#Intramedullary Nailing System
Text
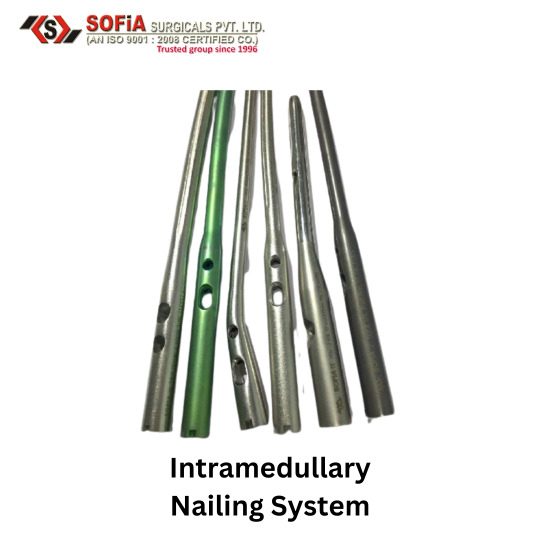
Intramedullary Nailing System
For more detail visit our website: www.sofiasurgicals.com
Call us or whatsapp on +919015555501
Email - [email protected]
#Intramedullary Nailing System#For more detail visit our website: www.sofiasurgicals.com#Call us or whatsapp on +919015555501#Email - [email protected]#orthopedicplates#surgicalinstruments#orthopedicsurgery#orthopedicsurgeon#orthopedicscrews#boneplate#orthopedic#orthopedics#orthopedicdoctor#lockingplates#orthoimplants#orthopedicimplants#orthoimplant#orthoimplantegroup#orthopedicimplant#surgicalimplant#ortho#lockingplate#bonefracture#bonefractures#surgicalimplants#orthopaedicimplant#orthopedicinstruments#dhsplate#titaniumimplant#medicalequipment
1 note
·
View note
Link
With 37 plates within 9 plate families addressing both Tri-malleolar and intra-articular fracture patterns, DJO Global’s Arsenal Foot Plating System is designed with the proven technology and expands offerings to address both tri-malleolar and intra-articular fracture patterns. To know more visit https://www.djoglobal.com/ or call us at 1.800.321.9549.
#Arsenal Ankle Plating System#Star Total Ankle Replacement#medical device companies#Foot and ankle training#Foot and ankle journals#intramedullary nail fixation#orthopedic medical device companies
1 note
·
View note
Text
Osteosynthesis Devices Market| Analysis and Forecast, 2024 – 2028
Originally published on Technavio: Osteosynthesis Devices Market Analysis North America, Europe, Asia, Rest of World (ROW) - US, Canada, Germany, UK, China - Size and Forecast 2024-2028
The global osteosynthesis devices market is anticipated to witness substantial growth across major regions, including North America, Europe, Asia, and the Rest of the World (ROW). A comprehensive analysis for the period 2024-2028 provides insights into market trends and factors influencing the industry, with a specific focus on major countries such as the United States, Canada, Germany, the United Kingdom, and China.
In North America, the osteosynthesis devices market is poised for robust expansion, driven by factors such as the increasing prevalence of orthopedic conditions, a growing aging population, and advancements in surgical techniques. The United States and Canada play pivotal roles in the regional market, with a high demand for osteosynthesis devices used in fracture fixation and orthopedic surgeries. The region benefits from a well-established healthcare infrastructure and a strong emphasis on technological innovations in medical devices.
Europe stands as a significant player in the global osteosynthesis devices market, with countries like Germany and the United Kingdom contributing significantly. The European market dynamics are shaped by factors such as the rising incidence of bone fractures, favorable reimbursement policies, and a strong presence of key market players. Germany, known for its advanced healthcare system and research capabilities, is a key market for osteosynthesis devices, including plates, screws, and intramedullary nails.
Asia is emerging as a promising market for osteosynthesis devices, with China at the forefront of adoption. The region's market growth is influenced by factors such as a large and aging population, an increase in trauma cases, and improving healthcare infrastructure. China, in particular, is witnessing a surge in orthopedic surgeries and a growing demand for innovative osteosynthesis devices to address various musculoskeletal conditions.
The Rest of the World (ROW) region, which includes regions outside North America, Europe, and Asia, is also contributing to the growth of the osteosynthesis devices market. Countries in this region are witnessing advancements in healthcare infrastructure and an increasing focus on orthopedic surgeries, leading to a rising demand for devices that aid in fracture fixation and bone healing.
To Learn deeper into this report , View Sample PDF
In summary, the global osteosynthesis devices market is experiencing dynamic growth across key regions, with a focus on North America, Europe, Asia, and the Rest of the World. The market dynamics in the United States, Canada, Germany, the United Kingdom, and China play crucial roles in shaping the industry landscape during the forecast period from 2024 to 2028. The increasing prevalence of orthopedic conditions, advancements in surgical techniques, and the aging population contribute to the positive trajectory of the osteosynthesis devices market globally.
For more information please contact.
0 notes
Text
Advanced Fracture Stabilization Techniques: A Comprehensive Guide to Treatment in Colony, Texas by MySpecialtyMD
Introduction:
Welcome to MySpecialtyMD's comprehensive guide on advanced fracture stabilization techniques, focusing on cutting-edge treatments available in Colony, Texas. Fractures can be debilitating, and proper stabilization is crucial for optimal recovery. In this article, we will delve into the latest advancements in fracture treatment, emphasizing the specialized care provided by MySpecialtyMD in the Colony area. We'll also explore neighboring areas, including Castle Hill, Frisco, Kings Ridge, and Plano, to highlight the best hospitals and referral options for fractures stabilization treatment.
Understanding Fractures:
Fractures, commonly known as broken bones, can result from various causes such as accidents, falls, or sports injuries. The severity of fractures varies, ranging from simple fractures to complex, multi-fragmented breaks. Effective treatment is essential to ensure proper healing and restoration of function.
Initial Assessment:
MySpecialtyMD employs a meticulous approach to fracture care, beginning with a thorough initial assessment. Advanced imaging techniques like CT scans and MRIs are utilized to precisely diagnose the extent and nature of the fracture. This detailed evaluation forms the basis for developing a personalized treatment plan.
State-of-the-Art Fracture Stabilization Techniques:
Minimally Invasive Surgery:
MySpecialtyMD specializes in minimally invasive surgical techniques for fracture stabilization. This approach involves smaller incisions, reduced tissue damage, and faster recovery times compared to traditional open surgery. It is particularly beneficial for fractures in delicate areas or those requiring precise alignment.
Intramedullary Nailing:
Intramedullary nailing is a technique where a metal rod is inserted into the marrow canal of the bone, providing internal stabilization. This method is frequently used for long bone fractures and allows for early mobilization and weight-bearing.
Plate Fixation:
MySpecialtyMD employs advanced plate fixation systems to secure fractured bones. These plates, made of durable materials, are designed to provide stability and support during the healing process. The use of locking plates ensures a secure fit and minimizes the risk of complications.
External Fixators:
In certain complex fractures, external fixators may be utilized. These devices, attached externally to the bone, assist in maintaining proper alignment during the healing process. MySpecialtyMD employs the latest designs that are both effective and patient-friendly.
Postoperative Care and Rehabilitation:
Following surgery, MySpecialtyMD focuses on comprehensive postoperative care and rehabilitation. This includes physical therapy, pain management, and regular follow-up appointments to monitor the healing progress. The goal is to facilitate a smooth recovery and restore the patient's optimal function.
Best Hospitals and Referrals:
When seeking fractures stabilization treatment in Castle Hill, Frisco, Kings Ridge, or Plano, MySpecialtyMD stands out as a leading choice. The expertise and innovation offered by MySpecialtyMD make it the best hospital for fractures stabilization treatment in Frisco, ensuring a swift and successful recovery. Additionally, for fractures referrals treatment hospital in Plano, MySpecialtyMD provides specialized care and personalized treatment plans to meet the unique needs of each patient.
Conclusion:
MySpecialtyMD in Colony, Texas, is at the forefront of advanced fracture stabilization techniques, providing patients with cutting-edge care tailored to their unique needs. If you or a loved one is facing a fracture, trust in the expertise and innovation offered by MySpecialtyMD for a swift and successful recovery. Your journey to healing begins with the leaders in advanced fracture treatment in Colony, Texas, and the surrounding areas.
For more information please visit www.MySpecialtyMD.com
0 notes
Text
A Comparative Overview of the Precice 2 and Precice Stryde Methods
Limb lengthening surgery has come a long way in providing life-changing solutions to individuals with limb length discrepancies. Among the remarkable innovations in this field, the Precice 2 and Precice Stryde methods have garnered significant attention.
Precice 2 Method
The Precice 2 method represents a significant milestone in limb lengthening surgery. Developed by Ellipse Technologies, now part of NuVasive Specialized Orthopedics, this technique utilizes an internal nail system. Surgeons make a small incision and insert a telescopic intramedullary nail into the bone. This nail contains a magnetic component, allowing for non-invasive, precise lengthening through an external remote control device. Patients can conveniently adjust the length of their limb by simply turning the controller.
One of the key advantages of the Precice 2 method is its minimally invasive nature. This results in reduced scarring, quicker recovery times, and decreased risk of infection. Additionally, the adjustable feature of the nail allows for fine-tuned adjustments, enhancing the overall control of the lengthening process. However, it’s important to note that the Precice 2 method may require a separate procedure for nail removal after the lengthening is complete.
Precice Stryde Method
The Precice Stryde method is a more recent advancement in limb lengthening surgery, also developed by NuVasive Specialized Orthopedics. It builds upon the success of the Precice 2 method with several notable improvements. In this approach, a motorized, telescopic intramedullary nail is implanted into the bone. What sets the Stryde method apart is its groundbreaking magnetic technology, which enables continuous, remote-controlled lengthening.
One of the primary advantages of the Precice Stryde method is the absence of the need for a separate surgery to remove the nail. The nail is designed to be fully reversible, eliminating the inconvenience of a secondary procedure. Furthermore, the continuous lengthening feature allows for smoother adjustments and potentially shorter overall treatment times compared to the Precice 2 method.
Comparative Analysis
When considering the Precice 2 and Precice Stryde methods, it’s crucial to weigh their respective advantages and disadvantages. Both techniques offer a significant improvement in the quality of life for patients with limb length discrepancies. The Precice 2 method boasts a track record of success with its minimally invasive approach and adjustability, while the Precice Stryde method offers the convenience of continuous, remote-controlled lengthening and simplified removal.
0 notes
Text
A Comprehensive Comparison of Precice 2 and Precice Stryde Methods
Limb lengthening surgery is a remarkable medical procedure designed to address various orthopedic conditions, such as limb length discrepancies, congenital deformities, and post-traumatic injuries. Over time, medical advancements have led to the emergence of innovative techniques, with the Precice 2 and Precice Stryde systems at the forefront of these developments.
Precice 2 Method
The Precice 2 method stands as a pioneering limb lengthening technique that offers several advantages over traditional approaches. It employs an intramedullary nail, typically inserted into the femur or tibia bone. The hallmark of the Precice 2 system is its remote-controlled magnetic mechanism, enabling precise and gradual bone lengthening.
The surgical procedure involves a minimal incision to insert the intramedullary nail and attach an external remote control. Patients can adjust the lengthening process under the guidance of their surgeon by turning the magnetic mechanism. This gradual approach significantly reduces pain compared to older methods and minimizes the risk of complications, such as nerve damage. Furthermore, the Precice 2 system provides real-time feedback, ensuring a safer and more accurate procedure.
Precice Stryde Method
The Precice Stryde method represents the pinnacle of limb lengthening technology. Like the Precice 2 system, it employs an intramedullary nail, but with a notable difference. The Precice Stryde nail is thinner yet stronger, reducing the risk of complications and improving patient comfort during the lengthening process.
A standout feature of the Precice Stryde system is its enhanced weight-bearing capacity. This enables patients to start walking with partial weight bearing earlier than with previous methods, leading to improved rehabilitation and overall quality of life during recovery. The Precice Stryde method is particularly advantageous for individuals with complex limb lengthening needs and those seeking a more efficient and comfortable experience.
Comparison and Conclusion
Both the Precice 2 and Precice Stryde methods mark significant advancements in limb lengthening surgery. They provide patients with the opportunity to achieve their desired limb length with greater precision, reduced discomfort, and enhanced overall outcomes. While the Precice 2 method offers remote control for precise adjustments and real-time feedback, the Precice Stryde method excels in strength, comfort, and quicker weight-bearing capabilities.
The choice between these two methods may depend on the patient’s unique requirements and the surgeon’s recommendations. It is crucial to consult with a skilled orthopedic surgeon who can evaluate individual circumstances and determine the most suitable approach.
0 notes
Text
A Comprehensive Overview of Precice 2 and Precice Stryde Methods
Limb lengthening surgery is a medical procedure designed to address various orthopedic conditions, such as limb length discrepancies, dwarfism, and deformities caused by congenital conditions or injuries. Over the years, advancements in medical technology have led to the development of innovative limb lengthening methods, including the Precice 2 and Precice Stryde systems.
Precice 2 Method
The Precice 2 method is a state-of-the-art limb lengthening technique that offers several advantages over traditional methods. This system utilizes an intramedullary nail that is surgically implanted into the bone, typically in the femur or tibia. The key component of the Precice 2 system is its remote-controlled magnetic mechanism, which allows for precise and gradual bone lengthening.
The surgical procedure involves making a small incision to insert the intramedullary nail and attach an external remote control. Patients can then adjust the lengthening process themselves, following the surgeon’s guidance, by turning a magnetic mechanism. This gradual process is less painful than older methods, and it minimizes the risk of complications such as nerve damage. Furthermore, the Precice 2 system provides real-time feedback to both the patient and the surgeon, enhancing safety and accuracy.
Precice Stryde Method
The Precice Stryde method represents the latest evolution of limb lengthening technology. Like the Precice 2 system, it also employs an intramedullary nail. However, the Precice Stryde nail is notably thinner and stronger, reducing the risk of complications and improving patient comfort during the lengthening process.
One of the standout features of the Precice Stryde system is its enhanced weight-bearing capacity. This allows patients to begin walking with partial weight bearing sooner than with previous methods, which can significantly improve rehabilitation and overall quality of life during the recovery period. The Precice Stryde method is particularly beneficial for individuals with complex limb lengthening needs and those seeking a more efficient and comfortable experience.
Comparison and Conclusion
Both the Precice 2 and Precice Stryde methods represent significant advancements in the field of limb lengthening surgery. They offer patients the opportunity to achieve their desired limb length with greater precision, reduced pain, and improved overall outcomes. While the Precice 2 method provides remote control for precise adjustments and real-time feedback, the Precice Stryde method excels in its strength, reduced discomfort, and quicker weight-bearing capabilities.
Ultimately, the choice between these two methods may depend on the patient’s specific needs and the surgeon’s recommendation. It is essential to consult with a qualified orthopedic surgeon who can assess individual circumstances and determine the most suitable approach.
0 notes
Text
What Are Femur Fractures? A Detailed Guide

Severe femur fractures like open fractures or comminuted fractures require external fixation. This is because such cases cannot be managed with ORIF. An external fixation system is the option for treatment in such cases. Here, the orthopedic surgeon will hold bone fragments using pins, orthopedic plates, rods, and bone screws and stabilize those implants to an external frame. This frame remains outside the body. In such conditions, a bone graft may also be used to compensate for the lost bone because of the fracture.
Siora Surgicals Pvt. Ltd. is an experienced and one of the oldest orthopedic implants manufacturers in India. Operating for over 30 years, the company produces a CE-certified range of orthopedic implants and instruments including external fixation systems, intramedullary nails, orthopedic implant plates, and more. We are also an experienced OEM/contract manufacturing service provider across the globe.

0 notes
Text
The particular growing tasks associated with GCN5L1 within mitochondrial along with vacuolar organelle the field of biology
Following therapy using imipenem and tobramycin and also extensive debridement, your skin lesions improved slowly. A. baumannii will be these days an essential source of nosocomial attacks, specifically in intensive treatment units.Relaxin offers earlier recently been examined in rodent hurt recovery designs and been proven to market angiogenesis also to rate recovery. However, pigs have been shown to be described as a greater design regarding human skin within skin care research, thus juvenile pigs were selected for a study associated with scar tissue lowering as well as cosmetic visual appeal. A dozen 20- through 6-mm excisional wounds are created being worn by just about all creatures. Relevant products involving relaxin together with 3, Zero.Your five, as well as Only two.Five mg/mL have been utilized twice daily pertaining to months 2-3 after which day-to-day for several weeks 3-6 in all pets. Furthermore, a number of pets gotten systemic relaxin, that was administered by way of infusion pumps for a price of 125 mu g/kg associated with system weight/day. Checks regarding therapeutic as well as plastic visual appeal were made by way of a health-care professional with days Only two, Four, along with Some. DNQX mw had been accumulated from About six weeks as well as looked at histologically regarding granulation muscle, irritation, as well as collagen organization. Pains inside pets acquiring endemic relaxin acquired a better physical appearance using significantly less inflammation, reduced granulation muscle, reducing quantities of swelling. These people confirmed any more-well-knit collagen framework compared to regulates. Injuries helped by topical cream products would not show advancement above handles. Your topical cream ingredients used was discovered to experience a quick home occasion, that likely restricted transmission regarding relaxin. Reformulated relaxin formulations using improved transmission could possibly be valuable as a topical cream strategy for wounds to prevent as well as minimize scarring.In the randomised test concerning 598 people together with 600 trochanteric breaks in the fashionable, the actual cracks have been addressed with the sliding fashionable twist (d Equates to Three hundred) or a Targon PF intramedullary toe nail (d = More than 200). The actual suggest age of the actual sufferers was 82 a long time (Twenty six in order to One hundred and four). Just about all enduring people had been examined in twelve months using practical result examined by the research health professional distracted for the remedy utilised. The intramedullary toe nail was discovered to possess a slightly improved indicate operative moment (46 min's (SD Twelve #link# .Three) versus 1949 moments (thus A dozen.6), r < 3.001) as well as an increased suggest radiological testing time (3.Three or more moments (SD Zero.Only two) versus 2.Five minutes (SD 0.3), r < 2.001). Operative troubles had been more widespread with all the intramedullary toenail. There wasn't any in past statistics significant difference among implants regarding injure recovery complications (p Equates to One particular), as well as requirement for post-operative bloodstream transfusion (s Is equal to One), along with medical issues had been likewise distributed in groups.
#Compstatin#Lonidamine#Tipifarnib#GSK461364#Brigatinib#Pralsetinib#Eribulin#SR-717#LY364947#Hydroxyurea#Tauroursodeoxycholic#SB590885#ARS-1620#XL413#ML162#SEL120#Vandetanib#VPS34 inhibitor 1#PF-04418948#BI-2852#BT5#GDC-1971#DNQX#(R#S)-3#5-DHPG#FINO2#Apatinib
0 notes
Text
0 notes
Text
Orthopedic Trauma Devices Market Segmentation By Product Type, End-User, Vendor Analysis, Top-Vendor Offerings 2027
Orthopedic Trauma Device Market Overview :
The global market for orthopedic trauma devices is projected to register CAGR of 8% during the forecast period (2015-2022), as predicted by Market Research Future (MRFR). Increasing number of trauma associated with road accidents and other causes is expected to fuel the market growth.

Rising geriatric population also aides the growth of the orthopedic trauma devices market, as people in this age group are highly prone to bone fractures resulting from fall injury and other orthopedic complications.
It has also been observed that an increasing number of people are getting interested in some form of sport, owing to increasing awareness about one’s health. This has resulted in an accelerated number of injuries associated with sport, thus having a knock-on effect on the global market size. Moreover, a handful of companies are involved in the development and marketing of orthopedic trauma devices, thereby leading to the market to evolve with growth opportunity.
But the market is not without its challenges as poor healthcare infrastructure in few developing economies impedes the said market growth. However, looking at the bright side, the industry is discovering new applications in orthopedics on the back of advances in 3D printing. Subsequently, 3D printed implants are trending rapidly across the globe. Also, the market is apprehended to attain massive revenues in coming years due to another market trend, namely reverse shoulder arthroplasty.
Orthopedic Trauma Device Market Segmentation :
The global orthopedic trauma device market is segmented on the basis of material type, product type and end-users.
The material types in the market are bio-absorbable materials, non-absorbable materials and others. The applications of bio-absorbable implants in orthopedic surgery are primarily mandated from the need to eliminate implant removal operations, thus gaining widespread popularity among orthopedic surgeons. Consistent development and product enhancement have given significant push to the bio-absorbable materials segment in the global market.
The product types in the global market are screws, plates, patient specific implants and others. The market for screws is expected to retain a massive share of the market due to favorable reimbursement policies and its wide array of applications in orthopedic surgeries. Moreover, benefits of orthopedic screws make them highly favorable, such as non-interference with MRI, decreased incidence of graft laceration and do not need implant removal. The end-users in the global market include hospitals, rehabilitation centers, clinics and others.
Orthopedic Trauma Device Market Regional Analysis :
Globally, North America currently occupies the largest market for global orthopedic trauma devices market and is bound to secure its top position in the global market throughout the forecast period. Soaring use of bio-absorbable plates and screws is mainly fuelling the orthopedic trauma devices market in the region. Also, the region is witnessing robust sales of hybrid plates and screws, which will work in favor of the market growth in coming years.
On top of that, intramedullary nails are steadily gaining traction in the majority of orthopedic surgeries owing to their increasing popularity as an ideal orthopedic trauma device for various anatomies, in the region.
Find Sample Report @ https://www.marketresearchfuture.com/sample_request/2080
Closely following the North America region stands the region of Europe, securing the second position in the global orthopedic trauma devices market. Trending incorporation of robotics technology during orthopedic surgeries is presumed to push the market in the region. The market also thrives on the back of constantly flourishing medical industry with well-established healthcare infrastructure.
According to the report, the Asia Pacific region is projected to be the fastest growing market. On the backdrop of an expanding market in developing nations in the region, flourishing medical tourism will continue to trigger the market for orthopedic trauma devices. Moreover, growing preference for minimally invasive fixation is expected to provide a tremendous thrust to the regional market as well. Growing geriatric population and increasing number of cases of injuries and road accidents also help the market captivate the region to a large extent.
The Middle East and Africa markets are exhibiting a positive outlook in terms of market expansion. This can be attributed to manufacturers consistently investing in research and development (R&D) activities to develop innovative and efficient devices, to cater to the growing demand.
Large number of R&D activities is presumed to ensure enhanced growth opportunities during the forecast period. Moreover, increasing awareness regarding availability of innovative products among patients is pushing the market to higher levels in the region.
Orthopedic Trauma Device Market Key Players :
Some of the key players in this market are: Invibio (UK), BIOTEK (India), DePuy Synthes Companies, Ortho Max Manufacturing Company Pvt. Ltd., Auxein Medical (India), Stryker, Johnson & Johnson Services, Inc. (US), Smith & Nephew, MEDTRONIC, B. Braun Melsungen AG and others.
Orthopedic Trauma Device Market Developments :
In June 2018, CoreLink acquired Expanding Orthopedics, a privately held medical device developer. The acquisition provides CoreLink with many benefits including growth in the inter-body product category along with growth in the portfolio of innovative orthopedic technology for advanced spine care. The acquisition will also boost the appeal of CoreLink’s recently launched FLXfit and FLXfit 15 titanium interbody systems.
Access Report @ https://www.marketresearchfuture.com/reports/orthopedic-trauma-devices-market-2080
#Orthopedic Trauma Devices Market Share#Orthopedic Trauma Devices Market Size#Orthopedic Trauma Devices Market Overview
1 note
·
View note
Photo

India's top orthopedic implant company, offering widest range of approved orthopedic implants including bone plates, bone screws, intramedullary nails, locking plate system, spinal implants, etc.at lowest prices. Send Your Buy Requirement For "Orthopaedic Implants & Instruments."
Visit - https://miraclus.com/instruments/
#Orthopedic Plates and Screws#Orthopedic Surgery#Plates Used for Fractures#Medical Instruments Manufacturers#Surgical Plates and Screws
1 note
·
View note
Text
Lupine Publishers | Outcomes of Distal Femur Non-Union Following Lateral Locked Plating Treated withan Addition of A Medial Locking Plate and Autogenous Bone Graft

Lupine Publishers | Orthopedics and Sports Medicine
Abstract
Background: Distal femur non-unions are difficult to treat and can result in chronic pain, significant disability as well as delayed return to preinjury activity functional status. Addition of medial locking plate and autogenous bone grafting adds biomechanical stability, prevents varus collapse and implant failure, and decreases the morbidity associated with non-union. We evaluated results of addition of medial locking plate and bone grafting in aseptic distal femur non-union with stable lateral implant.
Methods: Between 2009 and 2019, we retrospectively reviewed 14 cases of clinically and radiologically established aseptic distal femur non-union treated by single stage procedure involving addition of medial locking plate and autogenous bone grafting. The fractures were classified according to the AO classification system was used for distal femur fractures. Patients were regularly followed-up for a minimum period of 12 months for clinico-radiological signs of union, functional outcome and any complications associated with it.
Conclusion: Timely medial locking plate augmentation and bone grafting done is an effective procedure to achieve union and prevent failure of the already present lateral implant in distal femur nonunion
Level of Evidence: Therapeutic Level III.
Keywords: Distal Femur Fracture; Non-Union; Medial Plating; Autogenous Bone Grafting
MeSH Terms: Osteosynthesis, Distal Femur, Non-Union, Plates, Bone Graft
Introduction
Fractures of the distal third of the femur account for 4% to 6% of femur fractures and are a treatment challenge for orthopaedic surgeons despite new fixation options[1]. Fixed angle locking plates have become the most commonly used device for this indication replacing intramedullary nails, blade plates and condylar screws[1]. The biomechanical properties of locked plate designs make them attractive alternatives to conventional plates. Locked screws augment the stability of the construct by eliminating motion at the plate-bone interface providing greater pull-out strength[2,3]. The development of screw torque and plate-bone interface friction is unnecessary with locked plate designs, significantly decreasing the amount of soft tissue dissection required for implantation, preserving the periosteal blood supply[4]. Excellent stability provided by locking plates and minimally invasive biologically friendly insertion should lead to improved healing rates. Unfortunately, clinical experience and some reports in the literature indicate that fracture healing may not be better than that achieved with previous methods of fixation[4-11].Non-union rates ranging from 0% to 19% have been reported in the literature[10]. Difficulties with fracture healing in the distal femur may lead to poor quality of life, plate bending, plate fracture, plate pull-off and locking screw failure. Fractures treated with lateral locking plates that fail to heal usually maintain alignment and generate less callus, suggesting that callus inhibition because of overly rigid fixation rather than hardware failure is the primary problem[11-32].
We believe the augmentative medial plating and autogenous bone grafting done for healing problems associated with stable locked lateral distal femur plating provides greater stability leading to a successful union and prevent failure of the primary lateral implant. However, to the best of our knowledge, there is less literature available on non-union of distal femur treated with locking medial plate and autogenous bone grafting. We, therefore, sought to determine [1]the preliminary results of the non-union of the distal femur with an in situ stable locking lateral plate after treatment with the addition of a locking medial plate and autogenous bone grafting, and [2] any complications associated with the treatment.
Materials And Methods
A retrospective clinical evaluation of non-unions of distal femur fractures with an in situ stable lateral locking plate, treated by medial plate augmentation and autogenous bone grafting at was performed in our institute, a National Board of Examinations, India accredited teaching institute. We identified from the hospital data, that between 2009 and 2019, 14 patients of distal femur non-union following locked lateral plating of distal femur identified were treated by augmentative locking medial plate and autogenous bone grafting at a mean of 7.2 months after the primary surgery (range 5 months to 14 months). This study was approved by our institutional review board.In our institution, distal femoral fractures treated by locked lateral plating, not showing expected radiological and clinical signs after three months are kept non-weight bearing and strictly followed for next consecutive three months, for clinical and radiographic signs of progression to healing. Patients with persistent limp, pain and showing no clinical or radiographic signs of progression to healing on plain radiographs or CT (computed tomography) scan, the fracture is considered to be non-united. Inclusion criteria included skeletally mature patient above 18 years of age, absence of infection, a stable lateral locking plate with distal femur nonunion and acceptable alignment after previous/primary surgery. Patients excluded were those with infection, skeletally immature patients. None of the patients had prior treatment for non-union. Two patients reported to our institution with established non-union following surgery elsewhere, and non-union was diagnosed during the routine follow up in 12 patients operated in our institution. Preoperatively, all the patients had disability and pain with twelve of the patients was non-weight-bearing and two were partially weight-bearing on the injured side. The presence of an infected non-union was carefully scrutinized in all patients by clinical evaluation for signs of infection and biochemical markers including complete blood count, erythrocyte sedimentation rate, and C-reactive protein.Five fractures were primarily closed injuries and 9 were open injuries which were, grade I [2], grade II [2], grade III [5]-type a[2], type B [3] according to the Gustilo-Anderson classification system. The surgical procedure was performed by same qualified orthopaedic surgeon involved careful dissection and elevation of medial soft tissues with either medial parapatellar or subvastus approach, packing the non-union site with autogenous bone graft obtained from the posterior iliac crest and fixation using medial locking plate and screws.Information obtained for each patient included patient demographics, injury details (Table 1), type of fracture, soft tissues at the time of original injury (closed vs open), details of prior surgeries, type of non-union (atrophic, oligotrophic, hypertrophic), lateral and medial implant details, duration between the lateral locking plating and the secondary procedure, range of movements at the knee, pain score and ambulatory status before and after the surgery,postoperative complications (Table 2, 3). Our prime outcome measures were union time, weight-bearing ability, range of knee movements. Secondary outcome measures were pain score measured on Visual Analogue Scale (VAS) and postoperative complications.The patients were followed up in the outpatient department (OPD) at monthly intervals for clinical and radiological assessment. The fracture was considered united when the radiographs demonstrated bridging callus across the fracture site along three of the four cortices and the patient could bear full weight without any assisting device and pain. Functionalthe outcome was assessed using LEFS (lower extremity functional scale). The pain score, final weight-bearing ability and range of knee movements were recorded when the fracture was considered to be united. Any complications such as superficial or deep infection, neurovascular complications, mechanical failure of the implant, and absence of bone healing were noted during the follow-up period.
Statistical Data Analysis
Descriptive analysis was carried out by the mean and standard deviation for quantitative variables, N and proportion for categorical variables. All Quantitative variables were checked for a normal distribution within each category of an explanatory variable by using visual inspection of histograms and normality Q-Q plots. Shapiro-wilk test was also conducted to assess normal distribution. Shapiro-wilk test p-value of >0.05 was considered as a normal distribution.For normally distributed Quantitative parameters the mean values were compared between study groups using Independent sample t-test (2 groups) and ANOVA test for more than two groups and P-value < 0.05 was considered statistically significant. IBM SPSS version 20 was used for statistical analysis.
Results
Out of 12 patients treated in our hospital, 2 patients had a 33A2 fracture, 8 patients had 33C2 fractures and 2 patients had 33C3 fracture according to the AO classification. Nine holes to thirteen holes lateral locking plates were used for primary fixation. None of the patients received any bone graft during primary surgery. 1/14 (7.1%) patients had a history of diabetes, while there was no history of smoking in any patient.One patient (Figure 1), case 10, a simple fracture treated for a peri-prosthetic fracture following total knee replacement done at our hospital, did not show any signs of healing after 8 months. In 6 compound fractures, wounds could be closed primarily, and three grade 3B compound fractures required secondary skin grafting which was done 48 hours after the primary surgery. Four patients with compound injuries had associated compound tibia fractures which were treated by primary nailing in two cases and primary plating in two cases. Repeated debridement and gastrocnemius flap coverage and skin grafting was done for one compound tibia fracture treated with a plate [8].In this study, non-union was confirmed on plain radiographs in six cases, and the combination of CT scan and plain radiographs established the nonunion in 8 cases. In one case, due to the obvious radiolucent line on x-rays at 5 months, the diagnosis of non-union was considered and augmentative medial plating and bone grafting was done. All non-unions were oligotrophic in nature. None of the patients had an intra-articular non-union. Persistent pain and the limp were present in all the patients. Twelve patients were not bearing weight, and 2 patients were bearing partial weight with the help of a stick. Visible motion at the non-union site in [13] cases with varus/valgus stressing was observed under fluoroscopy intraoperatively. Medial sub vastus approach was used for the exposure of non-union site in 10 patients with more than 90/100 degree range of knee movements and medial para-patellar approach was used in 4 patients who had limited range of movements of the knee and required release the intra-articular adhesions. All plates used for medial augmentation were made of stainless steel. Autogenous iliac bone graft was added in all cases with the aim to stimulate local osteogenic activity and increase in stability with the addition of medial locking plate. During our follow-up period which was in average 2.1 years (range 12 months to 84 months), the union was achieved in all patients at a mean of 5 months (range 4-7months). Only subtle improvement in the range of motion of the knee (mean 9.2 degrees) was noted. Patients had a good functional outcome with an average LEFS score of 71 (50 to79). One patient [7] developed a deep infection after six years of the surgery and was managed with debridement and removal of both medial as well as lateral implants.
For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
5 notes
·
View notes
Link

Multifix Nails are designed to fit in Intramedullary Canal. These are used in the fixation of Proximal, Shaft, and Distal fractures of the Femur and Tibia. The system is the constitution of Multifix Tibial Cannulated and Unreamed Nails & ...
2 notes
·
View notes
Text
Best Orthopedic Doctor for Fracture Surgery
Intramedullary nailing
Intramedullary nailing is a surgery done to repair a broken bone to keep it stable. This procedure of fixing the fractures is mostly used for thigh, shin, hip, and upper arm.
Bone plates
Bone plates are widely used in internal fixation of the fracture. The plate is fixed on both sides of the fracture to hold the broken pieces together, they are fixed with screws. After healing, plates may be left or removed. This surgery is mostly used for fixation of diaphyseal of the upper extremity and metaphyseal and articular fractures.
Interlocking nail
Interlocking nail is a unique technology used for many types of fracture configuration including metaphyseal and periarticular fractures. This helps in preventing postoperative instability. These are metallic implants used for traumatic long bone fractures.
K wire
K wire also known as Kirschner wires, they are available in different sizes and are used to hold bone fragments together. These are used in operation for temporary fixation. They are used for definite fixation if the fracture fragments are small such as wrist and hand fractures.
To fix up a femur fracture (thighbone) which is the longest and strongest bone in your body, femur nailing operation is done using a metal rod. The metal rod is known as femoral nail also called as an intramedullary nail or interlocking nail.
Tibial shaft fractures
Tibial shaft fractures are the common long-bone fractures. The standard treatments for diaphyseal tibial fractures are tibial nailing, intramedullary nail (IMN), internal fixation with plate and screws.
Forearm plating
Forearm plating is done for forearm fractures that are common orthopedic injuries; plate fixation is the best treatment for displaced forearm shaft fractures in adults.
Wrist fracture
Wrist fracture may require surgery to hold your bone in place. Your doctor may use implant pins, rods, screws or plates if you have an open fracture, if bone pieces move before they heal, if any damage in the ligaments, nerves or blood vessels.
Elbow plating
Elbow plating is a procedure used to treat your broken elbow (olecranon). Open reduction and internal fixation are the types of surgeries used to stabilize and heal the broken bone.
Distal humerus
Distal humerus fracture is a crack in the lower end of the upper arm bone. The distal humerus plate has two plate techniques. It creates a girder like structure which provides strength to the fixation- The posterolateral plate acts as a tension band during elbow flexion, and the medial plate provides support to the medial side of the distal humerus.
One of the most difficult and challenging treatments of periarticular fractures is bending the plate to fit into the specific area of the bone. The Periarticular Plating System is pre-contoured to closely follow the shape of the bone and create a fit that requires little or no additional bending, unlike conventional plating systems.
The Distal Femoral Nail DFN is done for the stabilization of fractures of the distal femur. It can also be used for diaphyseal fractures in which a retrograde approach is indicated.
The Proximal Tibia Plating System is commonly used to treat nonunions, osteotomies, malunions, osteopenic bone and fractures of the proximal tibia, including simple, comminuted, lateral wedge, depression, medial wedge, periprosthetic and fractures with associated shaft fractures.
The proximal femur plate is used for femur fractures that include fractures of a trochanteric region or with additional fracture of the medial cortex, fractures of the proximal end of the femur, osteotomies of the proximal femur and also used in the fixation of osteopenic bone and nonunions or malunions.
Proximal humeral fractures
Proximal humeral fractures are the third most common type of fragility fracture for patients over 65 years of age, Most of these proximal humeral fractures are stable, minimally displaced, and can be managed conservatively. Proximal humeral locking plates offer several potential advantages in the treatment of these injuries. These are site-specific, low profile plates designed for fractures and dislocations, osteotomies and nonunions of the proximal humerus.
Unstable elbow
Unstable elbow is the looseness in the elbow joint that may cause the joint to catch, pop, or slide out of its place during some arm movements.
The elbow joint dislocation occurs due to an injury or trauma that may lead to fracture, injuries to arteries in the arm, and injury to the nerves.
Radial neck fractures
Radial neck fractures are more common in children than in adults. It usually occurs due to a fall on the outstretched hand causing direct longitudinal forces to act on the redial head and neck impacting against the capitellum.
A fractured neck of femur
A fractured neck of femur is a serious injury. It usually occur when the top part of the femur is broken, just below the ball and socket.
Trochanteric fractures
Trochanteric fractures of the thigh bone, or femur, are not common injuries. The trochanters can be fractured during hip fracture.
Proximal femur fractures
Proximal femur fractures are fractures that occur in the femur near the hip region
PFN (proximal femoral nail)
PFN (proximal femoral nail) is an intramedullary device used in the treatment of unstable pertrochanteric, subtrochanteric and intertrochanteric femoral fractures.
DHS (Dynamic hip screws) is a femoral head-sparing orthopedic device which is used to treat femoral neck fractures. The same is also referred to as a pin and plate.
Cannulated screw fixation of the hip is a widely accepted surgical method for managing the fractures caused in the neck of the femur especially in patients with poor premorbid conditions, minimally displaced fractures and those from a younger age group.
Osteosynthesis
Osteosynthesis is a surgical procedure that is used to join the ends of the fractured bones by metal implants such as metal plates, pins, rods, wires or screws. It is mainly for internal fixation of a fracture.
Ankle fracture
Ankle fracture is a fracture of one or more bones in the ankle joint. It is mainly caused by a rotational injury of the ankle or due to any fall or accident.
Medial malleolus fracture
Medial malleolus fracture is a break in the tibia, inside of the lower leg. This fracture often occurs with a fracture of the fibula which is a fracture of the back of the tibia, or due to an injury to the ankle ligaments.
A tibial plafond fracture also known as pilon fracture. It is a type of break that occurs at the bottom of the tibia (shinbone) and involves the ankle joint.
Intraarticular fractures
Intraarticular fractures are bone fractures in which the fracture line crosses into the surface of the joint and result in damage of the cartilage.
Joints are those areas where different parts of the skeleton come together. Often joint injuries occur at these intersections. The four types of joint injuries are strains, sprains, fractures, dislocations.
An avulsion fracture occurs when a small piece of bone attached to a tendon or ligament gets pulled away from the main part of the bone. Most of them get healed without any surgical intervention.
Best Doctor for Fracture Surgery Treatment:
Dr. Srinivas kasha is one of the Best Orthopedic Doctor in Begumpet, Secunderbad. He is Senior Consultant orthopedic, Pelvic acetabular, trauma Joint Replacement. He is a Sr. Orthopedic Specialist in Secunderabad & Hip replacement surgeon in Hyderabad with 15+ years of experience in joint replacement. Dr. Srinivas Kasha providing treatment for all the fractures in Hyderabad. He is the Best Open Fracture Surgeon in Hyderabad - Secunderabad.
0 notes