#One Dose of HPV Vaccine Prevents Infection for at Least Three Years
Link
Protection may last even longer, scientists reported. The finding may be a boon to low-income countries, where cervical cancer takes an enormous toll.
BY APOORVA MANDAVILLI | NYTimes Health | Disclosure
0 notes
Text
One Dose of HPV Vaccine Prevents Infection for at Least Three Years
Protection may last even longer, scientists reported. The finding may be a boon to low-income countries, where cervical cancer takes an enormous toll.
source https://www.nytimes.com/2023/05/02/health/hpv-vaccine-dose.html
View On WordPress
0 notes
Text
DO YOU KNOW THAT A CHANGE IN YOUR VOICE CAN BE A SIGN OF LARYNGEAL CANCER?By : Dr. Amrapali Pawar
DO YOU KNOW THAT A CHANGE IN YOUR VOICE CAN BE A SIGN OF LARYNGEAL CANCER?By : Dr. Amrapali Pawar
Hoarse voice, if it persists for more than 3 weeks , certainly needs to be evaluated as it can be a sign of laryngeal cancer or cancer of your voice box. But no need to panic! Just because your voice has changed its quality , it does not necessarily indicate that you have cancer. Other reasons why your voice may change or become hoarse are – laryngitis (inflammation of larynx), overuse or misuse of voice , acid reflux, allergies, trauma. So how do you know what has actually caused that change in your voice? For this you need to be properly evaluated by your ENT doctor who will infer from a proper and detailed history and examination, and if necessary , relevant investigations; your accurate diagnosis. He may need to do your laryngeal endoscopy to visualise and evaluate your voice box and surrounding structures. An examination of your neck to look for any enlarged lymph nodes, which may again be a sign of cancer is mandatory. If necessary, your ENT doctor will advise further investigations like a CT scan and / or biopsy. Although , most of the time , it is possible that your change of voice may be due to completely benign reasons which are stated above ; and if so, you will be prescribed some medications for your condition. If necessary, you will also be advised to undergo voice therapy for the same. The important thing to remember here is that- if at all you are suffering from a change of voice, please be sure to visit your ENT surgeon and get your condition diagnosed as soon as possible to avoid further complications. Any disease diagnosed in the early stage has the highest chance of recovery. The incidence of laryngeal cancer worldwide currently is 2.76 cases per year per one lakh inhabitants and 1.66 deaths per year per one lakh inhabitants . In India , laryngeal cancer contributes to approximately 3% -6% of all cancers in men. It is one of the 10 leading causes of cancer in Indian men. The 5 year survival rate for laryngeal cancer in India is approximately 28%. The factors most often implicated in the causation of laryngeal cancer according to Indian studies are : Smoking, alcohol consumption, tobacco, long term exposure to indoor air pollution ( from coal/ wood burning ) , spicy food . According to research more than 60% of laryngeal squamous cell carcinoma patients were cigarette smokers and nearly 75% of them had smoked for more than 30 years. In more than 75% of cases there was history of alcohol consumption. Change of voice or hoarse voice is not the only symptom of cancer of the larynx. Some of the patients also present with difficulty in swallowing, lump or swelling in the neck , weight loss, some even present with extreme pain in the ear (also known as referred nostalgia), in severe cases patients may present with difficulty in breathing. Depending on the stage and type of cancer , it can be treated by surgery (laryngectomy) , radiotherapy , chemotherapy or a combination of the above modalities of treatment. As stressed earlier, the management of laryngeal cancer is easier and the prognosis better if diagnosed early.
Read More..
Is Your Morning Coffee Interfering With The Absorption Of Your Thyroid Supplement?By : Dr. Amrapali Pawar
For many of us, the day cannot start without your morning dose of Java! And why shouldn’t it? We all require the caffeine to overcome that morning drowsiness and make us alert to the long day ahead of us! Apart from the boost that it gives us we justify the morning cup and several cups thereafter with a list of its benefits like its fat-burning quality, essential nutrients like vitamin B2, vitamin B5, magnesium and potassium, some studies say it reduces the risk of type 2 diabetes, contains antioxidants etc.etc. Because of all these reasons having that morning joe has become a routine part of our life as soon as we wake up just like brushing your teeth, or having a bath. Hence when we are affected with thyroid problems at some point in our life and have to take life long supplements, we fail to realize the big hurdle in the absorption of our thyroid medication simply because the thought does not cross our mind! Taking coffee within an hour of taking your thyroid supplement can reduce the absorption of your medication and thus makes it less effective. Caffeine in coffee is known to increase the intestinal motility i.e. it can increase the movement of your intestines. This makes your oral medication of thyroid supplement to pass through your intestines rapidly thus leading to decreased absorption. And since the prescribed dose is less absorbed, it obviously increases your chance of developing hypothyroidism. Coffee also inhibits the conversion and absorption of the thyroid hormone and as such is not considered good for your thyroid health. Hence coffee should be taken at least an hour or later than your daily thyroid supplement. Likewise, you have to keep in mind that fiber-rich foods, calcium supplements such as calcium carbonate and iron supplements such as ferrous sulfate can interfere with the absorption of your thyroid medication, and this effect can last longer than an hour. Hence the schedule of these drugs should be adjusted after consultation with your ENT doctor or your endocrine specialist. Calcium and Iron supplements in a patient with hypothyroidism should be taken at least 4 hours after taking thyroid supplements. Commonly used antacids like proton pump inhibitors can also interfere with the absorption of thyroid supplements. Remember that thyroid supplement interacts with minerals such as iron, calcium, and magnesium. Any supplements which contain these can lower the activity of your thyroid medicine. Supplements of herbal preparation like Ashwagandha and Bladderwrack used for a variety of problems like obesity, insomnia, dementia, etc. may contain dangerous levels of iodine and need to be definitely avoided if you are on thyroid supplement. This article is for all those who are regular in taking their thyroid supplement but are wondering why it is still not under control. This is for persons with hypothyroidism taking thyroid supplements to ensure that their thyroid health is not affected by the simple medication that they might sometimes be put on, ignorant of the effect these might have on their thyroid hormone levels. So, in conclusion, patients of hypothyroidism on thyroid supplement can definitely enjoy their morning cup of coffee ...they should just remember to space it adequately after their thyroid supplement.
Read More..
Can HPV Vaccination Prevent Head (Neck Cancers)By : Dr. Amrapali Pawar
What is HPV? HPV is Human Papilloma Virus and infection with the same is responsible for the development of genital warts , warts in the throat (recurrent respiratory papillomatosis), warts in the oral cavity (are uncommonly seen) but HPV infection here may manifest as mucosal hyperplasia. Many times these infections with HPV show absolutely no signs and symptoms but these persons still can transmit the infection. The type of HPV infection occurred depends on the strain of the HPV virus with which the person is infected. A person who has contracted a HPV infection is prone to development of cancer in that area. Studies have shown that about 14 million people including teens become infected with HPV every year. Many amongst these are prone to cancers caused by HPV infection. Screening tests are available for cervical cancer ( HPV related) for women . However no such screening tests are available for other cancers caused by HPV infection like cancers of the mouth and throat, cancer of anus, rectum, penis, vagina and vulva. Who should get HPV vaccination? • Recommended for preteens i.e. boys and girls at the age of 11–12 years. This ensures protection from the virus long before they are exposed to it or before they start being sexually active. Also young adults respond better to the vaccine than older ones. Vaccination given at this age requires only 2 doses as compared to three if given at a later age. • If they have missed the dose in their preteens , young men and women can be vaccinated till the age of 27yrs. The FDA (Federal Drug Authority) has approved HPV vaccination for males and females through age of 45 years but the ACIP (American Committee on Immunisation Practices) does not recommend routine vaccination after the age of 27 years as the effectiveness is questionable Ideally , HPV Vaccine should be administered before potential exposure to HPV through sexual contact. Are these vaccines easily available? These Vaccines are available with your Paediatrician, Gynaecologist, or ENT doctor and you can ask them for the same. For further information call us or email us at [email protected]
Read More..
If i am Gaining Weight, is it because i have a Thyroid Problem?By : Dr. Amrapali Pawar
Not necessarily. There are many causes of weight gain like lack of exercise i.e. having a sedentary life style, improper dietary habits, regular intake of junk food or processed food, certain metabolic diseases, genetic makeup, leptin resisitance and many more. Thyroid hormone abnormality like hypothyroidism i.e. 1. Decrease in the production of thyroid hormones by the thyroid gland can cause you to gain weight. The weight gain is generally unexplainable and occurs inspite of a decreased appetite. 2. It is associated with other symptoms also like fatigue, muscle weakness or muscle aches, feeling sluggish 3. Sensitivity to cold 4. In females, there may be menstrual irregularities 5. Skin can be dry and itchy and there can be hair loss 6.Other symptoms like feeling depressed, constipation or decrease in concentration can also be noted. On the other hand, increase in the production of thyroid hormone known as hyper- thyroidism can cause you to lose weight inspite of an increase in appetite.
Read More..
When is a Tonsillectomy Necessary?By : Dr. Amrapali Pawar
Tonsils are lymphoid tissues in the oral cavity which provide immunity in children till the age of 5 years. Inflammation of infection of these tissues is known commonly as Tonsillitis. Acute phase of this infection, known as acute Tonsillitis causes symptoms like pain in throat, difficulty in swallowing and fever and can be conventionally treated by antibiotics and anti-inflammatory agents. If these attacks of acute tonsillitis occur again and again, we call it Recurrent tonsillitis. If a person suffers from recurrent attacks of acute tonsillitis in a year for more than 2 years, we can say he is suffering from Chronic Tonsillitis.So how does the doctor decide that a person requires a Tonsillectomy? Tonsillectomy is done for a case of CHRONIC TONSILLITIS which means – “ If a person gets 3 or more attacks of acute tonsillitis for 2 or more consecutive years” What are the signs of chronic tonsillitis? The signs that your otolaryngologist looks for if he is suspecting a patient to be having chronic tonsillitis are – 1. Enlarged Jugulodigastric lymph nodes (these are lymph nodes present at the angle of jaw on either side) 2. congestion of anterior pillar ( the membranous structure in front of the the tonsils) 3. Enlarged / fibrosed tonsils Tonsillectomy is also performed 4-6 weeks after a case of PERITONSILLAR ABSCESS to prevent recurrence of the same. Peritosillar abscess or QUINSY is a condition or complication of acute tonsillitis in which pus collects in the tissues surrounding the tonsil and can cause severe symptoms of difficulty in swallowing , trismus ( difficulty in opening the jaw) , pain in throat and fever. Tonsillectomy is also indicated in cases of severly HYPERTROPHIC TONSILS (“KISSING TONSILS”) which actually meet in the midline and obstruct swallowing. Also in cases of SECRETORY OTITIS MEDIA (fluid collection in the middle ear) or ACUTE AND CHRONIC OTITIS MEDIA in children below the age of 12 yrs, Tonsillectomy is recommended as part of the treatment to reduce the attack of upper respiratory tract infection and prevent recurrence and halt progress of the disease. In adults , Tonsillectomy can be done as a part of surgery for OBSTRUCTIVE SLEEP APNEA and TONSILLAR CANCER.
Read More..
What Causes Hoarseness of Voice/Change of Voice?By : Dr. Amrapali Pawar
Voice is produced by vibration of your vocal cords or vocal folds, which are membranous band like tissues inside your voice box. Whenever these are affected by trauma, infection or tumor or when the nerve supplying them is damaged, your voice changes quality or becomes hoarse. Causes of hoarseness of voice are cited below: 1. Acute or chronic laryngitis – acute or chronic inflammation of the vocal cords due bacterial or viral infection. 2. Overuse or misuse of voice – shouting or singing in a loud voice can cause trauma to the delicate vocal cords and cause a hoarse voice. Speaking in a high pitch for a long period of time e.g. teachers, speakers can damage the vocal cords. 3. Swellings or benign cysts, polyps or nodules of the vocal cords are common causes of voice change. 4. Cancerous tumors of the vocal cords are a cause of hoarseness and should be evaluated properly for early detection of the disease. 5. Chronic systemic conditions like Gastro esophageal reflux disease, allergies, some thyroid disorders can cause hoarseness. 6. Smoking can affect the vocal cords and cause voice change. 7. Neurological conditions can cause paralysis of one vocal cord and can cause hoarseness. If both the vocal cords are affected then person will have difficulty in breathing too. Tips to improve vocal hygiene: 1. Voice rest – if your voice is affected, giving it complete rest i.e. not speaking will recover them faster 2. Do not shout or whisper- we all know that shouting causes trauma to the vocal folds but note that whispering is also similarly traumatic and can damage these delicate structures. 3. Hydrate the throat. Drink plenty of fluids. Also if your occupation entails speaking for a long period of time, have sips of water every 15 -20 minutes which will lubricate and protect your vocal cords 4. Treatment of acid reflux- if you tend to suffer from acid reflux, get it treated as reflux can contribute to or even exacerbate voice problems 5. Stop smoking – the relation between smoking and laryngeal cancer is well known but smoking can also cause respiratory diseases, which can lead to hoarseness of voice. 6. Avoid excess alcohol – alcohol has a drying effect on mucosal lining of tissues and also contribute to acid reflux which can affect vocal health 7. Stop that compulsive practice of ‘throat clearing’. 8. Maintain a good posture –Slouching over your desk for extensive hours can in the long run affect the respiratory system. This in turn leads to a weak or hoarse voice. Also cradling the phone between your shoulder and ear is not recommended for the same reason. If your job entails having to use the phone often and for a prolonged period, then it is advised you switch to a headset. 9. Do NOT gargle – if you are experiencing voice problems gargling will further cause trauma to your vocal cords. You can sip on warm liquids instead. These will hydrate the vocal cords and provide steam to soothe them. Conclusion: If conservative management to treat hoarseness of voice caused by benign pathology fails, vocal cord surgery also known as Microlaryngeal surgery maybe required. It is best to visit an ENT surgeon to get an opinion about this condition. The well-known otolaryngologist in Mumbai, Dr Amrapali Pawar, has been treating patients for over 15 years to address this ailment. Don’t let your voice bother you when one of the best ENT doctor in Mumbai is right near you!
Read More
#Doctor#entdoctor#ENTSurgeon#criticarehospital#chemburhospital#chemburENT#DrAmrapaliPawar#EarProblem#cancer#voicebox#laryngealcancer
0 notes
Text
HPV vaccine - Important Information
I thought I would repost a previous status of mine as scare campaigns against the HPV vaccine have been increasing. I’ve had an increase in people advising they won’t get their sons and daughters vaccinated against HPV. Scare tactics include “My teenager will become promiscuous” (Right. So exposure to a virus that causes various cancers should be a punishment for ((consensual and nonconsexual)) sex, apparently), and “My child won’t have sex” (Yeah, keep telling yourselves that).
Many people know about the association between HPV infection and cervical cancer in women. As a consequence, HPV has been dubbed a “woman’s infection.” However, approximately 40 percent of HPV-related cancers occur in men. Human papillomavirus (HPV) is a virus belonging to its own family: papillomaviridae, there are around 100 strains of HPV, with two types, cutaneous or mucocutaneous, based upon its tissue tropism or predilection for infecting specific areas of the human body.
The most common HPV-related cancers in men are oropharyngeal cancers, such as mouth, tongue or laryngeal cancer. Women can get these too, but men are three times as likely as women to carry oral HPV. Rarer HPV-related cancers in men include penile cancer and anal cancer. HPV can also cause warts in the head and neck region (example: laryngeal warts affecting the voice box) and on the genitals. While these warts are not life-threatening, they significantly impact quality of life.
Parents have often heard that the virus is sexually transmitted and wonder why their child would need vaccination. Most STDs affect a small portion of the population and can generally be avoided with safe sexual practices. HPV is different, because HPV is a skin-to-skin infection, sexual intercourse (anal/vaginal/oral) isn’t required to contract the infection. In rare cases it can be transmitted into the respiratory epithelium via an infected vaginal canal during birth. About 90 percent of all men and women will be infected with HPV at some point in their lives, even with safe sexual practices - Warts of the epidermis occur in approximately 10% of all children with peak ages between 12 to 16 years. Even if you only have one partner for your whole life, you can still get HPV and suffer its devastating consequences. HPV vaccination is the only dependable way to prevent it because it is almost impossible to avoid with lifestyle and behavioral decisions alone.
Respiratory papillomatosis is an unusual form of HPV disease. It presents in children between the ages of 2 and 10 years, all having been delivered as vaginal births, with signs of respiratory tract obstruction (https://tinyurl.com/yakruycr).
Parents may also wonder why it is necessary in childhood. Vaccines work best when they are given well before a person is exposed to a disease. The CDC recommends age 11-to-12 years old as the ideal time for vaccination. Recently, the CDC announced that if HPV vaccination is initiated before age 14, only two doses of the vaccine (at least six months apart) are required. If, however, vaccination begins at age 15 or older, three doses of the vaccine (at 0, 1-2 months and 6 months) are needed. This may be because the antibody response to the vaccine appears to be more robust in children 14 years and under, so fewer doses still provide sufficiently strong protection. (https://www.cdc.gov/hpv/index.html)
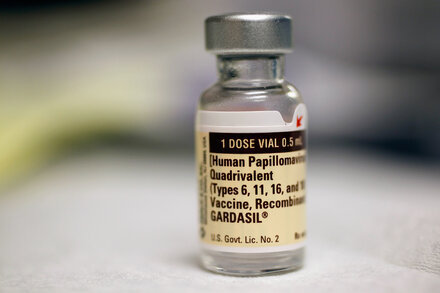
Two vaccines types have been manufactured, the Gardasil and Cervarix vaccine. Gardasil in particular has been developed to protect against the two high-risk HPV types (types 16 and 18), which cause 70% of cervical cancers in women and 90% of all HPV-related cancers in men. It also protects against two low-risk HPV types (types 6 and 11), which cause 90% of genital warts. (http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/immunise-hpv). Cervarix protects against types 16 and 18 only. Gardasil 9 has been manufactured which protects against a further 5 strains.
The HPV vaccine is a subunit vaccine. A subunit vaccine presents an antigen to the immune system without introducing viral particles at all. The HPV vaccine is created via genetic engineering. A gene coding for a vaccine protein is inserted into producer cells in a culture. When the producer cell metabolizes, the vaccine protein is also created. The end result of this approach is a recombinant vaccine: the immune system will recognize the expressed protein and provide future protection against the target virus. When these proteins are expressed, virus-like particles (VLPs) are created. These VLPs contain no genetic material from the viruses and can’t cause illness, but prompt an immune response that provides future protection against HPV.
(Other vaccines that use this technology include: Hepatitis B,Influenza (injection), Haemophilus influenza type b (Hib),Pertussis (part of DTaP combined immunization), Pneumococcal, Meningococcal)
The HPV vaccine is extremely safe. As of December 2015, almost 205 million doses of HPV vaccine had been distributed worldwide with no long-term serious adverse effects identified.
The HPV vaccine was developed in Australia (in my hometown). A groundbreaking effort from the University of Queensland's own Professor Ian Frazer from the UQ's Centre for Immunology and Cancer Research, and his team. Not by “Big Pharma” as some people falsely believe.
As Australia has had the vaccine the longest - the largest, most comprehensive studies have been conducted here. I have access to those studies as well as those from other countries. They are accessible below, including:
An Overview of Quadrivalent Human Papillomavirus
Vaccine Safety 2006 to 2015: https://drive.google.com/file/d/0BwNFCLOriAMMV1Z4cGJwSTh5V3c
Autoimmune, neurological, and venous thromboembolic adverse events after immunisation of adolescent girls with quadrivalent human papillomavirus vaccine in Denmark and Sweden: cohort study: https://drive.google.com/file/d/0BwNFCLOriAMMWHN0NXVzOG1xTFk
Early effect of the HPV vaccination programme on cervical abnormalities in Victoria, Australia: an ecological study: https://drive.google.com/file/d/0BwNFCLOriAMMM0hjUWZnSjg1aGs
Impact and Effectiveness of the Quadrivalent Human Papillomavirus Vaccine: A Systematic Review of 10 Years of Real-world Experience: https://drive.google.com/file/d/0BwNFCLOriAMMamlCSTNISXB0Slk
Long-term efficacy and safety of human papillomavirus vaccination: https://drive.google.com/file/d/0BwNFCLOriAMMbkwxQ3B5NnZvSGM
Pregnancy and Infant Outcomes in the Clinical Trials of a Human Papillomavirus Type 6/11/16/18 Vaccine: A Combined Analysis of Five Randomized Controlled Trials: https://drive.google.com/file/d/0BwNFCLOriAMMRUpJa3RHN2ViSz
Sexual Activity–Related Outcomes After Human Papillomavirus Vaccination of 11- to 12-Year-Olds: https://drive.google.com/file/d/0BwNFCLOriAMMSDJSQ0hseUtFbms
This vaccine is a must, not only for young women but also young men.
Further information: http://conditions.health.qld.gov.au/HealthCondition/condition/14/217/80/Human-Papilloma-Virus-HPV
http://www.who.int/biologicals/areas/human_papillomavirus/en/
1 note
·
View note
Text
Should my son get the HPV vaccine?
Maya Kumar, MD, adolescent medicine specialist at UC San Diego Health answers:
“According to the Centers for Disease Control, 79 million Americans are infected with human papillomavirus (HPV), with 14 million new infections each year. Many people know about the association between HPV infection and cervical cancer in women. As a consequence, HPV has been dubbed a “woman’s infection.” However, approximately 40 percent of HPV-related cancers occur in men.
The most common HPV-related cancers in men are oropharyngeal cancers, such as mouth, tongue or laryngeal cancer. Women can get these too, but men are three times as likely as women to carry oral HPV. Rarer HPV-related cancers in men include penile cancer and anal cancer. HPV can also cause warts in the head and neck region (example: laryngeal warts affecting the voice box) and on the genitals. While these warts are not life-threatening, they significantly impact quality of life.
Parents have often heard that the virus is sexually transmitted and wonder why their child would need vaccination. Most STDs affect a small proportion of the population and can generally be avoided with safe sexual practices alone, making vaccination against these diseases on a large scale unnecessary. HPV is different. About 90 percent of all men and women will be infected with HPV at some point in their lives, even with safe sexual practices. Even if you only have one partner for your whole life, you can still get HPV and suffer its devastating consequences. HPV vaccination is the only dependable way to prevent it because it is almost impossible to avoid with lifestyle and behavioral decisions alone.

Parents may also wonder why it is necessary in childhood. Vaccines work best when they are given well before a person is exposed to a disease. The CDC recommends age 11-to-12 years old as the ideal time for vaccination. Recently, the CDC announced that if HPV vaccination is initiated before age 14, only two doses of the vaccine (at least six months apart) are required. If, however, vaccination begins at age 15 or older, three doses of the vaccine (at 0, 1-2 months and 6 months) are needed. This may be because the antibody response to the vaccine appears to be more robust in children 14 years and under, so fewer doses still provide sufficiently strong protection.
The HPV vaccine is an extremely safe vaccine. It contains no mercury, thimerosal or any other harmful preservatives. It also does not contain any live virus, or even any inactivated viral components that could cause infection. Because it is a completely synthetic vaccine, getting infected from it is impossible. As with any vaccine there are some risks. However, as of March 2016, almost 90 million doses of HPV vaccine had been distributed in the United States with no new long-term serious adverse effects identified.
On a personal note, I elected to be vaccinated against HPV when the vaccine became available years ago. I would have no hesitation vaccinating my own children or the children of my friends or relatives. So take it from someone who walks the walk: I strongly recommend the HPV vaccine for both your sons and your daughters.”
140 notes
·
View notes
Text
New Studies Suggest HPV Vaccines Could End Cervical Cancer
The HPV vaccine was introduced only in 2006 but it’s already making an impact. Gardasil was the first HPV vaccine to be launched, followed by other products like Cervarix. New studies today show that HPV vaccines have contributed to a reduction in cervical pre-cancer rates, regardless of the fact that immunisation programs don’t cover all girls and boys yet.
Cervical Pre-Cancer Reduction: The Latest Study
HPV vaccines prevent infections with the human papillomavirus (HPV) – the primary cause of cervical cancer.
HPV spreads through sexual contact and there are multiple viral strains. Two strains in particular – HPV types 16 and 18 – are responsible for causing 70 percent of all cervical cancer cases. Luckily, all of the available and approved vaccines right now target these viral strains, as well as other types of HPV that are responsible for causing genital warts.
A very important new study was carried out in the US to determine whether the introduction of HPV vaccines in 2006 has already contributed to a reduction in the incidence of cervical cancer. The results are more than optimistic.
While only 50 percent of adolescents in the US have received the vaccine, the incidence of cervical pre-cancer in the period from 2012 to 2016 went down 40 per cent in women aged 20 to 24.
What’s even more important – infections with HPV in teenage girls were massively reduced by 86 per cent.
This is the latest study but it’s not the only one establishing a link between HPV vaccination and a reduction in HPV infections/cervical pre-cancer rates.
Cervical Pre-Cancer Down 88% in a Decade
Countries that already have immunisation programmes have initiated research projects to assess the long-term effect of HPV vaccination on cervical cancer rates.
One of the most extensive studies comes from the UK.
The UK launched an HPV immunisation programme among adolescents in 2008. The programme targets girls aged 12 and 13. There’s also a catch-up programme for those who haven’t been vaccinated and who are up to 18-year-old.
Researchers followed the evolution of the programme over the course of a decade. They examined infection rates and cervical pre-cancer incidence in the period from 2008 to 2018. Their findings are similar to what researchers uncovered in the US.
The first group of women to go through the vaccination programme in 2008/2009 has seen an 88 per cent reduction in cervical pre-cancer rate. It’s also interesting to point out another finding – women born during these years who hadn’t receive the HPV vaccine yet were less likely to develop cervical pre-cancer. There’s a simple reason why. Vaccination reduces the risk of exposure and contributes to much higher safety even for those who have not been vaccinated yet.
Infections with high risk HPV strains were also reduced significantly as a result of the immunisation programme.
Because of these findings, medical professionals are optimistic that HPV vaccines could bring on the end of cervical cancer in the future.
According to researchers in Canada, infection rates with HPV types 16 and 18 are already down 83 per cent for teenage girls and 66 per cent for young women. In Canada, vaccination was introduced five to six years prior to the announcement of the findings.
Research suggests that the greatest benefits are observed in countries where at least 50 per cent of adolescents are vaccinated.
Health professionals also stress on the importance of getting boys vaccinated. When the HPV vaccine is administered among boys and men, it reduces the risk of infections and it also helps for some protection against the other types of cancer caused by HPV – penile, mouth and throat cancer.
HPV Vaccination in Singapore
HPV vaccines are readily available in Singapore.
You can choose the two types of Gardasil (the quadrivalent Gardasil that targets HPV 6, 11, 16 and 18, and Gardasil 9 that targets nine HPV strains) and Cervarix.
Typically, three doses have to be administered for optimal results.
It’s best for adolescents to get the vaccine before they become exposed to HPV. Young adults up to the age of 26 could also benefit. If you’re 26 or older, talk to your doctor or visit a facility like Shim Clinic where you’ll get more information about the appropriateness of the HPV vaccine for you.
According to statistics, 2,700 students have been vaccinated against HPV in Singapore so far. This is a part of a free vaccination programme that’s available to adolescent girls in 25 schools. The programme began in April 2019 and hopefully, its scope will increase in the future. The Health Promotion Board (HPB) aims to vaccinate 18,000 girls in 139 secondary schools by the end of the year.
In Singapore, 200 new cervical cancer cases are diagnosed each year. Around 70 women will die from this type of cancer on an annual basis.
The newest findings show just how promising HPV vaccines are. Chances are that such medical advances will help for the eradication of this cancer type in the near future.
If you’re older and you don’t qualify for the school vaccination programmes, get in touch with Shim Clinic. We offer consultations, STD testing and HPV vaccination following the approved guidelines. Relying on others to protect you is not the best option and you should definitely take charge of your reproductive health.
Original content here: https://www.shimclinic.com/blog/new-studies-suggest-hpv-vaccines-could-end-cervical-cancer
0 notes
Text
New TB Vaccine Could Save Millions of Lives, Study Suggests
In what may be a watershed moment in the fight against tuberculosis, the world’s most lethal infectious disease, an experimental new vaccine has protected about half the people who got it, scientists reported on Tuesday.
While a 50 percent success rate is hardly ideal — the measles vaccine, by contrast, is about 98 percent protective — about 10 million people get tuberculosis each year, and 1.6 million die of it. Even a partly effective vaccine may save millions of lives.
A year ago, when preliminary trial results of the new vaccine were released, the World Health Organization called it “a major scientific breakthrough.”
Researchers not involved in the vaccine’s development were enthusiastic about the latest results, but said it needed to be studied in more people and in different populations.
“The vaccine looks promising, and likely better than our century-old BCG vaccine,” said Dr. Mario C. Raviglione, a global health expert at the University of Milan who headed the W.H.O.’s global tuberculosis program from 2003 to 2017.
BCG, which is not used in the United States, protects infants against some types of tuberculosis, but does not protect adolescents or adults against the form that attacks the lungs, which is the most common type.
Tuberculosis patients suffer fevers and night sweats, lose weight, cough up blood and, if left treated, ultimately die. Five years ago, tuberculosis surpassed AIDS as the deadliest infectious disease worldwide.
The new vaccine, made by GSK and now known as M72/AS01E, was tested in about 3,300 adults in Kenya, South Africa and Zambia. All of them already had latent tuberculosis — a silent infection that might or might not progress to active tuberculosis.
Of those who got two doses of the GSK vaccine, only 13 developed active tuberculosis during three years of follow-up, according to the new study published in The New England Journal of Medicine. By contrast, 26 of those who got a placebo progressed to active tuberculosis.
Also, using antibiotics for prevention increases the risk that antibiotic-resistant TB will appear, while a vaccine does not.
Because so many people die of tuberculosis, Dr. Seth Berkley, chief executive of Gavi, the Vaccine Alliance, a public-private partnership that buys vaccines for poor countries, said his agency would “certainly give the vaccine a hard look.”
Gavi already supports some vaccines that are only partly effective, he noted. For example, some vaccines for human papillomavirus, or HPV, stop only 70 percent of the strains of the cancer-causing virus, and a new malaria vaccine being field-tested in Africa is only 39 percent effective.
An important question raised by the study, researchers said, is who should receive the vaccine.
Tuberculosis rates vary enormously not just between countries, but even from neighborhood to neighborhood. The disease thrives in people who live in crowded conditions, inhaling one another’s germs, and the bacterium dies quickly in sunlight.
Tuberculosis can be transmitted even through something as simple as a cough on a crowded bus. But the people at the highest risk include family members of patients with active tuberculosis, the doctors and nurses caring for them and, in countries where tuberculosis is common, people living or working in crowded conditions, such as prisoners and miners.
But in any country, people are also at risk of infection if they have H.I.V., are severely malnourished, are taking immune-suppressive cancer chemotherapy or organ-transplant drugs, have diabetes or are on dialysis.
The new study, however, tested the vaccine only in people who were H.I.V.-negative and whose blood tests showed they had latent tuberculosis.
[Like the Science Times page on Facebook. | Sign up for the Science Times newsletter.]
But at least a quarter of the world’s population would come up positive for latent tuberculosis on a blood or skin test. The result means only that they have been exposed to tuberculosis germs some time in the past.
“We have no idea if they have been infected last month or 20 years ago,” Dr. Raviglione said. Those infected long ago may have already have cleared their bodies of the infection.
Most people who are ever going to develop active tuberculosis do so within two years of their first infection. Therefore, some prominent researchers argue that latency tests greatly exaggerate the number of people at risk.
As a result, relying on them would cause many more people to be vaccinated than could benefit.
Dr. Lalita Ramakrishnan, a tuberculosis expert at the University of Cambridge in Britain, noted that participants in the vaccine study were less likely to develop active tuberculosis in the first year than in the second.
That result — the opposite of what would normally be expected, she said — implied that the careful screening done by the GSK team for the clinical trial, which included taking medical histories and sputum samples, must have weeded out people with early-stage tuberculosis.
To pick people who would benefit most from the vaccine under normal circumstances, she argued, a more accurate diagnostic test must be developed.
Alternatively, the vaccine could be restricted to people at obvious high risk, such as nurses in tuberculosis wards — but that would miss too many potential beneficiaries.
In the future, experts said, the GSK vaccine should be tested on people with H.I.V. and on people in other countries, because susceptibility to tuberculosis appears to vary widely.
The authors agreed, saying, “These results need confirmation in larger and longer studies conducted in a broader range of populations.”
Those groups should include people who did not test positive for latent tuberculosis, and people of varying ages and races.
It is not known whether genetic differences make some people more susceptible to tuberculosis, or whether the bacteria circulating in various countries vary in infectiousness.
Sahred From Source link Science
from WordPress http://bit.ly/2NhEXaS
via IFTTT
0 notes
Text
Federal experts’ advice on HPV vaccine could leave adults confused
Vaccination decisions are usually pretty straightforward. People either meet the criteria for the vaccine based on their age or other factors or they don’t. But when a federal panel recently recommended an update to the human papillomavirus (HPV) vaccine guidelines, it left a lot of uncertainty.
The panel recommended that men and women between ages 27 and 45 decide — in discussion with their health care providers — whether the HPV vaccine makes sense for them.
But some public health advocates criticize that advice because it doesn’t provide doctors and patients clear guidance about who in this expansive age group are good candidates. They worry that many people may get immunized who won’t benefit, adding needless cost to the health care system and possibly shortchanging people overseas, where the vaccine is in short supply.
“My concern is that there will be a whole lot of people or doctors recommending this vaccine,” said Debbie Saslow, managing director of HPV and gynecological cancers for the American Cancer Society. “But I think that the benefit is so small and we just don’t have guidance.”
The human papillomavirus is the most common sexually transmitted infectionin the United States; nearly everyone who’s sexually active will get it at some point. People typically clear the virus on their own and often don’t even realize they’ve been infected. But in some people, HPV remains in the body and may cause several types of cancer as well as genital warts.
Every year, HPV causes more than 33,000 cancers, including more than 90% of cervical cancers as well as cancers of the vagina, vulva, penis, anus and the area at the back of the throat called the oropharynx, according to the Centers for Disease Control and Prevention.
More than 40 types of HPV affect the genital area. Merck’s Gardasil 9, the vaccine used in the United States, provides protection against nine types, which together are associated with the majority of HPV-related cancers and cause 90% of genital warts.
Because HPV is so common among people who are sexually active, the best time to vaccinate is before people start having sex and risk being exposed to the virus. The CDC’s Advisory Committee on Immunization Practices recommends HPV vaccination for all 11- and 12-year-old girls and boys. Catch-up immunizations for young people outside that age window are recommended through age 21 for men and 26 for women (the proposed HPV vaccine update would change the catch-up vaccination guideline for men to align it with the age-26 cutoff for women).
In its June meeting, the immunization committee, which includes public health experts, recommended widening the vaccination window to include adults between 27 and 45.
But rather than give the thumbs-up for everyone in that age group, the panel said people should engage in “shared clinical decision-making” with their health care professional to decide if the vaccine is right for them.
“ACIP made this type of recommendation because most people in this age group are not likely to benefit from getting the vaccine,” Kristen Nordlund, a spokeswoman for the CDC, wrote in an email.
The vaccine won’t protect people against types of HPV to which they’ve already been exposed, and many sexually active people have been exposed to at least some HPV types by their late 20s.
That makes it tougher for the vaccine to have an impact in this age group. According to an economic modeling study presented at the ACIP meeting, under current guidelines that recommend immunization through age 26, 202 people would have to be vaccinated to prevent one case of HPV-related cancer. When the recommendations are broadened to include people through age 45, the number that would have to be vaccinated to prevent one case of cancer increases exponentially to 6,500.
However, it’s unlikely that people in the older group have been exposed to all nine types of HPV the vaccine protects against.
“There’s some sense that you can get some protection against some future cancers,” said Dr. William Schaffner, professor of preventive medicine and infectious diseases at Vanderbilt University School of Medicine, who is the ACIP liaison for the National Foundation for Infectious Diseases.
Yet, patients — and their doctors — would be hard pressed to know if immunization would be beneficial.
“The problem is that no individual person is likely to know which individual type of HPV they’ve been exposed to,” said Dr. Christopher Zahn, vice president of practice activities at the American College of Obstetricians and Gynecologists.
Vaccine experts have some suggestions about which people older than 26 might consider getting the three-shot series. They include people with multiple sex partners and those who are newly single and dating after being in a monogamous marriage or relationship.
Jennifer Sienko is in a better position than most people to evaluate whether to get the vaccine. She is co-director of the National HPV Vaccination Roundtable, a coalition of groups aimed at reducing HPV cancers that is hosted by the American Cancer Society.
But she was recently surprised when a new doctor asked the 40-year-old if she wanted the vaccine. She opted against it.
Sienko, who lives in Chicago, has been married to her second husband for three years, and that contributed to her decision. But perhaps, she said, it would have been different when she was single for a time.
“So there may have been a window where, had the vaccine been indicated for older women, perhaps between my marriages I would have looked into that,” she said.
The CDC is reviewing the ACIP recommendation. If it approves the recommendation, experts hope the CDC will provide further guidance on determining who the vaccine is appropriate for.
If the CDC approves broadening the age for the vaccine in consultation with a health care provider, most insurers would cover the costs, which can run a few hundred dollars per dose. Under the Affordable Care Act’s preventive coverage rules, patients generally won’t have to pay anything out of pocket for it.
The post Federal experts’ advice on HPV vaccine could leave adults confused appeared first on HviRAL.
from WordPress https://ift.tt/2KCP2hj
0 notes
Text
Another Unaccounted Expense of the Flu Vaccine
Any time you undergo a medical procedure, including vaccination, there is a risk of side effects, ranging from mild to severe. This is particularly important to remember if you’re receiving the procedure outside of a medical space, such as is the case with an increasing number of vaccinations.
Influenza vaccines, commonly referred to as flu shots, are available in the U.S. at drug stores, grocery stores and workplaces. Should you choose to receive a flu shot at your office, for instance, and an adverse reaction occurs, there will be no medical staff on hand to come to your aid. Instead, you’ll be at the mercy of whoever is nearby to provide help, which will typically be to call 911.
This is precisely what happened to Matt Gleason, a healthy 30-something from North Carolina who received a flu shot at his workplace, then fainted five minutes later.
Man Faints After Flu Shot, Gets Hospital Bill for Thousands of Dollars
The flu shot offered at Gleason’s workplace in October 2018 was free, but the medical bills he racked up as a result were far from it. Gleason, who has a history of fainting but otherwise is in good health, fainted after receiving the flu shot. He came to quickly but his colleagues called 911 just in case.
When paramedics arrived, Gleason began vomiting, prompting them to transport him to a nearby hospital by ambulance. There he spent eight hours in the emergency room — primarily in the waiting area — where he spoke to a doctor via teleconference and received an electrocardiogram, chest X-ray and blood and urine tests.
Everything came back normal and Gleason was allowed to go home with a clean bill of health — and a steep ER bill too match.
As reported by NPR, Gleason’s total bill was as follows, “$4,692 for all the hospital care, including $2,961 for the ER admission fee, $400 for an EKG, $348 for a chest X-ray, $83 for a urinalysis and nearly $1,000 for various blood tests. Gleason’s insurer … negotiated discounts for the in-network hospital and reduced those costs to $3,711.”1
This is a cautionary tale not only for vaccination side effects but also the exorbitant costs of medical care in the U.S. Hospitals often use criteria for emergency room billing that’s based on a level system from 1 to 6, with 1 being the lowest level of care and 6 being critical care, such as a gunshot wound or major injuries from a car accident.
Gleason’s fainting episode was coded at level 5 — the second most expensive. While he argued that a lower level fee should have been charged, especially with the amount of time he spent in the waiting room, the hospital backed up its charge because he received at least three medical tests. According to NPR:2
“David McKenzie, reimbursement director at the American College of Emergency Physicians, said the guidelines were set up to help hospitals charge appropriately.
Asked if hospitals have an incentive to perform extra tests to get patients to a higher-cost billing code, McKenzie said: ‘It’s not a perfect system. Hospitals have an incentive to do a CT exam, and taxi drivers have an incentive to take the long way home.’”
How Common Is Fainting After Vaccination?
Fainting, medically known as syncope, is the temporary loss of consciousness as a result of decreased blood flow to the brain — and it’s quite common after vaccination.
According to the U.S. Centers for Disease Control and Prevention (CDC), fainting has been reported following nearly all vaccines, and the federal vaccine adverse event reporting system (VAERS) receives many reports of fainting following vaccination every year, with many more cases likely going unreported.3
Adolescents appear to be particularly at risk of fainting following vaccination, although the CDC doesn’t know why. More than half (62 percent) of fainting episodes following vaccination reported to VAERS involved adolescents 11 to 18 years old.4 Among this age group, fainting occurs most often following these three vaccines: HPV, MCV5 (meningococcal vaccine) and Tdap.
“Because the ingredients of these three vaccines are different, yet fainting is seen with all of them, scientists think that fainting is due to the vaccination process and not to the vaccines themselves,” according to the CDC. “However, there is not yet a definite answer about whether an ingredient of the vaccines is responsible for the fainting or if adolescents are simply more likely than children or adults to experience fainting.”5
While fainting itself is rarely serious, and most people regain consciousness and recover quickly, it can lead to fall-related injuries that can cause significant injury. In fact, the journal Vaccine lists fall-related injuries associated with fainting after vaccinations as one of the “rare cases where a known or plausible theoretical risk of death following vaccination exists.”6
A CDC report described one case study of a 13-year-old girl who fainted within 10 minutes of receiving HPV and MCV4 vaccinations. “She fell backward and hit her head on the carpeted floor of the clinic. The girl was admitted to the pediatric intensive-care unit because of skull fractures and subarachnoid hemorrhage.”7
Fainting-Related Falls After Vaccination Can Be Fatal
The girl recovered, but in another case reported in the Archives of Pediatrics and Adolescent Medicine, the child was not so lucky. The boy, who was 15 years old with no known medical problems, fainted several minutes after receiving the third dose of hepatitis B vaccine. He fell backward onto a concrete floor covered by a thin carpet, striking the back of his head.
He regained consciousness but had convulsions, went into cardiopulmonary arrest and died. An autopsy revealed he suffered from traumatic brain injury, including frontal lobe contusions, along with brain swelling and bleeding, even though he had no skull fracture.8 According to one study of vaccine-related fainting reported to VAERS, 7 percent of the reports were serious and 12 percent involved head injuries.
The CDC recommends that vaccine providers follow their Advisory Committee on Immunization Practices (ACIP) guidance, which suggests observing patients for 15 minutes after vaccination to prevent fainting-related injuries.9 However, it’s unclear how often this is actually done, not only in doctors’ offices but also in workplaces where vaccines are administered.
The CDC reported that nearly 70 percent of vaccine-related fainting episodes occurred within 15 minutes of vaccination, but this still means that 30 percent occurred after this timeframe — by which time a person could be in their car and driving, walking down stairs or engaging in a multitude of other activities that would pose a threat to themselves and others should fainting occur.10
They reported at least one case of a vehicle accident that occurred because the patient lost consciousness while driving. The problem is so widespread that the U.S. Food and Drug Administration (FDA) states the following in their information about Gardasil, an HPV vaccine:11
“Fainting is common after injections and vaccinations, especially in adolescents. Falls after syncope may sometimes cause serious injuries, such as head injuries, which can be prevented with simple steps, such as keeping the vaccinated person seated for up to 15 minutes after vaccination.
FDA and CDC have taken steps to remind immunization providers about the recommendation that individuals be watched carefully for 15 minutes after vaccination to avoid potential injury from a fall.
FDA approved revised labeling on June 9, 2009, to highlight this information in the Warnings and Precautions section, and new information was added noting that individuals who faint sometimes have tonic-clonic (jerking) movements and seizure-like activity.
As a part of a Back to School immunization campaign, FDA and CDC are also continuing to remind health care providers to take measures to prevent fainting and the possible traumatic injury resulting from fainting.”
What Other Adverse Events May Occur Following a Flu Vaccine?
Aside from fainting, flu vaccine most commonly causes fever, joint pain, muscle aches, nausea and headaches. It may also be associated with Guillain-Barre Syndrome (GBS), an autoimmune disease that can cause paralysis. Not only are vaccine injury claims related to the influenza vaccine the most common type submitted to VICP, but GBS is the leading injury in the claims.12
“Some studies have found a possible small association of injectable flu vaccine with Guillain-Barré syndrome (GBS),” the CDC notes. “Overall, these studies estimated the risk for GBS after vaccination as fewer than 1 or 2 cases of GBS per 1 million people vaccinated.”13 The National Vaccine Information Center (NVIC) further describes GBS as:14
“An immune mediated painful and disabling neurological disorder that can occur after viral infection or vaccination, GBS involves inflammation of the peripheral nervous system and can cause temporary or permanent paralysis that may lead to death. GBS usually develops within two to four weeks of vaccination.
Characterized by muscle weakness, unsteady gait, numbness, tingling, pain, GBS can cause paralysis of the face or one or more limbs. It can take several months for recovery or leave the affected person with chronic health problems and disability.”
Shoulder injury related to vaccine administration, or SIRVA, is another risk. A vaccine given in your shoulder is intended to go into your muscle. If it mistakenly goes into the bursa, a fluid-filled sac that protects your shoulder tendons, trouble can result. Specifically, the vaccine may provoke your immune system to attack the bursa, sometimes leading to debilitating symptoms.
In adults, SIRVA occurs most often after flu shots and other vaccines that a person has already received, which may pave the way for a heightened inflammatory response.15 GBS and SIRVA were both added to the Vaccine Injury Table in 2017.
By adding those vaccine complications to the table, vaccine-related GBS and SIRVA cases brought before the “Vaccine Court” in the U.S. Court of Federal Claims in Washington, D.C., will be more likely to receive federal vaccine injury compensation.
Flu vaccination during early pregnancy has also been linked in one study to an eightfold increased risk of miscarriage, particularly among women who had been vaccinated for the flu in the previous flu season as well.16
Flu vaccination may also increase your risk of contracting more serious flu infections, as research suggests those who have been vaccinated annually may be less protected than those with no prior flu vaccination history.17
Do the Benefits Outweigh the Risks?
The important question to ask, then, before choosing to receive a flu shot (or any other medical procedure) is whether or not the benefits outweigh the risks. In the case of the flu vaccine, the risk of adverse events — and their associated medical costs — is real. But what about its purported benefit — reducing your risk of the flu?
Be aware that in the decade between 2005 and 2015, the influenza vaccine was less than 50 percent effective more than half of the time.18 The 2017/2018 flu vaccine was another example of this less-than-impressive trend. The overall adjusted vaccine effectiveness against influenza A and B virus infection was just 36 percent.19
Fortunately, other methods exist to help you stay healthy during the flu season and all year, and they’re far safer than annual flu vaccination. Vitamin D testing and optimization have been shown to cut your risk of respiratory infections, including colds and flu, in half if you are vitamin D deficient, for instance.20,21
In my view, optimizing your vitamin D levels is one of the absolute best respiratory illness prevention and optimal health strategies available, and when combined with a healthy lifestyle represents one of the safest and most effective ways to stay healthy year-round.
from Articles http://articles.mercola.com/sites/articles/archive/2019/02/09/fainting-after-flu-shot.aspx
source https://niapurenaturecom.tumblr.com/post/182675218141
0 notes
Text
Another Unaccounted Expense of the Flu Vaccine
Any time you undergo a medical procedure, including vaccination, there is a risk of side effects, ranging from mild to severe. This is particularly important to remember if you’re receiving the procedure outside of a medical space, such as is the case with an increasing number of vaccinations.
Influenza vaccines, commonly referred to as flu shots, are available in the U.S. at drug stores, grocery stores and workplaces. Should you choose to receive a flu shot at your office, for instance, and an adverse reaction occurs, there will be no medical staff on hand to come to your aid. Instead, you’ll be at the mercy of whoever is nearby to provide help, which will typically be to call 911.
This is precisely what happened to Matt Gleason, a healthy 30-something from North Carolina who received a flu shot at his workplace, then fainted five minutes later.
Man Faints After Flu Shot, Gets Hospital Bill for Thousands of Dollars
The flu shot offered at Gleason’s workplace in October 2018 was free, but the medical bills he racked up as a result were far from it. Gleason, who has a history of fainting but otherwise is in good health, fainted after receiving the flu shot. He came to quickly but his colleagues called 911 just in case.
When paramedics arrived, Gleason began vomiting, prompting them to transport him to a nearby hospital by ambulance. There he spent eight hours in the emergency room — primarily in the waiting area — where he spoke to a doctor via teleconference and received an electrocardiogram, chest X-ray and blood and urine tests.
Everything came back normal and Gleason was allowed to go home with a clean bill of health — and a steep ER bill too match.
As reported by NPR, Gleason’s total bill was as follows, “$4,692 for all the hospital care, including $2,961 for the ER admission fee, $400 for an EKG, $348 for a chest X-ray, $83 for a urinalysis and nearly $1,000 for various blood tests. Gleason's insurer … negotiated discounts for the in-network hospital and reduced those costs to $3,711.”1
This is a cautionary tale not only for vaccination side effects but also the exorbitant costs of medical care in the U.S. Hospitals often use criteria for emergency room billing that’s based on a level system from 1 to 6, with 1 being the lowest level of care and 6 being critical care, such as a gunshot wound or major injuries from a car accident.
Gleason’s fainting episode was coded at level 5 — the second most expensive. While he argued that a lower level fee should have been charged, especially with the amount of time he spent in the waiting room, the hospital backed up its charge because he received at least three medical tests. According to NPR:2
“David McKenzie, reimbursement director at the American College of Emergency Physicians, said the guidelines were set up to help hospitals charge appropriately.
Asked if hospitals have an incentive to perform extra tests to get patients to a higher-cost billing code, McKenzie said: ‘It's not a perfect system. Hospitals have an incentive to do a CT exam, and taxi drivers have an incentive to take the long way home.’”
How Common Is Fainting After Vaccination?
Fainting, medically known as syncope, is the temporary loss of consciousness as a result of decreased blood flow to the brain — and it’s quite common after vaccination.
According to the U.S. Centers for Disease Control and Prevention (CDC), fainting has been reported following nearly all vaccines, and the federal vaccine adverse event reporting system (VAERS) receives many reports of fainting following vaccination every year, with many more cases likely going unreported.3
Adolescents appear to be particularly at risk of fainting following vaccination, although the CDC doesn’t know why. More than half (62 percent) of fainting episodes following vaccination reported to VAERS involved adolescents 11 to 18 years old.4 Among this age group, fainting occurs most often following these three vaccines: HPV, MCV5 (meningococcal vaccine) and Tdap.
“Because the ingredients of these three vaccines are different, yet fainting is seen with all of them, scientists think that fainting is due to the vaccination process and not to the vaccines themselves,” according to the CDC. “However, there is not yet a definite answer about whether an ingredient of the vaccines is responsible for the fainting or if adolescents are simply more likely than children or adults to experience fainting.”5
While fainting itself is rarely serious, and most people regain consciousness and recover quickly, it can lead to fall-related injuries that can cause significant injury. In fact, the journal Vaccine lists fall-related injuries associated with fainting after vaccinations as one of the “rare cases where a known or plausible theoretical risk of death following vaccination exists.”6
A CDC report described one case study of a 13-year-old girl who fainted within 10 minutes of receiving HPV and MCV4 vaccinations. “She fell backward and hit her head on the carpeted floor of the clinic. The girl was admitted to the pediatric intensive-care unit because of skull fractures and subarachnoid hemorrhage.”7
Fainting-Related Falls After Vaccination Can Be Fatal
The girl recovered, but in another case reported in the Archives of Pediatrics and Adolescent Medicine, the child was not so lucky. The boy, who was 15 years old with no known medical problems, fainted several minutes after receiving the third dose of hepatitis B vaccine. He fell backward onto a concrete floor covered by a thin carpet, striking the back of his head.
He regained consciousness but had convulsions, went into cardiopulmonary arrest and died. An autopsy revealed he suffered from traumatic brain injury, including frontal lobe contusions, along with brain swelling and bleeding, even though he had no skull fracture.8 According to one study of vaccine-related fainting reported to VAERS, 7 percent of the reports were serious and 12 percent involved head injuries.
The CDC recommends that vaccine providers follow their Advisory Committee on Immunization Practices (ACIP) guidance, which suggests observing patients for 15 minutes after vaccination to prevent fainting-related injuries.9 However, it’s unclear how often this is actually done, not only in doctors’ offices but also in workplaces where vaccines are administered.
The CDC reported that nearly 70 percent of vaccine-related fainting episodes occurred within 15 minutes of vaccination, but this still means that 30 percent occurred after this timeframe — by which time a person could be in their car and driving, walking down stairs or engaging in a multitude of other activities that would pose a threat to themselves and others should fainting occur.10
They reported at least one case of a vehicle accident that occurred because the patient lost consciousness while driving. The problem is so widespread that the U.S. Food and Drug Administration (FDA) states the following in their information about Gardasil, an HPV vaccine:11
“Fainting is common after injections and vaccinations, especially in adolescents. Falls after syncope may sometimes cause serious injuries, such as head injuries, which can be prevented with simple steps, such as keeping the vaccinated person seated for up to 15 minutes after vaccination.
FDA and CDC have taken steps to remind immunization providers about the recommendation that individuals be watched carefully for 15 minutes after vaccination to avoid potential injury from a fall.
FDA approved revised labeling on June 9, 2009, to highlight this information in the Warnings and Precautions section, and new information was added noting that individuals who faint sometimes have tonic-clonic (jerking) movements and seizure-like activity.
As a part of a Back to School immunization campaign, FDA and CDC are also continuing to remind health care providers to take measures to prevent fainting and the possible traumatic injury resulting from fainting.”
What Other Adverse Events May Occur Following a Flu Vaccine?
Aside from fainting, flu vaccine most commonly causes fever, joint pain, muscle aches, nausea and headaches. It may also be associated with Guillain-Barre Syndrome (GBS), an autoimmune disease that can cause paralysis. Not only are vaccine injury claims related to the influenza vaccine the most common type submitted to VICP, but GBS is the leading injury in the claims.12
“Some studies have found a possible small association of injectable flu vaccine with Guillain-Barré syndrome (GBS),” the CDC notes. “Overall, these studies estimated the risk for GBS after vaccination as fewer than 1 or 2 cases of GBS per 1 million people vaccinated.”13 The National Vaccine Information Center (NVIC) further describes GBS as:14
“An immune mediated painful and disabling neurological disorder that can occur after viral infection or vaccination, GBS involves inflammation of the peripheral nervous system and can cause temporary or permanent paralysis that may lead to death. GBS usually develops within two to four weeks of vaccination.
Characterized by muscle weakness, unsteady gait, numbness, tingling, pain, GBS can cause paralysis of the face or one or more limbs. It can take several months for recovery or leave the affected person with chronic health problems and disability.”
Shoulder injury related to vaccine administration, or SIRVA, is another risk. A vaccine given in your shoulder is intended to go into your muscle. If it mistakenly goes into the bursa, a fluid-filled sac that protects your shoulder tendons, trouble can result. Specifically, the vaccine may provoke your immune system to attack the bursa, sometimes leading to debilitating symptoms.
In adults, SIRVA occurs most often after flu shots and other vaccines that a person has already received, which may pave the way for a heightened inflammatory response.15 GBS and SIRVA were both added to the Vaccine Injury Table in 2017.
By adding those vaccine complications to the table, vaccine-related GBS and SIRVA cases brought before the "Vaccine Court" in the U.S. Court of Federal Claims in Washington, D.C., will be more likely to receive federal vaccine injury compensation.
Flu vaccination during early pregnancy has also been linked in one study to an eightfold increased risk of miscarriage, particularly among women who had been vaccinated for the flu in the previous flu season as well.16
Flu vaccination may also increase your risk of contracting more serious flu infections, as research suggests those who have been vaccinated annually may be less protected than those with no prior flu vaccination history.17
Do the Benefits Outweigh the Risks?
The important question to ask, then, before choosing to receive a flu shot (or any other medical procedure) is whether or not the benefits outweigh the risks. In the case of the flu vaccine, the risk of adverse events — and their associated medical costs — is real. But what about its purported benefit — reducing your risk of the flu?
Be aware that in the decade between 2005 and 2015, the influenza vaccine was less than 50 percent effective more than half of the time.18 The 2017/2018 flu vaccine was another example of this less-than-impressive trend. The overall adjusted vaccine effectiveness against influenza A and B virus infection was just 36 percent.19
Fortunately, other methods exist to help you stay healthy during the flu season and all year, and they’re far safer than annual flu vaccination. Vitamin D testing and optimization have been shown to cut your risk of respiratory infections, including colds and flu, in half if you are vitamin D deficient, for instance.20,21
In my view, optimizing your vitamin D levels is one of the absolute best respiratory illness prevention and optimal health strategies available, and when combined with a healthy lifestyle represents one of the safest and most effective ways to stay healthy year-round.
from
http://articles.mercola.com/sites/articles/archive/2019/02/09/fainting-after-flu-shot.aspx
source http://niapurenaturecom.weebly.com/blog/another-unaccounted-expense-of-the-flu-vaccine
0 notes
Text
Another Unaccounted Expense of the Flu Vaccine
Any time you undergo a medical procedure, including vaccination, there is a risk of side effects, ranging from mild to severe. This is particularly important to remember if you’re receiving the procedure outside of a medical space, such as is the case with an increasing number of vaccinations.
Influenza vaccines, commonly referred to as flu shots, are available in the U.S. at drug stores, grocery stores and workplaces. Should you choose to receive a flu shot at your office, for instance, and an adverse reaction occurs, there will be no medical staff on hand to come to your aid. Instead, you’ll be at the mercy of whoever is nearby to provide help, which will typically be to call 911.
This is precisely what happened to Matt Gleason, a healthy 30-something from North Carolina who received a flu shot at his workplace, then fainted five minutes later.
Man Faints After Flu Shot, Gets Hospital Bill for Thousands of Dollars
The flu shot offered at Gleason’s workplace in October 2018 was free, but the medical bills he racked up as a result were far from it. Gleason, who has a history of fainting but otherwise is in good health, fainted after receiving the flu shot. He came to quickly but his colleagues called 911 just in case.
When paramedics arrived, Gleason began vomiting, prompting them to transport him to a nearby hospital by ambulance. There he spent eight hours in the emergency room — primarily in the waiting area — where he spoke to a doctor via teleconference and received an electrocardiogram, chest X-ray and blood and urine tests.
Everything came back normal and Gleason was allowed to go home with a clean bill of health — and a steep ER bill too match.
As reported by NPR, Gleason’s total bill was as follows, “$4,692 for all the hospital care, including $2,961 for the ER admission fee, $400 for an EKG, $348 for a chest X-ray, $83 for a urinalysis and nearly $1,000 for various blood tests. Gleason's insurer … negotiated discounts for the in-network hospital and reduced those costs to $3,711.”1
This is a cautionary tale not only for vaccination side effects but also the exorbitant costs of medical care in the U.S. Hospitals often use criteria for emergency room billing that’s based on a level system from 1 to 6, with 1 being the lowest level of care and 6 being critical care, such as a gunshot wound or major injuries from a car accident.
Gleason’s fainting episode was coded at level 5 — the second most expensive. While he argued that a lower level fee should have been charged, especially with the amount of time he spent in the waiting room, the hospital backed up its charge because he received at least three medical tests. According to NPR:2
“David McKenzie, reimbursement director at the American College of Emergency Physicians, said the guidelines were set up to help hospitals charge appropriately.
Asked if hospitals have an incentive to perform extra tests to get patients to a higher-cost billing code, McKenzie said: ‘It's not a perfect system. Hospitals have an incentive to do a CT exam, and taxi drivers have an incentive to take the long way home.’”
How Common Is Fainting After Vaccination?
Fainting, medically known as syncope, is the temporary loss of consciousness as a result of decreased blood flow to the brain — and it’s quite common after vaccination.
According to the U.S. Centers for Disease Control and Prevention (CDC), fainting has been reported following nearly all vaccines, and the federal vaccine adverse event reporting system (VAERS) receives many reports of fainting following vaccination every year, with many more cases likely going unreported.3
Adolescents appear to be particularly at risk of fainting following vaccination, although the CDC doesn’t know why. More than half (62 percent) of fainting episodes following vaccination reported to VAERS involved adolescents 11 to 18 years old.4 Among this age group, fainting occurs most often following these three vaccines: HPV, MCV5 (meningococcal vaccine) and Tdap.
“Because the ingredients of these three vaccines are different, yet fainting is seen with all of them, scientists think that fainting is due to the vaccination process and not to the vaccines themselves,” according to the CDC. “However, there is not yet a definite answer about whether an ingredient of the vaccines is responsible for the fainting or if adolescents are simply more likely than children or adults to experience fainting.”5
While fainting itself is rarely serious, and most people regain consciousness and recover quickly, it can lead to fall-related injuries that can cause significant injury. In fact, the journal Vaccine lists fall-related injuries associated with fainting after vaccinations as one of the “rare cases where a known or plausible theoretical risk of death following vaccination exists.”6
A CDC report described one case study of a 13-year-old girl who fainted within 10 minutes of receiving HPV and MCV4 vaccinations. “She fell backward and hit her head on the carpeted floor of the clinic. The girl was admitted to the pediatric intensive-care unit because of skull fractures and subarachnoid hemorrhage.”7
Fainting-Related Falls After Vaccination Can Be Fatal
The girl recovered, but in another case reported in the Archives of Pediatrics and Adolescent Medicine, the child was not so lucky. The boy, who was 15 years old with no known medical problems, fainted several minutes after receiving the third dose of hepatitis B vaccine. He fell backward onto a concrete floor covered by a thin carpet, striking the back of his head.
He regained consciousness but had convulsions, went into cardiopulmonary arrest and died. An autopsy revealed he suffered from traumatic brain injury, including frontal lobe contusions, along with brain swelling and bleeding, even though he had no skull fracture.8 According to one study of vaccine-related fainting reported to VAERS, 7 percent of the reports were serious and 12 percent involved head injuries.
The CDC recommends that vaccine providers follow their Advisory Committee on Immunization Practices (ACIP) guidance, which suggests observing patients for 15 minutes after vaccination to prevent fainting-related injuries.9 However, it’s unclear how often this is actually done, not only in doctors’ offices but also in workplaces where vaccines are administered.
The CDC reported that nearly 70 percent of vaccine-related fainting episodes occurred within 15 minutes of vaccination, but this still means that 30 percent occurred after this timeframe — by which time a person could be in their car and driving, walking down stairs or engaging in a multitude of other activities that would pose a threat to themselves and others should fainting occur.10
They reported at least one case of a vehicle accident that occurred because the patient lost consciousness while driving. The problem is so widespread that the U.S. Food and Drug Administration (FDA) states the following in their information about Gardasil, an HPV vaccine:11
“Fainting is common after injections and vaccinations, especially in adolescents. Falls after syncope may sometimes cause serious injuries, such as head injuries, which can be prevented with simple steps, such as keeping the vaccinated person seated for up to 15 minutes after vaccination.
FDA and CDC have taken steps to remind immunization providers about the recommendation that individuals be watched carefully for 15 minutes after vaccination to avoid potential injury from a fall.
FDA approved revised labeling on June 9, 2009, to highlight this information in the Warnings and Precautions section, and new information was added noting that individuals who faint sometimes have tonic-clonic (jerking) movements and seizure-like activity.
As a part of a Back to School immunization campaign, FDA and CDC are also continuing to remind health care providers to take measures to prevent fainting and the possible traumatic injury resulting from fainting.”
What Other Adverse Events May Occur Following a Flu Vaccine?
Aside from fainting, flu vaccine most commonly causes fever, joint pain, muscle aches, nausea and headaches. It may also be associated with Guillain-Barre Syndrome (GBS), an autoimmune disease that can cause paralysis. Not only are vaccine injury claims related to the influenza vaccine the most common type submitted to VICP, but GBS is the leading injury in the claims.12
“Some studies have found a possible small association of injectable flu vaccine with Guillain-Barré syndrome (GBS),” the CDC notes. “Overall, these studies estimated the risk for GBS after vaccination as fewer than 1 or 2 cases of GBS per 1 million people vaccinated.”13 The National Vaccine Information Center (NVIC) further describes GBS as:14
“An immune mediated painful and disabling neurological disorder that can occur after viral infection or vaccination, GBS involves inflammation of the peripheral nervous system and can cause temporary or permanent paralysis that may lead to death. GBS usually develops within two to four weeks of vaccination.
Characterized by muscle weakness, unsteady gait, numbness, tingling, pain, GBS can cause paralysis of the face or one or more limbs. It can take several months for recovery or leave the affected person with chronic health problems and disability.”
Shoulder injury related to vaccine administration, or SIRVA, is another risk. A vaccine given in your shoulder is intended to go into your muscle. If it mistakenly goes into the bursa, a fluid-filled sac that protects your shoulder tendons, trouble can result. Specifically, the vaccine may provoke your immune system to attack the bursa, sometimes leading to debilitating symptoms.
In adults, SIRVA occurs most often after flu shots and other vaccines that a person has already received, which may pave the way for a heightened inflammatory response.15 GBS and SIRVA were both added to the Vaccine Injury Table in 2017.
By adding those vaccine complications to the table, vaccine-related GBS and SIRVA cases brought before the "Vaccine Court" in the U.S. Court of Federal Claims in Washington, D.C., will be more likely to receive federal vaccine injury compensation.
Flu vaccination during early pregnancy has also been linked in one study to an eightfold increased risk of miscarriage, particularly among women who had been vaccinated for the flu in the previous flu season as well.16
Flu vaccination may also increase your risk of contracting more serious flu infections, as research suggests those who have been vaccinated annually may be less protected than those with no prior flu vaccination history.17
Do the Benefits Outweigh the Risks?
The important question to ask, then, before choosing to receive a flu shot (or any other medical procedure) is whether or not the benefits outweigh the risks. In the case of the flu vaccine, the risk of adverse events — and their associated medical costs — is real. But what about its purported benefit — reducing your risk of the flu?
Be aware that in the decade between 2005 and 2015, the influenza vaccine was less than 50 percent effective more than half of the time.18 The 2017/2018 flu vaccine was another example of this less-than-impressive trend. The overall adjusted vaccine effectiveness against influenza A and B virus infection was just 36 percent.19
Fortunately, other methods exist to help you stay healthy during the flu season and all year, and they’re far safer than annual flu vaccination. Vitamin D testing and optimization have been shown to cut your risk of respiratory infections, including colds and flu, in half if you are vitamin D deficient, for instance.20,21
In my view, optimizing your vitamin D levels is one of the absolute best respiratory illness prevention and optimal health strategies available, and when combined with a healthy lifestyle represents one of the safest and most effective ways to stay healthy year-round.
from HealthyLife via Jake Glover on Inoreader http://articles.mercola.com/sites/articles/archive/2019/02/09/fainting-after-flu-shot.aspx
0 notes
Text
Human papillomavirus genotype distribution and socio-behavioural characteristics in women with cervical pre-cancer and cancer at the start of a human papillomavirus vaccination programme: the CIN3+ plus study
Abstract
Background
The Swiss Federal Office of Public Health has recommended vaccination against human papillomavirus (HPV) to prevent cervical cancer since 2008. To establish monitoring of the future public health impact of vaccination, baseline population-based data are required. The objectives of this study were to examine the distribution of oncogenic HPV genotypes in biopsies with cervical intraepithelial neoplasia stage 3 or more severe lesions (CIN3+) at the beginning of HPV vaccination programmes and to compare sociodemographic and behavioural factors of women with CIN3+ with women in the Swiss general population.
Methods
We conducted a retrospective and prospective cross-sectional study with women diagnosed with CIN3+ in Switzerland. Ten pathology institutes from six cantons and three language regions participated. We conducted HPV typing on formaldehyde fixed-paraffin embedded specimens from 2014 and 2015. Women enrolled in 2015 were asked to complete a questionnaire. We described frequencies of HPV types. We also compared demographic characteristics and socioeconomic status in the CIN3 + plus group with the Swiss National Cohort in 2014 and compared risk factors for HPV infection with the Swiss Health Survey in 2012.
Results
We included 768 biopsies from 767 women. Four hundred and seventy-five (61.8%) biopsies were positive for HPV 16 and/or 18, 687 (89.5%) were positive for oncogenic HPV genotypes 16, 18, 31, 33, 45, 52, and/or 58 and five (0.7%) were HPV negative. Twenty-eight (10.3%) of the 273 women who completed the patient questionnaire reported having received at least one dose of an HPV vaccine. When compared with Swiss women in the six study cantons, fewer women in the CIN3+ plus study group were of Swiss nationality, more were born abroad and more were single. The study group also had a higher proportion of women with ≥2 partners in the last year, current smokers and was younger at age of first sexual intercourse.
Conclusions
Introduction of the nonavalent vaccine could cover approximately 90% of CIN3+ lesions in Swiss women compared with around 60% with the quadrivalent vaccine. Surveillance of HPV genotype distribution in CIN3+, together with information about vaccination and CIN3+ incidence will allow monitoring of the public health impact of vaccination programmes.
Trial Registration
ClinicalTrials.gov, NCT02323997. Registered 24 December 2014.
http://bit.ly/2Ur9gxO
0 notes
Text
China researchers make cancer vaccine breakthrough
Chinese researchers have taken a major step forward in developing a new-generation vaccine that has the potential to protect against almost all the most potentially lethal forms of human papilloma virus (HPV).
HPV is primarily transmitted through sexual contact. More than 200 distinct HPV types have been identified, of which at least 18 are high-risk types associated with 99 percent of cervical cancers, the second most common cancer among women after breast cancer.
Gardasil 9 is the current market-available HPV vaccine providing the broadest protection against infection from nine HPV types, seven of which can cause 90 percent of cervical cancers.
The research paves the way for an improved HPV vaccine made of seven-type virus-like particles to protect against as many as 20 HPV types.
Xia Ningshao, Researcher, Xiamen University
However, it remains unclear whether widespread immunization with vaccines like Gardasil 9 could lead to an increase in infection rates from the other cancer-related HPV types, responsible for the remaining 10 percent of cervical cancers.
To expand type coverage, the approach used in previous-generation vaccines was to increase the number of virus-like particles. One particle resembles one HPV type, and it can elicit immunity to one HPV type. The more particles a vaccine has, the broader protection it provides.
However, this approach is fraught with difficulties, as an increase in type coverage will dramatically enhance protein amounts and immunological agent levels per dose, which will cause side effects, such as pain, swelling and fever, and raise the manufacturing complexity and production costs.
Researchers at Xiamen University, in east China's Fujian province, have developed a highly effective vaccine candidate that can protect against more HPV types with fewer particles.
They divided 20 major HPV types, including HPV6 and HPV11, which accounts for 90 percent of genital warts, into seven groups based on genetic relationships, and found that genetically close HPV types shared high structural similarities.
Xia Ningshao, lead researcher, compared the virus or the vaccine to a "ball". All HPV types are similar in appearance, but are significantly different in the surface of the "ball", such as veins, convex and concave areas. These structural features on the surface are called loops.
"Because of the loops, one type of vaccine can stimulate the production of antibodies only against the infection of one type of virus, and is unable to prevent the infection of other types," he said.
Using a loop swapping approach, researchers engineered a complex virus-like particle with the loops of three genetically close HPV types: HPV33, HPV58 and HPV52.
They tested the triple-type particle in experiments on mice and monkeys, and found it could provide high immune potency comparable with a combination of three virus-like particles.
The new approach was equally successful in developing another four triple-type particles using the other 12 major HPV types.
"The research paves the way for an improved HPV vaccine made of seven-type virus-like particles to protect against as many as 20 HPV types," said Xia.
The results were recently published in the international Nature Communications journal. Reviewers said the new-generation vaccine candidate was "a remarkable achievement" for having broader type coverage, lower cost and lower amounts of proteins and agents, and "will be moved forward into a clinical trial."
Three HPV vaccines have been introduced to China, covering two, four and nine types. The three-shot HPV vaccination covering nine types is priced for 3,894 yuan. In some areas, scalpers sell it for over 6,000 yuan, which is prohibitive for many poor women.
Researchers say the new-generation vaccine candidate will be available for women aged 9 to 45. Its cost will not exceed the current market-available vaccines.
Two HPV vaccines previously developed by the Xiamen University have reached the clinical test stage and are expected to enter the market in 2019 and 2022.
The world's first HPV vaccine, Gardasil, was developed by Chinese cancer researcher Zhou Jian and Australian immunologist Ian Frazer. In 1995, Zhou and Frazer started cooperating with Merck and Co. to develop the vaccine. After Zhou's sudden death from hepatitis in 1999, Frazer continued the work until the vaccine was ready for market.
According to the World Health Organization, about 570,000 new cases and 311,000 deaths of cervical cancer are reported worldwide every year. China has a very high incidence and death rate, with 106,000 new cases reported and about 48,000 deaths in 2018.
Cervical cancer can be fatal. HPV vaccination has been promoted in China in recent years. Women are also advised to prevent the disease through regular health checks.
0 notes
Video
youtube
Erie County Health Commissioner Dr. Gale Burstein talks about back-to-school vaccines. Make sure you kids are up-to-date on school immunizations whether they will be in elementary school, middle/high school or starting college. Before heading back to school, three vaccines are recommended for 11-12 year-olds – HPV, Tdap and meningococcal conjugate vaccine. The HPV vaccines is important because it can prevent HPV infections that can cause cancer later in life. This vaccine is for protection from most of the cancers caused by human papillomavirus (HPV). Immunize at 11-12 years old. This vaccine is a series of shots given over several months. The risk for females decreases after age 25 but the risk for males getting HPV stays the same throughout their lifetime so males can still be vaccinated if they haven’t already. All public and private school students entering 7th and 12th grades in New York State must be fully vaccinated against meningococcal disease types A, C,W and Y in order to attend school. The meningitis B vaccine is not required for school but is recommended. Meningococcal vaccine protects against serious diseases such as meningitis and sepsis. The vaccine is sometimes called the meningitis vaccine. Students who are not up-to-date will not be allowed to attend school until they are vaccinated. For some diseases, like whooping cough, the protection from vaccine doses received in childhood fades over time. That is why it is recommended that 11-12 years-old’s get the Tdap booster shot to help protect them from whooping cough, tetanus, and diphtheria. Flu can be serious, even for healthy, young people. Preteens and teens are no exception. Older kids should get at least one flu vaccine every year. If you are unable to pay for vaccines check out the “Vaccines For Children (VFC) Program”, a federally funded program that provides vaccines at no cost to children who might not be vaccinated because of the cost. by WKBW TV | Buffalo, NY
0 notes
Text
Preventive Health Screenings and health care for Women
Be proactive about your health by staying on top of necessary screenings and health care visits. This schedule is a suggested timeline for routine screenings. Talk with your health care provider for specific personal guidance. More frequent screenings may be recommended based on your personal health history.
General Health
What
When
Why
Physical examination
Every 2–3 years; discuss with your health care provider.
To screen for diseases; assess risk for future problems; discuss lifestyle habits; and keep vaccinations up to date.
Thyroid test
Discuss with your health care provider.
To identify an under- or overactive thyroid, both of which are very treatable and either of which can lead to more serious conditions if left untreated.
Bone Health
What
When
Why
Bone mineral density test
At least once beginning at age 65; earlier depending on your risk factors for osteoporosis.
There are no obvious signs of osteoporosis until you fracture a bone. Bone density screenings identify problems early, enabling you to start treatment and prevent further bone loss.
Breast Health
What
When
Why
Mammogram
Every 1–2 years starting at age 40.
To identify possible early signs of breast cancer.
Clinical breast exam
About every 3 years for women in their 20s and 30s, and every year for women 40 and over.
Not all breast cancers are found on mammograms; a good clinical breast exam can also help identify cancers relatively early.
Colorectal Health
What
When
Why
Colonoscopy
Every 10 years starting at age 50. Alternatively, you may get a flexible sigmoidoscopy every 5 years or a double-contrast barium enema every 5 years or a CT colonography (virtual colonoscopy) every 5 years, but a colonoscopy will be needed if any of those results are positive.
To identify (and remove) precancerous polyps or early cancers.
Fecal occult blood test (also called stool guaiac test) or fecal immunochemical test or stool DNA test
Annually starting at age 50 for the fecal occult blood test or the fecal immunochemical test; stool DNA test may be given at intervals recommended by your doctor.
To provide an early warning sign about colon cancer. Not as good as a colonoscopy in identifying cancers or precancerous cells.
Digital rectal exam
Starting at age 50, every 5–10 years with each colon screening.
To help find early signs of colon cancer in the anal canal and lower rectum. Because of its limitations, it is not recommended as the only test for colorectal cancer.
Diabetes
What
When
Why
Fasting plasma glucose test (also called blood glucose test)
Every three years starting at age 45; more often or earlier if you're overweight or at risk for diabetes.
To provide an early warning sign of high blood sugar levels, which could mean an increased risk for diabetes.
Eye, Ear and Teeth Health
What
When
Why
Eye exam
At least once from ages 20 to 29; at least two exams between ages 30 and 39. At age 40, get a baseline eye disease screening. Based on results, follow ophthalmologist's recommendations until age 65. After that, complete eye exam every one to two years.
To test your vision and screen for glaucoma and macular degeneration, two common, often age-related conditions.
Hearing test
Beginning at age 18, then once every 10 years until age 50, after which it should be once every three years.
To make sure you're hearing all life has to offer.
Dental exam and cleaning
At least once a year; twice a year is best.
To remove plaque and bacteria that could lead to tooth and gum disease; to check for tongue and mouth cancer. Problems with your teeth can indicate osteoporosis.
Heart Health
What
When
Why
Blood pressure screening
At least every 2 years in your health care professional's office.
The only way to identify hypertension is with blood pressure screenings.
Cholesterol screening
Every 5 years starting at age 35. Begin screening at age 20 if you smoke, are obese, have diabetes or high blood pressure or have a family history of heart disease.
Treating cholesterol abnormalities can help reduce your risk of heart disease.
Reproductive/Sexual Health
What
When
Why
Pap test
Every 3-5 years for women ages 21-65. Women 21-30 should get a Pap test every 3 years. Women over 30 should get a combined Pap test and HPV test every 5 years; if HPV testing is not available, they may get a Pap test every 3 years. Screening may be stopped for women over age 65 who have been adequately screened with normal results and are not at high risk for cervical screening. If you have had your cervix and uterus removed, ask your health care provider if you need to continue screening.
Helps identify women at risk for developing cervical cancer.
HPV test
Every 5 years along with Pap test in women ages 30-65 (and in younger women with inconclusive Pap tests).
The HPV test in combination with the Pap test is better at identifying women at risk for developing cervical cancer than the Pap test alone.
Pelvic exam
Annually for women starting at age 21 or younger if indicated by medical history.
As part of a preventive care visit to assess health, lifestyle and health risks.
Chlamydia test
Yearly until age 25 if sexually active; for age 26 and older, get the test if you have new or multiple sexual partners.
Prevents spread of chlamydia.
Sexually transmitted disease (STD) screening
All sexually active women and their partners should be tested for HIV and other STDs before starting sexual activity.
Prevents spread of HIV and other STDs, many of which can only be detected through testing.
Skin Health
What
When
Why
Skin exam by a doctor
Talk to your health care provider about what’s right for you. If you have risk factors for skin cancer, your health care provider may recommend periodic skin exams.
To track worrisome moles and identify skin cancer early.
Skin self-exam
Monthly skin exam starting at age 18.
To know your own skin and be able to report changes to your health care provider.
Immunizations
What
When
Why
Influenza (flu) vaccine
Annually for everyone 6 months and older.
Protection again some flu viruses (will include H1N1 starting in fall 2010).
Hepatitis A
Given in 2 doses, 6-18 months apart, to children 1 year of age and to adults at risk or who want protection from hepatitis A.
Protects against hepatitis A, a serious liver disease that can cause flu-like illness, jaundice and severe stomach pains and diarrhea.
Hepatitis B
Given to children at birth in 3 doses at 0, 1 and 6 months. Also given to children or adults who weren't vaccinated and are at risk for hepatitis B, such as health care workers.
Protects against hepatitis B, a serious liver disease that can develop into a chronic infection.
Herpes zoster
Once only at age 60 or older.
Shingles prevention.
Human papillomavirus (HPV)
Age 11–12 or 13–26 if not previously vaccinated; 3 doses at 0-, 2- and 6-month intervals; no booster necessary.
Protects against four common types of HPV, including the two most likely to cause cervical cancer.
Pneumonia
Once only at age 65 or older.
Protects against pneumonia.
Tetanus, diphtheria, pertussis (Td/Tdap)
Every 10 years.
Protects against tetanus, diphtheria and pertussis.
Meningococcal
College freshmen, military recruits and other at-risk persons; discuss with your health care provider.
Protects against some types of meningococcal disease (meningitis).
Varicella (chickenpox)
Given in 2 doses at 0- and 4- to 8-week intervals to those 19 or older who have not been vaccinated or had chickenpox.
Protects against chickenpox, a usually mild but highly contagious childhood disease, which can be serious in infants and adults.
Read the full article
0 notes
Text
The HPV Vaccine is Still Woefully Underutilized—Here’s How We Can Change That
The human papillomavirus (HPV) is the most common sexually transmitted infection. In addition to genital warts, it has the potential to cause a wide range of cancers, including cancers of the cervix, anus, and throat. A vaccine that can prevent HPV (and its associated cancers) has been around for nearly a decade; however, it continues to be widely underutilized in the United States.
The vaccine is most effective if administered in childhood before sexual activity begins. It is encouraging that, nationwide, a majority of parents—6 in 10—are now opting to have their kids vaccinated. This number has risen steadily in recent years and is at an all-time high. However, it still means that millions of children and adolescents are going without and therefore will be at risk for the potential negative health effects of this virus later in life.
It’s important to note that vaccination rates vary widely across the country. For instance, in some states—like Texas, Indiana, South Carolina, and Kentucky—fewer than half of adolescents have received the vaccine. By contrast, in California, New York, and Massachusetts, more than 70% have received at least one dose (for maximum effectiveness of the vaccine, three injections must be administered a few months apart). For a closer look at how vaccination rates vary across the U.S., check out the figure below created by the CDC.
In order to increase vaccination rates, we need to do a few things. First, we need to combat persistent myths and misinformation, such as the claim that this vaccine poses serious health risks. The truth is that this vaccine is safe and effective, and no riskier than other vaccines [1]. Likewise, persistent concerns have been raised in the media about whether the vaccine will increase rates of risky sexual behavior; however, research has not found any support for that idea either [2].
Second, physicians need better education about the vaccine because it turns out that many of them are engaging in behaviors that are discouraging many teens from receiving it, such as not giving timely vaccine recommendations, failing to recommend same-day vaccination, and only recommending it to those deemed “at risk” [3].
Finally, we also need to get policy makers on board. There’s a lot that states can do legislatively that have the potential to help, such as by creating policies that increase HPV awareness and encouraging vaccination. Efforts to mandate the vaccine have proved controversial; however, if politicians can at least work toward increasing awareness of this infection and reducing barriers to vaccination, that would be a huge step in the right direction.
Want to learn more about Sex and Psychology ? Click here for previous articles or follow the blog on Facebook (http://ift.tt/1gJEOW0), Twitter (@JustinLehmiller), or Reddit (http://ift.tt/1gJEOW8) to receive updates.
[1] Reiter, P. L., Brewer, N. T., Gottlieb, S. L., McRee, A. L., & Smith, J. S. (2009). How much will it hurt? HPV vaccine side effects and influence on completion of the three-dose regimen. Vaccine, 27(49), 6840-6844.
[2] Smith, L. M., Kaufman, J. S., Strumpf, E. C., & Lévesque, L. E. (2015). Effect of human papillomavirus (HPV) vaccination on clinical indicators of sexual behaviour among adolescent girls: the Ontario Grade 8 HPV Vaccine Cohort Study. Canadian Medical Association Journal, 187(2), E74-E81.
[3] Gilkey, M.B. et al. (2015). Quality of physician communication about human papillomavirus vaccine: Findings from a national survey. Cancer Epidemiology, Biomarkers & Prevention. doi: 10.1158/1055-9965.EPI-15-0326
Image Source: Centers for Disease Control and Prevention (CDC)
You Might Also Like:
Am I Too Old For The HPV Vaccine?
Six Myths About Sexually Transmitted Infections Debunked
from Meet Positives SMFeed 8 http://ift.tt/2f3AdWe
via IFTTT
0 notes