#can gastric causes chest pain
Text
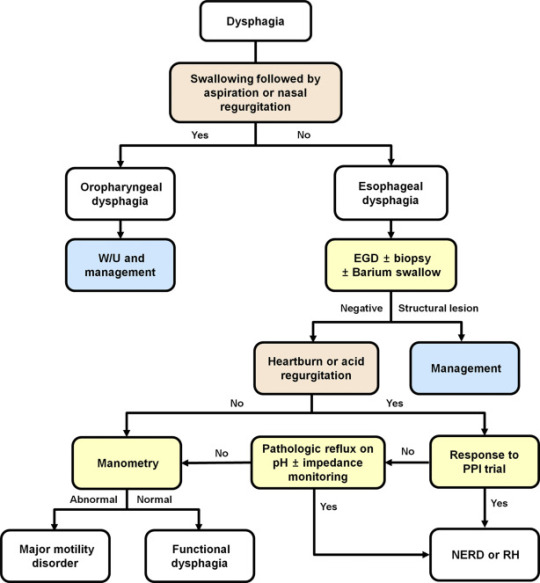
Explaining dysphagia
Dysphagia is simultaneously a symptom and a diagnosable condition. Most people think of it (if they think of it at all) as the choking on food disease but in reality it's much more complicated than that.
There are four categories of dysphagia: oropharyngeal, esophageal, esophagogastric, and paraesophageal
only two of those categories (oropharyngeal and esophageal) are commonly used and diagnosed so those are the main two I'll be talking about.
The diagnosis of dysphagia is a fairly complicated process involving a lot of radiological testing and things stuck up your nose and down your throat.
lost the source :(
source
the ICD 10 further divides dysphagia into unspecified, oral phase, oropharyngeal phase, pharyngeal phase, pharyngoesophageal phase, and other dysphagia which includes cervical dysphagia and neurogenic dysphagia
Oropharyngeal dysphagia
Oropharyngeal dysphagia occurs when someone has difficulty initiating a swallow. It's often accompanied by coughing, choking, feeling food stick in the throat, and nasal regurgitation. Other symptoms include frequent repetitive swallows, frequent throat clearing, a gargly voice after meals, hoarse voice, nasal speech and dysarthria, drooling, and recurrent pneumonia.
Oropharyngeal dysphagia is diagnosed with a modified barium swallow and/or a transnasal video endoscopy.
Some of the consequences of oropharyngeal dysphagia include aspiration pneumonia, upper respiratory infections, and weight loss. Common treatment includes rehabilitative swallowing exercises, botox, surgery, and/or a feeding tube.
Esophageal Dysphagia
Esophageal dysphagia is dysphagia where there is a problem with the passage of food or liquids through the esophagus between the upper and lower esophageal sphincter. Esophageal dysphagia is usually a result of abnormal motility in the esophagus or a physical obstruction to the esophagus. Symptoms of esophageal dysphagia vary depending on cause.
Motility: People with esophageal motility disorders will experience problems with swallowing both liquids and solids. Motility disorders consist of abnormal numbers of contractions in the esophagus, abnormal velocity of contractions, abnormal force of contractions, abnormal coordinated timing of contractions, or several of these simultaneously. People with esophageal motility disorders may also experience spasms or chest pain.
Obstruction: People with an esophageal obstruction will have more difficulty swallowing solids than liquids.
Some symptoms of both include pain when swallowing, the inability to swallow, sensation of food being stuck in your throat or chest, drooling, and regurgitation.
Esophageal dysphagia can be diagnosed with a barium swallow, upper endoscopy, esophageal manometry, and an endoFLIP.
Some common treatments for esophageal dysphagia include medication, esophageal dilation, surgery, stent placement, and/or a feeding tube.
Esophagogastric Dysphagia
Esophagogastric dysphagia occurs when there is a problem with material passing from the lower esophageal sphincter into the gastric fundus.
Paraesophageal Dysphagia
Paraesophageal dysphagia occurs when the esophagus is narrowed due to extrinsic compression.
The ICD 10 Classifications
Oral phase - difficulty moving food or liquid to the back of the throat
Oropharyngeal phase - difficulty initiating swallowing
Pharyngeal phase - difficulty swallowing when food or liquid is at the top of the throat
Pharyngoesophageal phase - unable to find information
Other dysphagia- cervical dysphagia (caused by problems with the cervical spine) or neurogenic dysphagia (caused by problems with the central or peripheral nervous system)
Sources
x x x
+ some others I definitely (/sarcasm) didn't lose the link to
88 notes
·
View notes
Text
Unveiling The Gastric Problems: Common Symptoms And Their Causes
Gastric problems, ranging from mild discomfort to severe pain, can significantly impact daily life. Understanding the symptoms and their underlying causes is crucial for effective management and treatment. In this article, we'll explore seven common symptoms of gastric problems and delve into their potential causes, providing valuable insights for better health and well-being.

Abdominal Pain: Abdominal pain is a hallmark symptom of various gastric issues, including gastritis, ulcers, and gastroesophageal reflux disease (GERD). The pain may vary in intensity and location, ranging from a dull ache to sharp, stabbing sensations. Gastric ulcers, caused by the erosion of the stomach lining, often result in a burning pain in the upper abdomen. GERD, characterized by the reflux of stomach acid into the esophagus, can cause a burning sensation in the chest, known as heartburn.
Bloating and Gas: Excessive gas and bloating are common complaints associated with gastric problems. Gas can accumulate in the digestive tract due to factors such as swallowing air, bacterial fermentation of undigested food, or impaired digestion. Bloating, characterized by a feeling of fullness or tightness in the abdomen, often accompanies excessive gas production. Conditions like irritable bowel syndrome (IBS) and small intestinal bacterial overgrowth (SIBO) are frequently implicated in chronic bloating and gas.
Nausea and Vomiting: Nausea and vomiting are symptoms that can occur in various gastric disorders, including gastritis, gastroparesis, and peptic ulcers. Gastritis, inflammation of the stomach lining, can trigger nausea and vomiting, particularly after meals or when the stomach is empty. Gastroparesis, a condition characterized by delayed stomach emptying, may lead to persistent nausea and vomiting, especially after consuming solid foods. Peptic ulcers, open sores in the stomach or duodenum, can cause nausea and vomiting if they irritate the stomach lining.
Indigestion (Dyspepsia): Indigestion, also known as dyspepsia, encompasses a range of symptoms, including discomfort or pain in the upper abdomen, bloating, and a feeling of fullness during or after meals. It can occur as a result of various factors, such as overeating, eating too quickly, or consuming spicy or fatty foods. Gastric disorders like GERD, gastritis, and peptic ulcers can also manifest as indigestion. Persistent or recurrent indigestion warrants medical evaluation to identify and address the underlying cause.
Acid Reflux: Acid reflux occurs when stomach acid flows back into the esophagus, causing a burning sensation in the chest (heartburn) and a sour taste in the mouth. It is a common symptom of GERD, a chronic condition characterized by frequent episodes of acid reflux. Certain dietary and lifestyle factors, such as consuming acidic or fatty foods, smoking, and obesity, can exacerbate acid reflux. In some cases, structural abnormalities like a hiatal hernia may contribute to the development of GERD.
Loss of Appetite: A decreased appetite, or anorexia, can be a symptom of various gastric disorders, including gastritis, peptic ulcers, and inflammatory bowel disease (IBD). Gastritis, characterized by inflammation of the stomach lining, can lead to a loss of appetite due to discomfort or nausea associated with eating. Peptic ulcers, particularly those located in the stomach, can cause a feeling of early satiety or discomfort after meals, leading to reduced food intake. Inflammatory bowel disease, which includes Crohn's disease and ulcerative colitis, can affect the entire digestive tract and cause appetite loss.
Changes in Bowel Habits: Changes in bowel habits, such as diarrhea, constipation, or alternating episodes of both, can indicate underlying gastric issues. Conditions like IBS, characterized by abdominal pain and altered bowel habits without any detectable structural abnormalities, often present with diarrhea, constipation, or a combination of both. Inflammatory conditions like Crohn's disease and ulcerative colitis can cause diarrhea, often accompanied by abdominal pain, rectal bleeding, and weight loss. Constipation may occur due to factors such as inadequate fiber intake, dehydration, or certain medications.
Gastric problems can manifest in various ways, ranging from abdominal pain and bloating to acid reflux and changes in bowel habits. Identifying the symptoms and understanding their underlying causes are essential steps in managing gastric disorders effectively. If you experience persistent or severe symptoms, it is important to seek medical advice for proper evaluation and treatment. With the right approach, many gastric issues can be effectively managed, allowing for improved quality of life and overall well-being.
3 notes
·
View notes
Note
I hate to add onto this Kate Middleton discourse, but as someone who is in medical, it is quite curious. Because they said she had abdominal surgery to "correct something" and wants it to remain private (as it should), and not only that, but she had to be in the hospital for 10-14 days. That tells me, usually, it's about two things: it's either crohns or correcting weight loss surgery. Kate is a skinny tall woman. Almost too skinny for her height. I think they said she's like 5'10" or 5"11". But everyone's body is different. So you really can't always say "well they are this height, so their BMI should be this." Right?
However, Kate use to have a lot more meat on her. Even when they had their engagement announcement and she wore that iconic blue dress. As it got closer to her wedding, she get skinnier and skinnier. And she remained like that. When she was pregnant, she looked healthier. After pregnancies, some will lose weight and some won't snap back right away. Sometimes it takes a full year for your body to recover after pregnancy. Some people do lose a LOT of weight, especially if they are breast feeding. Breast feeding burns a lot of calories. This girl got sickly skinny. Especially after she had Prince Louis, her last baby. She will wear these long fancy gowns and you can just see the bones sticking out of her chest sometimes and her hips. Mermaid gowns are usually more flattering on taller women. We all know the stories about Diana. We know that a lot of the royals like to be well kept. They are in the public eye and critic all the time. Diana ate like a bird sadly even after she got over making her self sick. We also know too that Kate, while she was dating William, was just ripped apart by the media.
I highly suspect that:
1. Kate got a gastric sleeve that went haywire and she got it corrected. A lot of the times those don't hold, because the sleeve will get air pockets which will cause the person to get sick a lot. You can correct it, but there is a good chance that it's going to do it again. Thus having it removed is the best option.
2. Kate had gastric surgery and again, there are complications. A lot of people, especially smaller people who don't need the surgery, will constantly get sick. It's a very painful operation because they are re-routing your intestines etc etc. They have to limit what they eat. They have to cut out a lot of foods. There are people that get so sick and frail. With this surgery, it's not as easy to correct like the sleeve. There is a chance your body will NEVER go back to normal and you may have 10-20 years to live depending on the severity of it.
3. Kate may have crohns disease. Which is understandable if she wants to keep it private. Because a lot of people think it's always caused by starving yourself. But it is a very heraditory disease. And being in the public eye and the way that newspapers love to run with lies... Yeah, I don't blame her if this is the case. Especially since again, she's tall and very skinny for her height.
Deadass who cares what this woman doing or why she’s missing.
Bottom of my heart I do not care about to royals

( no offense to you anon )
3 notes
·
View notes
Text
natural remedy for gastroparesis

Gastroparesis or stomach paralysis is a condition in which the movement of the stomach (due to spontaneous muscle contraction) does not work properly. When the stomach muscles are strong and healthy, they push food forward along the digestive tract in preparation for release into the intestines.
In gastroparesis, this mobility is limited or absent at all, and therefore the contents of the stomach are not emptied completely. In this way, the natural digestion process is disrupted and the conditions for symptoms such as nausea, vomiting, increased blood sugar, etc. are provided.
Currently, there is no definitive treatment for this problem and only the symptoms can be improved. We recommend to start with home treatment of stomach paralysis and traditional medicine. If they are not effective, go to drug therapy. Because most home remedies are safe and without side effects.
Treatment of gastroparesis with home and natural methods
According to statistics, the probability of contracting gastric paralysis is about 50 cases per 100,000 people. Women are 4 times more prone to this problem than men.
Although experience has shown that home remedies are really effective in managing gastroparesis, it is very important to seek medical advice from a gastroenterologist and a neurologist. Because the complications of this disease, such as dehydration, malnutrition, and blood sugar fluctuations, can negatively affect the overall quality of life. In the following, we will mention the most important home remedies for stomach paralysis.
Change in eating habits
Here are some tips on how to eat that you can pay attention to in order to improve the condition and reduce the symptoms of gastroparesis. Things like:
Eating smaller meals
Eating smaller meals in several sessions will make your stomach completely empty and reduce bloating.
Proper chewing of food
the more food is chewed, the easier it is digested in the stomach. So, spend time chewing your food properly to help with digestion.
Avoid lying down during and after eating
When you lie down after eating, you stop the digestion process and slow down the digestion, because digestion needs gravity to function properly. In addition, lying down after a meal also helps the reflux of stomach acid into the esophagus.
Drink fluids between meals
Avoid drinking fluids with meals, as they take up space in the stomach and can slow digestion and cause bloating. Instead, drink fluids between meals to stay hydrated.
Regular practice of yoga
Yoga has been found to stimulate the normal function of the liver and pancreas to regulate blood sugar levels. As a result, if the blood sugar level increases or decreases, it can improve the symptoms of gastroparesis.
On the other hand, it has been found that performing abdominal exercises and yoga breathing exercises are useful as a means to better control gastroparesis. To do them, place one hand on your stomach and the other hand on your chest and focus on your breathing with your eyes closed. Inhale and exhale slowly through your nose and sometimes try to pinch your nose and tilt your chin to let all the air out. Slow down your breathing while concentrating.
Another movement is to rotate the spine while sitting on a chair. Place one arm behind the chair and look behind you while inhaling and exhaling slowly through your nose. Return to center and do the same for the other arm.
Another movement is to bring your arms towards your back with the help of interlaced fingers and extend them until the chest opens and the ribs are pushed out. Make sure to keep your attention on your breath in this situation.
Daily use of aloe vera for home treatment of stomach paralysis
Aloe vera helps the process of digestion and regulating bowel movement. In fact, as a natural laxative, it is effective in supporting the proper functioning of digestion and relieves bloating and stomach pain.
We recommend that you take a cup of aloe vera juice every morning before defecation for the home treatment of stomach paralysis. You can make this mixture by mixing two tablespoons of aloe vera gel with a cup of water or orange juice in a blender. Before meals, you can drink aloe vera juice. Avoid consuming more than two tablespoons of aloe vera gel per day.
Add apple cider vinegar to your diet
Apple cider vinegar helps to alkalize the body, which is effective in improving stomach pain, heartburn and bloating and improving the digestion process. Dissolving a teaspoon of apple cider vinegar in a cup of warm water and consuming it 15 to 20 minutes before meals is all you need to improve the symptoms and home remedies for gastric paralysis. Avoid undiluted apple cider vinegar, as it is too acidic and can damage your teeth.
Stomach paralysis diet
Paying attention to diet is another key measure that can help improve gastroparesis. In fact, knowing what to eat and what to avoid is important. In the following, we will refer to the complete details of the diet of gastric paralysis patients.
Suitable foods in gastroparesis diet
Common foods include fruits and vegetables in the form of purees and smoothies, canned peaches and pears, well-cooked fruits and vegetables, juices and soups. Because in the condition of stomach paralysis, the stomach does not have the power to digest well and we have to help this problem by chopping or heating the food. Of course, consulting a nutritionist can help you determine more suitable foods.
You should be careful with your fiber intake, because its increase in gastric paralysis can cause constipation and bloating. Therefore, consumption of low-fiber foods is recommended.
Try to eat more carbohydrates and starches such as corn tortillas, cookies, toasted grains, sweet potatoes (without the skin) and white or refined bread, crackers, bagels, pasta or rice.
To provide protein and calcium, low-fat cheese, custard, boiled eggs, minced or pureed meat, low-fat milk and milkshakes, plain yogurt and frozen yogurt, skinless chicken, oysters, tofu, and fish. Tons are great.
When following a gastroparesis diet, it is best to go for coconut oil, as it contains essential fatty chains that can aid in digestion.
In general, it's important to eat softer foods because they're easier to digest and put less stress on your digestive system. This issue is more important in following the gastric paralysis diet for children.
Prohibited foods in the gastroparesis diet
Experience has shown that avoiding certain foods can help reduce symptoms because they are difficult for the digestive system to digest.
To begin with, it is better to know that fatty and trans-containing foods delay gastric emptying. On the other hand, choosing the right fats such as unsaturated fats can help digestion. So be aware of the types of fats you consume.
As mentioned, consuming too much fiber can make symptoms worse, so low-fiber foods are a better option. High-fiber foods include fruits such as apples, berries, figs and oranges, vegetables such as broccoli, cauliflower, green beans, whole grains, nuts and seeds, beans and lentils.
Also, avoid eating foods that are not easily chewed, because they are harder to break down through the digestive process. These consist of corn, seeds, and nuts.
Avoid eating unhealthy foods such as fast food because they can cause blood sugar levels to fluctuate. Finally, cut back on alcohol as it significantly slows down gastric emptying.
Treatment of gastroparesis in traditional medicine
In addition to emphasizing the points mentioned about diet in gastroparesis or delayed gastric emptying, traditional medicine experts also emphasize the use of ginger as an anti-nausea herbal medicine. Drinking peppermint or chamomile tea may also be helpful.
On the other hand, placing a warm pad on the abdomen or a warm water bath may also help reduce abdominal pain associated with gastroparesis. Recently, traditional medicine has been able to prove the beneficial effects of acupuncture and acupressure for the treatment of gastric paralysis. In fact, these alternative solutions use the manipulation of trigger points on the body, either with pressure or with needles, to treat gastric paralysis with traditional medicine.
Some studies have also been able to show relief of bloating and other digestive symptoms in patients who have done acupressure or acupuncture. Usually, the wrist, forefoot and under the kneecap are the most effective trigger points for the treatment of gastric paralysis in traditional medicine.
Always talk to a traditional medicine practitioner before doing acupressure or acupuncture, as they know more about the key areas of the body to heal stomach and digestive problems.
When should we see a doctor?
We recommend that you see a doctor or traditional medicine specialist as soon as you experience the symptoms of stomach paralysis. Because any delay increases the possibility of complications of this disease.
Read the full article
2 notes
·
View notes
Text
Iron Deficiency/Anemia
Symptoms include:
Brittle nails
Cold hands and feet
Dizziness/Lightheadedness
Fatigue
Cravings for ice, dirt, or starch
Chest pain
Fast heartbeat
Shortness of breath
Sudden weight gain
Increased risk of anxiety and depression
Increased risk of sleep disorders
Causes:
Blood loss due to menstruation.
Inability to absorb iron due to conditions such as Celiac disease, Ulcerative Colitis, or Crohn's disease. Gastric Bypass surgeries remove part of the intestines and affect iron absorption. Medicines used to lower stomach acid can also affect iron absorption.
Vitamin B12 deficiency. Vitamin B12 is required for the production of red blood cells.
Recommendations:
Iron supplements can introduce more iron into your body. It can take 2-3 weeks of taking them regularly to see results and it may be recommended that you take them for several months to build up your iron reserves.
Iron-rich foods naturally introduce iron into your body. Examples of these foods include green leafy vegetables, raspberries, almonds, cashews, beans, seafood, dried fruit, red meat, pork, poultry, and peas.
An increase of Vitamin C can assist in iron absorption. Citrus fruits, bell peppers, broccoli, strawberries, cantaloupe are all sources of Vitamin C.
Organs to target:
Your liver is responsible for making iron.
The thyroid gland is possibly underactive and causing a sudden weight gain.
6 notes
·
View notes
Text
5 Reasons to See a Best gastro doctor in Delhi
What is a Gastroenterologist?
A gastroenterologist is a medical specialist who diagnoses and treats disorders of the digestive tract or gastrointestinal (GI) system. People turn to a gastroenterologist when their condition is beyond the capabilities of their primary physician. The primary doctor is generally the person who refers a patient to a Best gastro clinic. A gastroenterologist treats both women and men.
5 Reasons to See a Gastroenterologist
Heartburn: Heartburn can be described as burning or pain in the throat or chest. It is caused by acid that comes from the stomach re-enters to the esophagus. It's the tube which connects the mouth with the stomach. Many suffer from heartburn every now and then. It is usually gone on its own or by taking prescription medications. However, signs that appear more frequently than once a week may be an indication of a more serious issue: gastro esophageal reflux disease (GERD). GERD is caused by acid that comes from the stomach causes irritation to the esophagus's lining. GERD is more prevalent among smokers or those who are overweight. Pregnant women are also more likely to be affected by the condition. There are medications available to treat GERD. Severe cases may need surgery. If left untreated, GERD could lead to more serious issues, like chronic inflammation of the esophagus, as well as breathing issues.

Gallstones : Gallstones are tiny, hard nuggets formed inside the gallbladder, which is an organ that is located inside the abdomen. Gallstones could be as small as the size of a grain of sand, or as large as the size of a golf ball. Many people possess one huge stone. Other people have multiple stones with different dimensions. A sudden discomfort at the back of the stomach may be due to a gallstone. Gallstone pain disappears after they are moved. Gallstones form due to unbalanced components that form the bile. This is the digestive fluid produced by liver. Doctors aren't sure what causes these imbalances. Pregnant women and overweight people are more likely than other women to develop gallstones. Gallstones are also more frequent with age. Anyone who has suffered from one gallstone is likely to be at the risk of having another. Most patients who suffer from gallstones undergo surgery to eliminate their gallbladder. In some instances, medications can help dissolve the stones.
Lactose Intolerance: Individuals who experience uncomfortable symptoms when drinking or eating milk products could suffer from lactose-intolerant. Lactose is a type of sugar that can be found in milk. The body produces lactase, a protein in order to breakdown milk-based products like yogurt and cheese.
However, people suffering from an intolerance to lactose aren't able to produce enough lactase to completely absorb even tiny portions of these food items. This may cause gastric pain, bloating gas, diarrhea, and upset stomachs. The symptoms usually manifest at least two hours after having eaten dairy. They can be moderate to severe. Gastroenterologists may check to determine if you have lactose intolerance. Treatment can involve supplements to your diet and modifications in your food.
Celiac Disease: Celiac Disease is an inherited disease which affects an immune system. The sufferers should avoid eating gluten. Gluten can be found that is found in wheat, rye , and barley. It is also found in certain medications or vitamins as well as supplements. When those suffering from celiac disease consume gluten, their immune system is triggered by causing damage to their small intestine. This may cause pain or diarrhea. A blood test is a good way to determine if you have celiac disease. A gastroenterologist might also be required to analyze a sample from the small intestine in order to check for any damage. Celiac disorder is not similar to gluten sensitivities. Both conditions have similar symptoms. The primary distinction is that those with gluten sensitivities do not develop damage to their small intestines. Eliminating gluten completely can help ease signs of celiac illness as well as gluten sensitivity. It is possible that you will require further treatment to treat intestinal damage.
Colon Cancer Screening: A gastroenterologist may examine for the signs of certain conditions, like colon cancer even if you do not have symptoms. In an colonoscopy such as a colonoscopy the doctor inserts the thin tube and tiny cameras inside the rectum in order to view how the colon is constructed. Imaging scans as well as stool samples can aid in diagnosing cancer.

Colon cancer typically develops due to abnormal growths that occur on the rectum, or the colon. Rectifying these abnormalities early can help doctors eliminate them before they stand an opportunity to develop into cancerous. Early detection and treatment of cancer helps save lives. At the age 50, all patients should be screened regularly for colon cancer.
2 notes
·
View notes
Text
The Impact of Stress on Digestive Health and Strategies for Coping

In this fast life, stress has become an all too familiar companion for us. From work deadlines to family responsibilities, financial worries to health concerns, stress can manifest in various forms and take a toll on our physical and mental well-being. But stress has a negative impact on not just emotional but physical aspects of our body too. In this blog, doctors from SIDS Hospital, one of the best hospitals in Surat, have explored the connection between stress and digestive health, as well as strategies for coping and promoting a healthy balance.
Understanding the Gut-Brain Connection
The gut-brain connection refers to the bidirectional communication between the brain and the gastrointestinal (GI) tract. This complex relationship involves a network of nerves, hormones, and neurotransmitters that influence digestive function and overall well-being. Whether acute (short-term) or chronic (long-term), stress can disrupt the delicate balance and affect the functioning of the digestive system.
The Impact of Stress on Digestive Health
Doctors from the best gastro hospital in Surat, SIDS Hospital, have seen the negative impact of stress on the digestive health, leading to symptoms such as:
Digestive Upset:
Stress can trigger or exacerbate symptoms of digestive upset, including abdominal pain, cramping, bloating, gas, and diarrhoea. These symptoms may be related to changes in gut motility, increased sensitivity to pain, or alterations in the gut microbiome.
Heartburn and Acid Reflux:
Stress can worsen symptoms of gastroesophageal reflux disease (GERD), including heartburn, regurgitation, and chest pain. Stress may increase the production of stomach acid and relax the lower esophageal sphincter, allowing stomach acid to reflux into the oesophagus and cause discomfort.
Changes in Appetite:
Stress can affect appetite regulation, leading to changes in eating habits such as overeating or undereating. Some individuals may turn to comfort foods high in sugar, fat, and calories during times of stress, while others may experience a loss of appetite and decreased food intake.
Exacerbation of Digestive Disorders:
For individuals with pre-existing digestive disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), or functional dyspepsia, stress can exacerbate symptoms and trigger flare-ups. Stress may contribute to increased gut inflammation, heightened visceral sensitivity, and alterations in gut microbiota composition.
Impaired Digestion and Nutrient Absorption:
Chronic stress can impair digestive function by diverting blood flow away from the digestive organs and inhibiting secretion of digestive enzymes and gastric acid. This can lead to impaired digestion and absorption of nutrients, potentially affecting overall nutritional status and health.
Strategies for Coping with Stress and Promoting Digestive Health
While stress is an inevitable part of life, these strategies shared by the experts of SIDS Hospital, well-known as one of the best gastro hospitals in Surat, can help you to cope with stress and promote digestive health:
Mindfulness and Relaxation Techniques:
Practice mindfulness meditation, deep breathing exercises, progressive muscle relaxation, or guided imagery to promote relaxation and reduce stress levels. These techniques can help calm the mind, alleviate physical tension, and improve overall well-being.
Regular Physical Activity:
Engage in regular physical activity such as walking, jogging, yoga, or swimming to reduce stress and promote digestive health. Exercise helps release endorphins, neurotransmitters that boost mood and reduce stress, while also promoting regular bowel movements and healthy digestion.
Healthy Eating Habits:
Adopt a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats to support digestive health. Avoiding excessive intake of caffeine, alcohol, processed foods, and high-fat or spicy foods can help reduce the risk of digestive upset and promote overall well-being.
Adequate Sleep:
Prioritize quality sleep by establishing a regular sleep schedule, creating a restful sleep environment, and practicing good sleep hygiene habits. Adequate sleep is essential for reducing stress, supporting immune function, and promoting optimal digestive health.
Social Support:
Seek support from friends, family members, or support groups to help cope with stress and promote emotional well-being. Talking about your feelings, sharing experiences, and connecting with others can provide comfort, validation, and perspective during difficult times.
Stress Management Techniques:
Explore stress management techniques such as journaling, art therapy, or spending time in nature to help cope with stress and promote emotional resilience. Finding activities that bring joy, relaxation, and fulfillment can help buffer the effects of stress on digestive health.
Professional Support:
If stress is significantly impacting your quality of life or digestive health, consider seeking support from a healthcare professional such as a therapist, counsellor, or gastroenterologist. They can provide personalized guidance, resources, and treatment options to help address your specific needs and concerns.
Conclusion
Stress can have a profound impact on digestive health, leading to symptoms such as digestive upset, heartburn, changes in appetite, and exacerbation of digestive disorders. Practicing mindfulness, engaging in regular physical activity, adopting healthy eating habits, prioritizing sleep, seeking social support, exploring stress management techniques, or seeking professional support — these are some practices shared by the best gastroenterologists in Surat that can help in nurturing digestive health in times of stress.
0 notes
Text
Navigating the Gastric Maze: Understanding Esophageal and Gastric Diseases
Introduction:
The esophagus and stomach form essential parts of the digestive system, facilitating the passage and digestion of food. However, various diseases can affect these organs, causing discomfort, pain, and potentially serious complications. In this blog, we'll explore common esophageal and gastric diseases, their causes, symptoms, diagnosis, and treatment options.
Gastroesophageal Reflux Disease (GERD):
GERD is a chronic condition characterized by the reflux of stomach contents into the esophagus, leading to symptoms such as heartburn, regurgitation, chest pain, and difficulty swallowing. Contributing factors may include obesity, hiatal hernia, dietary habits, and smoking. Diagnosis is based on clinical evaluation, symptom assessment, and diagnostic tests such as upper endoscopy and esophageal pH monitoring. Treatment options range from lifestyle modifications (e.g., dietary changes, weight loss) to medications (e.g., proton pump inhibitors, H2 blockers) and, in severe cases, surgical intervention (e.g., fundoplication) to reinforce the lower esophageal sphincter.
Peptic Ulcer Disease:
Peptic ulcer disease involves the development of open sores (ulcers) in the lining of the stomach (gastric ulcers) or the duodenum (duodenal ulcers). Helicobacter pylori infection and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) are common risk factors. Symptoms may include abdominal pain, bloating, nausea, vomiting, and gastrointestinal bleeding. Diagnosis is made through endoscopic evaluation, with treatment aimed at eradicating H. pylori infection (if present), reducing acid secretion with medications (e.g., proton pump inhibitors, H2 blockers), and promoting ulcer healing.
Gastric Cancer:
Gastric cancer, also known as stomach cancer, is a malignant tumor that develops in the lining of the stomach. Risk factors include Helicobacter pylori infection, chronic gastritis, smoking, family history, and certain dietary factors. Symptoms may include abdominal pain, unintended weight loss, loss of appetite, nausea, vomiting, and blood in the stool. Diagnosis involves imaging studies such as CT scans, endoscopy with biopsy, and staging procedures. Treatment options depend on the stage of the cancer and may include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy.
Barrett's Esophagus:
Barrett's esophagus is a condition in which the normal lining of the esophagus is replaced by tissue similar to the lining of the intestine, often due to long-standing GERD. While many individuals with Barrett's esophagus remain asymptomatic, it is associated with an increased risk of esophageal adenocarcinoma, a type of cancer. Diagnosis is made through endoscopic evaluation with biopsy, and surveillance is recommended to detect dysplasia or early cancerous changes. Treatment may involve acid suppression therapy, endoscopic surveillance, and, in cases of dysplasia or early cancer, endoscopic or surgical interventions.
esophageal and gastric diseases involves exploring a range of conditions affecting the esophagus and stomach, from inflammatory disorders to malignancies. Here’s a comprehensive overview of some key diseases:
Esophageal Diseases
Gastroesophageal Reflux Disease (GERD):
Definition: A chronic condition where stomach acid flows back into the esophagus, causing irritation.
Symptoms: Heartburn, regurgitation, chest pain, and difficulty swallowing.
Diagnosis: Clinical evaluation, endoscopy, esophageal pH monitoring, and manometry.
Treatment: Lifestyle modifications (diet, weight loss), antacids, H2-receptor antagonists, proton pump inhibitors (PPIs), and in severe cases, surgical interventions such as fundoplication (MDLinx) (MGMA Homepage).
Esophageal Stricture:
Definition: Narrowing of the esophagus, often due to chronic GERD, radiation therapy, or ingestion of corrosive substances.
Symptoms: Difficulty swallowing, pain when swallowing, and food impaction.
Diagnosis: Barium swallow, endoscopy.
Treatment: Endoscopic dilation, PPIs, and managing the underlying cause (MDLinx) (MGMA Homepage).
Barrett’s Esophagus:
Definition: A condition where the normal esophageal lining changes to a type similar to the intestinal lining, often due to chronic GERD.
Symptoms: Often asymptomatic but can include symptoms of GERD.
Diagnosis: Endoscopy with biopsy.
Treatment: Regular monitoring with endoscopy, PPIs, and in some cases, endoscopic or surgical removal of abnormal tissue to prevent progression to esophageal cancer (MDLinx) (MGMA Homepage).
Esophageal Cancer:
Definition: Malignancy of the esophagus, with two main types: adenocarcinoma (associated with Barrett’s esophagus) and squamous cell carcinoma.
Symptoms: Dysphagia, weight loss, chest pain, and chronic cough.
Diagnosis: Endoscopy with biopsy, imaging studies (CT, PET scans).
Treatment: Surgery, chemotherapy, radiation therapy, and palliative care (MDLinx) (MGMA Homepage).
Gastric Diseases
Gastritis:
Definition: Inflammation of the stomach lining, which can be acute or chronic.
Causes: Helicobacter pylori infection, NSAIDs, alcohol, stress.
Symptoms: Abdominal pain, nausea, vomiting, and in chronic cases, bleeding.
Diagnosis: Endoscopy, biopsy, testing for H. pylori.
Treatment: Antibiotics for H. pylori, PPIs, H2-receptor antagonists, and avoiding irritants (MDLinx) (MGMA Homepage).
Peptic Ulcer Disease (PUD):
Definition: Open sores that develop on the inside lining of the stomach or the upper part of the small intestine.
Causes: H. pylori infection, long-term use of NSAIDs.
Symptoms: Burning stomach pain, bloating, heartburn, nausea.
Diagnosis: Endoscopy, urea breath test, stool antigen test, blood test for H. pylori.
Treatment: Antibiotics for H. pylori, PPIs, H2-receptor antagonists, antacids, and lifestyle changes (MDLinx) (MGMA Homepage).

Gastric Cancer:
Definition: Malignancy of the stomach lining, often diagnosed at an advanced stage.
Symptoms: Weight loss, abdominal pain, nausea, vomiting, early satiety, and in advanced cases, gastrointestinal bleeding.
Diagnosis: Endoscopy with biopsy, imaging studies (CT, PET scans).
Treatment: Surgery, chemotherapy, radiation therapy, and targeted therapies (MDLinx) (MGMA Homepage).
Diagnostic Techniques
Endoscopy: A key tool for visualizing the esophagus and stomach, obtaining biopsies, and diagnosing conditions like GERD, Barrett’s esophagus, gastritis, and cancer.
Imaging: Barium swallow, CT scans, and PET scans help in diagnosing structural abnormalities, strictures, and cancers.
Laboratory Tests: Blood tests for anemia and H. pylori, stool tests, and esophageal pH monitoring for GERD.
Conclusion:
Esophageal and gastric diseases present diverse challenges in clinical practice, requiring a comprehensive approach to diagnosis and management. Early recognition of symptoms, targeted diagnostic evaluations, and timely intervention are essential for optimizing outcomes and preventing complications. Through ongoing research, advancements in diagnostic techniques, and innovative therapeutic modalities, healthcare providers continue to make strides in the understanding and treatment of esophageal and gastric diseases, offering hope to patients affected by these complex conditions.
Important Information:
Conference Name: 14th World Gastroenterology, IBD & Hepatology Conference
Short Name: 14GHUCG2024
Dates: December 17-19, 2024
Venue: Dubai, UAE
Email: [email protected]
Visit: https://gastroenterology.universeconferences.com/
Call for Papers: https://gastroenterology.universeconferences.com/submit-abstract/
Register here: https://gastroenterology.universeconferences.com/registration/
Exhibitor/Sponsor: https://gastroenterology.universeconferences.com/exhibit-sponsor-opportunities/
Call Us: +12073070027
WhatsApp Us: +442033222718
0 notes
Text
Suffering from Abdominal Pain? When to Seek Help
Abdominal pain is a common complaint that can range from mild discomfort to severe agony. While occasional abdominal discomfort may not raise concerns, persistent or severe pain should never be ignored. In this blog, we’ll delve into the various causes of abdominal pain, when to seek medical attention, and the importance of consulting a trusted healthcare provider.

Causes of Abdominal Pain
Abdominal pain can originate from numerous organs within the abdomen, including the stomach, intestines, liver, gallbladder, pancreas, kidneys, and reproductive organs. Some common causes of abdominal pain include:
1. Gastric Issues: Acid reflux, gastritis, and ulcers can lead to stomach discomfort or pain.
2. Gastrointestinal Disorders: Conditions such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and gastroenteritis can cause pain in the abdomen, bloating, and changes in bowel habits.
3. Gallbladder and Liver Problems: Gallstones, gallbladder inflammation, and liver conditions like hepatitis can result in abdominal pain, particularly in the upper right.
4. Pancreatitis: Inflammation of the pancreas can cause severe abdominal pain, often radiating to the back.
5. Urinary Tract Infections (UTIs): Infections of the bladder or kidneys can cause abdominal pain or discomfort in the lower abdomen.
6. Reproductive Issues: Conditions affecting the reproductive organs, such as ovarian cysts, endometriosis, or pelvic inflammatory disease, can lead to abdominal pain, particularly in women.
When to seek Medical attention
While mild abdominal discomfort may resolve on its own or with home remedies, certain symptoms warrant prompt medical attention. You should seek medical help if you experience:
– Severe or persistent abdominal pain
– Abdominal pain accompanied by fever, nausea, vomiting, or diarrhea
– Abdominal pain that worsens with movement or certain positions
– Abdominal pain following injury or trauma to the abdomen
– Abdominal pain in conjunction with difficulty breathing or chest pain
– Abdominal pain during pregnancy
Ignoring abdominal pain or attempting to self-diagnose could lead to delayed treatment and potentially serious consequences.
Treatment Care at Thangam Multispecialty Hospital
When confronted with abdominal pain, seek consultation from the best Gastroenterology doctor in Palakkad to obtain an accurate diagnosis and appropriate treatment regimen. Our Gastroentrology department at Thangam Hospital is a well-respected medical institution renowned for its expertise in diagnosing and treating a wide spectrum of medical conditions.
Our highly skilled healthcare professionals utilises the latest diagnostic tools and techniques to accurately identify the underlying cause of your abdominal pain. Once a diagnosis is established, they will tailor a treatment plan specifically designed to alleviate your symptoms and address the root cause of your discomfort.
The hospital’s commitment to providing comprehensive and compassionate care extends to all patients seeking treatment for abdominal pain. Whether you require conservative management or more specialized interventions, our experienced doctors at Thangam Hospital is dedicated to providing the highest quality of care.
Trust Thangam Multispecialty Hospital to provide you with the expert diagnosis and effective treatment you need to manage your abdominal pain and restore your well-being. Furthermore, we prioritize patient comfort, safety, and well-being, providing compassionate care in a supportive environment. Whether you require medical intervention, diagnostic tests, or expert advice, Thangam Hospital’s dedicated team is committed to providing the highest quality of care at every step of your journey to recovery.
Don’t Ignore Abdominal Pain
In conclusion, abdominal pain is a symptom that warrants attention, especially when accompanied by other concerning symptoms. Ignoring abdominal pain or attempting to self-diagnose can lead to complications and worsen underlying conditions. Trust our expertised healthcare professionals at Thangam Multi speciality Hospital to accurately diagnose and effectively treat abdominal pain, ensuring your health and well-being are prioritized.
If you’re experiencing abdominal pain, don’t delay— Make an appointment with your doctor
and seek medical attention promptly for proper evaluation and care.
0 notes
Text
Navigating the Digestive Maze: Exploring Gastroenterology
Introduction:
The human digestive system is a marvel of complexity, comprising a series of organs and processes that work together to break down food, absorb nutrients, and eliminate waste. From the moment food enters the mouth to its journey through the esophagus, stomach, intestines, and beyond, the digestive tract plays a crucial role in maintaining our overall health and well-being. However, when problems arise within this intricate system, the field of gastroenterology steps in to unravel the mysteries and provide solutions. In this blog, we'll embark on a journey through the digestive maze, exploring the fascinating world of gastroenterology and its significance in healthcare.
UCJournals provide a platform for , We cordially extend an invitation to researchers from all around the globe to submit their research work for publishing in our Global Journal Of Gastroenterology & Hepatology Research.
To know more, visit here: https://www.ucjournals.com/journals/global-journal-of-gastroenterology-hepatology-research/

Understanding the Digestive System:
Before delving into the realm of gastroenterology, it's essential to have a basic understanding of the digestive system's anatomy and function. The process begins in the mouth, where enzymes in saliva start breaking down food as it's chewed. The food then travels down the esophagus and into the stomach, where gastric juices further break it down into a semi-liquid substance known as chyme. From there, chyme enters the small intestine, where the majority of nutrient absorption occurs, facilitated by specialized structures called villi and microvilli. Finally, any remaining waste passes into the large intestine, where water is absorbed, and feces are formed before being expelled from the body.
The Role of Gastroenterology:
Gastroenterology is the branch of medicine focused on the digestive system and its disorders. Gastroenterologists are highly trained specialists who diagnose and treat a wide range of conditions affecting the esophagus, stomach, intestines, liver, gallbladder, and pancreas. They utilize various diagnostic tools and procedures, such as endoscopy, colonoscopy, imaging studies, and laboratory tests, to identify gastrointestinal (GI) issues accurately. From common ailments like acid reflux and irritable bowel syndrome (IBS) to more complex conditions such as Crohn's disease and liver cirrhosis, gastroenterologists play a vital role in managing digestive health and improving patients' quality of life.
UCJournals provide a platform for , We cordially extend an invitation to researchers from all around the globe to submit their research work for publishing in our Global Journal Of Gastroenterology & Hepatology Research.
To know more, visit here: https://www.ucjournals.com/journals/global-journal-of-gastroenterology-hepatology-research/

Common Gastrointestinal Disorders:
Let's take a closer look at some of the most prevalent gastrointestinal disorders that gastroenterologists encounter:
Gastroesophageal Reflux Disease (GERD): Characterized by chronic acid reflux, GERD can lead to heartburn, regurgitation, chest pain, and complications like esophagitis and Barrett's esophagus.
Inflammatory Bowel Disease (IBD): Including Crohn's disease and ulcerative colitis, IBD involves chronic inflammation of the digestive tract, causing symptoms such as abdominal pain, diarrhea, rectal bleeding, and weight loss.
Irritable Bowel Syndrome (IBS): A functional disorder of the intestines, IBS manifests as abdominal pain or discomfort, bloating, and changes in bowel habits without any evidence of structural damage.
Gallstones: Hardened deposits in the gallbladder, gallstones can cause abdominal pain, nausea, vomiting, and complications such as cholecystitis and pancreatitis.
Celiac Disease: An autoimmune disorder triggered by gluten consumption, celiac disease damages the small intestine and leads to symptoms like diarrhea, abdominal pain, fatigue, and malnutrition.
The Importance of Seeking Professional Care:
While some gastrointestinal symptoms may resolve on their own or with minor interventions, others require medical attention from a gastroenterologist. Ignoring persistent digestive issues or attempting to self-diagnose and treat can lead to complications and delayed recovery. Gastroenterologists have the expertise and resources to accurately diagnose GI disorders and develop personalized treatment plans tailored to each patient's needs. Whether it's lifestyle modifications, medications, endoscopic procedures, or surgery, their goal is to alleviate symptoms, promote healing, and improve overall digestive health.
UCJournals provide a platform for , We cordially extend an invitation to researchers from all around the globe to submit their research work for publishing in our Global Journal Of Gastroenterology & Hepatology Research.
To know more, visit here: https://www.ucjournals.com/journals/global-journal-of-gastroenterology-hepatology-research/

Conclusion:
Navigating the digestive maze can be challenging, but with the guidance of skilled gastroenterologists, patients can find their way to better gastrointestinal health. From routine screenings and preventive care to advanced treatments for complex conditions, gastroenterology offers a comprehensive approach to managing digestive disorders and optimizing well-being. By understanding the importance of digestive health and seeking timely medical care when needed, individuals can enjoy a higher quality of life and digestive comfort for years to come.
0 notes
Text
Rooting Out Heartburn: A Functional Medicine Perspective

Are you tired of experiencing that burning sensation in your chest after a meal? Do antacids seem like your constant companion? You're not alone. Acid reflux disease, also known as heartburn or gastroesophageal reflux disease (GERD), affects approximately 20% of the population in the United States alone, with numbers steadily rising globally. But there's more to relief than just relying on medications. Let's delve into the lesser-known aspects of acid reflux disease: its causes, effects, and holistic solutions, including my 7-day detox program tailored for its victims.
Understanding Acid Reflux Disease:
Acid reflux disease goes beyond being merely uncomfortable—it's a signal from your body that something is amiss. While commonly associated with overeating, consuming trigger foods like chocolate or spicy dishes, or eating late at night, the root cause is often more complex. Contrary to popular belief, most cases of acid reflux aren't solely due to excess stomach acid but are instead influenced by various lifestyle choices and underlying conditions.
"The thing about heartburn is that most of the time it's not too much acid. Your body needs and wants to have acid in the stomach to help you breakdown your food. The only exception are people with a rare digestive disorder (Zollinger-Ellison syndrome) that results in too much acid. This excess gastric acid can cause peptic ulcers in your stomach and intestine. Symptoms include abdominal pain, nausea, vomiting, weight loss, and diarrhea." -Dr. Todd Lepine on the Doctor's Farmacy podcast with Mark Hyman, MD.
The unspoken Dangers Of Medication
While medications like proton pump inhibitors (PPIs) are frequently prescribed for acid reflux, they carry significant risks. Long-term use can lead to nutrient deficiencies, including magnesium and vitamin B12, as well as increase the risk of osteoporosis and dependency on the medication. These dangers are often overlooked in mainstream discussions about acid reflux treatment.
A Holistic Approach Through Functional Medicine:
Functional medicine takes a comprehensive approach to understanding the root causes of heartburn and reflux, recognizing that these symptoms can be indicative of underlying issues beyond just dietary habits or lifestyle choices. One such underlying cause that functional medicine explores is the presence of H. pylori infection.
Helicobacter pylori (H. pylori) is a bacterium that commonly resides in the stomach lining. While it doesn't always cause symptoms, H. pylori infection has been associated with various gastrointestinal conditions, including gastritis, peptic ulcers, and even gastric cancer in some cases. The bacterium is typically transmitted through oral-oral or fecal-oral routes, often in childhood, and can persist for years if left untreated.
Functional medicine practitioners recognize the importance of testing for H. pylori infection as part of a comprehensive approach to managing heartburn and reflux. There are several methods available for detecting the presence of H. pylori:
Stool Testing: Stool tests can detect the presence of H. pylori antigens in fecal samples, providing a non-invasive way to diagnose the infection. This method is particularly useful for individuals who may not tolerate other testing methods well.
Antibody Testing: Blood tests can measure the presence of antibodies produced by the immune system in response to H. pylori infection. While antibody testing can indicate past or current infection, it may not distinguish between active and inactive infection, so additional testing may be necessary.
Breath Testing: Breath tests involve consuming a substance containing carbon-labeled urea, which is metabolized by H. pylori in the stomach. As the bacteria break down the urea, they release carbon dioxide, which can be detected in the breath. This non-invasive method is often used to confirm the presence of active H. pylori infection.
SEE ALSO: Simple Aids For Digestion [Video]
Natural Solutions and Lifestyle Modifications:
While medications may provide temporary relief, long-term management of acid reflux involves natural solutions and lifestyle changes. Dietary modifications, such as avoiding trigger foods and incorporating supplements like deglycyrrhizinated licorice (DGL) and aloe vera, can significantly alleviate symptoms. Lifestyle changes such as quitting smoking, elevating the head of the bed, and practicing stress-reducing techniques like yoga or meditation are also essential components of holistic management.
The Path to Lasting Relief:
By seeking guidance from functional medicine practitioners and adopting a proactive approach to health, individuals suffering from acid reflux disease can reclaim control over their lives. It's not just about masking symptoms—it's about addressing the underlying causes and restoring vitality. With the right support and strategies, relief from acid reflux is achievable, allowing you to enjoy meals and daily activities without the fear of discomfort.
Recommended Functional Medicine Doctors In Florida:
1) Phil Kaplan, a pioneer in health and fitness for over three decades, boasts a lifetime achievement award and over half a million satisfied clients. His own misdiagnosis in 2005 ignited his journey to revolutionize medical fitness, bridging the gap between fitness and medicine. Partnering with renowned scientist Dr. Kristin Comella, Phil founded Infinite Impact in Boca Raton, Florida. This integrative center offers a unique blend of medical expertise and fitness coaching, providing real solutions for chronic disease and weight loss resistance. Join them on the journey to rediscover your greatest potential at Infinite Impact.
2) Dr. Aixa Goodrich, a trusted figure in functional medicine, goes beyond conventional approaches. Through her Instagram platform, she educates on big pharma's pitfalls and insurance limitations. With 24 years of experience in Miami, her dedication shines through testimonials, like Marie C.'s, showcasing her commitment to holistic patient care. Additionally, certified as a Transformational Life Coach by Jack Canfield, Dr. Goodrich ensures her clients receive comprehensive guidance for long-term health.
Introducing the 7-Day Detox Program:
If you can't afford to see a functional medicine right now, at the very least consider incorporating my 7 day detox program. Designed specifically for victims of acid reflux disease, this program focuses on eliminating trigger foods, reducing inflammation, and supporting digestive health. By following a structured plan under the guidance of a healthcare professional, you can kickstart your journey towards lasting relief from acid reflux symptoms. Don't let financial constraints hold you back from reclaiming your health. Start your journey towards wellness today.
0 notes
Text
7 Post-Bariatric Surgery Disorders: Guidelines & Diet Phases
Post-Bariatric Surgery Complications: Exploring Potential Disorders
Dumping Syndrome: After undergoing bariatric surgery, individuals may experience Dumping Syndrome, characterized by rapid passage of food from the stomach to the small intestine. This condition is often triggered by the consumption of sugary or high-carbohydrate foods, leading to symptoms like nausea, vomiting, abdominal discomfort, and dizziness. Hormonal changes resulting from this rapid transit contribute to the manifestation of these symptoms.
Nutritional Deficiencies: Bariatric surgery can disrupt the absorption of essential nutrients, potentially causing deficiencies in iron, vitamin B12, calcium, and vitamin D. These deficiencies may present as fatigue, weakness, hair loss, and bone issues. Alterations to the digestive tract’s anatomy reduce the surface area available for nutrient absorption, necessitating careful dietary management and supplementation.
Gastroesophageal Reflux Disease (GERD): Following bariatric surgery, some individuals may develop or experience worsening symptoms of GERD, particularly after procedures like gastric sleeve or gastric bypass. GERD involves the backward flow of stomach acid into the esophagus, leading to symptoms such as severe heartburn, chest pain, regurgitation, and difficulty swallowing. Changes in stomach anatomy post-surgery can exacerbate GERD by altering the mechanism that prevents acid reflux.
Gallstones: Rapid weight loss post-surgery increases the risk of gallstone formation. Gallstones may cause symptoms such as abdominal pain, nausea, vomiting, and jaundice. Increased cholesterol excretion and reduced bile acid secretion post-surgery contribute to gallstone development.
Maladaptive Eating Behaviors: Some individuals may develop unhealthy eating habits or disordered eating patterns following bariatric surgery, such as binge eating or grazing. These behaviors can hinder weight loss efforts and overall well-being, possibly stemming from psychological factors or changes in hunger hormones post-surgery.
Stomal Stenosis: In gastric bypass surgery, the connection between the stomach pouch and the small intestine (stoma) may narrow over time, leading to symptoms like difficulty eating, nausea, vomiting, and abdominal discomfort. This complication may require interventions such as endoscopic dilation or surgical revision.
Ulcers : Post-bariatric surgery, some patients may develop ulcers in the stomach or small intestine, especially those using NSAIDs or tobacco. Symptoms include sudden vomiting, abdominal pain, nausea, and bleeding. Changes in stomach acid secretion and mucosal protection post-surgery contribute to ulcer formation.
Read More: https://toneop.com/blog/post-bariatric-surgery-disorders
0 notes
Text
Clinical Applications of Spandan ECG in Distinguishing Gastric Pain from Cardiac Chest Pain
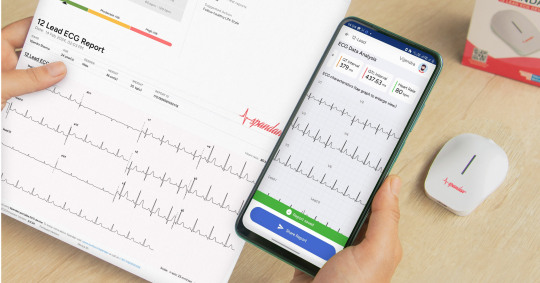
The Spandan ECG device is instrumental in clinical practice for differentiating between Gastric pain and Cardiac chest pain. It helps identify specific electrocardiographic changes associated with cardiac ischemia or infarction, such as ST-segment elevation or depression, T-wave inversion, and pathological Q waves. By continuously monitoring ECG patterns, it enables the detection of dynamic changes over time, aiding in the diagnosis of cardiac chest pain, particularly in cases of intermittent myocardial ischemia.
While gastric pain typically does not produce distinct ECG alterations, the absence of significant abnormalities can help rule out cardiac causes, supporting the diagnosis of gastric pain. Interpretation of ECG findings with the Spandan device is complemented by clinical correlation, considering factors like the onset, duration, and character of pain, as well as associated symptoms.
Collaboration with specialists, especially cardiologists, enhances the accuracy of interpretation and guides decision-making regarding further diagnostic tests or interventions. Additionally, the device assists in risk stratification, helping identify patients at high risk of cardiac events for appropriate management.
In summary, the Spandan ECG device is invaluable in clinical settings, providing timely and accurate electrocardiographic data to aid healthcare providers in distinguishing between gastric and cardiac causes of chest pain, leading to prompt and appropriate patient management.
0 notes
Text
How to Recognize the Signs of a Heart Attack by Dr Richard Zelman
Heart attacks are medical emergencies requiring urgent medical intervention, typically manifested as chest pain and dizziness.
Recognizing the early warning signs of a heart attack can save lives by getting you to medical professionals sooner. By calling emergency services immediately upon experiencing symptoms, medical personnel can start work to restore blood flow and lessen damage more quickly.
Early Warning Signs
When we think of heart attacks, they usually conjure images from movies - someone clutching their chest and collapsing. In reality, however, most heart attacks don't start suddenly - they typically begin slowly. They may be challenging to recognize as heart attacks because their symptoms mimic other conditions, such as acid reflux or influenza.
As per Dr Richard Zelman, chest pain or pressure may feel like uncomfortable pressure, squeezing, fullness, or tightening and can spread to other body parts - including arms, back, neck, jaw, or stomach. This could be the early warning sign of a heart attack, so medical attention must be sought immediately.
Concern should arise if pain increases with activity or rest, as this indicates inadequate blood flow to your heart. Other warning signs could include lightheadedness or feeling as though you could pass out, sweating, nausea, and vomiting are other symptoms to be aware of.
Difficulty Breathing
Breathing difficulties don't necessarily indicate a heart attack, but if they occur unannounced and you experience other indicators of one, it is wise to consult your physician immediately.
As an example, you might notice yourself getting winded more easily when exercising or walking up stairs; having difficulty breathing when lying down; coughing up bloody-looking spit; experiencing an irregular and rapid heartbeat or blue or gray skin color; neck or jaw pain is an indicator that something may be off. Women are particularly prone to these symptoms even without experiencing chest discomfort.
Dr Richard Zelman MD emphasizes that plaque build-up in the arteries carrying oxygen-rich blood to the heart can hinder its proper function and cause irreparable damage, so we must be aware of potential signs of heart attacks as soon as they emerge and recognize them quickly if one should occur.
Shortness of Breath
People often assume they will recognize when they're having a heart attack, but that may not always be the case. While chest pain and discomfort are the most commonly observed signs, they don't always occur in every instance.
Shortness of breath, also known as dyspnea, is another telltale sign of cardiac issues, as suggested by Dr Richard Zelman. This condition often feels like you're exerting yourself more than usual or that you cannot catch your breath; it may come and go and may also be accompanied by other symptoms like pressure in the chest, breaking out in cold sweats, or nausea.
If you experience any of these symptoms and suspect you're having a heart attack, call 911 immediately and head to the hospital directly as soon as treatment can start working to restore blood flow and reduce the risk of further heart damage.
Feeling Fatigued
Heart attacks typically include chest discomfort that lasts more than several minutes and comes and goes, often leaving fatigued and lightheaded feelings behind. Furthermore, symptoms may affect other body parts, including the jaw, neck, throat area, tummy, arms, back, and legs. These signs could indicate that blood is not receiving enough oxygen from being appropriately oxygenated in your system.
Sensations of sickness or an upset stomach are often indicators of heart attacks in women, according to Dr Richard Zelman. According to this source, gastric symptoms occur when your organs don't receive enough blood.
If someone is experiencing any of the above symptoms, they must call 911 immediately. Emergency medical workers can check heart rhythm using an EKG machine and give the individual some water and chewed-up aspirin to reduce blood clots and improve circulation to the heart.
Pain or Pressure in the Neck or Jaw
Pain or pressure in your neck, jaw, or stomach may be an early warning sign of a heart attack. The discomfort could range from pressure, squeezing, or fullness and may last more than several minutes before going away or returning - it is crucial to recognize these early warning signs immediately and seek medical assistance immediately, even if you don't think it is directly related.
People often mistake chest pain as the sole indicator of heart attack symptoms, yet many heart attacks do not manifest with pain. They can be challenging to recognize, as highlighted by the insights of Dr Richard Zelman. They can also develop slowly over several hours. Furthermore, symptoms vary between males and females and depend on factors like your age and lifestyle - it could happen quickly!
Other signs of heart attacks beyond chest pain or pressure include breaking out in a cold sweat, feeling sick to your stomach, and lightheadedness - symptoms that may manifest with or without physical chest discomfort; they are particularly alarming for women.
Feeling Sick to Your Stomach
An intense heart attack may cause severe chest pain that feels like you're choking, leading many people to misinterpret it as something other than what it is, such as a stomach ulcer or flu. If this sensation arises during a heart attack, seek medical assistance immediately if this sensation occurs.
Women tend to experience this symptom more frequently, though men can also be affected. Many describe the feeling as an elephant sitting on your chest; sometimes, there can be shortness of breath, lightheadedness, and nausea.
Some heart attacks can strike quickly and dramatically; others may progressively worsen over several hours. Any new or changing symptoms must be recognized immediately so they can get treatment in time to protect the health of your heart and prevent further damage to it.
0 notes
Text
acidity homeopathy treatment | homeopathic treatment
Acidity, Homeopathy treatment is very effective.
Annoying burning pain in the chest after eating food is one of the most distressing things for most people. Due to the disgusting burning pain, they avoid most of their favourite food items or some are even afraid to take necessary food. Homeopathy is a piece of good news for such suffering people. For acidity, homeopathy offers a natural and complete cure. Homeopathy empowers the body’s immunity and repairing power. This enables the body to cure without any remnants.
Numerous clinical studies validate homeopathy as an effective intervention for various types of acid reflux and related digestive complaints. And regulatory bodies across the globe have found preparations to be safe for adults and children.
What is acidity?
Acidity refers to a condition in which stomach acid levels are higher than normal or the stomach’s protective lining has been damaged by too much acid.
Acidity is also called acid reflux, gastroesophageal reflux disease (GERD), or heartburn. It can cause uncomfortable burning sensations moving up from the stomach to the oesophagus or throat.
It occurs when the valve between the stomach and oesophagus doesn’t fully close, allowing gastric acid to reverse course into the more delicate oesophagal tissues. This valve is called the lower oesophagal sphincter (LES).
Everyone experiences minor reflux on occasion after eating too much or eating trigger foods. But for some, it becomes a chronic condition requiring management due to frequent symptoms interfering with the quality of life.
If left untreated, the acid can damage oesophagal tissues and cause painful complications like ulcers, strictures, Barrett’s oesophagus, and increased cancer risk.
What are the risk factors
👉Eating fatty, fried, or spicy foods can relax the oesophagal sphincter and trigger reflux. Alcohol, chocolate, citrus fruits, tomato products, garlic, onions, peppermint, and coffee can also make GERD symptoms worse.
👉Obesity – Excess weight increases abdominal pressure which can push stomach contents upwards into the esophagus.
👉Obesity – Excess weight increases abdominal pressure which can push stomach contents upwards into the esophagus.
👉Hiatal Hernia
👉Smoking/Vaping
👉 Certain medications
👉Stress and Anxiety – When the “fight or flight” nervous system is activated from mental/emotional triggers, digestion is impaired. Stress affects stomach acid production and causes indigestion. Relaxation helps.
Eating Too Late – Going to bed too soon after eating leaves excess food in the stomach promoting increased overnight acidity while lying flat makes reflux more likely due to position.
For acidity, Homeopathy treatment is the best.
Homeopathy offers a safe, gentle approach to treating acidity by stimulating the body’s healing response rather than just suppressing symptoms. Some key points about hom
eopathic treatment for issues like acid reflux and heartburn include:
Remedies are customized to each person’s unique pattern of signs and symptoms – there is no one-size-fits-all treatment. A trained homoeopath selects the most fitting preparation.
Common homoeopathic remedies used for acidity include Arsenicum album, Carbo vegetabilis, Lycopodium, Nux vomica, Phosphorus, Pulsatilla, Robinia and Sulphur. Each has an affinity for improving specific digestive complaints.
Extremely diluted natural mineral, botanical, or biological substances are prepared in homeopathy labs under stringent protocols. Though highly diluted, the remedies retain a stamp of the original substance that stimulates healing responses when correctly matched constitutionally.
Tiny lactose pellets are placed under the tongue to dissolve, absorbing into the mucous membranes. Dosing protocols are adapted as the person improves to find the minimum frequency needed to get maximum benefit without suppressing symptoms.
In addition to managing acute flare-ups, homeopathic treatment aims to address underlying contributors like food sensitivities, hormonal imbalances, and stress that make someone prone to excess acidity. It works deeply to strengthen digestion holistically.
Numerous studies validate homeopathy’s efficacy and safety for improving chronic acid reflux and related esophageal inflammation. Patients often report long-term improvement of troublesome symptoms as well as reduced dependency on conventional medications.
In summary, homeopathy works gently to stimulate the body’s self-regulating capacity to heal acid imbalance at its roots – providing more than palliative relief of GERD and heartburn symptoms. A constitutional approach delivers a better quality of life.
0 notes
Text
New Post has been published on Dog N Treats
New Post has been published on https://dogntreats.com/what-is-bloat-in-dogs/
Gastric Dilatation-Volvulus (Bloat) in Dogs: Everything You Need to Know
When it comes to safeguarding your canine companion’s health, knowledge is your greatest ally. Gastric Dilatation-Volvulus (GDV), commonly known as “Bloat,” is a potentially life-threatening condition that predominantly affects large and deep-chested dog breeds. In this comprehensive guide, we’ll explore the intricate details of GDV, from its causes and symptoms to preventive measures and treatment options.
What is Gastric Dilatation-Volvulus (Bloat)?
GDV, short for Gastric Dilatation-Volvulus, is a medical emergency in which a dog’s stomach fills with gas, fluid, or food, leading to rapid distension. This distension can escalate to the point where the stomach twists on itself, cutting off blood flow to the stomach and spleen, and depriving these vital organs of oxygen. Without immediate intervention, GDV, or Bloat, can be fatal.
Recognizing the Symptoms: The Silent Threat
Gastric Dilatation-Volvulus (GDV) is notorious for its sudden onset, which makes recognizing the symptoms of paramount importance. Understanding the first signs of bloat in a dog can mean the difference between life and death for your canine companion.
1. Restlessness and Pacing
GDV often begins with restlessness. Your dog may seem agitated, constantly trying to find a comfortable position, or pacing without any apparent reason. They may appear anxious and unable to settle down. This restlessness is a clear indication of discomfort. Imagine yourself in a state of persistent discomfort, and you’ll grasp the urgency of this symptom.
2. Unsuccessful Vomiting
Another hallmark of GDV is the repeated, but fruitless, attempts to vomit. Your dog may retch, gag, or attempt to vomit, but little to nothing comes up. This is because the twisted stomach obstructs the normal path for food and fluids to exit the body. It’s a painful and frustrating experience for your dog.
3. Visible Abdominal Distension
One of the most evident signs of GDV is a visibly bloated abdomen. The stomach becomes greatly distended due to the accumulation of gas, fluid, and partially digested food. This distension can be so severe that the abdomen may take on the appearance of a “potbelly.” This is not the result of overeating; it’s a medical emergency.
4. Excessive Drooling
GDV can lead to excessive salivation, and your dog may drool profusely. This is a natural response to the discomfort they are experiencing. The drool may be thick and stringy, and it can become a noticeable and distressing symptom.
5. Pale Gums and Increased Heart Rate
When GDV progresses, it can lead to poor circulation, resulting in pale or bluish gums. The gums may also feel dry or tacky to the touch. An increased heart rate is often observed as the body tries to compensate for the decreased blood flow. Checking your dog’s gums for color and capillary refill time (the time it takes for the gums to return to their normal color after pressing on them) is a valuable diagnostic tool.
6. Anxiety and Distress
Your dog may exhibit signs of anxiety and distress, often trying to communicate their discomfort through whining, whimpering, or other vocalizations. It’s crucial to pay attention to your dog’s behavioral changes and act upon them promptly.
Remember, bloat in dogs can progress rapidly, and each of these symptoms, when observed in combination, is a red flag that necessitates immediate veterinary attention. Your dog may be unable to convey their distress in words, but they rely on you to recognize and act on these critical signs of bloat. Swift intervention can save their life.
What causes bloat in dogs
Several factors are believed to contribute to the development of bloat in dogs. These include:
Breed Predisposition: Larger breeds with deep chests are more prone to GDV. Breeds such as Great Danes, German Shepherds, Saint Bernards, and Standard Poodles have a higher susceptibility. This is likely due to their anatomy, which allows for more room in the abdominal cavity for the stomach to distend and twist.
Diet and Feeding Habits: Feeding your dog one large meal a day or allowing them to engage in vigorous physical activity immediately after eating can increase the risk of GDV. For example, a large meal before bedtime or strenuous exercise directly after eating can be problematic.
Genetics: There is evidence to suggest a genetic predisposition to GDV in certain breeds. It’s crucial to research your dog’s breed and familial history to understand their risk better. In some cases, it may be advisable to consult a veterinarian about preventive measures.
Stress and Anxiety: Stressful situations, such as thunderstorms, fireworks, or significant changes in the household, can trigger GDV in susceptible dogs. The exact mechanisms of how stress contributes to GDV are not fully understood, but it’s essential to minimize stressful circumstances for your pet.
By understanding these specific causes and the complex nature of GDV, you can take proactive measures to reduce the risk and ensure the well-being of your beloved canine companion. It’s a multifaceted condition that necessitates vigilance and responsible pet ownership.
How to prevent bloat in dogs
Preventing bloat in dogs involves a combination of strategic choices and attentive care. Large and deep-chested dog breeds are at a higher risk, so it’s crucial to implement measures that reduce the likelihood of this condition. Here’s an in-depth exploration of how to safeguard your dog against bloat:
Feeding Habits: The way you feed your dog plays a significant role in preventing bloat in dogs. Instead of providing one large meal a day, consider dividing their daily food into multiple smaller meals. For example, if your dog’s daily intake is four cups of food, you can offer two cups in the morning and two cups in the evening. This approach helps prevent overeating, reduces the volume of food in the stomach at any given time, and minimizes the risk of distension.
Slow Eating: Some dogs are prone to fast eating, which can increase the risk of bloat. Consider using specialized slow-feeding bowls or puzzle feeders. These are designed with ridges and obstacles that make it more challenging for the dog to gulp down their food quickly. Slower eating allows the stomach to adjust to food intake more gradually, reducing the likelihood of excessive air ingestion.
Elevated Food Bowls: Raising your dog’s food and water bowls to an elevated level can be beneficial. This minimizes the need for your dog to bend down too far to eat or drink, reducing the risk of swallowing excess air during mealtime. It also promotes more comfortable digestion.
Stress Management: Minimizing stress in your dog’s environment and routine can contribute to bloat prevention. Recognize stress triggers such as thunderstorms, fireworks, or significant household changes, and take steps to alleviate your dog’s anxiety. This might involve creating a safe and quiet space for them or using anxiety-reducing products like calming pheromone diffusers.
Regular Exercise: Encourage your dog to engage in regular but moderate exercise. Exercise is essential for overall health, but strenuous activity immediately after meals can be problematic. A leisurely walk after eating is a safer approach. Remember that exercise can stimulate digestion, so allow some time for the food to settle before rigorous activity.
Consider Anti-Bloat Dog Bowls: Anti-bloat dog bowls are specifically designed to prevent dogs from gulping down their food. These bowls have raised partitions or ridges that make it harder for the dog to ingest air while eating. They can be an effective tool in reducing the risk of bloat in dogs.
Regular Veterinary Checkups: Schedule regular checkups with your veterinarian to monitor your dog’s health. Your vet can provide guidance on GDV prevention tailored to your dog’s specific needs and any breed-related risk factors.
Treatment and Prognosis for Bloat in Dogs
If you notice that your dog might be suffering from bloat, the most immediate course of action will involve stabilizing your dog, relieving the gastric distension, and performing surgery to untwist the stomach. The prognosis depends on how quickly the condition is addressed. Prompt intervention increases the chances of a positive outcome.
1. Immediate Veterinary Care
Immediate veterinary care is the crucial first step when dealing with bloat in dogs. Recognizing the signs and symptoms of bloat is critical, and upon suspicion, it’s essential to seek emergency veterinary attention without delay. Here’s a more detailed look at what immediate veterinary care entails:
Stabilization
Oxygen: When a dog is suffering from bloat, they may be in distress and have difficulty breathing. Oxygen therapy is administered to ensure that the dog receives sufficient oxygen to support oxygen-deprived tissues.
Intravenous (IV) Fluids: Dogs with bloat often experience a drop in blood pressure due to the distended stomach. Intravenous fluids are administered to maintain blood pressure and provide necessary hydration. These fluids also help to restore electrolyte balance and circulation.
Pain Management: Bloat in dogs is painful, and pain management is a critical aspect of immediate care. Pain medications, such as opioids, are administered to alleviate the dog’s suffering.
Decompression
Relieving the Gastric Distension: Rapid gastric distension is a hallmark of GDV, and it causes immense discomfort. One of the first actions taken is to pass a tube through the dog’s mouth or nose into the stomach. This tube serves the dual purpose of relieving the accumulated gas and fluids and allowing the stomach to return to its normal position.
Assessing the Situation: As the stomach is decompressed, the veterinarian will assess the condition and stability of the dog. This assessment informs the subsequent steps in the treatment process.
2. Surgery
Emergency surgery is a critical part of treating bloat in dogs. Once the dog is stabilized and the stomach has been decompressed, the surgical intervention involves several important aspects:
Untwisting the Stomach (Gastropexy)
Stomach Untwisting: The primary objective of surgery is to untwist the stomach and return it to its normal position. This is a delicate procedure, and it requires the skill and experience of a veterinary surgeon.
Gastropexy: In many GDV cases, the veterinarian will perform a procedure called gastropexy. This involves attaching the stomach to the body wall to prevent it from twisting again in the future. Gastropexy is a preventive measure and is especially crucial in breeds prone to GDV.
Assessment of Tissue Damage: During surgery, the veterinarian will assess the stomach and other abdominal organs for signs of tissue damage. Portions of the stomach or spleen may need to be removed if they are irreparably damaged.
Perfusion Assessment: The surgeon will also assess blood flow to the stomach and other organs to ensure proper circulation has been restored. This is critical to the dog’s overall well-being.
Postoperative Care
Intensive Care: After surgery, dogs require intensive postoperative care. This includes ongoing monitoring of vital signs, ensuring pain management, and maintaining intravenous fluids as needed.
Controlled Diet: A controlled diet is crucial during the recovery phase. Dogs are typically introduced to small, easily digestible meals, and their food intake is gradually increased as they recover.
Follow-up Appointments: Follow-up appointments with the veterinarian are essential to monitor the dog’s progress and address any complications or concerns that may arise.
Prognosis
The prognosis for a dog with bloat largely depends on several critical factors:
Timeliness of Treatment: The speed at which the bloat in your dog is recognized and treated is perhaps the most significant factor in determining the prognosis. Swift intervention increases the chances of a positive outcome. Delayed treatment significantly reduces the chances of survival.
Extent of Tissue Damage: The extent of tissue damage caused by the twisted stomach is another crucial factor. Severe damage may affect the prognosis, as it can lead to complications during or after surgery.
Age and Overall Health: The age and overall health of the dog also play a role. Younger, healthier dogs tend to have a better prognosis than older dogs or those with pre-existing health issues.
Recovery and Postoperative Care: After surgery, dogs will require intensive postoperative care. This includes ongoing monitoring, pain management, and a carefully controlled diet. It’s vital to follow the veterinarian’s postoperative care instructions to ensure a successful recovery.
Complications: Bloat in dogs can lead to complications such as sepsis, heart arrhythmias, or blood clotting disorders. These complications can impact the prognosis.
Conclusion
In the world of pet ownership, knowledge is indeed power. Being aware of conditions like Gastric Dilatation-Volvulus (Bloat) and understanding its symptoms and risk factors can make all the difference in ensuring your dog’s well-being. Remember, early recognition and swift action are your best allies in the fight against bloat!
0 notes