Photo
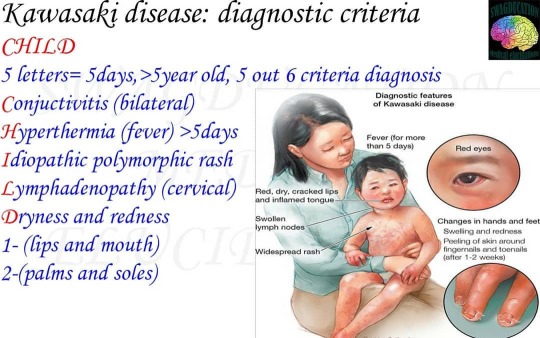
Kawasaki disease is a syndrome of unknown cause that results in a fever and mainly affects children under 5 years of age. It is a form of vasculitis where blood vessels become inflamed throughout the body. The fever typically lasts for more than 5 days and is not affected by usual medications. Other common symptoms include large lymph nodes in the neck, a rash in the genital area, and red eyes, lips, palms, or soles of the feet. Within three weeks of onset, the skin from the hands and feet may peel, after which recovery typically occurs. In some children coronary artery aneurysms form in the heart. While the specific cause is unknown, it is thought to result from an excessive immune system response to an infection in children who are genetically predisposed . It does not spread between people. Diagnosis must take into account many other conditions that may present similar features, including scarlet fever and juvenile rheumatoid arthritis. SIGNS & SYMPTOMS Kawasaki disease has telltale symptoms and signs that appear in phases. The first phase, which can last for upto 2 weeks, usually involves a fever that lasts for at least 5 days. Other symptoms include ->red (bloodshot) eyes ->A pink rash on the back, belly, arms legs and genital area -> Red dry cracked lips -> A strawberry tongue (white coating with red bumps on the tongue) -> A sore throat -> Swollen palms of the hands and soles of the feet with a purple- red-color -> Swollen lymph glands in the neck The second phase usually begins 2 weeks after the fever started Symptoms can include: -Peeling skin on the hands and the feet -Joint pain -Diarrhea -Vomiting -Belly pain If the conditions isn't found later, patients can have serious complication that affect the heart such as: - An aneurysm (a bulge in the wall) of the coronary arteries, which supply blood to the heart -Inflammation of the heart muscle, lining, valves and the outer membrane around the heart -Arrhythmias which are changes in the normal pattern of the heartbeat -Problems with some heart valves CAUSE cause of kawasaki disease is idiopathic It's most common among children of japanese and korean descent, but can affect any child. (at Kharkov, Ukraine) https://www.instagram.com/p/CFExf9Ug6cE/?igshid=17rj5rn6l6fm5
0 notes
Photo
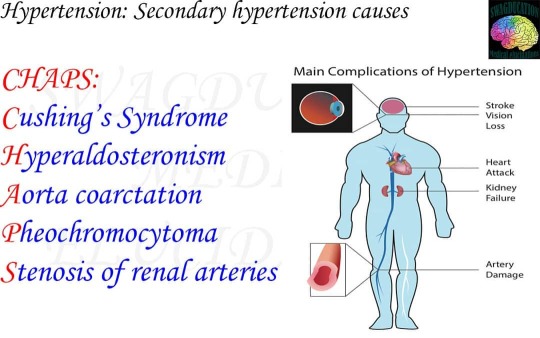
Hypertension Refers to a persistent elevation of arterial blood pressure. Hypertension is a major risk factor for MI, stroke and chronic kidney disease (CKD). AETIOLOGY The majority of hypertension is essential (primary), however in a significant number of cases there may be a secondary cause or contibutory factor. Primary- 95% - No identifiable underlying cause. (Essential or idiopathic hypertension) Secondary- 5% ->Endocrine :Primary aldosteronism (increasingly recognised as a major cause of hypertension) :Pheochromocytoma :Cushing's disease :Acromegaly ->Renal :Renovascular disease (eg- atheromatous, fibromuscular dysplasia) :Intrinsic renal disease (eg- CKD,AKI,glomerulonephritis) ->Drugs :Glucocorticoids :oral contraceptives :SSRIs :NSAIDs :EPO ->Coarctation of the aorta (consider in children/young adults with hypertension) CLINICAL FEATURES Hypertension is typically asymptomatic. However, signs and symptoms may reflect underlying end-organ damage or a potential secondary cause. SYMPTOMS :Palpitations :Angina :Headache :Blurred vision :New neurology (limb weakness paraesthesia) SIGNS :Retinopathy :Cardiomegaly :Arrhythmias :Proteinuria :Uraemia DIAGNOSIS If clinoc BP is 140/90 mmHg or higher, ABPM is used to confirm the diagnosis (except in stage 3 hypertension, in which immediate treatment is initiated). With ABPM, at least two measurements an hour are taken during the patient's usual waking hours( eg: 8am - 10 pm). The average value of these measurements is used to confirm the diagnosis. (at Kharkov, Ukraine) https://www.instagram.com/p/CEgl66OpIac/?igshid=94g710kd0adv
0 notes
Photo

Hemolytic anemia Red blood cells have the important mission of carrying oxygen from the lungs to the heart and throughout to the entire body. When destruction of RBC's outspaces the bone marrow's production of cells hemolytic anemia occurs. Hemolytic anemia can be extrinsic or intrinsic. Extrinsic hemolytic Anemia develops by several methods, such as when the spleen traps and destroys healthy red blood cells, or an autoimmune reaction occurs. It can also come from RBC destruction due to: ->Infection ->Tumors ->Autoimmune disorders ->Medication side effects ->Leukemia ->Lymphoma Intrinsic hemolytic Anemia develops when the red blood cells produced by the body , don't function properly. This condition is often inherited, such as in people with sickle cell anemia or thalassemia, who have abnormal hemoglobin. Other time, an inherited metabolic abnormality can lead to this condition, such as in people with G6PD deficiency, or red blood cell membrane instablity, such as herediatry spherocytosis. Anyone of any age can develop hemolytic anemia. Causes of hemolytic anemia Underlying causes of extrinsic hemolytic anemia include: ->Enlarged spleen ->Infectious hepatitis ->Epstein Barr virus ->Typhoid fever -> E.coli toxin -> Leukemia -> Lymphoma -> Tumors ->Systemic lupus erythematosus (SLE) an autoimmune disorder -> Wiskott-Aldrich syndrome, an autoimmune disorder -> HELLP syndrome (named for its characterstics which include hemolysis,elevated liver enzymes, and low platelet count) Drug induced hemolytic anemia. - Acetaminophen - Antibiotics such as cephalexin,ceftriaxone, penicillin, ampicillin or methicillin -chlorpromazine(Thorazine) -Ibuprofen (Advil, Motrin IB) -Interferon alpha -Procainamide -Quinidine -Rifampicin(Rifadin) One of the most severe forms of hemolytic anemia is the kind caused by receiving a red blood cell transfusion of the wrong blood type. SYMPTOMS -Paleness of the skin -Fatigue -Fever -Confusion -Lightheadedness -Dizziness -Weakness or inability to do physical activity Other signs and symptoms that are seen in those with hemolytic anemia include: -Dark urine -Yellowing of the skin and the whites of the eyes -Heart murmur -Increased heart rate (at Kharkov, Ukraine) https://www.instagram.com/p/CDYkIYSpB0u/?igshid=hy7cw34kyps4
0 notes
Photo
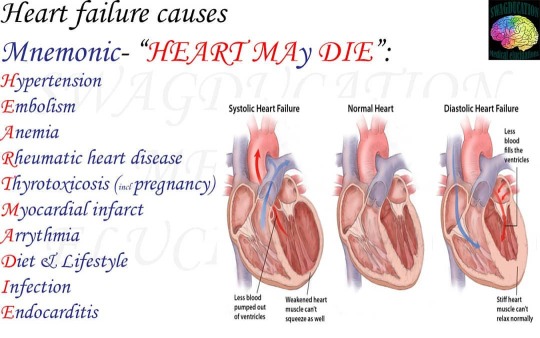
The definition of heart failure is when the heart cannot pump efficiently enough for blood to circulate oxygen-rich blood throughout the body. When the heart becomes weak or when it becomes thickened and stiff. The heart muscle cannot keep up with it's workload. Types of heart failure 1->Systolic heart failure (left-sided heart failure) When the heart loses strength on the left side(left ventricle) and cannot pump the blood into circulation. It is called systolic heart failure or left-sided heart failure. When this occurs, the heart becomes dilated and weak. The strength of the heart muscle can be measured with an echocardiogram that measures the ejection fraction. An ejection fraction of 70% is normal. The term congestive heart failure, or CHF,refers to the accumulation of fluid in the tissues. Fluid can accumulate in the legs causing swelling (edema),into the lungs causing pulmonary edema, or into the abdomen where it is called ascites. A type of heart failure termed acute decompensated heart failure is an emergency. 2-> Diastolic heart failure (right-sided heart failure): The second type of heart failure is diastolic heart failure, characterized by the bottom chambers of the heart becoming thicker and stiffer. When this happens, the left ventricle cannot fill with sufficient blood, and not enough blood is pumped into circulation, even if the pumping action is still strong. This is why diastolic heart failure is sometimes referred to as heart failure with preserved ejection fraction or right-sided heart failure. If the signs and symptoms of heart failure are present and the ejection fraction is greater than 50% diastolic heart failure may be considered, especially if an echocardiogram shows the heart muscle is thickening. Symptoms of heart failure 1-Shortness of breath 2-Fatigue 3-Lightheadedness 4-Exercise intolerance 5-Loss of appetite 6-Nausea 7-coughing (or chronic cough) 8-Wheezing 9-Pounding or racing heart 10-Excessive tiredness 11-Confusion 12-Problems thinking 13-Swelling in the ankles 14-Swelling in the abdomen 15-Chest pain (at Kharkov, Ukraine) https://www.instagram.com/p/CDGXbeZJWa6/?igshid=1ns4ozkgxham8
0 notes
Photo

A fat embolism is a piece of intravascular fat that lodges within a blood vessel and causes a blockage of blood flow. Fat emboli commonly occur after fractures to the long bones of the lower body, particularly the femur (thigh bone), tibia (shinbone) and pelvis. While fat emboli are common and generally resolve on their own, they can lead to serious condition called fat embolism syndrome (FES). FES can cause inflammation, multi-organ dysfunction and neurological changes that can be deadly. Symptoms of fat embolism syndrome Signs of FES generally appear 12 to 72 hours after trauma. Symptoms tend to occur throughout the body and include: -Rapid breathing -Shortness of breath -Mental confusion -Lethargy -Coma -Pinpoint rash (called a petechial rash), often found on the chest, head, and neck area, which occurs due to bleeding under the skin -Fever -Anemia RISK FACTORS -Being male -Being between the ages of 20 and 30 -Having a closed fracture(the broken bone doesn't penetrate the skin) -Having multiple fractures, especially in the lower extremities and pelvis DIAGNOSIS Gurd's major criteria -petechial rash -respiratory distress -mental concussion Gurd's minor criteria include: -Fat in the blood -Fever -Jaundice -Anemia -Fast heartbeat -Renal dysfunction TREATMENT Once FES develops, the person should be admitted into intensive care unit, preferably with central venous pressure monitoring. CVP monitoring would be helpful to guide the volume resucitation. Supportive treatment is the only proven tratment method. Supplemental oxygen can be given if a person has mild respiratory distress. However, if a person has severe respiratory distress, either continous positive pressure ventilation or mechanical ventilation using positive end-expiratory pressure may be indicated. Fluid replacement is required to prevent shock. Volume resuscitation with human albumin is recommended because it can restore blood volume in the circulatory system while also binds to free fatty acids in order to reduce lung injuries. In severe cases, dobutamine should be used to support the right ventricular failure. (at Kharkov, Ukraine) https://www.instagram.com/p/CC0LRf2Fd6C/?igshid=767b3zpldluh
0 notes
Photo

Disseminated intravascular coagulation is a condition in which small blood clots develop throughout the bloodstream, blocking small blood vessels. The increased clotting depletes the platelets and clotting factors needed to control bleeding, causing excessive bleeding. There are a number of possible causes,including infection,surgery and complications of childbirth. ->Excessive clotting is followed by excessive bleeding -> The amount of clotting factors in the blood is measured. ->The underlying disorder is treated. Disseminated intravascular coagulation begins with excessive clotting. The excessive clotting is usually stimulated by a substance that enters the blood as part of a disease(such as infection or certain cancers) or as a complication of childbirth, retention of a dead fetus, or surgery. People who have a severe head injury or who have tissue damage caused by shock,burns,frostbite other injuries, or even a bite by a poisnous snakeare also at risk.As the clotting factors and platelets (cell fragments that circulate in the blood stream and help blood clot) are depleted,excessive bleeding occurs. DIC may develop -> suddenly -> slowly Slowly developing disseminated intravascular coagulation typically results from cancer,aneurysm or cavernous hemangiomas (Collections of dilated blood vessels). SYMPTOMS DIC that develops suddenly usually causes bleeding, which may be very severe. If the condition follows surgery or childbirth bleeding may be uncontrollable. Bleeding may occur at the site of an intravenous injection or in the brain, digestive tract, skin , muscles or cavities of the body. If DIC develops more slowly, as in people with cancer, then clots in veins (deep venous thrombosis) are more common than bleeding. If clots form in veins (usually in legs) the person may have swelling,redness or pain in the are. However,sometimes no symptoms develop. A clot that forms in a vein may break free and travel (becoming an embolus) to the lungs. (at Kharkov, Ukraine) https://www.instagram.com/p/CCiQInzJkWY/?igshid=1jrcct681u9n5
0 notes
Photo

Buerger's disease is a rare disease of the arteries and veins in the arms and legs. In buerger's disease also called thromboangitis obliterans the blood vessels become inflamed,swell and can become blocked with blood clots (thrombi). This eventually damages or destroys skin tissues and may lead to infection and gangrene. Buerger's disease usually first shows in the hands and feet and may eventually affect larger areas of the arms and legs. Virtually everyone diagnosed with Buerger's disease smokes cigarettes or uses other forms of tobacco is the only way to stop Buerger's disease. For those who don't quit, amputation of all or part of a limb is sometimes necessary. CAUSES The exact cause of Buergers disease is unknown. While tobacco use clearly plays a role in the development of Buerger's disease, it's not clear how it does so.It's thought that chemicals in tobacco may irritate the lining of the blood vessels,causing them to swell. RISK FACTORS Tobacco use- Buerger's disease can occur in people who use any form of tobacco, including cigars and chewing tobacco. People who smoke hand rolled cigarettes using raw tobacco and those who smoke more than a pack and half of cigarettes a day may have the greatest risk of Buerger's disease. Chronic gum disease- Long-term infection of the gums has been linked to the development of Buerger's disease, though the reason for this connection isn't clear. Sex Buerger's disease is far more common in males than in females. Age The disease often first appears in people less than 45 years old. COMPLICATIONS If buerger's disease worsens, blood flow to the arms and legs decreases. This is due to blockages that that makes it hard for blood to reach the tips of fingers and toes. Tissues that don't recieve blood don't get to reach the tips of fingers and toes. Tissues that don't recieve blood don't get the oxygen and nutrients they need to survive. Diagnosis ->Based on signs and symptoms ->Blood tests For blood clotting disorders and diabetes ->Allen's test ->Angiogram TREATMENT -Smoking cessation -Medication to dilate blood vessels -Spinal cord stimulation -Amputation, if infection or gangrene occurs (at Kharkov, Ukraine) https://www.instagram.com/p/CBAgPVupoH9/?igshid=1ri765dcmi6fd
0 notes
Photo
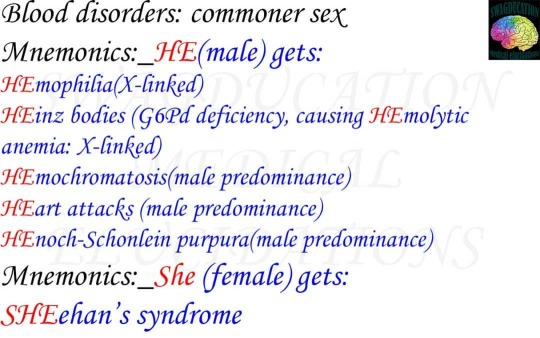
Blood disorders can affect any of the three main components of blood: -Red blood cells which carry oxygen to the body's tissues -White blood cells, which fight infections -Platelets which help blood clot. Blood disorders can also affect the liquid portion of blood, called plasma. *Blood disorders affecting RBCs Anemia -iron-deficiency anemia -Anemia of chronic disease -Pernicious anemia -Aplastic anemia -Autoimmune hemolytic anemia -Thalassemia -Sickle cell anemia -Polycythemia vera *Blood disorders affecting WBCs -Lymphoma -Leukemia -Multiple myeloma -Myelodysplastic syndrome *Blood disorders affecting platelets -Thrombocytopenia -Idopathic thrombocytopenic purpura -Heparin-induced thrombocytopenia -Thrombotic thrombocytopenic purpura -Essential thrombocytosis *Blood disorders affecting blood plasma -Hemophilia -Von willebrand disease -Hypercoaguable state -Deep venous thrombosis -Disseminated intravascular coagulation (at Kharkov, Ukraine) https://www.instagram.com/p/CA7SaV8JC-2/?igshid=1e8jjetbqz183
0 notes
Photo

Arteriosclerosis occurs when the blood vessels that carry oxygen and nutrients from your heart to the rest of the body (arteries) become thick and stiff- sometimes restricting blood flow to your organs and tissues.Healthy arteries are flexible and elastic, but over time, the walls in the arteries can harden. Atherosclerosis is a specific type of arteriosclerosis, but the tems are sometimes used interchangeably. Atherosclerosis refers to the buildup of fats, cholestrol and other substances in and on the artery walls (plaque) which can restrict blood flow. The plaque can burst, triggering a blood clot. Although atherosclerosis is often considered a heart problem, it can affect arteries anywhere in the body . SYMPTOMS Atherosclerosis develops gradually.Mild atherosclerosis usually dosen't have any symptoms. -chest pain or pressure(angina) -sudden numbness or weakness in arms or legs -difficulty speaking or slurred speech -Temporary loss of vision in one eyeor drooping muscle in face, these signal a transientischemic attack (TIA) Which,if left untreated, may progress to stroke. -Symptoms of peripheral artery disease, such as leg pain when walking (claudication) COMPLICATIONS -Coronary artery disease -Carotid artery disease -Peripheral artery disease -Aneurysms -Chronic kidney disease DIAGNOSIS 1-A weak or absent pulse below the narrowed area or artery 2-Decreased BP in affected limb 3 Whooshing sounds over arteries Lab tests 1-Blood tests 2-Doppler ultra sound 3- Ankle-brachial index 4- Electrocardiogram 5- Stress test 6- Cardiac catheterization and angiogram TREATMENT ->Cholestrol medications ->Anti-platelet medications ->Beta blocker medications ->Angiotensin converting enzyme ->Calcium channel blockers ->Water pills (diuretics) SURGICAL PROCEDURES 1- Angioplasty and stent placement. 2- Endarterectomy 3- Fibrinolytic therapy 4- Bypass surgery (at Kharkov, Ukraine) https://www.instagram.com/p/CAj7CwFAPH2/?igshid=1x7gv3ch812lx
0 notes
Photo

An aneurysm occurs when an artery's wall weakens and causes an abnormally large bulge. This bulge can rupture and cause internal bleeding . They are most common in the: -Brain -Aorta -Legs -Spleen Exact cause of aneurysm is unclear, certain factors contribute to the condition. For exmple damaged tissue on the arteries can play a role. The arteries can be harmed by blockages,such as fatty deposits. These deposits can trigger the heart to pump harder than necessary to push blood past the fatty buildup. This stress can damage the arteries because of the increased pressure. Atherosclerotic disease can also lead to an aneurysm . People with atherosclerotic disease have a form of plaque buildup in their arteries. Plaque is a hard substance that damages the arteries and prevents blood from flowing freely. High blood pressure High blood pressure may also cause an aneurysm. The force of blood as it travels through your blood vessels is measured by how much pressure it places on artery walls. If the pressure increases above a normal rate, it may enlarge or weaken the blood vessels. Blood pressure for an adult is considered normal at or below 120/80 mmhg or millimeters of mercury. A significantly higher blood pressure can increase the risk of heart,blood vessel and circulation problems. Higher than normal blood pressure doesn't necessarily put you at risk for an aneurysm. Symptoms -Bleeding -Increased heart rate -Pain -Feeling dizzy or lightheaded Risk factors -A diet high in fats and cholestrol -A family history of heart conditions, including heart disease and heart attack -Smoking -Obesity -Pregnancy, which may increase your risk of having an aneurysm of the spleen. Diagnosis CT scans and Ultrasound methods are common tools used to diagnose or find blood vessel irrgularities. CT scans use X-rays to examine . Treatment A weak area of a vessel in the chest and abdomen may require a type of surgery called an endovascular stent graft. This minimally invasive procedure may be chosen over traditional open surgery because it involves reparing and reinforcing damaged blood vessels. The procedure also reduces the chances of infection,scarring and other problems. (at Kharkov, Ukraine) https://www.instagram.com/p/CAhhJQOgR-m/?igshid=150rbpldxdae5
0 notes
Photo
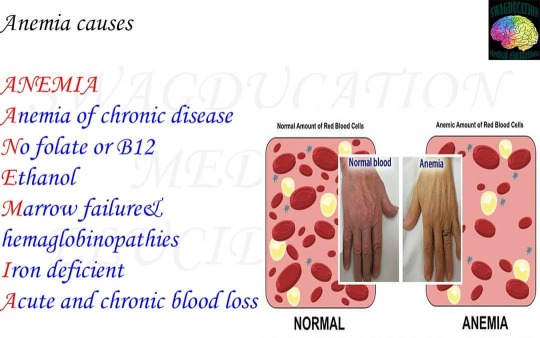
Anemia is a medical condition in which the red blood cell count or the hemoglobin is less than normal. In men, anemia is typically defined as hemoglobin level of less than 13.5 gram/100ml and in women as hemoglobin of less than 12.0gram/100ml Anemia is caused by either a decrease in production of red blood cells (decreased erythropoiesis) or hemoglobin, or an increase in loss (usually due to bleeding) or destruction of red blood cells. Some patients with anemia have no symptoms. Those who do have symptoms may -> Feel tired -> become easily fatigued -> appear pale -> have a feeling of heart racing -> Feel short of breath -> Have worsening heart problems A more common classification of anemia (low hemoglobin) is based on the mean corpuscular volume (MCV) which signifies the average volume of individual red blood cells. 1-> If the MCV is low (less than 80), the anemia is categorized as microcytic anemia (low red blood cell volume). 2-> If the MCV is in the normal range (80-100), it is called a normocytic anemia (normal blood cell volume) 3-> If the MCV is high, then it is called a macrocytic anemia (large blood cell volume) Iron deficiency is a very common cause of anemia. This is because iron is a major component of hemoglobin and essential for it's proper function. Chronic blood loss due to any reason is the main cause of low iron level in the body as it depletes the body's iron stores to compensate for ongoing loss of iron. Anemia that is due to low iron levels is called iron deficiency anemia. Aplastic anemia Aplastic anemia is a life threatening form of complete bone marrow failure. As a result, the blood contains inadequate numbers of red blood cells(anemia) as well as insufficient white blood cells (leukopenia) and platelets (thrombocytopenia). Diagnosis Anemia is usually detected or at least confirmed by a complete blood cell count Six component measurements make up a CBC test: 1-Red blood cell count 2-Hematocrit 3-Hemoglobin 4-WBC (count) 5-Differential blood count 6-Platelet count Treatment Effective treatment consists of certain medications, transfusions or bone marrow stem cell transplants. (at Kharkov, Ukraine) https://www.instagram.com/p/CASZRNnAKkV/?igshid=1ozcmivd5q3ci
0 notes
Photo
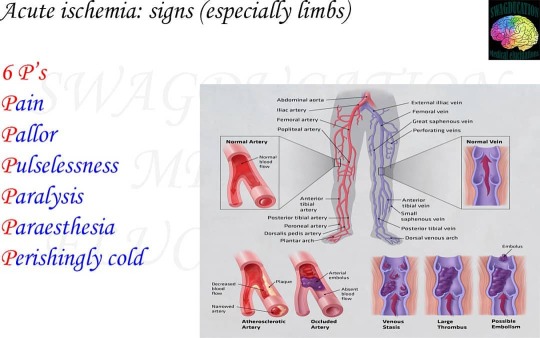
Acute limb ischaemia is defined as the sudden decrease in limb perfusion that threatens the viability of the limb. Complete or even partial occlusion of the arterial supply to a limb can lead to rapid ischaemia and poor functional outcomes within hours. AETIOLOGY Acute limb ischaemia has an incidence of around 1.5 per 10,000 person years. It's causes can be classified into 3 main groups: Embolisation Whereby a thrombus from a proximal source travels distally to occlude the artery(most common) The original thrombis source may be as a result of AF, post-MI mural-thrombus, abdominal aortic aneurysm or prosthetic heart valves. Thrombosis in Situ whereby an atheroma plaque in the artery ruptures and a thrombus forms on the plaque's cap (presenting an acute or acute-on-chronic) Trauma (less common) including compartment syndrome Differential DIAGNOSIS The differential diagnosis for acute limb ischaemia include critical chronic limb ischaemia ,acute DVT (can present as phlegmasia cerulea dolens and Phlegmasia alba dolens) or spinal cord or peripheral nerve compression. INVESTIGATION Routine bloods, including a serum lactate (to assess the level of ischaemia), a thrombophilia screen (if <50 yrs without known risk factors) and a group and save, should be taken, aling with an ECG. Suspected cases should be initially investigated with beside doppler ultrasound scan(both limbs), followed by considering a CT angiography If the limb is considered to be salvageable, a CT arteriogram can provide more information regarding the anatomical location of the occlusion and can help decide the operative approach (such as femoral and popliteal incision). MANAGEMENT Initial management Acute limb ischaemia is a surgical emergency. Complete arterial occlusion will lead to irreversible tissue damage within 6 hours. Start the patient on high-flow oxygen and ensure adequate IV access. A therapeutic dose heparin or preferably a bolus dose then heparin infusion should be initiated as soon as is practical. (at Kharkov, Ukraine) https://www.instagram.com/p/B-mabzJA5oh/?igshid=1y0ekbt9px7ox
0 notes
Photo

Ulcerative colitis is an inflammatory bowel disease(IBD). IBD comprises a group of diseases that affect the gasteointestinal tract. Ulcerative colitis occurs when the lining of the large intestines (also called the colon), rectum or both becomes inflamed. This inflammation produces tiny sores called ulcers on the lining of the colon. It usually begins in the rectum and spreads upward. It can involve your entire colon. The inflammation causes the bowel to move its contents rapidly and empty frequently . As cells on the surface of the lining of bowel die, ulcers form. The ulcers may cause bleeding and discharge of mucus and pus. While this disease affects people of all ages, most people are diagnosed between the ages of 15 and 35. After age 50, another small increase in diagnosis for this disease is seen, usually in men. SYMPTOMS The seriousness of ulcerative colitis symptoms varies among affected people. The symptoms can also change overtime. People diagnosed with UC may experience periods of mild symptoms or no symptoms at all. CAUSES:- Ulcerative colitis may be the result of an overactive immune system. However, it's unclear why some immune systems respond by attacking the large intestines and not others. Risk factors causing UC 1-Genes 2-Other immune disorders 3-Environmental factors DIAGNOSIS ->Stool test ->Endoscopy ->Colonoscopy ->Biopsy ->CT-scan TREATMENT The goal of treatment is to reduce the inflammation that causes the symptoms so to prevent the flare-ups and have longer periods of remission. Medication The Doctor may prescribe a medication to reduce inflammation and swelling. This will help alleviate many symptoms. These types of medications include: ->Mesalamine ->Sulfasalazine ->Balsalazide ->Olsalazine (at Kharkov, Ukraine) https://www.instagram.com/p/B-jjuSMg6Y5/?igshid=1uh3iaoguysln
0 notes
Photo

Peptic ulcers are sores that develop in the lining of the stomach, lower esophagus, or small intestin. They're usually formed as a result of inflammation caused by the bacteria H.pylori, as well as from erosion from stomach acids. Peptic ulcers are a fairly common health problem. There are 3 different type of peptic ulcers: 1) Gastric ulcers: ulcers tat develop inside the stomach 2) Esophageal ulcers: Ulcers that develop inside the esophagus 3) Duodenal ulcers: Ulcers that develop in the upper section of the small intestines, called the duodenum. SYMPTOMS Most common symptom of a peptic ulcer is burning abdominal pain that extends from the navel to the chest, which can range from mild to severe. Small peptic ulcers may not produce any symptoms in early phases. Other common signs -> Channges in appetite -> Nausea -> Bloody or dark stools -> Unexplained weight loss -> Indigestion -> Vomiting -> Chest pain DIAGNOSIS 1) Endoscopy 2) Upper gastrointestinal (X-ray with contrast pack) TREATMENT Medications include antibiotics to help kill infections and proton pump inhibitots (PPI's) to help reduce stomach acid. Acid blockers like ranitdine or famotidine also reduce stomach acid and ulcer pain. COMPLICATIONS Unteated ulcers can become worse over time. They can lead to other serious health complications. >Perforation: A hole develops in lining of the stomach or small intestine and causes an infection. A sign of a perforated ulcer is sudden, severe abdominal pain. >Internal bleeding: Bleeding ulcers can result in significant blood loss and thus require hospitalization. Signs of bleeding ulcer include lightheadedness, diziness and black stools. >Scar tissue: This is thick tissue that develops after an injury. This tissue makes it difficult for food to pass through the digestive tract. Signs of scar tissue include vomiting and weight loss. (at Kharkov, Ukraine) https://www.instagram.com/p/B-hRaSHF_fI/?igshid=llmjj629m4d2
0 notes
Photo
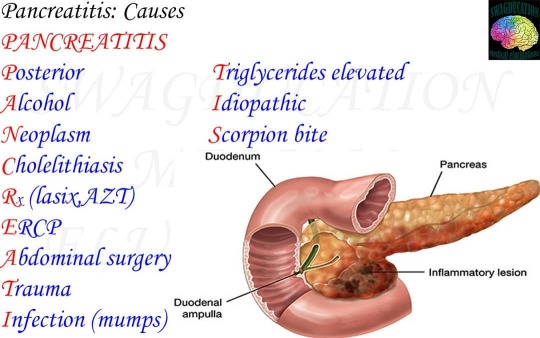
Pancreatitis is pathologic inflammation of the pancreas Once the gland becomes inflamed, the condition can progress to swelling of the gland and surrounding blood vessels, bleeding,infection, and damage to the gland. Pancreatitis may be acute (short term) or chronic (ongoing, long-term). Either type can be very severe, even life threatening. Acute pancreatitis- Usually begins soon after the damage to the pancreas begins. Attacks are typically very mild, but about 20% of them are very severe. An attack lasts for a short time and usually resolves completely as the pancreas returns to its normal state. Some people have only one attack,whereas other people have more than one attack, but the pancreas always returns to its normal state unless necrotizing pancreatitis develops and becomes life threatening. Chronic pancreatitis begins as acute pancreatitis. If the pancreas becomes scarred during the attack of acute pancreatitis. It cannot return to it's normal state. The damage to the gland continues, worsening over time. SYMPTOMS 1- Abdominal pain(cardinal symptom): characterstically dull,boring and steady; usually sudden in onset and gradually becoming more severe until reaching a constant ache; most often located in the upper abdomen and may radiate directly through to the back 2-Nausea vomiting sometime with anorexia 3- Diarrhea DIAGNOSIS Lab tests:- -> Serum amylase and lipase -> Liver-associated enzymes -> Blood urea nitrogen (BUN), creatinine and electrolytes -> Blood glucose -> serum cholestrol and triglyceride -> Complete blood count and hematocrit -> C-reactive protein (CRP) -> Arterial blood gas values -> Serum lactic dehydrogenase and bicarbonate -> Immunoglobulin G4 Diagnostic imaging 1-Abdominal radiography 2-Abdominal ultrasonography 3- Endoscopic ultrasonography 4-Abdominal computed tomography 5- Endoscopic retrograde cholangiopancreatography 6- Magnetic resonance cholangiopancreatography TREATMENT -> A hospital stay to treat dehydration with intravenous fluids and if the patient can swallow them then fluid intake orally -> Pain medicine and antibiotics by mouth or through an I.V if there is infection in pancreas -> A low-fat diet (at Kharkov, Ukraine) https://www.instagram.com/p/B-ebtU1FKZv/?igshid=743wm6vgk1en
0 notes
Photo
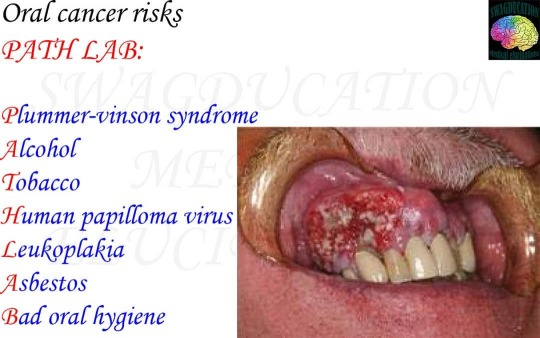
Mouth cancer refers to cancer that develops in any of the parts that make up the mouth (oral cavity). Mouth cancer can occur on the: -Lips -Gums -Tongue -Inner lining of the cheeks -Roof of the mouth -Floor of the mouth (under the tongue) SYMPTOMS 1-A lip or mouth sore that doesn't heal 2- A white or reddish patch on the inside of the mouth 3- Loose teeth 4- A growth or lump inside the mouth 5- Mouth pain 6- Ear pain 7- Difficult or painful swallowing CAUSES Mouth cancers form when cells on the lips or in the mouth develop changes (mutations) in their DNA. The accumulating abnormal mouth cancer cells can form a tumor. With time they may spread inside the mouth and on to other areas of the head and neck or other parts of the body. Mouth cancers most commonly begin in the flat, thin cells (squamous cells) Most oral cancers are squamous cell carcinomas. RISK FACTORS 1-Tobacco use of any kind including cigarettes,cigars,pipes,chewing tobacco and snuff 2-Heavy alcohol use 3-Excessive sun exposure to lips 4-A sexually transmitted virus called human papilloma virus (HPV) 5-A weakened immune system DIAGNOSIS tests and procedures used to diagnose mouth cancer include 1-Physical exam 2-Removal of tissue for testing (biopsy) Determining the extent of cancer 1- Using a small camera to inspect the throat using the method of endoscopy 2-Imaging tests (x-ray, CT, MRI and positron emission tomography (PET) scans, among others. TREATMENT Treatment for mouth cancer depends on patient's cancer location and stage. As well as health and personal preference -SURGERY 1-To remove the tumor 2-To remove cancer that has spread to the neck 3-To reconstruct the mouth -Radiation therapy :- using high energy beams, such as X-rays and protons, to kill cancer cells. -Chemotherapy Chemotherapy is a treatment that uses chemicals to kill cancer cells. Chemotherapy drugs can be given alone, in other combinaton with other chemotherapy drugs or in combination with other cancer treatments. -Targeted drug therapy Targeted drugs treat mouth cancer by alerting specific aspects of cancer cells that fuel their growth. (at Kharkov, Ukraine) https://www.instagram.com/p/B-byeJogMtT/?igshid=1dxrgpf453if8
0 notes
Photo

Hepatocellular carcinoma is the most common type of primary liver cancer. Hepatocellular carcinoma occurs most often in people with chronic liver diseases, such as cirrhosis caused by hepatitis B or hepatitis C RISK FACTORS:- The risk of hepatocellular carcinoma, the most common type of liver cancer, is the higher in people with long-term liver diseases. It's also higher if the liver is scarred by infection with hepatitis B or hepatitis C . Hepatocellular carcinoma is more common in people who drink large amount of alcoholand who have an accumulation of fat in the liver. DIAGNOSIS:- Tests and procedures used to diagnose hepatocellular carcinoma include: Blood tests - to measure liver functions Imaging tests- such as CT and MRI Liver biopsy- in some cases to remove a sample of liver tissue for laboratory testing. TREATMENT:- 1)Surgery- to remove the cancer and a margin of healthy tissue that surrounds it may be an option for people with early stage liver cancers. 2)Liver transplant surgery-Surgery to remove the entire liver and replace it with a liver from donor. 3)Destroying cancer cells with heat or cold- Ablation procedures to kill the cancer cells in the liver using extreme heat or cold may be recommended for people who can't undergo surgery. 4)Deliveringchemotherapy or radiation directly to cancer cells- Using a catheter that's passed through the blood vessels and into the liver to deliver the chemotherapy drugs (chemoembolization) or glass spheres containing radiation (radioembolization) 5)Radiation therapy 6)Targeted drug therapy 7)Immunotherapy (at Kharkov, Ukraine) https://www.instagram.com/p/B-ZP6yhA2vx/?igshid=gfj499r5jooj
0 notes