#Positron Emission Tomography (PET) Systems
Text
#Positron Emission Tomography (PET) Systems Market Size#Positron Emission Tomography (PET) Systems Market Scope#Positron Emission Tomography (PET) Systems Market Trend#Positron Emission Tomography (PET) Systems Market Growth
0 notes
Text
Positron Emission Tomography (PET) Systems Market Growth Outlook, Regional Insights, Size Estimation to 2032 | Zecotek Photonics, Brain Biosciences, GE Healthcare LLC
Positron Emission Tomography (PET) Systems Market Growth Outlook, Regional Insights, Size Estimation to 2032 | Zecotek Photonics, Brain Biosciences, GE Healthcare LLC
An overview of the market segment, size, share, sectional analysis, and revenue forecast, as well as a complete analysis, are included in the Positron Emission Tomography (PET) Systems Market study. It engulfs micro and macroeconomic factors, industry trends, dynamics, and the strengths and weaknesses of the top competitors. It also includes details on sales channels, distributors, traders, and…

View On WordPress
#Future Trends of Positron Emission Tomography (PET) Systems industry#Positron Emission Tomography (PET) Systems#Positron Emission Tomography (PET) Systems manufacturing Vendors#Positron Emission Tomography (PET) Systems market#Positron Emission Tomography (PET) Systems market share#Positron Emission Tomography (PET) Systems market size#Positron Emission Tomography (PET) Systems market SWOT analysis#Scope of Positron Emission Tomography (PET) Systems industry
0 notes
Text
The innovation of a 3D-printed device from the University of Edinburgh could pave the way to the abolition of animal testing.
The plastic “body-on-chip” device contains human cells from five major organs — the brain, heart, lungs, kidneys, and liver — and simulates chemicals moving through the circulatory system by using positron emission tomography (PET) scanning.
“This device is the first to be designed specifically for measuring drug distribution … essentially, allowing us to see where a new drug goes in the body and how long it stays there, without having to use a human or animal to test it,” Liam Carr, inventor of the device, told The Guardian.
Future models could also show how organs in different stages of disease react to medicine — as well as how everyday items like foods, aerosols, and cleaners affect the human body — improving precision in biomedical experiments.
This device is an example of innovation in biomedical models that could replace animal testing. It could also be cheaper and faster than testing new drugs on live animals.
“This device shows really strong potential to reduce the large number of animals that are used worldwide for testing drugs and other compounds, particularly in the early stages, where only 2% of compounds progress through the discovery pipeline,” said Dr. Adriana Tavares of the University’s Centre for Cardiovascular Science according to WION News.
#ecology#enviromentalism#science#animal testing#experimentation#Remember reading about early versions of this tech years ago#Always fascinated me#But I ended up seeing a bunch of people rally against it for the dumbest reasons#I'm sorry I thought the point was to try and get research data and results that can eventually help people#Even the “best animal testing” is still fairly off due to the sheer biological differences#This can help save time and resources AND yield more useful results AND at the very least massively reduces animal testing#But some people decided the scientists who've spend years on this were “attacking scientific traditions” or were “ARAs GONE MAD”#First off “Grand scientific traditions”????#Second way to either admit you have no relevant knowledge or straight up ignore all the many valid criticisms of animal testing#What were they rallying against? Better testing with less waste? More usable data faster?#The potential reduction in animal testing? (They were mostly mad about that)
2 notes
·
View notes
Text
Staging of Leukemia
Unlike most solid tumors, leukemia is not classified by stage based on tumor size or spread. Different staging systems exist for each leukemia subtype. Overall, leukemia staging consists of multiple criteria including the type, count, and degree of maturation of specific blood cells, as well as the presence of enlarged lymph nodes.
Acute lymphoblastic leukemia (ALL) staging is based on the type and maturity of affected blood cells. The two main types of ALL are B-cell and T-cell ALL. Each type is staged according to the maturity of the blood cells. For example, B-cell ALL is classified as early pre-B, pre-B, common, or mature B-cell. T-cell ALL is classified as pre-T or mature T-cell.
There are two staging systems for acute myeloid leukemia (AML). The French-American-British (FAB) system consists of eight stages based on blood cell type and maturity. Stages M0 to M5 refer to cancers that develop from immature white blood cells like myeloblasts and promyelocytes. Stage M6 refers to acute erythroid leukemia, where malignancy originates from immature red blood cells, whereas stage M7 develops from megakaryoblasts, or platelet-forming cells. Alternatively, the World Health Organization (WHO) stages AML based on prognostic factors such as genetic abnormalities, comorbidities, and cellular differentiation.
Doctors can stage chronic lymphocytic leukemia (CLL) using the Rai or the Binet system. The Rai system is used in the United States. Comprising five stages, it assesses the severity of CLL based on three criteria: lymphocyte count, enlargement of lymph nodes, liver, or spleen, and development of blood disorders like anemia or thrombocytopenia. Rai stage 0, or low-risk CLL, is characterized by high lymphocyte count only, whereas stage 1 also includes enlarged lymph nodes. The liver or spleen may become enlarged in stage 2. Anemia and thrombocytopenia may develop in stages 3 and 4, or high-risk CLL.
In Europe, the Binet staging system focuses on enlargement of lymphoid tissue. Stage A describes CLL cases where some lymph nodes are swollen, stage B includes swollen lymphoid tissues in more than three areas, and stage C - like high-risk CLL in the Rai system - features anemia or thrombocytopenia.
The staging system for chronic myeloid leukemia (CML) is composed of phases that describe the number of immature white blood cells, also known as blasts, found in the bone marrow and bloodstream. Chronic CML is the earliest stage, where blasts account for less than 10 percent of total blood cells and patients present mild symptoms. In accelerated CML, blast growth progresses rapidly and results in more severe symptoms, such as weight loss. The most aggressive stage of CML is the blast phase, where blasts account for at least 20 percent of all blood cells and patients exhibit symptoms as severe as those with AML.
Doctors conduct various tests to accurately stage leukemia. They use diagnostic methods such as blood tests, bone marrow biopsy, and imaging modalities. A complete blood count, or CBC, determines the number of different cells in the bloodstream, and plays an important role in evaluating the severity of leukemia. Similarly, a bone marrow biopsy, taken from the patient’s hip bone, allows doctors to detect and identify the type of leukemia cells present in the bone marrow. Imaging modalities like x-rays and positron emission tomography (PET) scans can locate leukemia metastases in other parts of the body.
2 notes
·
View notes
Text
Medical Abbreviations on Pharmacy Prescriptions
Here are some common medical abbreviations you may see on pharmacy prescriptions:
qd - once a day
bid - twice a day
tid - three times a day
qid - four times a day
qh - every hour
prn - as needed
pc - after meals
ac - before meals
hs - at bedtime
po - by mouth
IV - intravenous
IM - intramuscular
subQ - subcutaneous
mL - milliliter
mg - milligram
g - gram
mcg - microgram
stat - immediately, right away
NPO - nothing by mouth
cap - capsule
tab - tablet
susp - suspension
sol - solution
amp - ampule
inj - injection
Rx - prescription
C - Celsius
F - Fahrenheit
BP - blood pressure
HR - heart rate
RR - respiratory rate
WBC - white blood cell
RBC - red blood cell
Hgb - hemoglobin
Hct - hematocrit
PT - prothrombin time
INR - international normalized ratio
BUN - blood urea nitrogen
Cr - creatinine
Ca - calcium
K - potassium
Na - sodium
Cl - chloride
Mg - magnesium
PO2 - partial pressure of oxygen
PCO2 - partial pressure of carbon dioxide
ABG - arterial blood gas
CBC - complete blood count
BMP - basic metabolic panel
CMP - comprehensive metabolic panel.
ECG - electrocardiogram
EEG - electroencephalogram
MRI - magnetic resonance imaging
CT - computed tomography
PET - positron emission tomography
CXR - chest x-ray
CTX - chemotherapy
NSAID - nonsteroidal anti-inflammatory drug
DMARD - disease-modifying antirheumatic drug
ACE - angiotensin-converting enzyme
ARB - angiotensin receptor blocker
SSRI - selective serotonin reuptake inhibitor
TCA - tricyclic antidepressant
ADHD - attention deficit hyperactivity disorder
COPD - chronic obstructive pulmonary disease
CAD - coronary artery disease
CHF - congestive heart failure
DVT - deep vein thrombosis
GI - gastrointestinal
UTI - urinary tract infection
OTC - over-the-counter
Rx - prescription
OD - right eye
OS - left eye
OU - both eyes.
TID - thrombosis in dementia
TDS - ter die sumendum (three times a day)
BOM - bilaterally otitis media (infection in both ears)
BT - body temperature
C&S - culture and sensitivity
D/C - discontinue or discharge
D/W - dextrose in water
ETOH - ethyl alcohol
FUO - fever of unknown origin
H&P - history and physical examination
I&D - incision and drainage
I&O - intake and output
KVO - keep vein open
N&V - nausea and vomiting
PERRLA - pupils equal, round, reactive to light and accommodation
PR - per rectum
QAM - every morning
QHS - every bedtime
QOD - every other day
S/P - status post (after)
TPN - total parenteral nutrition
UA - urinalysis
URI - upper respiratory infection
UTI - urinary tract infection
VO - verbal order.
XRT - radiation therapy
YOB - year of birth
BRBPR - bright red blood per rectum
CX - cervix
DVT - deep vein thrombosis
GB - gallbladder
GU - genitourinary
HCV - hepatitis C virus
HPI - history of present illness
ICP - intracranial pressure
IVP - intravenous pyelogram
LMP - last menstrual period
MRSA - methicillin-resistant Staphylococcus aureus
MVA - motor vehicle accident
NKA - no known allergies
PEG - percutaneous endoscopic gastrostomy
PRN - pro re nata (as needed)
ROS - review of systems
SOB - shortness of breath
TAH - total abdominal hysterectomy.
TIA - transient ischemic attack
Tx - treatment
UC - ulcerative colitis
URI - upper respiratory infection
VSD - ventricular septal defect
VTE - venous thromboembolism
XR - x-ray
w/c - wheelchair
XRT - radiation therapy
ASD - atrial septal defect
Bx - biopsy
CAD - coronary artery disease
CKD - chronic kidney disease
CPAP - continuous positive airway pressure
DKA - diabetic ketoacidosis
DNR - do not resuscitate
ED - emergency department
ESRD - end-stage renal disease
FFP - fresh frozen plasma
FSH - follicle-stimulating hormone.
GCS - Glasgow Coma Scale
Hct - hematocrit
Hgb - hemoglobin
ICU - intensive care unit
IV - intravenous
JVD - jugular venous distension
K - potassium
L - liter
MCH - mean corpuscular hemoglobin
MI - myocardial infarction
Na - sodium
NGT - nasogastric tube
NPO - nothing by mouth
OR - operating room
PCN - penicillin
PRBC - packed red blood cells
PTT - partial thromboplastin time
RBC - red blood cells
RT - respiratory therapy
SOA - short of air.
SCD - sequential compression device
SIRS - systemic inflammatory response syndrome
STAT - immediately
T - temperature
TPN - total parenteral nutrition
WBC - white blood cells
ABG - arterial blood gas
A fib - atrial fibrillation
BPH - benign prostatic hypertrophy
CBC - complete blood count
CO2 - carbon dioxide
COPD - chronic obstructive pulmonary disease
CPR - cardiopulmonary resuscitation
CT - computed tomography
CXR - chest x-ray
D5W - dextrose 5% in water
Dx - diagnosis
ECG or EKG - electrocardiogram
EEG - electroencephalogram
ETO - early termination of pregnancy.
FHR - fetal heart rate
GSW - gunshot wound
H&P - history and physical exam
HCG - human chorionic gonadotropin
I&D - incision and drainage
IBS - irritable bowel syndrome
ICP - intracranial pressure
IM - intramuscular
INR - international normalized ratio
IOP - intraocular pressure
LFT - liver function test
LOC - level of consciousness
LP - lumbar puncture
NG - nasogastric
OA - osteoarthritis
OCD - obsessive-compulsive disorder
OTC - over-the-counter
P - pulse
PCA - patient-controlled analgesia
PERRLA - pupils equal, round, reactive to light and accommodation.
PFT - pulmonary function test
PICC - peripherally inserted central catheter
PO - by mouth
PRN - as needed
PT - physical therapy
PT - prothrombin time
PTSD - post-traumatic stress disorder
PVC - premature ventricular contraction
QD - once a day
QID - four times a day
RA - rheumatoid arthritis
RICE - rest, ice, compression, elevation
RSI - rapid sequence intubation
RSV - respiratory syncytial virus
SBP - systolic blood pressure
SLE - systemic lupus erythematosus
SSRI - selective serotonin reuptake inhibitor
STAT - immediately
TB - tuberculosis
TIA - transient ischemic attack.
TID - three times a day
TKO - to keep open
TNTC - too numerous to count
TPN - total parenteral nutrition
URI - upper respiratory infection
UTI - urinary tract infection
V-fib - ventricular fibrillation
V-tach - ventricular tachycardia
VA - visual acuity
WNL - within normal limits
AED - automated external defibrillator
ARDS - acute respiratory distress syndrome
BID - twice a day
BP - blood pressure
BUN - blood urea nitrogen
CAD - coronary artery disease
CHF - congestive heart failure
CVA - cerebrovascular accident
D/C - discontinue
DKA - diabetic ketoacidosis.
DM - diabetes mellitus
DVT - deep vein thrombosis
EGD - esophagogastroduodenoscopy
ER - emergency room
F - Fahrenheit
Fx - fracture
GI - gastrointestinal
GTT - glucose tolerance test
HCT - hematocrit
Hgb - hemoglobin
HRT - hormone replacement therapy
ICP - intracranial pressure
IDDM - insulin-dependent diabetes mellitus
IBS - irritable bowel syndrome
IM - intramuscular
IV - intravenous
K - potassium
KVO - keep vein open
L&D - labor and delivery
LASIK - laser-assisted in situ keratomileusis.
ROM - range of motion
RT - radiation therapy
Rx - prescription
SCD - sequential compression device
SOB - shortness of breath
STD - sexually transmitted disease
TENS - transcutaneous electrical nerve stimulation
TIA - transient ischemic attack
TSH - thyroid-stimulating hormone
UA - urinalysis
US - ultrasound
UTI - urinary tract infection
VD - venereal disease
VF - ventricular fibrillation
VT - ventricular tachycardia
WBC - white blood cell
XRT - radiation therapy
XR - x-ray
Zn - zinc
Z-pak - azithromycin (antibiotic).
AAA - abdominal aortic aneurysm
ABG - arterial blood gas
ACS - acute coronary syndrome
ADL - activities of daily living
AED - automated external defibrillator
AIDS - acquired immunodeficiency syndrome
ALS - amyotrophic lateral sclerosis
AMA - against medical advice
AML - acute myeloid leukemia
APAP - acetaminophen
ARDS - acute respiratory distress syndrome
ASCVD - atherosclerotic cardiovascular disease
BPH - benign prostatic hyperplasia
BUN - blood urea nitrogen
CABG - coronary artery bypass graft
CBC - complete blood count
CHF - congestive heart failure
COPD - chronic obstructive pulmonary disease
CPAP - continuous positive airway pressure
CRF - chronic renal failure.
CT - computed tomography
CVA - cerebrovascular accident
D&C - dilation and curettage
DVT - deep vein thrombosis
ECG/EKG - electrocardiogram
EEG - electroencephalogram
ESRD - end-stage renal disease
FSH - follicle-stimulating hormone
GERD - gastroesophageal reflux disease
GFR - glomerular filtration rate
HbA1c - glycated hemoglobin
Hct - hematocrit
HIV - human immunodeficiency virus
HPV - human papillomavirus
HTN - hypertension
IBD - inflammatory bowel disease
IBS - irritable bowel syndrome
ICU - intensive care unit
IDDM - insulin-dependent diabetes mellitus
IM - intramuscular.
IV - intravenous
LFT - liver function test
MI - myocardial infarction
MRI - magnetic resonance imaging
MS - multiple sclerosis
NPO - nothing by mouth
NS - normal saline
OCD - obsessive-compulsive disorder
OSA - obstructive sleep apnea
PCOS - polycystic ovary syndrome
PMS - premenstrual syndrome
PPD - purified protein derivative
PSA - prostate-specific antigen
PT - prothrombin time
PTT - partial thromboplastin time
RA - rheumatoid arthritis
RBC - red blood cell
RSV - respiratory syncytial virus
SLE - systemic lupus erythematosus
TB - tuberculosis.
It is important to remember that medical abbreviations can vary based on location and specialty.
Healthcare professionals should use medical abbreviations with caution and only when they are familiar with their meanings.
Patients should always communicate any questions or concerns they have about their medications or medical care to their healthcare provider or pharmacist to ensure they receive safe and accurate medical care.

7 notes
·
View notes
Text
Clinical Trial Imaging Market 5.9% CAGR Projection Over The Next Five Years
Market Overview
Clinical Trial Imaging is the use of imaging modalities, analysis services, and software to ascertain the effectiveness of innovative drugs before they are made available for purchase. Clinical imaging methods are being utilised more frequently in oncology treatment trials to demonstrate the efficacy and safety of the drug. Positron Emission Tomography (PET), Optical Coherence Tomography (OCT), Magnetic Resonance Imaging (MRI), and Ultrasound are the imaging technologies most frequently employed in clinical trials. During the projection period, the market is anticipated to be driven by the rise in cancer diagnoses and deaths globally. However, it is anticipated that the industry's growth prospects will be constrained by the severe government regulations in the field.
View Detailed Report Description: https://www.globalinsightservices.com/reports/clinical-trial-imaging-market/
Market Dynamics
The most important aspect, like an increase in R&D expenditures, is an increase in R&D expenditures. Companies in the pharmaceutical and biotechnology industries spend a lot of money on research to create novel compounds. The market for clinical trial imaging is predicted to grow as a result of rising government and pharmaceutical R&D spending as well as a growing emphasis on life science projects to create new therapeutic and diagnostic products. Similarly, developing nations like India, South Korea, Brazil, and Mexico present substantial potential opportunities to market participants in clinical trial imaging, primarily as a result of the rising R&D investment in these nations.
A notable trend in these emerging markets is the commercialization of life science research. These economies are expected to present the clinical trial imaging market with substantial growth prospects due to considerable advancements in life sciences research. Additionally, there are other CROs that provide drug development services to pharmaceutical and biotechnology businesses in Asian markets, particularly China and India. The need for clinical trial imaging is predicted to rise in emerging nations in the next years due to the large increase in R&D spending and CROs operating in these nations.
The key players in the global clinical trial imaging market are ICON plc. (Ireland), BioTelemetry Inc. (US), Biomedical Systems Corporation (US), Medpace Holdings, Inc. (US), IXICO plc. (UK), Resonance Health Ltd. (Australia), Radiant Sage LLC. (US), BioClinica Inc. (US), Intrinsic Imaging LLC. (US), Cardiovascular Imaging Technologies LLC. (US), Medical Metrics Inc. (US), Prism Clinical Imaging, Inc. (US), Boston Imaging Core Lab LLC. (US), anagram 4 clinical trials (Spain), Lyscaut Medical Imaging Company (Belgium), Calyx Group (UK), Bioseptive Inc. (Canada), ProScan Imaging LLC. (US), Micron Inc. (Japan), Imaging Endpoints LI, LLC (US), Perspectum Ltd. (UK), Pharmtrace Klinische Entwicklung GmbH (Germany), WorldCare Clinical, LLC (US).
About Global Insight Services:
Global Insight Services (GIS) is a leading multi-industry market research firm headquartered in Delaware, US. We are committed to providing our clients with highest quality data, analysis, and tools to meet all their market research needs. With GIS, you can be assured of the quality of the deliverables, robust & transparent research methodology, and superior service.
Contact Us:
Global Insight Services LLC
16192, Coastal Highway, Lewes DE 19958
E-mail: [email protected]
Phone: +1–833–761–1700
2 notes
·
View notes
Text
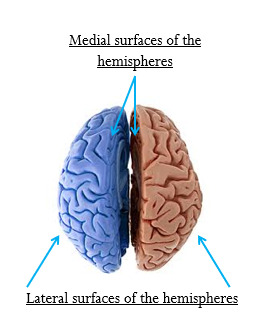
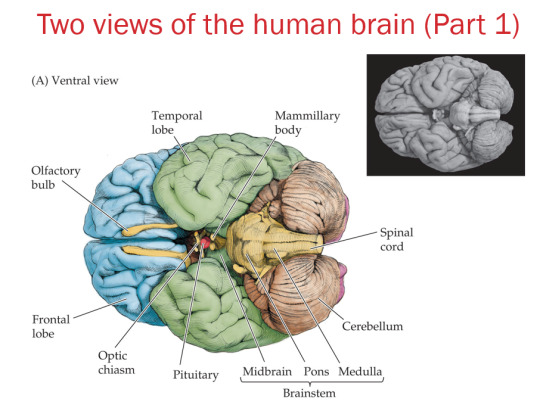
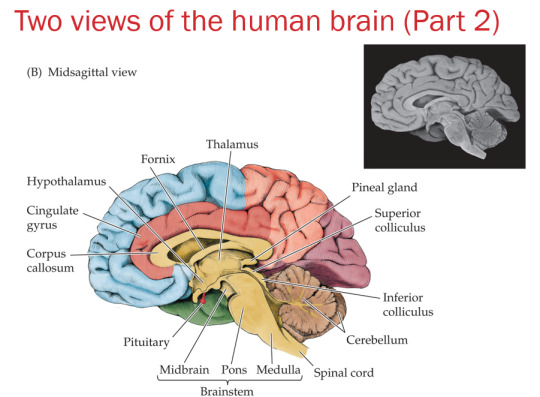
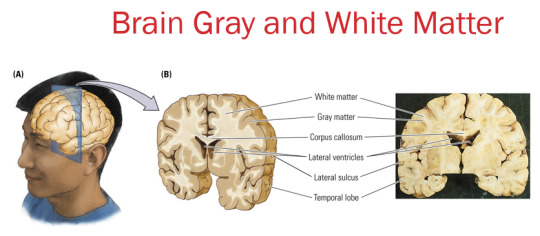
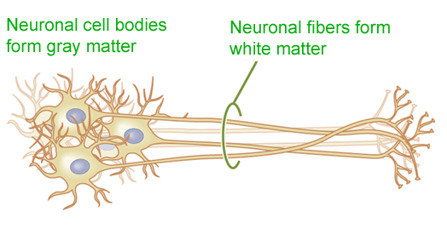
Anatomy of the Nervous System
Structure of the Nervous System
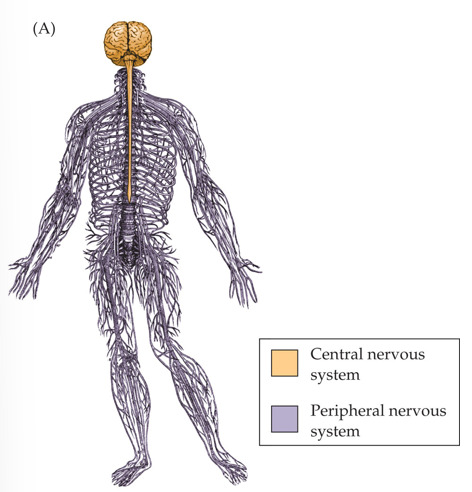
The brain is inside the skull; the spinal cord is inside the vertebral column (spine).
Somatic nervous system:
controls skeletal muscles
conscious control
Autonomic nervous system:
balances internal organs
unconscious control
Functions of the Nervous System
Control of behaviors:
Sensory function: get and integrate information about the world and create a sensory reality.
Motor function: control movements.
Plasticity: adapt to the world by changing its physical or chemical properties; functions to adapt to environmental change or to compensate for injury.
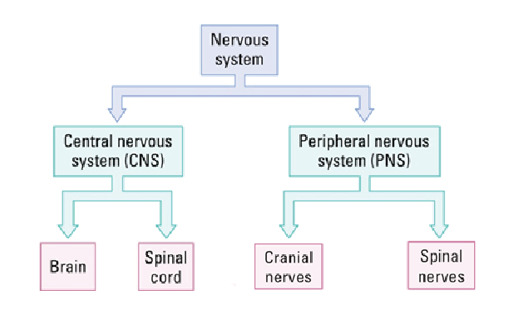
Navigating Your Nervous System
front/back = anterior/posterior
up/down = superior/inferior
belly/back = ventral/dorsal
beak/tail = rostral/caudal
along the middle = medial
left or right side = lateral
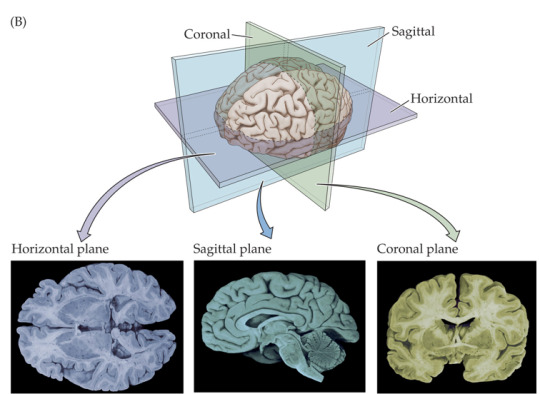
How can we visualize brain structures?
A. Dead Brain
Postmortem examination:
Brain is stored in fixative solution
Sliced with a knife to see brain structures
B. Live Brain
Optically sliced:
Computer tomography (CT)
Magnetic resonance imaging (MRI, structural or functional)
Positron emission tomography (PET)
Functional MRI and PET help to assess activity of brain regions
Rat Brains vs. Human Brains
Rats are commonly used as research models. Brain structures have not changed very much during mammalian evolution, so the basic brain plan is similar for rats and humans.

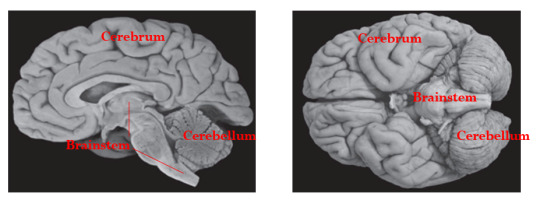
Brain Divisions (based on surface features)
A. Cerebrum: consists of two virtually identical hemispheres (left and right)
B. Cerebellum (”little brain”)
C. Brain stem
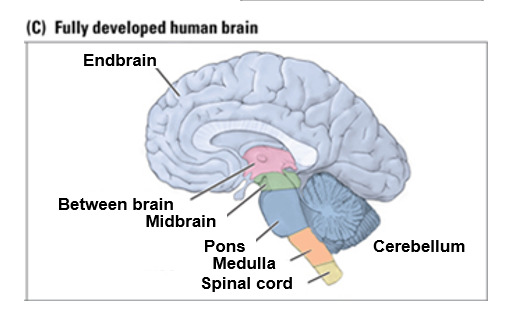
Brain divisions (based on development and evolution)
Forebrain
A. End brain
Cortex
Corpus callosum
Limbic system
Basal ganglia
Olfactory bulb
B. Between brain
Thalamus
Hypothalamus
Midbrain
Tectum
Tegmentum
Hindbrain
Pons
Cerebellum
Medulla
2 notes
·
View notes
Text
Preclinical Imaging Market Innovations, Growth Drivers, and Future Prospects
The preclinical imaging market is experiencing robust growth, driven by advancements in technology, increased investment in research and development, and a growing focus on early disease detection and drug development. Preclinical imaging refers to the visualization techniques used in animal studies to understand disease mechanisms, evaluate drug efficacy, and monitor biological processes at the molecular level before clinical trials in humans. This article explores the key drivers, technological advancements, market segmentation, and future outlook of the preclinical imaging market.
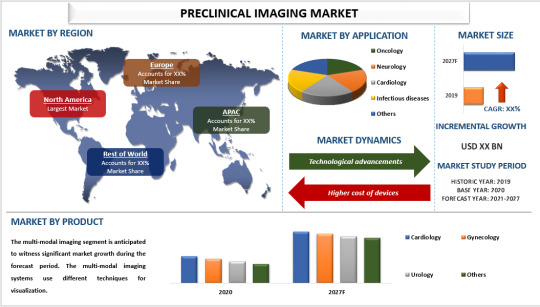
Key Market Drivers
1. Advancements in Imaging Technologies: The continuous evolution of imaging technologies is a significant driver of the preclinical imaging market. Techniques such as magnetic resonance imaging (MRI), positron emission tomography (PET), computed tomography (CT), and optical imaging have advanced significantly, offering higher resolution, better accuracy, and more detailed images. These improvements enable researchers to gain deeper insights into disease mechanisms and drug effects at the cellular and molecular levels.
2. Increased Investment in R&D: There has been a substantial increase in research and development investments by pharmaceutical and biotechnology companies, academic institutions, and government bodies. These investments aim to accelerate the development of new drugs and therapies, driving the demand for advanced preclinical imaging technologies. The ability to visualize and monitor biological processes in vivo is crucial for assessing the safety and efficacy of new treatments before they reach clinical trials.
3. Growing Focus on Personalized Medicine: The shift towards personalized medicine, which tailors treatments to individual patients based on genetic, environmental, and lifestyle factors, is another key driver. Preclinical imaging plays a vital role in identifying biomarkers, understanding disease progression, and evaluating targeted therapies. This personalized approach enhances the effectiveness of treatments and reduces the risk of adverse effects.
For a comprehensive analysis of the market drivers, visit: https://univdatos.com/report/preclinical-imaging-market/
Technological Advancements
1. Hybrid Imaging Systems: The development of hybrid imaging systems, such as PET/CT and PET/MRI, has revolutionized preclinical imaging. These systems combine the strengths of different imaging modalities, providing comprehensive data in a single scan. For example, PET/CT combines the functional imaging capabilities of PET with the anatomical detail of CT, enabling more precise localization of disease sites.
2. Optical Imaging: Optical imaging techniques, including bioluminescence and fluorescence imaging, have gained popularity in preclinical research. These methods are non-invasive and highly sensitive, allowing real-time monitoring of cellular and molecular processes. Optical imaging is particularly useful for studying cancer, infectious diseases, and gene expression.
3. Molecular Imaging: Molecular imaging techniques enable the visualization of specific molecular targets and pathways within living organisms. This approach is invaluable for studying the underlying mechanisms of diseases, evaluating the effectiveness of new drugs, and developing targeted therapies. Advances in molecular imaging agents and probes have significantly enhanced the capabilities of preclinical imaging.
Future Prospects
The future of the preclinical imaging market looks promising, with several trends and opportunities poised to drive further growth:
1. Integration of Artificial Intelligence (AI): The integration of AI and machine learning in preclinical imaging is set to enhance image analysis, automate data interpretation, and improve diagnostic accuracy. AI algorithms can process vast amounts of imaging data, identify patterns, and provide insights that may be missed by human observers.
2. Expansion in Emerging Markets: The preclinical imaging market is expanding in emerging economies due to increasing R&D activities, improving healthcare infrastructure, and growing investments in biotechnology and pharmaceutical research. Countries in Asia-Pacific, Latin America, and the Middle East offer significant growth opportunities.
3. Collaboration and Partnerships: Collaborations between academic institutions, research organizations, and industry players are fostering innovation in preclinical imaging. These partnerships facilitate the development of new imaging technologies, the sharing of expertise, and the acceleration of translational research.
For a sample report, visit https://univdatos.com/get-a-free-sample-form-php/?product_id=22817
Conclusion
The preclinical imaging market is on a trajectory of rapid growth, driven by technological advancements, increased R&D investments, and the rising demand for personalized medicine. As imaging technologies continue to evolve and integrate with AI, the market is expected to witness further innovations and expanded applications. These developments will not only enhance our understanding of diseases but also expedite the discovery and development of new treatments, ultimately improving patient outcomes.
Contact Us:
UnivDatos Market Insights
Email - [email protected]
Contact Number - +1 9782263411
Website -www.univdatos.com
#Preclinical Imaging Market#Preclinical Imaging Market Size#Preclinical Imaging Market Growth#Preclinical Imaging Market Forecast
0 notes
Text
Exploring the Depths of Gastrointestinal Radiology: Techniques, Innovations, and Insights
Gastrointestinal radiology, a specialized branch of medical imaging, plays a crucial role in diagnosing and treating diseases of the digestive tract. This field leverages various imaging techniques to visualize the structure and function of the gastrointestinal (GI) system, providing invaluable insights that guide clinical decision-making. In this blog, we'll delve into the core techniques, recent innovations, and key insights within gastrointestinal radiology.
Core Techniques in Gastrointestinal Radiology
1. X-Ray Imaging
X-rays are the cornerstone of gastrointestinal radiology. Techniques such as fluoroscopy, barium studies, and plain radiographs allow for the visualization of the esophagus, stomach, and intestines. Barium swallow and barium enema are commonly used to detect structural abnormalities, such as strictures, diverticula, and tumors.
2. Computed Tomography (CT)
CT scans provide detailed cross-sectional images of the abdomen and pelvis, offering a comprehensive view of the GI tract and surrounding organs. CT enterography and CT colonography are specialized techniques that enhance visualization of the small intestine and colon, respectively. These methods are essential for detecting inflammatory diseases, such as Crohn's disease, and identifying neoplasms.
3. Magnetic Resonance Imaging (MRI)
MRI, particularly magnetic resonance enterography (MRE), is increasingly used in gastrointestinal radiology. MRE offers high-contrast images without radiation exposure, making it ideal for patients requiring frequent imaging, such as those with inflammatory bowel disease (IBD). MRI is also valuable in liver imaging, providing detailed information about hepatic lesions and vascular structures.
4. Ultrasound
Ultrasound is a non-invasive, real-time imaging technique commonly used to evaluate the liver, gallbladder, and biliary system. Endoscopic ultrasound (EUS) combines endoscopy and ultrasound to obtain high-resolution images of the GI tract and surrounding tissues, facilitating the diagnosis of pancreatic and esophageal disorders.
5. Nuclear Medicine
Nuclear medicine techniques, such as positron emission tomography (PET) and single-photon emission computed tomography (SPECT), are used to assess metabolic activity and detect malignancies. These modalities are particularly useful in staging cancers and evaluating treatment response.
Innovations in Gastrointestinal Radiology
The field of gastrointestinal radiology is continually evolving, with technological advancements enhancing diagnostic accuracy and patient care. Some notable innovations include:
1. Artificial Intelligence (AI) and Machine Learning
AI and machine learning are revolutionizing radiology by improving image analysis and interpretation. Algorithms can assist radiologists in detecting subtle abnormalities, reducing diagnostic errors, and increasing efficiency. AI-driven tools are particularly promising in screening for colorectal cancer and assessing liver fibrosis.
2. Advanced Imaging Techniques
Innovations such as dual-energy CT, diffusion-weighted MRI, and contrast-enhanced ultrasound offer enhanced tissue characterization and better differentiation between benign and malignant lesions. These advanced techniques provide more precise diagnostic information, aiding in early disease detection and personalized treatment planning.
3. Minimally Invasive Procedures
Interventional radiology (IR) techniques, such as percutaneous biopsies, ablations, and drainage procedures, are becoming more refined. These minimally invasive procedures, often guided by imaging, reduce the need for surgical interventions, decrease patient recovery time, and minimize complications.

Insights and Clinical Applications
Gastrointestinal radiology provides critical insights that impact patient management across various conditions:
1. Inflammatory Bowel Disease (IBD)
Imaging plays a vital role in diagnosing and monitoring IBD, including Crohn's disease and ulcerative colitis. MRI and CT enterography are essential for evaluating disease extent, detecting complications, and guiding therapeutic decisions.
2. Gastrointestinal Cancers
Early detection and accurate staging of GI cancers are paramount for successful treatment. CT, MRI, and PET scans are integral in identifying tumors, assessing their spread, and planning surgical or therapeutic interventions. Regular imaging follow-ups help monitor treatment efficacy and detect recurrences.
3. Liver Disease
Imaging modalities are indispensable in evaluating liver diseases such as cirrhosis, hepatitis, and hepatocellular carcinoma. MRI and ultrasound are particularly valuable for assessing liver morphology, vascular structures, and detecting focal lesions.
4. Functional Disorders
Radiological techniques, including motility studies and defecography, aid in diagnosing functional GI disorders such as achalasia, gastroparesis, and chronic constipation. These studies provide insights into the dynamic processes of the GI tract, guiding appropriate therapeutic interventions.
Conclusion
Gastrointestinal radiology is a dynamic and integral part of modern medicine, offering essential diagnostic and therapeutic capabilities. The continuous advancements in imaging technology and the integration of AI are enhancing the precision and efficacy of GI radiology, ultimately improving patient outcomes. As we continue to explore the depths of gastrointestinal radiology, the future holds promise for even more innovative solutions to complex clinical challenges.
Important Information:
Conference Name: 14th World Gastroenterology, IBD & Hepatology Conference
Short Name: 14GHUCG2024
Dates: December 17-19, 2024
Venue: Dubai, UAE
Email: [email protected]
Visit: https://gastroenterology.universeconferences.com/
Call for Papers: https://gastroenterology.universeconferences.com/submit-abstract/
Register here: https://gastroenterology.universeconferences.com/registration/
Exhibitor/Sponsor: https://gastroenterology.universeconferences.com/exhibit-sponsor-opportunities/
Call Us: +12073070027
WhatsApp Us: +442033222718
0 notes
Text
0 notes
Text
Advanced Brain Surgery Techniques Available in Orange County
Introduction:
Brain surgery represents a critical frontier in modern medicine, with advancements in technology and surgical techniques continuously pushing the boundaries of what is possible. In Orange County, California, a hub of medical innovation and excellence, neurosurgeons are at the forefront of pioneering advanced brain surgery techniques. This comprehensive discussion explores the cutting-edge approaches available in Orange County, highlighting their advancements, applications, and impact on patient care.

Evolution of Brain Surgery:
The history of brain surgery is marked by remarkable progress, from the early rudimentary procedures of trepanation to the sophisticated techniques and technologies available today. Over the centuries, pioneers in neurosurgery have made significant contributions, refining surgical techniques, developing innovative instruments, and expanding our understanding of brain anatomy and pathology. With each advancement, the field of brain surgery has evolved, enabling neurosurgeons to offer safer, more effective treatments for a wide range of neurological conditions.
Advanced Neuroimaging:
Neuroimaging plays a pivotal role in modern brain surgery, providing detailed anatomical and functional information essential for surgical planning and navigation. In Orange County, neurosurgeons utilize state-of-the-art imaging modalities such as magnetic resonance imaging (MRI), computed tomography (CT), and positron emission tomography (PET) to visualize brain structures, identify pathology, and map critical functional areas. High-resolution imaging combined with advanced software algorithms enables surgeons to create precise three-dimensional reconstructions of the brain, facilitating accurate localization of lesions and optimal surgical approach.
Minimally Invasive Techniques:
Minimally invasive brain surgery techniques have revolutionized the field by offering patients less traumatic procedures, shorter recovery times, and improved outcomes compared to traditional open surgery. In Orange County, neurosurgeons employ a variety of minimally invasive approaches, including endoscopic surgery, keyhole craniotomy, and stereotactic-guided procedures, to access deep-seated brain lesions with precision and minimal disruption to surrounding tissues. These techniques utilize small incisions, specialized instruments, and advanced imaging guidance to target lesions while preserving normal brain function.
Endoscopic Surgery:
Endoscopic surgery has emerged as a versatile and minimally invasive approach for treating various brain conditions, including pituitary tumors, colloid cysts, and hydrocephalus. In Orange County, neurosurgeons utilize endoscopes equipped with high-definition cameras and lighting systems to access and visualize deep-seated brain structures through natural orifices or small incisions. Endoscopic techniques offer enhanced visualization, improved illumination, and reduced morbidity compared to traditional open approaches, making them ideal for select patients requiring precise, targeted intervention.
Stereotactic Radiosurgery:
Stereotactic radiosurgery (SRS) is a non-invasive technique that delivers precisely targeted radiation to intracranial lesions while sparing surrounding healthy tissue. In Orange County, neurosurgeons utilize advanced SRS platforms such as Gamma Knife and CyberKnife to treat brain tumors, arteriovenous malformations (AVMs), and trigeminal neuralgia with unparalleled accuracy and efficacy. SRS offers several advantages, including high conformity, minimal side effects, and the ability to treat multiple lesions in a single session, making it an attractive option for patients with inoperable or recurrent tumors.
Intraoperative Neurophysiological Monitoring:
Intraoperative neurophysiological monitoring (IONM) is an integral component of modern brain surgery, providing real-time feedback on neural function to minimize the risk of neurological complications during surgery. In Orange County, neurosurgeons utilize sophisticated IONM techniques such as electromyography (EMG), somatosensory evoked potentials (SSEP), and motor evoked potentials (MEP) to monitor the integrity of the brain and spinal cord pathways during complex procedures. By continuously assessing neural function, IONM helps surgeons navigate critical structures, optimize surgical outcomes, and mitigate the risk of postoperative deficits.
Robotic-Assisted Surgery:
Robotic-assisted surgery has emerged as a promising adjunct to traditional brain surgery Orange County techniques, offering enhanced precision, dexterity, and visualization for intricate procedures. In Orange County, neurosurgeons utilize robotic platforms such as the ROSA robot and the StealthStation system to assist with cranial navigation, tumor resection, and electrode placement for deep brain stimulation (DBS). Robotic assistance enables surgeons to perform complex maneuvers with submillimeter accuracy while minimizing tissue trauma and operative time, ultimately improving patient safety and outcomes.
Conclusion:
In Orange County, California, neurosurgeons are pioneers in advancing the field of brain surgery, offering patients access to cutting-edge techniques and state-of-the-art treatments. From advanced neuroimaging and minimally invasive approaches to intraoperative monitoring and robotic-assisted surgery, these innovations have transformed the landscape of modern neurosurgery, providing patients with safer, more effective treatments for complex neurological conditions. By leveraging these advanced techniques, neurosurgeons in Orange County continue to push the boundaries of what is possible in brain surgery, offering hope and healing to patients in need.
0 notes
Text
Best PET CT Scan in Mohali - Superb Diagnostics
Unrivalled diagnostic services find superb match in PET CT scan best performance in Mohali. Excellent precision and reliability being powered therewith. State-of-art technology is also combined with extremely qualified medical specialists to bring high standard imaging, for professional diagnosis and treatment planning.
To make maximum utilization of the top quality facilities, way of strict pursuit is assured at the premier PET CT centers in Mohali to have the best patient care and accomplishment.
Using the latest PET-CT devices, these clinics gives you a possibility for acquisition of very clear and detailed pictures and these images are really helpful in revealing and following-up on different medical conditions such as cancer, cardiovascular diseases and neurological disorders.
Fusing positron emission tomography (PET) and computed tomography (CT) injections leads to a more comprehensive assessment of metabolism as well as anatomical structures compared to diagnostic tools that are limited to only one of these factors, which could ultimately improve decision making.
Patients are assured that the PET CT scans performed in Mohali will be quick, homely and secure though it is true that the patients seeking the best services need to pay little extra. Through a commitment of superior diagnostic centers, these centers and constitute a core part of the healthcare system that helps in delivering better outcomes for patients and improving their quality of life.
0 notes
Text
Positron Emission Tomography (PET) Systems Market Growth Outlook, Regional Insights, Size Estimation to 2032 | Zecotek Photonics, Brain Biosciences, GE Healthcare LLC
Positron Emission Tomography (PET) Systems Market Growth Outlook, Regional Insights, Size Estimation to 2032 | Zecotek Photonics, Brain Biosciences, GE Healthcare LLC
insightSLICE publishes a Global Positron Emission Tomography (PET) Systems Market from 2023 to 2032 research report that assesses the industry and significant market trends, as well as historical and forecasted market data. The study also includes market overview, as well as definitions and applications.
Get a FREE Sample Copy @ https://www.insightslice.com/request-sample/1162
The exhaustive…

View On WordPress
#Future Trends of Positron Emission Tomography (PET) Systems industry#Positron Emission Tomography (PET) Systems#Positron Emission Tomography (PET) Systems manufacturing Vendors#Positron Emission Tomography (PET) Systems market#Positron Emission Tomography (PET) Systems market share#Positron Emission Tomography (PET) Systems market size#Positron Emission Tomography (PET) Systems market SWOT analysis#Scope of Positron Emission Tomography (PET) Systems industry
0 notes
Text
Chest Wall Cancer: Symptoms, Diagnosis, and Treatment
Symptoms of Chest Wall Cancer
The symptoms of chest wall cancer can vary depending on the type and stage of the tumor but generally include:
Pain: Persistent pain in the chest area that may worsen with movement or breathing.
Swelling or Lump: Noticeable mass or swelling in the chest wall.
Breathing Difficulties: Shortness of breath or difficulty breathing.
Chest Discomfort: General discomfort or tightness in the chest.
Weight Loss: Unintended weight loss.
Fatigue: Persistent tiredness or fatigue.
Neurological Symptoms: If the tumor presses on nerves, it can cause numbness, tingling, or weakness in the arms or legs.
Diagnosis of Chest Wall Cancer
Diagnosis involves several steps and tests to confirm the presence of cancer and its extent:
Physical Examination: Initial assessment by a healthcare provider, including a review of medical history and symptoms.
Imaging Studies:
X-rays: Basic imaging to identify abnormalities in the chest wall.
CT Scan (Computed Tomography): Detailed cross-sectional images to evaluate the size and spread of the tumor.
MRI (Magnetic Resonance Imaging): High-resolution images for detailed view, particularly of soft tissues.
PET Scan (Positron Emission Tomography): Detects metabolic activity of cancer cells to determine the extent of spread.
Biopsy:
Needle Biopsy: A sample of the tumor tissue is taken using a needle for microscopic examination.
Surgical Biopsy: Sometimes, a surgical procedure is necessary to obtain a tissue sample.
Blood Tests: To assess overall health and detect markers that might suggest cancer.
Treatment of Chest Wall Cancer
Treatment options depend on the type, size, location, and stage of the tumor, as well as the patient’s overall health:
Surgery:
Resection: Removal of the tumor and some surrounding healthy tissue.
Reconstructive Surgery: May be necessary to rebuild the chest wall using synthetic materials or tissue from other parts of the body.
Radiation Therapy: High-energy rays to kill cancer cells or shrink tumors. Often used before surgery (neoadjuvant) to reduce tumor size or after surgery (adjuvant) to destroy remaining cancer cells.
Chemotherapy: Drugs that kill cancer cells or stop them from growing. It can be systemic (throughout the body) or localized.
Targeted Therapy: Uses drugs or other substances to specifically target cancer cells without affecting normal cells.
Immunotherapy: Boosts the body's immune system to fight cancer.
Pain Management and Palliative Care: Focuses on relieving symptoms and improving quality of life for patients with advanced cancer.
Conclusion
Early detection and treatment are crucial for improving the prognosis of chest wall cancer. If you experience any persistent symptoms such as chest pain, swelling, or difficulty breathing, consult a healthcare provider promptly. Multidisciplinary approaches combining surgery, radiation, and systemic therapies offer the best outcomes, tailored to the individual needs of the patient.
0 notes
Text
PET scans have a wide range of applications across various fields of medicine, including:
Oncology: PET scans are extensively used in cancer diagnosis, staging, treatment planning, and monitoring. They can detect cancerous tumors, evaluate the extent of cancer spread (metastasis), assess treatment response, and detect cancer recurrence.
Neurology: PET scans help in studying brain function and diagnosing neurological disorders such as Alzheimer's disease, Parkinson's disease, epilepsy, and brain tumors. They can visualize brain metabolism, blood flow, and neurotransmitter activity, providing valuable insights into brain function and dysfunction.
Cardiology: PET scans are utilized in cardiology to assess myocardial perfusion (blood flow to the heart muscle), viability of heart tissue after a heart attack, and the presence of coronary artery disease. They can also identify areas of ischemia (inadequate blood supply) in the heart.
Psychiatry: PET scans aid in understanding psychiatric disorders by imaging neurotransmitter systems in the brain. They help in studying conditions such as depression, schizophrenia, bipolar disorder, and addiction, providing insights into the underlying neurochemical imbalances.
Infectious diseases: PET scans can detect sites of infection or inflammation in the body. They are used in diagnosing infections, assessing the extent of inflammatory processes, and monitoring response to treatment, particularly in conditions like tuberculosis and certain types of pneumonia.
Research: PET imaging is valuable in biomedical research for studying various physiological processes, drug development, and understanding disease mechanisms. It helps researchers investigate molecular pathways, evaluate new therapies, and develop diagnostic tools.
The procedure for a PET (Positron Emission Tomography) scan typically involves several steps:
Preparation: Before the scan, you may be instructed to avoid eating or drinking for a certain period, typically several hours, depending on the type of PET scan being performed. You may also need to abstain from strenuous physical activity to ensure accurate results.
Tracer Injection: Once you arrive at the imaging facility, a small amount of radioactive tracer material will be injected into a vein, usually in your arm. The tracer is often a compound containing a radioactive atom, such as fluorine-18, attached to a substance like glucose or ammonia. This tracer is chosen based on the specific area or function of the body being studied.
Uptake Period: After the tracer injection, you will typically need to wait for a period known as the uptake period. During this time, the tracer circulates through your bloodstream and is absorbed by the tissues or organs being studied. The length of the uptake period can vary depending on the specific tracer and the area of the body being imaged.
Scanning: Once the tracer has had time to distribute throughout your body, you will be positioned on a flat table that slides into the PET scanner. The scanner is a large, doughnut-shaped machine that contains detectors to measure the gamma rays emitted by the tracer.
Image Acquisition: As you lie still on the table, the PET scanner will move slowly around you, capturing a series of images from different angles. The scanner detects the gamma rays emitted by the tracer and uses this information to create detailed, three-dimensional images of the distribution of the tracer in your body.
Data Processing: After the scan is complete, the raw data collected by the scanner are processed by a computer to create the final PET images. These images are then reviewed by a radiologist or nuclear medicine physician, who interprets the findings and prepares a report for your referring healthcare provider.
Post-Scan: Once the scan is finished, you can typically resume your normal activities unless your healthcare provider advises otherwise. The radioactive tracer used in PET scans usually has a short half-life, meaning it decays rapidly and is eliminated from your body within a few hours.
Get best treatments and diagnosis done at best hospitals in India like Saifee Hospital Mumbai.
#health#surgery#mri scans#pet scan#full body checkups#brain tumor#tumor#saifee hospital#best hospital in mumbai
0 notes
Text
The Power of Antibody Reagents in Biomedical Applications
In the realm of biomedical research and clinical diagnostics, the significance of antibody reagents cannot be overstated. Antibodies are versatile molecules that play crucial roles in various applications, ranging from basic research to the development of diagnostic tests and targeted therapies. This article explores the profound impact of antibody reagents in advancing biomedical science and healthcare.
Understanding Antibody Reagents
Antibodies, also known as immunoglobulins, are specialized proteins produced by the immune system in response to foreign substances known as antigens. These proteins are highly specific and can recognize and bind to unique epitopes on antigens, initiating a series of immune responses. In laboratory settings, antibodies are harnessed as reagents for their ability to selectively target and bind to specific molecules of interest.
Antibodies in Basic Research
One of the primary applications of antibody reagents is in basic research. Scientists use antibodies to identify and localize proteins within cells and tissues, facilitating the study of biological processes and disease mechanisms. Techniques such as immunohistochemistry (IHC) and immunofluorescence (IF) rely on antibodies to visualize specific molecules under a microscope. By labeling antibodies with fluorescent or enzymatic markers, researchers can gain valuable insights into cellular structures and functions.
Moreover, antibodies are indispensable tools in techniques like Western blotting and enzyme-linked immunosorbent assay (ELISA), enabling the detection and quantification of proteins in complex biological samples. These assays are fundamental for characterizing biomarkers, studying protein-protein interactions, and assessing changes in gene expression.
Diagnostic Applications of Antibodies
Antibody-based diagnostics are widely employed in clinical settings for disease detection and monitoring. For instance, rapid diagnostic tests for infectious diseases often utilize antibodies to detect pathogen-specific antigens in patient samples. ELISA-based tests can identify antibodies produced by the immune system in response to infections, aiding in the diagnosis of viral or bacterial diseases.
Antibodies are also pivotal in medical imaging techniques like positron emission tomography (PET) and single-photon emission computed tomography (SPECT). In these methods, radiolabeled antibodies selectively bind to tumor cells or other diseased tissues, allowing for non-invasive visualization and localization of pathological sites within the body.
Therapeutic Potential of Antibody Reagents
The therapeutic landscape has been revolutionized by the development of monoclonal antibody therapies. Monoclonal antibodies, derived from a single clone of cells, are engineered to target specific antigens involved in diseases like cancer, autoimmune disorders, and inflammatory conditions. These antibodies can block harmful pathways, enhance immune responses against tumors, or deliver therapeutic payloads directly to affected cells.
Examples of successful monoclonal antibody therapies include trastuzumab for HER2-positive breast cancer and rituximab for B-cell lymphomas. The precision and efficacy of these therapies highlight the therapeutic potential of antibody reagents in personalized medicine.
Challenges and Future Directions
Despite their remarkable utility, antibody reagents face challenges such as batch-to-batch variability, stability issues, and the potential for immunogenicity. Researchers are actively addressing these issues through advanced techniques in antibody engineering and production.
The future of antibody reagents lies in developing novel formats and improving their specificity and affinity. Emerging technologies like bispecific antibodies, antibody-drug conjugates, and antibody fragments hold promise for enhancing therapeutic outcomes and expanding the scope of antibody-based applications.
Conclusion
In conclusion, antibody reagents represent a cornerstone of modern biomedical research and healthcare. From elucidating molecular pathways in basic science to enabling precise diagnostics and targeted therapies, antibodies continue to drive innovation and impact patient outcomes. As technology advances and our understanding of antibody biology deepens, the potential of antibody reagents in biomedical applications is poised to grow exponentially, ushering in a new era of personalized medicine and transformative therapies.
Through their versatility, specificity, and therapeutic potential, antibody reagents stand as testament to the enduring power of immunological tools in improving human health and combating disease.
0 notes