#Digital Dentistry in Howell
Text
Dive into the future of dental care! Explore the latest digital dentistry trends of 2024 in our newest blog post. Ready to revolutionize your smile? Read more and contact us today!
#howell dentistry#dentist in howell#howell dentist#dentistinhowell#howelldentist#Dental Technology#Digital Dentistry#Digital Dentistry in Howell#smile makeover#dental care#dentistry#smile transformation#howell smiles
0 notes
Text
Improve Your Products and Service Quality through the Best Business Website Designs
Improve Your Products and Service Quality through the Best Business Website Designs

A lot of business website improvement companies have a troubling knowledge wherein to start. But sincerely the standards are equal in this industry for any professional and carried out Dentistry Marketing Ideas improvement professionalism of your business. But its miles how a vacationer finds you see you and the experience that they have to decide how a fulfillment your website is. Your website…
View On WordPress
#dentistry marketing ideas#digital marketing for restaurant#Howell Michigan social media marketing#Marketing Agency Michigan#marketing for landscaping
0 notes
Text
Juniper Publishers-Open Access Journal of Head Neck & Spine Surgery
The Use of Digital Sub-Periosteal Implants in Severe Maxillary Atrophies Rehabilitation: A Case Report
Authored by Lorenzo Viviani
Abstract
Development in osteointegration and bone-implant interface led through the years to different prosthetic procedures, varying from tilted implant to zygomatic or pterygoid implant. Though feasibility of these prosthetic rehabilitations is to be determined for each patient. Here we suggest a paradigm shift in subperiosteal implant technique, where rigid fixation, load bearing concept, virtual planning and digital engineering are mandatory. A clinical case is reported in order to better explain and help understand the technique.
Keywords: Subperiosteal implants; Alternative implantology; Juxtabone implants; Bone atrophy; Atrophic maxilla
Introduction
The success of an implant-prosthetic oral rehabilitation relies on multiple factors: an optimal and firm bone tissues support, dental implant device features, peri-implant soft tissues favorable conditions and a proper prosthetic finalization [1]. These assumptions are indeed needed to define a correct implant-surgery planning and to assure a long-term successful rehabilitation, reducing at minimum possibilities of complications, such as peri-implant diseases. Up to 56% of the totality of implant-patients [2], during their life, develop peri-implant diseases which can lead to an ingravescence of a pre-existent severe bone atrophy condition, especially if peri-implant diseases arise in a non-clinically controllable way. Continuous evolving of implant surfaces, unitedly with clinical studies and systematic reviews conducted on implant-bone contact, allowed clinicians through years to introduce innovative rehabilitative protocols finalized to resolve increasingly severe bone atrophies cases reducing implant fixture lengths; new surgical protocols lead to a fewer number of bone-volume augmentation surgeries and a consequent implant-positioning following anatomical directions previously prevented.
Prosthetic-guided implant-protocols such as “All-on-six” protocol, characterized by tipped distal implants, “All-on-4” protocol, “Pterigo” and “Quad zygoma” protocols have been introduced and scientifically validated over the years. Nevertheless, for anatomical, systemic, economical and logistical reasons, these protocols may result inapplicable in certain clinical situations. Mommaerts et al. [3] in 2017 proposed a peculiar surgical protocol which may be considered a valuable answer to these problematic cases, introducing into implant dentistry concepts borrowed from reconstructive and traumatological areas of maxillo-facial surgery: “custom-made device” and “rigid fixation”. The present article describes an upper-maxillary severe bone atrophy clinical case (Cawood and Howell classification’s Class V-VI [4]) treated with a modern prosthetic and surgical implant protocol, which, in his variants, revisits subperiosteal implants concept, developed under current precepts such as rigid fixation and “digital workflow”, characterized by an entirely virtual project starting from occlusal plane and computer aided custom-made realization.
Case Reports
A 65 year old male patient presented a fully edentulous upper jaw, having lost all his teeth about 20 years before for periodontal problems. This absence determined an alveolar and basal maxillary process progressive and severe atrophy up to the actual stage, classified as a Cawood and Howell’s class VI [4]. Patient presented a clean medical history (no hypertension, diabetes or heart disease history) and no risk factors (non-smoker). He refused a tri-dimensional reconstructive project for anterior and posterior maxilla through multiple bone grafts because of its surgical invasiveness and long timings to achieve a stable prosthetic situation (12 months in total). In addition, he firmly asked for a provisional prosthetic loading, impossible to obtain in case of bone grafts therapeutic option because of the optimal engraftment timing needed. Therefore, surgical and prosthetic project consisted into a maxillary sub-periosteal implant equipped with an immediate loading and screwed full-arch provisional dental prosthesis. Prosthetic-guided Cad-Cam construction protocol was strictly followed, as digital sub-periosteal implant (Iuxta-3D) contemplates; in particular, patient undergoes a CB-CT exam wearing a previously prepared radiological template (after his removable prosthesis duplication).
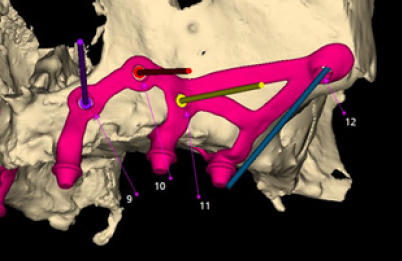
The radiological template undergoes a CB-CT exam alone. Once radiological examination’s correctness is verified, both DICOM files series obtained are unified to achieve a digital reconstruction of the upper jaw and its occlusal relation with lower one (Figure 1). Next phase is characterized by sub-periosteal implant digital design starting from occlusion and positioning future prosthetic prominences into their final positions. Implant fixing screws positions are then determined to assure a correct bone rigid fixation, starting from facial buttresses lines, in particular respecting nasal-maxillary and zygomatic-maxillary ones: in fact, canine fossa and zygomatic bone displays ideal thicknesses (6- 8mm) to allow synthesis screw’s stable fixation (Figure 2) [5]. Designing phase ends with surgeon’s project validation and subperiosteal implant production [6,7]: this process is conducted by “laser melting technique” (homogeneous layers of titanium powders are fused together in an additive way by a laser beam, following the 3D virtual model), employing grade V Titanium alloy (Ti-6-Al-4V). Then, the structure is electropolished and decontaminated, before sterilization. Together with the subperiosteal implant, a stereolithographic and autoclavable clone model of the structure is provided (Figure 4).
Intervention is entirely conducted under conscious sedation; surgical protocol assumes a mucosal incision on the edentulous ridge, bilaterally full thickness detachment of antero-lateral maxillary region up to zygomatic bones and the hard palate anterior third. Ridge ostectomies are then performed in correspondence of passage region of structure’s titanium arms and prosthetic connection pins, in order to ease sub-periosteal implant tanking towards bone ridge and avoid possible future complications, such as structure expositions (Figure 5). Plastic custom- and digital-made guides are provided to help surgeon to carry out ostectomies, which assure precision and safety during surgery (Figure 3). After a perfect fitting check between structure and underlying bone, sub-periosteal implant is placed in its final position and rigid fixated through synthesis screws (Figure 6).
Once stitching stage is over, preferably with 4.0 and 5.0 resorbable braided wire, the prosthetic phase begins: covering screws (mounted before stitching) are removed from structure’s transmucosal pins and digital-designed abutments are placed in position. These abutments held information digitally preestablished, such as height and tri-dimensional orientation. Respecting occlusion relationships, provisional prosthetic structure fitted on abutments is fixed with them through bicomponent resin and then screwed in position (using a torque wrench) after resin polymerization completely occurred. Surgical wound needs to be completely freed from any prosthetic compression (Figure 7). Patient is given of precise post-surgical instructions (anti-inflammatory and antibiotic therapies, cold and semi-liquid diet) and clinically controlled after 3 and 15 days (Figure 8). Stiches are removed on the 15th day, after provisional prosthetic structure is unscrewed and put back in position. Definitive prosthetic structure is delivered after 4-5 months from surgery.
Results
Borrowed from original sub-periosteal protocols, the described method deeply revisited sub-periosteal implantology concept. This has been made possible thanks to technological progresses and their subsequent application in medical and surgery fields, to many years of surgical techniques’ refinement, evolution of implant and radiological devices, which allowed entire workflow digitalization. These factors, although constant evolving, made this method adequate to third millennium realization standards. First, and probably most important, renewal consists in digital project and realization, starting from prosthetic pins position, a completely individualized STL model, prelude of a 3-D structure capable of a perfect fitting with underlying bone.
A correct interocclusal relationship, which holds a fundamental role, is precisely and digitally replicated and the only shrewdness to main remains avoiding undercuts in design phase or to correct them in surgical phase through ostectomy maneuvers. Moreover, digitally-planned ostectomies allow a sub-periosteal implant correct fitting even when bone structure presents natural undercuts (a frequent occurrence in atrophic maxillary bones) and help peri-implant tissues to heal properly all-around prosthetic pins. The possibility to have a screw-connected prosthesis to 3D sub-periosteal implant represents certainly one of the most important innovation of this technique: it allows a connections size balancing and occlusal force resistance improving, as well as a faster and more atraumatic prosthetic handling during healing phases. In fact, 3D sub-periosteal implant is meant to be an immediate and provisional loading implantology technique, with three post-surgical follow-up and a definitive prosthetic loading after an average healing time of 4-5 months. Furthermore, as traditional endosseous implantology, sub-periosteal implants need a close monitoring and three-months periodontal support therapy, with a minimum annual unscrewing of the prosthesis.
Rigid fixation grants most of the final stability: different osteosynthetic screws are used to fix sub-periosteal implants to not reabsorbtion-subject skeletric regions, such as nasalmaxillary (anteriorly) and zygomatic-maxillary (posteriorly) facial buttresses, through a multivectorial fixation. This kind of fixation prevents early mobility of the structure, a dangerous factor which ease infections developing or foreign-body fibrous reactions; moreover, it represents a fundamental prerequisite for osseointegration possibilities of titanium structure, when in contact with bone cortical and coated by osteogenetic periosteal tissue. Minimum titanium thickness allows the surgeon to preserve at maximum periosteum during surgical phase, in order to release wound tensions.
Synthesis site is kept away from oral cavity interface, reducing risks of peri-implant inflammatory and infective complications. Soft tissues management, both in the immediate post-surgical term and in the long term, results one of the key factors of this technique: flogistic and infective infiltrations to level of transmucosal connection pins could determine its failure in the short time. Fabrication material topic also needs to be pointed out: sub-periosteal implants were once made by a cobalt-chromiummolibdenum alloy, employing lost-wax technique; the non-perfect correspondence between bone and vitallium elastic modules determined an high tissue stress and the lack of biological properties prevented osseointegration. Currently employed grade V titanium, on the other hand, presents a more favorable elastic modulo and holds a higher grade of biocompatibility, and therefore, osseointegration possibilities.
Discussion
In view of the above, we can highlight in the 3D sub-periosteal technique digital engineering advantages of a prosthetic guided design, with a retro-planning. If properly managed and carried out by a close cooperation between surgeon and biomedical engineer, it represents an effective, plastic and totally customizable response to multiple severe maxillary atrophies clinical situations, very difficult or impossible to handle, if not with a classic removable prosthetic solution. Resective surgery exiti, severe sinusal pathologies and progressive edentulous patients’ bone resorption could lead to these types of clinical situations, definable as Cawood and Howell’s V or VI classes.
This technique results also in an optimal management of reduced prosthetic spaces, particularly in mandibular posterior areas with a poor skeletrical vertical dimension, which is disputed between dental crowns’ highness and bone volume augmentation. Several decades maxillo-facial surgery experience in rigid fixation field, borrowed from traumatic, malformative and reconstructive surgery flows in digital sub-periosteal implant technique. Real purpose of this method is to integrate the current optimum endosseous implantology standard and to give a valid and predictable alternative to more complex, multi-distrectual (i.e., autologous bone graft) and with longer timelines bone augmentation surgical procedures. Described protocol is meant to propose itself as a design for clinical cases at the edge of limit, where bone quality and quantity not fulfill needed requirements for different prosthetic treatment plans; it also represents a lesser challenging treatment option for clinicians with shorter surgical timescales and immediate provisional functional loading. In vitro and in vivo studies regarding this technique still needs to be conducted. Resistance-thickness relationship of sub-periosteal implant should be better investigated, such as the clinical cases follow-up in vivo, in order to validate this protocol in the longterm.
For more articles in Open access Journal of Head Neck & Spine Surgery | Please click on: https://juniperpublishers.com/jhnss/index.php
For more about Juniper Publishers | Please click on: https://juniperpublishers.com/pdf/Peer-Review-System.pdf
#Head and neck surgery#Subperiosteal implants#Alternative implantology#Juxtabone implants#Atrophic maxilla#Bone atrophy
0 notes
Text
Different Benefits Of Ceramic Reconstruction
By Laura Williams
Invented back in the 80s and further developed in the last decade, this innovative new technology is getting more popular lately. Ceramic reconstruction makes it easier to regain your beautiful smile. Thanks to this innovative technology, the whole process of dental restoration in Howell, MI takes significantly less time and fewer dental visits, the procedure itself is less invasive and less uncomfortable, and the results are beautiful, high-quality, translucent and natural looking, long lasting teeth.
Chair-side Economical Restoration of Esthetic Ceramic, or shortly CEREC, is the technology that transformed the usual dentistry. Using of computer assisted and manufactured methods for designing and making new teeth allows more precise results, and all this takes less time, causing much less discomfort to the patients. CAM/CAD makes a great difference.
CAM/CAD involves several stages in this process. First, your dentist will use a special, intraoral camera, to make several scans of the spot where the tooth is missing and has to be replaced, or repaired, and the surrounding teeth. These images will then be used in the process of designing new tooth, choosing appropriate materials and colors etc. Once designed, all this info will be sent to CNC milling or 3D printing.
Intraoral camera creates a virtual model not only of your missing tooth, but also the antagonist tooth and the bite situation. This virtual model helps in constructing the restoration. Finally, the model is milled out of a color-matching ceramic block, using diamond coated units, or printed in the 3D printer, using the appropriate type of ceramic material made for this purpose.
There are two main types of material used for this purpose, silicate ceramics and lithium disilicate ceramics. While the first one is ideal for single tooth replacement and restoration, as well as for similar aesthetic procedures, lithium disilicate is harder and more appropriate for making high-strength bridge frameworks that require higher flexural strength. Although there are some other materials, these two are generally used.
Digital impressions are much more comfortable for patients, and make things easier for any dentist. If your dentist has all the technology needed for designing and manufacturing the tooth, the whole procedure can be done in only one visit, and you can leave with your brand new, perfectly matched tooth the very same day. Not so long ago this might take much longer.
CEREC created restoration lasts around ten years or so, and often much longer, according to some studies. Gold and other reconstructive materials used before cannot provide such a durability, or longevity, and they cannot look so naturally, either. Of course, you still have to take care of your teeth, and this will also contribute to their looks and longevity.
All in all, there are several benefits of this great new restoration method that justify its popularity. It is comfortable, fast, reliable, the results are really amazing, the color can be matched just perfectly, you can smile again the very same day, without scheduling numerous visits, and you don't have to chew plaster and other nasty stuff. Your teeth will be all in place again, and your bite will be improved, and all this will look simply great.
About the Author:
When you are in need of the facts about ceramic reconstruction, come to our web pages today. More details are available at http://ift.tt/2fYFGPg now.
from http://ift.tt/2hlutun
0 notes
Text
The Benefits Of Ceramic Reconstruction
By Laura Williams
Although it was first developed in the 80s, this new technology is now developed and even more successful. The method known as ceramic reconstruction became more popular in the last decade, when innovative new technologies allowed easier and more precise procedures. In the city of Howell, MI, there are several dentists that successfully apply this highly effective, less invasive technology for achieving really impressive results in their area of business. Your new teeth can be perfect in only one visit to your dentist.
Chair-side Economical Restoration of Esthetic Ceramic, or shortly CEREC, is the technology that transformed the usual dentistry. Using of computer assisted and manufactured methods for designing and making new teeth allows more precise results, and all this takes less time, causing much less discomfort to the patients. CAM/CAD makes a great difference.
CAD involves making a digital impression, provided by an intraoral camera that can use different methods of providing one or more 3D scans, and these data are used for designing the restoration on the computer. Resulting 3D design is manufactured with the help of computer, using CNC milling or 3D printing, from the ceramic material of the appropriate color, chosen by your dentist, and the color will depend of the color of your natural teeth.
Creating comprehensive virtual model that involves surrounding are as well allows designing the perfect new teeth to fill the gap, and to improve your bite. Using these images, the dentist can decide about the appropriate material, shape and the best matched color. CNC milling device has diamond coated units, to mill the restoration out of a ceramic block. 3D printer uses the same material but slightly different method.
When it comes to material used for this particular purpose, two main types are the most common. The first one, known as silicate ceramics, is mainly used for replacing missing parts or missing teeth. Translucent, natural-looking material is really durable and highly appreciated. Lithium disilicate is even stronger, and therefore used for making tooth-bridges as well, and other parts that require better flexural strength.
Digital impressions are much more comfortable for patients, and make things easier for any dentist. If your dentist has all the technology needed for designing and manufacturing the tooth, the whole procedure can be done in only one visit, and you can leave with your brand new, perfectly matched tooth the very same day. Not so long ago this might take much longer.
Beauty and longevity of the CEREC restoration proved to be extraordinary, compared to other common replacement methods, such as gold etc. You can expect at least ten years. Not to mention the perfect appearance these replacements provide. Good oral care is something you should not forget about, nevertheless.
All in all, there are several benefits of this great new restoration method that justify its popularity. It is comfortable, fast, reliable, the results are really amazing, the color can be matched just perfectly, you can smile again the very same day, without scheduling numerous visits, and you don't have to chew plaster and other nasty stuff. Your teeth will be all in place again, and your bite will be improved, and all this will look simply great.
About the Author:
When you are in need of the facts about ceramic reconstruction, come to our web pages today. More details are available at http://ift.tt/2fYFGPg now.
The Benefits Of Ceramic Reconstruction
from NEXT GENERATION http://ift.tt/2gZepy3
0 notes
Text
Teledentistry Leader MouthWatch Appoints TeleDent™ COVID-19 Advisory Board
Advisors Will Provide Guidance on Teledentistry-Delivered Urgent Care
and Expanding Teledentistry Beyond the Coronavirus Pandemic
Metuchen, NJ – April 2, 2020 – MouthWatch, LLC recently announced the formation of a TeleDent COVID-19 Advisory Board. This group of teledentistry thought leaders will help MouthWatch develop best practice protocols for implementing teledentistry in the new reality of urgent care only. The team will also assist the company with creating very timely teledentistry-focused education and training materials. Topics covered will include the following:
Establishing Oral Triage Protocols
Implementing Proper Coding
Coordinating Dental Team Participation
Developing Virtual Workflows
Conducting Live Consultations
Explaining Legal & Regulatory Parameters
According to MouthWatch CEO and Founder, Brant Herman, “Many care providers are trying to figure out how to properly implement teledentistry so they can deliver urgent patient care. Our goal is to fill this information gap and to also ensure that teledentistry adoption and utilization continues long after the pandemic is over. I’m confident that we have the right advisory board in place to help us achieve these goals.”
The TeleDent COVID-19 Advisory Board consists of the following teledentistry thought leaders:
Margaret Scarlett DMD is an infectious and chronic disease prevention specialist, dentist and author. For thirty years, Dr. Scarlett has provided expert guidance on infectious diseases and infection control as a consultant to the Centers for Disease Control and Prevention, the World
Health Organization, the Pan American Health Organization, the United States Agency for
International Development, the American Red Cross and many consumer health companies.
Paul Glassman, DDS, MA, MBA: Dr. Glassman is the founder of the Virtual Dental Home Program, whereby he and his team at the University of the Pacific developed a more efficient
way to connect patients to dental care through the combination of technology and innovation. This care-delivery model, combined with his efforts in education, in supporting legislative changes that support teledentistry and improve access to care have helped create a landscape where more and more programs and providers are interested in teledentistry and the opportunities it creates.
Dr. Scott Howell, DMD, MPH, FSCD, is an assistant Professor and Director of Teledentistry at A.T. Still University, Arizona School of Dentistry & Oral Health. He has a strong background in mobile dentistry and innovative care models focused on teledentistry and public health. Dr. Howell developed imaging protocols to implement comprehensive teledentistry assessments and continues to contribute innovative care delivery programs to the ATSU curriculum and dental students.
Scott H. Froum, DDS is a Board-certified periodontist and a clinical associate professor at SUNY Stony Brook School of Dental Medicine in the Department of Periodontics. He is also chief editor of the Perio-Implant Advisory. Dr. Froum has lectured on the national and international level on implant therapy, bone and gum regeneration, and complications. Dr. Froum recently began using teledentistry in his New York City practice to provide his patients with emergency care services.
Patti DiGangi, RDH, BS believes dentistry is no longer just about fixing teeth; dentistry is oral medicine and it’s time we got around to truly practicing it. Patti’s specialty is medically necessary coding. Her efforts have assisted thousands of professionals to code more accurately and efficiently. The American Dental Association recognized her expertise by inviting her to write a chapter in its CDT 2017 Companion book and again for CDT 2018 Companion. Patti holds publishing and speaking licenses with ADA for Current Dental Terminology©2020. She is a strong advocate of teledentistry and is the co-author of Teledentistry: Pathway to Prosperity, Critical Choices.
Michelle Strange, MSDH, RDH, has been a dental clinician since 2000 and is currently a practicing hygienist, speaker, writer, content developer, consultant, and podcast cohost for A Tale of Two Hygienists. With a master's degree in dental hygiene education and a belief in lifelong learning, she hopes to continue to learn and grow within the dental profession and one day see the gap bridged between medicine and dentistry. Michelle currently uses teledentistry in her volunteer work with a dental clinic in South Carolina.
The dental community will soon be able to gain a deeper understanding of how to use teledentistry during the coronavirus epidemic thanks to white papers, guest blogs, webinars, e-books and articles that will be developed in close collaboration with the TeleDent COVID-19 Advisory Board. In the meantime, visit www.mouthwatch.com for more information.
About MouthWatch LLC
Headquartered in Metuchen, New Jersey, MouthWatch, LLC is a leader in innovative clinician-focused teledentistry solutions, digital case presentation tools and intraoral imaging devices. The company is dedicated to finding new ways to constantly improve the dental health experience for both patient and provider. The founders and management team of MouthWatch have relevant backgrounds and successful track records in dentistry, consumer products and communications. Since 2012, this team has pioneered the integration of digital imagery and communications technology in the field of dentistry. Their cumulative experience makes it possible for the company to take the lead in introducing the benefits of telemedicine to the world of dentistry. For more information, visit www.MouthWatch.com .
# # #
0 notes