Text
Tomorrow is Eid.
and suddenly i don't feel the joys of eid... it dissipated and got replaced with dread..sadness..loneliness..
human emotions are incredibly fickle. they change and transform from one moment to next, unexpectedly
Alhumdulillah.
I am trying hard not to cry...its only 5pm lets see how i fare..
#i think the optimism i felt towards my step2 ck prep is non existent today and it got replaced with doubt#usmle step2#its combination of emotions..
0 notes
Text
I watched Haikyuu while studying for boards in the final weeks and watching Ep24 of both Season 1 and Season 2 is my story in parallel.
where season 1 Aoba Johsai was my wall, my nemesis - step 1- the thing that defeats me and crushes my soul…but also ignites a fire to start from scratch and build myself ground up.
Hinata was my undying spirit. Every time he jumped and got better, that was me making small steps and achieving something new every week.
Karasuno in season 2 defeating Aoba Joshai is me right now. Honestly season2 climax was probably more exciting and nerve wracking then my actual 8hr board exam. But its the same level of excitement, slowly sinking in. I feel light, free and content.
Alhumdlillah!
7.20.22
3 notes
·
View notes
Text
A couple job interview hacks from someone who has to give a job interview every single goddamn day: (disclaimer: this goes for my process and my company’s process, other companies and industries might be different)
1. There are a few things I check and a few questions I ask literally just to figure out if you can play the game and get along with others in a professional setting. Part of the job I interview for is talking to people, and we work in teams. So if you can’t “play the game” a tiny bit, it’s not going to work. Playing the game includes:
- Why do you want to work here? (just prove that you googled the company, tell me like 1 thing about us, I just want to know that you did SOME kind of preparation for this interview)
- Are you wearing professional clothing? I don’t need a suit just don’t show up in a ratty t-shirt and sweatpants.
- Are you able to speak respectfully and without dropping f-bombs all the time? Not because I’m offended but because I don’t want to be reported to HR if you wind up on my team.
- Can you follow simple directions in an interview?
2. Stop telling me protected information. I don’t want to know about what drugs or medications you’re on, I don’t want to know about you being sick, I don’t want to know if you’re planning to have children soon, I don’t want to know anything about your personal life other than “can you do the job?”
3. When we ask, “What questions do you have for me?” here are my favorites I’ve heard:
- What does the day-to-day look like for a member of your team?
- If one of your team members was not performing up to his usual standard, what steps would you take to correct that?
- What can I start doing now to accelerate my learning process in this job?
- What are some reservations you have about me as a candidate? (be ready for this emotionally….it will REALLY help you in the future, and I’ve had people save themselves from a No after this, but can be hard to hear)
- In your opinion, what skills and qualities does the ideal candidate for this job possess?
- What advice would you give to a new hire in this position/someone who wanted to break into this industry, as someone who has worked here for a while?
Those are just my tips off-the-cuff. I work in sales in marketing/SAAS, so these can be very different depending on the industry, but I wish the people I interview could read this before they show up.
36K notes
·
View notes
Text
A shorter, festive edition of my ambient sounds & music to study to masterpost for everyone whose vigorous academic program won’t let them take the holidays off entirely - i see ya, i feel ya, here’s some christmassy tunes to help make holiday studying more bearable 🎶
(x) - indicates how long the track is (i.e. (2) = 2 hrs)
*** - current fave

Narnia Winter Woods Music + Ambience (5)
Harry Potter Winter/Christmas Music (1)
Winter at Hogwarts (2)
Hogwarts Christmas Music w/ Snow sounds (1)

Good Mood Christmas Jazz (4)
Christmas Classics (Piano Jazz) (10)
Coffee Shop Christmas Playlist (3)*** - exactly what you’d listen to if you took your laptop to a café this time of year, so this one’s perfect for everyone who misses coffee shop study sessions :)
Tchaikovsky’s The Nutcracker (1.5) - bc the christmas vibes are simply magical in this one
The Royal Philharmonic Orchestra Plays ABBA (<1) - not festive per se, but it SLAPS. so. hard.
24/7 Lofi Christmas Radio
24/7 Christmas Songs Radio

45/15 Pomodoro Study With Me at a Café w/ Christmas Music (4)***
Mellow Christmas Music + Fireplace Sounds Study w/ Me (1)
Lofi Christmas Music Study With Me (1)

my other masterposts: dealing with failure⎪chrome extensions for students⎪aliexpress stationery for students (coming soon!)
389 notes
·
View notes
Text
Okay I’m currently furious that migraines are often so blindly easy to treat and I had to find this out myself at the age of 26 when I’ve been to a neurologist since I was 11 lol so I’m about to teach you two neat and fast little tricks to deal with pain!
The first is the sternocleidomastoid muscle, or the SCM muscle.
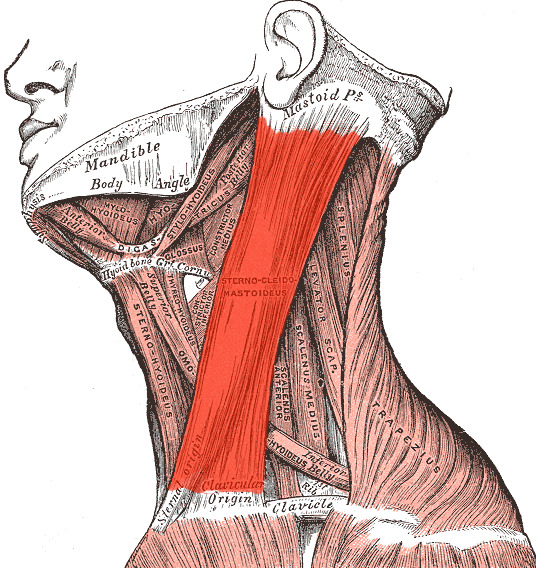
This big red section is responsible for pain around the eye, cheekbone, and jaw, as well as some temple pain. Literally all you have to do is angle your head down a little, angle it away from the side that hurts, and then you can gently pinch and rub that muscle. I find it best to start at the bottom and travel upwards. The relief is so immediate! You can increase pressure as you feel comfortable doing so.
Here is a short and easy video showing this in action
The second is a fast and easy stretch that soothes your vagus nerve, which is the nerve responsible for calming you down. The vagus nerve, for those unfamiliar, is stimulated by deep breathing such as yawning, sighing, singing, or taking a deep breath to calm your anger in a tense situation.
You can stretch this out by sitting up as straight as possible (this does not have to be perfect to work) and interlacing your fingers. Put your hands on the back of your head with your thumbs going down the sides of your neck and, while keeping your face forward, look all the way to one side with just your eyes. Hold that until you feel the urge to breathe deeply or yawn, or until you can tell there’s a change. Then do the same thing on the other side. When you put your arms down, you should clearly be able to turn your head farther in both directions. If the first session doesn’t get rid of your migraine, rest and repeat as many times as necessary. I even get a little fancy with it and roll my eyes up and down along the outer edge sometimes to stretch as much as I can.
If you need a visual here’s a good video on it. I know some of the language they use seems questionable but this is real and simple science and should not be discarded because it’s been adopted by the trendy wellness crowd!
I seriously cannot believe I didn’t hear a word of this from any doctor in my life. Additionally, if you get frequent recurring migraines, you may want to see a dietician. Migraines can be caused by foods containing histamines, lectin, etc. and can also be caused by high blood pressure in specific situations such as exercise, stress, and even sex.
If any of this information helps you I’d love to hear it btw! It’s so so fast and easy to do. Good luck!
119K notes
·
View notes
Text
Action is there to curate motivation.
That's right.
Motivation isn't something that just comes to you.
You get motivated by doing.
This is why the idea of needing motivation to succeed is wrong.
You succeed by taking action.
Which leads to having motivation.
Which leads to more action.
Which leads to more success.
That's the true formula.
So whenever you think "I wish I was more motivated"
Get up right away and perform any positive action.
You will miraculously find motivation appear right after.
6 notes
·
View notes
Text
This time last year I had one goal. To pass step1. I had the focus, zeal, and a-never- ending-pit-of-pettiness-and-fire to fuel my goal. To prove every mother fucker wrong, including myself.
I was my own competition. I didnt know how, but I knew i was gonna make it.
Now im sitting here making this dumb post trying to remember how I got here and how the fuck do I recreate that magic.
0 notes
Text
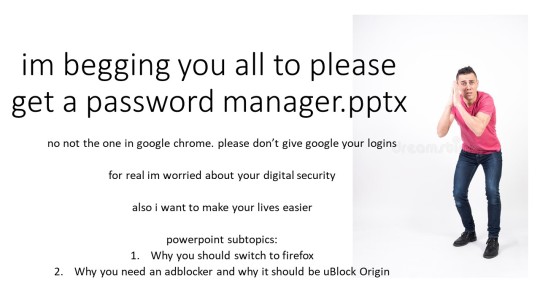


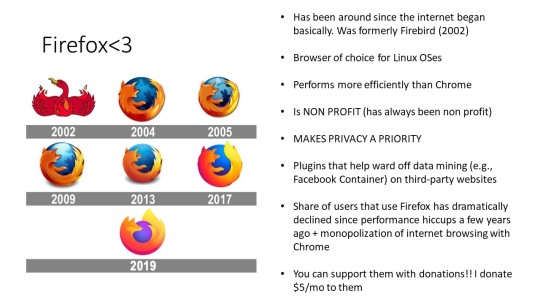

slides im sharing w my family this week bc it pains me to see how they manage their passwords. and also easy steps they can take to protect their privacy (firefox mainly). if u have any questions let me know.
also. uBlock origin is better than adblock plus bc: it allows NO ADS (ABP will allow certain ads and let bigger companies thru - its "acceptable ads" program) + is more lightweight and easier on your computer's resources than ABP.
51K notes
·
View notes
Text
Advice to Med Students/Interns: How to Talk During a Pelvic Exam*
Say: This may be uncomfortable but it shouldn’t hurt. Please tell me if it hurts and I will stop.
Don’t say: this won’t hurt
Say: This is my hand touching your leg
Don’t say: these are my fingers down here
Say: now I’m going to insert the speculum
Don’t say: I’m putting it in/ sticking it in now
Say: you will hear a click as I open the speculum
Don’t say: that noise is me opening you up
Say: you may feel some cramping as I collect some cells from your cervix with this brush
Don’t say: now I’m gonna take a scraping of your cervix
Say: how are you doing? Are you okay?
Don’t say: everything feel good?
Say: Everything looks normal
Don’t say: everything looks great down here
Say: Now I’m going to remove the speculum
Don’t say: I’m backing out/pulling out now
*yes, the don’ts are things I’ve heard in exam rooms
Tl;dr: if you can make a “that’s what she/he said” joke out of it, don’t say it during a pelvic exam. Keep it totes profesh.
1K notes
·
View notes
Photo

From the LearnTheHeart.com Cardiology Blog
So you are on the wards rounding and happen to have one of those cardiology attendings that gets some evil pleasure out of asking questions randomly to students (commonly known as “pimping”). I have seen some attendings get upset if students don’t know the correct answer and basically will send them to the library, tell them to look it up, then come back when they are smarter!
As a medical student, you MUST get these questions right if you are looking to get into a competitive residency/fellowship or just want to avoid embarrassment in front of your peers. Here is a list of the top 50 pimp questions that you may get on a cardiology rotation…know them and impress everyone! Want to really knock everyone’s socks off? I included some “Bonus” tidbits that are interesting and most people don’t know and links for those gunners who want to read more.
I have organized all of this into general cardiology pimps, physical exam pimps and ECG pimps. This is a lot to know, but should prepare you well!
General Cardiology Pimps
1. What are the toxicities of amiodarone?
I dare you to look your attending in the eye with a serious face and say “BITCH” if asked this question! It is probably not wise to do this unless you are sure they have a good sense of humor. Remember the mnemonic BITCH to recall the issues with amiodarone
Bradycardia/Blue man syndrome
Interstitial lung disease
Thyroid (hyperthyroid OR hypothyroid)
Corneal/Cutaneous
Hepatic/Hypotension
Another way to remember is “Check PFTs, TFTs and LFTs” for pulmonary, thyroid and liver function tests. But really the only monitoring that is done is a TSH level every 6 months as routine PFTs and LFTs are not recommended.
2. What are the causes of atrial fibrillation?
Remember PIRATES for the causes of atrial fibrillation. This is quite a comprehensive list:
Pulmonary embolism, Pulmonary disease, Post-operative
Ischemic heart disease, Idiopathic (“lone atrial fibrillation”), IV central line (irritating the right atrium)
Rheumatic valvular disease (mitral stenosis or regurgitation)
Anemia, alcohol (“holiday heart”), Age, Autonomic tone (vagal atrial fibrillation)
Thyroid disease (hyperthyroidism)
Elevated blood pressure (hypertension), Electrocution
Sleep apnea, Sepsis, Surgery
3. What are the different types of shock and their treatment?
This picture summarizes it all:
4. What are the causes of congestive heart failure (CHF) exacerbations?
You will very likely get this one. Congestive heart failure (CHF) is the #1 cause of hospital admission in the US. Whenever a patient comes in with volume overload from CHF, you must always as the question “Why did this patient’s heart failure get worse”. Here are the reasons from most common to least:
1. Medication non-compliance (not taking diuretics or other medications)
2. Fluid/sodium restriction non-compliance
3. Acute worsening of cardiac output:
Arrhythmia
Ischemia or acute coronary syndrome
Worsening/Progression of cardiomyopathy/valve disease
5. Which medications for systolic congestive heart failure reduce mortality?
Easy…beta-blockers, ACE inhibitors or ARBs, and spironolactone. If ACE inhibitor and ARB intolerant, then the combination of hydralazine and nitrates are used and reduce mortality, especially in African Americans. Note that digoxin and diuretics DO NOT reduce mortality! They are for symptom relief and to prevent heart failure hospitalization only. The gunners can review Heart Failure here.
6. Which beta-blockers are FDA approved to treat systolic congestive heart failure?
Not all beta-blockers have clinical trials to support their use in systolic heart failure. Use these three:
Carvedilol (Coreg)
Bisoprolol
Metoprolol succinate (Toprol) and NOT metoprolol tartrate (Lopressor)
Atenolol, propranolol and the other beta-blockers SHOULD NOT be used in systolic heart failure.
7. What is the most common cause of right heart failure?
Left heart failure! When anything causes left heart failure (ischemia, valve disease, cardiomyopathy etc…), the LV pressure increases and transmits back to the lungs causing pulmonary hypertension. This then strains the right heart and eventually causes right heart failure. Know the difference between signs/symptoms of left versus right heart failure.
8. A patient comes in with chest pain, what are the 4 life-threatening causes that should be exclude?
Acute coronary syndrome
Pulmonary embolism
Aortic dissection
Esophageal rupture (Boerhaave’s syndrome)
9. What are the signs/symptoms and issues with digoxin toxicity?
This is a good one:
Nausea/Vomiting/Abdominal pain
Weakness/dizziness
Symptoms of arrhythmia
Altered mental status
Vision changes (yellow vision or “Xanthopsia”)
Digoxin causes EVERY arrhythmia EXCEPT rapidly conducted atrial rhythms (atrial fibrillation or flutter with a rapid ventricular rate). The classic ECG has the “reverse check” sign:
The two pathognomonic rhythms in digoxin toxicity are atrial tachycardia with 2:1 block and bidirectional ventricular tachycardia.
Atrial Tachycardia with 2:1 AV Block ECG Example 1
Atrial Tachycardia with 2:1 AV Block ECG Example 2
Bidirectional Ventricular Tachycardia ECG Example
Reverse with digibind if:
Evidence of end-organ damage (altered mental status, shock liver etc…)
Life threatening arrhythmia
Potassium level > 5.5
Digoxin CAUSES hyperkalemia, but is potentiated by hypokalemia (also hypocalcemia)
Wow…thats a lot to know.
BONUS: The “Stone Heart” theory. Digoxin toxicity can cause hyperkalemia. Recall that the treatment for hyperkalemia causing ECG changes is usually intravenous calcium administration. In the setting of digoxin toxicity and hyperkalemia, giving IV calcium may be potentially fatal. The massive influx of calcium into myocytes after the IV calcium is given has been theorized to induce a non-contractile state and has been termed “Stone Heart” (recall the end-point effect of digoxin’s actions is to open calcium channels increasing influx into cells).
BONUS BONUS: Vincent Van Gogh (the artist) was toxic on digoxin (he used the flower foxglove for a seizure disorder) and this is why he painted everything yellow before he reportedly commited suicide. Check out this painting of his:
10. What are the FIVE life-threatening complications of aortic dissection?
Coronary dissection, usually the right coronary artery (RCA) causing inferior ST elevation MI
Carotid dissection causing stroke
Aortic rupture
Cardiac tamponade from rupture into pericardium
Acute aortic valve regurgitation causing cardiogenic shock
11. Which atrial fibrillation patients can we use only aspirin (ASA) for and who needs full anticoagulation to prevent stroke?
Use the CHA2DS2 Vasc Score:
If 0-1 points then aspirin 81 mg - 325 mg
If > 2 points then full anticoagulation (warfarin, dabigatran, rivaroxiban, apixiban)
Congestive heart failure
Hypertension
Age ( > 65 = 1 point, > 75 = 2 points)
Diabetes
Stroke/TIA (2 points)
Vascular disease (peripheral arterial disease, previous MI, aneurysm aortic atheroma)
NOTE: Female gender is also included in this scoring system = 1 point!
12. What are the different properties of beta-blockers and name specific drugs?
Cardioselectivity: All beta-blockers act upon both beta-1 and beta-2 receptors. The “Cardioselective” beta-blockers act upon beta-1 receptors much more than the beta-2 receptors. For this reason, the cardioselective beta-blockers are safer to use in patients with asthma or reactive airway diseases.
Lipid solubility: Beta-blockers that are lipid soluble, such as propranolol or metoprolol, can cross the blood-brain barrier easily. These medications are commonly used for migraine headaches, stage fright and panic attacks for these reasons.
Intrinsic sympathomimetic activity (ISA): Beta-blockers with ISA only partially antagonize while actually causing a small degree of activation of the beta receptors. So they will have some beta-blocking effects, but not to the degree of beta-blockers without ISA. These are commonly used in younger patients or in athletes where heart rates need to elevate (allowing overall increased cardiopulmonary effort) in order to compete in sports. Examples include pindolol and acebutolol.
Membrane stabilization: Stabilizing membranes decreases the propagation of action potentials. This is also the mechanism that local anesthetics work (lidocaine). Class I antiarrhythmic drugs possess this characteristic as well. The importance of this is not clear in clinical medicine in regards to beta-blockers. Perhaps this is partially an explanation for propranolol treating migraine headaches.
13. What are the side effects and other issues with ACE inhibitors?
Just remember the mneumonic “CAPTOPRIL”
Cough
Angioedema
Potassium excess
Taste changes
Orthostatic hypotension
Pregnancy contraindication/Pressure drop (hypotension)
Renal failure/Rash
Indomethacin inhibition
Leukopenia (rare)
14. What class of antiarrhythmic drug is ______ in?
Remember what drug is in what class was hard for me, even in fellowship! Now that I use them all the time I can remember them. Just keep going over them and eventually they will stick. A more detailed review of antiarrhythmic drugs is here.
Class IA: “Queen Amy Proclaims Diso’s Pyramid” = Quinidine, Amiodarone, Procainamide, Disopyrimide
Class IB: Lidocaine, mexiletine
Class IC: Flecainde, propafenone
Class II: Beta-blockers
Class III: Sotalol, amiodarone (yes…again), dronedarone, dofeilide
Class IV: Calcium channel blockers (diltiazem, verapamil)
Class V: Mechanism unknown
15. How do you diagnose and treat cardiac tamponade?
Beck’s triad: Hypotension, muffled heart sounds, elevated neck veins
Pulsus paradoxus: Abnormal if > 12 mmHg. Review how to measure here.
Water Bottle Heart: Chest x-ray finding - heart shaped like a canteen
Cardiac tamponade is a CLINICAL diagnosis, not an echocardiographic one, but an echo will show a pericardial effusion and if the right ventricle is collapsing in diastole, then tamponade is thought to be present (right ventricle is lowest pressure chamber, so collapses first. Pressure is lower in diastole than systole).
Treat with IV fluids to increase preload and prevent right ventricular collapse. Pericardiocentesis is therapeutic.
BONUS: DO NOT rely on analysis of pericardial fluid like we to pleural fluid after thoracentesis of ascites after paracentesis as the whole “transudate or exudate” thing is not validated here.
16. What is the classic triad of symptoms in aortic stenosis?
Angina, Syncope and Dyspnea (from heart failure) is the classic triad.
BONUS: Back in the day aortic valve replacement was not available, so they watched people with severe aortic stenosis to see how long they live. A classic pimp question is mortality based on that triad of symptoms if the aortic valve is not replaced. Average life expectancy is:
Dyspnea = 2 years
Syncope = 3 years
Angina = 5 years
This pic shows it all:
17. What is the most common cause of mitral valve stenosis?
By far the most common cause is rheumatic heart valve disease. Gunners read on mitral stenosis here.
BONUS: Mitral stenosis is in the differential diagnosis of hemoptysis which can occur due to rupture of a bronchial vein (they call this “pulmonary apoplexy”).
18. What are the indications for aortic valve replacement (AVR) in aortic stenosis and aortic regurgitation?
For either aortic regurgitation or stenosis, aortic valve replacement is indicated when symptoms occur or if the left ventricular systolic function declines, but there is one more tricky one for aortic regurgitation. AVR is indicated even if the left ventricular ejection fraction is normal when the end systolic dimension increases to > 55 mm or end diastolic dimension to > 75 mm on echocardiography.
19. What are the causes of mitral valve regurgitation?
Mitral regurgitation is either organic (actual valve apparatus problem) or functional (dilation of the annulus).
20. What is the treatment for coronary vasospasm?
DO NOT give beta-blockers!!! So they say this causes “unopposed” agonism at alpha receptors since the circulating catecholamines can’t act on the beta-receptors if a beta-blocker is given. The catecholamines decide to go to the alpha receptors and stimulate them which can worsen vasospasm. Use a non-dihydropyridine calcium channel blocker (i.e. amlodipine). Maybe the two beta-blockers that also block alpha receptors are OK (carvedilol and labetalol), but who knows…there is no data on this.
BONUS: Coronary vasospasm can occur with cocaine intoxication, so the same above principle applies (don’t use beta-blockers).
21. Which statin lowers the LDL the most? Which has fewest side-effects?
Rosuvastatin lowers LDL the most. Pravastatin fewest side-effects and safest in liver disease. Probably not much more to know but for the gunners here is a HMG CoA Reductase inhibitor review.
22. What are the mechanical complications of myocardial infarction?
Acute ventricular septal defect (VSD)
Acute mitral regurgitation (MR)
Left ventricular free wall rupture
For the gunners read about more complications of MI in the STEMI review.
23. What is the most common cause of aortic valve stenosis in a patient over the age of 70? Under the age of 70?
Over the age of 70 = senile calcific aortic stenosis
Under the age of 70 = bicuspid aortic valve
24. In a patient with unstable angina or a non-ST elevation MI (NSTEMI), when should an early invasive strategy be used?
Invasive coronary angiography (an “early invasive” approach) in unstable angina or non-ST elevation MI is indicated when:
1. Increased cardiac biomarkers (troponin, CK-MB)
2. New ST segment depression
3. Signs or symptoms of congestive heart failure (rales on examination, hypoxia with pulmonary edema on chest x-ray)
4. Hemodynamic instability
5. Sustained ventricular tachycardia or ventricular fibrillation
6. Recent coronary intervention within 6 months
7. Prior coronary artery bypass grafting
8. High TIMI risk score
9. Reduced left ventricular systolic function (EF < 40%)
10. Recurrent angina at rest or with low level activity
11. High risk findings from non-invasive testing
25. What are the absolute and relative contraindications to thrombolytics?
Absolute contraindications to thrombolytic therapy include:
1. Prior intracranial hemorrhage
2. Ischemic stroke within 3 months
3. Known cerebrovascular abnormality such as aneurysm or arteriovenous malformation
4. Known malignant intracranial tumor
5. Significant closed head trauma or facial trauma within 3 months
Relative contraindications to thrombolytic therapy include:
1. Uncontrolled hypertension (blood pressure > 180/110) either currently or in the past
2. Intracranial abnormality not listed as absolute contraindication (i.e. benign intracranial tumor).
3. Ischemic stroke > 3 months prior
4. Bleeding within 2-4 weeks (excluded menses)
5. Traumatic or prolonged cardiopulmonary resuscitation (CPR)
6. Major surgery within 3 weeks
7. Pregnancy
8. Current use of anticoagulants
9. Non-compressible vascular puncture
10. Dementia
26. What are the indications for valve replacement in patients with endocarditis?
Congestive heart failure from valvular regurgitation
Failure of antibiotic therapy to successfully suppress the infection or infection with difficult to treat organisms (fungal, Pseudomonas, Brucella, drug-resistant organisms)
Valvular annular abscess
Peripheral embolism of vegetation
Size of vegetation > 1.0 cm
27. What are the common causes of endocarditis?
Streptococcal viridins, Staph aureus, and Enterococcus are the leading three.
BONUS: If Streptococcus bovis endocarditis is associated with colon cancer.
BONUS BONUS: Know the culture negative causes of endocarditis (vegetation on the valve but no organism growing in blood cultures). These are known as the “HACEK” organisms:
Haemophilus aphrophilus
Actinobacillus actinomycetemcomitans
Cardiobacterium hominis
Eikenella corrodens
Kingella kingae
28. What are the secondary causes of hypertension?
Remember “ABCDEF”
Apnea (obstructive sleep apnea), Acromegaly, Accuracy (incorrect measurement)
Birth control, Bad kidney
Coarctation of the aorta, Cushing’s syndrome, Conn’s syndrome, Catecholamines
Drugs (alcohol, nasal decongestants, estrogens)
Endocrine disorders, Erythropoietin
Fibromuscular dysplasia
BONUS: The most common cause of difficult to control hypertension is uncontrolled obstructive sleep apena followed by renal artery stenosis.
29. Which cardiac biomarker elevates first? Which stays elevated the longest?
Myoglobin elevates first (30 minutes), then troponin and creatine kinase (CK). Troponin stays high for 7-10 days, but CK for only 3-4 days.
30. What are the three types of cardiomyopathy?
Dilated cardiomyopathy: This results in left ventricular systolic dysfunction and clinical manifestations of congestive heart failure. Etiologies include viral, alcoholic, idiopathic, familial and other rare causes.
Hypertrophic cardiomyopathy: Also known as hypertrophic obstructive cardiomyopathy (HOCM), this results in abnormal hypertrophic changes most commonly in the interventricular septum with pathologic “myocardial disarray”. HOCM is familial in about 50% of cases and transmitted in an autosomal dominant fashion. HOCM can result in clinic heart failure, life-threatening arrhythmias, mitral regurgitation and sudden cardiac death.
Restrictive cardiomyopathy: This results in heart failure related to severe diastolic dysfunction. Causes include amyloid heart disease, infiltrative disorders, and familial.
Physical Examination Pimps
31. Take a listen to his heart, do you hear the S4 heart sound?
NO YOU DON’T!!! The patient is in atrial fibrillation and CAN’T have an S4 heart sound! Recall that an S4 happens when the atrium contracts into a non-compliant left ventricle causing the blood to forcefully strike the left ventricle creating the sound. Patients with atrial fibrillation DO NOT have any atrial contraction and are not able to have an S4 heart sound. Don’t let your attending trick you…
32. What causes an S3 heart sound versus an S4 heart sound?
An S3 heart sound, a.k.a. the ventricular gallop can be present in systolic heart failure, but can also be there in normal healthy hearts. The S4 heart sound is almost always pathologic and can occur in the setting of diastolic heart failure and/or myocardial ischemia.
33. How severe is the aortic stenosis on exam?
There are only 3 ways to tell how severe the aortic stenosis is on physical exam:
1. Timing of the murmur peak (late in systole = severe)
2. The intensity of the S2 heart sound (soft or absent = severe)
3. Pulsus Parvus et Tardus (carotid upstroke weak and late)
34. What are the three causes of a holosystolic murmur?
Mitral regurgitation, tricuspid regurgitation, ventricular septal defect.
BONUS: The “Galliveridin” phenomenon in aortic stenosis is when the murmur radiates to the apex and can sound holosystolic mimicking mitral regurgitation. Handgrip maneuvers or transient arterial occlusion will increase mitral regurgitation and not the aortic stenosis murmur. Gunners read an aortic stenosis review here.
35. Describe the murmur of aortic regurgitation.
Early diastolic decrescendo. If an actual valve problem caused the aortic regurgitation (i.e. endocarditis), then the murmur is at the left lower sternal border BUT if it is from dilation of the aorta (i.e. ascending aortic aneurysm as occurs in Marfan’s), then the murmur is at the aortic listening post which is the right upper sternal border. Tricky.
BONUS: The murmur is best heard with the patient leaning forward at end-expiration.
BONUS BONUS: When the aortic regurgitation is severe the murmur is quite short in early diastole since sooooo much blood leaks back into the left ventricle that the pressure between the aorta and the LV equalize quickly. Conversely, if mild it takes quite some time for the pressure to equalize so the murmur is longer (see pic)
36. What is the Austin-Flint murmur?
This is when the aortic regurgitation get strikes the anterior leaflet of the mitral valve in diastole forcing it partially closed. This kind of creates a mitral stenosis-like picture and a “diastolic rumble” at the cardiac apex called the Austin-Flint murmur.
37. What are some of the peripheral signs of aortic regurgitation?
Reel off all of these and people will be staring with their mouths wide open:
Corrigan’s pulse: A rapid and forceful distension of the arterial pulse with a quick collapse.
De Musset’s sign: Bobbing of the head with each heartbeat (like a bird walking).
Muller’s sign: Visible pulsations of the uvula.
Quincke’s sign: Capillary pulsations seen on light compression of the nail bed.
Traube’s sign: Systolic and diastolic sounds heard over the femoral artery (“pistol shots”).
Duroziez’s sign: Gradual pressure over the femoral artery leads to a systolic and diastolic bruit.
Hill’s sign: Popliteal systolic blood pressure exceeding brachial systolic blood pressure by 60 mmHg or greater (most sensitive sign for aortic regurgitation).
Shelly’s sign: Pulsation of the cervix.
Rosenbach’s sign: Hepatic pulsations.
Becker’s sign: Visible pulsation of the retinal arterioles.
Gerhardt’s sign (aka Sailer’s sign): Pulsation of the spleen in the presence of splenomegaly.
Mayne’s sign: A decrease in diastolic blood pressure of 15 mmHg when the arm is held above the head (very non-specific).
Landolfi’s sign: Systolic contraction and diastolic dilation of the pupil.
38. What maneuver makes the murmur of hypertrophic obstructive cardiomyopathy (HOCM) louder?
Valsalva decreases left ventricular filling. In HOCM this allows the very thick interventricular septum to buldge more into the left ventricular cavity causing more of a left ventricular outflow tract obstruction, thus making the murmur louder. Much different than the murmur of aortic stenosis (see pic).
39. What murmur gets louder with inspiration?
Tricuspid regurgitation does. This is called “Carvallo’s sign”. Pulmonic regurgitation can sometimes as well.
BONUS: Severe tricuspid regurgitation causes large “V waves” in the jugular venous pulsations from blood leaking back from the right ventricle into the internal jugular during systole. Also look for a pulsatile liver.
ECG Pimps
First of all, you need to know the basics, like how to diagnose a left and right bundle branch block, chamber enlargements, axis, heart rate, myocardial infarctions etc… read the ECG Review here. Below are some of the specific ECG pimp questions that I have run into.
40. What is the most common ECG findings of pulmonary embolus?
Everyone wants to reflexively say “S1Q3T3” and if you do, then you are wrong. It is sinus tachycardia. The S1Q3T3 pattern is the classic finding (see pic below), but sinus tachycardia is more common.
BONUS: The S1Q3T3 pattern is not just for pulmonary embolism, but for anything that causes acute right heart strain (can occur in COPD or asthma exacerbations, respiratory failure etc…) and it is also called the McGinn-White sign.
41. Can you diagnose a myocardial infarction on ECG if there is a left bundle branch block (LBBB)?
Whoooo hoooo! You are ready for this one! You know that traditionally the answer is no, ischemia is not readily detected if a left bundle branch block (LBBB) is present, but there are some means to do this. The Sgarbossa criteria, Chapman’s sign, Caberera’s sign and also by examining the T waves in lead V5 and V6. Know these and you will look like a superstar!
Sgarbossa criteria: This is a point scoring system.
1. ST elevation > 1 mm and in the same direction (concordant) with the QRS complex. 5 points
2. ST depression > 1 mm in leads V1, V2, or V3. 3 points
3. ST elevation > 5 mm and in the opposite direction (discordant) with the QRS. 2 points
A score of 3 points is required to diagnose an acute myocardial infarction. Criteria #3 is under debate as to its usefulness, so basically you need to have either criteria 1 or criteria 2. Below is an image of ST elevation in V5 and V6 with a LBBB:
Chapman’s sign: A notch in the upslope of the R wave in lead I, aVL or V6. This has a low sensitivity, but a specificity of about 90%. See Chapman sign ECG here.
Cabrera’s sign: Notching at 40 milliseconds in the upslope of the S wave in lead V3 and V4. This has a poor sensitivity of 27% for myocardial infarction. See Cabrera’s sign ECG here.
T waves in V5 and V6: If upright in these leads when a left bundle branch block is present, then ischemia is more likely present, although sensitivity is low for this finding.
42. What are the causes of AV dissociation on ECG?
Ventricular tachycardia (VT) and complete heart block (3rd degree AV block)
Here is AV dissociation from VT:
Here is AV dissociation in complete heart block:
BONUS: When AV dissociation is present, this causes the atria to contract at the same time as the ventricle when the P wave falls on top of the QRS complex. Thus, the atrium is contracting against a closed mitral/tricuspid valve. This makes blood forcefully go backwards causing intermittent “cannon A waves” in the jugular venous waveform.
BONUS BONUS: That huge stretch of the atrium during AV dissociation due to the above mentioned atrial contraction against closed valves causes release of ANP (atrial natriuretic peptide) which causes diuresis and thus polyuria! Yes…polyuria can be a symptom of complete heart block! BAAAMMM!!! Not too many people know this and it will certainly impress.
43. What are the ECG changes of hyperkalemia and what can you give to resolve them?
Peaked T waves is the answer most people are looking for. The QRS complex can widen in a non-specific pattern (not left or right bundle) a.k.a. a “non-specific intraventricular conduction delay”. Eventually
44. The patient has 2:1 AV block - How can you tell if it is 2nd degree type I or 2nd degree type II AV block?
First quick rule: If the PR interval of the conducted beat is prolonged AND the QRS complex is narrow, then it is most likely second degree type I AV nodal block (Wenckebach). Alternatively, if the PR interval is normal and the QRS duration is prolonged, then it is most likely second degree type II AV block and a pacemaker is probably warranted.
Less quick rule: Exercise the patient. Walk them in the hall or on a treadmill. If it is 2nd degree type I, the heart rate will increase and you will see prolonging PR intervals until a beat is dropped. If it is 2nd degree type II, then nothing will happen. You can also give atropine or do a carotid massage and see what happens.
Here is a pic of 2:1 AV block:
45. What is a _____ wave on the ECG?
Detla wave = Wolff-Parkinson White (short PR interval that is slurred into the QRS complex)
Osborne wave (a.k.a. J wave) = Classically hypothermia, but also hypercalcemia
U wave = hypokalemia
Epsilon wave = Arrhythmogenic right ventricular dysplasia (ARVD) which is RARE
46. What are the causes of ST elevation on ECG besides acute MI?
ECG Causes of ST segment elevation: ELEVATION
Electrolyte abnormalities
Left bundle branch block
Aneurysm of left ventricle
Ventricular hypertrophy
Arrhythmia disease (Brugada syndrome, ventricular tachycardia)
Takotsubo/Treatment (iatrogenic pericarditis)
Injury (myocardial infarction or cardiac contusion)
Osborne waves (hypothermia or hypocalcemia)
Non-atherosclerotic (vasospasm or Prinzmetal’s angina)
47. What are the ECG findings of a posterior MI?
You better know anterior and inferior MI ECG changes. The posterior MI ECG findings are a bit more tricky:
ST segment depression (not elevation) in the septal and anterior precordial leads (V1 to V4). This occurs since these ECG leads will see the MI backwards (since the leads are placed anteriorly, but the myocardial injury is posterior).
The ratio of the R wave to the S wave in leads V1 or V2 is > 1.
ST elevation in the posterior leads of a posterior ECG (leads V7 to V9). Suspicion for a posterior MI must remain high, especially if inferior ST elevation is also present.
ST elevation in the inferior leads (II, III, and aVF) may be seen if an inferior MI is also present
48. What are the three irregularly irregular rhythms on ECG?
The three irregularly irregular rhythms are atrial fibrillation, atrial flutter with VARIABLE conduction and multifocal atrial tachycardia (MAT)
49. What are the causes of a prolonged QT interval?
Electrolyte abnormalities (hypokalemia, hypocalcemia, hypomagnesemia)
Medications (quinolones, macrolides, haloperidol, class IA and class III antiarrhymics)
Genetic long QT syndromes
Myocardial ischemia
BONUS: Patients with a prolonged QT interval are at risk for Torsades de Points or polymorphic ventricular tachycardia (see pic). Treat with IV magnesium.
50. How can you distinguish the ECG findings of pericarditis from myocardial infarction or early repolarization?
The ST elevation that occurs in pericarditis is “diffuse” meaning in every lead. Acute MI frequently has “reciprocal” ST depression and less commonly PR segment depression as is present in pericarditis.
BONUS: Another cause of PR depression is “atrial infarction”.
Any other pimp questions you have run into that you think we should know?
Leave a comment on the LearnTheHeart.com blog article “Top 50 Cardiology Pimp Questions”
4K notes
·
View notes
Note
I’m in my second week of intern year (IM) and I know it’s supposed to be tough, but I’m already so depressed and overwhelmed. I feel like I’m failing miserably, missing things, making stupid mistakes, and just sucking in general. I dread coming in every day because I don’t want to think about all the things I might do wrong. I can’t sleep because I lie awake wondering if I forgot to do something or if I made a poor decision that will negatively affect my patients. I am miserable.
(cont) Same intern who sent an ask about being depressed. I did most of my 4th year rotations at the hospital where my program is, so the residents got to know me and they pushed so hard for me to get ranked here because they liked me and thought I would be a great resident. So now I feel like I’m letting them down and it kills me because they all really rooted for me. I don’t wanna disappoint anyone. :(
=======================================================
Hey there, anon!
I feel you. The start of intern year is ROUGH. Intern year as a whole is challenging for all the ways you’ve mentioned: it’s physically, mentally, emotionally, and psychologically demanding.
First things first, know that everyone who has ever done intern year has felt exactly as you have felt. I have been there, oh man have I been there. The first week of intern year, there were so many days that I was close to tears. Guess what? Talk to your co-interns and talk to those residents who were excited to have you here: they have been where you are and they have felt what you have. So please please know: you are not alone in feeling what you are experiencing.
That said, a couple things that you’ve brought up that I want to address in an orderly fashion to help relieve some of your discomfort and potentially help expedite some of the growing pains you are currently experiencing with intern year:
1. Making mistakes: Let’s be clear: you’re going to make mistakes. The residents that you look up to have and are still making mistakes. The attendings, especially the best ones, got to where they are by making mistakes. I make mistakes basically daily, several times a day. Because we are human. Because we are learning. So why aren’t patients dying left and right? Why are you coming to work and your patients are still alive?
This is one of the keys to medical training that I think alleviates a lot of unnecessary self-imposed criticism and allows people such as you or me to finally enjoy the medicine: We’re making mistakes under a LOT of supervision. Therefore, it is very unlikely that those mistakes are every going to reach a patient or hurt someone.
When you make an error placing an order, writing the name of a medication, just straight up writing a medication incorrectly, or presenting the wrong plan, as an intern you do so under a lot of supervision and with a lot of systems in place to catch those errors. Why? Because humans are inherently going to make mistakes, so it’s best that we have systems in place to check for them. If you put an order in incorrectly or mispell/misorder a medication, the nurse pages you, the pharmacist pages you to correct it, right? Your senior may correct it too if they’re particularly EMR-agile.
When you miss something, know that good attendings and good residents are checking all your work, ESPECIALLY at the beginning of the year, to make sure none of those normal beginner’s errors reach the patients.
To reiterate (because you WILL need sleep during residency, it’s such a precious commodity and I don’t want you losing any more sleep):
A. Mistakes are human and normal
B. Numerous systems and people are in place to prevent errors from hurting patients in a disastrous way
C. With time and organization, you WILL make fewer mistakes and miss fewer things. But you need to be patient with yourself.
2. Letting people down. Especially in medicine, we derive a lot of teaching and education through external validation, so it is always worth stating: residents and attendings do not carry the same expectations for a med student that they do an intern; these expectations are not carried over when you stay at an institution you know. I can speak from firsthand experience; I also stayed, as you did, at the hospital where I did most of my 4th year rotations. And let’s be honest: I WAS ONLY MEDIOCRE AT BEST AS A MED STUDENT. I never stood out; and when I did, it was never for good reasons. I even had an attending tell me once that she wouldn’t write me a letter of rec because “you’re just not that impressive.” So you can imagine how scared I felt starting intern year. I was sure the residents were going to bemoan my presence on the floors.
So it was a relief to find that my prior rotations here didn’t color the residents’ or attendings’ opinions of me. When you step through the doors as an intern, you’re an intern. The assessment is only of the here and now, who you are now. And you have only been there two weeks as an intern. You cannot let anyone down; you’ve not spent enough time there as an intern to do that.
What are strategies to decrease missed things and errors?
1. Keep your written info organized: Ever seen scutsheets? I used the medfools scutsheets religiously to organize myself for my first month on wards until I developed my own way to organize info on paper. This is a visual/kinesthetic means to retain information and learn, decrease errors.
2. Never feel ashamed to ask that your senior run the list again with you, especially in intern year. This is an auditory and interpersonal strategy to retain information and decrease errors.
3. Organize your day: Ask residents you admire or are deemed highly organize how they structure their day. Try some of their styles and see what works best for you. As for the tasks you are assigned to do over the day, try to prioritize by the acronym COLD or D-COL (for me, the latter worked better but do what works for you). C=consults, O=orders, L=labs, D=discharges. Place your consults first, put your orders and labs into the EMR, prep or do your Discharges.
4. Not to tout my own horn, but if your program didn’t give you a survival guide type document, you can check out mine here.
You got this, let me know how week 3 goes!
md-a
42 notes
·
View notes
Text
Medblr Question: Patient Histories
I just started my first year of Medical School and we are learning how to take patient histories. I noticed that doctors tend to have certain lines or go-to phrases they say when they address different issues in the conversation, so I’m wondering if medblrs can reblog this and add some of the things they like to say when taking a history.
(Nurblr responses are welcome too, as are signal boosts, thanks! 😊)
1K notes
·
View notes
Text
Some of my patients are Native American. I am white.
I have an angry post sitting in my drafts about something another white person said to me about Native pharmacists. I don’t think releasing that anger into the world will be helpful. It’s not about me and my feelings and my voice. It’s about listening to what First Nations voices tell us about how to provide healthcare to them. I’m going to try to amplify some of the things I’ve learned in my career so far.
What I have learned from Native American patients and providers:
Don’t think of Native Americans as a single culture. They are multiple separate nations and my individual patient’s culture is a combination of their nation plus varying influence of mainstream North American culture.
Never underestimate the genocide.
Learn about Indian Boarding Schools. The trend to close them only came about in the 1980s and 90s; some are still open, hopefully under Native leadership, but I don’t know. I do know that people with my skin tone took some of my patients from their families and abused them when they were children.
The children did not know when the white people would be coming and were often not told about it by their families. The white people didn’t speak their language.
From the 1700s to the 1990s.
This makes some patients afraid to tell me that they don’t understand when I ask for consent, but agree quickly. I don’t touch a Native American patient until I’m very sure that they understand why and that they consent, even if they already agreed. I check in the middle of the procedure, too—and all I do are point of care tests, vaccines, and vital signs.
Elders are held in higher respect than in my culture. It can help to build trust if I enter a geriatric patient’s room with the attitude that they have more wisdom and status than I do.
Wearing something from a Native culture that you bought at Target or Urban Outfitters can tear down that trust. If you bought it from a Native craftsman, however, you’re good.
Know the taboos of your local tribes. I sometimes need to interview patients by asking them about why their children or aunts think they should come to the doctor, because talking about things makes them worse.
Ask them about their tribal affiliation. Ask them if they’ve taken traditional medicine for the condition. Ask them if they’ve used ceremonial medicine. Some of them are just glad that they are treated as if their culture isn’t dead.
Sometimes they are assumed to be Latin@s due to skin tones, which is annoying if they’re not. If they’re bilingual, it’s their native language, not Spanish and English.
Two-spirit traditionally was more about a third gender. Younger generations are using it for sexual orientation, and they don’t necessarily mean bisexual. Gay and lesbian people may claim it as well.
Navajo-specific: don’t talk about skin walkers. If they bring it up, follow their lead, but it’s never my place to start this conversation topic. This seems to be the only topic I’ve discovered that crosses generations and the urban/reservation divide.
Navajo-specific: asking women about their turquoise jewelry isn’t taboo, but could be awkward for all involved.
Sometimes urban Native patients have very little traditional culture influence and it’s not nice to assume that you know what their cultural identity is just because they wrote “Cherokee” on the form
The DSM-5’s Cultural Formulation Interview is a really great tool for just asking the patient how they want their culture addressed in healthcare situations and I really think it should be used more outside of psychiatry too.
My CV may be miles long but a Native American pharmacist will almost always be better for these patients than me, because you just can’t put down a lifetime of experience at being a Native American on a CV, but it matters way more to the patients than the number of lectures that I’ve delivered, and rightfully so.
This is their land, and they know I’m not personally responsible for their genocide, but my ancestors may have had a hand in the cause, and either way, I’m certainly profiting from it in ways that I can’t really see. They forgive me, I think most of them do, but they know my part in their loss, and I think it helps me provide better care if I know it too.
Become very comfortable with discussing supplements and alternative medicine because a larger percentage of them still don’t quite trust that the chemicals that I provide won’t make them sicker. The willingness to discuss alternate and traditional medicine with respect will build that bridge of trust. It might even lead them to trust the other drugs that I have.
Honestly I have a lot more understanding for a Native person wanting to talk about alternative medication than a hipster, is all I’m saying
Though I’ve treated Native hipsters too. Didn’t ask me for alternative drugs though so I didn’t have to resolve the paradox there.
Generational poverty and trauma may be a greater cultural influence than their nation, but you can’t separate the topics. Make sure that your patient has the ability to actually access the treatment you’re recommending. Carbs are cheap.
I’ll add more if I think of more things they’ve taught me. If you’re Native and I messed up on something here, I hope you feel comfortable correcting me. Thank you.
309 notes
·
View notes
Text
Mansplaining protip:
When a man starts explaining a concept you already told him you understand, instead of saying “I know” over and over until you die, try one of these:
Ok, which aspect is confusing you?
It seems like you have the basics down; Would you like me to recommend some good articles so you can get a more nuanced understanding?
So did you have a specific question, or do you just want a more in depth explanation?
321K notes
·
View notes
Text
When you guys have visited potential apartments, what kind of questions did you ask besides the basics like what rent and utilities include?
217K notes
·
View notes
Photo

It started as a small experiment and turned out to be one word - AWESOME.
What’s the study group for?
A bunch of medical students from all over the world, discussing study related concepts!
You may share your experiences, what you studied today, ask interesting questions to help other people learn or simply revise, ask doubts about things you don’t understand, answer other people or just tell a fact you learnt that fascinates you.
We learn something new on a daily basis <3
How do I sign up for the group?
All you’ve got to do is message me your number. You can email me at [email protected] with “Whatsapp study group” in the subject.
Important: Make sure you include your proper country code when you email me your number. (Otherwise your number won’t be displayed in my Whatsapp list and I might miss you out!)
After you have emailed me your number, you’ll receive a verification email from us. It’s just some basic questions that helps us decide which group should you be added in (And whether you are a regular human being or a internet creep! :P ).
Replying to this mail is essential otherwise you might not be added to the group.
I’m a pre-med/nursing/pharmacy/EMS/other medical fraternity student. Can I join too?
YES!
I want to join but.. I’m hesitant because I’ll be sharing my number to a lot of people.
It’s risky, I know, but we have solutions - Block users. So I don’t think you should hold back on your awesomeness. I have added over 90 people so far and they are loving it.. No complaints so far. Take a chance and hop in! <3
You can read our previous experiences and discussions here:
Medicowesome study group on Whatsapp
Study group experience #1
Study group experience #2
Study group experience #3
Study group experience #4
Study group experience #5
So.. See you in the group, awesomite!
-IkaN
331 notes
·
View notes