#ema guidelines for clinical trials
Text
Clinical Trial Safety and Monitoring
Safety monitoring is a critical component of clinical trials to ensure the well-being of participants and the integrity of the study data. Here are key aspects of clinical trial safety and monitoring:
Adverse Event Reporting: Adverse events (AEs) are any undesirable or unintended signs, symptoms, or illnesses that occur during a clinical trial. Participants are monitored for AEs throughout the trial, and any AEs are recorded, evaluated, and reported to the study sponsor and regulatory authorities as required.
Safety Data Review: An independent Data Safety Monitoring Board (DSMB) or Safety Monitoring Committee (SMC) may be established to review safety data during the trial. These committees monitor participant safety, review AEs, and make recommendations regarding the continuation, modification, or termination of the trial based on safety concerns.
Protocol Compliance: Monitoring visits are conducted to ensure that the trial is being conducted according to the study protocol. This includes verifying that participants meet eligibility criteria, study procedures are followed correctly, and data is recorded accurately.
Informed Consent: Monitoring includes ensuring that participants have provided informed consent to participate in the trial. This involves providing participants with information about the study, including its purpose, procedures, risks, and benefits, and obtaining their voluntary consent to participate.
Data Quality Monitoring: Data quality is monitored throughout the trial to ensure that data is accurate, complete, and reliable. This includes verifying that data is entered correctly, checking for missing data, and identifying any discrepancies or errors.
Compliance with Regulatory Requirements: Clinical trials must comply with regulatory requirements and guidelines set forth by regulatory authorities, such as the Food and Drug Administration (FDA) in the United States or the European Medicines Agency (EMA) in Europe. Monitoring ensures that the trial meets these requirements and that data is collected and reported appropriately.
Risk Management: Risk management plans are developed to identify, assess, and mitigate potential risks to participant safety during the trial. This includes measures to minimize risks, such as monitoring for side effects and implementing safety protocols.
Emergency Procedures: Protocols are established for managing medical emergencies that may occur during the trial. This includes ensuring that participants have access to appropriate medical care in case of an emergency.
Continual Monitoring and Oversight: Monitoring continues throughout the trial to ensure that safety measures are effective and that any emerging safety concerns are addressed promptly.
Safety monitoring in clinical trials is a collaborative effort involving researchers, study sponsors, regulatory authorities, and independent oversight committees. By implementing robust safety monitoring procedures, clinical trials can ensure participant safety and maintain the integrity of the study data.
0 notes
Text
Clinical Trial Supply Management: Ensuring Seamless Operations

Clinical trials are vital components of the pharmaceutical and healthcare industries, providing valuable insights into the safety and efficacy of new treatments and medications. Behind the scenes of these trials lies a complex and intricate process known as clinical trial supply management. In this blog post, we'll delve into the essential aspects of clinical trial supply management, its significance in the research process, and the challenges it entails.
At its core, clinical trial supply management involves the coordination and oversight of all materials and resources required to conduct a clinical trial effectively. This includes not only the investigational drug or treatment being tested but also ancillary supplies such as placebos, medical devices, and laboratory equipment. The goal of supply management is to ensure that all necessary resources are available in the right quantities and at the right time, facilitating the smooth execution of the trial.
One of the primary challenges in clinical trial supply management is forecasting and planning for demand. Unlike traditional supply chains, where demand can be relatively stable and predictable, clinical trials are inherently dynamic and subject to numerous uncertainties. Factors such as patient recruitment rates, regulatory requirements, and unforeseen protocol changes can all impact demand for trial supplies, making accurate forecasting a challenging task.
To address this challenge, clinical trial supply managers rely on sophisticated forecasting models and algorithms that take into account various factors affecting demand. These models analyze historical data, patient enrollment projections, and other relevant variables to generate forecasts that guide procurement and inventory management decisions. By leveraging data-driven insights, supply managers can optimize inventory levels, minimize wastage, and ensure that sufficient supplies are available throughout the duration of the trial.
Another critical aspect of clinical trial supply management is ensuring compliance with regulatory requirements and quality standards. As clinical trials are subject to rigorous oversight by regulatory authorities such as the FDA and EMA, it is essential to adhere to strict guidelines regarding the handling, storage, and distribution of trial supplies. Failure to comply with these regulations can result in delays, fines, or even the suspension of the trial, highlighting the importance of robust supply management processes.
In addition to regulatory compliance, supply managers must also address logistical challenges related to supply chain logistics. This includes coordinating the transportation of trial supplies from manufacturers to clinical sites, managing temperature-sensitive products, and ensuring timely delivery to meet study timelines. In some cases, trials may involve multi-site or international collaborations, further complicating logistics and requiring careful coordination among stakeholders.
To overcome these challenges, many organizations are turning to advanced technologies and solutions to streamline their clinical trial supply management processes. This includes the adoption of cloud-based supply chain management platforms, automated inventory tracking systems, and real-time monitoring tools that provide visibility into supply chain performance. By embracing digital innovations, supply managers can enhance efficiency, reduce costs, and mitigate risks associated with clinical trial supply management.
In conclusion, clinical trial supply management is a critical function that plays a central role in the success of clinical trials. By effectively managing the procurement, distribution, and inventory of trial supplies, supply managers ensure that trials are conducted smoothly, safely, and in compliance with regulatory requirements. While the challenges associated with supply management are significant, the adoption of advanced technologies and best practices can help organizations overcome these hurdles and drive innovation in the field of clinical research.
0 notes
Text
How to start a pharmaceutical company?

Starting a pharmaceutical company is a complex endeavor that requires careful planning, substantial investment, and compliance with regulatory requirements. Here is a step-by-step guide to help you navigate the process:
1. Conduct Market Research:
Before diving into the pharmaceutical industry, it's crucial to conduct thorough market research. Identify potential gaps or opportunities in the market, assess the demand for specific types of drugs or therapies, and analyze the competitive landscape.
2. Define Your Business Model:
Decide on the type of pharmaceutical company you want to establish. Will you focus on generic drugs, specialty medications, biologics, or innovative therapies? Determine your target market, pricing strategy, and distribution channels.
3. Develop a Business Plan:
Create a comprehensive business plan that outlines your company's objectives, market analysis, product portfolio, operational strategy, financial projections, and marketing plan. A well-defined business plan will serve as a roadmap for your company's growth and development.
4. Secure Funding:
Starting a pharmaceutical company requires significant financial investment. Explore funding options such as personal savings, loans, venture capital, angel investors, or partnerships with other companies. Ensure you have sufficient capital to cover startup costs, research and development expenses, regulatory fees, and operational expenses.
5. Establish Legal Structure:
Choose a legal structure for your pharmaceutical company, such as a sole proprietorship, partnership, limited liability company (LLC), or corporation. Consult with legal and financial advisors to determine the most appropriate structure based on your business goals and risk tolerance.
6. Obtain Necessary Licenses and Permits:
Compliance with regulatory requirements is essential for pharmaceutical companies. Obtain the necessary licenses, permits, and certifications from regulatory authorities such as the Food and Drug Administration (FDA) in the United States or the European Medicines Agency (EMA) in Europe. This may include a pharmaceutical manufacturing license, drug establishment registration, and Good Manufacturing Practice (GMP) certification.
7. Develop Products:
Invest in research and development to develop pharmaceutical products that meet unmet medical needs or address market demand. Collaborate with scientists, researchers, and contract manufacturing organizations (CMOs) to develop and manufacture high-quality drugs or therapies.
8. Conduct Clinical Trials:
Before seeking regulatory approval, conduct clinical trials to evaluate the safety and efficacy of your pharmaceutical products. Design and implement clinical trial protocols in accordance with regulatory guidelines, and collect data to support future regulatory submissions.
9. Navigate Regulatory Approval Process:
Prepare and submit regulatory applications for product approval, such as Investigational New Drug (IND) applications, New Drug Applications (NDAs), or Marketing Authorization Applications (MAAs), depending on your target market. Work closely with regulatory consultants and legal advisors to navigate the regulatory approval process efficiently.
10. Establish Distribution Channels:
Develop distribution channels to ensure widespread access to your pharmaceutical products. This may involve partnering with wholesalers, distributors, pharmacies, hospitals, or specialty pharmacies to distribute your products to healthcare providers and patients.
11. Implement Quality Control Systems:
Implement robust quality control systems to ensure the safety, purity, and potency of your pharmaceutical products. Adhere to Good Manufacturing Practices (GMP) and other quality standards to maintain product quality and regulatory compliance.
12. Launch and Market Products:
Once regulatory approval is obtained, launch your pharmaceutical products in the market and implement marketing strategies to promote awareness and adoption. Collaborate with healthcare professionals, key opinion leaders, patient advocacy groups, and payers to maximize market penetration and sales.
13. Monitor and Evaluate:
Continuously monitor the performance of your pharmaceutical products, gather feedback from healthcare professionals and patients, and evaluate market trends. Adapt your strategies as needed to optimize product performance and maintain competitiveness in the market.
Conclusion:
Starting a pharmaceutical company is a complex and challenging process that requires careful planning, substantial investment, and compliance with regulatory requirements. By following these steps and seeking expert guidance, you can navigate the complexities of the pharmaceutical industry and establish a successful company that brings innovative therapies to market, improves patient outcomes, and contributes to the advancement of healthcare.
0 notes
Text
Clinical Trial Imaging Market Eyes 7.8% CAGR Growth
Clinical Trial Imaging Market achieved a significant milestone, reaching a valuation of USD 1.3 billion. Looking ahead, the market is poised for substantial growth, projected to maintain a robust Compound Annual Growth Rate (CAGR) of 7.8%.
This trajectory underscores the industry's resilience and potential, driven by advancements in imaging technologies and increasing demand for innovative healthcare solutions. As clinical trials become more complex and data-intensive, the role of imaging in evaluating treatment efficacy and safety becomes increasingly crucial.
With ongoing developments in medical imaging techniques and data analysis capabilities, the clinical trial imaging market is well-positioned to address evolving research needs and contribute to advancements in medical science.

Request Sample Report: https://datahorizzonresearch.com/request-sample-pdf/clinical-trial-imaging-market-2779
Here’s an overview of key trends and factors shaping the clinical trial imaging market:
Growing Importance of Imaging in Clinical Trials: Imaging techniques such as MRI (Magnetic Resonance Imaging), CT (Computed Tomography), PET (Positron Emission Tomography), and ultrasound play a crucial role in assessing disease progression, treatment response, and safety endpoints .
Advancements in Imaging Technologies: Technological advancements have led to the development of more advanced imaging modalities with improved resolution, speed, and sensitivity.
Integration of Artificial Intelligence (AI) and Machine Learning: AI and machine learning algorithms are being increasingly integrated into imaging analysis software to automate image interpretation, enhance accuracy, and streamline workflow processes.
Increasing Regulatory Acceptance: Regulatory agencies such as the FDA and EMA have recognized the importance of imaging biomarkers in clinical trials and have provided guidelines for their use in drug development.
Shift towards Decentralized Trials and Remote Imaging: The COVID-19 pandemic has accelerated the adoption of decentralized trial models, where imaging procedures can be conducted remotely or in decentralized imaging facilities.
Top Companies are:
· IXICO plc
· Navitas Life Sciences
· Resonance Health
· ProScan Imaging
· Radiant Sage LLC
· Koninklijke Philips N.V
· WIRB-Copernicus Group
· Medpace
· Biomedical Systems Corp
· Cardiovascular Imaging Technologies
Market Segmentations:
By Imaging Modality — CT (Computed Tomography), MRI (Magnetic Resonance Imaging), Ultrasound, PET (Positron Emission Tomography), X-ray, Echocardiography
By Services- Operational Imaging, Read Analysis, System and Technical Support, Trial Design & Consulting
By End-user- Pharmaceutical and Biotechnology companies, Medical Device Manufacturer, Contract research organizations (CROs), Academic institutions
For Further Information Regarding this Report: Ask For Discount:
https://datahorizzonresearch.com/ask-for-discount/clinical-trial-imaging-market-2779
Regional Analysis:
The Clinical Trial Imaging market, segmented geographically into North America, Latin America, Europe, Asia Pacific, and the Middle-East and Africa, is poised for significant growth. North America is expected to dominate this expansion, thanks to its robust infrastructure, extensive R&D efforts, and the presence of leading pharmaceutical and biotech firms. At the forefront of this surge is the United States, boasting numerous top-tier research institutions and a stringent regulatory framework upheld by the FDA.
As a central hub for drug development and manufacturing, the U.S. benefits from supportive government initiatives like the 21st Century Cures Act, which promotes innovative technologies, including imaging modalities and precision medicine, in clinical trials. These factors collectively bolster market growth in the region.
Key highlights of the report include:
1. The report delivers thorough Market analysis, furnishing valuable insights to guide strategic decision-making.
2. The comprehensive research outlined in the study enhances the depth of your presentations and marketing strategies.
3. By offering crucial insights into key market competitors, the study empowers businesses with a strategic edge.
4. It delivers a precise assessment of evolving market dynamics, ensuring readers stay abreast of the latest industry trends.
5. With meticulous breakdowns of various market niches, the report facilitates informed decision-making processes.
Check Out More Related Reports:
Mobility as a Service Market
Check Cashing Services Market
0 notes
Text
Unleashing Growth in Neurological Biomarkers Market: 2024-2028
Originally Published on: TechnavioNeurological Biomarkers Market Analysis North America, Europe, Asia, Rest of World (ROW) - US, Germany, UK, France, China - Size and Forecast 2024-2028
In the ever-evolving healthcare domain, the global neurological biomarkers market is gearing up for substantial expansion, targeting USD 7.82 billion with a 13.01% CAGR by 2028. Driving this growth are pivotal factors such as the surge in clinical trials, widespread adoption of disease-specific biomarkers, and significant regulatory acknowledgment propelling market evolution.
Global Momentum in Clinical Trials: Catalyst for Market Dynamics
The upswing in clinical trials, characterized by structured approaches, active participant engagement, and cost-effective trials in emerging economies, propels the neurological biomarkers market. Disease-specific biomarkers hold the promise of rapid and precise disease diagnosis, potentially reducing clinical trial timelines and sample sizes. Regulatory bodies such as the US FDA and EMA recognize the pivotal role of biomarkers, anticipating accelerated drug development and fostering market growth.
Dominance of Hospital End-Users: A Pivotal Element
Hospital Segment Taking the Lead: The hospitals segment assumes a leading role in shaping market dynamics within the end-user spectrum. Large and medium-sized hospitals, each wielding distinct influences, contribute significantly to accessibility and overall impact. Valued at USD 2.18 billion in 2018, the hospitals segment is on the brink of growth, driven by heightened demand for neurological biomarker products in medium-sized healthcare facilities.
Focus on Disease-Specific Segmentation: Alzheimer's and Parkinson's in the Limelight
Ascendance of Alzheimer's Disease Segment: Alzheimer's disease, marked by memory loss, propels growth in the AD segment. Neurobiological biomarkers emerge as effective tools for early AD detection, offering insights into disease progression. The segment's trajectory is fueled by evolving diagnostic guidelines and ongoing research exploring interventions to combat this debilitating condition.
Momentum in Parkinson's Disease Segment: Parkinson's disease, a neurodegenerative disorder causing movement issues, gains momentum with breakthroughs in dopamine presynaptic biomarkers. Advanced imaging techniques hold promise for PD treatment, coupled with a focus on restoring the gut microbiome to impede PD progression.
Regional Dynamics: North America Leading the Charge
Pivotal Role of North America: Projected to contribute 40% to the global market share by 2028, North America emerges as a major player. Factors such as the escalating prevalence of neurological disorders, a growing aging population, substantial healthcare expenditure, and favorable reimbursement policies propel market growth. Government initiatives, research expenditures, and collaborative efforts in the US and Canada underscore the region's commitment to neurological disorder research.
Strategic Maneuvers by Key Market Players
Focused Strategic Initiatives: Market players strategically navigate the landscape through alliances, partnerships, mergers, acquisitions, and product launches. Key player Abbott Laboratories introduces I STAT Alinity, a portable blood analyzer ensuring real-time diagnostic results. A competitive landscape analysis of 20 market companies provides insights into their strategies, strengths, and weaknesses.
Market Dynamics: Influential Factors
Government Initiatives as Growth Catalysts: Support from global governments to enhance neurological healthcare access emerges as a significant driver. Collaborative efforts, research funding, and initiatives targeting diseases like epilepsy and Alzheimer's underscore the global commitment to neurological healthcare.
Blood-Based Biomarkers Trend: The rise of blood-based biomarkers emerges as a noteworthy trend shaping market growth. Non-invasive and easily obtainable blood biomarkers, including amyloid beta monomers and tau proteins, play a pivotal role in diagnosing neurodegenerative disorders. Breakthroughs in ultrasensitive assays fuel interest in blood-based biomarkers for neurological disorder detection.
Challenges in Neurological Research: A Hindrance
Inherent Challenges Persist: Despite promising developments, inherent challenges persist in transitioning from biomarker discovery to clinical practice. Stringent validation strategies, slow disease progression necessitating extended patient treatments, and the need for extensive patient involvement pose hurdles. A global lack of ambition and long-term vision in neurological research impedes market growth.
Navigating Adoption Phases: Customer Landscape
Overview of Adoption Lifecycle: The market report offers insights into the adoption lifecycle, spanning innovators to laggards. It assesses adoption rates in different regions, evaluating purchase criteria and price sensitivity drivers. Companies can leverage this information for market growth strategies and forecasting.
Innovative Solutions Driving Future Growth
As the neurological biomarkers market advances, innovative solutions, strategic partnerships, and an unwavering commitment to neurological healthcare will propel sustained growth. Stakeholders navigating these dynamics are poised to unlock unprecedented opportunities and contribute to the evolving landscape of neurological disorder diagnostics and treatment.
Contact us.
#NeurologicalBiomarkers#HealthcareInnovation#ClinicalTrials#MedicalResearch#GlobalHealth#Diagnostics#StrategicHealthcare#MarketAnalysis
0 notes
Text
Unlocking Clinical Trial Success: The Crucial Role of Biostatisticians
Introduction:
Clinical trials are the backbone of medical advancements, offering hope and innovative solutions to combat diseases and improve human health. However, behind every groundbreaking discovery lies a meticulous process of data analysis and interpretation, spearheaded by biostatisticians. These unsung heroes of the medical field play a pivotal role in ensuring the reliability and validity of clinical trial results. Let's delve into the indispensable contributions of biostatisticians and their significance in shaping the future of healthcare.
Understanding Clinical Trials:
Clinical trials, and structured experiments evaluating medical interventions, require meticulous protocols detailing objectives, participant criteria, and data collection. Biostatistics in Clinical Trials is indispensable, guiding trial design, analysis, and interpretation. Biostatisticians collaborate closely to ensure methodological soundness, reliable results, and meaningful conclusions, vital for advancing medical knowledge and improving patient care.

The Role of Biostatisticians:
Biostatisticians are statistical experts who specialize in designing, analyzing, and interpreting data from biomedical studies, including clinical trials. Their expertise lies in applying statistical methods to ensure the accuracy, reliability, and significance of study findings. Throughout the various stages of a clinical trial, biostatisticians play multifaceted roles:
Study Design:
Biostatisticians collaborate with researchers to design robust study protocols that optimize the collection of relevant data while minimizing biases and confounding variables. They determine appropriate sample sizes, randomization techniques, and statistical endpoints to achieve the study's objectives with precision.
Statistical Analysis Planning:
Before the commencement of data collection, biostatisticians develop detailed analysis plans outlining the statistical methods and techniques to be employed. They anticipate potential challenges, such as missing data or skewed distributions, and devise strategies to address them effectively.
Clinical Data Management:
Biostatisticians oversee the collection, storage, and management of study data to ensure its integrity and confidentiality. They develop data collection forms, implement quality control measures, and establish protocols for data entry and validation.
Statistical Analysis:
Once the data collection phase concludes, biostatisticians conduct rigorous statistical analyses to assess the outcomes of the clinical trial accurately. They employ a diverse array of statistical techniques, including hypothesis testing, regression analysis, survival analysis, and Bayesian methods, depending on the nature of the data and research questions.
Interpretation and Reporting:
Biostatisticians collaborate closely with researchers to interpret the study results in a meaningful context. They communicate statistical findings effectively, highlighting key insights, trends, and associations. Their expertise ensures that conclusions drawn from the data are robust, transparent, and scientifically sound.
Ensuring Regulatory Compliance:
Biostatisticians also play a critical role in ensuring regulatory compliance throughout the clinical trial process. They adhere to stringent regulatory guidelines set forth by organizations such as the Food and Drug Administration (FDA) or the European Medicines Agency (EMA), providing the necessary statistical documentation and support for regulatory submissions.
Conclusion:
Biostatisticians are the silent architects behind the success of clinical trials, wielding the power of statistics to unlock the mysteries of disease and drive medical innovation. Their expertise transcends mere number crunching; they are guardians of scientific rigor, ensuring that clinical trial results are reliable, reproducible, and ethically sound. As we navigate the complex landscape of healthcare, let us acknowledge and celebrate the invaluable contributions of biostatisticians in shaping a healthier, brighter future for all. Global Pharma Tek provides Biostatistics services, which are instrumental in upholding the integrity and validity of clinical research, steering the advancement of new drugs, and devices, and enhancing patient outcomes.
0 notes
Text
Antipsychotic Drugs Market is Estimated to Witness High Growth Owing to Rising Incidence of Mental Disorders

Antipsychotic drugs help manage symptoms of psychosis associated with mental disorders such as schizophrenia and bipolar disorder. These drugs aim to restore normal thinking and behaviors.
Market Dynamics:
The rising incidence of mental disorders such as schizophrenia and bipolar disorder globally is expected to drive the growth of the antipsychotic drugs market. According to the National Institute of Mental Health, about 1% of U.S. adults aged 18-54 years suffer from schizophrenia annually. Moreover, the increasing adoption of atypical antipsychotic drugs for treating schizophrenia, bipolar disorder, Alzheimer's disease, and depression over conventional antipsychotic drugs is also expected to fuel the market growth during the forecast period. These atypical drugs have lesser side effects as compared to conventional antipsychotic drugs.
Increasing prevalence of psychiatric disorders is driving the growth of antipsychotic drugs market
The increasing prevalence of psychiatric disorders such as schizophrenia, bipolar disorder and major depressive disorder across the globe is a major factor driving the growth of the antipsychotic drugs market. According to the World Health Organization (WHO), over 264 million people suffer from depression worldwide. Similarly, schizophrenia affects over 21 million people globally. The social and economic burden of these mental illnesses have led governments and private organizations to spread more awareness and improve diagnosis and treatment rates. This has resulted in higher demand for effective therapeutic drugs such as antipsychotics. Moreover, the development of novel drug delivery technologies and newer drug molecules with improved safety profiles is also fueling the usage of antipsychotic medications.
Stringent regulatory requirements is restraining the development of new antipsychotic drugs
While the need for effective antipsychotic treatment is increasing exponentially, the stringent regulatory environment for the approval of new central nervous system (CNS) drugs is hindering research progression and product development in this market. Regulatory agencies like the FDA and EMA impose rigorous guidelines for clinical trial protocols and data requirements before approving antipsychotic medications due to concerns over serious side effects such as weight gain, metabolic abnormalities and extrapyramidal symptoms. This results in long approval timelines of 8-10 years on an average for a new antipsychotic entity. The high costs and risks involved also discourage investments in development of novel molecules. Generic manufacturers also face regulatory obstacles regarding bioequivalence trials for complex drugs acting on the brain. Overall, the strict regulations make market entry and commercialization quite challenging for new players.
Increasing healthcare expenditure in emerging countries presents lucrative opportunities
With rapid economic growth and rising affluence, many emerging Asian, African and Latin American countries are witnessing significant increase in government and private healthcare spending over the past decade. This presents lucrative opportunities for major antipsychotic drug manufacturers to expand into high growth potential markets. According to the WHO, low and middle income countries currently contribute to more than 85% of the global disease burden from neurological and mental disorders. However, treatment rates remain low due to lack of resources and awareness. The growing healthcare expenditure provides opportunities to cater to this huge unmet need through strategic collaborations and innovative access programs. Multinational pharmaceutical companies can leverage their R&D expertise and portfolio to grab a share of this emerging antipsychotic drugs market.
Personalized treatment based on disease biomarkers and genetics is emerging as a key trend in antipsychotic drug development
With advancements in diagnostic technologies, the trend is shifting towards developing more personalized treatment approaches based on a patient’s specific disease biomarkers, genetics and other clinical characteristics. Currently, antipsychotic prescribing mainly depends on clinical symptoms presentation. However, personalized medicine using biomarkers can help identify what type and dose of medication will work best for an individual. It can also help select the right patients for clinical trials of new drugs. Biomarker-driven approaches are being studied to facilitate early diagnosis of mental illnesses and guide treatment management. Big data analytics using real-world evidence is also aiding the development of more targeted drug therapies. This emerging trend holds potential to transform antipsychotic drug R&D and optimize treatment outcomes.
0 notes
Text
Pharmaceuticals, drug safety remains a top priority for both regulatory agencies and pharmaceutical companies. Ensuring the safety and efficacy of medications is crucial to protect public health. Over the years, drug safety regulations have undergone significant changes and advancements to adapt to emerging challenges and technologies. In this blog, we will explore the latest developments in drug safety regulatory Services and their profound impact on pharmaceutical companies.
Evolution of Drug Safety Regulations
Drug safety regulations have come a long way since their inception. Historically, regulatory agencies such as the FDA (Food and Drug Administration) in the United States and the EMA (European Medicines Agency) in Europe have been responsible for setting guidelines and conducting safety assessments of pharmaceutical products. These agencies have continuously refined their processes to enhance drug safety.
1. Risk-Based Approaches: One significant development in recent years is the adoption of risk-based approaches to drug safety. This means that regulatory agencies and pharmaceutical companies focus their resources on evaluating and mitigating risks associated with specific drugs. This approach allows for a more efficient allocation of resources and a faster response to potential safety concerns.
2. Real-World Evidence: The use of real-world evidence (RWE) has gained prominence in drug safety evaluations. RWE encompasses data from sources such as electronic health records, patient registries, and claims databases. Incorporating RWE into safety assessments provides a more comprehensive view of a drug's performance in real-world settings, beyond clinical trials.
3. Pharmacovigilance Systems: Regulatory agencies now require pharmaceutical companies to have robust pharmacovigilance systems in place. These systems enable the continuous monitoring and reporting of adverse events associated with their products. The implementation of advanced pharmacovigilance Services and technologies has become essential.
4. Signal Detection and Evaluation: Advanced data mining and signal detection techniques have improved the ability to identify potential safety signals earlier. This allows for prompt investigation and risk mitigation, reducing the likelihood of adverse events reaching the public.
Impact on Pharmaceutical Companies
The evolving drug safety regulatory landscape has a profound impact on pharmaceutical companies. Here are some of the key ways in which these developments affect their operations:
1. Increased Compliance Costs: Pharmaceutical companies must invest in technologies and personnel to meet the evolving regulatory requirements. This includes the development and maintenance of pharmacovigilance systems, real-world evidence capabilities, and compliance with risk-based approaches.
2. Enhanced Risk Management: While compliance costs have increased, pharmaceutical companies benefit from a more refined approach to risk management. By focusing resources on higher-risk products, they can make better-informed decisions about development, marketing, and post-market surveillance.
3. Improved Product Safety: Ultimately, the biggest advantage of these developments is improved product safety. Early detection and mitigation of safety concerns help pharmaceutical companies avoid costly recalls, litigation, and damage to their reputation.
4. Competitive Advantage: Companies that excel in drug safety and compliance with the latest regulatory guidelines gain a competitive advantage. They are more likely to gain the trust of healthcare providers and patients, leading to increased market share.
Conclusion
The latest developments in drug safety regulatory services represent a significant shift towards a more proactive and data-driven approach to pharmaceutical safety. While these changes bring increased compliance costs and operational challenges, they also offer pharmaceutical companies the opportunity to enhance their risk management practices and improve the safety of their products.
Staying abreast of these evolving regulations is essential for pharmaceutical companies aiming to thrive in this dynamic industry and, most importantly, to safeguard public health.
0 notes
Text
The Crucial Role of Verification and Validation in Medical Devices
In the rapidly advancing field of healthcare technology, medical devices play a pivotal role in diagnosis, treatment, and patient care. As these devices become increasingly complex, ensuring their safety, efficacy, and reliability becomes paramount. This is where the processes of verification and validation come into play, serving as critical components in the development and deployment of medical devices.
Verification and Validation Defined:
Verification and validation are distinct but interconnected processes in the lifecycle of a medical device.
Verification is the process of confirming that the design and development of a medical device meet the specified requirements. It involves rigorous testing and analysis to ensure that each component and the overall system functions as intended. This phase ensures that the device is designed correctly and operates according to the predefined specifications.
Validation, on the other hand, focuses on confirming that the medical device, when used in its intended environment, meets the user's needs and expectations. This involves real-world testing scenarios and often includes clinical trials to evaluate the device's performance in diverse conditions. Validation ensures that the device is effective and safe for its intended use.
Importance of Verification and Validation in Medical Devices:
1. Patient Safety:
- The primary concern in healthcare is patient safety. Verification and validation processes are designed to identify and rectify potential hazards or malfunctions in a medical device before it reaches the end-user, minimizing the risk of harm to patients.
2. Compliance with Regulations:
- Regulatory bodies, such as the Food and Drug Administration (FDA) in the United States and the European Medicines Agency (EMA) in Europe, enforce strict guidelines for the development and deployment of medical devices. Verification and validation processes ensure compliance with these regulations, facilitating market approval and commercialization.
3. Reliability and Performance:
- Medical devices must perform reliably and consistently in a variety of conditions. Verification and validation processes rigorously test the device under different scenarios to ensure its dependability, accuracy, and overall performance.
4. User Confidence:
- Healthcare professionals and patients need to trust the devices they use. Verification and validation instill confidence in end-users by demonstrating that a medical device has undergone comprehensive testing, making it more likely to perform as expected in real-world situations.
5. Cost Reduction:
- Identifying and rectifying issues early in the development process through verification can significantly reduce the overall cost of bringing a medical device to market. It is more cost-effective to address potential problems during the design phase than to make changes after mass production has begun.
6. Continuous Improvement:
- Verification and validation are not one-time processes; they are iterative and ongoing. Continuous monitoring, feedback, and improvement are essential to adapt to emerging technologies, evolving regulations, and changing healthcare needs.
0 notes
Text
The Importance of Active Pharmaceutical Ingredients in Drug Development
Introduction
The role of Active Pharmaceutical Ingredients (APIs) in drug development is often understated, yet it's the cornerstone of any effective medication. These critical components are responsible for the therapeutic effects of a drug, making their quality and efficacy vital. This article delves into the significance of APIs in the pharmaceutical industry, particularly focusing on drug development and manufacturing.

Understanding APIs
APIs are the substances that produce the intended effects in pharmaceutical drugs. They interact with specific biological targets to bring about therapeutic outcomes. In essence, the API is the 'active' element that treats the condition or symptom for which the drug is prescribed.
The Role in Drug Development
In the initial stages of drug development, identifying or synthesizing a potential API is often the first step. This is followed by rigorous preclinical testing in the lab and in animal models to evaluate its safety and efficacy. Once the API shows promise, it moves to clinical trials involving human subjects to confirm its safety and effectiveness.
Quality and Purity
Importance: The quality and purity of an API directly impact the drug's safety and efficacy.
Regulatory Guidelines: To ensure these standards, APIs must meet stringent quality guidelines set by regulatory bodies like the FDA and EMA.
Manufacturing Considerations
APIs can be synthesized through various methods, including chemical synthesis, fermentation, and extraction. Regardless of the method, rigorous quality control is essential. This ensures that the API's purity and potency meet the required standards, which is crucial for the success of the final drug product.
Challenges and Solutions
API drug development is not without its challenges. The increasing complexity of APIs, especially with the advent of biologics, makes the manufacturing process intricate. Additionally, APIs are subject to stringent regulatory requirements, making the development process both time-consuming and costly. However, advances in technology and a focus on sustainable methods are paving the way for more efficient and eco-friendly API production.
The Future of APIs
The pharmaceutical industry is continuously evolving, and APIs are at the forefront of this change. Advances in genomics are paving the way for personalized medicine, where APIs can be tailored to individual genetic profiles. Moreover, the rise of biologic drugs has led to the development of more complex APIs, opening new avenues for innovation.
Conclusion
Understanding the critical role of Active Pharmaceutical Ingredients in drug development can provide valuable insights for stakeholders in the pharmaceutical industry. As the industry continues to evolve, APIs will undoubtedly remain at its core, driving innovations in drug development, personalized medicine, and more.
For those looking to venture into API manufacturing, partnering with an experienced company like Saurav Chemicals can offer invaluable expertise and solutions, helping you navigate the complexities of API drug development and manufacturing.
0 notes
Text
Clinical Research Regulatory Compliance: Navigating the Complex Landscape in Bangalore
Clinical research plays a pivotal role in advancing medical knowledge and improving patient care. However, the journey from concept to application is fraught with challenges, and one of the key aspects that demand meticulous attention is regulatory compliance. In the bustling hub of clinical research in Bangalore, where numerous companies are contributing to scientific advancements, understanding and navigating the complex landscape of regulatory compliance is crucial. This article explores the nuances of clinical research regulatory compliance and sheds light on the significance of adhering to these standards in Bangalore's vibrant clinical research community.
Understanding Regulatory Compliance:
Clinical research regulatory compliance involves adhering to a set of laws, regulations, and guidelines that govern the conduct of clinical trials. These regulations are in place to ensure the safety, rights, and well-being of research participants and to maintain the integrity and reliability of the data generated during the trials. In Bangalore, a city known for its burgeoning clinical research sector, companies must be well-versed in the local and international regulatory frameworks governing their work.
The Regulatory Framework in Bangalore:
Bangalore is home to a myriad of clinical research companies, ranging from global pharmaceutical giants to innovative startups. Navigating the regulatory landscape in this dynamic environment requires a comprehensive understanding of the regulatory bodies involved. In India, the Central Drugs Standard Control Organization (CDSCO) and the Indian Council of Medical Research (ICMR) play pivotal roles in regulating clinical trials. Additionally, companies in Bangalore must align with global regulatory bodies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) when conducting trials for international markets.
Challenges in Clinical Research Regulatory Compliance:
Bangalore's clinical research sector faces unique challenges when it comes to regulatory compliance. The diversity of clinical trials conducted, ranging from early-phase exploratory studies to large-scale multicenter trials, adds complexity. Furthermore, staying updated with the evolving regulatory landscape both in India and globally is a continuous challenge. Adherence to ethical guidelines, obtaining informed consent, and managing data privacy concerns are additional hurdles that demand constant attention.
The Role of Clinical Research Companies in Bangalore:
Clinical research companies in Bangalore play a crucial role in ensuring regulatory compliance. These organizations must establish robust systems and processes to monitor and manage compliance throughout the research lifecycle. This involves conducting regular internal audits, staying informed about regulatory updates, and providing continuous training to staff involved in clinical trials. Companies must also collaborate with regulatory authorities and institutional review boards (IRBs) to facilitate a smooth regulatory approval process.
The Importance of Regulatory Compliance in Reputation Management:
Maintaining a stellar reputation is paramount for clinical research companies in Bangalore. One aspect that significantly contributes to a company's reputation is its ability to adhere to regulatory standards. Any lapse in compliance can lead to severe consequences, including legal actions, fines, and damage to the company's image. Ensuring regulatory compliance not only fosters trust among stakeholders but also establishes the company as a reliable and ethical player in the clinical research field.
Clinical Research Companies in Bangalore: A Hub for Excellence:
Bangalore has emerged as a hub for clinical research excellence, attracting talent and investments from around the world. The city's diverse pool of professionals, cutting-edge infrastructure, and collaborative ecosystem make it an ideal location for conducting clinical trials. However, this prominence comes with a responsibility to uphold the highest standards of regulatory compliance.
Strategies for Ensuring Compliance in Bangalore's Clinical Research Landscape:
Clinical research companies in Bangalore can adopt proactive strategies to navigate the complex regulatory landscape effectively. Regular training programs for staff, collaboration with regulatory experts, and leveraging technology for streamlined compliance management are essential components of a successful strategy. Additionally, fostering a culture of ethics and compliance within the organization contributes to long-term success.
Conclusion:
Clinical research regulatory compliance is a multifaceted challenge that demands the attention of companies operating in Bangalore's thriving clinical research sector. Navigating the complex landscape requires a deep understanding of local and global regulations, continuous monitoring, and a commitment to upholding the highest ethical standards. By prioritizing regulatory compliance, clinical research companies in Bangalore can not only safeguard the well-being of research participants but also enhance their reputation as contributors to scientific advancement on a global scale. As the city continues to be a focal point for clinical research, maintaining regulatory compliance will be a cornerstone for sustained success.
If you are searching for the clinical research jobs in Hyderabad then CRBtech is the best clinical research jobs in Hyderabad. It has focused on training candidates in IT, Mechanical, Electrical,Civil and Clinical Research. It helps students to start their career journey with a good beginning in the industry.
0 notes
Text
The Vital Role of Regulatory Support in the Pharmaceutical Industry

In the realm of pharmaceuticals, ensuring the safety, efficacy, and quality of medicinal products is paramount. The journey from drug discovery to market availability involves navigating a complex web of regulations and guidelines set forth by regulatory authorities worldwide. This process necessitates comprehensive regulatory support, a crucial component that serves as a guiding force for pharmaceutical companies to meet compliance standards and bring life-saving treatments to patients efficiently.
Understanding Regulatory Support
Regulatory support encompasses a range of activities aimed at assisting pharmaceutical companies in adhering to regulatory requirements throughout the drug development lifecycle. It involves interpreting and implementing regulations, facilitating interactions with regulatory agencies, and ensuring compliance with evolving standards. This support is indispensable for streamlining processes, minimizing risks, and expediting the approval of new drugs and therapies.
Navigating Regulatory Frameworks
The pharmaceutical industry operates within a complex landscape of regulations governed by agencies such as the Food and Drug Administration (FDA) in the United States, the European Medicines Agency (EMA) in Europe, and similar bodies in other regions. These regulatory bodies establish guidelines for drug development, clinical trials, manufacturing practices, labeling, and post-market surveillance to safeguard public health.
Regulatory support teams play a pivotal role in interpreting these regulations and translating them into actionable strategies for pharmaceutical companies. They stay abreast of regulatory updates, anticipate changes, and provide guidance on compliance, helping companies adapt to evolving requirements seamlessly.
Facilitating Regulatory Interactions
Engaging with regulatory agencies is a fundamental aspect of the drug approval process. Regulatory support professionals act as intermediaries between pharmaceutical companies and regulatory authorities, facilitating effective communication and negotiation. They assist in preparing and submitting regulatory submissions, responding to queries, and addressing concerns raised during reviews.
By fostering transparent and collaborative relationships with regulatory agencies, regulatory support teams foster trust and credibility, ultimately enhancing the likelihood of regulatory approval for new drugs and therapies.
Ensuring Compliance and Quality Assurance
Maintaining compliance with regulatory standards is essential for pharmaceutical companies to uphold the integrity and safety of their products. Regulatory support professionals work closely with cross-functional teams to establish robust quality management systems, standard operating procedures (SOPs), and documentation practices that align with regulatory expectations.
Through meticulous oversight and adherence to Good Manufacturing Practice (GMP) guidelines, regulatory support teams help mitigate the risk of quality deviations and regulatory non-compliance. By conducting audits, inspections, and assessments, they identify areas for improvement and implement corrective actions to uphold product quality and regulatory compliance standards.
Driving Innovation and Patient Access
While regulatory compliance is critical, regulatory support also plays a pivotal role in driving innovation and expanding patient access to life-saving treatments. By providing guidance on expedited pathways, orphan drug designations, and regulatory incentives, regulatory support professionals enable pharmaceutical companies to navigate regulatory hurdles more efficiently, accelerating the development and approval of breakthrough therapies.
Moreover, they advocate for patient-centric approaches to drug development, ensuring that regulatory decisions prioritize patient safety, efficacy, and unmet medical needs. By championing initiatives such as patient engagement and real-world evidence generation, regulatory support professionals contribute to the development of innovative therapies that address the diverse needs of patients worldwide.
Conclusion
In the dynamic landscape of the pharmaceutical industry, regulatory support serves as a cornerstone for success, guiding companies through the intricate maze of regulatory requirements and ensuring the delivery of safe and effective treatments to patients. By fostering collaboration, compliance, and innovation, regulatory support professionals empower pharmaceutical companies to navigate regulatory challenges effectively and fulfill their mission of improving global health outcomes. As the industry continues to evolve, the role of regulatory support will remain indispensable in shaping the future of healthcare and driving advancements in medical innovation.
0 notes
Text
Demystifying Pancreatitis Disease: Causes, Symptoms, and More
Pancreatitis Disease Overview:
Pancreatitis Disease is a serious medical condition that affects thousands of individuals worldwide. In this informative article, we will delve into various aspects of pancreatitis, from diagnostic analysis to treatment options, regulatory frameworks, competitive analysis, market trends, and clinical data assessment. By the end of this read, you'll have a comprehensive understanding of pancreatitis and the efforts to combat this disease.
The Market Competitors Listed Below are Revolutionizing Healthcare with Innovative Inventions:
Diagnostic Market Player-
Treatment Market-
Price & Market Access
Diagnostic Analysis of Pancreatitis:
Pancreatitis is the inflammation of the pancreas, an organ located behind the stomach. Diagnosing pancreatitis is essential for early intervention and treatment. Common diagnostic methods include:
Medical History: Doctors often start by reviewing the patient's medical history to identify risk factors such as heavy alcohol consumption, gallstones, or family history of the disease.
Physical Examination: A physical examination may reveal abdominal tenderness, which can be a sign of acute pancreatitis.
Blood Tests: Elevated levels of amylase and lipase in the blood are common markers of pancreatitis.
Imaging Studies: CT scans and MRIs can help visualize the pancreas and identify inflammation or damage.
Pancreatitis Treatment Analysis:
Treatment options for pancreatitis depend on the severity of the condition. In mild cases, the following approaches are taken:
Hospitalization: Patients with acute pancreatitis may require hospitalization for monitoring, fasting, and pain management.
Pain Relief: Medications, including analgesics and antispasmodics, are used to manage pain.
Nutritional Support: Nutritional support, often through a feeding tube, is vital to ensure that the pancreas gets the rest it needs.
In more severe cases, surgery may be required to remove damaged tissue or manage complications. Chronic pancreatitis may require enzyme replacement therapy and lifestyle changes to manage symptoms and improve quality of life.
Browse More Information:
Regulatory Framework for Pancreatitis:
The regulatory framework for pancreatitis involves guidelines and standards for diagnosis, treatment, and research. Health agencies and medical organizations worldwide work together to ensure that patients receive the best possible care and that treatment options are continually improved.
Competitive Analysis:
Several pharmaceutical companies and research institutions are actively engaged in developing new treatments and therapies for pancreatitis. Competition in this field is fierce, with a focus on improving patient outcomes and reducing the burden of the disease.
Market Trends:
Pancreatitis is a growing concern worldwide. Market trends indicate an increasing demand for better diagnostic tools, more effective treatments, and improved patient care. Advances in technology, such as minimally invasive surgery and targeted drug therapies, are expected to drive positive market trends.
Clinical Data Assessment:
Clinical trials play a crucial role in evaluating the effectiveness of new treatments and interventions for pancreatitis. Clinical data assessment allows researchers to gather evidence on the safety and efficacy of new therapies, bringing us closer to finding a cure or better management strategies.
Conclusion:
Pancreatitis is a complex disease that demands our attention, research, and concerted efforts to combat it effectively. From diagnosing the condition to exploring treatment options and assessing clinical data, the medical community and researchers are working diligently to provide hope and relief to those affected by pancreatitis. As we unite in this fight against pancreatitis, the future holds promise for improved treatments and, ultimately, a world free from the burden of this debilitating disease.
Browse Through More Gastrointestinal Disease Research Reports
Related Reports:
Unmasking the Enigma: Solid Tumors and Their Intricate Nature
Unravelling Hemophilia Disease: Understanding a Lifelong Challenge
Demystifying Demodex Blepharitis: Causes, Symptoms, and Treatment
Breathing Easier: A Comprehensive Guide to Cystic Fibrosis Disease
Understanding Appendicitis Disease: Symptoms, Causes, and Treatment
Contact Us:
Disease Landscape Insights LLP
6th Floor, Sr No.207, Office A H 6070 Phase 1
Solitaire Business Hub, Viman Nagar
Pune, Maharashtra, 411014
Email: [email protected]
Email: [email protected]
Blog: https://www.diseaselandscape.com/blogs
Case Study: https://www.diseaselandscape.com/casestudies
Pharma consulting Services
Follow Us: LinkedIn | Twitter | Facebook
0 notes
Text
Revolutionizing the Ovarian Cancer Market: Strategies for Success | DLI
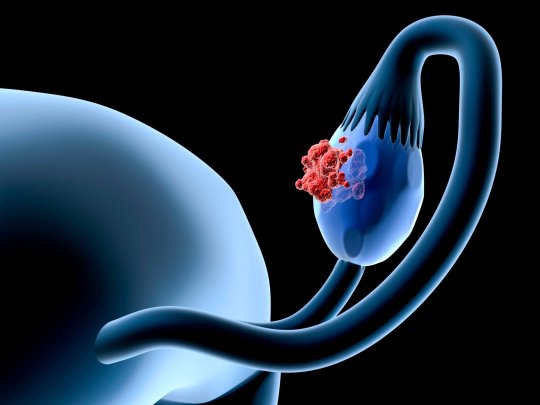
Ovarian Cancer Overview:
Ovarian Cancer is a formidable health challenge affecting women globally. It is characterized by the abnormal growth of cells in the ovaries, which are vital components of the female reproductive system. Often diagnosed at an advanced stage, ovarian cancer poses significant clinical and therapeutic complexities.
Ovarian cancer silently appears as a powerful foe that demands undivided attention. It is unyielding and resilient. It affects women of all ages and socioeconomic backgrounds and spares no one. This sneaky illness hides its presence, frequently coming to light only when the fight grows more difficult.
The Market Competitors Listed Below are Revolutionizing Healthcare with Innovative Diagnostic Inventions:
Price & Market Access
Diagnostic Analysis:
Early Detection Challenges:
Early diagnosis of ovarian cancer remains a critical issue due to its asymptomatic nature in the initial stages. Lack of specific symptoms and effective screening tools makes timely detection a formidable task.
Screening Methods:
Currently, screening methods primarily include pelvic examinations, transvaginal ultrasounds, and blood tests measuring CA-125 levels. However, these methods often lack the sensitivity and specificity needed for reliable early detection.
Treatment Analysis:
Standard Treatment Modalities:
Treatment approaches for ovarian cancer encompass a multidisciplinary approach, including surgery, chemotherapy, radiation therapy, and targeted therapy. The extent of surgical intervention and choice of chemotherapeutic agents are determined by factors like stage, histology, and patient's overall health.
Emerging Therapies:
Immunotherapy and personalized medicine are emerging as promising avenues in ovarian cancer treatment. These approaches aim to enhance the body's natural immune response and tailor treatments based on the genetic profile of the tumor.
Regulatory Framework:
FDA and EMA Guidelines:
Regulatory bodies like the FDA (Food and Drug Administration) in the United States and EMA (European Medicines Agency) in Europe play a pivotal role in approving and regulating treatments for ovarian cancer. Rigorous clinical trials and safety assessments are mandatory before a therapy can be marketed.
Therapeutics:
Targeted Therapies:
Targeted therapies like PARP inhibitors and angiogenesis inhibitors have shown promise in treating specific types of ovarian cancer. They work by interfering with the specific molecular pathways that cancer cells rely on for growth.
Immunotherapies:
Immunotherapies, including checkpoint inhibitors, are being investigated for their potential to enhance the body's immune system to recognize and attack ovarian cancer cells.
Diagnostic Techniques:
Genomic Profiling:
Advancements in genomic profiling have revolutionized the understanding of ovarian cancer. DNA sequencing and molecular profiling enable a more precise characterization of the tumor, guiding treatment decisions.
Liquid Biopsies:
Liquid biopsies, analyzing blood or other bodily fluids, offer a non-invasive method to monitor tumor genetics and detect minimal residual disease.
Treatment Techniques:
Minimally Invasive Surgery:
Minimally invasive techniques, such as laparoscopy, have gained prominence in ovarian cancer surgery. They offer shorter recovery times and reduced post-operative complications.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC):
HIPEC is an innovative technique that delivers heated chemotherapy directly to the abdominal cavity during surgery. This approach targets residual cancer cells and has shown promise in improving survival rates.
Browse More Information:
Clinical Assessment:
Multidisciplinary Teams:
Ovarian cancer treatment requires collaboration among various specialists, including gynecologic oncologists, surgeons, medical oncologists, and radiologists, to create personalized treatment plans.
Survivorship Care:
Long-term survivorship care plans are essential to address the physical, emotional, and psychological aspects of recovery after ovarian cancer treatment.
Expanding Therapeutic Landscape:
The ovarian cancer therapeutics market is witnessing a surge in research and development efforts, with a growing number of targeted and immunotherapeutic agents in the pipeline.
Regional Research Initiatives:
Different regions are contributing to ovarian cancer research with unique perspectives and approaches, fostering a global network of knowledge-sharing and collaboration.
Conclusion:
Ovarian cancer poses significant clinical challenges, but with advances in diagnostics, treatment modalities, and regulatory frameworks, there is hope for improved outcomes and a brighter future for those affected by this disease.
Browse Through More Oncology Diseases Research Reports.
Related Reports:
Diverticulitis: A Complete Guide to the Symptoms, Causes, and Treatments
When it comes to strategic Diabetes Disease consultancy, some of the areas we assist you understand include Regulatory Insights, Disease Landscape, and Market Access Expertise.
Find treatments for HPV illness using specialized market entry strategies. FDA/EMA insights and clinical trial advice. Examine right away!
Learn about specific approaches to Pancreatic Cancer Disease market access, pricing, and reimbursement. Learn about market research and clinical trials. Change your business immediately.
Learn about KOLs, the FDA, epidemiology, price reimbursement, and more in this market report on Anemia Disease. Your trustworthy source for info on anemia. Examine right away!
#clinical assessment#diagnostic analysis#market trends analysis#regnal insights#treatment analysis#disease#lung cancer#branding#economics#editorial design
1 note
·
View note
Text
Unlocking Success in Clinical Trials: The Role of Contract Research Organizations (CROs)
In the dynamic world of pharmaceuticals, biotechnology, and medical research, the journey from concept to market-ready product can be both intricate and time-consuming. This is where Contract Research Organizations (CROs) step in as invaluable partners, streamlining the path to success for countless companies and research initiatives. In this blog, we'll delve into the world of CROs and understand why they are essential players in the realm of clinical trials, drug development, and research solutions.
What is a Contract Research Organization (CRO)?
A Contract Research Organization, often referred to as a CRO Pharma, is a specialized company that provides a wide range of research and development services to pharmaceutical, biotechnology, and medical device companies, as well as academic institutions and government agencies. These organizations act as strategic partners, offering expertise, infrastructure, and resources to expedite the development of new drugs, therapies, and medical innovations.
The Key Roles of CROs
Clinical Trials Management: One of the primary roles of CROs is to manage clinical trials efficiently. They handle various aspects, including patient recruitment, site selection, regulatory compliance, data collection, and monitoring. This expertise ensures that trials are conducted rigorously and in compliance with industry standards and regulations.
Regulatory Expertise: Navigating the complex landscape of regulatory requirements is a daunting task. CROs possess in-depth knowledge of regulatory guidelines and can help companies navigate the intricacies of approval processes with regulatory agencies like the FDA, EMA, and others.
Data Management: Data is the lifeblood of clinical trials and research. CROs employ advanced data management and analysis tools to ensure the accuracy, integrity, and security of data collected during trials. This is crucial for drawing meaningful conclusions and making informed decisions.
Scientific Expertise: CROs often house a diverse team of scientific experts, including pharmacologists, statisticians, clinicians, and other specialists. Their collective knowledge and experience contribute to the successful execution of research projects.
Resource Optimization: By outsourcing various research functions to CROs, companies can focus their resources on core competencies, thereby reducing overhead costs and accelerating project timelines.
Why Choose a CRO?
Choosing a CRO as a partner offers several advantages:
Cost Savings: CROs operate with efficiency, reducing the cost of research and development.
Speed to Market: CROs streamline the research process, helping companies bring new products to market faster.
Access to Expertise: CROs provide access to specialized expertise and resources that may not be available in-house.
Risk Mitigation: With their experience and knowledge, CROs help mitigate risks associated with research and development, ensuring smoother project execution.
Conclusion
Contract Research Organizations are the unsung heroes behind many breakthroughs in medicine and healthcare. Their dedication, expertise, and commitment to advancing scientific knowledge make them indispensable partners for companies and institutions striving to improve human health. By collaborating with CROs, researchers and innovators can turn their visions into reality, bringing new treatments and therapies to those who need them most.
visit - https://pihealthsciences.com/cro-solutions
0 notes
Text
Unlocking the Keys to Massive Commercial Success in Pharma: Europe's Untapped Goldmine!
Europe's pharmaceutical market is vast and diverse, offering significant commercial potential for pharmaceutical companies. However, tapping into this potential requires a strategic approach tailored to the complexities of the European landscape. In this blog, we will explore key strategies and techniques that pharmaceutical companies can employ to unlock their commercial potential in Europe.
Read Full Blog Here: https://www.anervea.com/pharmas-untapped-goldmine-in-europe-unleashing-the-secrets-to-massive-commercial-success
Tailored Market Entry Strategies
Europe is not a one-size-fits-all market. Each European country has its unique healthcare system, regulatory environment, and patient demographics. Successful pharmaceutical companies customize their market entry strategies for each country, considering factors such as pricing, reimbursement policies, and market access pathways. They adapt their approaches to align with local regulations while addressing specific healthcare needs.
Innovative Product Development
Innovation is a driver of success in the pharmaceutical industry. To stand out in the European market, companies must focus on developing innovative medications and therapies that address unmet medical needs or offer superior alternatives to existing treatments. Investing in research and development (R&D) and clinical trials within Europe can also enhance a company's reputation and credibility.
Strategic Partnerships and Alliances
Collaboration is a powerful tool for success in Europe. Forming strategic partnerships and alliances with local pharmaceutical companies, research institutions, and healthcare providers can provide invaluable access to local expertise, networks, and market insights. These partnerships can facilitate faster market entry and growth.
Market Access Optimization
Understanding the intricacies of each European country's pricing, reimbursement, and market access processes is essential. Pharmaceutical companies must work closely with healthcare authorities to ensure that their products are accessible and affordable. Demonstrating the economic value of medications through real-world evidence and economic evaluations can be instrumental in gaining approval and reimbursement.
Patient-Centric Approach
Putting patients at the center of commercial strategies is a winning approach. Develop patient-centric solutions and support programs that enhance patient outcomes and adherence to treatment plans. Educate patients about their conditions and treatment options, fostering trust and loyalty.
Regulatory Expertise
Navigating the regulatory landscape in Europe requires a deep understanding of European Medicines Agency (EMA) guidelines and country-specific regulations. Stay up-to-date with evolving pharmaceutical regulations and compliance requirements to expedite approvals and market entry.
Data-Driven Decision Making
Data analytics is a valuable tool for gaining insights into market trends, patient preferences, and physician behaviors. Employ data-driven decision-making processes to inform commercial strategies, optimize marketing efforts, and target the right healthcare providers and patients effectively.
Unlocking commercial potential in Europe requires a multifaceted approach that combines tailored market entry strategies, innovation, strategic partnerships, market access optimization, patient-centricity, regulatory expertise, and data-driven decision making. Pharmaceutical companies that employ these key strategies and techniques are well-positioned to thrive in the diverse and dynamic European pharmaceutical landscape. The opportunities in Europe are abundant, and success is within reach for those willing to embrace the complexities and nuances of this thriving market.
Visit our website now: https://www.anervea.com/

#healthcare#pharmaceutical industry#data analytics#pharmasales#patient-centric#european market#marketsegmentation#Digital Transformation#Artificial Intelligence
0 notes