs!
So, how do we keep our archaea happy and thriving? Scientists are just at the beginning stages of understanding how diet impacts our archaea colonies (after all, archaea are relative newcomers to the microbiota research scene compared to bacteria!), but here’s what we know so far. In children, organic dairy (especially organic yogurt and organic milk) has been associated with the initial colonization of M. smithii, due to organic dairy serving as a vehicle for delivering it to our guts. And, some methanogens degrade methanol, which gets produced when bacteria degrade pectin in fruits—thus suggesting that archaea might benefit from including fruit in our diets! In Chinese goats, eating a high-grain diet appears to suppress methanogenic archaea relative to a high-hay diet—possibly due to the pH-lowering effect of grains in the rumen (which can then suppress methanogenic archaea that are sensitive to low pH environments). Obviously, we’re not Chinese goats, but it would certainly be interesting if a high-grain diet in humans had a similar effect!
More broadly, though, in humans, Methanobrevibacter abundance is positively associated with higher carbohydrate consumption (both recent and long-term), and negatively associated with recent consumption of fat (especially vegetable fat and polyunsaturated fat intake) and amino acids. Although more research is definitely needed, the picture getting painted so far is that archaea benefit from a variety of plant polysaccharides, and not so much from animal-based diets.
However, this isn’t because the archaea themselves eat carbohydrate. In fact, methanogenic archaea have an almost complete lack of enzymes for breaking down complex carbohydrates into simple sugars. What does appear to be happening is that archaea thrive off the metabolic products of carbohydrate-loving bacteria, and therefore are still dependent on dietary carbohydrate for their own survival!
The Study: Long-term Paleolithic diet is associated with lower resistant starch intake, different gut microbiota composition and increased serum TMAO concentrations
Whew! Now that we’ve covered the necessary background, let’s take a look at what this study is all about!
Researchers recruited a total of 44 participants who self-reported following a Paleo diet for over a year, along with 47 controls who more or less followed the national dietary recommendations of Australia (where the study was conducted). Within the Paleo group, participants were further divided based on how strictly they followed the Paleo framework (as gauged by the exclusion of grain and dairy products): 22 people fell into the “strict Paleo” group (less than one serving of grains and/or dairy per day), and 22 people fell into the “pseudo-Paleo” group (more than one serving of grains and/or dairy per day). (This is important, because “real-world” Paleo includes a variety of interpretations about what Paleo actually means, including how strictly to adhere to the diet—so a pseudo-Paleo group might be closer to reality for a lot of people!)
The study excluded anyone who’d taken antibiotics within the past six months, who had any type of GI tract surgery, who had past or present digestive disorders, who used cholesterol or blood pressure lowering medications, or who had been diagnosed with cardiovascular disease. This helped make sure the results weren’t confounded by preexisting health conditions or drugs, and allowed the researchers to better isolate the effects of the participants’ diets.
To ensure accurate dietary data, the researchers had participants undergo three-day weighed diet records (including two weekdays and one weekend day), which were then validated using urine nitrogen tests (which could detect whether participants were over- or under-reporting their protein intake) and the Goldberg cut point (which can identify which participants were under-reporting their energy intake, through the ratio of energy intake to basal metabolic rate). Participants who appeared to inaccurately report both their protein and energy intake were deemed unreliable dietary reporters (this ended up being two people from the strict Paleo group and three people from the control group).
Paleo Diet Adherents Had Increased TMAO
Now, the headline-grabbing finding. In the strict Paleo group, serum TMAO was a whopping 9.53 µM, the pseudo-Paleo group averaged 5.47 µM, and the control group averaged 3.93 µM. Higher TMAO levels were associated positively with red meat intake and negatively with grain intake.
Whether TMAO is a causative agent for disease or a marker for a disease-associated microbiota, those are some scary numbers—especially for the strict Paleo group!
What Study Participants Were Actually Eating
So, what were the Paleo groups actually eating? Here’s what the data showed!
Not surprisingly, both Paleo groups ate more protein than the controls (118 and 102.7 grams per day for the strict Paleo group and pseudo-Paleo group, respectively, compared to 92 grams for the controls), less carbohydrate (99 and 81.4 grams per day for the strict Paleo group and pseudo-Paleo group, respectively, compared to 202.6 grams for the controls), less sugar (51.8 and 44 grams per day for the Paleo groups, and 75.6 grams for the controls), and more fat—with the increase mostly coming from saturated and monounsaturated forms (117.9 total fat grams per day for the strict Paleo group, 133.1 grams for the pseudo-Paleo group, and 82.5 grams for the controls).
Importantly, total dietary fiber was adequate (and very similar!) for both the control group and the strict Paleo group—29.7 grams and 27.4 grams daily, respectively, which falls within the recommended daily intake of 25-30 grams for adults. The pseudo-Paleo group averaged 20.8 grams of fiber each day, which is still more than most people consume! For the Paleo groups, much of their fiber came from vegetables, with the strict Paleo group eating 6.7 servings of veggies per day and the pseudo-Paleo group averaging 4.3, compared to the control group’s 3.93. (We could definitely argue that the official recommendations for fiber are still too low for optimal health, but the point here is, these study participants weren’t slacking on the non-starchy veggies!)
While the control group averaged 4.5 – 14.2 grams of resistant starch per day, largely from grains (those are estimated minimum and maximum amounts, since the same foods can vary in resistant starch content), the strict Paleo group averaged only 2.6 – 6.1 grams per day, and the pseudo-Paleo group got a mere 1.3 – 2.9 grams of resistant starch. That’s a significant drop off!
Low-Carb Paleo Effects on the Microbiome
Remember that one of the favorite foods of Bifidobacteria is resistant starch? And that Roseburia also likes to munch on carbohydrates like beta-glucans? Maybe we shouldn’t be surprised that this study showed a significant decrease in these important bacteria among both Paleo groups.
Likewise, the relative abundance of Hungatella was significantly higher among the Paleo subjects. After adjusting for age, gender, stool frequency, and body fat, Hungatella abundance was significantly negatively associated with grain intake among the study’s participants, and was also significantly negatively correlated with Bifidobacteria and Roseburia abundance. Although we don’t have a lot of information about Hungatella in relation to human health (not yet, anyway!), we do know that some species originating from the genus Hungatella are associated with choline consumption and TMA production, including at least one species identified in this study. The researchers speculated that some components of grains and/or whole grains either interfere with Hungatella’s TMA production or prevent it from dominating in the gut. And, these components might not be resistant starch, since neither Hungatella nor TMAO was significantly associated with resistant starch intake!
Resistant Starch and Total Carb Intake Are Important!
One of the things that makes this study so interesting (and important!) is the fact that fiber and vegetable intake was relatively high for both Paleo groups. Often, when we talk about how ketogenic diets or low-carb or low-starch Paleo might affect the gut microbiome, we’re given a false sense of security thinking we’ll be fine as long as we eat plenty of fiber from leafy greens; see also How Ketogenic Diet Wreaks Havoc on Your Gut. As this study indicates, low-starch veggies alone are not enough to maintain a robust, diverse gut microbiome! The Paleo subjects clearly weren’t ingesting a broad enough array of fibers and starches to support some very important bacterial populations.
Given all that, can we just add some supplemental resistant starch to otherwise low-carb diet and call it a day?
Actually, the answer here seems to be no! Consistent with my post Resistant Starch: It’s Not All Sunshine and Roses, the research shows that isolated resistant starch doesn’t bring the same range of benefits as resistant starch from whole-food sources. And what’s more, when it comes to TMAO, supplemental resistant starch may even be counterproductive in the context of a low-carb and/or high fat diet. In a human cross-over trial from 2016, for example, 52 adults consumed four different diets in random orders—a low resistant starch, higher carbohydrate diet; a low resistant starch, lower carbohydrate diet; a high resistant starch, higher carbohydrate diet; and a high resistant starch, lower carbohydrate diet (with resistant starch coming from Hi-Maize 260, supplying RS2). Intriguingly, the highest TMAO levels occurred when subjects were eating the high resistant starch, lower carbohydrate diet, despite dietary levels of carnitine and choline being less on that diet compared to the low resistant starch periods. The researchers proposed that a high isolated resistant starch intake, in the presence of an overall lower carbohydrate diet, shifted the microbiota towards greater TMAO generation. Likewise, studies in rodents have shown that high fat consumption (which often goes hand-in-hand with low-carbohydrate diets), in the amount of of 42% of total energy, partially counteracts the beneficial effects of RS2 by suppressing levels of beneficial bacteria. So, low-carb diets can be a double whammy against our gut microbiota, both by failing to supply a wide range of fiber and starch types and by overloading our guts with levels of fat that become harmful to bacteria. (Don’t worry; we aren’t calling fat bad here—but a balanced intake of macronutrients seems to be where the evidence is pointing for optimal health!)
Other studies support the idea that resistant starch is most health-promoting in conjunction with other dietary carbohydrates. In pigs, resistant starch alone (in the form of RS2) was shown to get rapidly fermented in the proximal (beginning part) of the colon, while failing to reach further down into the distal (lower) colon—resulting in only a small portion of the colon receiving fermentation benefits. But, when additional carbohydrate in the form of wheat bran (a soluble non-starch polysaccharide) was included in the pigs’ diets, the amount of resistant starch getting fermented between the lower colon and feces nearly doubled—indicating that the bulk from the wheat bran was helping spread fermentation further down through the colon, flooding a much greater area with cancer-protective butyrate. The addition of wheat seed (RS1) to supplemental green banana flour and high-amylose starch (RS2) has been shown to help spread fermentation throughout the entire colon, as indicated by a decrease in fecal pH (which is a good thing!).
When it comes to low-carb Paleo diets, it’s easy to see how a similar effect could occur. Cutting out sources of bulky fermentable carbohydrate (like root veggies and legumes) limits how far isolated resistant starch can spread, resulting in bacteria in the proximal colon gobbling it up and leaving none for microbes further down the colon. Likewise, given what we know about the role of methanogenic archaea in regulating TMAO levels and interacting with other microbes like Bifidobacteria (as well as how much methanogenic archaea likes carbohydrates and doesn’t like fat!), we might suspect that low-carb diets can also enhance TMAO production by suppressing archaea growth.
As further confirmation, the main study we’ve been discussing in this article found that TMAO levels were more strongly negatively associated with grain intake than with resistant starch intake. That doesn’t mean we all need to eat grains to be healthy, but it does imply that diverse components of starchy plant foods (such as the other forms of fiber and carbohydrate they contain) contribute to a healthy microbiome, even more so than resistant starch on its own.
Short-Term Vs. Long-Term Microbiome Shifts
We should also stress the importance of the long-term nature of this study! While shorter dietary trials can be very useful (and in some cases, are the only studies we have at our disposal), they can’t capture potential health issues that develop months or years down the line (such as gradual changes in the core gut microbiota composition). That’s particularly relevant here, because the same researchers who conducted this study previously published a similar one, randomizing 22 women to a Paleo diet for four weeks and 17 women to a diet in line with Australian health recommendations. In that study, there wasn’t a significant change in TMAO concentration compared to the control group, despite a lower intake of resistant starch and higher intake of meat and eggs among the Paleo dieters. While those findings could have been due to the small sample size and limited data for resistant starch content of foods (making it difficult to precisely calculate resistant starch intake), it’s also possible that the Paleo group hadn’t yet exhibited some longer-term microbiota shifts that lead to higher TMAO generation as seen in the more recent study.
Indeed, the field of microbiota research has shown us that while some microbial changes happen rapidly when we alter our diet, others can occur on a more gradual basis. So, only using participants who had been eating Paleo for over a year gives this study greater insight into the full effects that low-carb Paleo has on the gut microbiota.
The Bottom Line: Paleo Should Not Be Low-Carb
Some people have seen this paper as an attack on red meat, which, given the TMAO link, is a valid concern (see also The Link Between Meat and Cancer). But what this paper is actually making a case for is that starch-free diets are a problem. Don’t get me wrong: fibrous, low-starch veggies are fantastic, and we should be filling our plates with them on the daily—but not at the exclusion of Paleo starches! Root veggies rich in resistant starch are consistently showing up as a vital component of a nutrient-dense Paleo diet, and there are no real “hacks” to get around that (see also Why Root Veggies Are Great for the Gut Microbiome and Resistant Starch: It’s Not All Sunshine and Roses).
When we combine this information with an examination of the non-metabolic roles that insulin plays (another rationale for moderate [not low] carb intake, see The Case for More Carbs: Insulin’s NonMetabolic Roles in the Human Body and How Many Carbs Should We Eat?), the potential problems of too-high-fat intake (not that we wan’t to eat low-fat; see Saturated Fat: Healthful, Harmful, or Somewhere In Between?, Adverse Reactions to Ketogenic Diets: Caution Advised), and understanding that micronutrient sufficiency is most easily attained with a balanced macronutrient diet (see The Diet We’re Meant to Eat, Part 3: How Much Meat versus Veggies?, The Importance of Nutrient Density, and Carbs Vs. Protein Vs. Fat: Insight from Hunter-Gatherers), it’s becoming harder and harder to make a compelling case against moderate carbohydrate intake, 30 to 60% of total calories, from whole food sources.
Citations
Bergeron N, et al. “Diets high in resistant starch increase plasma levels of trimethylamine-N-oxide, a gut microbiome metabolite associated with CVD risk.” Br J Nutr. 2016 Dec;116(12):2020-2029. doi: 10.1017/S0007114516004165. Epub 2016 Dec 20.
Borrel G, et al. “Genomics and metagenomics of trimethylamine-utilizing Archaea in the human gut microbiome.” ISME J. 2017 Sep;11(9):2059-2074. doi: 10.1038/ismej.2017.72. Epub 2017 Jun 6.
Charrier JA, et al. “High fat diet partially attenuates fermentation responses in rats fed resistant starch from high-amylose maize.” Obesity (Silver Spring). 2013 Nov;21(11):2350-5. doi: 10.1002/oby.20362. Epub 2013 Jul 2.
Cho, CE, et al. “Trimethylamine‐N‐oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: A randomized controlled trial” M. A., Mol. Nutr. Food Res. 2016, 1600324. Doi: 10.1002/mnfr.201600324
Dridi B, et al. “High prevalence of Methanobrevibacter smithii and Methanosphaera stadtmanae detected in the human gut using an improved DNA detection protocol.” PLoS One. 2009 Sep 17;4(9):e7063. doi: 10.1371/journal.pone.0007063.
Dridi B, et al. “High prevalence of Methanobrevibacter smithii and Methanosphaera stadtmanae detected in the human gut using an improved DNA detection protocol.” PLoS One. 2009 Sep 17;4(9):e7063. doi: 10.1371/journal.pone.0007063.
Genoni, A, et al. “Long-term Paleolithic diet is associated with lower resistant starch intake, different gut microbiota composition and increased serum TMAO concentrations.” European Journal of Nutrition, 2019; DOI: 10.1007/s00394-019-02036-y
Genoni A, et al. “A Paleolithic diet lowers resistant starch intake but does not affect serum trimethylamine-N-oxide concentrations in healthy women.” Br J Nutr. 2019 Feb;121(3):322-329. doi: 10.1017/S000711451800329X. Epub 2018 Nov 13.
Govers MJ, et al. “Wheat bran affects the site of fermentation of resistant starch and luminal indexes related to colon cancer risk: a study in pigs.” Gut. 1999 Dec;45(6):840-7.
Hoffmann C, et al. “Archaea and fungi of the human gut microbiome: correlations with diet and bacterial residents.” PLoS One. 2013 Jun 17;8(6):e66019. doi: 10.1371/journal.pone.0066019.
Jin W, Cheng Y, Zhu W. “The community structure of Methanomassiliicoccales in the rumen of Chinese goats and its response to a high-grain diet.” J Anim Sci Biotechnol. 2017 Jun 1;8:47. doi: 10.1186/s40104-017-0178-0.
Qi J, et al. “Circulating trimethylamine N-oxide and the risk of cardiovascular diseases: a systematic review and meta-analysis of 11 prospective cohort studies.” J Cell Mol Med. 2018 Jan;22(1):185-194. doi: 10.1111/jcmm.13307. Epub 2017 Aug 7.
Raymann K, et al. “Unexplored Archaeal Diversity in the Great Ape Gut Microbiome.” mSphere. 2017 Feb 22;2(1). pii: e00026-17. doi: 10.1128/mSphere.00026-17.
Tamanai-Shacoori Z, et al. “Roseburia spp.: a marker of health?” Future Microbiol. 2017 Feb;12:157-170. doi: 10.2217/fmb-2016-0130.
van de Pol JA, et al. “Gut Colonization by Methanogenic Archaea Is Associated with Organic Dairy Consumption in Children.” Front Microbiol. 2017 Mar 10;8:355. doi: 10.3389/fmicb.2017.00355. eCollection 2017.
Vanderhaeghen S, Lacroix C, Schwab C. “Methanogen communities in stools of humans of different age and health status and co-occurrence with bacteria.” FEMS Microbiol Lett. 2015 Jul;362(13):fnv092. doi: 10.1093/femsle/fnv092.
Vanessa DN, et al. “Archaea: Essential inhabitants of the human digestive microbiota.” Human Microbiome Journal, 2017 3:1-8. doi.org: 10.1016/j.humic.2016.11.005.
from https://www.thepaleomom.com/paleo-resistant-starch-and-tmao-new-study-warning-worth-heeding/
0 notes
Text
Quinoa Nutrition Facts
[arve url="https://www.youtube.com/embed/UQGQN-jxFxE" /] What Is It? A quick search on the internet reveals several facts of this grain crop which is grown primarily for its edible seeds. Simply put, Quinoa, a species of goosefoot (Chenopodium) is a pseudo cereal (that is their seeds can be ground into flour and consumed) rather than a true cereal, as it is not a member of the true grass family. It is also closely related to species such as beetroot, spinach and tumbleweed which have shrub like growth. Where Does It Grow? It originated in the Andean region of Ecuador, Bolivia, Colombia and Peru, where it was domesticated 3,000 to 4,000 years ago for human consumption and found its place into the humble Indian household (albeit being an upper middle class commodity). It gained popularity and has been cultivated away from natural distribution in places like the United States, Australia and Japan to name a few. What Are The Nutritional Benefits? Essential Amino Acids Quinoa seeds contain essential amino acids like lysine and acceptable quantities of calcium, phosphorus, and iron. A study showed that deficiency of essential amino acids leads to symptoms of nervousness, exhaustion, and dizziness to a greater or lesser extent and moderate consumption of Quinoa can help avoid such symptoms. Anti-Inflammatory Quinoa consists of a unique combination of anti-inflammatory compounds that show to an extent the decreased risk of inflammation-related problems (including obesity) when animals under study are fed quinoa on a daily basis. The list of anti-inflammatory phytonutrients in quinoa is now known to include: • Polysaccharides like arabinans and rhamnogalacturonans • Hydroxycinnamic and hydroxybenzoic acids • Flavonoids like quercetin and kaempferol which are found in concentrated levels often higher than those of high flavonoid berries like cranberry or ligonberry • Saponins including molecules derived from oleanic acid, hederagenin and serjanic acid. • Small amounts of the anti-inflammatory omega-3 fatty acid, alpha-linolenic acid (ALA), are also provided by quinoa. Gluten Free It is high in protein and lacks gluten which is good news for those who suffer from Celiac disease which is an autoimmune disease attacking the small intestine due to the presence of gluten for which the only remedy is maintaining a gluten free diet. While scientists are yet to confirm whether oats are a gluten free food, it is safe to say that Quinoa, like amaranth, is gluten free and good for your health as it is considered easy to digest. Because of these characteristics, it is being considered a possible crop for long-duration human occupied space flights undertaken by NASA. Super Food The nutrient composition of Quinoa is favorable compared with common cereals earning the Quinoa grain the title of being called a “super food”. Nutritional evaluations indicate that quinoa is a source of complete protein, that is, it contains all the essential amino acids required in a human diet in correct proportions. Other similar pseudo grains derived from seeds are similar in complete protein levels; buckwheat is 18% protein compared to 14% for Quinoa; Amaranth, a related species to Quinoa, ranges from 12 to 17.5%. High In Protein The protein content per 100 calories is higher than brown rice, potatoes, barley and millet, but is less than wild rice (Indian rice) and oats. In comparison to cereal grasses like wheat, quinoa is higher in fat content and can provide valuable amounts of heart-healthy fats like monounsaturated fat (in the form of oleic acid). High In Fiber The grain is additionally a good source of dietary fiber and phosphorus and is high in magnesium and iron. Vegan Friendly and Good For Those Who Are Lactose Intolerant It is also a source of calcium, and thus, is useful for vegans and those who are lactose intolerant. Exactly HOW does one consume Quinoa? The grain may be germinated in its raw form to boost its nutritional value, provided that the grains are rinsed thoroughly to remove any saponin that contains an unpalatable bitterness which in turn aids during cultivation as it wards off birds reducing the need for protecting it. The seeds are in general cooked the same way as rice and can be used in a wide range of dishes. The good news is processes of boiling, simmering, and steaming quinoa do not appear to significantly compromise the quality of quinoa's fatty acids, allowing us to enjoy its cooked texture and flavor while maintaining this nutrient benefit. The leaves are eaten as a leaf vegetable, much like amaranth, but the commercial availability of quinoa greens is limited. In some forms the seeds are softened making them suitable to be added to salads and other cold foods. What makes Quinoa special? While it may be called a “Pseudo-cereal” there is nothing fake about the health benefits of Quinoa. In fact, The Food and Agricultural Organization of the United Nations (FAO) has officially declared that the year 2013 be recognized as "The International Year of the Quinoa." http://www.slim-fit-well.com/?p=1391
0 notes
Text
Quinoa - Keen WHA!
Health Benefits
Overall Nutrient Richness
Perhaps the most striking health benefit provided by quinoa is its overall nutrient richness. When the nutrient composition of this food is analyzed in depth, the results are unusual and striking. While quinoa can be eaten in the same way as a grain, or ground into flour like is so commonly done with grains, it lacks some important nutritional shortcomings of grains.
One of the shortcomings overcome by quinoa involves its protein content. Most grains are considered to be inadequate as total protein sources because they lack adequate amounts of the amino acids lysine and isoleucine. The relatively low level of both lysine and isoleucine in the protein of grains is what causes these amino acids to be considered as the limiting amino acids (LAAs) in grains. In other words, these LAAs prevent grains from serving as complete protein sources in our diet. By contrast, quinoa has significantly greater amounts of both lysine and isoleucine (especially lysine), and these greater amounts of lysine and isoleucine allow the protein in quinoa to serve as a complete protein source.
In terms of fat content, quinoa once again overcomes some of the shortcomings of most grains. Since it takes nearly 350 calories' worth of whole wheat to provide 1 gram of fat, whole wheat is not generally regarded as a significant source of fat, including essential fatty acids or heart-healthy monounsaturated fats (like oleic acid). By contrast, since it only takes 63 calories' worth of quinoa to provide 1 gram of fat, quinoa is typically considered to be a valuable source of certain health-supportive fats. About 28% of quinoa's fatty acids come in the form of oleic acid, a heart-healthy monounsaturated fat, and about 5% come in the form of alpha-linolenic acid or ALA—the omega-3 fatty acid most commonly found in plants and associated with decreased risk of inflammation-related disease.
Neither quinoa nor any grains qualify as good vitamin E sources in our WHFoods rating system. However, in the case of quinoa, or rating system does not do full justice to the fact that quinoa contains significant amounts of certain tocopherols (vitamin E family members) largely absent from most grains. For example, one cup of quinoa provides 2.2 milligrams of gamma-tocopherol—a form of vitamin E that has been more closely associated with certain anti-inflammatory benefits in health research. Quinoa is also a good source of RDA nutrients like folate, zinc, and phosphorus in contrast to whole wheat, which does not qualify as a good source in our rating system.
Quinoa is an equally impressive food in terms of its overall phytonutrient benefits. In many Central and South American countries, the leaves of the quinoa plant are valued for their betacyanin pigments, which provide some of their bright reddish shades. But even the seeds themselves can be phytonutrient-rich and can provide significant amounts of antioxidants like ferulic, coumaric, hydroxybenzoic, and vanillic acid.
The antioxidant flavonoids quercetin and kaempferol are also especially plentiful in quinoa. In fact, the concentration of these two flavonoids in quinoa can sometimes be greater than their concentration of high-flavonoid berries like cranberry or lingonberry.
Considered in combination, these diverse nutrient benefits of quinoa give it uniqueness among grain-related foods. For us, this high overall level of nourishment provided by quinoa may qualify as its greatest health benefit.
Anti-Inflammatory Benefits
Most of the quinoa studies that we've seen in this area have been animal studies. However, we believe that the preliminary indications for humans are very promising. Research has shown the ability of daily quinoa intake to lower levels of inflammation in fat (adipose) tissue in rats and in the linings of their intestine as well.
We're not surprised at either of these results because a wide range of anti-inflammatory nutrients is already known to be present in quinoa. This list of anti-inflammatory nutrients includes phenolic acids (including hydroxycinnamic and hydroxybenzoic acids), members of the vitamin E family like gamma-tocopherol, and cell wall polysaccharides like arabinans and rhamnogalacturonans.
Somewhat more controversial in this anti-inflammatory nutrient list are the saponins found in quinoa. Saponins are the bitter tasting, water-soluble phytonutrients found in the outer seed coat layer of quinoa. (More specifically, the saponins found in quinoa are derived from hederagenin, oleanic acid, phytolaccagenic acid, and serjanic acid.) The quinoa saponins have been shown to have both anti-inflammatory and antioxidant properties. However, soaking, boiling, and milling can reduce their presence, and, in general, this reduced presence is usually regarded as a good thing since it can make the quinoa much more enjoyable for most people to eat. In research to date, the relationship between and anti-inflammatory benefits of quinoa and saponin levels has yet to be clarified. However, even though more research is needed in this particular phytonutrient area, the list of anti-inflammatory nutrients in quinoa remains impressive.
Other Benefits
We have yet to see large-scale human studies on intake of quinoa and risk of type 2 diabetes or risk of cardiovascular disease. However, we would expect such studies to show significantly reduced risks. With respect to type 2 diabetes, quinoa simply has too many things in common with other foods known to decrease risk. At the top of the list here would be its fiber and protein content. Quinoa is a good source of fiber—one of the key macronutrients needed for health blood sugar regulation. It also provides outstanding protein quality, even in comparison to commonly-eaten whole grains. Strong intake of protein and fiber are two dietary essentials for regulation of blood sugar. Because chronic, unwanted inflammation is also a key risk factor for development of type 2 diabetes, the diverse range of anti-inflammatory nutrients found in quinoa also make it a great candidate for diabetes risk reduction.
Animal studies have already demonstrated the ability of quinoa to lower total cholesterol and help maintain levels of HDL cholesterol (the "good" cholesterol). While we would expect these results in humans as well, we would also expect the anti-inflammatory nutrients in quinoa to help protect human blood vessels from inflammatory damage. Protection of this kind would also provide reduced risk of many cardiovascular diseases, including atherosclerosis. We expect to see future, large-scale human studies demonstrating the benefits of quinoa for risk reduction in this area of cardiovascular disease.
The antioxidant and anti-inflammatory phytonutrients in quinoa also make it a likely candidate for cancer risk reduction in humans. Given the preliminary animal results involving the digestive tract, risk reduction for colon cancer may turn out to be a special area of interest.
A final area of likely benefit involves decreased risk of allergy—especially for individuals who have adverse reactions to certain grains and seek practical alternatives. Already, several public organizations have recommended quinoa as a substitute for wheat whenever the avoidance of this gluten-containing grain is required. The low-allergy potential of quinoa—coupled with its relatively high digestibility—has also made it a food of special interest in the diet of children and toddlers.
Description
Because quinoa is typically consumed in the same way as the cereal grasses (wheat, oats, barley, and rye), we group it together with those foods on our website. However, quinoa is not a cereal grass at all, but rather a member of the same food family that contains spinach, Swiss chard, and beets. Many researchers refer to quinoa as a "pseudocereal." This term is typically used to describe foods that are not grasses but can still be easily ground into flour. The scientific name for quinoa is Chenopodium quinoa.
Researchers date the popularity of quinoa to approximately 3000 BC, when its consumption became widespread in the Andes mountains regions of South America. About 250 different varieties of quinoa were already present at that time, giving quinoa a remarkable tolerance for different growing conditions. Quinoa is able to survive high altitudes, thin and cold air, hot sun, salty or sandy soil, little rainfall, and sub-freezing temperatures. In addition, all parts of the plant could be eaten, including not only the seeds that we buy in the store and that may also have been dried and ground into flour, but also the leaves and stems. Betacyanin pigments presemt in some quinoa leaves given them their bright reddish color, but it's also possible to find orange, pink, purple, tan, and black quinoa as well. Quinoa leaves taste similar in flavor to the leaves of their fellow chenopods, namely, spinach, chard, and beets. Cooked quinoa seeds are fluffy and creamy, yet also slightly crunchy. They may also sometimes have an amazing translucent appearance. The flavor of the cooked seeds is delicate and somewhat nutty.
The word "quinoa" is pronounced "KEEN-wah." It comes from the Spanish word, quinua, which itself comes from the word "kinwa" or "kinua" in the Quechua dialect.
History
The history of quinoa is clearly rooted in South America, in the Andes region that is currently divided up between the countries of Argentina, Bolivia, Chile, Colombia, Ecuador, and Peru. Along with maize, quinoa was one of the two mainstay foods for the Inca Empire that had its start around 1200 AD. As previously mentioned in the Description section, quinoa was a food that could survive in a wide variety of growing conditions. Along with its unusual nutrient richness, its adaptability helped it gain popularity among the Incas for hundreds and hundreds of years.
Most quinoa consumed in the United States still comes from South America. Peru remains the largest commercial producer of quinoa, harvesting 41,079 metric tons in 2010. Bolivia was the second largest producer with 29,500 metric tons. Together, these two South American countries produced nearly 99% of all commercially grown quinoa in 2010. In terms of export sales, quinoa has risen to the level of an $87 million dollar business in these two countries.
Some commercial quinoa production takes place in the United States, although total cultivation remains under 10,000 pounds. The Colorado Rockies have been a place of special interest for quinoa production, and some production has also occurred in the states of California, Washington, and Oregon.
Interest in quinoa has recently spread to India (including the North-India Plains and high-altitude areas of the Himalayas), other parts of Asia (including Japan), as well as to Africa and part of Europe. Designation of the year 2013 as "The International Year of the Quinoa" by the Food and Agricultural Organization of the United Nations (FAO) may also trigger greater attention to this food worldwide.
How to Select and Store
Quinoa is generally available in prepackaged containers as well as bulk bins. Just as with any other food that you may purchase in the bulk section, make sure that the bins containing the quinoa are covered and that the store has a good product turnover so as to ensure its maximal freshness. Whether purchasing quinoa in bulk or in a packaged container, make sure that there is no evidence of moisture. When deciding upon the amount to purchase, remember that quinoa expands during the cooking process to several times its original size. If you cannot find it in your local supermarket, look for it at natural foods stores, which usually carry it.
The most common type of quinoa you will find in the store has an off-white color but red and black quinoa are becoming more available. You may even be able to find a tri-color mixture sold in packages or bulk bins.
Store quinoa in an airtight container. It will keep for a longer period of time, approximately three to six months, if stored in the refrigerator.
Tips for Preparing and Cooking
Tips for Preparing Quinoa
Processing methods used in the commercial milling of quinoa usually remove most of the saponins found in the outer coat of the quinoa seeds. Because the quinoa saponins are largely responsible for its bitter taste, many people chose to rinse and rub the seeds after purchase to remove any bitter taste that may remain in the seeds. An effective method to do so is to place the quinoa seeds in a fine-meshed strainer and run cold water over the quinoa while gently rubbing the seeds together in your hands. After completing this process, you can taste a few seeds to determine if a bitter taste remains. If it does, simply continue this rinsing and rubbing process until you no longer taste a bitter residue.
The Healthiest Way of Cooking Quinoa
To cook the quinoa, add one part of the grain to two parts liquid in a saucepan. After the mixture is brought to a boil, reduce the heat to simmer and cover. One cup of quinoa cooked in this method usually takes 15 minutes to prepare. When cooking is complete, you will notice that the grains have become translucent, and the white germ has partially detached itself, appearing like a white-spiraled tail. If you desire the quinoa to have a nuttier flavor, you can dry roast it before cooking; to dry roast, place it in a skillet over medium-low heat and stir constantly for five minutes.
Quinoa is a perfect food to include on a gluten-free diet, since it not only lacks gluten but doesn't even belong to the same plant family as wheat, oats, barley, or rye. Some studies also show quinoa flour to have higher-than-expected digestibility. Both of these factors would be expected to decrease the risk of an adverse reaction to quinoa—especially in comparison to a cereal grass like wheat. While it is possible to make baked goods and pastas out of 100% quinoa flour, most companies combine quinoa flour with other flours (like tapioca flour or rice flour) or with oatmeal to produce a lighter texture. (Products made with 100% quinoa flour typically have a heavy and dense texture, sometimes referred to as "truffle-like.") When combined with rice flour or tapioca flour, however, quinoa-based products definitely qualify as gluten-free and should help reduce risk of adverse reactions.
How to Enjoy
Combine cooked chilled quinoa with pinto beans, pumpkin seeds, scallions and coriander. Season to taste and enjoy this south-of-the-border inspired salad.
Add nuts and fruits to cooked quinoa and serve as breakfast porridge.
For a twist on your favorite pasta recipe, use noodles made from quinoa.
Sprouted quinoa can be used in salads and sandwiches just like alfalfa sprouts.
Add quinoa to your favorite vegetable soups.
Ground quinoa flour can be added to cookie or muffin recipes.
Quinoa is great to use in tabouli, serving as a delicious (and wheat-free) substitute for the bulgar wheat with which this Middle Eastern dish is usually made.
For some of our favorite recipes, click Recipes.
Individual Concerns
Quinoa is not a commonly allergenic food. Because quinoa does not belong to the plant family containing wheat, oats, barley, and rye, it is also a gluten-free food. Some studies also show a higher-than-expected digestibility for quinoa, making it a food less likely to produce adverse reactions.
Nutritional Profile
Quinoa is food of high protein quality and is typically regarded as an adequate source of all essential amino acids, including lysine and isoleucine. It provides a variety of antioxidant phytonutrients, including ferulic, coumaric, hydroxybenzoic, and vanillic acid. Antioxidant flavonoids including quercetin and kaempferol are also especially plentiful in quinoa. Anti-inflammatory polysaccharides in quinoa include arabinans and rhamnogalacturonans. Many members of the vitamin E tocopherol family are provided by quinoa, including important amounts of gamma-tocopherol. Quinoa is a very good source of manganese. It is also a good source of phosphorus, copper, magnesium, dietary fiber, folate and zinc.
Introduction to Food Rating System Chart
In order to better help you identify foods that feature a high concentration of nutrients for the calories they contain, we created a Food Rating System. This system allows us to highlight the foods that are especially rich in particular nutrients. The following chart shows the nutrients for which this food is either an excellent, very good, or good source (below the chart you will find a table that explains these qualifications). If a nutrient is not listed in the chart, it does not necessarily mean that the food doesn't contain it. It simply means that the nutrient is not provided in a sufficient amount or concentration to meet our rating criteria. (To view this food's in-depth nutritional profile that includes values for dozens of nutrients - not just the ones rated as excellent, very good, or good - please use the link below the chart.) To read this chart accurately, you'll need to glance up in the top left corner where you will find the name of the food and the serving size we used to calculate the food's nutrient composition. This serving size will tell you how much of the food you need to eat to obtain the amount of nutrients found in the chart. Now, returning to the chart itself, you can look next to the nutrient name in order to find the nutrient amount it offers, the percent Daily Value (DV%) that this amount represents, the nutrient density that we calculated for this food and nutrient, and the rating we established in our rating system. For most of our nutrient ratings, we adopted the government standards for food labeling that are found in the U.S. Food and Drug Administration's "Reference Values for Nutrition Labeling." Read more background information and details of our rating system.
Quinoa, cooked
0.75 cup
185.00 gramsCalories: 222
GI: low
Nutrient Amount DRI/DV
(%) Nutrient
Density World's Healthiest
Foods Rating
manganese 1.17 mg 59 4.7 very good
phosphorus 281.20 mg 40 3.3 good
copper 0.36 mg 40 3.2 good
magnesium 118.40 mg 30 2.4 good
fiber 5.18 g 21 1.7 good
folate 77.70 mcg 19 1.6 good
zinc 2.02 mg 18 1.5 good
World's Healthiest
Foods Rating Rule
excellent DRI/DV>=75% OR
Density>=7.6 AND DRI/DV>=10%
very good DRI/DV>=50% OR
Density>=3.4 AND DRI/DV>=5%
good DRI/DV>=25% OR
Density>=1.5 AND DRI/DV>=2.5%
In-Depth Nutritional Profile
In addition to the nutrients highlighted in our ratings chart, here is an in-depth nutritional profile for Quinoa. This profile includes information on a full array of nutrients, including carbohydrates, sugar, soluble and insoluble fiber, sodium, vitamins, minerals, fatty acids, amino acids and more.
Quinoa, cooked
(Note: "--" indicates data unavailable)
0.75 cup
(185.00 g) GI: low
BASIC MACRONUTRIENTS AND CALORIES
nutrient amount DRI/DV
(%)
Protein 8.14 g 16
Carbohydrates 39.40 g 18
Fat - total 3.55 g --
Dietary Fiber 5.18 g 21
Calories 222.00 12
MACRONUTRIENT AND CALORIE DETAIL
nutrient amount DRI/DV
(%)
Carbohydrate:
Starch 32.62 g
Total Sugars 1.61 g
Monosaccharides -- g
Fructose -- g
Glucose -- g
Galactose -- g
Disaccharides -- g
Lactose -- g
Maltose -- g
Sucrose -- g
Soluble Fiber -- g
Insoluble Fiber -- g
Other Carbohydrates 32.62 g
Fat:
Monounsaturated Fat 0.98 g
Polyunsaturated Fat 1.99 g
Saturated Fat 0.43 g
Trans Fat -- g
Calories from Fat 31.97
Calories from Saturated Fat 3.85
Calories from Trans Fat --
Cholesterol 0.00 mg
Water 132.48 g
MICRONUTRIENTS
nutrient amount DRI/DV
(%)
Vitamins
Water-Soluble Vitamins
B-Complex Vitamins
Vitamin B1 0.20 mg 17
Vitamin B2 0.20 mg 15
Vitamin B3 0.76 mg 5
Vitamin B3 (Niacin Equivalents) 2.37 mg
Vitamin B6 0.23 mg 14
Vitamin B12 0.00 mcg 0
Biotin -- mcg --
Choline 42.55 mg 10
Folate 77.70 mcg 19
Folate (DFE) 77.70 mcg
Folate (food) 77.70 mcg
Pantothenic Acid 0.50 mg 10
Vitamin C 0.00 mg 0
Fat-Soluble Vitamins
Vitamin A (Retinoids and Carotenoids)
Vitamin A International Units (IU) 9.25 IU
Vitamin A mcg Retinol Activity Equivalents (RAE) 0.46 mcg (RAE) 0
Vitamin A mcg Retinol Equivalents (RE) 0.92 mcg (RE)
Retinol mcg Retinol Equivalents (RE) 0.00 mcg (RE)
Carotenoid mcg Retinol Equivalents (RE) 0.92 mcg (RE)
Alpha-Carotene 0.00 mcg
Beta-Carotene 5.55 mcg
Beta-Carotene Equivalents 5.55 mcg
Cryptoxanthin 0.00 mcg
Lutein and Zeaxanthin 98.05 mcg
Lycopene 0.00 mcg
Vitamin D
Vitamin D International Units (IU) 0.00 IU 0
Vitamin D mcg 0.00 mcg
Vitamin E
Vitamin E mg Alpha-Tocopherol Equivalents (ATE) 1.17 mg (ATE) 8
Vitamin E International Units (IU) 1.74 IU
Vitamin E mg 1.17 mg
Vitamin K 0.00 mcg 0
Minerals
nutrient amount DRI/DV
(%)
Boron -- mcg
Calcium 31.45 mg 3
Chloride -- mg
Chromium -- mcg --
Copper 0.36 mg 40
Fluoride -- mg --
Iodine -- mcg --
Iron 2.76 mg 15
Magnesium 118.40 mg 30
Manganese 1.17 mg 59
Molybdenum -- mcg --
Phosphorus 281.20 mg 40
Potassium 318.20 mg 9
Selenium 5.18 mcg 9
Sodium 12.95 mg 1
Zinc 2.02 mg 18
INDIVIDUAL FATTY ACIDS
nutrient amount DRI/DV
(%)
Omega-3 Fatty Acids 0.18 g 8
Omega-6 Fatty Acids 1.81 g
Monounsaturated Fats
14:1 Myristoleic -- g
15:1 Pentadecenoic -- g
16:1 Palmitol -- g
17:1 Heptadecenoic -- g
18:1 Oleic 0.86 g
20:1 Eicosenoic 0.06 g
22:1 Erucic 0.05 g
24:1 Nervonic -- g
Polyunsaturated Fatty Acids
18:2 Linoleic 1.80 g
18:2 Conjugated Linoleic (CLA) -- g
18:3 Linolenic 0.16 g
18:4 Stearidonic -- g
20:3 Eicosatrienoic -- g
20:4 Arachidonic 0.01 g
20:5 Eicosapentaenoic (EPA) -- g
22:5 Docosapentaenoic (DPA) -- g
22:6 Docosahexaenoic (DHA) 0.03 g
Saturated Fatty Acids
4:0 Butyric -- g
6:0 Caproic -- g
8:0 Caprylic -- g
10:0 Capric -- g
12:0 Lauric -- g
14:0 Myristic -- g
15:0 Pentadecanoic -- g
16:0 Palmitic 0.36 g
17:0 Margaric -- g
18:0 Stearic 0.02 g
20:0 Arachidic -- g
22:0 Behenate -- g
24:0 Lignoceric -- g
INDIVIDUAL AMINO ACIDS
nutrient amount DRI/DV
(%)
Alanine 0.34 g
Arginine 0.63 g
Aspartic Acid 0.65 g
Cysteine 0.12 g
Glutamic Acid 1.07 g
Glycine 0.40 g
Histidine 0.23 g
Isoleucine 0.29 g
Leucine 0.48 g
Lysine 0.44 g
Methionine 0.18 g
Phenylalanine 0.34 g
Proline 0.44 g
Serine 0.33 g
Threonine 0.24 g
Tryptophan 0.10 g
Tyrosine 0.15 g
Valine 0.34 g
OTHER COMPONENTS
nutrient amount DRI/DV
(%)
Ash 1.41 g
Organic Acids (Total) -- g
Acetic Acid -- g
Citric Acid -- g
Lactic Acid -- g
Malic Acid -- g
Taurine -- g
Sugar Alcohols (Total) -- g
Glycerol -- g
Inositol -- g
Mannitol -- g
Sorbitol -- g
Xylitol -- g
Artificial Sweeteners (Total) -- mg
Aspartame -- mg
Saccharin -- mg
Alcohol 0.00 g
Caffeine 0.00 mg
0 notes
Text
Characterization of a pectin from Lonicera japonica Thunb. and its inhibition effect on Aβ42 aggregation and promotion of neuritogenesis.
PMID: Int J Biol Macromol. 2018 Feb ;107(Pt A):112-120. Epub 2017 Aug 31. PMID: 28863894 Abstract Title: Characterization of a pectin from Lonicera japonica Thunb. and its inhibition effect on Aβaggregation and promotion of neuritogenesis. Abstract: Pectin is a class of complex polysaccharides and recognized for its potential bioactivities. In this study, we showed that a pectic polysaccharide, LFA03-a, was extracted from Lonicera japonica Thunb. flowers and purified with DEAE-cellulose and Sephacryl S-100HR. LFA03-a was composed of rhamnose, arabinose, galactose and galacturonic acid in the molar ratio of 18.1:25.3:36.8:19.5. Its structure was determined to possess a rhamnogalacturonan I (RG-I) backbone consisting ofα-l-1,2-Rhap and α-d-1,4-GalAp disaccharide repeating unit, substituted at O-4 of l-rhamnose. The side chain was involved with β-d-1,4-Galp, β-d-1,3-Galp, β-d-1,3,6-Galp and branched α-l-1,5-Araf. Fluorescence spectroscopic analysis with thioflavine T (ThT) and atomic force microscopy (AFM) results showed that LFA03-a inhibited Aβaggregation in a dose dependent manner and impeded Aβoligomerization and fibril formation. In addition, LFA03-a mildly induced the differentiation of PC12 cells and promoted neuritogenesis.The results suggested that pectin LFA03-a might be a potential targeted therapeutic drug for Alzheimer's disease.
read more
0 notes
Text
Quinoa Nutrition Facts
[arve url="https://www.youtube.com/embed/UQGQN-jxFxE" /] What Is It? A quick search on the internet reveals several facts of this grain crop which is grown primarily for its edible seeds. Simply put, Quinoa, a species of goosefoot (Chenopodium) is a pseudo cereal (that is their seeds can be ground into flour and consumed) rather than a true cereal, as it is not a member of the true grass family. It is also closely related to species such as beetroot, spinach and tumbleweed which have shrub like growth. Where Does It Grow? It originated in the Andean region of Ecuador, Bolivia, Colombia and Peru, where it was domesticated 3,000 to 4,000 years ago for human consumption and found its place into the humble Indian household (albeit being an upper middle class commodity). It gained popularity and has been cultivated away from natural distribution in places like the United States, Australia and Japan to name a few. What Are The Nutritional Benefits? Essential Amino Acids Quinoa seeds contain essential amino acids like lysine and acceptable quantities of calcium, phosphorus, and iron. A study showed that deficiency of essential amino acids leads to symptoms of nervousness, exhaustion, and dizziness to a greater or lesser extent and moderate consumption of Quinoa can help avoid such symptoms. Anti-Inflammatory Quinoa consists of a unique combination of anti-inflammatory compounds that show to an extent the decreased risk of inflammation-related problems (including obesity) when animals under study are fed quinoa on a daily basis. The list of anti-inflammatory phytonutrients in quinoa is now known to include: • Polysaccharides like arabinans and rhamnogalacturonans • Hydroxycinnamic and hydroxybenzoic acids • Flavonoids like quercetin and kaempferol which are found in concentrated levels often higher than those of high flavonoid berries like cranberry or ligonberry • Saponins including molecules derived from oleanic acid, hederagenin and serjanic acid. • Small amounts of the anti-inflammatory omega-3 fatty acid, alpha-linolenic acid (ALA), are also provided by quinoa. Gluten Free It is high in protein and lacks gluten which is good news for those who suffer from Celiac disease which is an autoimmune disease attacking the small intestine due to the presence of gluten for which the only remedy is maintaining a gluten free diet. While scientists are yet to confirm whether oats are a gluten free food, it is safe to say that Quinoa, like amaranth, is gluten free and good for your health as it is considered easy to digest. Because of these characteristics, it is being considered a possible crop for long-duration human occupied space flights undertaken by NASA. Super Food The nutrient composition of Quinoa is favorable compared with common cereals earning the Quinoa grain the title of being called a “super food”. Nutritional evaluations indicate that quinoa is a source of complete protein, that is, it contains all the essential amino acids required in a human diet in correct proportions. Other similar pseudo grains derived from seeds are similar in complete protein levels; buckwheat is 18% protein compared to 14% for Quinoa; Amaranth, a related species to Quinoa, ranges from 12 to 17.5%. High In Protein The protein content per 100 calories is higher than brown rice, potatoes, barley and millet, but is less than wild rice (Indian rice) and oats. In comparison to cereal grasses like wheat, quinoa is higher in fat content and can provide valuable amounts of heart-healthy fats like monounsaturated fat (in the form of oleic acid). High In Fiber The grain is additionally a good source of dietary fiber and phosphorus and is high in magnesium and iron. Vegan Friendly and Good For Those Who Are Lactose Intolerant It is also a source of calcium, and thus, is useful for vegans and those who are lactose intolerant. Exactly HOW does one consume Quinoa? The grain may be germinated in its raw form to boost its nutritional value, provided that the grains are rinsed thoroughly to remove any saponin that contains an unpalatable bitterness which in turn aids during cultivation as it wards off birds reducing the need for protecting it. The seeds are in general cooked the same way as rice and can be used in a wide range of dishes. The good news is processes of boiling, simmering, and steaming quinoa do not appear to significantly compromise the quality of quinoa's fatty acids, allowing us to enjoy its cooked texture and flavor while maintaining this nutrient benefit. The leaves are eaten as a leaf vegetable, much like amaranth, but the commercial availability of quinoa greens is limited. In some forms the seeds are softened making them suitable to be added to salads and other cold foods. What makes Quinoa special? While it may be called a “Pseudo-cereal” there is nothing fake about the health benefits of Quinoa. In fact, The Food and Agricultural Organization of the United Nations (FAO) has officially declared that the year 2013 be recognized as "The International Year of the Quinoa." http://www.slim-fit-well.com/?p=1391
0 notes