#and misfolding always happens in general
Text
Learned a cool thing about proteins last week and it concerned cannibalism and I was like oh would Hannibal get mad cow disease too
#it's long to explain but it comes from a misfolded protein that has this fucking awsome power of infecting without having infectious agents#it's wrong but it's stable and it makes every other protein wrong#and it can come from a genetic mutation but it's very rare#the main transmission comes from ingesting brains of an infected subject#it can be a cow or a sheep (cows got it from sheeps) but humans got it from cannibalism and use of hormones and cornea transplants#first then when the mad cow disease spread scientists started to figure out how it worked#it's really interesting actually what a misfolding can do#and misfolding always happens in general#i mean that misfolding of that particular protein is rare but the interesting part is how it infects without being like. a virus
1 note
·
View note
Text
5 Symptoms that are Subtle Indications of Neurodegenerative Diseases Symptoms
The nerves act as the messenger of the electrical impulses in your body. And the process of transmitting these signals generates the response to the stimuli. When a person suffers from degenerative nerve diseases, it can affect the chief activities of the body, like movement, balance, breathing, talking, and heart functions.
It is necessary to learn about the neurodegenerative diseases symptoms to detect the same at an early phase and consult neuro specialists at the early stage.
Symptom #1: memory loss
Are you forgetting small things? It can happen when you are aging. But there is a difference between forgetfulness owing to aging and that due to neurodegeneration. Forgetting your address, being unable to recognize someone close, and forgetting the address where you have resided for almost all your life are the symptoms of neural health problems.
Symptom #2: Anxiety
Anxiety is always one of the most common symptoms of any neurodegenerative disease. You will be always in a tense state of mind. You may not even know what is causing the tension. Every small thing will make you worry, and you will end up perspiring abnormally.
Anxiety attacks are the early symbols of neural disorders. Most of the time's you not find a reason to have anxiety in mind.
Symptom #3: Mobility issues
Are you facing some problems in controlling the parts of your body like the arms and legs? It can be some mild symptoms at the beginning. But it can increase with time causing
Trouble in walking
Trouble to write
Speech disorders
The doctors always consider the roles of protein misfolding in such cases that can relate to neurodegenerative diseases.
Symptom #4: Unnecessary agitation
Do you feel irritated all the time? If it is only during some specific times, especially the menstrual cycles, it is normal. But it is not normal to have the feeling of agitation all the time. It can be a hint to check your neurological status that may show up some trouble.
Quick changes of mood and frequent mood swings without any other related health issues will always imply that you are suffering from some neural problems.
Symptom #5: Memory and language
The initial symptoms of issues related to memory are often hard to detect as people tend to forget things all the time. But when the trouble affects your language memory. It is a serious concern.
The role of protein misfolding in disease is undeniable. And it is also difficult to diagnose the symptoms as most of neural degenerative diseases have related symptoms. Visit a professional if you think you are suffering from something that is above your knowledge.
And if you see someone suffering from the above symptoms, there is no harm in consulting medical professionals. You can slow down the deterioration of neural degeneration with timely medical assistance.
Gain Therapeutics offers different innovative approaches to detect and treat the symptoms.
0 notes
Note
how did you get into pathogens and diseases and such? :0 very cool special interest
I've always liked biology type stuff so I think it started there! My first hyperfixation that I can remember was marine biology (specifically deep sea creatures + environments as well as bioluminescense) in kindergarten and then it kind of moved to 'strange and weird diseases and syndromes' because I was an edgy traumatized preteen who was like auuauusu dark evil scary auuauaua but THEN I finally started to really look into the mechanisms underlying these diseases and why they happen and thats when I began to realize I really do love the microbial as well as molecular world !!!! And so the past few years my interests and goals have been solidifying themselves as I learn more and more about the topics I love (prion disease + protein misfolding and the pathogenesis of neurodegenerative disorders in general, naegleria fowleri + other microbes and rare/neglected diseases and their mechanisms of infection as well as specific virulence factors, manifestation of disease in tissues and cells, protein synthesis)!
So basically as a kid my mom got me this big ocean book and now I want to be a clinical pathologist (maybe also do work in cytopath....or specialise in identifying rare disease and microbes....CDC's NCEZID hit me up 😏) and.I start my pre-med journey this fall n_n !!!
#that was rambly LOL but basically I love the interactions happening at a microscopic level between#different molecules and cells and organ systems ans yadda yadda yadda#with specific interest points on proteins 💖 specifically prp#as well as microbes ! like naegleria fowleri 💕
15 notes
·
View notes
Text
Prions from Brain Detectable in Skin Earlier Than Brain Damage
MedicalResearch.com Interview with:

Dr. Wen Quan Zou
Wenquan Zou, MD, PhD
Associate Professor
Departments of Pathology and Neurology
Director of CJD Skin Project
Associate Director
National Prion Disease Pathology Surveillance Center
Institute of Pathology
Case Western Reserve University School of Medicine
Cleveland, Ohio 44106
MedicalResearch.com: What is the background for this study?
Would you briefly explain the significance of prion-induced diseases and why they have been difficult to diagnosis?
Response: Our previous study has demonstrated that infectious prions are detectable in the skin samples of patients with sporadic Creutzfeldt-Jakob disease (sCJD), the most common form of human prion disease, at the terminal stage by the highly sensitive real-time quaking-induced conversion (RT-QuIC) assay and animal-based bioassay.
The prion-induced diseases are significant because they are infectious diseases that can be transmitted inter-species and intra-species. For instance, mad cow disease, a prion disease in cattle, has been documented to transmit to humans. Currently, there are no cures for these fatal diseases.
The definite diagnosis of prion diseases is difficult because it mainly depends on the availability of brain tissues obtained either by biopsy or autopsy for detection of prions. Brain biopsy is highly invasive and it is difficult to be accepted by patients and their families. Even for brain autopsy, it is not always feasible because of religious and cultural limitations in some regions or countries.
MedicalResearch.com: What are the main findings?
Response: The main findings in our current study are that the prions generated in the brain are detectable in skin tissue far earlier than the prion-caused brain damage, and that normal animals may obtain the infection via co-habitation with infected animals.
These findings are important because it may open a new avenue for prevention of the disease or for efficient treatment. It is known that once the brain cells are injured, the damage is often irreversible, which could be one of the reasons why so far no compounds have been proven to be effective. So, a strategy to prevent prion-induced brain damage may be developed if the disease can be diagnosed in the skin samples before brain damage occurs.
In addition, there are no epidemiological data supporting the possibility that prion disease is transmissible by co-habitation in humans. However, there is evidence that it could happen in animal prion diseases such as scrapie in sheep and goats as well as chronic wasting disease in elk and deer. Our finding of prion transmission via co-inhabitation suggests that skin may play a role in transmission of animal prion diseases.
MedicalResearch.com: What should readers take away from your report?
Response: The take away from our study is that skin prions could be a biomarker for early preclinical diagnosis of prion diseases.
MedicalResearch.com: What recommendations do you have for future research as a result of this work?
Response: We are going to use the highly sensitive RT-QuIC and sPMCA assays to develop premortem diagnostic tools for CJD patients by examining their skin biopsy samples. To verify that our skin-based approaches are able to be used for early preclinical detection of prions in CJD patients, it is necessary to conduct a longitudinal study in asymptomatic prion protein mutation carriers to find out how early we can detect skin prions before the mutation-carriers show clinical signs and symptoms. It would be also important to further determine what role the skin may play in the interspecies transmission of animal prion diseases such as scrapie and mad cow disease.
MedicalResearch.com: Is there anything else you would like to add?
Response: Unlike patients with Parkinson’s disease who may have prodromal non-motor symptoms and signs such autonomic disturbances, olfactory dysfunctions, depression and sleep disorders, no prodroma have been identified in patients with sporadic CJD. Once patients with sCJD show clinical symptoms, they are not early stage and already experienced significant brain damage. It is most likely that the skin-based longitudinal follow-up study of prion protein mutation-carriers may offer us a chance to identify those prodromal signs and symptoms in these individuals, which could also be applicable to sporadic CJD patients.
Like prion diseases, misfolded alpha-synuclein and tau protein associated with Parkinson’s disease and Alzheimer’s disease, respectively, also have been reported in skin tissues of patients with these conditions. Thus, it is most likely that skin could serve as a mirror not only for early diagnosis, but also for monitoring the accumulation of the misfolded proteins in the brain of these neurodegenerative diseases.
Citation:
Zerui Wang, Matteo Manca, Aaron Foutz, Manuel V. Camacho, Gregory J. Raymond, Brent Race, Christina D. Orru, Jue Yuan, Pingping Shen, Baiya Li, Yue Lang, Johnny Dang, Alise Adornato, Katie Williams, Nicholas R. Maurer, Pierluigi Gambetti, Bin Xu, Witold Surewicz, Robert B. Petersen, Xiaoping Dong, Brian S. Appleby, Byron Caughey, Li Cui, Qingzhong Kong, Wen-Quan Zou. Early preclinical detection of prions in the skin of prion-infected animals. Nature Communications, 2019; 10 (1) DOI: 10.1038/s41467-018-08130-9
More on this topic
The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.
Read the full article
1 note
·
View note
Text
Which Contagious Conditions Tend to be the Deadliest?
No person appreciates exactly what the Dying toll while in the Ebola epidemic will be. As of Tuesday, just about two,five hundred people have died and practically 5,000 have caught the virus, the earth Wellness Organization says.
So How can this epidemic Assess Along with the toll taken by other contagious conditions?
Comparing fatality costs could aid set the current Ebola outbreak in standpoint. Issues is, obtaining an precise value For lots of illnesses can be really hard, specifically in areas where by the well being care infrastructure is weak.
Just take the specific situation in West Africa at this time. "We can only count those who come to the medical doctor, not people who stayed house and received effectively, or those who stayed residence and died," suggests Carol Sulis, an epidemiologist at Boston College College of Drugs along with the Boston Health-related Centre.
An additional difficulty is the fact "deadliest" can indicate two points. It may check with the fatality level — the quantity of deaths for every range of conditions — or it might mean the number of deaths in overall a result of a illness.
What's more, ailments will take a unique toll in different elements of the globe. In very low- and middle-earnings nations around the world, only confined health-related care could be accessible, if that. This can elevate the fatality charge For numerous infectious disorders, such as tuberculosis, malaria and infectious diarrhea.
"Comparable to Ebola, individuals's possibilities of survival increase for A large number of [contagious] ailments, some radically, if folks obtain clinical therapy," says epidemiologist Derek Cummings, for the Johns Hopkins Bloomberg University of General public Health.
Even if lists have their limitations, they can shed light. We spoke to Cummings and Sulis and consulted info from the World Overall health Corporation and the U.S. Centers for Illness Management and Avoidance to come up with two lists: the deadliest contagious illnesses by Demise toll and by Demise amount if untreated.
Info are for all fatalities in 2012, aside from infectious diarrhea and pneumonia. For the people, death tolls characterize a annually estimate and stand for childhood victims only.

Associated NPR Tales Read [Como Acabar com Herpes]
Middle East respiratory syndrome
June five, 2014
Experimental Cocktail May Speed Up Cure Of Drug-Resistant TB
July 21, 2014
Tuberculosis Roars Back With A Deadly Edge
March 25, 2014
Experimental Malaria Vaccine Blocks The Bad Guy's Exit
Might 22, 2014
Deadliest Contagious Health conditions By Loss of life Toll
Comparison position: As of Sept. 7, the quantity of reporteddeaths in The existing Ebola epidemic is two,218.
HIV/AIDS: 1.6 million deaths
Though HIV can take a huge toll annually, the populace of men and women dwelling With all the disease is about 35 million.
Given that antiretroviral therapy — Artwork — grew to become readily available from the mid-1990s, life expectancy for someone infected with HIV has considerably elevated. Today, a individual who is immediately diagnosed with HIV and addressed can sit up for an in depth-to-normal lifestyle span.
But as with other illnesses, Sulas suggests, "we really have to possess the infrastructure to find the conditions and manage to afford to pay for the medication and provide it to People affected."
Tuberculosis: 1.3 million deaths
Regardless of the Loss of life toll for this airborne sickness, There is certainly encouraging information: 7.3 million persons designed TB and survived in 2012.
Restoration demands a program of quite a few medications above a 6- to nine-month period. Individuals who Really don't Keep to the drug schedule can produce drug-resistant TB. Drug-resistant kinds of TB are also airborne. For anyone individuals, remedy can lengthen to two yrs.
Pneumonia: 1.1 million small children beneath the age of five
It can be the world's top killer of kids, "in excess of AIDS, malaria and tuberculosis combined," WHO says. The threats may also be superior for the aged and those with other fundamental problems. In rich countries, just like the U.S., vaccines can stop the sickness, but that isn't the situation in Substantially of the planet.
Infectious Diarrhea: 760,000 children under the age of 5
"Which is an unlimited squander," Sulis says. Virtually all instances (about 1.7 billion globally yearly) may be prevented and dealt with with superior hygiene and sanitation, coupled with access to cleanse foodstuff and h2o. "There are various pathogens" that may cause these infections, she suggests, "but the whole course of disorders classified as infectious diarrhea is fatal." Read [Como Acabar com Herpes]
Malaria: 627,000 deaths
The globe data about 200 million malaria instances annually. In line with WHO, "most deaths take place among young children living in Africa in which a kid dies each and every minute from malaria."
There is a developing stress for both of those malaria and TB, Sulis states, since "the organisms that trigger These diseases are getting to be increasingly drug resistant all over the globe."
Deadliest Contagious Diseases By Fatality Price (If Not Treated)
In this article, as inside the checklist above, fatality prices might be decreased drastically depending upon the existence of sanitary conditions and The provision of medical care and vaccines.
We current the health conditions that look to acquire the best fatality prices Otherwise dealt with. If the speed is a range, we rated the condition by the highest attainable fatality charge.
Comparison Position: Outbreaks of Ebola may have fatality prices up to 90 percent, WHO suggests. But in The present outbreak, it's about 50 to 60 percent.
Rabies is sort of 100 percent deadly if not handled. You will discover around 55,000 deaths each year, generally in Asia and Africa.
Doses with the rabies vaccine after a Chunk from an infected animal will primarily abort the disorder. But anyone need to acquire cure quickly. Initial symptomsinclude irritation where by the Chunk happened, anxiousness and agitation. The moment medical signs like delirium and hallucinations arise, the patient almost always succumbs.
Creutzfeldt-Jakob ailment is seemingly one hundred pc fatal.
This neurodegenerative disease rapidly progresses. It's brought on by prions (nonviral, nonbacterial infectious agents that encompass a misfolded protein) that hurt balanced brain tissue. Prions create holes from the Mind that make it appear like a sponge under the microscope.
CJD is assessed to be a contagious sickness as it is often transmitted by means of connection with contaminated tissue during professional medical methods. But it is not distribute with the air or by everyday Speak to.
No remedy exists for CJD. Its incidence is rather low, influencing about 1 in one million people each year, with about 300 cases each year inside the U.S. CJD is usually hard to diagnose since indicators often resemble Individuals of dementia as well as other diseases, with memory lapses, behavioral modifications and sleep disturbances. Read [Como Acabar com Herpes]
Marburg hemorraghic fever: 24 to 88 %
Marburg is because of a virus just like Ebola, transmitted mostly by connection with bodily fluids from somebody who's been infected. Fever, chills, headache and muscle ache are the primary signs and symptoms, showing up in five to 10 times soon after infection. The following phase might cause vomiting, diarrhea, delirium and organ dysfunction or failure. There's no recognised remedy beyond supportive clinic therapy. Due to the fact 1967, when Marburg was to start with acknowledged by scientists, there are actually 571 documented scenarios.
H5N1 and H7N9 flu viruses: sixty % for the previous, 25 % to the latter
These two viruses "continue being two on the influenza viruses with pandemic prospective," WHO says. They are in extensive circulation amongst some groups of poultry; people usually do not surface to obtain any immunity. The whole quantity of human circumstances for equally viruses to date is about 1,000. Some antiviral remedies and vaccines can be obtained.
Middle East respiratory syndrome: forty one per cent
Very first detected in 2012, this disease may lead to coughing, shortness of breath, fever and pneumonia. When patients die, the lead to can be an absence of oxygen passing with the lungs in to the blood. Researchers theorize that MERS could have very first appeared in bats, which handed it to Arabian camels, which can then have contaminated human beings. Many the 800 cases are about the Arabian Peninsula.
Read [Como Acabar com Herpes]
2 notes
·
View notes
Note
Heyho lanani, as I was re-reading Ghosts From The Past (and willingly let it break my heart again, by the way) I noticed how Bruce explained to Jason how the double dose of fear toxin has apparently cured his insanity. And (if I'm not totally mistaken) that's something that's never really explained in IWGA. Is this your general solution for IWGA as well or is there another catch? Thanks already, Melody
Thanks for your ask, Melody! (And you are welcome for the repeated heartbreak ^^)
Ok, so this is gonna be such a useless answer, but… IWGA is almost 300k long and I honestly don’t remember writing half of it. I’m pretty sure the topic of Bruce’s mental state came up somewhere… but I’ll be damned if I know when and how.
In general, though, the game does follow the continuity of the Arkham games, in which the first directly injected dose of fear gas brought Bruce’s worst fear to life (him becoming the Joker) and the second dose brought Joker’s worst fear to life (being forgotten, especially by Bruce). As such, Bruce has finally been able to exorcise the last bits of Joker from his mind (he will always remember what Joker did, of course, but the important thing is that he no longer has the Joker infection thing going on.
How that happened, exactly, is anyone’s guess since a lot of stuff in the Arkham games is pseudoscience. In BAK, the Joker infection was explained as a highly mutated form of Creutzfeld-Jakob disease, which is caused by a misfolded protein called prion. Tim was researching an antibody. I’m guessing what happened is that the fear gas reacted with the infected cells, mutating the prion protein until it was practically ineffective.
I’m gonna have to re-read IWGA anyway, for general proof-reading purposes, because it is probably full of typos and formatting issues. I’ll have to keep an eye out for that plot hole then.
4 notes
·
View notes
Photo
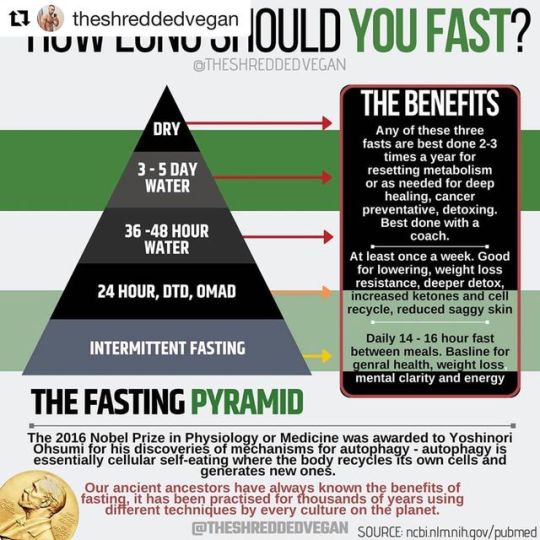
#Repost @theshreddedvegan with @get_repost ・・・ Being fully fed 24:7, eating at least 3-5 times has only recently been introduced into human lifestyle. The romans and Greeks saw eating more then one large meal a day as gluttony! - ℹThe research and evidence produced over the last few years backs the amazing health benefits of intermittent and prolonged fasting. We would of naturally had fasting periods before modern times as food would have not always been available. - ℹAutophagy now scientifically proves that the human body has a self healing mechanism. Autophagy in greek means "self-eating" and that is literally what is happening on a cellular level when you fast for long enough and enter autophagy. - 🛡 The five stages of intermittent and prolonged fasting - - 🧠 By 12 hours you have entered the metabolic state called ketosis. This is when your body starts to break down and burn fat. Some of this fat is used by the liver to produce ketone bodies. Ketones are said to produce less inflammatory products as they are being metabolized and kick star thr production of the brain growth factor. - 🔥By 18 hours, you've switched to fat burning mode and are generating significant ketones. As their level in your blood stream rises, ketones can act as signaling molecules, similar to hormones to tell your body to ramp up stress busting pathways that reduce inflammation and repair damaged DNA. - ♻️ Within 24 hours, your cells are increasingly recycling old components, breaking down misfolded proteins linked to alzheimer's and other diseases. This process is called autophagy. - 💪🏾By 48 hours without calories or with very few calories, carbs of protein, your growth hormone level is up to five times as high as when you started your fast. - 📉 By 54 hours your insulin has dropped to its lower level point since you started fasting and your body is becoming increasingly insulin sensitive. Lowering insulin levels has a range of health benefits, reduced inflammation which has been linked to the major culprit in cancer. - 🧬 By 72 hours, your body is breaking down old immune cells and generating new ones. Prolonged fasting reduces circulating IGF -1 levels and PKA activity in variou https://www.instagram.com/p/B0v0vbDADK_3f7xtNtT0FSm1gApKOAv_SLsVME0/?igshid=tdgdon6k645q
0 notes
Text
The Future of Detecting Brain Damage in Football
Sam Gandy had never seen anything like it. He was examining brain scans, color-coded to indicate problems. In healthy people, images appear almost entirely blue and green. But several areas on this particular scan were bright red.
Gandy, a neurologist at Mount Sinai Hospital in New York, was studying the brains of retired soldiers and football players, looking for signs of trouble like this. The scan that stood out was of a retired National Football League player who had suffered 22 concussions over the course of his 11-year career. Now approaching middle age, the player complained of memory lapses and a short fuse—symptoms associated with chronic traumatic encephalopathy, or CTE, a neurodegenerative disease linked to repetitive brain trauma.
Currently, CTE can only be definitively diagnosed after death. But the red areas Gandy saw on his computer screen closely corresponded to the damage that scientists see of the disease in autopsied brains. Gandy’s technique might be the first way to spot CTE in a living patient. If so, what he was looking at could change the future of contact sports—as well as treating the long-term damage they can cause.
A PET scan of the brain of an NFL player who sustained 22 concussions (Sam Gandy / Dara Dickstein / Lale Kostakoglu)
Since CTE was identified in the brain of former Pittsburgh Steelers player Mike Webster in 2005, the disease has plunged football into an ongoing brain-injury crisis. A recent study of the brains of 202 deceased former football players revealed that 110 of the 111 who had played in the NFL had the condition. Athletes whose gridiron careers ended at the high-school and college levels also also had the disease, though in lower percentages. (There are limitations to this research—more on that momentarily.)
Coming on the heels of multiple studies suggesting that repeated blows to the head can be bad for the brain—and of CTE being found in soccer players, soldiers, and others—this study only intensified concerns about football: Is the sport, which kicked off another season this month, safe enough for children? For high schools? For anyone?
The fact that CTE can only be diagnosed posthumously makes answers difficult. Researchers can’t say how common the disease really is, because studies suffer from unavoidable selection bias: The brains examined aren’t chosen at random from the general population, or even the overall population of contact-sport athletes and others exposed to repetitive head trauma. Rather, most are donated for study because donors and their families suspected something was wrong.
Researchers also don’t know exactly how CTE starts—though research on concussed mice has offered intriguing clues—or how it progresses over time. They don’t understand why some people who suffer repetitive head impacts develop the disease while others don’t. Nor can they target and test potential medications and therapies.
A reliable in-vivo way to diagnose the condition, says Robert Stern, the director of Boston University’s Chronic Traumatic Encephalopathy Center, is “the goal for all research now with CTE. We’ve learned a tremendous amount through the postmortem data and research. But that’s the starting place.”
Enter Gandy. A longtime Alzheimer’s researcher, he began to study contact sport–related brain disease in the 1990s, when he coauthored a study that found boxers who had fought in 12 or more professional bouts and had a particular genotype were more likely to have chronic neurological deficits.
Three years ago, a 73-year-old retired New York Jets player with memory problems named Dave Herman wanted to enroll in a Mount Sinai clinical trial for an Alzheimer’s drug, but the five doctors who examined Herman—Gandy among them—couldn’t agree on what was ailing him. Three thought he had Alzheimer’s. Two suspected CTE. So Gandy examined Herman’s brain twice using positron-emission tomography (PET) scans—once with a radioactive tracer that binds to beta-amyloid, a sticky protein that builds up in the brains of Alzheimer’s patients, and again with a new tracer that binds to tau, a different protein that misfolds, clumps, and forms toxic tangles in the brains of CTE patients.
A healthy brain (left) and the brain of an NFL player with a history of 22 concussions (right). The red and yellow areas in the NFL player’s brain are likely linked to CTE. (Sam Gandy / Dara Dickstein / Lale Kostakoglu)
The first scan came back negative. The second was positive. Herman likely had CTE. Only doctors couldn’t be entirely sure; the scans were lacking in detail, and scientists hadn’t agreed on a postmortem diagnostic standard for the disease, so Gandy couldn’t match with full confidence what he saw in Herman’s scan to the tau tangles seen in the autopsied brains of CTE patients. A year later, however, an expert panel commissioned by the National Institute of Neurological Disorders and Stroke, or NINDS, agreed on what distinguishes CTE from other diseases that also feature tau deposits: In CTE, the neuron-killing protein tangles build up around the wrinkled crevices along brain’s surface, particularly at the deepest points.
Armed with that definition and higher-resolution scans, Gandy was better able to tentatively diagnose the retired NFL player who had suffered 22 concussions, and who also showed neuropsychological testing deficits and diffuse brain damage through separate MRI scans. (The player discussed Gandy’s findings with The Atlantic, but requested anonymity because of the stigma associated with brain injury.) “With the better resolution in the [PET] scans, we could see the localization of the tau in exactly that spot, the bottom of the walls of the wrinkles,” Gandy says. “It looked very similar to what you would expect from a postmortem [CTE] brain.”
Since then, Gandy’s team has examined and scanned almost 30 combat veterans and former football players. Ten of those patients have clinical symptoms of CTE; of that group, eight have what Gandy describes as “clearly positive scans” for abnormal tau buildup, similar to that of the NFL retiree. The other two “may not have accumulated enough tau for us to see it yet,” Gandy says.
Before PET scans can be used to definitively diagnose CTE—or simply be used with a high degree of diagnostic confidence—more work needs to be done. A handful of cases are suggestive, but not conclusive; many more patients need to be scanned, evaluated by doctors, tracked over time, and eventually autopsied after death to validate the bright-red regions Gandy and his team are seeing on their computer screens. “That’s the gold standard,” Gandy says. “It will take a while to accumulate enough data to feel confident that a certain amount of signal represents a certain amount of tau.”
A number of tau tracers have been developed in recent years, and researchers are still figuring out which ones are the most useful for identifying various neurodegenerative diseases. Two years ago, researchers at the University of California, Los Angeles, published a brain-imaging study of 14 former football players using a tracer called FDDNP to identify what appeared to be CTE. But that same tracer also binds to amyloid, making it difficult to differentiate the disease from Alzheimer’s.
Gandy uses a compound called Flortaucipir, which binds much more readily to tau than to amyloid. But he cautions that it may not prove to be the best available imaging agent. “Most people who get the scans want a definitive result,” he says. “But we always tell them this is experimental, and we could find out something tomorrow that changes things. ”
Better answers may come from a recently announced seven-year, $16 million study funded by the National Institutes of Health and NINDS that’s aimed at diagnosing CTE—a project the NFL was also slated to fund before backing out amid controversy. Headed by Stern, the project is the largest and most thorough study of the disease ever conducted, and will put former football players through a series of tests including an MRI; two PET scans; blood, saliva, and spinal-fluid collection; genetic evaluations; neuropsychological testing; and clinical examinations and histories.
The goal, Stern says, is to create a reliable clinical tool kit—that is, multiple methods of diagnosing CTE, similar to how doctors detect prostate cancer by using relatively cheap and simple blood tests to determine which patients need more thorough examinations. “PET scans are really good, but are also are really expensive,” he says. “We need other ways of detecting CTE that are really good and less expensive, or not really good and less expensive.”
Stern believes that doctors will be able to diagnose the disease in the living within five years. If and when that happens, it will allow researchers to better study potential treatments. In particular, PET scans may enable them to see if a drug is working. Sometime in the next year, Gandy’s team hopes to have the tau-positive patients from its imaging study participate in a small clinical trial of a new medication that has shown the ability to repair and clear out misfolded tau in animals.
“Once someone has the symptoms of a neurodegenerative disease like CTE, it usually means that there is already damage to the brain, destruction of tissue and atrophy. We can’t get those cells back once they die,” Stern says. “If we see [the disease] early enough, we might be able to intervene in a way that slows down or even stop the disease progression.”
The ramifications for contact sports—especially football—could be equally profound. Youth football participation is declining, and a number of college and NFL players have walked away from the game, citing concern over brain injuries. It’s not hard to imagine someone like Gandy giving brain scans to entire high-school, college, and pro teams. The results might restore confidence in the overall safety of the sport—or further erode it.
“Every fall, I read how fewer and fewer kids are coming out to play high-school football,” Gandy says. “With scans, we could figure out what the risk really is. And we could have informed consent for people who want to get into this kind of activity—be able to say that you have a one in 100, or 1,000, or 1,000,000 chance of getting CTE. But we need to get to the point where every doctor can look at an image and say, ‘that is CTE, no question about it.’ Otherwise, it would be a mess.”
from Health News And Updates https://www.theatlantic.com/health/archive/2017/09/football-brain-injury-chronic-traumatic-encephalopathy/540459/?utm_source=feed
0 notes
Text
The Future of Detecting Brain Damage in Football
Sam Gandy had never seen anything like it. He was examining brain scans, color-coded to indicate problems. In healthy people, images appear almost entirely blue and green. But several areas on this particular scan were bright red.
Gandy, a neurologist at Mount Sinai Hospital in New York, was studying the brains of retired soldiers and football players, looking for signs of trouble like this. The scan that stood out was of a retired National Football League player who had suffered 22 concussions over the course of his 11-year career. Now approaching middle age, the player complained of memory lapses and a short fuse—symptoms associated with chronic traumatic encephalopathy, or CTE, a neurodegenerative disease linked to repetitive brain trauma.
Currently, CTE can only be definitively diagnosed after death. But the red areas Gandy saw on his computer screen closely corresponded to the damage that scientists see of the disease in autopsied brains. Gandy’s technique might be the first way to spot CTE in a living patient. If so, what he was looking at could change the future of contact sports—as well as treating the long-term damage they can cause.
A PET scan of the brain of an NFL player who sustained 22 concussions (Sam Gandy / Dara Dickstein / Lale Kostakoglu)
Since CTE was identified in the brain of former Pittsburgh Steelers player Mike Webster in 2005, the disease has plunged football into an ongoing brain-injury crisis. A recent study of the brains of 202 deceased former football players revealed that 110 of the 111 who had played in the NFL had the condition. Athletes whose gridiron careers ended at the high-school and college levels also also had the disease, though in lower percentages. (There are limitations to this research—more on that momentarily.)
Coming on the heels of multiple studies suggesting that repeated blows to the head can be bad for the brain—and of CTE being found in soccer players, soldiers, and others—this study only intensified concerns about football: Is the sport, which kicked off another season this month, safe enough for children? For high schools? For anyone?
The fact that CTE can only be diagnosed posthumously makes answers difficult. Researchers can’t say how common the disease really is, because studies suffer from unavoidable selection bias: The brains examined aren’t chosen at random from the general population, or even the overall population of contact-sport athletes and others exposed to repetitive head trauma. Rather, most are donated for study because donors and their families suspected something was wrong.
Researchers also don’t know exactly how CTE starts—though research on concussed mice has offered intriguing clues—or how it progresses over time. They don’t understand why some people who suffer repetitive head impacts develop the disease while others don’t. Nor can they target and test potential medications and therapies.
A reliable in-vivo way to diagnose the condition, says Robert Stern, the director of Boston University’s Chronic Traumatic Encephalopathy Center, is “the goal for all research now with CTE. We’ve learned a tremendous amount through the postmortem data and research. But that’s the starting place.”
Enter Gandy. A longtime Alzheimer’s researcher, he began to study contact sport–related brain disease in the 1990s, when he coauthored a study that found boxers who had fought in 12 or more professional bouts and had a particular genotype were more likely to have chronic neurological deficits.
Three years ago, a 73-year-old retired New York Jets player with memory problems named Dave Herman wanted to enroll in a Mount Sinai clinical trial for an Alzheimer’s drug, but the five doctors who examined Herman—Gandy among them—couldn’t agree on what was ailing him. Three thought he had Alzheimer’s. Two suspected CTE. So Gandy examined Herman’s brain twice using positron-emission tomography (PET) scans—once with a radioactive tracer that binds to beta-amyloid, a sticky protein that builds up in the brains of Alzheimer’s patients, and again with a new tracer that binds to tau, a different protein that misfolds, clumps, and forms toxic tangles in the brains of CTE patients.
A healthy brain (left) and the brain of an NFL player with a history of 22 concussions (right). The red and yellow areas in the NFL player’s brain are likely linked to CTE. (Sam Gandy / Dara Dickstein / Lale Kostakoglu)
The first scan came back negative. The second was positive. Herman likely had CTE. Only doctors couldn’t be entirely sure; the scans were lacking in detail, and scientists hadn’t agreed on a postmortem diagnostic standard for the disease, so Gandy couldn’t match with full confidence what he saw in Herman’s scan to the tau tangles seen in the autopsied brains of CTE patients. A year later, however, an expert panel commissioned by the National Institute of Neurological Disorders and Stroke, or NINDS, agreed on what distinguishes CTE from other diseases that also feature tau deposits: In CTE, the neuron-killing protein tangles build up around the wrinkled crevices along brain’s surface, particularly at the deepest points.
Armed with that definition and higher-resolution scans, Gandy was better able to tentatively diagnose the retired NFL player who had suffered 22 concussions, and who also showed neuropsychological testing deficits and diffuse brain damage through separate MRI scans. (The player discussed Gandy’s findings with The Atlantic, but requested anonymity because of the stigma associated with brain injury.) “With the better resolution in the [PET] scans, we could see the localization of the tau in exactly that spot, the bottom of the walls of the wrinkles,” Gandy says. “It looked very similar to what you would expect from a postmortem [CTE] brain.”
Since then, Gandy’s team has examined and scanned almost 30 combat veterans and former football players. Ten of those patients have clinical symptoms of CTE; of that group, eight have what Gandy describes as “clearly positive scans” for abnormal tau buildup, similar to that of the NFL retiree. The other two “may not have accumulated enough tau for us to see it yet,” Gandy says.
Before PET scans can be used to definitively diagnose CTE—or simply be used with a high degree of diagnostic confidence—more work needs to be done. A handful of cases are suggestive, but not conclusive; many more patients need to be scanned, evaluated by doctors, tracked over time, and eventually autopsied after death to validate the bright-red regions Gandy and his team are seeing on their computer screens. “That’s the gold standard,” Gandy says. “It will take a while to accumulate enough data to feel confident that a certain amount of signal represents a certain amount of tau.”
A number of tau tracers have been developed in recent years, and researchers are still figuring out which ones are the most useful for identifying various neurodegenerative diseases. Two years ago, researchers at the University of California, Los Angeles, published a brain-imaging study of 14 former football players using a tracer called FDDNP to identify what appeared to be CTE. But that same tracer also binds to amyloid, making it difficult to differentiate the disease from Alzheimer’s.
Gandy uses a compound called Flortaucipir, which binds much more readily to tau than to amyloid. But he cautions that it may not prove to be the best available imaging agent. “Most people who get the scans want a definitive result,” he says. “But we always tell them this is experimental, and we could find out something tomorrow that changes things. ”
Better answers may come from a recently announced seven-year, $16 million study funded by the National Institutes of Health and NINDS that’s aimed at diagnosing CTE—a project the NFL was also slated to fund before backing out amid controversy. Headed by Stern, the project is the largest and most thorough study of the disease ever conducted, and will put former football players through a series of tests including an MRI; two PET scans; blood, saliva, and spinal-fluid collection; genetic evaluations; neuropsychological testing; and clinical examinations and histories.
The goal, Stern says, is to create a reliable clinical tool kit—that is, multiple methods of diagnosing CTE, similar to how doctors detect prostate cancer by using relatively cheap and simple blood tests to determine which patients need more thorough examinations. “PET scans are really good, but are also are really expensive,” he says. “We need other ways of detecting CTE that are really good and less expensive, or not really good and less expensive.”
Stern believes that doctors will be able to diagnose the disease in the living within five years. If and when that happens, it will allow researchers to better study potential treatments. In particular, PET scans may enable them to see if a drug is working. Sometime in the next year, Gandy’s team hopes to have the tau-positive patients from its imaging study participate in a small clinical trial of a new medication that has shown the ability to repair and clear out misfolded tau in animals.
“Once someone has the symptoms of a neurodegenerative disease like CTE, it usually means that there is already damage to the brain, destruction of tissue and atrophy. We can’t get those cells back once they die,” Stern says. “If we see [the disease] early enough, we might be able to intervene in a way that slows down or even stop the disease progression.”
The ramifications for contact sports—especially football—could be equally profound. Youth football participation is declining, and a number of college and NFL players have walked away from the game, citing concern over brain injuries. It’s not hard to imagine someone like Gandy giving brain scans to entire high-school, college, and pro teams. The results might restore confidence in the overall safety of the sport—or further erode it.
“Every fall, I read how fewer and fewer kids are coming out to play high-school football,” Gandy says. “With scans, we could figure out what the risk really is. And we could have informed consent for people who want to get into this kind of activity—be able to say that you have a one in 100, or 1,000, or 1,000,000 chance of getting CTE. But we need to get to the point where every doctor can look at an image and say, ‘that is CTE, no question about it.’ Otherwise, it would be a mess.”
Article source here:The Atlantic
0 notes